Chapter 12 The physiotherapy management of inflammation, healing and repair
Introduction
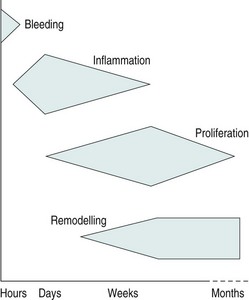
This chapter will introduce the reader to the processes involved in inflammation and tissue healing and repair, as well as discussing physiotherapeutic interventions that may be used to facilitate this process. The healing and repair process that occurs in response to tissue injury can, in broad terms, be described as a continuum of events that comprises of four stages: bleeding, inflammation, proliferation and remodelling.
These stages are not mutually exclusive and will overlap considerably, depending on the nature of the injury and the individual. However, for the purpose of this chapter, these four stages will be considered in sequence as underpinning a return to normal homeostasis and to normal function.
![]() Clinical note
Clinical note
The inflammatory and tissue repair processes are fundamental to many pathologies and injuries that are treated by physiotherapists. The treatment of the inflammation itself may be directly affected by physiotherapy modalities or may need to be treated primarily through drug and medical intervention. For example, the inflammation of the bronchioles in an acute exacerbation of asthma would be managed medically with corticosteroids.
Although inflammation and tissue repair are not exclusive to the musculoskeletal system it is in this system that the physiotherapist most closely works to influence these processes. This chapter will, therefore, focus on the sequence of events following soft tissue injury and its physiotherapeutic management. The aims of the chapter are as follows:
• to identify the aims of physiotherapy and how they change throughout the continuum of tissue healing and repair;
• to provide the reader with specific physiotherapy examples of managing inflammation and repair;
• to develop the reader’s ability to clinically reason the use of core physiotherapy modalities in the management of tissue healing and repair;
In order to clinically reason an appropriate physiotherapeutic approach to treatment for an individual’s problem, many factors need to be considered. The physiotherapist needs to understand the anatomical and histological make-up of the different tissues, as well as the normal processes of inflammation, tissue healing and repair. It is also vital that the physiotherapist has excellent assessment and clinical reasoning skills in order to correctly identify the tissues involved and the underlying pathology. The clinical reasoning process also requires the physiotherapist to consider psychological and social factors, which will undoubtedly influence an individual’s recovery and rehabilitation.
These factors may significantly alter the approach a clinician takes and maybe even exclude certain treatment modalities that would normally be considered. It is this individualised, holistic and evidence-based approach that makes the physiotherapist an invaluable contributor to the patient’s optimal recovery from disease or injury. The clinical reasoning process is illustrated in Figure 12.1.
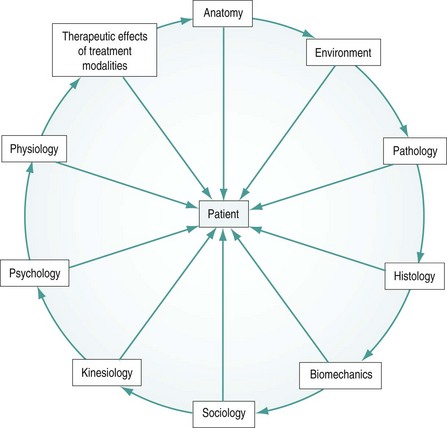
Figure 12.1 Factors influencing the clinical reasoning process for the management of patients’ tissue healing and repair.
Two case studies will be presented to illustrate the suggested application of physiotherapy interventions discussed in relation to the healing and repair processes.
The continuum of tissue healing and repair
When any soft tissue is injured, be it through trauma, injury, overuse or surgery, a natural sequence of events follows in order to repair the damaged tissue and restore homeostasis and normal function.
This process starts with a short period of tissue bleeding owing to the disruption of small blood vessels and capillaries. Immediately following this period of bleeding a complex cascade of biochemical events proceed, triggering an inflammatory reaction. The inflammatory process initiates the proliferation of new tissue cells, which eventually remodel with the aim of restoring normal tissue function. This sequence of events is illustrated in Figure 12.2.
This sequence of events does not take on exact timescales and it is useful to think of this as a continuum whereby each stage of healing will overlap with the next depending on many factors, such as the severity and nature of the injury, the patient’s age and tissue type and what the individual does or not do in terms of movement, activity and intervention. In many cases these healing processes occur without problems; however, several factors can cause this process to be delayed or exaggerated, leading to less than optimal tissue structure, pain and ultimately reduced function.
For many years physiotherapists have utilised a wide range of treatment modalities and interventions with the intention of promoting healing and repair. The main aim of using any physiotherapeutic modality or intervention should be to facilitate and progress tissue through this normal healing and repair continuum, thus facilitating early recovery and return to maximum function.
Soft tissue injury
When injury or trauma occurs producing forces necessary to damage soft tissues it is important to consider what happens to these tissues at a cellular level. The secondary injury model described by Merrick (2002) considers there to be two stages following tissue injury, namely the primary and secondary injury response:
• the primary injury is considered to be the damage to cells caused by the direct injury mechanism, be that a crush, contusion or strain force. The cells damaged by this mechanical force may have their cell membranes disrupted causing a loss in homeostasis and subsequent cell death. Many types of tissue may be involved, including ligament, tendon, muscle, nerve and connective tissues;
• secondary injury is thought to be caused by physiological responses to the initial primary injury. This occurs to tissues at the periphery of the injury to those cells not damaged by the primary injury. It is hypothesised that this damage may occur by two means. These are hypoxic (or maybe better described as ischaemic) and enzymatic mechanisms.
Ischaemic mechanisms
There are several proposed causes of ischaemia (reduced blood flow) to the damaged tissue, including haemorrhaging from blood vessels, increased blood viscosity secondary to inflammatory responses and increased extravascular pressure secondary to oedema. This reduced, or absent, blood supply will deprive cells which may have survived the primary injury of vital oxygen causing them to rely on the anaerobic energy systems which only have a short timescale (possibly up to six hours). If the ischaemia prolongs, many of these cells will subsequently die.
Phases 1 and 2 of tissue healing and repair
Phase 1: bleeding (0–10 hours)
This is a relatively short phase that will depend upon the initial injury type, the tissues damaged and the severity of injury. If there has been an injury to soft tissues some degree of bleeding will occur. When capillaries and small blood vessels sustain primary injury, blood will escape into surrounding tissues and, depending on the location, may gradually track distally as a result of gravity. The type of tissue involved and the type of injury will determine the degree of bleeding in terms of amount and duration. If very vascular tissue is damaged (e.g. muscle) a larger amount of bleeding will occur in comparison with less vascular tissues, for example ligament and tendon. The bleeding phase may only last a period of a few minutes or hours, but in large muscle contusion injuries, for example, bleeding may continue to a small degree for up to 24 hours (Watson 2004).
![]() Clinical note
Clinical note
When assessing bleeding it is also worth considering the location of the injury, as this will affect where the bleeding distributes. For example, with a tear of the anterior cruciate ligament the bleeding will be intracapsular in the knee and is unlikely to present as obvious bleeding and bruising with discolouration but as a tense swelling which, if aspirated, could be identified as blood causing a haemarthrosis.
Phase 2: inflammation (0–4 days)
Inflammation is a complex biochemical and cellular process which is still not fully understood. It can be triggered by many factors other than injury, such as infection and pathology.
Following an injury or pathological process there is an immediate inflammatory response. Scott et al. (2004) describe inflammation as a complex process that can be viewed at four levels: clinical, physiological, cellular and molecular, and suggest that it is the application of clinical reasoning skills that allows us to define which level is relevant in any given situation. Discussion of the complex biochemical sequences involved in the inflammatory process are beyond the scope of this chapter – the reader is referred to the wealth of books which discuss these biochemical and pathological aspects in more detail.
