Soft Tissue and Dentoalveolar Injuries
SOFT TISSUE INJURIES
The types of soft tissue injuries the dentist may see in practice vary considerably. However, it is fair to assume that given the current availability of other health care providers, the dentist will probably not be involved in the management of severe soft tissue injuries around the face. Those injuries seen with some frequency are the ones associated with concomitant dentoalveolar trauma or those that the dentist may inadvertently cause in practice.
In the following descriptions of the wounds the dentist may see in practice and their management, one must remember that patients may have combinations of these injuries; therefore, management may be more complicated.
Abrasion
An abrasion is a wound caused by friction between an object and the surface of the soft tissue. This wound is usually superficial, denudes the epithelium, and occasionally involves deeper layers. Because abrasions involve the terminal endings of many nerve fibers, they are painful. Bleeding is usually minor because it is from capillaries and responds well to application of gentle pressure.
The type of abrasions most commonly seen by laypersons are the scrapes that children sustain on their elbows and knees from rough play. If the abrasion is not particularly deep, reepithelialization occurs without scarring. When the abrasion extends into the deeper layers of the dermis, healing of the deeper tissues occurs with the formation of scar tissue, and some permanent deformity can be expected.
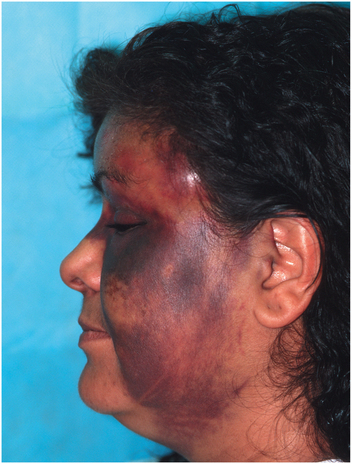
The dentist may see abrasions on the tip of the nose, lips, cheeks, and chin in patients who have sustained dentoalveolar trauma (Fig. 23-1). The abraded areas should be thoroughly cleansed to remove foreign material. Surgical hand soap and copious saline irrigation are useful for this purpose. All particles of foreign matter must be removed. If these particles are allowed to remain within the tissue, a difficult to treat permanent “tattoo” results. In deep abrasions that are contaminated with dirt or other material, it may be necessary to anesthetize the area and use a surgical scrub brush (or toothbrush) to remove the debris completely.

FIGURE 23-1 Patient with abrasions to the tip of nose, cheek, and forehead. Some of the abrasions are superficial, and some are deeper with peeling off of the epithelium.
Once the wound is free of debris, topical application of an antibiotic ointment is adequate treatment. A loose bandage can be applied if the abrasion is deep but is unnecessary in superficial abrasions. Systemic antibiotics are not usually indicated. Over the next week, reepithelialization will occur under the eschar, which is a crust of dried blood and serum that develops after an injury to soft tissue (e.g., a scab). The eschar will then drop off.
If a deep abrasion on the skin surface is discovered after wound cleansing, referral to an oral and maxillofacial surgeon is indicated because skin grafting may be necessary to prevent excessive amounts of scar formation.
The dentist may create abrasions iatrogenically, as occurs when the shank of a rotating bur touches the oral mucosa or when a gauze pack or other fabric (e.g., absorbent triangular pads) abrades the mucosa during removal from the mouth. Fortunately, the oral epithelium regenerates rapidly, and no treatment other than routine oral hygiene is indicated.
Contusion
A contusion is more commonly called a bruise and indicates that some amount of tissue disruption has occurred within the tissues, which resulted in subcutaneous or submucosal hemorrhage without a break in the soft tissue surface (Fig. 23-2).
Contusions are usually caused by trauma inflicted with a blunt object but are also frequently found with concomitant dentoalveolar injuries or facial bone fractures. In this instance, the trauma to the deeper tissues (e.g., floor of mouth or labial vestibule) has occurred from the disrupting effect of the fractured bones. The importance of contusions from a diagnostic point of view is that when they occur, one should search for osseous fractures.
A contusion generally requires no surgical treatment. Once the hydrostatic pressure within the soft tissues equals the pressure within the blood vessels (usually capillaries), bleeding ceases. If a contusion is seen early, the application of ice or pressure dressings may help constrict blood vessels and therefore decrease the amount of hematoma that forms. If a contusion does not stop expanding, a hemorrhaging artery within the wound is likely. The hematoma may require surgical exploration and ligation of the vessel.
Because there has been no disruption of the soft tissue surfaces, the body in time resorbs the hemorrhage formed within a contusion, and the normal contour is reestablished. In the next several days, however, the patient can expect areas of ecchymosis (i.e., purplish discoloration caused by extravasation of blood into the skin or mucosa; a “black-and-blue mark”), which turns a variety of colors (i.e., blue, green, and yellow) before fading. These areas may extend down below the clavicles and cause alarm, but they are innocuous.
When there has been no break in the surface of the soft tissue, infection is unlikely and systemic antibiotics are not indicated. If, however, the contusion results from dentoalveolar trauma, it is likely that communication may exist between the oral cavity and the submucosal hematoma. In this case, systemic antibiotics are warranted because coagulated blood represents an ideal culture medium.
Laceration
A laceration is a tear in the epithelial and subepithelial tissues. A laceration is perhaps the most frequent type of soft tissue injury and is caused most commonly by a sharp object, such as a knife or a piece of glass. If the object is not sharp, the lacerations created may be jagged because the tissue is literally torn by the force of the blow (Fig. 23-3). As with abrasions, the depth of a laceration can vary. Some lacerations involve the external surface only, but others extend deeply into the tissue, disrupting nerves, blood vessels, muscle, and other major anatomic cavities and structures.
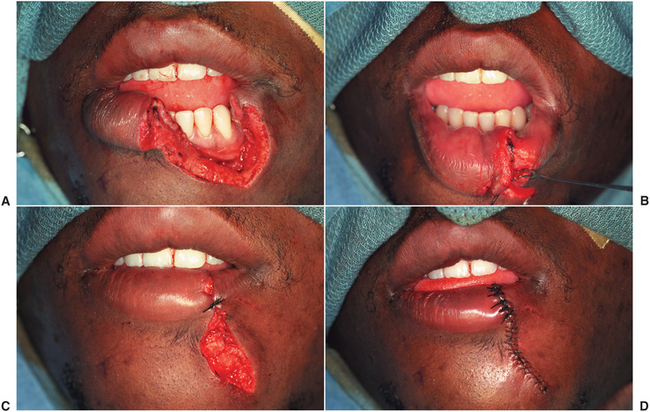
FIGURE 23-3 Photographs showing the repair of a full-thickness laceration of the lower lip. A, Tissues have been cleaned and hemostasis has been obtained. B, Muscle has been closed with interrupted 3-0 chromic catgut sutures. These sutures are the ones that primarily pull the tissues back together. The sutures should make it possible to close the skin without any tension. C, A 4-0 silk suture is placed at the mucocutaneous junction. This suture is critical because it aligns the vermilion border. If not done carefully, after healing a noticeable step or notch will show from misalignment. D, Skin and mucosal sutures are placed. Silk sutures were used to close the vermilion of the lip while nylon sutures were used to close the skin surface.
The dentist frequently encounters lacerations of the lips, floor of mouth, tongue, labial mucosa, buccolabial vestibule, and gingiva caused by trauma. One should explore the oral cavity thoroughly to identify ones that are not gaping. For instance, lacerations within the vestibule can be overlooked unless the lips are retracted, allowing a laceration to gape. Lip lacerations are commonly seen with dentoalveolar trauma, but in many instances of trauma the teeth are uninjured because the soft tissues have absorbed the force of the blow.
Soft tissue wounds associated with dentoalveolar trauma are always treated after the management of the hard tissue injury. If the soft tissue is sutured first, time is wasted because the sutures are likely to be stressed too much and pulled out of the tissue during the intraoral manipulation necessary to replant an avulsed tooth or treat a dentoalveolar fracture. Furthermore, once sutures have been pulled out of the tissues, the tissues will be more difficult to close on the second attempt.
