Chapter 3 Movement System Syndromes of the Cervical Spine
Introduction
The joints and all of the structures that move and support them are subjected to degenerative forces arising from repeated movements, prolonged postures, and simply through the process of aging. The cervical spine is particularly susceptible to degenerative changes because normal day-to-day activities require frequent movements of the head and cervical spine. The inevitable degeneration process leads to injury, altering the precision of movement that negatively impacts the rate and type of degeneration. In addition, many individuals perform excessive motions of their head and cervical spine as part of their body language or use undesirable prolonged postures such as holding the telephone to their ear with their shoulder. Based on the premise that the onset of painful and degenerative conditions of the cervical spine is precipitated by deviations in the alignment and movement patterns, this chapter discusses the normal anatomy and kinesiology of the cervical spine to form the basis for understanding and recognizing abnormal motion. The movement system syndromes are then described along with recommendations for rehabilitation.
A common misconception is that because an individual moves in a specific way and because that pattern feels normal, it is an optimal movement pattern. We believe that just as good posture has to be practiced so do optimal movement patterns. Optimal alignment and movement patterns are believed to slow the degenerative process that is associated with arthrokinematic hypermobility.1 This chapter describes the alterations in alignment and movement patterns that accelerate the degenerative process.
The cervical spine is susceptible to the stresses of daily activities, such as frequently rotating the head and cervical spine to position the eyes and ears2,3; flexing, extending, and translating the neck for the same reason; accommodating changes in the alignment of the thoracic spine; and sustaining the weight of the head and upper extremities.4-6 Malalignment of the cervical spine and adjacent regions can add excessive compressive load onto the tissues in the cervical region and affect the movement pattern.7-9 Repetitive upper extremity motions can have the same effect.10 Appropriate modification of the posture of the cervical, thoracic, and scapular regions can diminish the compressive load on the cervical structure.
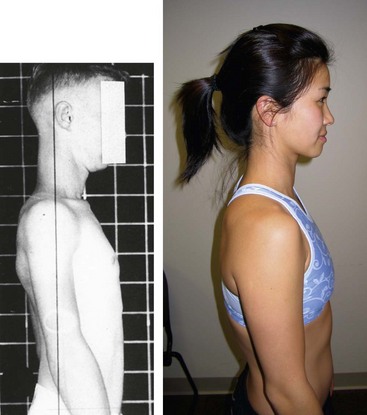
Cervical extension secondary to a forward-head posture (Figure 3-1), which is often associated with a thoracic kyphosis, is the most frequently observed alignment impairment of the cervical spine. A forward-head position is described as excessive extension and forward translation of the cervical vertebrae7,8 (Figure 3-2). Thoracic kyphosis commonly results in increased extension of the cervical spine contributing to the forward-head position11,12 (Figure 3-3). The extended position of the cervical vertebrae increases the compressive loading on tissues in this region, especially the facet joints.7
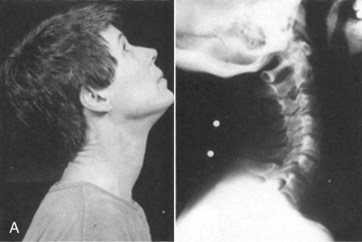
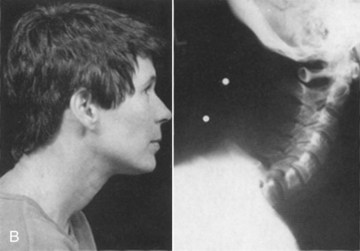
Figure 3-2 A, Cervical extension. B, Slumping to increase thoracic flexion. Forward head with cervical extension.
(From Kendall FP, McCreary EK, Provance PG: Muscles: testing and function, ed 4, Philadelphia, 1993, Lippincott Williams & Wilkins.)
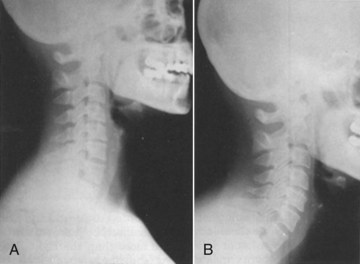
Figure 3-3 A, Erect sitting. Good cervical alignment. B, Same subject slumping with thoracic flexion. Forward head with cervical extension.
(From Kendall FP, McCreary EK, Provance PG: Muscles: testing and function, ed 4, Philadelphia, 1993, Lippincott Williams & Wilkins.)
Other positions of the head and cervical spine can also have an influence on scapular motion. For example, Ludewig et al13 demonstrated decreased scapular upward rotation and decreased posterior tipping with a flexed neck and head position. The focus of our strategy of alleviating symptoms and improving function of the cervical region is to start with exercises that correct any faults in the alignment of the cervical, thoracic, and scapular regions before focusing on the correction of faulty cervical movements.
Based on clinical observations, the principal movement impairments in the cervical region involve faulty patterns of extension and rotation. If these movements are not performed precisely, the eventual result is pain and limited range of motion (ROM). Correcting the alignment of the thoracic spine, scapulae, and the cervical spine while supporting the arms results in decreased pain and increased ROM during cervical rotation.9,14 The patient is also instructed to imagine rotating the cervical spine about an axle running through the cervical spine and to avoid any compensatory sidebending and/or extension. This strategy for performing cervical rotation exercises improves distribution of forces, such as shear and compression, that occur during rotational motions.
Maintaining precise movement in the cervical region is a challenge because of many factors, including the number of intervening segments, their degrees of freedom, and the influence of the alignment of the thoracic spine and the shoulder girdle musculature. Treatment of the cervical region requires attention to all of these key regions. Treatment strategies include obtaining optimal alignment of the trunk, shoulder girdle, and cervical spine; optimal length and recruitment of the intrinsic muscles of the cervical spine; and optimal movement patterns of the cervical spine and the shoulder girdle and ensuring no compensatory movements of the cervical spine during movement of the upper extremities. The patient should support the upper extremities when sitting by using chairs with armrests that are an appropriate height. Supporting the upper extremities diminishes the downward pull of the limbs that impose compressive forces on the cervical spinal structures, as well as minimizing the tension from the cervicoscapular muscles that can alter the pattern of cervical motion.5,6,9,14,15
Ideal Alignment of the Cervical Region
Ideal alignment of the cervical region allows the head to be positioned with minimal muscular effort.7,8 Ideal alignment is an inward lordotic curve with both the upper and lower cervical region in a position of slight extension7,8,16 (see Figure 3-3, A). With aging and the inevitable degenerative changes occurring in the cervical discs, the lordotic alignment decreases and there is an increase in forward translation.
As described earlier, the most common alignment impairment observed in the cervical spine is a forward-head posture. The forward-head posture is characterized by forward translation of the lower cervical region and hyperextension of the cervical region with typically, an increased kyphotic curvature in the thoracic region7,8 (see Figures 3-2 and 3-3, B). Patients with chronic neck pain have a decreased ability to maintain a correct alignment when distracted.17
The muscular adaptations associated with a forward-head position are shortening of the cervical spine extensors and a lengthening of the intrinsic cervical spine flexors.8,18 The forward-head position also requires increased activity of the extensor muscles of the cervical spine to counter balance the head against the effects of gravity.7,19 The muscular adaptations that occur with a forward-head position results in an increase of compressive forces acting on the articular facets.7,20 In addition, changes may also occur in the ligamentum nuchae that may increase demand on the upper trapezius muscle to stabilize and move the cervical spine.21
A forward-head posture is a common physical finding in patients with chronic tension headache and patients with unilateral migraine.22 Additional alignment faults that we have observed with headache patients include an increase in the degree of upper cervical extension in comparison to that of the lower cervical spine, suggesting possible muscular adaptations in the suboccipital region. These adaptations can include shortness of the suboccipital extensors, superior obliques, inferior obliques, and rectus capitis and lengthened position of the suboccipital flexors, rectus capitis lateralis, and anterior muscles.18
We have often observed that body language and deficits in hearing or vision have an influence on a patient’s cervical alignment and movement patterns. Patients who use movements and postures of their head and cervical spine as part of their communication strategy can add additional stresses to the cervical region. Common habits that we have observed include excessive extension of upper cervical region and forward translation of the cervical spine during talking, laughing, or reading or while working on a computer. These faults can be exaggerated when the patient wears eyeglasses, especially bifocals.2 These same patients may also have complaints of pain or headache in the upper cervical region.
Additional alignment faults can result from adaptations arising from asymmetrical use of the eyes or loss of hearing in one ear. Deficits in sight or hearing can result in prolonged posturing in one direction of cervical rotation with associated sidebending in the same direction. The muscular adaptations include unilateral hypertrophy of cervical paraspinals or sternocleidomastoids muscles. These asymmetrical adaptations could cause greater compression forces on the facet joints on one side of the cervical spine. The therapist needs to make the patient aware of these habits to decrease the frequency of the faulty movements and postures while teaching the patient exercises to offset the effects of the postural positions.3
Motions of the Cervical Spine
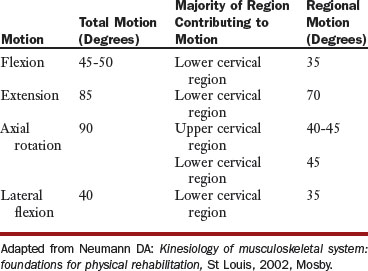
The cervical spine consists of seven vertebrae that are divided into two distinct regions: The upper cervical region includes the occiput, C1, and C2 vertebrae and the lower cervical region includes the vertebrae of C3 through to C7. The literature reports a wide variability of available motion in the craniocervical region. With consideration for the large intersubject variability, the typical available motion reported is shown in Table 3-1.19
Precise movements in the cervical spine require optimal arthrokinematics and osteokinematics and depend on the muscle length, strength, and recruitment patterns. Motions of the cervical spine are comprised of coupled motions. Coupled motion is defined as a primary motion that occurs in one plane that is accompanied automatically by motion in at least one other plane. “Motion in which rotation or translation of a vertebral body about or along one axis is consistently associated with a simultaneous rotation or translation about another axis.”23
Lysell demonstrated a coupled pattern of motion with cervical flexion and extension.24 The movement is a combination of translation about a horizontal axis and sagittal plane rotation about a frontal axis of the superior vertebrae.7 White and Panjabi have reported the total amount of sagittal plane translation to be approximately 3.5 mm at each vertebral level.23 This would include 1.9 mm in an anterior direction and 1.6 mm in the posterior direction.23 These reported values represent a small amount of motion and consequently are fairly undetectable to clinical observations, so translation motion observed during the clinical examination can be assumed to be excessive.
Available cervical flexion motion is reported to be 45 to 50 degrees with the lower cervical region contributing approximately 34 degrees. Cervical extension motion is approximately 85 degrees with the majority (about 79 degrees) occurring in the lower cervical region.19,23 The most common impairment observed during flexion and extension motions is the presence of a relatively greater degree of translation motion as compared to sagittal rotation motion. Observation of the relative amount and timing of upper versus lower cervical motion is also important when assessing the movement pattern of patients with neck pain.
Available rotation motion is comprised of the coupled motions of lateral flexion and rotation in the same direction.19,23 The observed coupled motion from C2 to C7 demonstrates a gradual decrease in the amount of axial rotation that is associated with lateral flexion as the motion progresses from superior to inferior. This finding has been attributed to the increase in the incline of the orientation of the cervical facet joint.23 Rotation occurs about a vertical axis with approximately 90 degrees of available motion with 45 degrees attributed to motion at the atlantoaxial joint complex and the remaining 45 degrees from the lower cervical region.19
Lateral flexion motion also consists of the coupled motion of lateral flexion and rotation in the same direction. The available lateral flexion motion is approximately 40 degrees, with the majority of motion (35 degrees) contributed by the lower cervical region.19
When assessing the active ROM, the therapist should consider the patient’s age, with consideration of the possible presence of degenerative changes and decrease in the amount of available ROM.25 Degenerative disc changes in the cervical spine are observed at a later age than lumbar degenerative changes. Asymptomatic degenerative changes are common on magnetic resonance imaging (MRI) in the cervical spine after 30 years of age with significant changes noted in subjects over 40 years of age.26-28
Cervical disc degeneration has been observed in 80% of asymptomatic subjects over the age of 60 years.29 Disc degeneration is more common in the lower cervical region than in the upper cervical region. The proposed explanation for this phenomena is that the lower cervical region has greater loads imposed on it with daily activities.7,30,31 In addition, a forward-head alignment with increasing anterior translation of the head increases the flexion moment on the C7-T1 junction.7
With aging, there is a decrease in the cervicovertebral ROM of approximately 5 degrees of motion for every 10 years.25,32 There is also an associated decline in ROM with observed degeneration of the cervical spine, approximately a decrease of 1.2 degrees at the level of the observed degenerative segment with an actual increase in range of 0.8 degrees at the level above the degenerated level.32 The challenge for the therapist is to attempt to restore the motion at the degenerative segment without causing greater motion at the cervical level above the degenerated segment.
