Correction of Dentofacial Deformities
PREVALENCE OF DENTOFACIAL DEFORMITIES
CAUSES OF DENTOFACIAL DEFORMITY
EVALUATION OF PATIENTS WITH DENTOFACIAL DEFORMITY
PREVALENCE OF DENTOFACIAL DEFORMITIES
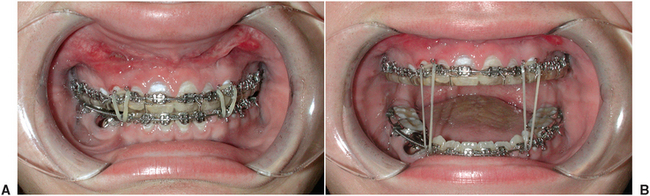
Epidemiologic surveys demonstrate that a large percentage of the United States’ population has a significant malocclusion.1–3 Very little data describe the exact prevalence of significant skeletal facial deformity. This information can be extrapolated from studies that have evaluated the prevalence of severe malocclusion. The National Health and Nutrition Examination Survey (NHANES III) conducted from 1989 to 1994 obtained a sample of 14,000 individuals ages 8 through 50 that roughly approximates the general U.S. population. In this study, information was collected describing overjet/reverse overjet, vertical overlap (deep bite and open bite), and posterior crossbites.1 It can be assumed that patients with extreme values in each of these categories have underlying facial deformities (Table 25-1). Because many patients have dental compensations for skeletal growth abnormalities (described later in this chapter), this study likely underestimates the severity of skeletal abnormalities. This type of data combined with other criteria that clearly define the most severe characteristics of a malocclusion, such as overjet versus crowding, can help to approximate more clearly the prevalence of skeletal abnormality that may require surgical correction as part of the treatment for malocclusion.2
TABLE 25-1
Percentage of the U.S. Population with Severe/Extreme Malocclusion
Adapted from Proffit WR, White RP Jr: Dentofacial problems: prevalence and treatment need. In Proffit WR, White RP Jr, Sarver DM, editors: Contemporary treatment of dentofacial deformity, St Louis, 2003, Mosby.
It appears that about 2% of the U.S. population has mandibular deficiency and/or vertical maxillary excess that is severe enough to be considered handicapping.3 Other abnormalities and their percentage of prevalence in the population include mandibular excess and/or maxillary deficiency, 0.3%; open bite, 0.3%; and asymmetry, 0.1%. Therefore, it appears that approximately 2.7% of the U.S. population may have a dentofacial deformity contributing to malocclusion that will require surgical treatment for correction.
Historically, treatment of malocclusions, even those associated with dentofacial deformities, has been aimed at correction of dental abnormalities, with little attention to the accompanying deformity of the facial skeleton. In the last 60 years, surgical techniques have been developed to allow positioning of the entire midface complex, mandible, or dentoalveolar segments to any desired position. The combining of surgical and orthodontic procedures for dentofacial deformities has become an integral part of the correction of malocclusions and facial abnormalities.
CAUSES OF DENTOFACIAL DEFORMITY
Malocclusion and associated abnormalities of the skeletal components of the face can occur as a result of a variety of factors, including inherited tendencies, prenatal problems, systemic conditions that occur during growth, trauma, and environmental influences. Although it is not within the scope of this book to present a detailed discussion of facial growth, an understanding of basic principles as they relate to the development of dentofacial deformities is essential. Enlow and Han’s Essentials of Facial Growth4 should be reviewed for a more complete discussion of the principles of facial growth.
General Principles of Facial Growth
The development of proper craniofacial form and function is a complex process affected by many factors. In the area of the craniofacial complex, areas exist that appear to have their own intrinsic growth potential, including the sphenooccipital and sphenoethmoidal synchondroses and the nasal septum. In addition, the majority of growth of the bones of the face occurs in response to adjacent soft tissue and the functional demands placed on the underlying bone. These soft tissue influences include the nasal, oral, and hypopharyngeal airway; facial muscles; and muscles of mastication.5
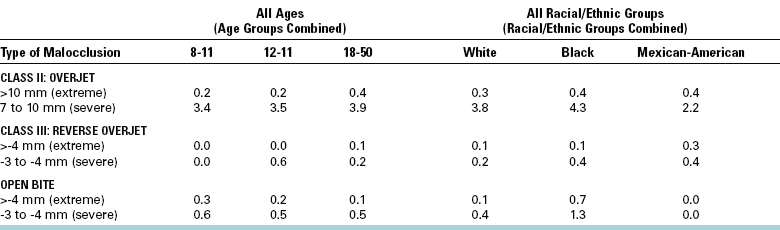
The general direction of normal growth of the face is downward and forward with lateral expansion. The maxilla and the mandible appear to grow by remodeling or differential apposition and resorption of bone, producing changes in three dimensions. Enlow and Hans4 describe this phenomenon as area relocation, with the maxillary-mandibular complex enlarging in the downward and forward direction as an “expanding pyramid” (Fig. 25-1). The direction and amount of growth characterize an individual’s growth pattern.6 Alterations in the pattern of growth or in the rate at which this growth occurs may result in abnormal skeletal morphology of the face and an accompanying malocclusion.
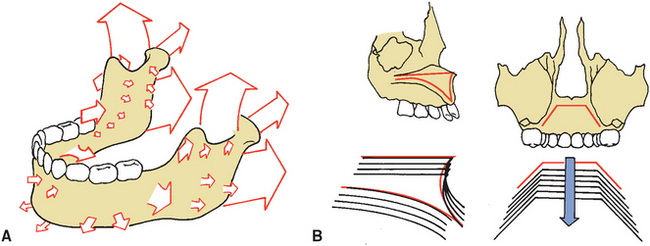
FIGURE 25-1 A, Mandibular growth resulting from apposition and resorption of bone. Primary areas of bony apposition include superior surface of alveolar process and posterior and superior surfaces of mandibular ramus. B, Forward and downward growth of nasal complex and maxilla in “expanding V.” Resorption of bone at superior surface of palate occurs simultaneously with apposition at inferior surfaces of palate and alveolar processes. In addition, growth in posterior area of maxilla results in downward and forward expansion of maxilla. (From Enlow DH: Handbook of facial growth, Philadelphia, 1975, WB Saunders.)
Genetic and Environmental Influence
Genetic influence certainly plays a role in dentofacial deformities. Patterns of inheritance, such as a familial tendency toward a prognathic or deficient mandible, are often seen in a patient with a dentofacial deformity. However, the multifactorial nature of facial development precludes the prediction of an inherited pattern of a particular facial abnormality.
Abnormal facial growth and associated malocclusions are sometimes associated with congenital abnormalities and syndromes. Some of these syndromes such as hemifacial microsomia and mandibulofacial dysostosis (Treacher Collins syndrome) are related to embryonic abnormalities of neural crest cells. Other congenital abnormalities affecting jaw growth include cleft lip and palate and craniosynostosis (premature fusions of craniofacial sutures). Facial growth abnormalities may be caused by maternal systemic influences such as fetal alcohol syndrome, which may result in hypoplasia of midface structures.
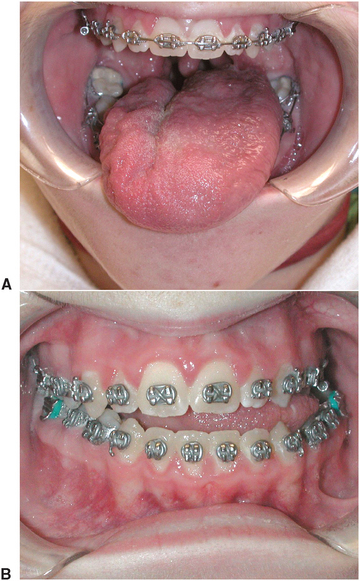
Environmental influences also play a role in the development of dentofacial deformities. As early as the prenatal stage, intrauterine molding of the developing fetal head may result in a severe mandibular deficiency. Abnormal function after birth also may result in altered facial growth because soft tissue and muscular function often influence the position of teeth and growth of the jaws. Abnormal tongue position or size can affect the position and growth of the maxilla and mandible (Fig. 25-2). Respiratory difficulty, mouth breathing, and abnormal tongue and lip postures can adversely influence facial growth.7 Trauma to the bones of the face can result in severe abnormalities of the facial skeleton and the occlusion. In addition to the abnormality that occurs as an immediate result of trauma, further effects on the development of facial bones may occur. In the case of temporomandibular joint (TMJ) trauma in a growing child, significant restriction of jaw function may occur as a result of scarring or bony/fibrous ankylosis. Subsequent alteration of growth may result with deficient or asymmetric mandibular growth (Fig. 25-3).
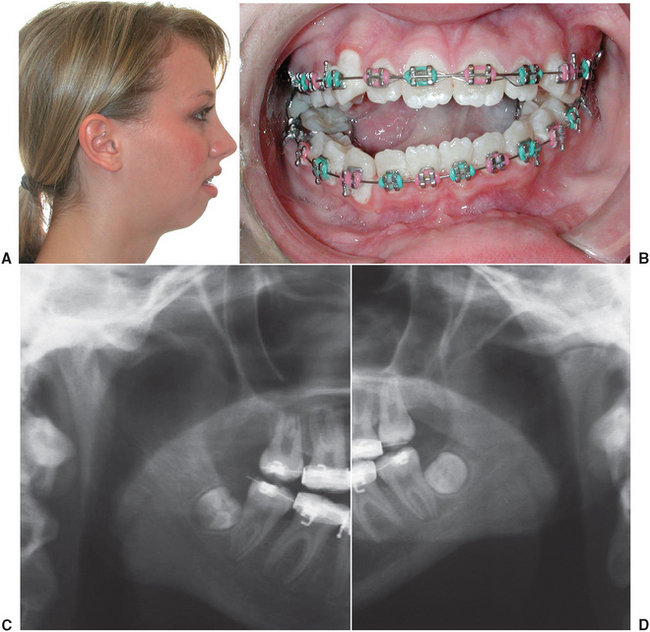
FIGURE 25-3 Condylar trauma at an early age resulting in restricted jaw function and subsequent deficient and asymmetric mandibular growth. A, Profile view. B, Occlusion with right side anterior open bite due to decreased growth in the left mandibular ramus area. C, Radiograph of right condyle and ramus (normal). D, Left side with decreased growth.
EVALUATION OF PATIENTS WITH DENTOFACIAL DEFORMITY
In the past, individual practitioners often treated patients with dentofacial deformities. Some patients have been treated with orthodontics alone, with a resultant acceptable occlusion but a compromise in facial esthetics. Other patients have had surgery without orthodontics in an attempt to correct a skeletal deformity, which resulted in improved facial esthetics but a less than ideal occlusion. In addition to orthodontic and surgical needs, these patients often have many other problems requiring periodontic, endodontic, complex restorative, and prosthetic considerations.
Many areas of dental practice, in addition to orthodontics and surgery, must be integrated to address the complex problems of patients with dental deformities. This integrated approach, used throughout the evaluation, presurgical, and postsurgical phases of patient care, provides the best possible results for these patients.8
The most important phase in patient care centers on evaluation of the existing problems and definition of treatment goals. At the initial appointment a thorough interview should be conducted with the patient to discuss the patient’s perception of the problems and the goals of any possible treatment. The patient’s current health status and any medical or psychological problems that may affect treatment are also discussed at this time.
The involved orthodontist and oral and maxillofacial surgeon should conduct a thorough examination of facial structure, with consideration of frontal and profile esthetics.
Evaluation of facial esthetics in the frontal view should assess the presence of asymmetries and evaluate overall facial balance. The evaluation should include assessment of the position of the forehead, eyes, infraorbital rims, and malar eminences; configuration of the nose, including the width of the alar base; paranasal areas; lip morphology; relationship of the lips to incisors; and overall proportional relationships of the face in the vertical and transverse dimensions. Figure 25-4 demonstrates normal facial proportions. The profile evaluation allows an assessment of the anteroposterior and vertical relationships of all components of the face. The soft tissue configuration of the throat should also be evaluated. Photographic documentation of the pretreatment condition of the patient should be a standard part of the evaluation. Video and digital computerized images have been introduced over the past decade as an additional aid in evaluating facial morphology.
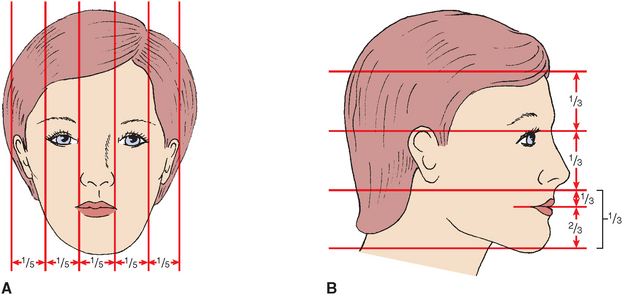
FIGURE 25-4 Normal facial proportions. A, Representation of proportional relationships of full-face view. Relationships of medial intercanthal distance, alar base width, and lip proportions to remainder of facial structures are demonstrated. B, Normal profile proportions demonstrates relationships of upper, middle, and lower thirds of face and proportional relationships of lip and chin morphology within lower third of face.
A complete dental examination should include assessment of dental arch form, symmetry, tooth alignment, and occlusal abnormalities in the transverse, anteroposterior, and vertical dimensions. The muscles of mastication and TMJ function should also be evaluated. A screening periodontal examination, including probing, should assess the patient’s hygiene and current periodontal health status. Impressions and a bite registration for dental cast construction and evaluation should also be obtained at this time.
