Paediatric dentistry I
Overview
The successful practice of paediatric dentistry requires an intimate knowledge of normal child development and behavior, as well as the technical and clinical skills that are necessary to work in a small mouth. The aim of every clinician who treats children should be to deliver that child into adolescence and young adulthood without fear and with tolerance for dental treatment. If that is achieved and, in addition, the young adult has an appreciation of the importance of oral health to overall general health, then the hours spent in behavior management and delivery of prevention will have been worthwhile.
7.1 Tooth development and eruption
Tooth development
Tooth germs develop from the dental lamina, which itself develops from the primary epithelial band. The dental lamina forms a series of epithelial buds that grow into surrounding connective tissue. The buds become associated with a condensation of mesenchyme and together they represent a tooth germ at its early ‘cap’ stage of development. The epithelial bud becomes the enamel organ and the mesenchymal cells the dental papilla and follicle. The cells at the margin of the enamel organ grow to enclose some mesenchymal cells, the ‘bell’ stage of development. Histodifferentiation of the enamel organ now forms the external and internal enamel epithelia, stratum intermedium and stellate reticulum.
On the lingual aspect of each primary tooth germ, the dental lamina proliferates to produce the permanent successor tooth germ. Permanent tooth germs with no primary precursors are produced by distal extension of the dental lamina.
Dentine formation occurs after differentiation of dental papilla cells into odontoblasts, which is induced by the internal enamel epithelium. Once dentine formation has begun, the adjacent cells of the internal enamel epithelium differentiate into ameloblasts and produce enamel. The dentine of the roots of teeth is produced in a similar fashion by differentiation of odontoblasts induced by the internal enamel epithelium, and root growth is controlled by the epithelial cells at the margins of the enamel organ – the root sheath of Hertwig. Root growth is not complete until 1–2 years in the primary dentition and 3–5 years in the permanent dentition after eruption of the crowns of the teeth. The beginning of mineralisation for both dentitions is given in Tables 7.1 and 7.2.
Table 7.1
Typical times for calcification and eruption of deciduous teeth
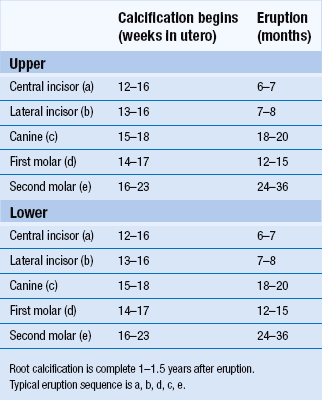
Table 7.2
Typical times for calcification and eruption of permanent teeth
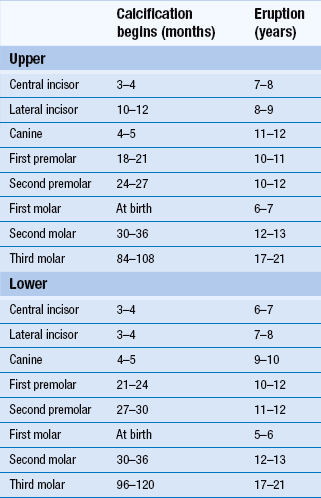
Root calcification is complete 2–3 years after eruption.
Typical eruption sequence: upper 6 1 2 4 5 3 7 8; lower 6 1 2 3 4 5 7 8.
Eruption
The exact controlling mechanism of eruption has not yet been identified. It is likely that the dental follicle has a major part to play as the connective tissue of the follicle is a rich source of factors responsible for the local mediation of bone deposition and resorption. Typical eruption times are given in Tables 7.1 and 7.2.
7.2 Management of the child patient
Psychological aspects
Development should be regarded as a continuum as it may differ from child to child. It is an uneven process and is influenced by periods of rapid bodily change. There are certain ‘psychological signposts’ that are important for the dentist and their staff to recognise.
Motor development: Motor development occurs in a predictable order and failure to attain ‘motor milestones’ enables remedial intervention that will aim to improve motor skills. The environment can influence motor development, and generalised motor development is completed in early life. Skills or changes that follow walking are refinements rather than new skills. Dominance of one hand emerges early. Motor retardation in a child may be manifested by no specific handed dominance. At 6–7 years of age, a child will have sufficient co-ordination to brush their teeth reasonably well. Below 6–7 years, many areas of the mouth will be inaccessible without parental help.
Sensorimotor at 0–2 years: The infant can think of things as permanent without having to see them directly.
Preoperational at 2–7 years: Thought patterns are not well developed; the child is egocentric and inflexible.
Perceptual development: By age 7 years, children do develop selective attention and can determine which advice merits attention and which can be ignored. Concentration skills also improve. By age 9 years, children achieve adult proficiency.
Language development: Language and thought are inter-related and lack of stimulation will retard both. Keep dental jargon to a minimum and always assess patients before offering advice.
Parental influence and dental treatment
Parents are vital for positive reinforcement over any treatment objective. Programmes of treatment must be designed to reduce any chances of making parents or their children feel guilty. Design of treatment programmes should also allow goals to be achieved one by one, never overloading parent or child.
Dentist–patient relationship
Each patient is a unique individual and should be treated as such. Overall, it is fair to conclude that while the technical skill of a dentist is of concern, the most important factors for a patient are gentle friendly manner, explanation of treatment procedures and the ability to keep pain to a minimum.
The structure of the dental consultation
2. Preliminary chat: non-dental topics first, then dental; listen to the answers!
3. Preliminary explanation: clinical and preventive objectives in language that can be understood.
4. Business: during treatment, constantly check the patient is not in pain and explain and discuss what you are doing; summarise what you have done to patient and parent and offer aftercare advice.
5. Health education: constantly reinforce advice about maintaining a healthy mouth and give advice as though you mean it; always set realistic objectives.
6. Dismissal: a clear signpost that the appointment is over, using the child’s name and a definite farewell.
Anxious and unco-operative children
The extent of anxiety does not relate to dental knowledge but is an amalgam of personal experiences, family concerns, disease levels and general personality traits. It is, therefore, not easy to pinpoint aetiological agents and measure anxiety. In addition, there is no standard measure of anxiety.
Helping anxious patients cope: Several approaches can help to reduce coping problems:
• Reducing uncertainty – tell, show, do.
• Previsit preparation, e.g. send letter home explaining details of proposed visit.
• Modelling: videos or a live model.
• Cognitive approaches – identification of beliefs: try to get individuals to identify and alter their dysfunctional beliefs, useful for all focused types of anxiety.
• Distraction attempts to shift attention from dental setting towards another kind of situation (e.g. videos, headphones with music or stories). A patient can also be distracted during difficult procedures such as local anaesthetic by firmly rubbing their cheek and talking loudly to them thus stimulating other senses.
• Relaxation: useful for high levels of tension; aims to bring about deep muscular relaxation – several simple techniques are available for use by dentists.
• Systematic desensitisation: working through various levels of feared situations from ‘mildest’ to ‘most anxiety’.
Care programme
History involves social, medical and dental information
Social: Name, address, age, school, siblings, parental occupations. This allows the clinician to establish rapport. Try and assess social background, knowledge of dentistry and the family’s expectations.
Medical: Apart from allowing safe delivery of dental care, two additional factors can be gleaned: children with medical conditions may have a negative attitude to treatment because of the time they have spent in hospitals; they may also be more likely to fail dental appointments owing to the disruption in education that the medical problem has already caused.
