Appendicitis
Introduction
Acute appendicitis is the most common cause of intra-abdominal infection in developed countries and appendicectomy the most common emergency operation. In the UK, 1.9 females per 1000 have the operation each year compared with 1.5 males, and about 1 in 7 people eventually undergo the operation. Surprisingly, the incidence of appendicitis fell by about 30% between the 1960s and the 1980s, for reasons unknown.
Appendicitis can occur at any age but is most common below 40 years, especially between 10 and 20. It is rare below the age of 10 and very rare below 2 years. Appendicitis is rare in rural parts of developing countries, but the incidence approaches that of the West in the cities. Different susceptibility in similar people is probably related to reduced dietary fibre in city-dwellers.
Acute appendicitis should be considered in any patients presenting to hospital with acute abdominal pain. Even previous appendicectomy does not absolutely rule out the diagnosis. Despite lay impressions, a positive diagnosis is often difficult to make; this is partly because of the lack of specific tests to confirm or exclude appendicitis. At open operation a non-inflamed appendix is sometimes found but a small number of ‘negative’ operations may be unavoidable. Laparoscopy improves diagnostic accuracy, particularly in young women, and is used therapeutically to remove an inflamed appendix; it also has lower complication rates.
Anatomy of the appendix
The appendix is a blind-ending tube arising from the caecum at the meeting point of the three taeniae coli, just distal to the ileo-caecal junction. The appendix base thus lies in the right iliac fossa, close to McBurney's point. This is two-thirds of the way along a line from umbilicus to anterior superior iliac spine (see below, Fig. 26.6, p. 348). In most cases, the appendix is mobile within the peritoneal cavity, suspended by its mesentery (meso-appendix), with the appendicular artery in its free edge. This is effectively an end-artery, with anastomotic connections only proximally.
The appendix is described as lying in several ‘classic’ sites, but apart from the true retrocaecal appendix, the organ probably floats in a broad arc about its base (see Fig. 26.1). Only inflammation will fix it in a particular place. Its position then determines the clinical presentation. In about 30% of appendicectomies, it lies over the pelvic brim the (‘pelvic appendix’). In some cases, the appendix lies retroperitoneally behind the caecum and often plastered to it by fibrous bands. Thus, an inflamed retrocaecal appendix may irritate the right ureter and psoas muscle, and may even lie high enough to simulate gall bladder pain.
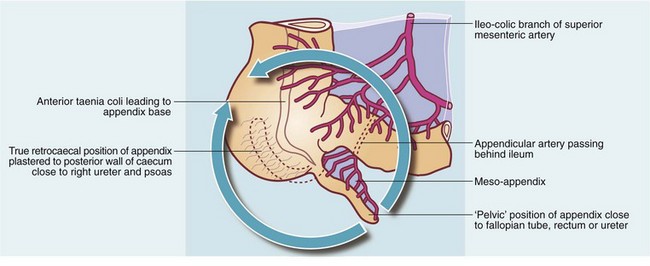
Fig. 26.1 Surgical anatomy of the appendix
The appendix can be positioned anywhere on the circumference shown by the arrowed arc
Histologically, the appendix has the same basic structure as the colon. It is covered by serosa (visceral layer of peritoneum) becoming continuous with the meso-appendix serosa. A retroperitoneal appendix has no serosal covering. A prominent feature of the appendix is its collections of lymphoid tissue in the lamina propria. This often has germinal centres and is prominent in childhood but diminishes with increasing age.
The mucosa contains a large number of cells of the gastrointestinal endocrine amine precursor uptake and decarboxylation (APUD) system. These secrete mainly serotonin and were formerly known as argentaffin cells. Carcinoid tumours commonly occur in the appendix and arise from these cells.
Pathophysiology of appendicitis
Appendicitis is probably initiated by luminal obstruction caused by impacted faeces or a faecolith. This explanation fits the epidemiological observation that appendicitis is more common with a low dietary fibre intake.
In the early stages of appendicitis, the mucosa becomes inflamed first. Inflammation eventually extends through the submucosa to involve the muscular and serosal (peritoneal) layers. A fibrinopurulent exudate on the serosal surface extends to any adjacent peritoneal surface, e.g. bowel or abdominal wall, causing localised peritonitis.
