Craniofacial growth, diagnosis and treatment planning
Craniofacial growth: A clinical perspective
Patient interview (Questionnaire)
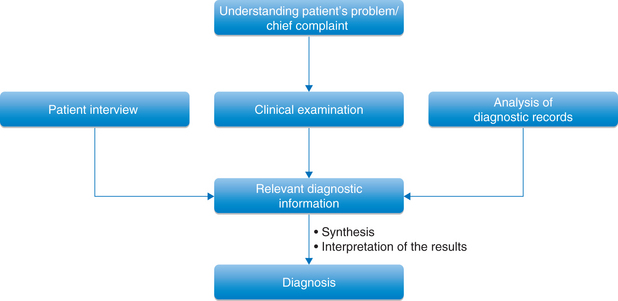
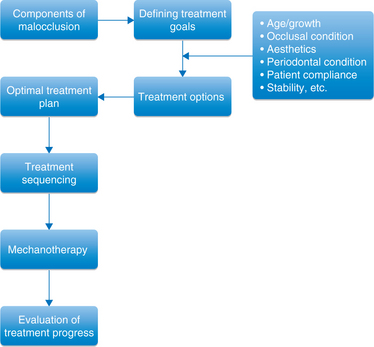
Advances in diagnostic technology, appliance design innovations and expansion of practises to include diverse patient populations have transformed the face of orthodontics over the past several years. These have resulted in ever increasing levels of well-conceived efficient and customized care, while simultaneously increasing the challenge of designing a treatment plan appropriate for each individual patient. Accurate diagnosis is a key element in the design of any successful treatment plan.
Diagnosis in orthodontics, like in other disciplines of dentistry and medicine, is the recognition of abnormal conditions, the practical synthesis of the diagnostic information that helps the clinician to plan an appropriate treatment strategy. A well-designed questionnaire for patient interview, numerous clinical observations, individual findings and analysis of relevant diagnostic records are essential to establish a correct diagnosis. It is a scientific procedure and does not offer any scope for individual opinion or judgment. The information generated must be objective, relevant and accurate.
This information is sourced from patient history – both dental and medical examinations, clinical examination and functional analysis. As a part of a routine examination, it is supplemented with the findings of the analysis of various diagnostic records like lateral cephalometric analysis. Certain cases may require further examination methods or specialized diagnostic records to generate additional information about a specific area. These various individual findings must be properly synthesized to result into a summary of the most important findings, devoid of any insignificant information having no relevance to the treatment. The clinician's ability to interpret and synthesize the relevant data is a key to establish comprehensive diagnosis. Improper or inaccurate diagnosis is often caused by insufficient information or predetermined decisions made in an effort to adapt the case to a particular type of treatment modality.
This requires that the practitioner should also have adequate knowledge about the craniofacial growth and its clinical implications.
Craniofacial growth: a clinical perspective
Majority of the problems that are encountered by the orthodontist in a day-to-day clinical practise are related to growth. The difficulty in dealing with such problems may involve a failure on the part of the orthodontist to diagnose a growth and development problem or a poor patient cooperation in which the orthodontist is not given the chance to solve the problem, or it may be a growth pattern that is beyond the control of both the patient and the orthodontist. It is, therefore, essential that the clinician gives due importance to the significance and assessment of craniofacial growth while dealing with variety of clinical situations.
The orthodontic practitioner must realize that the facial pattern is not constant; it is changed during growth and is also changed by orthodontic treatment. The treatment planning process must involve proper prediction of future growth and response to treatment, which requires better understanding of facial growth. This helps the clinician to institute optimal treatment to the patient. When jaws grow, they move and carry the dentition with them. If the amount and the direction of the movement of both the jaws as a result of growth is the same, the occlusion remains unchanged. However, disproportionate growth leads to the development of a new relationship of jaws to each other. This change in jaw relationships is often associated with compensatory tooth movements in one or both the jaws. Differential growth can occur anteroposteriorly, vertically or transversely. As the changes in the face and dentition continue throughout life, the clinician must consider both the immediate outcome of the treatment and the long-term stability and the benefits of the treatment as important goals.
