Pharmacology and Preparation for Drug Administration
Upon completing this chapter, you should be able to:
1 Describe how drugs are classified.
2 Explain the legal implications for administration of drugs by nurses.
3 Trace the general actions of drugs in the body.
4 Discuss areas of concern regarding medication administration to children or the elderly.
5 Describe issues of medication administration in home care.
6 List three reasons why patients may be noncompliant with drug treatment.
7 Discuss measures used to prevent medication errors.
1 Locate information about a drug, including action, use, usual dosage, side effects, interactions, recommended routes of administration, and nursing implications.
2 Identify information the patient must be taught to safely use a drug.
3 Demonstrate a method for accurately calculating a drug dosage.
4 Demonstrate safe practices in administration of medications.
5 Demonstrate the correct procedure for documenting medication administration.
adverse effects (p. 633)
agonists ( , p. 634)
, p. 634)
anaphylaxis ( , p. 634)
, p. 634)
antagonists ( , p. 634)
, p. 634)
contraindications ( , p. 642)
, p. 642)
degrade ( , p. 633)
, p. 633)
drug interactions (p. 630)
generic name ( , p. 630)
, p. 630)
half-life (p. 633)
Institute for Safe Medication Practices (p. 630)
medication administration record (MAR) (p. 642)
medication reconciliation (p. 642)
noncompliance ( , p. 640)
, p. 640)
nursing implications (p. 629)
peak action (p. 633)
pharmacodynamics ( , p. 633)
, p. 633)
pharmacokinetics (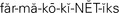 , p. 632)
, p. 632)
PRN (p. 639)
side effects (p. 633)
stat (p. 639)
synergistic effect ( , p. 634)
, p. 634)
therapeutic range ( , p. 634)
, p. 634)
toxic effects (p. 634)
trade name (p. 630)
unit dose (p. 639)
PHARMACOLOGY
The variety of drugs used in the treatment of diseases has increased tremendously in the past decade. New drugs continue to appear as medical researchers discover more chemicals that produce highly sophisticated effects on specific tissues and cells. Although some drugs, such as opium and castor oil, have been in use since 1600 B.C., the majority of drugs currently used are of more recent origin. For example, insulin was discovered by Banting in 1922, sulfanilamide was introduced in 1937, and the first patient was treated with penicillin in 1942.
Along with physicians and pharmacists, nurses are held legally responsible for the safe and therapeutic effects of the drugs. Medication errors account for a great number of occurrence reports.
In this chapter, the practical information needed to administer drugs competently and safely is presented. The chapter is not intended to supply all the information needed about how drugs work or to provide comprehensive practice for drug calculations; consult additional medication references and math workbooks. To prepare for medication administration, you need to (1) be able to locate the information about each drug, (2) consistently calculate drug dosages accurately, (3) devise a method for using the Five Rights and five “rules” of medication administration consistently, and (4) recognize the nursing implications (points you need to remember about the drug or teach to the patient) for each drug administered.
For pharmaceutical medical treatment to be effective, the patient must be compliant with the medication regimen. We assume that compliance increases when patients are knowledgeable about the medication. It is your responsibility to teach the patient about drugs and to acquire the information that you and the patient need to know about each medication.
The vast increase of pharmaceutical agents used for medical treatment, and the multiple drugs that many patients take, mean that nurses must be knowledgeable about possible drug interactions (one drug modifies the action of another). For the patient to receive the full benefit of the drug, nurses must also be aware of foods that interfere with the desired uptake or action of the medication.
Issues of cost containment demand that nurses be aware of how drugs affect diagnostic testing. If a drug causes a false-positive result, then unnecessary and expensive treatment may be erroneously ordered. Likewise, a drug that causes a false-negative result may lead a physician to overlook a disease condition until great damage has been done to the patient.
USES FOR DRUGS
Drugs or medications are substances used in the treatment, palliation, diagnosis, cure, and prevention of disease. Physicians, dentists, osteopaths, and veterinarians prescribe medications; physicians’ assistants, nurse practitioners, and advanced practice nurses (APNs) prescribe medications in collaboration with physicians and under written protocols or standing orders. Drugs may be dispensed and administered by pharmacists as well as those prescribing them. In accordance with Healthy People 2010, pharmacists and prescribers should provide counseling for patients about the risks and uses of medications. Nurses must support this effort by reinforcing the teaching and encouraging patients to ask questions.
Although drugs may have three names’a chemical name, a generic name (name not protected by trademark), and a trade name (name protected by a trademark)’usually knowing the generic and trade names is sufficient for the nurse. The chemical name provides a description of the chemical composition of the drug. Some drugs have many different trade names because they are manufactured by several different companies. For example, the generic-named drug ibuprofen may be marketed under the trade names of Advil, Motrin, and others.
Drugs come in a variety of forms and types of preparations. The form of a drug determines its route of administration. The composition of a particular form is designed to enhance its absorption and metabolism in the body. Many drugs come in several forms, such as tablets, capsules, ointments, solutions, suspensions, and suppositories (Safety Alert 33-1).
CLASSIFICATION OF DRUGS
Learn to categorize medications with similar characteristics by their class. Classifications may be defined by the effect of the drug on a body system (example: anticonvulsants),the symptoms the drug relieves (example: antihypertensives), or the drug’s desired effect (example: analgesics). Similar types of problems are treated by the same class of drug, although the class may be broken into subgroups depending on how the drug works in the body to produce the desired overall effect. A drug may also have a variety of properties and effects and therefore may belong to more than one class. A common example is aspirin, which has antipyretic, anti-inflammatory, analgesic, and anticlotting effects.
Another way is to learn the drugs by groups categorized by their generic drug name endings. Drugs with the same name ending often have similar characteristics and are for the same type of problem (Table 33-1).
Table 33-1
Major Drug Categories by Generic Name Endings
| GENERIC NAME ENDING | TYPE OF DRUG | COMMON ACTION |
| “Prils” (e.g., lisinopril) | ACE inhibitors | Antihypertensive that relaxes arterial vessels |
| “Sartans” (e.g., losartan) | Angiotensin receptor blockers | Antihypertensive that blocks action of vasoconstriction effects of angiotensin II |
| “Olols, alols, and ilols” (e.g., atenolol, labetalol, carvedilol) | Beta blockers | Antihypertensives/antianginals that block beta adrenergic receptors in vascular smooth muscle |
| “Statins” (e.g., atorvastatin) | Antilipemics | Inhibit HMG-COA reductase enzyme reducing cholesterol synthesis |
| “Dipines” (e.g., amlopidipine) | Peripheral vessel calcium channel blockers | Antihypertensives/antianginals that produce relaxation of coronary smooth muscle and vascular smooth muscle; dilate coronary arteries |
| “Afils” (e.g., sildenafil) | Erectile agents | Peripheral vasodilator that promotes a penile erection |
| “Floxacins” (e.g., ciprofloxacin) | Broad-spectrum antiinfectives | Inhibits bacteria by interfering with DNA |
| “Prazoles” (e.g., esomeprazole) | Proton pump inhibitors | Suppress gastric secretions preventing gastric reflux and gastric and duodenal ulcers |
| “Tidines” (e.g., famotidine) | Block histamine-2 receptors | Inhibits histamine at H2 receptor sites decreasing gastric secretions |
| “Azoles” (e.g., fluconazole) | Antifungals | Cause direct damage to fungal membrane |
| “Cyclovirs” (e.g., acyclovir) | Antiherpetic | Interferes with DNA synthesis causing decreased viral replication |
Adapted from a presentation by Barb Bancroft at the California Vocational Nurse Educators Conference in Sacramento, CA on April 25, 2008,
It is extremely important to learn the general characteristics of each drug classification and the nursing implications, which are your guide to safe and effective medication administration. The role of the nurse in drug therapy is to administer an individual dose of a medication at a specified time. You must be aware of state statutes regulating the type and forms of drugs you may administer because this varies somewhat from state to state.