By this stage the necrotic glandular mucosa sloughs into the lumen, which becomes distended with pus. Finally, the end-arteries supplying the appendix thrombose and the infarcted appendix becomes necrotic or gangrenous at the distal end and the appendix begins to disintegrate. Perforation soon follows and faecally contaminated contents spread into the peritoneum. If the spilled contents are enveloped by omentum or adherent small bowel, a localised abscess results; otherwise spreading peritonitis develops. Acute appendicitis is illustrated histologically in Figure 26.2.
Clinical features of appendicitis
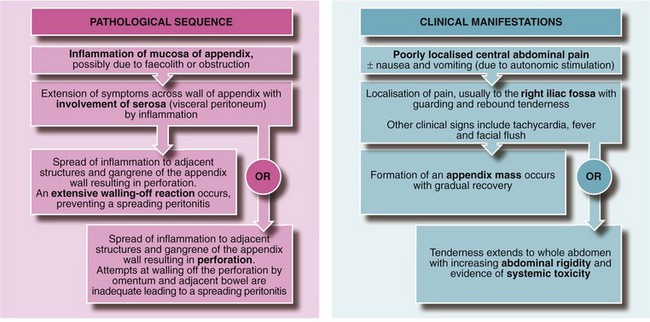
The pathophysiological evolution of appendicitis and corresponding symptoms and signs are illustrated in Figure 26.3.
Classic appendicitis
Acute appendicitis classically begins with poorly localised, colicky central abdominal visceral pain; this results from smooth muscle spasm as a reaction to appendiceal obstruction. Anorexia and vomiting often occur at this stage.
As inflammation advances over the ensuing 12–24 hours, it progresses through the appendiceal wall to involve the parietal peritoneum (innervated somatically). Then pain typically becomes localised to the right iliac fossa. Signs of local peritonitis can be elicited, i.e. tenderness, guarding and rebound tenderness. This classic picture is seen in less than half of all cases, largely because localising symptoms and signs vary with the anatomical relations of the inflamed appendix and the vigour of the body's defences.
Other presentations of acute appendicitis
If the inflamed appendix lies in the pelvis near the rectum, it may cause local irritation and diarrhoea. If it lies near the bladder or ureter, inflammation may cause urinary frequency, dysuria and (microscopic) pyuria, i.e. leucocytes in the urine. These findings may be mistakenly interpreted as urinary tract infection. An inflamed retrocaecal appendix produces none of the usual localising symptoms or signs, but may irritate the psoas muscle, causing involuntary right hip flexion and pain on extension. A high retrocaecal appendix may cause pain and tenderness below the right costal margin. An inflamed appendix near the Fallopian tube causes pelvic pain suggestive of an acute gynaecological disorder such as salpingitis or torsion of an ovarian cyst.
The early phase of poorly localised pain typically lasts for a few hours until peritoneal inflammation produces localising signs. If untreated, the inflamed appendix may become gangrenous after 12–24 hours and perforate, causing peritonitis unless sealed off by omentum. The whole abdomen becomes rigid and tender and there is marked systemic toxicity. Perforation is common in young children. Sometimes, the pathological sequence is extremely rapid and the patient presents with sudden peritonitis.
In older patients, a gangrenous or perforated appendix is more likely to be contained by greater omentum or loops of small bowel. This results in a palpable appendix mass. This may contain free pus and is then known as an appendiceal abscess. As with any significant abscess, there is a tachycardia and swinging pyrexia. An appendix mass usually resolves spontaneously over 2–6 weeks. In the elderly, an appendix abscess is often walled off by loops of small bowel. There may be no palpable mass and the symptoms and signs may not suggest appendicitis. These include non-specific abdominal pain and features of small bowel obstruction due to localised paralytic ileus. Occasionally, appendicitis may present in a most unusual way. Examples include discharge of an appendix abscess into the Fallopian tube presenting as a purulent vaginal discharge, or appendicitis within an inguinal hernia presenting as a groin abscess.
Making the diagnosis of appendicitis
Acute appendicitis is a clinical diagnosis, relying almost entirely on history and examination. Investigations are only useful in excluding differential diagnoses. Ideally, the diagnosis should be made and the appendix removed before it becomes gangrenous and perforates. This markedly reduces the risk of infective complications. However, unnecessary appendicectomies must be kept to a minimum.