Examination
Clinical examination: The clinical examination need not involve sitting in the dental chair at the first visit. Examine the child as a person not just a mouth.
Extraoral: General appearance is noted; percentile charts are a useful way of monitoring height and weight. The head and neck are examined making a sketch of any lesions/marks.
Intraoral: Soft tissues may be an indicator of systemic disease. The relationship between periodontal condition and oral hygiene may indicate an underlying condition. Occlusion factors include crowding, malalignments, mandibular deviations and habits. The condition of the teeth is noted; they must be clean and dry in order to facilitate caries diagnosis.
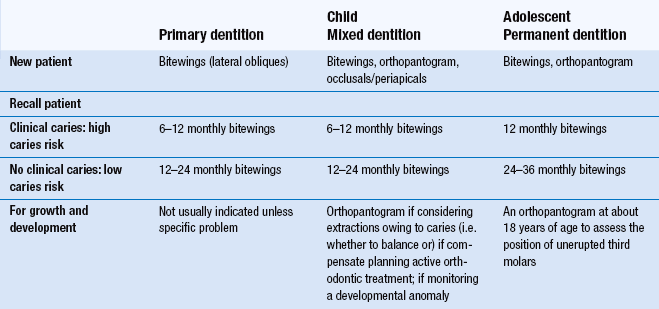
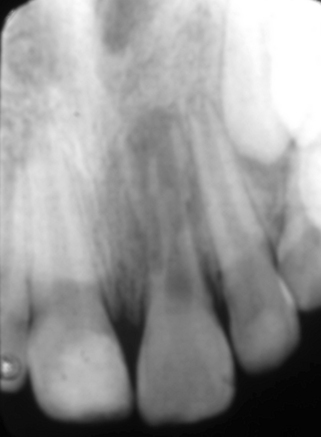
Radiographic examination: Guidelines for prescription of radiographs in children are shown in Table 7.3.
There are three general indications for taking radiographs in children:
Caries diagnosis: At least 50% more approximal lesions can be diagnosed by bitewing radiographs than with clinical examination. High-resolution digital orthopantogram (OPT) films at the appropriate setting (that which will separate the interproximal contacts) are efficient at diagnosing occlusal and approximal caries. Many standard OPT films are, however, still inadequate for caries diagnosis and, in this case, intraoral bitewing radiographs remain the method of choice.
Special investigations: There are a number of special tests that are sometimes relevant:
• Vitality testing: laser doppler flowtometry can be used to detect if a tooth has a patent blood supply.
• Sensitivity/sensibility testing: tests the nerve supply to a tooth. Hot and cold stimuli can be evoked using hot gutta-percha or ethyl chloride and electrical stimulation can be applied using an electric pulp tester. These tests are not suitable for the primary dentition, however, and are not completely reliable in the permanent dentition.
• Culture and sensitivity: bacterial, fungal and viral infections.
• Blood tests: haematological, biochemical, bacteriological and virological examination.
Treatment planning
• management of pain: consider all teeth of poor prognosis
• long-term treatment planning: to include attitudes and motivation
• preventive care: tailored to each individual
• restorative care: realistic aims are important
• aesthetic considerations: children can be under considerable peer pressure over their appearance.
7.3 Caries
Development of caries
Fermentation of dietary sugars by micro-organisms in plaque on the tooth surface produces organic acids. This rapid acid formation lowers the pH at the enamel surface below the level (critical pH 5.5) at which enamel will dissolve, a process known as demineralisation. When sugar is no longer available to the plaque micro-organisms, the pH within plaque will rise through the outward diffusion of acids and their metabolites. As a result, remineralisation of enamel can occur.
Dental caries progresses only when demineralisation is greater than remineralisation. The early caries lesion is subsurface with white surface demineralisation (precavitation). This may be because a layer of dental plaque on the tooth acts as a partial barrier to diffusion. Plaque forms on tooth surfaces that are not cleaned and is visually obvious within 2–3 days of ceasing toothbrushing. Plaque composition is 70% micro-organisms. Diet influences plaque flora composition; in diets rich in carbohydrate, Streptococcus mutans predominates and is very efficient at metabolising sugars to acids. Precavitated carious lesions can be reversible by remineralisation if the plaque pH is high (alkaline). This can occur during the periods where there is no sugar intake. The concentrations of calcium, phosphate and fluoride in plaque are very important in the remineralisation process.
Once cavitation has occurred and the thin white surface layer has collapsed, it is necessary to restore the tooth surface with a restoration. Cavitated lesions are not reversible.
Epidemiology of caries
The size of the problem of caries in the population has changed over time. Prevalence and extent have fallen markedly since the late 1970s in many countries and this fall can largely be attributed to fluoridated toothpaste. However, caries is becoming more of a problem in preschool children in many countries.
Diagnosis of caries
• Visual tactile (eye plus probe).
• Radiography (usually bitewing radiographs).
• Fibre-optic transillumination.
Visual and tactile detection supported by bitewing radiographs remain the most satisfactory combination for the diagnosis of occlusal and approximal caries. ERM shows great promise and is worthy of further development. However, overall systematic and random errors in diagnosis are great.
Caries risk assessment
Each child should undergo a caries risk assessment which will assist in future planning for the child, particularly in relation to the preventive regime you offer.
An effective caries risk assessment comprises seven elements:
1. Clinical evidence: this takes account of the past and present caries experience and the rate at which new lesions are developing. A child may be caries free at the time of examination, but if they have recently had carious teeth removed or repaired, they would remain as high risk. Other areas of clinical evidence adding to a child’s risk include the wearing of orthodontic appliances.
2. Dietary habits: intake and especially frequency of sugar intake is important in the development of caries.
3. Social history: main factors to look at are socioeconomic status and parental attitudes to oral health. Cost and availability of toothpaste and toothbrushes should also be explored as well as access to and cost of fresh fruit and vegetables.
4. Fluoride use: ask about toothbrushing habits and toothpaste strength and as to whether or not any other sources of fluoride are obtained.
5. Plaque control: amounts of plaque in the mouth are dependent on oral hygiene practices and sugars in the diet.
6. Saliva: some children may have specific problems in relation to the amount or composition of their saliva, making them at higher risk of developing caries.
7. Medical history: some children are at greater risk of developing caries due to their medications, prescribed diet or ability to practise oral hygiene effectively. Other children are classified as high risk if poor oral health could have a considerable detrimental effect on their current medical condition, for example cardiac or immunocompromised patients.
Prevention
The preventive regime offered will relate directly to the child’s caries risk assessment. A full preventive plan contains eight elements:
1. Radiographic frequency: for children at high risk of developing caries, radiographs for caries detection should be taken at 6-monthly intervals. For those at low risk, a more appropriate time interval would be 12–18 months. Radiographs are possible from around 3 years of age for very co-operative children. Many younger children will find this difficult and it is important to record in the casenotes why appropriate radiographs have not been taken if this is the case.
2. Toothbrushing instruction: it is important to offer children a lesson on effective toothbrushing when they are deemed to have enough manual dexterity; many will never have been shown how to brush their teeth properly. Disclosing solution or tablets can be useful in showing the child areas that they have missed. It is important to emphasise a systematic approach so that no surfaces are left unclean. They should be asked to brush gently onto their gums with the bristles angled 45° into the necks of the teeth. Powered toothbrushes, timers and sticker charts can all be good motivational tools. Caries reduction cannot be achieved by toothbrushing alone. However, brushing will control gingivitis and periodontal disease and is an important way of conveying fluoride to the tooth surface. Chemical control of plaque with chlorhexidine is effective but, because of its side-effects (staining of teeth, altered taste sensation), it should only be used as a short-term adjunct to periodontal care.
