 CHAPTER 44 Burns
CHAPTER 44 Burns
ETIOLOGY
The pathophysiology of burn injury is caused by disruption of the three key functions of the skin: regulation of heat loss, preservation of body fluids, and barrier to infection. Burn injury releases inflammatory and vasoactive mediators resulting in increased capillary permeability, decreased plasma volume, and decreased cardiac output. For treatment of severe burns, admission to a qualified burn center is necessary. Burns usually are classified on the basis of four criteria:
EPIDEMIOLOGY
Nearly 1% (>400,000) of all children sustains a burn injury each year. More than 25,000 require hospitalization, and more than 400 children 1 to 14 years of age die as a result of their burns each year. Scald burns are most common, comprising up to 85% of burns in children. Flame burns account for another 13%. Boys are more likely to sustain a burn injury, with the highest rate of injury occurring in boys younger than 5 years of age.
Most fire-related childhood deaths and injuries occur in homes without working smoke detectors. Mortality is primarily associated with burn severity (extent of body surface area and depth), although the presence of inhalation injury and young age also predict mortality.
CLINICAL MANIFESTATIONS
The depth of injury should be assessed by the clinical appearance. First-degree burns are red, painful, and dry. Commonly seen with sun exposure or mild scald injuries, these burns involve injury to the epidermis only. They heal in 5 to 10 days without scarring and are not included in burn surface area calculations. Second-degree burns, or partial-thickness burns, involve portions of the dermis; some dermis remains viable. Healing is dependent on the uninjured dermis. Severe second-degree burns may take about a month to heal, and scarring results. Third-degree burns, or full-thickness burns, require grafts if they are more than 1 cm in diameter. They are avascular, lack sensation, and have a dry, leathery appearance. Fourth-degree burns involve underlying fascia, muscle, or bone. Inhalation injuries should be suspected if there are facial burns, singed nasal hairs, or carbonaceous sputum. Inhalation injuries may result in bronchospasm, airway inflammation, and impaired pulmonary function.
Burns can be classified as major or minor for treatment purposes. Major burns consist of those covering more than 15% of body surface area (>10% in infants), involving the face or perineum, or those involving inhalation injury. Second-degree and third-degree burns of the hands or feet and circumferential burns of the extremities also are classified as major. A method for estimating the percentage of skin surface area involved in burns in children of various ages is presented in Figure 44-1. The extent of skin involvement of older adolescent and adult patients is estimated as follows: each upper extremity, 9%; each lower extremity, 18%; anterior trunk, 18%; posterior trunk, 18%; head, 9%; and perineum, 1%.
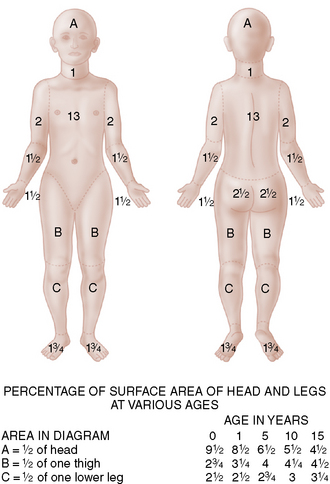
FIGURE 44-1 This chart of body areas, together with the table inserted in the figure showing the percentage of surface area of head and legs at various ages, can be used to estimate the surface area burned in a child.
(From Solomon JR: Pediatric burns. Crit Care Clin 1:159–174, 1985.)
The location of the burn is important in assessing the risk of disability. The risk is greatest when the face, eyes, ears, feet, perineum, or hands are involved. Inhalation injuries not only cause respiratory compromise but also may result in difficulty in eating and drinking.
LABORATORY AND IMAGING STUDIES
Initial laboratory testing, including complete blood count, type and crossmatch for blood, coagulation studies, basic chemistry profile, arterial blood gas, and chest radiograph, can be helpful for patients with major burns. A carboxyhemoglobin assessment should be performed for any suspected inhalation exposure (a house or closed-space fire or a burn victim who requires cardiopulmonary resuscitation). Cyanide levels should be considered in children who sustain smoke inhalation and have altered mental status. Unusual patterns of burns may increase suspicion of child abuse and result in appropriate evaluation to rule out nonaccidental trauma to the skeleton or central nervous system.
TREATMENT
The triage decision is based on:
Initial treatment should follow the ABCs of resuscitation. Airway management should include assessment for the presence of airway or inhalation injury. Smoke inhalation may be associated with carbon monoxide toxicity; 100% humidified oxygen should be given if hypoxia or inhalation is suspected. Hoarseness on vocalization also is consistent with a supraglottic injury. Some children with inhalation burns require endoscopy, an artificial airway, and mechanical ventilation.
