24 Alopecia X in a Pomeranian
INTRODUCTION
Symmetrical, truncal, non-inflammatory alopecia can occur for a number of different reasons, including follicular dysplasias and endocrinopathies. The most common endocrinopathies resulting in these symptoms are hypothyroidism and hyperadrenocorticism. There is a form of alopecia that occurs in plush-coated Nordic breeds characterized by bilaterally symmetrical, non-inflammatory alopecia with hyperpigmentation. The exact aetiology is not known and the condition has been designated ‘alopecia X’. This case report describes a case of alopecia X in a Pomeranian.
CASE HISTORY
The history in cases of alopecia X is of gradual, progressive onset of alopecia without systemic signs. There may be a history of hair regrowth over skin scrape, biopsy or other surgical sites.
The history in this case was as follows:
CLINICAL EXAMINATION
There were no abnormalities on full physical examination.
CASE WORK-UP
As with any case of alopecia, skin scrapes should be performed to rule out demodicosis. Routine haematological and biochemical examinations and further tests for hyperadrenocorticism and hypothyroidism were also indicated. In addition to a standard ACTH stimulation test measuring pre- and post-ACTH cortisol concentrations, the same test, measuring pre- and post-17-hydroxy-progesterone concentrations, has been used as an indicator of adrenal dysfunction. Post-ACTH 17-hydroxy-progesterone concentrations are frequently elevated in cases of alopecia X. Histopathological examination is unlikely to give a definitive diagnosis in a case of alopecia due to an endocrinopathy but would be helpful in ruling out other causes of hair loss.
The following diagnostic tests were performed:
DIAGNOSIS
The history, clinical signs and results of laboratory tests were consistent with a diagnosis of alopecia X.
PROGNOSIS
Alopecia X is a benign, essentially cosmetic, condition. There are no reported cases with severe systemic involvement. If left untreated, the hair loss can progress to involve the entire trunk but will spare the head and legs. There are treatment options that seem to be effective in inducing hair regrowth, although hair loss may recur after apparently successful therapy.
AETIOLOGICAL AND PATHOPHYSIOLOGICAL ASPECTS OF ALOPECIA X
The control of hair growth is complex and poorly understood but is influenced by many extrinsic and intrinsic growth factors. Extrinsic factors include hormones, neuropeptides and signals from immunologically active cells. Intrinsic factors include hormones working in a paracrine or autocrine fashion, cytokines and growth factors, neuropeptides, adhesion molecules and enzymes.
The aetiopathogenesis of alopecia X remains obscure. The controversial name was coined 10 years ago to encompass a number of clinical entities, affecting mainly the plush-coated breeds, with a similar clinical picture and named according to endocrinological abnormalities and/or response to various treatment regimes. These conditions include congenital adrenal hyperplasia-like syndrome, pseudo-Cushing’s syndrome, growth hormone-responsive alopecia, castration-responsive dermatosis and black skin disease of Pomeranians, amongst many others.
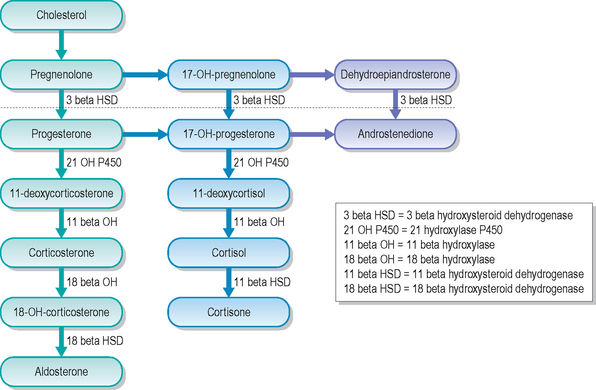
There have been various hypotheses put forward as to the cause of the hair loss in alopecia X, including a genetic predisposition to a hormone imbalance and/or a defect in hair follicle receptors, that seem to vary according to the breed involved. A deficiency of the steroidogenesis hormone, 21-hydroxylase, leading to an increase in the concentration of progesterone (Fig. 24.4), has been postulated to be a factor in the pathogenesis of alopecia X. This abnormality has been demonstrated in poodles, Pomeranians and Alaskan malamutes. There is also evidence that dogs with alopecia X have some increase in cortisol production. These factors are behind the rationale of treating alopecia X with trilostane. However, the significance of these apparent abnormalities in corticosteroid and sex hormone concentrations in relation to the alopecia is still in some doubt, as sex hormone concentrations did not return to the expected reference range concentrations in dogs with alopecia X successfully treated with either melatonin or mitotane. To date, although breed-specific hormonal abnormalities have been demonstrated (i.e. Pomeranians and Alaskan malamutes), these abnormalities do not consistently affect other plush-coated breeds affected by alopecia X, and no consistent hormonal abnormalities have been demonstrated in breeds such as the chow-chow and samoyed. Based on the results of one study, there is no single hormonal abnormality associated with the hair loss in alopecia X and it might be better to consider this condition to be one of hair follicle arrest rather than equating it with an adrenal hormone imbalance. Thus, at the time of writing, work still needs to be done to establish the aetiology of this condition.
