Evaluation and Treatment of Limited Occupational Performance Secondary to Cognitive Dysfunction
Cognition and occupational therapy
Overview of models that guide the practice of occupational therapy
Choosing appropriate assessments
Managing cognitive dysfunction that limits occupational performance: assessment and interventions
After studying this chapter, the student or practitioner will be able to do the following:
1 Understand the interplay between cognition and performance in areas of occupation.
2 Choose appropriate standardized, reliable, and ecologically valid tools to measure baseline status and client progression.
3 Understand the impact of impaired client factors and performance skills on performance in areas of occupation.
4 Develop an evidence-based treatment plan to maximize participation in chosen occupations for those with cognitive dysfunction.
Cognition and Occupational Therapy
Occupational therapy is one of several professions (e.g., psychology, psychiatry, neuropsychology, speech-language pathology, neurology) involved in the arena of working with those who are cognitively impaired. However, the approach of occupational therapy to this area of practice is unique and differentiated from other disciplines. The clinical focus of what most professions call cognitive rehabilitation or working on cognition is better described by occupational therapists (OTs) as the process of improving function and quality of life for individuals with cognitive impairments. In terms of maintaining this unique focus, the reader should consider the following points related to the process and domain of the practice of occupational therapy as it relates to this area of practice:
• Evaluations/assessment should be focused on clients performing relevant occupations. Simultaneously (as will be described later), the OT documents what impairment or patterns of impairment in client factors and performance skills are interfering with performance and participation.10
• Goals should be related to improving performance in areas of occupation, as described by the second edition of the Occupational Therapy Practice Framework.3
• Interventions should consist of primarily graded relevant occupations being performed in natural contexts.
• Finally, the outcomes of occupational therapy intervention for this population should document improved performance in areas of occupation.
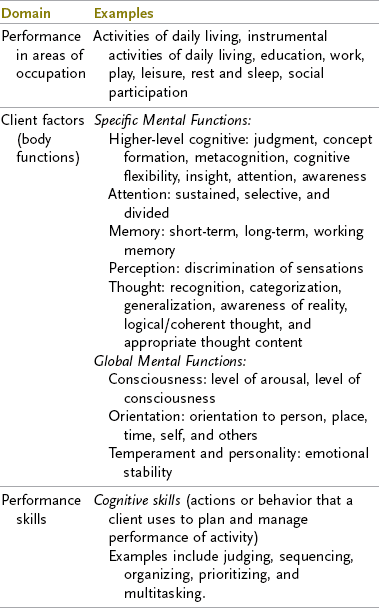
Although these points may seem obvious, until recently this area of occupational therapy practice has focused primarily on impairments in client factors, and the focus of intervention involved the use of contrived “cognitive tasks” to treat this population. Outcomes were then measured on the basis of tests of cognition that were not related to function. It was assumed that remediation of an identified impairment or impairments would generalize into the ability to perform meaningful, functional activities. In general, this assumption has not been supported by empiric research.41 It has become clear that this approach is not consistent with present approaches to occupational therapy.3 Current practice embraces interventions that focus on strategies for living independently, with a purpose, and with improved quality of life despite the presence of cognitive impairments. Likewise, outcome measures that focus on documenting improved functioning outside a clinic environment and those that include test items focused on performing functional activities are being embraced.41 The remainder of this chapter focuses on areas of occupation, client factors, and performance skills3 and their relationships (Table 26-1).
Overview of Models That Guide the Practice of Occupational Therapy
Various models that guide this practice area have been described in the literature. The reader is referred to Katz for a comprehensive description of these models.50 The following paragraphs are examples and summaries of commonly used approaches. A common theme used for this area of practice is maintaining a client-centered approach when providing rehabilitation services “which embraces a philosophy of respect for, and partnership with, people receiving services. Client-centered service fosters an active partnership where the client joins with the OT to design and implement an intervention program to best meet the client’s unique needs.”56
van den Broek specifically recommends using a client-centered approach as a way to enhance rehabilitation outcomes and states that treatment failure may be secondary to clinicians focusing interventions on what they believe the client needs rather than what the client actually wants.110 Another argument for using a client-centered approach to guide the focus of intervention for this population is that the interventions typically used for those with cognitive dysfunction are notoriously difficult to generalize to other real-world settings and situations. For example, strategies that are taught to accomplish a specific task (e.g., using an alarm watch to maintain a medication schedule for those with memory loss) will not necessarily generalize or “carry over” to another task such as remembering therapy appointments. Finally, there are a large number of clients whose level of brain damage precludes them from generalizing learned tasks.69 This issue of task specificity related to treatment interventions must always be considered by clinicians working with this population. A client-centered approach will help ensure that the outcomes, goals, and tasks used as the focus of therapy are at least relevant, meaningful, and specific to each client, as well as the caretaker or significant others, despite the potential lack of being generalizable for a segment of the population affected by various cognitive impairments.
Dynamic Interactional Approach
The Dynamic Interactional Approach views cognition as a product of the interaction among the person, activity, and environment.106 Therefore, performance of a skill can be promoted by changing either the demands of the activity, the environment in which the activity is carried out, or the person’s use of particular strategies to facilitate skill performance. Toglia describes several constructs associated with this model, including the following:
• Structural capacity or physical limits in the ability to process and interpret information
• Personal context or characteristics of the person, such as coping style, beliefs, values, and lifestyle
• Self-awareness or understanding your own strengths and limitations, as well as metacognitive skills such as the ability to judge demands of tasks, evaluate performance, and anticipate the likelihood of problems
• Processing strategies or underlying components that improve the performance of tasks, such as attention, visual processing, memory, organization, and problem solving
• The activity itself with respect to its demands, meaningfulness, and how familiar the activity is
• Environmental factors such as the social, physical, and cultural aspects.
Toglia summarizes that “to understand cognitive function and occupational performance, one needs to analyze the interaction among person, activity, and environment. If the activity and environmental demands change, the type of cognitive strategies needed for efficient performance changes as well. Optimal performance is observed when there is a match between all three variables. Assessment and treatment reflect this dynamic view of cognition.” This approach may be used with adults, children, and adolescents.
Toglia used the Dynamic Interactional Model to develop the Multicontext Treatment Approach.106,107 Combining both remedial and compensatory strategies, this approach focuses on teaching a particular strategy to perform a task and practicing this strategy across different activities, situations, and environments over time. Toglia summarizes the components of this approach to include the following:
• Awareness training or structured experiences should be used in conjunction with self-monitoring techniques so that clients may redefine their knowledge of their strengths and weaknesses.
• Use a personal context strategy. The choice of treatment activities is based on the client’s interests and goals. Particular emphasis is placed on the relevance and purpose of the activities. Managing monthly bills may be an appropriate activity for a single person living alone, whereas crossword puzzles may be used as an activity for a retiree who previously enjoyed this activity.
• Processing strategies are practiced during a variety of functional activities and situations. Toglia defines processing strategies as strategies that help a client control cognitive and perceptual symptoms such as distractibility, impulsivity, inability to shift attention, disorganization, attention to only one side of the environment, or a tendency to overly focus on one part of an activity.
• Activity analysis is used to choose tasks that systematically place increased demands on the ability to generalize strategies that enhance performance.
• Transfer of learning occurs gradually and systematically as the client practices the same strategy during activities that gradually differ in physical appearance and complexity.
• Interventions occur in multiple environments to promote generalization of learning.
Quadraphonic Approach
The Quadraphonic Approach was developed by Abreu and Peloquin for use with those who are cognitively impaired after brain injury.1 This approach is described as including both a “micro” perspective (i.e., a focus on the remediation of subskills such as attention, memory, etc.) and a “macro” perspective (i.e., a focus on functional skills such as activities of daily living [ADLs], leisure, etc.). The approach supports the use of remediation, as well as compensatory strategies.
The micro perspective incorporates four theories:
1. Teaching-learning theory is used to describe how clients use cues to increase cognitive awareness and control.
2. Information-processing theory describes how an individual perceives and reacts to the environment. Three successive processing strategies are described, including detection of a stimulus, discrimination and analysis of the stimulus, and selection and determination of a response.
3. Biomechanical theory is used to explain the client’s movement, with an emphasis on integration of the central nervous system, musculoskeletal system, and perceptual-motor skills.
4. Neurodevelopmental theory is concerned with quality of movement.
The macro perspective involves the use of narrative and functional analysis to explain behavior based on the following four characteristics:
1. Lifestyle status or personal characteristics related to performing everyday activities
2. Life stage status such as childhood, adolescence, adulthood, and marriage
3. Health status such as the presence of premorbid conditions
4. Disadvantage status or the degree of functional restrictions resulting from impairment
Cognitive-Retraining Model
The Cognitive-Retraining Model is used for adolescents and adults with neurologic and neuropsychologic dysfunction.11 Based on neuropsychologic, cognitive, and neurobiologic rationales, this model focuses on cognitive training by enhancing clients’ remaining skills and teaching cognitive strategies, learning strategies, or procedural strategies.
Neurofunctional Approach
The neurofunctional approach is applied to those with severe cognitive impairments secondary to brain injuries.37 The approach focuses on training clients in highly specific compensatory strategies (not expecting generalization) and specific task training. Contextual and metacognitive factors are specifically considered during intervention planning. The approach does not target the underlying cause of the functional limitation but focuses directly on retraining the skill itself.
Task-Oriented Approach
Though usually discussed in relation to motor control dysfunction, the Task-Oriented Approach has potential application to this population as well.78 Mathiowetz has discussed this approach in detail.64 Summary points related to the adoption of a framework for evaluation with this approach include evaluating the following areas in the described order64,65:
1. Role performance (social participation): Identify past roles and whether they can be maintained or need to be changed; determine how future roles will be balanced.
2. Occupational performance tasks (areas of occupation).
3. Task selection and analysis: What client factors, performance skills and patterns, and/or contexts and activity demands limit or enhance occupational performance?
4. Person (client factors, performance skills and patterns): Cognitive—orientation, attention span, memory, problem solving, sequencing, calculations, learning, and generalization; psychosocial; and sensorimotor.
5. Environment (context and activity demands): Including physical, socioeconomic, and cultural.
In terms of intervention, Mathiowetz and Bass Haugen65 and Mathiowetz64 recommend the following:
• Help patients adjust to their role and limitations in performing tasks.
• Create an environment that uses the common challenges of everyday life.
• Practice functional tasks or close simulations to find effective and efficient strategies for performance.
• Provide opportunities for practice outside therapy time.
• Remediate a client factor (impairment).
• Adapt the environment, modify the task, or use assistive technology.
Choosing Appropriate Assessments
It is important to reiterate that occupational therapy outcomes should be focused on areas of occupation. The following paragraphs will focus on Jane’s case to illustrate this point.
Potential (noninclusive) outcomes for Jane based on the practice framework may include the following3:
• Outcome 1: Following occupational therapy, Jane has improved her scores on a standardized memory scale (decreased impairment in client factors), but the changes are not detected on measures of instrumental activities of daily living (IADLs) and quality of life (stable performance in areas of occupation).
• Outcome 2: Following occupational therapy, Jane has no detectable changes on the standardized memory scale (stable impairment in client factors), but changes are detected on measures of IADL and quality of life (improved performance in areas of occupation).
• Outcome 3: Following occupational therapy, Jane has detectable changes on the standardized memory scale (decreased impairment in client factors), as well as changes detected on measures of IADL and quality of life (improved performance in areas of occupation).
Of the three outcome scenarios, outcome 1 is the least desirable. In the past this type of outcome may have been considered successful (i.e., “Jane’s memory has improved”). This outcome may be indicative of an intervention plan that is overly focused on attempts to remediate memory skills (e.g., memory drills, computerized memory programs) without consideration of generalization to real-life scenarios. If a change at the impairment level of function does not translate or generalize to improved ability to engage in meaningful activities, participate successfully in life roles, or enhance quality of life, the importance of the intervention needs to be reconsidered. Outcomes 2 and 3 are more clinically relevant and arguably more meaningful to Jane and her family and represent more optimal results of structured occupational therapy services. Outcome 2 may have been achieved by focusing interventions on Jane’s chosen tasks. Interventions such as teaching compensatory strategies, including the use of assistive technology, may have been responsible for this outcome. Jane is able to engage in chosen tasks despite the presence of stable impairments in memory.
Finally, outcome 3 represents improvement (decreased impairment, improved performance of activities, and improved quality of life) across multiple health domains. Although this outcome may be considered the most optimal, the relationships among the three measures are not clear. Clinicians may assume that the improved status detected by the standardized measure of memory was also responsible for Jane’s improved ability to perform household chores and child care. This reasoning is not necessarily accurate, however. The changes within the health domains may in fact be independent of each other. In other words, Jane’s improved ability to manage her household after participating in treatment may be related to the fact that the interventions specifically included teaching Jane strategies to manage her household. Similar to outcome 2, this positive change may have occurred with or without a documented improvement in memory skills.