Diagnosis of acute appendicitis poses little difficulty if the patient exhibits the classic symptoms and signs summarised in Box 26.1. However, the patient may present at a very early stage, or the signs may have some other pathological cause. At least two out of three children admitted to hospital with suspected appendicitis do not have the condition.
If evidence for acute appendicitis is insufficient and no other diagnosis can be made, the patient should be kept under observation, admitted to hospital if necessary and re-examined periodically. Eventually, the symptoms settle or the diagnosis becomes clear. Diagnostic laparoscopy may be needed in equivocal cases.
Special points in the history and examination
Acute appendicitis typically runs a short course, between a few hours and about 3 days. If symptoms have been present for longer, appendicitis is unlikely unless an ‘appendix mass’ has developed. A recent or current sore throat or viral-type illness, particularly in children, favours a diagnosis of mesenteric adenitis (inflammation of mesenteric lymph nodes analogous to viral tonsillitis). Urinary symptoms suggest urinary tract infection but may also occur with pelvic appendicitis.
The patient with appendicitis is typically quiet, apathetic and flushed; the lively child doing jigsaw puzzles almost never has appendicitis! Oral foetor may be present but is not a reliable sign. Cervical lymphadenopathy may suggest a viral origin for the abdominal pain. Mild tachycardia and pyrexia are typical of appendicitis but a temperature much over 38°C makes the diagnosis of acute viral illness or urinary tract infection more likely.
Signs of peritoneal inflammation in the right iliac fossa are often absent in the early stages. The patient should be asked to cough, blow the abdominal wall out and draw it in; these all cause pain if parietal peritoneum is inflamed. In children, it may be difficult to interpret apparent tenderness, especially if the child cries and refuses to cooperate. This can usually be overcome by distracting the child's attention whilst palpating the abdomen through the bedclothes or even with the child's own hand under the examiner's hand. Several signs (e.g. Rovsing's sign—pressure in the left iliac fossa causing pain in the right iliac fossa) are said to point to a diagnosis of appendicitis but all are unreliable. One useful test is to ask the child to stand, then to hop on the right leg. If this can be achieved, there is unlikely to be significant peritoneal inflammation.
Rebound tenderness was traditionally demonstrated by palpating deeply, then suddenly releasing the hand. However, this can cause excessive and unexpected pain. A kinder and more precise method is to perform gentle percussion in the right iliac fossa. This displaces and irritates inflamed peritoneum in a controlled way; if this is painful, then rebound is present. Anterior peritoneal tenderness on rectal examination (i.e. pelvic peritonitis) supports the diagnosis of appendicitis, provided other signs are consistent, but note the appendix itself cannot be palpated. In pelvic appendicitis, rectal tenderness may be the only abdominal sign. Lack of this sign does not, however, exclude appendicitis.
Differential diagnosis
This theoretically includes all the causes of an acute abdomen. However, the conditions of practical importance are summarised in Box 26.2. These other conditions rarely need operation. Certain uncommon conditions such as Yersinia ileitis and inflamed Meckel's diverticulum (Fig. 26.4) are included in the list but they can only be distinguished from appendicitis at laparoscopy or operation.
The equivocal diagnosis
If acute appendicitis can be confidently diagnosed clinically, no further investigations are needed except for potential co-morbidity, anaemia or dehydration. It is worth emphasising there are no specific diagnostic tests; where the diagnosis is in doubt, the patient must be re-examined every few hours to detect clinical changes to ensure deterioration is detected early. Missing an evident clinical diagnosis and sending the patient home causes unnecessary problems and is likely to prompt a claim for medical negligence.
Certain investigations may be useful where the diagnosis is in doubt. The white blood count is usually unhelpful, as a modest rise occurs in many conditions. If there is a great rise (say to over 16 × 103), appendicitis is usually already clinically obvious, but a low WBC helps exclude non-suppurative gynaecological pathology. Urinalysis must be performed if urinary tract infection is possible. A pregnancy test should be performed in females of child-bearing age.
Various scoring systems have been devised to improve the accuracy of clinical diagnosis. The best known is the Alvarado score (see Table 26.1) but results are too variable for it to be of much clinical benefit.
