CHAPTER 197 Orthopedics Assessment
CHAPTER 197 Orthopedics Assessment
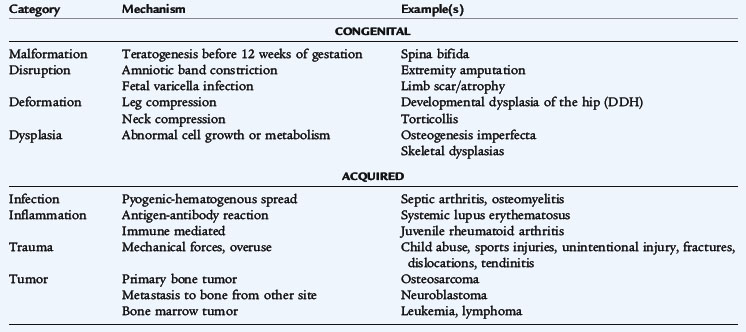
To care for the pediatric patient, one must understand the growth and development of the musculoskeletal system as well as common orthopedic terms (Table 197-1). Practitioners should recognize common mechanisms for congenital and acquired orthopedic disorders (Table 197-2).
TABLE 197-1 Common Orthopedic Terminology
| Abduction | Movement away from midline |
| Adduction | Movement toward or across midline |
| Apophysis | Bone growth center that has a muscular insertion but is not considered a growth plate (example: tibial tubercle) |
| Arthroscopy | Surgical exploration of a joint using an arthroscope |
| Arthroplasty | Surgical reconstruction of a joint |
| Arthrotomy | Surgical incision into a joint; an “open” procedure |
| Deformation | Changes in limb, trunk, or head due to mechanical force |
| Dislocation | Displacement of bones at a joint |
| Equinus | Plantar flexion of the forefoot, hindfoot, or entire foot |
| Femoral anteversion | Increased angulation of the femoral head and neck with respect to the frontal plane |
| Malformation | Defect in development that occurs during fetal life (example: syndactyly) |
| Osteotomy | Surgical division of a bone |
| Pes cavus | High medial arch of the foot |
| Pes planus | Flat foot |
| Rotation, internal | Inward rotation (toward midline) |
| Rotation, external | Outward rotation (away from midline) |
| Subluxation | Incomplete loss of contact between two joint surfaces |
| Tibial torsion | Rotation of the tibia in an internal or external fashion |
| Valgus/valgum | Angulation of a bone or joint in which the apex is toward the midline (example: knock-knee) |
| Varus/varum | Angulation of a bone or joint in which the apex is away from the midline (example: bowlegs) |
TABLE 197-2 Mechanisms of Common Pediatric Orthopedic Problems
GROWTH AND DEVELOPMENT
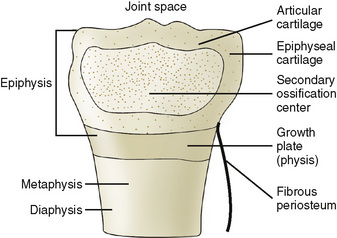
The ends of the long bones contain a much higher proportion of cartilage in the skeletally immature patient than an adult (Figs. 197-1 and 197-2). The high cartilage content allows for a unique vulnerability from trauma and infection (particularly in the metaphysis).
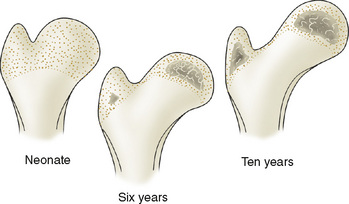
FIGURE 197-2 The ends of long bones at various ages. Lightly stippled areas represent cartilage composition, whereas heavily darkened areas are zones of ossification.
(From Tachjidan MO: Congenital Dislocation of the Hip. New York, Churchill Livingtone, 1982, p 105.)
The physis is responsible for the longitudinal growth of the long bones. Articular cartilage allows the ends of the bone to enlarge and accounts for growth of smaller bones, such as the tarsals. The periosteum can provide circumferential growth. Trauma, infection, nutritional deficiency (rickets), inborn errors of metabolism (mucopolysaccharidoses), and other metabolic disorders (renal tubular acidosis, hypothyroid) may affect each of the growth processes and produce distinct aberrations.
