Restorative paediatric dentistry
Erin Mahoney, Nicky Kilpatrick, Sally Hibbert and Timothy Johnston

Primary teeth
Why restore primary teeth?
Our child patients deserve the best dental treatment that clinicians can provide as any treatment, preventive or restorative, will shape their dental future. Doubts have been raised about the rationale behind restoring primary teeth, amid claims that the majority of carious primary teeth exfoliate without causing symptoms. While there is ample strong evidence to contradict this view, the quality of the restorative treatment performed remains paramount. However, it is essential that there is an understanding of the caries risk of the individual patient, the developmental stage of the dentition and the status of the dental pulp prior to determining the choice of restorative material and technique. The objective of any restorative technique is to:
• Restore the damage caused by dental caries.
• Protect and preserve the remaining pulp and tooth structure; thereby managing and preventing symptoms and pain.
• Restore aesthetics (where applicable).
• Facilitate easy maintenance of good oral hygiene.
• Maintain arch length and space for the developing permanent dentition.
Primary versus permanent teeth
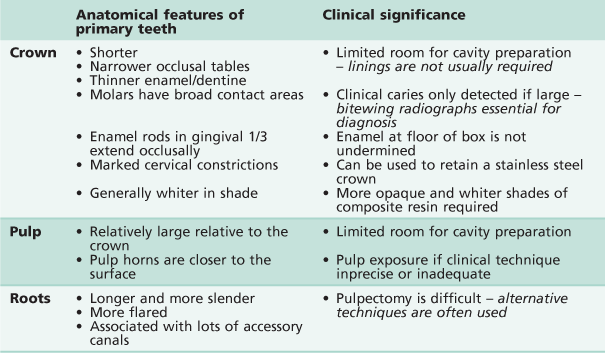
There are significant differences in the anatomy of the primary dentition in comparison with the permanent dentition that create some challenges when it comes to restoration of carious lesions (Table 6.1).
Restorative materials
There are a variety of restorative materials available to restore carious lesions in the primary dentition. Given the large number of techniques and products available on the market it is important for clinicians to understand the procedure they are using and to be aware that all approaches are operator and technique sensitive.
Table 6.2 summarizes the main advantages and disadvantages of the various dental restorative materials.
Amalgam
Historically, due to its simplicity, dental amalgam was the most popular restorative material. However today, as a result of concerns surrounding its potential toxicity and unfavourable aesthetics, amalgam is rarely used in the primary dentition. Indeed, in some parts of the world, it has been banned in children altogether. Today, dental amalgam has been largely superseded by alternative materials and techniques in the restoration of the primary dentition.
Glass ionomer cements (GICs)
A glass ionomer consists of a basic glass and an acidic water-soluble powder that sets by an acid–base reaction between the two components. A principal benefit of GIC is that it will adhere chemically to dental hard tissues. A number of GICs are available on the market today, each having its advantages and disadvantages, however indications for the use of GICs are limited and inappropriate use is likely to lead to failure.
Conventional GICs
Conventional GICs are chemical-set glass ionomers with the weakest mechanical properties. The initial setting reaction is complete within minutes but the material continues to ‘mature’ over the following months. It is important to protect these materials from salivary contamination in the hours following placement or the material may shrink, crack and even debond. Adhesion of all GICs may be enhanced by the use of a dentine conditioning agent before placement. Today, chemically curing GICs are available as both restorative and protective sealant types of materials with high fluoride releasing properties.
High-viscosity GICs
High-viscosity GICs were developed for the atraumatic restorative technique (ART). These chemically cured materials have significantly better mechanical properties than the conventional GICs and are fast setting. Research suggests that these materials have a durability comparable with amalgam, when used in occlusal (Class I) restorations in primary teeth, although the success rate is lower in inter-proximal (Class II) restorations, when other materials should be considered.
Resin-modified glass ionomer cements
Resin-modified glass ionomer cements were developed to overcome the problems of moisture sensitivity and low initial mechanical strength. They consist of a GIC along with a water-based resin system which allows photopolymerization to occur before the acid–base reaction of the glass ionomer is complete. This reaction then occurs within the light polymerized resin framework. The resin increases the fracture strength and wear resistance of the GIC. Resin modified GICs are manufactured as restorative and lining materials for use in both primary and permanent teeth.
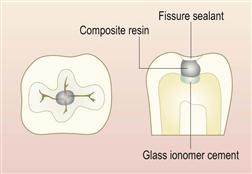
Composite resins
Resin-based composites (along with photopolymerization) have revolutionized clinical dentistry. In the primary dentition, composite resins are being increasingly used in combination with GICs in a ‘sandwich’-style aesthetic restoration. Placement of these materials is highly technique-sensitive, as there is no doubt that patient compliance and adequate moisture isolation can prove difficult in the younger, more challenging child. There is little evidence to support this approach and yet, the demand for aesthetic restorations makes this an attractive option.
Compomers (polyacid-modified composite resin)
Polyacid-modified resin composite resins or ‘compomers’ are materials that contain a calcium aluminium fluorosilicate glass filler and polyacid components. They contain either or both essential components of a GIC. However, they are not water-based and therefore no acid–base reaction can occur. As such, they cannot strictly be described as a glass ionomer. They set by resin photopolymerization. The acid–base reaction does occur in the moist intra-oral environment and allows fluoride release from the material. Successful adhesion requires the use of dentine-bonding primers before placement.