The inflammatory response has been reported to last for several days, or even weeks, but usually peaks around 2–3 days post-injury. During this inflammatory phase there may well be several clinical features evident. These include redness, swelling, pain and loss of function. During inflammation there is primarily a vascular and cellular response. The vascular response is a result of chemical inflammatory mediators and also a neural effect on the arterioles. There is an initial vasoconstriction that lasts only a period of seconds, followed by a more prolonged vasodilation response. There is also an increase in the permeability of the capillary walls allowing migration of large plasma proteins into the interstitial space. This alters the osmotic pressure in the tissue and exudate will gather in the interstitial space causing swelling. As cells migrate across the vessel wall into the interstitial fluid this will become cellular exudate. This exudate will contain mainly neutrophils initially and then lymphocytes and monocytes as the inflammatory process progresses (Mutsaers et al. 1997).
The cellular response is mediated and maintained by chemical mediators, which results in altered cellular activity. These processes will eventually aid the removal of any microorgansims and damaged tissue debris. Pain is caused by both irritation of damaged nerve endings from these chemical mediators and pressure on nocioceptors from the increase in exudate.
Often, clinically, this inflammatory phase is seen as a hindrance to the repair process and interventions that have an anti-inflammatory action are often employed with the aim of halting and slowing this process. It should be noted, however, that inflammation is, in fact, a normal response to injury and should be facilitated in order for the patient to progress through the healing and repair continuum.
![]() Clinical note
Clinical note
There is some debate as to whether non-steroidal anti-inflammatory drug (NSAID) therapy should be used in soft tissue injury as it may slow down this phase of tissue healing, thus slowing overall recovery. Alternatively, the suggestion is that if it controls the inflammatory response and prevents it becoming exaggerated or prolonged this may, in fact, facilitate progression through the healing continuum.
Occasionally, individuals will develop a prolonged or exaggerated inflammatory response that fails to resolve within the normal timeframes. The mechanisms behind the development of chronic inflammation are not yet fully understood and are beyond the scope of this chapter.
Physiotherapy interventions in phases 1 and 2 (0–72 hours post-injury)
When considering the physiotherapy approaches that we can employ at these early stages of tissue injury, we must consider the physiological processes occurring and the aims and physiological responses to treatment.
When treating any patient with an acute injury, for example a ligament sprain or a muscle contusion, the aims of treatment must be decided in specific relation to the individual, in order to plan treatment accordingly.
General physiotherapy aims of early phase management (phases 1 and 2)
• to limit and reduce inflammatory exudates;
• to reduce metabolic demands of tissue;
• to protect newly damaged tissue from further injury;
• to protect the newly-forming tissue from disruption;
• to promote new tissue growth and fibre realignment;
• to maintain general levels of cardiovascular and musculoskeletal fitness/activity.
The PRICE principles
PRICE is a mnemonic for the principal interventions commonly used in the immediate early stages following tissue injury. PRICE stands for :
These interventions together are applied in principle to address the seven aims of early phase tissue injury and healing management. These interventions are discussed below. The reader is also referred to the guidelines written in conjunction with the Association of Chartered Physiotherapists in Sports Medicine (ACPSM), on the immediate management of soft tissue injury using the PRICE principles (Bleakley et al. 2010).
Protection
When soft tissue injury has just occurred it is important to protect tissues from further damage, both chemical and mechanical (secondary), and also to protect newly forming collagen fibrils in the following days. Measures to prevent tissues from this further mechanical damage are generally described as protective modalities and may include treatments such as strapping, use of crutches, slings and braces, and modification of exercises and movements.
Strapping
There are various techniques of strapping that can be applied in the early stages to protect injured areas from further damage while allowing the individual to continue with other activities and exercise. When deciding on the use of a strapping technique it is important to consider the structure(s) damaged and the movement(s) which are likely to stress the damaged area. Strapping can be applied in a manner to allow maximal movement while protecting from the movement(s) likely to cause further damage. Again, this emphasises why it is essential that the physiotherapist has a detailed knowledge of anatomy and human movement when treating injured and healing tissues.
It is important to remember that any strapping applied in these early stages must be able to accommodate a change in size or circumference because of swelling, to prevent compromise of the circulatory system. Often compression bandaging (as discussed below) will alone restrict movement and may be sufficient to protect from unwanted movement. Alternatively, additional specific strapping may be applied to reinforce and prevent specific movement patterns.
![]() Clinical note
Clinical note
If someone has injured their anterior talofibular ligament in their ankle it will be necessary in these early stages to protect this structure from stresses into inversion and plantar flexion while allowing eversion and dorsiflexion movements. This can be achieved through accurate strapping.
Strapping needs to be reapplied regularly and also needs to be monitored regularly to ensure its safety and effectiveness. The physiotherapist will need to consider if the patient is able to reapply strapping independently or not, which may influence its use if the patient has limited contact with the physiotherapist.
The patient must also understand the limitations of the strapping. Some individuals may feel able to continue with all activities while wearing strapping when, in fact, this could be detrimental to the injured and surrounding tissues.
Other methods of protecting injured and healing tissues
The main factors affecting the physiotherapist’s decisions to use a protective device are the individual’s needs, the extent and nature of the tissue injury and the location of the damage. Devices such as slings may serve the purpose of elevating the limb while also having a protective role.
![]() Clinical note
Clinical note
In the case of a patient having had a fasciectomy for release of Dupuytren’s contracture, a splint is required immediately postoperatively to put the newly cut tissues under stress and encourage lengthening in order to prevent newly forming tissue from re-tightening, thus causing continued reduced function of the hand.
Walking aids
Walking aids will need to be provided if gait is altered. Also, partial weight-bearing may be advised in the early phases to protect damaged tissues, which will be stressed excessively during weight-bearing. Remember that the main aim of prescribing a walking aid is to promote a normal gait pattern within the limits of any restricted weight-bearing. This is essential to allow normal movement patterns of adjacent joints and body segments and to minimise any secondary problems.
Rest
Rest, in this context, usually refers to some form of relative rest in terms of general movement and activity to reduce metabolic demands and, hence, further secondary chemical damage to tissues. Rest from specific activities (relative rest) will also go some way towards protecting damaged and newly forming tissue.
However, it must be remembered that excessive unloading of the structures and prolonged rest can do harm to the patient so must be balanced carefully with appropriate activity (Bleakley et al. 2010). Therefore, the physiotherapist needs to carefully balance these protection and rest aims with those of promoting movement in order to maintain normal function of adjacent joints and structures.
In the very early stages (0–48 hours) when the tissues are still likely to be bleeding and the inflammatory process will be underway, the patient should be encouraged to rest the injured area fully to prevent increased bleeding and inflammatory response.
As this very early phase ends (around 48 hours), very gentle movement is needed to help improve circulation and removal of waste products, and to provide the necessary stresses for the correct alignment and orientation of newly forming tissue fibres. Both local and systemic exercise can assist in this process through changes in haemodynamics and lymphatic function (Bleakley et al. 2010).
This trade off between rest and activity can often form conflicting advice for the patient – the physiotherapist needs to ensure that advice regarding movement and activity is clearly understood by the patient for maximum benefit.
Again, it is worth remembering at this stage that effective physiotherapy practice is underpinned by firm clinical reasoning where individuals’ physical, social and psychological needs, their tissue damage and stage of healing are all considered in light of considered best practice in that treatment area.