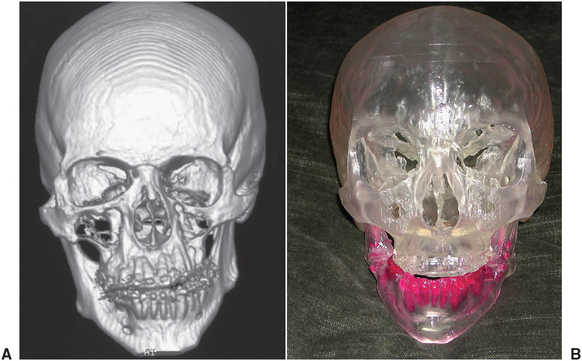
Lateral cephalometric and panoramic radiographs are routinely used in the patient evaluation and are an important part of the initial assessment. The cephalometric radiograph can be evaluated by several techniques to aid in the determination of the nature of the skeletal abnormality (Fig. 25-5; Table 25-2).9,10 An important note, however, is that cephalometric radiographs are only a part of the evaluation process; they are used as adjunctive diagnostic tools in the clinical assessment of the patient’s facial structure and occlusion. Other radiographic images may be helpful in evaluating patients for surgical correction. These may include posteroanterior facial films, TMJ images when indicated, and conventional and cone-beam computed tomography (Fig. 25-6). In difficult, complex cases, it may be helpful to obtain a stereolithic three-dimensional model constructed from computed tomography scan data. Computerized digital technology is currently available that helps to integrate the cephalometric data with digital images of the face to improve evaluation of the relationship of the underlying facial skeleton and overlying soft tissue. After careful clinical assessment and evaluation of the diagnostic records, a problem list and treatment plan should be developed that combines opinions from all practitioners participating in the patient’s care, including the orthodontist, oral and maxillofacial surgeon, periodontist, and restorative dentist.
TABLE 25-2
Orthognathic Cephalometric Analysis
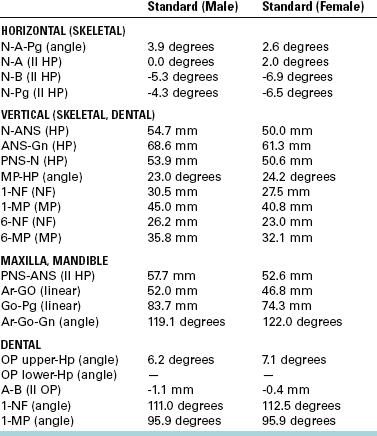
Modified from Burstone CJ, James RB, Legan H et al: Cephalometrics for orthognathic surgery, J Oral Surg 36:269, 1978.
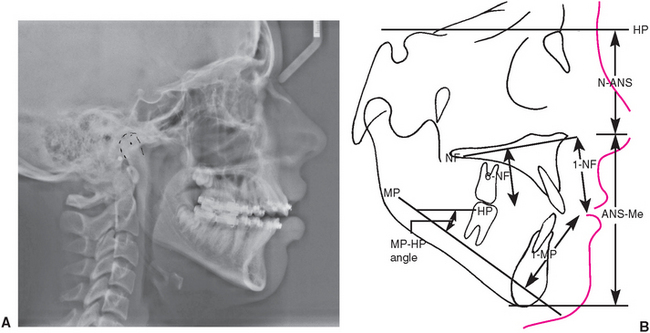
FIGURE 25-5 A, Lateral cephalometric radiograph. B, Tracing of lateral cephalometric head film, with landmarks identified for evaluating facial, skeletal, and dental abnormalities using system of cephalometrics for orthognathic surgery (Table 25-2). (B from Burstone CJ, James RB, Legan H et al: Cephalometrics for orthognathic surgery, J Oral Surg 36:269, 1978.)
PRESURGICAL TREATMENT PHASE
As the first step in treatment, gingival inflammation must be controlled and the patient’s cooperation ensured. In patients who are unwilling or unable to clean their teeth properly before the placement of orthodontic appliances, oral hygiene procedures will be even less effective when complicated by orthodontic band placement.
Periodontal therapy includes oral hygiene instruction, scaling, and root planing; in certain instances, flap surgery to gain access for root planing may be necessary to provide proper tissue health. Whenever possible, it is desirable to delay comprehensive treatment until adequate patient compliance and control of inflammation are achieved.
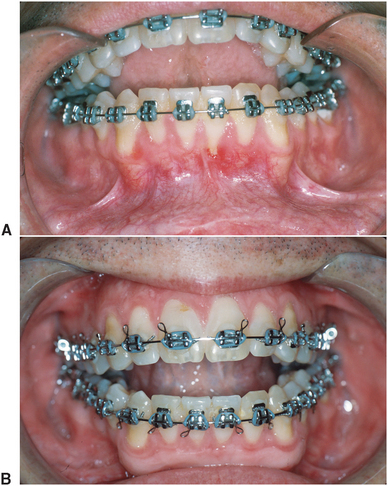
As a result of the periodontal examination findings and proposed orthodontic and surgical plan, mucogingival surgery is often accomplished during this initial phase of therapy to provide a zone of attached keratinized tissue that is more resistant to potential orthodontic and surgical trauma. Soft tissue grafting is indicated in areas that have no keratinized gingiva or where only a thin band of keratinized tissue with little or no attachment is found when an increase in tissue trauma is likely (Fig. 25-7). Such trauma to these areas includes labial orthodontic movement of teeth or a surgical procedure such as an inferior border osteotomy or segmental osteotomies in interdental areas.
Restorative Considerations
During the presurgical restorative phase, the patient is evaluated for carious lesions and faulty restorations. Teeth should be evaluated endodontically and periodontally for restorability, and any nonrestorable teeth should be extracted before surgical intervention. All carious lesions must be restored early in the presurgical treatment phase. Existing restorations must function for 18 to 24 months during the orthodontic and surgical treatment phases, requiring that more durable restorative materials (i.e., amalgam and composite resin) be used, even though they may be replaced during the definitive postsurgical treatment phase. It is wise to delay final restorative treatment until the proper skeletal relationships are achieved and the finishing orthodontics is completed.
In the edentulous or partially edentulous patient, particular attention is paid to residual ridge shape and contour in denture-bearing areas. The distance between the maxillary tuberosity, posterior mandible, and ramus areas must be evaluated to ensure that adequate space is present for partial or complete dentures. Teeth that serve as removable partial denture abutments should be evaluated for potential retentive undercuts. If minor orthodontic movement can enhance undercuts, this information is conveyed to the orthodontist.
Presurgical Orthodontic Considerations
Obviously, not all malocclusions require correction with surgery. When the skeletal discrepancy is minimal and orthodontic compensation does not adversely affect dental or facial esthetics or posttreatment stability, orthodontic treatment alone may be the treatment of choice. However, in some cases an adequate occlusal relationship cannot be achieved because of the skeletal discrepancy; some patients may be treated with orthodontic compensation for a skeletal abnormality, resulting in an adequate occlusion but poor facial or dental esthetics or a poor long-term prognosis for posttreatment retention. These patients should be considered for surgery combined with orthodontic treatment.
Treatment Timing
Treatment of the stable adult deformity can be started without delay, but questions often arise about how best to manage the growing child who is identified as having a developing dentofacial deformity. If the facial pattern is favorable and significant growth potential remains, growth modification with techniques such as functional appliance therapy or headgear may be the preferred approach. For patients with unfavorable growth patterns or severe skeletal abnormalities or who are unwilling to undergo attempts at growth modification, surgery is usually the preferred treatment. As a general guideline, orthognathic surgery should be delayed until growth is complete in patients who have problems of excess growth, although surgery can be considered earlier for patients with growth deficiencies.
Orthodontic Treatment Objectives
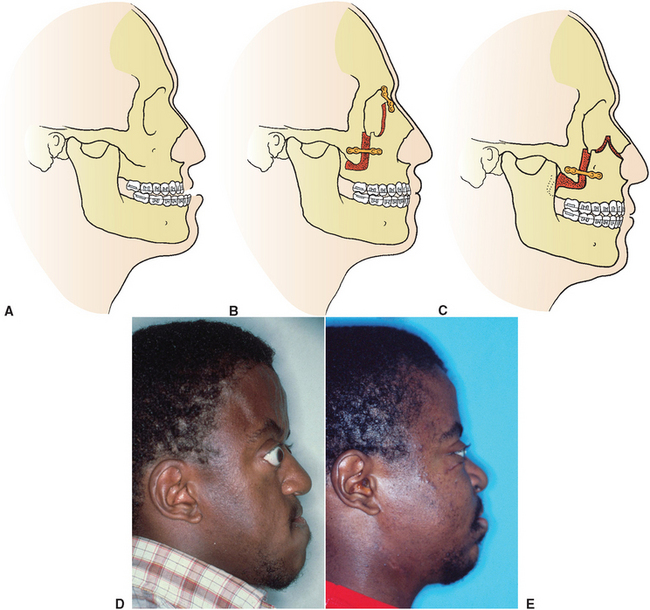
Undesirable angulation of the anterior teeth occurs as a compensatory response to a developing dentofacial deformity. For example, a patient with maxillary deficiency and/or mandibular excess often has dental compensation for the skeletal abnormality with flared upper incisors and retracted or retroclined lower incisors (Fig. 25-8, A to C). Dental compensations for the skeletal deformity are corrected before surgery by orthodontically repositioning teeth properly over the underlying skeletal component, without considerations for the bite relationship to the opposing arch. This presurgical orthodontic movement accentuates the patient’s deformity but is necessary if normal occlusal relationships are to be achieved when the skeletal components are properly positioned at surgery (Fig. 25-8, D to F). The surgical treatment then results in an ideal position of the skeletal and dental components (Fig. 25-8, G to I). The opposite dental compensation may occur in maxillary protrusion or mandibular deficiency (Fig. 25-9). Again, the decompensation is aimed at improving angulation of teeth over underlying bone, after which skeletal problems are corrected.
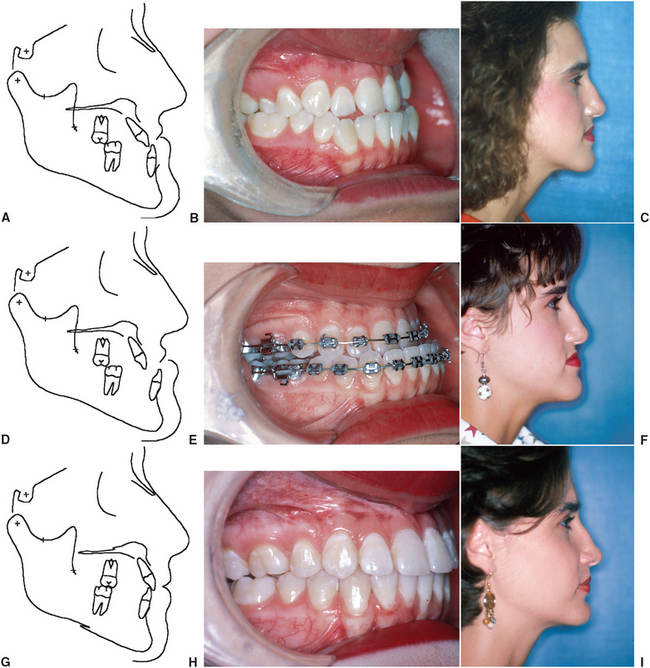
FIGURE 25-8 A, Class III skeletal malocclusion with maxillary deficiency and mandibular excess. B, Dental compensation includes retroclined lower incisors and proclined upper incisors. C, Facial profile. D, After initial orthodontic treatment before surgery. E, Dental compensation are removed with proclination of lower incisors and retroclination of upper incisors, which obviously increases the severity of malocclusion and facial discrepancy. F, Facial profile at this stage. G, Surgical correction with posterior positioning of mandible and advancement of maxilla. H, Ideal occlusion. I, Facial profile after treatment is complete.
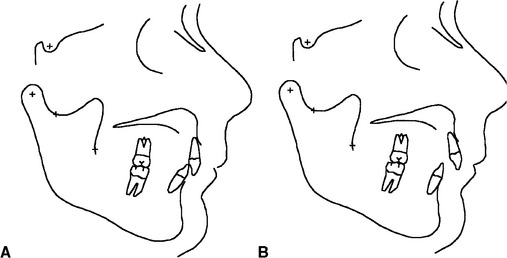
FIGURE 25-9 A, Class II occlusion with compensation demonstrating proclination of lower incisors and upright upper incisors. B, After orthodontic decompensation. C, After surgical correction with mandibular advancement.
The essential steps in orthodontic preparation are to align the arches individually, achieve compatibility of the arches or arch segments, and establish the proper anteroposterior and vertical position of the incisors. The amount of presurgical orthodontics can vary, ranging from appliance placement with minimal tooth movement in some patients to approximately 12 to 18 months of appliance therapy in those with severe crowding and incisor malposition.
As the patient is approaching the end of orthodontic preparation for surgery, it is helpful to take impressions and evaluate progress models for occlusal compatibility. Minor interferences that exist can be corrected easily with arch wire adjustment and significantly enhance the postsurgical occlusal result. After any final orthodontic adjustments have been made, large stabilizing arch wires are inserted into the brackets, which provide the strength necessary to withstand the forces resulting from intermaxillary fixation (IMF) and surgical manipulation.
Final Treatment Planning
After the completion of the presurgical periodontics, restorative dentistry, and orthodontics, the patient returns to the oral and maxillofacial surgeon for final presurgical planning. The evaluation completed at the initial patient examination is repeated. The patient’s facial structure and the malocclusion are reexamined. Presurgical digital photographs and radiographs are obtained. Presurgical models, a centric relation bite registration, and face-bow recording for model mounting are completed. Model surgery on a duplicated set of presurgical dental casts determines the exact surgical movements necessary to accomplish the desired postoperative occlusion (Fig. 25-10).