Stainless steel crowns
Stainless steel crowns are preformed extra-coronal restorations that are particularly useful in the restoration of large multisurface cavities and grossly broken down teeth. They cover the entire clinical crown and therefore recurrent or further caries is very unlikely. Placement of traditional stainless steel crowns is associated with considerable tooth preparation that can be challenging for patient and clinician alike. However, the introduction of minimal intervention sealed restorations (known as the ‘Hall crown technique’) has made the use of these restorations more realistic. They are, without doubt, the most durable restoration in the primary dentition and should be the technique of choice in the high-caries mouth.
Choice of materials
The choice of material to use in a given situation is not always simple and should not be based merely on technical considerations. Factors other than durability may be equally important in the choice of material, particularly in children.
Age
The age of a child will influence their ability to cooperate with procedures such as rubber dam application and local anaesthesia. The age of the child will also dictate for how long a restoration is required to remain satisfactory. A restoration in a first primary molar in a 9-year-old child does not require the same durability as a restoration in a second primary molar in a 4-year-old child.
Caries risk
Restorations in a child considered to be at high risk of caries may need to fulfil different objectives from restorations in a low-risk child. Although the use of a fluoride-releasing material has obvious preventive advantages, glass ionomer cements (GICs) may not be the most appropriate choice in a mouth that is at high risk of further acid attack. Stainless steel crowns may involve a significant amount of tooth destruction, but this will be appropriate if it eliminates the need to re-treat in the future. Alternatively, GICs have a useful role in initial caries control in cases of rampant caries.
Cooperation of the child
Many young children have behaviour that is not conducive to perfect, textbook, cavity preparation and restoration. In these cases, highly technique-sensitive procedures are inappropriate. A more forgiving restoration that can tolerate some moisture contamination, without detriment to its longevity, may be suitable. The use of GICs in the management of caries in anterior primary teeth may be an excellent method of slowing the carious process and temporarily restoring aesthetics in a 2-year-old child, without recourse to general anaesthesia. By the age of 3 or 4 years, the child may be able to cope with more definitive treatment with composite resin and strip crowns.
Restorative implications of behaviour management
Unfortunately, not all children are able to cooperate with dental treatment under local anaesthesia. This may be because of their age or due to physical or intellectual disabilities necessitating the completion of treatment under sedation or general anaesthesia. When treatment is provided this way, the highest standard of dentistry possible should be provided to reduce future dental treatment for these high-need children. Use of materials and techniques that are known to have longevity, such as stainless steel crowns, are mandatory.
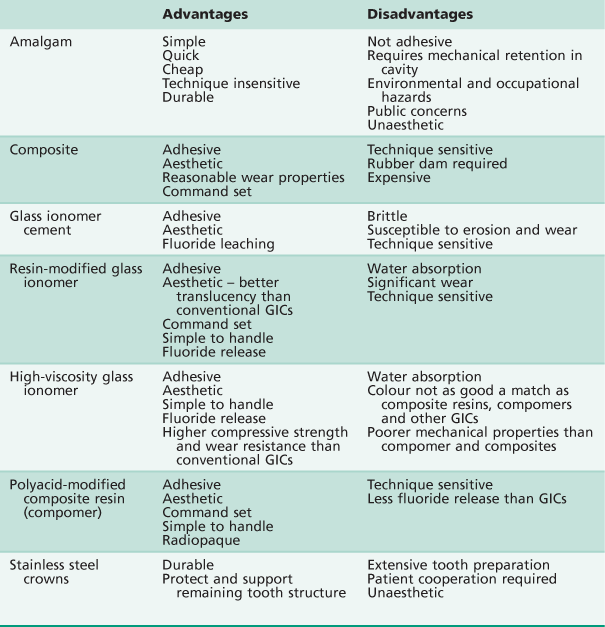
Restoring the primary dentition (Table 6.3)
Posterior teeth
GICs, resin-modified GICs and compomers
These materials have an increasingly important role in the management of carious lesions in primary molars because of their adhesive and fluoride-leaching properties.
Indications
Small occlusal and interproximal cavities. Because of their lack of strength, GICs should not be used in large restorations, particularly in teeth that need to be retained for 3 years or more. The use of polyacid-modified composite resins/compomers show considerable potential, particularly in terms of handling characteristics and radio-opacity. However, they have limited fluoride-leaching ability.
Success
The median survival time for conventional GICs is around 33 months. The failure rate of GICs is 33% over 5 years. High viscosity GICs demonstrate greater durability.
Technique
1. Local anaesthesia and rubber-dam isolation should be used where needed (Figure 6.1).
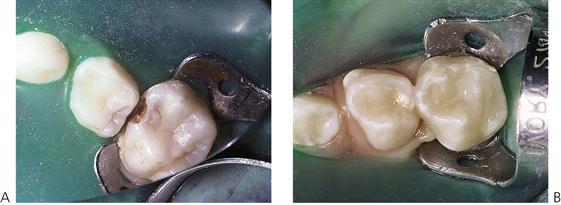
Figure 6.1 Two methods for using the rubber dam in children. (A) Traditional isolation of single teeth. (B) Split-dam technique, isolating the teeth from the canine to second primary molar with one large hole in the dam.
