Managing physiological change in the surgical patient
Systemic responses
Factors responsible for systemic responses (Box 2.1)
Surgical patients are subject to a variety of major injuries and catastrophes that make massive demands on the body's ability to sustain life and maintain physiological equilibrium. Examples of such stressors include:
• Major operations—anaesthesia (particularly head-down + pneumoperitoneum for laparoscopic surgery), tissue trauma, blood and fluid loss, healing and repair
• Major trauma including fractures and burns; head, abdominal and chest injuries
• Major cardiovascular events, e.g. myocardial infarction, pulmonary embolism, stroke
• Haemorrhage and fluid infusion including blood; fluid and electrolyte abnormalities
The way the body responds to major systemic insults depends on several factors—the physiological reserve of the patient's chief organ systems (i.e. basic fitness), the nature of the injurious process, the severity of physiological disruption, the duration of delay before resuscitation, and the virulence of any microorganisms involved. Most patients are remarkably resilient given good basic care but in a deteriorating patient, several physiological systems are likely to be impacted upon simultaneously, evoking a range of complex homeostatic mechanisms.
Management of the deteriorating patient
The aim is always to recognise problems early by regular clinical observation, and to correct abnormal physiology rapidly and accurately in order to prevent intrinsic compensatory mechanisms becoming overwhelmed. If this happens in one organ system without correction, snowballing decompensation of other systems follows.
Management requires careful monitoring, often in a high-dependency or intensive care unit, and repeated checks on organ function and dysfunction. In most elective operations, many of the responses discussed below can be mitigated by good preoperative preparation, accurate fluid replacement, ensuring oxygenation, adequate analgesia, reducing psychological stress, preventing infection and using careful operative technique to minimise tissue trauma, blood loss and complications. Enhanced recovery programmes are gradually being introduced which give special attention to these factors before, during and after operation (see: NHS Enhanced Recovery Partnership Programme document: Delivering enhanced recovery—Helping patients to get better sooner). The individual variables responsible for potentially excessive systemic responses to severe injury or major surgery are summarised in Box 2.1.
Stressors in the surgical patient
Direct and indirect tissue trauma: Tissue disruption (whether surgical or traumatic) leads to activation of local cytokine responses more or less in proportion to the damage. Responses are exaggerated if wounds are contaminated (e.g. debris, foreign bodies, faeces) or associated with tissue ischaemia.
Fall in intravascular volume: This is a key factor in initiating systemic responses. Hypovolaemia results from:
• Excess fluid loss (see Box 2.2)
• Interstitial sequestration of fluid as oedema in damaged tissues and generally as a result of systemic hormonal responses. This process is amplified in systemic sepsis
• Restricted oral intake during any perioperative period or whilst in intensive care
Falling intravascular volume stimulates sympathetic activity by removing baroreceptor inhibition in an attempt to maintain blood pressure by increasing cardiac output and peripheral resistance. This also explains the mild tachycardia commonly seen in postoperative patients. Compensation is most effective in young fit individuals, but decompensation is often sudden and rapid. Catecholamines also have profound metabolic effects, increasing the turnover of carbohydrates, proteins and lipids. Falling renal perfusion activates the renin–angiotensin–aldosterone system, increasing renal reabsorption of sodium and water. A centrally mediated increase in antidiuretic hormone (ADH) secretion promotes further conservation of water.
Reduced cardiac output and peripheral perfusion: Circulatory efficiency may be impaired by hypovolaemia, and myocardial contractility may be depressed by anaesthetic agents and other drugs. Anaesthetic drugs generally cause peripheral dilatation and positive-pressure ventilation impairs venous return. Head-down positioning and artificial pneumoperitoneum for laparoscopic surgery further stress cardiovascular physiology. Major events such as sepsis (septic shock), pulmonary embolism or myocardial infarction may precipitate cardiovascular collapse.
Systemic inflammatory responses and sepsis (see Ch. 3):
Stress: Psychological stress associated with injury, severe illness or elective surgery has an effect similar to pain on sympathetic function and hypothalamic activity.
Excess heat loss: This can occur during long operations and after extensive burns. Heat loss imposes enormous demands upon energy resources; if body core temperature falls, physiological processes such as blood clotting are impaired. Small babies are very vulnerable to heat loss. Heat loss in the operating theatre is counteracted as far as possible by raising the ambient temperature, insulating exposed parts of the body, using warm water underblankets or warm air ‘bear-huggers’ and by warming fluids during intravenous infusion.
Blood coagulation changes: General metabolic responses to injury activate thrombotic mechanisms and initially depress intrinsic intravascular thrombolysis. Thus the patient is in a prothrombotic state and may suffer intravenous thrombosis and consequent thromboembolism.
If substantial haemorrhage occurs, clotting factors eventually become exhausted, causing failure of clotting. The systemic inflammatory response syndrome (SIRS, see Ch. 3, p. 51) may initiate widespread intravascular thrombosis, using up clotting factors and precipitating disseminated intravascular coagulation (DIC), with failure of normal clotting.
Starvation and stress-induced catabolism: Patients with major surgical conditions are often malnourished before operation (see Nutritional management, below). Most are starved for 6–12 hours preoperatively and often do not start eating for 12–24 hours after surgery. After major GI surgery, food may be withheld for several days, or much longer with complications such as anastomotic breakdown or fistula formation.
Metabolic responses to pathophysiological stress
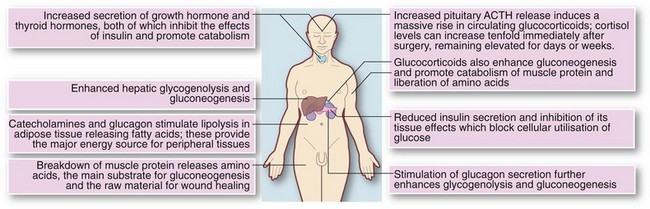
In severe trauma or extensive operative surgery, particularly if complicated by sepsis, the key factors in the systemic response are increased sympathetic activity together with increased circulating catecholamines and insulin. Cytokine responses signal other cells to prepare for action (e.g. polymorphs, T and B cells), to compensate for starvation, provide additional energy and building blocks for tissue repair, and conserve sodium ions and water.
Glucose production is massively increased by gluconeogenesis under the influence of catecholamines. There is also enhanced secretion of ACTH, glucocorticoids (cortisol), glucagon and growth hormone, all contributing to the general catabolic response. Insulin acts as an antagonist of most of these and is secreted in increased amounts from the second or third day after injury.
