ERUPTION AND SHEDDING OF THE TEETH
Possible Causes of Tooth Eruption
Sequence and Chronology of Tooth Eruption
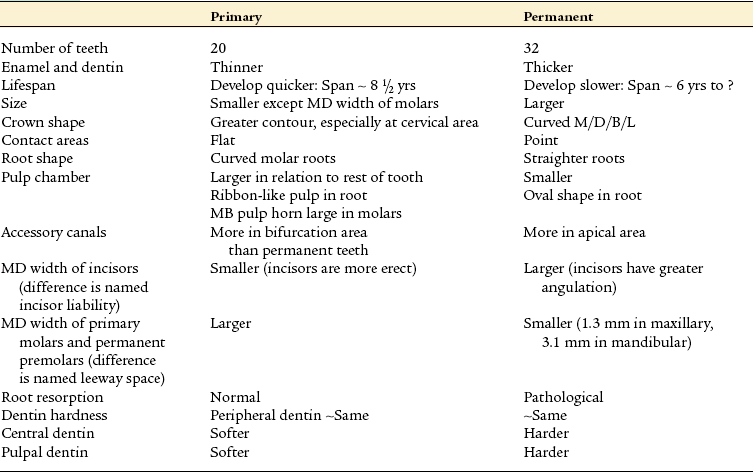
Comparisons of the Primary and Permanent Dentitions
After reading this chapter the student will be able to:
• describe the three phases of tooth eruption: preeruption, prefunctional, and functional
• describe the initial growth of the tooth and the compensational changes that occur in the surrounding overlying and underlying tissues
OVERVIEW
Tooth eruption is the process by which developing teeth emerge through the soft tissue of the jaws and the overlying mucosa to enter the oral cavity, contact the teeth of the opposing arch, and function in mastication. The movements related to tooth eruption begin during crown formation and require adjustments relative to the forming bony crypt. This is the preeruptive phase. Tooth eruption is also involved in the initiation of root development and continues until the tooth’s emergence into the oral cavity, which is the prefunctional eruptive phase. The teeth continue to erupt until they reach incisal or occlusal contact. Then they undergo functional eruptive movements, which include compensation for jaw growth and occlusal wear of the enamel. This stage is the functional eruptive phase. Eruption is actually a continuous process that ends only with the loss of the tooth. Each dentition, primary and permanent, has various problems during eruption and in the sequencing of eruption in the oral cavity. Teeth differ extensively in their eruptive schedules as well. This chapter describes these events. Finally, the process of tooth shedding or exfoliation of the primary dentition is discussed. Primary tooth loss results from three fundamental causes: root resorption, bone resorption, and size of crown too small to withstand mastication.
PREERUPTIVE PHASE
The preeruptive phase includes all movements of primary and permanent tooth crowns from the time of their early initiation and formation to the time of crown completion. Therefore this phase is finished with early initiation of root formation. The developing crowns move constantly in the jaws during the preeruptive phase. They respond to positional changes of the neighboring crowns and to changes in the mandible and maxilla as the face develops outward, forward, and downward away from the brain in its maturing growth path. During the lengthening of the jaws, primary and permanent teeth make mesial and distal movements. Eventually the permanent tooth crowns move within the jaws, adjusting their position to the resorptive roots of the primary dentition and the remodeling alveolar processes, especially during the mixed dentition period from 8 to 12 years of age.
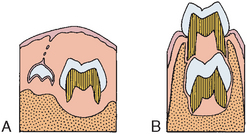
Early in the preeruptive period, the permanent anterior teeth begin developing lingual to the incisal level of the primary teeth (Figs. 6-1 and 6-2). Later, however, as the primary teeth erupt, the permanent successors are positioned lingual to the apical third of their roots. The permanent premolars shift from a location near the occlusal area of the primary molars to a location enclosed within the roots of the primary molars (see Fig. 6-2). This change in relative position is the result of the eruption of the primary teeth and an increase in height of the supporting structures. On the other hand, the permanent molars, which have no primary predecessors, develop without this type of relationship (Fig. 6-3). Maxillary molars develop within the tuberosities of the maxilla with their occlusal surfaces slanted distally. Mandibular molars develop in the mandibular rami with their occlusal surfaces slanting mesially (Fig. 6-3). This slant is the result of the angle of eruption as the molars arise from the curvature of the condyle of the posterior mandible. All movements in the preeruptive phase occur within the crypts of the developing and growing crown before root formation begins.

