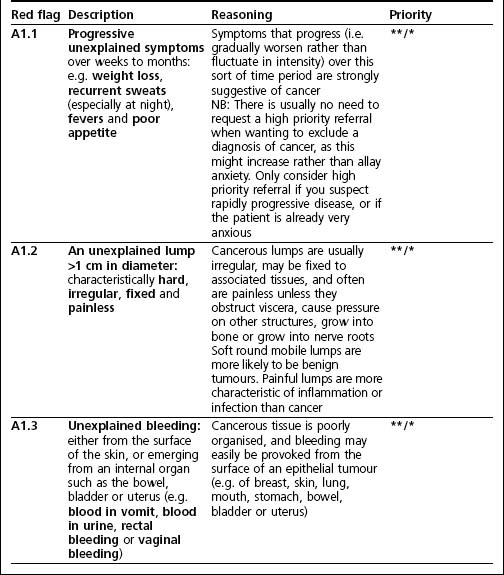
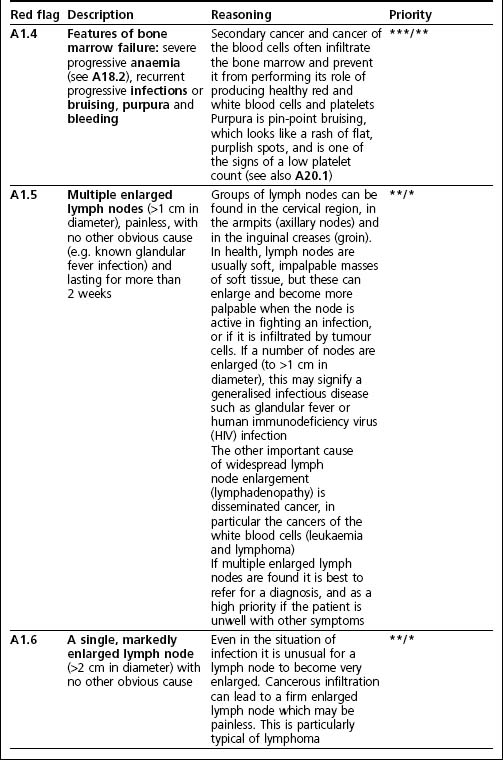
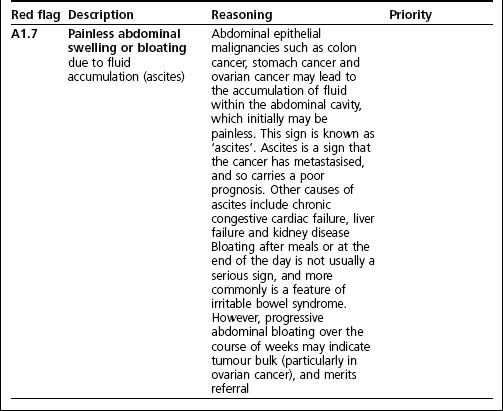
Chapter 2 A tables
Red flags ordered by physiological system
Introduction
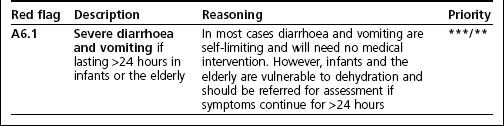
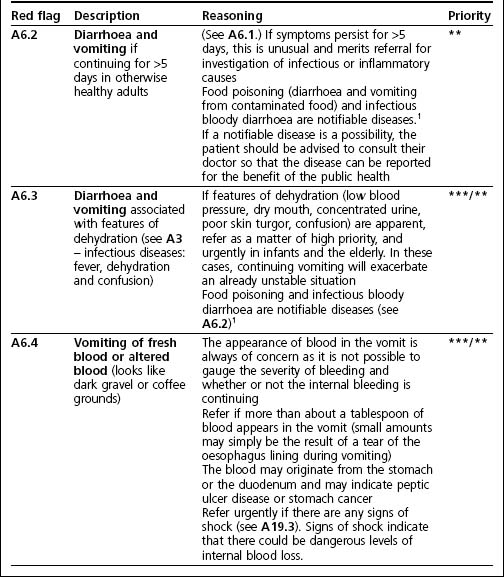
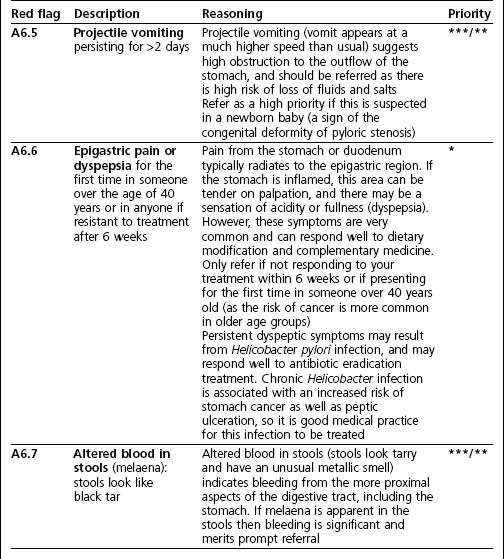
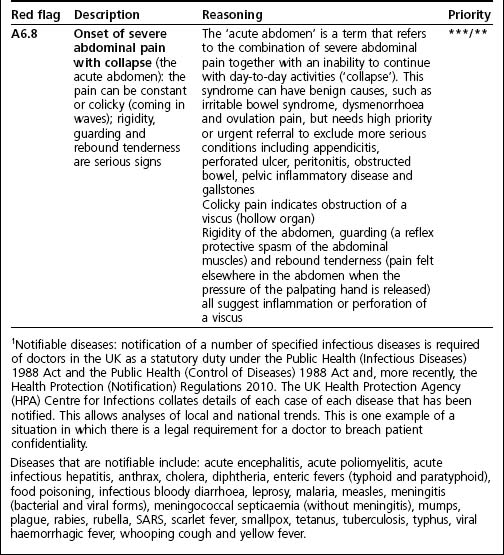
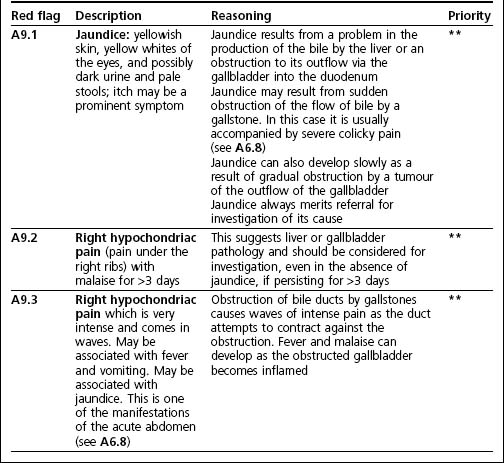
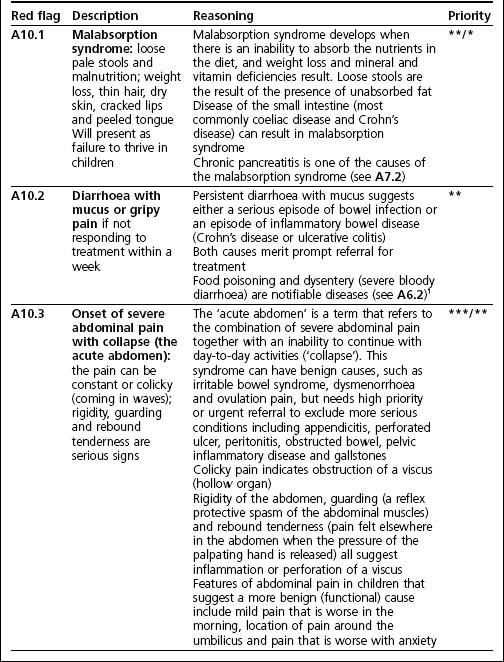
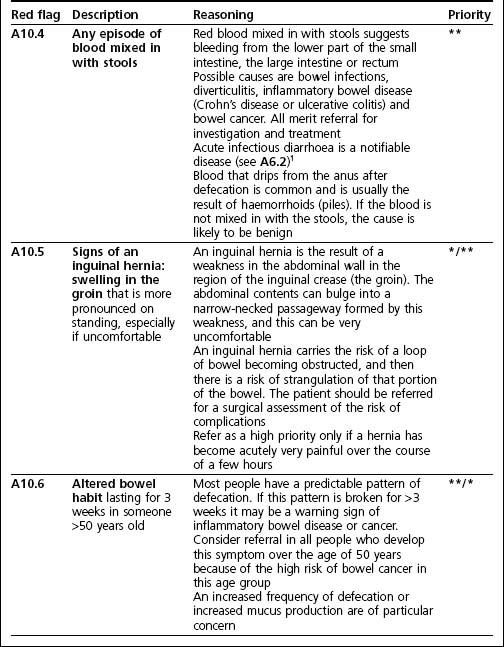
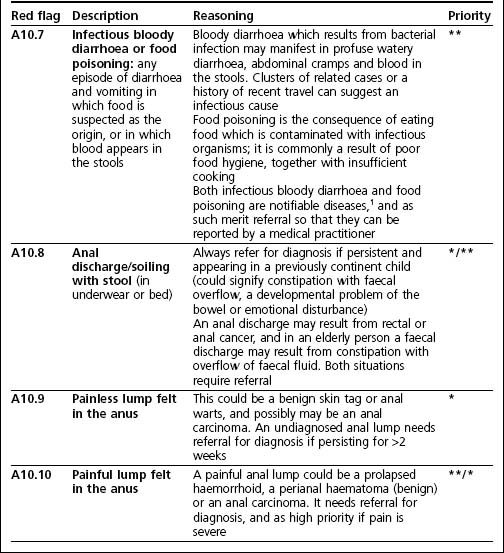
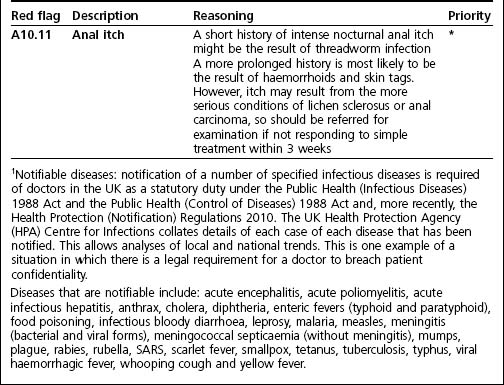
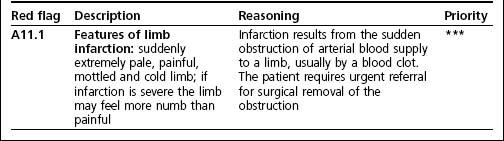
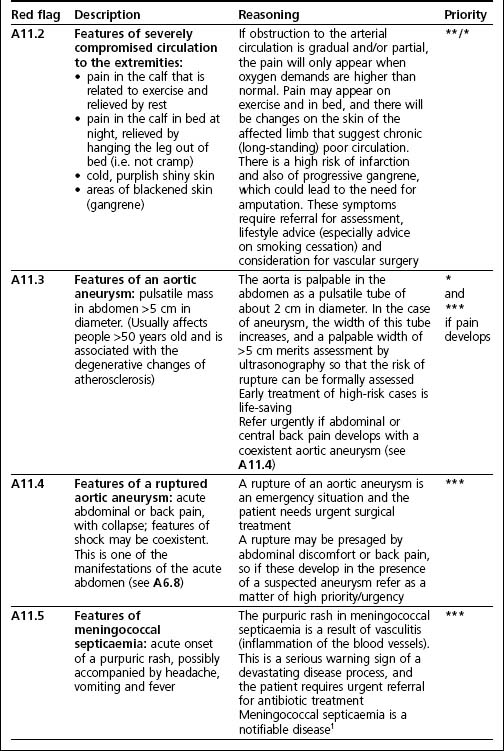
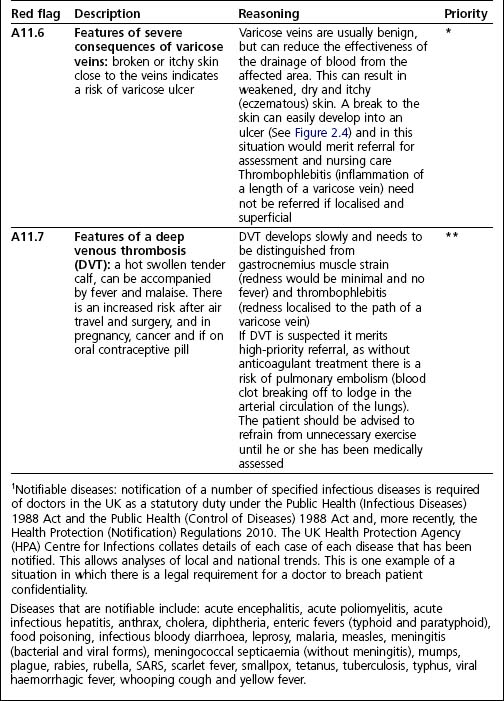
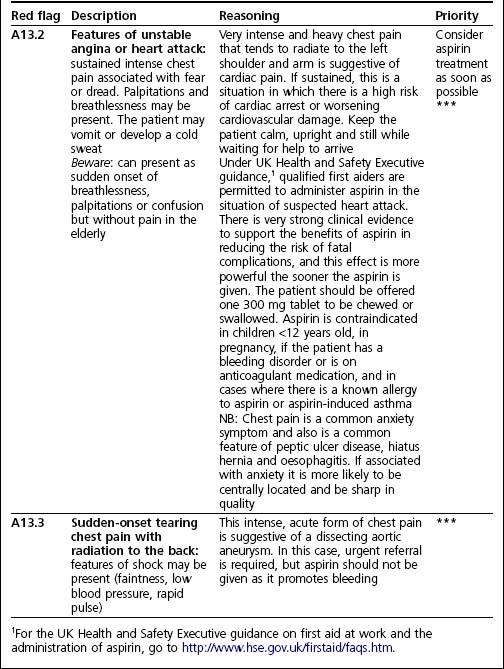
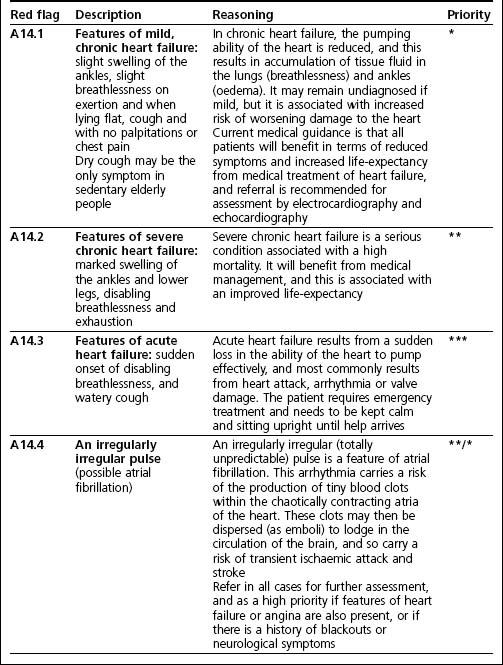
