Differential Diagnosis of Oral and Maxillofacial Diseases
The most important aspect of patient care is the accurate diagnosis of the patient’s disease. Unfortunately, the clinical presentation of many disease processes can be strikingly similar, despite their vast differences in etiology and pathogenesis. Because treatment and, ultimately, prognosis are based on the diagnosis, the diagnostic process is critical in optimal patient management. This appendix provides some guidelines for expediting and facilitating the diagnostic process from a clinical perspective.
The first step in gathering information is the acquisition of a thorough history of the disease process. This step typically includes items such as the onset, severity, location, duration, character, and course of the signs and symptoms being experienced by the patient. Additional information regarding medical, social, and family history may be necessary. With this information, the clinician can often start the process of formulating a list of possible diagnoses, even before performing an examination.
The information obtained during the clinical examination is also important because many lesions have characteristic appearances. By evaluating these characteristics in conjunction with the patient’s history, often the clinician can narrow the list of diag-nostic possibilities. This list, known as a differential diagnosis, essentially includes possible pathologic entities, usually ranked in order from most likely to least likely.
DEFINITIONS
To better describe the appearances of lesions and communicate these features to colleagues, the clinician should be familiar with the following terms:
Macule. Focal area of color change that is not elevated or depressed in relation to its surroundings.
Papule. Solid, raised lesion that is less than 5 mm in diameter.
Nodule. Solid, raised lesion that is greater than 5 mm in diameter.
Sessile. Describing a tumor or growth whose base is the widest part of the lesion.
Pedunculated. Describing a tumor or growth whose base is narrower than the widest part of the lesion.
Papillary. Describing a tumor or growth exhibiting numerous surface projections.
Verrucous. Describing a tumor or growth exhibiting a rough, warty surface.
Vesicle. Superficial blister, 5 mm or less in diameter, usually filled with clear fluid.
Bulla. Large blister, greater than 5 mm in diameter.
Pustule. Blister filled with purulent exudate.
Ulcer. Lesion characterized by loss of the surface epithelium and frequently some of the underlying connective tissue. It often appears depressed or excavated.
Erosion. Superficial lesion, often arising secon-dary to rupture of a vesicle or bulla, that is char-acterized by partial or total loss of the surface epithelium.
Fissure. Narrow, slitlike ulceration or groove.
Plaque. Lesion that is slightly elevated and is flat on its surface.
Petechia. Round, pinpoint area of hemorrhage.
Ecchymosis. Nonelevated area of hemorrhage, larger than a petechia.
Telangiectasia. Vascular lesion caused by dilatation of a small, superficial blood vessel.
Cyst. Pathologic epithelium-lined cavity, often filled with liquid or semi-solid contents.
Unilocular. Describing a radiolucent lesion having a single compartment.
Multilocular. Describing a radiolucent lesion having several or many compartments.
By using these terms, the clinician can describe the characteristics of lesions efficiently and uniformly. Applying these clinical descriptors to the lesions also can help categorize them with respect to the differential diagnosis. By adding additional characteristics such as prevalence, patient race or nationality, patient age at diagnosis, patient sex, and sites of predilection, the clinician can hone the differential diagnosis list considerably.
