Evaluation and Treatment of Visual Deficits Following Brain Injury
Role of vision in the adaptation process
An overview of visual processing within the central nervous system
Framework for assessment and treatment of visual perceptual dysfunction
Occupational therapy evaluation
Occupational therapy intervention
Occupational therapy assessment and intervention for specific visual impairments
Disruption of the ability to focus an image on the retina
Disruption of the ability of the retina to process the image
Disruption of the ability of the optic nerve to send the retinal image
Occupational limitations caused by reduced visual acuity
After studying this chapter, the student or practitioner will be able to do the following:
1 Describe the role that vision plays in enabling a person to complete daily occupations.
2 Describe how visual input is processed within the central nervous system to turn raw visual data into cognitive concepts of space and form through the process of visual perception.
3 Describe the concept and features of the visual perceptual hierarchy as a framework for assessment and treatment of visual perceptual dysfunction.
4 Describe how assessment is used to link visual performance and process deficits to limitations in daily occupations.
5 Describe how the sensory functions of visual acuity, visual field, oculomotor control, visual attention, and visual scanning change following brain injury.
6 Describe how the sensory functions of visual acuity, visual field, oculomotor control, visual attention, and visual scanning contribute to engagement in daily occupations.
7 Describe how to assess and develop intervention plans for deficits in visual acuity, visual field, oculomotor control, visual attention, and visual scanning.
8 Describe how to modify the client’s environment to increase visibility and facilitate engagement in daily occupations.
An understanding of visual perceptual dysfunction after a CVA and traumatic brain injury must be preceded by the realization that visual perception is a process used by the central nervous system (CNS) to adapt to context and complete daily occupations. Visual perception is not a series of discrete perceptual skills or the function of a single sensory modality, but rather a process that integrates vision with other sensory input for adaptation and survival.55,62,81,120 The activities that a person performs in a day dictates the visual perceptual processing needed. Whether a client has a visual perceptual deficit after a brain injury will depend on whether the ability to process visual information has been altered such that it prevents performance of a necessary daily activity or occupation.
Role of Vision in the Adaptation Process
According to Ayres,6 the overall function of the brain is to filter, organize, and integrate sensory information to make an adaptive response to the context surrounding the person. The brain or CNS receives a variety of sensory information, including visual, proprioceptive, tactile, vestibular, and auditory. Vision is used with information from these other sensory systems to adapt to the situational context—to act on it and to manipulate, mold, and improve it. In adapting, the CNS combines the isolated bits of sensory information that it receives and integrates them to form a picture. This picture, created by sensory input, becomes the context of a situation, and an individual uses this context to make decisions and formulate plans to respond to various situations.
Successful adaptation depends on the ability to anticipate situations and contexts. The key to survival is to stay one step ahead of circumstances, whether working with clients or navigating rush-hour traffic. Anticipation enables an individual to plan for situations and increases the chance of a successful outcome. Anticipation and planning are driven by the sensory context of a person’s circumstances, for example, “It looks like rain, so I’d better take an umbrella,” or “It’s dark in there, so I’d better take a flashlight.” When visual input is present, it dominates the sensory context for the simple reason that vision takes us farther into the environment than any of our other senses do. We can see lightning before we hear thunder and see a car careening toward us before we hear the squeal of the tires or smell the exhaust. By warning us of changes in our environment, vision enables us to anticipate developing situations and formulate a plan to handle them. So when an object is unexpectedly flung in our direction, we duck, or when we see a banana peel on the floor, we walk around it.
The decision-making process guided by vision is not limited to avoiding objects. We also rely on vision to “size up” situations. We say to ourselves, “He looks harmless,” or “That looks delicious.” Our language is peppered with phrases that reflect the importance of vision in decision making, such as “I’ll believe it when I see it,” “I’ll keep an eye out for it,” or “I can see what you mean.” Vision plays an important role in social communication by enabling a person to “read” and respond to the subtle gestures and facial expressions used to communicate emotional content in conversations. Vision also plays an important role in motor and postural accommodation by warning of upcoming challenges to postural control, such as the presence of a curb or a curb cut, and by alerting us to needed information, such as the “exit” sign.
Vision has the power to convey large amounts of detailed information in milliseconds. Although we are able to instantly identify an object with vision, we would require many more milliseconds to identify the same object tactually or by hearing a verbal description of it. This explains the power of television as a medium for conveying information and why we rush to view the television when we hear about a significant event such as the fall of the World Trade Towers on September 11th, 2001, or the tsunami in Japan in 2011.
The speed of information processing supplied by vision also enables us to successfully adapt to dynamic environments. In contrast to static environments in which we are the only moving object, dynamic community environments often contain several objects moving independent of ourselves and each other. In these environments, to successfully adapt we must not only monitor our own movement but also adapt it to the movement of other objects to avoid collisions and potential harm.
Much of our success in adaptation depends on the rapid processing of information. It does no good to recognize the car after it has struck you; you must be ready for the event before it occurs. Only vision supplies us with sufficient information quickly enough to match our movement to the objects surrounding us. The daily occupations most affected by visual impairment take place in dynamic, unpredictable environments such as those found in the community and workplace. Reintegrating a person with a visual impairment into the stable environment of the home is a relatively easy process, but reintegrating a person into community environments is much more difficult.
Visual impairment can occur secondary to disease, trauma, and aging.8,36,71,106 Frequently, a combination of at least two of these causes is observed, especially in older clients. Visual impairment can alter the quality and amount of visual input into the CNS or alter how the CNS is able to process and use incoming visual input. Either way, the result is a decrease in the ability to use vision to perform daily occupations. Changes are observed in occupations dependent on vision. Clients with visual impairment may process visual information so slowly that they are unable to navigate a dynamic environment or play a card game with friends. Changes in decision making may be observed in which the client makes errors because insufficient visual information was received or because the information received was faulty. Because of the pervasive use of vision in adaptation, visual impairment has the potential to change the client’s interaction with all aspects of the environment and the people and objects in it.
Recall, for example, the many daily activities that Penny is having difficulty completing both in the home and in the community. Yet despite its significance, the effect of visual impairment on occupational performance is often attributed to other causes because visual impairment is a hidden disability. Unlike a physical impairment, which can easily be observed, there are few outward signs of visual impairment. As a result, the limitations produced by visual impairment are often attributed to other causes such as motor or cognitive impairment, especially when a brain injury has occurred.
An Overview of Visual Processing within the Central Nervous System
For vision to be used for occupation, the raw material of vision (i.e., the pattern of light that falls onto the retina) must be transformed into images of the surrounding environment that can be compared with stored memories, combined with other sensory input and knowledge, and then be used for decision making. The process is known as visual perception, and the journey encompasses many of the major structures of the CNS. The processing route is a circular one, with visual information transported from the retina in the anterior of the brain to the occipital pole in the posterior brain and then back again to the prefrontal cortex in the anterior brain. Along the way visual input is sorted out, fine-tuned, combined, and repackaged with other sensory input to provide a product that can be used for adaptation.17,55,81
The process begins as light enters the eye and passes through the cornea and lens to focus on the retina. The retina conveys this information over the optic nerve and tract to the lateral geniculate nucleus (LGN) of the thalamus.54 Because of crossing of retinal nasal fibers (of the optic nerve) at the optic chiasm, the LGN receives information from the retinal hemifields of both eyes.54,81 After synapsing in the LGN, visual information travels over the geniculocalcarine tracts (GCTs) to the V1 area of the visual cortex (found within the occipital lobe).54 Figure 24-1 shows these pathways. The visual cortex sorts through the incoming visual information, sharpens and fine-tunes features such as orientation of line and color, and then disperses this information for cortical processing.54,55,128 From the visual cortex, visual information is processed by the temporal and parietal circuitry and eventually sent to the prefrontal circuitry to be used in decision making.55 Before it can be used by the prefrontal areas, visual information must be combined (integrated) with other incoming sensory information to establish images and relationships between the body and the environmental surroundings.55,56,81
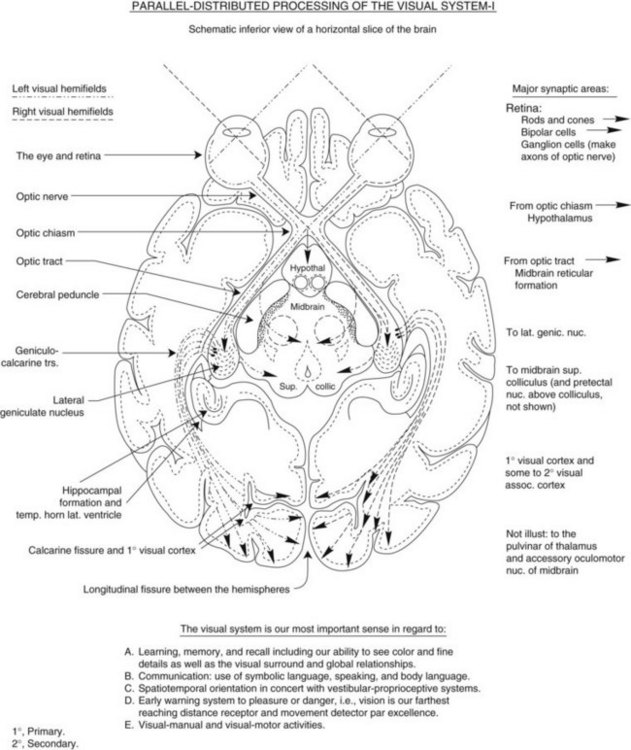
FIGURE 24-1 Pathways from the retina to the lateral geniculate nucleus to the visual cortex. (Courtesy Josephine C. Moore, PhD, OTR.)
To integrate vision with other sensory input, visual information is sent from the visual cortex to the prefrontal area over two routes: a “northern” or superior route, which takes it through the posterior parietal circuitry, and a “southern” or inferior route through the posterior temporal circuitry.44,55,56,81 This process is known as parallel-distributed sensory processing (Figure 24-2). Visual information traveling the southern route through the posterior temporal circuitry is combined with language and auditory input and processed for visual object information and recognition.55,81 The purpose of this processing is to identify objects and classify them. Neural processes in the posterior temporal lobe use precise visual input from the macular-foveal area of the retina to tune in to the visual details of objects. Processing by the posterior temporal circuitry is critical to the ability to distinguish discrete features of objects, such as the difference between the style of a can of diet Coke and regular Coke or particular facial features.55
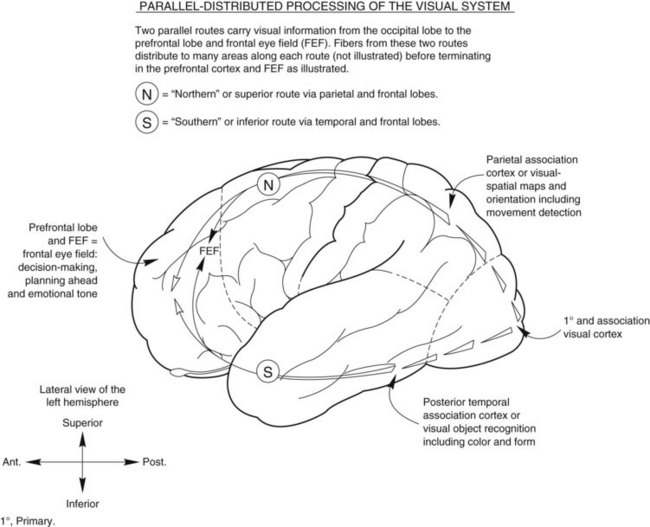
FIGURE 24-2 Visual input travels from the visual cortex through the parietal and posterior temporal circuitry to the prefrontal lobe to complete cortical visual processing. (Courtesy Josephine C. Moore, PhD, OTR.)
Visual information traveling simultaneously through the northern route to the prefrontal circuitry is processed in the posterior parietal lobe. The parietal lobe is a synthesizer of sensory information; it receives input from all of the sensory systems and integrates the input to create internal sensory maps that are used to orient the body in space.9,44,55,56,81,98,100 Visual information traveling through the parietal circuits is used to tune the CNS to the presence of objects surrounding the body and to determine the spatial relationship of these objects to the body and to each other. Visual information must be integrated with other sensory information to provide this orientation. Tactile, proprioceptive, kinesthetic, vestibular, and auditory information is necessary, along with visual input, to accurately assess the relationship between the self and surrounding objects. The map created by information synthesized in the parietal circuitry is body centered and dynamic; it changes in shape and content as the body moves through space.9,44,79,81,98,100
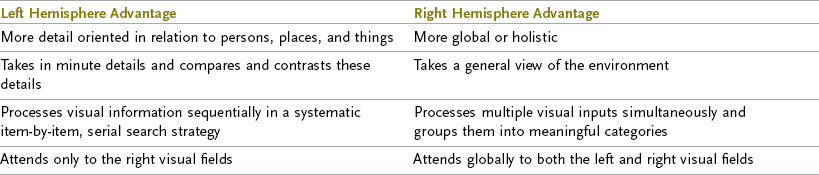
The posterior parietal circuitry in each hemisphere contains a map of the space on the contralateral side of the body. Thus, the right hemisphere contains a map of the left side of the body and surrounding space, and the left hemisphere contains a map of the right side of the body and surroundings.9,44,100 This map is not a detailed representation of space but provides a general impression of objects in space on that side of the body. The CNS relies on visual information from the peripheral areas of the retinal fields to create and maintain these maps. This area of the brain participates in directing general attention to and awareness of space.79
The final destination for visual information traveling through the posterior temporal and parietal circuitry is the prefrontal area of the brain, where the information is used for cognitive processing to make decisions and formulate plans. This area, in conjunction with the premotor circuitry and other areas, is responsible for planning skilled body movements, including eye movements.43,44,55,81 Important visual structures located in the prefrontal lobes are the frontal eye fields, which are responsible for voluntary visual search of the space on the contralateral side of the body.11,44,92,101,103 The frontal eye fields in the right hemisphere direct visual search toward the left visual space, and vice versa. The frontal eye fields conduct a visual search based on an expectation of where visual information will be found in the environment.42 For example, if you were looking for a light switch in a room, you would direct your visual search toward the walls because that is where you expect to find a light switch. You would not waste time searching the floor or the ceiling. By directing visual search based on the expected location of crucial visual information, the CNS is able to process visual information quickly. This arrangement enables us to successfully engage in activities that require rapid visual processing, such as driving.
Not all visual information travels over the GCTs for cortical processing. Many neural pathways leave the optic nerve and tract and travel to subcortical areas, including the hypothalamus and brainstem.54,71,81 The brainstem contains important neural structures involved in visual processing. The superior colliculi, located in the midbrain of the brainstem, are the primary brainstem processing centers for visual input. The superior colliculi are responsible for the detection of moving visual stimuli appearing in the peri-pheral visual fields.44,54,71,77 When motion is detected, the colliculi automatically initiate eye movement toward the direction of the detected motion. In performing this function, the colliculi serve as an early warning system to prevent the CNS from being caught off guard by events occurring in the environment.44,90 The nuclei of cranial nerves III, IV, and VI, which control the extraocular muscles of the eyes, are also located in the brainstem, along with basic visual functions such as the light (pupillary) reflex and the accommodation reflex.54
Many CNS areas are responsible for processing visual information, but all areas must work together for a person to make sense of what is seen and thus use this visual information to adapt.44,55,79,81,99 Millions of long and short neural fibers tie the various cortical and subcortical structures together to ensure effective and efficient visual processing. Like a car, in which the fuel injection system is as critical to performance as the spark plugs, the visual system will not run efficiently unless all of its components are working together. When brain injury or disease occurs, this communication system is disrupted and the organization of visual processing breaks down. Table 24-1 lists the effects of various CNS lesions on different aspects of the visual system. In reviewing the table, remember that a client will exhibit limitations only in daily occupations that require the type of visual processing compromised by the lesion. For example, a deficit in the ability to process visual detail caused by a lesion in the left posterior temporal lobe would significantly affect the ability of a proofreader to return to work but might have little effect on a piano tuner’s ability to return to work.
TABLE 24-1
Summary of Cortical Hemispheric Functions for Visual Processing and Deficits Secondary to Lesion Site
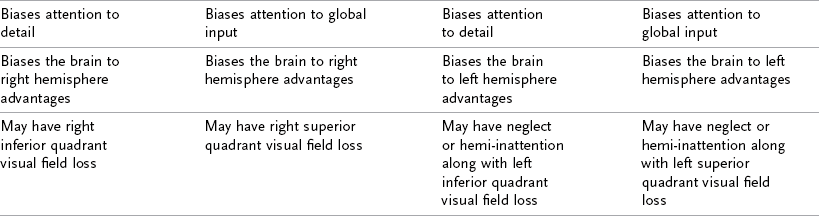
Modified with permission of Josephine C. Moore.
Penny’s CVA occurred in the middle cerebral artery feeding the left hemisphere of the cortex and affected an area known as the internal capsule. As a result of the stroke, the temporal and parietal loops of the GCTs were damaged along with areas in the posterior parietal lobe and the motor strip controlling the left upper and lower extremities.
Framework for Assessment and Treatment of Visual Perceptual Dysfunction
A Hierarchic Model of Visual Perceptual Processing
The ability to use vision to adapt to the environment requires the integration of vision within the CNS to turn the raw data supplied by the retina into cognitive concepts of the perception of space and objects that can be manipulated and used for decision making. The process by which this occurs is known as visual perception. Visual perceptual function can be conceptualized as an organized hierarchy of processes that interact with and subserve each other.120 Figure 24-3 illustrates this hierarchy. Within the hierarchy, each process is supported by the one that precedes it and cannot properly function without integration of the lower-level process. As Figure 24-3 shows, the visual perceptual hierarchy consists of the processes of visual cognition (visuocognition), visual memory, pattern recognition, visual scanning, and visual attention. These perceptual processes are supported by three basic visual functions that form the foundation of the hierarchy: oculomotor control, visual fields, and visual acuity.