![]() Clinical note
Clinical note
It is essential with both elite and recreational athletes that they are advised and managed in terms of maintaining cardiovascular fitness and musculoskeletal fitness. This may require the individual to do a reduced or non-weight-bearing activity/programme such as exercise in water or reduced impact activity, or activities that do not involve the affected area. Remember, athletes may be eager to restart activity prematurely and the physiotherapist must take an active role in ensuring the patient fully understands the implications of all activities on the likely outcome of their injury/problem.
Cryotherapy (ice therapy)
Cryotherapy is defined as the use of cold and cooling agents used for therapeutic benefits, and has long been considered an important part of early tissue injury management. There are various methods of cooling tissues including the application of crushed ice, ice/gel packs, cold compressive devices and ice submersion. The comparative effects of these have not been fully investigated and the method of application is still mainly determined by the nature of the injury, equipment variability and therapist preference. The use of cryotherapy has not been fully investigated in terms of scientific research and much of physiotherapy practice in this area is based upon experiential evidence.
The primary reason for applying ice in the immediate early injury management is to cool the affected tissues, hence reducing the metabolic demands of the neighbouring cells. This should enable more cells to survive the ischaemic phase, thus minimising secondary tissue damage. It is suggested that to maximise the therapeutic effects of cryotherapy, an optimal tissue temperature reduction of 10–15° is required (MacAuley 2001). If the application of cryotherapy can reduce the number of cells damaged overall, the healing and repair process will be quicker, hence speeding up return to function.
Traditionally, the application of cryotherapy may have been thought to induce vasoconstriction of the small blood vessels, thus reducing blood supply to the area and hence causing increased ischaemia to the tissues and further secondary damage as initially described by Knight (1989). Merrick (2002) suggests that the secondary injury model described above now better describes the effects of cryotherapy. It must be noted, however, that there is very little conclusive evidence that investigates how cryotherapy affects the metabolic processes and whether it can influence inflammation (Bleakley et al. 2010).
The duration, application and frequency of cooling to achieve maximum therapeutic benefits has not yet been determined scientifically, yet these factors will greatly affect the degree of tissue cooling. Not all modes of cooling are equally effective; however, crushed ice provides effective cooling and is probably the safest (Bleakley et al. 2010). Subcutaneous fat covering will insulate deeper tissues and thus limit cooling significantly. Therefore, some areas may require slightly longer cooling times. Other important points are that the cold application should cover the whole area of injured tissue and a damp towel should be placed between the cooling agent and the skin to avoid skin and tissue damage. Using a thick, dry protective layer is likely to significantly reduce the cooling effects. It is also worth noting that research suggests that deep tissue temperature stays the same or continues to cool for up to 10 minutes following removal of an ice pack (Bleakley et al. 2010).
The use of cryotherapy is widespread in practice and it is generally accepted that it is a very safe and easy-to-use modality, making it very popular. However, it is very important to remember that direct cold application can cause what are commonly described as ‘ice burns’. This may be described as superficial frostbite and the symptoms are similar to a thermal burn with pain, redness, swelling and blistering. It has been highlighted recently that ice burns are probably under-reported and are much more common than was previously thought. Remember to exercise caution when applying cryotherapy and reassess the patient regularly. If the patient has reduced sensation, or nerve injury is suspected, extreme caution must be used and it is advisable to avoid cryotherapy until this has been fully assessed.
Compression
Compression of the affected tissue and adjacent areas can also be used in the early phases to reduce exudate, protect tissues and possibly reduce pain.
The theory behind the application of compression is that the hydrostatic pressure of the interstitial fluid is raised, thus pushing fluid back into the lymph vessels and capillaries, and reducing the amount of fluid that can seep out into surrounding tissues (Rucinski et al. 1991). External compression through the application of an elastic wrap can stop bleeding, inhibit seepage into underlying tissue spaces and help disperse excess fluid (Thorsson et al. 1997).
Compression can be applied using a tubular bandage or some form of elasticated bandage strapping which may be adhesive or non-adhesive. It is vital that any product used is elasticated in order to accommodate changes in size or circumference of the body part without compromising circulation.
Compression can be used in direct conjunction with cryotherapy in the form of an ice compression device, for example Cryocuff, which allows simultaneous cooling and compression of tissues. If this method is not used there is generally some trade-off in terms of using cryotherapy and compression. It is not usually possible to sufficiently cool tissues through a compression bandage; therefore, intermittent use of cooling methods may be applied between compression.
Unfortunately, there are very few studies which look specifically at the effects of applying compression alone in acute soft tissue injury and, again, much of contemporary practice is based upon experiential evidence and consensus opinion (Bleakley et al. 2010).
![]() Clinical note
Clinical note
When applying compression you will need to consider the following points (Kerr et al. 1999).
1. Apply compression as soon as possible after injury.
2. Always apply compression from distally to proximally.
3. Where possible, apply the compression a minimum of six inches above and below the affected area.
4. Always follow the manufacturer’s instructions where available.
5. Do not apply compressive materials with the material at full stretch.
6. Ensure consistent overlap (half to two-thirds) of previous turn of compressive material.
7. Apply turns in a spiral fashion, never in a circumferential pattern.
8. Use protective padding, such as gauze, underwrap, foam, etc., over vulnerable areas such as superficial tendons and bony prominences.
9. Do not apply elasticated leggings in the lying position or in association with elevation.
10. Remove and reapply if the pressure appears not to be uniform or if the patient complains of discomfort. Otherwise, reapply within 24 hours.
11. Continue compression for first 48 hours when not lying down.
12. Always check the distal areas following compression to check for diminished circulation, i.e. colour changes or cold.
Elevation
Another treatment method aimed at reducing bleeding, swelling and, thus, pain in acutely injured soft tissues is elevation. Some studies have suggested that elevating the injured limb above the level of the heart reduces inter-arterial pressure and enhances draining of extravascular fluid away from the area; however, scientific evidence supporting this is minimal.
It is common practice to combine cryotherapy and compression with elevation in order to minimise swelling and gathering of interstitial fluid. However, continuously elevating the limb above the level of the heart is often impractical (especially if it is the lower limb) and may even compromise vascular supply to the body part if combined with compression. It may be more appropriate to advise the patient to elevate the affected limb intermittently during the day when possible and to remove compression at this time.
In the early stages a large amount of swelling is often evident if an individual with lower limb injury (particularly distal injury), stands and walks for a long time with the injured part in a dependent position. It would seem logical that if patients are advised to minimise the amount of standing and walking they do, and elevate the limb from the earliest point, this may reduce the accumulation of fluid which can quite quickly become thickened and fibrous owing to its high protein content. When an individual does stand and walk around then the use of compression would seem sensible to continue to minimise the accumulation of exudate in the surrounding tissues. One practical point to remember when advising elevation is to support the limb adequately during elevation through the use of pillows or a sling.
Again, evidence underpinning the use of elevation to promote healing and recovery is lacking and research often shows that improvements in swelling are short-lived and swelling often recurs when resuming gravity-dependent positions (Bleakley et al. 2010).
First-line management
Increasingly in modern physiotherapy practice the physiotherapist will be the first line of medical assessment, management and advice. This may occur, for example, in the sporting environment, in private practice or via direct access services. These roles require the physiotherapist to have excellent assessment skills and experience, and the understanding of differential diagnoses and indications for onward referral. Several guidelines are in place to aid clinicians in managing and diagnosing injuries, and using investigations such as radiology. Physiotherapists should be aware of these guidelines and implement them appropriately in order to promote best practice. For example, physiotherapists working in these settings should be familiar with the Ottawa guidelines for ankle injuries (Bachmann et al. 2003), which guide clinicians on when to X-ray the ankle to rule out fracture.