Muscle Actions of the Cervical Spine
Optimal muscle lengths and recruitment patterns are critical to the performance of cervical motions to allow the ideal ratio of coupled motion to occur. The muscles in the cervical region can be classified into two distinct groups according to the relationship of the attachment of the muscles to the axis of motion of the cervical spine.7 The intrinsic muscles of the cervical spine located close to the axis of motion are felt to provide precise control of motion during movement. The extrinsic muscles of the cervical spine are located farther from the axis of motion and provide power to the motion but not necessarily precision of motion. A balance of participation between these two groups is critical for precise and pain-free motion of the cervical spine.
Cervical Flexors
The function of the cervical intrinsic flexors is to produce forward sagittal plane rotation or “rolling” of the cervical vertebrae. The muscles producing the sagittal rotation motion in the upper cervical region are the rectus capitis anterior and rectus capitis lateralis33 (Figure 3-4). In the lower cervical region, forward sagittal rotation is produced by the longus capitis and longus colli. The longus capitis and colli are also active in protecting the anterior structures during forceful extension motions.7 Impairment of the cervical intrinsic flexors has been reported in patients with cervicogenic headaches and chronic cervical spine pain.34-38
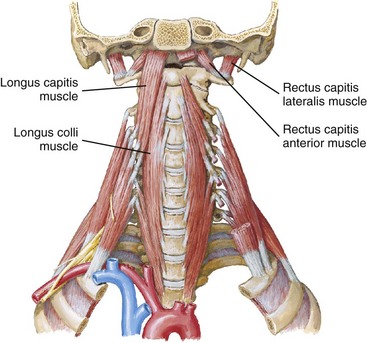
Figure 3-4 Rectus capitis anterior and rectus capitis lateralis muscles.
(Reprinted from www.netterimages.com © Elsevier, Inc. All rights reserved.)
The function of the cervical extrinsic flexors is to add force to the flexion movement and produce flexion motion associated with forward translation of the cervical vertebrae. The muscles contributing to the forward translatory motion in the cervical region are the sternocleidomastoids and anterior and medial scalenes (Figures 3-5 and 3-6). Commonly, these muscles are the dominant muscle group during flexion movements. The dominant effect of the extrinsic muscles can be attributed to the longer moment arm of this group as compared to the intrinsic muscle group and this may contribute to their increase use during cervical flexion. This faulty movement pattern would result in a movement of anterior translation of the head and cervical spine with diminished anterior sagittal plane rotation20 (Figure 3-7).

Figure 3-5 Sternocleidomastoid muscles.
(Reprinted from www.netterimages.com © Elsevier, Inc. All rights reserved.)
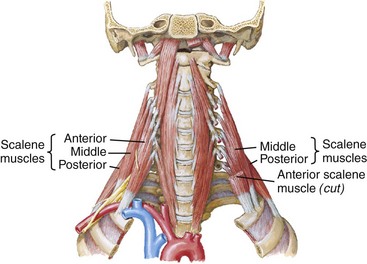
Figure 3-6 Anterior and medial scalenes muscles.
(Reprinted from www.netterimages.com © Elsevier, Inc. All rights reserved.)
Cervical Extensors
The function of the intrinsic cervical extensors is to produce posterior sagittal rotation or backward “rolling” of the cervical vertebrae (Figure 3-8). The muscles attributed to producing the posterior sagittal rotation motion in the upper cervical region are the rectus capitis posterior major and minor, the oblique capitis inferior and superior, and the semispinalis capitis, the splenius capitis, and the longissimus capitis. The muscles in the lower cervical region that produce posterior sagittal rotation are the semispinalis cervicis, the splenius cervicis, and the longissimus cervicis.20 The cervical multifidus spinae muscles are thought to produce cervical extension, axial rotation, and lateral bending movement, but the total moment-generating capacity is predicted to be less than 1 Nm and therefore not considered to be a clinically significant contribution to movement,39 although the fascicular attachments of the cervical multifidus to the cervical facet capsules have been proposed to be a possible contributor to neck pain and injury.39,40

Figure 3-8 Intrinsic cervical extensors.
(From Neumann, DA: Kinesiology of the musculoskeletal system: foundations for rehabilitation, ed 2, St Louis, 2010, Mosby.)
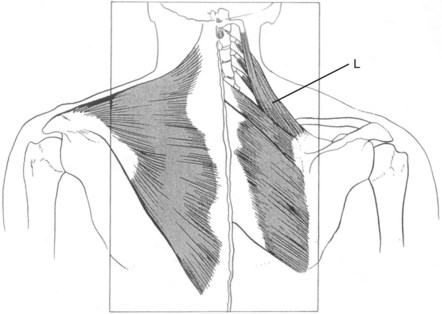
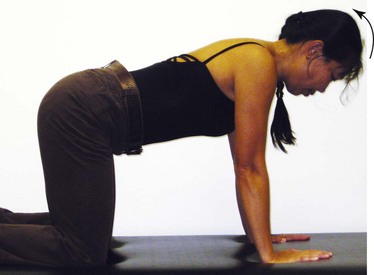
The function of the extrinsic cervical extensors is to produce extension with posterior translation of the cervical vertebrae. The muscles attributed to producing this posterior translatory motion in the cervical region are the upper trapezius and levator scapulae (Figure 3-9). A common faulty recruitment pattern can include greater recruitment of the extrinsic cervical extensors during cervical extension. This faulty recruitment pattern can best be observed in the hands and knees position (Figure 3-10) and the prone position (Figure 3-11). If the patient cannot assume the quadruped position, leaning on the forearms on a counter can be substituted. The objective is to have the scapula in a stabilized position and the head horizontal in relation to gravity.
Cervical Rotators
The intrinsic cervical rotators produce rotation about a vertical axis. These muscles include the rectus capitis posterior major, the oblique capitis inferior, the oblique capitis superior, and splenius. The oblique capitis inferior has been demonstrated to have a higher density of muscle spindles compared to other cervical muscles and is thought to be an important contribution to the sensation of cervical rotation.3
The extrinsic cervical rotators include the sternocleidomastoids, the scalenes, the upper trapezii, and the levator scapulae (see Figures 3-5 and 3-6). These muscles all have the action of rotation but also the simultaneous action of lateral flexion. If these groups of muscles are the dominant muscle group during cervical rotation, the precision of movement about a vertical axis may be compromised. The therapist will often observe rotation with concurrent lateral flexion. If the patient uses this strategy for rotation, they may complain of pain when the lateral flexion movement occurs. Repeating the rotation motion while maintaining a rotation movement about a vertical axis without concurrent lateral flexion can result in pain-free ROM.
The therapist may also observe rotation with simultaneous extension (Figure 3-12). This faulty movement pattern may be an indication of dominance of the sternocleidomastoid and its influence as an extensor of the upper cervical spine over the poorly recruited intrinsic cervical rotators, which would maintain motion about a vertical axis. The actions of the upper trapezius and/or the levator scapulae can also contribute to cervical extension during rotation.
In addition, the therapist may also observe cervical rotation with simultaneous flexion and/or forward translation of the head and neck (Figure 3-13). This faulty movement pattern may be an indication of dominance of the anterior scalenes, the middle scalenes, and the sternocleidomastoids during the movement of rotation. Dominance of these muscles and their propensity to increase translation and shear forces on the lower cervical spine can result in greater movement in the translatory plane rather than rotation about a vertical axis.
As is discussed later in the sections on the appropriate syndromes, manually guiding the patient’s pattern of rotation is often necessary. A frequently required intervention is to instruct the patient to turn the head and neck “easily” and with minimal effort to reduce the magnitude of muscular contractions and to encourage a more appropriate muscle recruitment pattern. A strong muscle contraction especially of the extrinsic rotators can add compression of cervical spine structures and favor the use of the muscles with the greatest mechanical advantage.
The upper trapezius and levator scapulae muscles have attachment from the cervical spine region directly to the scapula and clavicle41 (see Figures 3-5, 3-6, and 3-9). This attachment has clinical significance when examining cervical spine function. Specifically, we have noted in clinical examination that single arm movements can result in compensatory motion of rotation of a cervical spine segment or several segments.10
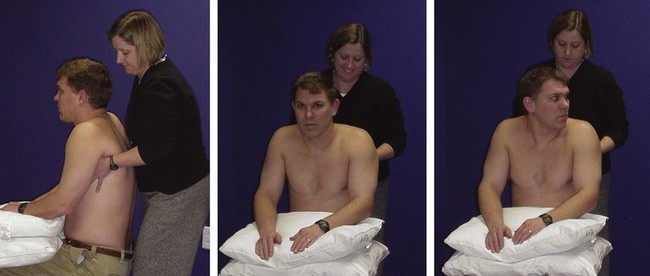
In addition, the attachment of these muscles will influence the ROM during active cervical motions, especially rotation. Examining active cervical rotation with passive support of the weight of the upper extremities can result in increase cervical ROM and decrease pain.9,14,15 The passive support of the upper extremities can reduce the passive stretch of the upper trapezius and levator scapulae that can potentially decrease the load on the cervical spine structures and permit improved motion and less painful movement9,14,15 (Figure 3-14).
MOVEMENT SYSTEM SYNDROMES of the Cervical Spine
Movement system syndromes of the cervical spine are precipitated by deviations in the alignment and movement patterns. Cervical spine syndromes in order of frequency and key findings are included in Table 3-2.
TABLE 3-2 Cervical Spine Syndromes in Order of Frequency of Observation
| Syndrome | Key Findings |
|---|---|
| Cervical extension-rotation | Forward head with asymmetrical findings: Asymmetry in cervical spinal musculature and/or scapula alignment; pain with rotation-associated sidebending and extension; weak intrinsic cervical flexors; dominance of extrinsic cervical rotators |
| Cervical extension | Forward head; pain with extension; translation greater than sagittal rotation; weak intrinsic cervical flexors |
| Cervical flexion-rotation | Decreased cervical lordosis, flat thoracic spine; pain with rotation-associated flexion; excessive recruitment of extrinsic cervical rotators, anterior and middle scalenes |
| Cervical flexion | Decrease cervical lordosis, flat thoracic spine; pain with flexion; lower cervical flexion greater than upper thoracic flexion; excessive recruitment of extrinsic neck flexors; poor recruitment of intrinsic neck extensors during extension |
Cervical Extension Syndrome
In individuals with minimal degeneration involving the cervical region, the principal movement impairment in the cervical extension syndrome is imprecise cervical extension that is often associated with pain and limited ROM. There is altered distribution of extension across the cervical region and an imbalance of muscle performance among the cervical extensors and flexors. The extrinsic muscles contribute to excessive horizontal translation of the cervical vertebrae rather than a combination of sagittal rotation produced by the intrinsic cervical muscles and horizontal translation produced by the extrinsic cervical muscles. Contributing factors in the cervical extension syndrome include the weight of the upper extremities, the alignment of the thoracic spine, and the alignment of the scapulae.
Symptoms and History
Pain is typically located in the posterior cervical region with possible radicular symptoms along the cervical nerve root dermatomes and/or scapula region specifically along the vertebral border.42 The patient complains of pain with cervical spine extension and/or prolonged posturing of a forward-head position (e.g., working at the computer or reading). The patient can commonly have complaints of headaches located in the suboccipital region.
Key Tests and Signs
Alignment Analysis
Alignment faults with cervical extension syndrome include a forward-head position with an increase in the cervical lordosis and anterior translation (see Figure 3-2). Often, patients with the diagnosis of cervicogenic headaches have an alignment of greater upper cervical spine extension and are positioned in 10 degrees of posterior sagittal extension, as referenced to the vertical plumb line.
Typically, in individuals older than 50 years of age, the forward-head alignment is a position of greater anterior translation in the lower cervical region and greater upper cervical sagittal extension.26 As described in the literature, degenerative changes are often present with increasing age and will affect the alignment and the loading of the joints. With degeneration of the cervical discs, there is narrowing of the intervertebral foramen and increased approximation and loading of the facet joints.7,29-31 The changes in alignment observed with degeneration, specifically the approximation of the facet joints, are similar to the same position of physiological extension. Thus a cervical spine with presence of degeneration may have low tolerance to additional extension forces.