HOW TO USE THIS APPENDIX
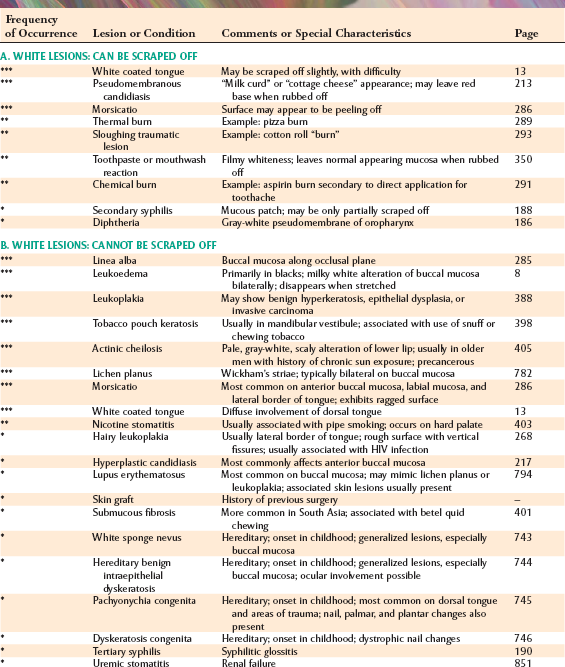
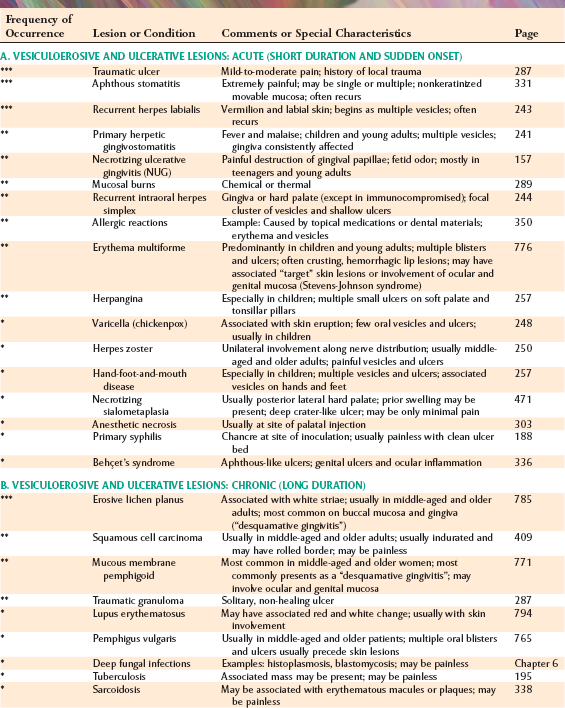
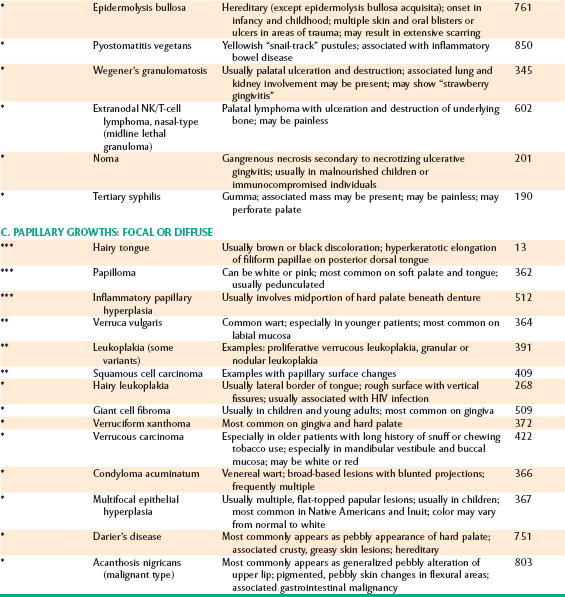
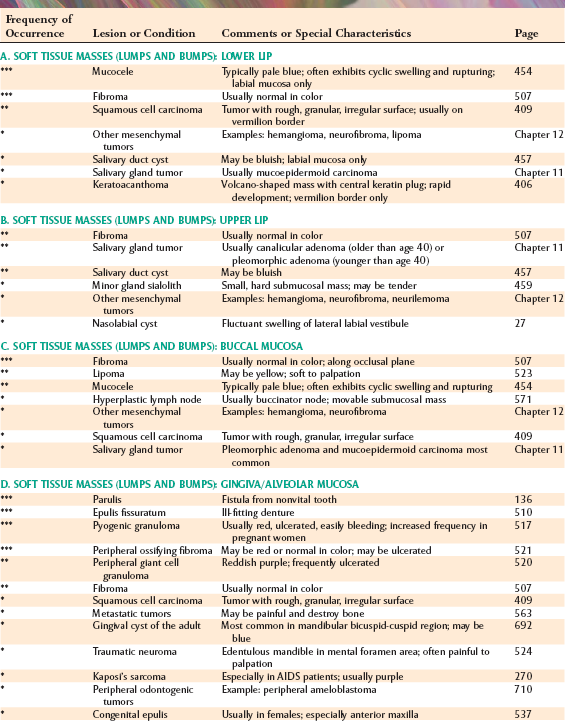
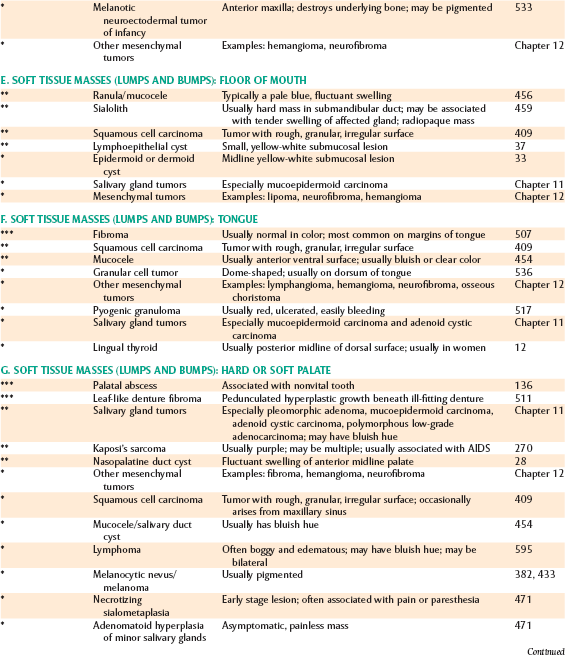
This appendix is designed to help the clinician formulate a differential diagnosis by organizing and categorizing disease entities according to their most prominent or identifiable clinical features. Under each “clinical feature” heading is a list of lesions with that clinical feature as a prominent component. Diseases are listed according to estimated frequency relative to similar diseases or lesions.
The most common lesions are marked with triple asterisks (***), less common lesions are marked with double asterisks (**), and rare lesions are marked with a single asterisk (*). Such estimated frequency