CHAPTER 15 Vascular Distensibility and Functions of the Arterial and Venous Systems
Vascular Distensibility (p. 167)
The distensibility of the arteries allows them to accommodate the pulsatile output of the heart and average out the pressure pulsations; this provides smooth, continuous flow of blood through the small blood vessels of the tissues. Veins are even more distensible than arteries, allowing them to store large quantities of blood that can be called into use when needed. On average, veins are about eight times as distensible as arteries in the systemic circulation. In the pulmonary circulation, the distensibility of veins is similar to that of the systemic circulation. The lung’s arteries, however, are more distensible than those of the systemic circulation.
Vascular distensibility is normally expressed as follows:
Vascular compliance (capacitance) is the total quantity of blood that can be stored in a given part of the circulation for each millimeter of mercury of pressure. It is calculated as follows:
The greater the compliance of the vessel, the more easily it can be distended by pressure.
Compliance is related to distensibility as follows:
The compliance of a vein in the systemic circulation is about 24 times as great as its corresponding artery because it is about eight times as distensible and has a volume that is three times as great (8 × 3 = 24).
Sympathetic Stimulation Decreases Vascular Capacitance
Sympathetic stimulation increases smooth muscle tone in veins and arteries, causing a shift of blood to the heart, which is an important method the body uses to increase heart pumping. For example, during hemorrhage, enhanced sympathetic tone of the vessels, especially of the veins, reduces vessel size so the circulation can continue to operate almost normally even when as much as 25% of the total blood volume has been lost.
Vessels Exposed to Increased Volume at First Exhibit a Large Increase in Pressure, but Delayed Stretch of the Vessel Wall Allows the Pressure to Return toward Normal
This phenomenon is often referred to as “delayed compliance” or “stress relaxation.” Delayed compliance is a valuable mechanism by which the circulation can accommodate extra amounts of blood when necessary, such as after a transfusion that was too large. Delayed compliance in the reverse direction permits the circulation to readjust itself over a period of minutes or hours to a diminished blood volume after serious hemorrhage.
Arterial Pressure Pulsations (p. 168)
With each heartbeat a new surge of blood fills the arteries. Were it not for the distensibility of the arterial system, blood flow through the tissues would occur only during cardiac systole, with no blood flowing during diastole. The combination of distensibility of the arteries and their resistance to flow reduces the pressure pulsations to almost none by the time the blood reaches the capillaries, allowing continuous rather than pulsatile flow through the tissues.
In the young adult, the pressure at the height of each pulse, the systolic pressure, is normally about 120 mm Hg; and pressure at its lowest point, the diastolic pressure, is about 80 mm Hg. The difference between these two pressures, about 40 mm Hg, is called the pulse pressure.
The two most important factors that can increase pulse pressure are (1) increased stroke volume (the amount of blood pumped into the aorta with each heartbeat) and (2) decreased arterial compliance. Decreased arterial compliance can result when the arteries “harden” with aging (arteriosclerosis).
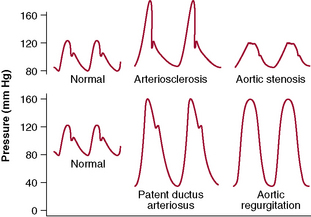
Abnormal Pressure Pulse Contours
Several other pathophysiologic conditions of the circulation can cause abnormal contours of the pressure pulse wave in addition to changing the pulse pressure (Fig. 15–1):
The Pressure Pulses Are Damped in the Smaller Vessels
Pressure pulsations in the aorta are progressively diminished (damped) by (1) the resistance to blood movement in the vessels and (2) the compliance of the vessels. The resistance damps the pulsations because a small amount of blood must flow forward to distend the next segment of the vessel; the greater the resistance, the more difficult it is for this to occur. The compliance damps the pulsation because the more compliant a vessel, the greater is quantity of blood required to cause a rise in pressure. The degree of damping of arterial pulsations is directly proportional to the product of the resistance and compliance.
Blood Pressure Can Be Measured Indirectly by the Auscultatory Method
With this method, a stethoscope is placed over a vessel, such as the antecubital artery, and a blood pressure cuff is inflated around the upper arm proximal to the vessel. So long as the cuff inflation is not sufficient to collapse the vessel, no sounds are heard with the stethoscope despite the fact that blood in the artery is pulsing. When the cuff pressure is sufficient to close the artery during part of the arterial pressure cycle, a sound is heard with each pulsation; these sounds are called Korotkoff sounds.
When determining blood pressure by the auscultatory method, pressure in the cuff is first inflated well above the arterial systolic pressure. So long as the pressure is higher than the systolic pressure, the brachial artery remains collapsed and no blood jets into the lower artery during the cardiac cycle; therefore, no Korotkoff sounds are heard in the lower artery. As soon as the pressure in the cuff falls below the systolic pressure, blood slips through the artery underneath the cuff during the peak systolic pressure, and one begins to hear tapping sounds in the antecubital artery in synchrony with the heartbeat. As soon as these sounds are heard, the pressure level indicated by the manometer connected to the cuff is about equal to the systolic pressure.
