Disorders of the thyroid and parathyroid glands
Introduction
Patients with thyroid disorders presenting to a surgeon usually have a neck lump, often asymptomatic but the patient may fear malignancy. In some, the mass may be causing pressure symptoms or cosmetic deformity. A discrete thyroid lump may be found or the whole gland may be enlarged. A large thyroid swelling is known as a goitre, from the Latin for throat ‘guttur’. Most patients are clinically euthyroid (i.e. normal hormone activity) and thyroid function tests are normal. Occasionally patients are referred with hyperthyroidism when medical treatment has failed, radioisotope treatment is unsuitable or there is an overactive nodule. All may require some form of thyroidectomy.
Patients with parathyroid disorders usually attend because of symptomatic or biochemically detected hypercalcaemia caused by excess parathormone, treatable only by surgery for a solitary adenoma, multi-gland hyperplasia or, very rarely, carcinoma.
Thyroid disorders
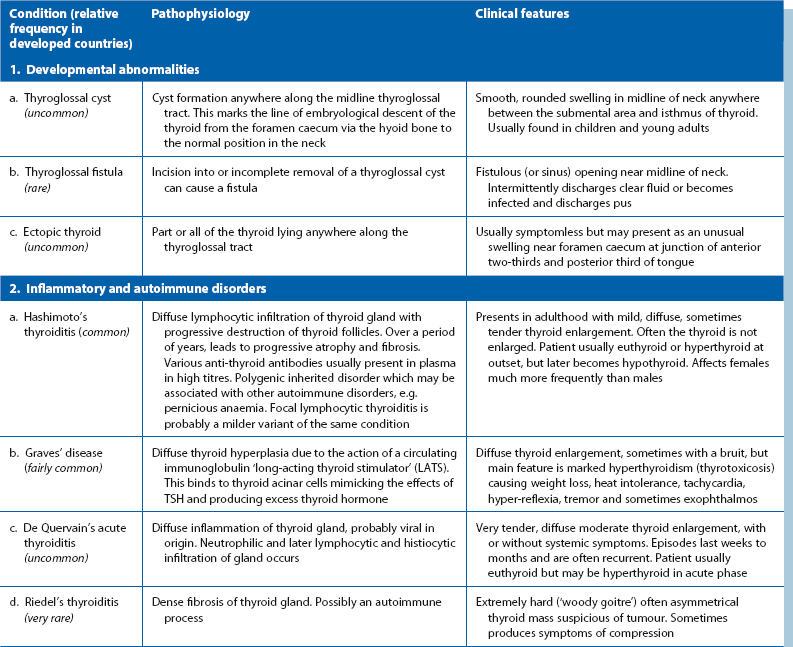
Pathophysiological and clinical features of the various disorders are summarised in Table 49.1, except for thyroid malignancy, outlined later in Table 49.2.
Main clinical presentations of thyroid disease in surgical practice
Diffuse or generalised enlargement of the thyroid
The term goitre is often used for any thyroid enlargement. Most large thyroid swellings in developed countries are simple colloid goitres i.e. idiopathic diffuse or multinodular hyperplasia. Multinodular goitres usually develop from diffuse goitres after some years.
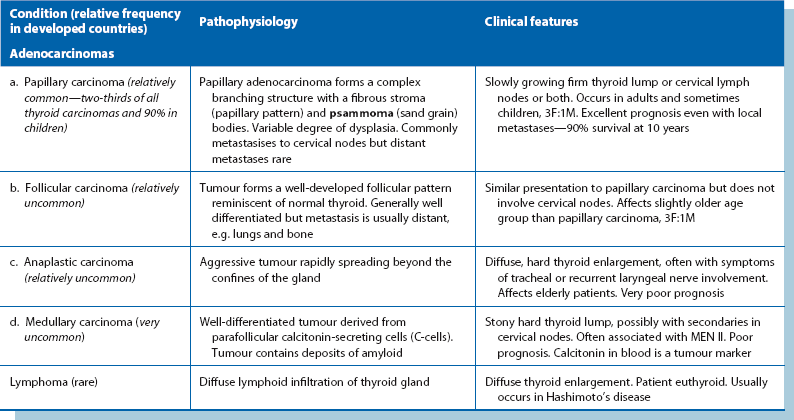
Iodine deficiency is the usual cause of endemic goitres (often in isolated, mountainous regions such as Nepal), preventable by adding iodine to the diet. These are often asymmetrical, soft and composed of hyperplastic nodules, and can reach enormous sizes (see Fig. 49.1). Although unsightly, endemic goitres cause surprisingly few symptoms and the patient is usually euthyroid.
Anaplastic carcinomas may cause thyroid swellings in elderly patients (see Fig. 49.2), usually with symptoms of invasion including hoarseness (recurrent laryngeal nerve), and stridor, particularly at night, with tracheal invasion. The gland is hard on palpation. The uncommon thyroid lymphomas also present with diffuse enlargement.
In Graves' disease (primary hyperthyroidism) there is usually some smooth thyroid enlargement, often increased by drug treatment but almost never the presenting feature. Similarly, in Hashimoto's thyroiditis, the thyroid may be moderately enlarged but firm and finely nodular on palpation.
Solitary thyroid nodule
A clinically solitary thyroid nodule is common but 50% are multinodular on imaging (Fig. 49.3). When small, these nodules are found incidentally, often noticed when the patient swallows. Less than 10% of true solitary nodules are malignant although this rises to about 40% after neck irradiation. Almost all thyroid nodules in childhood are malignant. Fallout from the Chernobyl nuclear meltdown caused many thyroid cancers in children. Malignancy should be excluded in any solitary nodule, and FNA cytology or core needle biopsy is the first step.
A solitary nodule is usually idiopathic hyperplasia which if discrete, is a thyroid adenoma. Thyroid cysts are fairly common. Both fall within the description ‘simple or multinodular colloid goitre’.
Other features associated with thyroid enlargement
A new area of enlargement in an existing goitre may result from haemorrhage into a cyst or nodule, enlargement of a hyperplastic nodule or a developing carcinoma. If the gland extends into the anterior mediastinum behind the sternum (see Fig. 49.6, below), the trachea may be compressed or displaced by this retrosternal goitre and cause stridor, often only obvious when the neck is in certain positions, for example, sleeping on one side. Hoarseness or stridor may also result from invasion of trachea or recurrent laryngeal nerve by anaplastic carcinoma.