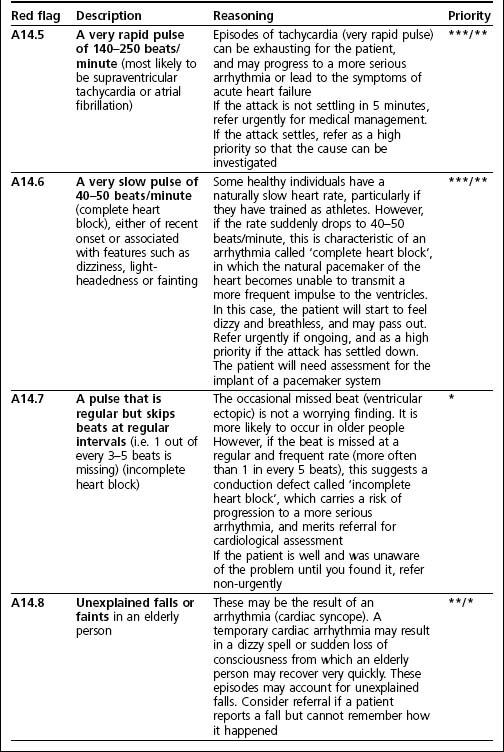
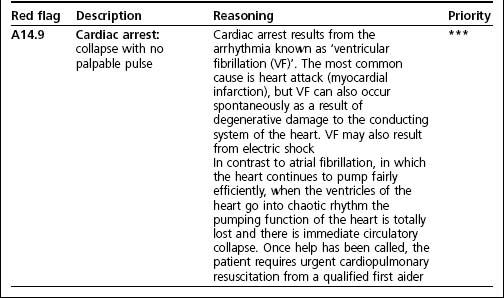
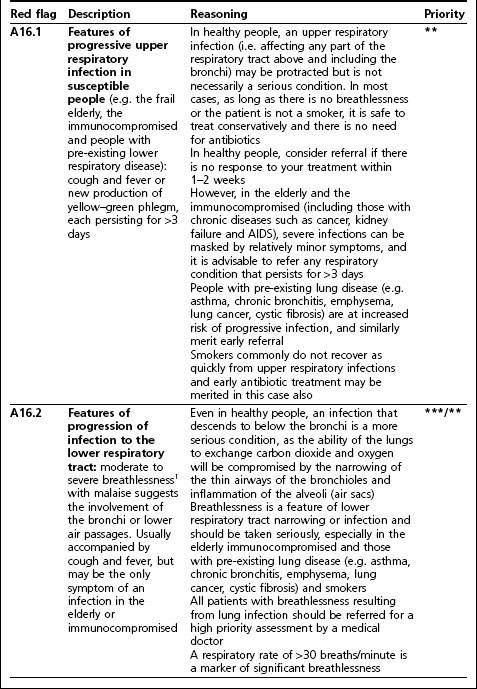
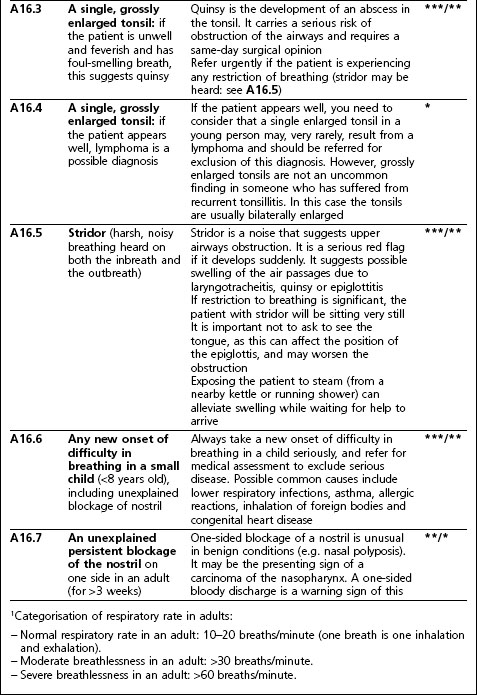
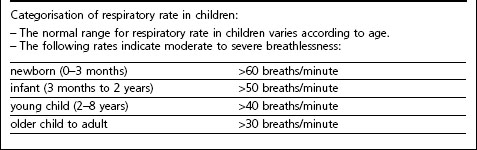
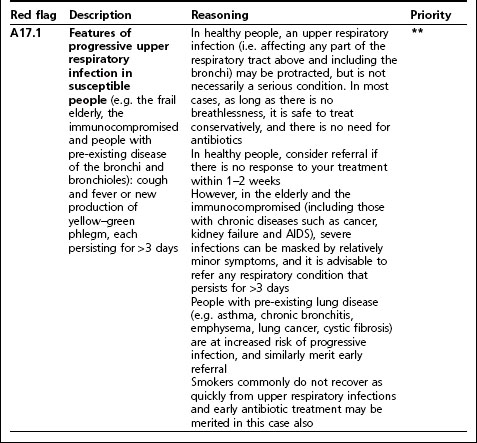
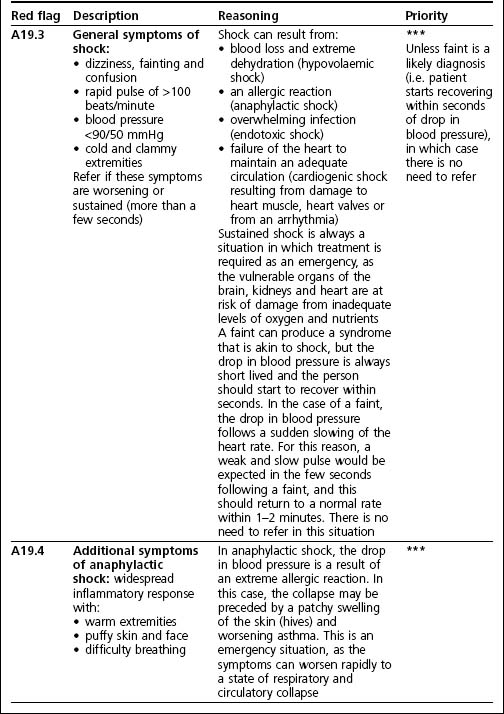
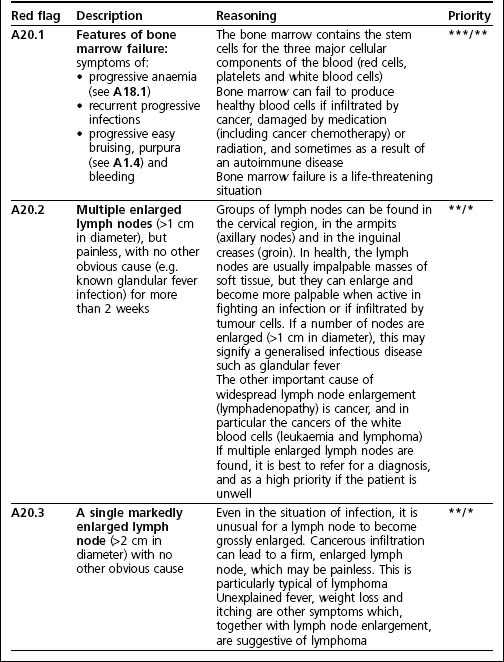
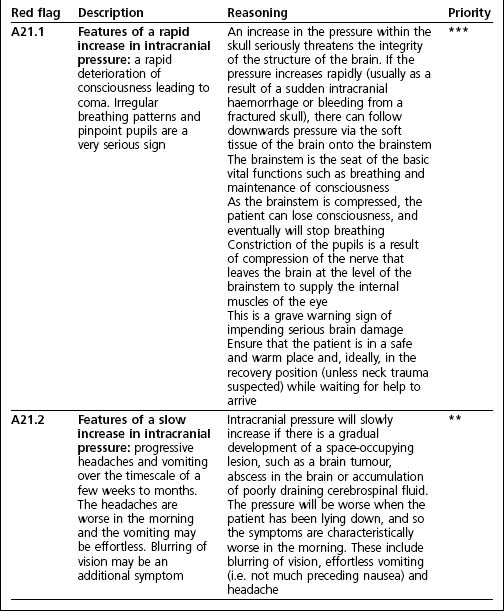
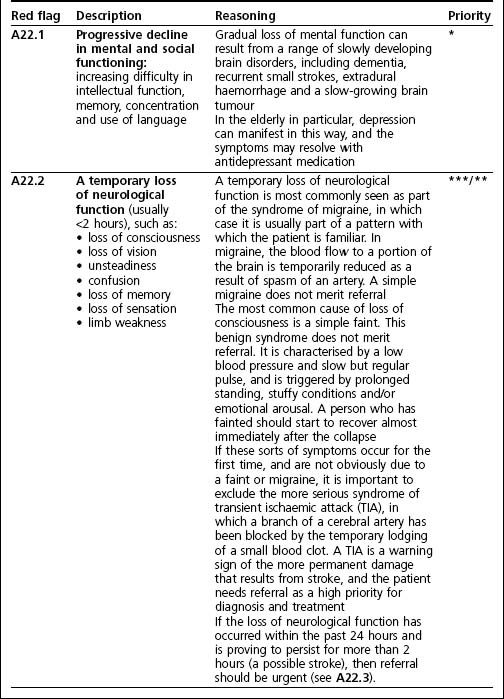
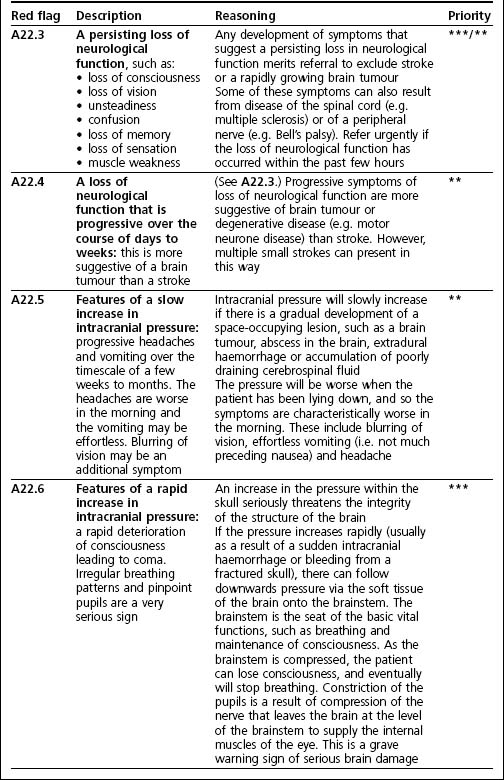
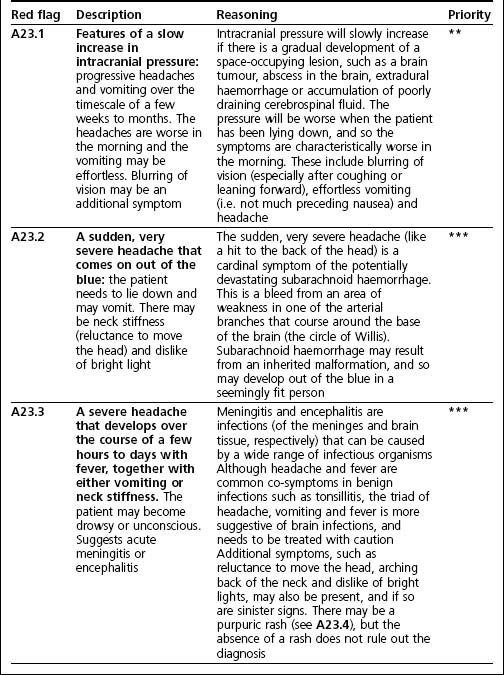
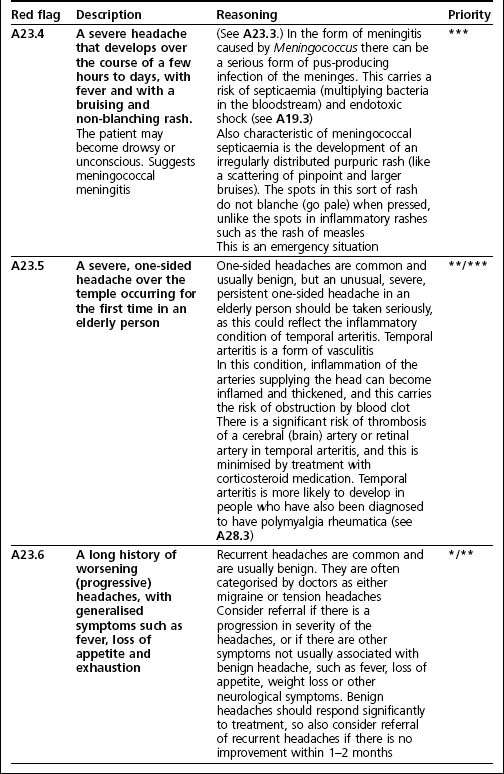
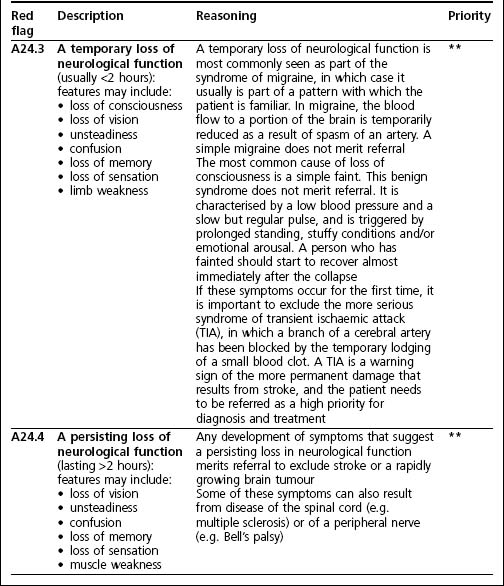
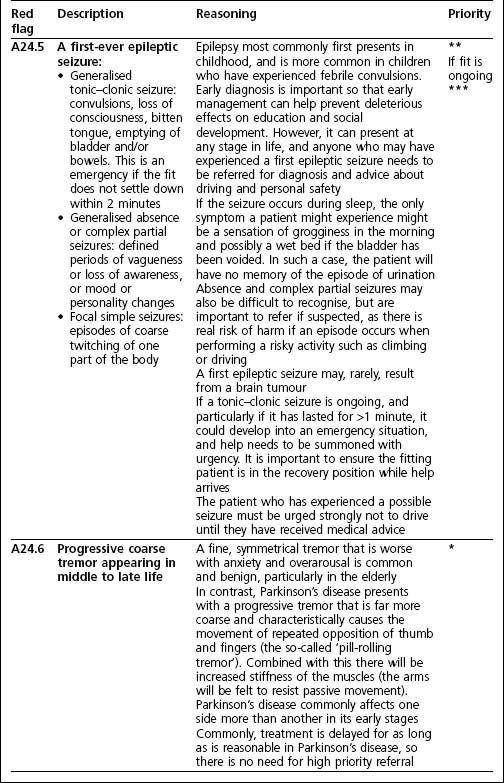
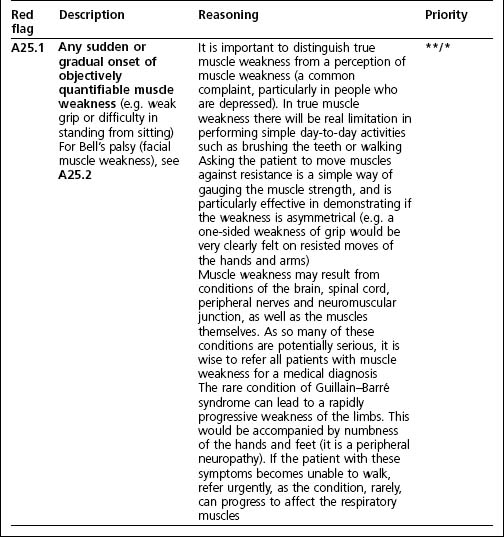
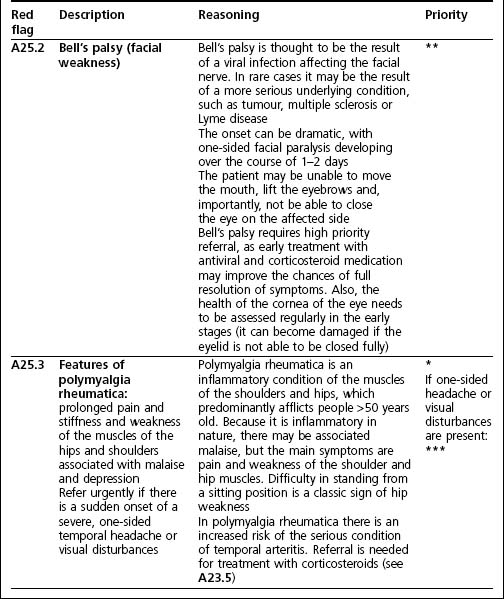
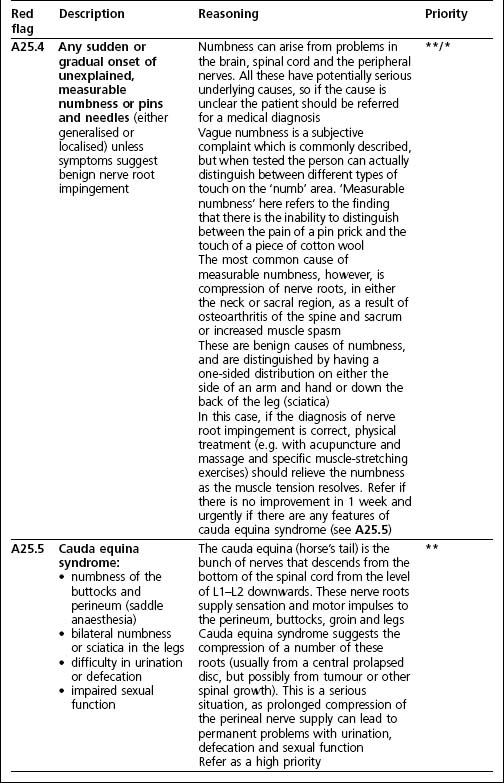