The characteristic alignment faults in the adjacent regions include a thoracic kyphosis and scapular malalignment.11,12,20 An increased thoracic kyphosis is highly correlated with an increase in a forward-head position11,12,20 (Figure 3-15; see Figure 3-3). Additional alignment faults include the scapulae in a position of excessive depression and/or abduction.9,14,43
Movement Impairment Analysis
Individuals with a cervical extension syndrome often complain of pain with movement into active extension (Figure 3-16). During assessment of active cervical extension, the younger spine (15 to 25 years old) may demonstrate a greater amount (or degree) of posterior translation than posterior sagittal rotation and/or an excessive ROM. Older individuals with spinal degeneration may have painful and limited extension because of a starting alignment of a forward-head position with excessive anterior translation. The starting alignment of anterior translation (extended position) limits the available physiological motion into extension. An additional movement impairment with active cervical extension includes a faster rate of upper cervical extension movement compared to that observed in the lower cervical extension movement (Figure 3-17).

Figure 3-16 Faulty active cervical extension; upper cervical motion is greater than lower cervical motion.

Figure 3-17 Cervical extension movement impairment: Greater upper cervical extension than lower cervical extension (the upper cervical spine is more extended than the lower cervical spine).
Patients with cervical extension syndrome may also demonstrate movement impairments during flexion. Active flexion motion can be limited (Figure 3-18) and painful, particularly when the degree of anterior translation is excessive and relatively greater than the normal anterior sagittal rotation.
The faulty movement of forward translation without the coupled motion of sagittal rotation results in the approximation of the facet joint surfaces. The approximation of the facet joint surfaces during performance of this faulty flexion movement results in similar approximation of the facet joint surfaces as that occurring during cervical extension, as well as complaints of pain similar to those during active extension (Figure 3-19).
In this system, the primary test is performed by asking the patient to perform the movement in the desired direction such as cervical extension or rotation. During the movement, the therapist asks about symptoms and carefully observes the characteristics of the movement. For the secondary test, the therapist has the patient correct the starting alignment and the movement faults and notes the effect on the symptoms. The corrected alignment and movement pattern is repeated a number of times to ensure the improvement in symptoms is consistent. The repetitions also help the patient learn how to move correctly and how to control the symptoms.
Sitting tests
Sitting tests should be performed in active cervical ROM and flexion, extension, and rotation.
Secondary tests
Correction of alignment: If there is pain at rest, then correction of the forward-head alignment of the cervical spine may alleviate or decrease the symptoms. To correct the head and neck alignment, the alignment of the thoracic spine and scapulae must also be corrected.
Passive elevation of the shoulder girdle: Passively elevating the shoulder girdle and/or supporting the weight of the upper extremities before the patient performs active cervical extension, flexion, or rotation may alleviate or decrease the symptoms and often results in increased cervical ROM and typically a decreased level of reported pain during motion14,15 (see Figure 3-14).
Passive support of the upper extremities can reduce the passive stretch of the upper trapezius and levator scapulae which can potentially reduce the loading and posterior shear forces on the structures of the cervical spine. The passive support typically results in increase ROM and less painful movement.*
Passive elevation of ribcage: Performing the test of passive elevation of the rib cage is indicated in patients with well-developed abdominals, particularly the rectus abdominis. Passive elevation of the rib cage will often improve active cervical ROM and decrease pain.
Elevating the rib cage affects the pain and increases the cervical ROM because well-developed abdominal muscles (rectus abdominis and external oblique) have enough stiffness to passively depress the rib cage. Active contraction of the abdominal muscles would further increase the passive tension and downward pull on the rib cage. The tension would also affect the scalene muscles that attach to the rib cage, thus adding to the compression on the cervical vertebrae and restricting motion. Passive elevation of the rib cage decreases the tension on the scalene muscles, thus decreasing the pain and increasing the cervical rotation ROM.
Supine tests
Active cervical flexion in supine
The primary movement impairment during cervical flexion is excessive anterior translation in relation to the amount of anterior sagittal rotation. The result is a forward-head position and often reports of pain.
Manual muscle test of cervical flexion
The cervical intrinsic flexor muscles will test weak.8 The patient will be unable to maintain a position of a “neck curl” and will assume an extended forward-head position that is characteristically associated with dominance of the sternocleidomastoid and anterior and middle scalenes and weakness of the deep neck flexors8,35,45 (Figure 3-20).
Secondary test
Corrected performance of cervical flexion: Manual assistance provided by the therapist is required to properly perform the “neck curl” movement. When the therapist supports the weight of the head and assists the proper anterior sagittal rotation motion and the patient actively holds the position, there is no pain as long as the patient avoids the extended forward-head position (see Figure 3-20).
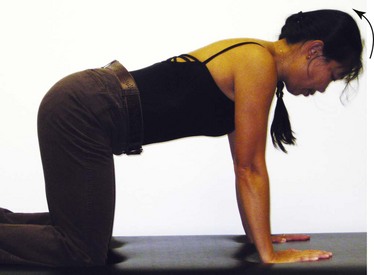
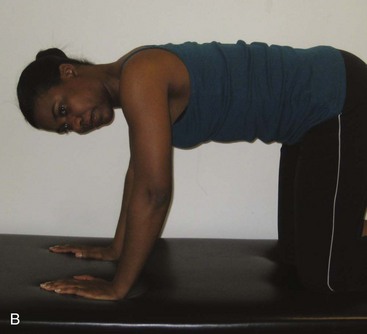
Prone and quadruped tests
Active cervical extension in prone or quadruped: Active cervical extension can be performed in both the prone and quadruped positions and is characterized by a greater degree of posterior translation as compared to posterior sagittal rotation. During this movement, the examiner will typically observe an increase recruitment of levator scapulae muscles that contribute to posterior translation and diminished recruitment of the intrinsic cervical extensors that produce posterior sagittal rotation (see Figure 3-10).
Secondary test
Correction of cervical extension: Appropriate instruction to initiate the cervical extension movement with posterior sagittal rotation of the head and cervical spine results in decreased pain. Verbal cues can include “roll your head back” or “pretend that there is a pole through your ears and you are rolling around the pole.”
Quadruped test
Active cervical extension in quadruped: During the quadruped rocking back, the examiner will often observe a compensatory motion of cervical extension. Typically, this movement impairment is not associated with the complaint of pain (Figure 3-21).


Figure 3-21 A, Compensatory cervical extension during quadruped rocking back. B, Correction of compensatory cervical extension.
The cervical extension during rocking back is believed to be the result of the lengthening or stretching of the levator scapulae, a downward rotator, as the scapula upwardly rotates during the motion of rocking back. The passive lengthening of the levator scapulae muscle causes extension of the cervical spine, which is also associated with posterior translation.
Secondary test
Correction of cervical extension: The patient is instructed to repeat the quadruped rocking back with the “chin to the Adam’s apple” or the anterior base of the neck to avoid extension of the cervical spine. The patient will commonly report a sensation of diminished pressure in the posterior cervical region during the performance of the secondary test movement. Encouraging the recruitment of cervical flexors during this movement will create the appropriate counteracting force to prevent the cervical extension and translation movements.
Treatment
The goal for treatment of the cervical extension syndrome is to diminish cervical extension movements and forces during daily activities. All exercises and functional instructions include improving the alignment and reducing the stress imposed by adjacent regions before initiating cervical movements. Specifically, these instructions include modification of the alignment of the thoracic spine and the shoulder girdle, as well as supporting the upper extremities.
In addition, instructions include strategies to be used during functional activities such as how to support the upper extremities and reduce compensatory motion at the adjacent regions during the day.5,6 Typical instructions for daily activities would include use of abdominals to maintain neutral position of the lumbar spine and avoiding thoracic flexion or “slumping” especially with sitting activities. The focus of the active exercise program for the cervical region is to improve the strength and motor control of the intrinsic cervical spine flexor muscles along with improving the flexibility of the posterior cervical structures.33,37,45-47 The active exercise program includes correction of the length, strength, and stiffness of the axioscapular muscles, abdominals, and posterior thoracic spinal musculature.48
In addition, upper extremity movements have a direct effect on the cervical spine via the attachment of cervicoscapular muscles. An examination and classification of the associated scapular movement impairments is critical in the management of the patients with cervical pain. Strategies to examine, classify, and manage scapular movement impairments are clearly described in Sahrmann.1
Exercise Program
Sitting with back to the wall—capital flexion
The upper extremities are supported on pillows to diminish the compressive loading of the cervical spine from the transfer of the weight of the upper extremities to the cervical region through the cervicoscapular muscle attachment.9,15 Each patient needs to be assessed for specific alignment impairments at the lumbar and thoracic spines and scapulothoracic region. The patient is then instructed in strategies to precisely correct alignment faults in these regions before proceeding with cervical movements (Figure 3-22, A). These instructions include recruiting the lower abdominal muscles to maintain a neutral lumbar spine alignment and patient-specific instructions to correct scapulae alignment. This will typically include correction of scapular alignment of depression, downward rotation, and/or abduction (internal rotation). The key instruction for faulty alignment of scapulae depression is to “elevate the acromions toward the ears,” and the key instruction for the position of the scapulae downward rotation is to “elevate the acromions toward the ears and then slightly adduct the scapulae.” Instruction for faulty position of excessive abduction (>3 inches from the spine) would be to “squeeze the shoulder blades together.” The ideal position of the scapulae would be (1) the vertebral borders of the scapulae oriented in a vertical position or slight upward rotation, (2) the scapulae positioned 2.5 to 3 inches from the vertebral spine, (3) the scapulae positioned between T2 and T7, (4) 10 degrees of anterior tilt, and (5) 30 to 40 degrees of internal rotation.1,8,19,43,49


Figure 3-22 A, Sitting against the wall, arms supported, correct scapulae position. B, Performing capital flexion.
The patient is instructed to place his or her head close to the wall and perform capital head flexion. The patient is encouraged to “roll” the head and chin toward the base of the anterior neck while trying to maintain the head close to the wall (Figure 3-22, B). The verbal cue to “roll” the head is to encourage recruitment of the intrinsic cervical muscle to perform sagittal rotation rather than anterior translation. Many patients report a “tightening” in the front of the cervical spine region while performing this exercise. This sensation is most likely the muscles in the front of the neck being appropriately recruited, and specifically, the muscles are being recruited in a shortened position rather than the lengthened position. In addition, patients also report a “stretch or pull” down the proximal posterior cervical region that can extend into the central upper thoracic region. Again, this is an appropriate stretch to the posterior structures. There should be no pain along the vertebral border of the scapula.
The patient is encouraged to maintain appropriate alignment of the adjacent regions during the movement of the cervical spine. This exercise can best be performed in sitting, but if the patient has difficulty maintaining the correct postural alignment during the cervical motion, the exercise can be performed in supine. The supine position will not be as challenging on the trunk musculature to maintain the alignment of the adjacent regions, although the demands on the deep neck flexors are greater in the supine position than in sitting.
Any radiation of symptoms to the vertebral border of the scapulae and away from the proximal spine would be considered a possible sign of cervical radiculopathy and an inappropriate response to the movement. If radiation of symptoms occurs, the therapist should reassess whether this exercise in this position is appropriate for the patient. Radiation of symptoms indicate that the exercise should be made easier by performing the same movement in a supine position with support of the arms with pillows or using the hands to assist with movement of the head and neck.
Strengthening the intrinsic cervical spine flexors in supine
Strengthening the intrinsic cervical spine flexors in supine begins with correcting the alignment of the thoracic spine and shoulders, as well as similar instructions as noted in the previous exercise. Patients are instructed to recruit the lower abdominal muscle to maintain a neutral lumbar spine alignment. Patient-specific instructions are provided to correct the scapulae alignment, typically including correction of scapular alignment of depression, downward rotation, and/or abduction (internal rotation).
The arms should be supported on pillows with the hips and knees in flexion. The patient may require a towel roll under the head. The thickness of the towel roll depends on the patient’s thoracic alignment and severity of the forward-head alignment. The greater the kyphosis and forward-head posture the greater the thickness of the towel roll. The following is a progression of exercises from the easiest to the hardest.
Capital flexion without head lift
The patient is instructed to roll the chin toward the front of the cervical spine. The patient should feel a stretch down the central posterior cervical region and muscle recruitment of the anterior intrinsic cervical spine flexors.33,34,45
Capital flexion with head lift—with and without assistance
The patient is instructed to roll the chin toward the front of the cervical spine and then continue to roll the cervical spine and head off the supporting surface while maintaining the chin positioned at the anterior cervical spine. Adding the lift of the head is more challenging, and the patient may have trouble maintaining the chin in contact with the anterior cervical spine region.46,47 Forward translation of the chin or the chin “jutting forward” indicates poor performance of the intrinsic cervical spine flexors and a dominance of the extrinsic cervical spine flexors8 (see Figure 3-19). If a patient is unable to maintain the head position, he or she can use the hands to lift the head to minimize the load on the cervical spine muscles (Figure 3-23). Patients are encouraged to allow only enough support to permit the appropriate “curl up” position of the head and cervical spine. Progression of the exercise would be to provide less support.
