Chapter 15 Structure and function of the foot
INTRODUCTION
The main function of the foot is to transmit loads between the lower leg and the ground. In static and, in particular, dynamic situations, such as walking, running, jumping, and landing, the foot is subjected to large loads, which, unless effectively transmitted, would be likely to excessively overload not only the foot but also other parts of the musculoskeletal system (Watkins 1999).
In dynamic situations the foot is required to act as both a shock absorber, to cushion the impact of contact of the foot with the ground, and as a propulsive mechanism to propel the body in the desired direction (Blackwood et al 2005). The foot often performs these functions on a variety of support surfaces. Whereas floor surfaces tend to be firm and level, there are many other situations, such as in cross-country running, where the surface of the ground is neither firm nor level, but continually changes in terms of slope, evenness and hardness. The ability of the foot to function effectively in relation to such diverse environmental constraints is due to its structure, in particular to its arched shape and complex movement capability.
SKELETON OF THE FOOT
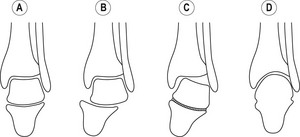
The foot consists of 7 tarsals, 5 metatarsals and 14 phalanges (Fig. 15.1). The tarsals constitute the tarsus, which forms the rear part of the foot. The foot articulates with the lower leg at the ankle joint (talocrural joint), i.e. the joint between the tibia, fibula and talus. The talus, the second largest tarsal, has a convex pulley-shaped articular surface on its superior aspect, called the trochlear surface of the talus, that articulates with the trochlear surface of the tibia. The trochlear surface of the talus is continuous with articular surfaces on its lateral and medial aspects that articulate with the lateral malleolus and medial malleolus, respectively.
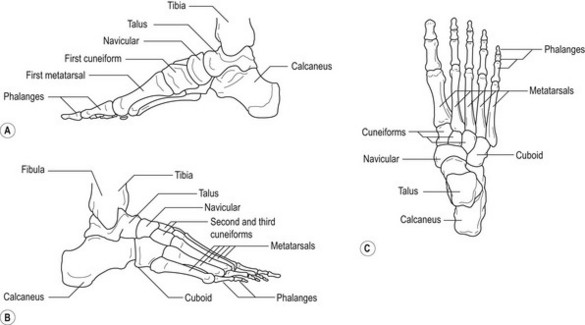
Figure 15.1 The bones of the right foot. (A) Medial aspect. (B) Lateral aspect. (C) Superior aspect.
The inferior aspect of the talus articulates with the anterior half of the superior aspect of the calcaneus by means of two or, in some cases, three articular facets, which together constitute the subtalar joint (talocalcaneal joint). The anterior aspect (head) of the talus articulates with the posterior aspect of the navicular, on the medial aspect of the foot, to form the talonavicular joint. The anterior aspect of the calcaneus articulates with the posterior aspect of the cuboid, on the lateral aspect of the foot, to form the calcaneocuboid joint. The calcaneocuboid and talonavicular joints are continuous with each other and constitute the midtarsal joint, also referred to as the transverse tarsal joint (Czerniecki 1988). The anterior aspect of the navicular articulates with the posterior aspects of the three cuneiforms (medial, middle, lateral), which lie side by side and articulate with each other. The posterior two-thirds of the lateral aspect of the lateral cuneiform articulate with the medial surface of the cuboid. The anterior aspects of the medial, middle and lateral cuneiforms articulate with the bases of the first, second and third metatarsals, respectively. The anterior aspect of the cuboid articulates with the bases of the fourth and fifth metatarsals. The joints between the four anterior tarsals and the metatarsals are referred to as the tarsometatarsal joints. The lateral four metatarsals are similar in length, but tend to increase in girth from the second to the fifth. In comparison, the first metatarsal is usually shorter, but has a greater girth than the other four. The metatarsals are collectively referred to as the metatarsus. The heads of the metatarsals articulate with the proximal phalanges of the toes to form the metatarsophalangeal joints. The great toe (also referred to as the big toe or the hallux) is composed of two phalanges and each of the other toes is composed of three phalanges. The phalanges of the toes become progressively shorter from proximal to distal.