For better understanding of the craniofacial growth, it is important to know the sites or the location of the growth and the type of growth occurring at that location. The growth of the craniofacial complex that is relevant to the orthodontic professional can be divided into following areas:
Cranial base
The cranial base is essentially a midline structure in which the bones are formed initially in a cartilage and later transformed to bone by endochondral ossification. The changes in the cranial base take place primarily as a result of endochondral growth, mainly at various synchondrosis (Figs 1.1 and 1.2). As ossification proceeds, bands of cartilage called synchondroses remain between the centres of ossification, which subsequently get converted into bone. The midline cranial base contains four primary cartilaginous sutures or synchondroses: the intersphenoidal sutures close by birth, the intraoccipital synchondrosis closes around 5 years of age, the sphenoethmoidal synchondrosis closes around 6–7 years of age and the sphenooccipital synchondrosis closes by 13–15 years of age.
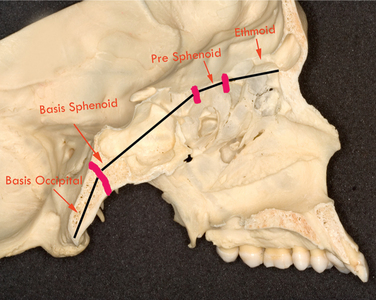
Figure 1.1 Sagittal section of the skull showing the cranial base and the approximate location of important growth sites.
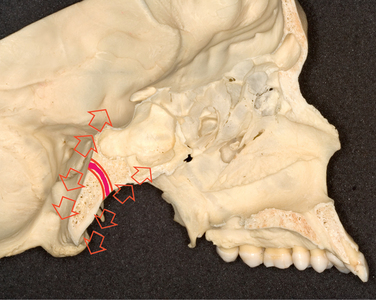
Figure 1.2 Growth at the sphenooccipital synchondrosis in which the maturing cartilage cells extend in both directions away from the centre as a part of endochondral ossification occurring at both margins. It contributes to the increase in length of this area of the cranial base.
As the sphenoethmoidal synchondrosis closes by 6–7 years of life, the segment of the anterior cranial base – designated as the planum sphenoidale – becomes relatively stable, early in life.1 Therefore, this area is usually used for cephalometric superimpositions to evaluate the changes in the face due to either growth or treatment. The sellanasion (SN) plane is frequently used as a reference plane in order to more accurately determine the changes occurring in the facial structures. The distance between sella and nasion normally increases by approximately 1 mm per year from 6 to 16 years of age. Another frequently used reference plane is nasion–basion plane. The distance between nasion and basion increases by approximately 1.7 mm per year between 6 and 16 years of age. After the closure of the sphenooccipital synchondrosis, any changes occurring either in the length or in the flexure of the cranial base are as a result of remodelling or surface deposition or resorption.2
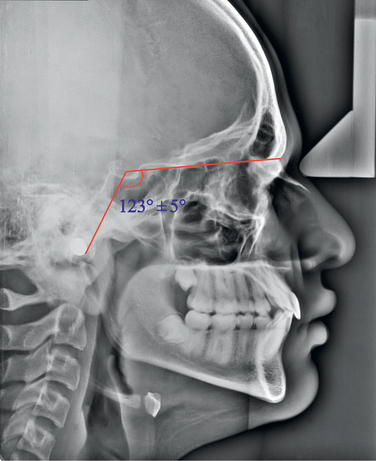
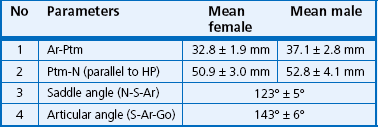
Though there are minor opening and closing movements in the cranial base angle, this angle is relatively stable for most part. The average cranial base angle is approximately 130°. Obtuse or open cranial base angles are usually associated with a more backward position of the mandible and hence a Class II type of facial pattern. A more acute or closed cranial base angle is normally associated with a more forward position of the mandible and hence a Class III type of facial pattern. The sagittal growth centre – the sphenooccipital synchondrosis – is located in the region of the posterior cranial base, and the growth changes in this area determine the position of the fossa. A large angle between the anterior and posterior cranial base, measured cephalometrically as N-S-articulare (Ar), indicates a posterior position, and a small angle indicates an anterior position of the fossa. The mean value is 123° ± 5° (Fig 1.3). This deviation in the position of the fossa is often compensated by the length of the ascending ramus. If there is no compensatory growth of the ascending ramus, this leads to either retrognathic or prognathic facial profile. Because the glenoid fossa determines the posterior/superior limit of the mandible, it holds important implications for mandibular displacement. Björk3 indicated that the distance between the fossa and the nasion increases by 7.5 mm between 12 and 20 years of age when the landmark Ar is used. As a result of the elongation of the posterior cranial base, the fossa and the temporal bone are displaced inferiorly and posteriorly.4 It was observed that the glenoid fossa was displaced between 1.8 and 2.1 mm posteriorly and between 1.0 and 1.8 mm inferiorly, and it demonstrated greater posterior and inferior displacement during adolescence than during childhood.5 Therefore, during the treatment planning process for skeletal correction, the clinician should consider posterior fossa displacements to be added to any existing anterior discrepancies and future growth deficiencies. Another important growth change that occurs in the cranial base is the remodelling that takes place in the anterior cranial fossa. This brings about a forward displacement of the frontal bone and the nasal area.6
