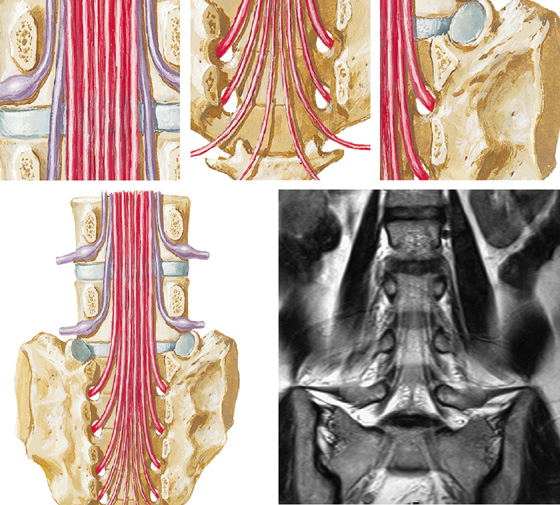
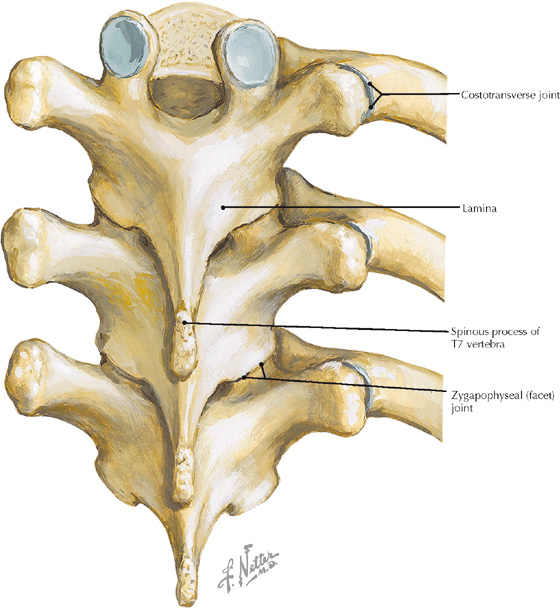
Posterior view of the thoracic spine (Atlas of Human Anatomy, 5th edition, Plate 151)
Volume rendered display, thoracic spine CT
• The thoracic region of the vertebral column is the least mobile because of thin intervertebral disks, overlapping spinous processes, and the presence of ribs. This minimizes the potential for disruption of respiratory processes and maximizes stability of the thoracic spine.
• The normal thoracic curvature (kyphosis) is due almost entirely to the bony configuration of the vertebrae, whereas in the cervical and lumbar regions thicker disks also contribute to the respective curvatures in these regions.
• The overlapping of angled osseous structures of the thoracic spine’s posterior elements and costovertebral junctions may result in confusion pertaining to bone changes caused by trauma or tumors on radiographs or cross-sectional images. Volume rendered displays can, in such cases, provide anatomic clarity not easily perceived on other image displays.
Clinical Note
Excessive kyphosis is an abnormal increase in the thoracic curvature. This occurs frequently in osteoporotic women who develop anterior wedging–type compression fractures of thoracic vertebrae.
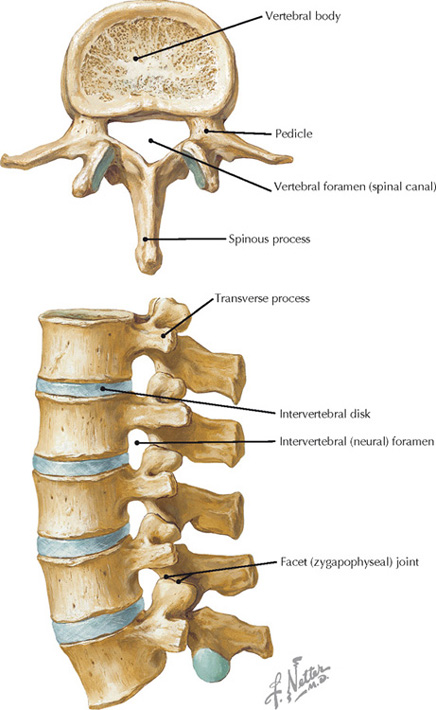
Superior and lateral views of lumbar vertebrae (Atlas of Human Anatomy, 5th edition, Plate 152)
Volume rendered display, lumbar spine CT
• Spondylolisthesis refers to the anterior displacement of a vertebra in relation to the inferior vertebra; it is most commonly found at L5/S1because of a defect or non-united fracture at the pars interarticularis (the segment of the vertebral arch between the superior and inferior facets).