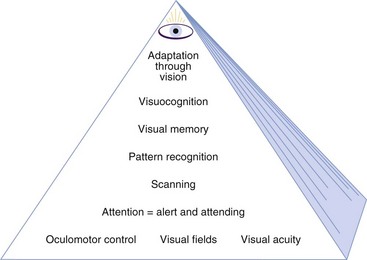
FIGURE 24-3 Hierarchy of visual perceptual development in the central nervous system. (Courtesy Josephine C. Moore, PhD, OTR. From Warren M: A hierarchical model for evaluation and treatment of visual perceptual dysfunction in adult acquired brain injury, part I, Am J Occup Ther 47[1]:55, 1993.)
The ability to use visual perception to adapt to the environment is a result of the interaction of all of the processes in the hierarchy in a unified system. Although each perceptual process is discussed individually in this section, the reader should remember that the ability to adapt through vision is a result of the processes working in synergy. Although discrete perceptual processes can be identified, they do not operate independently of one another.
The highest-order visual perceptual process in the hierarchy is visual cognition. Visual cognition can be defined as the ability to manipulate and integrate visual input with other sensory information to gain knowledge, solve problems, formulate plans, and make decisions. In other words, visual cognition is the ability to use vision to complete cognitive processing. The development of visual cognition begins in childhood when we combine visual input with somatosensory input to develop such cognitive concepts as size constancy and permanence. We then apply these concepts to decision making. For example, if we see a 12-inch-tall adult, we assume that the adult must be some distance away because by applying size constancy we know that adults are not 12 inches high. Because visual cognition enables complex visual analysis, it serves as a foundation for all academic endeavors, including reading, writing, and mathematics, as well as many vocations, such as artist, engineer, surgeon, architect, and scientist.
Visual cognition cannot occur without the presence of visual memory, the next process level in the hierarchy. Mental manipulation of visual stimuli requires the ability to create and retain a picture of the object in the mind’s eye while the visual analysis is being completed. In addition to being able to store visual images temporarily in short-term memory, a person must also be able to store and retrieve images from long-term memory. For example, to interpret the illustration in Figure 24-4, one must be able to access visual memories of the shape of both a goose and a hawk. Adults and older children can easily resolve this illusion, but most toddlers cannot because they have not yet stored memories of the shapes of these birds.
FIGURE 24-4 Is this a goose or a hawk? (From Warren M: A hierarchical model for evaluation and treatment of visual perceptual dysfunction in adult acquired brain injury, part I, Am J Occup Ther 47[1]:55, 1993.)
Before a visual image can be stored in memory, an individual must recognize the pattern making up the image. Pattern recognition, which subserves visual memory in the hierarchy, involves identifying the salient features of an object and using these features to distinguish the object from its surroundings.37 A salient feature is one that distinguishes a particular object from another. For example, the salient feature that differentiates an “E” from an “F” is the lower horizontal line on the “E.” Pattern recognition involves two abilities: the ability to identify the configural and holistic aspects of an object—to see its general shape, contour, and features—and the ability to identify specific features of an object, such as details of color, shading, and texture.18 Both aspects of recognition must occur for accurate identification.8
Pattern recognition cannot be accomplished without the next process in the hierarchy: organized and thorough scanning of the visual array. Visual scanning or search is accomplished through the use of saccadic eye movements. A saccade is a movement of the eye toward an object of interest in the environment. The purpose of a saccade is to focus on the object with the fovea, the area of the retina with the greatest ability to process detail.42 In scanning a visual array, the eyes selectively focus on the elements that are critical for accurately interpreting the array.35,48,83,95 The most important details are re-examined several times through a series of cyclic saccades to ensure that correct identification is made. Unessential elements in the scene are ignored.35,95,131
Visual scanning is actually a product of visual attention.35,45,48,90 The saccadic eye movements observed in scanning reflect the engagement of visual attention as it is shifted from object to object. Visual search occurs on two levels: an automatic or reflexive level largely controlled by the brainstem and a voluntary level driven by the cortical processes of cognition.79 On a reflexive level, visual attention (and therefore visual search) is automatically engaged by any novel object moving or suddenly appearing in the peripheral visual field, such as a flash of light.54,77 This response serves to protect an individual from unexpected intrusions in the environment. Voluntary visual search, directed by the cortex, is completed for the explicit purpose of gathering information. Visual search is purposefully and consciously driven by a desire to locate certain objects in the environment, such as a misplaced set of keys, or to obtain certain information, such as where an exit is located.35,79
Visual attention is a critical prerequisite for visual cognitive processing. If and how a person attends to an object or information determines whether and how that visual input is analyzed by the CNS, which becomes the basis for decision making. People who do not attend to visual information do not initiate a search for visual information, do not complete pattern recognition, do not lay down a visual memory, and cannot use this visual input for decision making. Likewise, those who attend to visual information in a random and incomplete way often do not have sufficient or accurate information on which to base a decision.
The type of visual attention engaged by the CNS depends on the type of visual analysis needed. For example, the type of attention needed for awareness that a chair is in the room is different from the type needed to identify the style of the chair. The first instance requires a global awareness of the environment and the location of objects within it; the second requires selective visual attention to the details of the chair to identify its features. In addition, it is necessary to be able to use more than one type of visual attention at the same time. When crossing a crowded room to talk to a friend, a person must be aware of the movement of people and the placement of obstacles in the room to avoid collisions while at the same time focusing on the friend (or target). The CNS uses several types of visual attention simultaneously and shifts constantly between types and levels of attention.79 Because a large amount of neural processing is devoted to directing visual attention, visual attention can easily be disrupted by brain injury, but at the same time it is a highly resilient visual perceptual process.79
Engagement of visual attention and the other higher-level processes in the hierarchy cannot occur unless the CNS is receiving clear, concise visual information from the environment.21,120 Visual input is provided through the visual functions of oculomotor control, visual field, and visual acuity. Oculomotor control enables eye movements to be completed quickly and accurately and ensures perceptual stability. The visual fields register the visual scene and ensure that the CNS receives complete visual information. Visual acuity ensures that the visual information sent to the CNS is accurate. Without these prerequisite visual functions, an inadequate image is generated, thereby preventing the engagement of higher-level visual perce-ptual processing.
Brain injury or disease can disrupt visual processing at any level in the hierarchy. Because of the unity of the hierarchy, if brain injury disturbs a lower-level process or function, the processes above it will also be compromised. When this occurs, the client may appear to have a deficit in a higher-level process even though the deficit has actually occurred at a lower level in the hierarchy. For example, a client who is unable to complete an embedded figures test appears to have a deficit in the visual cognitive process of figure-ground perception. In fact, this client may be experiencing inaccurate pattern recognition caused by an asymmetric scanning pattern that results from visual inattention, compounded by a VFD. Treatment of the higher-level process (figure-ground imperception) will not be successful unless the underlying deficits in visual attention and visual field are addressed first. This effect is similar to that observed in the motor system following brain injury. The high-level deficit observed is that the client cannot use the hand to pick up an object. The underlying deficits are reduced muscle tone and sensation and muscle weakness. Use of the hand for manipulation will not be possible until the deficits in muscle tone, strength, and sensation are addressed by intervention.
Left homonymous hemianopia was diagnosed in Penny. Because of this deficit, she does not see objects in the left half of her visual field. This visual field defect compromises her ability to attend to objects on her left side, and she fails to search for objects on her left side. Failure to search for objects on her left side limits her ability to complete pattern recognition and form visual memory of objects on her left side. Because she has no visual memory of objects on the left side, she is more likely to experience disorientation and collide with objects on the left when navigating environments.
Intervention
When working with a client with visual impairment following brain injury, the OT practitioner often encounters and works closely with two medical disciplines: ophthalmology and optometry. Specialists in both these eye care fields diagnose, manage, and treat visual impairment, and both may serve as a referral source to OT practitioners. However, there are distinctions between the two professions that OT practitioners must be aware of to collaborate effectively and benefit from their input. Ophthalmologists are medical doctors who complete a residency in ophthalmology. As physicians, ophthalmologists are primarily responsible for diagnosing and treating medical conditions that cause visual impairment. Neuro-ophthalmologists are board-certified in this specialty and often treat the largest number of persons with visual impairment as a result of brain injury. Consequently, they often work with OT practitioners and serve as referral sources and consultants to OT practice.
Optometrists are independent health care providers who have a doctorate in optometry from a postgraduate university program. Like OT practitioners, optometrists specialize in a variety of areas following training, including neuro-rehabilitative, developmental, and behavioral optometry. Although they are not medical doctors, they also diagnose and treat medical conditions causing vision loss and provide nearly two thirds of primary eye care in the United States. Neither discipline, at this time, routinely serves as a member of the rehabilitation team, and both provide mainly consultative services. Which specialty the team uses depends primarily on availability and reimbursement.
Occupational Therapy Evaluation
To develop an intervention plan, the OT practitioner must link limitations in activity and participation to the presence of a visual impairment. Establishing this relationship is the purpose of assessment of visual performance by an OT practitioner. This process is also known as establishing “medical necessity,” which is the prerequisite to receiving third party reimbursement for OT services. To achieve the link, the practitioner must be able to identify the limitation in occupation and then connect it to the presence of a visual impairment. This frequently requires that the OT practitioner also perform assessments to identify visual impairment. However, whereas an ophthalmologist or optometrist evaluates visual impairment for the purpose of diagnosing a visual disorder, OT practitioners assess visual impairment to explain the presence of a limitation in occupation and participation.
In an ideal treatment setting, the OT practitioner would work in partnership with an ophthalmologist or optometrist to identify the client’s visual impairment. These eye care professionals would serve as members of the rehabilitation team and screen the client’s vision at several intervals during the recovery period. They would provide the other rehabilitation professionals on the team information regarding the health of the eyes and the status of visual acuity, visual field, and oculomotor control, along with information on prognosis and medical and optical management. In reality, these two eye care specialists are rarely integrated into rehabilitation teams, and the process of obtaining a referral to either one is time-consuming and difficult.
To succeed, the OT practitioner must often first convince the physician or case manager overseeing the client’s recovery that a visual deficit exists and is limiting occupational performance. This requires the OT practitioner to be well versed in completing basic visual assessments such as acuity, contrast sensitivity function, and visual field to screen for visual impairment. The eye care specialist would use the information obtained from these evaluations to diagnose the client’s visual impairment, whereas the OT practitioner would use the information to justify referral to these specialists and to link the presence of an occupational limitation to visual impairment.
Several tests are available to OT practitioners for assessment of visual performance. Subtests from the Brain Injury Visual Assessment Battery for Adults (biVABA) developed by the author are used in this chapter to describe assessment techniques.121 The biVABA was designed specifically as a tool to assist OT practitioners in developing effective intervention plans for adults with visual impairment caused by brain injury. The biVABA consists of 17 subtests designed to measure visual processing ability. The assessments include evaluation tools used by ophthalmologists and optometrists to measure basic visual function, along with subtests designed specifically for OT practitioners.
Occupational Therapy Intervention
The focus of OT intervention is to change the outcome in the categories of visual disability and visual handicap. Two primary approaches are used in providing intervention. A remediation approach may be used in which intervention attempts to establish or restore the client’s ability to complete visual processing by improving aspects of visual performance such as increasing the efficiency of visual search or improving visual attention. A compensatory approach is also used in which the emphasis of intervention is on changing the context of the environment or task to enable the client to successfully use his or her current level of visual processing. These two approaches may be used alone or together, depending on the needs of the client. Education of the client and family is always used in conjunction with the two approaches to increase their insight into how the client’s visual processing has changed and how it has affected occupational performance. Education is a critical component of the intervention process because insight is crucial to the ability to learn compensatory strategies.1,110
Occupational Therapy Assessment and Intervention for Specific Visual Impairments
The concept of a visual perceptual hierarchy provides the framework for the discussion of assessment and intervention. It is assumed that many changes in visual perceptual function occur after brain injury because of the alteration in lower-level processes within the perceptual hierarchy, including visual acuity, visual field, oculomotor control, and visual attention and scanning. Deficits in these functions prevent the CNS from accurately carrying out complex visual processing and using vision for adaptation. Identification of deficiencies in these processes, followed by treatment to remediate the deficits, enables the CNS to process visual input more efficiently and facilitates adaptation. This section focuses on assessment and intervention for these processes within the visual perceptual hierarchy and examines how brain injury disrupts the functioning of each process, how the process is assessed, and how the implementation of intervention is provided.
Visual Acuity
Visual acuity is the ability to see small visual detail. Acuity contributes to the capability of the CNS to recognize objects. The dictionary defines acuity as “keenness or sharpness,” and with regard to vision, acuity ensures that clear and precise visual information is provided to the CNS for processing.2,109 The greater the quality of the visual input, the more precise the image created by CNS processing. The more precise the image, the faster and more accurate the ability of the CNS to recognize the object and discriminate it from other features in the environment. Good acuity therefore enables speed and accuracy of information processing and facilitates decision making.
Acuity occurs through a multistep process that begins with focusing of light onto the retina. Light rays enter the eye through the pupil and are focused on the retina by the anterior structures of the eye: the cornea, lens, and optic media (Figure 24-5).109 The retina, acting like film in a camera, processes the light and records a “picture” that is relayed to the rest of the CNS via the optic nerve and pathway.55 Although the concept is simple, the process is complex and involves many factors, including the ability to focus light precisely onto the retina, the ability to maintain sharp focus over various focal distances, the ability to obtain sufficient illumination of the retina to capture a quality image, and the ability of the optic nerve to transmit the image through the CNS for perceptual processing.54,55 Any compromise of the structures involved in this process will result in degradation of the image and reduced acuity.106
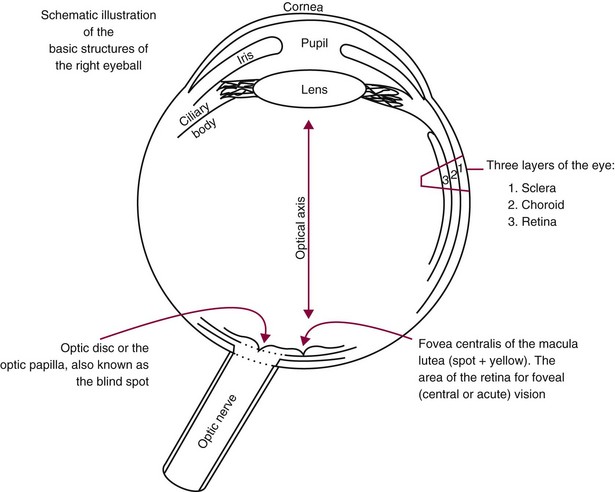
FIGURE 24-5 Anterior structures of the eyeball. Light passes through these transparent structures to focus on the receptor cells of the retina. (Courtesy Josephine C. Moore, PhD, OTR.)
Visual acuity is most commonly measured by having the client read progressively smaller optotypes on a chart. The optotypes may be letters, numbers, or symbols. The most common acuity measurement unit used in the United States is the Snellen fraction (20/20, 20/50, etc.).17 The fraction represents a ratio of distance to size of the optotype.26 In layman’s terms, a measurement of “20/20” means that when standing at a distance of 20 feet, the viewer can see the letter that a person with normal vision can see at 20 feet, and 20/200 would indicate that a person standing at a distance of 20 feet can see a letter that a person with normal vision could identify at 200 feet. In reality, 20/20 means that a person can identify an optotype that subtends 1 minute of arc at a distance of 20 feet, whereas 20/200 means that a person can identify an optotype that subtends 10 minutes of arc at the same distance.
Visual acuity is typically associated with the ability to see high-contrast, black-on-white optotypes. However, visual acuity is actually a continuum of visual function ranging from the ability to detect high-contrast features on one end of the continuum to the ability to detect low-contrast features (such as beige on white) on the other end.50 Low-contrast acuity, known as contrast sensitivity function (CSF), is the ability to detect the borders of objects reliably as they decrease in contrast (rather than size) from their backgrounds.50 CSF makes it possible to distinguish and identify faint features of objects, such as the curve of a concrete curb or protrusion of the nose on the face.50 Because much of the environment is made up of low-contrast features (gradations of colors between objects rather than stark contrasts), CSF is a critical visual function underlying the ability to negotiate an environment safely.50
For example, curbs and steps are routinely the same color throughout; without CSF, it would not be possible to see the depth in the curb or step. Carpets, walls, doors, door frames, and furniture are also often monochromatic in color; without the ability to distinguish low-contrast features, it would not be possible to locate the door or avoid the chair jutting out into the pathway in monochromatic environments. One of the most common low-contrast objects is the human face. Human faces contain very little differentiation in contrast between the facial features. That is, the nose is the same color as the forehead, cheeks, and chin, and eye and hair color are designed to blend with skin tones. To see the unique features of a human face requires very good CSF. Research has shown that CSF can be impaired in clients even when their high-contrast acuity is within normal limits.16,19,48 Therefore, both forms of acuity (high and low contrast) must be measured to obtain an accurate assessment of acuity function.
Two forms of high-contrast visual acuity are measured: distance acuity and reading (near) acuity. Distance acuity is the ability to see objects at a distance. Near acuity is the ability to see objects clearly as they come close to the eye. Near acuity is most accurately called “reading acuity” because reading is the primary activity enabled by near acuity. Reading acuity is measured by having the client read sentences in progressively smaller sizes of print. Reading acuity is dependent on the brainstem neural process of accommodation. Accommodation enables the eye to maintain clear focus on objects as they come closer.42 When an object approaches the eye, its point of focus on the retina is pushed farther back, which eventually causes the image to go out of focus. The CNS adjusts for this situation through the three-step process of accommodation. As the object comes closer, (1) the eyes converge (turn inward) to ensure that the light rays entering the eye stay parallel and in focus, (2) the crystalline lens of the eye thickens to refract the light rays more strongly and shorten the focal distance, and (3) the pupil constricts to reduce scattering of the light rays. These three steps enable objects to stay in focus in the near-vision range (distances between 3 and 16 inches from the eyes).
The accommodative process is controlled by the third cranial nerve (the oculomotor nerve), whose nucleus is located in the midbrain portion of the brainstem.42 Brain injuries that affect the brainstem or this nerve can disrupt the accommodative process. A person experiencing such disruption may demonstrate normal distance acuity (which does not require accommodation) and impaired reading acuity. Accommodation can also be affected by a normal by-product of aging called presbyopia. Until the fourth decade of life the accommodation process works efficiently to ensure equal acuity when an individual is viewing objects both up close and at a distance. As a person approaches the age of 50, the lens of the eye gradually becomes less flexible, thereby reducing its ability to keep images in focus as they come closer and creating presbyopia.102 Persons with this condition frequently complain of difficulty reading small print. Presbyopia is corrected either by using reading glasses to magnify print or, if the person already wears eyeglasses, by adding a magnifying lens or “reading ad” to the base of the lenses to create a bifocal. Because of the influence of accommodation, both forms of acuity, reading and distance, must be measured to obtain an accurate assessment of acuity function in some clients.
