Chapter 5 Communicating with medical practitioners
It is good both for patient care and also for interprofessional relationships that complementary medical practitioners maintain contact with the conventional medical practitioners who are involved in the ongoing healthcare of their patients. One important reason for complementary therapists to communicate with conventional doctors is to refer patients who demonstrate red flag conditions, so that the patient can access relevant medical advice and treatment. If the communication is made in a way which is both valid in terms of patient care and respectful of the professional to whom it is directed then it can only serve to improve relationships between complementary and conventional medical practitioners. In this way it can serve to promote the ideals of integrated health care.
Choice of method of communication
There are three methods by which a complementary medical practitioner might choose to communicate with a conventional medical doctor about a patient. By far the most commonly used and convenient method is to allow the patient to do the communicating by making an appointment with their doctor. Alternatively the practitioner can telephone the practice or hospital to speak to the patient’s health care professional in person. The most formal approach is to write a letter. These three approaches will be considered in turn.
Using the patient as the communicator
The most usual clinical situation in which it may help for the patient to communicate something about a complementary health consultation with their doctor is when a non-urgent red flag has been identified. An example of this is the situation when an elderly patient mentions they have been more thirsty than usual for the past 3 months and have been passing large amounts of urine (red flag of type 2 diabetes). In this situation the patient needs to be advised to make an appointment with their doctor so that the possibility of serious disease can be excluded or confirmed.
At the appointment, the patient can then explain to the doctor that their practitioner is concerned about their symptoms and that, for example, there is a possibility of diabetes. In many such situations, a letter is not necessary.
As long it is clear to the therapist that the necessary information can be communicated effectively by the patient, this may be the most empowering option for them.
Speaking to the doctor in person
Speaking to the doctor in person is the preferred mode of communication either if a patient needs to be referred urgently or if there is a matter of some complexity which needs to be discussed. Most doctors would be very happy to discuss a problem concerning a patient over the telephone (for example ‘Mrs Jones, who lives alone, seems to have been getting progressively more confused. Are you aware of this?’). Whenever possible, it is important to ensure that the patient is told in advance what is going to be said to ensure that there is no breach of confidentiality.
It is normal in UK general practice to have systems in place where doctors make telephone consultations on request, usually at a particular time of the day. However, in a situation of high urgency, the duty doctor may be contacted straight away. The practice receptionist is trained to discern which calls merit urgent handling. If the call is after office hours, then it will be transferred to an ‘on-call’ doctor when the practice telephone number is called. It is important to bear in mind that the doctor who is contacted may not know the patient, or have any access to details about them, although in office hours the doctor should have electronic access to patient records.
Communicating by letter
The letter is an appropriate method of referring complex patients and also of communicating clinical information about a patient in a non-urgent situation. A letter is not appropriate if information or advice is required, as the process of writing a reply is inconvenient for a busy doctor, and delays may occur if a letter has then to be typed and posted. If a problem needs to be discussed, such as Mrs Jones’ confusion, then the telephone is the best medium.
A letter is most useful when it either precedes or accompanies a patient who has made an appointment with the doctor. The letter can then communicate the additional information which it may be important to impart.
The structure and content of the communication
Whenever a referral is made, clear and succinct information needs to be imparted to the medical practitioner. Whether by the spoken word or by letter, this is best done in a structured way, and with the information offered in an order which is familiar to the doctor. If it is necessary to communicate by telephone, it is worthwhile for the complementary medical practitioner to prepare the information to be communicated in a systematic way before making contact. A list of the categories of information summarised below can be a useful aide-mémoire to ensure no important details are omitted from either a telephone call or in the writing of a letter. Referring to the list will also help ensure that all the necessary information is given in a logical order. General practitioners and hospital doctors tend to be overburdened with paperwork, and so it is important that telephone calls and referral letters offer information in brief and accessible format. It helps to keep written information in terse bulleted statements, and to confine a letter to less than one page in length.
In the UK, there is legislation designed to protect the rights of patients so that sensitive information about them is stored in a safe way. The Data Protection Act 1998 requires practitioners to register if they intend to keep electronic records of sensitive information about patients. This is not necessary if electronic copies of the letters are deleted once they have been printed out, in which case paper copies can be kept for the patient records.
