Patient Teaching for Health Promotion
Upon completing this chapter, you should be able to:
1 Discuss the purposes of patient teaching.
2 Describe three ways in which people learn and correlate the importance of these types of learning to teaching.
3 List and differentiate between conditions and factors that can affect learning.
4 Identify adjustments to the teaching plan needed for teaching the very young patient or the elderly patient.
5 Discuss types of resources available to assist in patient teaching.
6 Name three things that must be included in the documentation of patient teaching.
7 Use patient teaching to promote the national goals of health promotion and disease prevention as listed in Healthy People 2010 and the Canada Health Act.
8 Describe ways in which teaching can be continued following hospital discharge.
1 Assess an assigned patient’s learning needs.
2 Develop a teaching plan based on the patient’s learning needs.
PURPOSES OF PATIENT TEACHING
The ultimate goal of patient teaching is the prevention of illness and the promotion of wellness. Nurses teach patients about their disease or disorder, including diet, medications, treatment, and self-care. Preoperative teaching covers the various phases of the surgery, what will be experienced, what can be expected, and the exercises to be done afterward. With hospital stays being so short, patient education has become an even higher priority. Prior to discharge, the patient must be taught how to care for himself at home. Because of this, there must be collaboration on the teaching plan among the various health professionals involved in the care, as well as communication with the family and home care nurse, if any.
Patient teaching aids in achieving the goals of Healthy People 2010, a program of the U.S. Department of Health and Human Services, and the Canada Health Act. The goals of Healthy People 2010 are to increase the life span and quality of life and eliminate health disparities among different populations. Enabling goals include promoting healthy behaviors, protecting health, ensuring access to quality health care, and strengthening community health prevention programs. Canadian principles include universality, comprehensiveness, accessibility, portability, and public administration.
Discharge planning requires looking ahead in order to meet the patient’s ongoing needs at home. It is a process that begins at the time of admission. This includes assessing for special needs, learning to identify appropriate teaching moments, and providing learning opportunities that are brief and focused on preparing the patient for self-care. A teaching moment occurs when the patient is at an optimal level of readiness to learn and apply a particular piece of information. Take cues from the patient’s questions or try to stimulate interest in what he needs to know. Saying, “You’ll want to know things you can do to lower your risk of another heart attack” tends to stimulate interest in the recovering myocardial infarction patient.
MODES OF LEARNING
Research has shown that people learn in three ways: (1) visually, through what they see (visual learning); (2) aurally, through what they hear (auditory learning); and (3) kinesthetically, by actually performing a task or handling items (kinesthetic learning). Although most people can learn by any of these routes, one route is usually dominant. For example, if a person is primarily a visual learner, telling him everything and not using any written materials or visual examples will make learning much more difficult. Many people do not know how they learn best. It is important to use a variety of teaching techniques so that the patient both sees and hears the information, and performs the action being taught.
During the teaching sessions, listen to how the patient makes responses because the language used may give clues to the person’s best learning mode.
Learning can also be categorized by domains. In the cognitive domain, the learner takes in and processes information by listening to or reading the material. In the affective domain, the material is presented in a way that appeals to the learner’s beliefs, feelings, and values. For example, people must value cleanliness before you can teach them to wash their hands frequently. In the psychomotor domain, the learner processes the information by performing an action or carrying out a task. All three domains are important to the patient’s translation of the learning to desired behaviors.
ASSESSMENT OF LEARNING NEEDS
In order to prepare a teaching plan, you must first know what the patient needs to learn. What does the person need to know about the disease or condition, diet, activity, medications, wound care, treatments, or self-care at home? This information establishes the learning needs.
Patients may require far more complex teaching than can be accomplished in the short time before discharge. In this instance, the basic survival skills are taught first, and after discharge the advanced skills are taught in group or private sessions. Often, a home health nurse will continue with the teaching plan. Make a list of the learning needs and then prioritize them so that you can concentrate first on teaching the essential knowledge needed for safe care at home. Place the identified learning needs on the patient’s plan of care.
FACTORS AFFECTING LEARNING
Before beginning to teach, you must assess for factors that might interfere with the patient’s ability to learn. Conditions that can affect the learning process include poor vision or hearing, impaired motor function, illiteracy, and impaired cognition. Age may interfere with the strength or dexterity for performing certain tasks. Physical, occupational, or speech therapists can be helpful in assisting the individual to overcome these types of problems so teaching can begin.
Situational factors that interfere with learning include pain, nausea, fatigue, a sense of being overwhelmed by all that is happening, and multiple interruptions.
Cultural Values and Expectations
The patient’s cultural values and personal expectations regarding treatment and recovery may differ from those of the nurse and other health care providers. This can interfere with the patient’s ability to cooperate and learn needed skills for self-care (Cultural Cues 9-1). It is necessary to work within the patient’s values and cultural system. The patient may wish to use herb poultices on a wound rather than the medication the physician prescribes. Often a compromise can be worked out, such as alternating the poultice with the medication prescribed (as long as the poultice is not harmful). Patients may practice religious rituals as an aid to healing with which the nurse may not be familiar. In hospitals on American Indian reservations, it is common to see a physician and a tribal shaman working side by side, honoring the strong belief that physical healing must be accompanied by spiritual healing. Such practices rarely conflict with medical treatment and may greatly benefit the patient.