After adequate anesthesia is provided, the surgical management of lacerations involves four major steps: (1) cleansing, (2) débridement, (3) hemostasis, and (4) closure. These steps apply to lacerations anywhere in the body, including the oral cavity and perioral areas.
Cleansing of Wound
Mechanical cleansing of the wound is necessary to prevent debris from remaining. Cleansing can be performed with surgical soap and may necessitate the use of a brush. An anesthetic is usually necessary. Copious saline irrigation is then used to remove all water-soluble material and to flush out particulate matter. Pulsed irrigation has been shown to be more effective in removing debris than is a constant flow of irrigation.
Débridement of Wound
Débridement refers to the removal of contused and devitalized tissue from a wound and the removal of jagged pieces of surface tissue to enable linear closure. In the maxillofacial region, which enjoys a rich blood supply, the amount of débridement should be kept to a minimum. Only tissue that is obviously not vital is excised. For most of the lacerations a dentist encounters, no débridement is necessary, except for minor salivary gland tissue (discussed later).
Hemostasis in Wound
Before closure, hemostasis must be achieved. Continued bleeding might jeopardize the repair by creating a hematoma within the tissues that can break the tissues open once they are sutured closed. If any bleeding vessels are identified, they should be clamped and tied with ligatures or cauterized with an electrocoagulation unit. The largest vessel the dentist will probably encounter is the labial artery, which runs horizontally across the lip just beneath the labial mucosa. Because of its position, the labial artery is frequently involved in vertical lip lacerations. This artery is approximately 1 mm in diameter and usually can be clamped and tied, or clamped and cauterized.
Closure of Wound
Once the wound has been cleansed, débrided, and hemostasis achieved, the laceration is ready to be closed with sutures. However, not every laceration in the oral cavity must be closed with sutures. For example, a small laceration in the palatal mucosa caused by falling on an object extending from the mouth need not be closed. Similarly, a small laceration on the inner aspect of the lip or tongue caused by entrapment between the teeth during a fall usually does not require closure. These small wounds heal well by secondary intention and are best left to do so.
If closure of a laceration is deemed appropriate, the goal during closure is proper positioning of all tissue layers. The manner in which closure proceeds depends totally on the location and depth of the laceration.
When lacerations of the gingiva and alveolar mucosa (or floor of mouth) are noted, they are simply closed in one layer. If a patient has a laceration of the tongue or lip that involves muscle, resorbable sutures should be placed to close the muscle layer or layers, after which the mucosa is sutured. Minor salivary gland tissue protruding into a wound can be judiciously trimmed to allow for a more favorable closure.
In lacerations extending through the entire thickness of the lip, a triple-layered closure is necessary (Fig. 23-4). If the laceration involves the vermilion border, the first suture placed should be at the mucocutaneous junction. Perfect alignment of this junction of skin and mucosa is imperative, or it can result in a noticeable deformity that can be seen from a distance. Once this suture is placed, the wound is closed in layers from the inside out. The oral mucosa is first closed with silk or resorbable suture. The orbicularis oris muscle is then sutured with interrupted resorbable sutures. Finally, the dermal surface of the lip is sutured with 5-0 or 6-0 nylon sutures. The wound will look as good at the completion of suturing as it ever will. If the alignment of tissues appears poor, consideration should be given to removing the sutures and replacing them in a more favorable manner. The dermal surface should then be covered with an antibiotic ointment.
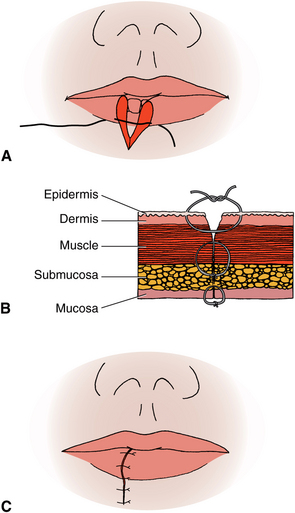
FIGURE 23-4 Illustrations showing the closure of a lip laceration or incision. A, Critical suture is placed at mucocutaneous junction. Realign of mucocutaneous junction is critical; otherwise, cosmetic deformity will be noticeable. B and C, Lip is closed in three layers: (1) oral mucosa, (2) muscle, and (3) dermal surface. Choice of suture for oral and dermal surfaces varies with surgeon; however, muscle layer should be closed with chromic or plain catgut (resorbable) suture.
Once a laceration is closed, the clinician must consider what supportive therapy can be instituted to bring about uneventful healing. Systemic antibiotics (e.g., penicillin) should be considered whenever a laceration extends through the full substance of the lip. In superficial lacerations, antibiotics are not indicated. The patient’s tetanus status should be ascertained; if in doubt, patients should be referred to their physicians. Patients should also be instructed in postsurgical diet and wound care.
Generally, facial skin sutures should be removed 4 to 6 days postoperatively. When removing a suture, it should be cut and then pulled in a direction that does not cause the wound to gape. Adhesive strips can be placed at the time of suture removal to give external support to the healing wound.
DENTOALVEOLAR INJURIES
Dentoalveolar and perioral soft tissue injuries frequently occur and are caused by many types of trauma. The most common causes are falls, motor vehicle accidents, sports injuries, altercations, child abuse, and playground accidents. Falling causes many injuries, which starts when a child begins to walk and peaks just before school age.1 The dentist is likely to be called by a frantic parent whose child has just fallen and is bleeding from the mouth. Dentists must be familiar with dentoalveolar injuries so that they can effectively manage them when they occur.
A force directly on a tooth or an indirect force, most commonly transmitted through overlying soft tissues (e.g., the lip), may cause dentoalveolar injuries. Injuries of the surrounding soft tissues almost always accompany injuries to the dentoalveolus. For example, gingival tissues may be torn; the lower lip may have been caught between the teeth during the injury, creating a full-thickness laceration; or the floor of the mouth may be lacerated. Knowledge of management techniques for injuries to the dentoalveolus and the soft tissues is necessary to allow the dentist to treat these injuries effectively.
Management of Dentoalveolar Injuries
Injuries to the teeth and alveolar process are common and should be considered emergency conditions because a successful outcome depends on prompt attention to the injury. Because proper treatment can be given only after an accurate diagnosis, the diagnostic process should commence immediately.
History
The first step in any diagnostic process should be to secure an accurate history. A comprehensive history of the injury should be obtained from the patient, incorporating information on who, when, where, and how. The dentist must ask the following questions of the patient, parent, or a reliable respondent:
1. Who is the patient? Included in the answer should be the patient’s name, age, address, telephone number, and other pertinent demographic data. It is imperative that this data be obtained quickly and that time not be wasted.
2. When did the injury occur? This is one of the most important questions to ask because studies have shown that the sooner an avulsed tooth can be repositioned, the better the prognosis.2 Similarly the results of treating displaced teeth, crown fractures (with and without exposed dental pulps), and alveolar fractures may be influenced by a delay in treatment.1,3
3. Where did the injury occur? This question may be important because the possibility and degree of bacterial or chemical contamination should be ascertained. For example, if a child falls on the playground and gets dirt in the wound, a tetanus prophylaxis history should be carefully established. However, if an injury occurs from a clean object held in the mouth, gross bacterial contamination from external sources is not expected.
4. How did the injury occur? The nature of the trauma provides valuable insight into what the resultant tissue injury is likely to be. For example, an unrestrained car passenger who is thrown forward into the dashboard with sufficient force to damage several teeth may also have sustained occult injuries to the neck. The manner in which the injury occurred is valuable information and should make the clinician investigate the possibility of further injuries. Additional information that can be gained from this question may relate to the cause of the injury. If a patient cannot remember what happened, a preexisting medical condition, such as a seizure disorder, may have caused the accident producing the injury. Injuries caused by possible negligence by others are open for litigation. These considerations should caution the clinician to document the findings carefully and word any discussions with the patient thoughtfully. One other thought that must be kept in the clinician’s mind when examining children whose injuries do not seem to be a likely result of the injury described by the parent is child abuse.