• There are typically five lumbar vertebrae, but the fifth lumbar may become fused with the sacrum (sacralization of L5) or the first sacral vertebrae may not be fused with the remaining sacral vertebrae (lumbarization of S1).
Clinical Note
Lumbar spinal stenosis may be congenital or acquired. Symptoms include pain, numbness, or weakness in the lower back or lower limbs; the symptoms may be temporally variable and are often worse after prolonged standing or walking.
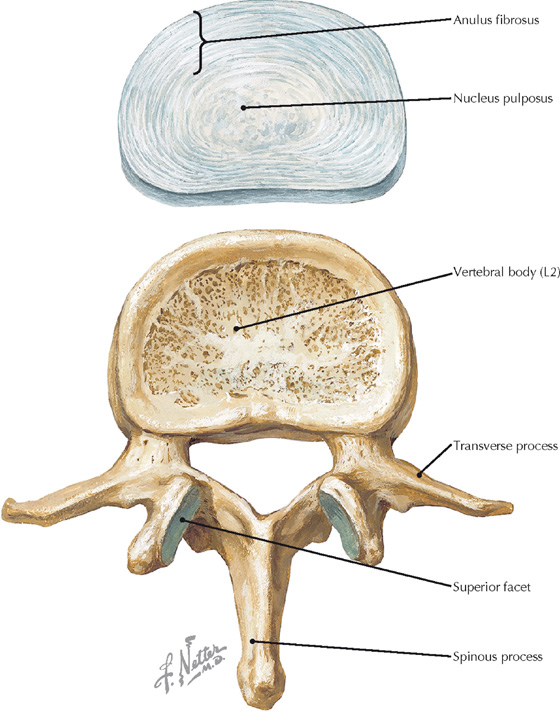
Structure of a lumbar vertebra and intervertebral disk (Atlas of Human Anatomy, 5th edition, Plate 152)
Oblique axial view tangent to the intervertebral disk, post-diskography CT (red lines in the reference images indicate the position and orientation of the main image)
• Contrast material that had been injected into the nucleus pulposus has extravasated through a tear in the anulus fibrosus in this CT scan.
• Note that the main (axial) section shows the spinous process, lamina, and inferior facets of the vertebra above and the superior facets of the segment below.
• The vertebral arch is composed of the two (right and left) pedicles and lamina.
Clinical Note
Degenerative disk disease is associated with dehydration of the nucleus pulposus, which typically occurs with aging.
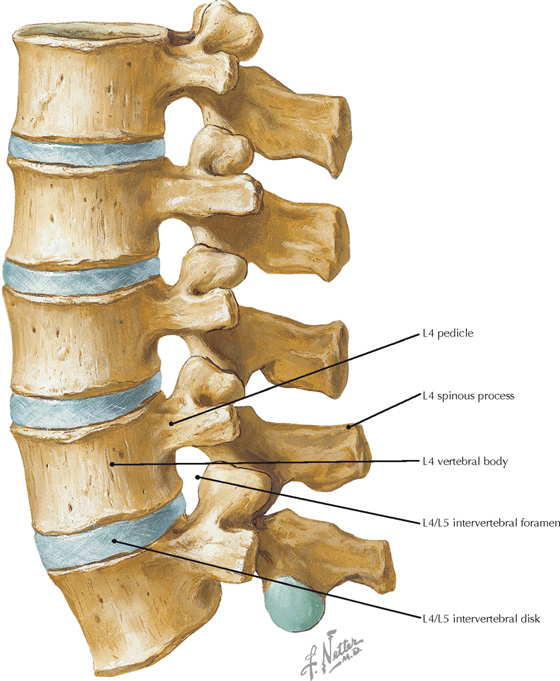
Sagittal view of the lumbar vertebral column (Atlas of Human Anatomy, 5th edition, Plate 152)
Multiplanar reconstructions, lumbar CT
• The parasagittal CT image is at the level of the blue lines in the coronal and axial views. The axial section is at the level indicated by the red line. The coronal reconstruction is at the level of the green line.