In addition to the tarsals, metatarsals and phalanges, a number of small accessory bones and sesamoid bones occur during fetal life ( Anwar et al 2005, Williams et al 1995). There are normally about ten irregular-shaped accessory bones distributed around the tarsus; most of these bones fuse with one of the tarsal bones prior to skeletal maturity. There are normally about 12 sesamoid (seed-shaped) bones. Each sesamoid bone is partially embedded in a tendon or ligament, with the free surface of the bone forming a synovial joint with a bone over which the tendon or ligament slides during normal function. In addition to preventing the tendon or ligament from rubbing on the adjacent bone, sesamoid bones tend to increase the mechanical efficiency (leverage) of the associated musculotendinous unit or ligament. The two most important sesamoid bones of the foot, which contribute significantly to stabilising the foot during propulsion (see the section on the windlass mechanism later in this chapter), are the sesamoids in the plantar aponeurosis (see later section on arches of the foot) beneath the base of the first metatarsophalangeal joint; the medial sesamoid is shown in Figure 15.1A.
MOVEMENTS OF THE ANKLE AND FOOT
Many of the 26 bones in each foot articulate with two or more other bones such that there are approximately 40 joints in each foot. Consequently, most movements of the foot involve a large number of joints, and the movement of individual joints in each movement is difficult to describe. However, as in most movements of the body, there tends to be high degree of functional interdependence between the joints of the foot, especially between the intertarsal and tarsometatarsal joints, such that movement of one joint tends to bring about fairly predictable movement in adjacent joints (Kitaoka et al 1997a, Nester 1997, Singh et al 1992). A group of joints with a relatively high degree of functional interdependence is called a joint complex (Peat 1986). The term ‘rearfoot complex’ is frequently used to describe the functional interdependence between the ankle, subtalar and midtarsal joints (Bowden & Bowker 1995, Downing et al 1978, Nester 1997).
Ankle joint
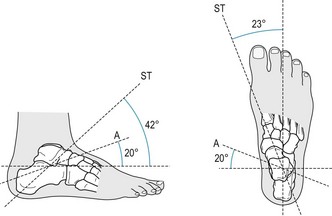
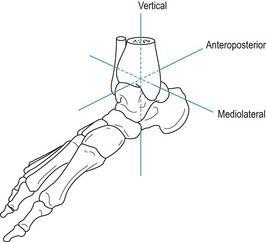
The ankle joint is a hinge joint that facilitates rotation about an axis of rotation which runs approximately 20° anterosuperiorly in the sagittal plane with respect to the horizontal plane and 20° anteromedially in the horizontal plane with respect to the coronal plane (Fig. 15.2) (Singh et al 1992). Consequently, the movement of the ankle joint is triplanar (i.e. movement occurs simultaneously in the sagittal, coronal and horizontal planes), with movement predominantly in the sagittal plane. Movement in the sagittal, coronal and horizontal planes occurs about the mediolateral, anteroposterior and vertical axes, respectively (Fig. 15.3). Sagittal plane motion of the foot about the ankle joint is usually referred to as plantar flexion and dorsiflexion. In dorsiflexion, sometimes referred to as true flexion of the ankle, the dorsal (superior) surface of the foot is drawn closer to the shin. In plantar flexion, sometimes referred to as extension of the ankle, the plantar (inferior) surface of the foot is pushed further away from the shin (pointing the toes).
Subtalar joint
The subtalar joint is part synovial and part syndesmosis. The anterior synovial part of the joint is separated from the posterior synovial part of the joint by a funnel-shaped channel called the sinus tarsi. The sinus tarsi runs more or less horizontally in an oblique posteromedial to anterolateral direction (Fig. 15.4) with the funnel opening out laterally. The posterior talar articular surface of the calcaneus is convex and articulates with the reciprocally shaped concave posterior calcanean articular surface of the talus. The anterior talar articular surface of the calcaneus (located on the superior aspect of the sustentaculum tali) is concave and articulates with the reciprocally shaped convex anterior calcanean articular surface of the talus. Whereas Figure 15.4 shows only one articular surface in the anterior synovial part of the subtalar joint, there are frequently two adjacent articular surfaces. Four distinct variations in the number (one or two), shape and orientation of the anterior synovial articular surfaces have been identified (Valmassy 1996). The syndesmosis part of the subtalar joint consists of a broad interosseous talocalcanean ligament, which runs obliquely downward and laterally from the sulcus tali (superior part of the sinus tarsi) to the sulcus calcanei (inferior part of the sinus tarsi). The interosseous talocalcanean ligament becomes taut in eversion (Williams et al 1995). Distal to the anterior end of the sinus tarsi is another broad ligament called the cervical ligament. The cervical ligament runs obliquely upward and medially from the anterior superior aspect of the calcaneus to the lateral aspect of the neck of the talus. The cervical ligament becomes taut in inversion (Williams et al 1995).
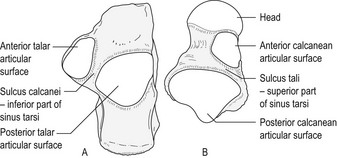
Figure 15.4 Articular surfaces of the right subtalar joint. (A) Superior aspect of the right calcaneus. (B) Inferior aspect of the right talus.