indica tors should not be compared between lists; they are intended only for the single differential diagnosis list in which they occur.
Clinical features that most readily distinguish the lesions are listed with each disease process to help focus the clinician’s search for the most accurate diagnosis. Finally, the corresponding page number in the book is provided for each disease entity so that the reader can refer to the text for a more detailed discussion.
INDEX TO THE APPENDIX: DIFFERENTIAL DIAGNOSIS LISTS
PART 1: MUCOSAL AND SOFT TISSUE PATHOLOGY: COLOR CHANGES
| A. White Lesions: Can Be Scraped Off | 920 |
| B. White Lesions: Cannot Be Scraped Off | 920 |
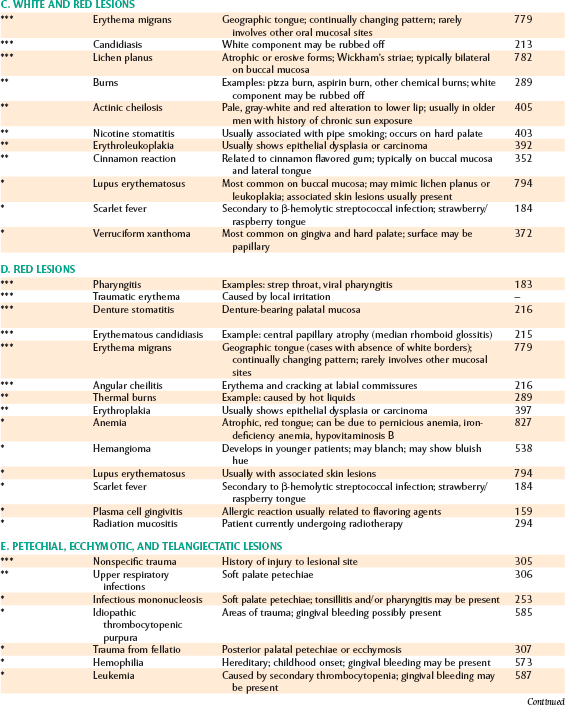
| C. White and Red Lesions | 921 |
| D. Red Lesions | 921 |
| E. Petechial, Ecchymotic, and Telangiectatic Lesions | 921 |