DEVELOPMENTAL MILESTONES
Neurologic maturation, marked by achievement of developmental motor milestones, is important for normal musculoskeletal development (see Section 2). A neurologic disorder may cause a secondary musculoskeletal abnormality (e.g., extremity contractures in Duchenne muscular dystrophy). Thus, normal motor development must be included in the definition of a normal musculoskeletal system.
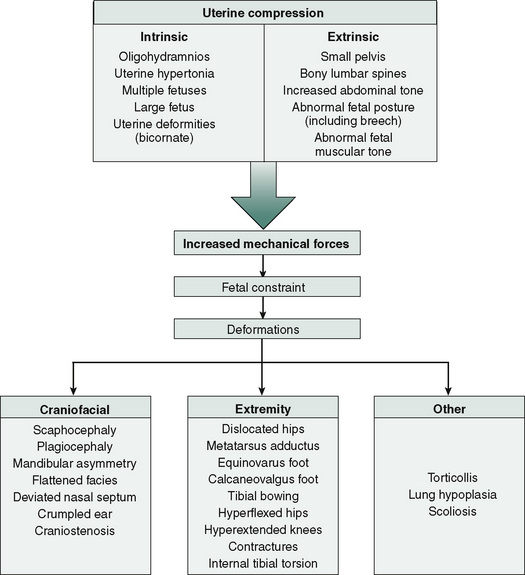
Infants
The in utero position of the fetus produces joint and muscle contractures that can affect the angular and torsional alignment (temporary or permanent) of the skeletal system, especially of the lower extremity (Fig. 197-3). The newborn’s hips are externally rotated. Pes planus and genu varum are common. Infants are usually born with a flexed posture. These contractures usually decrease to neutral within the first 4 to 6 months. The foot is often flat and tucked under at birth; the ankle will be inverted and the forefoot is adducted when compared with the hindfoot. The lateral border of the foot must straighten out, even with dorsiflexion, to be considered secondary to in utero positioning.
The head and neck may also be distorted by in utero positioning. The spine and upper extremities are less likely to be affected. By the age of 3 to 4 years, the effects of in utero positioning have usually resolved.
Gait
Normal gait has a stance phase and swing phase; each leg should have symmetrical timing with each phase. The stance phase represents 60% of the gait and begins with foot contact (usually the heel strike) and ends with the toe-off. During the swing phase (40%), the foot is off the ground. The gait cycle is the interval between stance phases on the same limb.
Toddlers will generally walk independently by 18 months of age. Their broad-based gait is usually inconsistent and is characterized by short, rapid steps and does not have the reciprocal arm swing. Gait coordination improves over time and a normal gait is usually achieved by the time a child enters elementary school. An excessively clumsy 3- or 4-year-old should spark concerns for muscular dystrophy.
The Limping Child
The differential diagnosis for a limping child is often categorized by age and painful or painless limp (Table 197-3). An antalgic gait is a painful limp; the stance phase and stride of the affected limb are shortened to decrease the discomfort of weight bearing on the affected limb. The Trendelenburg gait has a normal stance phase, but excessive swaying of the trunk. The gluteus medius muscle stabilizes the pelvis during the stance phase, preventing the pelvis from dropping toward the leg in swing phase. Trauma or weakness of the gluteal muscles is a common cause of painless limp. Waddling gait refers to a bilateral decrease in function of the gluteus muscles.
TABLE 197-3 Differential Diagnosis of Limping in Children
| Age Group | Diagnostic Considerations |
|---|---|
| Early walker: 1 to 3 years of age | |
| Child: 3 to 10 years of age | |
| Adolescent: 11 years of age to maturity |
Toe walking is a common complaint in early walkers. Any child older than 3 years of age who still toe walks should be evaluated by a physician. Although it may result from habit, a neuromuscular disorder (cerebral palsy, tethered cord), Achilles tendon contracture (heel cord tightness), or a leg-length discrepancy may be present.