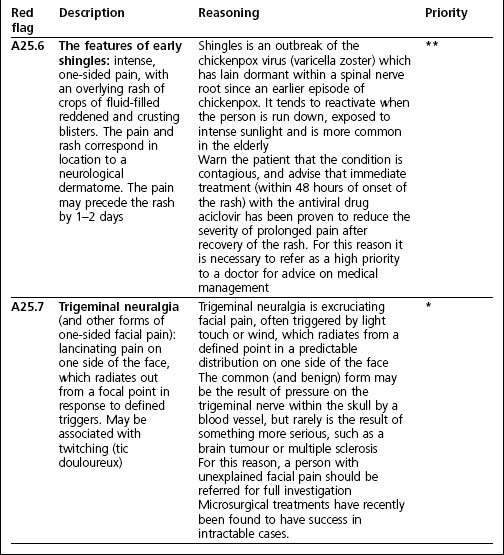
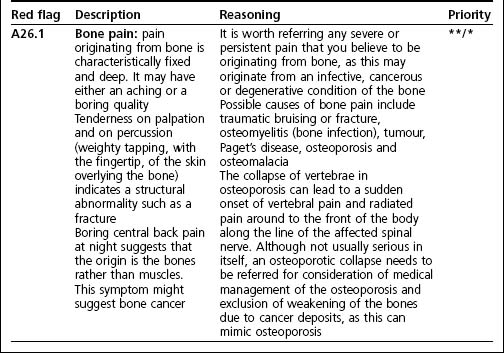
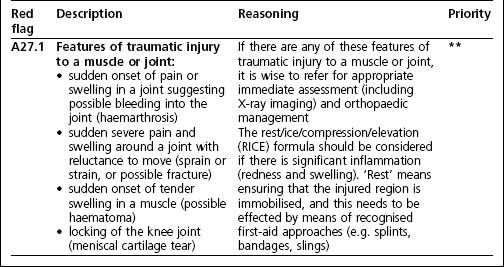
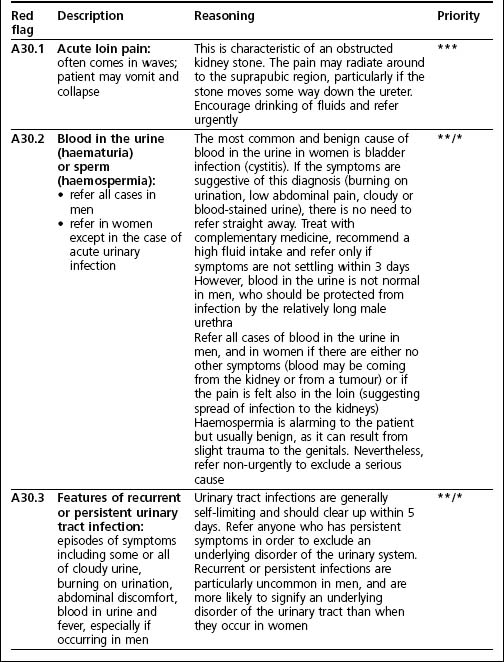
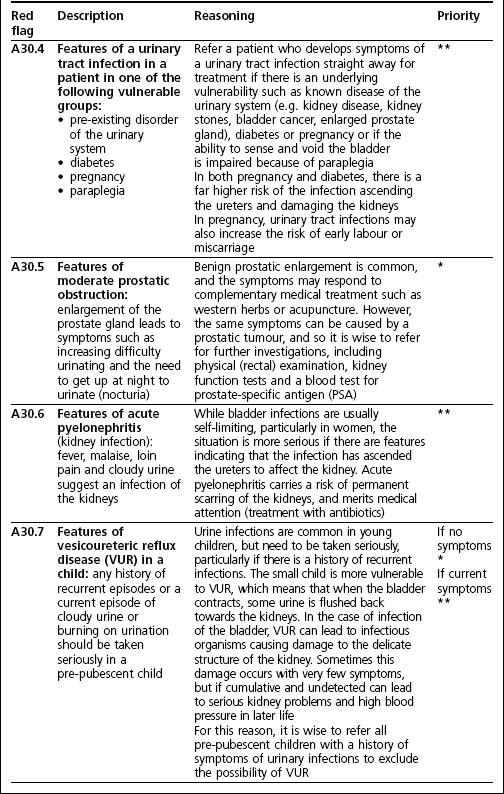
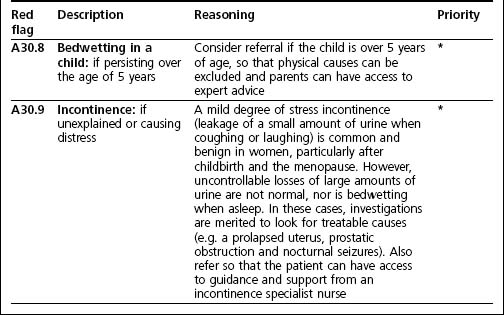
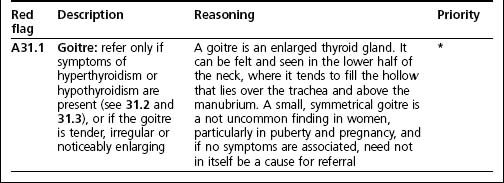
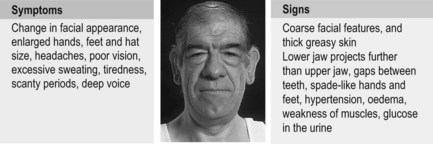
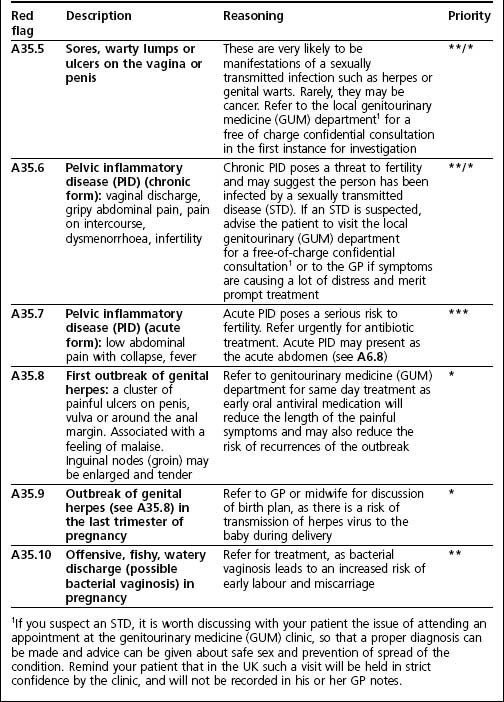
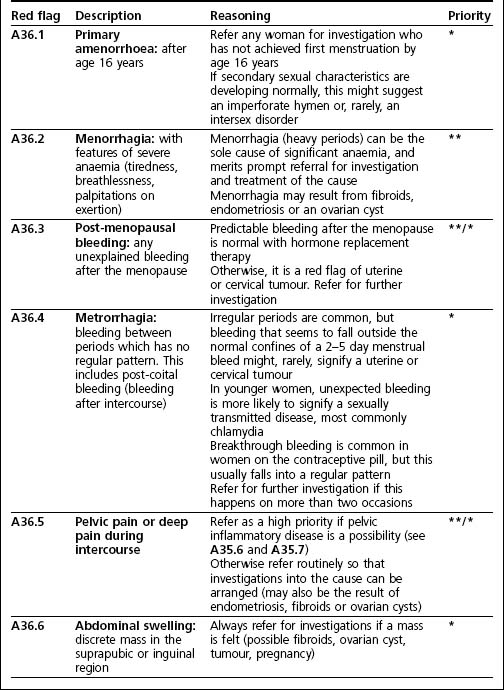
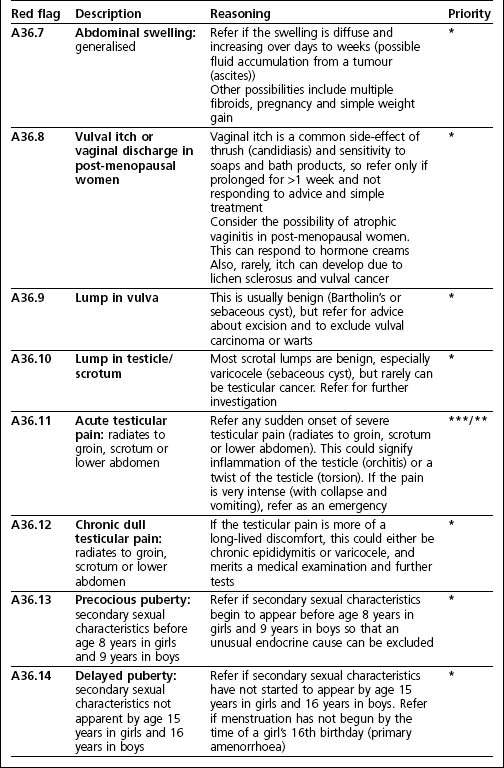
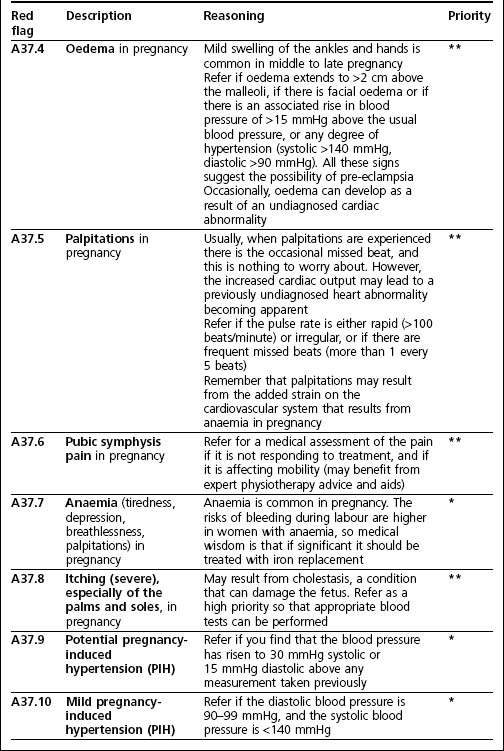
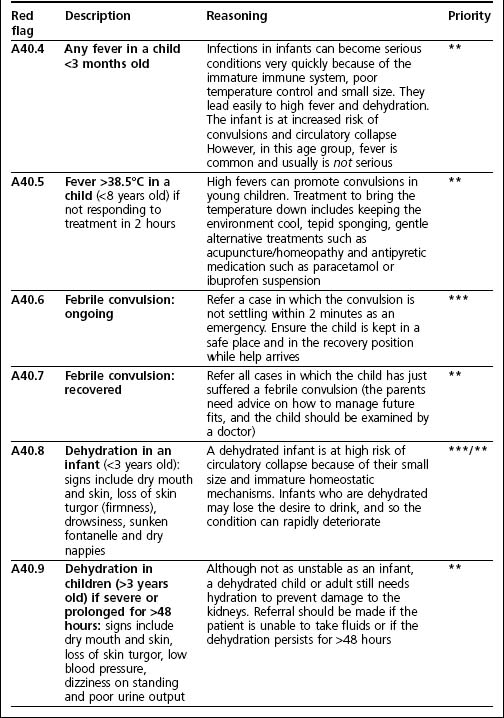
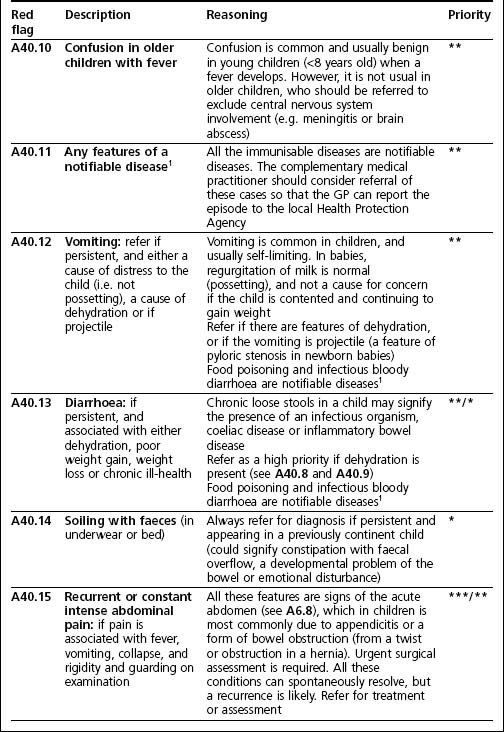
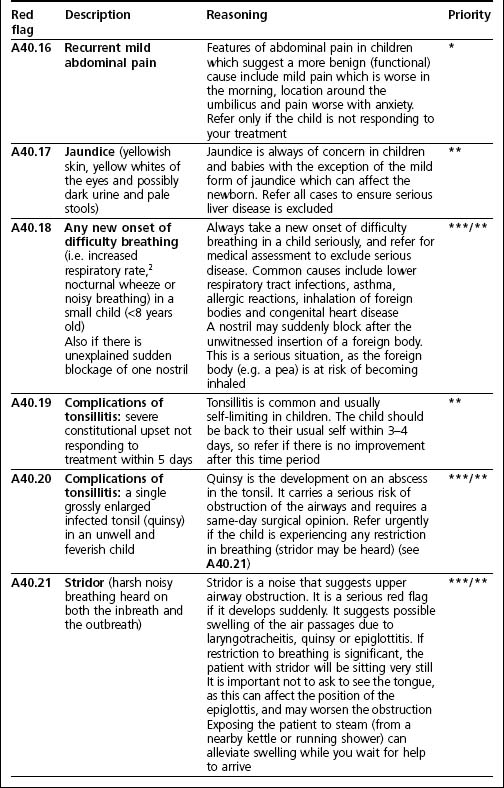
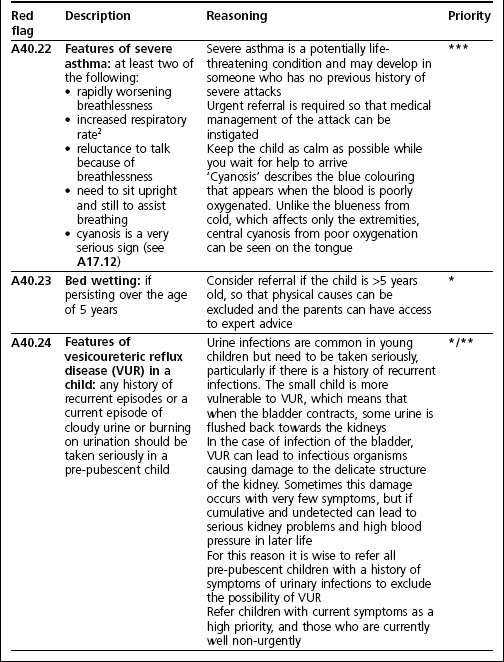
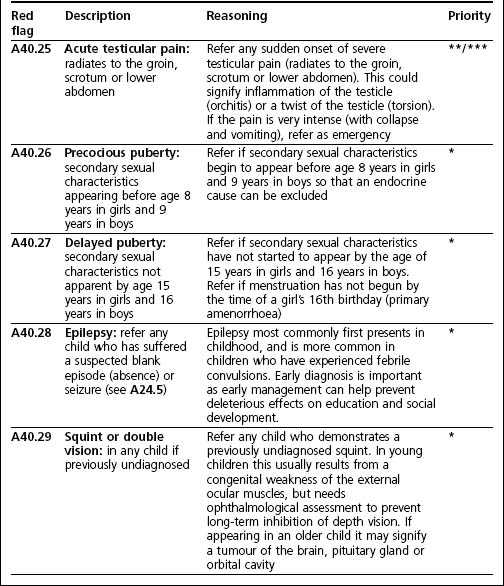
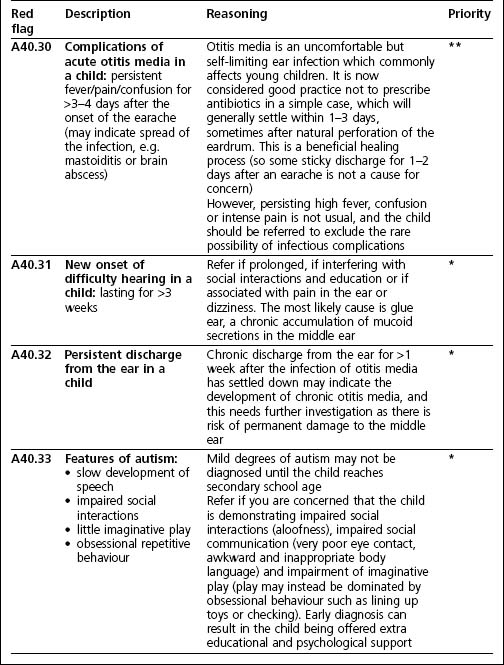
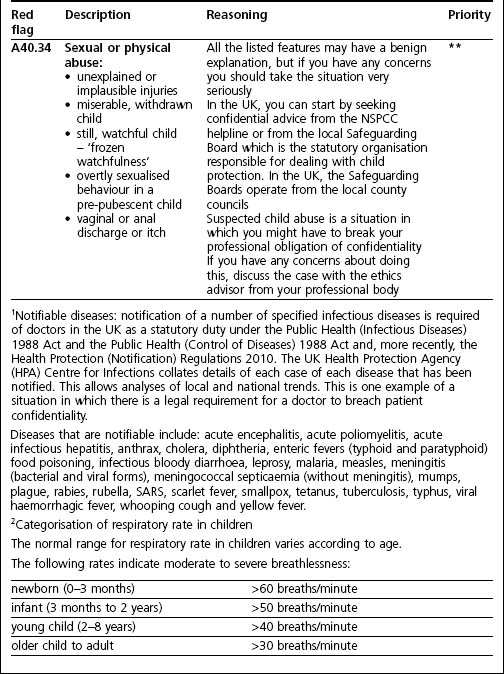