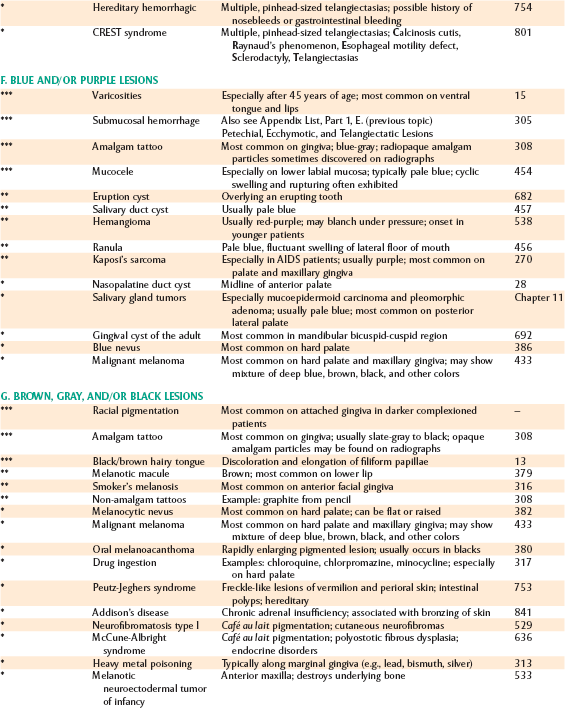
| F. Blue and/or Purple Lesions | 922 |
| G. Brown, Gray, and/or Black Lesions | 922 |
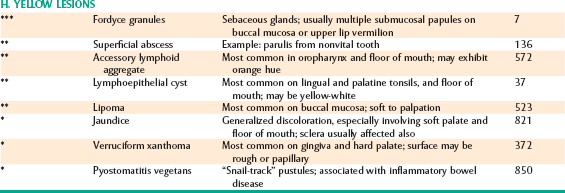
| H. Yellow Lesions | 923 |
PART 2: MUCOSAL AND SOFT TISSUE PATHOLOGY: SURFACE ALTERATIONS
| A. Vesiculoerosive and Ulcerative Lesions: | |
| Acute (Short Duration and Sudden Onset) | 924 |
| B. Vesiculoerosive and Ulcerative Lesions: Chronic (Long Duration) | 924 |
| C. Papillary Growths: Focal or Diffuse | 925 |
PART 3: MUCOSAL AND SOFT TISSUE PATHOLOGY: MASSES OR ENLARGEMENTS
| A. Soft Tissue Masses (Lumps and Bumps): Lower Lip | 926 |
| B. Soft Tissue Masses (Lumps and Bumps): Upper Lip | 926 |
| C. Soft Tissue Masses (Lumps and Bumps): Buccal Mucosa | 926 |
| D. Soft Tissue Masses (Lumps and Bumps): Gingiva/Alveolar Mucosa | 926 |
| E. Soft Tissue Masses (Lumps and Bumps): Floor of Mouth | 927 |