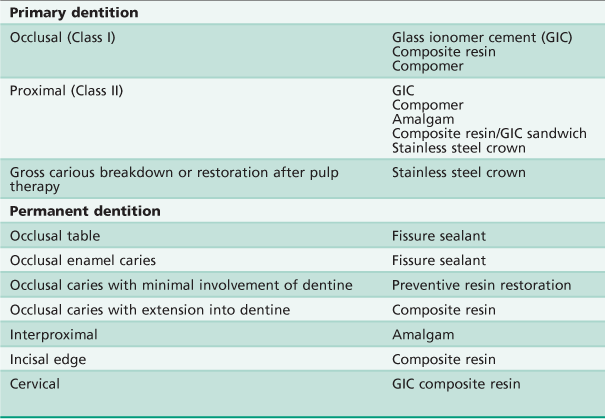
2. The outline of the cavity should follow the extent of the carious lesion. There is no need for extension for prevention. A small occlusal dovetail is not usually necessary for interproximal restorations, however, additional retention form for minimal proximal cavities can be achieved by placing grooves into the dentine using very small (size  ) round burs (Figure 6.2).
) round burs (Figure 6.2).
3. Remove all soft caries using a slow round bur or with hand instruments. Be aware of the large pulp chamber as it is easy to expose the pulp of a primary molar.
4. When placing GICs, precondition the dentine using 10% polyacrylic acid for 10 s, and wash and dry. When using a compomer, it is usually not necessary to condition the prepared tooth, however dentine-bonding primers should be used as per manufacturer’s instructions.
5. When using encapsulated materials, ensure that the capsules are compressed for at least 3 s to facilitate adequate mixing of the powder and liquid components. After mixing for 10 s in the amalgamator, discard the first 3–4 mm of the mixed material, as this is often unsatisfactory. Place the remainder directly into the cavity.
6. Once the relatively thick material has been placed into the cavity, it is compressed with a ball burnisher – dipping the tip in a small amount of bonding agent or unfilled resin prevents the material sticking to the instrument.
7. The final restoration must be protected from moisture contamination. This is best achieved by the placement of a thin layer of unfilled resin over the surface and polymerizing for 20 s. In young children with behaviour management problems, Vaseline, rather than unfilled resin, may be appropriate.
8. The occlusion should be checked on removal of the rubber dam.
Composite resins
In primary molars, composite is a satisfactory restorative material provided that the child is cooperative and good moisture control is achievable.
Indications
Small to moderately sized occlusal and proximal cavities.
Success
Clinical studies suggest that Class II composite restorations in primary molars are only moderately durable, with one study reporting <40% success after 6 years. However, recent studies have shown greatly improved success rates with the newer resin-based composites.
Technique
For interproximal lesions, the cavity design needs to be modified slightly in that a bevel should be prepared around the occlusal margins for additional adhesion to enamel. The biggest problem encountered with composite restorations is the integrity of the bond at the depth of the proximal box. Placement of composite is technically difficult and highly sensitive to moisture contamination. Placement of a glass ionomer liner over the dentine not only ensures a good bond at the base of the cavity, reducing microleakage, but also provides fluoride release locally. The use of rubber dam and incremental placement of composite in the proximal box may reduce handling and polymerization contraction problems.
Increasingly, parents are requesting tooth-coloured restorations. It should be recognized, however, that use of these materials is associated with increased technical demands and expense.
Stainless steel crowns
Indications
Stainless steel crowns are preformed extra-coronal restorations that are particularly useful in the restoration of:
Success
Stainless steel crowns undoubtedly provide the most durable restoration for the primary dentition with survival times in excess of 40 months.
Relatively expensive in relation to both time and money in the short term. However, the rate of replacement of these restorations is low (3% compared with 15% for class II amalgam restorations). This makes them economically more attractive over the long term.
Can be considered unaesthetic and require a significant amount of tooth preparation, and invariably local anaesthesia – unless using the ‘Hall crown technique’.
Method (Figure 6.3)
Irrespective of whether the tooth to be restored is vital or non-vital, local anaesthesia should be used when placing a stainless steel crown because of the soft-tissue manipulation. Rubber dam, although sometimes difficult to place in the broken down dentition, should be used where possible.
1. Restore the tooth using a GIC or compomer prior to preparation for the stainless steel crown.
2. Reduce the occlusal surface by about 1.5 mm using a flame-shaped or tapered diamond bur. Uniform occlusal reduction will facilitate placement of the crown without interfering with the occlusion.
3. Using a fine, long, tapered diamond bur, held slightly convergent to the long-axis of the tooth, cut interproximal slices mesially and distally. The reduction should allow a probe to be passed through the contact area (Figure 6.4).







Figure 6.3 Placement of a stainless steel crown. This tooth had a large distal lesion with loss of the marginal ridge. (A) Interproximal reduction is completed with a fine tapering diamond bur taking care not to damage the adjacent tooth. (B) Occlusal reduction of up to 1.5 mm is performed with a large diamond flat fissure bur, a small wheel or in this case a flame diamond bur. (C) Glass ionomer cement is used to build up the carious distal aspect of the crown. (D) Trial fit of the crown, by seating from the lingual onto the buccal surface.(E) A large spoon excavator can be used to remove the crown. (F) The crown is filled with glass ionomer cement for luting and (G) the crown placed with finger pressure (H). The completed restoration should last the lifetime of the tooth.