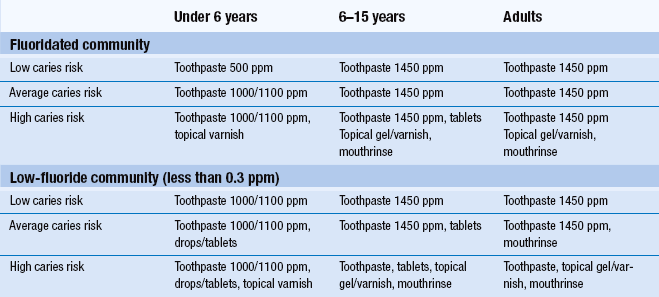
3. Toothpaste strength advice: fluoride has the ability to increase enamel resistance to demineralisation as well as decreasing acid production in plaque and increasing remineralisation. Although it has a pre-eruptive effect, its major role is posteruptive. Most adult pastes contain 1400–1500 ppm fluoride ions (used by those age 6 years and over). Children’s pastes containing 1000 ppm fluoride are available for those under 6 years (smear on brush for age 0–2, small pea sized amount for age 3–6). For very high caries risk children, adult strength toothpaste should be recommended. ‘Milk teeth’ toothpaste typically contains 400–500 ppm fluoride and should be recommended for low-risk children in areas where the water is fluoridated. Toothpaste amount should be restricted to a smear for under 2 years and a small pea size for 2–6 years. In this younger age group, supervision and assistance during brushing are needed for efficiency and to prevent excess swallowing of paste as this may lead to fluorosis.
4. Fluoride varnish frequency: professionally applied fluoride varnishes have been shown to be very effective. For children at high risk of caries, 22 600 ppm fluoride varnish can be placed 3 monthly for all ages.
5. Supplemental fluoride: fluoride mouthrinses for age 6 years and over are a valuable daily adjunct. The 0.05% NaF (225 ppm F−) mouthrinse probably has better compliance than weekly 0.2% NaF (900 ppm NaF) application. Fluoride drops and tablets for systemic use are now increasingly difficult to source and have been largely superseded by increased toothpaste strengths and regular professional application of fluoride varnish. Although each individual method of fluoride application is effective, a combination of methods may achieve greater benefit (Table 7.4).
6. Dietary advice: non-milk extrinsic sugars (NME) are most cariogenic – sucrose, glucose, fructose, maltose. Intrinsic sugars (lactose in milk and sugars in fruit and vegetables) are generally less harmful. However, even lactose in milk in a bottle overnight or nocturnal on-demand breast feeding can be cariogenic. Starchy staple foods (potatoes, bread, rice, pasta) are not a cause of dental caries, but mixtures of finely ground heat-treated starch and sugars (biscuits) are. The frequency of sugar intake and the total quantity of sugar intake are important. In British schoolchildren two-thirds of NME intake is from confectionery, soft drinks and table sugar. Unnecessary addition of extra sugars to milk and other feeds can be a cause of caries in young children.
A 3- or 4-day diet diary is more effective than simply asking a child and parent about their diet. The diet diary, if filled out correctly, will provide information about frequency and time of day with regard to sugar intake. It is also good practice for the diary to include toothbrushing times and bedtime which will increase the accuracy of your dietary analysis. The general advice here is to restrict sugary foods and drinks to mealtimes and not to consume them within 20 minutes of bedtime. Use of a feeder cup or bottle overnight with milk or juice should be strongly discouraged. If a child wants to drink throughout the night, the only safe liquid is plain water. In general, bottle-fed babies should not require overnight milk after 4–6 months old and on-demand breastfeeding overnight should also be discouraged from this time.
Non-sugar sweeteners allowed for use in food and drinks can be considered for practical purposes as non-cariogenic. There are two groups of non-sugar sweeteners:
Bulk sweeteners have a laxative effect and should not be given to children under the age of 3 years.
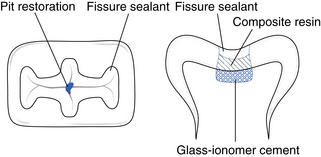
7. Fissure sealants: the most effective sealant is bisphenol-α-glycidyl methacrylate (bis-GMA) resin. At least 50% of sealants are retained for 5 years and their effectiveness in reducing and delaying the onset of caries is not in doubt. Both unfilled and filled resins and clear and opaque resins have been used to equal effect. Isolation after etching and drying is essential to success.
Indications or patient and tooth selection include: high caries risk; special needs (medical, physical, intellectual, social disability); occlusal surfaces of permanent molars, cingulum pits of upper incisors; seal as soon as moisture control permits; continue to monitor sealed teeth clinically and radiographically.
Glass ionomer fissure sealants may be used as a temporary measure in high-risk children when the tooth is partially erupted or in nervous children who cannot cope with the acid-etch procedure. Use of glass ionomer fissure sealant may also be useful for its fluoride leaching properties and can be very useful for sensitive hypomineralised molars; they have poor bonding properties and require regular replacement.
8. Sugar-free medicines: many children are on long-term medication which is often supplied to them in a sweetened elixir form. Where sugar-free formulations of the medicine are available, it is important to liaise with the patient’s general medical practitioner to ensure the child is prescribed the sugar-free version. In some cases, it is not possible to have a sugar-free alternative, such as lactulose which is prescribed to many children for constipation. If sugared medicine is required, it is prudent to check that the child can take their medications at mealtimes to lessen its cariogenic effect.
Treatment
The treatment of carious teeth should be based on the needs of the child; the long-term objective should be to help the child to reach adulthood with an intact permanent dentition, no active caries, as few teeth restored as possible and a positive attitude toward their future dental health.
Restorative materials
Amalgam: Its main advantage is that it is economical and simple to use. However, there is current concern over its safety. In Scandinavia, its use is banned in children, with concern over environmental issues rather than amalgam toxicity itself. It does seem prudent to avoid its use whenever possible, especially in the paediatric population where other materials may give sufficient longevity.
Glass ionomer cements (GIC): These consist of basic glass and acidic water-soluble powder; they set by an acid–base reaction between the two components. The cement bonds to enamel and dentine and releases fluoride to the surrounding tissues. This should be used as a temporary filling material only or for stabalisation of caries.
Resin-modified GIC: A hybrid of GIC/resin that retains significant acid–base reaction in its overall curing process to set in the dark. There are two setting reactions: the acid–base reaction between glass and polyacid and a light-activated, free radical polymerisation of methacrylate groups of the polymer. This material has some physical advantages over conventional GIC, together with its ability to ‘command set’. Again, this should be considered as a temporary or intermediate restorative material.
Polyacid-modified composite resin (compomer): This contains either or both essential components of a resin-modified GIC but it is not water based and, therefore, no acid–base reaction can occur. It will not set in the dark. This technique is very sensitive to moisture contamination and should be placed under rubber dam isolation.
Composite resins: Their introduction revolutionised clinical dentistry and their aesthetic benefits especially for the anterior teeth are unquestioned. Posterior composite resins have overcome initial problems of wear resistance, water absorption and polymerisation contraction. This technique is very sensitive to moisture contamination and should be used under rubber dam isolation.