Deficits in Visual Acuity
In the normal eye, most deficiencies in visual acuity are due to defects in the optical system (the cornea or lens or even the length of the eyeball), which cause images to be focused poorly on the retina.102 The three most common optical defects that reduce acuity are myopia (nearsightedness), hyperopia (farsightedness), and astigmatism. In myopia, the image of an object is focused at a point in front of the retina and is therefore blurred when it reaches the retina. Myopia is corrected by placing a concave lens in front of the eye. In hyperopia the image comes into focus behind the retina, which causes the image to remain out of focus on the retina. Hyperopia is corrected by placing a convex lens in front of the eye. Figure 24-6 illustrates these defects. In astigmatism, light is focused differently by two meridians 90 degrees apart. A cornea that is not perfectly spherical and smooth but is more spoon shaped or dimpled usually causes this defect. It results in blurring of the image because both meridians cannot be focused on the retina. Astigmatism is corrected by placing a cylindrical lens in front of the eye.
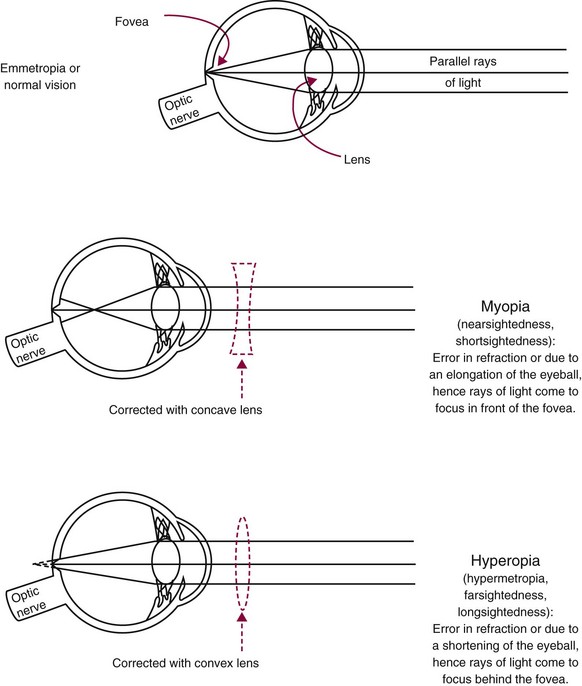
FIGURE 24-6 Normal, myopic, and hyperopic optical refraction of light coming into the eye and the type of lens used to correct myopic and hyperopic optical refractive errors. (Courtesy Josephine C. Moore, PhD, OTR.)
Visual acuity deficits primarily occur as a result of impairment in three areas of visual processing: disruption of the ability to focus light onto the retina, inability of the retina to accurately process the image, and inability of the optic nerve to transmit the information to the rest of the CNS for processing.106 These impairments may be the direct result of a brain injury, a disease process, or a change in the eye occurring incidental to the injury. It is not possible to describe all of the conditions that can result in reduced acuity after brain injury, but the most common are described in the sections that follow.
Disruption of the Ability to Focus an Image on the Retina: Sharp focusing of an image on the retina depends largely on the transparency of the intervening structures between the outside of the eye and the retina and on the ability of these structures to focus the light rays entering the eye. Light entering the eye passes through four transparent media: the cornea, aqueous humor, crystalline lens, and vitreous humor. An opacity or irregularity in these structures will prevent light from properly reaching the receptor cells in the retina. Conditions that can occur in conjunction with head trauma include corneal scarring, trauma-induced cataract, and vitreous hemorrhage.106 Corneal scarring may result from direct trauma to the eye sustained during an assault to the head. The inner layers of the cornea are damaged and scar as they heal, which creates an irregular surface that refracts the light unevenly. The person experiences blurred vision similar to that created by astigmatism. Trauma to the crystalline lens may cause displacement or result in the subsequent development of a cataract that clouds the lens and reduces acuity. Trauma to the eye can also result in bleeding into the vitreous humor. Because blood is an opaque medium, light cannot pass through it, and the client experiences floaters, shadows, and episodes of darkness as the blood passes in front of the retina. Of these conditions, only vitreal hemorrhage is temporary and resolves without treatment.
Impairment of accommodation is another condition that affects the focusing ability of the eye. This condition is associated with brainstem injury, either from head trauma or from stroke.53,71,72,102,106 As stated previously, brainstem injury can affect the functioning of one or all of the components of accommodation: convergence of the eyes, thickening of the lens, and pupillary constriction. When accommodation is impaired, the client has difficulty achieving and sustaining focus during near-vision tasks. The most frequent complaint voiced by the client is difficulty maintaining focus during reading, which may cause the print to blur and swirl on the page.25
Disruption of the Ability of the Retina to Process the Image: The health and integrity of the retina also influence the quality of the image sent to the CNS. The receptor cells of the retina can be damaged directly by injury or disease, thereby preventing them from responding to light. Diseases that affect retinal function, such as macular degeneration and diabetic retinopathy, are associated with age and significantly increase in incidence in the seventh and eighth decades of life.36 With damage to the retina (especially the macular area), both high- and low-contrast visual acuity is diminished, thus making accurate identification of features and objects difficult. It is estimated that approximately one in four persons older than 80 years has a visual impairment that affects the retina significantly enough to prevent reading standard print. It is not uncommon for an older adult who has been referred for treatment of a CVA (such as stroke) to also demonstrate reduced visual acuity secondary to eye disease. Too often the visual loss resulting from the disease is either overlooked or misdiagnosed as an impairment in attention or cognition associated with the CVA.
Disruption of the Ability of the Optic Nerve to Send the Retinal Image: The most common cause of optic nerve damage in brain injury is trauma.53 Damage can occur from a direct penetrating injury to the nerve, such as a missile wound to the head from a gunshot.53 Indirect trauma can also occur from an optic canal fracture associated with facial or blunt forehead fractures. These fractures are most common in children and young adults and usually result in unilateral injuries.53 Severe closed head injuries can cause stretching or tearing of the optic nerve and result in significant and generally bilateral damage to the nerves. Bilateral optic nerve injury can also result from compression of the nerves secondary to intracranial swelling or hematoma.53
Other common conditions that can cause optic nerve damage are glaucoma and multiple sclerosis. Glaucoma typically damages the optic nerve fibers carrying peripheral visual field input but can also affect the central visual field and reduce visual acuity. Multiple sclerosis can cause plaques to develop along the optic nerve, which results in optic neuritis, a condition accompanied by reduced visual acuity, VFD, and sensitivity to light (photophobia).106
Occupational Limitations Caused by Reduced Visual Acuity
Reduced visual acuity can cause limitations in a significant number of daily occupations. The severity of the limitation depends on the extent of the loss in acuity and whether there has been a loss of central acuity, peripheral acuity, or both. Loss of central acuity results in an inability to discriminate small visual details and to distinguish contrast and color. Activities dependent on reading, writing, and fine motor coordination (e.g., reading recipes and labels on foodstuffs, dialing a telephone, writing a check, paying a bill, applying makeup, shaving, identifying money, and shopping) will be affected. When peripheral acuity is reduced, as occurs with a VFD, mobility will be affected. The client may be unable to identify landmarks, see obstacles in the path of travel, or accurately detect motion, which may impair his or her ability to ambulate safely and maintain orientation in the environment. This may reduce independence in driving, shopping, and participation in community activities.
Assessment of Performance Skills
All assessment of performance skill begins with observation of the client’s performance in daily activities. Clients with deficits in visual acuity often complain of an inability to read print and may state that the print is too small or too faint to read. Complaints that print is distorted, that parts of words are missing, or that the words run together and swirl on the page are also common. Clients with deficits in CSF may complain of an inability to see faces clearly. These clients may also be unable to distinguish between colors of similar hue, such as navy blue and black, or to detect low-contrast substances such as water spilled on the floor.
If a decrease in visual acuity is suspected, a screening is completed to determine how the acuity has changed. To obtain a complete picture of the client’s visual acuity, both high- and low-contrast acuity are measured. High-contrast acuity is measured both for distance, using a test chart at a distance of 1 m or greater, and for reading, using a text card at 40 cm (16 inches). When measuring visual acuity, the practitioner must be sure that the chart is well illuminated and held at the specified distance from the client. Adequate illumination is important because as illumination decreases, so does acuity (no one can read a letter chart in the dark). Because acuity is depicted as a fraction of distance over letter size (e.g., 20/20 or 20/200), the measurement is not accurate unless the viewing distance is accurate. All test charts specify a distance at which they are to be used, and this should not be altered.
The client’s acuity level is determined by the smallest line of optotypes that can be read with good accuracy. The client is instructed to read the optotypes on the chart out loud, beginning with the largest line and continuing to lower lines until the print is too small to see. Clients with brain injury may have deficits in cognition, language, and perception that interfere with the ability to provide an accurate and timely response in a testing situation. Extra time may be needed for the client to locate the optotype, process the image, and respond. Slowness in responding therefore does not necessarily indicate that the client lacks the acuity to identify the optotype. If the client struggles with the identification of optotypes on each line but is accurate, the test should proceed until a line is reached on which the client can no longer accurately identify the majority of the optotypes.
The most useful chart for the OT practitioner is one that measures visual acuity as low as 20/1000 so that significant reductions in acuity can be measured. Standard charts measure visual acuity primarily in the range that can be compensated for with eyeglasses and measure nothing below 20/200 Snellen acuity. When acuity is below that level, the client is referred to a low-vision specialist for evaluation. Because some conditions such as optic nerve damage or macular diseases can result in profound vision loss (less than 20/400 acuity), it is important for a practitioner to be able to measure acuity in the lower ranges so that appropriate referral and modifications can be made. The LeaNumbers Low Vision Test Chart and the Warren Text Card from the biVABA are examples of test charts that measure visual acuity in the low-vision ranges.
CSF is also assessed by viewing optotypes printed on a chart that is held at a specified distance from the client. However, for this type of testing the optotypes (which may be letters, numbers, symbols, or sine wave gratings) remain the same size but diminish in contrast as one proceeds down or across the chart. The client is asked to identify as many optotypes as possible. There are many forms of CSF tests. The least expensive and most portable test charts are those designed by Dr. Lea Hyvarinen and include the Lea-Numbers Low Contrast Screener (part of the biVABA), the LeaSymbols Low Contrast Screener, and the LeaNumbers and LeaSymbols Low Contrast Tests. When CSF is measured, the client is asked to read down the chart as far as possible until the optotype is too faint to be identified. As with high-contrast acuity testing, the test chart must be held at a specific distance and must be well illuminated to obtain an accurate measurement.
In assessing visual acuity, the OT practitioner is not responsible for diagnosing the cause of the deficiency, but rather linking the presence of the deficiency to a limitation in occupational performance. This is a subtle but important distinction that affects the assessment procedure. When a client has reduced visual acuity, the ophthalmologist or optometrist uses the results of the assessment to determine the cause of the reduction (e.g., damage to the retina or cornea or the presence of a refractive error). With this information, the eye care specialist determines how to manage the condition to restore optimum sight with optical devices (glasses or contact lenses), a surgical procedure, or medication prescription. In contrast, when an OT practitioner determines that a client has reduced visual acuity, the information is used to modify activities and the environment so that the client can compensate for the loss and successfully complete daily activities. For example, if a client cannot read the size of print on a medication label, the OT practitioner determines whether the print can be enlarged to a size that the client can read or determines another way for the client to identify the medication bottle.
Intervention
If a significant reduction in visual acuity is noted, the client should be referred to an ophthalmologist or optometrist to determine the nature and cause of the visual loss and whether vision can be restored. Referring clients to specialists can take days, weeks, and even months to complete. The client’s intervention program cannot be placed on hold while the referral is being processed; therefore, the OT practitioner uses the information obtained from the assessment to modify the environment and activities and enable the client to use his or her remaining visual acuity. This is achieved by increasing the visibility of the environment and tasks through manipulation of physical context.
Increase Background Contrast: Changing the background color to contrast with an object can help the client see objects more clearly. Application of this technique can be as simple as using a black cup for milk and a white cup for coffee. In cases in which the background color cannot be changed, such as on carpeted steps, color can be applied to provide a marker. For example, a line of bright fluorescent tape can be applied to the end of each step riser on the carpeted stairs to distinguish between them.33
Increase Illumination: Increasing the intensity and amount of available light enables objects and environmental features to be seen more readily and reduces the need for high contrast between objects. For example, facial features can be identified more easily if a person’s face is fully illuminated. The challenge in providing light is to increase illumination without increasing glare. Halogen, fluorescent, and full-spectrum lights provide the best sources of bright illumination with minimum glare and are generally recommended over standard incandescent lighting for both room and task illumination. Lighting should be strategically placed to provide full, even illumination without areas of surface shadow. For example, if a 50-W halogen lamp is used for reading, it should be positioned behind the client’s shoulder so that the page of print is fully illuminated without the light shining directly in the client’s eyes.
Reduce Background Pattern: Patterned backgrounds have the effect of camouflaging the objects lying on them. The detrimental effect of pattern on object identification can be minimized by using solid colors for background surfaces such as bedspreads, place mats, dishes, countertops, rugs, towels, and furniture coverings. Objects in the environment also create a background pattern. Cluttered environments with haphazardly placed objects create challenges, even for persons with good acuity. If possible, the number of objects in the environment should be reduced and those remaining arranged in an orderly fashion. Closets, drawers, shelves, and countertops should be reorganized and simplified, as should such areas as sewing baskets, desks, and refrigerators.
Enlarge Objects or Features That Need to Be Seen: When possible, objects should be enlarged to make them more visible. Instructions can be reprinted in larger print, medications and other items relabeled, and calendars enlarged. The last line of print that is easily read on the reading acuity test card indicates the minimum size that print should be enlarged for the client. Contrast should also be increased because it does little good to enlarge print if the print is faint. Black on white or white on black print is usually more visible than any other color combination. Many items are now manufactured with larger print, including calculators, clocks, watches, telephones, check registers, glucose monitors, scales, playing cards, games, and puzzles. These items can be purchased through specialty catalogs.
Organize: Items used daily should be arranged on accessible shelves in single rows. Rarely used items should be stored on upper and lower shelves or removed. Commercially available organizing systems can be used to store similar items together to create workstations. Once closets and shelves are rearranged and simplified, every effort should be made to keep them organized. Putting items back where they belong and maintaining organization reduce frustration and facilitate independence. Establishing routines for tasks such as filing nails and paying bills prevents these tasks from becoming overwhelming. Task steps requiring vision to complete can be eliminated by using such items as pre-chopped and pre-measured food ingredients, wrinkle-free clothing, electronic funds transfer, and voice-activated telephone dialing.
Access Community Services: In addition to environmental modification, the client may benefit from the variety of services available to assist persons with vision loss. These services are generally free of charge and can be found in the resource section of the public library or by contacting an advocacy organization such as the American Foundation for the Blind (www.afb.org) or the Lighthouse Information and Resource Center (www.lighthouse.org). The following are some examples of available services:
1. The National Library Service for the Blind and Physically Handicapped offers books, magazines, and music on cassette tape through its Talking Books program.
2. Most states offer radio reading services in conjunction with a university-sponsored public radio station.
3. Local telephone companies often offer free directory assistance to persons with disabilities; most pharmacies will provide large-print medication labels, and many businesses will provide large-print bills.
Visual Field
The visual field is the external world that can be seen when a person looks straight ahead. It is analogous to the dimensions of a picture imprinted on the film in a camera (with the retina representing the film). The normal visual field extends approximately 60 degrees superiorly, 75 degrees inferiorly, 60 degrees to the nasal side, and 100 degrees to the temporal side.3,106 As shown in Figure 24-7, most of the visual field is binocular and is seen by both eyes. A small portion of the peripheral temporal field in each eye is mono-cular and can be seen by only one eye because the bridge of the nose occludes vision in the other eye. At the very center of the retinal visual field is the fovea, an area approximately 8 to 10 degrees in diameter that records the visual details for identification of objects. The fovea is located in the macular area of the field, also referred to as the central visual field (Figure 24-7). This area, which is packed with cone receptor cells, is approximately 20 to 30 degrees in diameter and is used for identification of objects.81,109 The rest of the visual field is the peripheral field. The peripheral visual field is composed of rod receptor cells that detect general shapes and movement in the environment. On the border between the central and peripheral visual fields on the temporal side is the blind spot, so called because the optic disc pierces the retina here and there are no sensory receptor cells.
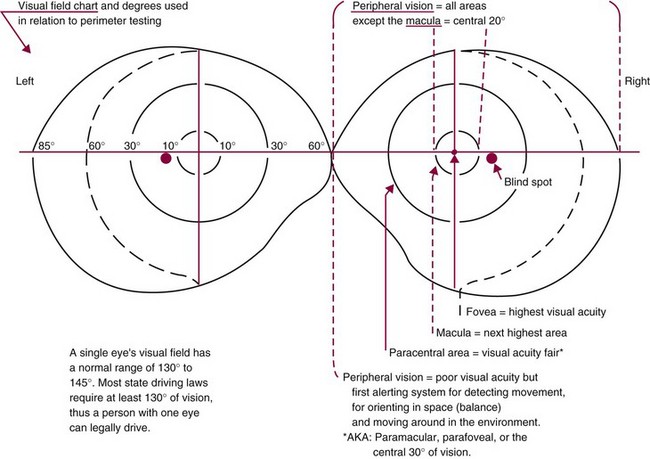
FIGURE 24-7 Visual field chart illustrating the divisions of the visual field related to visual acuity. (Courtesy Josephine C. Moore, PhD, OTR.)