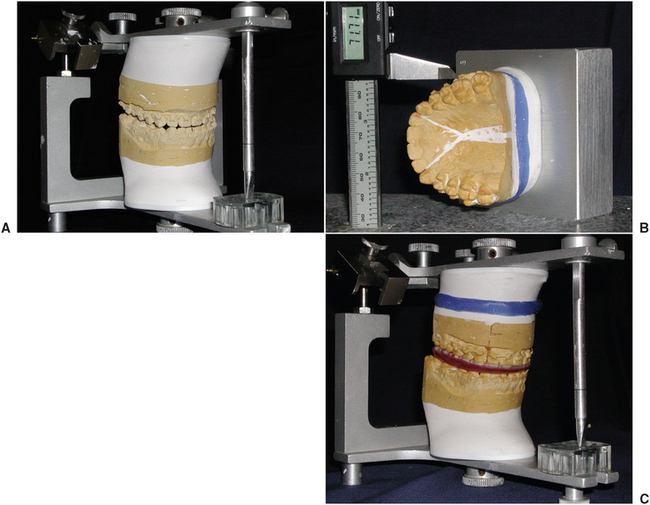
FIGURE 25-10 Model surgery used to determine direction and distance of surgical movement necessary to achieve desired postoperative occlusion and facial esthetics. A, Casts mounted on semiadjustable articulator. B, Repositioning of maxillary cast using precision measuring instrument. Distances of model surgical movements are coordinated between desired facial esthetics and movements necessary to create ideal postoperative occlusion. C, Maxillary cast remounted on semiadjustable articulator after precision movements have been completed and verified. Intraocclusal wafers are constructed on this final occlusal setup for use at time of surgery to align osteotomies and dental segments into desired postsurgical position.
One of the most useful adjuncts to treatment planning for patients with dentofacial deformity is computerized imaging. This technology allows computerized digital images of the patient’s face to be superimposed over bony landmarks obtained from the cephalometric radiograph. Cephalometric treatment planning can be completed with computer assistance. The computer can then produce a digital image that represents the facial esthetic result produced by the associated facial skeletal change (Fig. 25-11). The advantage of using this type of technology is the ability to predict more accurately the facial changes that may result from a particular surgical correction. The facial images are also more easily evaluated by patients, allowing them to assess the predicted results and provide input into the surgical treatment plan. The disadvantage of the technology is related to the inability of the computer to predict accurately every type of surgical change for every patient.11 Different muscle tone and skin thickness and variable soft tissue response to bone change, for example, make it impossible for the computer to predict each individual variation precisely. However, with continued development, this technology will most likely become more common in the treatment planning and presurgical education for patients with dentofacial deformity. Although the current technology is primarily limited to isolated lateral or frontal views, three-dimensional predictive imaging capabilities will likely be available in the near future.
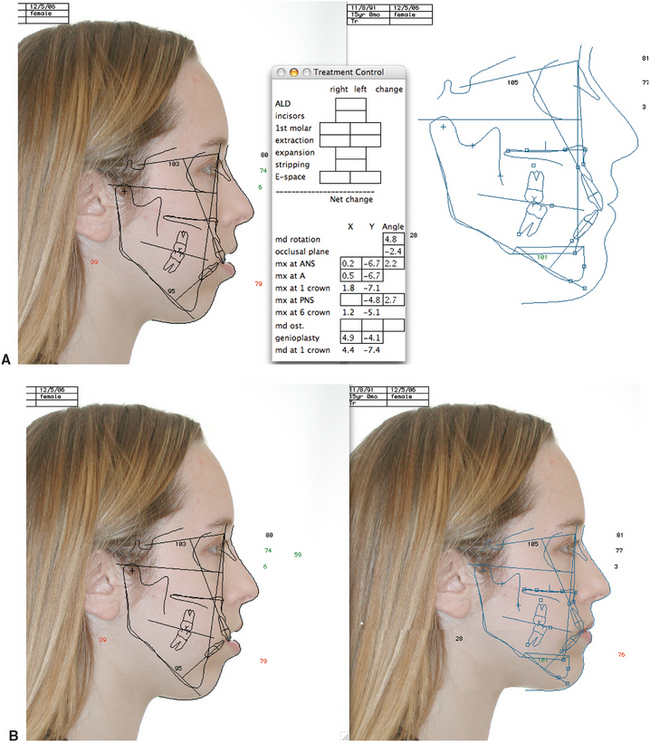
FIGURE 25-11 Computerized imaging for dentofacial surgical treatment planning. Digital image is obtained and placed in computer memory. Landmarks from cephalometric tracing are superimposed over digital image of face. A, Portions of cephalometric tracing can be moved to duplicate the anticipated surgical movements. The computer then manipulates the image to depict soft tissue changes. Digital images displayed on the computer monitor shows predicted facial changes (Quick Ceph Image System). B, View shows presurgical and estimated final images that would result from anticipated surgical procedure (in this case, maxillary superior repositioning and chin advancement).
After completion of the model surgery, prediction tracings, and computer imaging evaluation, the orthodontist or general dentist is often consulted to ensure that the predicted occlusal result is acceptable to all practitioners involved in the patient’s treatment. Any orthodontic or restorative changes necessary to improve postsurgical position should be planned at this time.
SURGICAL TREATMENT PHASE
Dentofacial abnormalities frequently can be treated by isolated procedures in the mandible or maxilla and midface area. Because abnormalities can obviously occur in the maxilla and the mandible, surgical correction frequently requires a combination of surgical procedures. The following sections describe a variety of surgical procedures completed as isolated osteotomies or as combination procedures.
Mandibular Excess
Excess growth of the mandible frequently results in an abnormal occlusion with Class III molar and cuspid relationships and a reverse overjet in the incisor area. An obvious facial deformity may also be evident. Facial features associated with mandibular excess include a prominence of the lower third of the face, particularly in the area of the lower lip and chin in the anteroposterior and vertical dimensions. In severe cases the large reverse overjet may preclude the patient’s ability to obtain adequate lip closure without abnormal strain of the orbicularis oris muscles.
Mandibular excess was one of the first dentofacial deformities recognized as being best treated by a combination of orthodontics and surgery. Although surgical techniques for correction of mandibular excess were reported as early as the late 1800s, widespread use of currently acceptable techniques began in the middle of this century. Early techniques for treatment of mandibular prognathism dealt with the deformity by removing sections of bone in the body of the mandible, which allowed the anterior segment to be moved posteriorly (Fig. 25-12). When the reverse overjet relationship is isolated to the anterior dentoalveolar area of the mandible, a subapical osteotomy technique can be used for correction of mandibular dental prognathism.12 In this technique, bone is removed in the area of an extraction site of a premolar or molar tooth, and the anterior dentoalveolar segment of the mandible is moved to a more posterior position (Fig. 25-13). Although these procedures are rarely used, they are occasionally performed in cases with unusual arch forms in combination with edentulous spaces.
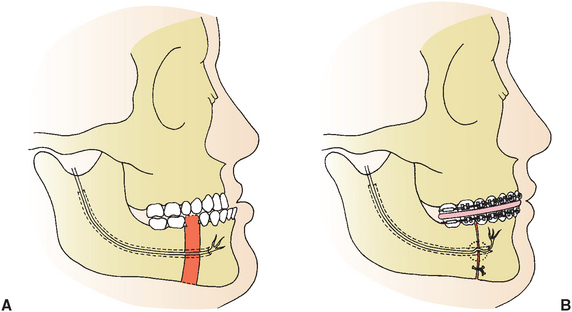
FIGURE 25-12 Body ostectomy with resection of portion of body of mandible followed by posterior repositioning of anterior segment. A, Preoperative view. B, Postoperative view.
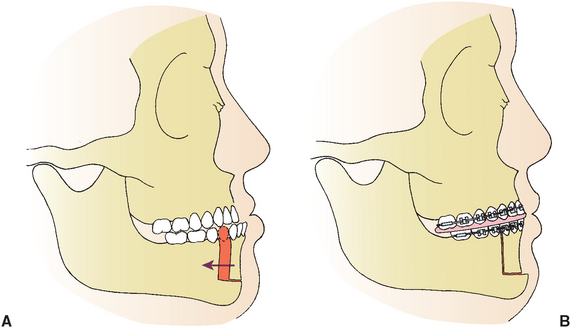
FIGURE 25-13 Anterior mandibular subapical osteotomy. A, Removal of premolar teeth and bone in area of extraction sites. B, After separation, anterior dentoalveolar segment is repositioned posteriorly, extraction sites are closed, and anterior reverse overjet relationship is corrected.
In the early 1950s, Caldwell and Letterman13 popularized an osteotomy performed in the ramus of the mandible for the correction of mandibular excess. In this technique the lateral aspect of the ramus is exposed through a submandibular incision, the ramus is sectioned in a vertical fashion, and the entire body and anterior ramus section of the mandible are moved posteriorly, which places the teeth in proper occlusion (Fig. 25-14).
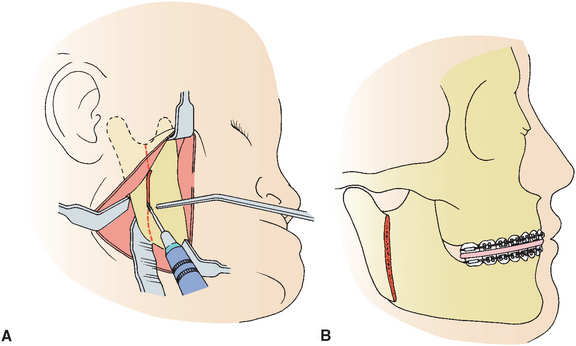
FIGURE 25-14 Extraoral approach for vertical ramus osteotomy. A, Submandibular approach to lateral aspect of ramus showing vertical osteotomy from sigmoid notch area to angle of mandible. B, Overlapping of segments after posterior repositioning of anterior portion of mandible. Proximal segment containing condyle is overlapped on lateral aspect of anterior portion of ramus.
The proximal segment of the ramus (i.e., the portion attached to the condyle) overlaps the anterior segment, and the jaw is stabilized during the healing phase with wiring of the bone segments combined with jaw immobilization using IMF. The extraoral approach is rarely used. A similar technique is performed with an intraoral incision and an angulated oscillating saw (Fig. 25-15).14 The design of the osteotomy is identical to that performed through an extraoral incision. The bone segments can be stabilized using IMF, with or without direct wiring of the segments or using rigid fixation with bone plates or screws, eliminating the need for IMF. The advantages of the intraoral technique include elimination of the need for skin incision and decreased risk of damage to the mandibular branch of the facial nerve. Figure 25-16 demonstrates the clinical results of a patient treated with an intraoral vertical ramus osteotomy to correct mandibular excess.
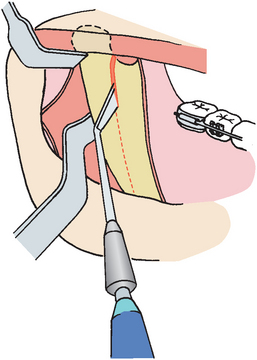
FIGURE 25-15 Intraoral technique for vertical ramus osteotomy through use of angulated oscillating saw.
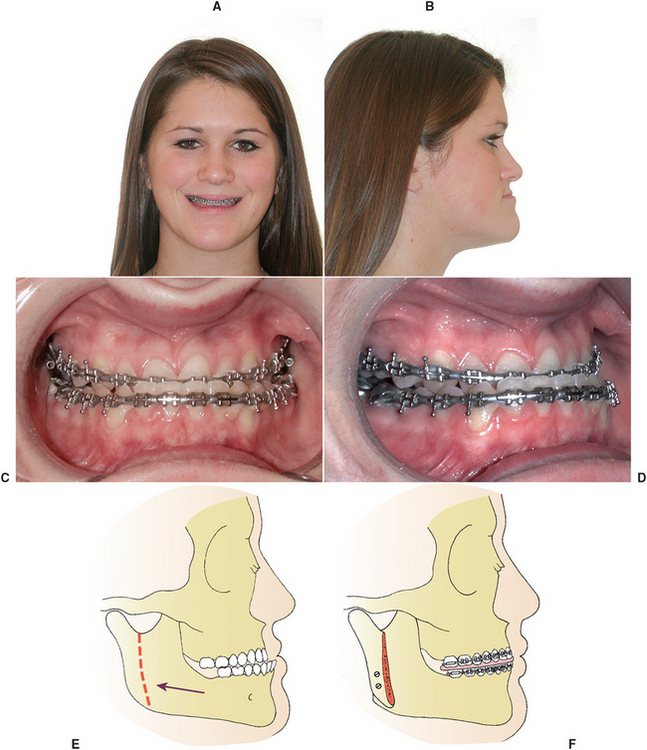
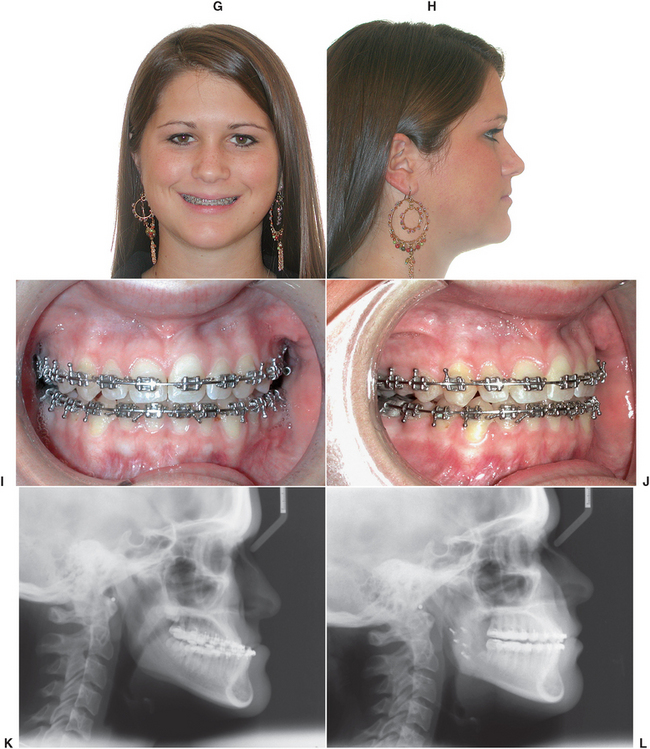
FIGURE 25-16 Case report of mandibular excess. A and B, Preoperative facial esthetics demonstrates typical features of Class III malocclusion resulting from mandibular excess. C and D, Presurgical occlusal photographs. E and F, Diagram of intraoral vertical ramus osteotomy with posterior positioning of mandible and rigid fixation. Postoperative frontal and profile view of patient seen in A and B. G and H, Postoperative occlusion seen in I and J. K and L show preoperative and postoperative radiographs.