• It is clinically important that the lumbar intervertebral foramina (also called neuroforamina or nerve root canals) extend superior to the associated disk. Herniated L4/5 disk fragments that extend upward and laterally may impinge on the exiting L4 root within the L4/5 intervertebral foramen, whereas herniation of an L4/5 disk fragment posteriorly may impinge on the L5 nerve root.
Clinical Note
Vertebral bodies are most frequently fractured by excessive flexion (compression) forces, whereas the vertebral arches tend to fracture when the vertebral column is excessively extended.
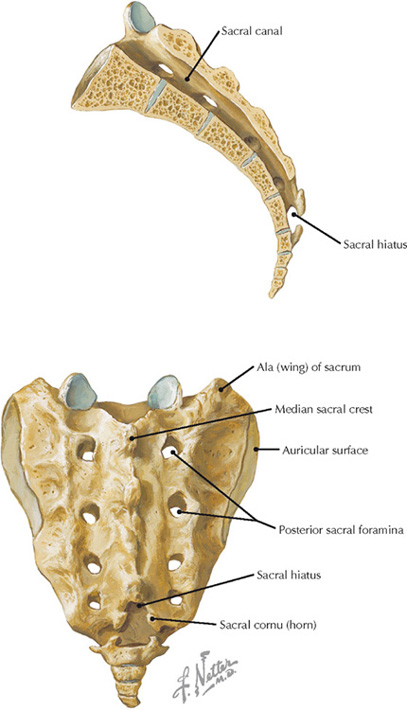
Midsagittal and posterior views of the sacrum (Atlas of Human Anatomy, 5th edition, Plate 154)
Volume rendered display, lumbosacral CT
• The division of spinal nerves into dorsal and ventral rami occurs within the sacral canal so that the primary rami exit the sacrum via the anterior and posterior sacral foramina.
• The auricular surface of the sacrum is for articulation with the ilium forming the complicated sacroiliac joint (SIJ). Arthritis in this joint may be a source of lumbago.
• In osteoporotic patients, the sacrum is less able to resist the shearing force associated with the transfer of upper body weight to the pelvis; this may result in a vertical “insufficiency” fracture.
Clinical Note
A caudal epidural block, often used during parturition, is administered by inserting an indwelling catheter into the sacral hiatus to release an anesthetic agent that eliminates sensation primarily from the S2-S4 spinal nerves. These nerves carry sensations from the uterine cervix, vagina, and perineum.
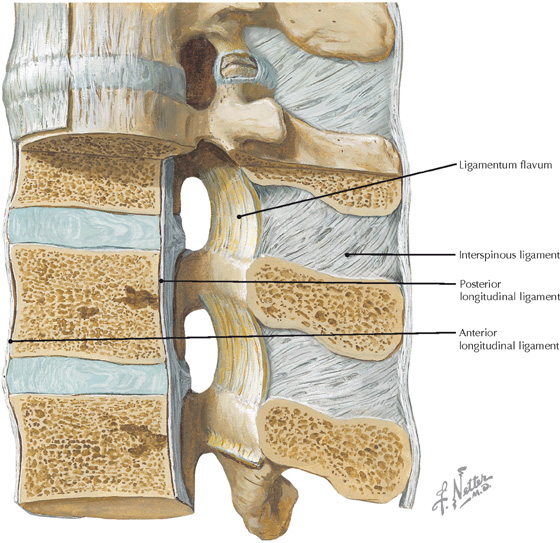
Vertebral ligaments in the lumbar region (Atlas of Human Anatomy, 5th edition, Plate 156)
Sagittal T2 MR image of the thoracolumbar spine
• The anterior longitudinal ligament tends to limit extension of the vertebral column, whereas the posterior ligament tends to limit flexion.