When choosing assessments, particular emphasis should be placed on the ecologic validity of an instrument. This term refers to the degree to which the cognitive demands of the test theoretically resemble the cognitive demands in the everyday environment, sometimes termed functional cognition. A test with high ecologic validity identifies difficulty performing real-world functional and meaningful tasks. Ecologic validity also refers to the degree to which existing tests are empirically related to measures of everyday functioning via a statistical analysis.21
In terms of a starting point (i.e., which areas of occupation should serve as the basis for assessment), as stated earlier, a client-centered approach is necessary. This can be assessed formally by using the Canadian Occupational Performance Measure56 or informally via an interview with the client/significant others. The clinical context must also be considered. OTs working in an acute care setting may be focused on areas such as basic mobility (moving in bed and transfers), bedside self-care, IADLs that can be performed at the bedside (e.g., money management, medication management), and sedentary leisure activities (e.g., reading fiction, doing crosswords). Those working in the home setting may focus on intervention related to community reintegration, more complex IADLs, and returning to work. The OT uses observation skills to determine which underlying cognitive (and other) deficits are interfering with functional performance by using error analysis. In other words, errors in performance (“occupational errors” as per Árnadóttir7) are allowed to occur as long as they are safe and not severe enough to halt performance. Árnadóttir gives the following example of this technique related to observing errors during grooming and hygiene8 (pp. 478-479):
Dysfunctions of global and specific mental functions with an effect on grooming and hygiene tasks include ideational apraxia, organization and sequencing problems related to activity steps, impaired judgment, decreased level of arousal, lack of attention, distraction, field dependency, impaired memory, and impaired intention. Ideational apraxia may appear during grooming and hygiene activities; an individual may not know what to do with the toothbrush, toothpaste, or shaving cream or may use these items inappropriately (e.g., smear toothpaste over the face or spray the shaving cream over the sink). An individual with organization and sequencing difficulties only may have the general idea of how to perform but may have problems timing and sequencing activity steps. Such a patient may not complete one activity step before starting another or may perform activities too quickly as a result of problems in timing activity steps, resulting in a poor performance.
Lack of judgment may appear as an inability to make realistic decisions based on environmental information, providing that perception of those impulses is adequate. An individual so affected may leave the sink area without turning off the water taps or may leave the wash cloth in the sink, not noticing that the water level is increasing and threatening to overflow.
Field dependency has an attention component and a perseveration component. Individuals with this dysfunction may be distracted from performing a particular task by specific stimuli that they are compelled to act on or incorporate into the previous activity. For example, if an individual with field dependency sees a denture brush while washing the hands, that person may incorporate the brush into the activity and scrub the hands with the denture brush.
An individual with short-term memory problems may not remember the sequence of activity steps or instructions throughout activity performance. The therapist may have to remind an individual several times to comb the hair, even though the individual does not have comprehension problems.
Lack of initiation may occur during performance of grooming and hygiene tasks; the individual may sit by the sink without performing, even after being asked to wash. With repeated instructions to begin, the individual may indicate that the activity is about to start, yet nothing happens. After several such incidents and if the therapist asks for a plan, the individual may state a detailed plan of action in which the water will be turned on, the washcloth will be picked up and put under the running water, soap will be put on the cloth, and washing will begin. The individual has a plan of action but cannot start the plan. This impairment may be associated with ideational problems as well.
Traditionally, clinicians and researchers involved in working with those who are cognitively impaired use standardized measures of cognitive impairment (i.e., standardized tests to determine impairments in attention, memory, executive functions, etc.) as the primary outcome measure to document the effectiveness of interventions. These measures tend to be categorized as “pen-and-paper” or “tabletop” assessments and have low ecologic validity, as opposed to assessments that use relevant occupations in naturalistic contexts. Although this is one important level of measurement, it is critical that clinical programs and research protocols not only include but also focus on measures of activity, participation, and quality of life as a key outcome. As stated, positive changes in these measures are more relevant than an isolated change in an impairment measure; the change in impairment must be associated with a change in other health domains. Individuals receiving services, family members, and third party payers alike are likely to be more satisfied with changes in these arguably more meaningful levels of function. Table 26-2 suggests instruments to document successful clinical and research outcomes related to improving function in those with functional limitations secondary to the presence of cognitive impairments. For a thorough review of performance-based measures, refer to Law and associates.57
TABLE 26-2
Examples of Instruments to Document Improved Function in Those with Functional Limitations Secondary to the Presence of Cognitive Impairments
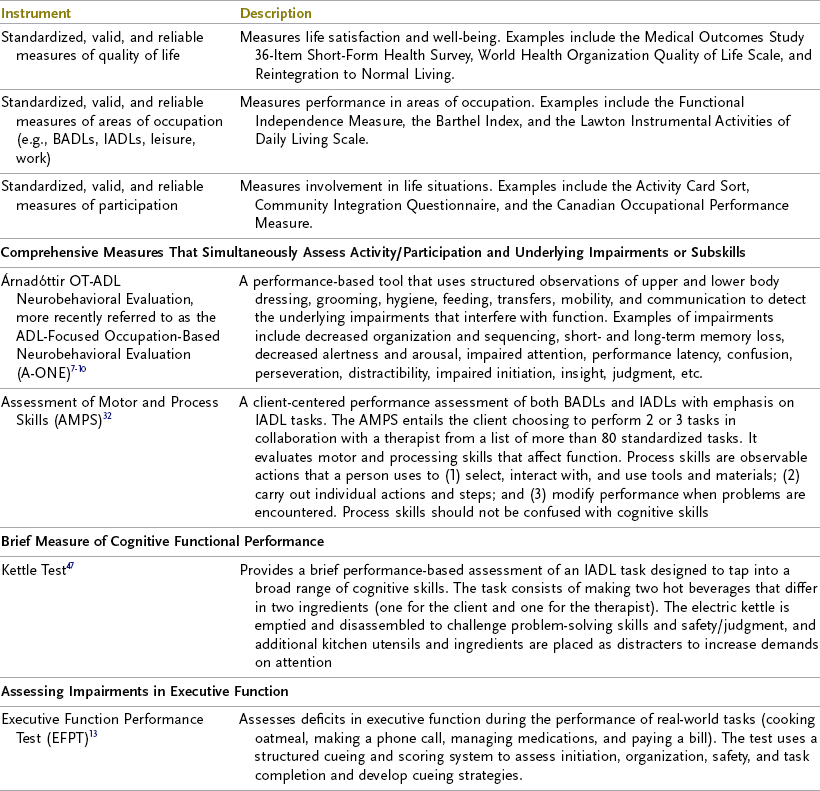
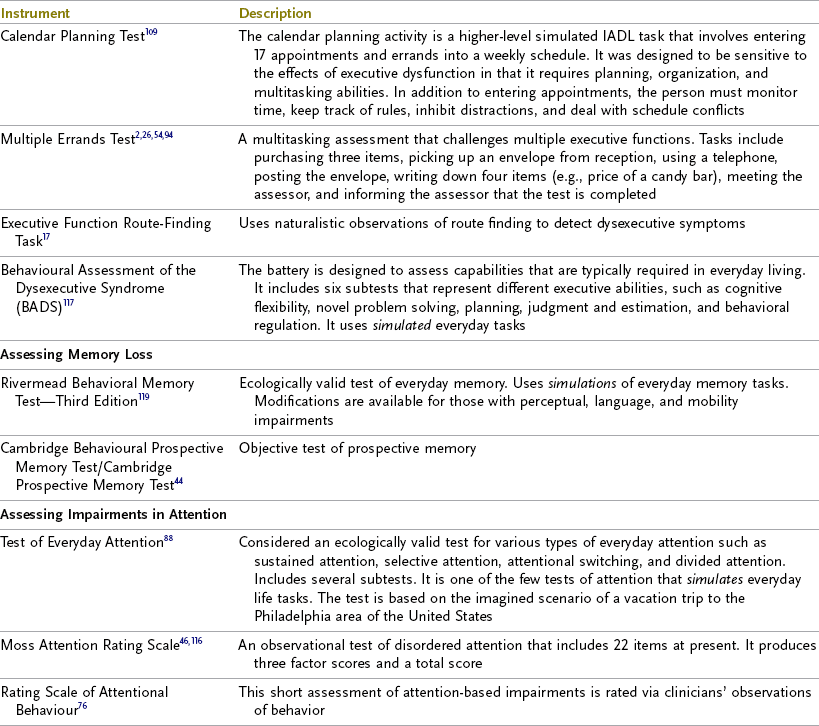
BADLs, basic activities of daily living; IADLs, instrumental activities of daily living.
It also is clinically useful to use self-report or caregiver report measures for this population. The rationale for this type of assessment is multifold:
1. Comparing self-reports with observed performance provides the OT with critical information on awareness of the severity of impairment and functional status.
2. Comparing self-reports and caregiver reports is helpful in getting a “snapshot” of how clients perform in their own environments, which may or may not be congruent with observed performance in an occupational therapy clinic.
3. It is important that clients and caregivers see benefit from the occupational therapy services provided. It is problematic if the OT is documenting improvements that cannot be detected by those to whom we provide services (Table 26-3).
TABLE 26-3
Examples of Self-Report and/or Caregiver Report Measures
| Instrument and Author | Instrument Description |
| Attention Rating and Monitoring Scale22 | Self-report measure of the frequency of everyday problems related to impairments in attention |
| Cognitive Failures Questionnaire18 | Self-report measure of the frequency of lapses in attention and cognition in daily life. Includes items related to memory, attention, and executive dysfunction |
| Prospective Memory Questionnaire45 | Behaviorally anchored self-rated evaluation of prospective memory |
| Comprehensive Assessment of Prospective Memory89,112 | Assessment of prospective memory related to BADLs and IADLs |
| Everyday Memory Questionnaire91,102,103 | Subjective report of everyday memory. A metamemory questionnaire. Self-report or via proxy |
| Prospective and Retrospective Memory Questionnaire52,96 | Measure of prospective and retrospective failures in everyday life. Self-rated or proxy rated. Published norms |
| Dysexecutive Questionnaire (part of the Behavioral Assessment of the Dysexecutive Syndrome [BADS] test battery)19,118 | A 20-item questionnaire sampling everyday symptoms associated with impairments in executive functions. Self-rating and ratings by significant others’ versions available |
| Behavior Rating Inventory of Executive Function—Adult Version90 | A measure that documents an adult’s executive functions or self-regulation in his or her everyday environment. Includes both a self-report and an informant report |
BADLs, basic activities of daily living; IADLs, instrumental activities of daily living.
Returning to the case study, the OT had access to Jane’s acute care medical record. He noted that the day before transfer to the inpatient rehabilitation unit, the neurology resident administered the Mini-Mental State Examination (a brief 30-item questionnaire used by multiple disciplines to screen for cognitive impairment). She scored 20 of 30, which is indicative of moderate cognitive impairment. Jane had difficulty on the specific items of orientation, attention and calculation, and recall. An assessment required in most inpatient rehabilitation units is the Functional Independence Measure (FIM). This tool measures the client’s ability to complete specific self-care and mobility tasks, and scoring is based on caregiver burden related to these tasks. The FIM provides information related to what tasks Jane requires assistance with. Jane’s OT used this opportunity to also document why Jane requires assistance with the FIM tasks. He used the error analysis approach described earlier and objectified his findings with the ADL-Focused Occupation-Based Neurobehavioral Evaluation (A-ONE). Jane required minimal physical assistance to initiate each FIM task but needed consistent verbal cues to organize and sequence the FIM tasks. Additional verbal cues were required to maintain alertness, to stay on task secondary to distractibility, and to compensate for short-term memory deficits, most notably keeping in mind and remembering the tasks that the OT asked her to demonstrate.
Managing Cognitive Dysfunction That Limits Occupational Performance: Assessment and Interventions
Awareness Deficits Having an Impact on Daily Function
Management of deficits in awareness may be considered a foundational intervention for this population.41 Findings from standardized assessments of awareness may dictate the overall management of a client’s functional limitations, as discussed later. Different terminology and definitions related to limited self-awareness are used in the literature, including lack of insight, lack of/impaired self-awareness or unawareness, anosognosia, and denial. Nonimpaired self-awareness has been defined as “the capacity to perceive the self in relatively objective terms, while maintaining a sense of subjectivity.”81–83 The terms impaired self-awareness and anosognosia are used interchangeably and are defined as follows: the clinical phenomenon in which a person “does not appear to be aware of impaired neurological or neuropsychological function, which is obvious to the clinician and other reasonably attentive individuals. The lack of awareness appears specific to individual deficits and cannot be accounted for by hyperarousal or widespread cognitive impairment.”80
Other authors reserve the term anosognosia for describing unawareness of physical deficits only (i.e., not including cognitive impairments), such as “anosognosia for hemiplegia” or “anosognosia for hemianopia.”