The sum of these factors is to cause inevitable catabolism and potentially extreme changes in fluid balance and electrolytes. These metabolic changes are shown in Figure 2.1.
Effects on carbohydrate metabolism: The overall effect is rising blood glucose (levels may reach 20 mmol/L), often resulting in hyperglycaemia and a pseudodiabetic state, and glucose may appear in the urine. This is in marked contrast to simple fasting, in which glucose levels are normal or low and glycosuria does not occur.
Effects on body proteins and nitrogen metabolism: In the normal healthy adult, nitrogen balance is constantly maintained. Protein turnover results in daily excretion of 12–20 g of urinary nitrogen which is made good by dietary intake. In a hypercatabolic state, nitrogen losses can increase three- or four-fold. Most importantly, the metabolic environment prevents proper utilisation of food or intravenous nutrition. There is therefore huge destruction of skeletal muscle. This state of negative nitrogen balance contrasts markedly with simple starvation in which body protein is preserved.
Effects on lipid stores and metabolism: The effects of major body insults on lipid metabolism are little different from simple starvation; most of the energy requirements are met from fat stores.
Surgical catabolism reverses only as the patient recovers from the illness and therefore early parenteral nutrition has little effect, although carbohydrate administration may spare some protein loss.
Note that when patients have been severely ill, carbohydrate metabolism is minimal and energy comes from catabolism of protein and fat. Once feeding recommences, there is a danger of refeeding syndrome which must be anticipated (see below).
Fluid, electrolyte and acid–base management
Introduction
Fluid, electrolyte and acid–base derangements can be minimised if high-risk patients are assessed before operation and closely monitored before, during and after operation. If abnormalities do develop, the diagnosis and management can be worked out with reasoning and common sense. Plasma urea and electrolytes should be checked at least daily in patients undergoing major surgery or those receiving intravenous fluids.
Severely ill patients with abdominal infection, sepsis and fistulae and patients with severe burns are likely to suffer major problems of fluid balance (and nutrition, see below). These are best managed with the help of experienced anaesthetists in intensive care or high-dependency units, where monitoring and therapy can be rigorously managed.
Normal fluid and electrolyte homeostasis
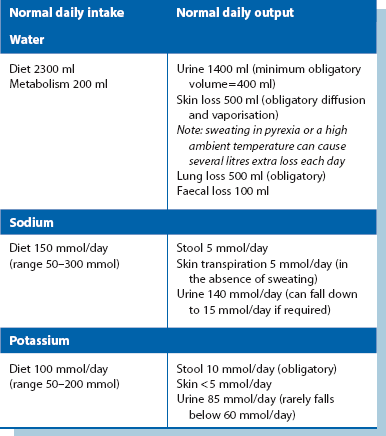
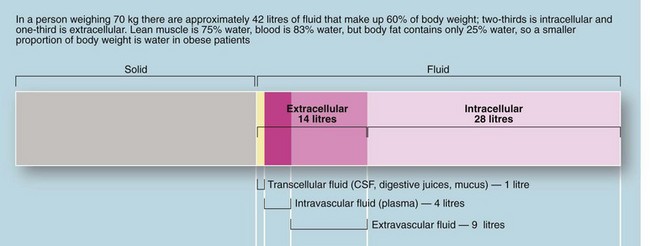
The body of an average 70 kg adult contains 42 litres of fluid, distributed between the intracellular compartment, the extracellular space and the bloodstream (see Fig. 2.2). Fluid input is mainly by oral intake of fluids and food but about 200 ml/day of water is produced during metabolism. Normal adult losses are between 2.5 and 3 litres/day. About one litre is lost insensibly from skin and lungs, 1300–1800 ml are passed as urine (about 60 ml/hour or 1 ml/kg/hour) and 100 ml are lost in faeces. About 100–150 mmol of sodium ions and 50–100 mmol of potassium ions are lost each day in urine and this is balanced by the normal dietary intake (see Table 2.1).
Maintenance of water and sodium
For most patients, the daily water and sodium requirements are best met by using appropriate quantities of normal saline solution (0.9% sodium chloride) and 5% dextrose (glucose) solution. Normal saline contains 154 mmol each of sodium and chloride ions per litre. One litre will thus satisfy the daily sodium requirement of uncomplicated patients. The additional requirement for water is made up with 2–2.5 litres of 5% glucose (see Box 2.3). The small amount of glucose this contains contributes little to nutrition but renders the solution isotonic. This prescription is altered for patients with electrolyte abnormalities by varying the volume of normal saline given.
Note that Hartmann's solution (or similar balanced electrolyte solutions such as Ringer's lactate) is often used as the sole fluid for intravenous infusion. This is more physiological and contains less chloride (111 mmol/L), some potassium (5 mmol/L) and insignificant amounts of calcium and lactate.
In children, water excretion is markedly reduced in the postoperative period as a result of increased ADH secretion. Maintenance fluids requirements are based on published guidelines and formulae (see: http://www.nda.ox.ac.uk/wfsa/html/u19/u1914_01.htm).
Maintenance of potassium
Basic potassium requirements are met by infusing 60–80 mmol of potassium chloride in divided doses over each 24-hour period. Premixed intravenous fluids are generally available with 20 or 40 mmol of potassium chloride per 1000 ml infusion bags. If concentrations of potassium chloride greater than 40 mmol in 500 ml are required, they should be given via a central venous infusion in a critical care unit, with cardiac monitoring. Bolus injections of KCl must never be given because rapid increases in plasma potassium can cause cardiac arrest.
Limits of compensatory mechanisms
Healthy kidneys are normally able to maintain fluid and electrolyte homeostasis in spite of large variations of fluid intake. The same also applies to fluid and electrolytes given intravenously.
The total blood volume in an adult male is about 5 litres, of which about 55–60% is water (about 3.5 litres). Falls in blood volume which are not too rapid or extensive can be compensated by fluid movement from the extracellular compartment which has a volume of more than 10 litres. A deficit of more than 3 litres in whole body fluid volume cannot be sustained and intravascular volume inevitably becomes depleted. This is reflected in compensatory cardiovascular changes. Vasoconstriction causes cold peripheries: this is an important warning sign of hypovolaemia and more reliable than the early mild tachycardia, particularly in children. When overall fluid deficit reaches about 3 litres, the pulse rate becomes very rapid and hypotension and shock develop. Note that patients on beta-adrenergic blocking drugs or with cardiac conduction defects may not be able to increase heart rate and will therefore decompensate earlier. With 4 or more litres of fluid deficit, the limit of cardiovascular compensation is reached and the patient develops hypovolaemic shock. Note that fit young people are able to sustain normal vital signs longer but when they do decompensate, they do so abruptly.
