Trauma to Teeth and Facial Structures
Radiologic examination is essential for evaluating trauma to the teeth and jaws. The presence, location, and orientation of fracture planes and fragments can be determined, and the involvement of nearby vital anatomic structures can be assessed. Furthermore, foreign objects that have become embedded within the soft tissues as a result of trauma can be detected. Follow-up images are useful in evaluating the extent of healing after an injury and long-term changes resulting from the trauma.
Applied Radiology
The ideal imaging study may be difficult to perform after trauma because of the nature of the injury and patient discomfort. although the prescription of the appropriate images should be ordered only after a careful clinical examination, in some cases this is not always possible. If plane radiography is to be used, multiple images should be made at differing angles, including at least two views made at right angles to each other. These views will typically consist of intraoral, panoramic, and lateral oblique projections of the mandible for dentoalveolar and mandibular injuries, and posteroanterior, Waters, submentovertex, Towne, and lateral projections for midface and skull injuries. In many centers, computed tomographic imaging (CT) has replaced plane radiography as the standard imaging modality whether for isolated trauma or more widespread complex injuries.
Although a panoramic image may be useful for localizing the area of an injury, it may not have the image resolution to reveal injuries involving the anterior mandible or maxillae or the teeth. Dentoalveolar trauma always requires intraoral images to obtain adequate anatomic detail. A minimum of two intraoral periapical images should be made at different horizontal x-ray beam angulations to identify fractures, and it is important to image not only the involved teeth but also the teeth of the opposing arch. Occlusal views may be particularly useful depending on the severity of the trauma and the ability of the patient to open the mouth.
If a tooth or a large fragment of a tooth is missing, a chest or abdominal image may be considered to locate the tooth. If there are lacerations in the lips or cheek, a soft tissue image of the area may be obtained by placing an intraoral film or receptor in the mouth adjacent to the traumatized soft tissue and then exposing it. If the laceration is in the tongue, a standard mandibular occlusal image may be exposed or the tongue can be protruded and then imaged.
MANDIBULAR FRACTURES
Although the panoramic image may be a good initial image to make for assessing mandibular fractures, the intraoral cross-sectional occlusal view of the mandible may provide important information about body or alveolar process fractures in the tooth-supporting areas. If a panoramic image is not available, lateral oblique views of the mandible should be made.
The open mouth Towne view may be particularly useful in cases of suspected trauma to the mandibular condylar head and neck areas. These views are important to supplement lateral views of the temporomandibular joint, especially in cases of nondisplaced greenstick fractures of the condylar neck. For suspected multiple and complex fractures of the mandible, CT is the imaging modality of choice. Magnetic resonance imaging may be useful to assess soft tissue injury to the temporomandibular joint capsule or articular disk.
MAXILLOFACIAL FRACTURES
Although some centers continue to rely on plane radiography for suspected localized trauma to the maxillofacial skeleton, CT is the imaging method of choice for more widespread complex fractures.
RADIOGRAPHIC SIGNS OF FRACTURE
Fractures are often erroneously referred to as “lines” in spite of their three-dimensional nature. Fractures represent planes of cleavage through a tooth or bone, and these planes extend deep into the tissues. Therefore, a fracture may be missed if the plane of the fracture is not aligned with the direction of the incident x-ray beam on a single-plane image.
The following are general signs that may indicate the presence of a fracture of a tooth or bone:
1. The presence of one or two usually sharply defined radiolucent lines within the anatomic boundaries of a structure. If the line or lines extend beyond the boundaries of the mandible, more than likely they represent an overlapping structure. If a line extends beyond the boundaries of a tooth root, the line may represent a superimposed neurovascular canal.
2. A change in the normal anatomic outline or shape of the structure. A mandible that is noticeably asymmetric between the left and right sides may be fractured. A fracture of the mandible may also manifest as a change in the contour of the occlusal plane at the location of the fracture site.
3. A loss of continuity of an outer border. This may appear as a gap in the continuity of the otherwise smooth tooth or cortical border. Such a gap may also produce a steptype defect where the two fragments have become displaced relative to one-another.
4. An increase in the radiopacity of a structure. This can be caused by the overlapping of two fragments of tooth or bone such that a particular area appears “doubly” radiopaque.
Traumatic Injuries of the Teeth
Definition
The term concussion refers to a crush injury to the vascular structures at the tooth apex and the periodontal ligament resulting in inflammatory edema. No displacement and only minimal loosening of the tooth occurs. The injury may result in mild avulsion of the tooth from its socket, causing its occlusal surface to make premature contact with an opposing tooth during mandibular closing.
Clinical Features
The patient usually complains that the traumatized tooth is tender to touch, which can be confirmed by gentle horizontal or vertical percussion of the tooth. The tooth may also be sensitive to biting forces, although patients will usually try to modify their occlusion to avoid contacting the traumatized tooth.
Radiographic Features
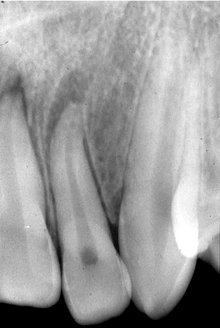
The radiographic appearance of a dental concussion may be subtle. No radiographic changes may be found or localized widening of the apical periodontal ligament space may be seen (Fig. 29-1).
Reduction in the size of the pulp chamber and root canals may develop in the months and years after traumatic injury to the teeth (Fig. 29-2). This may be particularly evident in teeth that are still developing. If the pulp becomes necrotic, there may be no further deposition of (secondary) dentin as the odontoblasts and the pulpal stem cell populations die. The development of rarefying osteitis may ensue, and in rare cases, internal root resorption (Fig. 29-2).

FIG. 29-2 Obliteration of the pulp chamber but not the root canal, internal root resorption, and an incisal fracture of the maxillary left central incisor after dental concussion. As well, note the area of rarefying osteitis involving the maxillary right central incisor and the widened pulp chamber and canal.
Management
Because significant displacement of the tooth or teeth does not occur, the appropriate treatment is conservative and may include slight adjustment of the opposing teeth (if necessary) or the application of a flexible splint. Periodic monitoring in the first year with repeated vitality testing and radiographs are indicated.
Definition
Luxation is a dislocation of the tooth from its socket after severing of the periodontal attachment. Such teeth are both abnormally mobile and displaced. Subluxation of the tooth denotes an injury to the supporting structures of the tooth that results in abnormal loosening of the tooth without frank dislocation.
Depending on their magnitude and direction, traumatic forces can cause intrusive luxation (displacement of a tooth into the alveolar process), extrusive luxation (partial displacement of a tooth out of its socket), or lateral luxation (movement of a tooth in a direction other than intrusive or extrusive displacement). In intrusive and lateral luxation, comminution or crushing of the alveolar process may accompany tooth dislocation.
The movement of the apex and disruption of the circulation to the traumatized tooth that accompanies luxation can produce either temporary or permanent changes to the dental pulp, and these changes may result in pulpal necrosis. If the pulp survives the traumatic incident, the rate of dentin formation may accelerate and continue until it obliterates the pulp chamber and root canal. This may take place in permanent and deciduous teeth.
Clinical Features
An adequate clinical history is helpful in identifying luxation and ordering the appropriate radiographs. Subluxated teeth are in their normal location but are abnormally mobile. There may be extravasated blood emanating from the gingival crevice, indicating periodontal ligament damage, and they may be extremely sensitive to percussion and masticatory forces.
The clinical crowns of intruded teeth may appear reduced in height. Maxillary incisors may be intruded so deeply into the alveolar process that they appear to be completely avulsed or lost. The displaced tooth may cause some damage to adjacent teeth, particularly if any developing permanent teeth are present in the underlying bone.
Depending on the orientation and magnitude of the force and the shape of the root, it may be pushed through the buccal or, less commonly, the lingual cortex of the alveolar process where it may be seen and palpated. On repeated vitality testing, the sensitivity of a luxated tooth may be temporarily decreased or undetectable, especially shortly after the injury. Vitality may return, however, after weeks or even several months.
Usually two or more teeth are involved in luxation injuries, and the teeth most frequently affected are the deciduous and permanent maxillary incisors. The mandibular teeth are seldom affected. The type of luxation appears to vary with age and this may reflect changes to the nature of maturing bone. Intrusions and extrusions are often found in the deciduous dentition. In the permanent dentition, the intrusive type of luxation is seen less frequently.
Radiographic Features
Radiographic examinations of luxated teeth may demonstrate the extent of injury to the root, periodontal ligament, and alveolar process. A radiograph made at the time of injury serves as a valuable reference point for comparison with subsequent radiographs. As with dental concussion, the minor damage associated with subluxation may be subtle and limited to elevation of the tooth from its socket. The sole radiographic finding may be a widening of the apical portion of the periodontal ligament space. Elevation of the tooth may not be radiographically apparent.