Although impaired self-awareness and anosognosia have clearly been used as overlapping terms in the literature, the term denial must be considered separately. Psychologic denial has been defined as “a subconscious process that spares the patient the psychological pain of accepting the serious consequences of a brain injury and its unwanted effects on his or her life.”25 Complicating the matter is that impaired self-awareness and denial may occur together. Differentiation between denial (a psychologic method of coping) and lack of awareness that is neurologically based is difficult because some individuals have both types of clinical manifestations.82
The pyramid model of self-awareness was developed by Crosson and colleagues.25 This model includes three interdependent types of awareness:
1. Intellectual awareness: The ability to understand at some level that a function is impaired. At the lowest level, one must be aware that one is having difficulty performing certain activities. A more sophisticated level of awareness is to recognize commonalities between difficult activities and implications of the deficits. It refers to knowing that you have a problem. In terms of the case study, Jane was demonstrating substantial impairment in intellectual awareness on the acute service. Her family reported that she kept repeating, “Why can’t I go home? I am fine.” The OT on the rehabilitation service noted that Jane consistently reported that she understood that she had a “stroke.” In addition, Jane was reporting that “simple” tasks seemed to take a long time and that she keeps “losing her train of thought.” Jane is showing signs of emerging (albeit still severely impaired) intellectual awareness.
2. Emergent awareness: The ability to recognize a problem when it is actually happening. Intellectual awareness is considered a prerequisite to emergent awareness in this model because one must first recognize that a problem exists (knowing that you are experiencing a problem when it occurs). Emergent awareness is included in the concept of online awareness or monitoring of performance during the actual task.
3. Anticipatory awareness: The ability to anticipate that a problem will occur as the result of a particular impairment in advance of actions. Anticipatory awareness is included in the concept of online awareness.
Those with brain injury or cognitive deterioration may be impaired across all three awareness domains70 or may have better skills in one or more domains of awareness. Crosson and associates further applied this model to the selection of compensatory strategies and categorized compensations appropriate to each type of awareness.25 They classified compensatory strategies according to the way that their implementation is triggered:
• Anticipatory compensation: Applied only when needed. This term refers to implementation of a compensatory technique by anticipating that a problem will occur (i.e., requires anticipatory awareness). An example is a person who needs groceries for the week and is aware that busy environments present a greater challenge to existing memory and attention deficits decides to defer shopping until 7 p.m. when the local store is not as busy.
• Recognition compensation: Also applied only when needed. This term refers to strategies that are triggered and implemented because a person recognizes that a problem is occurring (i.e., requires emergent awareness). An example is asking a person to speak slower because you realize that you are not processing information quickly enough and are having difficulty following the conversation.
• Situational compensation: Applies to compensatory strategies that can be triggered by a specific type of circumstance in which an impairment may affect function. These strategies are taught to be used consistently every time that a particular event occurs. An example is a student who because of impairments in memory after a traumatic brain injury (TBI) tape-records all lectures in class. Although recording may not be necessary at times (e.g., a particularly slow-moving lecture with limited content), the strategy is used anyway because this type of compensation does not rely on the judgment of the client. Intellectual awareness is necessary to use this strategy because one must be aware that a deficit exists to integrate a strategy for overcoming it.
• External compensation: Triggered via an external agent or involves an environmental modification. Examples include alarm watches, posted lists of steps related to meal preparation, and so on.
This pyramid model was constructively criticized and expanded on by Toglia and Kirk.108 Their model, the Dynamic Comprehensive Model of Awareness, suggests a dynamic rather than a hierarchic relationship. The model proposes a dynamic relationship among knowledge, beliefs, task demands, and the context of a situation based on the concept of metacognition. This model differentiates between metacognitive knowledge or declarative knowledge and beliefs about your abilities before performing the task (incorporating aspects of intellectual awareness) and online monitoring and regulation of the performance of a task (i.e., during task performance), which integrates aspects of emergent and anticipatory awareness.
Finally, Fleming and Strong discuss a three-level model of self-awareness34:
1. Self-awareness of the injury-related deficits themselves such as cognitive, emotional, and physical impairments (i.e., knowledge of deficits)
2. Awareness of the functional implications of deficits for independent living
3. The ability to set realistic goals; the ability to predict one’s future state and prognosis
Most authors recommend that self-awareness be evaluated before initiating an intervention program focused on retraining living skills. The findings from standardized evaluations of self-awareness will clearly guide choices of intervention. For example, a person who exhibits insight into an everyday memory deficit may be a candidate for teaching compensatory strategies such as using a diary or notebook (see later). However, a person who does not realize that he or she has severe unilateral neglect (a lateralized attention deficit) may not be able to learn compensatory strategies and thus may require environmental modifications (e.g., all clothing hung on the right side of the closet) to improve everyday function. In addition, ascertaining the level of insight into a disability is one factor that may determine how motivated one is to participate in the rehabilitation process. In the most simplistic interpretation, one must be aware and concerned about a deficit in everyday function to be motivated to participate in what may be a long and difficult rehabilitation process. Returning to the case study, Jane has goals of returning to school and engaging in complex ADLs on returning home. It is imperative that Jane continue to gain insight so that she can implement strategies to compensate for her persistent deficits. Examples of strategies to return to school may include tape-recording lectures, having a “note taker” assigned so that Jane can fully attend to the lecture, switching to a part-time school schedule, and using electronic aids to organize her day, assignments, etc.
A variety of assessment measures are typically recommended for ascertaining a person’s level of self-awareness, including questionnaires (self or clinician rated); interviews; rating scales; functional observations; comparisons of self-ratings and ratings made by others such as significant others, caretakers, or rehabilitation staff; and comparisons of self-ratings and ratings based on objective measures of function or cognitive constructs. No method is universally accepted for assessing the construct of awareness or lack thereof. In addition, naturalistic observations can provide further information related to how decreased awareness is interfering with the performance of everyday tasks. See Table 26-4 for examples of standardized assessments of awareness.
TABLE 26-4
Examples of Standardized Tests of Awareness
| Instrument | Brief Description |
| Self Awareness of Deficits Interview34 | This interviewer-rated structured interview is used to obtain quantitative and qualitative data on the status of self-awareness after brain injury. Specifically, it assesses a client’s level of intellectual awareness (the ability to understand that a function is decreased from the premorbid level and to recognize implications of the deficits) |
| Self-Regulation Skills Interview73 | This semistructured clinician-rated interview is based on the model by Crosson and associates25 discussed earlier. The tool includes six questions that assess metacognitive or self-regulation skills |
| The Patient Competency Rating Scale (PCRS)79 | This tool evaluates self-awareness following traumatic brain injury. It is a 30-item self-report instrument that uses a 5-point Likert scale (1 = can’t do and 5 = can do with ease) to self-rate the degree of difficulty in a variety of tasks and functions. More recently, Borgaro and Prigatano16 developed a modified yet still psychometrically sound version of the PCRS for use in an acute, inpatient neurorehabilitation unit. This version retains 13 items from the original PCRS |
| Awareness Questionnaire95 | This is a measure of impaired self-awareness after traumatic brain injury. The instrument consists of three forms (one form is completed by the client, one by a significant other, and one by a clinician). The self-rated and family/significant others forms contain 17 items, and the clinician form contains 18 items. The client’s ability to perform various tasks after the injury as compared with before the injury is rated on a 5-point scale |
| Awareness Interview6 | This tool is used to evaluate awareness of cognitive and motor defects after cerebral infarction, dementia, or head trauma. Operationally, the authors defined unawareness as a discrepancy between the client’s opinion of his or her abilities in the interview and his or her abilities as measured by neuropsychologic and neurologic examinations |
| Assessment of Awareness of Disability55 | This is an assessment based on a semistructured interview that is used in conjunction with the Assessment of Motor and Process Skills (AMPS). It consists of general and specific questions related to the activity of daily tasks, and the interview is conducted after performance of the AMPS |
Although most researchers and scholars agree that interventions focused on improving awareness are critical for maximizing rehabilitation and that greater awareness of deficits is associated with better treatment outcomes,71 others have documented functional changes via task-specific treatment without concurrent improvement in awareness. Overall, there is a lack of empiric studies that have examined the effectiveness of various interventions aimed at improving awareness. In addition, many of the published studies have not included functional outcomes. As a starting point in managing awareness, the entire team should encourage clients to predict their level of performance before any observed performance in areas of occupation. Those with brain injury or cognitive deterioration most often underestimate their level of cognitive impairment and overestimate their level of function. Clinicians should leave time at the end of each session to compare actual performance with predicted performance. This comparison of predicted versus actual performance is critical and should be done with all functional tasks. Examples of predictions include questions such as “How long will the task take?”, “How many times will you need to ask for help?”, “How many times will the therapist need to physically help you?”, and “How many times will the therapist need to verbally help you?” The goal is to decrease the discrepancy between the two levels of performance.
In is important for the OT to remember that the verbal or physical cues used to support participation in meaningful occupations are not provided simply to support the completion of tasks. Cues are used to facilitate insight and to encourage the client to solve problems by developing new strategies to overcome deficit areas (Table 26-5).
TABLE 26-5
Prompting Procedures to Promote Awareness of Errors during Functional Activities
| Prompts | Rationale |
| “How do you know this is the right answer/procedure?” or “Tell me why you chose this answer/procedure.” | Refocuses the client’s attention to task performance and error detection. Can the client self-correct with a general cue? |
| “That is not correct. Can you see why?” | Provides general feedback about error but is not specific. Can the client find error and initiate correction? |
| “It is not correct because…” | Provides specific feedback about error. Can the client correct error when it is pointed out? |
| “Try this [strategy]” (e.g., going slower, saying each step out loud, verbalizing a plan before starting, or using a checklist). | Provides the client with a specific, alternative approach. Can the client use the strategy given? |
| The task is altered. “Try it another way.” | Modifies the task by one parameter. Can the client perform the task? Begin again with grading of prompting described previously |
From Brockmann-Rubio K, Gillen G: Treatment of cognitive-perceptual impairments: a function-based approach. In Gillen G, Burkhardt A, editors: Stroke rehabilitation: a function-based approach, ed 2, St. Louis, Mo, 2004, Mosby, pp. 427-446. Modified from Toglia JP: Attention and memory. In Royeen CB, editor: AOTA self-study series: cognitive rehabilitation, Rockville, Md, 1993, American Occupational Therapy Association; Toglia JP: Generalization of treatment: a multicontext approach to cognitive perceptual impairment in adults with brain injury, Am J Occup Ther 45:505, 1991.
Tham and colleagues developed an intervention to improve awareness related to the effect of neglect (a lateralized attention deficit) on functional performance.104 Purposeful and meaningful (for the participant) daily occupations were used as therapeutic change agents to improve awareness of disabilities. Specific interventions included encouraging participants to choose motivating tasks as the modality of intervention and discussions about task performance. Examples include the following:
• Encouraging participants to describe their anticipated difficulties
• Linking their earlier experiences of disability to new tasks
• Planning how they would handle new situations
• Asking participants to evaluate and describe their performance
• Asking participants to think about whether they could improve their performance by performing the task in another way
• Providing feedback about the difficulties observed, including verbal feedback, discussion, and the use of compensatory techniques that could improve performance of the task
• Providing opportunities for further practice of the task by using newly learned compensatory techniques
With this approach, awareness of disabilities and ADL ability improved in all four participants, unilateral neglect decreased in three participants, and sustained attention improved in two participants. The authors concluded that training to improve awareness of disabilities might improve the ability to learn the use of compensatory techniques for performing ADLs by clients with unilateral neglect.
Fleming and coworkers completed a pilot study examining the effect of an occupation-based intervention program on the self-awareness and emotional status of four men after acquired brain injury.33 Each participant received an individualized program that focused on the performance of three client-chosen occupations (e.g., writing a job application, budgeting, meal preparation, playing lawn bowling, cooking with one hand) for which they had decreased awareness according to significant others. The intervention was based on Toglia’s multicontextual approach described earlier.105 Techniques included providing a nonthreatening environment to build positive therapeutic alliances; having the participants analyze their underlying skills, self-predict, and self-evaluate before and after the occupation; setting “just the right challenge”; supported and structured occupational performance; education on brain injury; timely and nonconfrontive verbal feedback in a sandwich format (negative comments are preceded and followed by positive feedback); and video feedback.
Repeated measures of participants’ self-awareness and emotional status were performed before and after intervention and analyzed descriptively. The authors found that their results indicated preliminary support for the effectiveness of the program in facilitating participants’ self-awareness, although baseline and follow-up data indicated a complex and inconsistent picture. Of note is that slightly increased anxiety was found to accompany improvements in participants’ self-awareness in all four cases and slight increases in depressive symptoms were noted in three participants. These findings are consistent with the literature discussed earlier focused on the relationships between emotional status and awareness, as well as the interconnections between denial and self-awareness (Box 26-1).