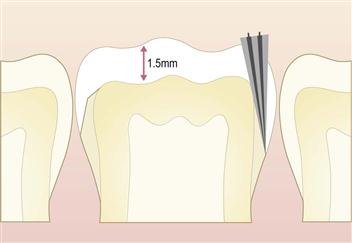
Figure 6.4 Coronal and proximal preparation required for the placement of a stainless steel crown. Note that in the proximal areas, there is a smooth contour without any ledge or step. Any such step will cause great difficulty in seating the crown.
4. Buccolingual reduction should be kept to a minimum, as these surfaces are important for retention. However, reduction may be needed when there has been significant proximal space loss or anatomical features, such as a prominent Carabelli’s cusp.
5. An appropriate size of a precontoured crown is chosen by measuring the mesiodistal width.
6. A trial fit is carried out before cementation. It is important that the crown should sit no more than 1 mm subgingivally. If there is excessive blanching of the gingival tissues, the length of the crown should be reduced and the margins should be smoothed with a white stone.
7. Cement the crown with a GIC. If the crown has been built up before the placement of the crown, a glass ionomer luting cement may be used, otherwise a restorative GIC should be used. Care should be taken while holding the crown as it can be easily dropped during placement. Excess cement should be wiped away and a layer of Vaseline placed around the margins while the cement is setting.
Minimal intervention
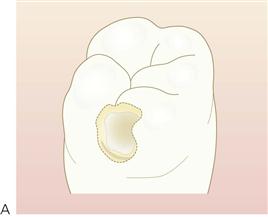
The philosophy of minimal intervention
Minimal intervention is based on an increasing body of evidence that traditional approaches to cavity design involved excessive removal of tooth structure. It is undisputed that beneath the layer of infected dentine lies a layer of affected dentine. Like the infected layer, this layer is discoloured, however in contrast to the infected layer, it may have odontoblast processes present, have a relatively intact collagen network and is bacteria free. Traditionally, all discoloured dentine was removed, however unlike the ‘infected zone’, the ‘affected’ layer can be remineralized and therefore should be preserved during cavity preparation (Figure 6.5).

Figure 6.5 Breakdown of GIC restorations from conservative (minimal intervention) dentistry. Note, however, that there has been a substantial slowing of the caries rate such that all the lesions are inactive and the teeth have been preserved in the mouth. While it is easy to criticize the quality of these restorations, these had been placed in a child whose behaviour was extremely difficult, without the access to general anaesthesia or other forms of sedation. Although some arch length has been lost, as the crowns have not been restored to their natural contour, the majority of the space occupied by the teeth has been preserved. This still permits the placement of stainless steel crowns in the future, when the child is better able to cope with more extensive treatment procedures in the event of an improvement in behaviour. The question should be asked whether these restorations have ‘successfully’ retained the teeth. Is this treatment better than having no treatment or having all these primary teeth extracted?
More recently, even this approach is being questioned as being too destructive, as researchers are beginning to query if any caries needs to be removed for a successful restoration. It has now been shown that dentists can provide long-lasting, sealed restorations, with minimal or no caries removal.
The sealed restoration
When placing any restoration, the importance of achieving a high quality coronal seal is now well recognized. Furthermore, there is growing evidence that providing a good seal is maintained, the complete removal of caries is no longer necessary. This enables us to minimize the amount of tooth tissue that is removed, which is of potential advantage in restoring primary molars with their thin enamel and dentine, and relatively large dental pulps.
When restoring occlusal lesions, adhesive materials such as GICs can usually provide an adequate seal. It can, however, be extremely difficult to achieve this seal using intracoronal techniques in primary molars with large proximal lesions. Stainless steel crowns provide an excellent coronal seal on primary molars and as such can prevent progression of caries. The placement of stainless steel crowns, with little or no caries removal, is known as the Hall crown technique.
The Hall crown technique
The Hall crown technique is essentially the ultimate minimally invasive restoration as it involves the placement of stainless steel crowns, directly over carious lesions, in primary molars, with little, or no, tooth preparation or caries removal. Initial trials in Scotland have shown that this simple technique can provide successful restorations in the medium term; indeed the technique not only outperformed conventional restorations but was preferred by the children and clinicians. This procedure can be a valid alternative, particularly when children are unable to accept conventional treatment with local anaesthetic. It is however, not appropriate in all cases and in particular should only be used for teeth that are symptom free and without signs or symptoms of pulpal pathology.
The question remains as to whether there is a place for this practice, when conventional techniques of proven efficiency are available. However, conventional restorations are very technique sensitive and commonly require the use of local anaesthesia and high speed handpieces, which many young children find difficult to accept. This technique can be a useful alternative under such circumstances. It is already being extensively used in some countries, although the paucity of long-term clinical trials prevents it from being recommended generally. Further trials are currently underway in the UK and Australasia and the results of these studies may change recommendations for its use.