Unfortunately, child abuse has become more prevalent in recent years, and a high degree of suspicion may be the only manner by which it can be discovered by health care providers.
5. What treatment has been provided since the injury (if any)? This question elicits important information regarding the original condition of the injured area. Did the patient or parent replant a partially avulsed tooth? How was the avulsed tooth stored before presentation to the dentist?
6. Did anyone note teeth or pieces of teeth at the site of the accident? Before an accurate diagnosis and treatment plan are made, it is imperative that each tooth the patient had before the accident be accounted for. If, during the clinical examination a tooth or crown is found missing and no history suggests that it was lost at the scene, radiographic examination of the perioral soft tissues, the chest, and the abdominal region is necessary to rule out the presence of the missing piece within the tissues or other body cavities (Fig. 23-5).
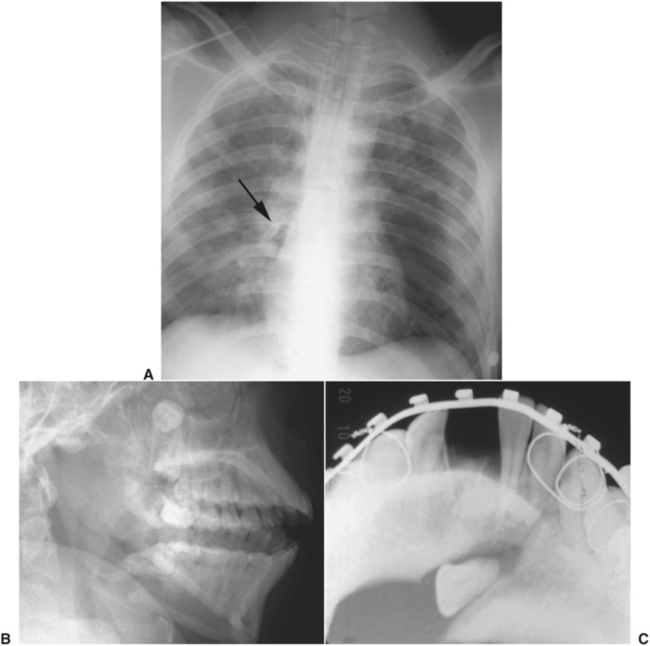
FIGURE 23-5 Teeth displaced into abnormal locations. A, Chest radiograph showing maxillary canine tooth in right main stem bronchus after traumatic displacement. B, Molar displaced into the maxillary sinus from maxillary fracture. C, Incisor tooth in line of fracture preventing anatomic reduction.
7. What is the general health of the patient? A succinct medical history is essential; it should not be ignored in the dentist’s haste to replant an avulsed tooth. The history, however, can be performed concomitantly with treatment or immediately thereafter. A history that touches on drug allergy, heart murmur, bleeding disorder, other systemic disease, and current medications should be taken before treatment because their existence affects the treatment the dentist will provide.
8. Did the patient have nausea, vomiting, unconsciousness, amnesia, headache, visual disturbances, or confusion after the accident? An affirmative answer to any of these questions may indicate intracranial injury and direct the dentist to obtain medical consultation immediately after completing treatment. Immediate referral should be made if the patient is still having any of the symptoms or if the patient does not feel or look well. The patient’s life should not be jeopardized to save an avulsed tooth.
9. Is there a disturbance in the bite? An affirmative answer to this question may indicate tooth displacement or dentoalveolar or jaw fracture.
Clinical Examination
The clinical examination is perhaps the most important part of the diagnostic process. A thorough examination of a patient who has had injury to the dentoalveolar structures should not focus only on that structure. Concomitant injuries may also be present; the history may direct the dentist to examine other areas for signs of injury. Vital signs such as pulse rate, blood pressure, and respiration should be measured. Such tests can usually be obtained during the taking of the history. The mental state of the patient is also assessed throughout the taking of the history and while performing the clinical examination by observation of the manner in which the patient reacts to the examination and responds to the questioning. During the clinical examination, the following areas should be examined routinely:
1. Extraoral soft tissue wounds. Lacerations, abrasions, and contusions of the skin are common with dentoalveolar injuries and should be noted. If a laceration is present, the depth of it should also be determined. Does the laceration extend through the entire thickness of the lip or cheek? Are there any vital structures, such as the parotid duct or facial nerve, crossing the line of the laceration? An oral and maxillofacial surgeon best treats major lacerations such as these.
2. Intraoral soft tissue wounds. Injuries to the oral soft tissues are commonly associated with dentoalveolar injuries. Before a thorough examination, it may be necessary to remove blood clots, irrigate with sterile saline, and cleanse the oral cavity. Areas of bleeding usually respond to pressure applied through gauze sponges. Soft tissue injuries should be noted, and an examination should ascertain whether any foreign bodies, such as tooth crowns or teeth, remain within the substance of the lips, floor of mouth, cheeks, or other areas. The dentist should also note areas of extensive loss of soft tissues; blood supply to a segment of tissue may thereby be lost.
3. Fractures of the jaws or alveolar process. Fractures of the jaws are most readily found on palpation. However, because pain may be severe after the injury, examination can be difficult. Bleeding into the floor of the mouth or into the labial vestibule may indicate a fracture of the jaw. Segments of alveolar process that have been fractured are readily detected by visual examination and palpation.
4. Examination of the tooth crowns for the presence of fractures or pulp exposure. For adequate examination, the teeth should be cleansed of blood. Any fractures should be noted. The depth of the fracture is important to note. Does it extend into dentin or into the pulp?
5. Displacement of teeth. Teeth can be displaced in any direction. Most commonly they are displaced in a buccolingual direction, but they may also be extruded or intruded. In the most severe type of displacement, the teeth are avulsed, that is, totally displaced out of their alveolar process. Observation of the dental occlusion may provide assistance in determining minimal degrees of tooth displacement.
6. Mobility of teeth. All teeth should be checked for mobility in the horizontal and vertical directions. A tooth that does not appear to be displaced but that has considerable mobility may have sustained a root fracture. If adjacent teeth move with the tooth being tested, a dentoalveolar fracture (in which a segment of alveolar bone and teeth are separated from the remainder of the jaw) should be suspected.
7. Percussion of teeth. When a tooth does not appear to be displaced but pain is felt in the region, percussion determines whether the periodontal ligament has undergone some injury.
8. Pulp testing of teeth. Although rarely used in acute injuries, vitality tests (which induce a reaction from the teeth) may direct the type of treatment the teeth will receive once the injury has healed. False-negative results may occur, so the teeth should be retested several weeks later and before endodontic therapy is performed.
Radiographic Examination
A host of radiographic techniques are available to evaluate dentoalveolar trauma. Most techniques can be readily performed in the dental office with available equipment. Most commonly a combination of occlusal and periapical radiographs is used. The radiographic examination should provide the following information4:
2. Degree of extrusion or intrusion
3. Presence of preexisting periapical disease
5. Size of the pulp chamber and root canal
7. Tooth fragments and foreign bodies lodged in soft tissues
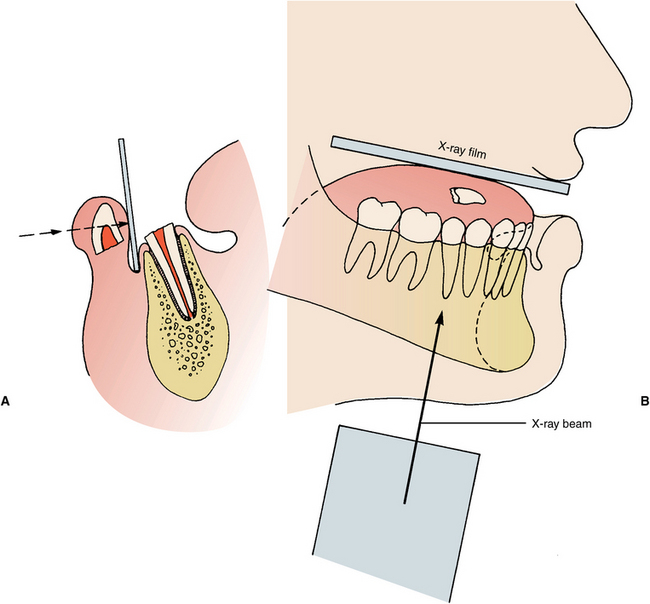
A single radiograph may not be sufficient to demonstrate a root fracture.1 For a radiograph to demonstrate a fractured root, the central beam of the x-ray device must be parallel to the line of fracture; otherwise, the fracture may not be clearly seen (Fig. 23-6). Multiple views with differing vertical and horizontal angulations of the central ray may be necessary.