Jane’s OT administered the Self Awareness of Deficits Interview. Gary was present for this session. Jane reported that she was not any different now from what she was like before her hospitalization, her brain injury has not had any effect on everyday life, and she hopes to be ready to graduate and look for her first job as a social worker in the next 6 months. The findings and ratings were indicative of severely limited self-awareness. The OT consistently used the time needed to complete a task as the prediction that Jane would make before each task. The OT chose time as the predictor because Jane had poor initiation, was disorganized, and repeated steps of the tasks. Such behavior increased the amount of time needed to complete tasks. Jane consistently predicted length of time based on her preinjury status. When the OT compared the predicted time with the actual time, Jane reacted with disbelief. As sessions progressed, Jane began to increase her accuracy in reporting the time needed for each task (increased awareness). As her awareness increased, the OT noted that Jane was frequently teary. The OT notified the team that although Jane was developing a better understanding of her current functional status, she required increased emotional support from the team, as well as monitoring for increased levels of depression and anxiety.
Attention Deficits Having an Impact on Daily Function
Attention in its various forms is one of the most important and basic functions of the human brain, and it constitutes the basis for other cognitive processes. Integrity of the attention system is considered a prerequisite for all other higher cognitive systems such as memory, executive functions, and so on.75 In particular, basic memory functions such as working memory are dependent on intact attention processes.22 If one does not attend to incoming information and cannot hold information in mind, information will not be remembered and cannot be used to guide appropriate behavior or successfully complete daily activities.67 It comes to follow that attention skills serve as a cognitive foundation and are a prerequisite to engage in most if not all meaningful activities and that any impairment in attention processes will result in observable difficulties in everyday life, which may in fact decrease quality of life. Termino-logy related to attention impairments is summarized in Table 26-6.
TABLE 26-6
Terminology Related to Impairments in Attention
| Attention Component | Definition | Functional Examples |
| Attention | Voluntary control over more automatic brain systems to be able to select and manipulate sensory and stored information briefly or for sustained periods74 | See later for examples of the specific components of attention |
| Arousal | A state of responsiveness to sensory stimulation or excitability115 Dependent on a widely distributed neural network, including the prefrontal areas and neurotransmitter systems108 |
Decreased responsiveness to incoming visual, auditory, or tactile cues during performance of a task Requires noxious or extreme sensory stimuli (e.g., a cold washcloth applied to the face) to elicit a behavioral response |
| Selective attention | The type of attention involved in the processing and filtering of relevant information in the presence of irrelevant stimuli87 The efficiency with which people can search and focus on specific information while ignoring distracters88 Because selective attention is critical for encoding information into memory, retaining and manipulating information in working memory, and successfully executing goal-directed behavior, a deficit in selective attention could contribute to the numerous cognitive deficits observed in those with neurologic impairments87 This skill is linked to the prefrontal and underlying anterior cingulated areas |
Attending to one conversation during a party Studying outside with the noise of traffic and children playing Attending to a therapist’s instructions and cues in a crowded therapy clinic Making dinner while the children are watching TV in the background Attending to a board game during recess |
| Sustained attention (vigilance) | Used to support tasks that require vigilance and the capacity to maintain attention over time5 Many times this construct is measured by time spent on task114 In adults this attention component is linked to prefrontal function in the right hemisphere, as well as white matter damage88 |
Being able to attend to long conversations, instructions, class lessons, television shows, or movies Attending to playing a game of chess Balancing a checkbook Watching your child on the playground |
| Attentional switching or alternating attention | The ability to switch attention flexibility from one concept to another. Related to cognitive flexibility The ability to change attentive focus in a flexible or adaptive manner4 The ability to move between tasks with different cognitive requirements This skill appears to be a function of the prefrontal cortex, as well as the posterior parietal lobe, thalamus, and midbrain68 |
While typing a paper, a friend comes into your room to discuss a completely different topic; when the conversation is over, you return to typing Cooking, taking care of a crying child, then returning to cooking A unit clerk at the hospital alternating between flagging orders on the medical chart, answering the phone, and writing down phone messages |
| Divided attention | Dividing attention between two or more tasks simultaneously Dual tasking or multitasking The capacity to attend to two competing stimuli simultaneously5 Deficits occur when limited attentional resources are divided between two sources |
Making toast and tea at the same time Texting while carrying on a conversation Playing cards while discussing the events of the day |
| Distractibility | A breakdown in selective attention An inability to block out environmental or internal stimuli when one is trying to concentrate on performing a particular task A symptom of prefrontal damage, particularly the dorsolateral cortex63 |
Noise in the hallway takes away your attention while taking notes during a class Inability to attend during a therapy session because of being distracted by watching someone else’s session |
| Field-dependent behavior | Distracted by and acting on an irrelevant impulse that interferes with performance of an activity and takes over goal-directed activity Includes both an attention and perseveration component8 |
While performing oral care, a person becomes distracted by a light switch; the person then stops the oral care activity while turning on and off the light switch (i.e., not relevant to the task at hand) |
| Unilateral neglect (a lateralized attention deficit) | See Chapter 33 | See Chapter 33 |
Adapted from Gillen G: Cognitive and perceptual rehabilitation: optimizing function, St. Louis, Mo, 2009, Mosby.
During performance of a task, impaired attention results in increased rates of off-task behavior (e.g., looking up and away from the task at hand, engaging in unsolicited conversations) in comparison to controls. Those with impairments in attention are markedly less attentive than controls both in the presence of distractions (noise, movements) and in their absence.114 Further compounding this problem is a relationship between attention impairment and awareness of errors. McAvinue and colleagues investigated the processes of error awareness and sustained attention in those with TBI.66 They found the following:
• In comparison to controls, participants with TBI displayed reduced sustained attention and awareness of error.
• The degree of error awareness was strongly correlated with sustained attention capacity, even when the severity of injury was controlled for.
• Error feedback significantly reduces errors.
• TBI leads to impaired sustained attention and error awareness.
The finding of a significant relationship between these two deficits in clients with TBI suggests that there may be a link between these two processes.
Posner and Peterson proposed the existence of three main functionally and anatomically distinct attentional control subsystems77:
1. An orienting system related to sensory events that relies on the posterior brain areas (superior parietal lobe and temporoparietal junction, in addition to the frontal eye fields). This system is involved in the selection of relevant sensory information. This subsystem brings attention to a specific location in space and generates perceptual awareness. It reflects involuntary orienting or automatic processing. The performance of this system is determined by the reaction time in responding to the detection of stimuli.
2. An executive system focused on selection and involving multiple structures (anterior cingulate, lateral prefrontal cortex, and basal ganglia). This system is responsible for exercising control over lower-level cognitive functions and resolving conflicts. The system is prominent in detecting signals for focal or conscious attention. Breakdown in this system results in difficulty managing tasks that require divided attention, screening out interfering stimuli, and responding to novelty.
3. An alerting or sustained attention system involving the frontoparietal regions that is responsible for achieving and maintaining sensitivity to incoming stimuli. Impairments related to this system result in short attention spans.
Dockree and colleagues summarize the following27:
• Attention deficits are among the most commonly observed deficits following brain injury.
• Damage to the frontal lobes of the brain, particularly the white matter connecting the frontal, parietal, and striatal regions, is in part responsible for these deficits.
• Frontal lobe damage in brain-injured clients results in a tendency to drift from intended goals and increases the frequency of action slips that were unintended.
• Self-reports from clients with TBI reveal that problems with attention and concentration rate among the highest complaints in this group of clients.
The usual and customary tests of attention include pen-and-paper measures or laboratory-type tasks, such as the Paced Auditory Serial Addition Test, Trail Making Test Part A, and Wisconsin Card Sorting Task. As discussed earlier, when using these measures the question of ecologic validity arises as regards difficulty generalizing the results to everyday living tasks. Suggested assessments are described in Tables 26-2 and 26-3. Impairments in attention are manifested as observables errors during performance of tasks and should be documented as such (see Table 26-4).
In their meta-analysis of attention rehabilitation after an acquired brain injury, Park and Ingles examined two approaches to treating attention deficits74:
1. Directly retraining the damaged cognitive function or direct cognitive retraining. This approach is used under the assumption that practice of carefully selected exercises promotes recovery of damaged neural circuits and restores function in the impaired attentional processes themselves, along with a further assumption that the tasks mediated by those circuits are then performed in a way that is similar to non–brain-damaged individuals. Intervention is then based on a series of repetitive exercises or drills in which clients respond to visual or auditory stimuli. This intervention has received the most attention in the literature with respect to interventions for those with impairments in attention.
2. Attempts to assist people with attention deficits by having them learn or relearn how to perform specific skills of functional significance (i.e., specific skill training). The premise here is that that through carefully structured practice of a specific skill that is impaired as a result of brain damage, it is possible for individuals to compensate and develop alternative neuropsychologic processes that rely on preserved brain functions (i.e., individuals learn to perform the skill in a way that is different from non–brain-damaged individuals). In terms of intervention, attention is trained either concurrently with or in the context of the specific skills. In addition, this approach applies behavioral principles and an understanding of how the impairment in attention affects the various skills.
Park and Ingles concluded that specific skills training significantly improved the performance of tasks requiring attention.74 In comparison, the cognitive-retraining methods (i.e., those focused on improving impairments in attention out of context) included in the meta-analysis did not significantly affect outcomes. Further analysis revealed that overall performance improved in 69% of the participants who received specific skills training (e.g., driving, ADLs) whereas performance improved in only 31% of those not so trained. In terms of effect size, the improvements in cognitive functions after direct retraining were small, whereas the improvements in performance after specific skills training were medium or large. Their findings demonstrate that acquired deficits in attention are treatable by specific skills training. The authors also proposed clinical implications of their study, including the following:
• The learning that occurs as a function of training is specific and does not tend to generalize or transfer to tasks that differ considerably from those used in training. This specificity of improvement was demonstrated in both the cognitive-retraining studies and the specific functional skill–retraining studies.
• Performance of a task after training will improve to the extent that the processing operations required to complete that task overlap with the processes engaged during training (i.e., performance will improve after training if the training task is similar to the targeted outcome measure).
• Many survivors of brain injury are impaired when performing controlled cognitive processes but not when performing automatic processes. Controlled processing is heavily involved in the early stages of learning a skill and is less involved as a skill becomes more routine with practice. Therefore, training programs that reduce the requirement for controlled processing during learning may be the most effective. Examples of reducing the demands of controlled processing include breaking down a complex functional skill into simpler components, providing practice on these components, and structuring training in such a way that performance feedback can be more easily interpreted. The authors recommend the technique of “shaping” as a way to train people with controlled processing deficits because shaping links the difficulty of a task to the person’s performance. As a result of using the technique of shaping, the person may make fewer errors and be able to interpret feedback more easily.
• Rehabilitation procedures are to be based on a set of learning principles.
Strategies aimed at modification of task and environments have proved to be beneficial for this population (Box 26-2). Specific strategies include the following:
• Time pressure management (TPM). Fasotti and colleagues noted that following severe closed head injury, deficits in speed of processing information are common and result in a feeling of “information overload” when performing daily tasks.31 The authors tested TPM as an approach for managing slow information processing. TPM uses alternative cognitive strategies to support participation in real-life tasks. The overall focus is to teach people to give themselves enough time to deal with life situations. Specific strategies used to prevent or manage time pressure include the following: enhancing awareness of errors and deficient performance, self-instruction training (e.g., trying to focus, not getting distracted by outside sounds and other information, not getting distracted by irrelevant thoughts, and trying to imagine things that are being said), optimizing planning and organization, rehearsing task requirements, modifying the task environment, and using an overall strategy of “Let me give myself enough time.”
• Self-instruction statements.112 Such statements can be suggested to improve listening and to ask for repetition if attention strays and include the following:
• “To really concentrate, I must look at the person speaking to me.”
• “I must also focus on what is being said, not on other thoughts that may want to intrude.”
• “I must concentrate on what I am hearing at any moment by repeating each word in my head as the person speaks.”
• “Although it is not horrible if I lose track of a conversation, I must tell the person to repeat the information if I have not attended to it.”
A case study by Webster and Scott demonstrated positive effects of this approach both immediately after treatment and at 18 months’ follow-up as the client demonstrated improved attention, which resulted in increased recall, increased sexual function, and improved job performance.113
• Self management strategies. Sohlberg and Mateer suggest the use of three self-management strategies99:
1. Orienting procedures. Encourage clients to consciously monitor activities to avoid/control a lapse in attention. Clients are taught to ask themselves orienting questions at various intervals (possibly reminded by an alarm watch). These include “What am I currently doing?”, “What was I doing before this?”, and “What am I supposed to do next?”
2. Pacing. Pacing is used to decrease task demands. Scheduling uninterrupted work times is an example. Sohlberg and Mateer give examples such as setting realistic expectations, building in breaks, and self-monitoring fatigue and attention.
3. Key ideas log. Clients are taught to quickly write or tape-record questions or ideas to address later so that the task at hand is not interrupted.