| F. Soft Tissue Masses (Lumps and Bumps): Tongue | 927 |
| G. Soft Tissue Masses (Lumps and Bumps): Hard or Soft Palate | 927 |
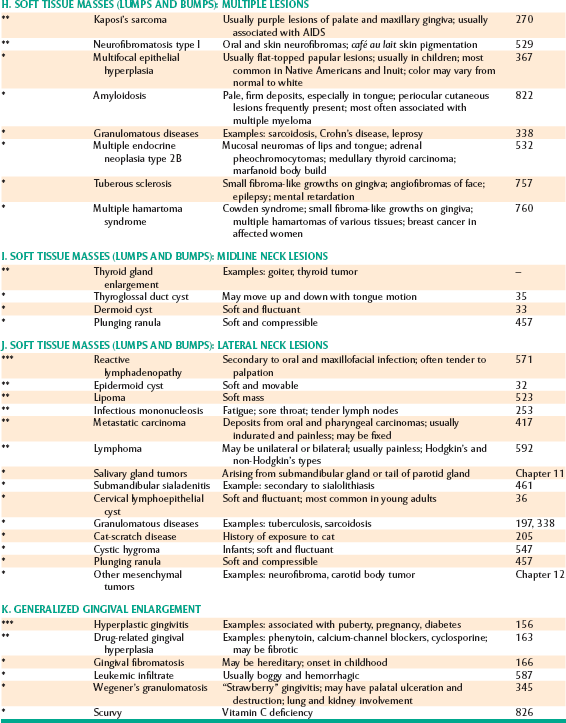
| H. Soft Tissue Masses (Lumps and Bumps): Multiple Lesions | 928 |
| I. Soft Tissue Masses (Lumps and Bumps): Midline Neck Lesions | 928 |
| J. Soft Tissue Masses (Lumps and Bumps): Lateral Neck Lesions | 928 |
| K. Generalized Gingival Enlargement | 928 |
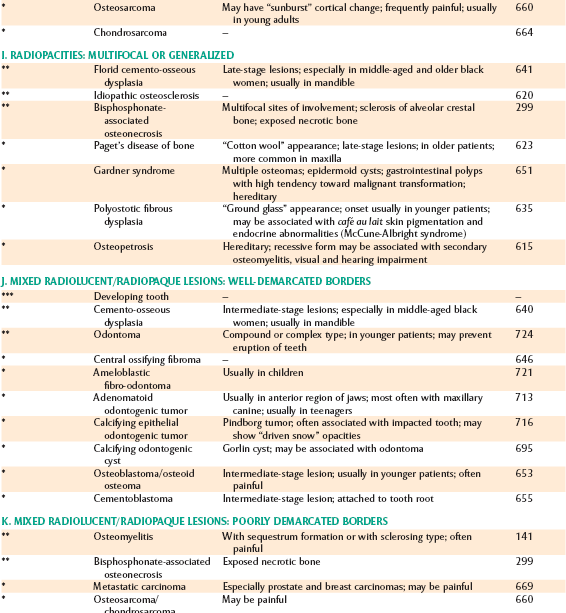
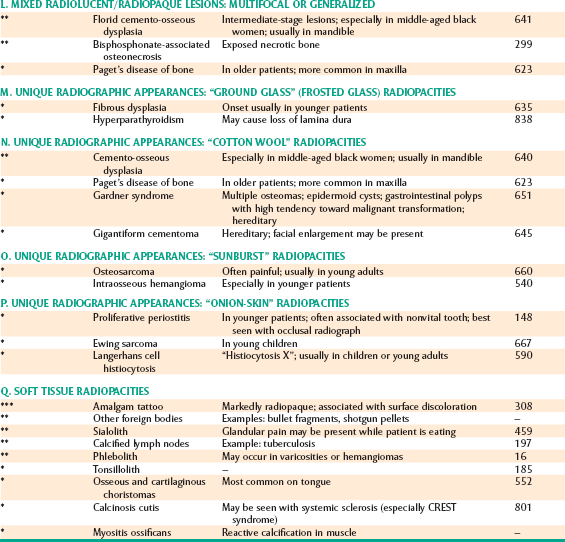
PART 4: RADIOGRAPHIC PATHOLOGY
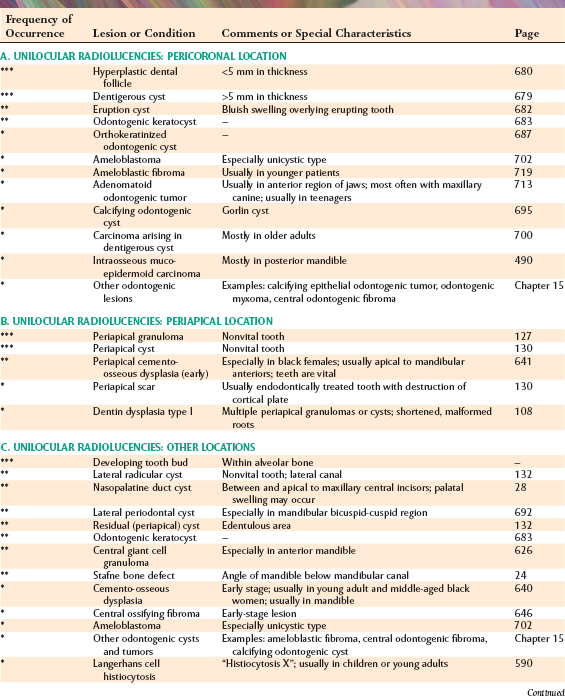
| A. Unilocular Radiolucencies: Pericoronal Location | 929 |
| B. Unilocular Radiolucencies: Periapical Location | 929 |
| C. Unilocular Radiolucencies: Other Locations | 929 |
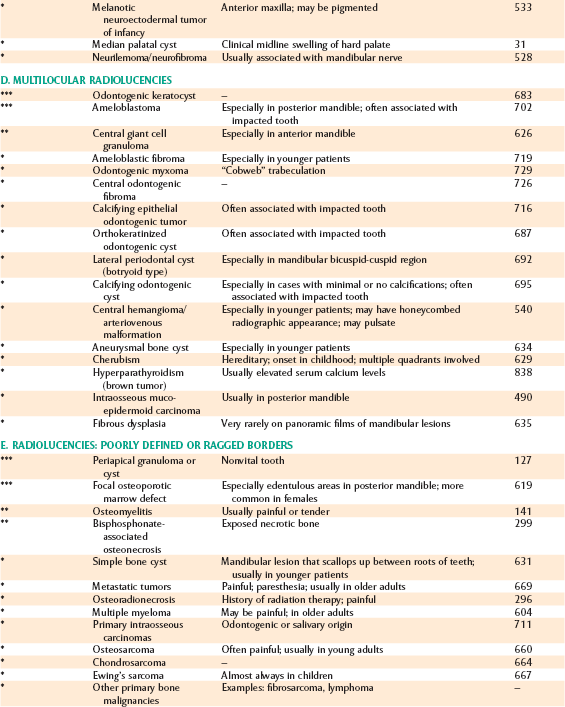