Another popular technique for correction of mandibular prognathism is the bilateral sagittal split osteotomy (BSSO) first described by Trauner and Obwegeser15 and later modified by Dalpont,16 Hunsick,17 and Epker.18 The BSSO is accomplished through a transoral incision similar to that for the intraoral vertical ramus osteotomy. The osteotomy splits the ramus and posterior body of the mandible in a sagittal fashion, which allows setback or advancement of the mandible (Fig. 25-17). The telescoping effect in the area of the osteotomy produces large areas of bony overlap that have the flexibility necessary to move the mandible in several directions. The BSSO technique has become one of the most popular methods for treatment of mandibular deficiency and mandibular excess. Disadvantages include potential trauma of the inferior alveolar nerve, with subsequent decreased sensation in the area of the lower lip and chin during the immediate postoperative period. This may be permanent.
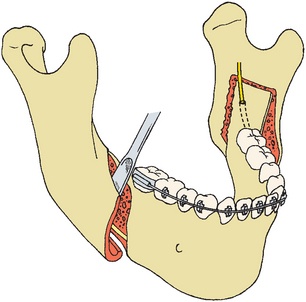
FIGURE 25-17 Sagittal split osteotomy. Ramus of mandible is divided by creation of horizontal osteotomy on medial aspect and vertical osteotomy on lateral aspect of mandible. These are connected by anterior ramus osteotomy. Lateral cortex of mandible is then separated from medial aspect, and mandible can be advanced or set back for correction of mandibular deficiency or excess, respectively.
Mandibular Deficiency
The most obvious clinical feature of mandibular deficiency is the retruded position of the chin as viewed from the profile aspect. Other facial features often associated with mandibular deficiency may include an excess labiomental fold with a procumbent appearance of the lower lip, abnormal posture of the upper lip, and poor throat form. Intraorally, mandibular deficiency is associated with Class II molar and canine relationships and an increased overjet in the incisor area.
Surgical correction of mandibular deficiency was described as early as 1909. However, early results with surgical advancement of the mandible before the 1950s were extremely disappointing. In 1957, Robinson19 described surgical correction of mandibular deficiency using an extraoral surgical approach, a vertical osteotomy, and iliac crest bone grafts in the area of the osteotomy defect. Several modifications of this technique were described over subsequent years. This type of extraoral approach may be useful in rare circumstances, including severely abnormal bony anatomy or for revision surgery (see Fig. 25-21). However, the extraoral incisions have the disadvantages of facial scarring and potential injury to branches of the facial nerve.
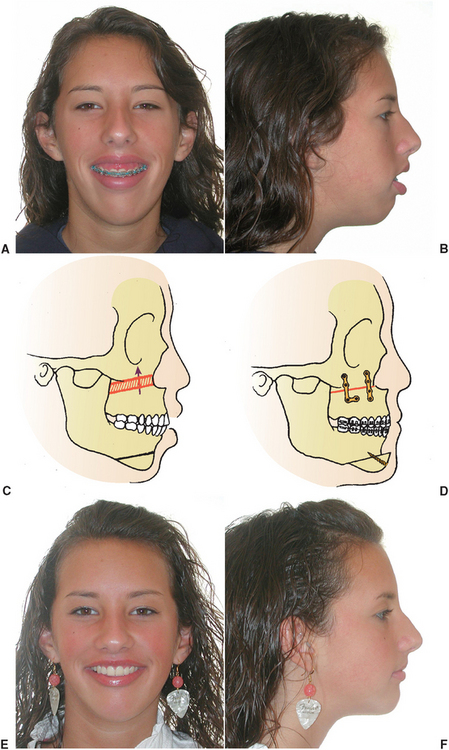
FIGURE 25-21 Typical clinical features of vertical maxillary excess. A and B, Full-face and profile views demonstrating elongation of lower third of face, lip incompetence, and excessive gingival exposure. C and D, Total maxillary osteotomy with superior repositioning combined with advancement genioplasty. E and F, Postoperative full-face and profile views after total maxillary osteotomy with superior repositioning and chin advancement.
Currently, the BSSO, described previously in this chapter for mandibular setback, is the most popular technique for mandibular advancement (Fig. 25-18). This procedure is readily accomplished through an intraoral incision. The significant bony overlap produced with the BSSO allows for adequate bone healing and improved postoperative stability. The osteotomy is frequently stabilized with rigid fixation plates or screws, eliminating the need for IMF.
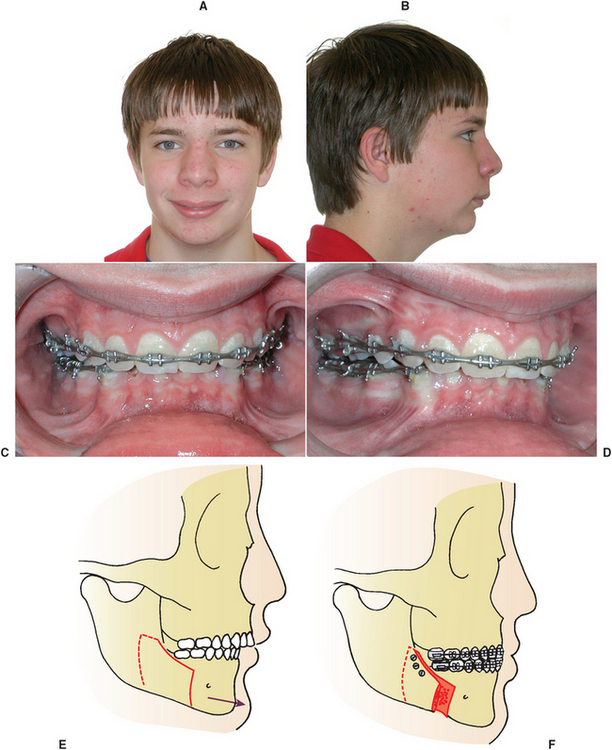
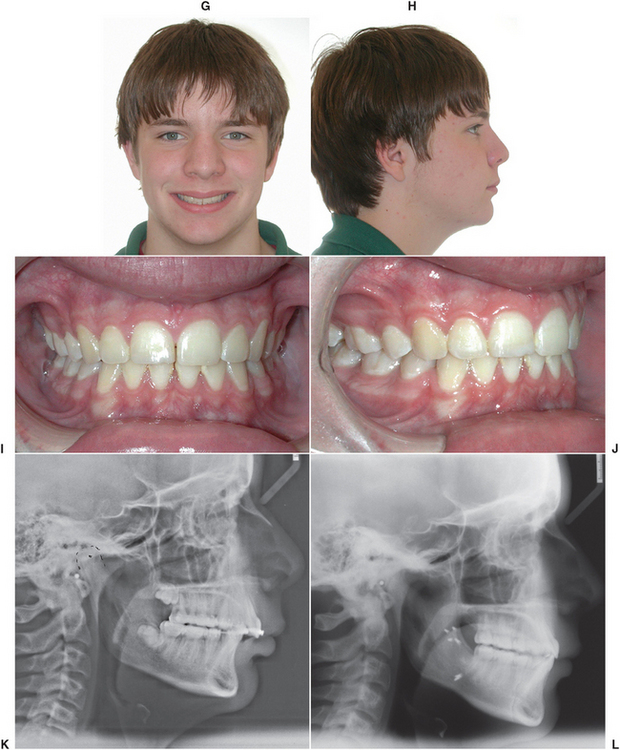
FIGURE 25-18 Case report of mandibular advancement. A and B, Preoperative facial esthetics demonstrating clinical features of mandibular deficiency. C and D, Preoperative occlusion demonstrating Class II relationship and overjet. E and F, Diagrammatic representation of bilateral sagittal split osteotomy with advancement of mandible. G and H, Postoperative facial appearance. I and J, Postoperative occlusion. K and L, Preoperative and postoperative radiographs.
If the anteroposterior position of the chin is adequate but a Class II malocclusion exists, a total subapical osteotomy may be the technique of choice for mandibular advancement (Fig. 25-19). By combining the osteotomy with interpositioned bone grafts, this technique can be used to increase lower facial height.
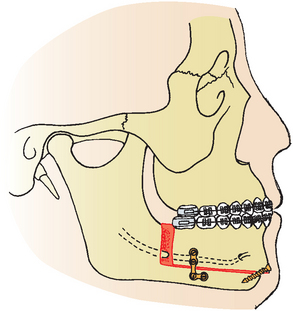
FIGURE 25-19 Total subapical osteotomy. Dentoalveolar segment of mandible is moved anteriorly, allowing correction of Class II malocclusion without increasing chin prominence.
When a proper occlusal relationship exists or when anterior positioning of the mandible would not be sufficient to produce adequate projection of the chin, an inferior border osteotomy (i.e., genioplasty) with advancement may also be performed. This technique is usually performed through an intraoral incision. The inferior portion of mandible is osteotomized, moved forward, and stabilized (Fig. 25-20, A, C, D, E, and F). In addition to anterior or posterior repositioning of the chin, vertical reduction or augmentation and correction of asymmetries can also be accomplished with inferior border osteotomies. Alloplastic materials can occasionally be used to augment chin projection; the material is onlayed in areas of bone deficiencies (Fig. 25-20, B).
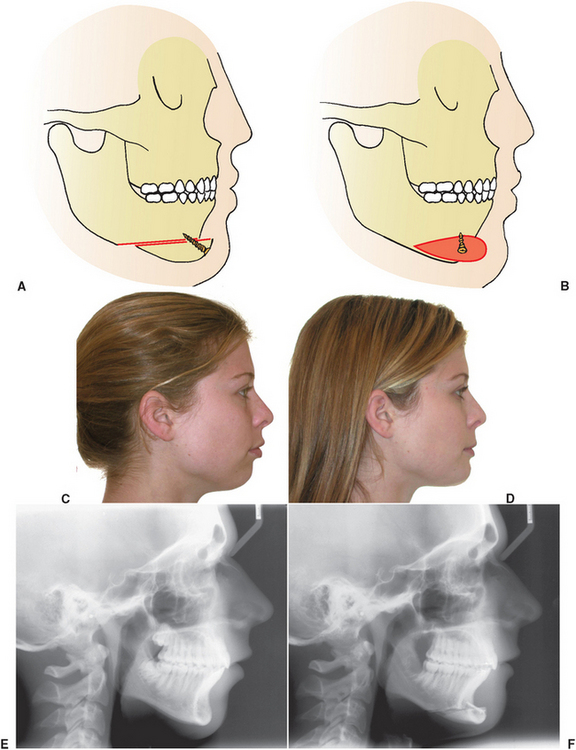
FIGURE 25-20 Inferior border modification (i.e., genioplasty) techniques. A, Advancement of inferior border of mandible to increase chin projection. B, Diagram of implant used to augment anterior portion of chin, eliminating need for osteotomy in this area. C, Clinical picture demonstrating chin deficiency. D, Postoperative photograph after advancement of inferior portion of anterior mandible. E, Preoperative radiograph. F, Postoperative radiograph.
Maxillary Excess
Excessive growth of the maxilla may occur in the anteroposterior, vertical, or transverse dimensions. Surgical correction of dentofacial deformities with total maxillary surgery (i.e., Le Fort I) has only become popular since the early 1970s. Before that time, maxillary surgery was performed on a limited basis, and most techniques repositioned only portions of the maxilla with segmental surgery. During the early years of maxillary surgery, many techniques were performed in two stages: facial or buccal cuts were performed during one operation; then sectioning of palatal bone was performed 3 to 4 weeks later. This staging was done under the assumption that this was necessary to maintain adequate vascular supply to the osteotomized segment. As experience and understanding of these techniques increased, several procedures for anterior and posterior segmental surgery evolved that used single-stage techniques.20–22
In the early 1970s, research by Bell et al.23 demonstrated that total maxillary surgery could be performed without jeopardizing the vascular supply to the maxilla. This work showed that the normal blood flow in the bony segments from larger feeding vessels could be reversed under certain surgical conditions. If a soft tissue pedicle is maintained in the palate and gingival area of the maxilla, the transosseous and soft tissue collateral circulation and anastomosing vascular plexuses of the gingiva, palate, and sinus can provide adequate vascular supply, which allows mobilization of the total maxilla. Total maxillary osteotomies are currently the most common procedures performed for correction of anteroposterior, transverse, and vertical abnormalities of the maxilla.24
Vertical maxillary excess may result in associated facial characteristics, including elongation of the lower third of the face; a narrow nose, particularly in the area of the alar base; excessive incisive and gingival exposure; and lip incompetence (Fig. 25-21).
These patients may exhibit Class I, Class II, or Class III dental malocclusions. A transverse maxillary deficiency with a posterior cross-bite relationship, constricted palate, and narrow arch form is often seen with this deformity.
Vertical maxillary excess is frequently associated with an anterior open-bite relationship (i.e., apertognathia). This results from excessive downward growth of the maxilla, causing downward rotation of the mandible as a result of premature contact of posterior teeth. To correct this problem, the maxilla is repositioned superiorly (impacted), particularly in the posterior area. This allows the mandible to rotate upward and forward, establishing contact in all areas of the dentition. In some cases the occlusal plane of the maxilla is level after orthodontic preparation, and the open bite can be corrected by repositioning the maxilla in one piece (Fig. 25-22, A to D). In other cases, a step in the occlusal plane must be leveled to achieve the desired occlusion. This requires repositioning of the maxilla in segments (Fig. 25-22, E to H).