Visual Field Deficits
Damage to receptor cells in the retina or to the optic pathway that relays retinal information to the CNS for processing results in a VFD.3,54,80,106,129 Figure 24-1 illustrates this pathway as it changes from the optic nerve to the optic tract to the GCTs. The location and extent of the VFD depends on where the damage occurs on the pathway. Although any type of VFD is possible after brain injury, homonymous hemianopia resulting from a lesion along the GCTs is the most commonly occurring deficit.134 Hemianopia (hemi = half, anopia = blindness) means that there has been loss of vision in half of the visual field in the eye. Homonymous means that the deficit is the same in both eyes. A lesion along the GCTs in the right hemisphere causes left homonymous hemianopia; a lesion along the GCTs in the left hemisphere causes right homonymous hemianopia. In stroke, most hemianopias are caused by occlusion of the posterior cerebral artery,40,134 although a middle cerebral artery stroke such as that experienced by Penny in the case example can also cause this deficit.
Occupational Limitations Caused by Visual Field Deficits
Although a VFD is often considered a mild impairment in comparison to the dramatic loss of use of the limbs, it can create changes in visual processing that significantly limit daily performance.40 The most important change occurs in the search pattern used by a person with a VFD to compensate for the blind portion of the visual field. Instead of spontaneously adopting a wider search strategy (turning the head farther to see around the blind field), the person tends to narrow the scope of scanning.89,132 The person typically turns the head very little and limits visual search to areas immediately adjacent to the seeing side of the body. The reason for this odd strategy is the influence of a visual process known as perceptual completion.48,73,91,99,105 Perceptual completion is a process whereby the CNS samples a visual array and internally completes a visual scene based on an expectation of the visual information that would be found in the array, as illustrated in Figure 24-8. The perceptual outcome of this process is that the viewer perceives that he or she is seeing a complete visual scene, even though part of the visual information in the scene was not recorded.55,105
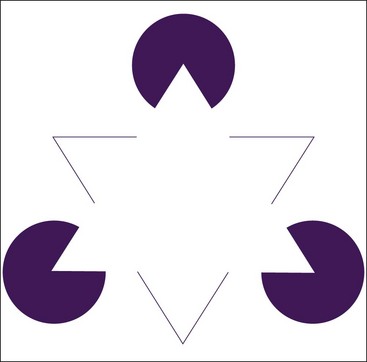
FIGURE 24-8 Example of perceptual completion. A person exercising perceptual completion is able to perceive the border of the solid white triangle in the center of this illustration even when no contrast exists between the border and the background to define the triangle. This perception is based on juxtaposition of the circles and black lines, which “suggests” the presence of the white triangle. (From Schuchard RA: Adaptation to macular scotomas in persons with low vision, Am J Occup Ther 49:873, 1995.)
Perceptual completion provides speed in information processing by enabling an individual to construct a complete visual scene based on partial visual input. Accordingly, it plays an important role in the person’s ability to adapt to fast-paced and dynamic environments. However, in the case of significant visual field loss, the presence of perceptual completion makes it difficult for the client to determine how his or her visual field has changed.73,99 Because of perceptual completion, a client with a VFD is not immediately aware of the absence of vision after onset of the deficit.71,73,105 He or she perceives the presence of a complete visual field without gaps or missing information. However, the CNS cannot place objects in a visual scene that it does not actually see. Therefore, the client may not be aware of unanticipated objects on the blind side. As a result, the client may run into a recently placed chair or other obstacles on the blind side or may not be able to find items placed within the blind field. Until the client becomes aware of the VFD, he or she will have the odd perception of a complete visual scene in which objects always seem to be appearing, disappearing, and reappearing, without warning, on the affected side. Uncertainty regarding the accuracy of visual input on the affected side causes the client to adopt a protective strategy in which he or she attends only to visual input from the intact visual field.89,132 This creates a narrowed scope of scanning restricted to the midline of the body and seeing side. The restriction creates significant limitations in occupations that require monitoring of the entire visual field, such as driving a car or traversing a busy environment.
Even when the person becomes aware of the presence of a VFD, visual search into the blind field is often slow and delayed.51,78,89,132 Again, the culprit is perceptual completion, which eliminates the presence of a marker to indicate the boundary between the seeing and nonseeing fields. Unable to determine the actual border of the seeing field or where a target might be within the nonseeing field, the client naturally slows down when scanning toward the blind field. The slow visual search toward the affected side increases the difficulty that the client has navigating and finding objects within the environment and also reduces reading speed.
If the hemianopia affects the macular portion of the visual field, especially the fovea, a client may miss or misidentify visual details when viewing objects because part of the object falls into the blind area of the field. This can create significant challenges in reading.13,18,29,30,32,68,69,114,133–135 Normal readers view words through a “window” or perceptual span that allows them to see approximately 18 characters (letters) with each fixation of the eye.133 The reader typically moves from word to word by using a series of consecutive saccadic eye movements to cross the line of print. The presence of hemianopia can reduce the width of the perceptual span from 18 characters to as few as 3 to 4. This may cause the client to view only part of a word during fixation and even skip over small words, which often results in misidentification and omission of words.
For example, a client with left hemianopia may read the sentence “She should not shake the juice” as “He should make juice,” with “she” transformed into “he” and “shake” into “make” and leaving out “not” and “the.” Errors such as these cause the client to have to stop and reread sentences, thereby reducing reading speed and comprehension. Accuracy in reading numbers generally creates more challenge for the client than reading words does. Whereas context alerts the client to an error when reading sentences (the sentence does not make sense), numbers appear without precise context, which causes mistakes to go unnoticed. For example, a bill for $28.00 may be misread as $23.00 and the error missed until a notice of insufficient payment is received. Clients making these kinds of errors quickly lose confidence in their ability to pay bills and manage their checkbook and turn over these important daily occupations to someone else.
If the VFD has occurred on the same side as the dominant hand, the client may have difficulty visually guiding the hand in fine motor activities. The most common functional change is a reduction in writing legibility. The client often cannot visually locate and maintain fixation on the tip of the writing instrument as the hand moves into the blind visual field, which causes the handwriting to drift up and down on the line. Writing over something that was just written and improperly positioning handwriting on a form are also common mistakes. Quilting, hand sewing, pouring liquids, and other fine motor activities are likewise frequently impaired.
The changes described (narrow scope of scanning, slow scanning toward the blind side, missing or misidentified visual detail, and reduced visual monitoring of the hand) contribute to a variety of limitations in performance. The primary activities affected include mobility, reading, writing, and the daily occupations dependent on these skills. Such occupations include personal hygiene and grooming, medication management, financial management, meal preparation, clothing selection and care, meal preparation, home management, telephone use, and yard work. In general, the more dynamic the environment where the occupation is completed and the wider the field of view required to perform the task, the greater the limitation. Therefore, only minor limitations are generally experienced in basic ADLs, as opposed to significant limitations in shopping and driving.
Persons with a VFD commonly face significant emotional challenges in adapting to this considerable visual loss. For example, clients with a VFD regularly report feeling a sense of anxiety when moving in unfamiliar environments. Sometimes the anxiety can be so severe that clients experience an autonomic nervous system reaction in which they become nauseated and short of breath and break out into a sweat in crowded environments. One individual with a VFD described this sensation as “crowditis” and reported that he became physically ill if he had to go into a department store or other crowded environment. This anxiety can become debilitating and lead to withdrawal from community activities and social isolation. Other clients report a tremendous loss of self-confidence because of the numerous mistakes that they make during the course of a day, and many state that they experience depression because of their limitations, especially in the ability to drive a car and read accurately.
Assessment
The process of measuring the visual field is known as peri-metry.3 Several types of perimeters are available. They range from simple bedside assessments (such as the confrontation test), which give a gross indication of field loss, to the very precise imaging of a scanning laser ophthalmoscope (SLO).3,46,102,105,116 The perimetry test selected depends on the availability and cost of the test and the ability of the client to participate in testing. For example, confrontation testing does not incur any expense and can be performed nearly anywhere, whereas imaging with an SLO must be completed by a specially trained technician in a center that has purchased the $120,000 instrument. In between these two extremes are the tangent screen, Damato Campimeter, manual bowl perimeters (the Goldmann), and automated bowl perimeters (the Humphrey), ranging in cost from $100 to $20,000. In general, the more expensive the apparatus, the more precise the measurement provided.
All perimetry testing involves three parameters: fixation on a central target by the client while the testing is performed, presentation of a target of a specific size and luminosity in a designated area of the visual field, and acknowledgment of the second target without breaking fixation on the central target.3 Testing is done with either static or kinetic presentation of the target. In static presentation, the target appears in a specified area of the visual field without being shown moving to that location. In kinetic testing the target moves in from the periphery until it is identified.3,102
The most accurate perimetry test available to clinicians is computerized, automated perimetry, which is completed by either an ophthalmologist or optometrist.3 During automated perimetry, the client places his or her chin on a chin rest and fixates on a central target inside a bowl-shaped device. As the person fixates on the central target, lights are displayed inside the bowl in varying locations and intensities. The client responds to each seen light by pushing a small button. The test can be very thorough, with lights presented in more than a hundred locations within the field and the intensity of the light increased in a step threshold sequence if the target is not appreciated the first time. The result is an accurate measurement of the areas of absolute loss (no response) and relative loss (decreased retinal sensitivity) within the field. An ophthalmologist or optometrist may also use a simpler screening test, the tangent screen, to assess the integrity of the central visual field. The tangent screen consists of a black felt screen with a grid stitched into the felt in black thread so that the grid is visible only to the examiner.3 The client sits directly in front of the screen at a distance of 1 m. The client is instructed to fixate on the center of the screen as the examiner moves or places a white target attached to a black wand in a certain area of the screen. Without breaking fixation on the center of the screen, the client indicates when the target is seen. If the client does not see the target when it is presented, that point in the visual field is recorded as a loss. The examiner uses the grid to determine the location of the field deficit.
OT practitioners can screen for a VFD by using simple perimetry testing in combination with careful observation of client performance of daily occupations. Confrontation testing is a bedside examination that provides a crude indication of visual field loss.102,116 To complete a static confrontation test, the examiner sits in front of the client at a meter distance and has the client fixate on a centrally placed target (the examiner’s eye). The examiner then holds up two targets in each of the four quadrants of the visual field (right upper, right lower, left upper, and left lower). The client indicates whether the targets are seen.57,102,106 For a kinetic test the examiner stands behind the client and moves a target (generally a penlight) in from the periphery while the client fixates on a central target. The client indicates as soon as the target is noticed. Standardized versions of these tests are included in the biVABA. Because confrontation testing has been shown to be unreliable in detecting all but gross defects, OT practitioners using this form of testing must be careful to correlate their findings with observations of client performance.116 If the confrontation test shows no deficit but clinical observations suggest that a deficit is present, the clinical observations should carry the greater weight in deciding whether a deficit exists.
Assessment using perimetry devices such as the Damato 30-Point Multifixation Campimeter (biVABA) enables OT practitioners to obtain a more accurate measurement of central visual field function. The Damato Campimeter, shown in Figure 24-9, is a portable test card that provides a precise measurement of the central 30 degrees of the visual field. The test grid consists of 30 numbered targets that place the test stimulus at known points in the visual field by moving the eye rather than the target. The test stimulus is a 6-mm black circle that is shown in the center part of the card. The client is instructed to fixate on one of the numbered targets. The test stimulus is then shown in the central window, and the client indicates whether the circle is seen. If the client does not see the black circle, that point in the visual field is recorded as a loss. The test proceeds with the client successively moving the eye to view the numbered targets until the entire field is mapped out.

FIGURE 24-9 Position of the examiner and client for completion of perimetry testing with the Damato 30-point Campimeter from the Brain Injury Visual Assessment Battery for Adults. (Courtesy Precision Vision, LaSalle, Ill.)
Clinical observation of the client’s behavior is especially important to confirm the presence of a VFD because of the limitations of perimetry testing.102 Clients with fluctuating or limited attention, language, and cognition may give unreliable perimetry results. It may also be difficult to distinguish between a VFD and a deficit in visual attention. However, the client’s performance of daily activities will strongly indicate the presence of a VFD. For example, the presence of a VFD may be indicated if any of the following are observed: the client changes head position when asked to view objects placed in a certain plane, the client consistently bumps into objects on one side, the client misplaces objects in one field, or the client makes consistent errors in reading.
Perimetry tests establish only whether a VFD is present and the size and location of the deficit. To determine whether intervention is needed, the practitioner must determine whether the client is able to compensate for the VFD in performing daily activities, as well as the quality and consistency of that compensation. The presence of a VFD can cause significant limitations in daily occupations. The level of impairment will depend on whether the VFD occurs alone or in conjunction with visual inattention. An analysis of occupational performance should be completed to identify limitations in basic and instrumental ADLs. If the client demonstrates difficulty completing an activity, the visual requirements of the activity should be analyzed to determine whether the VFD is interfering with performance. For example, if the client is unable to locate a toothbrush during grooming, is it because the toothbrush is stored on the side of the client’s field deficit?
Reading is another daily activity often affected by a VFD. The Visual Skills for Reading Test (VSRT) provides an effective way to measure interference of the VFD in reading performance. The VSRT is designed to assess the influence of a scotoma (or field loss) in the macula on the visual components of reading, including visual word recognition and control of eye movement.124 The client is asked to read single letters and words printed on a card. Three different versions of the test card in four font sizes are included in the test to accommodate clients with low vision and to permit retesting. The words are not in context and are designed so that they can be misread and still make sense (e.g., “shot” can be mistakenly read as “hot”). The test measures reading accuracy and corrected reading rate and provides information on the prevalent types of reading errors made by the client. The client’s performance on the letter and reading charts used to measure visual acuity may also indicate the influence of a VFD on reading performance. Because of the wider visual field, a client with a VFD may have more difficulty reading the larger symbols and words on the chart and may be able to read faster and more accurately as the optotypes (and field) decrease in size. Telephone Number Copy, part of the biVABA, provides information about the client’s accuracy in reading numbers. In this test the client is required to copy down telephone numbers that include numbers easily misread by persons with a VFD, such as 6, 8, 9, and 3.
To effectively compensate for the VFD, the client must execute an organized and thorough search of the blind field by using the seeing portion of the visual field. This means that a client with a left VFD must use the right visual field to search both the left and right fields. Clients with a VFD demonstrate difficulty searching both peripersonal space (the space immediately around the body) and extrapersonal space (the space extending from the body into the environment). Deficiencies in searching the peripersonal space affect the performance of basic ADLs such as grooming, dressing, reading, and writing, as well as instrumental ADLs requiring monitoring of a wider visual field, such as meal preparation or leisure activities. Deficiencies in searching the extrapersonal space have a pronounced impact on mobility and affect activities in outside and community environments, such as driving, shopping, and mowing the yard.
To navigate dynamic community environments, the client must use a wide scanning strategy that is initiated on the side of the deficit and executed quickly and efficiently. The client must also be able to shift attention and search rapidly between the central visual field and the peripheral visual field. A variety of observational tests can be used to measure the ability to compensate for the VFD during mobility. An objective assessment of the client’s ability to execute compensatory search strategies can be made with the Dynavision 2000, an apparatus increasingly used in rehabilitation to assess and train visual motor performance (Figure 24-10).63–66 OT practitioners without access to a Dynavision can use a laser pointer to observe the client’s search capability. The beam of light from the pointer is projected onto various areas of a blank white wall, and the client is instructed to locate and touch the projected red dot. The strategy used by the client to locate the dot and the efficiency of the strategy are noted. Integration of visual scanning with ambulation is the final component of the mobility assessment and must be completed to determine whether the client will be able to compensate for the deficit during body movement. This can be assessed by using tests such as the ScanCourse from the biVABA. To complete a ScanCourse, the client is instructed to walk through a course and identify targets placed in various locations on the left and right sides. The client’s ability to locate the targets on each side during ambulation is noted.

FIGURE 24-10 Example of a visual search task using the Dynavision 2000. The lights on the board are illuminated one at a time in random patterns. The client must locate the illuminated light and press it to turn it off. As a light is pressed, another light is illuminated. The client strikes as many lights as possible within a specified time. The activity can be used to teach and reinforce efficient search patterns to compensate for visual field deficits and visual inattention. (Courtesy Dynavision 2000, manufactured by Performance Enterprises, Ontario, Canada.)
Intervention
The performance limitations experienced by persons with a VFD generally fall into two categories: difficulty with mobility and difficulty with reading. Because of the mobility limitation, clients will experience limitations in daily occupations that must be performed in dynamic environments, such as shopping and participating in community events. Resumption of driving may or may not be a goal, depending on the driving statutes of the state in which the client resides. Some states do not specify a minimum degree of visual field for licensure. In these states a client may be able to safely resume driving if given the proper training. Challenges in reading will cause difficulty completing such activities as financial management and meal preparation.
Although a limited body of research shows that some restitution of the visual field may be possible with intensive rehabilitation,7,58,59,86 return of visual field function is unlikely.106 Therefore, the major focus of intervention is to improve compensation for the visual field loss. Compensation for the VFD requires adopting a conscious, cognitive strategy of using head movement to search and broaden the visual field. Because the CNS exercises perceptual completion, the client often lacks insight into the extent and boundaries of the field deficit. Successful compensation requires the client to firmly believe that the deficit exists and that the visual input from the blind side cannot be trusted. A client able to develop this level of insight will usually learn to effectively compensate for the deficit. Every effort must be made through activities and educational materials to make the client aware of the location and extent of the deficit.
Addressing Limitations in Mobility: The limitations experienced in mobility occur primarily because the client does not turn his or her head far enough, fast enough, or often enough toward the blind field to take in the information needed for safe mobility in the allotted time. If the inferior visual field has been affected, as occurs with hemianopia, the client may also experience difficulty monitoring the support surface on the side with the deficit. This can result in hesitancy in walking and a tendency to keep the head down and the eyes fixed on the floor directly in front of the client. Although this strategy may keep the client from colliding with objects, it also prevents the client from monitoring the surrounding environment and can cause disorientation during ambulation.