| D. Multilocular Radiolucencies | 930 |
| E. Radiolucencies: Poorly Defined or Ragged Borders | 930 |
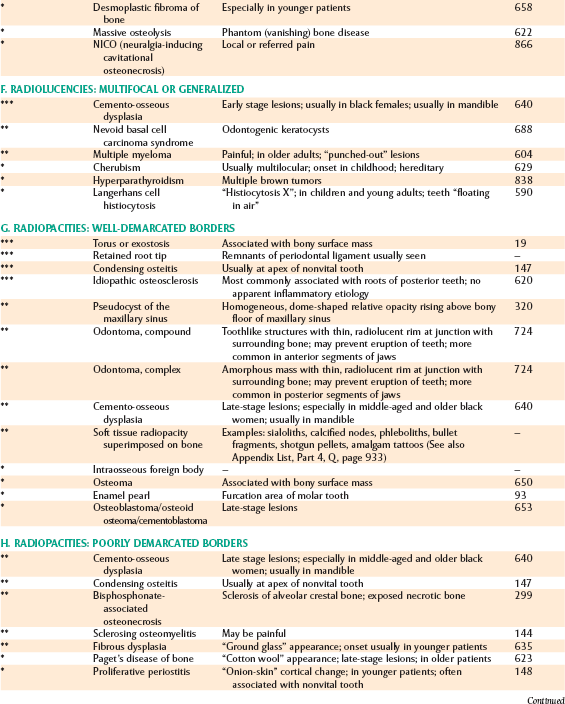
| F. Radiolucencies: Multifocal or Generalized | 931 |
| G. Radiopacities: Well-Demarcated Borders | 931 |
| H. Radiopacities: Poorly Demarcated Borders | 931 |
| I. Radiopacities: Multifocal or Generalized | 932 |
| J. Mixed Radiolucent/Radiopaque Lesions: Well-Demarcated Borders | 932 |
| K. Mixed Radiolucent/Radiopaque Lesions: Poorly Demarcated Borders | 932 |
| L. Mixed Radiolucent/Radiopaque Lesions: Multifocal or Generalized | 933 |
| M. Unique Radiographic Appearances: “Ground Glass” (Frosted Glass) Radiopacities | 933 |
| N. Unique Radiographic Appearances: “Cotton Wool” Radiopacities | 933 |
| O. Unique Radiographic Appearances: “Sunburst” Radiopacities | 933 |