The depressed position of the crown of an intruded tooth is often apparent on a radiograph (Fig. 29-3), although a minimally intruded tooth may be difficult to demonstrate radiographically. Intrusion may result in partial or total obliteration of the apical periodontal ligament space. Multiple radiographic projections, including occlusal views, may be necessary to show the direction of tooth displacement and the relationship of the displaced tooth to adjacent teeth and the outer cortex of bone.

FIG. 29-3 Intruded maxillary central incisor after trauma. Note the fractured incisal edges of both central incisors.
A tooth that has been extruded may demonstrate varying degrees of apical widening of the periodontal ligament space, depending on the magnitude of the extrusive force (Fig. 29-4). A laterally luxated tooth with some degree of extrusion may show a widened periodontal ligament space, with greater width on the side of impact.
Management
A subluxated permanent tooth may be restored to its normal position by digital pressure shortly after the accident. If inflammation precludes repositioning, minimal reduction of opposing teeth may be necessary to minimize any discomfort. The use of a flexible splint may provide additional stability and prevent further damage to the pulp and periodontal ligament. A subluxed deciduous tooth may potentially damage its underlying successor. Consequently, extraction may be considered. If the alveolar bone over the root of a luxated tooth has been fragmented and displaced, the fragments should be repositioned by digital pressure. A subluxated primary tooth should be periodically examined after the injury. If it causes some discomfort as the result of extrusion, it can be removed without undue concern for occlusal problems. Subluxed permanent teeth should be monitored in the same manner as those teeth that have been concussed.
Definition
Avulsion is the term used to describe the complete displacement of a tooth from the alveolar process. Teeth may be avulsed by direct trauma when the force is applied directly to the tooth or by indirect trauma (i.e., when indirect force is applied to teeth as a result of the jaws striking together). Avulsion occurs in about 15% of traumatic injuries to the teeth, with fights being responsible for the avulsion of most permanent teeth and accidental falls accounting for the traumatic loss of most deciduous teeth.
Clinical Features
Maxillary central incisors are the most commonly avulsed teeth from both dentitions. Most often only a single tooth is lost. Typically this injury occurs in a relatively young age group when the permanent central incisors are just erupting. Fractures of the alveolar process and lip lacerations may be seen with an avulsed tooth.
Radiographic Features
In a recent avulsion, the lamina dura of the empty socket is apparent and usually persists for several months. The missing tooth may be displaced into the adjacent soft tissue, and its image may project over the alveolar process on an image, giving the false impression that it lies within the bone. Therefore, to differentiate between an intruded tooth and an avulsed tooth lying within the adjacent soft tissues, a soft tissue image of the lacerated lip or tongue should be made. In some instances new bone within the healing socket may be very dense and simulate a retained root tip (Fig. 29-5).
Management
If the avulsed tooth is not found by clinical or radiographic examination, a chest or abdominal radiograph may be considered to locate it within the airway or gastrointestinal tract. Reimplanting permanent teeth after avulsion is possible; however, the prognosis of the reimplantation is dependent on the condition of the tooth while it is outside the mouth, the time it is out of its socket, and the viability of the residual periodontal ligament fibers. Endodontic therapy may be necessary after reimplantation and there may be external root resorption in the months and years after reimplantation. Reimplanting an avulsed deciduous tooth carries the danger of interfering with the underlying developing permanent tooth.
FRACTURES OF THE TEETH
Definition
Fractures of the dental crown account for about 25% of traumatic injuries to the permanent teeth and 40% of injuries to the deciduous teeth. The most common event responsible for the fracture of permanent teeth is a fall, followed by accidents involving vehicles (e.g., bicycles, automobiles) and blows from foreign objects striking the teeth. Fractures involving only the crown normally fall into three categories:
1. Fractures that involve only the enamel without the loss of enamel substance (infraction of the crown or crack)
2. Fractures that involve enamel or enamel and dentin with loss of tooth substance but without pulpal involvement (uncomplicated fracture)
3. Fractures that pass through enamel, dentin, and pulp with loss of tooth substance and exposure of the pulp (complicated fracture)
Clinical Features
Fractures of the dental crowns most frequently involve anterior teeth. Infractions or cracks in the enamel are quite common but frequently are not readily detectable. Illuminating crowns with indirect light (directing the beam along the long axis of the tooth) causes cracks to appear distinctly in the enamel. Histologic studies show that they pass through the enamel but not into the dentin. The pattern and distribution of these cracks are unpredictable and apparently relate to the trauma.
Uncomplicated crown fractures that do not involve dentin usually occur at the mesioincisal or distoincisal corners of the maxillary central incisor. Loss of the central portion of the incisal edge may also occur. Fractures that involve dentin can be recognized by the contrast in color between dentin and the peripheral layer of enamel. The exposed dentin is usually sensitive to chemical, thermal, and mechanical stimulation. In deep fractures, the pink blush of the pulp may be appreciated through the thin remaining dentin wall.
Uncomplicated fractures that involve both the enamel and the dentin of permanent teeth are more common than complicated fractures are. In contrast, the incidence of complicated and uncomplicated fractures is about equal in the deciduous teeth.
Complicated crown fractures are distinguishable by bleeding from the exposed pulp or by droplets of blood forming from pinpoint exposures. The pulp is visible and may extrude from the open pulp chamber if the fracture is old. The exposed pulp is sensitive to most forms of stimulation.
Radiographic Features
Radiographs provide information regarding the location and extent of the fracture and the relationship of the fracture plane and fragment to the pulp chamber. As well, the stage of root development of the involved tooth can be assessed with radiography (Fig. 29-6). This initial image also provides a means of comparison for follow-up examinations of the involved teeth.
Management
Although crown infractions do not require treatment, the vitality of the tooth should be evaluated. The sharp edges of enamel that result from an uncomplicated fracture should be smoothed and may require restoration for cosmetic reasons. It is reasonable to delay this procedure for a number of weeks until the pulp has recovered and secondary dentin is laid down. The prognosis for teeth with fractures limited to the enamel is quite good, and pulpal necrosis develops in fewer than 2% of such cases. If a fracture involves both dentin and enamel, the frequency of pulpal necrosis is about 3%. Oblique fractures have a worse prognosis than horizontal fractures because potentially a greater amount of dentin is exposed. The frequency of pulpal necrosis increases greatly with concussion and mobility of the tooth.
Treatment of complicated crown fractures of permanent teeth may involve pulp capping, pulpotomy, or pulpectomy, depending on the stage of root formation. If a coronal fracture of a deciduous tooth involves the pulp, it is usually best treated by extraction.
Definition
Fractures of tooth roots are uncommon and account for fewer than 7% of traumatic injuries to permanent teeth and about half that many in deciduous teeth. This difference probably results from the fact that the deciduous teeth are less firmly anchored in the alveolar process.
Clinical Features
Most root fractures occur in maxillary central incisors. The coronal fragments are usually displaced lingually and slightly extruded. The degree of mobility of the crown relates to the level of the fracture. That is, the closer the fracture plane is located to the apex, the more stable the tooth is. When testing the mobility of a traumatized tooth, place a finger over the alveolar process. If movement of only the crown is detected, a root fracture is likely. Fractures of the root may occur with fractures of the alveolar process, which are commonly not detected. This is most often observed in the anterior region of the mandible where root fractures are infrequent. Although root fracture is usually associated with temporary loss of sensitivity (by all usual criteria), the sensitivity of most teeth returns to normal within about 6 months.
Radiographic Features
Fractures of the dental root may occur at any level and involve one (Fig. 29-7) or all the roots of multirooted teeth. Most of the fractures confined to the root occur in the middle third of the root.
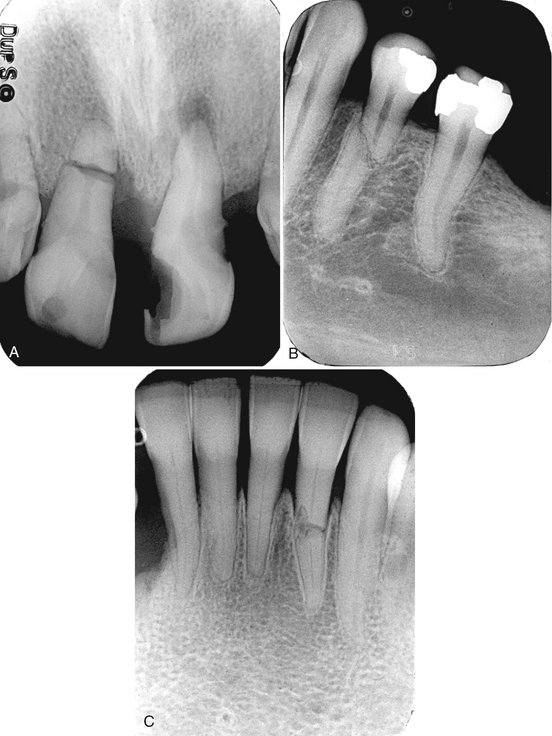
FIG. 29-7 A, A recent horizontal fracture of the right maxillary central incisor and apical rarefying osteitis involving the adjacent left central incisor. B, A healed fracture with slight displacement of the fragments. C, A healed fracture with an increase in the distance between the fracture segments as a result of root resorption.