LEGAL CONTROL OF DRUGS
The public health, safety, and welfare of citizens are concerns of state and federal governments. The Pure Food and Drug Act of 1906 was the first federal statute regulating drug use. It sought to combat misuse of narcotics and to prevent the manufacture of adulterated or misbranded foods, drugs, and liquors. The federal Food, Drug, and Cosmetic Act of 1938 updated earlier laws, especially those dealing with labeling. Federal laws have since been passed that extend and refine controls on drug distribution, sales, testing, naming, and labeling. The Comprehensive Drug Abuse Prevention and Control Act of 1970 further regulates dispensing and handling of all controlled substances (Table 33-2). This act defines a drug-dependent person in terms of physical and psychological dependence. It classifies drugs according to their medical usefulness as well as their potential for abuse. Because many controlled substances are used daily in health care agencies, you must know how to comply with regulations and agency policies to prevent misuse of these drugs.
Table 33-2
| CLASSIFICATION | CRITERIA AND EXAMPLES OF CONTROLLED DRUGS |
| Schedule I | Drugs with no accepted medical use, a high potential for abuse, and lacking accepted safety measures. Group includes some opioids, psychedelics, cannabis derivatives, methaqualone, and phencyclidine. Examples: heroin, lysergic acid diethylamide (LSD), phenolsulfonphthalein (PSP), and peyote |
| Schedule II | Drugs with a medical use, a high potential for abuse, with severe psychological or physical dependence. Group includes many opioids, psychostimulants, barbiturates, and cannabinoids. Examples: secobarbital (Seconal), amobarbital (Tuinal), amphetamine, meperidine, morphine, and methadone |
| Schedule III | Drugs that are medically useful but with less potential for abuse that lead to moderate or low physical and high psychological dependence. Group includes lesser opioids, stimulants, some barbiturates, miscellaneous depressants, and anabolic steroids. Examples: paregoric, butabarbital, and acetaminophen with codeine |
| Schedule IV | Drugs that are medically useful, but with less potential for abuse than the Schedule III drugs, their abuse causing limited physical or psychological dependence. Group includes some lesser opioids, stimulants that suppress appetite, some barbiturates, benzodiazepines, and miscellaneous depressants. Examples: tranquilizers such as chlordiazepoxide (Librium), diazepam (Valium), fenfluramine, temazepam, and chloral hydrate |
| Schedule V | Drugs with medical use, low potential for abuse, and producing less physical dependence than the Schedule IV drugs. Group includes a few opioids. Examples: mixtures with small amounts of narcotics (e.g., cough syrup containing codeine) |
In the hospital, the responsibility for the security of controlled drugs is shared by the pharmacists and the nurses. Stock supplies of controlled drugs are stored in the pharmacy safe and dispensed as needed to the nursing units.
In a majority of hospitals, Schedule II and III drugs are dispensed in limited amounts to the nursing units, where they are stored in a locked narcotics drawer, compartment, or automated dispensing unit. The licensed nurse is responsible for the security of these medications and must account for each dose that is used. Although the method of accounting varies among hospitals, a record is kept on which the nurse notes each dose that is given, to whom, and when. Other information may be included, such as the patient’s room and hospital number or the name of the physician. A proof-of-use record would be used to account for each dose dispensed to the nursing unit. Information is recorded when the dose is administered to the patient. When the contents of the locked narcotics drawer are counted at the change of shifts, there should be a record of each dose given, a dose of the drug remaining for each unrecorded line, and the total remaining. To ensure the accuracy of this inventory, it is common practice for two nurses from consecutive shifts to count the drugs together. The completed proof-of-use records are eventually returned to the pharmacy and must be kept for a specified period of time. Automated dispensing units track doses removed by each nurse by computer.
Drug Standards
Standards for drug quality, purity, packaging, safety, labeling, and dose form were set by the Pure Food and Drug Act of 1906. The standards are published in the United States Pharmacopeia (USP) and the National Formulary. The British Pharmacopoeia (BP) sets similar standards for drugs in Canada. For a drug to pass U.S. Food and Drug Administration (FDA) approval and be marketed, it must meet standards in five areas: purity, potency, bioavailability, efficacy, and safety (Table 33-3).
Table 33-3
Drug Standards that Must Be Met by Manufacturers
| STANDARD | DESCRIPTION |
| Purity | Types and concentrations of substances other than the drug that can be in the tablet, capsule, suspension, etc. |
| Potency | Amount of active drug in the preparation contributing to its strength |
| Bioavailability | Drug’s ability to dissolve, be absorbed, and be transported in the body to its desired site of action |
| Efficacy | Laboratory studies indicative of proof that the drug is effective for its intended use |
| Safety | Sufficient studies completed to indicate potential side effects, adverse effects, and toxic reactions; safety is determined from the data |
Health care institutions establish individual policies to prevent health problems resulting from drug administration. An example would be the automatic discontinuation of an antibiotic order after a certain number of days of therapy. The order may be renewed, but the physician should review the status of the patient and effectiveness of the antibiotic prior to doing so; physicians are alerted to the need for renewal.
BASIC CONCEPTS OF PHARMACOLOGY
Drug Action and Pharmacokinetics
Drugs are potent chemicals that affect the body by acting on body cells. Any drug can be either beneficial or harmful, depending on the cellular reaction. Essentially, cell functions are either stimulated or depressed, and these reactions can be achieved in various ways. Digoxin, for example, stimulates heart muscle fibers to contract more powerfully, and its effect on the heart’s electrical properties causes changes in rate and rhythm. Barbiturates depress the function of cell groups in the central nervous system, causing drowsiness. Antineoplastic drugs, such as vincristine, have the ability to block cell division. Although the exact effect on cellular function is not known for all drugs, such information is continually expanding.
The study of how drugs enter the body and reach their site of action, and how they are metabolized and excreted, is called pharmacokinetics. Knowledge of pharmacokinetics is used by nurses in timing drug administration. Nurses judge the patient’s risk for alterations in drug action considering physiologic condition and other drugs the patient is taking.
Absorption.: To reach the cellular level, solid drugs in the form of capsules, pills, or powders must be dissolved within the body before the medication is absorbed into the bloodstream and distributed to the tissues. Drugs already in solution, such as oral liquidsor injections, are generally absorbed more rapidly. Absorption may be affected by the patient’s physical status. Differences in absorption by route are shown in Table 33-4.