Table 26.1
Scoring system for the diagnosis of acute appendicitis based on the Alvarado score
| Feature | Score |
| Migration of pain from central abdomen to right iliac fossa | 1 |
| Anorexia | 1 |
| Nausea or vomiting | 1 |
| Tenderness in right iliac fossa | 2 |
| Rebound tenderness | 1 |
| Raised temperature (≥37.5°C) | 1 |
| Raised leucocyte count ≥10 × 109/L | 2 |
| Neutrophilia of ≥75% | 1 |
| Total | 10 |
The Alvarado scoring system is an objective, structured means of assessing patients with right iliac fossa pain, but has proved unreliable in diagnosing acute appendicitis. However, patients with an initial score of 4 or less are very unlikely to have appendicitis and do not need hospital admission unless symptoms worsen. In patients with appendicitis, 40% have rising scores, confirming this as a progressive disorder in which symptoms and signs evolve with time
Abdominal X-rays are not needed unless there is confusing evidence of abdominal pathology after a period of observation. A single right iliac fossa fluid level or even widespread small bowel dilatation suggests local adynamic bowel disorder due to appendicitis causing functional obstruction, but this is an uncommon finding. Even less commonly, a perforated appendix may allow sufficient free gas to escape to show on plain X-rays. In adults with an equivocal diagnosis of appendicitis, the plasma amylase should be measured to exclude acute pancreatitis. Abdominal ultrasound can be helpful to detect an abscess or mass, or non-appendiceal pathology, but cannot be relied upon to show uncomplicated appendicitis. CT scanning is claimed to be accurate but submits the patient to a high radiation dose and greatly increases the cost of investigation. Laparoscopy is increasingly used in women of menstruating age in whom gynaecological pathologies are common. However, this is an invasive investigation requiring a general anaesthetic and is best employed when an operation is clearly indicated but the diagnosis is still ambiguous.
Problems in the diagnosis of appendicitis
Appendicitis is rarely seen below 2 years of age, but when it does occur, the ‘typical’ abdominal symptoms and signs are obscure or absent. An infant or toddler may display signs of infection without revealing an abdominal origin. Abdominal X-rays may demonstrate dilated loops of bowel and fluid levels. Generalised peritonitis supervenes all too rapidly in this age group because abdominal defences are rudimentary, in particular the greater omentum ‘wrapping’ effect. Laparotomy is usually indicated in an ill infant with abdominal signs.
The elderly
Appendicitis usually develops more slowly in the elderly. The appendix wall becomes fibrotic with age and the area is more readily walled off by omentum and adherent small bowel. Indeed, many cases probably resolve spontaneously. In those who reach hospital, the history is often as long as 1 week. Features of obstruction may be present, including vomiting, colicky abdominal pain and obstructed bowel sounds. A mass may be palpable if the patient is relaxed and not too tender but often it can be palpated only under general anaesthesia. Abdominal X-rays may reveal fluid levels in the right iliac fossa.
Pregnancy
Appendicitis occurs at least as often during pregnancy as at other times but the diagnosis can be difficult. The appendix is displaced upwards by the enlarging uterus and abdominal pain and tenderness are in a higher position. The management of the pregnant patient must be shared with an obstetrician. Laparoscopy may be indicated but becomes technically difficult beyond 26 weeks. Mortality from appendicitis for both mother and fetus rises as the pregnancy progresses and can be as high as 9% for the mother and 20% for the fetus in the third trimester.
The ‘grumbling’ appendix
Recurrent bouts of right iliac fossa pain are often labelled ‘grumbling appendix’. Appendicular pathology is probably not the cause in most. Persistent chronic appendiceal inflammation probably does not occur, but recurrent bouts of appendicular colic or low-grade acute appendicitis undoubtedly do. These children may have several abortive admissions for abdominal pain and it may eventually be justifiable to remove the appendix to allay parental anxiety. A non-inflamed appendix containing a faecolith or threadworms (assumed to have caused the pain) is often found. The pain will be cured in no more than half.