Strengthening the intrinsic cervical spine extensors in prone or quadruped
Prone position
To strengthen the intrinsic cervical spine extensors in prone, the patient is positioned with the forehead on the palms of the hands (Figure 3-24). The patient is then instructed to “roll” the head back in a pain-free range. The instruction of rolling the head back is to encourage recruitment of intrinsic cervical spine muscles (splenius/semispinalis) to produce posterior sagittal rotation and diminish recruitment of the extrinsic cervical spine muscles (levator scapulae/upper trapezius) and the movement of the posterior translation. The therapist should observe the appropriate muscle recruitment of the intrinsic cervical spine muscles and diminished recruitment of the extrinsic muscles.
Quadruped position
To strengthen the intrinsic cervical spine extensors in quadruped, the patient is instructed to flatten the thoracic spine like a “table top” and align the head and cervical spine with the thoracic and lumbar spine. The patient is instructed to “roll” the head down and then roll the head back while imagining that there is a rod running through the middle of the neck and rotating about the rod. The instruction of rolling the head back encourages recruitment of intrinsic cervical spine muscles (suboccipitals, semispinalis, and splenius) to produce posterior sagittal rotation and diminish recruitment of the extrinsic cervical spine muscles (levator scapulae/upper trapezius) and posterior translation. The patient should be instructed to perform the movement in the “middle-third” of the range to avoid end-ranges. The therapist should observe the appropriate muscle recruitment of the intrinsic cervical spine muscles and diminished recruitment of the extrinsic muscles. Performing this movement in the quadruped position is a greater challenge because the patient must maintain proper trunk and scapulothoracic position in an upper extremity weight-bearing position during the movement of the cervical spine (Figure 3-25).
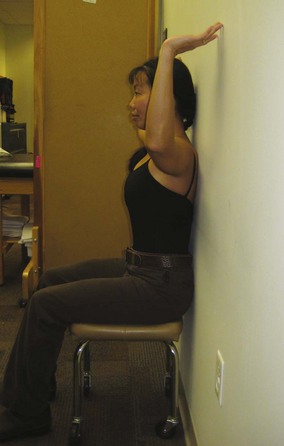
Sitting with back to wall—shoulder abduction lateral rotation
Sitting with back to wall—shoulder abduction lateral rotation exercise is a progression of the back to wall—capital flexion exercise. The patient assumes the position as described in the first exercise, which includes correct positioning of the lumbar spine, thoracic spine, scapulae, and cervical capital flexion. The patient then performs bilateral shoulder abduction and lateral rotation so that the arms are against the wall without compensatory thoracic, lumbar, or cervical extension. The patient slides the arms up the wall, maintaining spinal alignment, especially capital flexion. A typical response from the patient is a report of increased muscle activity in the midthoracic region, indicating increased recruitment of trapezius, rhomboid, and thoracic spinal musculature (Figure 3-26).
Modification: The arms do not make full contact with the wall. The arms can be parallel to the wall.
Modification: The fingertips can be placed on the wall with the elbows away from the wall.
Progression: When adding resistance with free weights or resistance bands, the patient is instructed to position the trunk, neck, and arms as described previously, then move through shoulder abduction with resistance. The patient continues to maintain the lumbar spine against the wall and capital cervical flexion during the shoulder movement.
Sitting with back to wall performing shoulder flexion
Sitting with the back to the wall performing shoulder flexion exercise is a progression of the back to wall—capital flexion exercise program. The patient assumes the same head and trunk alignment, as described, of correct positioning of the lumbar spine, scapulae, and cervical capital flexion. The patient performs shoulder flexion and lateral rotation to 90 degrees with the elbows flexed and the “palms facing you.” The patient is then instructed to perform shoulder flexion by “reaching up toward the ceiling.” The patient should maintain the lumbar spine against the wall and the cervical spine in the position of capital flexion. Since the movement of shoulder flexion is increased, there is a stretch to the latissimus dorsi and avoiding lumbar extension will be difficult if the muscle is short or stiffer than the abdominal muscles. In addition, during shoulder flexion, maintaining the humeral position of lateral rotation will also be difficult and the therapist should monitor the elbow position for indication of compensatory medial rotation. A verbal cue of “elbows in” can assist in preventing medial rotation. Also, as shoulder flexion motion increases, there often is associated cervical extension because of the stretch of the levator scapulae as the scapula upwardly rotate. Again, the patient should be encouraged to maintain capital cervical flexion and avoid compensatory cervical extension. Maintaining the position of cervical flexion during the movement of the arms encourages recruitment of the intrinsic cervical flexors to maintain cervical alignment (Figure 3-27).
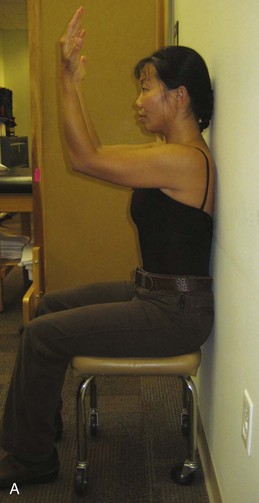

Figure 3-27 Back to wall sitting, shoulder flexion with lateral rotation. A, Start position. B, Shoulder flexion.
Modification: Position the humeri/arms in the scapular plane: 30 degrees of horizontal abduction.
Modification: Position the humeri in less lateral rotation: “Palms face each other, elbows in.”
Progression: When adding resistance with free weights or resistance bands, the patient is instructed to position the trunk, neck and arms as described previously then move through movement of shoulder flexion with resistance. The patient continues to maintain the lumbar spine against the wall and will find it a challenge to maintain capital cervical flexion and avoid cervical extension during the shoulder movement (Figure 3-28).
Wall slides: facing the wall—shoulder flexion
The patient is instructed to face the wall and place the ulnar side of the hands on the wall with the shoulders in flexion. The patient is instructed in the correct scapulae position and to bring the chin down toward the front of the neck. The patient is then instructed to slide the arms up the wall while maintaining the cervical spine position, avoiding any compensatory cervical extension during the movement of shoulder flexion and returning to the starting position (Figure 3-29).
Modification: Position the shoulders in the scapular plane.
Progression: When adding resistance with resistance bands, the patient is instructed to maintain the cervical position and to avoid any compensatory cervical extension during the movement of the shoulder flexion wall slide (Figure 3-30).
Functional Instructions
The goal in modification of functional activities of the cervical extension syndrome is to diminish cervical extension and forward translation movements of the cervical spine during daily activities. The most common activities that require instruction are prolonged sitting, especially at the computer, and the use of eyeglasses, in particular, multifocal lenses.
When sitting at the computer, patients are instructed to have a supportive chair that will reduce thoracic flexion and assist in maintaining good thoracic alignment. They should support their forearms either on the desk or an extended tray for a keyboard. The desk or tray should be at the appropriate height so that the patient does not need to “slouch” for the arms to be supported. Commonly, if the support is too low, the patient may increase thoracic flexion and/or scapular depression to position the arms for support. Raising the supporting surface or adding armrests can be helpful.
The therapist should observe the patient using his or her eyeglasses. Frequently, the patient can be observed assuming a forward-head position and/or increase upper cervical extension when using eyeglasses, especially multifocal lens.2 Alignment correction when wearing glasses should follow the same sequence that has been demonstrated in the sitting back to wall exercises: Start with correction of lumbar, thoracic, and scapular alignment and then neck and head position.
Cervical Extension-Rotation Syndrome
Cervical extension-rotation syndrome is characterized by pain associated with cervical extension and rotation. This syndrome is the most common cervical syndrome seen in our clinic. The principal movement impairment in this syndrome is imprecise cervical rotation with associated cervical extension and/or sidebend, which is often associated with pain, limited ROM and altered distribution of rotation motion across the cervical region. An imbalance of muscle performance among the cervical rotator muscles and the extrinsic muscles contributes to multiplanar movements rather than precise uniplanar motion produced by the intrinsic rotators. In addition, an imbalance of muscle performance of the intrinsic cervical extensors with the extrinsic extensors contributes to a compensatory extension movement during performance of rotation. The contributing factors in the cervical extension-rotation syndrome include weight of the upper extremities and alignment of the thoracic spine and scapulae. There may also be asymmetries in the appearance of the cervical spine, thoracic spine, and scapular regions.
Symptoms and History
Symptoms and history can be similar to the findings found in cervical extension syndrome. In addition, the patient with this syndrome may report a history of vision or hearing deficits that may require frequent movement of cervical rotation or sustained postures of cervical rotation to accommodate for the deficits. Symptom location is typically located more unilaterally.
Key Tests and Signs
Alignment Analysis
Alignment faults can be similar to the findings seen in cervical extension syndrome. Additional alignment faults include an asymmetry in muscle size of the cervical extensors. The asymmetry may be associated with the vision or hearing deficits as described earlier. Also, the asymmetry may be associated with activities that require repetitive resisted one arm activities or other work activities that required prolonged posturing in one direction of rotation. Patients who have the habit of posturing in one direction of rotation during an activity may also maintain the same position of slight rotation with activities that do not require the posture of rotation. Many times patients do not realize they are assuming this position because their eyes have adjusted to the altered head position. When patients use a mirror to monitor head alignment, they can easily correct the position and often alleviate the symptoms. Patients will initially need to practice alignment correction in front of a mirror to achieve a natural position of correct alignment.
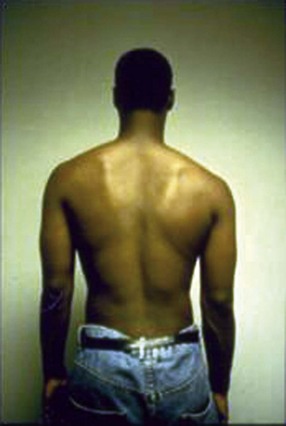
Similar alignment faults of the adjacent regions observed in the cervical extension syndrome can also be observed with this syndrome. In addition, we have noted unilateral impairments in the thoracic and scapulothoracic region. In the thoracic region, asymmetry may be noted with the rib cage rotated in one direction or increased spinal musculature on one side. In the scapulothoracic region one scapula can be positioned in excessive depression or downward rotation and impose an unbalanced stress on the cervical spine through the attachment of the scapulocervical muscles (Figures 3-31 and 3-32).
Movement Impairment Analysis
Movement impairments that are characteristic of cervical rotation extension syndrome include complaints of pain and limitation of motion during active rotation. During active rotation, there is imprecise cervical rotation with associated compensatory cervical extension and/or lateral flexion that is often associated with pain and limited ROM.
Sitting tests
Active cervical range of motion/rotation
The primary tests are the same as for the extension syndrome with the additional findings of painful and/or limited rotation often associated with concurrent cervical extension or lateral flexion as an associated movement direction. Performance of primary tests considers adjacent regions and the precision of movement.
Secondary tests
Correction of alignment and observed compensatory motions are key to diminishing pain and improving ROM. Passive elevation of the shoulder girdle and/or supporting the weight of the upper extremities results in an increase in rotation ROM and a decrease in pain14,15 (Figure 3-33).
Correction of alignment before movement
Correction of thoracic kyphosis and/or a forward-head posture before the initiation of active rotation motion results in increased rotation ROM and diminished symptoms.
Correction of compensatory movement
Correction of the movement fault of compensatory of cervical extension and lateral flexion during active rotation diminishes symptoms and increases ROM. The therapist guides the patient to maintain precise rotation about a vertical axis, and the ROM and the symptoms are reassessed.
Additional sitting tests
Single shoulder flexion/monitoring cervical spinous processes: During active single-arm flexion, rotation of a single or multiple vertebrae is noted via palpation of the cervical spinous processes.10 Patients do not typically complain of pain during this test. An alternative finding during single-arm flexion is compensatory sidebending of the cervical spine.
Secondary tests
Correction of this rotation movement impairment can be difficult. There are several strategies that can be attempted, as follows:
The patient’s individual response to the secondary tests assists the therapist in choosing the appropriate intervention strategies.
Supine test
Supine active cervical flexion: In supine, active cervical rotation is limited and painful.
Quadruped test
Active cervical rotation: In the quadruped position, active cervical rotation is limited and painful.
Secondary test
Correction of alignment, movement—verbal and manual cues: In quadruped, correcting the alignment of the thoracic spine, cervical spine, and head and manually guiding the motion to ensure precision rotation will increase the pain-free ROM. The verbal cues during this secondary test in quadruped include “keeping the head and neck in line with the thorax” and “keeping the chin rotated into the front of the neck.”
From the back, the therapist places the fingers around the patient’s neck and guides the active rotation motion. The guidance alleviates the faulty extension or sidebending motions. This secondary test movement results in improved ROM and diminished symptoms.