Strategy training is considered a practice standard for the postacute period of rehabilitation by the American Congress of Rehabilitation Medicine.23 Intervention should focus on strategy training to compensate for attention deficits in functional situations.
Memory Deficits Having an Impacting on Daily Function
Memory impairment is one of the most common consequences of brain injury and degenerative cognitive disorders. The severity and type of memory loss vary according to the structures affected. Human memory is composed of multiple and distinct systems that are required to support daily activities and participate in the community (Table 26-7).101 Examples include remembering your significant other’s birthday, remembering to take your medications, remembering to feed the dog, remembering how to type, remembering events that occurred during a vacation, and so on. Even this “simple” list of memory tasks requires intact functioning of multiple memory systems and includes knowledge of facts and events, procedures, and future intentions. Clearly, memory serves as a key cognitive support to facilitate independent living.
TABLE 26-7
Terminology Related to Impairments in Memory
| Term | Definition | Examples of Everyday Behavior |
| Anterograde amnesia | A deficit in new learning. An inability to recall information learned after acquired brain damage. An inability to form new memories after brain damage occurs | Not able to recall staff names, easily gets lost secondary to topographic disorientation, not able to recall what occurred in therapy this morning, difficulty learning adaptive strategies to compensate for loss of memory |
| Retrograde amnesia | Difficulty recalling memories formed and stored before the onset of disease. May be worse for recent events as opposed to substantially older memories | Inability to remember autobiographic information (address, social security number, birth order), not able to remember historical events (war, presidential elections, scientific breakthroughs) and/or personally experienced events (weddings, vacations) |
| Short-term memory | Storage of limited information for a limited amount of time | Difficulty remembering instructions related to the use of adaptive equipment, not able to remember the names of someone just introduced at a dinner party, not able to remember “today’s specials” in a restaurant |
| Working memory | Related to short-term memory and refers to actively manipulating information that is in short-term storage via rehearsals | While playing a board game, unable to remember and use the rules of the game; not able to perform calculations mentally while balancing the checkbook; difficulty remembering and adapting a recipe |
| Long-term memory (LTM) | Relatively permanent storing of information with unlimited capacity | May affect declarative memory of knowledge, episodes, and facts or nondeclarative memories such as those related to skills and habits |
| Nondeclarative/implicit or procedural memory | Knowing how to perform a skill, retaining previously learned skills, and learning new skills. Form of LTM | Driving, playing sports, hand crafts, learning to use adaptive equipment or a wheelchair for activities of daily living |
| Declarative/explicit memory | Knowing that something was learned, verbally retrieving a knowledge base such as facts, and remembering everyday events. Includes episodic and semantic information. Form of LTM (see the following) | See episodic and semantic memory |
| Episodic memory | Autobiographic memory for contextually specific events, personally experienced events. Form of declarative LTM | Remembering the day’s events, what one had for breakfast, occurrences on the job, the content of therapy sessions |
| Semantic memory | Knowledge of the general world and facts, linguistic skill, and vocabulary. (Note: may be spared after injury.) Form of declarative LTM | Remembering the dates of holidays, the name of the president, dates of world events |
| Explicit memory | Explicit memories consist of memories of events that have occurred in the external world. Information stored in explicit memory is about a specific event that happened at a specific time and place | Remembering places and names and various words. See declarative memory |
| Implicit memory | Does not require conscious retrieval of the past. Knowledge is expressed in performance without the person being aware of possessing this knowledge. Consists of memories necessary to perform events and tasks or to produce a specific type of response | Memory of skills, habits, and subconscious processes. See nondeclarative memory |
| Prospective memory | Remembering to carry out future intentions | Remembering to take medications, return phone calls, buy food, pick up the children from school, mail the bills. A critical aspect of memory to support everyday living |
| Metamemory | Awareness of your own memory abilities | Knowing when you need to compensate for memory capacity (making a list of errands or a shopping list, writing down a new phone number or driving directions), recognizing errors in memory, etc. |
Data from Baddeley AD: The psychology of memory. In Baddeley AD, Kopelman MD, Wilson BA, editors: The essential handbook of memory disorders for clinicians, Hoboken, NJ, 2004, John Wiley; Bauer RM, Grande L, Valenstein E: Amnesic disorders. In Heilman KM, Valenstein E, editors: Clinical neuropsychology, ed 4, New York, NY, 2003, Oxford University Press; Markowitsch HJ: Cognitive neuroscience of memory, Neurocase 4(6):429-435, 1998; and Sohlberg MM, Mateer CA: Memory theory applied to intervention. In Sohlberg MM, Mateer CA, editors: Cognitive rehabilitation: an integrative neuropsychological approach, New York, NY, 2001, Guilford Press.
From Gillen G: Cognitive and perceptual rehabilitation: optimizing function, St. Louis, Mo, 2009, Mosby.
The steps or stages of memory have been well documented.12,99 The flow of these stages follows (Table 26-8):
Traditional measures of memory have tended to tabletop laboratory-style tools. Contrived tasks commonly used are remembering a string of numbers, a list of words, or the details of a drawn figure and/or paired associate learning (i.e., requiring a person to recognize or recall recently presented material). How the results of these tests relate to everyday memory function is not clear, and associations between scores on this type of test and reports of everyday memory failure are not strong.102 Similarly, functional gains do not always correlate with improvement in memory processes based on objective testing.85
TABLE 26-8
| Stage of Memory | Description | Neuroanatomic Area of Function |
| Attention | The processes that allow a person to gain access to and use incoming information. Inclusive of alertness, arousal, and various attention processes such as selective attention | Brainstem Thalamic structures Frontal lobes |
| Encoding | How memories are formed. An initial stage of memory that analyzes the material to be remembered (visual vs. verbal characteristics of information). Correct analysis of information required for proper storage of the information | Dorsomedial thalamus Frontal lobes Language system (e.g., Wernicke’s area) Visual system (e.g., visual association areas) |
| Storage | How memories are retained Transfer of a transient memory to a form or location in the brain for permanent retention/access |
Hippocampus Bilateral medial temporal lobes |
| Retrieval | How memories are recalled Searching for or activating existing memory traces |
Frontal lobe |
Data from Sohlberg MM, Mateer CA: Memory theory applied to intervention. In Sohlberg MM, Mateer CA, editors: Cognitive rehabilitation: an integrative neuropsychological approach, New York, NY, 2001, Guilford Press.
A comprehensive evaluation of how impairments in memory affect everyday function includes the use of standardized assessments, nonstandardized observations, standardized self-reports, and standardized reports of caregivers and significant others. Tables 26-2 and 26-3 include descriptions of recommended assessments. The Contextual Memory Test is a useful screening tool.105 It allows clinicians to objectify three aspects of memory and screen for possible further evaluation:
1. Awareness of memory: via general questioning before the assessment, predicting performance before assessment, and estimating memory capacity following performance.
2. Recall of 20 line-drawn aspects: immediate and delayed (15 to 20 minutes) recall.
3. Strategy use: probes the use of memory strategies and determines the ability to benefit from strategy recommended by the clinician.
Interventions focused on those with memory deficits can be categorized as restorative approaches to improve underlying memory deficits, strategy training, use of nonelectronic memory aids, and use of electronic memory aids or assistive technology. Techniques aimed at improving the underlying memory impairment such as memory drills have been unsuccessful in terms of generalization to meaningful activities. In other words, an improvement may be detected on a laboratory-based measure of memory without a corresponding change in daily function or subjective memory reports.
The most promising interventions to improve function in those with memory deficits rely at least partially on compensatory techniques (Box 26-3). When using a compensatory approach, choosing the correct system of compensation is critical. Kime suggests a comprehensive evaluation that includes the following53:
• Severity of the impairment in memory
• Presence of comorbid conditions, including physical impairments, language deficits, and other cognitive deficits
• Client needs (e.g., will the system be used for work, home management, or other occupations)
Specific evidenced-based interventions include the following:
• Memory notebooks and diaries. Use of this strategy has been documented to improve orientation, as well as support everyday living tasks such as morning ADLs and simple IADLs.92 Sohlberg and Mateer published a systematic, structured training sequence for teaching individuals with severe impairments in memory to independently use a compensatory memory book.97,98 The training sequence that they proposed incorporates principles of learning theory, as well as procedural memory skills, which may be preserved in many clients with even severe impairments in memory. Donaghy and Williams suggested that the diary or notebook include a pair of pages for each day of the week.28 The notebook is set up to aid scheduling things to do in the future and record activities done in the past. Within each pair of pages the left-hand page contains two columns, one with a timetable for the day and the other for to-do items. The right-hand page contains the memory log. A “last week” section at the back stores previous memory log entries. A full year calendar allows appointments to be recorded. Ownsworth and McFarland compared two approaches to memory diary training72:
• Diary-only training. This approach focuses on functional skill building and compensation-based task-specific learning. The subjects were taught a behavioral sequence consisting of making a diary entry, checking it, and using the information as needed.
• Diary and self-instructional training. This approach emphasizes training of the subject’s capacity for the higher-level cognitive skills of self-regulation and self-awareness. The subjects were taught a WSTC strategy:
The authors found that during the treatment phase, those who were in the diary and self-instruction training group consistently made more diary entries, reported fewer memory problems, compensated better via use of strategies, and made more positive ratings associated with the efficacy of treatment. Potential sections of a memory notebook are included in Table 26-9.
TABLE 26-9
List and Purpose of Memory Notebook Sections
| Notebook Section | Purpose |
| Daily log | Used to record, store, and retrieve information about daily activities; forms contained for charting hourly information and scheduling appointments; forms contained for prioritizing a list of tasks |
| Calendar | Used for recording appointments and retrieving information about important meetings and upcoming events |
| Names | Used to record, store, and retrieve identifying information and “name drawings” of new people |
| Current work | Used for recording specific procedures about work assignments that may be needed at a later date |
| Personal notes | Used for recording important personal information such as personal goals or autobiographic information; also used for recording addresses, birthdays, etc. |
From Schmitter-Edgecombe M, Fahy JF, Whelan JP, et al: Memory remediation after severe closed head injury: notebook training versus supportive therapy, J Consult Clin Psychol 63(3):484-489, 1995.
Errorless Learning
Errorless learning is a learning strategy that is in contrast to trial-and-error learning or errorful learning. Interventions using an errorless learning approach are based on differences in learning abilities. It is typical for people with impairments in memory to more successfully remember their own mistakes as results of their own action than they remember corrections of their mistakes occurring via explicit means (e.g., a therapist’s cue). In other words, people may remember their mistakes but not the correction. With errorless learning a person learns something by saying or doing it rather than being told or shown by someone. A meta-analysis of errorless learning for treating memory loss conducted by Kessels and de Haan documented a large and statistically significant effect size for errorless learning treatment.51 In addition, no significant effect size was demonstrated for the vanishing cues method (i.e., teaching a skill by fading cues over time). It should be noted that the majority of studies that were analyzed used laboratory-type impairment measures such as word lists, face-name associations, and the like.
Assistive Technology
The literature focused on using technology to improve daily function in those with memory loss is substantial and consistently documents improvement in specifically trained tasks (managing medication, morning routines, IADLs, etc.). A variety of devices have been used (Box 26-4). Equipment that used to be specialized (paging systems, hand-held computers, etc.) continues to become commonplace; therefore, there is a larger population who may be amenable to using devices to compensate for memory loss. Typical smart phones have endless possibilities in terms of being used to cue performance of tasks in those with impaired memory. Examples include calendar functions, alarm functions, shopping list applications, dictation systems, map functions, contact lists, and others.
Mnemonics
Mnemonics is a broad term that refers to any strategy used to remember something, including rhymes, poems, acronyms, and imagery techniques. Examples include “Thirty days hath September…” (rhymes or poems to remember how many days are in each month), the acronym ROYGBIV to remember the colors of the spectrum, and imagining placing the items you want to remember in specific locations in a room with which you are familiar (method of loci).
Hux and colleagues assessed the effectiveness of three frequencies of intervention sessions focused on using mnemonics and visual imagery strategies to recall names of people: once per day, two times per week, and five times per day.49 Subjects included seven male TBI survivors ranging in age from 28 to 40 years. The results showed that sessions held daily and twice a week were more effective than sessions held five times per day. Mnemonics and visual imagery strategies were effective for four of the seven participants, regardless of the frequency of intervention sessions. More research is required to determine whether mnemonic strategies are generalizable to untrained tasks, as well as to provide information related to who is an appropriate candidate. At this point it seems that mnemonics are best suited for remembering specific and limited types of information (e.g., staff names).