The ability of an image to reveal the presence of a root fracture depends on the relative angulation of the incident x-ray beam to the fracture plane and the degree of distraction of the fragments. If the x-ray beam is well aligned with the fracture plane, a single sharply defined radiolucent line confined to the anatomic limits of the root may be seen. If, however, the orientation of the x-ray beam is not well aligned and meets the fracture plane in a more oblique manner, the fracture plane may appear as a more poorly defined single line or as two lines that converge at the mesial and distal surfaces of the root. The appearance of a comminuted root fracture may also appear less well defined. Most nondisplaced root fractures are usually difficult to demonstrate radiographically, and several views at differing angles may be necessary. In some instances when the fracture line is not visible, the only evidence of a fracture may be a localized increase in the width of the periodontal ligament space adjacent to the fracture site (Fig. 29-8).

FIG. 29-8 A, Subtle evidence of a root fracture involving the root of the maxillary right central incisor. Although a fracture plane is not apparent on the mesial aspect of the root because of malalignment of the x-ray beam, there is widening of the periodontal membrane space on the mesial surface (arrow) at the site of the fracture. B, Later dislocation of the root fragments.
Longitudinal root fractures are relatively uncommon but are most likely in teeth with posts that have been subjected to trauma. The width of the fracture plane tends to increase with time, probably because of resorption of the fractured surfaces. Over time, calcification and obliteration of the pulp chamber and canal may be seen.
Differential Diagnosis
The superimposition of soft tissue structures such as the lip, ala of the nose, or nasolabial fold over the image of a root may suggest a root fracture. To avoid this diagnostic error, it should be noted that the soft tissue image of the lip line usually extends beyond the tooth margins. Fractures of the alveolar process may also overlap the root and suggest a root fracture.
Management
Fractures in the middle or apical third of the root of permanent teeth can be manually reduced to the proper position and immobilized. Prognosis is generally favorable because the incidence of pulpal necrosis is about 20% to 24%. The more apical the fracture is, the better the prognosis. Endodontic therapy is performed when evidence of pulpal necrosis exists. It is common for bone resorption to occur at the site of the fracture rather than at the apex. When the fracture occurs in the coronal third of the root, the prognosis is poor and extraction is indicated unless the apical portion of the root fragment can be extruded orthodontically and restored. The roots of fractured deciduous teeth that are not badly dislocated may be retained with the expectation that they will be normally resorbed. Attempts at removal may result in damage to the developing succedaneous tooth.
Definition
Vertical root fractures represent fracture planes that run lengthwise from the crown toward the apex of the tooth. Usually both sides of a root are involved. The crack is usually oriented in the facial-lingual plane in both anterior and posterior teeth. These fractures usually occur in the posterior teeth in adults, especially in mandibular molars. They are usually iatrogenic, after insertion of retention screws or pins into teeth. Uncrowned posterior teeth that have been treated endodontically are most at risk. Large occlusal forces are another etiology for vertical root fracture, particularly in restored teeth.
Clinical Features
Patients with vertical root fractures complain of persistent low-level dull pain, often of long duration, the so-called cracked tooth syndrome. This pain is elicited by applying pressure to the involved tooth. The patient may have rarefying osteitis or a history of repeated failed endodontic therapy. Occasionally, definitive diagnosis can be made only by inspection after surgical exposure.
Radiographic Features
If the central ray of the x-ray beam lies along the plane of the fracture, the fracture may be visible as a radiolucent line on the image. Usually, however, radiography is not useful in identifying vertical root fractures in their early stages. Later, if rarefying osteitis develops, there will be evidence of bone loss (Fig. 29-9). The widening of the periodontal ligament space and this bone loss may not be centered at the apex but often positioned more coronally toward the alveolar crest. Inflammatory lesions may also extend apically from the alveolar crest and may resemble periodontal lesions.
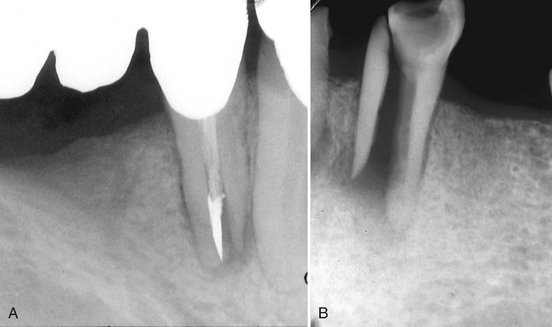
FIG. 29-9 A, Vertical fracture through the root of a mandibular first premolar that has been endodontically treated. The fracture plane extends through the root canal and there is more displacement between the root fragments at the apex of the root. B, A vertical root fracture through the root of a mandibular canine with significant displacement of the fragments.
Management
Single-rooted teeth with vertical root fractures must be extracted. Multirooted teeth may be hemisected and the intact remaining half of the tooth restored with endodontic therapy and a crown.
Definition
Crown/root fractures involve both the crown and root(s). Although uncomplicated fractures may occur, crown/root fractures usually involve the pulp. About twice as many affect the permanent as the deciduous teeth. Most crown/root fractures of the anterior teeth are the result of direct trauma. Many posterior teeth are predisposed to such fractures by large restorations or extensive caries.
Clinical Features
The fracture plane of a typical crown/root fracture of an anterior tooth extends obliquely from the labial surface near the gingival third of the crown to a position apical to the gingival attachment on the lingual surface. Displacement of the fragments is usually minimal. Crown/root fractures occasionally present with bleeding from the pulp. Because these teeth are sensitive to occlusal forces that may cause separation of the fragments, a patient with a crown/root fracture usually complains of pain during mastication.
Radiographic Features
These fractures are often not visible on the radiographic image because the x-ray beam is rarely aligned with the plane of the fracture. Also, distraction of the fragments is usually not present. Vertical crown/root fractures that are oriented in a mainly tangential orientation relative to the direction of the x-ray beam are readily apparent on the image. Unfortunately, this is not common.
Management
Removal of the coronal fragment permits the evaluation of the extent of the fracture. If the coronal fragment includes as much as 3 to 4 mm of clinical root, successful restoration of the tooth is doubtful and removal of the residual root is recommended. If the crown/root fracture is vertically oriented, prognosis is poor regardless of treatment.
If the pulp is not exposed and the fracture does not extend more than 3 to 4 mm below the epithelial attachment, conservative treatment is likely to be successful. Uncomplicated crown/root fractures are frequently encountered in posterior teeth, and with crown lengthening procedures the tooth is likely to be restorable. If only a small amount of root is lost with the coronal fragment but the pulp has been compromised, it is likely that the tooth can be restored after endodontic treatment.
Traumatic Injuries to the Facial Bones
Facial fractures most frequently affect the zygomatic bones or mandible and, to a lesser extent, the maxillae. Radiography plays a crucial role in the diagnosis and management of traumatic injuries to these and the other facial bones.
Superficial signs of injury such as soft tissue swelling, hematoma formation, or hemorrhage from a laceration or abrasion may focus the radiologic examination. Localized injuries may be investigated with plane radiography. In this instance, it is important to make at least two views of the injured site at right angles to one another to assess the presence, location, extent, and displacement of a fracture. Some fractures may not be readily apparent if the x-ray beam is not oriented parallel to the plane of the fracture. More and more commonly, plane radiography is being replaced by CT, even for localized injuries. For more widespread trauma, CT is the imaging modality of choice.
MANDIBULAR FRACTURES
The most common mandibular fracture sites are the condyle, body, and angle, followed less frequently by the parasymphyseal region, ramus, coronoid process, and alveolar process. Trauma to the mandible is often associated with other injuries, most commonly concussion (loss of consciousness) and other fractures, usually of the maxillae, zygomatic bones, and cranial vault.
The most common causes of mandibular fractures are assault, falls, and sports injuries. About half of all mandibular fractures occur in individuals between 16 and 35 years old, and injuries in males are reportedly three times more common than in females. Moreover, fractures are more likely to occur on weekend days than on other days of the week.