Maxilla
The maxillary complex is surrounded by a system of sutures such as zygomaticomaxillary, frontozygomatic, sphenopalatine and pterygomaxillary. The maxilla mainly grows by bone apposition at the sutures that connect the maxilla to the cranium and the cranial base and by surface remodelling (Fig 1.4). Björk7 in his implant study carried out to evaluate the changes in the growth direction of the nasomaxillary complex between 7 and 19 years of age and observed that the maxilla grew in a downward and forward direction at an angle of approximately 51° to the anterior cranial base (SN plane) with a very large range of 0–82° (Fig 1.5). This variation explains the fact that the maxilla would grow primarily in a horizontal direction in some patients, while it would grow primarily in a vertical direction in others. It has been observed that during the first decade of life, the maxillary growth proceeds normally in a horizontal direction, while during the second decade of life, it proceeds in a more vertical direction.7

Figure 1.5 The growth of the nasomaxillary complex from 7 to 19 years of age moves it downward and forward at an average angle of 51° with the cranial base.
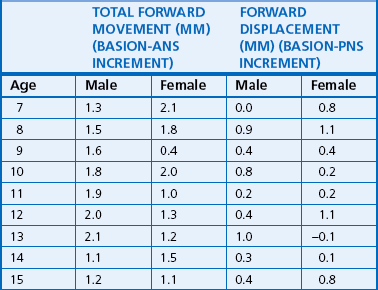
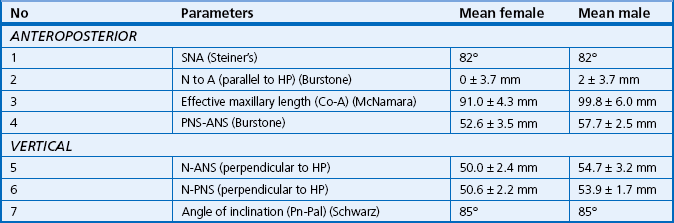
The displacement and remodelling changes play an important role in the growth of the maxilla.6 The horizontal displacement of the maxilla is primarily due to remodelling expansion within the middle cranial fossa. Also, deposition of bone on the posterior aspect of the maxilla, in the area of tuberosity, allows it to keep pace with the forward displacement of the frontal and nasal bones (as a result of expansion of the anterior cranial base) and to accommodate for the eruption of the permanent molars. The maxillary length changes are shown in Table 1.1. The vertical displacement of the maxilla occurs primarily by growth and expansion of the eyeballs and the nasal septum. The growth of the cartilaginous nasal septum, especially the vomer and the perpendicular plate of the ethmoid, carries the nasomaxillary complex downward and forward.1 At birth, the nasal septum is made up entirely of cartilage and extends down to lie within the U-shaped vomer in the vomerine groove. During the first year of life, ossification begins in the perpendicular plate of the ethmoid. By 3 years of age, ethmoid reaches the vomer, and by 10 years of age, it is in contact. After this period, the downward growth of the upper face occurs primarily by the process of apposition. On an average, the amount of this vertical displacement measured from the SN plane to the palatal plane is just over 1 mm per year.
The maxilla, as a result of remodelling changes, takes on periosteal deposits of bone on all of its surfaces. The most significant amount of bone deposition occurs on the posterior aspect of the maxilla. This, in addition to the lateral deposits, allows for lengthening of the dental arch and eruption of the upper teeth. The palate receives periosteal deposits on its oral surface and is resorbed on its nasal surface. In addition to these horizontal and vertical growth changes, the maxilla can undergo rotational change (Fig 1.6). The maxilla can rotate in a downward and forward direction anteriorly, as occurs in the anterior deep bite case, or it can rotate in an upward and forward direction, as occurs in anterior open bite case. The amount and the direction of these rotational changes can be determined by the angle between the SN plane and the palatal plane or by the angle of inclination (AM Schwarz) between the Pn line (perpendicular from N') and the palatal plane. The posterior end of the hard palate does not seem to be subjected to influence by Class III elastics.8 However, the maxillary molars may be encouraged to grow downward away from the palatal plane. Anterior end of the hard palate is easily influenced by Class II elastics and extraoral anchorage.9 Growth at the intermaxillary and interpalatine sutures, contributing mainly to the maxillary width, occurs during the first 5 years of life.