Table 33-4
Differences in Absorption by Route
| ROUTE | RATE OF ABSORPTION |
| Skin (transdermal) | Slow absorption |
| Mucous membranes | Quick absorption |
| Respiratory tract | Quick absorption |
| Oral | Slow absorption (liquids are faster than pills, tablets, or capsules) |
| Intramuscular | Depends on form of the drug: aqueous is quicker than oil, which slows absorption |
| Subcutaneous | Slow absorption |
| Intravenous | Most rapid absorption |
The rate of absorption is determined by many factors. Body weight, age, sex, disease conditions, genetic factors, immune mechanisms, and physiologic and emotional factors modify reactions to a given drug. Even such a factor as hot or cold weather affects the absorption rate. Infants display a lower tolerance for drugs than children; this relates to the immaturity of organs needed to detoxify and excrete the drugs.
Distribution.: Distribution to tissues and the cellular site of action depends on the chemical and physical properties of the drug and the physical status of the patient.
Other Factors Affecting Drug Action.: A direct relationship exists between the amount of drug administered and the amount of body tissue in which it is distributed. An increase in the percentage of body fat tends to cause a slower distribution of the drug. The less a patient weighs, the more concentrated the drug will be in the tissues, and consequently the more powerful the effect.
The rapidity with which concentration at a target site occurs depends on the blood supply to the site. Local vasodilation or vasoconstriction affects the rate of blood flow. Biologic membranes affect the distribution of drugs. The blood–brain barrier is permeable only to fat-soluble drugs, and only these drugs can reach the brain and cerebrospinal fluid. Most drugs cross the placental barrier and affect the fetus.
The protein-binding capacity of a drug affects distribution. Most drugs bind to the protein albumin to some extent. Only the unbound portion of the drug in the bloodstream is then distributed to the target tissue. If a patient is taking two drugs that are protein bound, one or the other drug may have a higher concentration in the unbound state than it would if it had been given alone. This is because the drug with the lower unbound concentration has a greater ability to bind to available protein, leaving less protein to bind to the other drug.
At the site of action, the drug is soon metabolized into an inactive form that can be more easily excreted (Cultural Cues 33-1). This occurs when enzymes detoxify, degrade (break down), and remove the active drug chemicals. Most drugs are metabolized in the liver, but the lungs, blood, intestines, and kidneys contribute to metabolism. When there is a decrease in liver function from disease or aging, a drug may be eliminated more slowly than usual, resulting in an accumulation of the drug that could lead to toxic levels.
Drugs are mainly excreted by the kidneys, but some excretion occurs via the bowel, liver, lungs, and exocrine glands. Alcohol and gaseous and volatile compounds such as anesthetics are excreted through the lungs. Deep breathing and coughing help the postsurgery patient rid the body of anesthetic more rapidly. Drugs metabolized in the liver may be excreted into the intestine in the bile. The chemicals may be reabsorbed through the intestines. Therefore, an increase in peristalsis accelerates drug excretion and factors that slow peristalsis may prolong the drug’s effect. Some drugs are excreted by the kidney unchanged, but most drugs are metabolized and then excreted by the kidney. If kidney function declines, drug excretion drops, placing the patient at risk for drug toxicity. Adequate fluid intake (50 mL/kg/day) is essential for the patient to eliminate drugs properly.
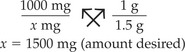
Drug Response and Pharmacodynamics
The study of a drug’s effect on cellular physiology and biochemistry and its mechanism of action is known as pharmacodynamics. Response to a drug can cause a primary or secondary physiologic effect, or both. The primary effect is the desired effect; the secondary effect may be desirable or undesirable, causing side effects (unintended actions) or adverse effects (very undesirable effects with more serious consequences) (Assignment Considerations 33-1). Antihistamines such as diphenhydramine hydrochloride (Benadryl) compete with histamine at receptor sites, producing a primary antihistamine effect. A secondary effect is the inhibition of central acetylcholine, which produces a sedative effect. The secondary effect is undesirable when driving a car, but might be desirable at bedtime.
Onset, peak, and duration of action differ for each drug. Peak action occurs when the highest blood or plasma concentration of the drug is achieved. The length of time the drug exerts a pharmacologic effect is the duration of action. The onset of drug action begins when the drug reaches a minimum effective concentration level. Each drug has a serum half-life, or the time it takes for excretion to lower the drug concentration by half. The next dose of a drug is scheduled at the time the previous dose should reach its half-life, thus sustaining a therapeutic level of the drug.
When giving sequential doses of a drug, it is important that the doses be timed so that the concentration level of the drug in the blood never drops below the minimum effective concentration level. However, if doses of a drug are given too close together, the peak may be exceeded, causing a toxic concentration of the drug in the body.
Drugs work by attaching to receptor sites on cells or preventing other substances from attaching to those sites. The action of many drugs is dependent on their ability to attach to specific receptor sites. The better the drug fits the receptor site, the better the drug’s intended action. Most cell receptors are protein in structure. Drugs that produce a response are agonists and drugs that block a response are antagonists.
Most drugs do not bind only to specific or selective sites. For this reason they produce multiple side effects as a result of binding at other sites as well as the intended ones. For example, a drug that binds to and therefore blocks cholinergic receptors will produce anticholinergic responses. The drug may be intended to dry up secretions by blocking gland secretion before surgery, but may also cause urinary retention due to effects on the bladder. An anticholinergic drug will also affect the heart, lungs, and eyes. For this reason, if you know how a drug works, you can usually figure out what its side effects will be. Those side effects depend on which receptor sites the drug is stimulating or blocking. Some drugs work nonselectively and affect multiple types of receptor sites. Epinephrine is such a drug; it acts on alpha1, beta1, and beta2 receptors. Other drugs produce a response by stimulating or inhibiting enzymes or hormones and do not act on receptor sites at all.
There are four types of drug action:
1. Stimulation or depression (direct action on a receptor site), such as when the rate of cell activity is stimulated or secretion from a gland is increased, or cell activity is depressed and the function of a specific organ is reduced.
2. Replacement, such as injected insulin for people who do not produce their own.
3. Inhibition or killing of organisms, such as the action of an antibiotic when it blocks synthesis of the bacterial cell wall.
4. Irritation, such as that produced by a laxative on the colon wall, resulting in peristalsis and defecation.
The less specific the action of the drug, the more side effects the drug may have. Most drugs have some side effects. The drowsiness produced by an antihistamine is a side effect because the intended effect is to suppress allergic reaction. Sometimes side effects include adverse effects. An example of an adverse reaction is nausea produced by an antibiotic when its desired action is to kill pathogenic organisms. Another type of adverse effect is an allergic reaction. Developing a rash or hives after taking penicillin is an example of an allergic reaction. When an allergic adverse reaction occurs, the patient is cautioned never to take the drug again because an allergic response will become more severe the next time a drug is encountered and could cause anaphylaxis (severe allergic reaction), which could lead to death. The possibility of adverse drug effects, side effects, allergic reactions, and undesirable interactions with other drugs and foods, increases with the number of drugs administered.
The therapeutic range is the range of levels of the drug in the blood that will produce the desired effectwithout causing toxic effects. Toxic effects (harmful effects) occur when the blood level of a drug rises above the therapeutic range and causes unintended damage to normal cells. For drugs that have a narrow therapeutic range, blood levels are monitored to prevent toxicity. For example the therapeutic range of phenytoin (Dilantin), an anticonvulsant, is 10 to 20 mcg/mL of blood serum. Toxic effects occur if the blood level rises above 30 mcg/mL. Figure 33-1 reviews the factors that affect drug therapy.