| P. Unique Radiographic Appearances: “Onion-Skin” Radiopacities | 933 |
| Q. Soft Tissue Radiopacities | 933 |
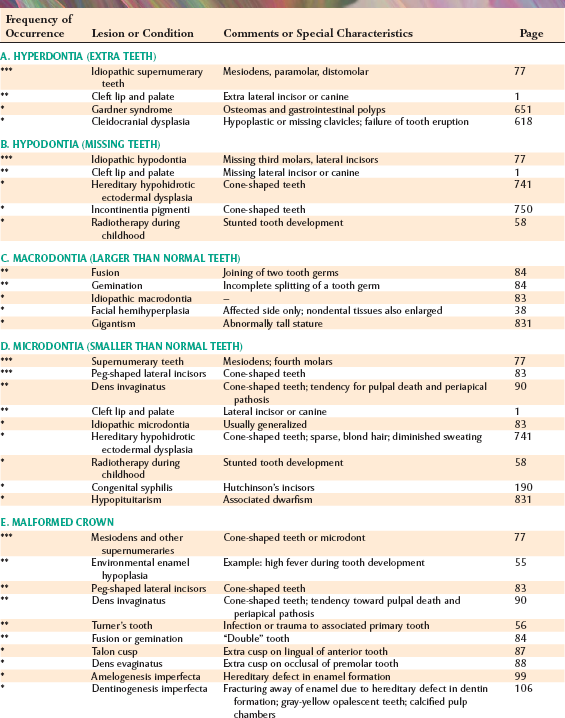
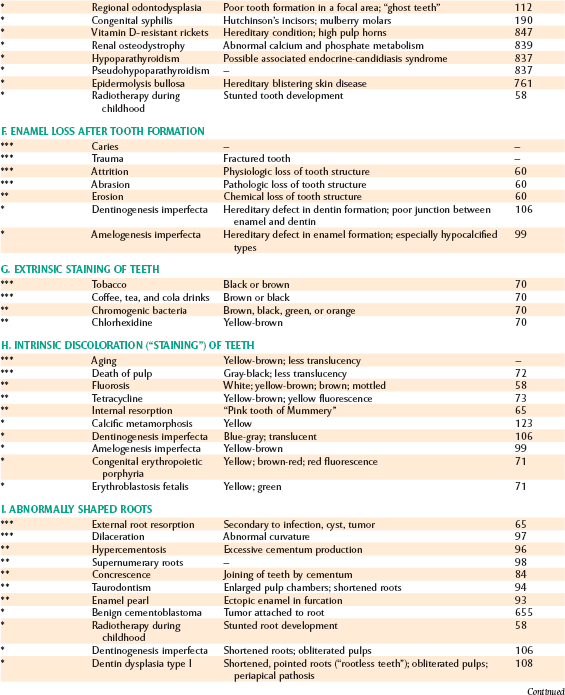
PART 5: PATHOLOGY OF TEETH
| A. Hyperdontia (Extra Teeth) | 934 |
| B. Hypodontia (Missing Teeth) | 934 |
| C. Macrodontia (Larger Than Normal Teeth) | 934 |
| D. Microdontia (Smaller Than Normal Teeth) | 934 |
| E. Malformed Crown | 934 |
| F. Enamel Loss After Tooth Formation | 935 |
| G. Extrinsic Staining of Teeth | 935 |
| H. Intrinsic Discoloration (“Staining”) of Teeth | 935 |
| I. Abnormally Shaped Roots | 935 |
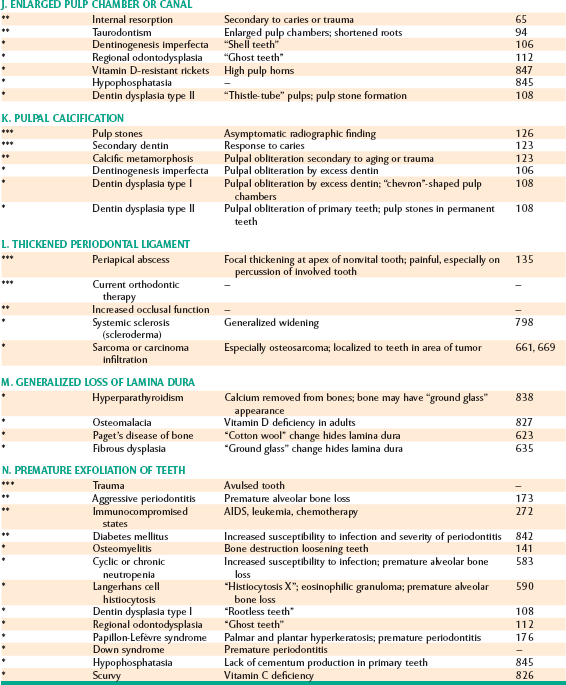
| J. Enlarged Pulp Chamber or Canal | 936 |
| K. Pulpal Calcification | 936 |
| L. Thickened Periodontal Ligament | 936 |
| M. Generalized Loss of Lamina Dura | 936 |
| N. Premature Exfoliation of Teeth | 936 |