Like the ankle joint, the movement of the subtalar joint is triplanar. Inman (1976) showed that the orientation of the axis of the joint varies considerably between individuals, with a mean orientation of approximately 42° anterosuperiorly in the sagittal plane with respect to the horizontal plane and 23° anteromedially in the horizontal plane with respect to the sagittal plane (Fig. 15.2).
Pronation and supination
In contrast to the ankle and subtalar joints, there would appear to be little empirical information on the movement of the midtarsal joint, which is composed of a biplanar/biaxial saddle joint (calcaneocuboid) and a triplanar/triaxial ball-and-socket joint (talonavicular) (Blackwood et al 2005). However, it is clear that the rearfoot complex facilitates triplanar movements of the foot, which are referred to as pronation and supination (Fig. 15.5) (Kitaoka et al 1997a, Nester 1997).
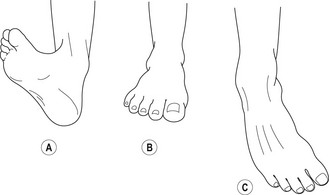
Figure 15.5 Supination and pronation of the foot. (A) Full pronation. (B) Neutral position. (C) Full supination.
Pronation involves simultaneous abduction (vertical axis), dorsiflexion (mediolateral axis) and eversion (anteroposterior axis) (Fig. 15.5A,B). Similarly, supination involves simultaneous adduction, plantar flexion and inversion (Fig. 15.5B,C). The orientation of the rearfoot axis varies considerably, with a mean orientation of approximately 51° anterosuperiorly in the sagittal plane with respect to the horizontal plane and 18° anteromedially in the horizontal plane with respect to the sagittal plane (Downing et al 1978).
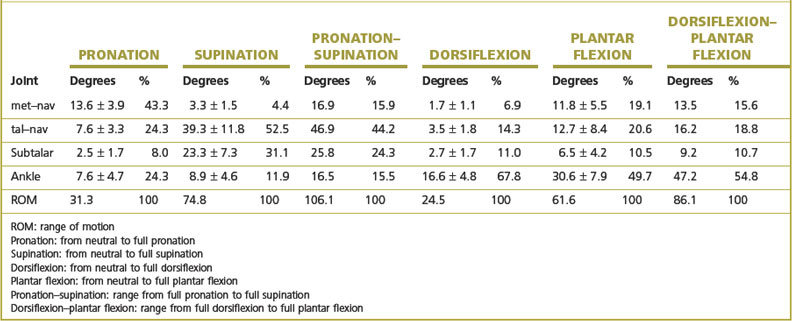
Using 13 cadaver specimens (mean age 65 years, range 20–89 years) and a magnetic tracking measurement system, Kitaoka et al (1997a) investigated the contribution of the ankle joint, subtalar joint, talonavicular joint and first metatarsal–navicular joint to pronation, supination, dorsiflexion and plantar flexion. The results are shown in Table 15.1. As expected, the ankle is the major contributor (47.2%) to the plantar flexion–dorsiflexion range of motion, but there are significant contributions from the other components. The subtalar joint is often regarded as the major contributor to the pronation–supination range of motion, but the results of the study indicate that the contribution of the subtalar joint (24.3%) is less than that of the talonavicular joint (44.2%).
Table 15.1 Contribution of movement between the navicular and first metatarsal (met–nav) and movement of the ankle, subtalar and talonavicular joints to pronation, supination, dorsiflexion and plantar flexion (adapted from Kitaoka et al 1997a)
The movements of supination and pronation as described above refer to movements of the rearfoot complex when the foot is not weight bearing. When the foot is weight bearing, these movements are constrained, depending on the magnitude and distribution of the ground reaction force acting on the plantar part of the foot. Under weight-bearing conditions the most noticeable movements of the foot occur about an anteroposterior axis through the foot (similar to inversion and eversion). For this reason, in describing the movement of the foot under weight-bearing conditions the terms supination and inversion are sometimes used synonymously, as are the terms pronation and eversion. However, the actual movements of the foot under weight-bearing conditions are modifications of supination and pronation and, as such, involve simultaneous triplanar movement in all the joints of the rearfoot complex.
ARCHES OF THE FEET
The tarsals and metatarsals are arranged in the form of two longitudinal arches (medial and lateral) and a single transverse arch. The medial longitudinal arch is formed by the calcaneus, talus, navicular, the three cuneiforms, and the first, second and third metatarsals. The lateral longitudinal arch, which is much flatter than the medial arch, is formed by the calcaneus, cuboid, and the fourth and fifth metatarsals. In combination, the longitudinal arches form a single arched structure between the posterior inferior aspect of the calcaneus and the heads of the metatarsals. The transverse arch runs across the foot from medial to lateral and is formed by the anterior five tarsals and the bases of the metatarsals. The shape of the arch is due to the cuboid, the lateral and middle cuneiforms, and the bases of the middle three metatarsals, which are wedge shaped inferiorly in coronal section.