• Herniation of intervertebral disks at the thoracic/lumbar junction is common because the thoracic region of the spine is relatively immobile compared to the lumbar and cervical regions.
Clinical Note
The posterior longitudinal ligament is well innervated with nociceptive fibers and is thought to be the origin of some of the pain associated with intervertebral disk herniation.
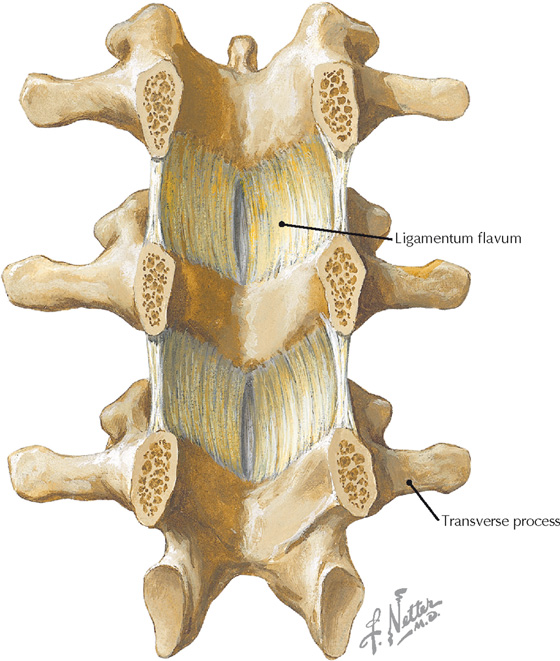
Anterior view of posterior vertebral arch (Atlas of Human Anatomy, 5th edition, Plate 156)
Sagittal T2 MR image of thoracic spine, just off midline
• The ligamentum flavum contains elastic tissue that prevents the ligament from being pinched between the lamina when the vertebral column is hyperextended.
• Anesthesiologists use penetration of the ligamentum flavum as an indicator that the needle has reached the epidural space for epidural anesthesia.
Clinical Note
In addition to posterior disk bulging and hypertrophic arthritic facet joints, thickening of the ligamentum flavum is often a major component of degenerative spinal canal stenosis. Symptoms of spinal stenosis are usually worse in extension and improved in flexion, presumably because of infolding of the ligament in extension and stretching out and thinning of the ligament in flexion.