In neonates, children, the elderly and the chronically ill, cardiovascular compensation capacity is greatly reduced. A relatively small fluid and electrolyte imbalance may cause life-threatening complications.
Physiological changes in response to surgery and trauma
The stresses of trauma or surgery cause a rise in circulating catecholamines. Stress also stimulates the hypothalamo–pituitary–adrenal axis, which increases secretion of cortisol and aldosterone. These hormones promote renal conservation of sodium and water and cause a reduction in urine volume and urine sodium concentration.
Effects of a fall in renal perfusion: Any substantial reduction in effective circulating volume may cause a fall in renal perfusion. In addition, aortic surgery involving aortic clamping may alter the dynamics of renal artery flow, whilst raised intra-abdominal pressure (see Abdominal compartment syndrome, below) disrupts renal blood flow.
A fall in renal perfusion activates the renin–angiotensin–aldosterone mechanism to sustain the blood pressure. As glomerular filtration falls, renin release is stimulated from the renal juxtaglomerular apparatus and this catalyses the conversion of angiotensin I to angiotensin II in the lungs. Angiotensin II has a powerful pressor effect on the peripheral vasculature, counteracting hypotension, as well as stimulating aldosterone release from the adrenal cortex. Aldosterone promotes active reabsorption of sodium ions from the distal convoluted tubules of the kidney, accompanied by passive reabsorption of water. Sodium reabsorption is linked to increased excretion of potassium and hydrogen ions.
The net effect is that in conditions causing renal perfusion to fall, the urine output falls by several hundred millilitres per day, and the urine that is produced is low in sodium (less than 40 mmol/L), high in potassium (greater than 100 mmol/L) and acidic. The loss of hydrogen ions causes a degree of metabolic alkalosis.
Other factors in water conservation: Water conservation is further enhanced by stress-mediated secretion of antidiuretic hormone (ADH), also known as vasopressin, from the posterior pituitary (neurohypophysis). Loss of water alone increases the plasma osmolality, stimulating ADH release, mediated by osmoreceptors in the hypothalamus. ADH binds to receptors in the distal renal tubules and promotes reabsorption of water. Release of ADH is also stimulated by falls in blood pressure and volume, sensed by stretch receptors in the heart and large arteries. Changes in blood pressure and volume are not nearly as sensitive a stimulator as increased osmolality, but are potent in extreme conditions (e.g. loss of over 15% volume in acute haemorrhage). Stress and pain probably also promote ADH release via other hypothalamic pathways.
Postoperative situation: At the site of trauma or major surgery, fluid is effectively removed from the circulation in the form of inflammatory oedema (isotonic local third space losses). This displaced volume is compensated by fluid retained by the hormonal changes described above. More potassium is released from damaged cells than the excess lost by exchange in the kidney. Thus, the postoperative plasma potassium level tends to rise in the first day or two. This is particularly true if stored blood has been transfused as this releases potassium from elderly red cells, so potassium supplements are not usually needed for the first few days after operation provided preoperative plasma potassium is normal and potassium-losing diuretics are not prescribed.
It is important to recognise the normal phase of relative oliguria and sodium retention that inevitably occurs for up to 48 hours after major injury or surgery as this influences fluid management. Like surgical catabolism, these effects are resistant to external manipulation but resolve with recovery of the patient.
Abdominal compartment syndrome: (see http://www.ncbi.nlm.nih.gov/pmc/articles/PMC137242/)
Abdominal compartment syndrome, with the adverse effects it can have on organ systems, is now recognised as an entity. Intra-abdominal pressure is normally less than 5 mmHg, but after surgery or trauma it may rise as high as 15 mmHg. Cardiac output begins to fall off at 10 mmHg, and hypotension and oliguria are likely between 15 and 20 mmHg. Anuria occurs with pressures over 40 mmHg.
The causes of abdominal compartment syndrome are often multifactorial and include fluid accumulating as a result of retroperitoneal haemorrhage, e.g. in ruptured abdominal aortic aneurysm, postoperative haemorrhage (particularly if clotting is disordered), organ trauma, pancreatitis, and interstitial oedema in sepsis or zealous fluid resuscitation. When abdominal pressure exceeds the capillary pressure perfusing abdominal organs, dysfunction and eventually infarction of these organs becomes likely.
• Oliguria due to renal hypoperfusion and collapsed renal veins
• Respiratory embarrassment due to restriction and elevation of the diaphragm, and compression of alveoli. This results in increased peak airways pressure, decreased tidal volume, hypoxaemia and hypercarbia
• Decreased venous return leading to falling cardiac output and hypotension
In patients with a distended and taut abdomen, measuring abdominal compartment pressure can help early recognition. Treatment involves reopening the abdomen and leaving it open until the risk of rising pressure subsides.
Problems of fluid and electrolyte depletion
Loss of whole blood or plasma: Rapid and copious blood loss in traumatic injury or operative surgery initially depletes the intravascular compartment and loss of only 1 litre may cause hypotension or even hypovolaemic shock. When haemorrhage is less rapid, there is time to replace fluid loss from the extracellular compartment, so greater volumes can be lost before the cardiovascular system becomes compromised, although losses still need to be restored physiologically or by transfusion.
If blood loss has ceased, the need for transfusion is based on estimated or measured volume lost and on known haemoglobin concentration. Acute blood loss of 500–1000 ml is usually treated by transfusing crystalloids. Larger volume losses are best replaced by transfusion of whole blood or packed red cells supplemented by normal saline. Slow chronic blood loss, e.g. from a peptic ulcer or hookworm infestation, does not cause fluid balance problems but may cause symptoms and signs of anaemia; transfusion is not usually required.
In severe burns, the amount of plasma likely to be lost is easily underestimated and should be calculated using a standard formula based on the burnt area to guide fluid replacement (see Ch. 17).