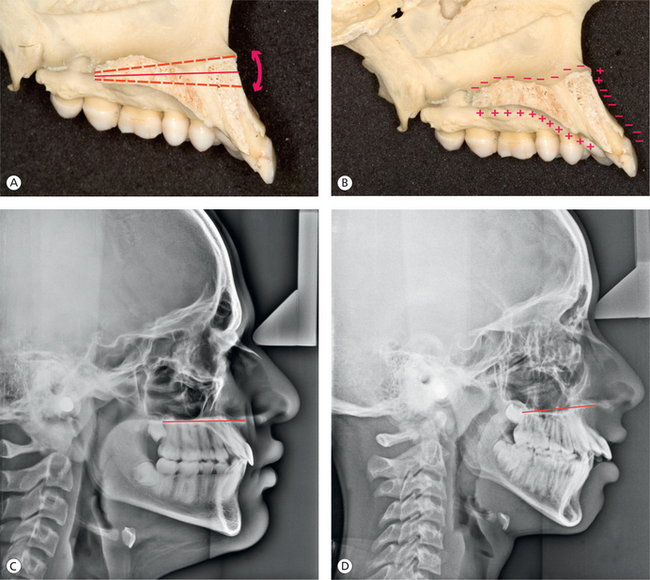
Figure 1.6 Rotational changes in the maxilla. (A) Diagrammatic representation of the rotational changes of the maxilla on the sagittal section of the skull. (B) Surface remodelling changes at the nasal floor, the roof of the mouth and the anterior surface below the anterior nasal spine. (C) Normal orientation of the palatal plane. (D) The palatal plane is tipped upward anteriorly.
Mandible
Compared with the growth of the maxilla, both endochondral and periosteal activity play an important role in growth of the mandible. For years, the condylar cartilage was considered a primary growth centre, acting in a manner similar to the epiphyseal growth plate of a long bone. However, histologically, the condylar cartilage is quite different from the cartilage of the epiphyseal growth plate. The mandible is a unique bone that grows in many different ways. It should not be considered a single growth entity but rather different entities, mainly at condyle and ramus, corpus, posterior alveolar process and anterior alveolar process. Other than condyle, all other areas of the mandible are formed and grow by direct surface apposition and remodelling.6 (Fig 1.7).
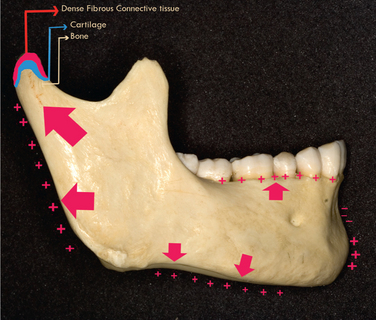
Figure 1.7 Surface remodelling changes in the mandible. Diagrammatic representation of the unique growth mechanism of the mandibular condyle showing both interstitial and appositional proliferation.
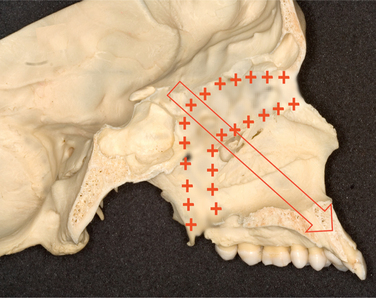
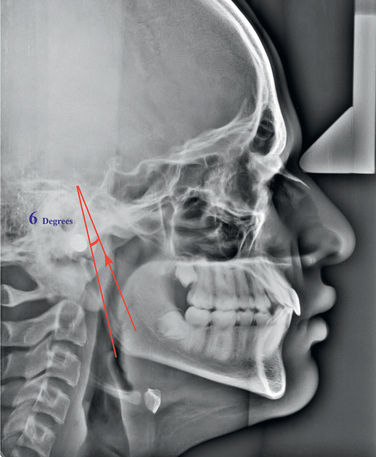
Björk10 provided an excellent information on the growth of the mandible with his implant studies. These studies revealed that average direction of condylar growth was 6° anterior to a line drawn tangent to the posterior border of the ramus (Fig 1.8). This emphasized the distinct curvature in the direction of condylar growth. He observed condylar growth of 3 mm per year during the childhood period, a slight decrease to prepubertal minimum, followed by an adolescent spurt peaking at 5.5 mm per year at approximately 14.5 years of age. Baumrind et al11 observed that condylar growth remains relatively constant between 8.5 and 15.5 years for both treated and untreated patients. The results of another study showed that the condyle grew between 0.8 and 1.3 mm posteriorly and between 9.0 and 10.7 mm superiorly over the 4-year period.5 The vertical condylar growth was approximately nine times greater than the posterior condylar growth. Boys showed significantly greater superior condylar growth during adolescence than during childhood.