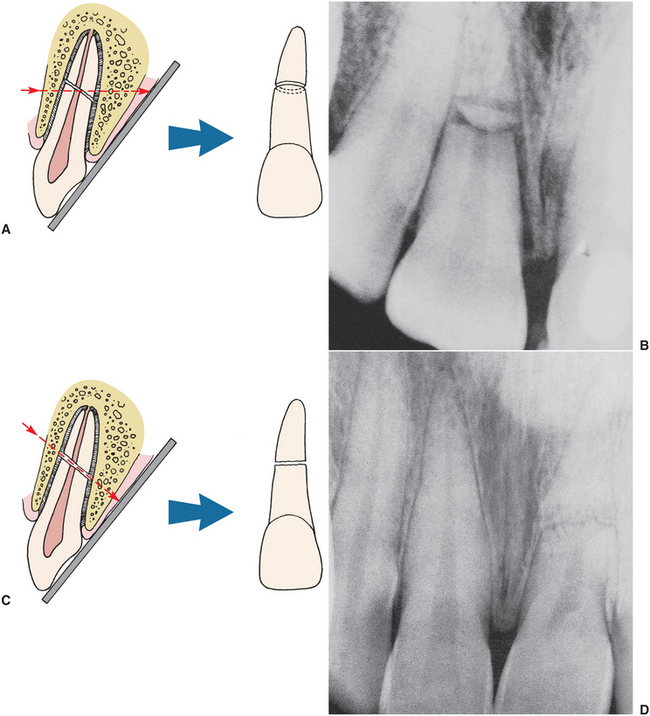
FIGURE 23-6 Effect of vertical angulation of central x-ray beam on the detection of horizontal root fracture. When central ray is not parallel to fracture (A), either a double fracture (B) or no fracture at all may be observed on radiograph. When central ray is parallel to fracture (C), fracture appears on radiograph (D).
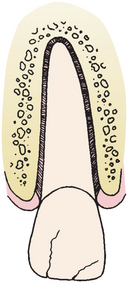
Displaced teeth may show a widening of the periodontal ligament space or displacement of the lamina dura. Extruded teeth may demonstrate a conic periapical radiolucency (Fig. 23-7). Intruded teeth may show minimal radiographic findings because of the continued close adaptation of the lamina dura and the root surface. Frequently, however, intruded teeth show an absence of the periodontal ligament space.
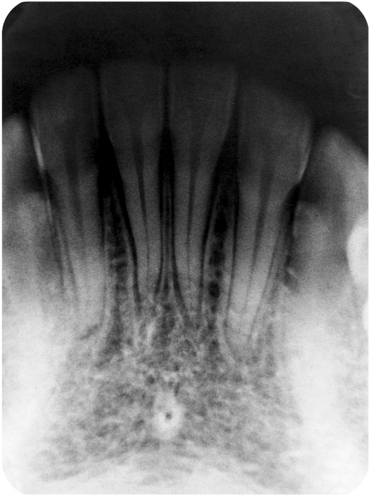
FIGURE 23-7 Radiograph showing widened periodontal ligament spaces around several teeth that are displaced coronally.
Radiographic evaluation for foreign bodies within the soft tissues of the lips or cheeks are taken with the radiographic film placed inside the soft tissues to be examined, labial to the alveolus (Fig. 23-8, A). A reduced radiographic exposure time is used (approximately one third of normal). Foreign bodies in the floor of the mouth are viewed with cross-sectioned occlusal radiographs, also with reduced radiographic exposure time (Fig. 23-8, B).
Classification of Traumatic Injuries to the Teeth and Supporting Structures
Many systems are used for the description of dentoalveolar injuries, all of which have advantages and disadvantages. A relatively simple yet useful classification was presented by Sanders et al.4 (Box 23-1). Their method is based entirely on a description of the injury sustained during the traumatic episode, describing the tooth structures involved, the type of displacement, and the direction of crown or root fracture.
Treatment of Dentoalveolar Injuries
After conducting a thorough history and clinical and radiologic examinations, the dentist should be able to determine whether the treatment plan for the patient’s type of injury is within the clinician’s range of expertise. Several circumstances may render an otherwise minor injury untreatable by the dentist alone. A problem the dentist frequently encounters is the uncooperative patient, most commonly a child. The combination of the traumatic episode and the child’s fear of the dentist may render a simple surgical procedure impossible without general anesthesia. Another difficulty is the patient with multiple medical problems. When dentists do not think that they can effectively manage a patient because of surgical difficulty, anesthesia requirement, concomitant medical problems, or other reasons, an oral and maxillofacial surgeon should immediately be consulted for assistance with treatment.
The goal in the treatment of dentoalveolar injuries is reestablishing normal form and function of the masticatory apparatus. When the pulp is directly involved, treatment differs from that of tooth injuries in which the pulp is not involved. Because of the training in operative dentistry and endodontics, a dentist has the knowledge, the instrumentation, and the medications routinely available to manage cases of tooth fracture. The treatment regimen for these injuries is therefore outlined only briefly. More severe injuries, such as tooth dislocations, avulsions, or dentoalveolar fractures, are fields in which the dentist may have had little training; these are presented in greater detail.
Primary teeth that have been injured are generally treated in a manner similar to that for permanent teeth. However, in many instances, the lack of cooperation by the child results in treatment compromises and, frequently, extraction of the damaged tooth. If this occurs, the dentist should consider space maintenance measures in the near future where indicated.
Crown Craze or Crack
Because the cracks are limited to the enamel (i.e., enamel infraction) and usually stop before reaching the dentinoenamel junction, no treatment is usually indicated. However, because any force to the tooth can result in injury to the pulp and periodontal tissues, periodic follow-up examinations are valuable (Fig. 23-9). Multiple cracks may be sealed with an unfilled resin to prevent their becoming stained.
Crown Fracture
The depth of tooth tissue involvement determines the treatment of crown fractures.5 For fractures that are only through the enamel or those with minimal amounts of dentin involvement, no acute treatment other than smoothing off the sharp edges is warranted. If reshaping the teeth would leave a noticeable deformity, replacement of the missing enamel by acid-etched composite resin techniques is indicated. The sooner the teeth are treated, the better the prognosis, because inflammatory hyperemia of the pulp is decreased. Periodic follow-up examinations are necessary to monitor pulp and periodontal health (Fig. 23-10).
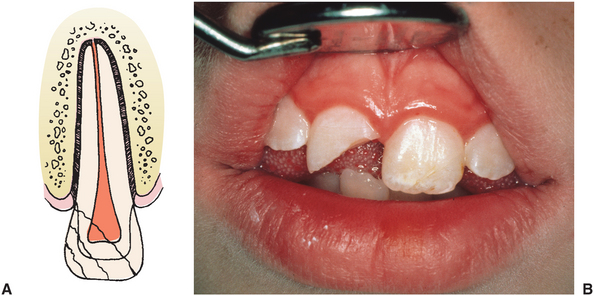
FIGURE 23-10 A, Coronal fractures involving enamel, dentin, and pulp. B, Photograph of a coronal fracture that involved enamel and dentin.