These A tables are ordered according to the physiological systems of the body. Each A table lists the red flags which are related to disease of that physiological system. The red flags are defined according to symptoms (the patient’s experience of disease) and/or signs (measurable physiological changes of disease). These tables also offer a brief explanation as to why the constellation of symptoms and signs constitute a red flag. These tables are introduced and explained in more depth in the relevant chapters of the companion text The Complementary Therapist’s Guide to Clinical Medicine to which the readers are referred should they wish to study these patterns of disease in more depth.
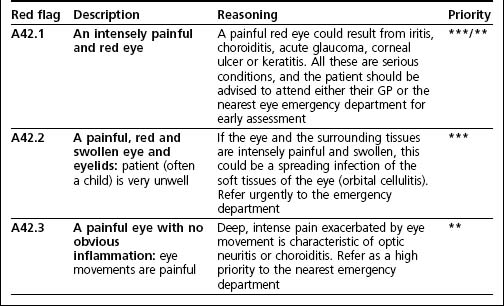
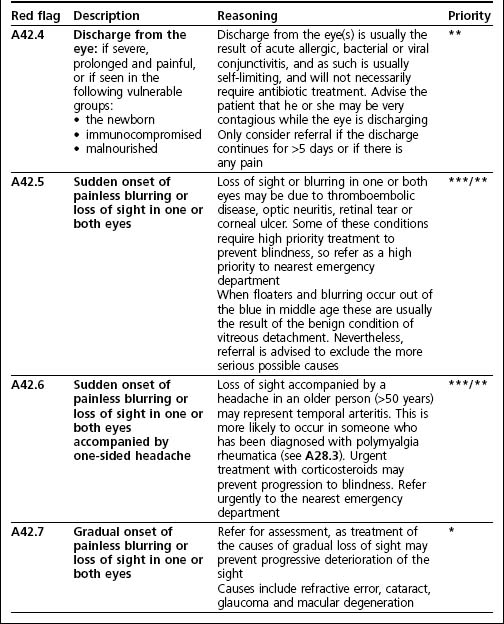