Preformed crowns: These preformed extra-coronal restorations are essential in the restoration of grossly broken down teeth, primary molars that have undergone pulp therapy, hypoplastic primary and permanent teeth and teeth in those children at high risk of caries, particularly those having treatment under general anaesthesia. The Hall technique is currently gaining favor in the treatment of high caries risk children or for those with poor co-operation for treatment. In this technique, caries is hermetically sealed inside the tooth by the preformed crown and its glass ionomer cement, and by removing dietary substrate as an energy source for bacteria, the caries underneath arrests.
Isolation
Adequate isolation is necessary for any restorative material to have a chance of success. Rubber dam isolation is the optimum and may necessitate local anaesthesia for the gingival tissues. Clamps should be secured individually with floss ligatures. Additional advantages of the rubber dam include airway protection, soft tissue protection and reduced risk of caries infection from saliva aerosol. In the absence of rubber dam, good moisture control can be achieved with cotton wool rolls, dry tips and saliva ejector. When placing a preformed metal crown without the aid of rubber dam, it is prudent to have the child in an upright position using a sponge or gauze for airway protection and a pick-up stick or other sticky device to ensure you do not drop the crown once it has been delivered to the mouth.
Primary teeth
Pit and fissure caries: The primary fissures are shallower than their permanent counterparts and the presence of caries is a sign of high caries activity. The material of choice is an adhesive material: compomer or composite. Manufacturers’ instructions for these materials should be followed assiduously utilising tooth conditioners and bonding resins where stated.
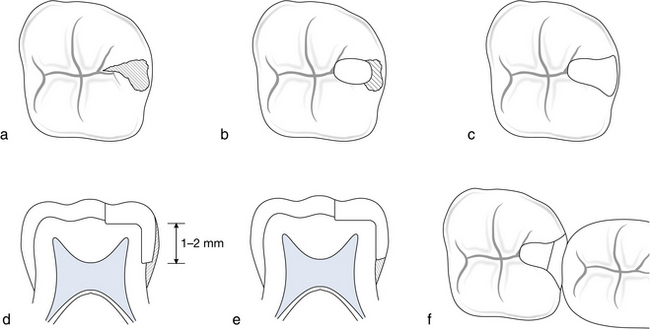
Minimal approximal cavity: A minimal approximal cavity with no occlusal dovetail is repaired using the ‘retentive box preparation’. The material of choice is a compomer or composite. The approximal box is prepared as in Box 7.1 but without an occlusal dovetail. Additional retention grooves may be achieved by placing grooves into dentine using half-round burs along the gingival floor and lingual wall. The buccal wall is avoided because of the large buccal pulp horn in primary molars (Fig. 7.1).
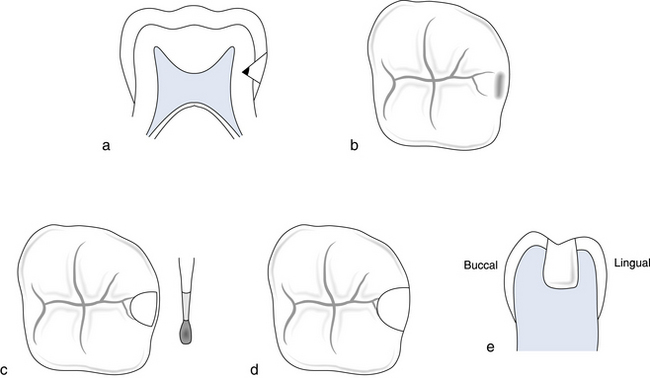
Fig. 7.1 Approximal posterior caries without pit and fissure caries: the ‘retentive box preparation’.
(a) Position of the caries. (b) Occlusal view showing cavity or shadow. (c) Access leaving sliver of enamel. (d) Extension of walls and removal of caries from the amelodentine junction. (e) Grooves placed on lingual wall and gingival floor, not on buccal wall.
Approximal caries with occlusal extension: The success rate of amalgam in approximal caries with occlusal extension has been reported as being 70–80% (Box 7.1). The material of choice is amalgam or preformed metal crown where moisture control cannot be guaranteed. An alternative is to place compomer or composite where rubber dam is possible.
Restorations on more than two surfaces: Restorations extending onto more than two surfaces include cusp replacement and endodontically-treated teeth. The preformed metal crown is the material of choice, with survival times in excess of 40 months. Their replacement rate is low at 3% compared with 15% for amalgams. Although initially they are more expensive, in the long term they are cost-effective. There are some commercially available tooth-coloured veneer crowns but these lack the flexibility of conventional preformed metal crowns and hence require an increased loss of tooth structure. Once learnt, their conventional placement technique (Box 7.2) is less technically demanding than intracoronal restorations in primary teeth and they should certainly be considered for any tooth for which the dentist cannot be sure that an alternative restoration would survive until the tooth is exfoliated.
Anterior teeth: Treatment options for anterior teeth depend on the severity of the decay and the age and co-operation of the patient. In the preschool child, caries of the upper primary incisors is usually a result of ‘early childhood caries’: frequent or prolonged consumption of fluids containing NME sugars from a bottle or feeder cup. Progression of decay is rapid, commencing on the labial surface and quickly encircling the teeth. Early treatment could involve interproximal discing and topical fluoride therapy. For more advanced decay, the most suitable form of restoration is the ‘strip crown technique’, which uses a celluloid crown former with light-cured composite resin to restore crown morphology. In older children over 3 or 4 years of age, new lesions of primary incisors indicate high caries activity. These lesions usually occur approximally and do not progress as quickly as nursing caries. They can be restored with compomer or composite resin.
Permanent teeth
Bitewing radiographs should be taken prior to any instrumentation of a tooth surface. For a clean fissure with no radiographic evidence of caries, a fissure sealant is the treatment of choice in molar teeth. If the fissure is stained with no radiographic evidence of caries, it will require clinical exploration. If clinical exploration reveals dentinal caries, then a restoration will be required. If dentinal caries is detected radiographically, a restoration is obviously necessary.
Fissure sealants: Consideration needs to be given whether to use a clear, coloured or opaque resin sealant or whether to use a non-filled or filled resin (Box 7.3). Early sealants were clear in order to check that caries was not developing under the sealant. However, the margins were difficult to see and coloured and opaque materials were introduced in order to see areas of sealant fracture and loss. The final choice is with the individual clinician. Bitewing radiographs are an important part of sealant review as it only needs failure of one small part of the sealant–enamel bond for leakage to occur.
GIC may be useful as temporary sealants in individuals with highly active caries until teeth have erupted sufficiently to allow conventional sealants (Box 7.4). Indeed, they are similarly applicable for patients in whom isolation for placement of conventional sealants is impossible. They may require more frequent replacement because of their brittleness in thin section but they will provide occlusal protection and a reservoir of fluoride for release to surrounding enamel.
Stained fissure with no radiographic caries: The fissure should be explored with a small round bur. If the lesion stays within enamel, a fissure sealant is placed. If the lesion extends into dentine, the treatment is as for pit and fissure caries.
Pit and fissure caries: Occlusal restorations can be placed using composite or amalgam. If some fissure pattern is retained, this should be fissure sealed. A preventive resin restoration is described in Box 7.5.
7.4 Tooth discoloration
The colour of a young person’s teeth is of great importance. Peer group pressure can be significant, and teasing about size, position and colour of teeth can be very harmful. The most useful method of classification for the clinical management of discoloration is one that identifies the main site of discoloration (Table 7.5).