Technique
This technique is used without local anaesthetic:
1. Pre-procedure radiograph and examination to exclude pulpal pathology.
2. Orthodontic separators may be placed at a prior appointment, to ease placement of the crown.
3. Child should be sat upright or semi-reclined, but not supine and gauze may be used to protect the airway.
4. The tooth can be cleaned with a toothbrush and if desired gross caries may be removed with a hand excavator.
5. A stainless steel crown is selected, which will fit over the tooth without any preparation.
6. A GIC cement is placed in the crown which is bitten into place by the child.
7. Excess cement may be washed or wiped away, before it has set.
Restoration of primary anterior teeth
GICs, resin-modified GICs, compomers
GICs (conventional and light-cured) and compomers all have a place as a one-surface restoration in primary anterior teeth. They provide aesthetically acceptable results and provide a degree of prevention as a result of fluoride release. However, it is important that the preparations must be caries-free for optimum results, as secondary caries is a reason for failure of all material types, even GICs. The durability of such restorations is, however, questionable and parents should be aware of this at the time of placement.
Composite resin strip crowns (Figure 6.6)
Composite is the material of choice for the restoration of primary anterior teeth. When used in conjunction with anterior strip crowns, composite resin provides an aesthetic and durable restoration.


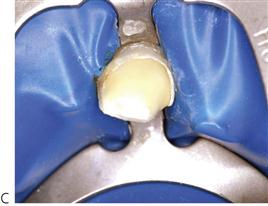
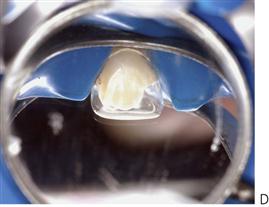


Figure 6.6 Placement of anterior strip crowns on the primary incisors. (A) Bottle caries affecting the upper anterior teeth. (B) Initial reduction of incisal edge and caries removal under the rubber dam (butterfly clamp). Proximal reduction is achieved using a high-speed tapering diamond bur. (C) Placement of a glass ionomer cement base over the dentine. (D) Trial fitting of the cellulose acetate strip crown, which is then filled with composite resin. (E) Removal of the strip crown with a small excavator. (F) Final restoration after polishing. (Courtesy of Dr E Alcaino.)
Method
1. Local anaesthesia and rubber-dam isolation should be used if possible. Alternatively, because of age and poor cooperation of younger children, the restorative work may be completed under general anaesthesia.
2. Select the correct celluloid crown form depending on the mesiodistal width of the tooth.
3. Remove the caries using a slow-speed round bur.
4. Using a high-speed tapered diamond or tungsten carbide bur, reduce the incisal height by around 2 mm, prepare interproximal slices and place a labial groove at the level of gingival and middle thirds of the crown.
5. Protect the exposed dentine with a glass ionomer lining cement.
6. Trim the crown form and make two holes in the incisal corners by piercing with a sharp explorer.
7. Etch the enamel for 20 s, wash and dry.
8. Apply a thin layer of bonding resin and cure for 20 s, ensuring all surfaces are covered equally.
9. Fill the crown form with the appropriate shade of composite and seat with gentle, even pressure, allowing the excess to exit freely. The use of small wedges may be helpful in avoiding interproximal excess.
10. Light cure each aspect (labially, incisally and palatally) equally.
11. Remove the celluloid crown gently, and adjust the form and finish with either composite finishing burs or abrasive discs.
Interproximal stripping
Stripping of interproximal enamel may be used occasionally for minimal caries in the anterior primary teeth. Opening of the contact points allows saliva and fluoride to arrest the carious process, even when the caries involves the dentine. Allowing open access for a toothbrush aids removal of cariogenic biofilm, which is difficult with a closed contact. This is often, however, an unaesthetic alternative. It goes without saying that the initiating cause, such as a nursing-bottle habit, must be eliminated.
Method
The contact points are removed with a long tapering diamond or tungsten carbide bur and a high percentage topical fluoride varnish (e.g. Duraphat® Varnish or Clinpro™ XT Varnish) is applied to the enamel and dentine. This should be repeated up to 4 times per year in high risk children.
Management of occlusal caries in permanent teeth
Dental amalgam is no longer considered the most appropriate technique for the restoration of caries lesions in the occlusal surfaces of permanent molars. The need to incorporate mechanical retention into the cavity design can lead to undermining of marginal ridges and weakens the cusps that will eventually fracture. Teeth restored in this manner often require further, even larger restorations with the risk of pulp disease, root canal treatment and finally full coverage restoration. The preventive resin restoration is more appropriate, as minimal tooth structure is lost in cavity preparation and the occlusal table is protected by a fissure sealant (Figure 6.7).
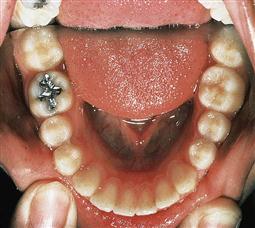
Figure 6.7 While this amalgam restoration has been well placed, it is an inappropriate restoration for a patient of 20 years, whose only caries is an incipient lesion on the occlusal surface. This amalgam will weaken the marginal ridges and supporting cusps and compromise the tooth in the long term. A preventive resin restoration would have been a much better alternative.
Fissure sealants
In fluoridated communities throughout Australasia, where the average DMFT (decayed, missing and filled permanent teeth) is <1, the majority of caries occurs in the pits and fissures of the first permanent molar teeth. A simple and economical way of preventing pit and fissure caries is by the use of fissure sealants.