A drug interaction may result in an increase or a decrease in the action of the other drug, or may alter the way in which the drug is absorbed, metabolized, or eliminated from the body. A synergistic effect (combined interaction) may occur when the action of the two drugs combined is increased or greater than the effect of the drugs given separately. Alcohol has a synergistic effect when combined with any drug that depresses the central nervous system (CNS) because it is also a CNS depressant.
Drug and Food Incompatibilities
Medications that have been taken orally can be affected by food in the digestive tract. The presence of food in the stomach can affect the drug in many ways: It can speed up, reduce, or even prevent the absorption of the drug into the bloodstream. Food delays the emptying of the stomach and so may delay the onset of the therapeutic effects of the drug. The acidic gastric juices may affect the rate of breakdown of tablets and may prevent the drug from reaching the intestinal wall, where it can be absorbed.
In addition, some drugs are incompatible with others. When such drugs are given at the same time, their effects are changed. Some drug actions are accentuated by other drugs, others have an additive effect, and still other drugs may be inactivated by the other medication. The nurse is responsible for knowing the factors affecting the use of each medication given. For updated information on food and drug incompatibilities, consult drug handbooks, pharmacology books, professional journals, or the drug package insert, or check with the pharmacist (Figure 33-2). Many prescription drugs include precautions on how the drug is to be taken in relation to food and liquids as part of the label for the patient’s information.
MEDICATION ADMINISTRATION AND SAFETY
When a prescription or order is created for a drug to be dispensed or administered to a patient, the drug name, the amount of the drug per dose, the number of doses (tablets, capsules, etc.), the route by which to administer the drug, and the frequency or number of times a day the drug is to be taken is written by the physician or qualified person. You must analyze the order and determine if the drug, dose, and timing of the drug are appropriate for the patient. For this reason, you must be aware of the usual dosages for an adult or for a child for each drug. Sometimes the route ordered is not appropriate; this might happen when a patient is experiencing nausea and vomiting, but has a medication order for an oral route. If the drug comes in a rectal suppository form or an injectable form, you can consult with the physician and have the order changed. Table 33-5 presents the various routes of administration.
Table 33-5
Routes for Drug Administration
| ORAL ROUTES | |
| Oral (PO) | Medication is given by mouth and swallowed with fluid. |
| Sublingual | Drug is placed under the tongue, where it readily dissolves. Should not be swallowed. |
| Buccal | Solid medication is placed in the mouth against the mucous membrane of the cheek until it dissolves. Should not be chewed or swallowed. |
| PARENTERAL ROUTES | |
| Intradermal | Medication is injected into the dermis just under the epidermis. |
| Subcutaneous | Medication is injected into the tissues just below the dermis of the skin. |
| Intramuscular (IM) | Medication is injected into a muscle. |
| Intravenous (IV) | Medication is injected into a vein. |
| Epidural | Medication is injected into the epidural space of spinal column.* |
| Intrathecal | Medication is injected into the intrathecal space of spinal column.* |
| SKIN | |
| Topical | Medication is applied to the skin, eye, or ear for local effect. |
| Transdermal | Medication is applied in a small area for slow systemic absorption. |
| MUCOUS MEMBRANES | |
| Vaginal | Medication is inserted into vagina for local treatment. |
| Rectal | Medication is inserted into rectum for local or systemic effect. |
| Inhalation | Medication is inhaled into the nose or lungs for local and systemic effect. |
*Medication administration via these routes is beyond the scope of LPN/LVN practice, but you may see this type order.
The nurse is also responsible for monitoring laboratory results related to drug administration. For example, if a patient is taking furosemide (Lasix), it would be appropriate to check the potassium level prior to administering the drug. In addition, the Institute for Safe Medication Practices (ISMP) suggests that lab values must be reported directly to licensed personnel.
Medication errors occur far more often than they should. According to the 2009 National Patient Safety Goals (2B), health care facilities should “standardize a list of abbreviations, acronyms, symbols, and dose designations that are not to be used.” Table 33-6 presents recommendations for discontinuing the use of certain abbreviations in dosage orders.
Table 33-6
The Joint Commission’s Dangerous Abbreviations or Dose Designations—Not Recommended
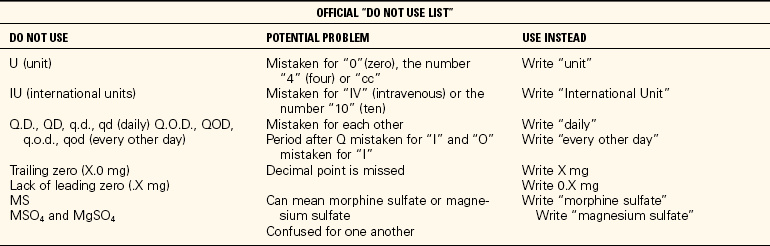
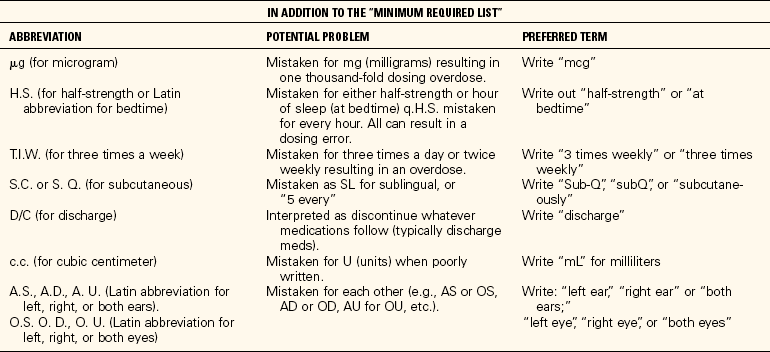
Copyright © 2007. The Joint Commission. Reprinted with permission.
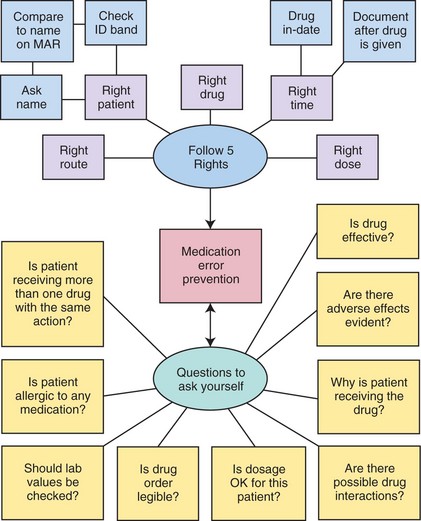
It will take a period of time before all health care professionals eliminate the use of these abbreviations, so they will still be seen in drug orders. When one of these abbreviations appears, consider the order very carefully in relation to the patient’s condition to be certain you understand its meaning. Developing a routine for safely giving medications and sticking to it each time you do the procedure can help you avoid making a medication error. Should an error be made, it must be reported immediately to your clinical instructor and/or charge nurse. A medication error can be a life-threatening event for a patient, and patient safety must come first (Safety Alert 33-2). In addition, the ISMP publishes a newsletter that provides educational information for health care providers related to safe medication administration (www.ismp.org/Nursing Articles/list.htm). There is also a phone number to report medication errors to the ISMP (1-800-FAIL-SAF[E]). Reporting errors is an opportunity to improve individual practice and health system policies. Reviewing Box 33-1 and Concept Map 33-1 will help you keep in mind all the information you need to safely administer medications.
