 CHAPTER 145 Heart Failure
CHAPTER 145 Heart Failure
ETIOLOGY AND EPIDEMIOLOGY
Myofibril contraction is translated into cardiac work or pump performance. The force generated by the muscle fiber depends on its contractile status and basal length, which is equivalent to the preload. As the preload (fiber length, left ventricular filling pressure or volume) increases, myocardial performance (stroke volume and wall tension) increases up to a point (the normal Starling curve). The relationship is the ventricular function curve (Fig. 145-1). Alterations in the contractile state of the muscle lower the relative position of the curve, but retain the relationship of fiber length to muscle work. Heart rate is another important determinant of cardiac work because the cardiac output equals stroke volume times the heart rate. Additional factors also affect cardiac performance (Table 145-1).
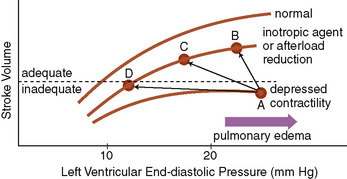
FIGURE 145-1 Ventricular function curve illustrating the effect of inotropic agents or arterial vasodilators. In contrast to diuretics, the effect of digitalis or arterial vasodilator therapy in a patient with heart failure is movement onto another ventricular function curve intermediate between the normal and the depressed curves. When the patient’s ventricular function moves from A to B by the administration of one of these agents, the left ventricular end-diastolic pressure may also decrease because of improved cardiac function; further administration of diuretics or venodilators may shift the function further to the left along the same curve from B to C and eliminate the risk of pulmonary edema. A vasodilating agent that has arteriolar and venous dilating properties (e.g., nitroprusside) would shift this function directly from A to C. If this agent shifts the function from A to D because of excessive venodilation or administration of diuretics, the cardiac output may decrease too much, even though the left ventricular end-diastolic pressure would be normal (10 mm Hg) for a normal heart. Left ventricular end-diastolic pressures of 15 to 18 mm Hg are usually optimal in the failing heart to maximize cardiac output, but to avoid pulmonary edema.
(From Andreoli TE, Carpenter CCJ, Griggs RC, Loscalzo J [eds]: Cecil Essentials of Medicine, 5th ed. Philadelphia, WB Saunders, 2001.)
TABLE 145-1 Factors Affecting Cardiac Performance
PRELOAD (LEFT VENTRICULAR DIASTOLIC VOLUME)
AFTERLOAD (IMPEDANCE AGAINST WHICH THE LEFT VENTRICLE MUST EJECT BLOOD)
CONTRACTILITY (CARDIAC PERFORMANCE INDEPENDENT OF PRELOAD OR AFTERLOAD)
HEART RATE
From Andreoli TE, Carpenter CCJ, Griggs RC, Loscalzo J: Cecil Essentials of Medicine, 5th ed. Philadelphia, WB Saunders, 2001.
Heart failure occurs when the heart is unable to pump blood at a rate commensurate with metabolic needs (oxygen delivery). It may be due to a change in myocardial contractility that results in low cardiac output or to abnormal loading conditions being placed on the myocardium. The abnormal loading conditions may be afterload (pressure overload, such as with aortic stenosis, pulmonary stenosis, or coarctation of the aorta) or preload (volume overload, such as in ventricular septal defect (VSD), patent ductus arteriosus (PDA), or valvular insufficiency). Volume overload is the most common cause of heart failure in children.
It is helpful to approach the differential diagnosis of heart failure based on age of presentation (Table 145-2). In the first weeks of life, heart failure is most commonly due to an excessive afterload being placed on the myocardium. Heart failure presenting around 2 months of age is usually due to increasing left-to-right shunts that become apparent as the pulmonary vascular resistance decreases. Acquired heart disease, such as myocarditis and cardiomyopathy, can present at any age.
TABLE 145-2 Etiology of Heart Failure by Age Group
FETUS
PREMATURE NEONATE
FULL-TERM NEONATE
INFANT/TODDLER
CHILD/ADOLESCENT
BPD, bronchopulmonary dysplasia; PDA, patent ductus arteriosus; VSD, ventricular septal defect.
CLINICAL MANIFESTATIONS
Heart failure presents in infants as poor feeding, failure to thrive, tachypnea, and diaphoresis with feeding. Older children may present with shortness of breath, easy fatigability, and edema. The physical examination findings depend on whether pulmonary venous congestion, systemic venous congestion, or both are present. Tachycardia, a gallop rhythm, and thready pulses may be present with either cause. If left-sided failure is predominant, tachypnea, orthopnea, wheezing, and pulmonary edema are seen. Hepatomegaly, edema, and distended neck veins are signs of right-sided failure.
IMAGING STUDIES
Noninvasive studies, such as chest radiography, are not specific, but the absence of cardiomegaly on a chest x-ray usually rules out the diagnosis of heart failure. An echocardiogram assesses the heart chamber sizes, measures myocardial function, and diagnoses congenital heart defects when present.
TREATMENT
Initial treatment is directed at improving myocardial function and optimizing preload and afterload. Diuretics, inotropic support, and, often, afterload reduction are employed (Table 145-3). Long-term therapy usually consists of diuretics and afterload reduction frequently is added. Long-term therapy with β-blockers also may be beneficial, although this remains somewhat controversial in pediatric patients.
TABLE 145-3 Treatment of Heart Failure
| Therapy | Mechanism |
|---|---|
| GENERAL CARE | |
| Rest | Reduces cardiac output |
| Oxygen | Improves oxygenation in presence of pulmonary edema |
| Sodium, fluid restrictions | Decreases vascular congestion; decreases preload |
| DIURETICS | |
| Furosemide | Salt excretion by way of ascending loop of Henle; reduces preload; afterload reduced with control of hypertension; may also cause venodilation |
| Combination of distal tubule and loop diuretics | Greater sodium excretion |
| INOTROPIC AGENTS | |
| Digitalis | Inhibits membrane Na+,K+-ATPase and increases intracellular Ca2+, improves cardiac contractility, increases myocardial oxygen consumption |
| Dopamine | Releases myocardial norepinephrine plus direct effect on β-receptor, may increase systemic blood pressure; at low infusion rates, dilates renal artery, facilitating diuresis |
| Dobutamine | β1-Receptor agent; often combined with dopamine |
| Amrinone/milrinone | Nonsympathomimetic, noncardiac glycosides with inotropic effects; may cause vasodilation |
| AFTERLOAD REDUCTION | |
| Hydralazine | Arteriolar vasodilator |
| Nitroprusside | Arterial and venous relaxation; venodilation reduces preload |
| Captopril/enalapril | Inhibition of angiotensin-converting enzyme; reduces angiotensin II production |
| OTHER MEASURES | |
| Mechanical counterpulsation | Improves coronary flow, afterload |
| Transplantation | Removes diseased heart |
| Extracorporeal membrane oxygenation | Bypasses heart |
| Carvedilol | β-Blocking agent |