A combination of remediation and compensation strategies is used to address these deficiencies in mobility. Remediation strategies focus on increasing the speed, width, and organization of the search pattern.49,61,63,66,104,115 The client must learn to quickly turn the head and completely search the blind visual field. The desired outcome behaviors include the following:
1. Initiation of a wide head turn toward the blind field
2. An increase in the number of head and eye movements toward the blind field
3. Faster completion of head and eye movement toward the blind field
4. Execution of an organized and efficient search pattern that begins on the blind side
5. Attention to and detection of visual detail on the blind side
6. Ability to quickly shift attention and search between the central visual field and the peripheral visual field on the blind side
To achieve these outcomes, the client must complete activities in which these skills are required during the performance of an occupation. This is difficult to achieve in the restricted environment of the clinic. The Dynavision 2000 apparatus has been shown to be effective in teaching these components of effective search patterns and is strongly recommended as an intervention tool.43
As the basic components of the search strategy are developed, they should be incorporated into activities that require combining search with ambulation. Indoor activities can include completing scan courses using cards with letters taped onto walls in various locations along hallways. Two examples are activities such as “find red,” where the client points out every red item while walking toward a destination within the rehabilitation center, and “narrated walks,” where the client points out landmarks and changes in the environmental surroundings while ambulating toward a destination. These activities reinforce keeping the head up during ambulation and thereby improve orientation. As skill is developed, practice in dynamic and in unfamiliar environments should be incorporated. The client completes activities in stores and malls, where he or she identifies the number of persons standing in an aisle or inside a store on the blind side while ambulating by, and locates stores within a mall and specific items within stores by using landmarks and organized search strategies.
Integrated into the intervention plan is instruction in compensatory strategies. The client is taught to identify features in the environment that could cause harm, such as steps, curb cuts, and other changes in the support surface. The client is also taught to be more observant of landmarks such as a picture on a wall or a change in wall color to assist in maintaining orientation.
Addressing Limitations in Reading: The client’s primary challenges in reading occur because his or her present saccade strategy does not match the new restricted size of the perceptual span. That is, the client is trying to read with a saccade strategy designed for a wider unrestricted perceptual span. To improve reading speed and accuracy, the client must learn how to adapt a saccade strategy to the new perceptual span. This requires significant practice and can be extremely frustrating for the client. To address this, a remediation approach is used. Prereading exercises, such as those designed by Warren123 or by Wright and Watson,130 and commercially available word and number searches are used to provide the practice that the client needs to learn to make the precise eye movements required to see words completely again. These exercises are designed so that the client searches for specified letters, numbers, or words on worksheets (Figure 24-11). As the client’s performance skill improves, large-print books of familiar stories are used to provide the needed practice and transition the client into reading continuous text.
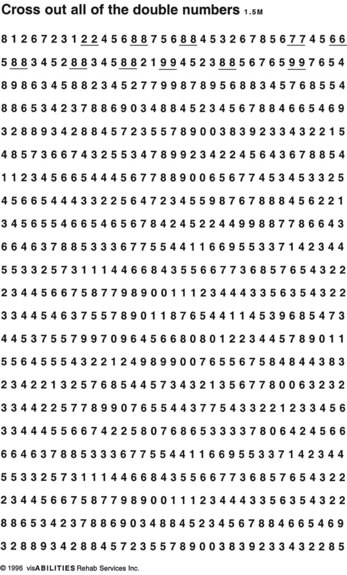
FIGURE 24-11 Example of a prereading exercise. The client is instructed to cross out all of the double numbers on the page. (From Warren M: Prereading and writing exercises for persons with macular scotomas, Birmingham Ala, 1996, visAbilities Rehab Services.)
A compensatory intervention approach is also used to address reading and writing challenges. Clients with left hemianopia often have difficulty accurately locating the next line of print on the left margin of the reading material and lose their place. Drawing a bold red line down the left margin provides the client with a visual cue to use as an “anchor” to find the left margin.125 The same technique used on the right margin helps a client with a right VFD who may be uncertain about the location of the end of the line of print. If the client has difficulty staying on line or moving from line to line, a ruler or card can be used to underline the line of print and keep the client’s place.
Difficulty staying on line when writing is addressed by teaching the client to monitor the pen tip and maintain fixation as the hand moves across the page and into the side with field loss. Activities that require the client to trace lines toward the side of the VFD are effective in re-establishing eye-hand coordination. Practice in completing blank checks, envelopes, and check registers is also helpful.
Occupational performance can be enhanced by increasing the visibility of tasks and environments. Adding color and contrast to the key structures in the environment needed for orientation (e.g., door frames and furniture) will help the client locate these structures. Using black felt-tipped pens can heighten the contrast in writing materials, and bold-lined paper can be used to help the client monitor handwriting. The simple addition of more light often increases reading speed and reduces errors. Reducing patterns in the environment by reducing clutter and using solid-colored objects enhances the client’s ability to locate items.
Visual Attention and Scanning
Visual attention is the ability to observe objects closely and carefully to discern information about their features and their relationship to oneself and other objects in the environment. It requires the ability to ignore irrelevant sensory input and random thought processes and to sustain focus for several seconds to several minutes. Visual attention also entails being able to shift visual focus from object to object in an organized and efficient manner. Engagement of visual attention is accomplished through visual scanning or search (these two terms are used interchangeably). Although these two processes are separated within the visual perceptual hierarchy to assist in understanding them, they cannot be separated in assessment and treatment of the client. Any change in visual attention will be observed in the client as a change in the scanning pattern used for visual search.
Visual attention can be divided into two categories: focal, or selective, visual attention and ambient, or peripheral, visual attention.37,55,85,94 Focal attention is used for recognition and identification of objects. Visual input from the macular area of the retina is used to complete this processing. Focal, or selective, attention enables an individual to accurately distinguish visual details such as differences between letters, numbers, and faces. Ambient, or peripheral, attention is concerned with the detection of events in the environment and their location in space and proximity to the person. It relies on input from the peripheral visual field. Peripheral attention ensures that a person is able to move safely through space and maintain orientation in space. Without peripheral attention, collisions with objects and disorientation when moving would be the norm. To have a fully operational and efficient visual system, these two modes of visual attention must work together. The contribution of each is equally important to perceptual processing.
In adults without brain injury, visual search is com-pleted by using an organized, systematic, and efficient pattern.34,38,48,90,122,126 The type of search pattern used depends on the demands of the task. In reading English, for example, a left-to-right and top-to-bottom linear strategy is used. In scanning an open array (such as a room), a circular, left-to-right strategy is generally used, following either a clockwise or a counterclockwise pattern.
Deficits in Visual Attention and Scanning
Studies have shown that disruption of the normal visual search strategy can occur after brain injury. The characteristics of the disruption vary, depending on which hemisphere was damaged. Visual search deficits associated with right hemisphere injury are characterized by avoidance in searching the left half of the visual space.10,22,24,37,38,45,47,90 This condition is known as hemi-inattention. Instead of initiating the normal left-to-right visual search pattern, clients with right hemisphere injuries often begin and confine the search to the right side of a visual array. This creates an asymmetric search pattern instead of the normal symmetric pattern. The client misses visual information on the left side and, as a result, may be deprived of the information needed to make accurate identification and decisions.
Hemi-inattention is associated with injuries to the right hemisphere and probably occurs because of a difference in the way that the hemispheres are programmed to direct visual attention.47,107 As illustrated in Figure 24-12, the left hemisphere directs attention toward the right half of the visual space surrounding the body. In contrast, the right hemisphere directs visual attention toward both the right and left halves of the space surrounding the body. If a lesion occurs in the left hemisphere, visual attention and search toward the right side are diminished, but some attentional capability is still provided by the right hemisphere. A similar lesion in the right hemisphere may completely eliminate attentional capability toward the left because there is no other area directing attention toward the left side.
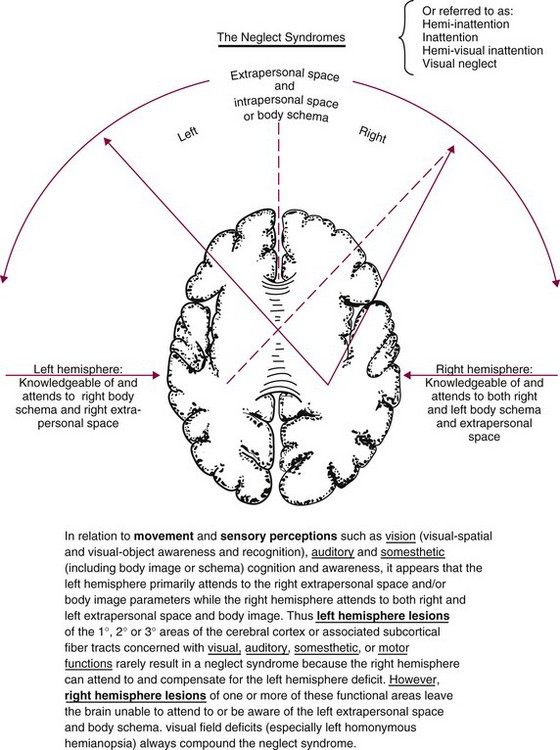
FIGURE 24-12 Difference between the right and left hemispheres in the direction of visual attention and the relationship of hemisphere lesions to hemi-inattention and neglect syndrome. (Courtesy Josephine C. Moore, PhD, OTR.)
Hemi-inattention is often confused with the presence of a left VFD in the client. Although both conditions may cause the client to miss visual information on the left side, they are distinctly different conditions and do not have the same effect on performance. When a left VFD occurs, the client attempts to compensate for the loss of vision by engaging visual attention.10,11,51,75 The client directs eye movements toward the blind left side in an attempt to gather visual information from that side. Because of the field deficit, however, the client may not move the eyes far enough to acquire the needed visual information from the left side and as a result may appear inattentive. In contrast, a client with hemi-inattention has lost the attentional mechanisms in the CNS that drive the search for visual information on the left. No attempt will be made by the inattentive client to search for information on the left side of the visual space, and no eye movement or head turns will be observed toward the left side.22,51 The most significant change in visual search takes place when the two conditions occur together in a client.10,20 In this case the client is not receiving visual input from the left side because of a VFD and does not compensate for the loss of visual input by directing attention toward the left side. The combination of hemi-inattention and left VFD creates severe inattention, often called visual neglect. Clients with this condition show exaggerated inattention toward the left half of the visual space surrounding the body and often do not move the eyes past midline toward the left or turn the head toward the left side. Visual neglect may be compounded by neglect of the limbs on the left side of the body or neglect of auditory input from the left side.45,61 The presence of neglect is consistently associated with poor rehabilitation outcomes.51
Another change in visual search associated with right hemisphere lesions is a tendency to fixate first on the most peripheral visual stimuli occurring in the right visual field.45 If two visual stimuli simultaneously appear in the right visual field, the client will attend first to the most peripheral stimulus.31 A client with this tendency makes frequent head turns to attend to events occurring in the right peripheral field, thus giving the impression of being distractible. Yet another change in visual search is a reluctance to rescan for additional information once an area has been viewed, especially if the area is on the left side.90 This may cause the client to miss certain visual details when viewing complex visual arrays.
Although several distinct changes in visual search have been observed with right hemisphere lesions, only one has been observed following left hemisphere lesions. Clients with left hemisphere injury may show a symmetric decrease in searching for detail when viewing a visual array.15,45,117 These clients symmetrically scan the visual array for information but do not examine specific aspects of the visual scene to gather additional information. Consequently, they may miss visual details and often cannot accurately interpret or identify the objects around them. Left hemisphere injury does not result in hemi-inattention or neglect.
In general, clients with injuries to either hemisphere are slower in scanning and show more erratic fixation patterns than do persons without brain injury.74,126 They also have greater difficulty engaging selective attention and executing an organized and efficient visual search strategy. Research has shown that when persons with brain injuries are asked to search complex visual arrays for specific targets, they have difficulty maintaining attention on the salient features of the target and mistakenly select targets with similar features.93,126 They also demonstrate an inability to superimpose an organized, efficient structure for visual scanning when asked to search an array of randomly displayed objects. For example, if asked to locate a certain individual seated among others on rows of benches (a structured visual array), the injured person would be able to accomplish the task. However, if asked to find the same individual standing in a jumbled crowd of persons (a random visual array), the injured person would display a random approach to searching the array and would probably miss the target.
Occupational Limitations Caused by Visual Inattention
Disruption of visual attention creates asymmetry and gaps in the visual information gathered through visual search. The quality of an individual’s adaptation to the environment decreases because the CNS is not receiving complete visual information in an organized fashion and is therefore unable to effectively use this information to make appropriate decisions. A reduction in visual attention will affect all aspects of the performance of daily occupations. However, the most affected activities will be those that require inspection and integration of significant amounts of visual detail and those completed in dynamic environments. Driving and reading are two diverse examples of tasks often significantly affected by inattention.
Because visual attention is modulated through an extensive neural network involving the entire CNS, some capacity for visual attention is generally retained even in individuals with severe brain trauma.81 Conversely, because so many neural structures contribute to attention, changes in visual attention occur even with mild injuries.99 Whether a change in visual attention affects occupational performance depends on the task to be completed. Tasks such as reading can require enormous amounts of selective visual attention if an individual is reading a highly technical textbook and less selective attention if the individual is reading an advertisement. The task of driving requires continuous global attention to monitor the speed and position of other vehicles and objects and sporadic selective attention to landmarks, street signs, and traffic lights. Whether a deficiency in visual attention occurs after brain injury depends on the circumstances and requirements of the tasks that the client completes.
Assessment
As a process found at the intermediate level of the visual perceptual hierarchy, visual attention can be affected by deficits in lower-level visual functions (visual acuity, oculomotor function, and visual field). Therefore, these functions should be assessed before visual attention is measured. The presence of aphasia and motor impairment can also affect performance on assessments for visual attention. How efficiently and completely a person attends to and takes in visual information determines the ability to use the information for adaptation. Therefore, the emphasis in assessment is on observing how a client initiates and carries out visual scanning to complete a task requiring visual search. During the assessment the OT practitioner should answer the following questions: Does the client initiate an organized search strategy? Can the client carry out the search strategy in an organized and efficient manner? Does the client obtain complete visual information from a visual search? Is the client able to identify visual detail correctly? Does the client’s ability to search for information decrease as the visual complexity of the task increases?
Research has shown that persons with good visual attention demonstrate specific characteristics of search patterns that make them effective in obtaining visual information.48,122,131 These characteristics include strategies that are organized, symmetric, thorough, resilient, and consistent. Use of these strategies generally results in good accuracy and speed in completion of visual search tasks. In contrast, persons with a significant VFD or inattention often have ineffective search strategies. These individuals demonstrate incomplete or abbreviated patterns in which only a portion of the visual array is searched, usually in a random, unpredictable fashion.15,23,37,48,51,74,78,93,126 The organization and accuracy of the pattern often break down when the person is challenged to search more complex visual arrays. Figure 24-13 provides examples of some of the ineffective search strategies used on the visual search subtests of the biVABA by persons with brain injury. A client using ineffective search strategies may not acquire sufficient visual information to complete perceptual processing accurately. The client may acquire the information in such a way that it cannot be used to complete perceptual processing, or the person may not acquire the information rapidly enough to enable adaptation. The subsequent disruption of perceptual processing may cause errors in decision making and adversely affect performance of a variety of ADLs.
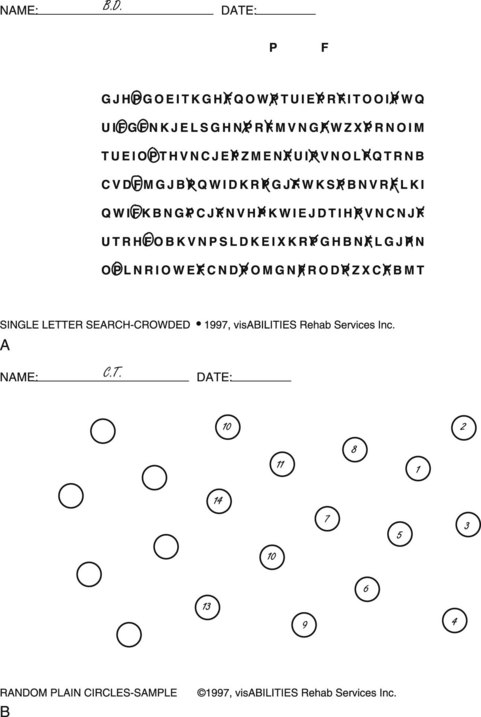
FIGURE 24-13 Examples of ineffective search patterns used by clients to complete two visual search subtests of the Brain Injury Visual Assessment Battery for Adults. A, An abbreviated search pattern used by a client with left hemianopia when crossing out the letters P and F on the subtest. The client executed an organized left-to-right linear search pattern but failed to locate the beginning of the line on the left side and as a result failed to cross out targets on that side (the circled letters). B, An asymmetric and abbreviated search pattern executed by a client with hemi-inattention and left hemianopia. The client was asked to number the circles consecutively in any pattern desired. The client began numbering the circles from the right rather than the left and failed to number circles on the left side of the array.
When measuring visual attention, the OT practitioner must be aware that visual search can be significantly affected by the presence of both a VFD and hemi-inattention. Because a VFD and hemi-inattention are not the same condition, it is necessary to distinguish between the two to establish an effective intervention plan. This can be difficult, both because similar errors are observed with the two conditions on search tasks and because the two can also occur together in the same client. However, differentiation can be accomplished by observing the strategies used by the client to complete visual search tasks such as those on the biVABA (Figure 24-13). Although both VFDs and hemi-inattention can result in decreased accuracy in identifying targets on a visual search task, the characteristics of the search deficiencies are different.10,22,27,28,41,51
For example, a client with left hemianopia may demonstrate a left-to-right linear search pattern that is abbreviated on the blind side. The search pattern is organized but results in a number of errors on the left because the client did not see that side of the array. In contrast, a client with hemi-inattention may demonstrate an asymmetric pattern in which visual search is initiated and confined to the right side with a disorganized and random search pattern. The pattern also results in a large number of errors on the left. Although accuracy in the search task may be similar for these two clients, the cause of the errors is different. By observing the strategy used by the client to complete the search task, it is possible to distinguish between the two conditions. Table 24-2 compares the characteristics of search patterns used by persons with hemianopia and those with hemi-inattention. When the two conditions occur together, it is important to determine the severity of the inattention because this will determine whether the client is able to learn the strategies needed to compensate for the VFD.