Fig. 6-1 Relative position of primary and permanent incisor teeth. A, Preeruptive period. B, Prefunctional eruptive period.
PREFUNCTIONAL ERUPTIVE PHASE
The prefunctional eruptive phase starts with the initiation of root formation and ends when the teeth reach occlusal contact. Four major events occur during this phase:
1. Root formation requires space for the elongation of the roots. The first step in root formation is proliferation of the epithelial root sheath, which in time causes initiation of root dentin and formation of the pulp tissues of the forming root. Root formation also causes an increase in the fibrous tissue of the surrounding dental follicle (Fig. 6-4).
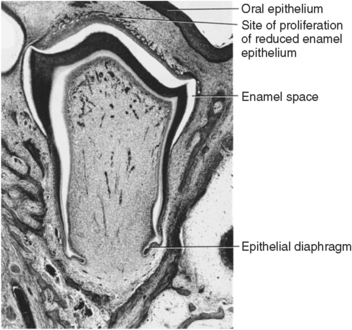
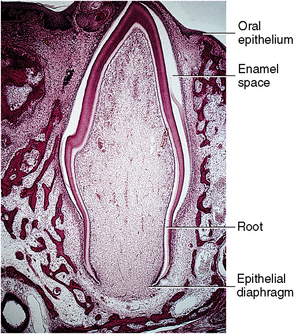
Fig. 6-4 Histology of the prefunctional eruptive phase. The root develops, and reduced epithelium overlying crown approaches oral mucosa. Reduced enamel epithelium proliferates, anticipating fusion.
2. Movement occurs incisally or occlusally through the bony crypt of the jaws to reach the oral mucosa. The movement is the result of a need for space in which the enlarging roots can form. The reduced enamel epithelium next contacts and fuses with the oral epithelium (Fig. 6-5). Both these epithelial layers proliferate toward each other, their cells intermingle, and fusion occurs. A reduced epithelial layer overlying the erupting crown arises from the reduced enamel epithelium (Fig. 6-6).

Fig. 6-6 Fused reduced enamel epithelium and oral epithelium overlie the enamel of crown. (Enamel space occurs as enamel is dissolved in preparation of slide.)
3. Penetration of the tooth’s crown tip through the fused epithelial layers allows entrance of the crown enamel into the oral cavity. Only the organic developmental cuticle (primary), secreted earlier by the ameloblasts, covers the enamel (Fig. 6-7).
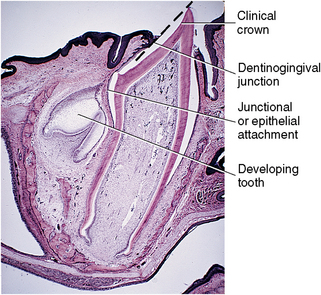
Fig. 6-7 An erupting primary tooth appears in the oral cavity. The permanent tooth’s position is shown on the left. The dotted line indicates cuticle overlying the enamel surface of the erupting tooth.
4. Intraoral occlusal or incisal movement of the erupting tooth continues until clinical contact with the opposing crown occurs. The crown continues to move through the mucosa, causing gradual exposure of the crown surface, with an increasingly apical shift of the gingival attachment (see Fig. 6-7). The exposed crown is the clinical crown, extending from the cusp tip to the area of the gingival attachment. In contrast, the anatomic crown is the entire crown, extending from the cusp tip to the cementoenamel junction.
Changes in Tissues
The prefunctional eruptive phase is characterized by significant changes in the tissues overlying, surrounding, and underlying the erupting teeth.
Overlying the teeth
The dental follicle changes and forms a pathway for the erupting teeth. A zone of degenerating connective tissue fibers and cells immediately overlying the teeth appears first (Figs. 6-8 and 6-9). During the process, the blood vessels decrease in number, and nerve fibers break up into pieces and degenerate. The altered tissue area overlying the teeth becomes visible as an inverted triangular area known as the eruption pathway. In the periphery of this zone, the follicular fibers, regarded as the gubernaculum dentis or gubernacular cord (Fig. 6-10), are directed toward the mucosa. Some scientists believe that these fibers guide the teeth in their movements to ensure complete tooth eruption.
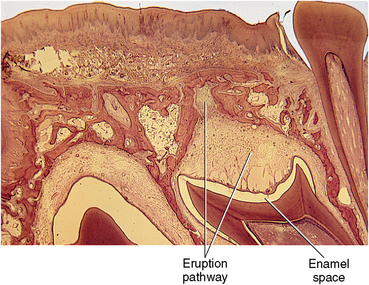
Fig. 6-8 Histology of a prefunctional erupting tooth. Observe the appearance of the eruption pathway developed overlying the crown.