The arched shape of the foot is maintained by ligaments (passive support) and muscles (active support). Although the ligaments and muscles are not very elastic, they are sufficiently so to enable the arches to flatten slightly following contact of the foot with the ground, such as following heel-strike in walking or running, and then recoil (restore their normal shape) following the impact. Consequently, the arches function like springs in order to help cushion impacts with the ground.
Passive arch support
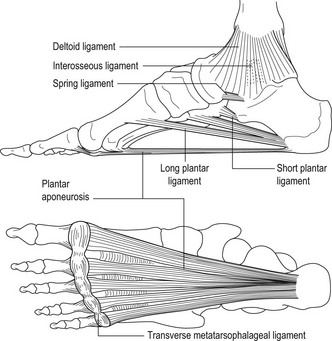
The ligaments on the plantar aspect of the foot are very strong and can normally maintain the arches of the foot in upright posture in the absence of assistance from muscles (Hicks 1961, Kitaoka et al 1997b). The main ligaments that support the arches of the foot are:
Mechanically, the plantar ligaments support the arches of the feet in two ways, as a beam and as a true arch (or truss) (Hicks 1961). Figure 15.8A shows the type of strain experienced by a loaded beam, i.e. compression strain on the upper surface and tension strain on the lower surface. This is similar to the strain on the tarsals and metatarsals imposed by the type of arch support provided by the long plantar ligament, short plantar ligament, spring ligament, interosseous talocalcanean ligament and deltoid ligament (Fig. 15.6 and Fig. 15.8B). The strain on a true arch is different to that on a beam. In a true arch the ends of the arch must move further apart if it is to become flatter and the strain on the segments of a true arch is basically compression between the segments (Fig. 15.8C). This is similar to the strain on the tarsals and metatarsals imposed by the type of arch support provided by the plantar aponeurosis (Fig. 15.6 and Fig. 15.8D).
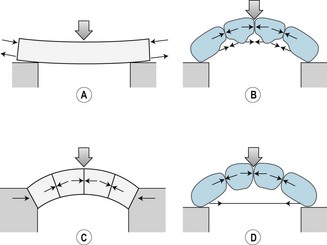
Figure 15.8 Beam and arch support mechanisms. (A) Strain on a horizontal beam when vertically loaded. (B) Strain on the bones of the foot and beam support mechanism when the foot is vertically loaded. (C) Strain on the components of a true arch when vertically loaded. (D) Strain on the bones of the foot and true arch support mechanism when the foot is vertically loaded.
Active arch support
The passive ligamentous beam and true arch support mechanisms are normally assisted by the muscles of the lower leg and foot. In relation to arch support, muscles that are located entirely (have their origins and insertions) within the foot are referred to as intrinsic muscles. Muscles that have their origins in the lower leg and insertions in the foot (i.e. cross the ankle joint) are referred to as extrinsic muscles.
The effect that a particular muscle has on the arches (i.e. tendency to raise or flatten) depends on the tendency of the muscle to:
On the basis of these criteria, Hicks (1961) classified all the intrinsic and extrinsic muscles into four groups:
Interaction of the arch support mechanisms
Whereas it is generally accepted that the passive (beam and true arch) and active (muscle) mechanisms both contribute significantly to arch support (Norkin & Levangie 1992), the relative contribution of the mechanisms in different weight-bearing activities has yet to be determined. This lack of information reflects the difficulty of measuring the forces in the ligaments and forces in vivo. Most studies of the arch support mechanisms have been based on cadavers. For example, Kitaoka et al (1997b) investigated the role of the plantar ligaments in the stability of the longitudinal arches of the feet under normal loading (upright standing posture) using 19 cadaver specimens (mean age 71 years, range 20–89 years). It was found that sectioning all the main plantar ligaments (long plantar ligament, short plantar ligament, spring ligament, interosseous talocalcanean ligament, plantar aponeurosis, deltoid ligament) resulted in complete collapse of the longitudinal arch. The arch did not collapse after sectioning any single ligament, but progressive collapse did occur when the ligaments were sectioned consecutively. The effect of sectioning individual ligaments on the degree of arch collapse (reflected in dorsiflexion of the intertarsal and tarsometatarsal joints) varied considerably between specimens, which suggested that the contribution of each ligament to arch stability varies between individuals. This is, perhaps, not surprising considering the variation in the size, shape and alignment of the bones of the feet in normal healthy individuals (Åström & Arvidson 1995).