Treatment
In addition to the strategies described previously in the section on cervical extension syndrome, the goal for treatment of the cervical rotation-extension syndrome is to decrease the compensatory cervical extension and lateral flexion during active cervical rotation. Correction of the pattern of movement during daily activities is particularly important. Instruction in strategies to be used during functional activities, such as supporting the upper extremities, is important. Additional strategies to manage the rotation impairment include using minimal effort to rotate the head and neck to diminish the disproportionate recruitment of the extrinsic cervical rotators (scalene and sternocleidomastoid) and correcting any sustained asymmetrical positions of the head and neck. Educating the patient and diminishing movements of the head and neck as part of the patient’s body language are essential.4,6,14,15 The focus of the active exercise program in the cervical region is to improve the strength and motor control of the intrinsic cervical spine rotators.
As noted in the description of the cervical extension syndrome, upper extremity movements have a direct effect on the cervical spine via the attachment of cervicoscapular muscles. An examination and classification of the associated scapular movement impairments is critical in the management of the patients with cervical pain. Strategies to examine, classify, and manage scapular movement impairments are clearly described in Sahrmann.1
Exercise Program
Sitting with back to wall performing cervical rotation
The initial positioning for the sitting with back to wall performing cervical rotation exercise is the same as the first exercise described in the section on cervical extension syndrome. The initial instructions address impairments in adjacent regions. The upper extremities are supported on pillows to diminish the compressive loading of the cervical spine from the transfer of the weight of the upper extremities to the cervical region through the cervicoscapular muscle attachment.9,15 Each patient needs to be assessed for specific alignment impairments at the lumbar and thoracic spines and scapulothoracic region. The patient is then instructed in strategies to precisely correct individual alignment faults in these regions before proceeding with the exercise (see Figure 3-22).
The patient is then instructed to perform cervical rotation about a “vertical axis” and to avoid the compensatory movements of extension and sidebending. The therapist should encourage the patient to “easily” turn the head and neck to minimize the recruitment of the extrinsic cervical rotators. Specific instructions include “keep the chin down” and “do not lean the head and neck toward the side you are rotating toward.” Additional instructions to sidebend in the opposite direction that the patient is rotating the head, typically result in a vertical position of the head and neck and diminished ipsilateral sidebending. Maintaining the precise motion of rotation without compensatory sidebending or extension promotes an increased use of the intrinsic rotators and diminished use of the extrinsic rotators, thus reducing shear forces on the cervical spine.
As described in cervical extension syndrome, the patient is encouraged to maintain appropriate alignment of the adjacent regions during this movement of the cervical spine. This exercise can be ideally performed in sitting, but if the patient has difficulty maintaining the correct postural alignment during the cervical motion, the exercise can be performed in supine. The supine position will not be as challenging on the trunk musculature to maintain the alignment of the adjacent regions.
Supine active cervical rotation
Performance of precise cervical rotation in supine can be performed if sitting cervical rotation is too difficult or painful. The patient assumes a hook lying position with the arms supported on pillows (Figure 3-34). The patient may require a towel roll under the head. The thickness of the towel roll depends on the patient’s thoracic alignment and severity of the forward-head alignment. The greater the kyphosis and forward-head posture the greater the thickness of the towel roll. The same initial instructions to address the adjacent regions impairments as explained in the sitting exercises. The patient is then instructed in strategies to precisely correct individual alignment faults in the adjacent regions—lumbar and thoracic spines and scapulothoracic region—before proceeding with the exercise. The patient is then instructed to perform cervical rotation about a “vertical axis” and to avoid the movements of cervical extension and sidebending.
Facing wall, arms supported—active cervical rotation
An additional position of facing the wall with the arms overhead supported on the wall can be used to perform precise cervical rotation with support to the upper extremities. The patient is instructed to rest his or her forearms on the wall, allowing the wall to support the upper extremities and relaxing the upper trapezius muscles (Figure 3-35). The patient is instructed to roll the chin down slightly and then perform precise cervical rotation about a vertical axis and to avoid movements of cervical extension and sidebending.
Quadruped active cervical rotation
The alternative position of quadruped can be used to perform precise cervical rotation if the previously described positions of sitting or supine are too difficult or painful with cervical rotation motion (Figure 3-36). The patient is instructed to flatten the spine like a “table top,” align the head and cervical spine with thoracic and lumbar spine and then rotate the head and neck about an axis of motion. The patient is instructed to avoid movements of cervical extension and sidebending.
Functional Instructions
The goal for instruction in modification of functional activities of the cervical extension-rotation syndrome is to diminish cervical extension and forward translation movements, as described in the cervical extension syndrome, and to minimize asymmetrical stresses of the cervical spine during daily activities. Asymmetrical stresses may come from posturing of the cervical and/or thoracic spine in sidebend or rotation, especially during sitting activities. Asymmetrical stresses may also be imposed by unilateral movements of an upper extremity via the attachment of the cervicoscapular muscles.10
When sitting at the computer, patients are instructed to have a supportive chair with armrests that will reduce thoracic flexion and assist in maintaining good thoracic alignment. They should support their forearms on the armrests, the desk, or an extended tray for a keyboard. The armrests, desk, or tray should be at the appropriate height so that the patient does not need to “slouch” for the arms to be supported. The computer or work station should be centered to the chair so there is no prolonged posturing in rotation or sidebend of the cervical or thoracic spine.
The patient should be instructed to avoid prolonged positions of rotation or sidebend of the cervical or thoracic spine during daily activities. These positions can commonly occur while watching TV, playing video games, and so on, without the patient being aware of the posturing. Using the telephone in a prolonged cervical sidebend position is common, and the patient should be encouraged to consider the use of a head set or “blue tooth” apparatus to diminish use of the prolonged cervical sidebend position.
Additional activities on which to counsel the patient include avoiding repetitive and/or resistive one arm activities. These activities can inflict asymmetrical stresses on the cervical spine via the attachment of the cervicoscapular muscles. If the patient must continue with one-arm activities, it will be very important that he or she maintains proper alignment of the thoracic and cervical spines, especially avoiding cervical extension and/or a forward-head position during the activity. Instructing the patient to “keep the chin and nose down” will recruit the intrinsic cervical neck flexors to support the cervical spine during the one arm activities.
Case Presentation
Cervical Extension-Rotation Syndrome
Symptoms and History
A 24-year-old female student presents with a complaint of neck pain that has worsened in the last 4 months. Pain is located in the bilateral upper cervical region, right lower cervical region, and right upper trapezius muscle. She also complains of occasional numbness and tingling in the right forearm and hand. She rates her average daily pain 4/10. Pain can increase to 7/10 with prolonged sitting, working on the computer, and studying. Her neck disability index (NDI) score = 23 indicating moderate disability.50 Radiographs of the cervical spine were unremarkable.
She reports a history of chronic migraines since she was 16 years old. She averages about one migraine a month and manages the migraines with Imitrex and rest. In the last 4 months, as her neck pain has worsened, she has noted an increase frequency of migraines to 2 to 3 per month.
Alignment Analysis
In standing, she presents with a position of forward head with upper cervical extension, increased flexion at the upper thoracic region with a flat thoracic spine below and lumbar lordosis (Figure 3-37). The scapulae are positioned in abduction and slight depression. The right scapula is positioned 4 inches lateral from the spine, and the left scapula is positioned 3.5 inches lateral from the spine.
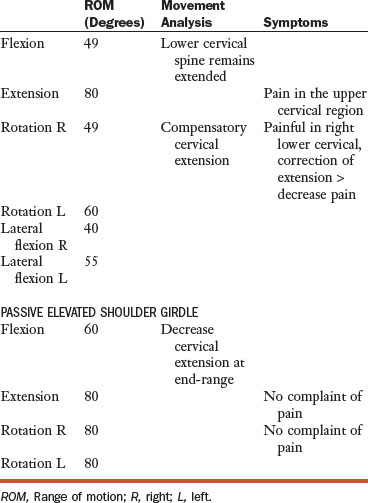
Movement Analysis and Active Range of Motion Findings
Passive mobility findings
Inspection of the posterior cervical region reveals that the left articular pillar appear more prominent than right. Central posterior to anterior (PA) pressures performed on the C5/6 and C6/7 spinous process indicate that they are hypomobile, and she complains of pain over the local area. Unilateral PA pressures on the left C5/6 and C6/7 articular pillar indicate that they are hypomobile, and she complains of pain over the local area.
Active shoulder movements
Shoulder flexion demonstrated a decreased upward rotation of scapulae: <60 degrees.49 Patient also demonstrates compensatory cervical extension and complaint of cervical pain (Figure 3-38).
The therapist corrects the starting alignment of the abducted scapulae and cervical spine extension position, then during active shoulder flexion, the therapist manually assists the scapulae into the greater upward rotation and instructs the patient to avoid compensatory cervical extension. The corrections resulted in greater scapular upward rotation and no complaint of neck pain.
Additional impairments
Supine shoulder flexion demonstrates limited shoulder motion with compensatory rib cage elevation, lumbar extension, and cervical extension (Figure 3-39).


Figure 3-39 A, Supine shoulder flexion with rib cage elevation. B, Supine shoulder flexion with correction.
The patient was then instructed to correct the starting scapular alignment by actively adducting the scapulae; to recruit lower abdominals to maintain lumbar spine alignment, and to avoid rib cage elevation and cervical extension. The patient was then instructed to actively perform shoulder flexion without compensatory motions. Shoulder flexion ROM is decreased, but she able to perform movement without compensatory motion. Passive length assessment of the latissimus dorsi bilaterally was determined to be short.8
Length test of the pectoralis minor: Passive length assessment of the pectoralis minor was determined to be short bilaterally with the right shorter than the left.8 Also noted was compensatory cervical rotation in the direction of the muscle being tested.
Manual muscle testing (MMT): The lower abdominal muscles were weak at a 2/5 level, with compensatory rib cage elevation and cervical extension during testing.1 The deep neck flexors were 2/5 muscle grade.8 The strength of the middle trapezius was determined to be 3/5 on both right and left.8
Diagnosis and Staging
The patient’s diagnosis is cervical extension-rotation syndrome with scapula abduction.1 The stage for rehabilitation is Stage 2. Her prognosis is good to excellent. Her positive moderators include her young age, overall good health, and moderate duration of symptoms. Her negative moderators include her reports of radiculopathy and long history of migraines.
| Diagnosis | Key Tests |
|---|---|
| Cervical extension-rotation | |
| Scapular abduction |
AROM, Active range of motion; ROM, range of motion.
Treatment
The patient was seen once a week for 4 weeks and then once every other week for 4 weeks. Each treatment session lasted approximately 30 minutes. The treatment included instruction in a specific home exercise program to improve cervical spine function and functional instructions to diminish excessive forces on the cervical spine during her daily activities.
Exercise program
Initially, the patient was instructed in active cervical ROM exercises. The initial “set up” for the patient was sitting in a chair with the back against the wall and the arms supported on pillows. This type of positioning diminished thoracic flexion and provided the patient with tactile feedback of “correct alignment.” The pillows allow support of the weight of the upper extremity and diminish the downward pull on the cervical spine via the attachment of the cervicoscapular muscles.9 The patient was then instructed in the following cervical exercises:
Capital flexion in sitting (see Figure 3-40): The patient was instructed to recruit the lower abdominal muscles to maintain a neutral lumbar spine alignment then correct her faulty scapular position of scapula depression and abduction. She was instructed to slightly elevate the shoulders toward the ears and then adduct the scapulae. Once she had corrected her starting alignment of her lumbar spine, thoracic spine, cervical spine, and scapulae, she was instructed to place her head close to the wall and perform capital head flexion. The patient was encouraged to “roll” the head and chin toward the base of the anterior neck while trying to maintain the head close to the wall. The verbal cue to “roll” the head is to encourage recruitment of the intrinsic cervical muscle to perform sagittal rotation rather than anterior translation. The patient reported a “tightening feeling” in the front of the neck and stretching in the back of the neck. She did not have complaints of reproduction of cervical spine pain or any complaints of peripheralization of symptoms into her arm. She was instructed to repeat the movement five times. At the completion of the repetitions, the patient reported that the exercise was difficult, but there was no increase or peripheralization of her symptoms. She reported that her neck felt “looser,” and she felt a decrease in her headache pain. She was instructed to repeat the exercise an additional five repetitions. She again reported a positive response.