Definition
The mandible is the most commonly fractured facial bone. It is important to realize that a fracture of the mandibular body on one side is frequently accompanied by a fracture of the condylar neck on the opposite side. Trauma to the anterior mandible may result in unilateral or bilateral fractures of the condylar necks. When a localized heavy force is directed posteriorly to the mandible, there may be fractures of the angle, ramus, or even the coronoid process. In children, fractures of the mandibular body usually occur in the anterior region.
Mandibular fractures are classified as being either favorable or unfavorable, depending on the orientation of the fracture plane. Unfavorable fractures are those in which the action of muscles attached to the mandibular fragments displace the fragments away from one another. For example, if a fracture plane in the body of the mandible slants obliquely posteriorly and inferiorly from the base of the anterior border of the ramus, the masseter and medial pterygoid muscles may displace the ramal fragment superiorly and away from the body of the mandible. In favorable fractures, the muscle action tends to reduce the fracture.
Clinical Features
A history of injury is typical, substantiated by some evidence of the trauma that caused the fracture, such as injury to the overlying skin. Frequently the patient has swelling and a deformity that is accentuated when the patient opens the mouth. A discrepancy is often present in the occlusal plane, and manipulation may produce crepitus or abnormal mobility. Intraoral examination may reveal ecchymosis in the floor of the mouth. In the case of bilateral fractures to the mandible, a risk exists that the digastric, mylohyoid, and omohyoid muscles will displace the anterior mandibular fragment posteriorly and inferiorly, causing impingement on the airway.
Radiographic Features
The radiographic examination of a suspected mandibular fracture may include intraoral or occlusal views, a panoramic view, posteroanterior or submentovertex plain radiographic views, or CT. Intraoral images may, given their higher resolution, reveal fractures that extraoral plane images may fail to reveal.
The margins of fracture planes usually appear as sharply defined radiolucent lines of separation that are confined to the structure of the mandible (Fig. 29-10). They are best visualized when the x-ray beam is oriented along the plane of the fracture. Displacement of the fragments results in a cortical discontinuity or “step” (Fig. 29-11) or an irregularity in the occlusal plane. Occasionally, the margins of the fracture overlap each other, resulting in an area of increased radiopacity at the fracture site.

FIG. 29-10 Cropped panoramic image shows a fracture through the right parasymphyseal region and a condylar neck fracture on the same side. Note the step defect on the posterior surface of the mandibular ramus.
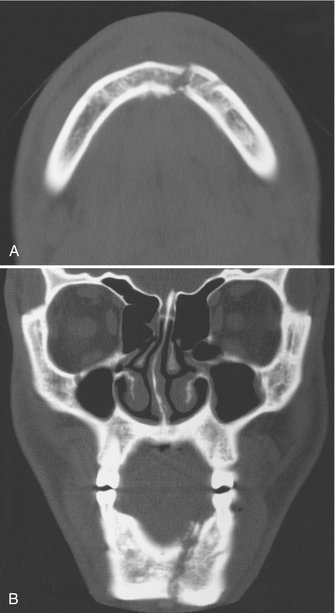
FIG. 29-11 CT images show a minimally displaced mandibular parasymphyseal fracture in the axial (A) and coronal (B) planes.
Nondisplaced mandibular fractures may involve one or both buccal and lingual cortical plates. An incomplete fracture involving only one cortical plate is often called a greenstick fracture; these usually occur in children. An oblique fracture that involves both cortical plates may cause some diagnostic difficulties if the fracture lines in the buccal and lingual plates are not superimposed (Fig. 29-12). In this case, two lines are seen that converge at the periphery, suggesting two distinct fractures when in reality only one exists. A right-angle view such as an occlusal view may be useful.
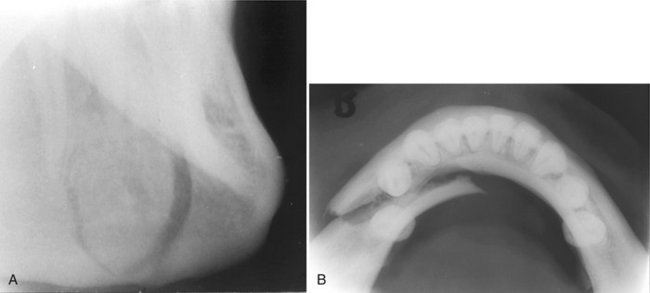
FIG. 29-12 A, A lateral oblique image of the right mandible in the premolar region shows what appears to be two fracture lines that converge at the inferior cortex. B, The true occlusal image of the mandible of the same case demonstrates only a single fracture plane. Therefore the two lines seen in A reflect the obliquity of the fracture plane relative to the x-ray beam.
Differential Diagnosis
The superimposition of soft tissue images on the image of the mandible may simulate fractures. A narrow air space between the dorsal surface of the tongue and the soft palate superimposed across the angle of the mandible in a panoramic image may simulate a fracture. The air space between the dorsal surface of the tongue and the posterior pharyngeal wall can appear similar to a fracture on lateral views of the mandible. Similar appearances can occur in the region of soft palate where it superimposes over the ramus.
Management
The management of a fracture of the mandible presents a variety of surgical problems that involve the proper reduction, fixation, and immobilization of the fractured bone fragments. Minimally displaced fractures are managed by closed reduction and intermaxillary fixation, whereas fractures with more severely displaced fragments may require open reduction. Treatment for fractures of the body often includes antibiotic therapy because a tooth root may be in the line of the fracture. When the fracture line involves third molars, severely mobile teeth, or teeth with at least half their roots exposed in the fracture line, the involved teeth are often extracted to reduce the risk of infection and problems with fixation.
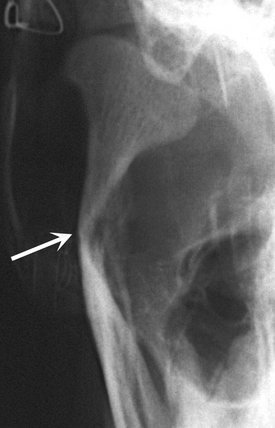
Definition
Fractures involving the mandibular condyle can be divided into condylar neck fractures and condylar head fractures. Condylar neck fractures are more common and are located below the condylar head. When a condylar neck fracture occurs, the head is usually displaced medially, inferiorly, and anteriorly as a result of contraction of the lateral pterygoid muscle (Figs. 29-13 and 29-14). Fractures of the condylar head may result in a vertical cleft dividing the condylar head fragments or may produce multiple fragments in a compression-like injury. Almost half the patients with condylar fractures also have fractures in the mandibular body.
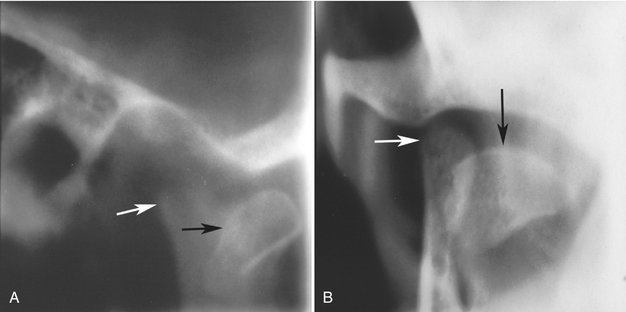
FIG. 29-13 Corrected sagittal and coronal multidirectional tomographic images of a fractured condylar head. The condylar head has been displaced anteriorly (black arrow) in the sagittal view (A) and medially (black arrow) in the coronal view (B) as a result of contraction of the lateral ptyergoid muscle. The residual condylar neck (white arrow in both images) can be seen.
Clinical Features
The clinical symptoms of a fractured condylar head are not always apparent, so the preauricular area must be carefully examined and palpated. The patient may have pain on opening or closing the mouth or trismus from local swelling. An anterior open bite may be present with only distal molar contacts and there may be deviation of the mandible on opening. A significant feature may be the inability of the patient to protrude the mandible because the lateral pterygoid muscle is attached to the condyle.
Radiographic Features
Nondisplaced fractures of the condylar process may be difficult to detect on plain radiographic or panoramic images. CT is the imaging modality of choice because it will enable the clinician to visualize the three-dimensional relationship of the displaced condylar head to the glenoid fossa and to adjacent anatomical structures in the skull base and infratemporal fossa (Figs. 29-15 and 29-16).

FIG. 29-15 An example of CT images of bilateral condylar neck fractures showing medial displacement of the condylar heads in line with the lateral pterygoid muscles in the axial image (A) and medial displacement in the coronal images (B and C); also in C there is osseous ankylosis between the residual condylar neck and the temporal bone.