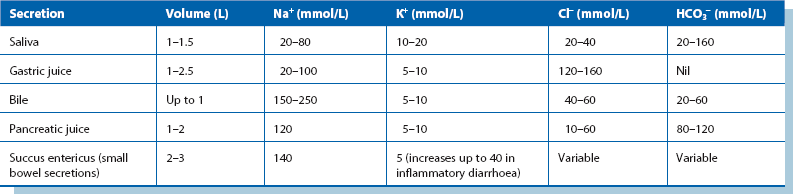
Gastrointestinal fluid loss: Between 5 and 9 litres of electrolyte-rich fluid is normally secreted into the upper GI tract each day as saliva, gastric juice, bile, pancreatic fluid and succus entericus (small bowel secretions; see Table 2.2). Most of the fluid is reabsorbed in the large intestine.
Huge volumes of water and electrolytes may be lost as a result of vomiting, nasogastric aspiration, diarrhoea, sequestration of fluid in obstructed or adynamic bowel or drainage to the exterior via a fistula or an ileostomy. If there is widespread bowel inflammation causing diarrhoea as in gastroenteritis or ulcerative colitis, inflammatory exudate may greatly increase the total fluid lost.
Cholera and other infective diarrhoeal diseases can cause the loss of up to 10 litres of electrolyte-rich fluid in one day and this fluid loss is a frequent cause of death, particularly in children.
Abnormal fluid losses in hospital must be measured or estimated accurately and recorded on a fluid balance chart. In addition, observations should be regularly made for signs of fluid depletion including pulse rate, blood pressure, periodic urine output and, if necessary, central venous pressure (CVP). These measures enable intravenous replacement to be predicted and the adverse consequences of fluid and electrolyte depletion to be prevented.
From Table 2.2, it can be seen that vomitus, nasogastric aspirate and diarrhoea are variably rich in sodium and potassium. As a general rule, GI fluid losses should be replaced by an equivalent volume of normal saline, with potassium chloride added as needed. In intestinal obstruction or adynamic ileus, fluid sequestrated in bowel is replaced in a similar manner, although volume requirements have to be estimated. Fistulae and overactive ileostomies cause chronic loss of fluid that is high in chloride and bicarbonate.
Intra-abdominal accumulation of inflammatory fluid: Severe intra-abdominal inflammation may cause several litres of fluid rich in plasma proteins and electrolytes to be lost into the peritoneal cavity. This typically occurs in peritonitis or acute pancreatitis and often in the context of the systemic inflammatory response syndrome (SIRS). This is best replaced (as well as can be estimated) by physiological saline or other suitable crystalloids.
Systemic sepsis (SIRS and multiple organ dysfunction syndrome): Systemic sepsis is associated with widespread endothelial damage and a large increase in capillary permeability mediated by a range of cytokines and other circulating mediators. The result is extensive loss of protein and electrolyte-rich fluid from the circulation into the extravascular space (‘third space loss’), which, combined with loss of peripheral resistance, results in cardiovascular collapse and shock.
The required fluid volume is difficult to estimate and replacement is usually given so as to maintain cardiovascular stability (pulse rate and blood pressure) and urinary output (at least 0.5 ml/kg body weight/hour) whilst avoiding fluid overload and cardiac failure. In the severely ill patient, in whom the volume requirements are particularly difficult to judge, a central venous pressure line or transoesophageal Doppler provide a more accurate method of assessing precise fluid replacement needs (see Enhanced recovery programmes, below).
Abnormal insensible fluid loss: Abnormal insensible fluid loss can greatly increase overall fluid loss, particularly in the seriously ill or elderly patient and must be included in the fluid balance equation. Pyrexia increases insensible loss by approximately 20% for each degree Celsius rise in body temperature, mainly in the form of exhaled water vapour. A pyrexia of 38.5°C for 3 days would therefore cause an extra litre of fluid loss. Sweating causes loss of sodium-rich fluid which can be easily overlooked in patients with fever and when the ambient temperature rises.
Preventing acute renal failure: Maintaining fluid balance in surgical patients depends on anticipating problems before they cause adverse effects and risk acute renal failure. Acute renal failure is a serious complication with a high mortality in surgical patients. Prevention involves similar strategies in all patients at risk, namely:
• Observing changes in vital signs—pulse rate, blood pressure and CVP if appropriate
• Checking hourly urine output is adequate
• Measuring fluid losses to guide replacement
• Seeking clinical signs of fluid imbalance (both dehydration and overload)
In patients with cardiac failure or shock, monitoring and treatment is best carried out in an intensive care or high-dependency/critical care unit, using invasive monitoring to help determine the required volume of fluid replacement.
Common fluid and electrolyte problems
Intermediate elective operations and uncomplicated emergency operations
Most operations fall into this category. Patients are generally in fluid and electrolyte equilibrium before operation, although diuretic therapy (for cardiac failure, hypertension or chronic renal failure) may cause problems. For these, plasma urea and electrolytes should be checked before operation. Note that loop and thiazide diuretics may cause hypokalaemia whilst potassium-sparing diuretics such as spironolactone may cause hyperkalaemia. If serious abnormalities are found, operation must be postponed until the problem is corrected. Hypokalaemia can usually be treated by oral potassium supplements or by adding a potassium-sparing diuretic. Hyperkalaemia is usually corrected by substituting a loop or thiazide diuretic.
Mild renal dysfunction (plasma urea up to about 15 mmol/L and creatinine up to about 170 mmol/L) is not usually a contraindication to surgery. These patients tend to be mildly dehydrated, however, and oral fluid intake should be strongly encouraged.
Introduction to management
For elective surgery, the patient is often kept ‘nil by mouth’ for 6–12 hours before operation, although most can take clear fluids by mouth up to 3 hours before operation. The patient is likely to take very little oral fluid for up to 6 hours after operation and a fluid deficit of 1000–1500 ml is therefore common. Mild fluid deficits can usually be quickly made up once the patient is drinking normally and intravenous fluid replacement is rarely required. For patients with mild renal failure, an infusion should be set up at the outset of the ‘nil by mouth’ period to prevent acute-on-chronic renal failure. Occasionally, and despite the use of anti-emetics, patients vomit after operation and intravenous fluids should be employed if vomiting is prolonged.
Children and especially infants and neonates are much more vulnerable to fluid deprivation because of their small total body fluid volume and disproportionate insensible losses. Even relatively minor operations can cause dehydration and intravenous fluids may be necessary, with the rate and volume calculated according to body weight and measured blood loss.
As a rule, the sooner the body can assume control over its own fluid and electrolyte homeostasis the better. Intravenous fluids should be discontinued as soon as normal oral intake has been resumed and urine output is satisfactory.