CONSIDERATIONS FOR INFANTS AND CHILDREN
Differences in size, age, weight, surface area, and organ maturity all affect the ability to absorb, metabolize, and excrete drugs. Drug dosages are lower for infants and children than for adults and must be very carefully calculated and administered. Doses are based on age, size, and weight of the child and are not given in a standardized amount. Each dose is calculated very carefully.
Check with the child’s parents for the most effective, least traumatic way to give the child a medication. Sometimes it is best to let the parent administer the oral medication while you supervise. You should explain in short sentences with simple language at the child’s level of understanding what the drug is for and how it is to be given. Be supportive, and approach the child with confidence and an attitude of expecting cooperation.
CONSIDERATIONS FOR THE ELDERLY
The following points should be considered before administering medications to an elderly person:
• Elderly patients may have chronic medical conditions and may be taking multiple medications; check drug interactions carefully.
• Metabolism of drugs is slowed in the elderly, and normal doses may build to toxic levels when liver or kidney function is decreased. Elderly patients experience twice as many adverse reactions as younger people; observe the patient closely for signs of adverse reaction.
• Older patients who are on long-term anti-inflammatory therapy for arthritis should be monitored for gastrointestinal bleeding and anemia.
• Elderly patients may need a pill organizer to help them remember which drugs to take and to remind them whether they have taken a dose of medication.
• Elderly patients are likely to have greater blood pressure fluctuations with position changes and are more susceptible to falls when taking drugs that can cause orthostatic hypotension.
• Elderly patients may become quickly dehydrated and experience electrolyte imbalances when taking diuretics; these drugs also may increase uric acid levels, making the patient susceptible to gout.
• Elderly patients who have decreased kidney function are particularly susceptible to digoxin toxicity and should be carefully watched for early signs of this condition, which include appetite loss, confusion, fatigue, and depression.
• Patients with limited financial resources may not be able to afford the purchase of needed medication; a tactful inquiry is sometimes necessary.
• Some elderly patients have very limited vision and can misread the label on medication containers; encourage the patient to have another person verify or color-code medications.
• With age, swallowing muscles weaken, and the patient is more susceptible to choking; position the patient upright and, if the person is not on fluid restrictions, have him take a sip of water and then the oral medication with more water.
• If the patient has had a stroke causing weakness on one side, be certain that the medication is placed on the strongest side of the mouth (always assess swallowing ability before giving anything by mouth to a patient who has had a stroke or neurologic problem causing weakness).
• Many older patients have difficulty opening “childproof” caps on medication bottles; they can request that medication be placed in bottles with caps that are easy to remove and replace.
• Approximately one third of elderly patients are noncompliant with their medication regimens because of confusion, forgetfulness, poor vision, and other socioeconomic reasons. In such cases, help is needed to promote understanding of the drug regimen and to provide a reliable method of adhering to a medication schedule.
CONSIDERATIONS FOR HOME CARE
For home care patients, be certain that the patient or caregiver can open the medication bottles or dispenser. A pill organizer may need to be set up for the patient to ensure that medications are taken on schedule. Written instructions about what to report to the physician should be left with the patient. If possible, observe the caregiver or patient as he or she prepares medication to validate the process of administration that is being used. Verify that the patient can obtain the needed medications; if not, notify the physician. Caution patients about keeping medications out of the reach of children. Check medicine cabinets for medications that are out of date and see that they are discarded.
If a caregiver is to administer the medications, thorough teaching must be performed. Obtain feedback that indicates the caregiver understands what each medication is for, when it is to be given, side effects to monitor, and adverse effects to report to the physician.
TYPES OF ORDERS
There are four common types of medication orders based on the frequency of drug administration.
• A standing order is carried out until it is canceled by the physician or until the prescribed number of doses has been given. “Ceftin 250 mg po bid × 10 days” is an example of a standing order.
• A PRN (as-needed) order is an order written for when the patient requires it. The nurse and patient determine the patient’s need. The physician sets time limits for the interval between doses. An example of a PRN order is “Morphine 4 mg IM q 4 hr PRN pain.”
• A one-time (single) order is written for a drug to be given just the one time. Such orders are common preoperatively or before a diagnostic procedure. An example is “Valium 10 mg IM on call to G.I. lab.”
• A stat (immediate) order is for a single dose of a medication to be given right away without delay. A stat order is used in emergencies when the patient’s condition has suddenly changed. An example is “Benadryl 50 mg IM stat” to help counteract an allergic reaction.
There are many abbreviations and symbols used in medication orders that you must know. Although it is recommended that use of some of these abbreviations and symbols be discontinued, you should learn all of them because they are still in use in some areas. The most common ones are given in Table 33-7.
Table 33-7
Abbreviations and Symbols Used in Medication Orders
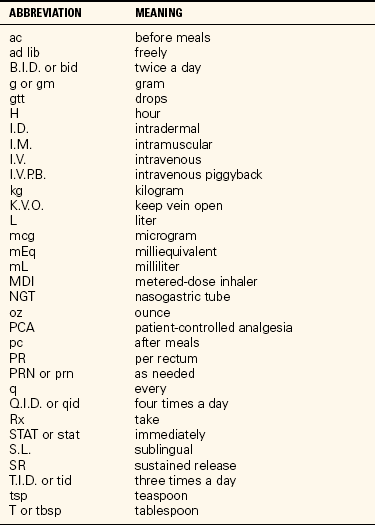
*Although the apothecary system and some other abbreviations are being discontinued because of medication safety concerns, these symbols and abbreviations are included because they are still sometimes encountered. For additional information and other error-prone abbreviations see www.ismp.org/tools/errorproneabbreviations.pdf.
DISTRIBUTION OF DRUGS
Health care facilities providing nursing care have a particular way of stocking and dispensing drugs. A medication room; a rolling, locked drug cart; a computerized drug cabinet; and individual storage units in the patient’s room are some of the methods used.
Stock supply drugs are in large, multidose containers, and each patient dose must be individually prepared. This is a time-consuming, costly method of dispensing drugs. An individual patient supply of drugs is usually kept in a bin or drawer labeled with the patient’s name. The pharmacist oversees placement in the drawer or bin of only the amount of a drug the patient will use for 12 to 72 hours. The patient is given only the drugs from the individual supply bin or drawer.
Unit dose refers to drugs packaged in single, individual doses (Safety Alert 33-3). Each unit dose contains the medication the patient is to receive at one particular time. Each dose is wrapped individually. In the unit-dose systems, the pharmacy will deliver a 24-hour supply of drugs for each patient. The patients’ medications are then stored in a drawer or a cart. The medications are refilled by the pharmacy each day. The cart or storage area may also contain a locked compartment with a select supply of common PRN and stock drugs for special needs. The system, when used properly, reduces medication errors and is time efficient.
A computer-controlled dispensing system such as the Pyxis system is especially useful for the delivery and control of narcotics and other scheduled drugs. Each nurse is assigned a security code allowing access to the system. The patient’s identification number must be entered and then the desired drug, dosage, and route are entered. The system gives the drug to the nurse, records it, and charges it to the patient. Sometimes a bar code system is used in conjunction with the dispensing system.