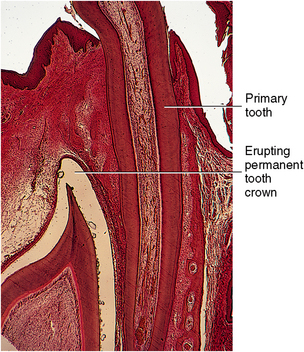
Fig. 6-9 Observe the relation of the functional primary tooth root on the right to the permanent prefunctional erupting crown on the left.
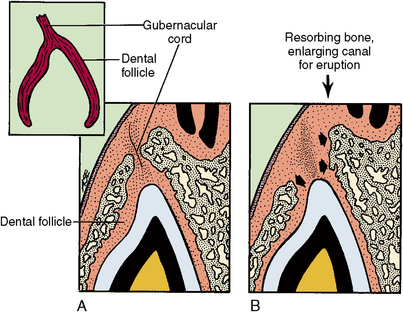
Fig. 6-10 Diagram of a developing eruption pathway. A, Early developing eruption pathway B, Resorption of bone in eruption pathway.
Macrophages appear in the eruption pathway tissue. These cells cause the release of hydrolytic enzymes that aid in the destruction of the cells and fibers in this area with the loss of blood vessels and nerves. Osteoclasts are found along the borders of the resorptive bone overlying the teeth. This bone loss adjacent to the teeth keeps pace with the eruptive movements of the teeth (see Fig. 6-9). Osteoclasts and osteoblasts constantly remodel the alveolar bone as the teeth enlarge and move forward in the direction of the growing face.
Although the process of eruption for permanent teeth is similar to that of the primary teeth, the presence of primary teeth roots poses a problem. The resorption of their roots is similar to the process of bone resorption for the emergence of primary teeth. Permanent teeth establish an eruptive path lingual to the primary anterior teeth and the premolars under the primary molars. Permanent molars erupt into the alveolar free space behind primary teeth (see Fig. 6-9). Small foramina just posterior to the primary tooth row are evidence of the eruption sites of the anterior permanent teeth (Fig. 6-11). As the roots resorb, the primary crowns are lost or shed (Fig. 6-12). Dentin resorption is similar to bone resorption (see Fig. 6-10).
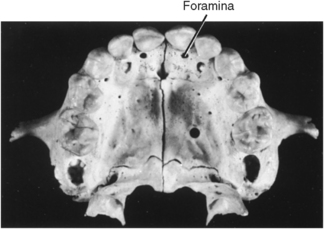
Fig. 6-11 Foramina palatal to maxillary primary incisors. These are sites of eruption for permanent incisors.

Fig. 6-12 Histology of maxilla in the mixed dentition period. Roots of erupted primary teeth are undergoing resorption. Crowns of developing permanent teeth appear below primary teeth.
The resorptive process of primary and permanent teeth results from action of osteoclasts that arise from monocytes of the circulating bloodstream. These monocytes appear and fuse with others to form the multinucleated osteoclasts. Their function is to resorb the hard tissue. They do so by first separating the mineral from the collagen matrix through the action of the hydrolytic enzymes secreted by the osteoclasts. This enzymatic action is believed to occur within lacunae, which are developed by the osteoclasts. The osteoclast’s cell membrane is in contact with the bone and becomes modified by an enfolding process termed the ruffled border (Figs. 6-13 and 6-14). This border greatly increases the surface area of the osteoclast and allows the cell to function maximally in bone resorption (Fig. 6-15).
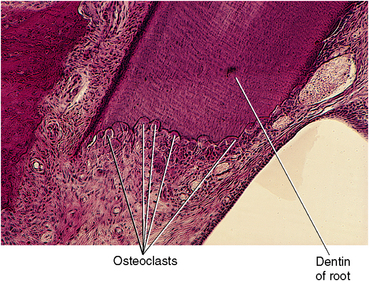
Fig. 6-13 Histology of active resorption sites on primary tooth roots. Osteoclasts appear in lacunae in root cementum and dentin.
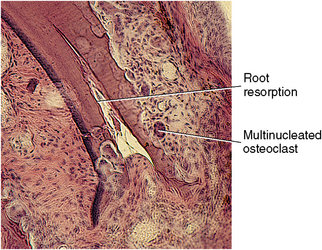
Fig. 6-14 Histology of osteoclasts in advancing resorption lacunae. Observe the large multinucleated cells shown within the lacunae.