The average individual experiences resorption below the ramus and deposition of bone below the symphysis. These two changes by themselves would tend to increase the gonial angle. The anterior aspect of the chin is generally unaffected and chin prominence occurred by horizontal growth and some resorption at point B. Due to extensive and variable remodelling changes on the inferior border of the mandible, it is considered unsuitable to be used as a reference plane. Björk stated that the four areas in the mandible that are most suitable for the purpose of superimposition are the tip of chin, the inner cortical surface of the inferior border of symphysis, the mandibular canal and the lower contour of the third molar germ from mineralization to root formation.
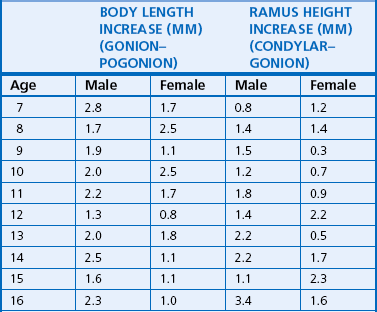
The posterior growth of the condyle and the posterior border of the ramus contribute to the elongation of the mandibular corpus and the primary displacement of the mandible. Table 1.2 shows growth changes in the mandibular length. The mandible also undergoes secondary displacement as a result of the enlargement of the middle cranial fossa. However, this is not as pronounced as that of the maxilla since the middle cranial fossa growth is mostly localized anterior to the condyles. On the average, ramus height increases by 1–2 mm per year and body length increases by 2–3 mm per year.12
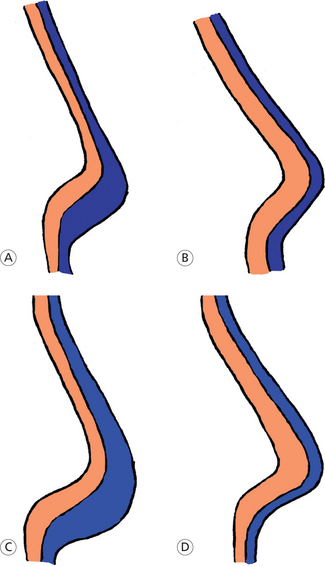
The mandible also undergoes rotational change due to the rotation that occurs in the core of the jaw, called internal rotation, and due to surface bone remodelling and alterations in the rate of tooth eruption leading to external rotation13 (Fig 1.9). The internal rotation essentially consists of rotation around the condyle (matrix rotation, 25%; Fig 1.9A) and rotation centred within the body of the mandible (intramatrix rotation, 75%; Fig 1.9B). The combination of internal and external rotation results into the overall change in the orientation of the jaw. In majority of the individuals, the core of the mandible, the bone that surrounds the inferior alveolar nerve, rotates during growth in a manner that tends to decrease the mandibular plane (MP) angle (up anteriorly and down posteriorly).
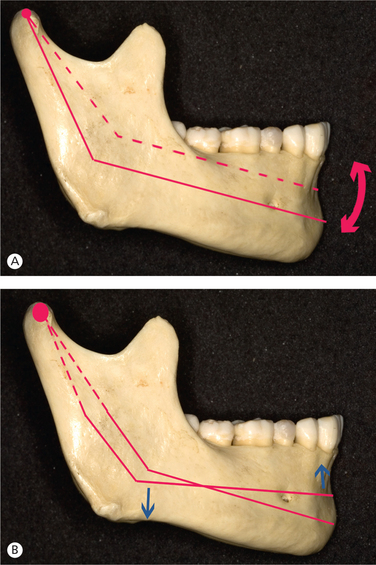
Figure 1.9 Internal rotation of the mandible. (A) Rotation around the condyle (matrix rotation). (B) Rotation within the body of the mandible (intramatrix rotation).