Major operations
Major elective or emergency operations, especially those involving bowel, pose particular problems with fluid management. The principal reasons are:
• Patients are often elderly and are likely to have a diminished cardiovascular reserve. They may have pre-existing fluid and electrolyte abnormalities
• Preoperative vomiting and restricted fluid intake may have caused dehydration and electrolyte abnormalities
• Blood loss during and after operation may be substantial
• Operations may take several hours with consequent insensible losses from the open wound
• Third space losses of 500–1000 ml can occur after major surgery or trauma as a result of systemic responses to trauma
• The recovery period when oral intake is nil or restricted may become extended—several days following complicated bowel surgery or peritonitis (e.g. perforated diverticulitis or an anastomotic leak)
Careful pre- and postoperative assessment of patients is crucial so problems can be anticipated. This should include clinical examination for dehydration (dry mouth and loss of normal skin turgor) or overhydration (elevated jugular venous pressure or cardiac failure). Plasma urea and electrolytes, creatinine and full blood count should be measured daily. Elevated urea concentration with little elevation of creatinine is characteristic of dehydration. An abnormally high haemoglobin concentration (providing polycythaemia is not present) also indicates dehydration, especially if it was normal beforehand.
In recent years, clinicians in surgery have been attempting to shorten hospital stays and reduce complication rates by developing structured systems that reduce the stress response to enhance recovery. These involve attention to all facets of surgical care, so-called ‘multimodal optimisation’ or ‘fast track recovery’. This includes special attention to perioperative fluid management, the use of minimal access surgical techniques and mechanisms to preserve postoperative organ function, including:
• Preoperative assessment and improved education and preparation of patients so that they understand what will happen and cope with planned early discharge
• Home care arrangements to cope with early discharge
• Improved methods of calculating fluid replacement that ensure the patient remains normovolaemic within narrow limits, preventing central hypovolaemia and fluid overload. NICE have recommended the use of transoesophageal Doppler ultrasound monitoring of left ventricular stroke volume to enable intraoperative assessment of fluid status and provide individualised goal-directed fluid therapy. Trials have shown this can reliably shorten hospital stays and reduce complication rates
• Planned and assisted early postoperative mobilisation
• Early enteral nutrient challenge and the use of gut-specific nutrients such as glutamine, antioxidants and synbiotics (nutritional supplements that improve the balance of intestinal microflora). Methods that enable earlier return of gut function may be fundamental to rapid recovery. Gastrointestinal gut-associated lymphoid tissue (GALT) forms more than half the body's immunological cell mass and is believed to play a key role in stress responses to surgery. Sustaining nutrition of the small bowel wall from within the lumen may prevent breakdown of intestinal barrier function. Healthy bowel function enables earlier tolerance of food, less postoperative ileus and less postoperative nausea and vomiting
Abnormalities of individual electrolytes
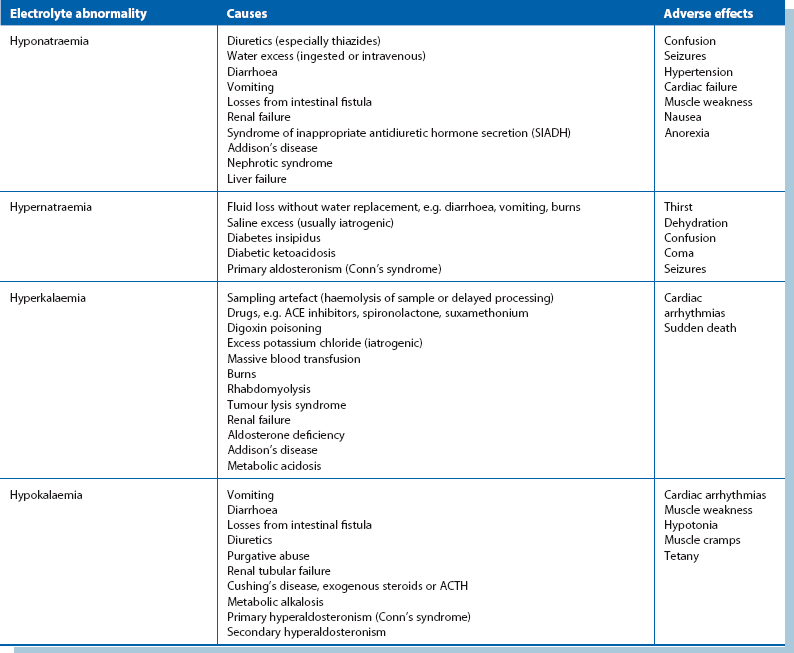
(see Table 2.3 for a summary of causes and effects)
Abnormalities of plasma sodium concentration: Plasma sodium abnormalities are usually discovered incidentally on regular measurement of electrolytes.
Hyponatraemia: A low plasma sodium level may be real or spurious. Spurious results commonly arise when blood is taken from an arm receiving an intravenous infusion; less commonly, false laboratory results can occur if there is lipaemia resulting from parenteral nutrition. If in doubt, the test should be repeated with appropriate precautions.
In hyponatraemia (except in severe hyperglycaemia or infusion of mannitol), the plasma becomes hypotonic. This causes cellular overhydration which in severe cases results in cerebral oedema. Mild hyponatraemia is symptomless but when the plasma sodium falls below about 120 mmol/L, patients often become confused. Convulsions and coma occur when concentrations fall below about 110 mmol/L. If hyponatraemia is confirmed biochemically, the next step is to clinically assess the state of hydration (i.e. the extracellular fluid volume) and this will guide therapy.
There are three possibilities:
• Water deficit with a larger sodium deficit (clinical signs—dry mouth, poor skin turgor, poor urine output, high urine osmolality): sodium insufficiency is usually due to diuretic therapy, vomiting, diarrhoea or other excessive losses of body fluids with inadequate replacement. Treatment involves rehydration with appropriate sodium-containing intravenous fluids
• Sodium normal with a larger water excess (clinical signs—weight gain, ankle swelling, raised jugular venous pressure): this usually results from organ dysfunction. Cardiac failure is the most common cause, followed by renal, liver and respiratory failure. Overhydration is compounded by excessive intravenous fluid administration. Management is based primarily on treating the organ failure, e.g. diuretics for cardiac failure
• Water excess: this is uncommon and is usually due to inappropriate antidiuretic hormone (ADH) secretion. This is rare on a surgical ward except for TUR syndrome in which excess fluid is absorbed during transurethral resection of the prostate. It can also occur following head injury or neurosurgery, or may occur in pneumonia, empyema, lung abscess or oat-cell carcinoma of the lung. Excess ADH increases water reabsorption by the renal tubules independently of sodium. The result is water overload and dilutional hyponatraemia. Inappropriate ADH secretion is the most likely diagnosis if the urine osmolality is found to be high and the plasma osmolality low. Hyponatraemia caused by inappropriate ADH secretion is managed by restricting fluid intake to 1 litre per day
Hypernatraemia: This is uncommon and is often iatrogenic in the surgical patient. The usual cause is either excess administration of sodium via intravenous fluids or inadequate water replacement. Hypernatraemia is more likely to occur after operation because increased aldosterone secretion causes sodium to be conserved by the kidney. Very rarely, hypernatraemia is caused by Conn's syndrome (primary hyperaldosteronism).