As pressure in the cuff is further lowered, the Korotkoff sounds change in quality, having a rhythmical, harsher sound. Finally, when the pressure in the cuff falls to the level of the diastolic pressure (the artery no longer closes during diastole), the sounds suddenly change to a muffled quality and then usually disappear entirely after another 5- to 10-millimeter drop in cuff pressure. When the Korotkoff sounds change to the muffled quality, the manometer pressure is about equal to the diastolic pressure, although this slightly overestimates the diastolic pressure. Many clinicians believe that the pressure at which the Korotkoff sounds completely disappear should be used as the diastolic pressure except in situations in which the disappearance of sounds cannot reliably be determined because sounds are audible even after complete deflation of the cuff. For example, in patients with arteriovenous fistulas for hemodialysis or with aortic insufficiency, Korotkoff sounds may be heard after complete deflation of the cuff.
The mean arterial pressure can be estimated from the systolic and diastolic pressures measured by the auscultatory method as follows:
For the average young adult, the mean arterial pressure is about ( × 80 mm Hg) (
× 80 mm Hg) ( × 120 mm Hg), or 93.3 mm Hg.
× 120 mm Hg), or 93.3 mm Hg.
Veins and Their Function (p. 171)
The veins, as discussed previously, are capable of constricting and enlarging and thereby storing either small or large quantities of blood, making this blood available when it is needed by the remainder of the circulation. Veins can also propel blood forward by means of a “venous pump,” and they help regulate cardiac output.
Venous Pressure: Relationship to Right Atrial Pressure (Central Venous Pressure) and Peripheral Venous Pressure
Because blood from systemic veins flows into the right atrium, anything that affects the right atrial pressure usually affects venous pressure everywhere in the body. Right atrial pressure is regulated by a balance between the ability of the heart to pump blood out of the right atrium and a tendency of blood to flow from the peripheral vessels back to the right atrium.
The normal right atrial pressure is about 0 mm Hg, but it can rise to as high as 20 to 30 mm Hg under abnormal conditions, such as with serious heart failure or after massive transfusion.
Increased Venous Resistance Can Increase the Peripheral Venous Pressure
When large veins are distended, they offer little resistance to blood flow. Many of the large veins entering the thorax are compressed by the surrounding tissues, however, so they are at least partially collapsed or collapsed to an ovoid state. For these reasons, large veins usually offer significant resistance to blood flow, and the pressure in the peripheral veins is usually 4 to 7 mm Hg higher than the right atrial pressure. Partial obstruction of a large vein markedly increases the peripheral venous pressure distal to the obstruction.
Increased Right Atrial Pressure Increases Peripheral Venous Pressure
When the right atrial pressure rises above its normal state of 0 mm Hg, blood begins to back up in large veins and open them up. Pressures in the peripheral veins do not rise until the collapsed points between the peripheral veins and the large central veins have opened, which usually occurs at a right atrial pressure of about 4 to 6 mm Hg. When the right atrial pressure rises still further, as occurs during severe heart failure, it causes a corresponding rise in peripheral venous pressure.
Gravitational Pressure Affects Venous Pressure
The pressure at the surface of a body of water exposed to air is equal to the atmospheric pressure, but the pressure rises 1 mm Hg for each 13.6 mm Hg distance below the surface. This pressure results from the weight of the water and therefore is called gravitational hydrostatic pressure.
Gravitational hydrostatic pressure also occurs in the vascular system because of the weight of the blood in the vessels. In an adult who is standing absolutely still, pressure in the veins of the feet is approximately +90 mm Hg because of the hydrostatic weight of the blood in the veins between the heart and feet.
The Venous Valves and “Venous Pump” Influence Venous Pressure
Were it not for the valves of the veins, the gravitational pressure effect would cause venous pressure in the feet to always be about +90 mm Hg in a standing adult. Each time one tightens the muscles and moves the legs, however, it compresses the veins either in the muscles or adjacent to them and squeezes the blood out of the veins.
The valves in the veins are arranged so the direction of blood flow can only be toward the heart. Consequently, each time a person moves the legs or tenses the muscles, a certain amount of blood is propelled toward the heart, and the pressure in the veins is lowered. This pumping system is known as the “venous pump” or “muscle pump,” and it keeps the venous pressure in the feet of a walking adult near 25 mm Hg.
If a person stands perfectly still, however, the venous pump does not work, and venous pressure quickly rises to the full hydrostatic value of 90 mm Hg. If the valves of the venous system become incompetent or are destroyed, the effectiveness of the venous pump is also decreased. When valve incompetence develops, greater pressure in the veins of the legs may further increase the size of the veins and finally destroy the function of the valves entirely. When this occurs, the person develops varicose veins, and the venous and capillary pressures increase to high levels, causing leakage of fluid from the capillaries and edema in the legs when standing.
The Veins Function as Blood Reservoirs
More than 60% of the blood in the circulatory system is usually contained in the veins. For this reason and because the veins are so compliant, the venous system can serve as a blood reservoir for the circulation. For example, when blood is lost from the body, activation of the sympathetic nervous system causes the veins to constrict, which takes up much of the “slack” of the circulatory system caused by the lost blood.
Certain portions of the circulatory system are so compliant they are especially important as blood reservoirs. These areas include (1) the spleen, which can sometimes decrease in size to release as much as 100 mL of blood into the reservoir of the circulation; (2) the liver, the sinuses of which can release several hundred milliliters of blood into the rest of the circulation; (3) the large abdominal veins, which can contribute as much as 300 mL; and (4) the venous plexus underneath the skin, which can contribute several hundred milliliters.