The indications for a fissure sealant are controversial. On a population basis, it has been suggested that only those children who are at moderate risk of caries should have sealants placed, but because nearly 90% of children up to 18 years have some caries (mainly in the first permanent molars) all children should be assessed for fissure sealants throughout the eruption of the permanent dentition. Treatment should be prescribed according to the individual patient’s need (Figure 6.8).




Figure 6.8 Fissure sealants. (A) An assessment must be made in the individual of caries risk. Not every tooth in every arch requires sealing, but it is important to remember that risk can change. These fissures are caries-susceptible fissures and sealing of the buccal pit in this child is essential. (B–D) Newly erupted first permanent molars can benefit from fissure protection and the placement of a high-fluoride releasing glass ionomer cement. Note how the material extends into the high-risk areas of the buccal and distal fissures.
All teeth being considered for a fissure sealant should be checked radiographically for the presence of occult caries. Other options to aid diagnostic accuracy before sealing of fissures include the use of miniature burs to investigate staining, laser fluorescence, electronic caries detectors and microabrasion. If caries is noted or suspected, a preventive resin restoration should be placed.
Indications
• All permanent molars in children at medium or high risk of caries. Premolars should be sealed in those children at high risk.
• In children at low risk, only the fissures that are deep and retentive need to be sealed.
• Primary posterior teeth in children at high risk of caries.
Risk assessment should continue throughout teenage years, even where caries risk was initially low. Risk status can change and fissure sealing continues to be protective into adulthood.
Sealant material
• Although some studies show differences, there seems to be no strong evidence to favour light-cured over chemically-cured sealants or either opaque, clear or coloured fissure sealants at this time.
• Sealants should be opaque so that they can be detected by other clinicians. Use of clear sealants shows stains in the fissures, which are most probably inactive caries. However, another clinician, on seeing these stains, may choose to cut a cavity into a sound tooth, defeating the whole purpose of the sealant.
• Taking into account individual caries risk, the use of resin-based sealants is appropriate for fully erupted molars or pre-molars.
• Glass ionomers are useful in high caries-active individuals, partially erupted and hypomineralized teeth that are difficult to isolate and as temporary sealants until the teeth have erupted sufficiently to allow conventional fissure sealing.
The main problem with the use of GICs as fissure sealants is the brittleness of the material when used in thin section over the occlusal surface. However, the incidence of fissure caries in these teeth is low and in the long term, similar to retained resin-based sealants. It has been suggested that either the GIC is retained in the depths of the fissures at a microscopic level or that fluoride, from the GIC, is taken up by the surrounding enamel, so increasing the resistance of the fissure walls to demineralization.
Method (Figure 6.9)
1. Isolate the tooth with a rubber dam. If the tooth cannot be isolated, then a high-dose fluoride treatment such as a fluoride varnish or a GIC material should be applied. Review the eruption of the tooth in the following months and when the tooth has erupted sufficiently, place a fissure sealant.
2. Remove gross debris with a blunt probe and if necessary, clean the occlusal surface with oil-free pumice and water. In many instances, minimal widening of the occlusal fissure with a very thin, small, tapered diamond fissure bur will facilitate the penetration of sealant material into the depth of the fissure. It also removes the more acid-resistant surface layer of enamel lining the walls of the occlusal fissure. However, it is preferable to avoid any removal of tooth structure if possible.
3. Etch the tooth with a gel etchant for 20 s and wash with copious water and dry with air irrigation for 20 s.
4. If the tooth is contaminated it should be re-etched for 15 s.
5. Apply a thin coat of sealant to the pits and fissures, making sure to include the buccal extension on lower molars and the palatal groove in upper molar teeth. Apply the polymerization light for 20 s.
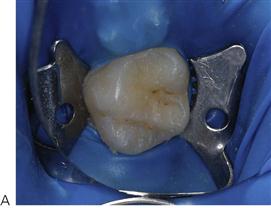


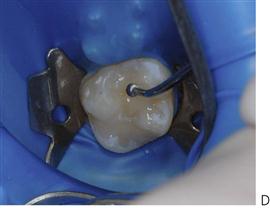

Figure 6.9 Placement of a fissure sealant. (A) Caries-susceptible fissure in an upper first permanent molar. The tooth is isolated with the rubber dam. (B) Tooth surface is etched. (C,D) A flowable composite resin has been used and is spread into the fissures with a ball-burnisher. (E) The completed sealant placement after curing.
Preventive resin restoration (PRR)/occlusal restoration
Due to its superior wear resistance and superior mechanical properties, composite resin materials rather than glass ionomers are the material of choice for the treatment of early occlusal caries in permanent teeth. The development of preventive resin restorations has changed the management of occlusal caries dramatically in young patients. The advantage of the PRR is the use of an unfilled resin base to seal over not just the underlying restoration itself but all the residual non-carious fissures, thus acting as a preventive restoration.
Success
The durability of preventive resin restoration has been proved to be as good as occlusal amalgam restorations and can be achieved with significantly less removal of sound tooth tissue. The proviso is that a sound hermetic seal is achieved such that there is no marginal leakage. Good technique is therefore essential.