Task-Specific Training
A series of experiments by Giles and colleagues documented improved daily function in those with severe memory loss via the following:
• An intervention program consisting of chaining nine discrete activities (shaving, oral care, etc.) by using linking phases. The phrases linked the performed activity to the one that immediately followed (e.g., “teeth cleaned, now shave”). The person was then asked to repeat the phrase as a cue to initiate the activity, which was followed by the behavioral techniques of verbal praise and a tangible reward.38
• An intervention that consisted of a cued ADL sequence that was determined by the client’s preinjury habits and responsiveness to cueing. Washing and dressing were conceptualized as a 16-step program in which the staff would cue the next step if behavior compatible with the next step in the sequence was not evident within approximately 5 seconds of completion of the previous step or if behavior incompatible with production of the next step in the behavioral chain was demonstrated. Although the client’s physical and cognitive status remained unchanged during the program, which lasted for 12 treatment days, he did become independent in washing and dressing. Initially requiring between 25 and 30 instructions, as well as physical assistance, to perform the tasks, the client progressed to independence. Independence was maintained at the 6-month follow-up.40
Similarly, Giles and associates present further support for these specific retraining protocols. Four clients were treated with the aforementioned washing and dressing protocol.39 Three sustained TBI, and one had brain injury after cerebral bleeding. All had moderate to severe memory loss. The training program consisted of behavioral observation, task analysis, consistent practice, and cue fading. The Adaptive Behavior Scale was used to measure change in behavior. The authors found that three subjects achieved rapid independence in washing and dressing (requiring 20 days, 37 days, and 11 days of treatment) and one did not show significant clinical improvement. Of note was that all clients admitted to the facility during a 3-year period and who required retraining in washing and dressing were treated with the same protocol. The authors further concluded that the consecutive series design prevented researchers from selecting clients whom they believed were good treatment candidates; therefore, the findings support the general applicability of the training program. See Box 26-5 for strategies for significant others.
Executive Dysfunction Having an Impact on Daily Function
Executive functions is an umbrella term that refers to complex cognitive processing requiring the coordination of several subprocesses to achieve a particular goal.29 This term has been defined as “a product of the coordinated operation of various processes to accomplish a particular goal in a flexible manner”36 or “those functions that enable a person to engage successfully in independent, purposive, self-serving behavior.”61 These higher-order mental capacities allow one to adapt to new situations and achieve goals. They include multiple specific functions such as decision making, problem solving, planning, task switching, modifying behavior in light of new information, self-correction, generating strategies, formulating goals, and sequencing complex actions. Unfortunately, there is a lack of consistency in the published literature related to whether a particular function is executive. Table 26-10 gives an in-depth list of the 20 most commonly reported dysexecutive symptoms, as well as the reported frequencies of these symptoms. Clearly, these executive functions support engagement in daily life activities and participation in the community, most important during new, nonroutine, complex, and unstructured situations (Table 26-11).
TABLE 26-10
Frequency of Reporting Dysexecutive Symptoms*
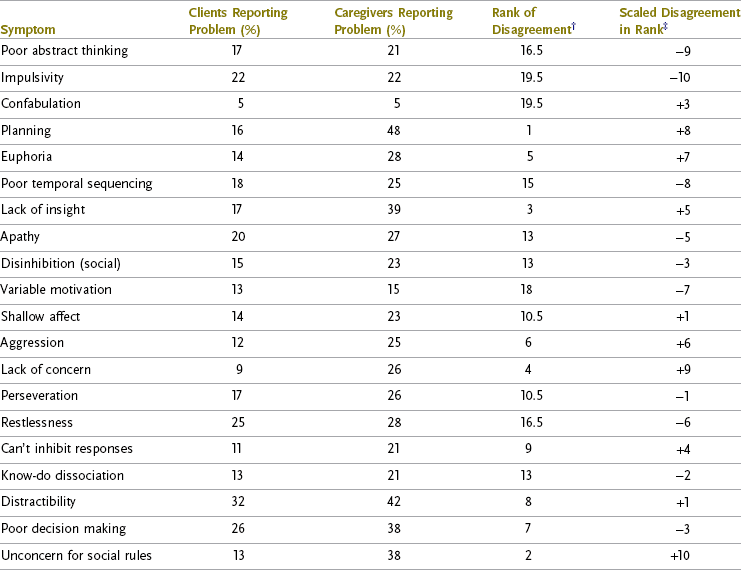
*Only ratings of 3 or 4 (out of a maximum of 4) for each item on the Dysexecutive Questionnaire were considered to indicate a problem. These correspond to classification of the symptom as “often” or “very often” observed. These results are based on data gathered as part of the study by Wilson and colleagues.
†This number represents the rank size of the disagreements (in proportions reporting the symptom) between clients and controls, in which 1 = the largest disagreement; that is, 1 means that caregivers reported this symptom much more often than clients did.
‡This number reflects the relative disagreement in rank frequency of reporting between clients and controls, scaled from −10 to +10, with 0 being absolute agreement in rank position of that symptom. On this scale, −10 means that this was a commonly reported symptom by clients, but not by caregivers, and +1 means that caregivers reported this symptom frequently, but it was relatively uncommon for clients to report it.
From Burgess PW, Simons JS: Theories of the frontal lobe executive function: clinical applications. In Halligan PW, Wade DT, editors: Effectiveness of rehabilitation for cognitive deficits, Oxford, UK, 2005, Oxford University Press.
TABLE 26-11
Examples of Executive Functions Related to Everyday Living: Preparing a Salad
| Executive Function | Associated Tasks |
| Initiation | Starting the task at the appropriate time without overreliance on prompts |
| Organization | Organizing the work space and performing the task efficiently (e.g., gathering the necessary vegetables at the same time from the refrigerator) |
| Sequencing | Sequencing the steps of the task appropriately (e.g., gather tools and vegetables, wash vegetables, chop and slice vegetables, mix in bowl, add dressing) |
| Problem solving | Solving the problem of a using a knife that is too dull to slice |
From Gillen G: Cognitive and perceptual rehabilitation: optimizing function, St. Louis, Mo, 2009, Mosby.
Indeed, recent studies examining meal preparation abilities in those with frontal lobe involvement support this hypothesis. Godbout and associates examined executive functions and ADLs in 10 clients with excised frontal lobe tumors and 10 normal controls by means of a neuropsychologic test battery, a script generation task, and a complex multitask ADL (planning and preparing a meal).42 The clients manifested numerous basic executive deficits on the pen-and-paper tests, were unimpaired on the script generation task (despite an aberrant semantic structure), and demonstrated marked difficulties in the meal preparation task. They concluded that the difficulties observed related to performing a lengthy complex multitask ADL can be explained by impairment of several executive functions, generalized slowness in performance, and paucity of behavior. Similarly, Fortin and colleagues investigated executive functions in performing ADLs in 10 clients with frontal lobe lesions after a mild to severe closed head injury (CHI) versus 12 normal controls by means of a neuropsychologic test battery, a script recitation task, and simulation of a complex multitask ADL.35 The authors found that the groups did not differ on any neuropsychologic test by nonparametric testing. However, the clients with CHI manifested marked anomalies in the meal preparation task. Although small sequences of actions were easily produced, large action sets could not be executed correctly. They concluded that an outstanding deficit in strategic planning and prospective memory appears to be an important underpinning of the impairment in ADLs observed in CHI clients with frontal lobe lesions. Similarly, it has been found that components of executive functioning such as categorization and deductive reasoning ability in persons with brain injury are good predictors of IADL functional performance.43
Lezak classified the various forms of executive disorders listed previously in a four-part schema60,61:
1. Volition and goal formulation: Including self-awareness, initiation, and motivation
2. Planning: Including the ability to conceptualize change, be objective, conceive alternatives, make choices, develop a plan, and sustain attention
3. Purposive action: To implement plans for achieving goals, including productivity, self-regulation, switching, and sequencing of actions
4. Performance effectiveness: Including quality control, self-correction, monitoring, and time management
Cicerone and associates also presented a schema based on executive functions. It includes four domains based on anatomy and evolutionary development23:
1. Executive cognitive functions (dorsolateral prefrontal cortex): Involved in the control and direction (planning, monitoring, activating, switching, inhibiting) of lower-level functions. Working memory and inhibition mediate executive functions.
2. Behavioral self-regulatory functions (ventral/medial prefrontal area): Involved in emotional processing and behavioral self-regulation when cognitive analysis, habit, or environmental cues are not sufficient to determine the best adaptive response.
3. Activation-regulating functions (medial frontal areas): Activation via initiative and energizing behavior. Pathology results in decrease in activation and drive, also known as apathy and abulia.
4. Metacognitive processes (frontal poles): Personality, social cognition, and self-awareness as reflected by accurate evaluation of one’s own abilities, as well as behavior, versus objective evaluation or reports by significant others.
People with impairments in executive functions, or dysexecutive syndrome, have impaired judgment, impulsiveness, apathy, poor insight, and lack of organization, planning, and decision making, as well as behavioral disinhibition and impaired intellectual abilities. Specific behavioral characteristics include impulsivity, poor attention, erratic response, lack of flexibility, and poor self-control.84,100 Of note is that people with impaired executive function may perform normally on pen-and-paper tests of cognition but unfortunately are found to have catastrophic everyday problems that are particularly evident in situations requiring multitasking and planning.94
The usual and customary tests of executive dysfunction include pen-and-paper measures or laboratory-type tasks, such as the Wisconsin Card Sorting Task, Trail Making Test, and Stroop Test, among others. As discussed earlier, the question of ecologic validity arises when using these measures, in addition to difficulty generalizing the results to everyday living tasks. These measures have only a low to moderate relationship to everyday skills.
Additionally, the standard clinical tests used to assess executive impairments are considered too structured and rater led; therefore, they fail to capture the common problems of initiation, planning, and self-monitoring. Recommended instruments are summarized in Tables 26-2 and 26-3.
Interventions for dysexecutive syndrome (Box 26-6) continue to be tested empirically.
Because executive functions act as a manager of other cognitive processes such as attention, memory, and language,62 some of the interventions previously described in this chapter are appropriate for those with dysexecutive symptoms, including TPM,31 self-instruction training,24 WSTC strategy,58 external cueing devices (paging system, recorded instructions, checklists, etc.),20,30,93 and manipulation of environmental variables with a focus on level of distraction.48 Other examples of specific interventions that have been tested and shown to be effective are described in the following sections.
Problem-Solving Training
The aim of this intervention is to substitute a participant’s impulsive approach to problem solving with a verbally mediated systematic analysis of the goal and the means by which it may be achieved.111 Participants were encouraged to act in the manner attributed to an intact executive system with a focus on five aspects of problem solving:
1. Problem orientation or identifying and analyzing. The difficulty in general recognition of a task or situation as a problem was the focus. The participant’s tendency to oversimplify problems and neglect relevant information was addressed.
2. Problem definition and formulation. Participants learned to survey information by reading and rereading directions and formulated questions to augment their understanding of the problem. Main and relevant points were written down. A focus was to teach participants to discriminate between relevant and irrelevant information.
3. Generating alternatives and solutions. Participants were asked to generate as many solutions as possible for a given problem. This was done individually, followed by the participants sharing solutions. The goal was to make participants aware that there were more solutions available than they had originally thought.
4. Decision making. Solutions were discussed and the pros and cons of the solutions were weighed. The feasibility of the solutions was also considered.
5. Solution verification and evaluation. Participants learned to recognize faulty solutions, self-correct errors, and return to other hypotheses. The focus here was on increased sensitivity to errors and discrepancies.
Others have recommended using problem-solving strategies such as stop and think; asking clear thinking questions; thinking your way through each step; defining the problem; using clear thinking questions to produce, evaluate, and examine the utility of as many alternative solutions as possible; and emotional self-regulation strategies.86 These problem-solving skills are then reinforced via role playing and practice of demanding real-life examples.
Goal Management Training
This intervention is aimed at decreasing disorganized behavior and improving one’s ability to maintain intentions in goal-directed behavior (goal management).59 Such disorganization results in one neglecting daily goals, such as never cleaning the house, forgetting to pack a lunch, or never getting around to making a shopping list, all of which compromise functional independence. Goal management training entails five stages that correspond to key aspects of goal-directed behavior:
• Stage 1: Orienting and assessing the current state. Stop current activity and direct awareness toward the task.
• Stage 2: Select the main goal.
• Stage 3: Partition the goals and make subgoals.
• Stage 4: Rehearse the steps necessary to complete the task. Encode, rehearse, and retain goals and subgoals.
• Stage 5: Monitor the outcome. Compare the outcome of action with the stated goal.
These steps are taught by using errorless techniques, and the cues for each stage are gradually faded to make sure that the person maintains nearly perfect performance.
Metacognitive Training
Birnboim and Miller tested the effectiveness of a metacognitive therapeutic approach14 in 10 people with multiple sclerosis and executive dysfunction.15 The approach focuses on the metacognitive aspects of behavior and assumes that metacognitive aspects can and should be learned explicitly via a structured process. Phases of the process include the following:
1. Understanding: The person must recognize his or her specific metacognitive deficits such as not planning. This was achieved by confronting various tasks in the clinic to increase awareness.