Applying the PRICE principles in practice
Having discussed the elements of the PRICE principles it is evident that there are sometimes conflicting demands and that it is often not possible or, indeed, appropriate to employ all five principles simultaneously. As discussed previously, the research evidence underpinning these interventions is insufficient and much of everyday practice is based upon historical approaches and consensus opinion (Bleakley et al. 2010). It is therefore important to consider this and the physiological processes occurring in the tissues when rationalising a treatment plan for an individual patient. It is also important to make realistic and reasoned treatment decisions considering all bio-psychosocial factors. This can be illustrated through the use of the case studies in this chapter.
Severity of injury and progression through the healing continuum
The speed of progress and recovery of those who have sustained soft tissue injury will vary depending on a large number of factors. These include the type, severity and location of injury, the individual’s tissue type and response to injury, and many extrinsic factors, such as their exposure to appropriate treatment and advice in the immediate stages, and any other psychosocial factors. For example, a minimal grade I ligament injury effectively managed in the early stages may move very quickly through the continuum of tissue injury to repair and remodelling within a few weeks, whereas major tissue injury induced through trauma or surgery may require a much longer process. Those individuals not having sought, or followed, advice and treatment in the early stages are more likely to develop problems such as chronic swelling, loss of range of movement and function in injured and adjacent structures, and may even have compromised the formation of appropriate new tissue.
In view of this it is desirable that individuals seek early advice from an appropriately trained professional and that they fully understand the advice and treatment approaches taken. Often, many of the treatment modalities discussed so far can be implemented by a patient independently at home and the frequency and accuracy by which they do this will have a large impact on their recovery and progress. It should, therefore, be ensured that physiotherapy intervention is focussed on establishing that the patient fully understands the advice and treatment approaches that will be implemented at home, especially if the frequency of physiotherapy contact will be limited. If the patient does not fully understand the advice given and instructions regarding their activities at home then any benefit gained from a physiotherapy treatment session will be undermined by the patient’s behaviour in the intervening period.
When deciding how long to continue to apply these principles consideration of the severity and size of the injured area is required. Despite common descriptions of grades of muscle and ligament injury being used, it is impossible to determine this accurately without radiological investigation such as ultrasound imaging. This is an area of increasing research; however, its clinical relevance in the management of muscle injuries is still under debate. Without the aid of valid and reliable imaging it would seem sensible to use the patient’s level of pain and possible gentle palpation to indicate the size of injury as indicators of when to progress rehabilitation.
As discussed earlier, it is often suggested to consider beginning early movement of the injured part at around 72 hours post-injury as initial pain is reducing, and progressing to gradually achieve full range of movement of the affected tissues before moving on to increase normal muscle power, strength, timing and proprioceptive control in light of the patient’s individual needs and abilities. In the early stages, acute pain is often a sign of further tissue injury and bleeding; thus, activity and movement of the injured area should be discouraged. However, as the continuum progresses, pain is often secondary to problems such as joint stiffness and lack of strength and control, and needs to be respected but not seen as a barrier to progressing rehabilitation. This will be discussed in detail in the following sections.
Phases 3 and 4: proliferation and remodelling
This section of the chapter deals specifically with the management of patients in the later stage of the healing and repair process. That is, beyond the initial bleeding and inflammation stages (the first 1–3 days following injury). Watson (2004) refers to these stages as the stages of proliferation and remodelling. The physiotherapeutic management of patients in these stages of the healing and repair process is still driven by the utilisation of physiotherapeutic measures which compliment, support and encourage these normal processes and therefore promote and facilitate repair. The underpinning reasoning behind physiotherapy in these stages of healing relates to the plastic properties of human tissue.
Plasticity in human tissue
Plasticity refers to a quality associated with being plastic, malleable, and capable of being shaped or formed (OED 2007). Although the term plasticity tends to be most frequently applied in the field of neurology it is important to recognise that it is a characteristic of all human tissue. Human tissues have the capacity to adapt to the nature and extent of the forces applied to them. For example, if we consider the practice of lifting weights. Over a period of time, within a progressive lifting programme, an individual will be able to progressively lift larger weights. The skeletal muscles and tendons loaded by lifting weights adapt over time as the individual progressively lifts more weight. These adaptations affect all components of the musculotendinous apparatus. The contractile component of the muscle gets larger and stronger (Kraemer and Ratamess, 2004) and capable of producing increased force.
In parallel with this process the non-contractile components get correspondingly stronger and thicker to accommodate the extra loading (Benjamin 2002). In addition, adaptations occur at the interface between the tendon and the bone so that the bony prominences also develop to withstand the increased force exerted. Consider an individual who suddenly lifts a weight or engages in an activity where the force generated with the musculotendinous apparatus exceeds that which the muscle, tendon or bone can withstand. In this situation the tissue fails to withstand the force applied and injury occurs. For example, excessive load generated in the quadriceps muscle may lead to muscle damage, patellar tendon damage or avulsion fracture of the tibial tubercle.
Human tissues undergo reversal of these adaptations during the periods of immobilisation or reduced activity which occur frequently following trauma. In these situations the effect of immobilisation causes the reverse of the processes identified above. This reduces the ability of the damaged tissues to withstand loading. Physiotherapeutic management of these patients focusses on trying to restore the affected tissues’ capacity to withstand normal loading therefore enabling the individual to return to normal function. It is important to remember that these soft tissue adaptation processes occur in both the injured and the uninjured tissues.
![]() Clinical note
Clinical note
A patient who sustains a severe second degree injury to the lateral ligament complex at the ankle and who subsequently has to non-weight-bear will experience soft tissue changes throughout the non-weight-bearing leg, not just in the tissues directly affected by the trauma.
Physiotherapeutic approaches are therefore fundamentally aimed at capitalising on this plastic property of human tissue so that therapy works alongside, and enhances, the normal healing and repair processes.
Factors influencing the rate of healing in the stages of proliferation and remodelling
An important consideration is that the processes of tissue proliferation and remodelling take place over significant periods of time (Watson 2004). The period of time for the completion of these pathophysiological processes can run into years and is dependent on a number of factors including:
• severity of initial trauma, e.g. a severe second-degree ligament sprain of the lateral ligament complex at the ankle will have a more prolonged proliferation and remodelling period than a first degree ligament sprain affecting the same structure;
• early management where the approach taken has laid the necessary foundations for proliferation and repair, e.g. an appropriate approach has been taken to rest/protect traumatised tissues (see earlier sections in this chapter). This has the potential to reduce the onset of chronic inflammation where an agent is responsible for the ongoing irritation of an injury and therefore perpetuates the period of the stages of bleeding and inflammation;
• tissue vascularity, e.g. skeletal muscle, which is highly vascular, has more potential for repair than a relatively avascular tendon;
• age, e.g. a similar grade of injury is likely to take longer in the repair process in an older individual than one who is younger (Myer 2000);
• nutrition – adequate nutrition (also related to blood flow) is required for healing to take place;
• medication, e.g. NSAIDs and steroidal drugs slow down proliferation and remodelling processes;
• appropriate loading of healing tissue during rehabilitation.
It is very important that the physiotherapist has a depth of understanding of the pathophysiological processes involved in proliferation and remodelling, as well as the clinical reasoning skills required to make the appropriate professional decisions. In addition to this knowledge, the ability to apply this knowledge of the clinical effects of a number of physiotherapeutic treatment modalities, as well as the psychological and sociological theory in order that treatments are effective, is also required. In this section, short case studies will be used to illustrate the main points.
Evans (1980) simplified these processes in his ‘graphs of hours’, ‘graphs of days’ and ‘graphs of months’. Although dated, this timeframe serves as a useful timeline against which to make judgements about physiotherapy approaches. An understanding of the timeframes involved in this continuum enables the physiotherapist to coordinate his/her approach to treatment and capitalise on the normal healing processes while ensuring that physiotherapy intervention does not induce further trauma and therefore delay healing and repair.