The systemic capillary leak that occurs after a serious burn makes initial fluid and electrolyte support of a burned child crucial. The first priority is to support the circulating blood volume, which requires the administration of intravenous fluids to provide maintenance fluid and electrolyte requirements and to replace ongoing burn-related losses. No formula accurately predicts the fluid needs of every burn patient. Children with a significant burn should receive a rapid bolus of 20 mL/kg of lactated Ringer solution. The resuscitation formula for fluid therapy is determined by the percent of body surface burned. Total fluids are 2 to 4 mL/kg/percent burn/24 hour, with half the estimated burn requirement administered during the first 8 hours. (If resuscitation is delayed, half of the fluid replacement should be completed by the end of the eighth hour postinjury.) The goal of this fluid replacement is maintenance equal to or greater than 1 mL/kg/hour of urine output. Fluids should be titrated to accomplish this goal. Controversy exists over whether and when to administer colloid during fluid resuscitation. Colloid therapy may be needed for burns covering more than 30% of body surface area and may be provided after 24 hours of successful resuscitation with crystalloids.
Because burn injury produces a hypermetabolic response, children with significant burns require immediate nutritional support. Although enteral feeding may be resumed on day 2 or 3 of therapy, children with critical burn injury may require parenteral nutrition if unable to tolerate full enteral feeds. The hypermetabolic state can be modulated through the effective management of anxiety and pain as well as prevention of hypothermia by maintenance of a neutral thermal environment.
Wound care requires careful surgical management. Initial management includes relief of any pressure on peripheral circulation caused by eschar and débridement to allow classification of burns. Coverage with topical agents aids pain control and decreases insensible losses. Burns generally are covered with silver sulfadiazine (1%) applied to fine-mesh gauze or, if the burn is shallow, with polymyxin B/bacitracin/neomycin (Neosporin) ointment. Silver nitrate (0.5%) and 11.1% mafenide acetate (which is painful, produces metabolic acidosis, and penetrates eschar) are alternative antimicrobial agents. These agents inhibit but do not prevent bacterial growth. Various grafts, such as cadaver allografts, porcine xenografts, artificial bilaminate (cross-linked chondroitin-6-sulfate and silicone) skin substitute, and cultured patient’s keratinocytes, have been used initially to cover wounds. For full-thickness burns, skin autografting and artificial skin substitutes are required for eventual closure. Burn management and rehabilitation are highly specialized skills, involving the recognition of many complications of burns (Table 44-1) and evaluation of the wound and its cause for suspected child abuse or neglect. Tetanus toxoid should be provided for patients with incomplete immunization status; immune globulin is indicated in the nonimmunized patient.
TABLE 44-1 Complications of Burns
| Problem | Treatment |
|---|---|
| Sepsis | Monitor for infection, avoid prophylactic antibiotics |
| Hypovolemia | Fluid replacement |
| Hypothermia | Adjust ambient temperature: dry blankets in field |
| Laryngeal edema | Endotracheal intubation, tracheostomy |
| Carbon monoxide poisoning | 100% oxygen, hyperbaric O2 |
| Cyanide poisoning | 100% O2 plus amyl nitrate, sodium nitrate, and sodium thiosulfate |
| Cardiac dysfunction | Inotropic agents, diuretics |
| Gastric ulcers | H2-receptor antagonist, antacids |
| Compartment syndrome | Escharotomy incision |
| Contractures | Physical therapy |
| Hypermetabolic state | Enteral and parenteral nutritional support |
| Renal failure | Supportive care, dialysis |
| Transient antidiuresis | Expectant management |
| Anemia | Transfusions as indicated |
| Psychological trauma | Psychological rehabilitation |
| Pulmonary infiltrates | PEEP, ventilation, O2 |
| Pulmonary edema | Avoid overhydration, give diuretics |
| Pneumonia | Antibiotics |
| Bronchospasm | β-agonist aerosols |
PEEP, positive end-expiratory pressure.
PROGNOSIS
Most children who sustain burns recover without significant disability; however, burns remain the third leading cause of injury-related pediatric deaths. Estimation of morbidity is difficult to ascertain from databases. Physical scarring and emotional impact of disfiguring burns are long-term consequences of burn injuries.
PREVENTION
About 92% of burns occur in the home. Prevention is possible by using smoke and fire alarms, having identifiable escape routes and a fire extinguisher, and reducing hot water temperature to 49°C (120°F). Immersion full-thickness burns develop after 1 second at 70°C (158°F), after 5 seconds at 60°C (140°F), after 30 seconds at 54.5°C (130°F), and after 10 minutes at 49°C (120°F).
 SEE
SEE