PROBLEMS OF NONCOMPLIANCE
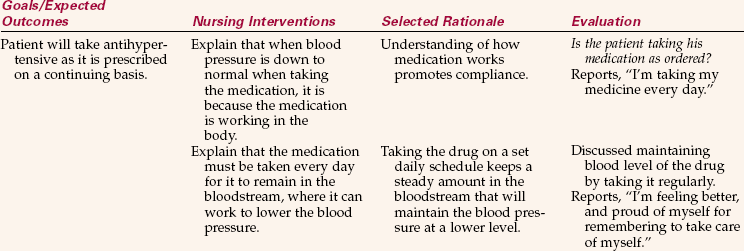
There are many reasons why patients do not take the drugs that are prescribed for them on the schedule that is indicated by the prescription (noncompliance). One reason is that the patient does not comprehend the action of the drug or why it is being taken. There is no understanding that a steady blood level is needed for it to work effectively. Understanding is needed to convince the patient to continue taking the drug when symptoms are gone.
Another reason for stopping a drug is that the patient cannot tolerate a side effect of the drug. In the male, urinary retention and sexual dysfunction are common reasons for noncompliance. Often a dosage adjustment or change in the drug prescribed will alleviate these problems. Otherwise if the drug is vital to the patient’s health, another medication may be used to ease the undesirable side effect in question.
Inability to purchase a medication is another reason for noncompliance. Medication is expensive, and many people do not have the extra money required to purchase their prescriptions. Patients often stop taking blood pressure medication because they cannot afford to buy more and, after taking the first round of the prescription, are feeling fine. Thorough patient teaching is needed so the patient understands that the medication is essential. Once the patient understands what can happen without medication, medication purchase may receive higher priority in the budget.
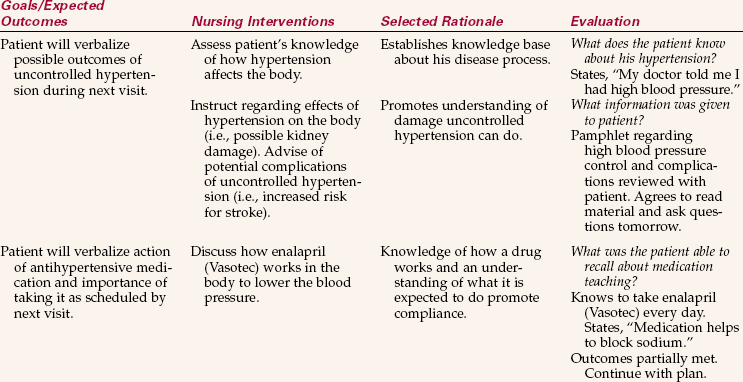
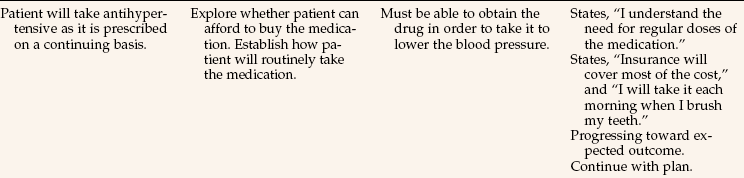
Some people do not like to have to depend on a chemical to get well or to maintain health. When alternative ways of alleviating their health problems can be found, they should be used. Otherwise good patient teaching is a tool available to increase compliance (Nursing Care Plan 33-1).
APPLICATION of the NURSING PROCESS
Assessment of the patient’s condition and medication history is essential before administering a medication. In accordance with 2009 National Patient Safety Goals, all health care staff should be participating in medication reconciliation. Medication reconciliation is a process of identifying all the patient’s medications and communicating this information to the patient and staff. This is particularly relevant when the patient is transferred to different providers, facilities, or units or discharged home. The process includes the following:
1. Listing all current medications
2. Listing all medications to be prescribed (i.e., preoperative medications)
3. Comparing lists for interactions
When you know about the patient’s medical problems, you can correlate the reason for the prescribed drug. When assessing for allergies, check all locations where allergies are listed on charts in your facility; also question the patient. You must know whether there are any contraindications (reasons not to administer) for giving the drug ordered by the route ordered. If giving a medication that affects vital signs, know the current readings prior to administration in order to determine if it will be safe to give the drug. If the drug has a narrow therapeutic range, it is important to assess the serum blood level of the drug. Check lab results for a serum drug level and determine whether it is within safe and therapeutic limits.
Assess information about each drug, noting how the drug works, its purpose, usual dosages, routes of administration, side effects, and the nursing implications for administration and monitoring the patient. Look at the other drugs listed on the medication administration record (MAR) (sheet listing medications prescribed and times to be given) and determine if there are any possible drug interactions with the drug you are about to give. Assess for any food interactions and counsel the patient appropriately.
Other factors to assess include whether the patient can swallow an oral medication, or has sufficient muscle tissue to absorb an intramuscular injection, and what site will be best to use for such an injection. Assess for side or adverse effects from previous doses of the drug. Determine the patient’s attitude about drugs because this may provide data about whether the patient is likely to be compliant with the medication regimen.
When working in a home care or clinic situation, assess for any patient limitations that might make self-administration difficult, such as poor eyesight, weakness or paralysis, or confusion and forgetfulness. If such limitations exist, assess for ways that the patient might receive the medications in a safe manner. Assess the patient’s knowledge about the drug therapy to determine areas of needed instruction.
Nursing Diagnosis
Possible nursing diagnoses for patients receiving drug therapy include the following:
Planning
Examples of expected outcomes are as follows:
• Patient verbalizes reason he is taking the drug.
• Before discharge, patient lists signs of adverse effects to report to physician.
Safely and accurately administering drugs requires preplanning. Unfamiliar drugs should be verified in reference handbooks before the scheduled time to give them. A medication administration schedule should be incorporated into the daily work organization plan. Specific planning is required to properly evaluate whether signs and symptoms of adverse effects are present in the patient. Time is planned for teaching the patient the information needed to safely take each drug prescribed.
Before administering a drug, check the Five Rights of medication administration (Safety Alert 33-4). Be sure you have the following:
During the 1990s, five more rules for safe administration of drugs were added to the Five Rights. They are as follows:
• Teach the patient about the drugs.
• Take a complete drug history.
• Assess the patient for drug allergies.
• Be aware of potential drug interactions with other drugs or foods.
Plan ahead whether you will need to take juice or milk and crackers to the patient in order for a particular drug to be taken. If a patient needs a drug crushed and mixed in applesauce or something else, take the supplies to the bedside with you. This saves a trip back to the workroom. If your patient will need to be helped to sit upright or has difficulty taking medications, plan to take extra time for that patient’s medication administration.
Before preparing medications for your assigned patients, verify which patients are NPO (nothing by mouth) for surgery or tests and which have an order to “hold breakfast.” Check with the charge nurse about giving these patients their medications when tests are completed. Dialysis patients also may need to have medications held, especially blood pressure medications, but this may vary by physician preference.
Check and replenish supplies such as medication cups, straws, water cups, and so forth on the medication cart before heading to patient rooms with the cart.
Implementation
When giving medications, the nurse is guided by many principles. Facility policies vary, but you will safely and accurately give medications if you follow these principles:
• Medications are given by the person who prepared them. If not given, the drug should not be returned to the drug cabinet or cart unless it is still in the unopened, labeled unit-dose package.
• Medications are not to be left at the bedside because they may be forgotten, lost, or taken by another patient. Exceptions may be made for drugs such as antacids, nitroglycerin, or birth control pills when so ordered in writing by the physician. Monitor their use and document the doses taken.
• Narcotics and other controlled drugs are kept in locked cabinets. You are legally responsible for the security of these cabinets and must account for each dose used.