Whereas cadaver studies provide useful information on the passive arch support mechanisms, they do not provide information about the contribution of active support mechanisms or the relative contribution of the passive and active mechanisms. Research is clearly needed in this area.
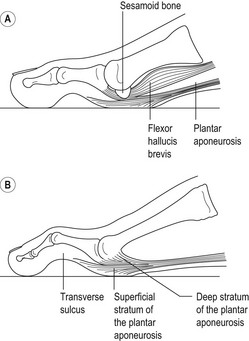
THE WINDLASS MECHANISM OF THE FOOT
As described earlier, the plantar aponeurosis spans the whole of the tarsus and metatarsus by linking the inferior aspect of the calcaneus with the plantar surfaces of the bases of the proximal phalanges of the toes (Fig. 15.6). Consequently, extension of the metatarsophalangeal joints winds the plantar aponeurosis around the heads of the metatarsals, like a cable being wound around a windlass, which simultaneously raises the longitudinal arch (Fig. 15.9). This action is referred to as the windlass mechanism of the foot (Hicks 1954). Flexion of the metatarsophalangeal joints unwinds the plantar aponeurosis and lowers the longitudinal arch; this action is referred to as the reverse windlass (Aquino & Payne 2000).
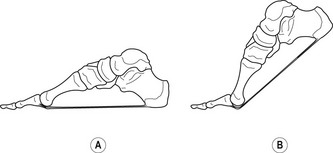
Figure 15.9 The windlass effect of the plantar aponeurosis resulting from dorsiflexion of the metatarsophalangeal joints.
The reverse windlass action is a feature of the loading phase (from heel-strike to foot-flat) and much of the single-support phase in gait. During this period, the rearfoot complex normally pronates, which unwinds the plantar aponeurosis and lowers the longitudinal arch. This movement is associated with extension of the midtarsal joint, which is sometimes referred to as ‘unlocking’ the midtarsal joint (Blackwood et al 2005, Sobel et al 1999). In the foot-flat position the tension in the plantar aponeurosis exerts a flexor moment on the proximal phalanges (pushes the pads of the toes against the ground), which extends the length of the base of support and, consequently, reduces the pressure on the plantar surfaces of the heads of the metatarsals. In addition, the tension in the plantar aponeurosis, in association with tension in the intrinsic muscles, prevents excessive flattening of the longitudinal and transverse arches and provides a stable base of support.
The windlass action is a feature of the push-off in gait (from heel-off to just before toe-off). During this period, the rearfoot complex normally supinates in association with extension of the metatarsophalangeal joints (Fig. 15.9B). These actions raise the longitudinal arch, which stabilises the foot and provides a firm base of support for the push-off. The windlass movement is associated with flexion of the midtarsal joint, which is sometimes referred to as ‘locking’ the midtarsal joint (Blackwood et al 2005, Sobel et al 1999).
The windlass action during push-off in gait is most effective (rapid initiation and completion of arch raise) when the leverage of the plantar aponeurosis is maximum. This occurs when (i) the sesamoids are located in their normal position beneath the head of the first metatarsal (Fig. 15.7A) and (ii) the long axes of the first metatarsal and phalanges of the hallux are more or less in line (Fig. 15.10A). Not surprisingly, this would appear to be the normal orientation of the sesamoid bones and first metatarsophalangeal joint, as significant non-alignment of the first metatarsal and proximal phalanx seems to be rare in children (Kilmartin 1991).
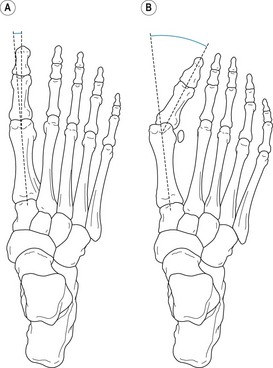
Figure 15.10 (A) Superior aspect of the right foot with a hallux abductus angle of approximately 5°. (B) Superior aspect of the right foot with a hallux abductus angle of approximately 35°.
With increase in age, many people develop hallux valgus, also referred to as hallux abducto valgus (Thomas & Barrington 2003). Hallux valgus is a complex progressive condition that is characterised by lateral deviation (valgus abduction) of the hallux and medial deviation of the first metatarsophalangeal joint (Fig. 15.10B). Unless treated, hallux valgus results in a progressive increase in the hallux abductus angle (i.e. the angle between the long axes of the first metatarsal and proximal phalanx) (Fig. 15.10B). When the hallux abductus angle is less than 15°, the condition tends to be asymptomatic. However, increases in the hallux abductus angle above 15° tend to be associated with increasing pain and discomfort around the first metatarsophalangeal joint (Easley & Trnka 2007, Menz & Lord 2005).