Studies of remodeled previously fractured condyles show that young persons have much greater remodeling potential than do adults. In children younger than 12 years, most fractured condyles show a radiographic return to normal morphology after healing, whereas in teenagers the remodeling is less complete. In adults, only minor remodeling is observed. The extent of remodeling is also greater with fractures of the condylar head than with condylar neck fractures with displacement of the condylar head. The most common deformities are medial inclination of the condyle, abnormal shape of the condyle, shortening of the neck, erosion, and flattening. Early condylar fractures commonly result in hypoplasia of the ipsilateral side of the mandible.
Management
The technical details of treating condylar fractures vary according to whether one or both condyles are involved, the extent of displacement, and the occurrence and severity of concomitant fractures. The treatment is directed to relieve acute symptoms, restore proper anatomic relationships, and prevent bony ankylosis. If a malocclusion develops, intermaxillary fixation may be provided in an attempt to restore proper occlusion. Often condylar head and neck fractures are not reduced because of the morbidity of the procedure and the size and position of the fracture fragments.
Definition
Simple fractures of the alveolar process may involve the buccal or lingual cortical plates of the alveolar processes of the maxillae or mandible. Commonly these fractures are associated with traumatic injuries to teeth that are luxated with or without dislocation. Several teeth are usually affected, and the fracture plane is most often horizontally oriented. Some fractures extend through the entire alveolar process (in contrast to the simple fracture that involves only one cortical plate), and the fracture plane may be located apical to the teeth or involve the tooth socket. These are also commonly associated with dental injuries and extrusive luxations with or without root fractures.
Clinical Features
A common location of alveolar fractures is the anterior maxilla. Simple alveolar fractures are relatively rare in the posterior segments of the arches. In this location, fracture of the buccal plate usually occurs during removal of a maxillary posterior tooth. Fractures of the entire alveolar process occur in the anterior and premolar regions and in an older age group.
A characteristic feature of an alveolar process fracture is marked malocclusion with displacement and mobility of the fragment, and when the practitioner tests the mobility of a single tooth, the entire fragment of bone moves. The teeth in the fragment will have a recognizable dull sound when percussed and the attached gingiva may have lacerations. The detached bone may include the floor of the maxillary sinus, in which case bleeding from the nose on the involved side may occur as well as ecchymosis of the buccal vestibule.
Radiographic Features
Periapical radiographs, if they can be made, will often not reveal fractures of a single cortical wall of the alveolar process, although evidence exists that the teeth have been luxated. However, a fracture of the anterior labial cortical plate may be apparent on an occlusal radiograph or on a lateral extraoral image of the mandible if bone displacement has occurred and the x-ray beam is oriented at near right angles to the direction of bone displacement. Fractures of both cortical plates of the alveolar process are usually apparent (Fig. 29-17).

FIG. 29-17 These two images demonstrate an alveolar process fracture extending from the distal aspect of the mandibular right cuspid in an anterior direction (arrows) and through the tooth socket of the right central incisor.
The closer the fracture is to the alveolar crest, the greater the possibility that root fractures are present. It may be difficult to differentiate a root fracture from an overlapping fracture line of the alveolar bone. Several images produced with different projection angles may help with this differentiation. If the fracture plane is truly associated with the tooth, the line should not shift relative to the tooth. Fractures of the posterior alveolar process may involve the floor of the maxillary sinus and result in abnormal thickening of the sinus mucosa or the accumulation of blood and sinus secretions, in which case an air-fluid level may be appreciated.
Management
Fractures of the alveolar process are treated by repositioning the displaced teeth and associated bone fragments with digital pressure. Gingival lacerations are sutured. If the luxated permanent teeth are splinted and stable, intermaxillary fixation may not be necessary. Teeth that have lost their vascular supply may eventually require endodontic treatment.
A soft diet for 10 to 14 days is recommended. Antibiotic coverage is provided because of communication with tooth sockets.
MIDFACIAL FRACTURES INCLUDING MAXILLARY FRACTURES
Definition
The blow-out fracture is generated as a result of a direct blow to the orbit by an object that is too large to enter the orbital cavity, such as a fist or a baseball. In this fracture, one or more of the walls of the orbit are damaged, but the orbital rim remains intact. The most common fractures involve the medial wall of the orbit formed by the lamina papyracea of the ethmoid bone and the floor of the orbit that separates this space from the maxillary sinus.
Clinical Features
Periorbital edema is a common feature of the orbital blow-out fracture, as is enophthalmos. Eye movements may be restricted if one or more of the periorbital muscles becomes entrapped in the bony defect created by the fracture. If the ethmoid air cells are involved, there may be epistaxis.
Radiographic Features
The Waters view or CT (Fig. 29-18) may demonstrate a discontinuity of the lamina papyracea in a medial wall blow-out fracture or the accumulation of soft tissue in the roof of the maxillary sinus in an orbital floor blow-out. Coronal CT may show the classic “trap door” appearance of the displaced orbital floor to best advantage. Soft tissue CT images will show soft tissue densities or air-fluid levels in the adjacent ethmoid air cells (Fig. 29-18) or maxillary sinus or herniation of periorbital fat and entrapment of periorbital muscle through the bony defect in the orbital floor.
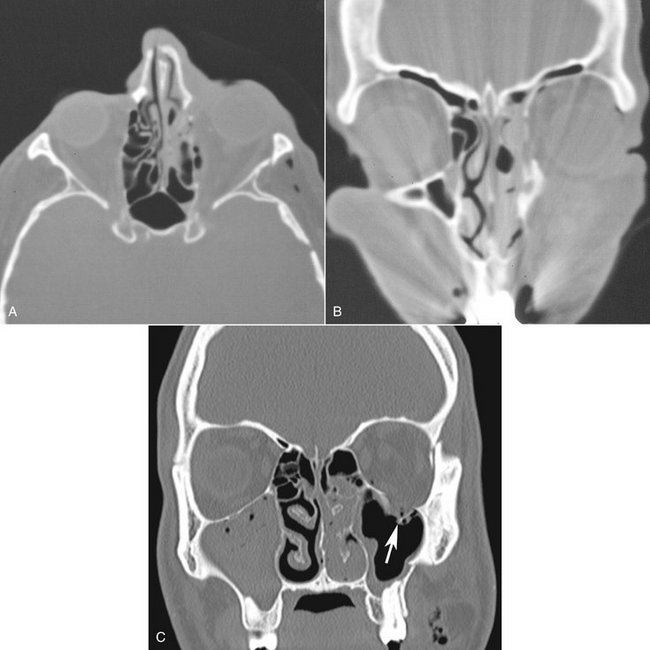
FIG. 29-18 CT images show fractures of the lamina papyracea of the left ethmoid bone in the axial (A) and coronal (B) planes. Note the fluid/soft tissue densities in the adjacent ethmoid air cells. C, This coronal CT image demonstrates a blow-out fracture of the orbit; note the discontinuity in the floor of the orbit and herniation of soft tissue into the maxillary sinus (arrow).
Management
Surgical repair may be attempted for patients who have severely affected eye movements as a result of muscle entrapment or unacceptable enopthalmos.
Definition
Unilateral fractures involving the zygomatic bone may include tripod fractures, in which the zygomatic bone and adjacent areas of the maxillary, frontal, sphenoid, and temporal bones may be involved, or zygomatic arch fractures, in which the zygomatic process of the temporal bone is fractured. Bilateral zygomatic fractures can occur in association with Le Fort type II and III fractures (described in the following section).
Injuries to the zygomatic bone or arch usually result from a forceful blow to the cheek or side of the face. Although zygomatic bone injuries may displace the fragment(s) medially, support by the adjacent temporalis and masseter muscles may limit displacement.
Clinical Features
Flattening of the upper cheek with tenderness and dimpling of the skin over the side of the face may occur, although some of the clinical characteristics of zygomatic fractures may not be apparent much longer than an hour after trauma because they may be masked by edema. In most cases, periorbital ecchymosis and hemorrhage into the sclera (near the outer canthus) occur. Additional symptoms may include unilateral epistaxis (for a short time after the accident), anesthesia or paresthesia of the cheek, and compromised eye movements. The presence of diplopia suggests a significant injury to the floor of the orbit. Mandibular movement may be limited if the displaced zygomatic bone impinges on the coronoid process.
Radiographic Features
Because of edema obscuring the clinical features, the radiographic examination may provide the only means of determining the presence and extent of the injury. The occipitomental (Waters) view provides a good image of the zygomatic bone and midface that will show the displaced fracture fragment (Fig. 29-19). An underexposed submentovertex projection (the so-called jug-handle view) provides a good view of the zygomatic arch and can often show the V-shaped deformity of the zygomatic process of the temporal bone. CT is, however, the imaging modality of choice for these fractures (Fig. 29-20).