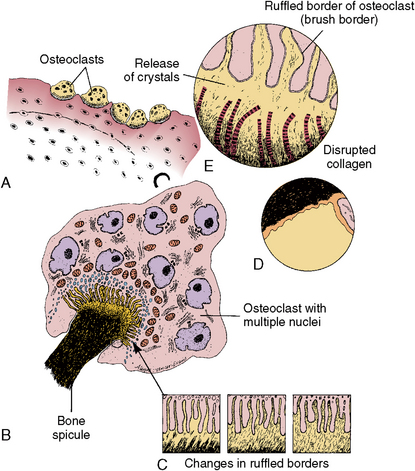
Fig. 6-15 Osteoclast activity. A, Osteoclasts in lacunae on bone surface. B, Large multinucleated osteoclasts with brush border in contact with bone spicule. C, High magnification of ruffled border of osteoclast showing mineral crystals passing into spaces between cell extensions. Unmasked collagen fibers are nearby. D, Clear zone on osteoclast surface. E, Ruffled border of osteoclast in constant motion or change.
Hard tissue resorption is believed to occur in two phases: the extracellular phase, in which the mineral is separated from the collagen and is broken into small fragments (see Fig. 6-15), and the intracellular phase, in which the osteoclast ingests these mineral fragments and continues the dissolution of this mineral. Crystals appear in cytoplasmic vacuoles of the osteoclast and are gradually digested within them. Resorption of mineral occurs at the ruffled border interface outside the cell, and the mineral is then taken within the cell (Fig. 6-16). Special fibroblast (fibroblast-fibroclast) cells are believed to destroy the remaining collagen fibers secondarily by ingesting them in an intracellular phagolysosome system (Fig. 6-17). Amino acids resulting from this breakdown are used in the formation of collagen within this same cell and can be used in this same area for bone formation. Only the posterior permanent molars, which have no primary predeciduous teeth, erupt through alveolar bone (Fig. 6-18). Figure 6-19 summarizes what happens in the tissues overlying the teeth during their prefunctional eruptive phase. Bone loss has occurred as the tooth approaches the oral epithelium (Fig. 6-19, A). The tooth organ epithelium makes contact with the oral mucosa (Fig. 6-19, B and C). This contact causes stretching and thinning of the oral membrane and finally its rupture and penetration by the tooth (Fig. 6-19, D and E). Only a thin developmental cuticle then covers the tooth (Fig. 6-19, E and F). As the tooth emerges farther into the mouth, more crown is exposed, and as clinical contact with the opposing tooth is made, the epithelial attachment shifts to the cervical area (Fig. 6-19, G). Clinically, tooth eruption is seen as a blanching of the mucosa, and this condition may persist for several days because the eruptive process is neither rapid nor continuous. Each eruptive movement, however, results in greater exposure of the crown. With successive eruptive movements, the area of attached epithelium becomes lower on the clinical crown.
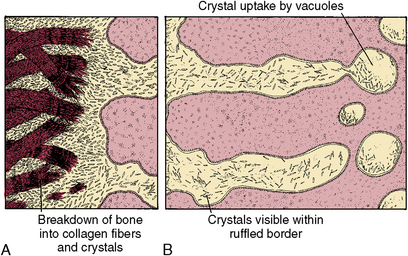
Fig. 6-16 Diagram of ruffled border of an osteoclast. A, High magnification of unmasked collagen fibers. Mineral crystals are near the osteoclast surface. B, Diagram of uptake of crystals into osteoclast vacuoles.
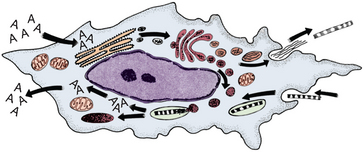
Fig. 6-17 Fibroblast (fibroblast-fibroclast) capable of synthesis of collagen as well as its breakdown. Collagen fibers are phagocytosed into cells and are broken down to release amino acids. These amino acids are then used to form new collagen molecules.
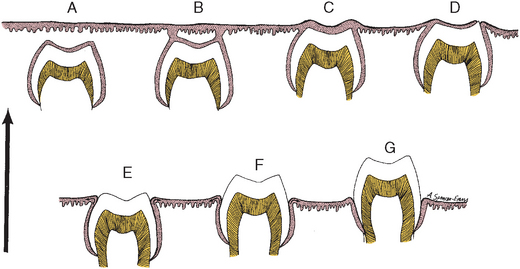
Fig. 6-19 Stages of tooth eruption. A, Tooth crown approaching oral epithelium in preeruptive stage. B, Contact of reduced enamel epithelium including the developmental cuticle fusing with oral epithelium. C, Fusion of reduced enamel epithelium including the developmental cuticle and oral epithelia. D, Thinning of fused epithelia. E, Rupture of oral epithelium, formation of the attached gingiva and emergence. F, Clinical crown appearance into the oral cavity (prefunctional stage). G, Tooth erupting into functional occlusion.