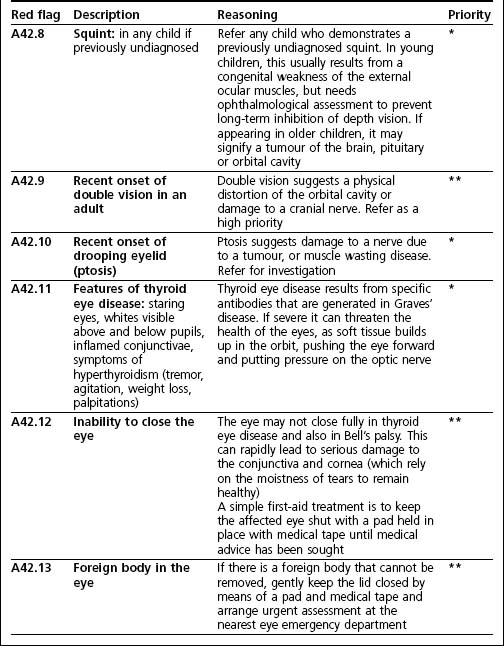
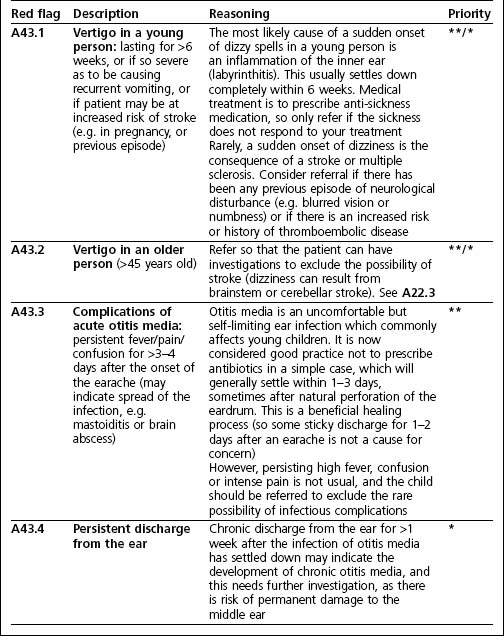
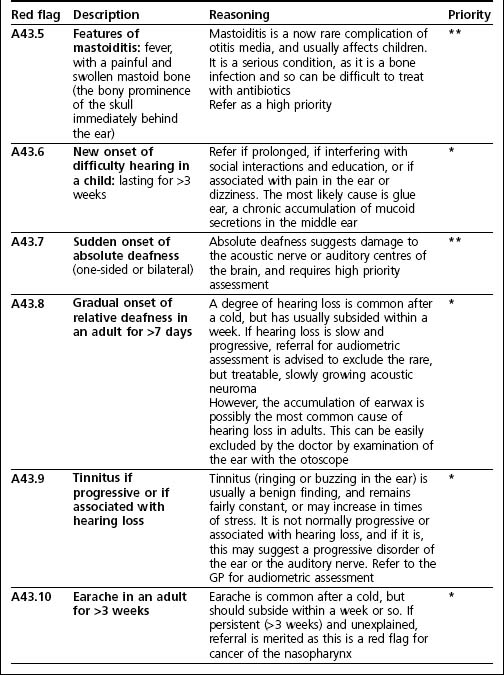
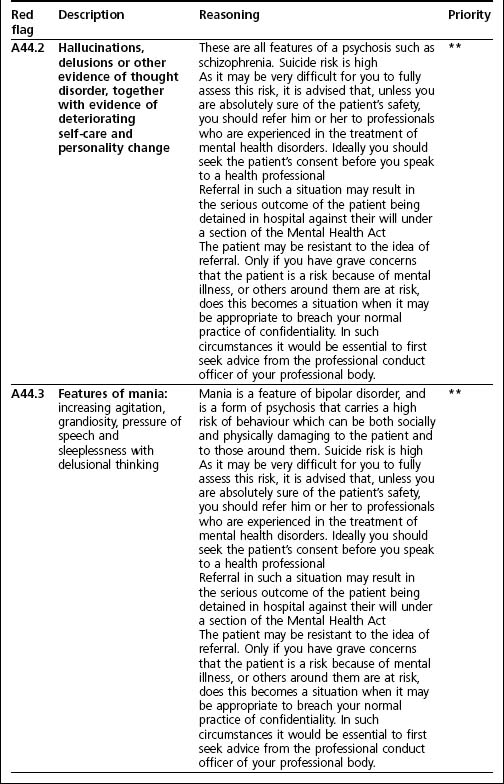
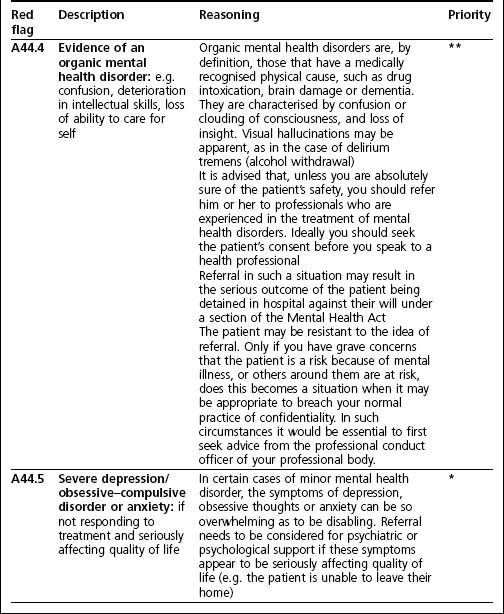
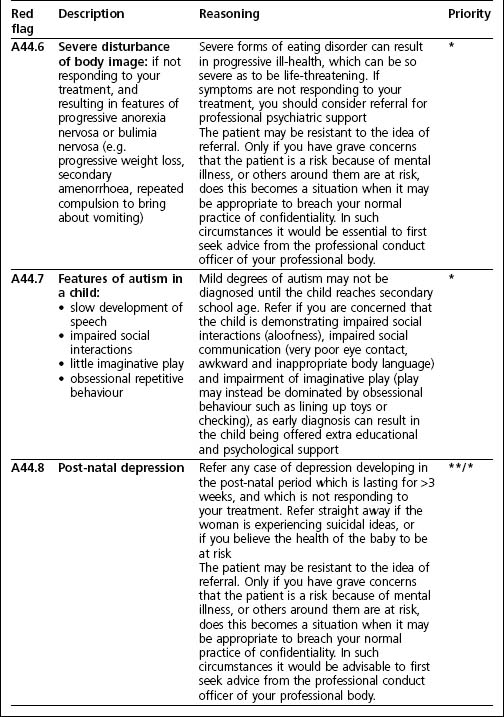
The A tables show the categorisation of urgency of referral which is described in Chapter 1:
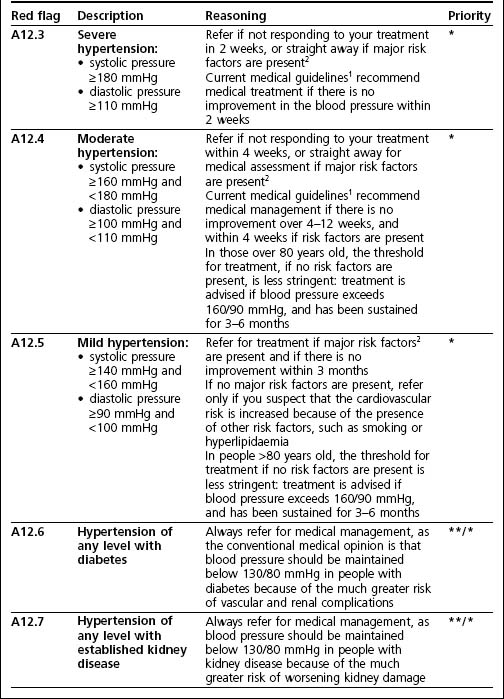
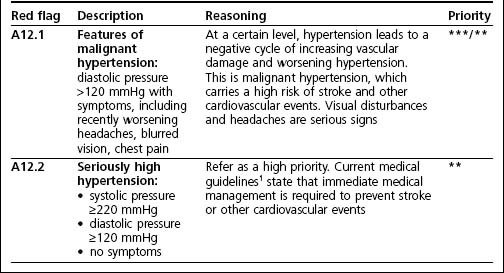
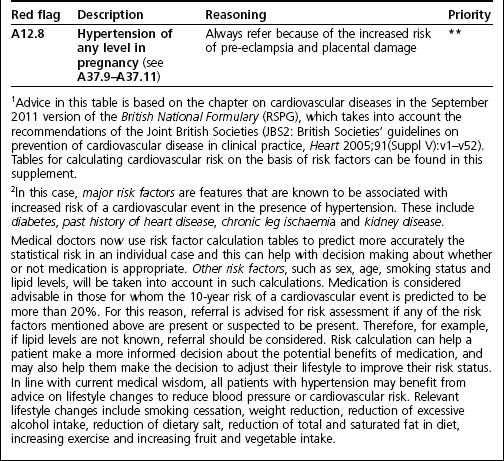
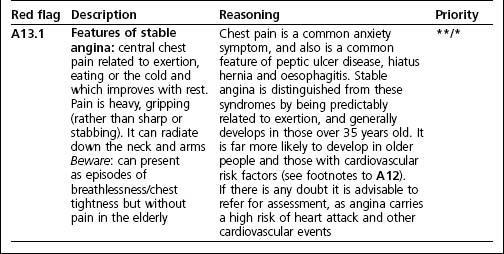
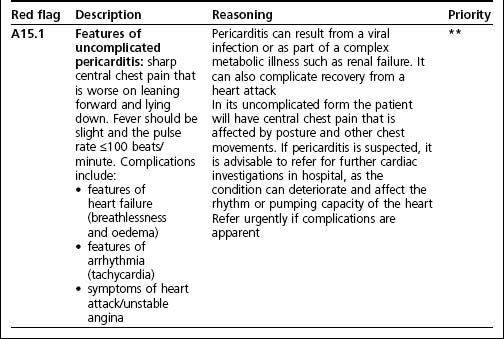
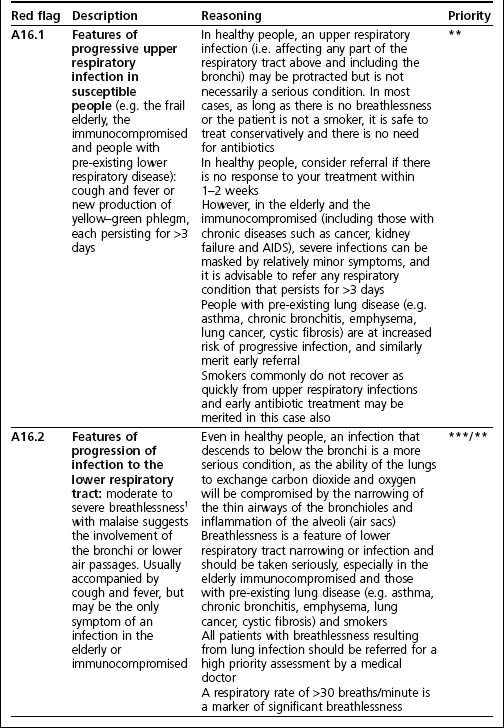
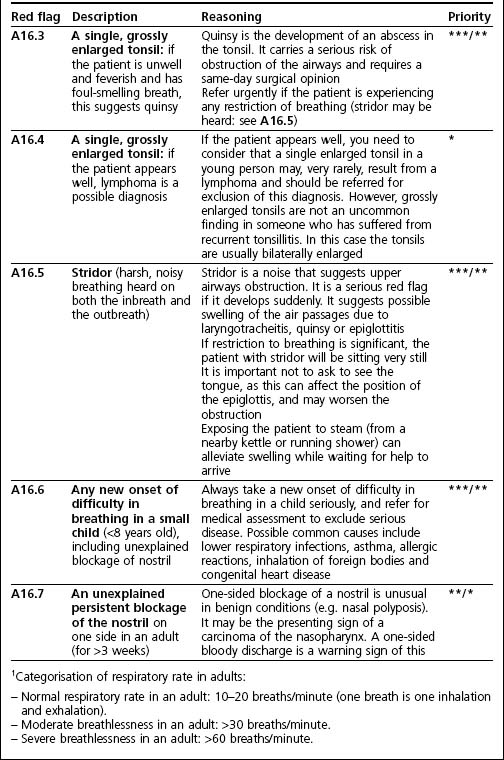
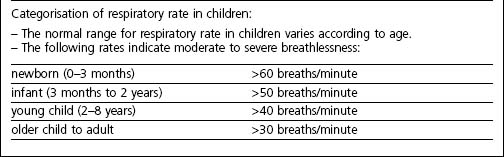