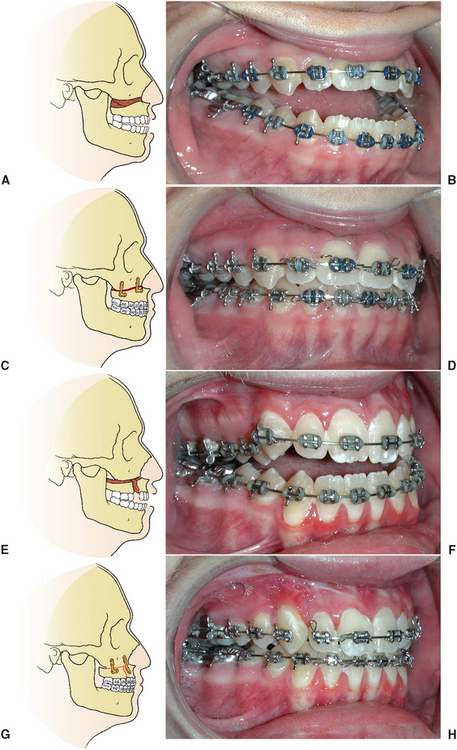
FIGURE 25-22 A, Anterior open bite as a result of vertical maxillary excess with entire maxillary occlusal plane on one level. B, Presurgical occlusion. C, Surgical correction with superior repositioning of maxilla in one piece. D, Postoperative occlusion. E, Open bite with maxillary occlusal plane on two levels. F, Presurgical occlusion. G, Segmental maxillary repositioning to close open bite and place segments on same plane of occlusion. H, Postoperative occlusion.
Anteroposterior maxillary excess results in a convex facial profile usually associated with incisor protrusion and a Class II occlusal relationship. Total maxillary surgery can be completed to correct this problem.25 In some cases the entire maxilla can be moved in one piece in a posterior direction. In addition to procedures in which the maxilla is moved in one piece, the bone can be sectioned into dentoalveolar segments to allow repositioning in the anteroposterior, superior, or inferior directions or to allow expanding in the transverse direction. Figure 25-23 demonstrates a three-piece maxillary osteotomy performed to correct anteroposterior maxillary excess combined with vertical deficiency.
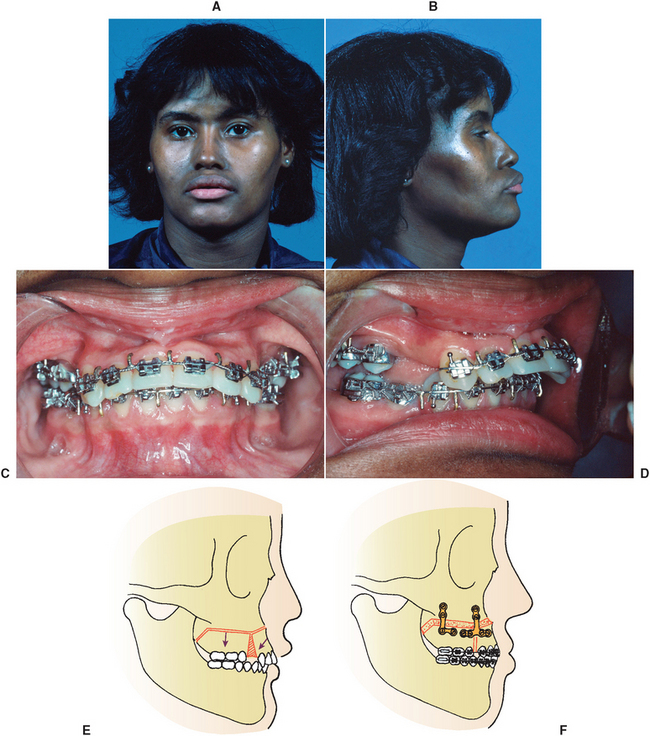

FIGURE 25-23 Case report of segmental maxillary osteotomy. A and B, Preoperative facial appearance demonstrates extreme protrusion of anterior maxillary segment and upper lip, decreased nasolabial angle, and decreased lower face height as a result of maxillary vertical deficiency. C and D, Preoperative occlusion demonstrates protrusive maxillary incisors and extraction space remaining after removal of maxillary premolar teeth bilaterally. E and F, Segmental maxillary osteotomy with closure of premolar extraction space, retraction of anterior segment of maxilla, and placement of bone graft in posterior maxillary area. G and H, Postoperative facial appearance. I and J, Postoperative occlusion. K and L, Preoperative and postoperative radiographs.
Maxillary and Midface Deficiency
Patients with maxillary deficiency commonly appear to have a retruded upper lip, deficiency of the paranasal and infraorbital rim areas, inadequate tooth exposure during smile, and a prominent chin relative to the middle third of the face. Maxillary deficiency may occur in the anteroposterior, vertical, and transverse planes. The patient’s clinical appearance depends on the location and severity of the deformity. In addition to the abnormal facial features, a Class III malocclusion with reverse anterior overjet is frequently seen.
The primary technique for correction of maxillary deficiency is the Le Fort I osteotomy. This technique can be used for advancement of the maxilla to correct a Class III malocclusion and associated facial abnormalities (Fig. 25-24). Depending on the magnitude of advancement, bone grafting may be required to improve bone healing and postoperative stability. In the case of vertical maxillary deficiency, elongation of the lower third of the face can be accomplished by bone grafting the maxilla in an inferior position with the Le Fort I osteotomy technique (Fig. 25-25). This technique improves overall facial proportion and normalizes exposure of the incisors during smiling. Also, in a large number of patients with Class III occlusions the jaw blamed by the patients and sometimes by dental providers is the mandible, when the problem is actually maxillary deficiency. Surgery in the wrong jaw in these cases can leave problematic facial esthetics, especially in male patients.
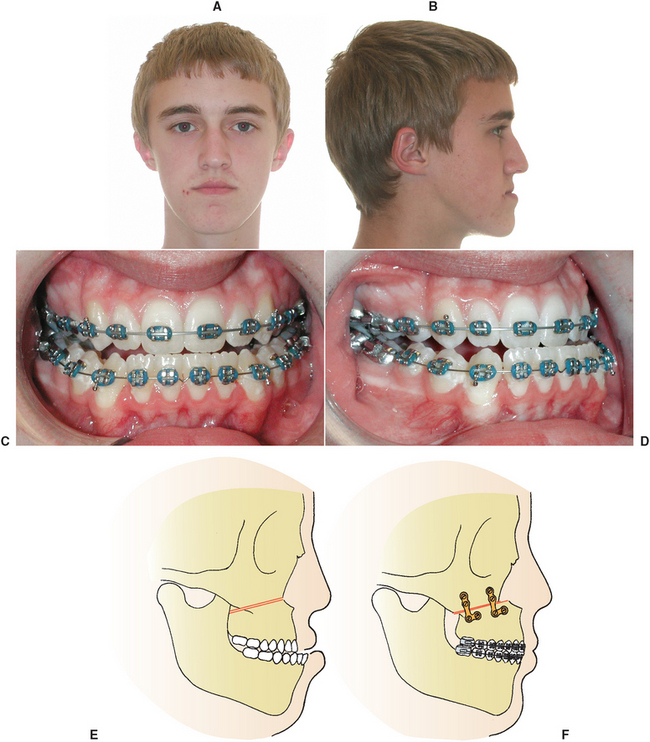
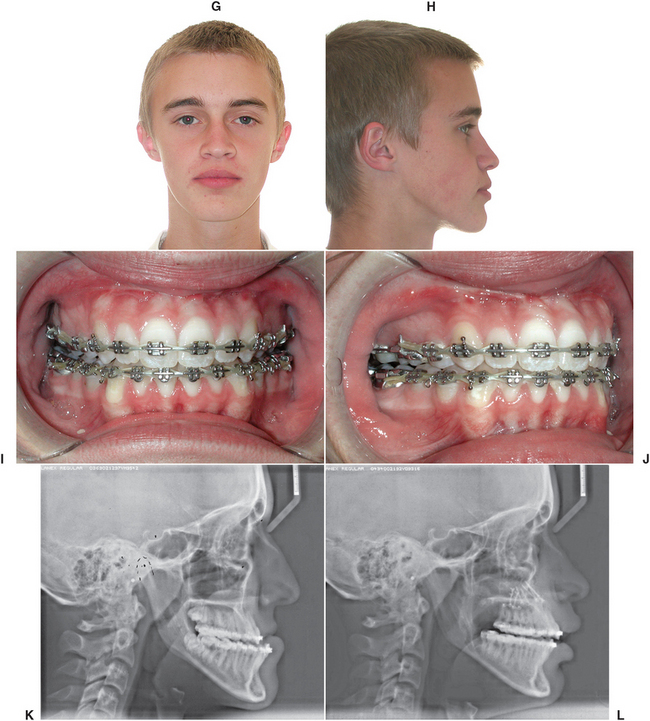
FIGURE 25-24 Case report of Le Fort I advancement. A and B, Preoperative facial esthetics demonstrating maxillary deficiency evident by facial concavity and paranasal deficiency. C and D, Preoperative occlusion demonstrating Class III relationship. E and F, Le Fort I osteotomy for maxillary advancement. G and H, Postoperative facial appearance. (This patient also underwent a simultaneous rhinoplasty procedure.) I and J, Postoperative occlusion. K and L, Preoperative and postoperative radiographs.
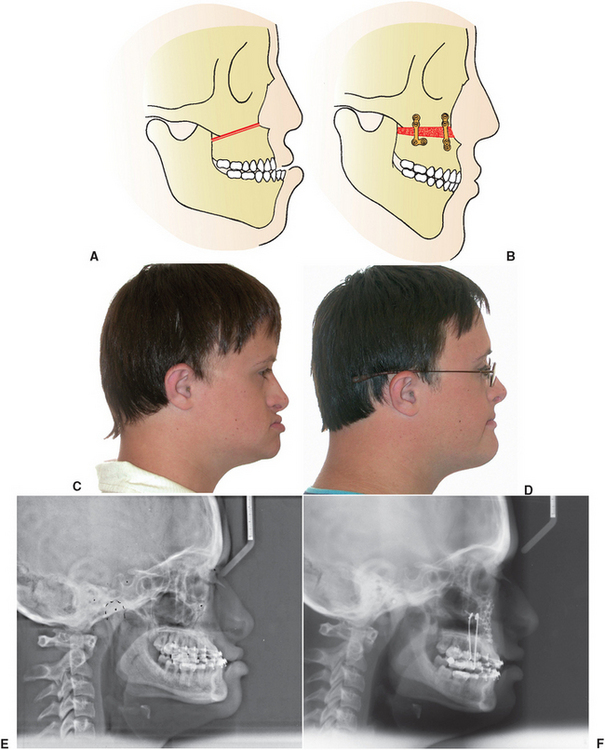
FIGURE 25-25 A and B, Inferior repositioning of maxilla and interpositional bone grafting. C, Preoperative profile view demonstrating vertical deficiency of lower third of face and resulting appearance of relative mandibular excess. D, Postoperative view after inferior repositioning of maxilla. Note normal facial vertical and anteroposterior relationships. E, Preoperative radiograph. F, Postoperative radiograph. Bone plates and auxiliary vertical struts are seen in this view.
In severe midface deformities with infraorbital rim and malar eminence deficiency, a Le Fort III or modified Le Fort III type of osteotomy is necessary. These procedures advance the maxilla and the malar bones and, in some cases, the anterior portion of the nasal bones. This type of treatment is commonly required in patients with craniofacial deformities such as Apert’s or Crouzon’s syndrome (Fig. 25-26).
Combination Deformities and Asymmetries
In many cases the facial deformity involves a combination of abnormalities in the maxilla and the mandible.26 In these cases, treatment may require a combination of maxillary and mandibular osteotomies to achieve the best possible occlusal, functional, and esthetic result (Figs. 25-27 and 25-28). In some cases, surgical treatment may involve a combination of standard surgical procedures described before in combination with more complicated osteotomies accomplished through extraoral approach using bone grafts harvested from the iliac crest (Fig. 25-29). Treatment of asymmetry in more than two planes of space frequently requires maxillary surgery, mandibular surgery, and inferior border osteotomies, as well as recontouring or augmentation of other areas of the maxilla and mandible (Fig. 25-30).