Pain and tenderness are uncommon presenting features, but characterise the rare infective de Quervain's thyroiditis. Sometimes the thyroid is painful and tender in Hashimoto's thyroiditis.
Hyperthyroidism
Clinical manifestations of hyperthyroidism are summarised in Box 49.1 (see also Fig. 49.4). Excessive thyroid hormone is a feature of Graves' disease. Mild hyperthyroidism also occurs in the early stages of Hashimoto's thyroiditis, burning out later with the patient becoming hypothyroid. A solitary adenomatous nodule may produce excess thyroid hormone causing hyperthyroidism. This is known as a toxic or hot nodule.
Hypothyroidism
Hypothyroidism is usually the late result of primary thyroid atrophy or Hashimoto's thyroiditis, or treatment for hyperthyroidism. In any case, the gland is small and fibrous. Hypothyroidism is a late complication in up to 25% of patients after subtotal thyroidectomy and even more after radioiodine therapy for thyrotoxicosis, and is inevitable after total thyroidectomy. Hypothyroidism should be considered in surgical patients presenting with constipation and has also been implicated in aortic thrombosis in middle-aged women.
Special points in examining a thyroid swelling
The patient should be seated in a chair (Fig. 49.5) with space to palpate from behind and have a glass of water available to swallow. General examination should look for signs of hyperthyroidism (tachycardia, atrial fibrillation, fine tremor, sweaty palms and hyper-reflexia) and for signs specific to Graves' disease (exophthalmos and ophthalmoplegia). Next, the front of the neck is inspected while the patient swallows; the characteristic rise of a thyroid swelling results from its investment in pretracheal fascia attached to the larynx above. A normal thyroid is not visible even on swallowing, and is not normally palpable.
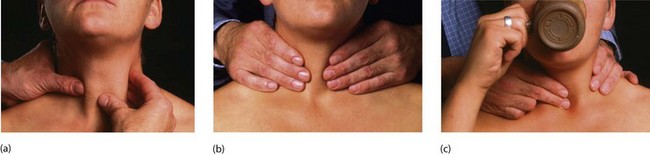
Fig. 49.5 Examination of the thyroid gland
The patient should be sitting upright in a chair with room for the examiner to approach from behind. (a) Gentle palpation from the front with slight sideways pressure from the left hand whilst palpating with the right. This is repeated for the right side of the gland. (b) General palpation of the gland from behind. Is there enlargement? Is it a single nodule or multinodular? How big is it? (c) Palpation of the gland while the patient swallows. Does the gland rise with swallowing? Is there retrosternal extension?
The thyroid area is next palpated from behind. This is best for examining the size, shape and consistency of the gland. It also allows the lower edge of a swelling to be palpated to identify retrosternal extension. The thyroid lobes wrap around the larynx and lie deep to the sternomastoid muscles which tend to conceal thyroid enlargement and make it tricky to examine the whole gland.
The jugular chain of lymph nodes should be palpated for metastases. In thyrotoxicosis, auscultation may reveal a bruit of increased vascularity.
If there is suspicion of recurrent laryngeal nerve palsy because of hoarseness, vocal cord function tests should be performed. The patient is asked to cough and to pronounce the sound ‘ee’; both are likely to be abnormal if there is nerve damage. In this case, or if surgery is contemplated, assessment of cord function should be performed by indirect laryngoscopy, usually in an ENT department.
Approach to investigation of a thyroid mass
The questions during investigation are summarised in Box 49.2 and described in detail below. Patients who have undergone previous neck radiotherapy should be considered at high risk of thyroid carcinoma.
General thyroid status
First establish whether the patient is euthyroid, hyperthyroid or hypothyroid. Initially, this is clinical but estimations of free thyroxine (fT4) and TSH are usually performed. Thyroid-binding globulin is elevated in pregnancy and puberty; using free thyroxine level corrects for this and avoids misinterpretation. If the patient is clinically hyperthyroid but the fT4 is normal, tri-iodothyronine (T3) levels are occasionally measured. TSH level is usually low in hyperthyroidism and elevated in hypothyroidism. Some laboratories prefer to measure just the TSH level initially and perform detailed tests if this is abnormal.
Thyroid autoantibodies are assayed if autoimmune disease is a possibility. Although not usually measured clinically, the presence of long-acting thyroid stimulating factor (LATS) is diagnostic of Graves' disease. Hashimoto's thyroiditis is characterised by elevation of anti-thyroid antibodies such as anti-thyroglobulin or anti-mitochondrial antibodies (anti-thyroid M).
Morphology of the gland
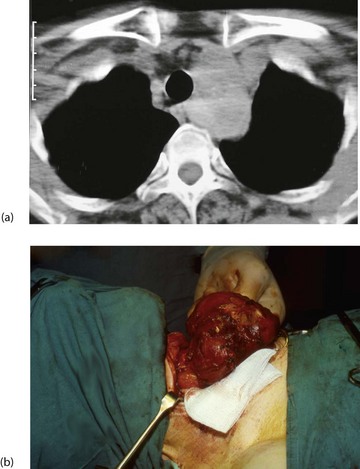
Ultrasound scanning is useful to establish morphology and diagnose cysts. It can also indicate retrosternal extension. CT scans of neck and thoracic outlet are taken if malignancy is suspected or if there appears to be tracheal displacement or compression (Figs 49.6).
Tissue diagnosis
Tissue diagnosis using fine needle aspiration cytology (FNAC) or core needle biopsy is usual for solitary nodules or recently enlarged nodules in multinodular goitres. This can be performed without ultrasound, but ultrasound gives a fuller picture and guides biopsies. Given a competent and involved thyroid cytologist, 90% of thyroid nodules can be categorised this way. Needle core biopsy gives larger specimens with a greater diagnostic potential. If a colloid nodule is diagnosed, excision is not necessary unless it causes compressive symptoms or cosmetic deformity. Obviously malignant lesions require operation. These include papillary, medullary and early anaplastic carcinomas. Most lymphomas are inadequately sampled by FNAC or core biopsy and follicular carcinomas cannot be distinguished cytologically from benign follicular adenomas; both display sheets of follicular cells. Lesions with this appearance should be removed, although most will be benign.
Incision biopsy at open operation is occasionally used for diagnosing generalised thyroid enlargement where the chances of malignancy are low, or lymphoma is suspected.