*Non-urgent: a non-urgent referral means that the patient can be encouraged to make a routine appointment with the medical practitioner (GP) and this ideally will take place within 7 days at the most.
**High priority: a high priority referral means that the patient is assessed by a medical practitioner within the same day. This can be either as a home visit or at the medical practice.
***Urgent: the urgent category is for those situations when the patient requires immediate medical attention, and this may mean summoning an on-call doctor or calling the paramedics to the scene.
The order of the A tables can be found in the contents pages of this text.
A1: Red flags of cancer
Cancer is characterized by progressive growth of diseased tissue over the course of weeks to months and the loss of function which can result from the damage caused by this growth. The patient may therefore experience a deterioration in function which may either be gradual or may appear with the sudden development of new symptoms which do not go away. The red flags of cancer include any progressive unexplained symptoms which persist over the course of weeks to months without resolution. Also unexplained sizeable lumps and lymph nodes may be indicative of cancerous change.
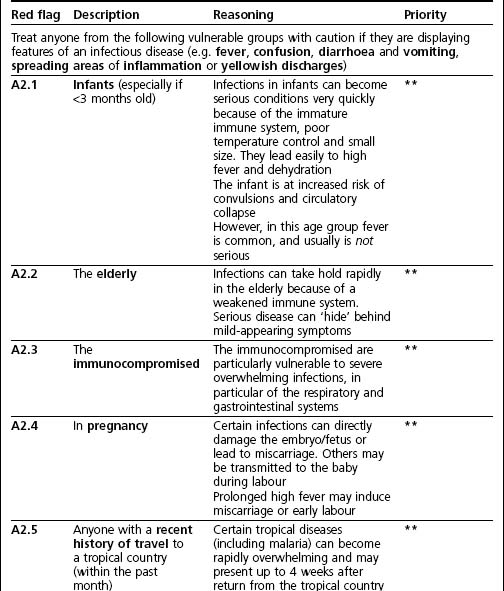
A2: Red flags of infectious diseases: vulnerable groups
Infections are more likely to cause problems in individuals who cannot sustain a strong immune response, either because of immaturity, old age, illness, pregnancy or because of exposure to unusual organisms (such as occurs during foreign travel).