Phase 3: tissue proliferation (fibrous repair) (1–10+ days post-injury)
Pathophysiology
Cellular processes during this stage include:
• angiogenesis (formation of new blood vessels);
• proliferation of fibroblasts;
• production of collagen fibres (initially these are produced in an unordered and random fashion);
As the initial processes of inflammation begin to lessen, the inflammatory exudate begins to be absorbed. This leads to a decrease in swelling. Pain is reduced as a result. An increase in swelling during this stage is usually indicative of a more severe injury. Alternatively, this may be a result of inappropriate early management, for example a patient who has sustained a severe second-degree sprain of the lateral ligament complex at the ankle joint returns to full weight-bearing activity before the injured tissue strength has developed to a point where it is capable of withstanding the forces that walking demands of it. Tissue proliferation begins to occur as early as 24 hours after trauma. This proliferation begins the stage of fibrous repair, which usually involves the production of scar (collagen) material. The nature of the tissue, which is produced in the proliferation phase, is dependent on which elements of the tissues are damaged initially. If the cellular framework (satellite cells) is not damaged then regeneration of these cells may be possible. If the cellular framework (satellite cells) is destroyed then the tissue is replaced by scar tissue. In addition, if the cells damaged have no capacity to regenerate because they are deemed to be permanent cells, for example nerve cell bodies and cardiac muscle, then scarring definitely occurs. Scar tissue is a non-differentiated form of fibrous tissue that may develop some properties of the original tissue but will not function in the same way as the normal tissue would. By 2–3 weeks after the injury the majority of the scar tissue is in place. After this time, the rate of proliferation diminishes but may continue for several months following the injury. There is no hard and fast rule about exactly when this occurs, as the timeframe will vary in accordance with the factors that influence repair identified at the beginning of this section, for example it will occur earlier in vascular tissues.
Around 3–4 days following trauma the process of cell death will be complete and this means that the physiotherapist can assess the injury more objectively. At this stage the risk of aggravating/increasing the trauma or identifying false-positive findings because the patient’s pain is masking the real symptoms is reduced. It is at this point that the physiotherapist can begin to use therapeutic techniques that promote an increase in circulation and tissue temperature without fear of inducing further tissue damage or further bleeding.
General physiotherapy aims in the tissue proliferation stage – phase 3
At this stage in the repair process the aims of physiotherapy may include the following:
• decreasing local temperature;
• increasing range of movement;
• maintaining/increasing muscle strength/timing and control;
The above represents an approach to a treatment that is impairment focussed and biomedical in approach. It is essential that this generic approach be modified to reflect the individual nuances of each patient and their individual and specific psychosocial needs. For example, increasing range of movement and improving function could be joined into one function-specific, patient-centred aim, for example ‘to able to tie own shoelaces’.
Physiotherapy in the tissue proliferation stage (1–10+ days post-injury)
In this tissue proliferation stage physiotherapeutic treatment approaches are aimed at the achievement of the goals as identified above by influencing the pathophysiological processes involved in this stage of healing and repair. While approaches to physiotherapy to address the first four aims have largely been covered in the earlier parts of this chapter when considering the management of the bleeding and inflammation stages of the healing and repair continuum these are still worthy of a mention here. In order to reduce pain the injury may require a degree of ongoing protection, such as limiting movement to that which is pain free. However, the degree of protection will slowly be reduced throughout this stage.
Use of cryotherapy at this stage
Cryotherapy can continue to be utilised if the area injured continues to have an elevated temperature. However, it is likely that this will probably only be required at this stage in more severe injuries. Often at this stage the physiotherapist might choose to apply cryotherapy at the conclusion of a treatment session. The clinical reasoning underpinning this is that during this stage the potential to cause minor bleeding and inflammation as a result of treatment is high owing to the frail and vulnerable nature of the newly developing tissue. Cryotherapy applied at the end of treatment can potentially minimise the risk of this occurring.
Prescribing activity and exercise in the proliferative stage
During this proliferative stage the main input by the physiotherapist is to encourage a graded return to exercise and activity. This is achieved through the prescription of a specific exercise programme tailored to each individual patient’s needs. This type of approach that involves active involvement of the patient is valuable as it promotes patient empowerment and prevents the patient from taking a passive approach to treatment.
The aims of increasing range of movement, maintaining/increasing muscle strength/timing/control, preventing soft tissue adaptation in non-injured tissues and improving function are all best achieved through application of graded exercise and activity. Inevitably, function will be improved to some extent by activity to increase range, increase muscle strength and prevent soft tissue adaptation. However, it is important that functional activities that are specifically pertinent to the individual are targeted specifically within an individual’s treatment programme as early as possible, for example increasing ankle range of movement is unlikely to produce a direct improvement in walking performance without a specific rehabilitation activity aimed at improving walking. The primary emphasis of activity and exercise in this proliferative phase is to increase range of joint movement.
Grading the level of activity
Ensuring that any activity undertaken by the patient early in the proliferative stage is completed within pain-free limits provides a mechanism to protect newly developing tissues and prevent further secondary damage to those tissues initially traumatised at the time of the injury. It is sensible throughout this proliferative stage of healing and repair to use the patient pain report during activity as an indicator of appropriate levels of activity and exercise. As a rule, any activity or exercise prescribed in the proliferative phase that provokes pain, which could be classified with a high SIN (pain severity, irritability and nature) factor should be avoided.
From around the second day post-injury, fibroblasts are increasingly prevalent around the site of the trauma. These are the precursors to the formation of new fibrous tissue that will enable the healing process. In the proliferative phase, it is inappropriate to do aggressive activities or exercises of the areas directly affected by the trauma, as this will only serve to further damage the newly developing tissue. The use of gentle, active movements controlled by the patient within the pain-free range is appropriate at this stage – they will stimulate fibroblast activity and promote the production of collagen tissue. This is an example of the plasticity described earlier in the chapter.
![]() Clinical note
Clinical note
Caution is needed with some injuries in the proliferative stage so that the movements produced do not promote calcification within the associated soft tissues, for example following quadriceps contusion, so called ‘dead leg’ (haematoma of the thigh). In dead leg, the quadriceps muscle is crushed against the femur by a direct blow. This injury commonly causes damage to the periosteum of the femur, which causes osteoblasts to move into the overlying soft tissues (quadriceps). Overly aggressive early movement can promote osteoblastic activity within the muscle, which may develop into myositis ossificans.
A large observed difference in uninjured–injured knee range immediately post-injury and being unable to play on following injury are both key early indicators of myositis ossificans developing as a likely complication (Alonson et al. 2000).
Beyond the fourth day post-injury, proliferation of new, developed collagen tissue begins to accelerate thereby strengthening the healing of the injured tissue. As a result of this, increasingly greater ranges of pain-free movement can be expected. The physiotherapist needs to encourage their patients to practise these movements frequently throughout the day. Taking the movements to their pain-free limit will begin to progressively load the newly developing tissues and will facilitate an inbuilt progression of activity because as the pain eases progressively more range of movement will be achievable. This will promote the further formation and alignment of collagen and hence promote repair and the development of a functional scar (Watson 2004). However, care must continue to be taken, as during this phase any excessive loading still has the potential to damage the newly-formed tissue thereby provoking further injury and delaying the repair process.
Range of movement exercises will contribute to the maintenance of muscle strength and promote tissue-loading, but during this stage it is normal practice to limit the amount of overt strengthening/timing/control exercise recommended to the patient until full, non-weight-bearing pain-free active and passive ranges of movement are achieved. The use of isometric contractions involving structures not directly affected by the injury can be commenced early in the process.