Relative to the first metatarsophalangeal joint, any increase in the hallux abductus angle will tend to displace laterally the lines of action of the plantar aponeurosis and tendons of the intrinsic and extrinsic muscles that cross over the first metatarsophalangeal joint from the metatarsal to the hallux. Consequently, the sesamoid bones will also be displaced laterally relative to the first metatarsophalangeal joint, resulting in subluxation of the joints between the sesamoid bones and the head of the first metatarsal (Fig. 15.10B). Subluxation of these joints will decrease the leverage of the windlass about the first metatarsophalangeal joint and, consequently, tend to result in increased force in the muscles supporting the arches during push-off in order to compensate for the loss in leverage of the windlass. The increased muscle force will tend to increase the hallux abductus angle and, consequently, increase (i) the pressure on the articular surfaces between the medial sesamoid and the head of the first metatarsal, (ii) the strain on the intertransverse ligament and metatarsophalangeal ligament between the first and second metatarsophalangeal joints, and (iii) the pressure exerted by the shoe on the medial aspect of the first metatarsophalangeal joint (Tanaka et al 1997). This pattern of loading, if prolonged, is likely to result in discomfort, pain, inefficient gait, impaired balance and an increased risk of falling, especially in the elderly (Menz & Lord 2005).
STRUCTURAL ADAPTATION OF THE MUSCULOSKELETAL SYSTEM
In any body position other than the relaxed recumbent position, the musculoskeletal system is likely to be subjected to considerable loading. In response to the forces exerted on them, the musculoskeletal components experience strain (i.e. they are deformed to a certain extent), and the greater the force, the greater the strain. Under normal circumstances the musculoskeletal components adapt their external form (size and shape) and internal architecture (structure) to the time-averaged forces exerted on them in order to more readily withstand the strain (Carter et al 1991). However, when the degree of strain experienced by a particular component exceeds its strength, it becomes injured. Consequently, there is an intimate relationship between the structure and function of the musculoskeletal system (Watkins 1999).
Structural adaptation in bone
The last 30 years have produced much of the present knowledge concerning the adaptation of musculoskeletal components to changes in time-averaged load (Frost 1988a,b, 1990). However, the fundamental concepts concerning the adaptation of bone were established over 100 years ago (Gross & Bain 1993). In 1892, Julius Wolff (1836–1902) summarised the contemporary views of bone adaptation to changes in time-averaged load in what came to be known as Wolff’s law (Wolff 1988). Wolff’s law, which has been shown to be more or less correct, hypothesised that bone adapts its external form and internal architecture to the time-averaged load exerted on it in an ordered and predictable manner to provide optimal strength with minimal bone mass.
The adaptation of bone to time-averaged load is referred to as ‘modelling’. In normal growth and development, modelling has been estimated to account for 20–50% of the dimensions of mature bones (Frost 1988b). Some of the load experienced by bone is due to the weight of body segments. However, this source of loading is small relative to the loads exerted by muscles (Schoenau & Frost 2002, Watkins 1999). From birth to maturity, bone has the capacity to model external form and internal architecture. However, the capacity to model external form gradually decreases and virtually ceases at maturity. The capacity to model internal architecture also decreases with age, but is retained to some extent throughout life. In general, bone adapts to changes in time-averaged loads by increasing or decreasing bone mass to maintain an optimum strain environment. In bone, the optimum strain environment is characterised by minimal flexure (or bending) strain and an even distribution of stress (usually compression stress) across articular areas. An even distribution of stress across articular areas is maintained by modelling in accordance with the phenomenon of chondral modelling (Frost 1973).
The chondral modelling phenomenon
All bones that develop from hyaline cartilage via endochondral ossification experience chondral modelling, i.e. the rate and amount of new bone formed by hyaline cartilage depends on the amount and form of load exerted on it. Chondral modelling applies to articular cartilage, epiphyseal plates, insertions of tendons and ligaments, apophyseal plates, end plates in symphysis joints, and sesamoid bones (Frost 1979).
In a long bone the size and shape of the epiphyses and metaphyses, and consequently the orientation of the epiphyses of a bone to its shaft, are determined by chondral modelling in articular cartilage and epiphyseal plates. When a synovial joint is maximally congruent, the loading on articular cartilage and epiphyseal plates tends to be evenly distributed. Incongruence results in an unequal distribution of load across articular cartilage and epiphyseal plates. If prolonged, such unequal loading results in modelling to restore maximal congruence. However, the actual changes that occur depend on the extent of the changes in the patterns of loading on the articular cartilage and epiphyseal plates. If the changes in loading remain within the normal range, then a negative-feedback mode of modelling is invoked, resulting in restoration of normal congruence with normal or slightly abnormal alignment of the bones. However, if the changes in loading are outside the normal range, then a positive-feedback mode of modelling is invoked, which aggravates the condition, resulting in progressively worsening malalignment.