Once the aetiology has been identified, the most appropriate method of treatment can be chosen. Treatment emphasis should be on minimal tooth preparation. As a general rule, microabrasion should be the first-line treatment for all cases of enamel opacities and mottling; composite resin in the form of localised or full veneers is used in preference to porcelain.
Treatments
Treatments for discoloured teeth can be used in children and adults, although some are not suitable for children younger than teenage. Techniques use abrasion, bleaching and restorations. The exact mechanism by which bleaching occurs remains unknown. Theories of oxidation, photo-oxidation and ion exchange have been suggested.
The hydrochloric acid–pumice microabrasion technique
The microabrasion method is a controlled removal of surface enamel in order to improve discolorations that are limited to the outer enamel layer (Box 7.6). It is achieved by a combination of abrasion and erosion and the term ‘abrosion’ is sometimes used. No more than 100 µm of enamel are removed. Once completed, the procedure should not be repeated. Too much enamel removal is potentially damaging to the pulp and cosmetically the underlying dentine colour will become more evident.
Effectiveness: Critical analysis of the effectiveness of the technique should not be made immediately but delayed for at least 1 month as the appearance of the teeth will continue to improve over this time. Experience has shown that although white mottling is often incompletely removed, it does become less perceptible. This phenomenon has been attributed to the relatively prismless layer of compacted surface enamel produced by the ‘abrosion’ technique which alters the optical properties of the tooth surface.
Long-term studies of the technique have found no association with pulpal damage, increased caries susceptibility or significant prolonged thermal sensitivity. Patient compliance and satisfaction are good and any dissatisfaction is usually a result of inadequate preoperative explanation. The technique is easy to perform for operator and patient and is not time-consuming. Removal of any mottled area is permanent and is achieved with an insignificant loss of surface enamel. Failure to improve the appearance by the microabrasion technique does not have any harmful effects and may make it easier to mask some lesions with veneers.
Non-vital bleaching
Non-vital bleaching is used for teeth that have become discoloured by the diffusion into the dentinal tubules of haemoglobin breakdown products from necrotic pulp tissue (Box 7.7).
Effectiveness: If the colour of a tooth has not significantly improved after three changes of bleach, it is unlikely to do so and further bleaching should be abandoned. The maximum number of bleach applications is usually accepted as ten. Failure of a tooth to bleach could be caused by inadequate removal of filling materials from the pulp chamber. This should be checked before abandoning a procedure.
Slight overbleaching is desirable, but the patient should be instructed to attend the surgery before the next appointment if marked overbleaching has occurred.
Non-vital bleaching has a reputation for causing brittleness. This may be the result of previous injudicious removal of dentine (which only needs to be ‘freshened’ with a round bur) rather than a direct effect of the bleaching procedure itself.
This method of bleaching has been associated with the later occurrence of external cervical resorption. The exact mechanism is unclear, but it is thought that the previously used hydrogen peroxide diffused through the dentinal tubules to set up an inflammatory reaction in the periodontal ligament around the cervical region of the tooth. In a small number of teeth, there is a gap between the enamel and the cementum, and in these the above explanation is tenable. The purpose of the 1 mm layer of glass ionomer cement is to cover the openings of the dentinal tubules at the level where there may be a communication to the periodontal ligament. In the same way, non-setting calcium hydroxide is placed in the pulp chamber for 2 weeks prior to final restoration in order to eradicate any inflammation in the periodontal ligament. It is unknown whether the perborate mixture is associated with external cervical resorption.
Clinical studies have demonstrated that regression can be expected with this technique. The longest study after 8 years gave a 21% failure rate. However, if white gutta-percha has been placed within the pulp chamber, it can be readily removed and the tooth easily rebleached.
Chair-side vital bleaching
Vital bleaching in the surgery involves the external application of hydrogen peroxide to the surface of the tooth followed by its activation with a heat source (Box 7.8). The technique is lengthy and time-consuming and demands a high degree of patient compliance and motivation. Within paediatric dentistry, it is appropriate only for the teenager. Its main remit is in the older patient to treat the yellowing of teeth that occurs with ageing.
Nightguard vital bleaching
The nightguard vital bleaching technique involves the daily replacement of carbamide peroxide gel into a custom-fitted tray of either the upper or lower arch (Box 7.9). Like the previous technique, it demands a high degree of patient compliance and motivation and is appropriate in paediatric dentistry only for the teenager. Its main remit is in the older patient to treat the yellowing of teeth. A full explanation of the current legal discussions concerning the use of products containing >0.1 hydrogen peroxide must be given to the patient and consent obtained.
Indications in paediatric dentistry:
Carbamide peroxide gel (10%) breaks down in the mouth into 3% hydrogen peroxide and 7% urea. Both urea and hydrogen peroxide have low molecular weights, which allow them to diffuse rapidly through enamel and dentine. This explains the transient pulpal sensitivity occasionally experienced with bleaching systems for use at home.
Localised composite resin restorations
Defective enamel can be replaced with a tooth-coloured restoration that bonds to, and blends with, enamel (Box 7.10). It is indicated for well-demarcated white, yellow or brown patches.
The localised restoration is quick and easy to complete. Despite the removal of defective enamel down to the amelodentine junction, there is often no significant sensitivity and, therefore, no need for local anaesthesia. If the hypoplastic enamel has become carious and extends into dentine, local anaesthesia will be required. Advances in bonding and resin technology make these restorations simple and obviate the need for a full labial veneer. Disadvantages are marginal staining and difficulty in achieving an accurate colour match.
Composite resin veneers
Although some form of porcelain restoration may be the most satisfactory long-term restoration for a severely hypoplastic or discoloured tooth, it is not an appropriate solution for children for two reasons: the large size of the young pulp horns and chamber, and the immature gingival contour.
Composite veneers may be direct (placed at initial appointment; Box 7.11) or indirect (placed at a subsequent appointment having been fabricated in the laboratory). Composite veneers are durable enough to last through adolescence.
Before proceeding with any veneering technique, the decision must be made whether to reduce the thickness of labial enamel before placing the veneer. Certain factors should be considered:
• Increased labiopalatal bulk makes it harder to maintain good oral hygiene; this may be courting disaster in the adolescent with dubious oral hygiene.
• Composite resin has a better bond strength to enamel when the surface layer of 200–300 µm is removed.
• If a tooth is very discoloured, some sort of reduction will be desirable as a thicker layer of composite will be required to mask the intense stain.
• If a tooth is already instanding or rotated, its appearance can be enhanced by a thicker labial veneer.
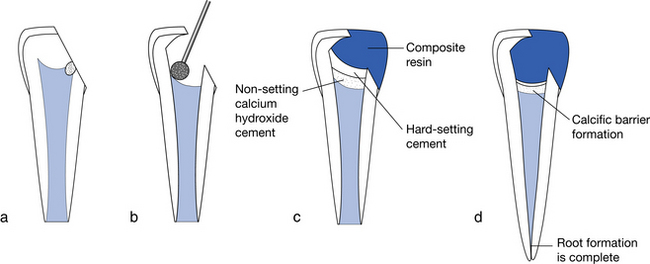
New-generation, highly polishable hybrid composite resins can replace relatively large amounts of missing tooth tissue as well as being used in thin sections as a veneer. Combinations of shades can be used to stimulate natural colour gradations and hues. The exact design of the composite veneer will vary with each patient. Usually, it will be one of four types: intra-enamel or window preparation, incisal bevel, overlapped incisal edge or feathered incisal edge (Fig. 7.4).