Functional activity of glandular tissue
Injected radionuclides of iodine are avidly taken up by functioning thyroid tissue and used to be widely employed for thyroid scanning. The increasing use of ultrasound and needle cytology and knowing that only 10% of cold nodules are malignant have greatly reduced the need for radionuclide scanning.
When scanning is employed, the gland is imaged after isotope injection to identify the distribution of isotope activity. This may fall into one of four patterns:
• Diffuse, homogeneous uptake—found in normal glands or in diffuse hyperactivity, e.g. Graves' disease
• Generalised but patchy uptake—in multinodular goitre where hyperplastic nodules are less active than the surrounding normal tissue
• The cold nodule—an area devoid of uptake indicates non-secreting tissue, i.e. tumour, inactive adenomatous nodule or cyst and requires tissue diagnosis
• The hot nodule—or toxic adenoma. This represents an autonomous focus of excess T4 secretion. Secretory activity of the thyroid is suppressed. The patient is usually euthyroid but sometimes thyrotoxic (‘toxic nodule’)
Very occasionally, thyroid malignancies secrete thyroid hormones and show up as warm or hot nodules on isotope scanning. Isotope scanning can also identify and localise ectopic thyroid tissue (in the tongue or along the course of the thyroglossal duct), retrosternal extension of a thyroid swelling and metastases of functioning thyroid carcinomas, provided the thyroid has been removed or ablated.
Specific clinical problems of the thyroid and their management
Hyperthyroidism (thyrotoxicosis)
Two percent of women and 0.2% of men in the UK have hyperthyroidism. Untreated, it causes weight loss, anxiety, tachycardia, palpitations and increased risk of cardiovascular death. Most are caused by Graves' disease, some by toxic multinodular goitre and a few by toxic adenoma. Carcinoma is a very rare cause, occasionally diagnosed incidentally when a hot nodule is examined histologically. Graves' disease is an autoimmune disorder in which circulating antibodies bind to TSH receptors in the thyroid and stimulate follicular cells to secrete thyroid hormones independent of pituitary feedback. Hashimoto's thyroiditis may produce mild hyperthyroidism in its early stages but is self-limiting. If in doubt, the aetiology can be determined by radioisotope scanning.
Treatment of hyperthyroidism: There are three main options: anti-thyroid drugs, radioisotope destruction of functioning thyroid tissue and subtotal (or total) thyroidectomy. Anti-thyroid drugs are the first-line except in the elderly and unfit; also patients with arrhythmias, angina and osteoporosis are usually treated with radioiodine from the outset. A randomised trial of all three treatments showed that of those treated with drugs, 34% developed recurrent hyperthyroidism. In the radioiodine group, half needed more than one dose but all became hypothyroid within a year. In those treated surgically, 8% recurred and needed further therapy. All groups reported 95% satisfaction with no differences in quality of life.
Thyrotoxic eye disease: Half of thyrotoxic patients develop eye signs known as thyrotoxic ophthalmopathy which can arise or regress independently of thyroid function. Eye disease does not occur in multinodular or adenoma thyrotoxicity. Eye disorders range from minor inflammation of conjunctiva with mild prominence of the globe to severe, debilitating and disfiguring eye disease that occurs in 3–5% of thyrotoxic patients.
Radioactive iodide therapy: Radioactive iodide (131I or 125I) is given by mouth as capsules or solution in doses 100 times higher than for diagnostic scanning (see Fig. 49.7). This is appropriate for middle-aged or elderly patients but is contraindicated in pregnancy because of the risk of fetal thyroid damage and genetic disruption. Iodide is avidly taken up by the gland, and beta particle emission destroys the most active thyroid tissue over a period of weeks or months. Note that anti-thyroid drugs usually need to continue until radioiodine achieves its greatest effect. After treatment, the rest of the isotope is excreted via the kidney, faeces, sweat, saliva and breath. Gamma rays are emitted from the patient's body and may be absorbed by others nearby. Patients should avoid pregnancy for 6 months afterwards.
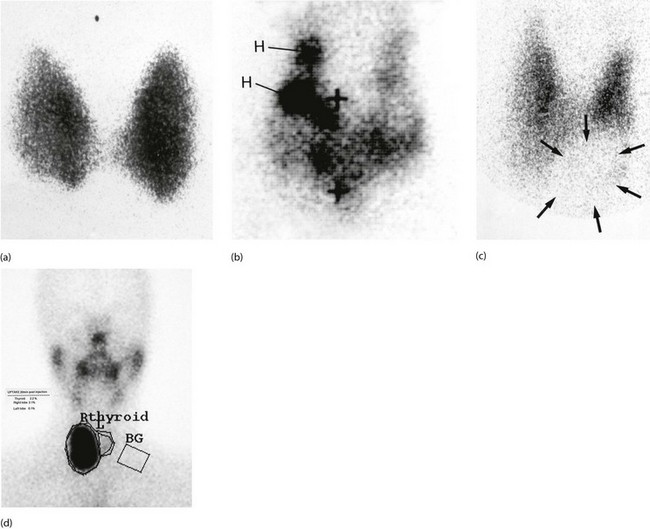
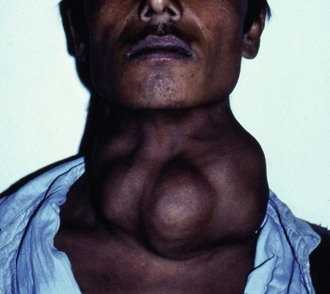
Fig. 49.7 Radioisotope thyroid scans
(a) This enlarged thyroid shows homogeneous tracer uptake typical of a simple colloid goitre. (b) Heterogeneous tracer uptake in a multinodular colloid goitre. The dark areas H are ‘hot nodules’; to maintain the euthyroid state, the rest of the gland exhibits diminished uptake. The + signs indicate the positions of the thyroid cartilage and the suprasternal notch. (c) Solitary ‘cold’ thyroid nodule. The area of low uptake (outline arrowed) at the lower left pole of the thyroid corresponds with a palpable nodule. In the case of a solid lesion (as confirmed by ultrasound), a cold nodule may indicate malignancy. (d) Solitary ‘hot’ thyroid nodule. The area of high uptake in the lower part of the right lobe corresponds to a palpable mass. This patient was hyperthyroid and the lesion could be described as a ‘toxic nodule’. Activity of the rest of the gland is suppressed by pituitary-mediated negative feedback from the high serum thyroxine level. The rectangle marked BG measures the background radiation in order to quantify the thyroid uptake
Different radioiodide doses are used in different units, with higher doses giving a better chance of eliminating hyperthyroidism but giving higher rates of hypothyroidism. Between 10% and 20% need a second dose but once treatment is effective, recurrence is unlikely. Most patients eventually become hypothyroid (about 2–3% each year), especially older patients, those treated with anti-thyroid drugs or those given a high dose. Many units now aim electively to make patients hypothyroid within 6 months and routinely provide levothyroxine replacement. This eliminates the risk of missing hypothyroidism years later and may lower the cardiovascular death risk in euthyroid patients after treatment. There is also a theoretical risk of radioiodine inducing malignancy and so treatment is not advisable in the young. Toxic multinodular disease and toxic adenoma also respond to this treatment; these patients rarely become hypothyroid afterwards.