Modelling of metaphyses and epiphyses
A functionally normal joint is a congruent joint that transmits loads across the articulating surfaces in a normal manner. An anatomical malalignment at the knee, or any other joint, will be functionally normal if the malalignment stabilises (does not get progressively worse). In these cases, the anatomical malalignments represent normal modelling in response to abnormal patterns of loading. The skeletal adaptations ensure normal transmission of loads across the joints. Figure 15.11 illustrates the effect of negative feedback in relation to abductor–adductor muscle imbalance at the knee. Figure 15.11A represents a knee with normal balance between the abductor and adductor muscles (i.e. the resultant horizontal force at the knee is zero). This situation is associated with normal alignment between the femur and tibia and an even distribution of load across the articular surfaces and epiphyseal plates (Fig. 15.11B). Figure 15.11C shows the same knee with an abductor–adductor imbalance such that there is a net medially directed horizontal force at the knee tending to increase the degree of genu valgum. Figure 15.11D shows the unequal pattern of loading on the articular surfaces and epiphyseal plates associated with the muscle imbalance. Assuming that the unequal loading is within the normal range, the negative-feedback mode is invoked. The rate of growth of the lateral aspects of the epiphyses and metaphyses is increased and the rate of growth of the medial aspects of the epiphyses and metaphyses is decreased such that normal congruence is restored (with net zero horizontal force at the knee) at the expense of an abnormal alignment between the femur and tibia (i.e. much reduced genu valgum or even slight genu varum relative to most individuals) (Fig. 15.11E,F).
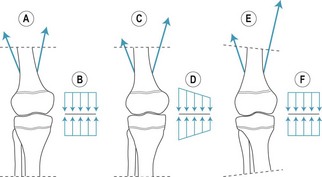
Figure 15.11 Modelling of metaphyses and epiphyses: effect of negative-feedback mode in relation to an abductor–adductor imbalance at the knee.
Whether or not a particular joint is anatomically malaligned during childhood, the only time when it may become painful (excluding injuries and pathological conditions not due to loading) is during adulthood, when the bones are no longer capable of modelling in response to abnormal loading. In most adults, abnormal patterns of loading are the result of an increasingly sedentary lifestyle in which body weight gradually increases and muscle strength gradually decreases.
Modelling of articular surfaces
Minor incongruences between articular surfaces in synovial joints tend to result in large changes in the compression stress experienced by different parts of the articular surfaces (Calhoun et al 1994). This is especially the case in joints with pulley-shaped articular surfaces such as the ankle joint (Fig. 15.12). Under normal circumstances, the subtalar joint contributes to inversion and eversion of the foot (Fig. 15.12A,B). However, if movement at the joint is absent or limited, inversion and eversion of the foot twists the talus in the tibiofibular mortise, resulting in excessive compression stress on those parts of the articular surfaces that remain in contact (Fig. 15.12C). The excessive loading on the impinging areas reduces or halts growth in these areas, while growth of the unloaded areas proceeds at the normal rate. Consequently, the shapes of the articular surfaces adapt to the abnormal loading conditions by forming a rounded surface in the coronal plane rather than a pulley-shaped surface, and the ankle joint as a whole resembles a ball and socket joint rather than a hinge joint (Fig. 15.12D) (Frost 1979).
Anwar R, Anjum SN, Nicholl JE. Sesamoids of the foot. Current Orthopaedics. 2005;19:40-48.
Aquino A, Payne C. The role of the reverse windlass mechanism in foot pathology. Australasian Journal of Podiatric Medicine. 2000;34(1):32-34.
Åström M, Arvidson T. Alignment and joint motion in the normal foot. Journal of Sports Physical Therapy. 1995;22(5):216-222.
Blackwood CB, Yuen TJ, Sangeorzan BJ, Ledoux WR. The midtarsal joint locking mechanism. Foot and Ankle International. 2005;26(12):1074-1080.
Briggs PJ. The structure and function of the foot in relation to injury. Current Orthopaedics. 2005;19:85-93.
Bowden PD, Bowker P. The alignment of the rearfoot complex axis as a factor in the development of running induced patellofemoral pain. Journal of British Podiatric Medicine. 1995;50:114-118.
Calhoun JH, Li F, Ledbetter BR, Viegas SF. A comprehensive study of pressure distribution in the ankle joint with inversion and eversion. Foot and Ankle International. 1994;15:125-133.