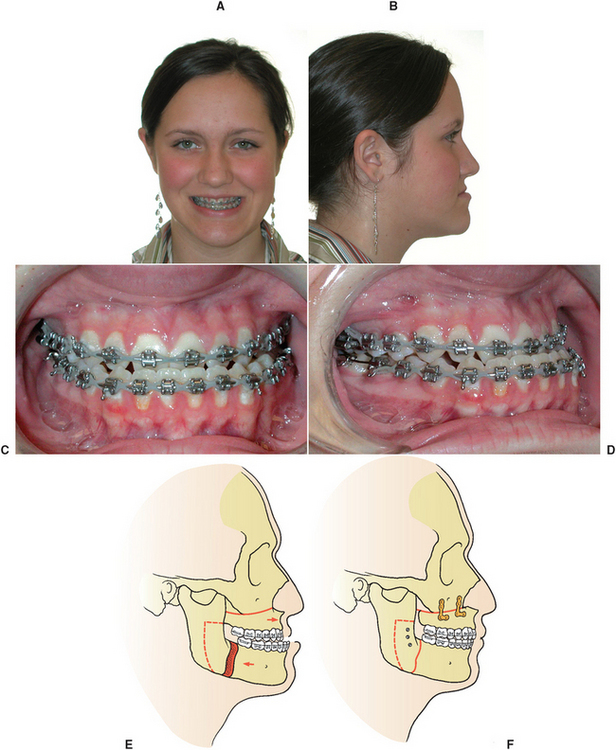
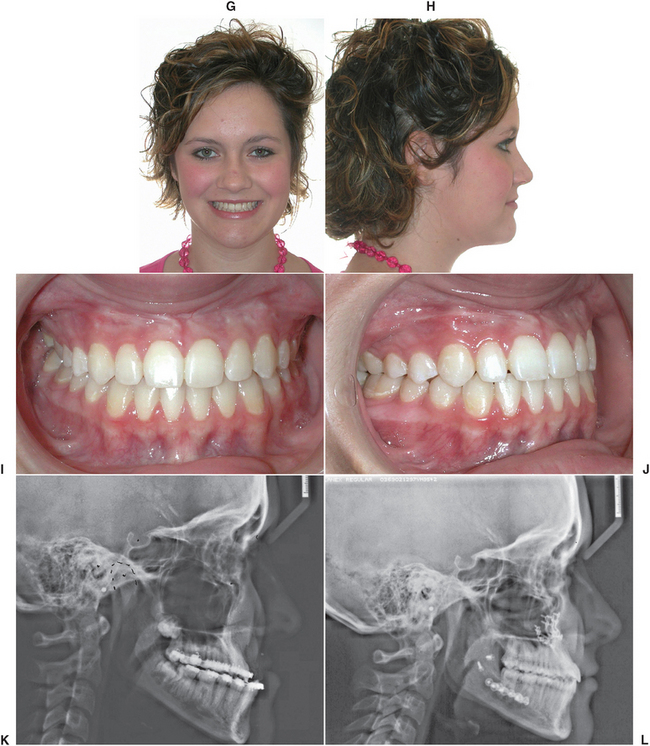
FIGURE 25-27 Case report of maxillary advancement and mandibular setback. A and B, Preoperative facial esthetics demonstrating severe maxillary deficiency combined with mandibular excess. C and D, Preoperative occlusion demonstrating Class III relationship. E and F, Le Fort I osteotomy for maxillary advancement and bilateral sagittal osteotomies for setback of the mandible. G and H, Postoperative facial appearance. I and J, Postoperative occlusion. K and L, Preoperative and postoperative radiographs.
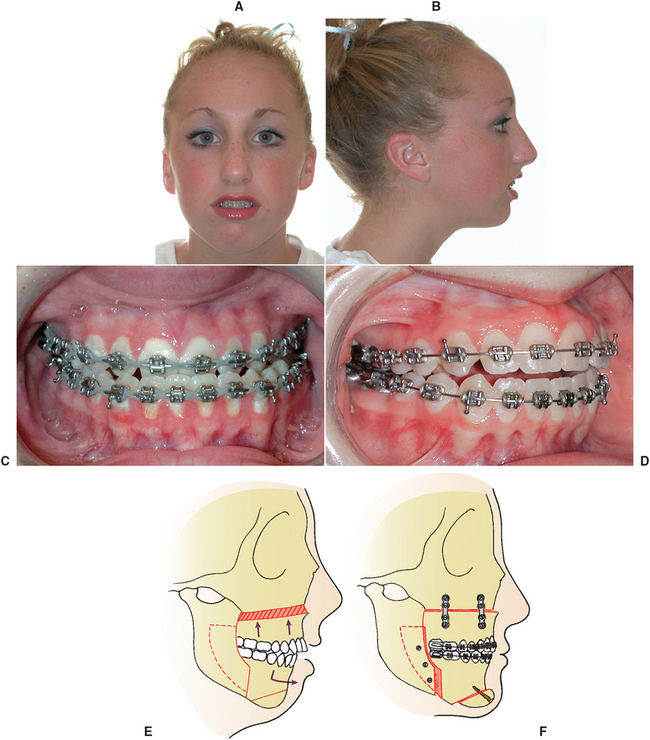
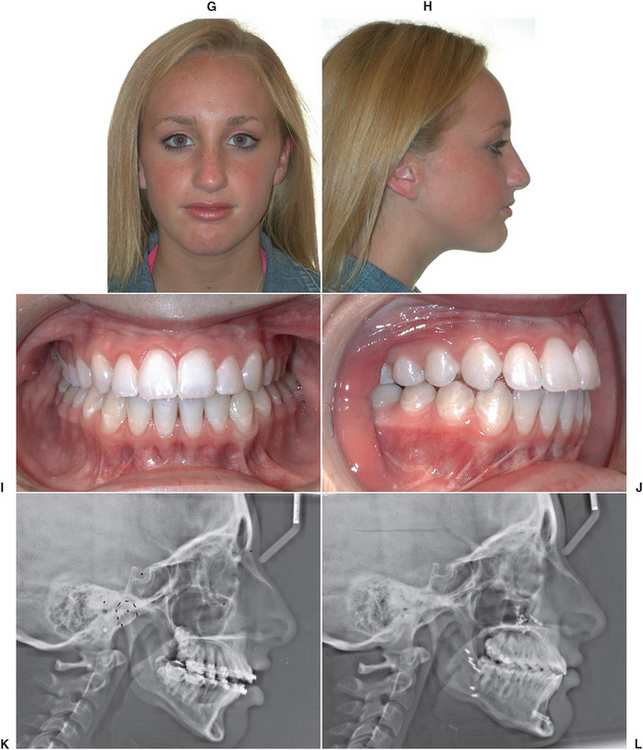
FIGURE 25-28 Case report of superior maxillary repositioning and advancement, mandibular advancement, and genioplasty. A and B, Preoperative facial esthetics demonstrating typical appearance of vertical maxillary excess and mandibular deficiency, including excess incisor exposure, lip incompetence, and lack of chin projection. C and D, Preoperative occlusion demonstrating Class II malocclusion. E and F, Diagram of Le Fort I osteotomy with superior repositioning of maxilla, sagittal osteotomies of mandible for advancement, and advancement genioplasty. G and H, Postoperative facial appearance. I and J, Postoperative occlusion. K and L, Preoperative and postoperative radiographs.
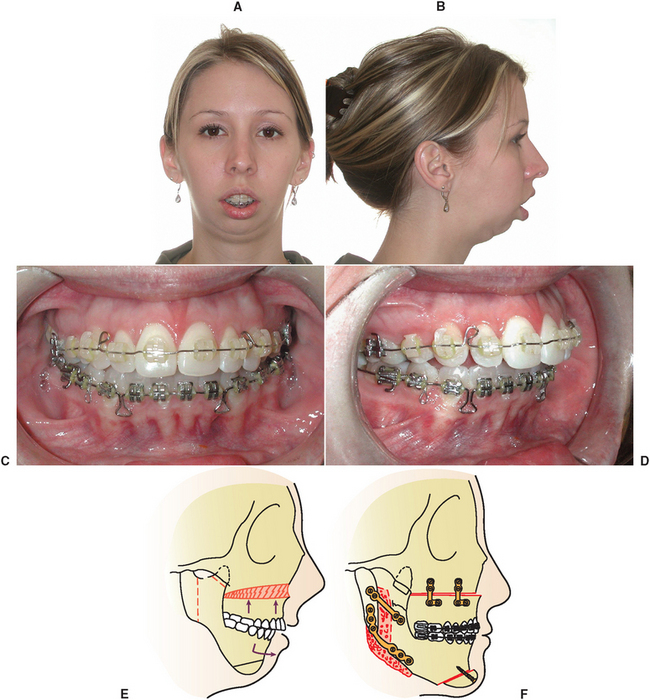
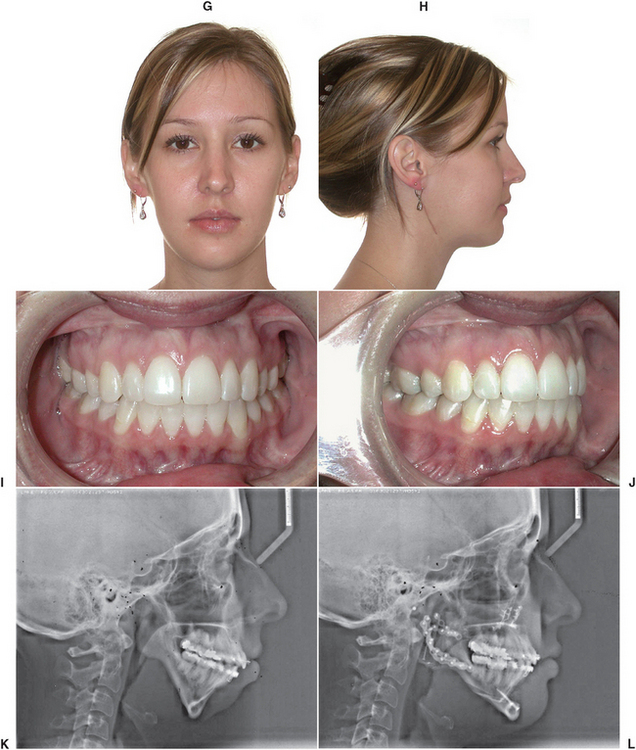
FIGURE 25-29 Case report of superior maxillary repositioning, extraoral approach for mandibular advancement, and genioplasty. A and B, Preoperative facial esthetics demonstrating typical appearance of vertical maxillary excess and mandibular deficiency, including excess incisor exposure, lip incompetence, and lack of chin projection. C and D, Preoperative occlusion demonstrating class II malocclusion. E and F, Diagram of Le Fort I osteotomy with superior repositioning of maxilla, extraoral osteotomies of mandible with bone grafts, and advancement genioplasty. G and H, Postoperative facial appearance. I and J, Postoperative occlusion. K and L, Preoperative and postoperative radiographs.
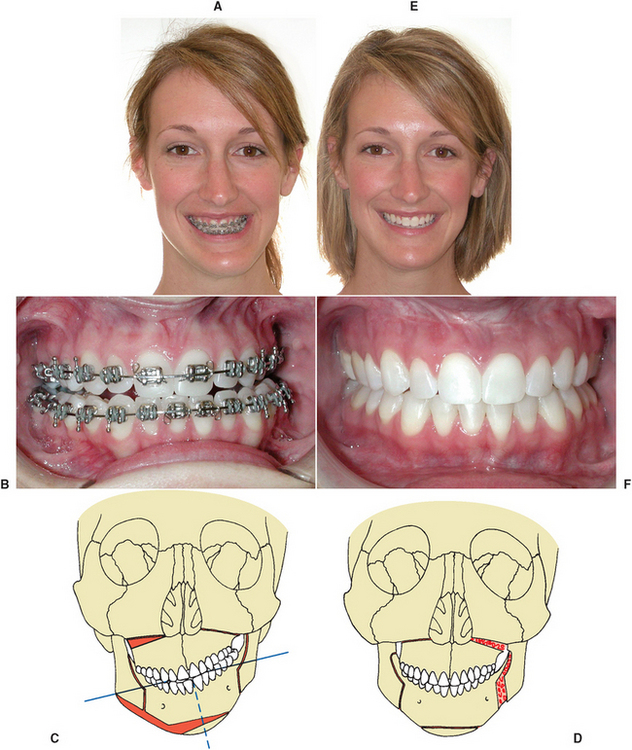
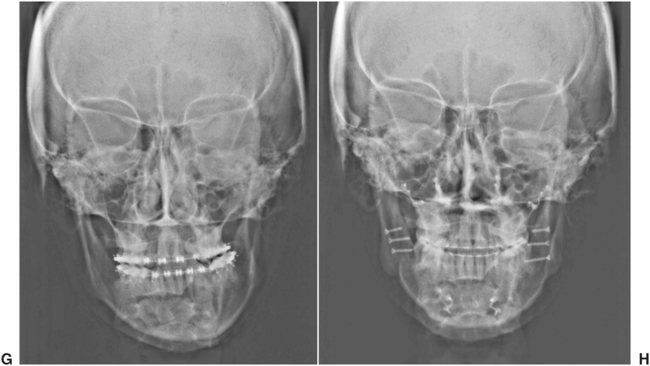
FIGURE 25-30 Facial asymmetry requiring maxillary and mandibular osteotomies, genioplasty, and inferior border recontouring for correction. A, Preoperative facial esthetics. B, Preoperative occlusion. C and D, Diagrams of Le Fort I osteotomy with inferior repositioning on left side and superior repositioning on right, sagittal osteotomies of mandible with advancement on left side and superior repositioning on right, asymmetric genioplasty, and right inferior border recontouring. E, Postoperative facial appearance. F, Postoperative occlusion. G, Preoperative radiograph. H, Postoperative radiograph.
Orthognathic Surgery for Obstructive Sleep Apnea
Obstructive sleep apnea is the occurrence of apneic events (breathing stops) during sleep such that a patient has cessation of airflow for more than 10 seconds. This can be a serious condition with manifestations ranging from sleep disruption/deprivation and daytime somnolence to severe hypoxia during sleep and the potential of associated respiratory and cardiac abnormalities, and even death.27
The primary problem is a collapse of the airway during sleep. This can be a result of decreased muscle tone in the palate, tongue, or pharyngeal musculature. This condition can be associated with mandibular deficiency and the subsequent lack of forward suspension of the tongue and hypopharyngeal musculature (Fig. 25-31, A). This is usually accentuated in the supine position. Other factors such as obesity and alcohol or sedative drug use during sleep can aggravate the problem.