EPIDEMIOLOGY
Alopecia X has been recognized most frequently in the plush-coated breeds, including Pomeranians, samoyeds, malamutes, huskies, chow-chows and keeshonds. Miniature poodles are also predisposed. Any age of dog can be affected, from early adulthood to 11 years of age. It is seen more frequently in neutered dogs.
TREATMENT OPTIONS
As this is a cosmetic condition with no serious systemic effects, some owners may decline treatment after counselling; however, there are numerous treatment options which may result in some hair regrowth.
Neutering: Neutering results in hair regrowth in some intact male and female animals, and should be considered as the first-line treatment.
Melatonin: In neutered animals, for reasons of cost and safety, melatonin is now considered the treatment of choice by most veterinary dermatologists. At the time of writing, in the USA, melatonin is considered to be a food supplement and is available over the counter. However, in the UK it is considered a drug; it is therefore an unlicensed product and its import is subject to restrictions. Work still needs to be done to optimize dosage and duration of treatment, but oral melatonin, at the rate of 3 mg/dog (b.i.d. or t.i.d.) for up to 3 months, is commonly used to treat alopecia X. Around one-third of cases can be expected to exhibit hair regrowth with this treatment.
Mitotane: Mitotane causes necrosis and atrophy of the adrenal cortex and, prior to licensing of trilostane, was routinely used for the treatment of hyperadrenocorticism. Mitotane has also been used successfully for the treatment of alopecia X, although this is a potent and unlicensed therapy.
Trilostane: More recently, there have been reports that trilostane, a competitive inhibitor of 3β-hydroxysteroid dehydrogenase which interferes with adrenal steroidogenesis, has resulted in hair regrowth in affected Pomeranians, miniature poodles and Alaskan malamutes. This is a treatment that has been shown to be effective in cases of spontaneous hyperadrenocorticism.
Treatment in this case: The owner was particularly keen to try further treatment and, as there had been no response to melatonin, the decision was made to start treatment with trilostane.
The initial dosage of trilostane administered was 3.5 mg/kg s.i.d. with food.
The protocol for measuring 17-hydroxy-progesterone before and after ACTH injection is the same as that used for cortisol assessment, and the same samples may be used for measurement of both hormones. If in doubt, contact your laboratory for confirmation of the protocol before you start. Blood samples should be spun down and the serum separated off, prior to sending it to the laboratory. It is not advisable to send samples for endocrine analysis in serum gel tubes as this can affect results.
The hair regrowth over the spay site is typical of alopecia X. Hair regrowth frequently occurs where there has been any minor trauma, including biopsy and skin scraping sites; the reason for this is uncertain but the trauma must result in some localized stimulation of hair follicles, possibly via release of cytokines, growth factors or other signalling molecules.
Similar histopathological abnormalities are found in most of the endocrine-type alopecias and therefore histopathology should not be relied upon to make a specific diagnosis. It is important in cases of suspected endocrine alopecia to take samples from the areas of the most advanced alopecia and, as usual, to take multiple samples.
FOLLOW-UP
Routine monitoring of this case involved re-examination at 10 days, 4 weeks, 3 months and every 3 months thereafter for routine biochemistry and repeat ACTH stimulation tests.
There were no abnormalities on any of the serum biochemical examinations.
After 10 days’ treatment with trilostane, pre- and post-ACTH cortisol concentrations were 134 and 375 nmol/l respectively, and the dosage of trilostane was increased to 7 mg/kg s.i.d.
Within 4 weeks of increasing the dosage of trilostane, there was some evidence of hair regrowth.
After 4 months of therapy, there was almost complete regrowth of hair, although some thinning of secondary hairs remained.
After 7 months of continuous trilostane treatment, hair regrowth was considered acceptable by the owner (Figs 24.5, 24.6 and 24.7) and the trilostance dosage was reduced to 7 mg/kg given on alternate days.
On re-inspection 6 weeks later, patches of alopecia had developed over the neck and caudal dorsum, and the trilostane dosage was once again increased to 7 mg/kg s.i.d. At the time of writing, the response to the increased trilostane dosage is not known.