Surrounding the teeth
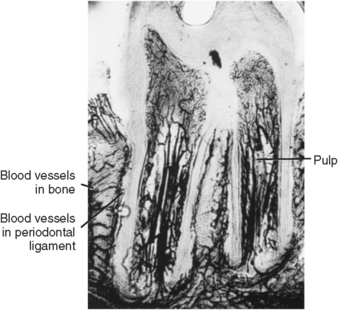
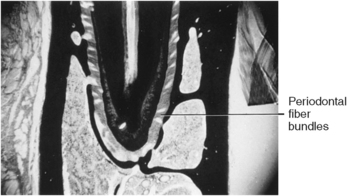
The tissues around the teeth change from delicately fine fibers lying parallel to the surface of the tooth to bundles of fibers attached to the tooth surface and extending toward the periodontium. The first fibers to appear are those in the cervical area as root formation begins (Fig. 6-20, A). As the root elongates, bundles of fibers appear on the root surface (Fig. 6-20, B and C). Fibroblasts are the active cells in both the formation and the degradation of the collagen fibers. With tooth eruption, the alveolar bone crypt increases in height to accommodate the forming root. After the teeth attain functional occlusion, the fibers gain their natural orientation (Fig. 6-20, C). Special fibroblasts have been found in the periodontium around the erupting teeth. These fibroblasts have contractile properties. During eruption, collagen fiber formation and fiber turnover are rapid, occurring within 24 hours. This mechanism enables fibers to attach and release and attach in rapid succession. Some fibers may detach and reattach later while the tooth moves occlusally as new bone forms around it. Gradually the fibers organize and increase in number and density as the tooth erupts into the oral cavity. Blood vessels then become more dominant in the developing ligament and exert additional pressure on the erupting tooth (Fig. 6-21).
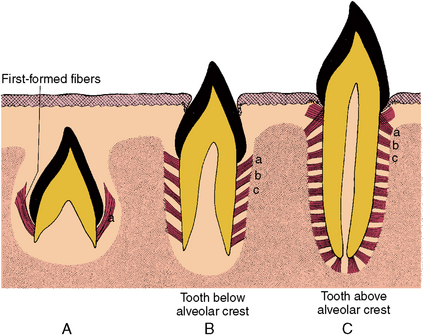
Fig. 6-20 Principal fiber development during tooth eruption. A, Origin of fibers at the cervical root area of crown. B, Fiber development with root growth. C, Change in orientation of the fibers with occlusal function. a, Initial fiber formation. b, Development of secondary fibers. c, Further fiber development. Initial fiber groups change direction with function.
Underlying the teeth
As the crown of a tooth begins to erupt, it gradually moves occlusally, providing space underlying the tooth for the root to lengthen (Fig. 6-22). In the fundic region these changes in the soft tissue and the bone surrounding the root apex are believed to be largely compensatory for the lengthening of the root. During root formation, the dentin of the root apex tapers to a fine edge that terminates in the epithelial diaphragm (Fig. 6-23). Fibroblasts form collagen around the root apex, and these fiber bundles become attached to the cementum as it begins to form on the apical dentin. Fibroblasts appear in great numbers in the fundic area, and some of these fibers form strands that mature into calcified trabeculae. These trabeculae form a network, or bony ladder, at the tooth apex. This is believed to fill the space left behind as the tooth begins eruptive movement (see Fig. 6-23). Gradually this delicate bone ladder becomes denser as additional bony plates appear (Fig. 6-24). The bony plates remain until the teeth are in functional occlusion at the end of this phase. Dense bone then forms around the tooth’s apex, and bundles of fibers attach to the apical cementum and extend to the adjacent alveolar bone to provide more support (Fig. 6-25).