Unwanted effects: There is a risk of exposing others to radiation during treatment. Current advice is that patients should keep 1 m away from anyone over 5 years for 11 days, from children aged 3–5 for 16 days and from those under 3 for 21 days.
Radioiodine tends to make thyrotoxic ophthalmopathy worse whereas anti-thyroid drugs and surgery do not affect its course. There is no increase in overall cancer death rate in treated patients.
Anti-thyroid drugs: Most thyrotoxicosis patients are initially managed with anti-thyroid drugs to block hormone synthesis. This treatment is not suitable for nodular toxicity because hyperactivity inevitably recurs. Carbimazole is the most popular drug and is generally well tolerated. Carbimazole restores plasma hormone levels to normal over 4–8 weeks and treatment is continued for 12–18 months. Unfortunately, hyperthyroidism recurs in about half within 2 years. Between 5% and 10% develop a rash and there are rare cases of agranulocytosis, usually reversible. The white blood count should be monitored during treatment; a sore throat or other infection should alert the patient and doctor to this possible complication. Propylthiouracil is an effective anti-thyroid drug without these side-effects but poor control, frequent relapses, other side-effects and non-compliance lead to eventual referral for definitive treatment in up to 40%. In unstable patients with hypothyroidism alternating with hyperthyroidism, a block and replace regimen may succeed. Patients are given a higher dose of carbimazole to completely block thyroid hormone production, together with a standard replacement dose of thyroxine.
Beta-adrenergic blocking drugs such as propranolol rapidly control the distressing and dangerous effects of thyrotoxicosis. These drugs may be used initially in extremely toxic patients until anti-thyroid drugs take effect, or if a patient urgently needs to be stabilised before thyroidectomy.
Indications for surgery: Surgery for thyrotoxicosis may be indicated as follows:
• When a quick and effective cure is desired that avoids long-term drug therapy. It is often the best treatment for Graves' disease, particularly in younger patients, where the disease is unlikely to burn itself out for years
• When anti-thyroid drugs have proved unsatisfactory and radioiodide treatment is unsuitable
• In toxic multinodular goitre. Response to drug treatment is variable, and surgery also deals with the cosmetic deformity
• Toxic solitary nodules (‘hot nodules’) may be best excised to allow the suppressed normal thyroid to recover
Preoperative assessment and management of thyrotoxicosis: For all thyroid operations, preoperative assessment often includes laryngoscopy to demonstrate vocal cord function. This evaluates recurrent laryngeal nerve function should there be a question of operative damage later. Even without demonstrable cord damage, there is often a subtle change in voice quality after thyroidectomy, sometimes due to external laryngeal nerve damage. Patients should be warned of this before operation, especially if they are singers or politicians!
Wherever possible, thyroid function should be normalised before operation. The thyrotoxic state carries anaesthetic risks, especially of cardiac arrhythmias. Furthermore, manipulation of the gland may provoke massive release of thyroid hormone, precipitating a potentially lethal thyrotoxic crisis or ‘thyroid storm’. Control is usually achieved with anti-thyroid drugs in the weeks preceding operation. If this fails, or if operation is very urgent, beta-adrenergic blockade can be used.
Anti-thyroid drugs increase the vascularity and this may add to surgical difficulty in toxic enlargement. It is standard practice to administer Lugol's iodine solution orally for 10 days before operation while continuing anti-thyroid therapy. This is believed to reduce vascularity and increase the firmness of the gland, making the operation easier.
Subtotal thyroidectomy: Surgery (Fig. 49.8) for hyperthyroidism aims to remove enough thyroid tissue to render the patient euthyroid whilst preserving enough to prevent hypothyroidism. For Graves' disease or toxic multinodular goitre, about 5–8 g of the gland is left intact. The technique of subtotal thyroidectomy leaves the posterior rim of each lobe in situ, minimising the risk of parathyroid or recurrent laryngeal damage. However, the risk of permanent hypoparathyroidism is 1–4% and of permanent recurrent laryngeal nerve damage 1–5%. Patients need to be warned of these risks before giving their consent to operation. A low transverse collar incision along a skin crease gives the best cosmetic result. Meticulous care is required in ligating the inferior thyroid artery (after identifying the recurrent laryngeal nerve) and the upper pole vessels. Primary or reactionary haemorrhage is a serious complication causing major blood loss and laryngeal compression. To avoid suffocation from a postoperative bleed, instruments for emergency reopening of the wound should be kept at the patient's bedside after operation. The potential complications of thyroidectomy are summarised in Box 49.3.