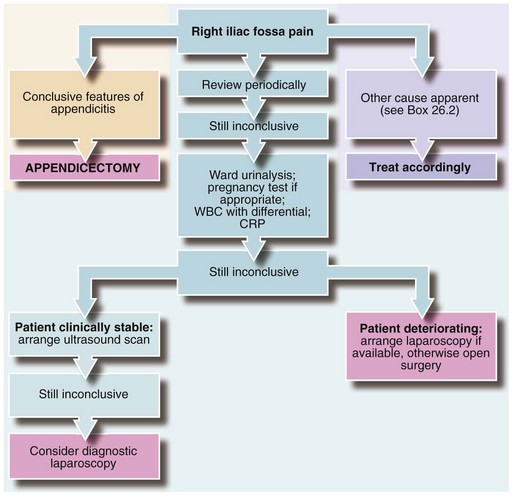
The management of suspected appendicitis is summarised in Figure 26.5.
Appendicectomy
The annual death rate from appendicitis has fallen dramatically since 1960. There were 3193 deaths in 1934 in the UK, whereas by 1982 this had fallen to 110. This results from better general nutrition, earlier presentation, better preoperative preparation and better anaesthesia. Deaths that now occur are usually due to dehydration and electrolyte changes unrecognised or ineffectively treated before surgery, often as a result of a late or missed diagnosis. Infective complications of appendicitis have fallen dramatically since the 1970s because of the widespread use of prophylactic antibiotics.
Antibiotic prophylaxis
In appendicitis, most intra-abdominal infective complications and wound infections occur in perforated or gangrenous appendicitis (see Box 26.3). Most infecting organisms are anaerobic and infections can largely be prevented by prophylactic metronidazole. Rectal suppositories are as effective as intravenous metronidazole and are cheaper but are best given 2 hours before operation. Aerobic organisms are involved in fewer cases and some surgeons advocate additional prophylaxis with an antibiotic such as a cephalosporin. In adults with moderate appendicitis, trials of antibiotic treatment alone compare favourably with appendicectomy but about a quarter present later with recurrent appendicitis.
Technique of appendicectomy
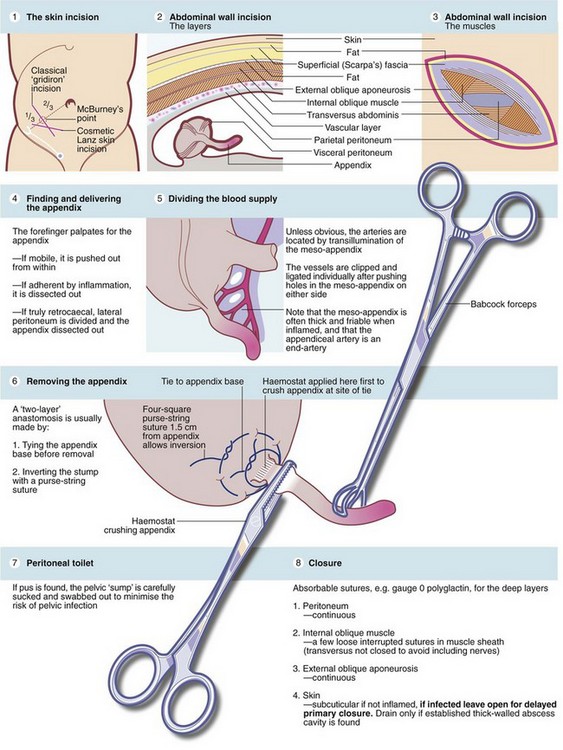
The principal steps are illustrated in Figure 26.6 and should be understood by any doctor assisting with the operation. Increasingly, laparotomy is being replaced by laparoscopic diagnosis and surgery, but the principles are similar. Surgeons performing appendicectomy need to be aware of possible appendiceal neoplasms, present in 0.5—0.9% of appendectomies. Most are innocent carcinoid-type tumours but others are mucinous adenocarcinomas.
Open appendicectomy
A low skin-crease incision (Lanz) rather than a higher and more oblique one centred on McBurney's point is now favoured as it gives a better cosmetic result. The superficial (Scarpa's) fascia (well marked in children) is incised and the three musculo-aponeurotic abdominal wall layers split along the line of their fibres. This produces the ‘gridiron’ incision, described as such because the fibres of external oblique and internal oblique run at right angles to each other. Peritoneum is then lifted and opened and may reveal pus or mucopurulent watery fluid; a swab is taken for microscopy and culture. The appendix is located with a finger and delivered into the wound; further exploration may be needed if it does not lie nearby. A retrocaecal appendix requires mobilisation of the caecum by dividing the peritoneum along its lateral side.