Carter DR, Wong M, Orr TE. Musculoskeletal ontogeny, phylogeny, and functional adaptation. Journal of Biomechanics. 1991;24(Suppl 1):3-16.
Czerniecki JM. Foot and ankle biomechanics in walking and running: a review. American Journal of Physical Medicine and Rehabilitation. 1988;67:246-252.
Downing BS, Klein BS, D’Amico JS. The axis of motion of the rearfoot complex. Journal of the American Podiatric Association. 1978;68:484-499.
Easley ME, Trnka H-J. Current concepts review: hallux valgus part 1: pathomechanics, clinical assessment, and nonoperative management. Foot and Ankle International. 2007;28(5):654-659.
Frost HM. Orthopedic biomechanics. Vol. 5. Charles C Thomas. Springfield, IL. 1973
Frost HM. A chondral modelling theory. Calcified Tissue International. 1979;28:181-200.
Frost HM. Structural adaptations to mechanical usage: a proposed three-way rule for bone modelling. Part I. Veterinary and Comparative Orthopaedics and Traumatology. 1988;1:7-17.
Frost HM. Structural adaptations to mechanical usage: a proposed three-way rule for bone modelling. Part II. Veterinary and Comparative Orthopaedics and Traumatology. 1988;2:80-85.
Frost HM. Skeletal structural adaptations to mechanical usage: four mechanical influences on intact fibrous tissues. The Anatomical Record. 1990;226:433-439.
Gross TS, Bain ST. Skeletal adaptation to functional stimuli. In: Grabiner MD, editor. Current issues in biomechanics. Champaign, IL: Human Kinetics Corp, 1993.
Hicks JH. The mechanics of the foot. II. The plantar aponeurosis and the arch. Journal of Anatomy. 1954;88(1):25-31.
Hicks JH. The three weight-bearing mechanisms of the foot. In: Evans FG, editor. Biomechanical studies of the musculoskeletal system. Springfield, IL: Charles C. Thomas, 1961.
Inman VT. Joints of the ankle. Baltimore, OH: Williams & Wilkins; 1976.
Kilmartin TE, Barrington RL, Wallace AW. Metatarsus primus varus, a statistical study. Journal of Bone and Joint Surgery. 1991;73B(6):937-940.
Kitaoka HB, Luo ZP, An K-N. Three-dimensional analysis of normal ankle and foot mobility. American Journal of Sports Medicine. 1997;25(2):238-242.
Kitaoka HB, Ahn T-K, Luo ZP, An K-N. Stability of the arch of the foot. Foot and Ankle International. 1997;18(10):644-648.
Menz HB, Lord SR. Gait instability in older people with hallux valgus. Foot and Ankle International. 2005;26(6):483-489.
Nester CJ. Rearfoot complex: a review of its interdependent components, axis orientation and functional model. The Foot. 1997;7:86-96.
Norkin CC, Levangie PK. Joint structure and function: a comprehensive analysis. Philadelphia: F.A Davis Company; 1992.
Peat M. Functional anatomy of the shoulder. Physical Therapy. 1986;66:1855-1865.
Roberts TDM. Understanding balance: the mechanics of posture and locomotion. London: Chapman and Hall; 1995.
Schoenau E, Frost HM. The ‘muscle–bone unit’ in children and adolescents. Calcified Tissue International. 2002;70:405-407.
Singh AK, Starkweather KD, Hollister AM, et al. Kinematics of the ankle: a hinge axis model. Foot and Ankle. 1992;13(8):439-446.
Sobel E, Levitz SJ, Caselli MA. Orthoses in the treatment of rearfoot problems. Journal of the American Podiatric Medical Association. 1999;89(5):220-233.
Tanaka Y, Takakura Y, Takaoka T, et al. Radiographic analysis of hallux valgus in women on weightbearing and nonweightbearing. Clinical Orthopaedics and Related Research. 1997;336:186-194.
Thomas S, Barrington R. Hallux valgus. Current Orthopaedics. 2003;17:299-307.
Valmassy RL. Clinical biomechanics of the lower extremity. St Louis, MI: CV Mosby; 1996.
Watkins J. Structure and function of the musculoskeletal system. Champaign, IL: Human Kinetics Corp; 1999.
Williams PL, Bannister LH, Berry MM, et al, editors. Gray’s anatomy. Edinburgh: Longman, 1995.
Wolff J. The law of bone modelling (trans. Maquet P, Furlong R). New York: Springer Verlag; 1988. [Originally published as: Wolff J 1892 Das gesetz der transformation der knochen. A. Hirschwald, Berlin.]