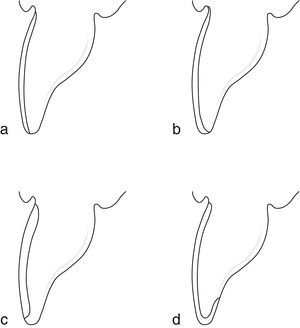
Fig. 7.4 Types of veneer preparation.
(a) Feathered incisal edge. (b) Incisal bevel preparation. (c) Intra-enamel or window preparation. (d) Overlapped incisal edge preparation.
Porcelain veneers
Normally, porcelain veneers are considered at around 18 years of age when the gingival margin is at an adult level and the standard of oral hygiene is acceptable. However, a non-standard application which may be applicable at an earlier age is the restoration of the peg lateral with a three-quarter wrap-around veneer finished to a knife edge at the gingival margin.
7.5 Tooth surface loss (wear)
Dentists have been aware of the problem of tooth wear or non-carious loss of tooth tissue for a long time. However, it is only more recently that it has been associated increasingly with our younger population. There are three processes that make up the phenomenon of tooth wear:
1. Attrition: wear of tooth as a result of tooth contact.
2. Erosion: irreversible loss of tooth substance brought about by a chemical process that does not involve bacterial action.
3. Abrasion: physical wear of tooth substance produced by something other than tooth-to-tooth contact.
In children, abrasion is relatively uncommon. The most frequent cause of abrasion is overzealous toothbrushing, which tends to develop with increasing age. Attrition during mastication is common, particularly in the primary dentition where almost all upper incisors show some signs of attrition by the time they exfoliate. However, in the 1990s, the contribution of erosion to the overall process of tooth wear in the younger population has been highlighted.
While erosion may be the predominant process, attrition and abrasion may be compounding factors (e.g. toothbrush abrasion may be increased if brushing is carried out immediately after the consumption of erosive foodstuffs or drinks). It is often difficult to identify a single causative agent in a case of tooth wear so the general term tooth surface loss may be more appropriate.
Prevalence
There is very little published evidence on the prevalence or severity of tooth wear in children. In 1993, the National Child Dental Health Survey included assessment of the prevalence of erosion of both primary and permanent incisor teeth for the first time. The survey reported that 52% of 5-year-old children had erosion of the palatal surfaces of their primary incisors with 24% showing progression into the pulp. The prevalence of erosion of the palatal surfaces of permanent incisors was also alarmingly high: 27% in 15-year-olds. However, only 2% in this age group showed progression into the pulp. What is unclear is whether the problem of tooth surface loss is actually increasing or whether these figures reflect an increased awareness.
Aetiology
In young patients, there are three main causes of tooth surface loss:
In addition to these, certain environmental factors have been linked to tooth wear. With the exception of frequent use of chlorinated swimming pools, most environmental and occupational hazards do not apply to children.
Dietary causes of tooth surface loss: The most common cause of erosive surface loss is excessive intake of acidic food or drink. Food and drink implicated in erosive tooth surface loss in young patients include:
• citrus fruits (e.g. lemons, oranges, grapefruits)
• carbonated drinks, including low-calorie varieties, sparkling mineral water and ‘sports’ drinks
Acidic drinks, in particular, are available to all age groups of children. Pure ‘baby’ fruit juices are marketed for consumption by infants and these have been shown to have pH values below the critical pH for the dissolution of enamel (pH 5.5). Many of these drinks are given to infants in a feeding bottle, and the combination of the highly acidic nature of the drink and the prolonged exposure of the teeth to the acidic substrate may result in excessive tooth surface loss as well as dental caries. While a wide range of foods and drinks is implicated in the aetiology of tooth surface loss, soft drinks make up the bulk of the problem. These are now widely available in vending machines located in schools, sports centres and other public areas. Both normal and so-called ‘diet’ carbonated drinks have very low pH values and are associated with tooth surface loss, as are other fruit juices and diluting juices. While there is no direct relationship between the pH of a substrate and the degree of tooth surface loss, pH does give a useful indication as to the potential to cause damage. Other factors, such as titrateable acidity, the effect on plaque pH and the buffering capacity of saliva, will influence the erosive potential of a given substrate. In addition, it has been shown that erosive tooth surface loss tends to be more severe if the frequency and volume of drink consumed is high or if the intake occurs at bedtime or during the night.
The pattern of dietary erosive tooth surface loss depends on the manner in which the substrate is consumed. Carbonated drinks are commonly held in the mouth for some time as the child ‘enjoys’ the sensation of the bubbles. This habit may result in a generalised loss of surface enamel. Generalised loss of surface enamel of posterior teeth is often evident, particularly on the first permanent molars. Characteristic saucer-shaped lesions develop on the cusps of the molars. This phenomenon is known as perimolysis.
Gastric regurgitation and tooth surface loss: The acidity of the stomach contents is below pH 1.0; therefore, any regurgitation or vomiting is potentially damaging to the teeth. As many as 50% of adults with signs of tooth surface loss have a history of gastric reflux. The aetiology of gastric regurgitation may be divided into those with upper gastrointestinal disorders and those with eating disorders.
In young patients, long-term regurgitation is associated with a variety of underlying problems:
• Chronic respiratory disease.
• Disease of the liver/pancreas/biliary tree.
• Feeding problems/failure to thrive conditions.
In addition, there is a group of patients that suffer from gastro-oesophageal reflux disease (GORD). This may be either symptomatic, in which case the individual knows what provokes the reflux, or the more insidiously asymptomatic GORD, in which the patient is unaware of the problem and continues to ingest reflux-provoking foods.
Parafunctional activity: Localised tooth surface loss frequently occurs in patients who exhibit abnormal parafunctional habits. The excessive grinding that is a feature of this problem is not always apparent to the patient. However, apart from the marked tooth tissue loss, other signs of bruxism may be evident including hypertrophy of the muscles of mastication, cheek biting and tongue faceting. An example of erosion and parafunction having a disastrous effect on the dentition may be seen (and heard) in children who have cerebral palsy. These children often have chronic gastric regurgitation and also severe bruxism, resulting in excessive tooth surface loss.
Management
The most important part of management is early recognition. It is important to establish the aetiology and, where possible, eliminate the cause prior to treating any sensitivity. Dietary counselling should be personal, practical and positive. Suitable alternatives should be suggested with the most appropriate times for their intake:
• Inform patients of types of foods and drinks that have greatest erosive potential.
• Suggest still/non-carbonated drinks as an alternative.
• Limit the intake of acidic foods/drinks to meal times.
• Advocate use of neutral fluoride mouthwash or gel for daily use to try and minimise the effect of the acids.
• Encourage use of bicarbonate of soda mouthrinse in those with recurrent gastric reflux.
• Where attrition is marked, neutral fluoride gel can be placed into an occlusal guard during the night or during episodes of vomiting.
Immediate temporary coverage of sensitive teeth with GIC or composite resin can relieve symptoms and act as a diagnostic aid.
Definitive management
The main treatment objectives are to:
Study models must be taken at initial diagnosis and at periodic intervals to monitor progress. Table 7.6 outlines the merits of the restorative materials available.