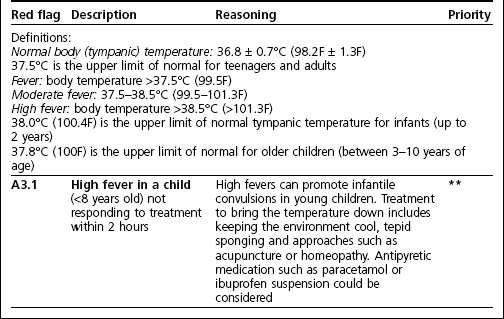
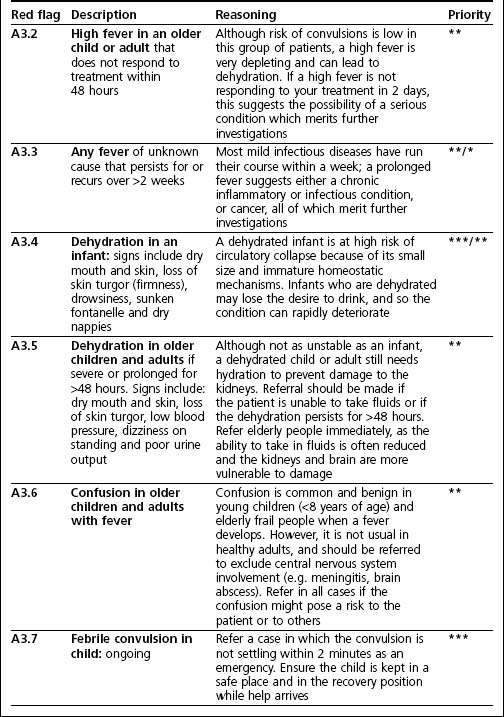
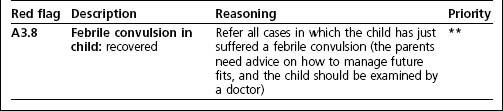
A3: Red flags of infectious diseases: fever, dehydration and confusion
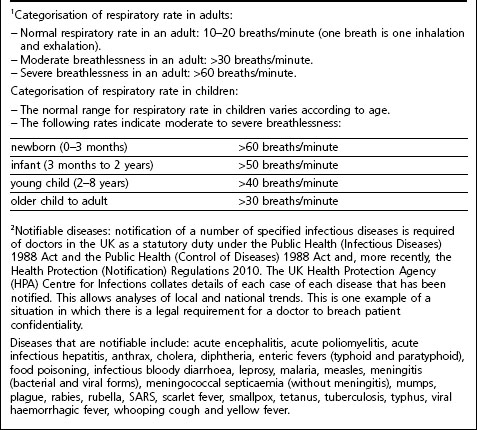
Fever can be assessed by means of thermometers of various designs which may measure body temperature from various locations in the body (e.g. forehead skin, ear, rectum and mouth). The measured temperature is slightly different according to the site, so it is important to be clear from the thermometer manufacturer’s instructions what the normal range is for the device which is being used.
The core temperature of a well person tends to follow a diurnal variation with core temperature peaking in the late afternoon at up to 1°C (1.8F) higher than the temperature measured in the early morning. Also, for temperatures less then 37.5°C (99.5F) what is normal for one person may represent a fever in another who tends to run at a generally lower core temperature. This makes interpretation of lower levels of fever difficult, and in such cases it is very helpful to know what the normal range is for that person in health.
Increasingly the tympanic (eardrum) temperature is rapidly assessed by means of user-friendly hand-held devices. The normal ranges below represent tympanic readings in adults. The tympanic temperature range is higher than the oral range by up to 0.7°C, and so the guidance below should be adjusted accordingly if oral readings are being interpreted. It must also be remembered that the normal range of temperature for children is slightly higher than for adults (see below).
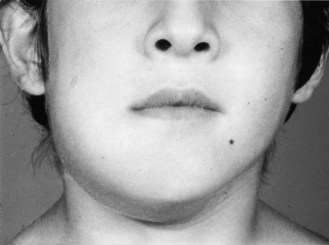
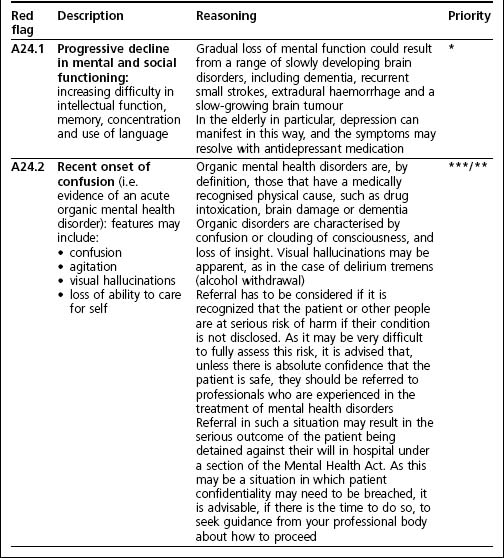
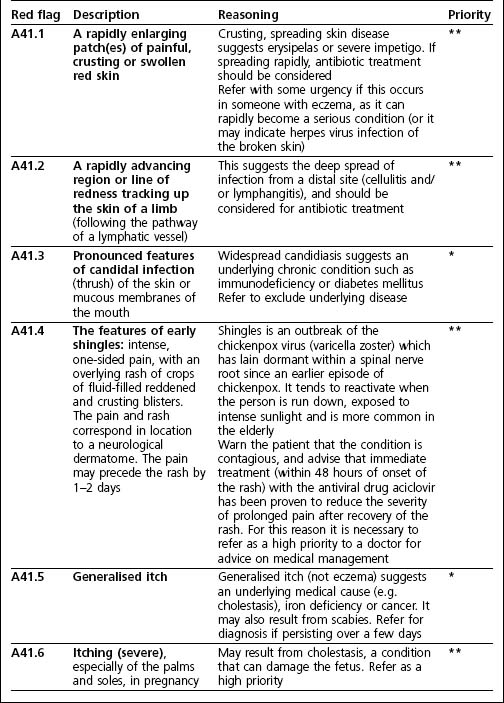
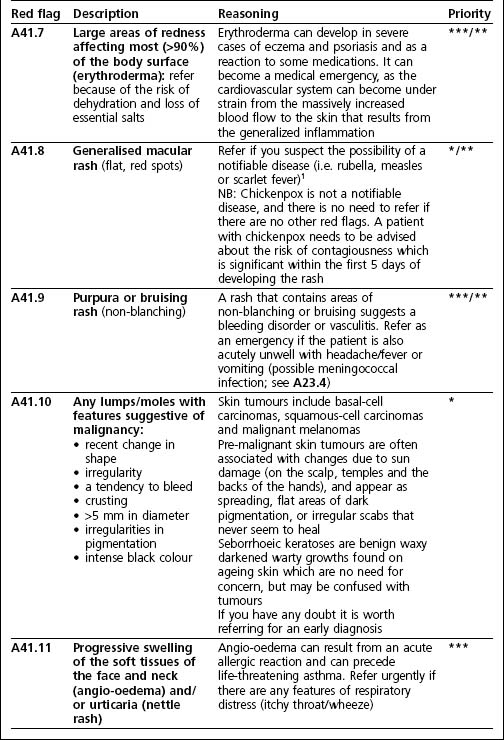
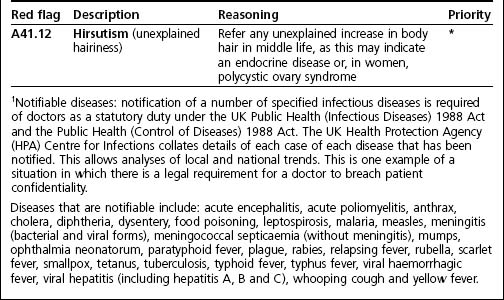
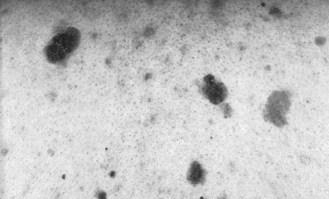
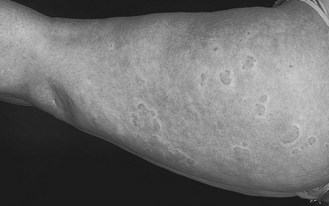
A41: Red flags of diseases of the skin

Figure 2.11 A malignant but slow growing basal cell carcinoma on the cheek (see A41.10).
(From CTG Figure 6.1c-XIX.)

Figure 2.12 A malignant but slow growing squamous cell carcinoma on the earlobe (see A41.10).
(From CTG Figure 6.1c.)
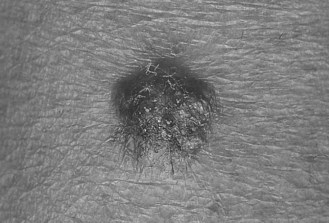
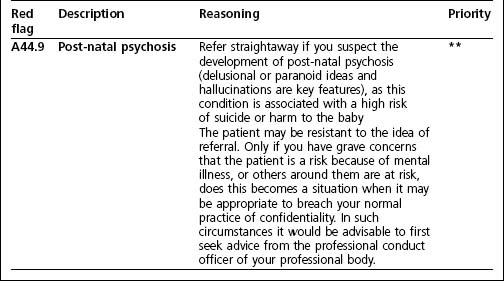
Figure 2.13 A malignant skin tumour (nodular melanoma) (see A41.10).
(From Kumar and Clark, 6th edn, Figure 23.34.)
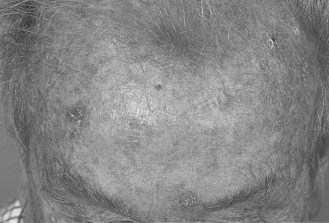
Figure 2.14 Pre-malignant solar keratoses on the sun-exposed forehead (see A41.10).
(From CTG Figure 6.1c-XVIII.)