TABLE 24-2
Comparison of Search Patterns: Persons with a Visual Field Deficit vs. Persons with Hemi-inattention
| Visual Field Deficit | Hemi-inattention |
| Search pattern is abbreviated toward the blind field | Search pattern is asymmetric; initiated/confined to the right side |
| Attempts to direct search toward the blind side | No attempt to direct search toward the left side |
| Search pattern is organized and generally efficient | Search pattern is random and generally inefficient |
| Client rescans to check accuracy of performance | Client does not rescan to check accuracy of performance |
| Time spent on task is appropriate to the level of difficulty | Client completes the task quickly; the level of effort applied is not consistent with the difficulty of the task |
From Warren M: Brain Injury Visual Assessment Battery for Adults Test Manual, Hoover, Ala, 1998, visAbilities Rehab Services.
The visual search tests that have been described are pencil-and-paper tasks presented in a restricted and well-defined personal space. Determining how the client applies a search strategy to the broader extrapersonal space requires the use of a test such as the ScanBoard described by Warren.122 The test, part of the biVABA, consists of a large (20 by 30 inch) board with a series of 10 numbers displayed in an unstructured pattern. The board is placed at eye level and centered at the client’s midline. The client is asked to scan the board and point out all of the numbers that he or she sees. The examiner records the pattern that the client follows in identifying the numbers. Research using this test has shown that adults with normal visual search use an organized, sequential search pattern, beginning on the left side of the board and proceeding in either a clockwise or counterclockwise fashion until all of the numbers are identified. In contrast, adults with deficits in visual attention demonstrate disorganized, random, and often abbreviated search strategies, with numbers frequently being missed on one side of the board. Those with hemi-inattention often show an asymmetric pattern, with visual search initiated and confined to the right side of the board. Clients with a VFD may miss numbers on the blind side but demonstrate an organized search strategy.
Intervention
Information gathered from observing the client complete visual search tests should reveal specific deficiencies in the scanning pattern that the client uses to acquire visual information during the performance of daily tasks. For example, it may be observed that the client does not search toward the left side of visual arrays. If this deficiency is significant, similar performance should be observed when the client completes a daily activity. This could be an inability to locate items placed on the left side of the sink while grooming or a tendency to begin reading a recipe in the middle of the line of print instead of at the left margin.
Depending on the severity of the deficit, some clients with inattention are able to complete basic and habitual daily activities and experience difficulty only with tasks that are unfamiliar or require search of a complex visual array.76 Others, especially those with neglect, may have difficulty with such a simple task as finding all the food on their plate. By combining information from visual search tests with that gained from observation while performing ADLs, it is possible to determine whether and how the client’s performance of daily activities has been affected by the impairment in visual search. The goals on the intervention plan should be worded to reflect the specific daily activities compromised by the inattention. For example, the intervention plan could include such goals as “The client will be able to complete grooming independently” or “The client will be able to prepare a simple meal independently.”
The goals established for independent performance of ADLs are achieved by ensuring that the client learns to take in visual information in a consistent, systematic, and organized manner. Before clients can learn to reorganize a visual search, they must understand how their visual search and attention have changed. To facilitate development of this insight, the OT practitioner should carefully review the results of the client’s performance on the visual search tests and show the client how his or her search pattern differed from the norm and caused errors. If after receiving this feedback the client wishes to retake one of the tests, he or she should be allowed to do so. If the client’s performance improves on the retest, this is an indication of the capability of benefiting from therapy intervention and serves as a justification for intervention. Likewise, if the client’s performance does not improve, this helps verify the significance of the deficit and also may indicate reduced rehabilitation potential.
The intervention plan should incorporate compensatory strategies and environmental modification. The primary compensatory strategy taught to a client with hemi-inattention is to reorganize the scanning pattern to begin visual search on the left side of a visual array and progress from left to right.5,28,88,125,127 Use of this pattern will counteract the client’s tendency to restrict all visual search to the right side and will increase the symmetry of the search pattern. Clients with left hemisphere injuries do not demonstrate asymmetry in visual search but often fail to notice details when searching visual arrays. These clients should be taught to initiate careful item-by-item search of visual arrays. Two scanning strategies are taught to all clients: a left-to-right linear pattern for reading and inspection of small visual detail and a left-to-right clockwise or counterclockwise pattern for viewing unstructured and extra-personal visual arrays.4 Activities should be selected that encourage and reinforce the use of these patterns.
Compensatory strategies can be taught more effectively if intervention activities are designed in accordance with the following guidelines:
1. Intervention activities should require the client to scan as broad a visual space as possible. Most daily activities require orientation to a broad visual space. To help the client complete a wide visual search, the working field of the activity should be large enough to require the client either to turn the head or to change body positions to accomplish the task.127 Many activities and games can be enlarged to require head turning for scanning. For example, a deck of playing cards can be laid out, facing up, in rows 2 to 3 feet wide. The client is given another deck of playing cards and instructed to match the cards in hand to the cards on the table. The practitioner ensures that the client initiates a left-to-right, top-to-bottom, organized scanning pattern when searching for the matching cards to complete the task.
2. Intervention activities will be more effective if the client is required to interact physically with the target once it is located. Research has shown that a stronger mental representation of a visual image is formed if what is seen is verified by tactual exploration.4,67 Whenever possible, the intervention activity should be designed to be interactive. Games such as solitaire, dominoes, and ball games or activities such as putting together large puzzles are examples of activities with interactive qualities.
3. Intervention activities should emphasize conscious attention to visual detail and careful inspection and comparison of targets. Because complex visual processing is dependent on initiation of the item-by-item search strategy of selective visual attention, it is important to include scanning activities that require discrimination of subtle details and matching. Clients should be taught consciously to study objects for their relevant features, with emphasis placed on attending to detail in the impaired space. Many games such as solitaire, double solitaire, Concentration, Connect Four, checkers, Scrabble, and dominoes have these qualities. Large 300- to 500-piece puzzles, word or number searches, crossword puzzles, and needlecrafts such as latch hook also require these performance skills. Throughout performance of these tasks, clients should be encouraged to recheck their work to make sure that critical details are not missed.
4. Facilitate attention to the left half of the visual space by occluding vision in the right half of the visual space. Occlusion of the right half of the visual field has been shown to be effective in increasing the client’s attention toward the left.14 The occluder, made by placing opaque tape over the right side of a pair of safety lenses, is worn while the client completes a therapeutic activity to facilitate attention. The lenses are removed once the activity is completed.
5. Practice the search strategy within context to ensure carryover of application to ADLs. Clinic activities provide a starting place to begin teaching the strategies needed for successful visual perceptual processing. Research has shown, however, that clients with brain injury often do not spontaneously transfer skills from one learning situation to the next. Toglia113 suggested that having the client apply the learned strategy in different contexts of daily living can facilitate transfer of learning. For example, the client can be required to use a left-to-right search strategy when selecting clothes from a closet, searching for items in a refrigerator, or shopping for groceries. The more often the strategy is repeated under varied circumstances, the more the skill is generalized and transferred to new situations. There is no substitute in therapy for the practice of real-life situations to help the client develop insight into abilities and compensation for limitations. Cafeterias, gift shops, and office areas within the hospital and fast-food restaurants and shops surrounding the hospital can be used to expose the client to more realistic and demanding visual environments.
Insight on the part of the client into the nature of the visual deficit and how it has affected functional performance is critical to learning compensation.110–112 According to Toglia,113 one of the reasons that clients with brain injury do not spontaneously recognize their limitations and the need to compensate is that their concept of their capabilities is based on premorbid experiences. This causes these clients to overestimate their abilities after injury. Without a realistic understanding of limitations, the client may be unwilling to use compensatory strategies. To increase insight, Abreu and Toglia1 advocate teaching a client to monitor and control his or her performance by learning to recognize and correct for errors in performance. Giving the client immediate feedback about the performance and pointing out deficiencies facilitate this process of error detection. The process can also be facilitated by teaching the client to use self-monitoring techniques such as activity prediction, in which the client predicts how successfully an activity will be performed and identifies the aspects of the activity in which errors are likely to occur. The client then compares actual performance with predicted performance. This technique helps the client develop anticipatory skills and increase awareness of how the deficit affects functional capabilities. The use of video feedback has also been shown to be useful in enabling clients to understand how their neglect behavior affects occupational performance.112
Some clients, because of the severity of their deficits, lack the cognition to benefit from training in compensatory strategies. Although treatment intervention is limited, such clients may benefit from a modification of the environment to help the client use his or her limited attentional capabilities. The environment can be made more visible and “user-friendly” by reducing factors that place stress on visual processing. Suggested environmental modifications include the following:
1. Reduce the background pattern so that objects in the foreground can be seen more easily. The more densely packed the background pattern, the greater the amount of selective attention needed to locate the desired object. Clients with severe brain injuries may not be able to sustain the effort needed to complete this level of processing and may view their environments as being filled with “visual noise” rather than meaningful objects. Backgrounds can be simplified by eliminating patterned designs and using solid colors on surfaces. Eliminating superfluous objects such as knickknacks and old magazines and organizing frequently used items on shelves and in containers also simplify the background. As a general rule, environments should be sparse and contain only the items needed by the client for completion of daily activities. Items that contain a lot of intrinsic pattern, such as reading material, can be enlarged to decrease the density of the pattern.
2. Ensure that room and task illumination is adequate. Both too little and too much illumination can impair visual processing. However, environments usually contain too little rather than too much light. The type of lighting used should provide bright, even illumination without glare.
3. Increase contrast between background and foreground objects to enhance the visibility of items in the environment that need to be noticed. For example, the edge of a white plate placed on a black place mat is more visible than it would be if placed on a white place mat, and milk is more visible in a black cup than in a white cup. The use of glass or clear plastic items should be avoided because these items reduce contrast by absorbing whatever pattern or color is around them.
Oculomotor Function
The purpose of oculomotor function is to achieve and maintain foveation of an object.42 That is, oculomotor function ensures that the object that the person wishes to view is focused on the fovea of both retinas (to ensure a clear image) and that focus is maintained as long as needed to accomplish the desired goal. This is a daunting task because human beings interact within dynamic, moving environments. An image focused on the fovea is always in danger of slipping off as the head or object is moved. Foveation is achieved and maintained by eye movements that keep the target stabilized on the retina during fixation, gaze shift, and head movement.42,70,77,97
Another function of oculomotor control is to provide binocular vision. Binocular vision ensures perception of a single image even though the CNS is receiving two separate visual images (one from each eye). The process of combining two visual images into one is called sensory fusion. For sensory fusion to occur, corresponding points (or receptor cells) on the two retinas must be stimulated with the same image. If the retinas are thus stimulated and if the images match in size and clarity, the CNS is able to fuse the two images perceptually into one. If the eyes do not align with each other or if there is a significant difference in acuity between the eyes, a double image (diplopia) may occur.42,71,119
Deficits in Oculomotor Function
Deficits in oculomotor control following brain injury generally result from either of two types of disruption: specific cranial nerve lesions causing paresis or paralysis of one or more of the extraocular muscles that control eye movements or disruption of central neural control of the extraocular muscles affecting the coordination of eye movements.5,60,72,74,96,97 In the first case, the message to the extraocular muscles through the cranial nerve is blocked; in the second case, the message comes through but is scrambled. In both cases, the functional results are decreased speed, control, and coordination of eye movements. Three pairs of cranial nerves control the extraocular muscles: the oculomotor nerve (III), the trochlear nerve (IV), and the abducens nerve (VI). Among them, these nerves are responsible for controlling seven pairs of striated muscles that surround and attach to the two eyeballs.
When a cranial nerve lesion is sustained, the muscles controlled by that cranial nerve are weakened or paralyzed, a condition known as paralytic strabismus.82,119 As a result, the eye is unable to move in the direction of the paretic muscles and may even be unable to maintain a central position in the eye socket (i.e., it drifts in or out). Because the eyes must always move in synergy and line up evenly to maintain a single visual image, an individual sees a double image when the movement of one eye is impeded or when the eye’s position changes and does not match that of the other. This condition, diplopia or double vision, is the primary functional disruption observed in individuals with cranial nerve lesions.82,119
Occupational Limitations Caused by Oculomotor Deficits
The presence of diplopia creates perceptual distortion, which may affect eye-hand coordination, postural control, and binocular use of the eyes. The limitations in performance experienced by the client depend on where the diplopia occurs within the focal range (the range in which a person can keep objects in focus). Diplopia occurring within 20 inches of the face will disrupt reading and activities requiring eye-hand coordination, such as pouring liquids, writing, and grooming. Diplopia occurring at a distance (greater than 4 feet) will affect walking, driving, television viewing, and playing sports such as golf and tennis.
To eliminate the double image, the client will often assume a head position that avoids the field of action of the paretic muscle.8,72,119 For example, a client with a left lateral rectus palsy (cranial nerve VI) will turn the head toward the left to avoid the need to abduct the eye. A client with paralysis of the right superior oblique muscle (cranial nerve IV) will tilt the head to the right and downward to avoid the action of that muscle.8 Unless oculomotor function is carefully assessed, these alterations in head position may be interpreted as resulting from changes in muscle tone in the neck rather than as a functional adaptation purposely assumed to stabilize vision.
Often it is not the cranial nerves that are damaged during brain injury but the neural centers that coordinate their actions. These structures are scattered throughout the brainstem and communicate extensively with cortical, cerebellar, and subcortical areas of the CNS and the spinal cord.52,77 In cases of traumatic brain injury, diffuse damage may take place throughout the brainstem and affect these control centers. If the centers are damaged, the person will have difficulty executing eye movements even though the cranial nerves are intact.72,96,97,107 Disconjugate eye movements may occur and cause the client to have difficulty using the eyes together in a coordinated fashion. Dysmetric eye movement, in which the eye undershoots or overshoots a target, may also be observed.106
Damage to the pretectal nuclei in the brainstem can cause convergence insufficiency, a condition in which the client is unable to obtain or sustain convergence of the eyes.25,72 Convergence is the muscle action of moving the eyes inward in adduction. It is one of the three components of accommodation, the process that keeps objects in focus as they come into close view. When convergence insufficiency occurs, clients have difficulty obtaining or sustaining adequate focus during near-vision tasks (tasks within 20 inches of the face). Clients with this condition often complain of fatigue, eye pain, or headache after a period of sustained viewing in near tasks such as reading. As the eye muscles fatigue from the exertion of sustaining convergence during reading, clients may begin to complain that the print is swirling and moving on the page. The condition is frequently overlooked in evaluation because cranial nerve function is usually intact and clients’ complaints are instead attributed to inattention, lack of effort, or dyslexia.25,72
These disturbances in ocular motility can create a variety of functional deficits for the client.72,84 The speed and range of eye movement may be diminished. This will reduce the speed at which the client is able to scan the environment and take in visual information, thereby causing delays in responding to the environment. The client may have difficulty maintaining a clear image and may experience doubling and blurring of visual images.53,72 There may be difficulty focusing at different distances from the body. Depth perception may be diminished. These conditions will create significant visual stress for the client and reduce concentration and endurance for activities. The client may respond to this increased stress by becoming agitated and uncooperative in therapy sessions or by complaining of headaches, eyestrain, or neck strain.
Because a number of factors can disrupt the control of eye movements, much skill and expertise are needed to accurately diagnose the oculomotor deficit and design an appropriate treatment intervention. Practitioners who treat this type of dysfunction should do so under the guidance of an optometrist or ophthalmologist who specializes in visual impairment caused by neurologic conditions.39,84
Assessment
The purpose of an assessment completed by the OT practitioner is to determine whether the client is experiencing limitations in daily occupations because of dysfunction within the oculomotor system. It is not to determine whether the oculomotor dysfunction is the result of a cranial nerve lesion, brainstem injury, or other conditions. Determining the etiology of the dysfunction is the responsibility of the ophthalmologist or optometrist. However, the OT practitioner is often one of the first members of the rehabilitation team to observe that the client may have an oculomotor impairment affecting occupational performance. This frequently places the OT practitioner in the position of requesting further evaluation by an eye care specialist. To make an appropriate referral, it is necessary to perform a screening to identify patterns of oculomotor dysfunction that may account for the functional limitations observed in the client.
In assessing the client, a “listen and look” approach is used wherein the practitioner listens to the complaints being voiced by the client or the rehabilitation staff working with the client and looks for deviations in oculomotor control that may be contributing to these complaints. This approach is described in the biVABA, and the following steps in evaluation are from that assessment.
The first step in assessment is to obtain a visual history from the client. The history is necessary because adults with childhood histories of oculomotor dysfunction or reduced acuity often display oculomotor abnormalities that do not affect functional performance. These individuals frequently wear eyeglasses to correct for the deficiencies; in this case the eyeglasses must be worn during the assessment to obtain accurate results. Areas addressed in this part of the evaluation include whether the client had good vision before the brain injury, whether the client wears eyeglasses, and whether the client has a history of conditions that may affect oculomotor control, such as congenital strabismus, lazy eye, or amblyopia.
Next, the client is asked whether he or she is experiencing diplopia. If the response is affirmative, the client should be questioned about the characteristics of the diplopia. Does the diplopia disappear when one eye is closed? This indicates impairment of the extraocular muscles. Do objects double side to side or on top of one another? Is the diplopia present at near distances or at far distances? Is there any area within the range of focus at which the client is able to achieve single vision? The answers to these questions may suggest which cranial nerve has been injured (Table 24-3) and can also supply important information about limitations that the client may experience in daily activities. The OT practitioner concludes the interview by identifying activities that the client has difficulty performing that could be caused by oculomotor dysfunction. The practitioner should look for a pattern in the client’s response, such as difficulty with activities that require sustained focus in near space (reading, writing, and quilting). The practitioner should pay attention to whether the client’s visual difficulty seems to change with the focal length of the task and whether the client’s fatigue and reduced concentration appear to be related to activities requiring sustained focusing.