![]() Clinical note
Clinical note
A patient with a severe second-degree sprain of the lateral complex of the ankle can safely exercise the knee and thigh area during the proliferative stage. The degree to which the muscles of the thigh can be loaded may be influenced by the ability of the patient to weight-bear.
Other available physiotherapeutic techniques suitable at this stage include reciprocal inhibition. This can be useful to increase range of movement and increase tissue length (Waddington 1976). Reciprocal inhibition is the physiological phenomena which occurs when a skeletal muscle (antagonist) contracts and the opposing muscle (antagonist) relaxes. These techniques can be useful when trying to encourage elongation of the musculotendinous apparatus. Their main use is when muscle tension or muscle spasm is identified as the reason for limited range of motion.
![]() Clinical note
Clinical note
A person with a grade 2 hamstring injury that occurred six days ago is likely to be at the stage where some encouragement of increasing length in the hamstrings is desirable to load the newly forming collagen tissue in order to promote further proliferation and repair. In clinical practice this is often difficult owing to protective muscle spasm in the affected hamstring group. Reciprocal inhibition whereby active contraction/shortening of the quadriceps group is used to induce relaxation and lengthening in the hamstrings can be used. This can be achieved by placing the individual on their unaffected side, fixing the hip of the affected leg in 40 degrees of flexion (thereby ensuring minimal stretch on the hamstrings over the hip joint), moving the knee into extension until slight stretch in the hamstrings is felt and then providing isometric resistance to the quadriceps. As this resistance is applied to the quadriceps, the opposing muscle group (hamstrings) relaxes reciprocally and allows further elongation. This provides a load to the newly forming fibrous tissue and therefore facilitates repair. The skill in this technique is in ensuring that the lengthening achieved in the hamstrings is slow and controlled. In addition, undue pain in the hamstring group should not be provoked by this technique.
Very gentle passive static stretching of affected tissues can begin at this stage as long as precautions are taken not to be over zealous. Again, the patient’s pain report is the main indicator of the amount of stretch that it is safe to apply. Ballistic stretching would not be advocated at this stage, as the potential to overstretch the newly forming tissues and reinjure while performing this technique is high.
As the tissues continue to proliferate, more fibrous tissue is laid down and the healing tissues begin to get stronger. During this time corresponding increases in the forces applied to the tissues can be made by increasing the force of stretch applied, increasing the range of movement produced and increasing the number of repetitions of any activity.
As a progressively greater load is applied to newly forming fibrous tissue it begins to remodel in response to the increasing forces applied. In addition, it is proposed that the haphazard arrangement of collagen laid down in the early healing stages begins to take on a more organised pattern as load is applied to it. The collagen fibres begin to align themselves along the lines of the stress. It is important, therefore, that the stresses applied to newly forming tissue are directed along the functional lines of stress normally required by that tissue. This requires the physiotherapist to apply their anatomical knowledge in an effective way.
From about the sixth day post-injury onwards there are increasing amounts of fibrous tissue laid down and, correspondingly, increasing levels of activity can be promoted. Tissues should be stressed progressively. It is considered to be both safe and advantageous to warm-up the affected tissues prior to activity – this has the effect of reducing the amount of load required to stress the tissues (compared with cold tissue) and therefore the tissue can be stressed more safely.
Electrotherapy in tissue healing and repair
The use of electrotherapy in the healing and repair processes has long been discussed and, again, there is varied evidence to support or discount the use of modalities such as ultrasound (US), pulsed electromagnetic energy and laser therapy in facilitating these processes. Electrotherapy as a topic is very large and this chapter does not claim to fully address all the literature and physiology surrounding it. The reader is referred to the electrotherapy chapter and other texts and literature for further information and discussion of these topics.
The most common electrotherapy modalities that appear to have the potential to have a direct action on the tissue repair process are US, pulsed shortwave diathermy (PSWD) and laser therapy. There is substantial evidence to support the notion that these modalities all have the capacity to influence the normal physiological processes of tissue repair, particularly the early inflammatory stage; however, clinical trials that demonstrate their efficacy in the clinical situation are lacking.
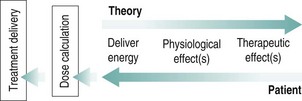
Watson (2006) describes a simple model of electrotherapy (Figure 12.3). This model summarises that the machine-generated energy in one form or another is delivered to the tissue. This energy is then absorbed by the tissue (to varying degrees depending on type), which then results in a change in one or more physiological events. It is the result of the energy being absorbed by the tissues resulting in a physiological shift, which is referred to as the therapeutic effect.
Choosing when and how to use electrotherapy?
Like any modality such as manual therapy, exercise or drug therapy there is an optimal time to apply it and appropriate dosage or intensity.
Watson (2006) suggests that the clinical reasoning process behind the use of electrotherapy can be illustrated by working through a reversal of the model shown (Figure 12.3).
Starting with the patient and knowing their identified physiotherapy problems and stage of healing and repair, the clinician can now work out what physiological effect is required and on what type of tissue. Once this is known the appropriate modality can be chosen based on the best available evidence. It must be remembered that if there is no electrotherapy modality suitable to achieve the desired result then electrotherapy has no place in the management of this condition at this particular time (Watson 2006).
Research suggests that it is the dosage applied and the specific tissue type that appears to most greatly influence this physiological shift. Studies have shown that different modalities applied at different dosages can have very different physiological effects. There does not yet seem to be an optimal dosage identified for any of these modalities for specific tissue types, thus making it difficult for the clinician to fully justify their choice in dosage.
In the proliferation stage it may be appropriate to continue to apply electrotherapeutic modalities, again ensuring that this is only used when an appropriate therapeutic window for the modality selected exists. During this phase of tissue proliferation the processes of phagocytosis, fibroblast and myofibroblast proliferation, and protein synthesis are prevalent. These processes can be therapeutically enhanced by the use of US, laser or PSWD. All of these modalities have the potential if selected appropriately (i.e. related to their specific tissue absorption properties), applied at the appropriate time and at an appropriate dose to exert a pro-proliferative effect whereby collagen synthesis is enhanced. This enables a speeding up of the proliferative phase and can therefore facilitate the rehabilitation process.
Phase 4: tissue remodelling (10 days + post-injury)
Pathophysiology
Key processes involved in the phase of tissue remodelling are:
• ongoing fibroblast activity and collagen production (usually peaking 2–3 weeks following injury);
• absorption of older fibrous tissue;
• deposition of new fibrous tissue;
• type III collagen fibres being replaced by type I collagen fibres.
You must remember that the different phases of the healing and repair process do not occur in perfect sequence. The phase of tissue remodelling and soft tissue contraction overlaps significantly with the earlier proliferation phase (see Figure 12.2). Remember that the peak of fibrous tissue repair occurs 2–3 weeks after the injury and the whole healing process is a dynamic one as older fibrous tissue is removed and new scar tissue is laid down. The continued application of physical stress to the developing tissues is one of the most significant factors influencing this phase of the repair process. The newly laid down fibrous tissue becomes ‘more organised’, being arranged less randomly and beginning to orientate itself along the lines of stress, thus enabling them to function more normally. This is the beginning of the remodelling phase which can continue for months and, possibly, for more than a year. It is clear, therefore, that this process continues long after the noticeable healing process and definitely beyond the time in which the patient would be in direct contact with the physiotherapist within the active rehabilitation process. This means that it is important that therapy, usually in the form of activity and exercise, continues long after an individual has been discharged from the ongoing care of the physiotherapist. Some evidence shows that even at this stage remodelling is still ongoing and tissues have not returned to their full functional capacity. Research in anterior cruciate ligament repair in monkeys indicated that the repaired anterior cruciate ligament reached 56%, 76% and 96% of its normal tensile strength 6 weeks, 12 weeks and 24 weeks after repair respectively. While this extent of remodelling may be acceptable in some members of the population it may not be so in others.