• Check medication orders before giving drugs. Routinely compare medication records or medication cards with those drugs listed on the MAR to see that there are no errors or omissions. If there is a question about the accuracy, refer to the original order on the physician’s order sheet.
• Avoid distractions or interruptions when preparing or administering medications. Concentrate on the task to be done.
• Know about the drugs being given. Research information on unfamiliar drugs concerning their action, dosage, and any precautions to be followed.
• Observe the Five Rights and five rules when administering drugs.
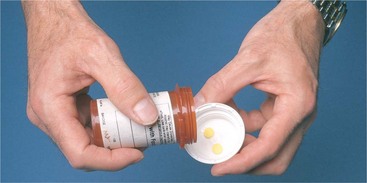
• Observe the principles of aseptic technique. Perform hand hygiene before beginning to dispense medications and after patient contact. Avoid touching the inside of medication containers or cups. Dispose of pills dropped on the floor. Do not handle or touch medications; pour the pills or tablets into the bottle cover and then transfer them into the medication cup (Figure 33-3).
• Obtain a complete medication history from the patient and look for possible drug interactions among the medications the patient is taking.
• Is the medication order consistent with the patient’s diagnosis and plan of treatment? If the answer is no, or if there is doubt, check it out with the charge nurse or physician.
• Is the medication similar in action to another medication the patient has been receiving? Is he still getting the other drug? If so, question both orders.
• Check the chart and MAR for listed patient allergies and ask the patient about allergies whenever you are administering medication; look for an allergy identification band.
• Teach the patient about the drug: what it looks like, its intended action, possible side effects, and how to take it. Explain why it should be taken with food or on an empty stomach and why it isimportant to take it on schedule (Patient Teaching 33-1).
• Check all MAR entries with the original order for accuracy at least once every 24 hours.
• If the patient questions the dose or the medication you are about to give, stop and verify the order.
• Check pertinent laboratory values and assess for side effects of the drug before giving the next dose of a medication.
• Avoid contamination of your own skin or inhalation to minimize chance of allergy or development of drug sensitivity.
• Document after the drug is given. Note the route, time, and site (if pertinent). Information about assessment for side effects from previous doses of the drug should be documented also. Include any patient teaching that was done about the medication, dosage schedule, or precautions.
Evolving technologies will contribute to safe and accurate medication administration. For example, eMedPass is a new user-friendly system that incorporates a touch screen of patient photos and medication icons. A nurse fingerprint identification process allows easy access while ensuring patient privacy. The nurse scans the medication bar code prior to administration and the system automatically documents this on an electronic MAR and reorders medications as needed.
Calculating the Drug Dosage to Be Given
Several methods can be used to accurately calculate the dosage to be given for a particular drug order. An example is given here as a refresher, because this information is usually covered in a nursing mathematics or pharmacology course.
Examples of Conversion Problems.: Sometimes it is still necessary to convert from one system of measurement to another, for example, from the metric to the apothecary system. The apothecary system is not exact for measurements. Current recommendations for safety in medication administration state not to use the apothecary system, but change in physician habits for prescribing medication comes slowly. There is variation of measurement conversion to the metric system. For example, one grain varies from 60 to 65 mg. The conversion should not vary by more than 10%. The equivalents must be memorized first (Box 33-2).
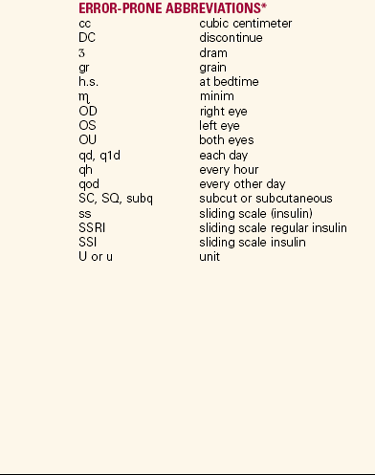
To set up a conversion problem, let us assume that grains need to be converted to milligrams. The order requests that 5 grains of medication be given (dose desired). On hand are tablets that contain 300 mg of medication (dose on hand). The following formula is used:
First convert milligrams to grains. The conversion problem is
Then calculate the total dose desired in milligrams. Dose on hand is 300 mg/tablet.

Give one tablet because one tablet is equivalent to 5 grains.
This method can also be used to convert within a measurement system, such as when grams need to be converted to milligrams. The order reads:
The order calls for 1.5 g of medication (amount desired). First convert the 1.5 g to milligrams. The conversion problem is:
On hand are 500-mg tablets. The dosage problem then would be:

One tablet contains 500 mg (amount on hand); 3 tablets = 1500 mg, or 1.5 g.
Drug Problem Formula.: You have an order for glipizide (Glucotrol), 2.5 mg to be given orally (D = dose desired). On hand you have Glucotrol, 5 mg per tablet (H = amount on hand). Set up the problem putting the unknown factor on top. (D and H need to be measured in like units, so do conversion problem first.)
Now cross-multiply, ignoring the units until the end.

(Because the x was in front of tablets, then x = 0.5 tablets.) Give ½ tablet.
For liquid medications, follow the same formula.
The order specifies guaifenesin, 75 mg PO tid. On hand is guaifenesin syrup, 100 mg per 5 mL.
The problem is set up as follows:

Give 3.75 mL of guaifenesin syrup.
For an injection, use the same formula.
The order reads meperidine, 35 mg IM q 4 hr PRN pain. On hand is meperidine, 50 mg per mL.

Practicing the Five Rights
1.: Give the Right Drug. Check MARs against the physician’s original orders on the chart periodically to make certain that the order was transcribed correctly. This task is usually done by the registered nurse during the night shift. Each time a drug dose is administered, the order is checked against the drug label for the correct name of drug. Check the expiration date of the drug at this time. If the spelling is different on the MAR or medication card than on the drug label, the original order is checked. If there is a discrepancy, the physician should be consulted. The patient is told the name of the drug and shown the medication before taking it.
Many nurses are now using a palm-held device (PHD) to quickly access drug information or do dosage calculations. Drug information software is available that can be installed and updated on these little computers.
2.: Give the Right Dose. Carefully compare the dose you are about to give with the dose indicated, as ordered on the MAR or medication card. The oral doses are supplied in standard amounts per pill or capsule. When the dose ordered is in milligrams rather than in capsules, tablets, or milliliters, a mathematical calculation is needed to ensure accuracy (Safety Alert 33-5). Many medication errors occur because the dosage given to the patient is not the dosage ordered.
3.: Give the Right Drug by the Right Route. If a drug is ordered intramuscularly, it must be given that way or the physician should be consulted and asked to change the order. The fact that the patient does not feel the need for pain medication by injection anymore does not mean that the nurse can give it in oral form. The order must be changed for the drug to be legally given orally.
In some cases, a drug is ordered to be given orally, but the patient cannot swallow the capsule or tablet. Look for how the drug is supplied to determine the safety of crushing. For example, sublingual, buccal, enteric-coated, and extended-release products and products with carcinogenic potential should not be crushed. The list of such drugs is extensive, covering several pages, and cannot be included here. When in doubt, check with the pharmacist. Certainly when a liquid form of the drug is available, a more exact dosage is achieved than with a crushed pill; a liquid dose is also more time-efficient for the nurse. When a liquid form is available, ask the physician to change the order.