TABLE 24-3
Summary of Oculomotor Deficits Associated with Cranial Nerve Lesions
| Oculomotor Nerve III | Trochlear Nerve IV | Abducens Nerve VI |
| Impaired vertical eye movements | Impaired downward and lateral eye movements | Impaired lateral eye movements |
| Lateral diplopia for near-vision tasks | Vertical diplopia for near-vision tasks | Lateral diplopia for far-vision tasks |
| Dilation of pupil and impaired accommodation | With bilateral lesion assumes downward head tilt | |
| Ptosis of eyelid |
The next part of the assessment is observing the client’s eyes and eye movements for deficiencies. First, the eyes are evaluated for asymmetries in pupil size, eyelid function, and eye position as the client focuses on a distant object. Asymmetries such as a dilated pupil in one eye or a droopy eyelid (ptosis) may indicate cranial nerve involvement and suggest difficulty adjusting to light (light sensitivity) and reading. Next, movement of the eyes is observed by asking the client to track a moving object (such as a penlight) through the nine cardinal directions of gaze plus convergence.87 This test can be thought of as an active range-of-motion test of the eyes because the nine cardinal directions represent the directions through which the eyes move. The test is used to determine whether there are deviations in strength and function of the extraocular muscles and is completed by observing the eyes move in a binocular test.
During the test, the OT practitioner observes the following: (1) symmetry of eye movement, (2) whether the eyes move the same distance in each direction, (3) whether the eyes are able to stay on target with a minimum of jerking movements, and (4) whether the client is able to hold the eyes in a deviated position at the end of the range for 2 to 3 seconds. Restriction of eye movement in a specific direction or difficulty moving the eyes in a specific direction may indicate impaired oculomotor function.82 Observing the eyes as they track an object moving toward the bridge of the nose tests convergence. Most adults can maintain focus and track an object to a distance of approximately 3 inches from the bridge of the nose. At that point one eye usually breaks fixation and moves outward. The point at which convergence is broken is known as the near point of convergence.82
Although the near point of convergence is 2 to 3 inches from the bridge of the nose, few adults ever view objects that closely. Therefore, limitations in convergence are not generally functionally significant unless the client is unable to converge the eyes and easily maintain convergence to a distance of 12 to 16 inches from the bridge of the nose. An inability to converge the eyes to this distance and maintain convergence for several seconds while focusing on an object may cause the client to have difficulty performing tasks in near vision that require sustained focus. Observation of convergence insufficiency may explain complaints made by the client regarding such tasks as reading, writing, quilting, or sewing.
The final component of the assessment is diplopia testing, which is completed only if the client is complaining of diplopia.106 Diplopia testing is used to determine the severity of the diplopia and whether it is caused by a “tropia” or a “phoria.” Tropia is the suffix applied when there is a noticeable deviation of the position of one eye in relation to the other when the client is viewing an object.106,119 Phoria is the suffix used when there is a deviation of the eye that is held in check by fusion and is therefore not noticeable when the client is focusing on an object. These terms are used in conjunction with a prefix describing the direction of the deviation. Four prefixes are used: “eso,” meaning turning in of the eye; “exo,” turning out of the eye; “hypo,” turning downward of the eye; and “hyper,” turning upward of the eye. Esotropia therefore describes an observable, inward deviation of the eye commonly described as “crossed eyes,” whereas esophoria indicates that the eye drifts inward when the client is not focusing on an object but is held in check when the client is focusing on an object.72
Diplopia testing is based on the principle that when an eye is required to fixate on an object, it will do so with the fovea. If an eye that is not fixating on a target is suddenly required to foveate, it will achieve foveation by making a saccade toward the target. By requiring the client to fixate with both eyes on a target and then covering one of the client’s eyes during fixation, the examiner can determine whether both eyes are aligned in focusing on the target and, if not, which eye is the deviant (strabismic) one.87,118 Two tests are used: a cover/uncover test, which is completed when a tropia is suspected, and a cross or alternate-cover test, which is completed when a phoria is suspected.87,118 If both eyes are aligned equally and fixating on the target, no movement of either eye will be observed when one is covered. If the eyes are not aligned, the deviating eye will move to take up fixation when the nonaffected eye is covered. Clients with tropias generally complain of constant diplopia when viewing objects and must have one eye occluded to eliminate the diplopia. Clients with phorias often complain of diplopia only intermittently, usually when fatigued or stressed by sustained viewing of a target. Although a phoric client may complete most activities without diplopia, he or she may experience significant visual stress, which can be manifested as headaches, eye strain, or decreased concentration.
The information gathered from the assessment should be compared with the client’s visual complaints and observations of his or her occupational performance to determine whether the oculomotor dysfunction is contributing to the client’s functional limitations. For example, the presence of convergence insufficiency may help explain the difficulty that the client is having in maintaining concentration when reading. As another example, the observation of downward movement of the left eye during the cover/uncover test may explain why the client complains of feeling off balance and unsure when descending stairs. If oculomotor deficiencies are observed that appear to limit occupational performance, referral should be made to an ophthalmologist or optometrist for further evaluation to determine the cause of the deficiency, the prognosis for improvement, and treatment options.
Intervention
The presence of oculomotor dysfunction does not usually prevent the completion of daily occupations; however, it does make completion of daily activities both tedious and fatiguing. The client may express reluctance to perform some activities or even stop performing them because of the constant visual stress. Motor and postural control may also be compromised and consequently reduce safety when navigating the environment. For these reasons, oculomotor dysfunction must be addressed during intervention, although it is not specifically identified as a goal on the intervention plan. That is, the goal remains a functional one such as safe and accurate completion of meal preparation, shopping, or bill paying, and management of the oculomotor dysfunction becomes one of the methods used to achieve the goal.
Intervention can be divided into four types: occlusion, application of a prism, eye exercises, and surgery.12,19,108,119 The last three interventions are used to re-establish fusion and binocularity and are performed only by ophthalmologists or optometrists. OT practitioners, under the direction of a physician, may apply occlusion. Most oculomotor dysfunction clears up without intervention within 6 to 12 months after the brain injury.97,119 Accordingly, ophthalmologists do not generally believe that it is necessary to provide any intervention other than eliminate the diplopia for the client’s comfort during the recuperation period. If the diplopia persists and becomes chronic, surgery can be used to re-establish fusion. Optometrists often choose a remediation approach and prescribe eye exercises to re-establish binocularity, in addition to using occlusion and a prism.12,102 Brief descriptions of these interventions follow. The treatment option selected for a client depends on the prognosis for recovery, the client’s ability to participate in therapy, family and financial resources, and the eye specialist providing consultation.
Occlusion: The presence of diplopia causes perceptual distortion. This distortion creates confusion for the client and limits participation in daily activities. Therefore, diplopia must be eliminated if the client is to fully benefit from rehabilitation. Diplopia is eliminated by occluding the image presented to one eye. Occlusion can be achieved by assuming a head position or by covering one eye. Because assuming a deviant head position often affects motor and postural control, the preferred method is to cover one eye. Occlusion of the eye can be achieved through either full or partial occlusion.12,19,102,108,119
With full occlusion, vision is completely occluded in one eye by the application of a “pirate patch,” a clip-on occluder, or opaque tape. The challenge with complete occlusion is that it eliminates peripheral visual input, which disrupts normal CNS mechanisms for control of balance and orientation to space. This often causes the client to feel off balance and disoriented and reduces depth perception. Another challenge is that the client cannot generally tolerate long periods of occlusion of an eye, especially of the dominant eye. Therefore, for the comfort of the client, the period of occlusion is alternated between the eyes every hour. Alternating occlusion between the eyes also reduces the likelihood of the development of secondary contracture of the muscles antagonistic to the paretic muscle.
For partial occlusion, a strip of opaque material (such as 3M Transpore surgical tape) is applied to a portion of the eyeglass lens to block visual stimulation in the central visual field, with the peripheral visual field being left unoccluded (Figure 24-14). The client is instructed to view a target within the diplopic field. Tape is applied from the nasal rim toward the center of the lens until the client reports that the diplopia is gone when viewing the target. The tape is applied to the nondominant eye for the greater comfort of the client. The width of the tape is gradually reduced as the muscle paresis resolves. An advantage of partial occlusion is that the client is more comfortable and therefore compliance is increased. Another advantage is that peripheral vision is left intact and available for use in orientation to space and balance. The main disadvantage of this type of occlusion is that the client must either wear prescription lenses or have tape applied to a pair of frames with plano (nonrefractive) lenses.
Prisms: Ophthalmologists and optometrists may use a prism to re-establish single vision in the primary directions of gaze: looking straight ahead and looking down. Application of a prism displaces the image and causes the disparate images created by the strabismus to fuse into a single image.12,19,102 The prism can be ground into the eyeglass lenses worn by the client or temporarily applied to the lens of the glasses, as with a plastic Fresnel press-on prism. A prism is used only as long as it is needed to maintain fusion. If the paresis is resolving, the client is gradually weaned from the prism by reducing the dioptic strength of the prism over a period of time commensurate with the rate of recovery.
Eye Exercises: There has yet to be objective research unequivocally demonstrating that the use of eye exercises will restore binocular function following paretic strabismus. Eye exercises do not appear to adversely affect muscle function, however, and the use of eye exercises can empower the client by increasing his or her participation in the recovery process. An optometrist directs the use of eye exercises in this aspect of the rehabilitation program.102
Surgery: Surgery is recommended when the degree of strabismus is too large to be overcome consistently and easily by fusional effort or when the client has a significant strabismic condition that does not resolve in 12 to 18 months.119 The general approach in surgery is to make the action of one of the extraocular muscles either weaker or stronger by changing the position of its attachment on the eyeball. The position of the eye in the socket is changed by the procedure, and the image is realigned. Surgery is performed by an ophthalmologist specially trained in strabismus surgery.
Because Penny sustained a posterior cerebral artery occlusion, the lesion was confined to the right cerebral hemisphere. Subsequently, she did not experience any oculomotor deficits.
Complex Visual Processing
The processes of pattern recognition, visual memory, and visual cognition involve complex processing and integration of vision with other sensory information, past experiences, and cognitive function. To complete this sophisticated level of processing requires not only organized, high-quality sensory input but also good cognitive ability such as the ability to categorize information and complete abstract reasoning. Complex visual processing, like other cognitive functioning, is elicited by the demands of a particular event. It is a learned skill established by one’s experiences in mastering the environment. With few exceptions, complex visual processing is always applied within the context used to solve a problem, formulate a plan, or make a decision regarding a specific situation. Because of the contextual nature of complex visual processing, the best way to assess it is not to ask the client to complete some abstract, two-dimensional visual task but rather to observe the client complete daily tasks requiring this level of processing. For example, if the client is an architect planning to return to work, his or her ability to design and execute building plans or other aspects of the job should be assessed, preferably at the client’s place of employment. If the client wants to return to driving, his or her ability to handle complex traffic situations should be assessed with a behind-the-wheel assessment.
Visual input that is of poor quality or is incomplete or inaccurate will affect the ability to perform complex visual processing. Therefore, visual acuity, visual field, oculomotor control, and visual attention and search should be assessed first to determine whether deficits exist that might be contributing to deficiencies in complex processing. If deficits are identified, their effect on the client’s performance of daily occupations requiring complex visual processing should be observed. For example, after having determined that a client has a left VFD and an incomplete search pattern indicative of hemi-inattention, the OT practitioner should observe the client complete a daily occupation requiring attending, planning, and decision making. The activity may be preparing a meal, sorting and doing laundry, shopping for groceries, measuring the oil level in the car, or completing a job-related task. In observing the client, the practitioner should make special note of how the client’s visual deficit affects his or her ability to process the more complex visual information needed to complete the task. If the client has difficulty successfully completing the task and if the visual deficit appears to be the cause, the practitioner should determine whether it is possible to improve the client’s performance by treatment of the visual deficit.
Summary
The CNS relies on visual information to anticipate and plan adaptation to the environment and perform daily occupations. Brain injury or disease disrupts the processing of visual information, thereby creating gaps in the visual input sent to the CNS. The quality of a person’s occupational performance decreases because the CNS does not have sufficient or accurate visual information to make decisions. Penny’s left hemianopia, for example, caused her to misread words and sentences because she did not always see letters and words on the left side; she also collided with persons and objects and experienced disorientation because of missing information on the left side. Whether a person’s deficit in visual perceptual processing necessitates thera-peutic intervention depends on the person’s lifestyle and whether the visual deficit prevents successful completion of ADLs. In Penny’s case, as the primary caregiver for an ailing husband, she needed to be able to complete the family finances, drive, and shop; if her husband had been fit, she may not have needed to perform these activities.
The framework for assessment and intervention rests on the concept of a hierarchy of visual perceptual proc-essing levels that interact with and subserve one another. Because of the unity of the hierarchy, a process cannot be disrupted at one level without an adverse effect on all perceptual processing. Assessment must be directed at measuring function at all process levels, with particular emphasis placed on the foundation of visual functions and visual attention and scanning. The absence of visual input on the left side caused Penny to appear to ignore visual stimuli on the left, which gave the impression of hemi-inattention. Assessment demonstrated that she has normal attentional capability but had not yet learned to compensate for the hemianopia.
Intervention focuses on increasing the accuracy and organization of visual input into the system through mani-pulation of the environment and by providing the client with strategies to compensate for or minimize the effect of the deficit in daily occupations. Penny benefited from a variety of compensatory and remediation strategies aimed at improving her ability to use her remaining right visual field to compensate for the left VFD and to adapt her environment to assist her in using her remaining vision to complete daily activities.
1. What determines whether treatment intervention is needed for a client with a visual impairment?
2. What three aspects of environments/tasks can be modified to increase their visibility for a client with visual impairment?
3. What prevents a client from automatically compensating for a VFD by turning the head farther to see around the blind field?
4. What kind of protective behaviors do persons adopt following onset of a VFD? Why do they adopt these strategies?
5. What is the normal search pattern executed by most adults when viewing an unstructured visual array? A structured array?
6. What is the primary compensatory strategy taught to the client with hemi-inattention?
7. What is the most crucial lower-level visual process contributing to the ability to complete visual cognitive processing?
8. What changes occur in the visual search pattern of a client with hemi-inattention?
9. When would partial occlusion be used for the client? Describe the technique used to apply partial occlusion.
10. How does convergence insufficiency affect reading performance?
References
1. Abreu, BC, Toglia, JP. Cognitive rehabilitation: a model for occupational therapy. Am J Occup Ther. 1987;41:439.
2. American Heritage dictionary of the English language. New York, NY: Houghton Mifflin, 1969.
3. Anderson, BR. Perimetry with and without automation, ed 2. St. Louis, Mo: Mosby; 1987.
4. Andrews, TJ, Copolla, DM. Idiosyncratic characteristics of saccadic eye movements when viewing different visual environments. Vision Res. 1999;39:2947.
5. Antonucci, G, Guariglia, C, Judica, A, et al. Effectiveness of neglect rehabilitation in a randomized group study. J Clin Exp Neuropsychol. 1995;17:383.
6. Ayres, AJ. Sensory integration and learning disorders. Los Angeles, Calif: Western Psychological Services; 1972.
7. Azzopardi, P, Cowey, A. Is blindsight like normal, near-threshold vision? Proc Natl Acad Sci U S A. 1997;94:14190.
8. Baker, RS, Epstein, AD. Ocular motor abnormalities from head trauma. Surv Ophthalmol. 1991;36:245.
9. Barinaga, M. The mapmaking mind. Science. 1999;285:189.
10. Barton, JJ, Behrmann, M, Black, S. Ocular search during line bisection. The effects of hemi-neglect and hemianopsia. Brain. 1998;121:1117.
11. Barton, JJ, Black, SE. Line bisection in hemianopsia. J Neurol Neurosurg Psychiatry. 1998;66:122.
12. Bedrossian, EH. Non surgical management: acquired ocular muscle paralysis. In: The surgical and non surgical management of strabismus. Springfield, Ill: Charles C Thomas; 1969.
13. Behrmann, M, Shomstein, SS, Black, SE, Barton, JJ. The eye movements of pure alexic patients during reading and nonreading tasks. Neuropsychologia. 2001;39:983.
14. Beis, JM, André, JM, Baumgarten, A, Challier, B. Eye patching in unilateral spatial neglect: efficacy of two methods. Arch Phys Med Rehabil. 1999;80:71.
15. Belleza, T, Rappaport, M, Hopkins, HK, Hall, K. Visual scanning and matching dysfunction in brain damaged patients with drawing impairment. Cortex. 1979;15:19.
16. Bodis-Wollner, I, Diamond, SP. The measurement of spatial contrast sensitivity in cases of blurred vision associated with cerebral lesions. Brain. 1976;99:695.
17. Bower, B. Joined at the senses: perception may feast on a sensory stew, not a five-sense buffet. Science News. 2001;160:204.
18. Brendler, K, Trauzettel-Klosinski, S, Sadowski, B. Reading disability in hemianopic field defects: the significance of clinical parameters. Invest Ophthalmol Vis Sci. 1996;37:S1079.
19. Bulens, C, Meerwaldt, JD, van der Wildt, GJ, Keemink, CJ. Spatial contrast sensitivity in unilateral cerebral ischaemic lesion involving the posterior visual pathway. Brain. 1989;112:507.
20. Cassidy, TP, Bruce, DW, Lewis, S, Gray, CS. The association of visual field deficits and visuo-spatial neglect in acute right hemisphere stroke patients. Age Ageing. 1999;28:257.
21. Cate, Y, Richards, L. Relationship between performance on tests of basic visual functions and visual perceptual processing in persons after brain injury. Am J Occup Ther. 2000;54:326.
22. Chédru, F, Leblanc, M, Lhermitte, F. Visual searching in normal and brain damaged subjects. Cortex. 1973;9:94.
23. Chen Sea, MJ, Henderson, A, Cermak, SA. Patterns of visual spatial inattention and their functional significance in stroke patients. Arch Phys Med Rehabil. 1993;74:355.
24. Chokron, S, Colliot, P, Bartolomeo, P. The role of vision in spatial representation. Cortex. 2004;40:281.
25. Cohen, M, Groswasser, Z, Barchadski, R, Appel, A. Convergence insufficiency in brain-injured patients. Brain Inj. 1989;2:187.
26. Colenbrander, A. The functional vision score, a coordinated scoring system for visual impairments, disabilities and handicaps. In: Kooijan AC, et al, eds. Low vision: research and new development in rehabilitation. Amsterdam: IOS Press, 1994.
27. Daini, R, Angelelli, P, Antonucci, G, et al. Exploring the syndrome of spatial unilateral neglect through an illusion of length. Exp Brain Res. 2002;144:224.