FIG. 29-19 Waters view shows a tripod fracture involving the right zygomatic bone. Note the fracture through the right orbital rim and lateral wall of the maxillary sinus. As well, there is radiopacification of the right maxillary sinus.

FIG. 29-20 Axial (A) and coronal (B) CT images show depression and rotation of a left tripod fracture. An air-fluid level is also visible in the left maxillary sinus.
The zygomatic arch may fracture at its weakest point, about 1 cm posterior to the zygomaticotemporal suture. Separation or fracture of the frontozygomatic suture may also occur. Fractures do not usually occur through the zygomaticomaxillary suture; however, in some cases, a fracture plane may extend obliquely involving the inferior rim of the orbit and the lateral wall of the maxilla. If the fracture plane involves the maxillary sinus, the sinus may exhibit increased radiopacity as a result of the accumulation of blood and mucus secretions, an air-fluid level.
Panoramic images of the zygomatic arch often reveal the zygomaticotemporal suture as a radiolucent line that may even have the appearance of a discontinuity in the inferior border. This is a variation of normal anatomy and should not be misinterpreted as a fracture.
Management
When symptoms include minimal displacement of the zygomatic arch and no cosmetic deformity or impairment of eye movement, no treatment may be required. Otherwise, reduction is usually indicated. Fractures of the zygomatic bone and arch may be reduced through an intraoral or extraoral approach.
LE FORT FRACTURES
Complex fractures involving multiple facial bones may be quite variable but often follow general patterns classified by the French surgeon Rene Le Fort. By definition, all Le Fort fractures include fractures of one of the pterygoid plates of the sphenoid bone, and although Le Fort fractures may be bilateral, they are most often unilateral.
The radiographic interpretation of fractures of the midface is difficult because of the complex anatomy in this region and the multiple superimpositions of structures. CT is the diagnostic imaging method of choice for complex facial fractures. CT imaging provides multiple image slices in orthogonal planes through the face, allowing for the display of osseous structures without the complication of overlapping anatomy that is problematic with plane radiography. CT also provides suitable image detail to detect secondary changes associated with trauma, including herniation of orbital fat and extraocular muscle, soft tissue swelling or emphysema, and blood/fluid accumulation. As an aid in determining the spatial orientation of fractures or bone fragments, the CT images may be reformatted so that three-dimensional images may be evaluated.
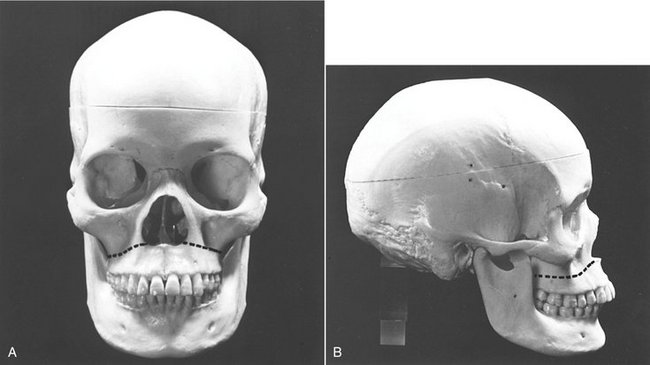
Definition
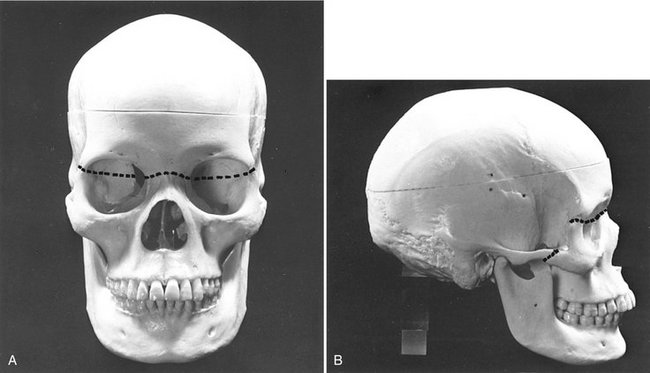
The Le Fort I fracture is a relatively horizontal fracture in the body of the maxilla that results in detachment of the alveolar process and adjacent bone of the maxilla from the middle face. This fracture is the result of a horizontally directed traumatic force directed posteriorly at the base of the nose. The fracture plane passes superior to the roots of the teeth and nasal floor and posteriorly through the base of the maxillary sinus and the tuberosity to the pterygoid processes (Fig. 29-21). In the unilateral fracture, an auxiliary fracture exists in the midline of the palate. The unilateral fracture must be distinguished from a fracture within the alveolar process (discussed previously) that does not extend to the midline or involve the ptyergoid plates posteriorly. Fractures of the mandible (54%) and zygomatic bone (23%) may also be found in these patients.
Clinical Features
If the fragment is not distally impacted, it can be manipulated by holding onto the teeth. If the fracture line is at a high level, the fragment may include the pterygoid muscle attachments, which pull the fragment posteriorly and inferiorly. As a result, the posterior maxillary teeth contact the mandibular teeth first, resulting in an anterior open bite, retruded chin, and long face. If the fracture is at a low level, no displacement may occur. Other symptoms may include associated swelling and bruising about the eyes, pain over the nose and face, deformity of the nose, and flattening of the middle of the face. Epistaxis is inevitable, and occasionally double vision and varying degrees of paresthesia over the distribution of the infraorbital nerve may occur. Manipulation may reveal a mobile maxilla and crepitation.
Radiographic Features
CT imaging will reveal an air-fluid level or radiopacification in the maxillary sinus (Fig. 29-22, A). Coronal images may reveal the plane of the fracture extending posteriorly through the maxilla, whereas coronal or axial images together may reveal involvement of the pterygoid plates posteriorly. Three-dimensional reconstructions of the CT data set may show the plane of the fracture to greatest advantage (Fig. 29-22, B).
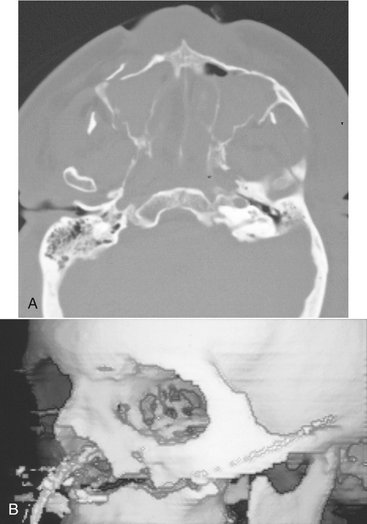
FIG. 29-22 A, Axial image of Le Fort I fractures involving the anterior and posterolateral walls of the right and left maxilla and the pterygoid plates. Radiopacification of the maxillary sinuses is also seen with a small retained collection of air in the left maxillary sinus. B, Three-dimensional reconstruction of the image data shows extension of the fracture plane from above the base of the nose posteriorly through the maxillary tuberosity.
Management
If the fracture is not displaced and is at a relatively low level in the maxilla, it can be treated by intermaxillary fixation. Those that are high, with the fragment displaced posteriorly or with pronounced separation, require craniomaxillary fixation in addition to intermaxillary fixation.
Definition
The Le Fort II fracture has a pyramidal shape on posteroanterior skull images, hence the name. It results from a violent force applied posteriorly and superiorly through the base of the nose. This force separates the maxilla from the base of the skull. The fracture plane extends from the bridge of the nose inferiorly, laterally, and posteriorly through the nasal and lacrimal bones, the orbital floor and inferior rim obliquely, and inferiorly across the maxilla and posteriorly to the pterygoid processes (Figs. 29-23 and 29-24). The frontal and ethmoid sinuses are involved in about 10% of cases, especially in severe comminuted fractures.
Clinical Features
In contrast to the Le Fort I fracture, which may be characterized by only slight swelling about the upper lips, the Le Fort II injury results in massive edema and marked swelling of the middle third of the face. Typically, ecchymosis develops around the eyes within minutes of the injury. The edema is likely to be so severe that it is impossible to see the globes. The conjunctivas over the inner quadrants of the eyes are bloodshot, and if the zygomatic bones are involved, this ecchymosis extends to the outer quadrant.
The broken nose is displaced because the face has fallen, and the nose and face are lengthened. An anterior open bite occurs. Epistaxis is inevitable, and cerebrospinal fluid rhinorrhea may also result. Palpation reveals the discontinuity of the lower borders of the orbits. By applying pressure between the bridge of the nose and the palate, the “pyramid” of bone can be moved. Other common symptoms include double vision and variable degrees of paresthesia over the distribution of the infraorbital nerve.