Method for preventive resin restoration
1. Use local anaesthesia and rubber-dam isolation if caries extends into dentine.
2. With a small high-speed diamond bur obtain access into the questionable fissure.
3. Remove the carious dentine. Although it is important not to remove more enamel than necessary it is essential to have adequate access to the underlying dentine to be certain of complete caries removal. Unsupported enamel need not be removed if access and vision are clear. The cross-section most closely resembles a tear drop shape (Figures 6.10, 6.11).
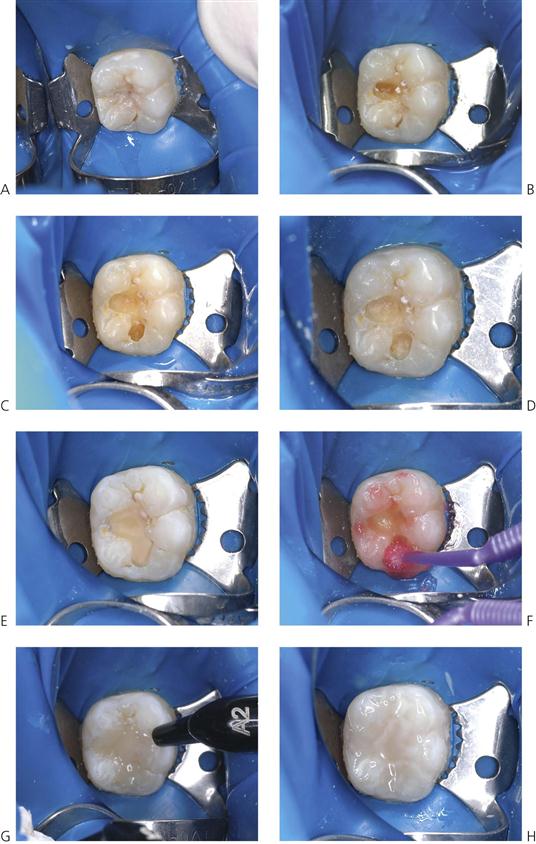
Figure 6.11 Technique for Class I composite restoration in a permanent molar. (A) The true extent of the caries may not be visible from the occlusal surface. (B–D) Progressive investigation of the fissures reveals further extension of dentinal caries. (E) Placement of a glass ionomer base. (F) Etching. (G) Incremental placement with nano-filled composite resin. (H) Final restoration with sealant placed over surface.
4. Deeper dentinal caries should be removed using a slow-speed round bur.
5. Place a glass ionomer liner over the dentine extending it up to the amelodentinal junction and light cure for 40 s.
6. Gel etchant is placed for 20 s on the enamel margins and occlusal surface, and washed and dried. It is not necessary to etch the liner; sufficient roughening of the surface of the GIC will result from the washing process.
7. Place a thin layer of bonding resin into the cavity and cure for 20 s. An excess of resin will produce pooling and reduce the integrity of the bond.
8. Incrementally fill and polymerize the cavity with hybrid composite resin until it is level with the occlusal surface.
9. Flow opaque unfilled fissure sealant over the restoration and the entire occlusal fissure pattern and cure for 20 s. There is no need to re-etch the occlusal surface prior to placing the fissure sealant.
New techniques for tooth preparation
From the discussion above, it is clear that paediatric dentistry relies heavily on the use of standard high-speed and low-speed handpieces. Standard handpieces allow clinicians to remove carious dentine and shape a cavity. However, in recent years, several hard-tissue removal techniques have been developed that also have a place in modern paediatric dentistry.
Air abrasion
Air abrasion is a technique that uses kinetic energy to remove carious tooth structure. When the aluminium oxide particles hit the tooth surface, without heat or noise of vibration, they remove tooth tissue. This technique requires additional equipment in the dental office for safe particle extraction and requires the use of a rubber dam, but has been shown to be useful in some child patients who may be nervous of the noise or the feeling of conventional handpieces. Care should be taken due to the possibility of particle inhalation when using this method in children with severe dust allergy, open wounds and lung diseases such as asthma.
Laser-assisted dentistry
Laser is an acronym for light amplification by stimulated emission radiation. Dental lasers are devices that use the energy generated by atomic electron shifts producing coherent monochromatic electromagnetic radiation between the ultraviolet and the far infrared section of the electromagnetic spectrum. The photobiological effects of the lasers most commonly used in dentistry are:
• Laser-induced fluorescence (caries/calculus detection).
• Photoacoustics causing disruption and ablation (soft-and hard-tissue treatments).
• Photothermal effect inducing coagulation and vaporization (soft-tissue treatments).
Bio-stimulation and photochemical effects induced by short-wavelength lasers for treatments including wound healing, analgesia and tissue growth will become more commonplace in time. Laser-assisted fluoride and bleaching treatments also show promising application.
Erbium lasers display bio-resonant properties on neural tissue causing Na+/K+ pump blockade and polarization of the A delta fibres and possibly C fibres. For many applications, local anaesthesia can be reduced and occasionally eliminated due to the analgesic properties of the lasers themselves.