If a considerable amount of dentin is exposed, the pulp must be protected. Measures to seal the dentinal tubules and promote secondary dentin deposition by the pulp can be undertaken. Calcium hydroxide has been the traditional material applied to the exposed dentin before the fractured part is covered with a suitable restoration, most commonly a composite with or without acid etching. Current recommendations are the placement of a dentin-bonding agent or glass ionomer cement over the exposed dentin, followed by the placement of a resin composite restoration.6 Glass ionomer cements chemically bind to dentin, facilitating placement and restoration. The status of pulp vitality at periodic follow-up visits dictates what the final treatment plan will be. If pulp and periodontal health are satisfactory, no more intervention is necessary other than for esthetic reasons.
If the pulp is exposed, the aim of treatment is to preserve it in a vital, healthy state. This can usually be accomplished by pulp capping if five conditions are present: (1) the exposure is small, (2) the patient is seen soon after injury, (3) the patient had no root fractures, (4) the tooth has not been displaced, and (5) no large or deep fillings exist that might indicate chronic inflammation within the pulp. The most common injury for which pulp capping is instituted is in a tooth in which a single pulp horn was exposed with a crown fracture.
The more apically immature the tooth, the more favorable is the response the dentist can expect from pulp capping. As with any operative procedure on the dental pulp, isolation with a rubber dam is recommended. After application of calcium hydroxide on the exposed pulp, glass ionomer cement is placed over the exposed dentin and a watertight acid-etch composite restoration is placed (Fig. 23-14).
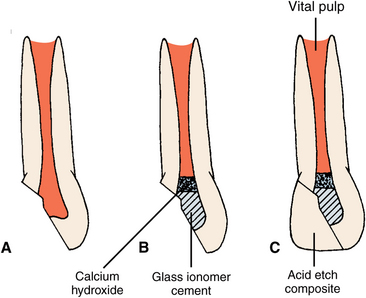
FIGURE 23-14 Pulpotomy technique. A, Apically immature tooth with coronal fracture involving pulp. B, Coronal pulp removed aseptically, after which calcium hydroxide solution is applied over exposed pulp. Glass ionomer cement can then be used to fill remainder of coronal pulp chamber, and temporary or permanent (i.e., composite) filling is placed (C).
A pulpotomy involves aseptic removal of damaged and inflamed pulp tissue to the level of clinically healthy pulp, after which calcium hydroxide is applied. A pulpotomy is usually implemented in larger exposures in which the apex is not closed. In these instances a pulpotomy should be only a temporary measure to maintain the vitality of the radicular pulp until the apex is closed. Endodontic therapy should then be instituted.
Periodic follow-up examinations are mandatory after any pulpal procedure. The final restorative decision is based on the pulpal health of the tooth. Because the prognosis is guarded, endodontic treatment may be necessary if the pulp degenerates.
Another technique that can be used to restore the tooth is by replacing the original fractured tooth fragment using the acid-etch technique or with the newer enamel and dentin adhesives.7 This technique is particularly useful for large fractures.
Crown-Root Fracture
The treatment of crown-root fractures depends on the location of the fracture and local anatomic variance. If the coronal fragment is still in place, it must be removed to assess the depth to which the fracture has gone. If the fracture does not descend too far apically (and the tooth is therefore restorable) and if the pulp has not been exposed, the tooth is treated as already discussed for crown fracture.
Depending on the apical extent of the fracture, it may be necessary to perform periodontal procedures to make the apical margin of the fracture accessible for restorative procedures. Alternatively, orthodontic extrusion of the root can make it accessible for restorative procedures. If the pulp is involved and the tooth is restorable, endodontic treatment is implemented. If, however, the tooth is not restorable, removal is indicated. If a concomitant alveolar fracture is found, the extraction may be delayed for several weeks to permit the fracture to heal and thus prevent undue loss of alveolar bone at the time of extraction (Fig. 23-11).
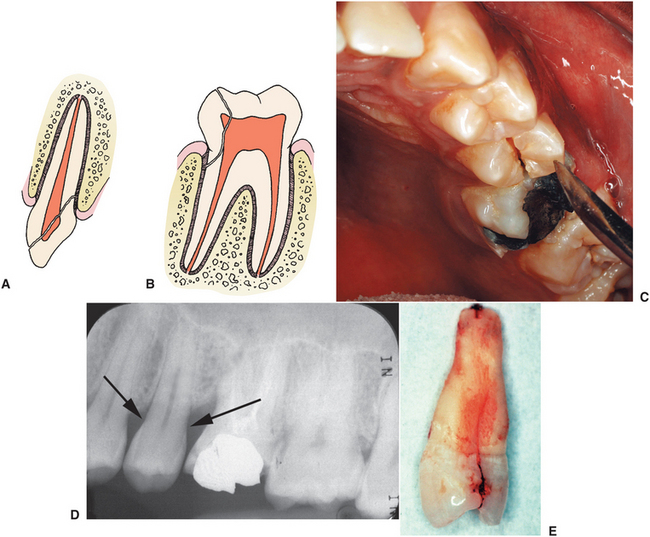
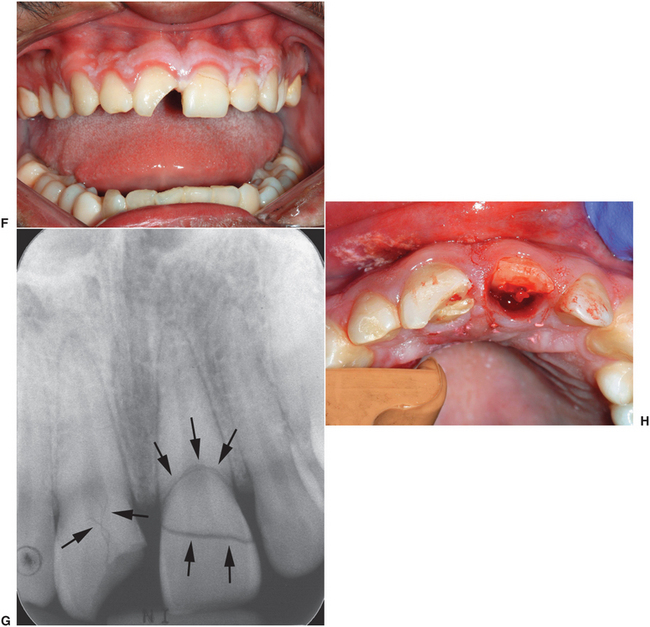
FIGURE 23-11 Crown-root fractures. A and B, Illustrations of crown-root fractures in incisor and molar, respectively. Fractures extend below alveolar crest of bone. C, Clinical photograph of crown-root fracture in premolar. This tooth is commonly fractured in this manner, especially when there is a restoration extending across the occlusal surface (i.e., MOD). D, Radiograph of this premolar showing no obvious fracture because the fracture is in the mesiodistal direction. E, Tooth after extraction showing the fracture extending apically. F, Clinical photograph of two incisors with crown-root fractures. Tooth No. 8 appears to have only a fracture of the crown, but the radiograph (G) shows that there are fracture lines extending into the root. Similarly, the clinical examination does not reveal the depth of the fracture on tooth No. 9, but the radiograph (G) shows it extends apical to the cementoenamel junction. After the loose crown portion was removed, the fracture was found to involve the pulp and to extend well above the cementoenamel junction (H). Both of these teeth were removed and replaced with dental implants.
Horizontal Root Fracture
When a horizontal or oblique fracture of the root occurs, the main factor in determining the prognosis and therefore in directing treatment is the position of the fracture in relation to the gingival crevice. If the fracture is above or close to the gingival crevice, the tooth should be removed or the coronal fragment should be removed and endodontic treatment performed on the root. The root can then be restored with a post and core restoration. Fractures in the middle to apical one third of the root have a good prognosis for survival of the pulp and healing of the root fragments to one another. These fractures should be treated with repositioning (if any mobility is detectable) and firm immobilization for 2 to 3 months (these techniques are described later). During this time, bridging of the fracture with calcified tissue usually occurs, and the tooth remains vital (Fig. 23-6 and 23-12).