Radiographic Features
The radiographic examination reveals fractures of the nasal bone, frontal process of the maxilla, infraorbital rim, and orbital floor. More inferiorly and posteriorly, there would be involvement of the zygomatic bone or zygomatic process of the maxilla, separation of the zygomaticomaxillary suture, and fracture of the lateral wall of the maxillary sinus and the pterygoid plates. Involvement of the ethmoid air cells, and frontal and maxillary sinuses, would result in thickening of the sinus mucosa or the accumulation of blood-fluid levels in the air spaces. CT is the imaging modality of choice for such complex fractures.
Management
The treatment of this fracture is accomplished by reduction of the displaced maxilla by intermaxillary fixation, open reduction, and interosseous wiring of the infraorbital rims and plating of the accompanying fractures of the nose, nasal septum, and orbital floor. Repair of the detached medial canthal ligaments may also be required. Leakage of cerebrospinal fluid requires the attention of a neurosurgeon if the posterior or superior walls of the frontal sinuses are involved.
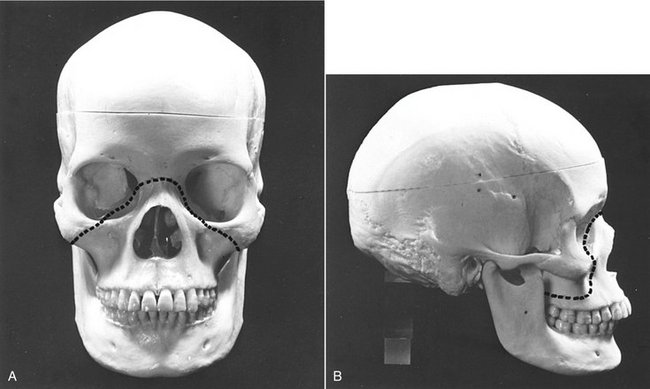
Definition
A Le Fort III midface fracture results when the traumatic force is of sufficient magnitude to completely separate the middle third of the facial skeleton from the cranium. The fracture plane usually extends from the nasal bone and frontal process of the maxilla or nasofrontal and maxillofrontal sutures, across the orbital floor, through the ethmoid air cells and sphenoid sinus to the zygomaticofrontal sutures (Fig. 29-25). More posteriorly and inferiorly, the fracture plane passes across the pterygomaxillary fissure and separates the bases of the pterygoid plates from the sphenoid bone. If the maxilla is displaced and freely movable, a fracture must also have occurred in the area of the zygomaticotemporal suture. Because the zygomatic bone or zygomatic arch is involved, these injuries are, as a rule, associated with multiple other maxillary fractures. Mandibular fractures are also observed in half the cases.
Clinical Features
Craniofacial disjunction produces a clinical appearance similar to that of a pyramidal fracture. However, this injury is considerably more extensive. The soft tissue injuries are severe, with massive edema. The nose may be blocked with blood or blood clot, or cerebrospinal fluid rhinorrhea may be present. Bleeding may occur into the periorbital tissues and the conjunctiva, and a number of eye signs of neurologic importance are likely to be present. A “dished-in” or concave deformity of the face is characteristic of this fracture pattern, as is an anterior open bite because of the retroclined positions of the maxillary incisors with only the posterior teeth in occlusion. Even on mandibular opening, the patient is unable to separate the molars. Intraoral and extraoral palpation reveals irregular contours and step deformities, and crepitation is also apparent when the fragments are moved.
Radiographic Features
It is virtually impossible to document these multiple fractures with plain films. Therefore CT images in concert with the clinical information are required. The main radiographic findings are distractions of the frontonasal, frontomaxillary, zygomaticofrontal, and zygomaticotemporal sutures and fractures through the nasal bone, frontal process of the maxilla, orbital floor, and pterygoid plates (Fig. 29-26). Associated fractures involving the walls of all the paranasal sinuses will result in radiopaque air-fluid levels with mucosal thickening. Three-dimensional reconstructions show the fracture planes and the large bone fragments (Fig. 29-26, D and E).
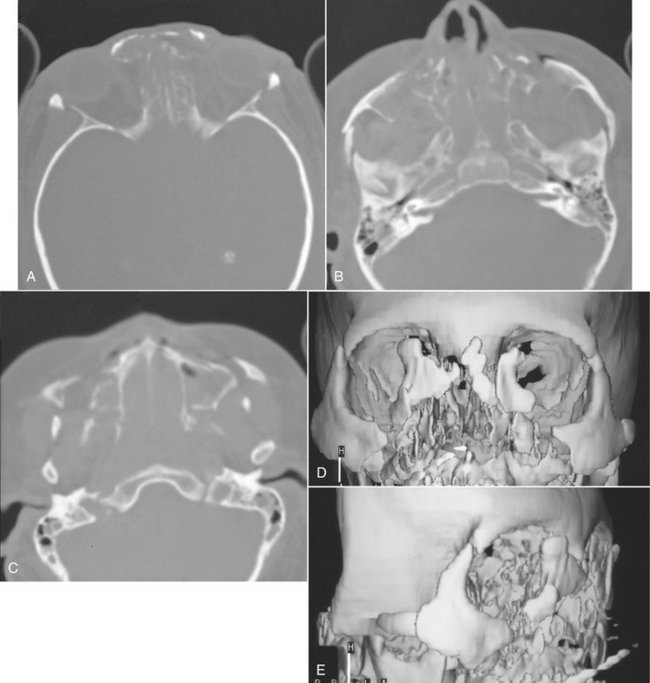
FIG. 29-26 Axial CT images showing a bilateral Le Fort III fracture with distractions of frontonasal (A), frontomaxillary, zygomaticofrontal, and zygomaticotemporal sutures (B) and fractures of nasal bone, frontal process of the maxilla, orbital floor, and pterygoid plates (C). Note the near-total radiopacification of the maxillary sinuses. Three-dimensional reconstructions, frontal view (D) and lateral view (E), of the axial CT images reveal substantial fragmentation of the periorbital bones, zygomatic bone, and arch, posteriorly.
Management
The associated severe soft tissue injury necessitates airway management, initial hemorrhage control, and repair of lacerations. Surgery may be delayed until the edema has sufficiently resolved. The treatment of transverse fractures is complicated because fixation of the loose middle third of the facial skeleton is difficult because of the fact that fractures of the zygomatic arch occur. The only possibilities are external immobilization or immobilization within the tissues. In the former, the loose maxilla is suspended by wires through the cheeks from a metal head frame (halo) or fixed by external pins anchored in bone. The other possibility is immobilization within the tissues by using internal wiring to the closest solid bone superior to the fracture. A number of complications may develop during or after this treatment.
Monitoring the Healing of Fractures
Radiographic examination of the facial bones after trauma is usually necessary to measure the degree of reduction from treatment and to monitor the continued immobilization of the fracture site during repair. Typically, monitoring of this type is accomplished by use of plain radiography. The monitoring of fracture repair should include examination of both the alignment of the cortical plates of the involved bone and remodeling and remineralization of the fracture site. During normal healing the fracture line increases in width about 2 weeks after reduction of the fracture. This results from the resorption of the fractured ends and small sequestered fragments of bone. Evidence of remineralization usually occurs 5 to 6 weeks after treatment. Unlike the long bones of the skeleton, rarely is a callus formed in healing jaw fractures. The complete remodeling of the fracture site with obliteration of the fracture line may take several months. On rare occasions, fracture lines may persist for years, even when the patient has made a clinically complete recovery. Possible complications of healing include malalignment of the fracture segments and inflammatory lesions related to nonvital teeth near or in the line of the fracture. Other complications include nonunion of the fractured segments seen as increased width of fracture line, cortication of the fractured surfaces, and rounding of the sharp edges of the segments. The development of osteomyelitis of the fracture site will appear as an increase in sclerosis of the surrounding bone, inflammatory periosteal new bone, and development of sequestra.
Brook, IW, Wood, N. Aetiology and incidence of facial fractures in adults. Int J Oral Surg. 1983;12:293–298.
Daffner, RH. Imaging of facial trauma. Curr Probl Diagn Radiol. 1997;26:153–184.
Dingman, TM, Natvig, AC. Surgery of facial fractures. Philadelphia: WB Saunders; 1967.
Gerlock, AJ, Jr., Sinn, DP, McBride, KL. Clinical and radiographic interpretation of facial fractures. Boston: Little, Brown; 1981.
Hunter, JG. Pediatric maxillofacial trauma. Pediatr Clin North Am. 1992;39:1127–1143.
Kaban, LB. Diagnosis and treatment of fractures of the facial bones in children 1943-1993. J Oral Maxillofac Surg. 1993;51:722–729.