A key feature of the remodelling phase is soft tissue contraction. This is a process by which the newly formed tissues begin to physically shorten. This process has the potential for the healing tissues to begin to restrict and limit mobility and range of movement in the affected tissue. This process of soft tissue contraction begins to occur around the third week post-injury and continues long into the remodelling phase. As this process continues long after a patient would normally be discharged by the therapist, it is a key influence on the nature of the ongoing prescription of activity and exercise given to patients following discharge.
![]() Clinical note
Clinical note
The potential for tissue reinjury during the process of soft tissue contraction is clear. Failure to address this and plan activity and exercises strategies to avoid it is a potential key influence on reinjury patterns.
This phase of remodelling process takes place following the proliferative phase and is referred to as the chronic stage in some texts. Within this chapter, this phase is seen as a natural progression following the proliferative stage in an uncomplicated process of proliferation and remodelling.
General physiotherapy aims in the remodelling stage (phase 4)
The aims of physiotherapy in the remodelling stage may include any, or all, of the following:
Physiotherapy in the remodelling phase (Phase 4)
These aims can be related to the ongoing pathophysiological processes involved. Fibroblastic activity increases and new collagen fibres continue to be laid down. This process peaks around 2–3 weeks post-injury, continues through to 4–6 weeks following injury and is clearly extended beyond this timeframe in more severe injuries. Ongoing attention to progressive activities started in days 3–10 post-injury is required. The purpose of the physiotherapeutic treatment is to promote movement and mobility of the injured structures/tissues.
Preventing tissue contraction and adhesion formation
Beginning around the third week post-injury the healing scar tissue begins to undergo a process known as soft tissue contraction. This means that the physical length of the tissue actually begins to get shorter. Consider this in the case of a hamstring injury as described above. At the same time that you are working with the patient therapeutically to lengthen the hamstrings the remodelling tissue begins to cause the healing scar tissues to shorten. This is a process that can go on for a considerable period of time after the injury. At this stage, it is normal for the patient to experience some discomfort during end-range stretching activity.
![]() Clinical note
Clinical note
In practice this means that end of range stretching should commence on the third week following injury and should continue until the scar tissue contracture process is completed. The reality of this is that this is a very long-term process which may need to continue for as long as the remodelling process goes on. As indicated earlier this may be in excess of a year.
Contractures can sometimes become permanent. In these cases it becomes impossible to stretch the scar tissue. This is known as fixed contracture. Fixed contractures develop when the normal connective tissues (which are elastic) are replaced by fibrous tissue (which is inelastic). This means that the tissue will not stretch and this prevents normal movement. Contractures can occur in any tissue. The key to preventing the development of fixed contractures lies in ongoing therapeutic exercise and activity aimed at ensuring that as the scar tissue forms it remains a mobile, functionally-able structure. At the end of the remodelling stage the injured soft tissue will be repaired by scar tissue. The desired outcome is that this final scar is able to be a functional replacement for the tissues initially injured.
A potential problem during the remodelling phase is the formation of soft tissue adhesions. This is where newly forming fibrous tissue has been produced between adjacent layers of tissue such that these layers become bound together. These adhesions, when formed, can severely limit movement and soft tissue function. Normal movement requires that adjacent layers of tissue are able to move independently, for example a tendon moves over a bony surface or beneath a fascial band such as retinacula while the bone/retinacula stays still. As the formation of fibrous tissue during the proliferation phase is completely random, the potential for the development of adhesions is real. Movement in the early stages of healing and repair helps to ensure that the newly forming tissues do not create these adhesions. In some healing processes, where long periods of immobility are part of the patient management, their formation is probably inevitable. Soft tissue adhesions are normally easily palpable – tissues feel thickened and immobile to soft tissue palpation and mobilisation.
![]() Clinical note
Clinical note
It is worth considering what happens in the soft issue repair processes following fracture, for example a patient sustaining a fracture of the distal radius is normally immobilised within 6–8 hours of the fracture in a plaster cast, which remains in place for a minimum of four weeks. During this time the normal soft tissue repair phases of bleeding, inflammation, proliferation and some remodelling all occur while the arm is immobilised. During this time, the tissues are not subject to any of the beneficial loading described in this chapter. When the plaster is removed, improving mobility and range of movement in the tissues can take significant periods of time.
Passive and accessory mobilisation techniques
Other techniques aimed at restoring full working/functional length in tissues include passive and accessory movement techniques. The application of these demands the use of an in-depth knowledge of human anatomy. This means that the physiotherapist can select the appropriate techniques to attempt to influence a specific structure.
Activity and exercise continue to play a key part in the physiotherapy management. A shift towards an activity and exercise programme placing more emphasis on improving muscle strength/timing/control is normally seen at this stage. It is important to consider all the ways in which the tissues in question are loaded during normal functional activity. This enables the physiotherapy programme to be tailored appropriately to an individual’s need.
Muscle tissue will need to be able to withstand load from active and passive forces, from concentric, eccentric and isometric contractions at varying points within its range. It may need to work in an open-chain or closed-chain environment; it may need to function as an agonist, antagonist, synergist or fixator; it may need to generate strength, power or endurance. All of these factors must be considered when developing patient-specific exercise and activity programmes in the remodelling phase. Only when all of these things are considered and incorporated effectively into an exercise and activity programme is the potential for rehabilitation of individuals back to their full and maximum functional capacity realised.
The context of an individual’s normal functional activity is paramount to effective physiotherapy practice, whether it be playing a 90-minute game of football in the premiership or getting into and out of a car. The key skill that the physiotherapist utilises here is that of movement analysis. By analysing the demands of the activities that an individual aspires to be involved in, the physiotherapist is able to plan rehabilitation to meet individuals’ needs with the aim of maximising each individual’s capacity. Too often, in the author’s opinion, the lowest common denominator of functional ability is accepted. This becomes the norm and physiotherapeutic intervention fails to enable individuals to achieve their full potential.
![]() Clinical note
Clinical note
Returning a patient to full road-running function following a second degree sprain of the hamstring muscles requires full range of motion in the joints of the lumbar spine, hip and knee, appropriate muscle control of the leg musculature (a combination of concentric, eccentric and isometric contractions), the ability to run at different speeds on different surfaces (including inclines) and to varying distances. All of these aspects must be covered in the final rehabilitation programme if the individual is to reach their maximum potential.
![]() Clinical note
Clinical note
Returning a patient to playing rugby following a dislocated shoulder requires an analysis not only of the demands of rugby per se but also an analysis of the specific position that a player may take on the field. They need to be able to throw and catch while running, to be able to run with the ball, and to tackle and be tackled. In addition, they will need to be able to withstand a direct fall onto the affected arm.
![]() Clinical note
Clinical note
A window cleaner returning to work after a second degree sprain of the lateral ligament complex of the ankle requires full range of motion in the joints of the ankle complex and foot, appropriate muscle control of lower leg musculature (a combination of concentric, eccentric and isometric contractions), and the ability to walk at different speeds on different surfaces and to varying distances. He must also be able to balance on a limited base of support, at a variety of heights, for significant time periods while cleaning windows. Finally, he will probably need to be able to land steadily on his foot when jumping from a height. All of these aspects must be covered in the final rehabilitation programme if the individual is to reach their maximum potential.