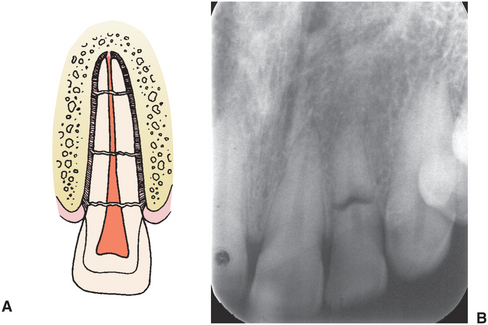
FIGURE 23-12 A, Illustration showing horizontal root fractures at apical, middle, and coronal levels of root (top, middle, and bottom, respectively). B, Radiograph of a horizontal root fracture at the junction of the coronal and middle thirds. This tooth was extremely mobile, so it was removed and replaced with an immediate dental implant. Figure 23-6, B, shows a radiograph of a horizontal root fracture at the junction of the apical and middle thirds. This tooth had slight mobility but was stabilized, and it healed.
Sensitivity
No acute treatment is recommended for sensitivity (i.e., concussion) other than symptomatic relief, such as relieving the tooth from occlusal contact. This is easiest to perform by grinding the occlusal contacts from the opposing tooth. Follow-up examinations should be instituted to monitor periodontal and pulpal health.
Mobility
If the tooth is only mildly mobile, relieving the occlusal contact is effective treatment. Most mobile teeth stabilize (i.e., “tighten up”) with time. If the tooth is extremely mobile, splinting it to adjacent teeth is recommended (described later). Periodic observation is then necessary.
Intrusion
Traumatic intrusion of teeth indicates that the alveolar socket has sustained a compression fracture to permit the new tooth position. On percussion the tooth emits a metallic sound similar to an ankylosed tooth, distinguishing it from a partially erupted or unerupted tooth. The intrusion may be so severe that the tooth actually appears to be missing on clinical examination. Traumatic tooth intrusion is less frequent than lateral displacements; when seen, intrusion usually involves maxillary teeth. This type of nonavulsive tooth displacement has the worst prognosis (Fig. 23-13).
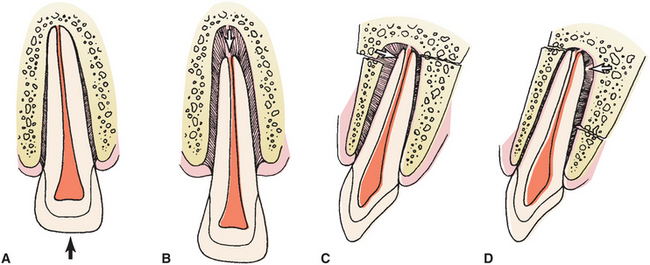
FIGURE 23-13 Tooth displacement. A, Intruded tooth. The absence of periodontal ligament space along apex is demonstrated. B, Tooth displaced from its socket in coronal direction (i.e., extruded). C and D, Displacement of incisor tooth crown buccally and lingually, respectively. Associated alveolar wall fractures, which are frequently present, are visualized.
The treatment of intruded teeth is controversial. Some clinicians favor surgically repositioning and splinting the teeth; however, this treatment has resulted in serious periodontal and pulpal consequences. Others think that, if left alone, many intruded teeth will reerupt. Others use orthodontic forces to assist reeruption of the tooth (Fig. 23-15).

FIGURE 23-15 Treatment of intruded maxillary incisors with immature apices. Buccal (A) and palatal (B) views of intruded maxillary incisor teeth. C, Orthodontic traction instituted to extrude teeth a few weeks after traumatic episode. D, Appearance after 6 weeks of traction. E, Stabilization of teeth after orthodontic-guided reeruption with acid-etch technique for 11 weeks. F, Appearance after 1 year. This patient had calcium hydroxide pulpectomies and apexification during period of orthodontic extrusion and subsequently had root canals. (From Spalding PM, Fields HW Jr, Torney D et al: The changing role of endodontics and orthodontics in the management of traumatically intruded permanent incisors, Pediatr Dent 7:104, 1985.)
When orthodontic assisted eruption is used, the tooth should be extruded slowly, over a 3- to 4-week period. Once the tooth is in position within the dental arch, it is splinted for 2 to 3 months. Recent evidence suggests that immediate application of orthodontic force is necessary to prevent ankylosis in the intruded position.8 The decision to perform endodontic treatment is based on the follow-up findings of each case.
However, if the intrusion occurred in an apically mature tooth, pulpal degeneration is likely and endodontic treatment should be performed as described later.
If a deciduous tooth has been intruded to the point that it is touching the follicle of a succedaneous tooth, the deciduous tooth should be removed as atraumatically as possible. If the deciduous tooth is not in direct proximity to the succedaneous tooth, a period of observation should be followed because reeruption is common. If the dentist is in doubt about the position of a deciduous tooth, removal is a sound prophylactic approach that helps to ensure the health of the succedaneous tooth.
Extrusion
Extruded teeth can usually be manually seated back into their sockets if the injury was recent. After replacement of the tooth within the socket, splinting for 1 to 3 weeks is usually necessary, as is endodontic treatment (discussed later; Fig. 23-13, B, and 23-16).
Lateral Displacement
If a tooth is minimally displaced, the accompanying alveolar wall fractures may not be grossly displaced. In this case, manual repositioning of the tooth and splinting for several weeks is indicated. When substantial tooth displacement has occurred, displaced alveolar bone fractures have also been sustained (Fig. 23-13, C and D). Gingival lacerations frequently accompany this type of injury. The tooth and the alveolar bone must be manually repositioned, the tooth splinted, and soft tissues sutured (Fig. 23-17).
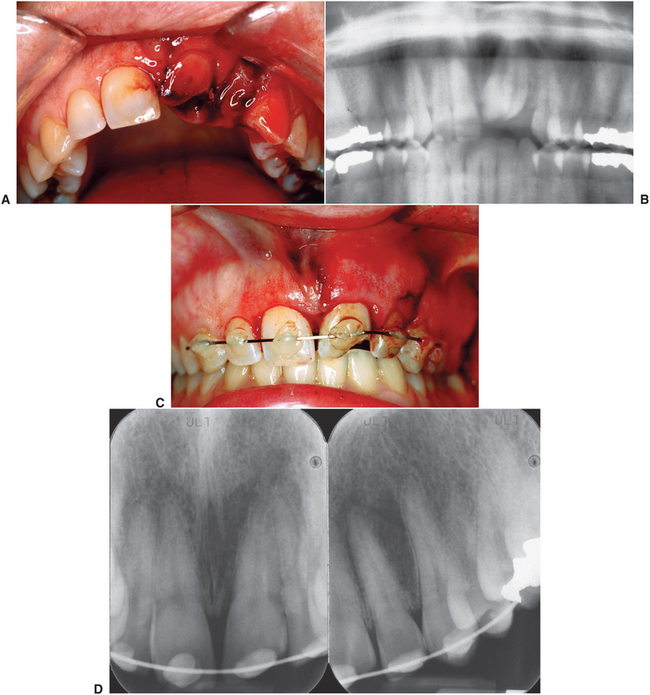

FIGURE 23-17 Treatment of lingually displaced central and lateral incisors in apically mature tooth. A, Appearance on presentation. B, Radiograph showing position of the teeth and the lack of root fracture(s). C, Position of teeth after digital reduction and stabilization with an arch wire bonded to the teeth with composite resin. D, Immediate postreduction radiograph showing that the teeth have been replaced into their sockets. E, Clinical appearance at 3 weeks just before the arch wire was removed. F, Clinical appearance 1 week after arch wire removed. The patient was sent for endodontic therapy (G), and composite was used to reconstruct the missing portion of the crown of tooth No. 9 (H).