Koltai, PJ, Rabkin, D. Management of facial trauma in children. Pediatr Clin North Am. 1996;43:1253–1275.
Laine, FJ, Conway, WF, Laskin, DM. Radiology of maxillofacial trauma. Curr Probl Diagn Radiol. 1993;22:145–188.
Matteson, SR, Deahl, ST, Alder, ME, et al. Advanced imaging methods. Crit Rev Oral Biol Med. 1996;7:346–395.
Matteson, SR, Tyndall, DA. Pantomographic radiology. Part II. Pantomography of trauma and inflammation of the jaws. Dent Radiogr Photogr. 1983;56:21–48.
Newman, J. Medical imaging of facial and mandibular fractures. Radiol Technol. 1998;69:417–435.
Shumrick, KA. Recent advances and trends in the management of maxillofacial and frontal trauma. Facial Plast Surg. 1993;9:16–28.
Andreasen, JO. Traumatic injuries of the teeth. Philadelphia: WB Saunders; 1981.
Andreasen, JO, Andreasen, FM, Skeie, A, et al. Effect of treatment delay upon pulp and periodontal healing of traumatic dental injuries—a review article. Dent Traumatol. 2002;18:116–128.
Josell, SD, Abrams, RG. Traumatic injuries to the dentition and its supporting structures. Pediatr Clin North Am. 1982;29:717–741.
Andreasen, JO. Luxation of permanent teeth due to trauma: a clinical and radiographic follow-up study of 189 injured teeth. Scand J Dent Res. 1970;78:273–286.
Donaldson, M, Kinirons, MJ. Factors affecting the time of onset of resorption in avulsed and replanted incisor teeth in children. Dent Traumatol. 2001;17:205–209.
Ravn, JJ. Follow-up study of permanent incisors with enamel fractures as a result of acute trauma. Scand J Dent Res. 1981;89:213–217.
Ravn, JJ. Follow-up study of permanent incisors with enamel-dentin fracture after acute trauma. Scand J Dent Res. 1981;89:355–365.
Stockton, LW, Suzuki, M. Management of accidental and iatrogenic injuries to the dentition. J Can Dent Assoc. 1998;64:378–382.
Fox, K, Youngson, CC. Diagnosis and treatment of the cracked tooth. Prim Dent Care. 1997;4:109–113.
Turp, JC, Gobetti, JP. The cracked tooth syndrome: an elusive diagnosis. J Am Dent Assoc. 1996;127:1502–1507.
Cvek, M, Mejare, I, Andreason, JO. Healing and prognosis of teeth with intra-alveolar fractures involving the cervical part of the root. Dent Traumatol. 2002;18:57–65.
Hovland, EJ. Horizontal root fractures: treatment and repair. Dent Clin North Am. 1992;36:509–525.
Luebke, RG. Vertical crown-root fractures in posterior teeth. Dent Clin North Am. 1984;28:883–894.
Majorana, A, Pasini, S, Bardellini, E, et al. Clinical and epidemiological study of traumatic root fractures. Dent Traumatol. 2002;18:77–80.
Schetritt, A, Steffensen, B. Diagnosis and management of vertical root fractures. J Can Dent Assoc. 1995;61:607–613.
Schmidt, BL, Stern, M. Diagnosis and management of root fractures and periodontal ligament injury. J Calif Dent Assoc. 1996;24:51–55.
Walton, RE, Michelich, RJ, Smith, GN. The histopathogenesis of vertical root fractures. J Endodont. 1984;10:48–56.
Wright, EF. Diagnosis, treatment, and prevention of incomplete tooth fractures. Gen Dent. 1992;40:390–399.
COMPUTED TOMOGRAPHY OF JAW FRACTURES
Creasman, CN, Markowitz, BL, Kawamoto, HK, Jr., et al. Computed tomography versus standard radiography in the assessment of fractures of the mandible. Ann Plast Surg. 1992;29:109–113.
Johnson, DH. CT of maxillofacial trauma. Radiol Clin North Am. 1984;22:131–144.
Kassel, EE, Noyek, AM, Cooper, PW. CT in facial trauma. J Otolaryngol. 1983;12:2–15.
Marsh, JL, Vannier, MW, Gado, M, et al. In vivo delineation of facial fractures: the application of advanced medical imaging technology. Ann Plast Surg. 1986;17:364–376.
Raustia, AM, Pyhtinen, J, Oikarinen, KS, et al. Conventional radiographic and computed tomographic findings in cases of fracture of the mandibular condylar process. J Oral Maxillofac Surg. 1990;48:1258–1264.
Bailey, BJ, Clark, WD. Management of mandibular fractures. Ear Nose Throat J. 1983;62:371–378.
Chayra, GA, Meador, LR, Laskin, DM. Comparison of panoramic and standard radiographs for the diagnosis of mandibular fractures. J Oral Maxillofac Surg. 1986;44:677–679.
Clark, WD. Management of mandibular fractures. Am J Otolaryngol. 1992;13:125–132.
III Ellis, E, Moos, KF, El-Attar, A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg. 1985;59:120–129.
Olson, RA, Fonseca, RJ, Zeitler, DL, et al. Fractures of the mandible: a review of 580 cases. J Oral Maxillofac Surg. 1982;40:23–28.
Reiner, SA, Schwartz, DL, Clark, KF, et al. Accurate radiographic evaluation of mandibular fractures. Arch Otolaryngol Head Neck Surg. 1989;115:1083–1085.
Winstanley, RP. The management of fractures of the mandible. Br J Oral Maxillofac Surg. 1984;22:170–177.
Consensus Conference on Open or Closed Management of Condylar Fractures, 12th ICOMS, Budapest, 1995. Int J Oral Maxillofac Surg. 1998;27:243–267.
Dahlström, L, Kahnberg, KE, Lindahl, L. 15 year follow-up on condylar fractures. Int J Oral Maxillofac Surg. 1989;18:18–23.
Dimitroulis, G. Condylar injuries in growing patients. Aust Dent J. 1997;42:367–371.
Hall, MB. Condylar fractures: surgical management. J Oral Maxillofac Surg. 1994;52:1189–1192.
Hayward, JR, Scott, RF. Fractures of the mandibular condyle. J Oral Maxillofac Surg. 1993;51:57–61.
Sahm, G, Witt, E. Long-term results after childhood condylar fractures: a computer-tomographic study. Eur J Orthod. 1989;11:154–160.
Silvennoinen, U, Iizuka, T, Lindqvist, C, et al. Different patterns of condylar fractures: an analysis of 382 patients in a 3-year period. J Oral Maxillofac Surg. 1992;50:1032–1037.
Walker, RV. Condylar fractures: nonsurgical management. J Oral Maxillofac Surg. 1994;52:1185–1188.
FRACTURES OF THE ALVEOLAR PROCESS
Andreasen, JO. Fractures of the alveolar process of the jaw: a clinical and radiographic follow-up study. Scand J Dent Res. 1970;78:263–272.
Giovannini, UM, Goudot, P. Radiologic evaluation of mandibular and dentoalveolar fractures. Plast Reconstr Surg. 2002;109:2165–2166.
Banks, P. Kiley’s fractures of the middle third of the facial skeleton. Bristol, UK: Wright; 1981.
Close, LG. Fractures of the maxilla. Ear Nose Throat J. 1983;62:365–370.
Luce, EA. Developing concepts and treatment of complex maxillary fractures. Clin Plast Surg. 1992;19:125–131.
Marciani, RD. Management of midface fractures: fifty years later. J Oral Maxillofac Surg. 1993;51:960–968.
Teichgraeber, JF, Rappaport, NJ, Harris, JH, Jr. The radiology of upper airway obstruction in maxillofacial trauma. Ann Plast Surg. 1991;27:103–109.
Tung, TC, Chen, YR, Santamaria, E, et al. Dislocation of anatomic structures into the maxillary sinus after craniofacial trauma. Plast Reconstr Surg. 1998;101:1904–1908.
Fujii, N, Yamashiro, M. Classification of malar complex fractures using computed tomography. J Oral Maxillofac Surg. 1983;41:562–567.
McLoughlin, P, Gilhooly, M, Wood, G. The management of zygomatic complex fractures—results of a survey. Br J Oral Maxillofac Surg. 1994;32:284–288.
Prendergast, ML, Wildes, TO. Evaluation of the orbital floor in zygoma fractures. Arch Otolaryngol Head Neck Surg. 1988;114:446–450.
Sands, T, Symington, O, Katsikeris, N, et al. Fractures of the zygomatic complex: a case report and review. J Can Dent Assoc. 1993;59:749–755.
Winstanley, RP. The management of fractures of the zygoma. Int J Oral Surg. 1981;10(1 Suppl):235–240.