Treatment involves encouraging the patient to drink more water, or infusing fluids with a low sodium content.
Abnormalities of plasma potassium concentration: Acid–base abnormalities (see below) can have a profound effect on plasma potassium concentration but are likely to correct spontaneously as the acid–base problem is treated.
Hypokalaemia: In the preoperative patient, hypokalaemia usually results from poor dietary intake, diuretic therapy, chronic diarrhoea, losses from a malfunctioning ileostomy or, rarely, excess mucus secretion from a rectal villous adenoma. Rarely, hypokalaemia may be caused by primary hyperaldosteronism (Conn's syndrome).
Postoperatively, hypokalaemia is usually caused by inadequate potassium supplementation in intravenous infusions. The lack of intake is compounded by increased urinary losses from stress-induced secondary hyperaldosteronism.
Hypokalaemia causes skeletal muscle weakness and reduces GI motility, with paralytic ileus in extreme cases. When severe, there is also a risk of sudden cardiac arrhythmias or even cardiac arrest. Hypokalaemia can usually be corrected with oral potassium supplements (effervescent or slow-release tablets). For patients on intravenous fluids, potassium supplements are added as appropriate. The infusion rate should not generally exceed 15–20 mmol per hour, but larger quantities may be required following operations involving cardiopulmonary bypass.
Hyperkalaemia: This is less common than hypokalaemia in surgical patients but may require urgent correction. In the preoperative patient, it is most commonly caused by chronic renal failure, high doses of ACE inhibiting drugs or potassium-sparing diuretics. Occasionally, non-steroidal anti-inflammatory drugs cause hyperkalaemia. Postoperative hyperkalaemia is usually iatrogenic, caused by excessive intravenous potassium administration, although it may be associated with acute renal failure or blood transfusion.
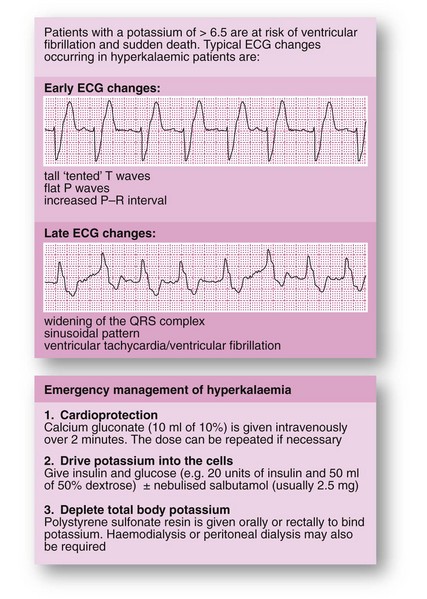
Hyperkalaemia is asymptomatic in its early stages but there is a high risk of sudden death from asystole when plasma potassium concentration reaches about 7.0 mmol/L. The emergency management of hyperkalaemia is shown in Figure 2.3.
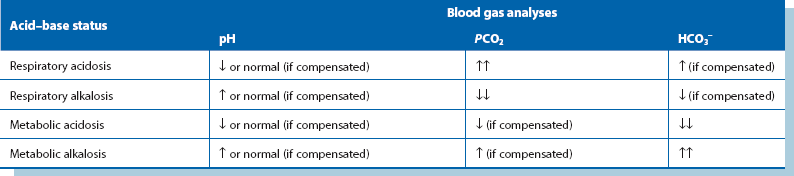
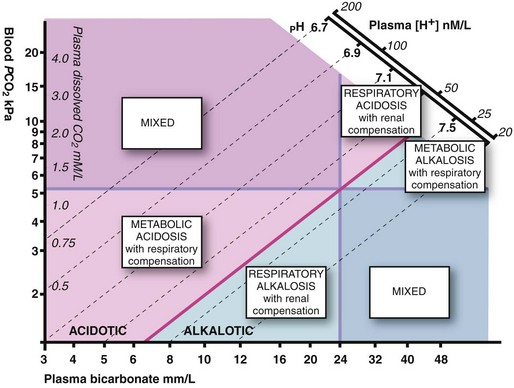
Acid–base disturbances (see Fig. 2.4 and Table 2.4)
Major acid–base abnormalities are rare in uncomplicated surgery and usually arise in seriously ill patients. In a nutshell, when breathing is inadequate, carbon dioxide builds up and combines with water to produce carbonic acid (‘respiratory acid’) which contributes to an acidic pH. Treatment is to lower the PCO2 by assisted breathing. In addition, when normal metabolism is impaired, oxidative metabolism declines and lactic acid accumulates. Treatment is directed at the cause of metabolic impairment, e.g. sepsis, together with organ support therapy, e.g. oxygen, intravenous fluids and antibiotics.
Metabolic acidosis: Metabolic acidosis usually follows an episode of severe tissue hypoxia resulting from hypovolaemic shock, myocardial infarction or systemic sepsis. The most common cause is inadequate tissue oxygenation leading to accumulation of lactic acid. In surgical patients, the onset of metabolic acidosis is often an indicator of serious intra-abdominal problems such as an anastomotic leak. Metabolic acidosis is also seen in acute renal failure and uncontrolled diabetic ketoacidosis. Clinically, patients have rapid, deep, sighing ‘Kussmaul’ respirations as they hyperventilate to blow off carbon dioxide (a respiratory compensatory mechanism). Arterial blood gas estimations show the characteristic picture of raised hydrogen ion concentration and low standard bicarbonate with a low arterial PCO2. Plasma potassium concentration is elevated because of a shift from the intracellular compartment to the extracellular compartment. Treatment is directed at the underlying cause.