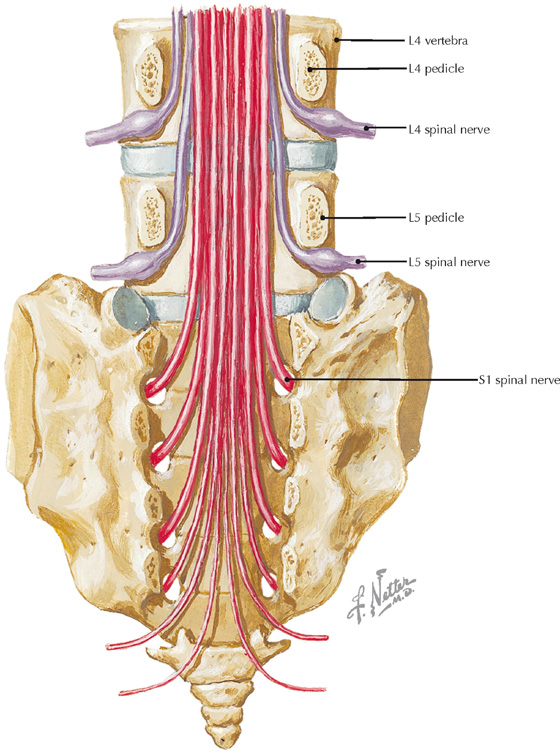
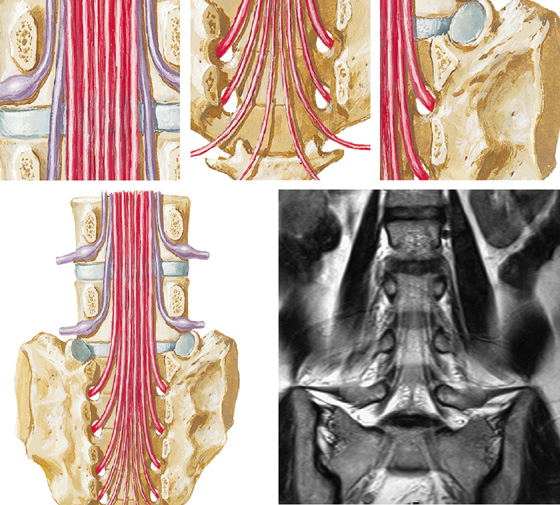
Relationship between the lower spinal nerves and their respective neuroforamina (intervertebral foramina) (Atlas of Human Anatomy, 5th edition, Plate 158)
Coronal T2 MR image of the lower spine
• The L4 spinal nerve passes caudal to the L4 pedicle to exit the spinal canal through the L4/L5 neuroforamen (intervertebral foramen).
• Similarly, the L5 nerve passes caudal to the L5 pedicle to exit the spinal canal through the L5/S1 neuroforamen.
• Coronal MR images may clearly show disk fragments that have herniated laterally and how they potentially affect nerve roots within or lateral to the neuroforamen.
Clinical Note
Lower lumbar disk herniation may produce sciatica, which is pain along the path of the sciatic nerve. This occurs because the sciatic nerve consists of components from L4-S2 spinal segments.
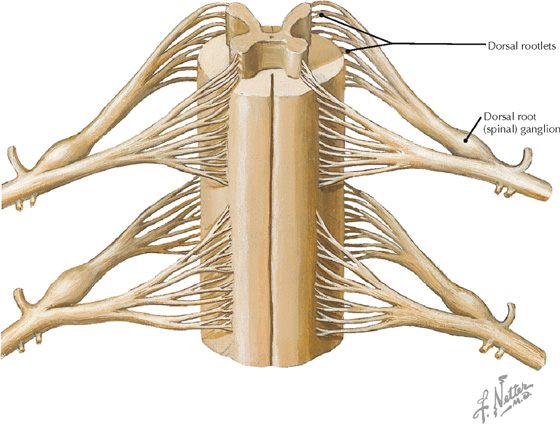
Anterior view of spinal cord showing nerve roots (Atlas of Human Anatomy, 5th edition, Plate 162)
Curved coronal reconstruction at the level of the posterior rootlets, CT cervical myelogram (curved green line in the reference axial image shows the plane of section for the coronal image)
• In this CT image the rootlets of the dorsal roots are represented by the delicate black inclined lines; the gray material represents opacified (contrast-enhanced) cerebrospinal fluid (CSF) within the subarachnoid space. The CSF was opacified by an intradural injection of iodinated contrast material that was injected with a very fine needle during a simple outpatient procedure.
• For patients who cannot undergo MRI—for example, those with a pacemaker—CT myelography is an alternative imaging procedure that is capable of showing very delicate anatomy (e.g., spinal nerve rootlets).
Clinical Note
The dorsal root (spinal) ganglia contain the cell bodies of the sensory neurons entering the spinal cord at a particular level. These cell bodies may be specifically targeted in certain disease states (e.g., herpes zoster infection, “shingles”) resulting in a sensory neuropathy.