Table 7.6
Treatment technique for tooth surface loss
| Technique | Advantages | Disadvantages |
| Cast metal (nickel/chrome or gold) | Fabrication in thin section: requires only 0.5 mm space Very accurate fit possible Very durable Suitable for posterior restorations in parafunction Does not abrade opposing dentition |
May be cosmetically unacceptable because of ‘shine through’ of metallic grey Cannot be simply repaired or added to intraorally |
| Composite direct | Adequately durable for labial veneers only Least expensive May be used as a diagnostic tool |
Technically difficult for palatal veneers Limited control over occlusal and interproximal contour Inadequate as a posterior restoration |
| Indirect | Can be added to and repaired relatively simply Aesthetically superior to cast metal Control over occlusal contour and vertical dimension |
Requires more space: minimum of 1.0 mm Unproven durability |
| Porcelain | Best aesthetics Good abrasion resistance Well tolerated by gingival tissues |
Potentially abrasive to opposing dentition Inferior marginal fit Very brittle: has to be used in bulk section Hard to repair |
7.6 Endodontics
Primary teeth
The question of whether to retain primary teeth should be based on three factors: medical, behavioural and dental.
Pulpal treatment options
Indirect and direct pulp capping: Pulp capping can be applied successfully to the primary dentition provided strict selection criteria are applied.
Indirect capping: Gentle excavation of the majority of softened dentine is achieved without exposing the pulp. The remaining softened dentine is covered with setting calcium hydroxide to destroy any remaining micro-organisms and to promote the deposition of reparative secondary dentine. The tooth is then restored at the same visit.
Direct capping: The small mechanical exposure on a vital symptom-free tooth that is well isolated is the only situation where direct capping should be applied. If direct capping is applied in other situations, pulp inflammation usually persists and results in total pulp necrosis. In the majority of children, pulpotomy is the preferred treatment, with a high rate of success.
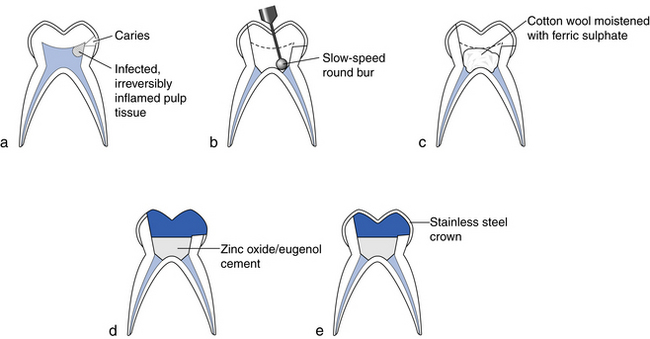
Pulpotomy: Pulpotomy involves the extirpation of vital inflamed pulp from the coronal chamber as a means of preserving the vitality and function of the remaining portion of radicular pulp (Box 7.12).
There remains some controversy over the most appropriate medicaments for use in vital primary molar pulpotomies. Currently ferric sulphate is held as the most appropriate and safe medicament with a success rate of around 95%. It is postulated that ferric sulphate works by controlling pulpal bleeding and promotes formation of a ‘protective’ metal/protein clot over the underlying vital radicular pulp. The use of mineral trioxide aggregate is gaining vogue; this material has excellent bioactive properties and essentially stimulates cytokine release from pulpal fibroblasts, which in turn stimulates dental hard tissue formation. A well-condensed layer of pure calcium hydroxide powder applied directly over the radicular pulp has also been advocated. If successful, the treated tooth should be asymptomatic. Failure will result in pain, swelling, increased mobility, fistulae and radiographic signs of either radiolucency at the furcation or apex or internal/external resorption of the root.
Radiographic assessment every 12 months is necessary to check the above and the developing underlying permanent successor.
Pulpectomy: Pulpectomy involves the chemomechanical preparation of primary root canals with endodontic hand instruments and irrigants (Box 7.13). Because of the anatomy of the root canals and the presence of the permanent successor, greater emphasis is often placed on the use of the antimicrobial properties of the obturating material, especially in primary posterior teeth. Success rates involving zinc oxide eugenol have been reported as 60–80% but more recent studies have found success rates of up to 100% with the use of Vitapex™; (calcium hydroxide and iodoform paste).
Pulpectomy for anterior primary teeth: The procedure can be completed in one visit (see Box 7.13).
Pulp treatments under general anaesthesia: It is usual to extract all teeth of dubious prognosis in a child who is not co-operative or cannot co-operate and requires treatment under general anaesthesia. However, one-stage procedures are possible and the operator will have to assess pulpal status and radiographic signs accordingly.
Clinical problems with pulpally involved primary teeth: There are situations where it is clinically impossible or inappropriate to complete ideal pulp therapy and these are usually associated with the behaviour of the child:
• When an unexpected exposure is encountered and no local anaesthetic has been given.
The aim of treatment is to control pain and to prevent further pain (Box 7.14).
Young permanent molar teeth with immature apices
The treatment of choice for the cariously exposed young permanent tooth is dependent on:
The final decision has to balance the long-term advisability of retaining the tooth and the practicality of restoring the crown. Coronal destruction in an immature molar tooth is associated with pulpal exposure, which will mean that this tooth will require maintenance throughout life.
Vital teeth with immature roots
For vital teeth with immature roots, the aim of therapy is to preserve vitality to ensure completion of root development.
Indirect pulp cap: An indirect pulp cap is indicated in teeth with minimal symptoms (Fig. 7.7). A thin layer of carious dentine is left over the pulp because its removal would create an exposure. Calcium hydroxide cement is usually placed over the softened dentine but glass ionomer cement has also been advocated. The ‘step-wise technique’ can be used to avoid pulpal exposure in deeply carious lesions. In this technique, soft and stained dentine is given an opportunity to remineralise and can then be checked or removed at a subsequent visit some months later.
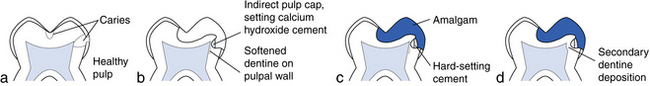
Fig. 7.7 Indirect pulp capping.
(a) Symptom-free molar tooth with deep proximal caries. (b) The caries is excavated to the brink of pulpal exposure leaving a small amount of softened dentine. A thin layer of setting calcium hydroxide cement is applied to the softened dentine as an indirect pulp cap. (c) The indirect pulp cap is covered with hard cement and the tooth restored with amalgam. (d) Some months later, the pulp has remained vital and secondary dentine deposition is evident. (From Whitworth, Nunn 2001. In: Welbury RR (ed.) Paediatric dentistry, 2nd edn, Fig. 9.9, p. 168. By permission of Oxford University Press, www.oup.com.)
Direct pulp cap: Permanent teeth respond well to direct pulp capping procedures, unlike primary teeth. Selection of appropriate cases is important.
Non-vital teeth with immature roots
Non-vital teeth with immature roots often require to be removed, although short-term retention for orthodontic reasons may be desirable. After root canal instrumentation and cleaning, a medicament such as non-setting calcium hydroxide should be placed and the crown restored.
Young permanent incisor teeth with immature apices
Permanent vital incisors can be treated with calcium hydroxide pulpotomy or Cvek pulpotomy (apexogenesis). The aim is removal of contaminated pulp tissue with a clean, round, high-speed diamond bur in order to allow radicular growth with vital radicular pulp (Box 7.15).