Respiratory acidosis: This results from carbon dioxide retention in respiratory failure. The usual causes in surgical patients are underlying chronic respiratory disease made worse by postoperative chest complications or prolonged respiratory depression due to sedative, hypnotic or narcotic drugs. Plasma hydrogen ion concentrations and PCO2 are elevated but standard bicarbonate is initially normal. A degree of metabolic compensation may occur as the kidneys excrete excess hydrogen ions and retain bicarbonate. Treatment is directed at the underlying cause and to providing assisted ventilation.
Metabolic alkalosis: Metabolic alkalosis is usually caused by severe and repeated vomiting or prolonged nasogastric aspiration for intestinal obstruction. The latter classically occurs in pyloric stenosis with gross loss of gastric acid. The patient becomes severely dehydrated and depleted of sodium and chloride ions; the condition is thus known as hypochloraemic alkalosis. The kidney attempts to compensate by conserving hydrogen ions but this occurs at the expense of potassium ions lost into the urine. Patients become hypokalaemic not only from excess urinary loss but also because potassium shifts into the cells in response to the alkalosis. Treatment of hypochloraemic hypokalaemic alkalosis involves rehydration with normal saline infusion including potassium supplements; large volumes (up to 10 litres) are often required. Renal excretion of bicarbonate ions eventually corrects the alkalosis.
Nutritional management in the surgical patient
Malnutrition is a wasting condition resulting from deficiencies in energy (i.e. calorie), protein and sometimes vitamins and trace elements. Recognising and treating pre-existing malnutrition and preventing postoperative starvation are important aspects of surgical management that are often neglected. Basic evaluation for malnutrition should be a standard part of assessing surgical patients (see Box 2.4) because untreated malnutrition predisposes to a range of problems that substantially increase morbidity and mortality rates and delay recovery (see Box 2.5).
Causes of malnutrition include reduced food intake (anorexia, fasting, pain on swallowing, physical or mental impairment), malabsorption (impaired digestion or absorption, or excess loss from gut) and altered metabolism (trauma, burns, sepsis, surgery, cancer cachexia). Patients with any of these predisposing factors need to be scrutinised more thoroughly for malnutrition.
In practice, most surgical patients have no special nutritional requirements and easily withstand the short period of starvation associated with their illness and operation. All hospitalised patients should be screened using a recognised screening tool and their nutritional state optimised preoperatively as far as is feasible. In any case, optimal nutritional support should be provided after operation.
Nutritional support in hospital is usually provided by a dedicated team and input ranges from encouraging the patient to eat regularly through offering easily prepared but tasty oral diets (e.g. liquidised normal food), through concentrated sip feeds (e.g. Fortisip) and various types of supplementary enteral nutrition given via tube, to managing long-term total parenteral nutrition (TPN) for patients unable to absorb nutrients from the gastrointestinal tract.
Recognising the patient at risk
Malnutrition is common in surgical patients and often goes unrecognised. Studies have shown that as many as 50% of surgical inpatients suffer from mild malnutrition and 30% from severe malnutrition. Simple clinical assessment is the best determinant of the state of nutrition, although other indices can also be used (see Box 2.4).
For patients found to be malnourished, studies have shown that simple pretreatment with regular proprietary sip feeds can stave off postoperative muscle weakness, reduce fatigue and markedly lessen complication rates. However, the evidence of clinical benefit is weak for more complex and prolonged endeavours to improve nutrition by the parenteral route (for example, in oesophageal cancer). Even if it is impracticable to improve the preoperative nutritional state, malnutrition still needs to be recognised and attention given in the postoperative period. The duration of starvation should be kept as short as possible and appropriate nutrition provided. This contributes to healing, improves resistance to infection and reduces complications caused by muscle weakness (see Box 2.5).
Effects of starvation
Simple starvation: During simple starvation (i.e. in the absence of illness or trauma), blood glucose concentration is maintained by lowering of insulin secretion and increasing glucagon production. Liver glycogen becomes exhausted within 24 hours but gluconeogenesis in liver and kidneys is enhanced, utilising amino acids from protein breakdown and glycerol from lipolysis as substrates. Much of the glucose thus produced is used by the brain, as most other tissues are able to metabolise fatty acids and ketones derived from adipose tissue. Overall energy demands fall in simple starvation and energy is obtained largely from body fat. Protein is conserved until a late stage.
Trauma, surgery or sepsis: In severe trauma or major surgery, and particularly in sepsis, energy requirements increase by 20–100% of normal. As in simple starvation, lipid becomes a major fuel source; this decreases glucose utilisation, but fatty acids other than glycerol cannot be used for glucose synthesis. Hepatic glucose production increases, but peripheral glucose utilisation is impaired, often leading to hyperglycaemia.
Skeletal muscle proteolysis and urinary nitrogen excretion increase enormously compared with the fasted state. Protein from skeletal muscle is catabolised to release amino acids (particularly alanine), lactate and pyruvate. The stimulus for proteolysis is likely to be macrophage cytokines (e.g. IL1, IL6, TNF). IL1 reduces hepatic albumin synthesis in favour of more urgently needed acute-phase proteins and gluconeogenesis. Amino acids are also used directly in wound healing and in haemopoiesis.
In sepsis, there is a progressive inability at mitochondrial level to fully oxidise substrates for energy generation, leading to a fall in oxygen consumption as sepsis worsens. Fatty acids are increasingly mobilised from adipose tissue, manifesting as hypertriglyceridaemia; mobilisation is governed by raised levels of glucagon, catecholamines, cortisol and TNF. Fatty acids are oxidised for adenosine triphosphate (ATP) production in order to fuel synthesis of new glucose and proteins. If liver failure develops, amino acid clearance deteriorates and plasma concentrations rise. Some amino acids are then metabolised into false neurotransmitters which promote the vasodilatation and hypotension seen in sepsis and cause septic encephalopathy.
Supplementary nutrition
Supplementary nutrition other than liquidised diets and sip feeds is a complicated and sometimes expensive process with distinct risk of complications. It should not be undertaken without proper assessment. Deciding whether a patient is likely to benefit from supplementary nutrition depends on determining:
• That the patient is malnourished or will be deprived of nutrition for at least 5 days
• That the patient is likely to benefit—certain conditions make supplemental nutrition ineffective (e.g. enteral feeding in high output enterocutaneous fistula)
• Whether there is an appropriate route for administration, e.g. suitable gut function
Nutritional support is generally recommended in well-nourished patients who are unable to tolerate oral feeding for 7–10 days, or 5–7 days if already malnourished.