Information to include when communicating about a patient to a medical practitioner
Patient identifiers
Give full name, date of birth and address. All three of these are required for medical records.
Brief summary of reason for referral
In one sentence: something like: ‘I’d be grateful if you could assess this 28-year-old man who tells me he has had three episodes of nocturnal bed wetting.’
More detailed history of main complaint
A brief synopsis of the key events in the history of the main complaint, including:
Signs
Then describe any findings (including relevant negatives like ‘blood pressure was normal’) on clinical examination.
Summarise what is wanted of the medical practitioner
For example: ‘I am concerned that this man might be experiencing nocturnal seizures, and would value your opinion on whether he needs further investigations.’
If appropriate, take the opportunity to describe how you have been treating with complementary medicine
A referral is a good opportunity to explain more about what complementary medicine involves. It is probably best not to use too much professional jargon in a referral situation, but a couple of sentences on why the patient is having complementary therapy and how they are benefiting can do no harm.
Important additional points which apply to letters
The important points to follow when structuring letters are as follows:
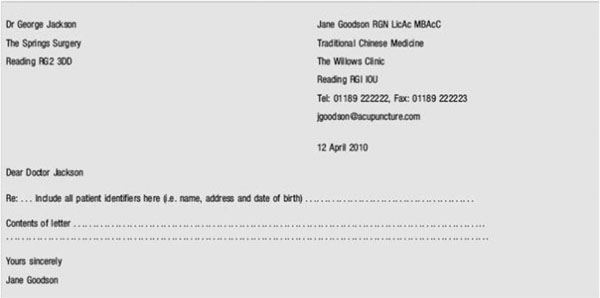
Headed notepaper (see Figure 5.1)
Headed notepaper should include the name of the practitioner, professional title and qualifications, address, telephone numbers, fax number, e-mail address and Web site address.
Choice of language
It will help with all communications if the practitioner aims to match the medical use of professional language as much as possible, and to avoid using complementary medical terminology which may be misinterpreted or dismissed as meaningless.
Confidentiality
Although letters between conventional health professionals are often written and sent without the express permission of the patient, it is advisable whenever possible to ensure that the patient is happy for you to be writing to another professional about them, even if they have been originally referred to you by that professional. A helpful hint is to always write a letter which you would be prepared for the patient to read. There should be very few situations in which it is legally advisable give information to the doctor without the patient knowing about it.
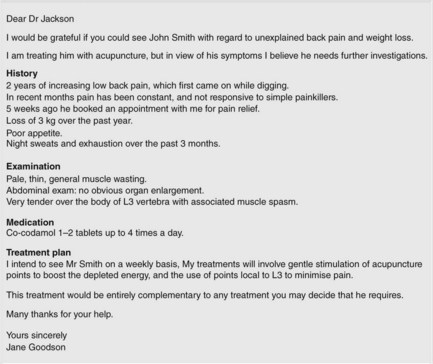
Sample letter for referring patients to medical practitioners
The use of standard letter format as indicated in Figure 5.2 is advised for the referral of patients who merit the opinion or treatment of a conventional medical practitioner. In such a letter, it is important to clearly describe the red flags which are of concern. A medical diagnosis is not required in such a letter as the red flags will usually speak for themselves.
In urgent situations, a hand-written letter is perfectly acceptable. Hand-written letters should be structured in exactly the same way as typed letters.
In all cases, letters should be on headed notepaper and contain the general information about the patient and the referrer as indicated in Figure 5.1.
The letter in Figure 5.2 indicates that the practitioner has questioned and examined the patient appropriately and has discerned a red flag situation, a condition in which there is bone pain and also unexplained weight loss. The red flags of concern are described at the beginning of the letter. The structured approach to listing information as described earlier in this chapter has been adhered to. The doctor who receives this letter will be in no doubt that the patient needs urgent investigation to exclude malignancy or some other serious chronic disease such as TB, and will recognise that the patient’s situation has been handled safely and professionally by the therapist.