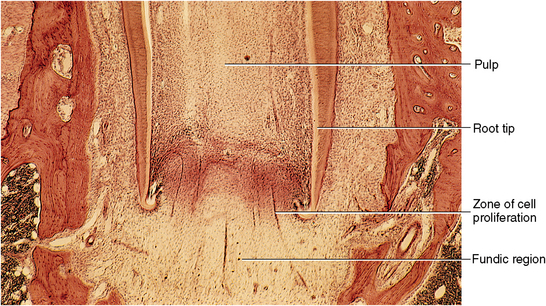
Fig. 6-22 Histology of erupting tooth with immature roots and open apex. As the tooth erupts, the roots will develop and fill in the wide pulpal tooth apex.
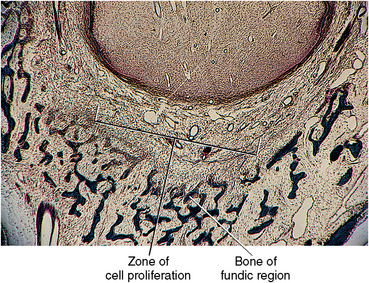
Fig. 6-23 Histology of changes in fundic region during tooth eruption. Fine trabeculae of new bone appear near tooth apices that will aid in stabilizing the tooth during eruption.
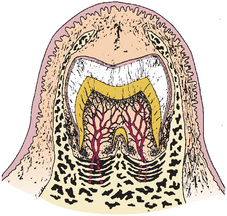
Fig. 6-24 Diagram of a later stage of tooth eruption. The fundic region further develops a bony ladder.
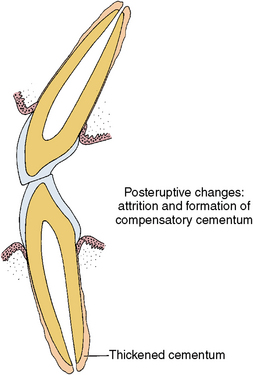
FUNCTIONAL ERUPTIVE PHASE
The final eruptive phase takes place after the teeth are functioning and continues as long as the teeth are present in the mouth. During this period of root completion, the height of the alveolar process undergoes a compensating increase. The fundic alveolar plates resorb to adjust for formation of the root tip apex. The root canal narrows as a result of root tip maturation, during which the apical fibers develop to help cushion the forces of occlusal impact. Root completion continues for a considerable length of time, even after the teeth begin to function. This process takes about 1 to 1.5 years for deciduous teeth and 2 to 3 years for permanent teeth.
The most marked changes occur as occlusion is established. At that time, the mineral density of the alveolar bone increases, and the principal fibers of the periodontal ligament increase in dimension and change orientation in their mature state. These fibers separate into groups oriented about the gingiva, the alveolar crest, and the alveolar surface around the root. Such fibers stabilize the tooth to a greater degree, and the blood vessels become more highly organized in the spaces between the bundles of fibers (see Fig. 6-25). Later in life, attrition and abrasion may wear down the occlusal or incisal surface of the teeth, causing the teeth to erupt slightly to compensate for this loss of tooth structure. Any such change results in deposition of cementum on the root’s apex (Fig. 6-26). Cementum is also deposited in the furcation area of a two- or three-rooted tooth.
POSSIBLE CAUSES OF TOOTH ERUPTION
Of the numerous causes of tooth eruption, the most frequently cited are root growth and pulpal pressure. Other important causes are cell proliferation, increased vascularity, and increased bone formation around the teeth. Additional possible causes that have been noted are endocrine influence, vascular changes, and enzymatic degradation. Probably all these factors have an influencing role, not necessarily independent of one another.
Although not all factors associated with tooth eruption are known, elongation of the root and modification of the alveolar bone and periodontal ligament are thought to be the most important ones. These events are coupled with changes overlying the tooth that produce the eruption pathway. Blood vessels in this area are compressed by the influence of the advancing crown and become nonfunctional. Connective tissue in the eruption pathway gradually disappears as the tooth epithelium and the oral epithelium fuse. In summary, the erupting tooth moves from an area of increased pressure to an area of decreased pressure.
SEQUENCE AND CHRONOLOGY OF TOOTH ERUPTION
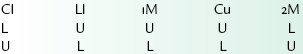
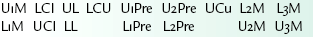
The formula for the eruptive sequence of the primary and permanent dentition appears in Box 6-1. Table 6-1 shows the chronologic development and eruption of the primary dentition, and Table 6-2 shows the development and eruption of the permanent dentition.