Cervical rotation in sitting: The patient was instructed to position herself in the same position as in the previous exercise. This incorporated support of the upper extremities and correction of spinal and scapulae alignment, including rolling the head and chin down to the correct cervical spinal extension position. Once positioned, the patient was instructed to perform rotation. The patient was then instructed to perform cervical rotation about a “vertical axis” and to avoid the movements of extension and sidebending. Specific instructions included “keep the chin down” and “do not lean the head and neck toward the side of rotation.” Additional instructions included to sidebend in the opposite direction of the rotation, which results in a vertical position of the head and neck and diminished ipsilateral sidebending. Maintaining the precise motion of rotation without compensatory sidebending or extension promotes increased use of the intrinsic rotators and diminished use of the extrinsic rotators, thus diminishing shear and translatory forces on the cervical spine. Initially, the patient was able to perform approximately 60 degrees of pain-free rotation without compensatory cervical extension. She was reminded to keep her “nose down” during the rotation movement. Practice during the first session resulted in approximately 70 degrees of pain-free rotation without compensatory extension.
Sitting—shoulder abduction lateral rotation (see Figure 3-41, A): The patient was instructed to position herself in the same position as the previous exercises. She correctly positioned her lumbar spine, scapulae and cervical spine (capital flexion). The patient then performed shoulder abduction and lateral rotation and maintained the position by placing her arms against the wall. The patient then slid the arms up the wall (abduction-elevation), maintaining spinal alignment, especially capital flexion. The patient reported and increased muscle activity in the midthoracic region, indicating increased recruitment of trapezius, rhomboid, and thoracic spinal musculature.


Figure 3-41 A, Sitting-shoulder abduction with lateral rotation. B, Sitting-shoulder flexion with lateral rotation.
Sitting—shoulder flexion (see Figure 3-41, B): The patient was instructed to position herself as noted in the first two exercises. The patient then performed 90 degrees of shoulder flexion and lateral rotation of the humerus “palms facing each other.” The patient was then instructed to perform shoulder flexion: “reach up toward the ceiling.” The patient was instructed to “keep elbows in” to prevent humeral medial rotation, and to maintain the lumbar spine against the wall and the cervical spine in the position of capital flexion.
Supine capital flexion without head lift: In a supine position with the arms supported on pillows, the patient was instructed to recruit the lower abdominals to maintain the lumbar spine position, adduct the scapula to properly align the scapulae, and then perform capital cervical flexion without a head lift. The patient was instructed to maintain the lumbar spine and scapulae alignment during the movement of the neck. The patient should feel a stretch in the posterior neck region and a recruitment of the intrinsic cervical flexor muscles.
Supine neck flexor strengthening—with assisted head lift (Figure 3-42): The patient was instructed to roll the chin toward the front of the cervical spine and assist with her hand to roll the cervical spine off the supporting surface while maintaining the chin positioned at the anterior cervical spine. The assisting hand should be placed at the back of the head to help direct the movement of capital flexion and assist in lifting the weight of the head. The patient was encouraged to only allow enough support that permits the appropriate “curl up” position of the head and cervical spine. Progression of the exercise would be to provide less support.
Trapezius exercises in sidelying (Figure 3-43): The patient is positioned in sidelying with her head supported on a towel roll and her arm overhead. The therapist supports the arm with one hand and guides the scapula into adduction, external rotation and posterior tilt with the other hand. The patient is asked to adduct the scapula, and at the end of the scapula adduction ROM, the therapist instructs the patient to hold the weight of the arm while keeping the scapula adducted and avoiding any position of neck extension. The therapist should observe appropriate recruitment of the trapezius muscle. The patient can perform this exercise at home with her arms supported on pillows.
Wall slides: Facing the wall—shoulder flexion: The patient is instructed to face the wall and place the ulnar side of the hands on the wall with the shoulders in the flexion plane. The patient is instructed how to use correct scapulae position and bring the chin down toward the front of the neck. The patient is then instructed to slide the arms up the wall and gently push into the wall to recruit the serratus anterior while maintaining the cervical spine position. The patient should avoid any compensatory cervical extension during the movement of shoulder flexion and return from shoulder flexion.
Facing wall, arms supported—active cervical rotation (Figure 3-44): An additional position of facing the wall with the arms overhead and supported on the wall can be used to perform precise cervical rotation with support to the upper extremities. The patient is instructed to rest the forearms on the wall, allow the wall to support the upper extremities, and relax the upper trapezius muscles. The patient is instructed to roll the chin down slightly, perform precise cervical rotation about a vertical axis, and avoid movements of cervical extension and sidebending. These instructions are similar to the instructions used in cervical rotation in sitting.
Quadruped rocking back without associated extension (Figure 3-45): The patient was instructed to assume the quadruped position, flatten the spine like a “table top,” and align the head and cervical spine with thoracic and lumbar spine. She was then instructed to rock back on to her heels while maintaining a “flat spine” and “chin rolled in toward the front of the neck.” She was instructed to avoid cervical extension during the movement of rocking back. The patient had difficulty maintaining the thoracic and cervical spine position as she rocked back. Her rocking back range was limited to the range in which there was no spinal movement.
Functional Instruction
The patient was encouraged during sitting activities to support the arms and periodically recruit abdominals and scapular posterior tilt and external rotation muscles, while maintaining neutral neck position with the chin and nose slightly down.5 She was encouraged to use a chair that would support her thoracic spine and not allow thoracic flexion.11 She was instructed in proper use of eyeglasses to allow a neutral neck position during computer use. The instructions were directed to diminish upper cervical extension and forward translation.2 She was also instructed in the typical “gestures” and “habits” of cervical extension that she demonstrated during the examination while she was communicating and expressing herself. She was instructed in strategies to diminish these habits during her day.
At the end of 4 weeks of treatment (4 treatment sessions), the patient reported no episodes of numbness/tingling in her forearm or hand. She reported only 1 migraine headache during the 4-week period (previously 2 to 3 a month). She rated her daily average pain 2/10 and also 2/10 with prolonged sitting at a computer. Her NDI score was 14, indicating minimum disability. At the end of 8 weeks of treatment (6 treatment sessions), she reported her daily average pain 0/10 and occasional pain (2/10) if she sat more than 2 hours at the computer without a break or did not support her arms during the sitting activity. Her headache behavior was now typical of what she experienced before the recent neck pain flare-up, or one migraine a month. She reported that she was using her eyeglasses properly while working on her computer and had become more “aware” of her gestures and habits that contribute to stress on her cervical spine. She was making an effort to diminish cervical extension movements during her daily activities. She continued to remind herself to keep her “nose down” to avoid excessive extension.
This case is a useful illustration of the importance of addressing the adjacent regions, shoulders and thoracic spine, when treating a patient with cervical extension-rotation syndrome and associated headache. Alignment, length, and strength of muscles in the adjacent region are critical to address before attending to the cervical movement impairments. In addition, demonstrating to the patient that she had a tendency to frequently move in the direction of extension rotation and teaching her that this movement needed to be reduced during her daily activities helped alleviate her pain. Patient awareness of her daily movement habits and postures is essential in managing her symptoms and possible future flare-ups. Essential components for management of her problem included (1) improving the strength of her scapula posterior tilt and external rotator muscles, serratus anterior, rhomboids, and middle trapezius to maintain appropriate alignment of her scapula. Improving the participation of the serratus anterior muscle reduces the loading from the cervicoscapular muscles on the cervical spine and increases the support from the axioscapular muscle for the weight of her upper extremities. Proper support of her upper extremities is necessary for decreasing the compressive load on the cervical spine structures and allows pain-free motion of the cervical spine.44 Improving the strength and recruitment of her abdominal muscles supports the appropriate alignment of her lumbar spine and rib cage during movements of the extremities and neck. Education in the patient’s preferred daily habits and postures contribute to stress on cervical spine structures. All of these components contributed to a successful outcome and enabled her to manage her symptoms.
Cervical Flexion Syndrome
The principal movement impairment in cervical flexion syndrome is imprecise cervical flexion that is often associated with pain and limited ROM. There is an altered distribution of flexion across the cervical and thoracic regions, with the lower cervical region flexing more than the upper thoracic region. The imbalance of muscle performance of the cervical flexors with dominance of intrinsic cervical flexors can create a kyphotic position of the cervical spine and/or insufficient recruitment of cervical extensors during cervical extension movements.
History and Symptoms
Symptom location can be similar to the findings in cervical extension syndrome. The patient complains of pain with flexion. This syndrome is typically seen in younger patients because their spines have the flexibility and extensibility to move in the direction of flexion. The patients that demonstrate this syndrome characteristically have a history of activities that require repetitive positioning in “correct alignment.” They may be required to maintain a “military posture” or a ballet position that may necessitate extreme “straightening” or flexing of the cervical spine.
Key Signs and Symptoms
Alignment Analysis
Alignment faults for cervical flexion include a decrease of the normal cervical inward curve. The cervical spine may appear flat (Figure 3-46). The patients with this syndrome may also have associated thoracic alignment fault of a decreased thoracic curve. The reduced flexion curve in the thoracic spine is typically associated with loss of flexion ROM in the thoracic region. The reduced thoracic flexion curve may influence or require greater flexion motion in the cervical region. There may also be scapular alignment faults, including scapular depression and/or downward rotation. Frequently, specific verbal cueing and manual assistance to promote thoracic flexion and cervical extension can diminish symptoms during standing. The patient can be encouraged to assume a “slumped position” to promote an increase in thoracic flexion and instructed to slightly lift the chin and nose to encourage a position of less cervical flexion. These directions can result in a normal curve of the thoracic spine and a normal inward curve of the cervical spine, which can result in a decrease in symptoms in standing or sitting.
Movement Impairment Analysis
During the performance of active cervical flexion in standing, patients complain of pain and demonstrate greater motion of flexion in the lower cervical region than the upper thoracic region (Figure 3-47).
Secondary test
Correction by increasing thoracic flexion: During active cervical flexion the therapist encourages greater flexion motion in the upper thoracic region and limits the amount of cervical flexion ROM, resulting in decreased pain. One strategy to achieve greater thoracic flexion can include an instruction to the patient to “slump” or flex the thoracic spine before initiating active cervical flexion.
Muscle Strength and Performance
Poor performance and recruitment of the intrinsic cervical extensors are primarily demonstrated in the prone and/or quadruped position. During performance of active cervical extension, there is poor recruitment of the intrinsic cervical extensors and dominant recruitment of the extrinsic cervical extensors, primarily the levator scapulae. The cervical extension movement results in greater posterior translation and diminished posterior sagittal rotation.
Secondary tests
Correction by increasing recruitment of intrinsic cervical extensors: Repeating the movement of cervical extension in prone or quadruped position with verbal cues to “roll the head back” typically results in improved recruitment of the intrinsic cervical spinal extensors and diminished recruitment of the extrinsic cervical extensors. The modified extension movement results in greater posterior sagittal rotation and less pain.
Performance of cervical flexors: There is excessive recruitment of all neck flexors, particularly the recruitment of anterior and middle scalene during use of the arms or during daily activities or personality gestures. The therapist observes excessive straightening of the cervical spine.
Correction by improving recruitment of intrinsic cervical extensors: Instruct the patient to lift the chin and nose to promote the appropriate recruitment of cervical extensors and assumption of a normal inward curve during arm movements.
Treatment
The primary goals in the treatment of cervical flexion syndrome are to restore a normal inward cervical curve, improve function of the intrinsic cervical extensors, and to avoid positions and movements that would encourage excessive cervical flexion. A common alignment fault associated with cervical flexion is a reduced thoracic curve. The straight thoracic spine has decreased flexibility in the direction of flexion, which potentially results in compensatory flexion in the cervical flexion. Treatment strategies include instructing the patient on how to increase thoracic flexion or encouraging the patient to “slump,” which is not a typical functional instruction but appropriate if the patient’s thoracic impairments necessitate these instructions.
Exercise Program
The key exercises to improve intrinsic cervical extensor function include exercises that can be performed in prone and/or quadruped.
Prone active cervical extension
In prone or in quadruped, the patient is instructed to “roll” head and neck back in the direction of extension (Figure 3-48). The verbal cue of rolling is to facilitate the recruitment of the intrinsic neck extensors and reduce recruitment of the extrinsic neck extensors. The patient is encouraged not to reach full end-range extension to avoid excessive compression on the cervical facets and discs.
Quadruped active cervical extension
The quadruped position can be a more difficult exercise because the exercise requires good axioscapular muscle function while weight bearing through the upper extremities (Figure 3-49). When performing the cervical extension exercise in the quadruped, the patient is encourage to perform the movement in the middle third of the ROM to avoid end-range extension or flexion.