Hard-tissue application
The two lasers most commonly used for dental hard-tissue treatments are in the 2790 nm (ErCr: YSGG (erbium-chromium: yttrium-scandium-gallium-garnet) and 2940 nm (Er: YAG (erbium-doped yttrium aluminium garnet) wavelengths. The tissue is removed by a non-contact beam that ablates based on the photoacoustic affect on water molecules. The water content of the treated tissue and the power density of the laser beam affect the cutting efficiency. Hard-tissue applications include cavity preparation, caries and calculus removal, endodontic treatments, desensitization and bone surgery. The advantages of lasers include:
• Ability to selectively remove only carious dental tissue.
• Ability to cut dental tissue without the need for local anaesthesia (in some cases).
Therefore, lasers can be extremely useful for nervous patients; however, they are expensive and care must be taken during use to ensure that excess heat is not generated, which may be detrimental to the pulp tissue.
It should be noted that these newer modalities result in significant changes to the smear layer compared with those of traditional techniques and clinicians should be aware that these may alter the choice of materials used and their bonding characteristics to both enamel and dentine (Figure 6.12).
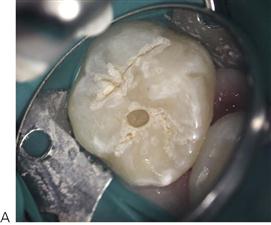
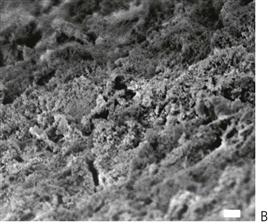
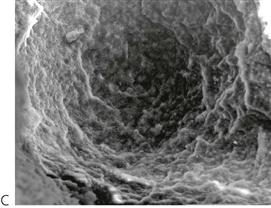
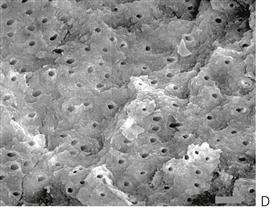
Figure 6.12 Effects of new techniques for tooth preparation on enamel and dentine. (A) Use of an Erbium YAG laser to prepare the enamel prior to placement of a preventive resin restoration and occlusal fissure sealant. (B) Scanning electron micrograph (SEM) enamel surface prepared with air abrasion (×4300 magnification). This may assist in the retention of sealants but it is not superior to normal enamel etching. (C) SEM of dentinal carious lesion prepared with an Erbium YAG hard tissue laser (×180) and at higher power (×700) (D) with complete absence of the smear layer and open dentinal tubules.
Further reading
Restoration of primary teeth
1. Attari N, Roberts JF. Restoration of primary teeth with crowns: a systematic review of the literature. European Archives of Paediatric Dentistry. 2006;7:58–62.
2. Chadwick BL, Evans DJ. Restoration of class II cavities in primary molar teeth with conventional and resin modified glass ionomer cements: a systematic review of the literature. European Archives of Paediatric Dentistry. 2007;8:14–21.
3. Gross LC, Griffen AL, Casamassimo PS. Compomers as class II restorations in primary molars. Pediatric Dentistry. 2001;23:24–27.
4. Innes NP, Ricketts DN, Evans DJ. Preformed metal crowns for decayed primary molar teeth. Cochrane Database of Systematic Reviews 2007.
5. Innes NP, Evans DJ, Stirrups DR. Sealing caries in primary molars: randomized control trial, 5 year results. Journal of Dental Research. 2011;90(12):1405–1410.
6. Kilpatrick NM, Neumann A. Durability of amalgam in the restoration of class II cavities in primary molars: a systematic review of the literature. European Archives of Paediatric Dentistry. 2007;8:5–13.
7. Qvist V, Manscher E, Teglers PT. Resin-modified and conventional glass ionomer restorations in primary teeth: 8-year results. Journal of Dentistry. 2004;32:285–294.
8. Randall RC. Preformed metal crowns for primary and permanent molar teeth: review of the literature. Pediatric Dentistry. 2002;24:489–500.
9. Ricketts DN, Kidd EA, Innes N, et al. Complete or ultraconservative removal of decayed tissue in unfilled teeth. Cochrane Database of Systematic Reviews 2006.
10. Scott JM, Mahoney EK. Restoring proximal lesions in the primary dentition: is glass ionomer cement the material of choice? New Zealand. Dental Journal. 2003;99:65–71.
11. Van’t Hof MA, Frencken JE, Van Palenstein Helderman WH, et al. The atraumatic restorative treatment (ART) approach for managing dental caries: a meta-analysis. International Dental Journal. 2006;56:345–351.
12. Yengopal V, Harnekar SY, Patel N, et al. Dental fillings for the treatment of caries in the primary dentition. Cochrane Database of Systematic Reviews 2009.
Restoration of permanent teeth
1. Ahovuo-Saloranta A, Hiiri A, Nordblad A, et al. Pit and fissure sealants for preventing dental decay in the permanent teeth of children and adolescents. Cochrane Database of Systematic Reviews 2008.
2. Mejare I. Indications for fissure sealants and their role in children and adolescents. Dental Update. 2012;38:699–703.
3. Simonsen R. From prevention to therapy: minimal intervention with sealants and resin composite materials. Journal of Dentistry. 2011;39:S27–S33.
4. Yengopal V, Mickenautsch S, Bezerra AC, et al. Caries preventive effect of glass ionomer and resin based fissure sealants on permanent teeth: a metal analysis. Journal of Oral Science. 2009;51:373–382.