TABLE 6-1
CHRONOLOGY OF DEVELOPMENT OF THE PRIMARY DENTITION*
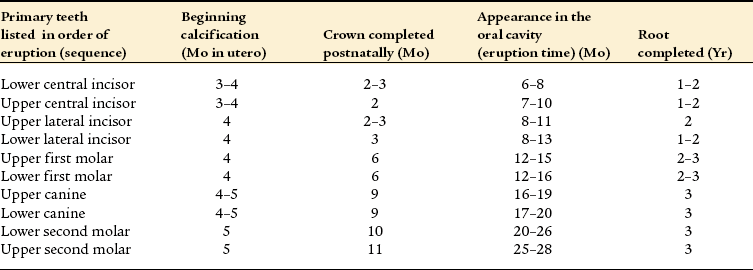
*The normal range of eruption times indicates a wide variation in eruption times. It is important to know that a difference of 1 or 2 months either side of the normal range does not necessarily indicate that a child’s eruption out of this range should be considered abnormal.
SHEDDING OF PRIMARY TEETH
Humans are considered diphyodont because they possess two dentitions, primary and permanent. Teeth in the primary dentition are smaller and fewer in number than the permanent dentition to conform to the smaller jaws of the young person. Teeth in the permanent dentition are larger, longer, and more numerous, which the larger jaws of the adult can accommodate.
The primary dentition functions from about 2 to 8 years of age. Teeth from both dentitions are present in the mixed dentition period, which extends from about 8 to 12 years of age. This is an interesting period because only part of the primary teeth roots are present while they undergo resorption, and only part of the permanent roots are present while they are in the formative stage. In this way, nearly 50 teeth can be accommodated in the jaws during this 4-year span (see Fig. 6-12).
The period of tooth shedding follows the mixed dentition period. Shedding is the loss of the primary dentition caused by the physiologic resorption of the roots, the loss of the bony supporting structure, and therefore the inability of these teeth to withstand the masticatory forces.
The degeneration of primary pulp tissue is similar to that of the tissues in the eruption pathway with a loss of cells, nerves, and blood vessels. When a primary tooth is extracted, blood is still likely to be in the crown, although only the oral epithelium holds the tooth in the socket. Figure 6-27 shows the correlation between root growth and eruption. It illustrates changes that occur in the preeruptive (A, B), prefunctional (C, D), and functional eruptive (E) stages of the tissues overlying and around the root surface as the tooth develops functionally.
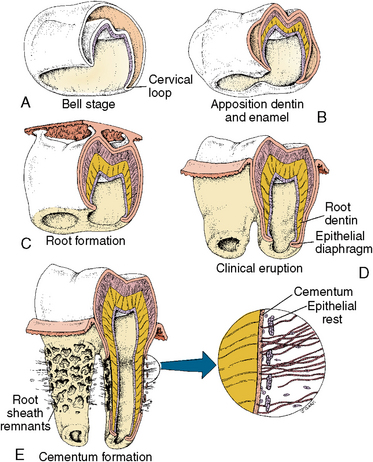
Fig. 6-27 Summary of tooth eruption. A, Early preeruptive changes in enamel organ at the bell stage. B, Late preeruptive changes as enamel and dentin form. C, Early prefunctional changes as the tooth moves to oral epithelium. D, Late prefunctional changes as the tooth emerges into the oral cavity. E, Functional eruptive phase with clinical contact. Root growth is shown with the root sheath detaching from the root surface. Epithelial rests and cementum formation by cementoblasts are now occurring.
COMPARISONS OF THE PRIMARY AND PERMANENT DENTITIONS
This section will compare the morphology and histology of the primary and permanent dentition and describe some clinical problems in the developing jaw of the growing child as compared with the jaw in the adult and related characteristics of the developing primary and permanent teeth and their supporting structures (Table 6-3).
Tooth Number and Size
The main difference between the primary and permanent dentition is the number of teeth, which is 20 in the primary, and 32 in the permanent. The permanent teeth replacing the primary teeth are called successional. There are 12 permanent teeth, which have no predecessor. They are called accessional. As the permanent molars are added, arch length and occlusal surface are increased (see Fig. 6-18). Primary and permanent teeth differ in size and form. Several of these differences influence decisions about clinical treatment. Crowns of primary teeth are smaller than the crowns of their successors, with only a few key exceptions. Crowns of permanent incisors and canines are larger than their primary counterparts in all dimensions. (see Fig. 6-3). The difference between the cumulative mesiodistal diameters of the primary molars and canines and those of the permanent molars and canines is called the leeway space, which totals 1.3 mm in the maxillary arch and 3.1 mm in the mandibular arch.