Postsurgical follow-up examinations will determine the state of the pulp and periodontal damage.
Avulsion
Total avulsion from its socket is the gravest situation for a tooth because the health of the pulp and the periodontal tissues is in severe jeopardy. The factors most important for determining how successful treatment measures will be are the length of time the tooth has been out of the socket, the state of the tooth and periodontal tissues, and the manner in which the tooth was preserved before replantation. The sooner the tooth can be replanted, the better the prognosis.2
Therefore, when the dentist receives a call from a patient, parent, teacher, or other responsible person regarding a totally avulsed tooth, the dentist should direct the caller to rinse the tooth immediately with the patient’s saliva, tap water, or saline solution and to replant the tooth. The patient should hold the tooth by the crown, while trying to not touch the root, and then hold the tooth in place and go immediately to the dentist. If the patient cannot replace the tooth, it should be placed into an appropriate medium until care by a dentist can be delivered. Many storage mediums have been recommended, including water, the vestibule of the mouth, physiologic saline, milk, and cell culture media in specialized containers. Water is the least desirable because it is hypotonic and causes cell lysis. Saliva keeps the tooth moist but is not ideal because of incompatible osmolality and pH and the presence of bacteria. The most ideal storage medium is Hanks balanced salt solution, which can be purchased as part of a commercial tooth-preserving system (Save-A-Tooth, Biologic Rescue Products, Conshohocken, Pennsylvania). Many schools, sporting venues, and ambulances have these kits on hand for use in cases of tooth avulsion. If this solution is not available, milk is considered the best alternative storage medium because it is readily available at or near an accident site, it has a pH and osmolarity compatible with vital cells, and it is relatively free of bacteria. Milk has been shown effectively to maintain the vitality of periodontal ligament cells.9
When the patient gets to the dentist’s office, the dentist must decide whether the tooth is salvageable. If the tooth has already been replanted and seems to be in good position, it should be radiographed and then splinted for 7 to 10 days. If the tooth is carried into the office and it has been out of its socket less than 20 minutes, it should be immediately rinsed in saline and replanted by the dentist. Removal of all of the blood clot from within the socket is not necessary; however, careful suctioning and gentle irrigation with sterile saline will remove the bulk of the clot. The root surface and tooth socket should never be scraped, “sterilized,” or manipulated before replantation because this destroys viable periodontal tissue.
If the tooth has been out of the socket for more than 20 minutes, it should not be replanted until after it has been placed into Hanks balanced salt solution for 30 minutes and then in doxycycline (1 mg/20 mL saline) for 5 minutes. The tooth should then be replanted and splinted. Soaking the tooth in Hanks solution seems to reduce the incidence of ankylosis by improving the survival of periodontal cells on the root. The solution also helps cleanse debris from the root and dilutes bacteria. The doxycycline helps inhibit bacteria in the pulpal lumen, which reduces a major obstacle to revascularlization. Even teeth that were stored in milk or saline should undergo this regimen before implantation.
Stabilization of an avulsed tooth can be achieved using a variety of materials, such as wires, arch bars, and splints. However, several factors must be considered: The stabilizing device should be as hygienic as possible and should be positioned away from the gingiva and tooth roots, if possible. During the healing response, inflammation must be kept to a minimum or inflammatory root resorption will be favored, which is one of the drawbacks to interdental wiring and cold-cured acrylic splints. Patients have difficulty cleansing teeth that are covered with wires or splints. Furthermore, wire can slip apically around the cervical aspect and damage the cementum. The stabilization applied to the tooth need not be absolutely rigid because this may predispose to ankylosis and external root resorption. Physiologic movements of the tooth are thought by some to promote fibrous (i.e., desired) instead of osseous (i.e., tending toward ankylosis) attachment of the root to the alveolar bone. The stabilization device should also be easy to apply and remove with readily available instruments.
A technique that serves admirably for the stabilization of avulsed teeth is the use of an acid-etched composite system (Fig. 23-17 and 23-18). A wire of moderate stiffness but that still has some flexibility, such as braided orthodontic wire, is adapted to the facial surfaces of one or two teeth on each side of the avulsed tooth. The fewer teeth required to stabilize the avulsed tooth, the more physiologic movement that can be imparted to the replanted tooth during function. If braided orthodontic wire is unavailable, any wire—even a paper clip—will suffice. The facial surfaces of the avulsed and the adjacent teeth are acid-etched, and the wire is cemented to them with composite. This technique makes cleansing the teeth easy because the wire is away from the gingiva. The wire can be readily removed, and most dentists have the necessary supplies and instrumentation available for its use.
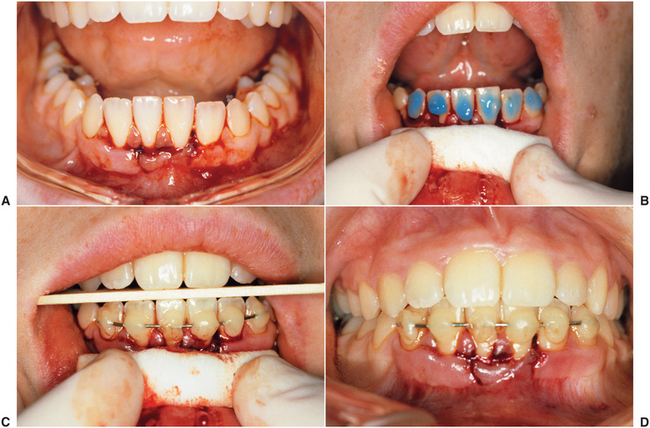
FIGURE 23-18 Technique of acid-etch composite stabilization of displaced teeth. A, Lower incisor teeth displaced lingually. B, After digital repositioning, acid is applied to facial surfaces of displaced incisors and one or two teeth on each side after isolation and drying. C, Composite material and wire applied. D, Occlusion checked during and after stabilization.
The duration of stabilization (Table 23-1) should be as short a time as necessary for the tooth to become reattached, usually 7 to 10 days. Studies have shown that the more rigid and the longer the stabilization, the more root resorption that can be expected.1,10
TABLE 23-1
Stabilization Periods for Dentoalveolar Injuries
| Dentoalveolar Injury | Duration of Immobilization |
| Mobile tooth | 7-10 days |
| Tooth displacement | 2-3 weeks |
| Root fracture | 2-4 months |
| Replanted tooth (mature) | 7-10 days |
| Replanted tooth (immature) | 3-4 weeks |
On removal of the stabilization device, the tooth will still be mobile. Therefore, it is important that the stabilization device be removed with great care and that the patient be instructed to avoid this region during mastication. If, however, the apical foramen is wide open, pulp may survive and revascularize. To promote this possibility, the tooth is usually stabilized for 3 to 4 weeks instead of the shorter time for apically mature teeth.
Patients who have no recollection of a tetanus booster within the past 5 to 10 years should be referred to their physician for one. The use of antibiotics (e.g., penicillin) for 7 to 10 days is appropriate.
The patient should be told that several outcomes are possible after replantation. The best result to be expected is a relatively normal, functional tooth that in most instances will require endodontic therapy (described later). However, varying amounts of root resorption and ankylosis may occur. The development of these signs determines the prognosis of the tooth. Although acute dental infection is rare, it can lead to loss of the replanted tooth. These patients must be followed carefully at regular and frequent intervals for some time after replantation. Andreasen and Hjorting-Hansen3 list the following five factors to be considered before replanting avulsed teeth:
1. The avulsed tooth should have no advanced periodontal disease.
2. The alveolar socket should be reasonably intact to provide a seat for the avulsed tooth.
3. There should be no orthodontic contraindications, such as significant crowding of teeth.
4. The extraalveolar period should be considered; periods exceeding 2 hours are usually associated with poor results. If the tooth is replanted within the first 30 minutes, excellent results can be expected.