2. Practice: Efficient and specific strategies that the participant and therapist identify together (e.g., set priorities) are learned and practiced.
3. Transfer: Participants and their therapist consider when and where these strategies can be applied in real-life situations.
Computer strategy games (e.g., “Mastermind) and tabletop exercises were used during the first two phases of the training. Individualized daily activities were the focus of the generalization phase (e.g., specific work tasks). Positive results were noted on a strategy application test, tests of attention, memory tests, tests of executive function, and most important, the Occupational Therapy Functional Assessment Compilation Tool, which showed improved occupational role.
Summary
Jane’s case will be revisited to serve as a summary and conclusion. Jane’s initial evaluation was structured to first and foremost foster a client-centered approach to ensure that her occupational therapy sessions were tailored to her goals. Gary, Jane’s husband, was also involved in this process because Jane was demonstrating poor self-awareness related to her functional limitations. Gary reported that he worked full-time and Jane would be alone for a portion of the day. He stated that he would help in any way needed but was concerned that helping with self-care would change the dynamic in their new marriage and wanted self-care to be a focus of occupational therapy. Jane was focused on (sometimes perseverating on) finishing school. It was determined that morning sessions would focus on self-care and afternoon sessions would focus on school skills. As described earlier, the standardized FIM (required on most units) was administered. The FIM findings were supplemented by the standardized A-ONE, which documented the reasons for Jane’s limited performance in areas of occupation. Since it was quickly apparent the Jane was not aware of her limitations (one of Gary’s greatest concerns), the standardized Self Awareness of Deficits Interview was also administered as a priority. The OT performed nonstandardized assessments of school tasks. To assess performance, the OT requested that Gary bring in her current semester’s work and supplies at the end of the second week of therapy. The OT was able to document Jane’s reading comprehension, ability to attend to lectures (Jane always recorded lectures and Gary was able to locate the recordings), ability to structure note taking, and use of her laptop for e-mail functions. Deficits were noted in the areas of sustained attention, short-term memory, and being distracted by environmental stimuli.
The OT along with Jane and Gary set the following short-term goals focused on documenting improvements in areas of occupation:
1. Jane will complete upper body dressing with one tactile cue for initiation and no more than two verbal cues for sequencing.
2. Jane will complete grooming tasks (oral hygiene and hair care) with one tactile cue for initiation and the use of a checklist outlining the steps of the tasks.
3. Jane will persist in feeding herself for 10 minutes after one tactile cue for initiation.
1. All self-care tasks except for bathing will be completed with no more than one general verbal cue and external cueing devices as needed.
2. Jane will accurately write down three key points from a 10-minute lecture with one general verbal prompt to stay on task.
3. Jane will retrieve her e-mail from her laptop with no more than one verbal cue for sequencing.
In terms of interventions to meet the aforementioned goals and others, the general treatment approach chosen by Jane’s OT was the multicontext approach described earlier. This model was chosen primarily because of its emphasis on awareness training so that Jane could redefine her knowledge of her strengths and weaknesses. The OT hypothesized that improving awareness would be the starting point for intervention because he felt confident that if Jane were aware of her errors, he could teach her strategies that would allow her to meet her goals. In addition, the choice of intervention activities was based on Jane’s interests and goals (school tasks, reading fiction, cooking). Various processing strategies were practiced during a variety of functional activities and situations. Processing strategies were chosen to allow Jane to control the cognitive symptoms detected on her assessment. As Jane’s awareness improved, the OT was vigilant in monitoring her for signs of depression and anxiety. Jane’s OT began to place emphasis on teaching specific strategies to keep Jane “on task” (sustained attention), as well as determining which external cueing devices would allow Jane to stay organized and perform the steps of various tasks in the proper sequence. The OT planned interventions to occur in multiple environments (bedside, occupational therapy clinic, hospital gift store, staff office, hospital library) to promote generalization of learning.
1. Name and described three levels of self-awareness.
2. What does the concept of ecologic validity refer to when discussing cognitive assessments?
3. What is the rationale for using self-report/caregiver report measures for those with cognitive impairment?
4. What are two general approaches to managing attention deficits?
5. How does the occupational therapy approach for this population differ from that by other disciplines?
References
1. Abreu, BC, Peloquin, SM. The quadraphonic approach: a holistic rehabilitation model for brain injury. In: Katz N, ed. Cognition and occupation across the life span. Bethesda, Md: AOTA Press, 2005.
2. Alderman, N, Burgess, PW, Knight, C, et al. Ecological validity of a simplified version of the Multiple Errands Shopping Test. J Clin Exp Neuropsychol. 2003;9(1):31–44.
3. American Occupational Therapy Association. Occupational therapy practice framework: domain and process. Am J Occup Ther. 2008;62(6):625–683.
4. Amos, A. Remediating deficits of switching attention in patients with acquired brain injury. Brain Inj. 2002;16(5):407–413.
5. Anderson, V, Fenwick, T, Manly, T, et al. Attentional skills following traumatic brain injury in childhood: a componential analysis. Brain Inj. 1998;12(11):937–949.
6. Anderson, SW, Tranel, D. Awareness of disease states following cerebral infarction, dementia, and head trauma: standardized assessment. Clin Neuropsychol. 1989;3:327–339.
7. Árnadóttir, G. The brain and behavior: assessing cortical dysfunction through activities of daily living. St. Louis, Mo: Mosby; 1990.
8. Árnadóttir, G. Impact of neurobehavioral deficits of activities of daily living. In Gillen G, ed.: Stroke rehabilitation: a function-based approach, ed 3, St. Louis, Mo: Mosby, 2011.
9. Árnadóttir, G, Fisher, AG. Rasch analysis of the ADL scale of the A-ONE. Am J Occup Ther. 2008;62(1):51–60.
10. Árnadóttir, G, Fisher, AG, Löfgren, B. Dimensionality of nonmotor neurobehavioral impairments when observed in the natural contexts of ADL task performance. Neurorehabil Neural Repair. 2009;23(6):579–586.
11. Averbuch, MA, Katz, N. Cognitive rehabilitation: a retraining model for clients with neurological disabilities. In: Katz N, ed. Cognition and occupation across the lifespan. Bethesda, Md: AOTA Press, 2005.
12. Baddeley, AD. The psychology of memory. In: Baddeley AD, Kopelman MD, Wilson BA, eds. The essential handbook of memory disorders for clinicians. Hoboken, NJ: John Wiley, 2004.
13. Baum, CM, Edwards, DF, Morrison, T, et al. The reliability, validity, and clinical utility of the Executive Function Performance Test: a measure of executive function in a sample of persons with stroke. Am J Occup Ther. 2008;62:446–455.
14. Birnboim, SA. Metacognitive approach to cognitive rehabilitation. Br J Occup Ther. 1995;58:61–64.
15. Birnboim, S, Miller, A. Cognitive rehabilitation for multiple sclerosis patients with executive dysfunction. J Cogn Rehabil. 2004;22:11–18.
16. Borgaro, SR, Prigatano, GP. Modification of the Patient Competency Rating Scale for use on an acute neurorehabilitation unit: the PCRS-NR. Brain Inj. 2003;17(10):847–853.
17. Boyd, TM, Sautter, SW. Route-finding: a measure of everyday executive functioning in the head-injured adult. Appl Cogn Psychol. 1993;7(2):171–181.
18. Broadbent, DE, Cooper, PF, FitzGerald, P, et al. The Cognitive Failures Questionnaire (CFQ) and its correlates. Br J Clin Psychol. 1982;21:1–16.
19. Burgess, PW, Alderman, N, Emslie, H, et al. The Dysexecutive Questionnaire. In: Wilson BA, Alderman N, Burgess PW, et al, eds. Behavioural assessment of the dysexecutive syndrome. Bury St. Edmunds, UK: Thames Valley Test Company, 1996.
20. Burke, WH, Zencius, AH, Wesolowski, MD, et al. Improving executive function disorders in brain-injured clients. Brain Inj. 1991;5(3):241–252.
21. Chaytor, N, Schmitter-Edgecombe, M. The ecological validity of neuropsychological tests: a review of the literature on everyday cognitive skills. Neuropsychol Rev. 2003;13:181–197.
22. Cicerone, KD. Remediation of “working attention” in mild traumatic brain injury. Brain Inj. 2002;16(3):185–195.
23. Cicerone, KD, Dahlberg, C, Malec, JF, et al. Evidence-based cognitive rehabilitation: updated review of the literature from 1998 through 2002. Arch Phys Med Rehabil. 2005;86(8):1681–1692.
24. Cicerone, KD, Giacino, JT. Remediation of executive function deficits after traumatic brain injury. NeuroRehabilitation. 1992;2(3):12–22.
25. Crosson, B, Barco, PP, Velozo, CA, et al. Awareness and compensation in postacute head injury rehabilitation. J Head Trauma Rehabil. 1989;4(3):46–54.
26. Dawson, DR, Anderson, ND, Burgess, P, et al. Further development of the Multiple Errands Test: standardized scoring, reliability, and ecological validity for the Baycrest version. Arch Phys Med Rehabil. 2009;90(11 suppl):S41–S51.
27. Dockree, PM, Kelly, SP, Roche, RAP, et al. Behavioural and physiological impairments of sustained attention after traumatic brain injury. Cogn Brain Res. 2004;20(3):403–414.
28. Donaghy, S, Williams, W. A new protocol for training severely impaired patients in the usage of memory journals. Brain Inj. 1998;12:1061–1076.
29. Elliott, R. Executive functions and their disorders. Br Med Bull. 2003;65:49–59.
30. Evans, JJ, Emslie, H, Wilson, BA. External cueing systems in the rehabilitation of executive impairments of action. J Int Neuropsychol Soc. 1998;4(4):399–408.
31. Fasotti, L, Kovacs, F, Eling, PATM, et al. Time pressure management as a compensatory strategy training after closed head injury. Neuropsychol Rehabil. 2000;10(1):47–65.
32. Fisher, AG. Assessment of motor and process skills, Volume I, Development, Standardization, and Administration, ed 6. Fort Collins, Colo: Three Star Press; 2006.
33. Fleming, JM, Lucas, SE, Lightbody, S. Using occupation to facilitate self-awareness in people who have acquired brain injury: a pilot study. Can J Occup Ther. 2006;73(1):44–55.
34. Fleming, J, Strong, J. Self-awareness of deficits following acquired brain injury: considerations for rehabilitation. Br J Occup Ther. 1995;58(2):55–60.
35. Fortin, S, Godbout, L, Braun, CM. Cognitive structure of executive deficits in frontally lesioned head trauma patients performing activities of daily living. Cortex. 2003;39(2):273–291.
36. Funahashi, S. Neuronal mechanisms of executive control by the prefrontal cortex. Neurosci Res. 2001;39:147–165.
37. Giles, GM. A neurofunctional approach to rehabilitation following severe brain injury. In: Katz N, ed. Cognition and occupation across the life span. Bethesda, Md: AOTA Press, 2005.
38. Giles, GM, Morgan, JH. Training functional skills following herpes simplex encephalitis: a single case study. J Clin Exp Neuropsychol. 1989;11(2):311–318.
39. Giles, GM, Ridley, JE, Dill, A, et al. A consecutive series of adults with brain injury treated with a washing and dressing retraining program. Am J Occup Ther. 1997;51(4):256–266.
40. Giles, GM, Shore, M. The effectiveness of an electronic memory aid for a memory-impaired adult of normal intelligence. Am J Occup Ther. 1989;43(6):409–411.
41. Gillen, G. Cognitive and perceptual rehabilitation: optimizing function. St. Louis, Mo: Mosby; 2009.
42. Godbout, L, Grenier, MC, Braun, CM, et al. Cognitive structure of executive deficits in patients with frontal lesions performing activities of daily living. Brain Inj. 2005;19(5):337–348.
43. Goverover, Y, Hinojosa, J. Categorization and deductive reasoning: can they serve as predictors of instrumental activities of daily living performance in adults with brain injury? Am J Occup Ther. 2002;56:509–516.
44. Groot, YC, Wilson, BA, Evans, J, et al. Prospective memory functioning in people with and without brain injury. J Clin Exp Neuropsychol. 2002;8(5):645–654.
45. Hannon, R, Adams, P, Harrington, S, et al. Effects of brain injury and age on prospective memory self-rating and performance. Rehabil Psychol. 1995;40(4):289–298.
46. Hart, T, Whyte, J, Millis, S, et al. Dimensions of disordered attention in traumatic brain injury: further validation of the Moss Attention Rating Scale. Arch Phys Med Rehabil. 2006;87(5):647–655.
47. Hartman-Maeir, A, Harel, H, Katz, N. Kettle test—a brief measure of cognitive functional performance: reliability and validity in stroke rehabilitation. Am J Occup Ther. 2009;63(5):592–599.