The description of treatment for the previous diagnoses indicates that examination and classification of associated scapular movement impairments is critical in the management of the patients with cervical pain. Strategies to examine, classify, and manage scapular movement impairments are clearly described in Sahrmann.1
Functional Instructions
Instructions during key functional activities of patients with the cervical flexion syndrome include encouraging flexion in adjacent regions to minimize the amount of cervical flexion that is required during daily activities. This includes encouraging the patient to “slump” or increase thoracic flexion to diminish the amount of cervical flexion that is required. This strategy is the opposite instruction and effect that the therapist would use with a patient with cervical extension syndrome with a thoracic kyphosis. When the patient attempts to slump, it may initially feel very awkward and unfamiliar. The patient may have conscientiously worked to maintain correct alignment, but overcompensated with excessive thoracic extension that then required excessive cervical flexion to maintain the eyes and head in a functional position. Allowing greater flexion in the thoracic spine will reduce the cervical flexion. The instructions of “slumping” can make the patient feel self-conscious about his or her appearance. Using a mirror to demonstrate that the strategy does not result in excessive thoracic flexion or kyphosis can be very useful in reassuring the patient that he or she is not going to develop the type of alignment characteristic of the elderly.
To avoid excessive cervical flexion and translation during sitting activities, the patient can be encouraged to lean forward by increasing the degree of hip flexion.
Strategies to diminish excessive cervical flexion during daily activities include raising the computer screen or using a book holder to raise the work items so that the patient does not have to flex the cervical spine as far.
Additional functional instructions include use of cervical pillow or towel to support the cervical spine in a cervical lordosis. This can be helpful with sleeping or prolonged sitting and computer work. The support of the cervical spine should be provided in both the supine and sidelying positions.
The therapist should review use of eyeglasses. The habit the patient may demonstrate is excessive flexion to position his or her eyes with the use of reading glasses. The patient will be encouraged to properly position the glasses on the nose that will allow a neutral position of the neck so the patient has to raise the nose and chin when using the glasses.
Cervical Flexion-Rotation Syndrome
The principal movement impairment in cervical flexion-rotation syndrome is imprecise cervical rotation with associated compensatory cervical flexion, which is often associated with pain and limited ROM. The imbalance of muscle performance among the cervical rotator muscles with extrinsic muscles contributes to multiplanar movements rather than precise uniplanar motion produced by the intrinsic rotators. An imbalance of muscle performance of the cervical flexors contributes to compensatory flexion movement during performance of rotation. The contributing factors in the cervical rotation-flexion syndrome include weight of the extremities and alignment of the thoracic spine and the scapulae. There may also be asymmetries in the appearance of the neck and scapula region.
Symptoms and History
Symptoms and history can be similar to the findings found in cervical flexion syndrome. In addition, the patient with this syndrome may report pain with rotation movements.
Key Tests and Signs
Alignment Analysis
In addition to the alignment faults that were noted in the cervical flexion syndrome, the cervical spine may also be in a sidebend and/or rotated position. Commonly, this position may be an indication of a hearing or vision impairment, as discussed in the section on cervical extension-rotation syndrome. The therapist should obtain this information when taking the history. Asymmetrical alignment of the scapulae may also be present. Verbal cueing and manual assistance to correct alignment of the cervical spine position and scapulae position can decrease symptoms. Use of a mirror is also a helpful tool for patient feedback and independent correction.2
Movement Impairment Analysis
In addition to the movement impairments noted in the section on the cervical flexion syndrome, the patient can complain of pain with rotation and demonstrate associated cervical flexion and sidebending movements during rotation.
Secondary tests
Secondary follow-up tests can include several strategies, including repeating active rotation without associated flexion and/or sidebending movement. In addition, instructing the patient to “slump” before performing active rotation can promote an improved starting alignment of the cervical spine with reduced cervical flexion. Other corrections include passive support of the upper extremities during performance of active rotation and/or the therapist can passively assist the cervical vertebrae and guide precise rotation motion.
During active single arm flexion, rotation of a single or multiple vertebrae are noted via palpation of the cervical spinous process. The patient does not typically complain of pain. An alternative finding during single-arm flexion is compensatory sidebending or rotation of the cervical spine.10
Correction of this rotation movement impairment can be difficult. Several strategies can be attempted, as follows:
Treatment
The primary goals of treatment for cervical flexion-rotation syndrome are similar to the goals of cervical flexion syndrome, which are to restore the normal cervical inward curve, instruct the patient in strategies to avoid excessive flexion in the cervical spine, and encourage increase flexion movements in other regions, usually the thoracic spine. Additional treatment includes restoration of precise motion of active cervical rotation by performing motion without associated flexion and using minimal effort to rotate the head and neck. The focus of the active strengthening exercise program in the cervical region is to improve the strength and motor control of the intrinsic cervical spine rotators. Correcting sustained asymmetrical positions of the head and neck and avoiding movements of the head and neck as part of body language is essential.
Additionally, as described in the treatment section for cervical extension syndrome, the patient is instructed in functional activities such as supporting the upper extremities.5,6,14,15 Correction of the pattern of movement during daily activities is particularly important. An examination and classification of the associated scapular movement impairments is critical in the management of the patients with cervical pain. Strategies to examine, classify, and manage scapular movement impairments are clearly described in Sahrmann.1
Exercise Program
Sitting Cervical Rotation
The patient may not need to assume the position of sitting with the back to the wall as has been previously described for the cervical extension syndrome. Sitting in a chair with good thoracic spine support may be appropriate and may encourage a normal thoracic alignment of slight flexion and discourage a flat thoracic spine. As described in cervical flexion syndrome, an exaggerated straightening or reduced flexion of the thoracic spine may result in compensatory flexion of the cervical spine. Initial instructions address the impairments of adjacent regions, which were previously described. The upper extremities are supported on pillows to diminish the compressive loading of the cervical spine from the transfer of the weight of the upper extremities to the cervical region through the cervicoscapular muscle attachment.9,15 Each patient needs to be assessed for his or her specific alignment impairments at the lumbar and thoracic spines and scapulothoracic region. The patient is then instructed in strategies to precisely correct his or her individual alignment faults in these regions before proceeding with the exercise.
The patient is then instructed to perform cervical rotation about a “vertical axis” and to avoid the movements of flexion and sidebending. Specific instructions include “raise the chin up slightly” to avoid compensatory flexion during rotation and “do not lean the head and neck toward the side to which you are rotating.” Additional instructions to sidebend in the opposite direction that the patient is rotating his or her head typically result in a vertical position of the head and neck and diminished ipsilateral sidebending. Maintaining the precise motion of rotation without compensatory sidebending or flexion promotes increased use of the intrinsic rotators and diminished use of the extrinsic rotators, thus diminishing shear and translatory forces on the cervical spine.
The patient is encouraged to maintain appropriate alignment of the adjacent regions during this movement of the cervical spine. This exercise can be ideally performed in sitting, but if the patient has difficulty maintaining the correct postural alignment during the cervical motion, the exercise can be performed in supine. The supine position will not be as challenging as control by the trunk musculature in maintaining alignment of the adjacent regions.
Supine active cervical rotation
Performance of precise cervical rotation in supine can be performed if sitting cervical rotation is too difficult or painful. The patient assumes a hooklying position with the arms supported on pillows. The patient may require a towel roll under the cervical spine to support a normal cervical curve and prevent a position of excessive flexion. The same instructions used for the sitting exercises can be used to address the adjacent regions impairments. The patient is then instructed in strategies to precisely correct his or her individual alignment faults in the adjacent regions (lumbar and thoracic spines and scapulothoracic region) before proceeding with the exercise. The patient is then instructed to perform cervical rotation about a “vertical axis” and to avoid the movements of cervical flexion and sidebending. Other key verbal cues are similar to ones used for the sitting exercises: “raise the chin up slightly” to avoid compensatory flexion during rotation and “do not lean the head and neck toward the side you are rotating toward.”
Quadruped active cervical rotation
The alternative position of quadruped can be used to perform precise cervical rotation if the previously described positions of sitting or supine are too difficult or painful with cervical rotation motion (see Figure 3-36). The patient is instructed to allow the thoracic spine to be slightly flexed. The patient should raise the head and chin slightly to avoid a position of excessive flexion of the cervical spine. The patient is instructed to rotate the head and neck about an axis of motion. The patient is instructed to avoid movements of cervical flexion and sidebending.
Facing wall, arms supported—active cervical rotation
An additional position of facing the wall with the arms overhead supported on the wall can be used to perform precise cervical rotation (see Figure 3-35). The patient is instructed to rest the forearms on the wall, allow the wall to support the upper extremities, and relax the upper trapezius muscles. The patient is then instructed to raise the head and chin slightly to avoid the position of excessive cervical flexion, then perform precise cervical rotation about a vertical axis, and to avoid movements of cervical flexion and sidebending.
Functional Instructions
Key functional instructions for cervical flexion rotation syndrome include the strategies described in the section on cervical flexion syndrome to encourage flexion in the thoracic spine, which can minimize the amount of cervical flexion that is required during daily activities. In addition, strategies should be implemented to minimize asymmetrical stress on the cervical spine through decreasing repetition of one arm activities or prolonged positioning in sidebend or rotation (see section on Cervical Extension-Rotation Syndrome).
Case Presentation
Cervical Flexion-Rotation Syndrome
History and Symptoms
A 26-year-old male complains of lower cervical neck and right upper trapezius pain that is increased with sustained sitting postures working at the computer. He rates his pain 2/10 at rest and 4/10 with neck movements. His NDI score = 14, indicating mild disability. He reports that in high school he was a competitive swimmer and presently enjoys surfing.
Alignment
In standing, he has a swayback posture, with the thoracic region swayed posterior.8 The spinal alignment was remarkable for a reduced curve in the cervical region and also a reduced curve or “flat” thoracic spine (Figure 3-50, A). The clavicular alignment appears horizontal with a diminished upward slope of the distal end of the clavicle. The scapulae were in a position of depression with the superior angle of scapula positioned below T28 (see Figure 3-50, B).
Reduced muscle bulk was noted in the cervical paraspinal musculature. He also complained of pain on palpation of right upper trapezius and levator scapulae muscles.
Movement Analysis and Active Range of Motion Findings
Active ROM test results are given in the following table.
Passive mobility findings
Central PA pressure performed on the C4/5 and C5/6 spinous process indicated they were hypomobile and painful over the local area. Unilateral PA pressures on the right C4/5 and C5/6 articular pillar indicated that these areas were hypomobile and caused pain over the local area.
Active shoulder movements
Shoulder flexion demonstrated decreased scapulae elevation with the result of decrease upward rotation of the scapulae. Also noted was associated cervical flexion with active shoulder flexion and an increase of the posterior thoracic sway.
The therapist corrected the cervical starting alignment by having the patient lift the chin and nose slightly and maintain head and neck position during shoulder flexion. In addition, the starting scapulae alignment and thoracic sway were corrected, and he was cued to maintain the thoracic position and elevate the scapulae during shoulder flexion. The patient was able to correct the movement impairments during shoulder flexion but he reported difficulty performing this motion.
Single-arm flexion monitoring cervical spine: Palpation of the lower cervical vertebrae during left shoulder flexion demonstrated compensatory rotation of the spinous process to the left. These findings indicated relative flexibility of the lower cervical segments in the direction of rotation with left arm movements. No compensatory motion of lower cervical rotation was noted with right arm movements. There was no complaint of neck pain with either arm movements. Bilateral shoulder flexion did not cause cervical rotation.
Diagnosis and Staging
The patient’s diagnosis is cervical flexion rotation with scapula depression and the stage for rehabilitation is Stage 3. His prognosis is excellent. His positive moderators include young age, good health, minimal duration of symptoms, and low NDI score.
| Diagnosis | Key Tests |
|---|---|
| Cervical flexion rotation | |
| Scapular depression |
AROM, Active range of motion; ROM, range of motion.
Treatment
The patient was seen once a week for 2 weeks and then once every other week for 4 weeks. Each treatment session lasted approximately 30 minutes. The treatment included instruction in a specific home exercise program to improve cervical spine function and functional instructions to diminish excessive forces on the cervical spine during daily activities.
Exercise program
Initially, the patient was instructed in active cervical ROM exercises. The initial “set up” for the patient was sitting a chair but not with his back against the wall as was described in the cervical extension case presentation. The patient arms were supported on pillows to decrease the downward pull on the neck and to improve scapulothoracic alignment by diminishing the amount of scapulae depression. The patient was also instructed to “relax” the thoracic spine to allow greater thoracic flexion.
Cervical rotation: The patient was instructed to support his arms on the pillows and relax the trapezius muscles. The patient was then instructed to rotate the head and neck about a vertical axis. The patient was instructed to imagine that there is “a pole” down his spine and rotate about that pole. The patient was also instructed to keep his nose and chin up to avoid compensatory flexion during active cervical rotation and to minimize the effort during the rotation to diminish recruitment of the extrinsic neck rotators (sternocleidomastoid and scalene) and compressing on the stabilizing force of the contracting muscles.