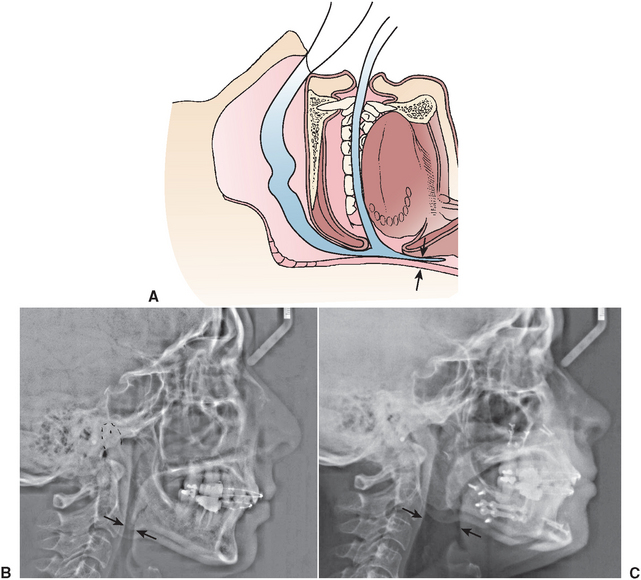
FIGURE 25-31 A, Narrow or collapsed airway as a result of mandibular deficiency. B, Preoperative cephalometric radiograph showing narrow hypopharyngeal airway. C, Postoperative cephalogram showing significant expansion of the airway.
The complete workup for the patient with obstructive sleep apnea is beyond the scope of this chapter but usually includes a comprehensive physical evaluation, nasopharyngoscopy, a dentofacial evaluation, and polysomnography sleep study. Treatment may included nonsurgical measures such as weight loss, positional changes during sleep, jaw positioning devices, or continuous positive airway pressure using a facial or nasal mask during sleep.28,29
Surgical correction may include a limited uvulopalatoplasty or uvulopharyngealpalatoplasty in which varying portions of the soft palate, uvula, tonsils, and pharyngeal walls are resected to open the airway. Maxillary and mandibular advancement with orthognathic surgery has also been shown to be effective in improving the airway in many patients.30 This improvement is a result of expanding the airway at the level of the soft palate, base of the tongue, and hypopharyngeal airway. This can be seen by comparing preoperative and postoperative radiographs (Fig. 25-31). The airway expansion resulting from surgery actually includes all dimensions, even lateral expansion.31
DISTRACTION OSTEOGENESIS
One new approach to correction of deficiencies in the mandible and the maxilla involves the use of distraction osteogenesis (DO). When correcting deformities associated with these deficiencies, the conventional osteotomy techniques have several potential limitations (described previously in this chapter). When large skeletal movements are required, the associated soft tissue often cannot adapt to the acute changes and stretching that result from the surgical repositioning of bony segments. This failure of tissue adaptation results in several problems, including surgical relapse, potential excessive loading of the TMJ structures, and increased severity of neurosensory loss as a result of stretching of nerves. In some cases the amount of movement is so large that the gaps created require bone grafts harvested from secondary surgical sites such as the iliac crest.
DO involves cutting an osteotomy to separate segments of bone and the application of an appliance that will facilitate the gradual and incremental separation of bone segments (Fig. 25-32). The gradual tension placed on the distracting bony interface produces continuous bone formation. Additionally, the surrounding tissue appears to adapt to this gradual tension, producing adaptive changes in all surrounding tissues, including muscles and tendons, nerves, cartilage, blood vessels, and skin. Because the adaptation involves a variety of tissue types in addition to bone, this concept should also include the term distraction histogenesis.
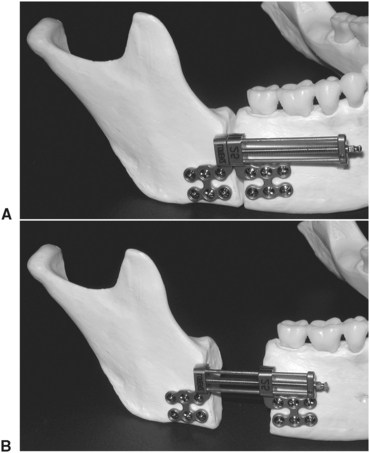
FIGURE 25-32 Distractor appliance used for mandibular advancement. A, Osteotomy of posterior mandibular body and ramus area with distractor in place. B, View showing distraction appliance fully expanded. Regenerate bone fills the intrabony gap during slow incremental activation of distractor that slowly separates the segments.
The concept of distraction is not new. Use of traction techniques to help bones heal to a correct length can be traced back to the time of Hippocrates when an external device was used to apply traction to a fractured and shortened leg.32 A Russian surgeon, Gavril Ilizarov, developed the current concept of correcting bony deficiencies in the 1950s. The result of his work was not widely disseminated to the rest of the world until the late 1970s and early 1980s.33,34 Since that time, the application of these principles has extended to all forms of orthopedic correction, including craniofacial surgery.35,36
DO involves several phases, including the osteotomy or surgical phase, latency period, distraction phase, consolidation phase, appliance removal, and remodeling. During the surgical phase an osteotomy is completed and the distraction appliance is secured. The latency phase is the period when very early stages of bone healing begin to take place at the osteotomy bony interface. The latency phase is generally 7 days during which time the appliance is not activated. After the latency period the distraction phase begins at a rate of 1 mm per day. This distraction rate is usually applied by opening or activating the appliance 0.5 mm twice each day. The amount of activation per day is termed the rate of distraction; the timing of appliance activation each day is termed the rhythm. During the distraction phase the new immature bone that forms is called the regenerate. Once the appropriate amount of distraction has been achieved, the appliance remains in place during the consolidation phase, allowing for mineralization of the regenerate bone. The appliance is then removed, and the period from the application of normal functional loads to the complete maturation of the bone is termed the remodeling period.
Because the use of these techniques in orthognathic surgery is relatively new, few long-term studies are available that document all of the potential benefits of DO. Possible advantages include the ability to produce larger skeletal movements, elimination of the need for bone grafts and the associated secondary surgical site, better long-term stability, less trauma to the TMJs, and decreased neurosensory loss. DO also has certain disadvantages: The placement and positioning of the appliance to produce the desired vector of bone movement is technique sensitive and sometimes results in less than ideal occlusal positioning, resulting in discrepancies such as small open bites or asymmetries. Other disadvantages include the need for two procedures: (1) placement and (2) removal of the distractors, as well as increased cost and longer treatment time, with more frequent appointments with the surgeon and the orthodontist.
One of the earliest uses of the DO concept in orthognathic surgery involved widening of the maxilla with a technique termed surgical-assisted rapid palatal expansion.37 An adult maxilla with significant transverse deficiency is nearly impossible to correct with conventional orthodontic treatment. Even correction with segmental maxillary surgery to produce expansion has often shown disappointing results.38 The use of surgical assisted palatal expansion, incorporating the concepts of DO, seems to produce better long-term results in these cases.39 In these cases the expansion device is secured in place by the orthodontist. A surgical procedure is then completed by performing the bony cuts as described for a Le Fort I osteotomy, with the exception that the most posterior attachment of the lateral nasal wall and perpendicular plate of the palatine bone are not divided. A midline cut is also completed to create separation between the central incisors extending along the midpalatal suture. After a latency period the expansion device is activated 1 mm per day until the desired expansion takes place (Fig. 25-33). During this time a space develops between the central incisors, along the midpalatal suture, and at the area of the osteotomy along the lateral maxillary wall.

FIGURE 25-33 Distraction osteogenesis with surgically assisted palatal expansion for correction of transverse maxillary deficiency. A, Severe constriction of maxilla with inadequate arch length (note that severe crowding exists even though premolars have been extracted). B, Expansion device in place. C, Maxilla expanded (note space between central incisors). Osteogenesis, with bone formation, and histogenesis, with formation of gingival tissue, are occurring. D, Space closed with anterior teeth orthodontically aligned using newly formed regenerate bone. E, Radiograph showing expansion with immature regenerate bone in anterior space. F, Radiograph after orthodontic alignment.
Bony regenerate gradually fills and matures in these areas. The appliance is then removed, and active orthodontic treatment is begun to close space between teeth, properly align the arch, and maintain the expansion.
In the case of mandibular deficiency, the initial surgical procedure involves performing an osteotomy and placement of the distraction appliance. After a latency period of 7 days, the distraction occurs with a rate and rhythm of 1 mm per day (completed by activating the appliance 0.5 mm twice each day). Once this distraction is complete, the appliance is left is place for the consolidation phase, which is usually 2 or 3 times the amount of time required for the distraction phase. The appliance is then removed, and active orthodontic treatment continues. Figure 25-34 demonstrates a case of DO of the mandible.

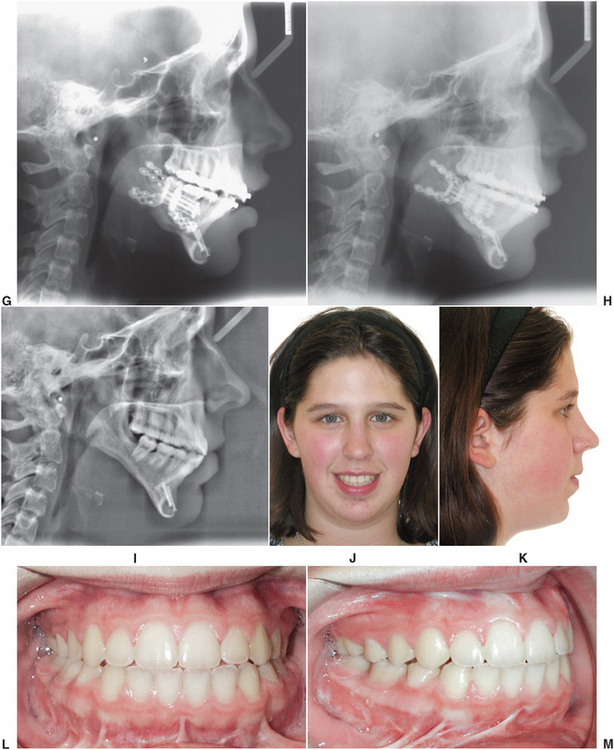
FIGURE 25-34 Case report of distraction osteogenesis to correct severe mandibular deficiency. A and B, Preoperative facial esthetics demonstrating severe mandibular deficiency. C and D, Preoperative occlusion demonstrating Class II relationship. E, Preoperative cephalometric radiograph. F, Surgical procedure to create osteotomy and place distraction appliance. G, Postoperative radiograph after latency phase complete and distraction started (chin advancement was completed at the same time distractors were applied). H, Radiograph after 16 days of distraction at 1 mm per day. I, Radiograph after distraction appliances removed, completion of orthodontic treatment, and debanding. J and K, Postoperative facial appearance. L and M, Postoperative occlusal views.
Distraction appliances are also available for maxillary and midface advancement. In some cases of traditional maxillary repositioning, autogenous bone may be required for grafting into the bony defect. The need for grafting obviously requires donor site surgery with the associated morbidities. DO eliminates the need for graft harvest in many of these patients. In patients with a cleft lip and palate there is often substantial scarring from multiple previous surgical procedures. This scarring combined with significant growth abnormalities creates soft tissue limitations that may prevent single-stage correction with conventional orthognathic surgical techniques. DO can be effective in treatment of these patients by gradually stretching the soft tissue envelope, generating new soft and hard tissue, eliminating the need for graft harvest, and providing good long-term stability.40 Figure 25-35 demonstrates the effective use of DO for maxillary advancement in such a patient. Maxillary repositioning with DO may allow larger advancements with improved long-term stability.41,42
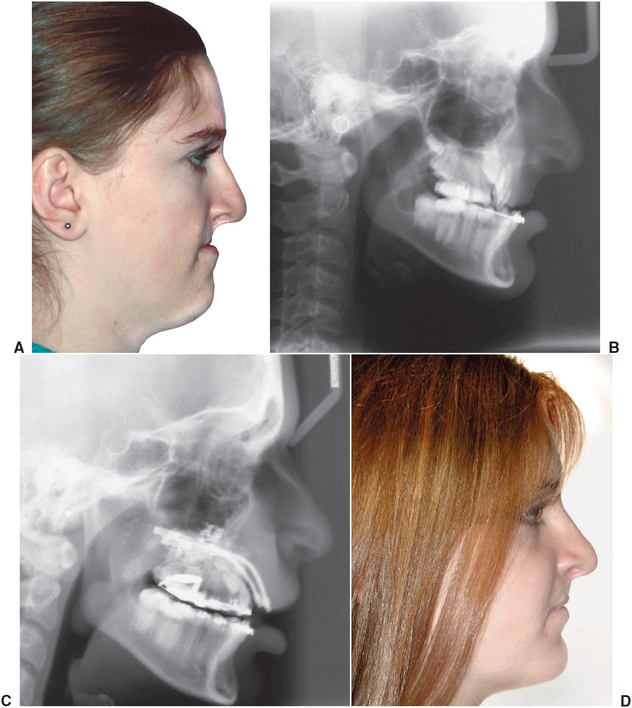
FIGURE 25-35 Distraction osteogenesis for correction of maxillary deficiency. A, Severe midface deficiency resulting from cleft lip and palate and multiple surgical interventions. B, Radiograph demonstrating maxillary hypoplasia and Class III malocclusion. C, Radiograph showing advancement of the maxilla using distractors. D, Final profile demonstrating improved facial balance and occlusion. (Photos courtesy Dr. Dan Spagnoli.)
PERIOPERATIVE CARE OF THE ORTHOGNATHIC SURGICAL PATIENT
Patients undergoing orthognathic surgery are usually admitted to the hospital on the day of surgery. Before surgery the medical history, complete physical examination, preoperative laboratory tests, radiographic examinations, and consultation with the anesthesiologist are completed. Orthognathic surgery is accomplished in the operating room with the patient under general anesthesia. After surgery, the patient is taken to the postanesthesia care unit (i.e., recovery room) for an appropriate period, usually until alert, oriented, comfortable, and exhibiting stable vital signs; then the patient is returned to the hospital room. The nursing staff trained and experienced in the postoperative care of surgery patients continually monitor postoperative progress. The patient is discharged when feeling comfortable, urinating without assistance, taking food and fluid orally without difficulty, and ambulating well. The postsurgical hospital stay usually ranges from 1 to 4 days. Patients generally require only mild to moderate pain medication during this time and often require no analgesics after discharge. As soon as is feasible, postoperative radiographs are obtained to ensure that the predicted bone changes have taken place and that stabilization devices are in the proper position.