48. Hayden, ME, Moreault, AM, LeBlanc, J, et al. Reducing level of handicap in traumatic brain injury: an environmentally based model of treatment. J Head Trauma Rehabil. 2000;15(4):1000–1021.
49. Hux, K, Manasse, N, Wright, S, et al. Effect of training frequency on face-name recall by adults with traumatic brain injury. Brain Inj. 2000;14(10):907–920.
50. Katz, N. Cognition and occupation across the life span. Bethesda, Md: AOTA Press; 2005.
51. Kessels, RP, de Haan, EH. Implicit learning in memory rehabilitation: a meta-analysis on errorless learning and vanishing cues methods. J Clin Exp Neuropsychol. 2003;25(6):805–814.
52. Kim, HJ, Craik, FI, Luo, L, Ween, JE. Impairments in prospective and retrospective memory following stroke. Neurocase. 2009;15(2):145–156.
53. Kime, SK. Compensating for memory deficits using a systematic approach. Bethesda, Md: AOTA Press; 2006.
54. Knight, C, Alderman, N, Burgess, PW. Development of a simplified version of the multiple errands test for use in hospital settings. Neuropsychol Rehabil. 2002;12(3):231–256.
55. Kottorp, A, Tham, K. Assessment of Awareness of Disability (AAD), manual for administration, scoring, and interpretation. Stockholm, Sweden: Karolinska Institute, NEUROTEC Department, Division of Occupational Therapy; 2005.
56. Law, M, Baptiste, S, Carswell, A, et al. The Canadian occupational performance measure, ed 4. Ottawa, Canada: CAOT Publications ACE; 2005.
57. Law, M, Baum, C, Dunn, W. Measuring occupational performance: supporting best practice in occupational therapy. Thorofare, NJ: Slack; 2005.
58. Lawson, MJ, Rice, DN. Effects of training in use of executive strategies on a verbal memory problem resulting from closed head injury. J Clin Exp Neuropsychol. 1989;11(6):842–854.
59. Levine, B, Robertson, IH, Clare, L, et al. Rehabilitation of executive functioning: an experimental-clinical validation of goal management training. J Clin Exp Neuropsychol. 2000;6(3):299–312.
60. Lezak, MD. Newer contributions to the neuropsychological assessment of executive functions. J Head Trauma Rehabil. 1993;8(1):24–31.
61. Lezak, MD. Executive function and motor performance. In: Lezak MD, Howieson DB, Loring DW, eds. Neurological assessment. New York, NY: Oxford University Press, 2004.
62. Manchester, D, Priestley, N, Jackson, H. The assessment of executive functions: coming out of the office. Brain Inj. 2004;18(11):1067–1081.
63. Manly, T, Ward, S, Robertson, IH. The rehabilitation of attention. In: Eslinger PJ, ed. Neuropsychological interventions: emerging treatment and management models for neuropsychological impairments. New York, NY: Guilford Press, 2000.
64. Mathiowetz, V. Task oriented approach to stroke rehabilitation. In Gillen G, ed.: Stroke rehabilitation: a function-based approach, ed 3, St. Louis, Mo: Mosby, 2011.
65. Mathiowetz, V, Bass-Haugen, J. Assessing abilities and capacities: motor behavior. In Radomski MV, Latham CAT, eds.: Occupational therapy for physical dysfunction, ed 6, Baltimore, Md: Lippincott Williams & Wilkins, 2008.
66. McAvinue, L, O’Keeffe, F, McMackin, D, et al. Impaired sustained attention and error awareness in traumatic brain injury: implications for insight. Neuropsychol Rehabil. 2005;15(5):569–587.
67. Michel, JA, Mateer, CA. Attention rehabilitation following stroke and traumatic brain injury, a review. Eura Medicophys. 2006;42(1):59–67.
68. Mirsky, AF, Anthony, BJ, Duncan, CC, et al. Analysis of the elements of attention: a neuropsychological approach. Neuropsychol Rev. 1991;2(2):109–145.
69. Neistadt, ME. Perceptual retraining for adults with diffuse brain injury. Am J Occup Ther. 1994;48(3):225–233.
70. O’Keeffe, F, Dockree, P, Moloney, P, et al. Awareness of deficits in traumatic brain injury: a multidimensional approach to assessing metacognitive knowledge and online awareness. J Clin Exp Neuropsychol. 2007;13(1):38–49.
71. Ownsworth, T, Clare, L. The association between awareness deficits and rehabilitation outcome following acquired brain injury. Clin Psychol Rev. 2006;26(6):783–795.
72. Ownsworth, TL, McFarland, K. Memory remediation in long-term acquired brain injury: two approaches in diary training. Brain Inj. 1999;13(8):605–626.
73. Ownsworth, TL, McFarland, KM, Young, RM. Development and standardization of the Self-Regulation Skills Interview (SRSI): a new clinical assessment tool for acquired brain injury. Clin Neuropsychol. 2000;14(1):76–92.
74. Park, NW, Ingles, JL. Effectiveness of attention rehabilitation after an acquired brain injury: a meta-analysis. Neuropsychology. 2001;15(2):199–210.
75. Penner, IK, Kappos, L. Retraining attention in MS. J Neurol Sci. 2006;245(1-2):147–151.
76. Ponsford, J, Kinsella, G. The use of a rating scale of attentional behaviour. Neuropsychol Rehabil. 1991;1(4):241–257.
77. Posner, MI, Peterson, SE. The attention system of the human brain. Annu Rev Neurosci. 1990;13:25–42.
78. Preissner, K. Use of the occupational therapy task-oriented approach to optimize the motor performance of a client with cognitive limitations. Am J Occup Ther. 2010;64:727–734.
79. Prigatano, GP. Neuropsychological rehabilitation after brain injury. Baltimore, Md: Johns Hopkins University Press; 1986.
80. Prigatano, GP. Anosognosia. In: Beaumont JG, Kenealy PM, Rogers MJC, eds. The Blackwell dictionary of neuropsychology. Cambridge, Mass: Blackwell, 1996.
81. Prigatano, GP. Disturbances of self-awareness and rehabilitation of patients with traumatic brain injury: a 20-year perspective. J Head Trauma Rehabil. 2005;20(1):19–29.
82. Prigatano, GP, Klonoff, PS. A clinician’s rating scale for evaluating impaired self-awareness and denial of disability after brain injury. Clin Neuropsychol. 1998;12(1):56–67.
83. Prigatano, GP, Schacter, DL. Awareness of deficit after brain injury: clinical and theoretical implications. New York, NY: Oxford University Press; 1991.
84. Proctor, A, Wilson, B, Sanchez, C, et al. Executive function and verbal working memory in adolescents with closed head injury (CHI). Brain Inj. 2000;14(7):633–647.
85. Quemada, JI, Cespedes, JMM, Ezkerra, J, et al. Outcome of memory rehabilitation in traumatic brain injury assessed by neuropsychological tests and questionnaires. J Head Trauma Rehabil. 2003;18(6):532–540.
86. Rath, JF, Simon, D, Langenbahn, DM, et al. Group treatment of problem-solving deficits in outpatients with traumatic brain injury: a randomised outcome study. Neuropsychol Rehabil. 2003;13(4):461–488.
87. Ries, M, Marks, W. Selective attention deficits following severe closed head injury: the role of inhibitory processes. Neuropsychology. 2005;19(4):476–483.
88. Robertson, IH, Ward, T, Ridgeway, V, Nimmo-Smith, I. The structure of normal human attention: the Test of Everyday Attention. J Clin Exp Neuropsychol. 1996;2(6):525–534.
89. Roche, NL, Fleming, JM, Shum, DH. Self-awareness of prospective memory failure in adults with traumatic brain injury. Brain Inj. 2002;16(11):931–945.
90. Roth, RS, et al. Cognitive complaints are associated with depression, fatigue, female sex, and pain catastrophizing in patients with chronic pain. Arch Phys Med Rehab. 2005;86(6):1147–1154.
91. Royle, J, Lincoln, NB. The Everyday Memory Questionnaire—revised: development of a 13-item scale. Disabil Rehabil. 2008;30(2):114–121.
92. Sandler, AB, Harris, JL. Use of external memory aids with a head-injured patient. Am J Occup Ther. 1992;46(2):163–166.
93. Schwartz, SM. Adults with traumatic brain injury: three case studies of cognitive rehabilitation in the home setting. Am J Occup Ther. 1995;49(7):655–667.
94. Shallice, T, Burgess, PW. Deficits in strategy application following frontal lobe damage in man. Brain. 1991;114(Pt 2):727–741.
95. Sherer, M, Bergloff, P, Boake, C, et al. The Awareness Questionnaire: factor structure and internal consistency. Brain Inj. 1998;12(1):63–68.
96. Smith, G, Della Sala, S, Logie, RH, Maylor, EA. Prospective and retrospective memory in normal ageing and dementia: a questionnaire study. Memory. 2000;8:311–321.
97. Sohlberg, MM, Mateer, CA. Training use of compensatory memory books: a three stage behavioral approach. J Clin Exp Neuropsychol. 1989;11(6):871–891.
98. Sohlberg, MM, Mateer, CA. Management of attention disorders. In: Sohlberg MM, Mateer CA, eds. Cognitive rehabilitation: an integrative neuropsychological approach. New York, NY: Guilford Press, 2001.
99. Sohlberg, MM, Mateer, CA. Memory theory applied to intervention. In: Sohlberg MM, Mateer CA, eds. Cognitive rehabilitation: an integrative neuropsychological approach. New York, NY: Guilford Press, 2001.
100. Sohlberg, MM, Mateer, CA. Management of dysexecutive symptoms. In: Sohlberg MM, Mateer CA, eds. Cognitive rehabilitation: an integrative neuropsychological approach. New York, NY: Guilford Press, 2001.
101. Squire, LR. Memory systems of the brain: a brief history and current perspective. Neurobiol Learn Mem. 2004;82:171–177.
102. Sunderland, A, Harris, JE, Baddeley, AD. Do laboratory tests predict everyday memory? A neuropsychological study. J Verbal Learn Verbal Behav. 1983;22(3):341–357.
103. Sunderland, A, Harris, JE, Baddeley, AD. Assessing everyday memory after severe head injury. In: Harris JE, Morris PE, eds. Everyday memory, actions, and absent-mindedness. London, UK: Academic Press, 1984.
104. Tham, K, Ginsburg, E, Fisher, AG, et al. Training to improve awareness of disabilities in clients with unilateral neglect. Am J Occup Ther. 2001;55:46–54.
105. Toglia, J. Contextual memory test. San Antonio, Tex: Harcourt Assessments; 1993.
106. Toglia, J. A dynamic interactional approach to cognitive rehabilitation. In: Katz N, ed. Cognition and occupation across the life span. Bethesda, Md: AOTA Press, 2005.
107. Toglia, J. Generalization of treatment: a multicontext approach to cognitive perceptual impairment in adults with brain injury. Am J Occup Ther. 1991;45(6):505–516.
108. Toglia, J, Kirk, U. Understanding awareness deficits following brain injury. Neurorehabil. 2000;15(1):57–70.
109. Toglia, J. Examiner guidelines for the weekly calendar planning test: unpublished manual. Dobbs Ferry, NY: Mercy College; 2010.
110. van den Broek, MD. Why does neurorehabilitation fail? J Head Trauma Rehabil. 2005;20(5):464–543.
111. von Cramon, DY, Matthes-von Cramon, G, Mai, N. Problem-solving deficits in brain-injured patients: a therapeutic approach. Neuropsychol Rehabil. 1991;1(1):45–64.
112. Waugh, N. Self report of the young, middle-aged, young-old, and old-old individuals on prospective memory self-rating performance. Honours thesis, Brisbane, Australia: School of Applied Psychology, Griffith University; 1999.
113. Webster, JS, Scott, RR. The effects of self-instructional training on attentional deficits following head injury. Clin Neuropsychol. 1983;5(2):69–74.
114. Whyte, J, Polansky, M, Fleming, M, et al. Sustained arousal and attention after traumatic brain injury. Neuropsychologia. 1995;33(7):797–813.
115. Whyte, J. Attention and arousal: basic science aspects. Arch Phys Med Rehabil. 1992;73(10):940–949.
116. Whyte, J, Hart, T, Bode, RK, et al. The Moss Attention Rating Scale for traumatic brain injury: initial psychometric assessment. Arch Phys Med Rehabil. 2003;84(2):268–276.
117. Wilson, BA, Alderman, N, Burgess, PW, et al. Behavioural assessment of the dysexecutive syndrome. Flempton, UK: Thames Valley Test Company; 1996.
118. Wilson, BA, Evans, JJ, Emslie, H, et al. The development of an ecologically valid test for assessing patients with dysexecutive syndrome. Neuropsychol Rehabil. 1998;8(3):213–228.
119. Wilson, BA, Sopena, S, Cockburn, J, et al. The Rivermead Behavioural Memory Test, ed 3. London, UK: Pearson Assessment; 2008.