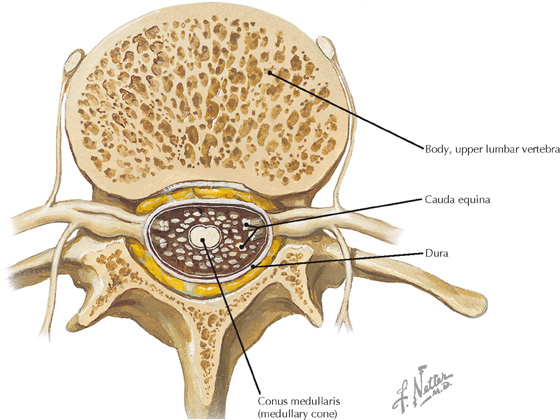
Axial section through an upper lumbar vertebra (Atlas of Human Anatomy, 5th edition, Plate 163)
A, Axial image from upper lumbar CT myelogram; B, Sagittal FS T2 MR image lumbar spine
• The conus medullaris may terminate as high as T12 or as low as L3.
• The cauda equina consists primarily of the spinal nerve roots that innervate the lower limb.
Clinical Note
Lumbar puncture to obtain cerebrospinal fluid (CSF) is done inferior to L3 because the conus medullaris typically terminates at L1/L2, allowing for needle penetration below this level with little risk of injury to the freely floating spinal nerve roots that are suspended in the lumbar cistern.
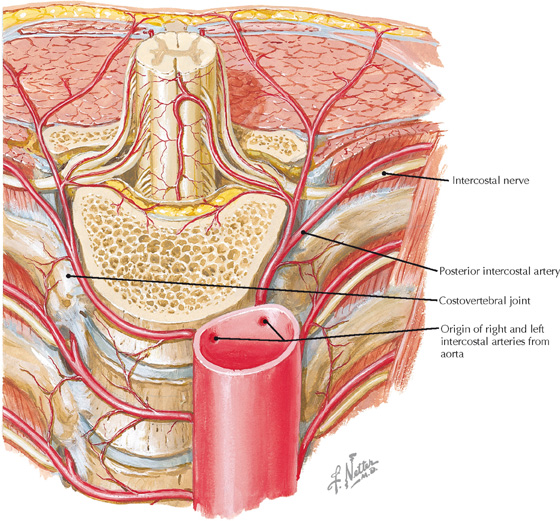
Posterior thoracic wall showing origin of posterior intercostal arteries (Atlas of Human Anatomy, 5th edition, Plate 165)
Curved coronal 10 mm slab, volume rendered display, CE CT of the chest
• The intercostal nerves and vessels traverse the potential space between the internal and innermost intercostal muscles.
• From superior to inferior the typical order of structures in an intercostal space is vein, artery, and nerve (VAN).
Clinical Note
The intercostal neurovascular bundle usually traverses the subcostal groove under the superior rib of the intercostal space. When a surgical incision or procedure (thoracotomy, thoracocentesis) is performed, the superior aspect of the intercostal space is avoided.
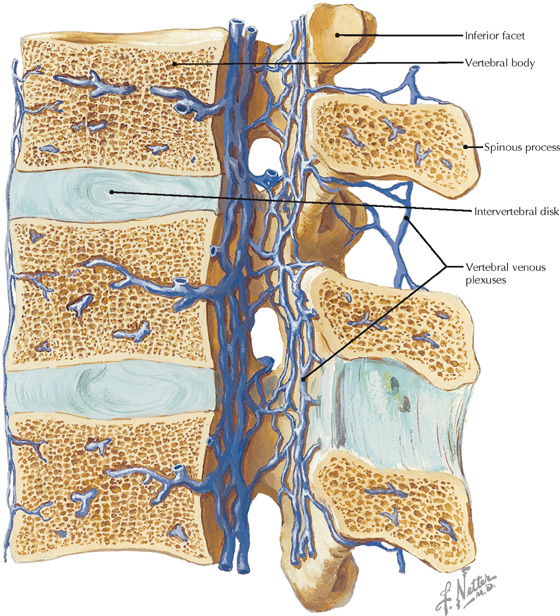
Veins of the spinal cord and vertebral column (Atlas of Human Anatomy, 5th edition, Plate 166)
Coronal CE FS T1 MR image of the posterior abdomen
• The internal (Batson’s) vertebral venous plexus is within the spinal canal whereas the external surrounds the vertebrae.