4.: Give the Right Drug at the Right Time. The times at which patients are to receive medications should be written down on the work organization sheet. This is particularly important when a medication is slated to be given at a time other than the most common medication times during the shift.
Day-shift medications are most commonly given at 9 A.M. and 1 A.M.; medications ordered for 7:30, 8, 9:30, or 11 A.M., or any other nontraditional time, should be highlighted on the work sheet so that they are not forgotten. The agency protocol may state that a drug may be given within 30 minutes of the time ordered simply because it is not possible to give all the drugs ordered for a particular time to all patients exactly at the appointed time. In some acute care agencies, this flexibility means that the drug may be given from 30 minutes before the ordered time to 30 minutes after that time. Other agencies require that the drug be given within a 30-minute window from 15 minutes before the ordered time to 15 minutes after the time.
Nurses must remember that drug scheduling is for the purpose of maintaining a consistent level of the drug in the blood. For that reason, drugs should be given as close to the ordered time as possible. Antiarrhythmic heart medications in particular should be given very close to the appointed time. Document at the right time. Too often, nurses are in the habit of signing off on medications when they are taken from the medication cart drawer or bin. Frequently, the patient is not available to take the drug when the nurse reaches the room and, if things become hectic on the unit, the dose is forgotten. The patient may be off the floor, in the shower, severely nauseated, or in the middle of a respiratory treatment. Never document that a dose was given until it is in the patient. When a dose is not administered, it should also be noted on the MAR.
5.: Give the Right Drug to the Right Patient. Even though you are working with the patient continually throughout the shift and are very familiar with the person, you must identify the patient correctly by checking the armband information. It is safest to check the identification band for both name and identification number, verifying that these match the imprint on the MAR sheet.
A new method designed to prevent medication errors is using a bar code system. The FDA has formally recommended that the bar code method be adopted by all hospitals. The patient is issued a bracelet with an individual bar code on it. The same bar code is placed on the patient’s MAR and on each unit-dose medication dispensed by the pharmacy. The nurse scans the patient’s bracelet when administering medications. The scanner verifies that the same code is on the patient’s bracelet and on the medication packet (Figure 33-4). The nurse may also scan the bar code on her own identification tag and the system then documents that this particular nurse gave the medication.
To prevent medication errors, it is best to check each medication three times. Each of the Five Rights should be checked all three times. The third check should be done at the bedside before opening the unit-dose package. Because unit-dose systems have become the standard, nurses do not seem to check medications as carefully as they did when they used a stock drug supply. One method for instituting three checks using the Five Rights for each medication is listed in Box 33-3.
Oral medications should be given with the patient in as upright a position as possible and with sufficient fluid to carry the pills to the stomach. If the patient must remain recumbent, the side-lying position should be used to prevent aspiration.
Injection sites should be chosen carefully using anatomic landmarks and considering the size and physical condition of the patient. Sterility of medication and injection equipment must be maintained. To maintain Standard Precautions, gloves must be worn for administration of all injections. Intravenous medications must be given diluted in the recommended amount of fluid and administered no faster than the time recommended. Otherwise, toxicity or tissue damage may occur.
Evaluation
Evaluation of drug therapy is related to whether the desired therapeutic effect is occurring. For example, when antibiotics are being given, the temperature, the white blood cell count, and perhaps other laboratory values are assessed along with an evaluation of the patient’s general condition (e.g., how the patient feels). For other drugs, determine if the condition being treated is improving. Evaluation is also necessary regarding the occurrence of side effects of medications. Each patient is assessed for the signs and symptoms of side effects for every drug being administered.
Evaluate whether the expected outcomes listed on the nursing care plan or critical pathway are being met. If they are not, the plan of care must be revised.
Documentation
Record the drug given, dose, time, route, and your initials when documenting on an MAR. When documenting a PRN medication in the chart, write the date, time, reason the medication was given, dose and route, and location if it was given by injection, and sign with first initial, last name, and designation (student vocational nurse; SVN, SPN). When the medication has had sufficient time to take effect, the patient’s response to it should be documented. The PRN medication is also recorded on the MAR, noting the date, time, vital signs if required, and your initials.
Any time the patient has an adverse reaction or suffers from a side effect of a drug, a notation should be made in the chart. Any type of allergic reaction should be noted in all locations in which allergies are recorded in the patient record. Any patient concerns about the drug therapy should also be mentioned when documenting care. The patient is taught to carry allergy information in a billfold or to wear an allergy bracelet.
NCLEX-PN © EXAMINATION–STYLE REVIEW QUESTIONS
Choose the best answer(s) for each question.
1. The patient is to receive sequential doses of a drug. Based on your knowledge of pharmacologic action, the drug must be administered as close to the time scheduled as possible to:
1. maintain a minimum concentration of the drug in the patient’s bloodstream.
2. follow hospital policy and procedure and the physician’s orders.
3. help the patient understand the importance of taking drugs at regular intervals.
4. determine if side effects or adverse effects of the drug are going to occur.
2. The physician orders a medication blood level after making an adjustment in a patient’s prescribed dose of antiseizure medication. The purpose of monitoring this level would be because:
1. there are synergistic effects with other drugs.
2. the patient is suspected of noncompliance.
3. the drug has a narrow therapeutic range.
4. there is danger of anaphylaxis and other adverse effects.
3. When an elderly patient is taking an anti-inflammatory drug for arthritis on a continuing basis, the nurse would:
1. ask questions about whether constipation is occurring.
2. caution the patient to stay out of the sun because the skin is more sensitive.
4. The physician has just written several medication orders for several different patients. Which order has the highest priority?
1. Hydrocodone/acetaminophen (Lortab) 5 mg PO q 4-6 hr PRN pain
2. Lorazepam (Ativan) 2 mg IV bolus stat
5. The surgeon orders 500 mg PO tablets q 8 hr. The pharmacy delivers the medication in tablet form, but the patient tells the nurse that he cannot swallow the tablets and that his family doctor always gives him liquid medications. What is the most appropriate nursing action?
1. Gently encourage the patient to take the medication that the surgeon has ordered.
2. Call the pharmacy and ask them to send the liquid form of the medication.
3. Call the patient’s family doctor to verify what the patient usually takes.
4. Call the surgeon, explain the situation, and ask for the order to be changed.
6. A nurse has completed teaching a patient about several medications that he must use at home. These include Coumadin, vitamin C supplement, and a blood pressure medication. Which statement by the patient indicates an understanding of the medication teaching?
1. “If I need a follow-up blood test, the office nurse will call me.”
2. “I’ll take the medication because my doctor told me to.”
3. “My wife knows what to do if I miss a dose.”
4. “I know which foods to avoid while I am taking the medication.”
7. The nurse must give a medication to a child. The medication is ordered in mg/kg. The child weighs 44 lb. Convert the child’s weight to kilograms. ______
8. The pharmacy delivers a 6-oz bottle of take-home medication for a patient. The patient needs to take 25 mL of the medication every morning. The patient wants to know how many days the bottle will last. _________days
? CRITICAL THINKING ACTIVITIES Read each clinical scenario and discuss the questions with your classmates.
Scenario B
Florence Simoneski, age 78, is receiving Ecotrin, an enteric-coated aspirin, for her arthritis. She is hospitalized with dehydration and is very weak. She cannot swallow the Ecotrin tablets. What would you do?
 )
) )
)