The importance of postoperative nutrition should be discussed with patients and their families before the hospital admission for surgery. During the postoperative hospital stay, a member of the dietary staff may instruct the patient in methods of obtaining adequate nutrition during the period of IMF or limited jaw function. Special cookbooks designed for patients undergoing jaw surgery contain instructions for the preparation of diets in a blender.
In the past, one of the major considerations in the immediate postoperative period was the difficulty resulting from IMF. When the jaws are wired together, the patient has initial difficulties in obtaining adequate nutrition, performing necessary oral hygiene, and communicating verbally. The average IMF period ranges from 6 to 8 weeks.
During the past few years, several systems using small bone screws and bone plates have been developed to provide direct bony stabilization in the area of the osteotomies (Fig. 25-36).43–46 The most recent development in rigid internal fixation is the use of screws and plates made of resorbable material. The materials are capable of maintaining adequate strength to stabilize bone during the healing period and are then resorbed by hydrolyzation. The use of these rigid fixation systems allows for early release from or total elimination of IMF, which results in improved patient comfort, convenience of speech and oral hygiene, and improved postsurgical jaw stability and function.
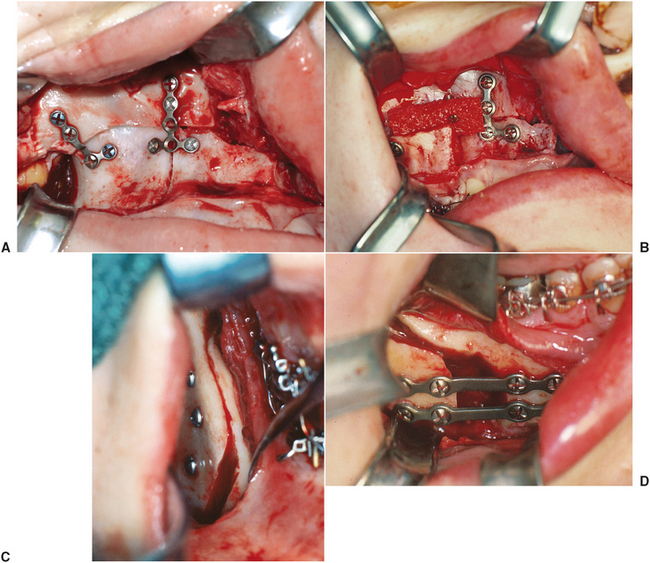
FIGURE 25-36 A, Use of small bone plates for stabilization of maxillary osteotomy. B, Maxillary advancement and downgraft with iliac crest bone graft stabilized with bone plates. C, Lag screws used to secure mandibular sagittal split osteotomy. D, Bone plates used to stabilize sagittal split osteotomy.
At the time of surgery, a small acrylic occlusal wafer is used to help position and stabilize the occlusion. When the IMF is released (usually in the operating room), the splint is wired to the upper or lower jaw. Light elastics are then placed on the surgical wires, and the combination of the splint and elastics serves to guide the jaw into the new postsurgical occlusion (Fig. 25-37). After an adequate accommodation period, the occlusal splint is removed and the patient is returned to the orthodontist’s care.
POSTSURGICAL TREATMENT PHASE
When a satisfactory range of jaw motion and stability of the osteotomy sites are achieved, the orthodontic treatment can be finished. The heavy surgical arch wires are removed and replaced with light orthodontic wire. Final alignment and positioning of the teeth is accomplished, as is closure of any residual extraction space. The light vertical elastics are left in place at this time to override proprioceptive impulses from the teeth, which otherwise would cause the patient to seek a new position of maximal intercuspation. The settling process proceeds rapidly and rarely takes longer than 6 to 10 months.
Retention after surgical orthodontics is no different from that for other adult patients, and definitive periodontal and prosthetic treatment can be initiated immediately after the final occlusal relationships have been established.
Postsurgical Restorative and Prosthetic Considerations
When patients require complex final restorative treatment, it is important to establish stable, full-arch contact as soon after orthodontic debanding as possible. Posterior vertical contacts are important in patients who have only anterior components of occlusion remaining. Well-fitting, temporary, removable partial dentures may suffice, and these appliances should be relined with tissue-conditioning materials as needed to maintain the posterior support during healing. When postsurgical orthodontics is complete, the remainder of restorative treatment can be accomplished in the same manner as for any nonsurgical patient.
Postsurgical Dental and Periodontal Considerations
The patient should be seen for a maintenance dental and periodontal evaluation approximately 10 to 14 weeks postoperatively. The mucogingival status is reevaluated, the mouth deplaqued, and areas of inflammation or pocketing lightly scaled. Frequent recall maintenance should continue during the remainder of orthodontic care when necessary. After the orthodontic appliances are removed, a thorough prophylaxis with a review of oral hygiene techniques is advisable. A thorough periodontal reevaluation 3 to 6 months after completion of the postsurgical orthodontics will determine future treatment needs. Periodontal surgery, including crown-lengthening or regenerative procedures, should be performed after the inflammation associated with orthodontic appliances has resolved. Areas of hyperplastic tissue should be observed for 3 to 6 months after orthodontic therapy, unless esthetic or restorative considerations necessitate earlier tissue removal. After completion of periodontal treatment, recall intervals should be adjusted to accommodate the individual patient’s needs.
SUMMARY
The treatment of patients with dentofacial deformity involves the evaluation and treatment of many types of dental and skeletal problems. These problems require that all practitioners involved in patient care interact in a multidisciplinary team approach to treatment. This sequential, team approach yields the most satisfying results.
REFERENCES
1. Brunelle, JA, Bhat, M, Lipton, JA. Prevalence and distributions of selected occlusal characteristics in the US population, 1988-1991. J Dent Res. 1996;75:706–713.
2. Proffit, WR, Fields, HW, Moray, LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the N-HANES III survey. Int J Adult Orthodon Orthognath Surg. 1998;13:97–106.
3. Proffit, WR, White, RP, Jr. Dentofacial problems: prevalence and treatment need. In: Proffit WR, White RP, Jr., Sarver DM, eds. Contemporary treatment of dentofacial deformity. St Louis: Mosby, 2003.
4. Enlow, DH, Hans, M. Essentials of facial growth. Philadelphia: WB Saunders, 1996.
5. Enlow, DH. Wolff’s law and factor of architectonic circumstance. Am J Orthod. 1968;54:803.
6. Enlow, DH. Craniofacial growth and development. In: Posnick JC, ed. Craniofacial and maxillofacial surgery in children and young adults. Philadelphia: WB Saunders, 2000.
7. Fields, HW, Warren, DW, Black, K, et al. Relationship between vertical dentofacial morphology and respiration in adolescents. Am J Orthod Dentofacial Orthop. 1991;99:147–154.
8. Tucker, MR, Moriarty, JM, Koth, DL, et al. Evaluation of treatment of patients with dentofacial deformities: a multidisciplinary approach. North Carolina Dental Review. 1985;3:13.
9. Burstone, CJ, James, RB, Legan, H, et al. Cephalometrics for orthognathic surgery. J Oral Surg. 1978;36:269.
10. Steiner, CC. Cephalometrics in clinical practice angle. Orthodontics. 1959;28:8.
11. Smith, JD, Thomas, PM, Proffit, R. A comparison of current prediction imaging programs. Am J Orthod Dentofacial Orthop. 2004;125:527.
12. Bell, WH, Dann, JJ. Correction of dentofacial deformities by surgery in the anterior part of the jaws. Am J Orthod. 1973;64:162.
13. Caldwell, JB, Letterman, GS. Vertical osteotomy in the mandibular rami for correction of prognathism. J Oral Surg. 1954;12:185.
14. Hall, HD, Chase, DC, Payor, LG. Evaluation and realignment of the intraoral vertical subcondylar osteotomy. J Oral Surg. 1975;33:333.
15. Trauner, R, Obwegeser, H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg Oral Med Oral Pathol. 1957;10:677.
16. Dalpont, G. Retromolar osteotomy for the correction of prognathism. J Oral Surg. 1961;19:42.
17. Hunsuck, EE. A modified intraoral sagittal splitting technique for mandibular prognathism. J Oral Surg. 1968;26:249.
18. Epker, BN. Modifications in the sagittal osteotomy of the mandible. J Oral Surg. 1977;35:157.
19. Robinson, M. Micrognathism corrected by vertical osteotomy of ascending ramus and iliac bone graft: new technique. Oral Surg Oral Med Oral Pathol. 1957;10:125.
20. Kufner, J. Experience with a modified procedure for correction of open bite. In: Walker RV, ed. Transactions of the Third International Congress of Oral Surgery. London: E&S Livingstone, 1970.
21. Schuchardt, K. Experiences with the surgical treatment of deformities of the jaws: prognathia, micrognathia, and open bite. In: Wallace AG, ed. Second Congress of International Society of Plastic Surgeons. London: E&S Livingstone, 1959.
22. Wunderer, S. Erfahrungen mitder operativen Behandlung hochgradiger Prognathien. Dtsch Zahn Mund Kieferheilkd. 1963;39:451.
23. Bell, WH, Fonseca, RJ, Kenneky, JW, Levy, BM. Bone healing and revascularization after total maxillary osteotomy. J Oral Surg. 1975;33:253.
24. Tucker, MR, White, RP, Jr. Maxillary orthognathic surgery. In: Tucker MR, White RA, Jr., Terry BC, et al, eds. Rigid fixation for maxillofacial surgery. Philadelphia: JB Lippincott, 1991.
25. Jacobson, R, Sarver, DM. The predictability of maxillary repositioning in LeFort I orthognathic surgery. Am J Orthod Dentofacial Orthop. 2002;122:142.
26. Busby, BR, Bailey, LJ, Proffit, WR, et al. Long-term stability of surgical Class III treatment: a study of 5-year postsurgical results. Int J Adult Orthodon Orthognath Surg. 2002;17:159.
27. Guilleminault, C. Obstructive sleep apnea: the clinical syndrome and historical perspective. Med Clin North Am. 1985;69:1187.
28. Veasey, SC, Guilleminault, C, Strohl, KP, et al. Medical therapy for obstructive sleep apnea: a review by the Medical Therapy for Obstructive Sleep Apnea Task Force of the Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep. 2006;29:1036–1044.
29. Senn, O, Bloch, KE, Iseli, A, et al. Oral appliances for the treatment of snoring and obstructive sleep apnea. Oto-Rhino-Laryngologia Nova. 2001;11:168.
30. Waite, PD, Vilos, GA. Surgical changes of posterior airway space in obstructive sleep apnea. Oral and Maxillofacial Surgery Clinics of North America. 2002;14:385.
31. Fairburn, SC, Waite, PD, Vilos, G, et al. Three-dimensional changes in upper airways of patients with obstructive sleep apnea following maxillomandibular advancement. J Oral Maxillofac Surg. 2007;65:6.
32. Peltier, LF. External skeletal fixation for the treatment of fractures. In: Fractures: a history and iconography of their treatment. San Francisco: Norman Publishing; 1990.
33. Ilizarov, GA. The principles of the Ilizarov method. Bull Hosp Jt Dis. 1997;56:49–53.
34. Ilizarov, G, Devyatov, A, Kameran, V. Plastic reconstruction of longitudinal bone defects by means of compression and subsequent distraction. Acta Chir Plast. 1980;22:32.
35. Altuna, G, Walker, DA, Freeman, E. Rapid orthopedic lengthening of the mandible in primates by sagittal split osteotomy and distraction osteogenesis: a pilot study. Int J Adult Orthodon Orthognath Surg. 1995;10:59.
36. Guerrero, CA, Bell, WH. Intraoral distraction. In: Distraction of the craniofacial skeletal. New York: Springer-Verlag; 1999.
37. Lines, PA. Adult rapid maxillary expansion with corticotomy. Am J Orthod. 1975;67:44.
38. Proffit, WR, Turvey, TA, Phillips, C. Orthognathic surgery: a hierarchy of stability. Int J Adult Orthodon Orthognath Surg. 1996;11:191.
39. Betts, NJ, Vanarsdall, RL, Barber, HD, et al. Diagnosis and treatment of transverse maxillary deficiency. Int J Adult Orthodon Orthognath Surg. 1995;10:75.
40. Figueroa, AA, Polley, JW. Management of severe cleft maxillary deficiency with distraction osteogenesis: procedure and results. Am J Orthod Dentofacial Orthop. 1999;115:1–12.
41. Rachmiel, A. Treatment of maxillary cleft palate: distraction osteogenesis verses orthognathic surgery. Part one: maxillary distraction. J Oral Maxillofac Surg. 2007;65:753–757.
42. Precious, DS. Treatment of retruded maxilla in cleft lip and palate: orthognathic surgery verses distraction osteogenesis—the case for orthognathic surgery. J Oral Maxillofacial Surg. 2007;65:758–761.
43. Spiessl, B. New concepts of maxillofacial bone surgery. Berlin: Springer-Verlag, 1975.
44. Borstlap, WA, Stoelinga, PJW, Hoppenreijs, TJM, van’t Hof, MA. Stabilisation of sagittal split advancement osteotomies with miniplates: a prospective, multicentre study with two-year follow-up. I. Clinical parameters. Int J Oral Maxillofac Surg. 2004;33:433.
45. Sittitavornwong, S, Waite, PD, Dann, JJ, Kohn, MW. The stability of maxillary osteotomies fixated with biodegradable mesh in orthognathic surgery. J Oral Maxillofac Surg. 2006;64:1631.
46. Tucker, MR, Frost, DE, Terry, BC. Mandibular surgery. In: Tucker MR, White RA, Jr., Terry BC, et al, eds. Rigid fixation for maxillofacial surgery. Philadelphia: JB Lippincott, 1991.