Confidence and Abilities
Often patients express a lack of self-confidence, saying, “I’ll never be able to do that.” In such instances you must explore these feelings, being careful to enhance rather than harm the patient’s self-esteem. Praise and encouragement go much further than admonishment in promoting needed learning. Teaching may need to be broken down into very small steps (Communication Cues 9-1 on p. 122).
Play techniques can be very successful when teaching younger children. The use of dolls and play equipment is appropriate and helpful. Teaching must be done in short segments to allow for the child’s limited attention span. Language must be tailored to the child’s level of understanding. Children interpret language literally, so avoid idioms because they can be easily misunderstood.
When teaching the elderly, the pace is slowed to allow more time for processing the information. Patient Teaching 9-1 presents other points to consider.
Never assume that patients are literate. Many adults have gotten through school without learning to read adequately, and they may have spent a lifetime hiding this fact from friends, employers, spouses, and children. A teaching plan using visuals and kinesthetic learning will often be the most effective for these individuals.
Some patients who speak English as a second language may not be able to read English, even if they are fully literate in their original language. When working with a patient for whom another language is primary, offer printed, audiovisual materials in their native language, if available.
When printed materials are used, go over them with the patient and ask questions to determine whether the information has been understood. You should be aware of the patient’s educational level so that you can appropriately tailor your vocabulary and teaching materials, but avoid talking down to people. Assess what patients already know about the skills they need to learn so that you can build upon their current knowledge base. Do they have a basic knowledge of anatomy and how the body works? What do they already know about their medications? If they are going to give their own injections, have they ever handled a needle and syringe before? Teaching is most effective when you can relate the material to a subject that patients already understand. It can also be very helpful to determine if they have a relative or close friend who is knowledgeable about their health issues and willing to help them after discharge.
Readiness to Learn
You must assess the patient’s readiness to learn. Motivation plays a large role in effective learning. The desire to return to independence or to return to the comfort of home is often the motivating factor. Work with patients to show them the advantages of learning what they need to know. Teaching sessions will be more successful if the patient is comfortable and rested and there are a minimum of interruptions.
Begin by establishing rapport and developing trust, and maintain a warm, sincere attitude.
Although there are several nursing diagnoses that can be utilized for learning needs, the most commonly used one is Deficient knowledge, with the specific need finishing the statement. Deficient knowledge related to wound care is one example.
THE TEACHING PLAN
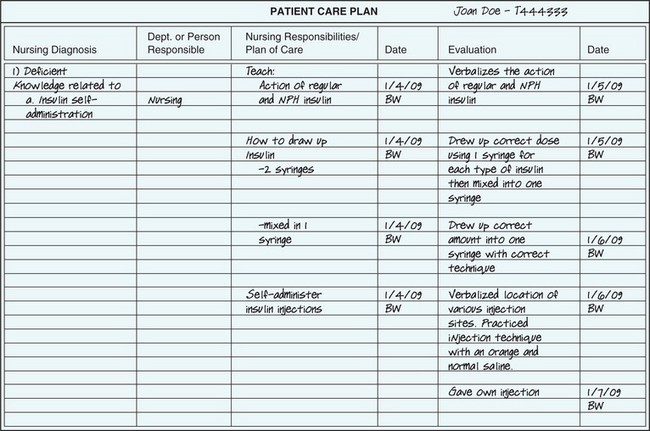
Preparing a teaching plan involves analyzing the assessment data, establishing behavioral objectives or goals, and creating a plan for assisting the patient to achieve these goals in the most timely and effective manner. Behavioral objectives represent the desired changes or additions to current behaviors and attitudes. They state what you are trying to teach the patient to do. “Patient will change the wound dressing using aseptic technique” is a behavioral objective. Behavioral objectives should be stated in terms that make achievement of the objective easy to evaluate. Evaluation of the above objective would be achieved by watching the patient change the wound dressing and determining if correct aseptic technique was used. The teaching plan is part of the care plan. Some agencies use a separate form for the teaching plan so that there is plenty of room to note the specifics (Figure 9-1). In specialty areas there may be a standardized teaching plan. An example would be postpartum teaching plans for self-care after delivery or for basic infant care.
It is essential that the teaching plan be developed collaboratively, with input from all of the disciplines involved in the patient’s care. The specifics of the plan should be discussed and agreed upon. Each knowledge deficit is listed as it is identified, and the date is included. The person responsible for providing teaching in each area is also noted. The teacher may be the nurse, physical or occupational therapist, dietitian, speech therapist, or respiratory therapist. The nurse is responsible for overseeing the plan specifics. Even when another person is doing the teaching, the nurse reinforces it. Consistency in teaching is important if the patient is to master and retain the new information.
RESOURCES FOR TEACHING
Many books and articles are available that provide suggested methods and teaching aids for particular topics. Audiovisual materials, pamphlets, and hands-on equipment are also good resources. Become familiar with what is available in your facility. Community agencies may also provide these educational tools. Local government agencies often provide printed and online listings of community public service programs. Nursing specialists may be available to assist with information and teaching plans or to do the actual teaching. Hospital social workers and patient representatives are also good sources of information about what is available.