Primary teeth resemble permanent teeth. Both permanent and primary incisors have single roots and incisal edges. Both primary and permanent canines also have single roots and a single cusp. Primary molars, however, bear no resemblance to the premolars that will succeed them. The crowns of the permanent molars are larger than crowns of primary molars; the latter have a larger mesiodistal diameter than crowns of the succeeding premolars. This difference has clinical significance in caries patterns on approximal surfaces and in cavity design for caries removal. Interproximal lesions will be cervical to the contact areas and of similar shape.
Roots
The roots of primary teeth are shorter than roots of permanent teeth and are more divergent. The flat curved roots of primary teeth permit development of the crown of the permanent successor (see Fig. 6-18). As the permanent teeth erupt, the roots of the primary teeth are resorbed. Root shape dictates the shape of the root pulp and is correlated with two important clinical considerations. First, curved roots with thin walls make mechanical access of root canals more difficult in primary molars than in permanent molars. Secondly, the flat ribbon-shaped root canals of the primary teeth are in sharp contrast to the tubelike canals of the permanent teeth. Significant developmental differences occur in the root canals of the primary molars; the root canal fills in unevenly with secondary dentin, which leaves calcified bridges, making endodontic instrumentation difficult.
Tooth Structure
Primary and permanent teeth have a similar enamel prism structure, except at the tooth surface. Primary teeth are more likely to have a prismless surface, and this reflects on the clinician’s ability to etch the surface and provide an interface for attachment of sealants and other restorative procedures. Enamel is about twice as thick in permanent teeth as in primary teeth and is more highly pigmented. Primary tooth dentin is slightly softer than the permanent teeth.
Pulp Shape and Size
The coronal pulps of primary teeth are relatively larger than in permanent teeth. The largest pulp horn in primary molars is the mesiobuccal and the second largest is the mesiolingual. These differences are used in the design of dental restoration. Primary and permanent are similar in basic histological architecture and the vasculature, connective tissue and odontoblastic and subodontoblastic zones are similar in appearance. Permanent teeth have a larger number of nerves than primary teeth. The usual location of accessory canals in primary teeth is in the furcation zone and in permanent teeth at the apical one third of the completed root.
Arch Shape
Arch shape is similar in the anterior portion of the two dentitions but the permanent dentition extends further distally. Tooth-size differences are critical in assessment of potential space for permanent teeth to erupt into alignment.
The succession of smaller primary incisors with larger permanent incisors is called incisor liability, and the difference in the mesial distal dimension between the primary molars and permanent premolars is called the leeway space.
Root Resorption and Pulp Degeneration
The primary tooth roots have a higher susceptibility to resorption than permanent teeth. The process of resorption is accompanied by gradual changes in the pulp. The first sign is a reduction in the number of cells in the pulp: nerve trunks degenerate and some fibrosis occurs. Blood vessels remain until the tooth is exfoliated.
During root formation, the primary tooth pulp is highly cellular. As the roots are completed, fewer cells and more fibers are evident. The proliferation of fibers continues during the root resorption phase with fiber bundles becoming more prominent.
Nerve fibers gradually organize in the pulp chamber of the primary tooth. As the tooth reaches functional occlusion, the nerve fibers form a parietal plexus. These nerve fibers are lost during resorption of the primary tooth roots, which makes teeth insensitive to pulpal pain at the time of exfoliation.
The periodontal support of primary and permanent teeth is similar in basic architecture.
Acknowledgments
Dr. N.M. Elnesr contributed to the production of chapters in Avery JK: Oral development and histology, ed 3, Stuttgart, 2002, Thieme Medical. Some of the figures in that text have been used in preparation of this chapter.
SELF-EVALUATION QUESTIONS
1. Define tooth eruption and each of its phases.
2. Describe the changes overlying the tooth during eruption.
3. Describe the changes occurring around the tooth during eruption.
4. Describe the significant changes in the area underlying the teeth that relate to eruption.
5. What are the three fundamental causes of tooth shedding?
6. Give the sequence of eruption of the primary and permanent teeth.
7. What is the origin of osteoclasts?
8. Give the sequence of events that occur in hard tissue resorption.
9. Give the chronology of eruption for the primary teeth.
10. Give the chronology of eruption for the permanent teeth.

 CLINICAL COMMENT
CLINICAL COMMENT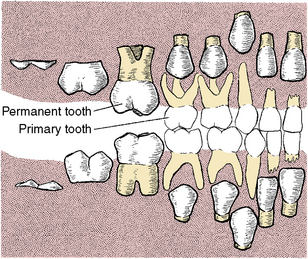
 Consider the Patient
Consider the Patient