5. The stage of root development should be evaluated. Survival of the pulp is possible in teeth with incomplete root formation if replantation is accomplished within 2 hours after injury.
If the tooth to be replanted is not favorable for replantation, as determined by these factors, the patient should be made aware that the prognosis will be worse. One should keep in mind the alternatives to replantation in cases where the factors involved are unfavorable, such as teeth with existing periodontal disease, large restorations, alveolar disruption, and long extraalveolar duration. Today the use of dental implants can offer patients who suffered tooth avulsion an option that was not available in the past. In hopeless cases, one might elect to defer tooth replantation for placement of a dental implant once the alveolus has healed.
Alveolar Fractures
Small fractures through the alveolar process, as mentioned previously, frequently accompany injuries to the teeth. However, injuries to the alveolar process often occur independently and can be challenging to manage. In most instances the segment of bone contains at least one tooth but more frequently several.
Concomitant injuries, such as crown fractures, root fractures, and soft tissue injuries, may have occurred. These injuries may best be managed by referral to an oral and maxillofacial surgeon because management may involve open surgical treatment to reposition the bony segments.
The treatment of this type of injury, as for any fracture, is first to place the segment into its proper position and then to stabilize it until osseous healing occurs. This procedure may be simply performed with digital pressure applied after an appropriate anesthetic is administered (Fig. 23-19). Frequently, however, splintering of the dentoosseous segment margins makes repositioning difficult, and open surgical treatment might then be required.

FIGURE 23-19 Treatment of dentoalveolar fracture. A, Clinical appearance of fracture involving four mandibular incisors. The teeth are apically mature and have minimal bone around lateral and apical areas. B, Clinical appearance after digital reduction of fracture. Occlusal relationship is verified before stabilization of these teeth. C, Radiographic appearance of teeth after digital reduction. D, Appearance after application of Essig wire and suturing of mucosa. E, Cold-curing acrylic added for rigidity (Note: Bonding an arch wire to the teeth with the acid-etch composite technique demonstrated in Figure 23-18 would be preferable). Because of maturity of apices, root canal treatment should be performed on these teeth in 1 to 2 weeks after trauma. (B Courtesy Dr. Stephen Feinberg, University of Michigan, Ann Arbor.)
Teeth with root apices that are denuded within a dentoalveolar fracture should undergo endodontic treatment within 1 to 2 weeks to help prevent inflammatory root resorption and infection. The dentoosseous segment must be stabilized for approximately 4 weeks to allow osseous healing. Several acceptable methods can be used to stabilize the segment: The simplest is to ligate an arch bar to the teeth both mesial and distal to the segment and within the fractured alveolar segment. The teeth immediately adjacent to the fracture are frequently not wired to the arch bar, so these teeth are more amenable to oral hygienic measures. Not wiring them also helps to prevent their loosening from the forces placed by the wire. The use of an acid-etched arch wire, as just described, is also acceptable. A cold-cured acrylic splint can be made in situ or on casts obtained by taking an impression immediately after repositioning the alveolar segment. The splint can be wired to adjacent teeth and to teeth within the fractured segment.
Treatment of Pulp
The dental pulp may be damaged during any of the tooth injuries just described, as a result of direct exposure, the inflammatory response of near exposure, concussive effects, or disruption of the nutrient artery of the pulp. In any injury to the tooth, the possibility for pulpal degeneration is real, and early detection is imperative. If a pulp degenerates, an inflammatory response occurs that leads to tooth resorption and ankylosis (Fig. 23-20). Therefore, for all injuries described, the status of the pulp must be ascertained. Because it is difficult to establish the health status of the pulp immediately after injury, the dentist must assume that if the apex of a mature tooth has moved more than 1 mm in any direction, pulpal degeneration will occur.

FIGURE 23-20 A and B, Two cases of inflammatory root resorption that occurred several months after dentoalveolar trauma without root canal treatment.
Root canal treatment should not be performed at the time of tooth repositioning or replantation because the extra time necessary to perform this treatment is not warranted and exposes the tooth to more chance of external damage. However, in all teeth with closed apical foramina, endodontic treatment should be instituted after approximately 2 weeks. This treatment helps minimize inflammatory root resorption by eliminating nonvital tissue from the pulp. A standard biomechanical preparation of the root canal system is then performed. However, instead of filling the root canal with gutta-percha, the clinician treats the canal in a manner similar to an apexification technique; that is, a 1:1 mixture of calcium hydroxide and barium sulfate is placed within the canal for 6 to 12 months. The barium sulfate allows radiographic evaluation of the amount of calcium hydroxide present because it slowly dissipates within the root canal after placement. Periodic radiographic evaluations should be performed, and the calcium hydroxide should be replaced every 3 months if noted to be absent from the root canal system. A conventional root canal can be performed when successive radiographs indicate no further root resorption. This regimen should be used instead of placing a permanent endodontic filling soon after biomechanical preparation because it appears to minimize inflammatory root resorption.
In teeth with apical foramina that are wide open, endodontic treatment may be delayed for several weeks while careful follow-up examinations, including pulp vitality tests, determine its necessity. When the apices are open, it is likely that revascularization of the root canal system will occur. If root canal therapy appears necessary, apexification procedures with use of calcium hydroxide can be used before filling of the root canal system with a permanent filling material. The technique of apexification is illustrated in Figure 23-21.
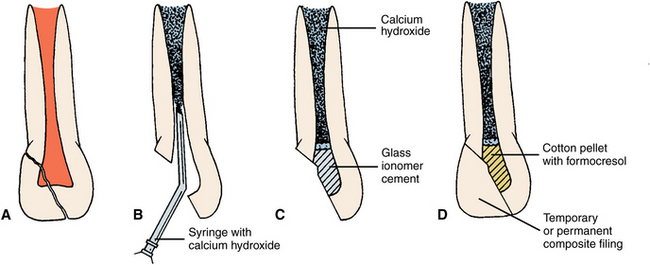
FIGURE 23-21 Apexification procedure. A, Coronal fracture involving pulp of apically immature tooth. B, Removal of entire pulp and filling with calcium hydroxide solution. Calcium hydroxide can be injected from syringe or spun in with spiral on rotating instrument. C, Cotton pledget (with or without formocresol) is then placed, after which coronal pulp chamber is filled with glass ionomer cement. D, Temporary or permanent composite filling is then placed. Calcium hydroxide solution may require replacing every 3 months until apex is closed.
REFERENCES
1. Andreasen, JO. The effect of splinting upon periodontal healing after replantation of permanent incisors in monkeys. Acta Odontol Scand. 1975;33:313.
2. Andreasen, JO, Andreasen, FM. Textbook and color atlas of traumatic injuries to the teeth, ed 3. Copenhagen: Munksgaard, 1994.
3. Andreasen, JO, Hjorting-Hansen, E. Replantation of teeth. I. Radiographic and clinical study of 110 human teeth replanted after accidental loss. Acta Odontol Scand. 1966;24:263.
4. Sanders, B, Brady, FA, Johnson, R. Injuries. In: Sanders B, ed. Pediatric oral and maxillofacial surgery. St Louis: Mosby, 1979.
5. Donley, KJ. Management of sports-related crown fractures. Dent Clin North Am. 2000;44:85.
6. Rauschenberger, CR, Hovland, EJ. Clinical management of crown fractures. Dent Clin North Am. 1995;39:25.
7. Pagliarini, A, Rubini, R, Rea, M, et al. Crown fractures: effectiveness of current enamel-dentin adhesives in reattachment of fractured fragments. Quintessence Int. 2000;31:133.
8. Turley, PK, Joiner, MW, Hellstrom, S. The effect of orthodontic extrusion on traumatically intruded teeth. Am J Orthod. 1984;85:47.
9. Trope, M. Clinical management of the avulsed tooth. Dent Clin North Am. 1995;39:93.
10. Andreasen, JO. Etiology and pathogenesis of traumatic dental injuries. Scand J Dent Res. 1970;78:339.