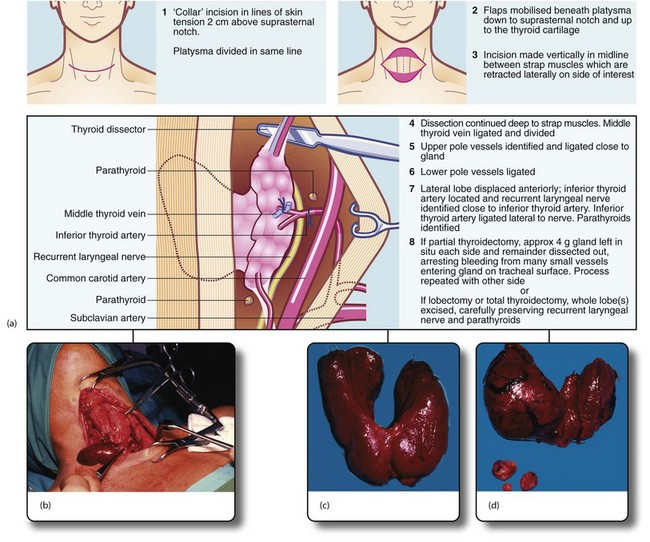
Fig. 49.8 Thyroid and parathyroid operations
(a) The drawings show the standard neck exploration approach to thyroid and parathyroid operations, and the structures at particular danger—the recurrent laryngeal nerve and parathyroid glands. In the photographs, (b) shows neck exploration for hyperparathyroidism. A collar incision has been made and upper and lower flaps are held apart with the specially designed Joll's retractor. A single large parathyroid adenoma is clearly visible. (c) Subtotal thyroidectomy specimen after operation for hyperthyroidism. (d) Total thyroidectomy specimen after operation for right-sided medullary carcinoma. Involved lymph nodes were ‘cherry picked’ and are also shown
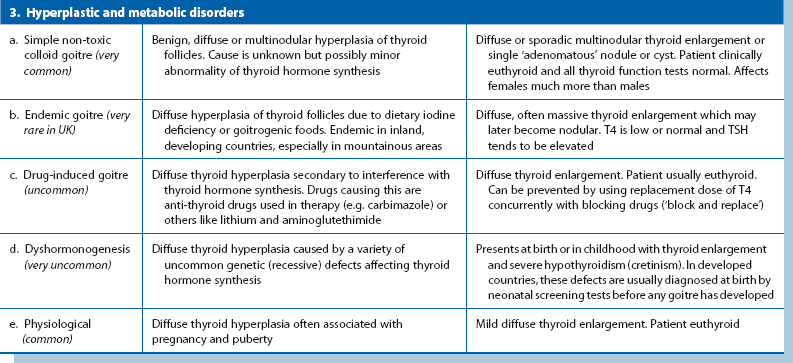
Thyroid malignancies (Table 49.2)
Thyroid malignancies are uncommon, comprising less than 1% of all malignant tumours. Nearly all originate from thyroid follicular cells and form distinct pathological entities: papillary, follicular and anaplastic carcinomas, each with a characteristic pattern of behaviour and prognosis. Papillary and follicular carcinomas are usually well differentiated with low metastatic potential, whereas anaplastic carcinomas behave aggressively. With rare exceptions, none of these secrete thyroid hormones.
About 7% of thyroid carcinomas arise from calcitonin-secreting APUD C-cells. These are known as medullary carcinomas. Lymphomas occasionally involve the gland, usually in pre-existing Hashimoto's disease.
Exposure to ionising radiation during childhood predisposes to thyroid cancer. This includes radiotherapy (once popular for treating ‘status thymolymphaticus’ and other benign disorders) and radioactive fallout. Many people exposed at the Hiroshima and Nagasaki bombings and the Bikini Atoll nuclear tests developed thyroid cancers and, more recently, children exposed to the Chernobyl fallout had a high rate. In most cases of thyroid cancer no aetiological factor is identified.
Papillary carcinoma: Papillary carcinoma constitutes about two-thirds of thyroid malignancies in adults and nearly all in children. Females are affected three times more than males and the peak incidence is 30–45 years. Histologically, the tumour forms a complex branching papillary structure with a fibrovascular stroma, often containing characteristic calcified ‘psammoma bodies’. Epithelial dysplasia ranges between apparently benign and obviously malignant but all tumours grow slowly. Papillary carcinomas are microscopically multicentric in about 80% and about one-third affect both lobes; this is important in planning treatment. The tumour occasionally invades locally into trachea or oesophagus.
Metastasis is to central and later lateral cervical lymph nodes and only rarely to distant sites such as lung or bone. At presentation, lymph nodes are involved in about 40% (90% in children). Node enlargement is often the sole presenting feature and the histology is so close to normal that at one time this was known as ‘lateral aberrant thyroid’. The prognosis is the best of all thyroid carcinomas with only about 10% of patients dying of it by 10 years (of remote metastases); it is remarkable that survival is hardly prejudiced by node metastases. The prognosis is even better for ‘minimal papillary carcinoma’, defined as a single tumour less than 1 cm in diameter in a young patient with no local invasiveness or metastases.
Symptoms and signs: Clinically, papillary carcinoma presents as a slow-growing solitary thyroid or an enlarged lymph node close to the gland. The patient is euthyroid. Isotope scanning shows no uptake in the nodule. Sometimes, other tumour foci in the gland are large enough to manifest as ‘cold nodules’ too. The diagnosis is usually made nowadays by FNAC. A patient presenting with just an enlarged cervical lymph node may be diagnosed unexpectedly after excision and histological examination.
Management: The standard management is total thyroidectomy because of the high risk of other foci in the gland. Palpable cervical nodes are removed at the same operation. Total thyroidectomy is also recommended because recurrent local disease, lymph node or distant metastases can then be treated effectively with radioiodine (131I); this requires a very high TSH level which only occurs if no normal thyroid tissue remains. A further advantage is that plasma thyroglobulin can be used as a tumour marker to detect recurrent disease.
After treatment, oral thyroxine replacement is always necessary at levels appropriate for keeping TSH close to zero. This minimises the risk of stimulating any residual malignant cells; the treatment rarely causes problems. Tumour recurrence in cervical nodes is treated by excision and even this does not adversely affect prognosis. External radiotherapy may be employed for local recurrence, or chemotherapy with doxorubicin for remote metastases.
Since papillary carcinomas progress so slowly and only about 15% develop contralateral lobe recurrence, some surgeons prefer to retain one thyroid lobe if the primary tumour is small and there are no palpable or isotope-detectable nodules. Their reasoning is that further tumours can be removed later without reducing life expectancy.
Follicular carcinoma: Follicular carcinoma is another well-differentiated malignancy. Histologically, neoplastic cells form a well-developed follicular pattern, impossible to distinguish from benign adenomatous hyperplasia on FNAC and even on histology of the surgical specimen. Malignancy may be difficult to diagnose unless there is evident capsular or vascular invasion. Unlike papillary carcinoma, multicentricity is far less common. The peak incidence is 40–50 years, older than papillary carcinoma, but it is three times commoner in women. Generally, follicular carcinoma grows slowly and metastasises late. In contrast to papillary carcinoma, metastasis occurs via the bloodstream to lungs, bone and other remote sites rather than local nodes.