Success rate is 80–96%. Prognosis is best if the procedure is completed within 24 hours of exposure.
Non-vital incisors
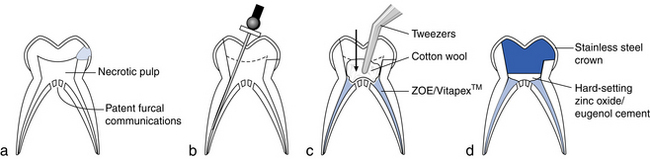
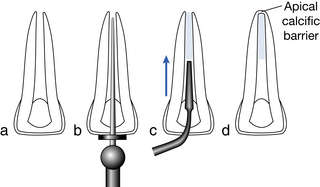
Non-vital incisors require an apical barrier onto which a gutta-percha can be condensed. The most appropriate way to achieve this is with mineral trioxide aggregate (MTA). Some still induce calcific barrier formation with non-setting calcium hydroxide (apexification) but this is losing popularity as its long-term use makes the tooth root brittle and liable to fracture (Box 7.16).
Endodontic complications in young permanent incisor teeth
Root canal therapy can often be confined to the non-vital coronal portion of the canal. Instrumentation by rotation of hand files and placement of MTA to the fracture line aims to produce a stop at the coronal side of the fracture line. The coronal portion can then be obturated with gutta-percha and sealer.
If the apical portion is non-vital, it may be possible to instrument across the fracture line, although it can be very difficult to prevent bleeding into the canal. Failure to instrument a non-vital apical fragment necessitates surgical removal of the fragment. Splinting across fracture lines with a post is a radical temporary solution with a poor long-term prognosis.
Root resorption
External: Resorption is initiated by damage to the periodontal ligament but propagated by necrotic pulp tissue via dentinal tubules. Diagnosis is by asymmetrical radiolucent shape of surface of root with intact root canal walls (Fig. 7.10).
Internal: Resorption is initiated by cells of the pulp within the root canal. Diagnosis is as a ballooning of the root canal with intact root surface (Fig. 7.11).
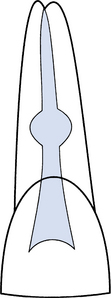
Fig. 7.11 Ballooning of the root canal caused by internal resorption. (From Whitworth, Nunn 1997. In Welbury RR (ed.) Paediatric dentistry. By permission of Oxford University Press, www.oup.com.)
Treatment of both types is by thorough mechanical and chemical debridement followed by non-setting calcium hydroxide paste for 4–6 weeks. Obturation with thermoplastic gutta-percha is then completed although if resorption continues, the tooth will eventually be lost.
Cervical: This is an unusual form of external inflammatory resorption initiated by damage to the root surface in the cervical region and propagated either by infected root canal contents or by periodontal microflora. Treatment is usually by obturation of the root canal followed by surgical external repair and restoration.
Replacement: Replacement is progressive resorption of tooth structure and its replacement with bone as part of continued bone remodelling. It occurs after trauma in which there is significant periodontal ligament injury (i.e. luxation, intrusion and avulsion). It cannot be treated. The tooth should be maintained in the mouth for as long as possible with intracanal non-setting calcium hydroxide dressings while plans are made for permanent prosthetic replacement.
![]() Self-assessment: questions
Self-assessment: questions
Multiple choice questions (True/False)
1. The mineralisation of these teeth may be affected by maternal illness during pregnancy:
2. With regard to childhood development and dental treatment:
a. Separation from parents is possible after age 5 years
b. Adequate manual dexterity for good oral hygiene is possible at age 5 years
c. Parental influence is important
d. By age 5 years, children have developed selective attention
3. Bitewing radiographs should be taken every 6 months for:
a. Primary dentition with high caries risk
b. Primary dentition with low caries risk
c. Mixed dentition with low caries risk
4. Conventitional orthopantograms:
a. Diagnose occlusal caries accurately
b. Diagnose interproximal caries accurately
c. Identify abnormalities in dental development of number, position or form
a. Plaque consists mainly of food debris
b. Precavitation lesions are reversible
c. Cavitated lesions are reversible
a. Diagnosis of interproximal caries in the primary dentition is easy
b. Marginal ridge breakdown in primary molars suggests pulpal involvement
c. Stained fissures in first permanent molars should be explored
a. The fall in caries prevalence since the 1970s is largely a consequence of toothbrushing
b. Preschool caries is related to maternal Streptococcus mutans levels
c. Nursing caries is associated with frequent use of sugared drinks
d. Nursing caries can be prevented by correct advice
e. Caries prevention can be maximised by professional application of fluoride varnish
8. Fluoride supplementation should be given:
a. Systemically to all patients with special needs
b. As a mouthwash to a 5-year-old
d. In only one systemic form of delivery
e. In topical form to all patients with orthodontic appliances
9. With regard to restorative materials in the primary dentition:
a. Amalgam is the material of choice for pit and fissure caries where moisture control is good
b. Nursing caries is best treated with glass ionomer cement
c. Approximal box cavities without occlusal extension should be restored with amalgam
d. Preformed metal crowns are the most durable restorations for large cavities and endodontically-treated teeth
e. Glass ionomer cement is suitable for two-surface cavities
10. With regard to the restoration of permanent teeth:
a. Composite can be placed in pit and fissure location as long as good moisture control is possible
b. Composite can be placed in approximal cavities
c. Regular bitewing radiographs are required for fissure-sealed teeth
d. Stained fissures should be investigated early to conserve tooth tissue
11. In extrinisc tooth discoloration:
a. Stains can be removed by polishing
b. Bleaching is an accepted treatment
c. Mouthwashes can be an important factor
a. May be caused by internal resorption
c. If caused by fluorosis, it can be treated by microabrasion
13. In primary molar endodontics:
a. Vital pulpotomy has a low success rate
b. Calcium hydroxide can be used over the pulp stumps
c. Teeth with furcation caries should be extracted
d. Treatment is indicated in children with cardiac defects
e. Treatment is indicated in children with bleeding coagulopathies
14. In permanent incisors with open apices:
a. Pulpotomy is preferred to pulp cap for pulpal exposures over 1 mm in size
b. Pulpotomy medicament of choice is non-setting calcium hydroxide
c. Pulpotomy enables radicular development with vital pulp tissue
d. Pulpectomy with non-setting calcium hydroxide can allow continued root end growth
e. MTA is the material of choice for apical barrier formation.
Extended matching items questions
Theme: Dental diagnosis in children
For each of the case scenarios (a–e), select from the list below (1–12) the single most appropriate diagnosis for the signs and symptoms given. Each diagnosis may be used once, more than once or not at all:
2. External cervical resorption.
12. Nursing/early childhood caries.
a. A 3-year-old child attends your surgery with caries affecting the upper incisors and first primary molars.
b. An 8-year-old boy suffers from GORD and you notice the enamel on the palatal surface of his upper incisors has a glass-like surface.
c. You take a radiograph of a non-vital tooth for which you have previously provided internal bleaching. You notice a radiolucency around the amelocemental junction.
d. You decide to provide hydrochloric acid microabrasion for a 10-year-old boy with a previous history of eating toothpaste.
e. You decide to provide a pulpectomy and stainless steel crown for a 6-year-old haemophiliac child.
Case history question
An 8-year-old child who was previously caries free suddenly develops interproximal lesions.
Picture questions
Figure 7.12 shows teeth that erupted 12 days after birth.