Once the appendix has been delivered, its blood supply in the meso-appendix is divided between clips and ligated. The appendix base is crushed with a haemostat which is then reapplied more distally. An absorbable ligature is tied around the crushed area. After this preparation, the appendix is then excised. A ‘purse-string’ suture may be placed in the caecum near the appendix base to invert the appendix, although this is not used in laparoscopic surgery and patients have not suffered from its omission. If the appendix is perforated or gangrenous, or if pus was found, thorough peritoneal toilet is performed. A sump sucker is guided down into the pelvis with a finger to aspirate fluid, and the area is gently swabbed with gauze to remove adherent infected material. Any pus or a faecolith left behind predisposes to a pelvic abscess.
The peritoneum, internal oblique and external oblique are each closed with two or three absorbable sutures. Drainage is not usually recommended unless there is a thick-walled abscess cavity which will not collapse. If the appendix is perforated or gangrenous, delayed primary closure of the skin is advisable as this reduces the high risk of wound infection. The superficial layers are left open initially and closed after 48 hours if the wound is clean.
After operation, oral fluids, followed by solids, are gradually increased unless vomiting or other complications occur, and most patients can be discharged on the second or third postoperative day.
Laparoscopic appendicectomy
Laparoscopy is a valuable technique that allows the appendix to be found wherever it lies. It also permits visual examination of the rest of the abdominal cavity and pelvis, improving diagnostic accuracy over open operation and minimising negative appendicectomies. It is strongly indicated in patients who are clearly unwell and in need of an operation but in whom the diagnosis is not clear. It is also useful in women of menstruating age and in any patient with pelvic symptoms. If the appendix is abnormal or if there is free fluid in the peritoneal cavity for which no other cause can be found, appendicectomy is performed. Laparoscopic appendicectomy is valuable in the obese, obviating the need for a large incision and a high risk of wound infection. Some surgeons use laparoscopy as a diagnostic tool and then convert to an open operation but laparoscopic appendicectomy may be performed if appropriate skills and instruments are available.
The principles and techniques are similar to open surgery but laparoscopy is more technically demanding. The meso-appendix may be clipped or divided by diathermy and the appendix base is ligated using pre-formed ‘endo-loop’ sutures. The appendix base is rarely buried and must never be diathermied. Superior visualisation and good access allow a thorough washout to be performed. Laparoscopic removal of the appendix has a lower wound infection rate and may allow an earlier return to normal activities.
The ‘lily-white’ appendix
If the appendix is found not to be inflamed at open operation (colloquially termed ‘lily-white’), it should always be removed because an appendicectomy scar would lead future doctors to assume the appendix has been removed. The abdomen is explored as allowed by the incision to search for a cause for the symptoms:
• Mesenteric lymph nodes in children may be grossly enlarged by mesenteric adenitis—probably viral in origin
• The terminal ileum may be thickened and reddened by Crohn's disease or, more rarely, by Yersinia ileitis. The latter is a self-limiting condition caused by the organism Yersinia pseudotuberculosis and requires no specific treatment. The appendix is removed but the bowel left untouched. If possible, an enlarged mesenteric node is removed for histological examination
• A Meckel's diverticulum may be found within 60 cm of the ileocaecal valve—if inflamed, this is removed but a wide-mouthed non-inflamed diverticulum is usually left alone
• Both ovaries can usually be palpated—ovaries may be twisted, inflamed or enlarged or an inflamed Fallopian tube may be seen
• Cholecystitis, sigmoid diverticulitis (with the sigmoid displaced to the right), inflammation of a caecal diverticulum, hydronephrosis or a leaking aneurysm are rarely found
The appendix mass
A vigorous response to appendicitis may result in a right iliac fossa mass, often with fever. Usually the patient has few systemic symptoms or signs of ill health. A conservative regimen followed by interval appendicectomy 6 weeks later (Ochsner–Sherren regimen) was advocated in pre-antibiotic days but is now less favoured. Early operation under antibiotic cover is now performed more frequently.