Since follicular carcinoma is rarely multicentric, management depends on local invasion. A tumour with only microinvasion of the capsule has a very good prognosis and only requires removal of the tumour-containing lobe. If there is gross capsular or vascular invasion (or known remote metastases), total thyroidectomy is performed to enhance the radioiodine uptake of metastases for diagnosis, or for treatment with high-dose radioiodine.
Prognosis for the primary can be predicted by the degree of capsular and vascular invasion. Without invasion, 10-year survival is close to 100% but falls to about 30% if there is extensive local invasion.
Anaplastic carcinoma: Anaplastic carcinomas are extremely aggressive with an appalling prognosis and are found almost exclusively in the elderly. Most other cancers are less aggressive in older age groups. Most patients die within a year of diagnosis.
Anaplastic carcinoma consists of sheets of very poorly differentiated cells which proliferate rapidly. The result is a diffuse, hard thyroid enlargement. The tumour soon invades surrounding structures, causing tracheal and oesophageal obstruction and recurrent laryngeal nerve damage. There is also early dissemination to regional lymph nodes and haematogenous spread to lungs, skeleton and brain.
Anaplastic carcinomas respond poorly to radiotherapy and chemotherapy. The distressing symptoms of tracheal obstruction can sometimes be relieved by placing a luminal metal tracheal stent which avoids the need for surgery but does nothing to slow tumour growth.
Medullary carcinoma: This uncommon malignancy arises from parafollicular or C-cells. The tumour often secretes abnormal quantities of calcitonin, a marker of tumour recurrence after excision. Tumours may also secrete other peptides and amines such as serotonin and ACTH-like peptide. Medullary carcinoma usually arises sporadically but may be transmitted genetically in multiple endocrine neoplasia syndrome type II (MEN II). This is an autosomal dominant trait with 50% penetrance and is associated with other APUD cell tumours, particularly phaeochromocytoma and parathyroid adenomas. Thus patients with medullary carcinoma should be examined for these before surgery as a phaeochromocytoma would take operative precedence.
Medullary carcinoma is of pathological interest because the stroma contains extensive amyloid which makes the tumour mass stony hard. Medullary carcinoma grows relatively slowly, metastasising first to regional lymph nodes and later to lungs, bone, liver and elsewhere. The tumour does not take up radioiodine and is resistant to radiotherapy; hence an aggressive surgical approach is required. Standard treatment is total thyroidectomy and clearance of involved anterior cervical and superior mediastinal lymph nodes. Without metastases, operation is often curative but when nodes are involved, 10-year survival falls to about 50%. During follow-up, calcitonin levels are monitored and raised levels indicate tumour recurrence. Surgical re-exploration of the neck may be undertaken to remove involved nodes.
Thyroid lymphoma: Thyroid lymphomas are rare and usually arise in pre-existing autoimmune (Hashimoto's) thyroiditis. Most are non-Hodgkin lymphomas. Diagnosis can only be made histologically, by core needle biopsy or open biopsy, as FNA is inadequate. Treatment is with radiotherapy, and survival depends on whether spread has extended beyond the thyroid capsule. For lesions within the capsule, 5-year survival is 85%, falling to 40% when local spread has occurred.
Goitres and thyroid nodules
Several hyperplastic and metabolic disorders cause diffuse or nodular thyroid enlargement (see Table 49.1).
Idiopathic non-toxic hyperplasia: In developed countries, most goitres referred to surgeons are simple, idiopathic hyperplasia of thyroid follicles. The condition probably begins with diffuse micronodular enlargement; later nodules become heterogeneously enlarged to form a multinodular colloid goitre. Within the same spectrum are solitary hyperplastic nodules (often adenomas) and thyroid cysts, which are huge colloid-filled follicles or else contain straw-coloured fluid.
The aetiology of simple thyroid hyperplasia is unknown, but is probably related to disordered sensitivity to TSH. The patient is usually euthyroid with normal thyroid function tests. Sometimes, hormone secretion escapes from hypothalamic control so the patient becomes hyperthyroid and occasionally thyrotoxic.
Secretory activity within the gland is patchy, explaining the patchy distribution of radioiodine uptake on scanning. Overall hormone secretion may still be within the euthyroid range. Diffuse or multinodular idiopathic goitres develop slowly and cause little trouble until present for many years.
The reasons patients reach surgeons with thyroid enlargement are:
• A goitre has become so large as to be cosmetically unacceptable
• A localised lump has appeared in the thyroid region. This may be a solitary adenomatous nodule, a cyst or, in 10%, thyroid cancer. The apparent solitary lump may be part of an asymmetrical multinodular or multicystic enlargement
• A pre-existing multinodular goitre has undergone rapid asymmetric change
• The patient has become hyperthyroid
• The patient has developed stridor from tracheal compression caused by enlargement of a retrosternal extension
Surgical management of goitre: The indications for surgery in idiopathic goitre are:
In principle, only enough thyroid tissue is removed to achieve the objective, but in multinodular goitre, recurrence is likely and best treatment is total thyroidectomy with lifetime thyroxine replacement.
Patients presenting for cosmetic reasons with moderate thyroid enlargement have often been treated with thyroxine. The theory is the gland may shrink to an acceptable size when TSH is suppressed. Unfortunately, clinical trials have shown this is ineffective. In hyperthyroidism caused by idiopathic thyroid hyperplasia, this is unresponsive to anti-thyroid drugs and ineffectively treated with radioiodine; hence surgery is required if treatment is needed.
Thyroid cysts are diagnosed as fluid-filled lesions on ultrasound or by aspiration. Cytology should be performed to exclude malignancy. Large or recurrent cysts are best treated surgically.
Embryology: The thyroid originates as a midline diverticulum between the first two branchial pouches. Its origin is represented in the adult by the foramen caecum, visible at the junction of the anterior two-thirds and the posterior third of the tongue. The thyroid diverticulum forms the thyroglossal duct which extends caudally through the developing tongue. It passes down in relation to the hyoid bone (in front of, through or behind it) to reach its normal position below the larynx. By this time, it has become a bilobed structure with the lobes connected by a narrow central isthmus. The thyroglossal duct later degenerates. The calcitonin-secreting C-cells originate from the ultimobranchial body of the fifth pouch.