Tissue remodelling is a prolonged process which is especially pertinent in young patients who are remodelling and growing at the same time. In this client group, remodelling periods are often prolonged beyond the normal periods for adult members of the population.
![]() Clinical note
Clinical note
It should be acknowledged that while this chapter identifies the key influences that physiotherapy could have on the process of tissue healing and repair, in cases of severe and extensive soft tissue trauma a degree of permanent loss of function of the tissues affected is inevitable. This loss of function within the tissues may lead to a degree of long-term disability for the individual affected.
Case study
An injured hamstring
Joe is a 25-year-old university student who plays football on a weekly basis. He injured his right hamstring while playing football yesterday. He describes a sudden onset of pain in the posterior thigh while he was running. He was unable to play on and hobbled off the pitch. There was no first-aid advice available. He spoke to a friend who recommended he went to see a local physiotherapist. Joe has self-prescribed ibuprofen and paracetamol. He is otherwise well and has had no previous injuries.
Joe attends the physiotherapy clinic the next day and limps into the clinic, weight-bearing only through his toes on the affected leg.
Table 12.1 Case study: An injured hamstring
| Treatment aim | Treatment intervention |
|---|---|
| To protect newly damaged tissue from further damage | Cryotherapy: apply ice pack or ice compression device to injury site (20 mins minimum duration regularly through day) Compression application of elasticated strapping (as described above) Elevate affected limb for intermittent periods. Beware of combination with prolonged extensive compression |
| To reduce metabolic demands of tissue | |
| To prevent and reduce swelling | |
| To reduce pain | Use of crutches initially to protect injured area, encourage weight-bearing as pain allows Pain at the early stage should be seen as a protective mechanism to protect and prevent further damage; encourage movements of hip and knee within pain limits Anything that provokes pain at anything other than a minimal level should be discouraged initially Increase passive and active movements of the hip and knee, and then combine movement of both joints to increase stretch and load on tissues |
| To protect newly forming tissue from disruption | |
| To prevent soft tissue adaptation in non-injured tissues | |
| To promote collagen growth and fibre realignment | |
| To increase and restore normal joint range of movement (passive, active and accessory) | |
| To maintain and increase muscle strength, timing and control | Progress active and dynamic activity looking at lower limb and pelvis as a whole. Increase activity/football-specific tasks to improve proprioception, timing and neuromuscular control |
| To increase proprioception of affected lower limb | |
| To increase tensile strength of new collagen tissue | |
| To restore and encourage optimal function in relation to patient’s needs |
Case study
An injured ankle
Margaret is a 55-year-old hotel receptionist who slipped while coming down the stairs this morning sustaining an inversion injury to her left ankle. She is unable to weight-bear and has severe pain in her foot and ankle, and therefore attended the accident and emergency (A&E) department at her local hospital. X-ray revealed no bony injury. She is provided with crutches and taught to non-weight-bear. She is given an appointment to see the physiotherapist in A&E that afternoon.
Table 12.2 Case study: An injured ankle
| Treatment aim | Treatment intervention |
|---|---|
| To protect newly damaged tissue from further damage | Cryotherapy: apply ice pack or ice compression device to ankle/foot (of about 15 min minimum duration regularly through day). Monitor for reactions. Remember tissues are superficial and minimal subcutaneous fat Compression: application of elasticated strapping, particularly when patient is mobilising and not elevating distal limb (as described above) Elevate affected limb for intermittent periods. Beware of combination with prolonged extensive compression Advise regarding minimising walking and standing in first 5 days to minimise accumulation of swelling |
| To reduce metabolic demands of tissue | |
| To prevent and reduce swelling | |
| To reduce pain | Teach safe use of crutches initially to protect injured ankle with weight-bearing as pain allows Pain at the early stage should be seen as a protective mechanism to protect and prevent further damage Encourage movements of knee, ankle and foot within pain limits Anything that provokes pain at anything other than a minimal level should be discouraged initially Encourage normal gait pattern without use of crutches as pain and acute stage ends Increase passive, and active movements of the knee, ankle and foot, and then increase stretch and load on tissues Consider using accessory joint mobilisations to maintain/increase range of movement at the distal tibiofibular, talocrural, subtalar and mid-tarsal joints |
| To protect newly forming tissue from disruption | |
| To prevent soft tissue adaptation in non-injured tissues | |
| To promote collagen growth and fibre realignment | |
| To increase and restore normal joint range of movement (passive, active and accessory) | |
| To maintain and increase muscle strength, timing and control | Progress active and dynamic activity looking at lower limb and pelvis as whole. Increase activity/specific tasks to increase proprioception, timing and neuromuscular control of lower limb, particularly around the foot and ankle Consider occupation and return to work. Can job be adapted initially to allow early return to work or is time off appropriate. Consider all patient’s needs in terms of sport and activities |
| To increase proprioception | |
| To increase tensile strength of new collagen tissue | |
| To restore and encourage optimal function in relation to patient’s needs |
Alonson A., Hekeik P., Adams R. Predicting recovery time from the initial assessment of a quadriceps contusion injury. Aust J Physiother. 2000;46(3):167–177.
Bachmann L.M., Kolb E., Koller M.T., et al. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review. BMJ. 2003;326:417–425.
Benjamin M. Tendons are dynamic structures that respond to changes in exercise levels. Scand J Med Sci Sports. 2002;12(2):63–64.
Bleakley C., Glasgow P., Phillips N., et al. Management of acute soft tissue injury using Protection, Rest, Ice Compression and Elevation: Recommendations from the Association of Chartered Physiotherapists in Sports and Exercise Medicine (ACPSM). London: ACPSM; 2010.
Evans P. The healing process at cellular level. Physiotherapy. 1980;66(8):256–259.
Kerr K.M., Daily L., Booth L. Guidelines for the management of soft tissue (musculoskeletal) injury with protection, rest, ice, compression and elevation (PRICE) the first 64 hours. London: Chartered Society of Physiotherapy; 1999.
Knight K.L. Cryotherapy in sports injury management. Int Perspect Physiother. 1989;4:163–185.
Kraemer W.J., Ratamess N.A. Fundamentals of resistance training: progression and exercise prescription. Med Sci Sports Exerc. 2004;36(4):674–688.
MacAuley D. Ice therapy: How good is the evidence? Int J Sports Med. 2001;22:379–384.
Merrick M. Secondary injury after musculoskeletal trauma: A review and update. J Athletic Train. 2002;37(2):209–217.
Mutsaers S.E., Bishop J., McGrouther G., et al. Mechanisms of tissue repair: from wound healing to fibrosis. Int J Biochem Cell Biol. 1997;29(1):5–17.
Myer A.H. The effects of aging on wound healing [wound care and seating]. Topics Geriatr Rehab. 2000;16(2):1–10.
Oxford English Dictionary, http://dictionary.oed.com, 2007.
Rucinski T.J., Hooker D.N., Prentice W.E., et al. The effects of intermittant compression on oedema in post-acute ankle sprains. J Orthop Sports Phys Ther. 1991;14(2):65–69.
Scott A., Khan K., Roberts C., et al. What do we mean by the term ‘inflammation’? A contemporary basic science update for sports medicine. Br J Sports Med. 2004;38(3):372–380.
Thorsson O., Lilja B., Nilsson O., et al. Immediate external compression in the management of an acute muscle injury. Scand J Med Sci Sports. 1997;7:182–190.
Waddington P.J. PNF Techniques. In: Hollis M., Fletcher-Cook P., eds. Practical Exercise Therapy. Oxford: Blackwell Science, 1976.
Watson T. Soft tissue wound healing review. http://www.electrotherapy.org, 2004.
Watson T. Electrotherapy and tissue repair. Sportex Med. 2006;29:7–13.