28. Delis, DC, Robertson, LC, Balliet, R. The breakdown and rehabilitation of visuospatial dysfunction in brain injured patients. Int Rehabil Med. 1983;5:132.
29. DeLuca, M, Spinelli, D, Zoccolotti, P. Eye movement patterns in reading as function of visual field defects and contrast sensitivity loss. Cortex. 1996;32:491.
30. Demb, JB, Boynton, GM, Heeger, DJ. Brain activity in visual cortex predicts individual differences in reading performance. Proc Natl Acad Sci U S A. 1997;94:13363.
31. De Renzi, E, Gentilini, M, Faglioni, P, Barbieri, C. Attentional shift towards the rightmost stimuli in patients with left visual neglect. Cortex. 1989;25:231.
32. Di Pace, E, Guariglia, C, Judica, A, et al. Selective reading slowness in a traumatic patient with impairment in basic visual processes. J Clin Exp Neuropsychol. 1995;17:878.
33. Duffy, M. Making life more livable: simple adaptations for living at home after vision loss. New York, NY: American Foundation for the Blind Press; 2002.
34. Festinger, L. Eye movements and perception. In: Bach Y, Rita P, Collins CC, eds. The control of eye movements. New York, NY: Academic Press, 1971.
35. Findlay, JM, Kapoula, Z. Scrutinization, spatial attention, and the spatial programming of saccadic eye movements. Q J Exp Psychol. 1992;45:633.
36. Fletcher, DC, Shindell, S, Hindman, T, Schaffrath, M. Low vision rehabilitation: finding capable people behind damaged eyeballs. West J Med. 1991;154:554.
37. Gainotti, G, Giustolisi, L, Nocentini, U. Contralateral and ipsilateral disorders of visual attention in patients with unilateral brain damage. J Neurol Neurosurg Psychiatry. 1990;53:422.
38. Gianutsos, R, Matheson, P. The rehabilitation of visual perceptual disorders attributable to brain injury. In: Meier MJ, Benton AL, Diller L, eds. Neuropsychological rehabilitation. New York, NY: Guilford Press, 1987.
39. Gianutsos, R, Ramsey, G, Perlin, RR. Rehabilitative optometric services for survivors of acquired brain injury. Arch Phys Med Rehabil. 1988;69:573.
40. Gilhotra, JS, Mitchell, P, Healey, PR, et al. Homonymous visual field defects and stroke in an older population. Stroke. 2002;33:2417.
41. Glass, I, Groswasser, Z, Groswasser-Reider, I. Impersistent execution of saccadic eye movements after traumatic brain injury. Brain Inj. 1995;9:769.
42. Goldberg, ME. The control of gaze. In Kandel ER, Schwartz JH, Jessell TM, eds.: Principles of neural science, ed 4, New York, NY: McGraw-Hill, 2000.
43. Graziano, MS, Yap, GS, Gross, CG. Coding of visual space by premotor neurons. Science. 1994;266:1054.
44. Gross, CG, Graziano, MSA. Multiple representations of space in the brain. Neuroscientist. 1995;1:40.
45. Halligan, PW, Burn, JP, Marshall, JC, Wade, DT. Visuo-spatial neglect: qualitative difference and laterality of cerebral lesion. J Neurol Neurosurg Psychiatry. 1992;55:1060.
46. Harrington, DO. The visual fields: a textbook and atlas of clinical perimetry, ed 2. St. Louis, Mo: Mosby; 1964.
47. Heilman, K, Van Den Abel, T. Right hemisphere dominance for attention: the mechanism underlying hemispheric asymmetries of inattention (neglect). Neurology. 1980;30:3.
48. Hess, RF, Pointer, JS. Spatial and temporal contrast sensitivity in hemianopsia: a comparative study of the sighted and blind hemifields. Brain. 1989;112:871.
49. Holt, LJ, Anderson, SF. Bilateral occipital lobe stroke with inferior altitudinal defects. Optometry. 2000;71:690.
50. Hyvarinen, L. Vision testing manual. Villa Park, Ill: Precision Vision; 1996.
51. Ishiai, S, Furukawa, T, Tsukagoshi, H. Eye fixation patterns in homonymous hemianopsia and unilateral spatial neglect. Neuropsychologia. 1987;25:675.
52. Jung, DS, Park, KP. Post traumatic bilateral internuclear ophthalmoplegia with exotropia. Arch Neurol. 2004;60:429.
53. Kahn, J. Blunt trauma to orbital soft tissues. In: Shingleton BJ, ed. Eye trauma. St. Louis, Mo: Mosby, 1991.
54. Kandel, E, Wurtz, R. Central visual pathways. In Kandel ER, Schwartz JH, Jessell TM, eds.: Principles of neural science, ed 4, New York, NY: McGraw-Hill, 2000.
55. Kandel, E, Wurtz, R. Constructing the visual image. In Kandel ER, Schwartz JH, Jessell TM, eds.: Principles of neural science, ed 4, New York, NY: McGraw-Hill, 2000.
56. Kandel, E, Wurtz, R. Perception of motion, depth and form. In Kandel ER, Schwartz JH, Jessell TM, eds.: Principles of neural science, ed 4, New York, NY: McGraw-Hill, 2000.
57. Kanski, JJ. Clinical ophthalmology. Toronto, Canada: Mosby; 1984.
58. Kasten, E, Poggel, DA, Sabel, BA. Computer-based training of stimulus detection improves color and simple pattern recognition in the defective field of hemianopic subjects. J Cogn Neurosci. 2000;12:1001.
59. Kasten, E, Wüst, S, Behrens-Baumann, W, Sabel, BA. Computer-based training for the treatment of partial blindness. Nat Med. 1998;4:1083.
60. Keane, JR. Fourth nerve palsy: historical review and study of 215 patients. Neurology. 1993;43:2439.
61. Kerkhoff, G, Artinger, F, Ziegler, W. Contrasting spatial hearing deficits in hemianopsia and spatial neglect. Neuroreport. 1999;10:3555.
62. Kerkhoff, G, Münssinger, U, Meier, EK. Neurovisual rehabilitation in cerebral blindness. Arch Neurol. 1994;51:474.
63. Klavora, P, Gaskovski, P, Heslegrave, RJ, Young, M. Rehabilitation of visual skills using the Dynavision: a single case experimental design. Can J Occup Ther. 1995;62:37.
64. Klavora, P, Gaskovski, P, Martin, K, et al. The effects of Dynavision rehabilitation on behind-the-wheel driving ability and selected psychomotor abilities of persons post-stroke. Am J Occup Ther. 1995;49:534.
65. Klavora, P, Heslegrave, RJ, Young, M. Driving skills in elderly persons with stroke: comparison of two new assessment options. Arch Phys Med Rehabil. 2000;81:701.
66. Klavora, P, Warren, M. Rehabilitation of visuomotor skills in poststroke patients using the Dynavision apparatus. Percept Mot Skills. 1998;86:23.
67. Làdavas, E, Berti, A, Ruozzi, E, Barboni, F. Neglect as a deficit determined by an imbalance between multiple spatial representations. Exp Brain Res. 1997;116:493.
68. Leff, AP, Crewes, H, Plant, GT, et al. The functional anatomy of single-word reading in patients with hemianopic and pure alexia. Brain. 2001;124:510.
69. Leff, AP, Scott, SK, Crewes, H, et al. Impaired reading in patients with right hemianopia. Ann Neurol. 2000;47:171.
70. Leigh, RJ, Brandt, T. A reevaluation of the vestibulo-ocular reflex: new ideas of its purpose, properties, neural substrate and disorders. Neurology. 1993;43:1288.
71. Leigh, RJ, Zee, DS. Neurology of eye movements, ed 2. Philadelphia, Pa: FA Davis; 1991.
72. Lepore, FE. Disorders of ocular motility following head trauma. Arch Neurol. 1995;52:924.
73. Levine, DH. Unawareness of visual and sensorimotor deficits: a hypothesis. Brain Cogn. 1990;13:233.
74. Locher, PJ, Bigelow, DL. Visual exploratory activity of hemiplegic patients viewing the motor-free visual perception test. Percept Mot Skills. 1983;57:91.
75. Marshall, JC, Halligan, PW. Imagine only half of it. Nature. 1993;364:193.
76. Marshall, SC, Grinnell, D, Heisel, B, et al. Attentional deficits in stroke patients: a visual dual task experiment. Arch Phys Med Rehabil. 1997;78:7.
77. Marx, P. Supratentorial structures controlling oculomotor functions and their involvement in cases of stroke. Eur Arch Psychiatry Clin Neurosci. 1989;239:3.
78. Meienberg, O, Zangemeister, WH, Rosenberg, M, et al. Saccadic eye movement strategies in patients with homonymous hemianopia. Ann Neurol. 1981;9:537.
79. Mesulam, MM. Spatial attention and neglect: parietal, frontal and cingulate contributions to the mental representation and attentional targeting of salient extrapersonal events. Phil Trans R Soc London. 1998;354:1325.
80. Miki, A, Nakajima, T, Fujita, M, et al. Functional magnetic resonance imaging in homonymous hemianopsia. Am J Ophthalmol. 1996;121:258.
81. Moore, JC. The visual system, course syllabus for OT Australia national CPE program. Melbourne: Australian Occupational Therapy Association; 1997.
82. Neger, RE. The evaluation of diplopia in head trauma. J Head Trauma Rehabil. 1989;4:31.
83. Noton, D, Stark, L. Scanpaths in eye movements during pattern perception. Science. 1971;171:308.
84. Padula, WV. A behavioral vision approach for persons with physical disabilities. Santa Anna, Calif: Optometric Extension Program Foundation; 1988.
85. Palmer, T, Tzeng, OJL. Cerebral asymmetry in visual attention. Brain Cogn. 1990;13:46.
86. Pambakian, ALM, Kennard, C. Can visual function be restored in patients with homonymous hemianopia? Br J Ophthalmol. 1997;81:324.
87. Park, M. Eye movements and positions. In: Duane TD, ed. Clinical ophthalmology: strabismus, refraction, the lens. Philadelphia, Pa: Harper & Row, 1981.
88. Paul, S. Effects of computer assisted visual scanning training in the treatment of visual neglect: three case studies. Phys Occup Ther Geriatr. 1996;14:33.
89. Pommerenke, K, Markowitsch, HJ. Rehabilitation training of homonymous visual field defects in patients with postgeniculate damage of the visual system. Restor Neurol Neurosci. 1989;1:47.
90. Posner, MI, Rafal, RD. Cognitive theories of attention and the rehabilitation of attentional deficits. In: Meier MJ, Benton AL, Diller L, eds. Neuropsychological rehabilitation. New York, NY: Guilford, 1987.
91. Ramachandran, VS, Blakeslee, S. Phantoms in the brain: probing the mysteries of the human mind. New York, NY: William Morrow; 1998.
92. Rao, SC, Rainer, G, Miller, EK. Integration of what and where in the primate prefrontal cortex. Science. 1997;6:821.
93. Rapcsak, SZ, Verfaellie, M, Fleet, WS, Heilman, KM. Selective attention in hemispatial neglect. Arch Neurol. 1989;46:178.
94. Reuter-Lorenz, PA, Kinsbourne, M. Hemispheric control of spatial attention. Brain Cogn. 1990;12:240.
95. Robinson, DL, Petersen, SE. The pulvinar and visual salience. Trends Neurosci. 1992;15:1.
96. Ron, S, Gur, S. Gaze and eye movement disorders. Curr Opin Neurol Neurosurg. 1992;5:711.
97. Ron, S, Najenson, T, Hary, D, Pryworkin, W. Eye movements in brain damaged patients. Scand J Rehabil Med. 1978;10:39.
98. Rubin, N, Nakayama, K, Shapley, R. Enhanced perception of illusory contours in the lower versus upper visual hemifields. Science. 1996;1:651.
99. Safran, AB, Landis, T. Plasticity in the adult visual cortex: implications for the diagnosis of visual field defects and visual rehabilitation. Curr Opin Ophthalmol. 1996;7:53.
100. Sasaki, Y, Hadjikhani, N, Fischl, B, et al. Local and global attention are mapped retinoptically in human cortex. Proc Natl Acad Sci U S A. 2001;98:2077.
101. Schall, JD, Hanes, DP. Neural basis of saccade target selection in frontal eye field during visual search. Nature. 1993;2:467.
102. Scheiman, M. Understanding and managing vision deficits: a guide for occupational practitioners. Thorofare, NJ: Slack; 1997.
103. Schiller, PH, Chou, IH. The effects of frontal eye field and dorsomedial frontal cortex lesions on visually guided eye movements. Nat Neurosci. 1998;1:248.
104. Schoepf, D, Zangemeister, WH. Target predictability influences the distribution of coordinated eye-head gaze saccades in patients with homonymous hemianopia. Neurol Res. 1996;18:425.
105. Schuchard, RA. Adaptation to macular scotomas in persons with low vision. Am J Occup Ther. 1995;49:870.
106. Simon, RP, et al. Disturbances of vision. In: Clinical neurology. Norwalk, Conn: Appleton & Lange; 1989.
107. Spiers, PA, Schomer, DL, Blume, HW, et al. Visual neglect during intracarotid amobarbital testing. Neurology. 1990;40:1600.
108. Sterk, CC. The conservative management of diplopia. In: Sanders EACM, DeKeizer RJW, Zee DS, eds. Eye movement disorders. Boston, Mass: Martinus Nijhoff/Dr W Junk, 1987.
109. Tessier-Lavigne, M. Visual processing by the retina. In Kandel ER, Schwartz JH, Jessell TM, eds.: Principles of neural science, ed 4, New York, NY: McGraw-Hill, 2000.
110. Tham, K, Borell, L, Gustavsson, A. The discovery of disability: a phenomenological study of unilateral neglect. Am J Occup Ther. 2000;54:398.
111. Tham, K, Ginsburg, E, Fisher, AG, Tegnér, R. Training to improve awareness of disabilities in clients with unilateral neglect. Am J Occup Ther. 2001;55:46.
112. Tham, K, Tegner, R. Video feedback in the rehabilitation of patients with unilateral neglect. Arch Phys Med Rehabil. 1997;78:410.
113. Toglia, J. Generalization of treatment: a multicontext approach to cognitive perceptual impairment in adults with brain injury. Am J Occup Ther. 1991;45:505.
114. Trauzettel-Klosinski, S, Brendler, K. Eye movements in reading with hemianopic field defects; the significance of clinical parameters. Arch Clin Exp Ophthalmol. 1998;236:91.
115. Trexler, LE. Volitional control of homonymous hemianopsia. Neuropsychologia. 1998;36:573.
116. Trobe, JD, Acosta, PC, Krischer, JP, Trick, GL. Confrontation visual field techniques in the detection of anterior visual pathway lesions. Ann Neurol. 1981;10:28.
117. Tyler, HR. Defective stimulus exploration in aphasic patients. Neurology. 1969;19:105.
118. Van Vliet, AGM. Bedside examination. In: Sanders EACM, De Keizer RJW, Zee DS, eds. Eye movement disorders. Boston, Mass: Martinus Nijhoff/Dr W Junk, 1987.
119. Von Noorden, GK, Paralytic strabismus. Binocular vision and ocular motility: theory and management of strabismus, ed 6, St. Louis, Mo, Mosby, 2001.
120. Warren, M. A hierarchical model for evaluation and treatment of visual perceptual dysfunction in adult acquired brain injury. I, II. Am J Occup Ther. 1993;47:42.
121. Warren, M. Brain injury visual assessment battery for adults test manual. Birmingham, Ala: visAbilities Rehab Services; 1998.
122. Warren, M. Identification of visual scanning deficits in adults after cerebrovascular accident. Am J Occup Ther. 1990;44:391.
123. Warren, M. Prereading and writing exercises for persons with macular scotomas. Birmingham Ala: visAbilities Rehab Services; 1996.
124. Watson, GR, Baldasare, J, Whittaker, S. The validity and clinical uses of the Pepper Visual Skills for Reading Test. J Visual Impair Blind. 1990;84:119.
125. Weinberg, J, Diller, L, Gordon, WA, et al. Visual scanning training effect on reading-related tasks in acquired right brain damage. Arch Phys Med Rehabil. 1979;60(11):491.
126. Weintraub, S, Mesulam, MM. Visual hemispatial inattention: stimulus parameters and exploratory strategies. J Neurol Neurosurg Psychiatry. 1988;51:1481.
127. Wiart, L, Côme, AB, Debelleix, X, et al. Unilateral neglect syndrome rehabilitation by trunk rotation and scanning training. Arch Phys Med Rehabil. 1997;78:424.
128. Winckelgren, I. How the brain “sees” borders where there are none. Science. 1992;256:1520.
129. Wong, AM, Sharpe, JA. Representation of the visual field in the human occipital cortex: a magnetic resonance imaging and perimetric correlation. Arch Ophthalmol. 1999;117:208.
130. Wright, V, Watson, G. Learn to use your vision for reading workbook. LUV reading series. Trooper, Pa: Homer Printing; 1995.
131. Yarbus, AL. Eye movements during perception of complex objects. In: Yarbus AL, ed. Eye movements and vision. New York, NY: Plenum, 1967.
132. Zangemeister, WH, Meienberg, O, Stark, L, Hoyt, WF. Eye head coordination in homonymous hemianopsia. J Neurol. 1982;226:243.
133. Zihl, J. Eye movement patterns in hemianopic dyslexia. Brain. 1987;118:891.
134. Zihl, J. Rehabilitation of visual impairments in patients with brain damage. In: Kooijan AC, ed. Low vision: research and new development in rehabilitation. Amsterdam: IOS Press, 1994.
135. Zihl, J. Visual scanning behavior in patients with homonymous hemianopia. Neuropyschologia. 1995;33:287.
Brain Injury Visual Assessment Battery for Adults
visAbilities Rehab Services, Inc.
LeaNumbers and LeaSymbols Low Contrast Tests
Visual Skills for Reading Test
Lighthouse International, Professional Low Vision Products
Warren Pre-reading and Writing Exercises for Persons with Macular Scotomas
visAbilities Rehab Services, Inc.
Learn to Use Your Vision for Reading Workbook