• The veins of these plexuses are valveless and connect to segmental intervertebral veins and to the cerebral venous sinuses.
Clinical Note
Dilation of the internal (Batson’s) venous plexus within the lumbar epidural space, associated with an epidural varix, can compress the thecal sac or nerve roots, causing lumbar radiculopathy.

Intermediate muscle layer of the back (Atlas of Human Anatomy, 5th edition, Plate 169)
Curved coronal reconstruction, CT lumbar spine
• Spasm in the erector spinae is associated with lumbago as the muscles spastically contract to reduce spinal movements.
• The erector spinae muscle group is entirely innervated by segmental dorsal rami.
• The three longitudinal components of the erector spinae (from lateral to medial) are the iliocostalis, longissimus, and spinalis.
Clinical Note
Disease or degenerative processes that result in the generation of abnormal activation patterns of the different components of the erector spinae can produce a functional scoliosis.
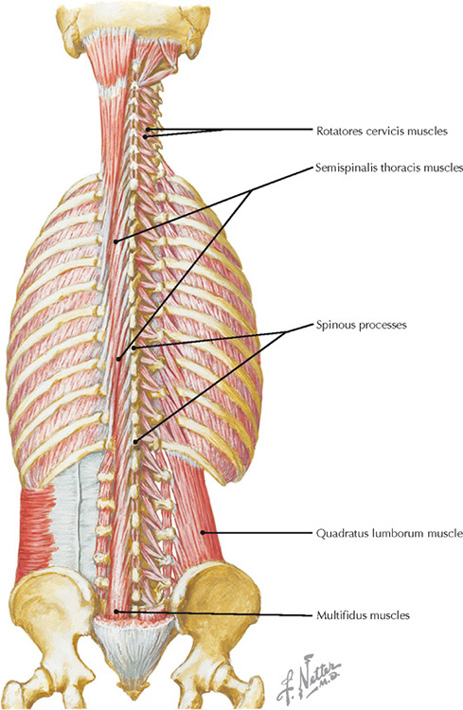
Multifidus, rotatores, and other deep back muscles (Atlas of Human Anatomy, 5th edition, Plate 170)
Coronal T1 MR image of the back
• The deep back muscles are primarily responsible for delicate adjustments between individual vertebrae that correlate with changes in posture.
• The three components of the transversospinalis muscle group are semispinalis, multifidus, and rotatores, but they are not equally developed in all regions (multifidus is best developed in the lumbar region).
• The deep back muscles are all innervated by segmental dorsal rami.
Clinical Note
Although often not considered important clinically, spasms in the deep back muscles (especially multifidus) may be associated with radiculopathy and pain.
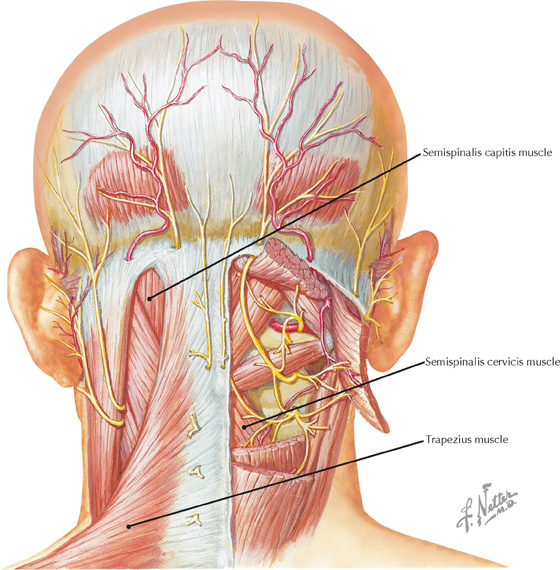
Superficial and deep muscles of the posterior neck (Atlas of Human Anatomy, 5th edition, Plate 172)
Curved coronal reconstruction, CT cervical spine
• The semispinalis capitis muscle forms the bulk of the muscle mass on either side of the nuchal furrow.