Some of the instructional materials are designed to assist the medical professional and others are directed to the patient. The Internet has a wide variety of resources available for patient teaching. An Internet search by topic will provide links to myriad resources. Leading medical centers and universities across the United States and Canada, as well as governmental agencies such as the National Institutes for Health (NIH), the Centers for Disease Control and Prevention (CDC), and the National Institute of Mental Health (NIMH), provide websites with excellent teaching resources.
IMPLEMENTING THE PLAN
Begin by establishing a time with the patient to begin the teaching. Teaching should be done at a time when visitors, physician rounds, and treatments will not cause interruptions. Teaching can be done one-on-one or in a group setting. Be certain that the room temperature is acceptable and the patient is comfortable. Medicate the patient prior to the teaching session if pain control is needed. Provide good lighting. Be certain he can hear you and can see adequately.
Keep the teaching session short. Involve the patient in the process; call him by name, and ask for feedback as you progress. If teaching a group, establish eye contact frequently with each person in the group. Pause at intervals and ask if there are questions. When teaching a procedure, talk about the steps of the procedure, demonstrate the procedure, and then talk patients through each step while they perform it (Figure 9-2). Have them write down the steps, or provide them with a written guide they can follow.
At times, you may need to incorporate teaching into daily care. Teaching patients to perform range-of-motion exercises on their weak extremities can be done while bathing. Teaching about wound care can accompany the process of changing the dressing. Reinforcing information about a medication can be done when administering the medication.
The patient needs to receive written or printed information about what has been taught to take home’for instance, a pamphlet or clearly written list of steps to accomplish a procedure, such as performing a blood glucose determination. When possible, this should be in the patient’s primary language (Legal & Ethical Considerations 9-1).
Each teaching session should begin with a review of what was previously learned. If the patient was taught a specific skill, such as drawing up insulin, have the patient demonstrate that skill. This is called a return demonstration.
EVALUATION
Evaluating the effectiveness of teaching is critical to the success of the process. It involves obtaining feedback (return of information about the process) from the patient regarding what was taught, then using this feedback to determine whether effective learning has in fact taken place. A return demonstration of a skill is one way of evaluating the learning that has occurred. When the learning is not of a skill nature, but is on an information level, asking questions will obtain feedback about retention and comprehension of the material taught. Allow the patient time to think through the answers. Let the patient use any printed materials handed out. This lets you see that the patient can appropriately use the resources you provided.
Allow patients to perform at their own speed. The first step is learning to do the skill correctly. Performance will become more rapid with practice. Learning is a process of many steps, and rushing these steps can cause confusion, frustration, and a sense of failure for both the patient and the nurse.
If the return demonstration or the review questions indicate that the patient has not mastered the skill or material taught, you will need to repeat the instruction and reevaluate performance before going on to a new area of learning. It may also be necessary to alter the method of teaching to more effectively use the patient’s strongest learning strategies. The teaching plan should be adjusted and updated according to the evaluation data obtained. New learning needs may also be identified during the teaching and evaluation sessions. These also need to be included in the teaching plan.
DOCUMENTATION
Teaching often occurs informally while performing a nursing task such as administering medications. This makes it a challenge to consistently document patient education. Every staff nurse is legally responsible for providing patient education, and documentation is essential. If the facility does not use a patient education flow sheet, the following information should be entered into the nurse’s notes: specific content taught, the method of teaching that was used, and evidence of evaluation with specific results of the teaching. This allows nurses providing continuing care for the patient to follow up and reinforce the teaching.
COORDINATION WITH DISCHARGE PLANNING
Patients may be discharged home before necessary learning is complete. It is important that information regarding the patient’s education needs be communicated to the primary physician’s office. If the patient is being referred for home health services, it is necessary to also communicate the information to the home care nurse. In addition, the family or significant others who will be caring for the patient may need to be included in some of the teaching sessions Specific learning needs that remain should be discussed with all involved parties, including the patient, and the plan for teaching shared. It is necessary that a printed plan be sent home with the patient. A telephone call to the home health agency or to the physician’s office helps provide continuity of teaching.
NCLEX-PN® EXAMINATION–STYLE REVIEW QUESTIONS
Choose the best answer(s) for each question.
1. The primary purpose of patient teaching is to ensure that patients:
1. can share with others what they have learned.
2. can reduce the time they are hospitalized.
2. There are three types of learning: auditory, visual, and kinesthetic. Learning to apply an ostomy appliance by doing it step by step is an example of __________________________________ learning. (Fill in the blank.)
3. A patient newly diagnosed with diabetes has stated that he doesn’t understand why he needs insulin. His statement indicates a learning need regarding:
1. the disease process of diabetes.
2. the types of insulin available.
4. When starting the second teaching session for a patient, you should first:
1. present the new material to be covered in this session.
2. question the patient about learning from the first session.
5. When teaching a young child, it is appropriate to:
6. When teaching the elderly about a needed diet change, it is best to:
 ,
,  ,
,  ,
,  ,
,  ,
,