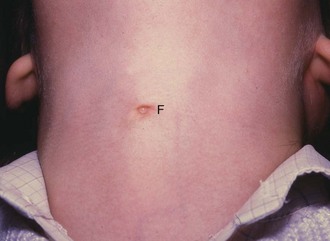
Thyroglossal cyst and ‘fistula’: Part of the thyroglossal duct may persist and become cystic. A thyroglossal cyst presents in children and occasionally adolescents as a smooth, rounded, midline swelling in the neck. Most thyroglossal cysts occur below the hyoid, although rarely they occur in the submental region. A diagnostic feature is that the cyst rises when the patient swallows or protrudes the tongue. Most thyroglossal cysts are asymptomatic but they are prone to inflammation which causes pain and swelling. If an inflamed cyst is surgically drained, it may become an intermittently discharging sinus, often incorrectly described as a thyroglossal fistula (Fig. 49.9).
Thyroglossal cysts are usually excised along with the thyroglossal tract up to the base of the tongue. This requires removing the middle third of the hyoid bone (Sistrunk's operation). A persistent sinus or a recurrent cyst is likely to complicate incomplete excision.
Ectopic thyroid tissue: An ectopic thyroid is a rare congenital abnormality resulting from interruption of normal descent. It may present like a thyroglossal cyst or as a lump in the tongue. As this may be the patient's only thyroid tissue, isotope scanning should check if there is thyroid tissue in the normal position before proceeding to excision.
Disorders of parathyroid glands
Hyperparathyroidism is characterised by excessive secretion of PTH, a polypeptide hormone containing 84 amino acids. Primary hyperparathyroidism (PHPT) is caused by excessive production. It usually occurs in adults and is slightly more common in females. Increased parathormone increases osteoclastic activity, causing reduced bone density and hypercalcaemia. Many cases remain undetected but estimates from ‘routine’ calcium estimations suggest that about 1% of the adult population has primary hyperparathyroidism. About 80% of these are due to benign parathyroid adenoma. Most of the rest are due to hyperplasia of multiple parathyroid glands and less than 1% are due to parathyroid cancer.
Symptoms and signs
Hyperparathyroidism is the most common clinical disorder of the parathyroids. Patients are usually referred to a surgeon after discovery of hypercalcaemia during investigation of musculoskeletal pain or recurrent urinary tract calculi. About half the affected people are likely to have the classical clinical features of hypercalcaemia in addition to non-specific muscle weakness, thirst, polyuria, anorexia, weight loss and constipation. Classical features of hypercalcaemia are bone pain (sometimes with radiological changes of osteomalacia or osteitis fibrosa cystica), urinary tract stones, abdominal pain (caused by peptic ulcer or recurrent pancreatitis), and mental changes such as confusion, depression or even psychosis. These can be remembered by the aide-mémoire bones, stones, abdominal groans and psychic moans.
In multiple endocrine neoplasia type I (MEN I), primary hyperparathyroidism may be associated with other hyperplastic endocrine disorders such as pancreatic islet cell tumours secreting insulin or gastrin or pituitary tumours. In MEN II, it may be associated with medullary carcinoma of the thyroid and/or phaeochromocytomas.
Hypercalcaemia is frequently found incidentally on biochemical screening and if patients have raised parathormone levels, hyperparathyroidism can be diagnosed. Many of these apparently asymptomatic patients turn out to have suffered non-specific fatigue and malaise for years or have signs of hypertension or renal failure.
Secondary hyperparathyroidism occurs in renal failure and vitamin D deficiency (see below). In addition to osteomalacia and osteitis fibrosa cystica, these patients also develop ectopic calcification, for example around joints and in arteries.
Raised plasma calcium levels cannot be tolerated for long without causing serious systemic problems or damage to bone. From Figure 49.10, it might seem paradoxical that urinary tract calculi are a common presenting feature of hyperparathyroidism, since parathormone reduces urinary calcium excretion. The probable reason for stone formation is the excess phosphate excretion. This is associated with increased urinary alkalinity, which predisposes to precipitation of calcium salts.
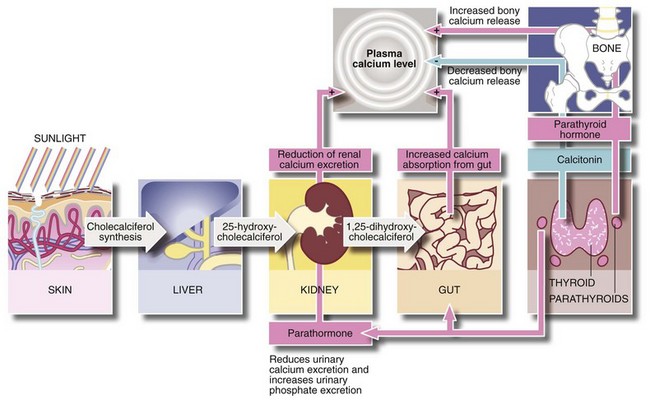
Control of plasma calcium (Fig. 49.10)
The plasma calcium level is maintained within a very narrow range by the combined effects of parathormone and vitamin D. Parathormone secretion rate is governed directly by the plasma concentration of ionised calcium. If parathormone is overproduced, this raises the plasma calcium and causes phosphaturia, thereby decreasing serum phosphate.
Parathormone raises plasma calcium levels in the following ways:
• Increases osteoclastic activity and release of calcium from bone matrix, liberating calcium into the circulation
• Enhances renal tubular reabsorption of calcium and diminishes reabsorption of phosphate, thereby increasing the renal clearance of phosphate
• In the presence of vitamin D, it promotes calcium absorption from the small intestine
Vitamin D (as cholecalciferol) is produced by the action of sunlight on cholesterol derivatives in skin. Cholecalciferol is then converted to 25-hydroxycholecalciferol in the liver, and is further hydroxylated by the renal tubules to the active compound 1,25-dihydroxycholecalciferol. This active compound is required for intestinal absorption of calcium. Calcitonin, produced by C-cells of the thyroid gland, probably plays little part in normal calcium homeostasis.
Calcium homeostasis is thus dependent on normal functioning of parathyroids, liver and kidney, together with adequate dietary intake of calcium and suitable quantities of vitamin D from diet or exposure to sunlight.