• The semispinalis capitis muscle extends and laterally flexes the neck.
Clinical Note
The insertion of the semispinal capitis is a reliable indicator of the location of the transverse sinus and thus can be used by neurosurgeons to avoid damaging this structure in surgical approaches to the posterior fossa and craniovertebral junction.
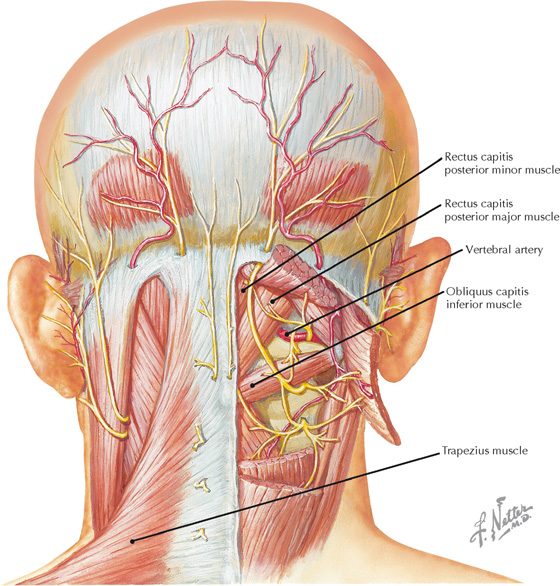
Superficial and deep muscles of the posterior neck (Atlas of Human Anatomy, 5th edition, Plate 172)
Curved 15 mm slab, volume rendered display, cervical spine CT
• The rectus posterior muscles function in lateral rotation and extension of the head.
• All the muscles of the suboccipital triangle are innervated by the suboccipital nerve (dorsal ramus of C1).
Clinical Note
The rectus posterior muscles may play a role in cervicogenic headaches via a dense fascial connection between these muscles and the cervical dura.
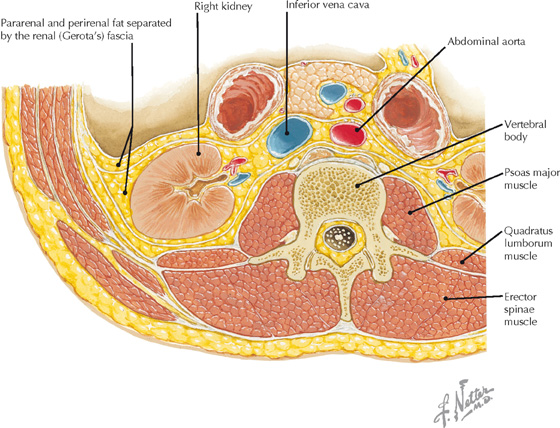
Cross section of back and posterior abdominal wall at L2 (Atlas of Human Anatomy, 5th edition, Plate 173)
Axial T1 MR image of the lumbar region
• Imbalanced patterns of erector spinae muscle activity and reduced trunk extension strength are associated with low back pain.
• Perirenal and pararenal fat is thought to act as a cushion that protects the kidney from injury.
• The diaphragm, psoas, quadratus lumborum, and transversus abdominis comprise the posterior relations of the kidney.
Clinical Note
Back pain may be cause by retroperitoneal disease. Occasionally, a lumbar spine MR image requested to evaluate back pain will reveal, for example, an abdominal aortic aneurysm or retroperitoneal adenopathy.