Additional exercises
Additional exercises to improve intrinsic cervical extensor muscle function include the following:
Prone cervical extension to improve the strength and recruitment of the intrinsic cervical extensors (see Figure 3-48): The patient is positioned prone with his forehead resting in the palm of his hands. The patient is to perform active cervical extension by “rolling” the head and neck back in the direction of extension but not to end-range. The patient is instructed to imagine an “axial running through the middle of his cervical spine” and rotate about the axial as he performs active extension. The therapist should observe if the patient is properly recruiting the intrinsic neck extensors and not excessively recruiting the extrinsic muscles (levator scapulae and upper trapezius).
Quadruped active cervical extension (see Figure 3-49): An alternative exercise that can improve cervical extensor function is to perform the previously described motion in the quadruped position. The patient is encouraged to avoid excessive thoracic extension and assume slight thoracic flexion. The patient is to perform active cervical extension by “rolling” the head and neck back in the direction of extension but not to end-range. The patient is instructed to imagine an “axial running through the middle of his cervical spine” and rotate about the axial as he performs active extension. The therapist should observe if the patient is properly recruiting the intrinsic neck extensors and not excessively recruiting the extrinsic muscles (levator scapulae and upper trapezius). The patient is also instructed to “roll” his head and neck forward as he returns from cervical extension. The patient is instructed to perform the movement of flexion and extension with precision and in the middle-third of the range, avoiding end-range extension or flexion.
Facing the wall—shoulder flexion with scapula elevation (Figure 3-51): This exercise improves strength and length of the upper trapezius and serratus anterior muscles.51 The patient’s scapulae position was determined to be in a position of depression, which results in a lengthened upper trapezius muscle. The objective of the exercise is to strengthen the upper trapezius muscle in a shortened position. The patient is instructed to face the wall and rest his hands on the wall just above shoulder level. As he slides his hands up the wall, he is instructed to elevate the scapula/acromion toward his ears. He is instructed to “keep his nose and chin slightly up” to avoid cervical flexion. In addition, he can return from flexion, slide his hands down while maintaining the scapulae in an elevated position and not allow excessive depression while returning from the flexion position.
Functional Instruction
During sitting activities, the patient is encouraged to “Slump!” He is encouraged not to attempt to have a very straight thoracic spine and to relax the neck position. He is encouraged to allow the chin and nose to be slightly up. The patient may feel that he is excessively slumped because he is accustomed to being very straight. A mirror can provide visual feedback that the correction does not result in excessive slumping but rather appropriate alignment of thoracic and cervical spines. In addition, the patient is encouraged to support the arms on pillows or the desk to minimize the downward pull on the upper trapezius and levator scapulae muscles. The patient is instructed in a strategy of allowing the thoracic spine to flex, which will also minimize excessive flexion in the cervical spine.
The patient was also instructed in the appropriate cervical and head positions when using his eyeglasses. The patient is to position his eyeglasses to allow a neutral neck position during computer use and should exaggerate a flexed cervical position.
The patient was also instructed to minimize one-arm activities with the left arm to avoid compensatory lower cervical rotation. When possible, he should consider using the right arm or both arms with functional activities.
At end of 6 weeks of treatment (4 treatment sessions), the patient reported 0/10 pain at rest and with movements of the neck. His neck disability index score = 4, indicating no disability. He also reported that he was doing his exercises several times a week, but he found that the functional instructions were the most helpful in managing his symptoms. He found that supporting his arms during the day, relaxing his upper back, and trying not to sit up too straight decreased the stress through his neck region.
This case is an illustration of how excessive motion in one region of the spine and lack of motion in adjacent regions can increase stress on the spinal tissue that demonstrates excessive motion. This patient’s attempts for “correct” posture were exaggerated. The flat thoracic spine and loss of a normal thoracic curve did not permit proper neck alignment. Relaxing the upper back to allow some flexion also allows the cervical spine to acquire a normal lordotic curve of the cervical spine. It was important that the patient avoid excessive flexion and encourage extension or a normal inward curve of the cervical spine. This acquired posture allows appropriate distribution of stresses across the spine. In addition, support of the upper extremities and improving the alignment of the scapulae into an elevation out of a depressed position also decreased the compressive load on the cervical spine structures.
1 Sahrmann SA. Diagnosis and treatment of movement impairment syndromes. St Louis: Mosby; 2002.
2 Willford CH, Kisner C, Glenn TM, et al. The interaction of wearing multifocal lenses with head posture and pain. J Orthop Sports Phys Ther. 1996;23:194-199.
3 Bexander CS, Mellor R, Hodges PW. Effect of gaze direction on neck muscle activity during cervical rotation. Exp Brain Res. 2005;167:422-432.
4 Schuldt K, Ekholm J, Harms-Ringdahl K, et al. Effects of changes in sitting work posture on static neck and shoulder muscle activity. Ergonomics. 1986;29:1525-1537.
5 Schuldt K, Ekholm J, Harms-Ringdahl K, et al. Effects of arm support or suspension on neck and shoulder muscle activity during sedentary work. Scand J Rehabil Med. 1987;19:77-84.
6 Straker L, Burgess-Limerick R, Pollock C, et al. The effect of forearm support on children’s head, neck and upper limb posture and muscle activity during computer use. J Electromyogr Kinesiol. 2008;19(5):965-974.
7 Otis CA. Kinesiology: the mechanics and the pathomechanics of human movement. Philadelphia: Lippincott Williams & Wilkins; 2004.
8 Kendall FP, McCreary EK, Provance P. Muscles: testing and function, ed 4. Baltimore: Williams & Wilkins; 1993.
9 McDonnell MK, Sahrmann SA, Van Dillen LR. A specific exercise program and modifications of postural alignment for treatment of cervicogenic headache: a case report. J Orthop Sports Phys Ther. 2005;35(1):3-15.
10 Takasaki H, Hall T, Kaneko S, et al. Cervical segmental motion induced by shoulder abduction assessed by magnetic resonance imaging. Spine. 2009;34(3):E122-E126.
11 Black KM, McClure P, Polansky M. The influence of different sitting positions on cervical and lumbar posture. Spine. 1996;21(1):65-70.
12 Kebaetse M, McClure P, Pratt NA. Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch Phys Med Rehabil. 1999;80:945-950.
13 Ludewig PM, Cook TM. The effect of head position on scapular orientation and muscle activity during shoulder elevation. J Occup Rehab. 1996;6(3):147-158.
14 Van Dillen LR, McDonnell MK, Susco TM, et al. The immediate effect of passive scapular elevation on active cervical rotation range of motion and symptoms in patients with neck pain. Clin J Pain. 2007;23(8):641-647.
15 Andrade GT, Azevedo DC, Lorentz ID, et al. Influence of scapular position on cervical rotation range of motion. J Orthop Sports Phys Ther. 2008;38(11):668-673.
16 Harrison DD, Harrison DE, Janik TJ, et al. Modeling of the sagittal cervical spine as a method to discriminate hypolordosis: results of elliptical and circular modeling in 72 asymptomatic subjects, 52 acute neck pain subjects, and 70 chronic neck pain subjects. Spine. 2004;29(22):2485-2492.
17 Falla D, Jull G, Russell T, et al. Effect of neck exercises on sitting posture in patients with chronic neck pain. Phys Ther. 2007;87:4.
18 Fernandez-de-las-Penas C, Alonso-Blanco C, Cuadrado ML, et al. Forward head posture and neck mobility in chronic tension-type headache: a blinded, controlled study. Cephalagia. 2005;26:314-319.
19 Neumann DA. Kinesiology of the musculoskeletal system: foundations of rehabilitation. St Louis: Mosby; 2002.
20 Porterfield JA, DeRosa C. Mechanical neck pain: perspectives in functional anatomy. Philadelphia: WB Saunders; 1995.
21 Allia P, Gorniak G. Human ligamentum nuchae in the elderly: its function in the cervical spine. J Man Manip Therapy. 2006;14(1):11-21.
22 Fernandez-de-las-Penas C, Cuadrado ML, Pareja JA. Myofascial trigger points, neck mobility and forward head posture in unilateral migraine. Cephalagia. 2006;26:1061-1070.
23 White AA, Panjabi MM. Kinematics of the spine. In: Cooke DB, editor. Clinical biomechanics of the spine. Philadelphia: JB Lippincott, 1990.
24 Lysell E. Motion in the cervical spine. Acta Orthop Scand. 1969;123(Suppl):1-61.
25 Salo PK, Hakkinen AH, Kautiainen H, et al. Quantifying the effect of age on passive range of motion of the cervical spine. J Orthop Sports Phys Ther. 2009;39(6):478-483.
26 Lehto IJ, Tertti MO, Komu ME, et al. Age-related MEI changes at 0.1 T in cervical discs in asymptomatic subjects. Neuroradiology. 1994;36(1):49-53.
27 Dvorak J, Antinnes J, Panjabi M, et al. Age and gender related normal motion of the cervical spine. Spine. 1992;17:393-398.
28 Netzer O, Payne VG. Effects of age and gender on functional rotation and lateral movements of the neck and back. Gerontology. 1993;39:320.
29 Matsumoto M, Fujimura Y, Suzuki N, et al. MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br. 1998;80:19-24.
30 Joosab M, Torode M, Rao PV. Preliminary findings on the effect of load-carrying to the structural integrity of the cervical spine. Surg Radiol Anat. 1994;16:393-398.
31 Moroney S, Schultz AB, Miller JA. Analysis and measurement of neck loads. J Orthop Res. 1988;6:713-720.
32 Simpson AK, Biswas DBA, Emerson JW, et al. Quantifying the effects of age, gender, degeneration, and adjacent level degeneration on cervical spine range of motion using multivariate analyses. Spine. 2008;33(2):183-186.
33 Falla D, Jull G, Dall’Alba P, et al. An electromyographic analysis of the deep cervical flexor muscles in performance of craniocervical flexion. Phys Ther. 2003;83:899-906.
34 Beazell JR. Dysfunction of the longus colli and its relationship to cervical pain and dysfunction: a clinical case presentation. J Man Manipulative Ther. 1998;6(1):12-16.
35 Watson DH, Trott PH. Cervical headache: an investigation of natural head posture and upper cervical flexor muscle performance. Cephalalgia. 1993;13:272-284.
36 Placzek J. The influence of the cervical spine on chronic headache in women: a pilot study. J Manual Manipulative Ther. 1999;7(1):33-39.
37 Jull G, Kristjansson E, Dall’Alba P. Impairment in the cervical flexors: a comparison of whiplash and insidious onset cervical spine pain patients. Manual Ther. 2004;9:89-94.
38 Falla D, Jull G, Hodges P, et al. An endurance-strength training regime is effective in reducing myoelectric manifestations of cervical flexor muscle fatigue in females with chronic cervical spine pain. Clin Neurophysiol. 2006;117:828-837.
39 Anderson JS, Hsu AW, Vasavada AN. Morphology, architecture and biomechanics of human cervical multifidus. Spine. 2005;30(4):E86-E91.
40 Siegmund GP, Blouin JS, Carpenter MG, et al. Are cervical multifidus muscles active during whiplash and startle? An initial experimental study. BMC Musculoskel Disord. 2008;9:80.
41 Johnson G, Bogduk N, Nowitzke A, et al. Anatomy and actions of the trapezius muscle. Clin Biomech. 1994;9:44-50.
42 Dwyer A, April C, Bogduk N. Cervical zygapophyseal joint pain patterns. Spine. 1990;15:453-457.
43 Sobush DC, Simoneau GG, Dietz KE, et al. The Lennie test for measuring scapular position in healthy young adult females: a reliability and validity study. J Orthop Sports Phys Ther. 1996;23:39-50.
44 Azevedo D, de Lima Pires T, de Souza Andrade F, et al. Influence of scapular position on the pressure pain threshold of the upper trapezius muscle. Eur J Pain. 2007;12(2):226-232.
45 Jull G, Barrett C, Magee R, et al. Further clinical clarification of the muscle dysfunction in cervical headache. Cephalalgia. 1999;19:179-185.
46 O’Leary S, Jull G, Kim M, et al. Specificity in retraining craniocervical flexor muscle performance. J Orthop Sports Phys Ther. 2007;37:3-9.
47 O’Leary S, Falla D, Elliott JM, et al. Muscle dysfunction in cervical spine pain: implications for assessment and management. J Orthop Sports Phys Ther. 2009;39(5):324-333.
48 Jull G, Trott P, Potter H, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine. 2002;27:1835-1843.
49 Ludewig PM, Phadke V, Braman JP, et al. Motion of the shoulder complex during multiplanar humeral elevation. J Bone Joint Surg Am. 2009;91:378-389.
50 Vernon H, Mior S. The neck disability index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409-415.
51 Hardwick DH, Beebe JA, McDonnell MK, et al. A comparison of serratus anterior muscle activation during a wall slide exercise and other traditional exercises. J Orthop Sports Phys Ther. 2006;36(12):903-910.