Types of hyperparathyroidism
Hyperparathyroidism is classified as follows:
a: Single parathyroid adenoma The most common cause of primary hyperparathyroidism, found in 80% of cases. One of the four parathyroid glands becomes replaced by an enlarged benign neoplasm which secretes parathormone in excessive amounts. Secretion by the other parathyroids is suppressed.
Secondary and tertiary hyperparathyroidism: In secondary hyperparathyroidism, there is an abnormal chronic stimulus to parathormone production and the glands undergo diffuse hyperplasia. This occurs most often in chronic renal failure (including nearly all patients on dialysis to some degree) but also occurs in vitamin D deficiency. The altered calcium/phosphate physiology in chronic renal insufficiency includes:
• Damage to the glomerulus causing phosphate retention which leads to hyperphosphataemia
• Hyperphosphataemia inhibits calcium absorption by the gut, reducing absorption of calcium to a minimum
• Renal tubular injury leads to reduced renal production of 1,25-dihydroxycholecalciferol (1,25-DHCC)
• The low blood calcium causes the negative feedback system to increase elaboration of parathormone. This promotes osteoclastic activity, restoring calcium levels but causing the bone disorders of osteomalacia and osteitis fibrosa cystica
• The raised product of calcium and phosphate in the blood leads to ectopic calcification in abnormal sites
After renal transplantation, hyperparathyroidism may persist if the hypertrophied parathyroid glands fail to return to normal. The glands continue to over-secrete in an autonomous fashion with normal or even elevated serum calcium levels. This is described as tertiary hyperparathyroidism with clinical effects similar to secondary hyperparathyroidism.
Malignant hypercalcaemia
Hyperparathyroidism is only one cause of hypercalcaemia; the other main cause is malignant diseases. In 70%, this is due to secretion of parathormone-related protein (PTH-rP) and in the rest to widespread bone destruction from lytic bone metastases. The most common tumours to secrete PTH-rP are squamous cell carcinoma of lung, renal cell carcinoma and bladder cancer. Tumours causing hypercalcaemia by bone destruction include breast cancer, leukaemias and multiple myeloma.
Management of hyperparathyroidism
Corrected plasma calcium levels are elevated but precise diagnosis was difficult before immunoassay for parathormone (PTH). Modern techniques use polyclonal antibodies marked by radioactive, luminescent or enzyme labels to recognise the PTH molecule. Elevated plasma calcium and PTH levels confirm the diagnosis of hyperparathyroidism in virtually all patients who do not have renal failure or metastatic disease.
In primary hyperparathyroidism, an adenoma can often be identified by radioisotope scanning using sestamibi, which is 2-methoxy isobutyl isonitrile labelled with technetium-99m. This is taken up by thyroid and any active parathyroid tissue but persists longer in the parathyroid, enabling an adenoma or sometimes a carcinoma to be localised. Normal or even hyperplastic parathyroids are so small that they are not detected by this method. In practice, ultrasound is usually employed in addition. Diffuse hyperplasia is best dealt with by surgical exploration of the neck and examination of all four parathyroid glands. Preoperative localisation can also be valuable prior to re-exploratory operations for recurrent hypercalcaemia.
Surgical management: Surgery is the only definitive treatment for primary and tertiary hyperparathyroidism. Secondary hyperparathyroidism is managed by treating renal failure and giving phosphate absorbing agents, although parathyroidectomy may be necessary if there is severe bone resorption. Hypercalcaemia due to ectopic parathormone production is managed medically as it is rarely possible to resect a tumour secreting parathormone-like protein.
There are normally two pairs of parathyroid glands, superior and inferior on each side, lying close to the thyroid. The superior pair usually lie close to where the inferior thyroid artery enters, near the middle of the gland. The inferior pair are usually located below the lower poles of the thyroid or sometimes within the thymus gland retrosternally. They may be located elsewhere in a variety of sites including as low down as the aortic arch.
Parathyroid surgery is exacting and time-consuming, often interrupted by histological examination of frozen section biopsies during the operation. Surgical access is as for thyroidectomy. The likely anatomical position of each parathyroid is then meticulously explored. Although the parathyroids have a characteristic yellow-brown colour, they are often difficult to distinguish from thyroid, especially if the tissues have been traumatised.
If one of parathyroid gland is enlarged and the others are normal, the diagnosis is parathyroid adenoma or, rarely, adenocarcinoma. In either case, the abnormal gland is completely removed and the others left in situ. If an adenoma can be localised before operation, there is a trend to minimal surgery, simply removing the enlarged gland without exploring the rest of the neck.
If no individual gland is disproportionately enlarged, a diagnosis of diffuse hyperplasia is made. In this case, there is a trend towards total parathyroidectomy rather than incomplete removal, now that plasma calcium can be better controlled medically. Some surgeons remove three and a half glands, while still others remove all the parathyroid tissue and reimplant tissue in a forearm muscle pouch. If hyperparathyroidism persists, this parathyroid tissue is more readily removed than from the neck. The main problem in diffuse hyperplasia is that some parathyroid tissue may remain unidentified, however meticulous the surgery. In some units, plasma PTH is measured intraoperatively to ensure the operation is complete.
Complications of parathyroidectomy are similar to those of thyroid surgery (see Box 49.3 earlier). Hypoparathyroidism is more likely and plasma calcium must be carefully monitored in the early postoperative period and treated if abnormally low.
Hypoparathyroidism
The most common cause of hypoparathyroidism is surgical removal or devascularisation of the parathyroids during thyroid or parathyroid surgery. Autoimmune hypoparathyroidism also occurs occasionally.
Hypoparathyroidism presents clinically with the effects of hypocalcaemia. A fall in plasma calcium level increases neuromuscular excitability causing cramps or even tetany in severe cases. An early symptom is paraesthesia, especially around the lips. After thyroid or parathyroid operations, patients should be asked if they have experienced tingling around the mouth, and plasma calcium estimations should be performed the morning after operation, and 24 hours later.
Clinical tests for hypocalcaemia include tapping over the parotid gland. This provokes transient contraction of the facial muscles and is known as Chvostek's sign. A further test involves inflating a sphygmomanometer cuff on the upper arm to above systolic pressure. This induces carpal spasm within about 3 minutes (‘main d’accoucheur' or obstetrician's hand).
Early postoperative hypocalcaemia is treated with intravenous calcium gluconate. Persistent hypocalcaemia is controlled by oral administration of high doses of calcium and vitamin D.