Methods of giving supplementary nutrition: Box 2.6 summarises the range of nutritional regimens and their main surgical indications. The gastrointestinal tract should be used whenever possible because any form of enteral feeding is intrinsically safer than parenteral nutrition and is much cheaper. In addition, the small intestinal mucosa tends to atrophy when not used. Enteral feeding supports the gut-associated immunological shield and prevents microorganisms translocating into the circulation, reducing the chances of blood-borne infection. Contraindications to enteral feeding include intestinal obstruction, high-output intestinal fistula, intractable vomiting or diarrhoea, and severe malabsorption.
Sip feeds: If the patient is able to eat, fluid diets (total or supplementary) can be given orally. Proprietary sip feeds containing easily absorbed calories, protein, minerals and vitamins are available in a variety of formulations and flavours and are well tolerated.
Tube feeds: Certain patients are unsuitable for sip feeding but can be fed by one of several tube feeding routes. Indications include patients with swallowing difficulties (including overspill and lack of cooperation), anorexia, lack of palatability of liquid feeds, the need for a higher volume of feed than the patient can comfortably manage and anticipated substantial delay in resuming oral feeding after operation.
Even if the patient is unable to swallow (for example, because of bulbar palsy, unconsciousness or facial fractures), complete enteral nutrition can be delivered by means of a fine-bore nasogastric or nasojejunal tube, the latter for those who require post-pyloric enteral feeding, e.g. in acute pancreatitis). An individual fluid diet is formulated and is delivered at a controlled rate using a pump, often overnight.
Feeding tubes can also be placed percutaneously into stomach or jejunum, either at operation (if feeding problems are anticipated) or with endoscopic or laparoscopic help. Gastrostomies are often employed in patients after stroke or in those with upper gastrointestinal anastomoses or obstructing lesions. The usual technique nowadays is by percutaneous endoscopic gastrostomy (PEG), combining gastroscopy and percutaneous placement. PEG tubes are contraindicated in peritonitis, ascites and prolonged ileus.
For jejunostomy placement, the tube is tunnelled submucosally for a distance before entering the bowel lumen using a wide-bore needle; this minimises the risk of leakage. Jejunostomy tubes must be placed under direct vision at operation or laparoscopically.
Certain patients not requiring full enteral or parenteral feeding may benefit from vitamin supplements, for example, folic acid and thiamine for alcoholics, or vitamin K injections for patients on prolonged antibiotic therapy where disturbed gut flora may impair absorption of vitamin K.
Total parenteral nutrition (TPN)
Parenteral nutrition should be reserved for appropriate cases of intestinal failure (see below) and should not be embarked upon lightly.
TPN formulations principally contain a mixture of glucose, amino acids, lipids, minerals and vitamins. Non-nitrogenous sources of energy in the form of glucose and lipids have a protein-sparing effect and minimise the consumption of amino acids as energy.
The osmolality of the mixture is usually high so that administration needs to be via a dedicated central venous line to minimise the risk of venous thrombosis; formulations for peripheral infusion are available but the technique is losing favour. The usual aim of TPN is to provide sufficient nitrogen and energy to offset the catabolic demands of surgery and/or trauma and their complications and, if possible, compensate for any pre-existing malnutrition.
In calculating requirements, protein intake should be matched to estimated nitrogen losses; this can be calculated by measuring urinary nitrogen losses as urea or else a standard formula (which also estimates other requirements) can be employed. For example, basic adult daily requirements are 100 g protein (as amino acids), 350 g glucose and 50 g lipid to provide energy. These quantities need to be adjusted according to individual requirements.
Excessive nutrition can be a problem. Hyperglycaemia can be corrected with modest doses of insulin but in the longer term disturbances of liver function may reflect intrahepatic cholestasis caused by fatty infiltration. In intrahepatic cholestasis blood tests show elevated plasma alkaline phosphatase and gamma glutaryl transferase.
Indications for TPN: Parenteral nutrition should be reserved for patients who are already malnourished (or are likely to become malnourished), in whom the GI tract is not functional or is inaccessible and is likely to remain so for a substantial period of days or weeks. Note that in major sepsis, the metabolic changes described earlier mean that TPN brings little benefit.
Methods of giving TPN: Parenteral nutrition is usually delivered into the superior vena cava via the internal jugular or subclavian vein. This is so that high venous flow rapidly dilutes the hyperosmolar solution, minimising thrombosis risk. If long periods of nutritional support are anticipated, a designated tunnelled line is usually employed, with the skin access point remote from the venous entry point to minimise risk of line infection.
The choice and quantity of nutrients starts from a standard baseline for body weight and is varied (with specialist advice) according to individual needs.
Parenteral nutrition is costly in materials and staff time and is prone to complications; it should be discontinued as soon as nutrition can be supplied by an enteral route. Patients on TPN need close and regular monitoring for a range of problems including line problems, local and systemic infection, fluid balance and deficiencies of electrolytes (see Box 2.7). Complications of TPN are detailed in Box 2.8.
Refeeding syndrome
Refeeding syndrome was first described in prisoners in the Far East after the Second World War who developed cardiac failure when starting to eat after prolonged starvation. With reduced carbohydrate intake, insulin secretion falls and fat and protein are catabolised in place of carbohydrate. This results in loss of intracellular electrolytes, particularly phosphate, which becomes depleted. Phosphate is essential for generating adenosine triphosphate and for other vital phosphorylation reactions.
When enteral or parenteral feeding is restarted after starvation, there is sudden reversion from fat to carbohydrate metabolism. Insulin secretion rises and cellular uptake of glucose, phosphate, potassium and water increases. This can lead to profound hypophosphataemia, often with hypokalaemia and hypomagnesaemia. Note that all extracellular fluid is affected by declining levels of these electrolytes. In the starved state, there is total body depletion of electrolytes but plasma concentrations can be misleadingly normal because of renal compensation.
Refeeding syndrome occurs when plasma phosphate falls to less than 0.50 mmol/L. Clinical features include cardiac and respiratory failure, arrhythmias, rhabdomyolysis, white cell dysfunction, seizures, coma and sudden death. Early signs may go unrecognised; the plasma phosphate may not be measured or the significance of grossly abnormal results not appreciated.
Malnourished patients at risk of refeeding syndrome should start artificial feeding with a quarter to half of the expected calorie requirements. Plasma phosphate, magnesium, calcium, potassium, urea and creatinine concentrations should be measured daily and deficiencies corrected. If required, 50 mmol of intravenous phosphate is given over 24 hours and may need repeating. Thiamine must also be replaced in these patients.