The compensatory surface changes (external rotation) do not allow proportionate decrease in the MP angle as a result of the forward rotation of the core of the mandible. In the average individual during childhood and adolescence, approximately 15° of internal rotation (forward rotation), as observed normally, results into just 3°–4° of decrease in MP angle due to compensatory 11°–12° of external rotation (backward rotation). This compensatory external rotational change is considered to be due to resorption at the posterior part of the lower border of the mandible and due to the apposition at the anterior part of the lower border.
Dental arches
The growth of the maxillary and mandibular alveolar bone is significantly influenced by the presence and eruption of the teeth. Alveolar processes undergo selective remodelling changes through bone deposition and resorption. The facial height is increased primarily due to the vertical growth of the maxillary and the mandibular alveolar processes, which in turn is determined by the eruption of the teeth.
As mentioned earlier, the growth of the alveolar processes is influenced by the presence and the eruption of the teeth. After the eruption of teeth, the progression of the primary dentition to the permanent dentition has an impact on dental arch length, circumference and intercanine and intermolar widths14 (Fig 1.10). In the maxillary arch, there is an increase in the intercanine width by an average of 6 mm between 3 and 13 years of age and by an average of 1.7 mm between 13 and 45 years of age.14 The intermolar width in the primary dentition increases by 2 mm between 3 and 5 years of age. The inter-first-molar width increases by 2.2 mm between 8 and 13 years of age, and by 45 years of age, it decreases by 1 mm.
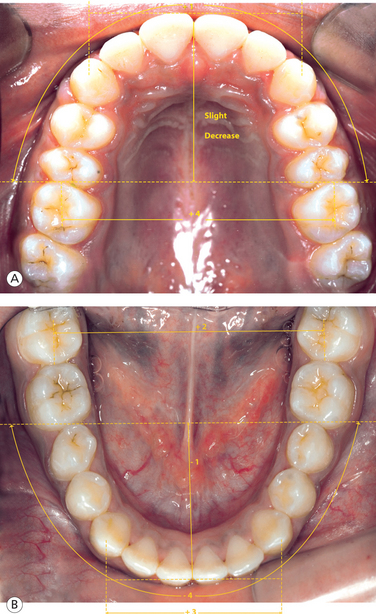
Figure 1.10 Dimensional changes (in millimetres) in dental arches between 6 and 18 years of age. (A) Maxillary arch changes. (B) Mandibular arch changes.
In the mandibular arch, the intercanine width increases by approximately 3.7 mm and then decreases by 1.2 mm between 13 and 45 years of age.14 There is an increase in intermolar width of 1.5 mm between 3 and 5 years of age. An increase in inter-first-molar width of 1 mm between 8 and 13 years of age is followed by a decrease of 1 mm by 45 years of age.14 Certain changes in the mixed and permanent dentition like uprighting of the incisors and the loss of the leeway space result in decrease in the arch length.
Horizontal and vertical growth interrelationship
It has been recognized that the growth at the mandibular condyles brings the chin forward, not downward, nor downward and forward. Then, how does the chin move downward and forward or downward and backward? It is only when the vertical growth increments of facial growth begin to influence the condylar growth through occlusal contact that a downward and forward/backward direction of the chin is produced. Therefore, the final vector of growth of the chin is a resultant of the interaction between horizontal growth (condylar growth) and vertical growth (vertical growth of molars). If the condylar growth is greater than the vertical growth in the molar region, there is counterclockwise rotation of the mandible with a resultant horizontal change in the chin position and a less increase in anterior facial height. The greater change in this relationship leads to deep bite. However, if the vertical growth in the molar region is greater than the growth at the condyles, the mandible rotates clockwise with a resultant vertical change in the chin position (less horizontal change) and an increased anterior facial height. The greater change in this relationship causes open bite.
Fred Schudy15 pointed out that the following vertical growth increments contribute to an increase in facial height:
1. Growth at nasion and in the corpus of the maxilla increases the distance between the nasion and the anterior nasal spine and the movement of the maxillary molars and posterior nasal spine away from the SN plane.
2. Growth of the maxillary posterior alveolar processes causes the maxillary molars to move away from the palatal plane.
3. Growth of the mandibular posterior alveolar processes leads to the movement of molars towards the occlusal plane.
It should be remembered that, in a patient with clockwise rotation of the mandible, an excessive vertical growth would not help to reduce the ANB angle and also the correction of Class II molar relationship. However, it does facilitate the correction and retention of overbite.15 On the other hand, counterclockwise rotation of the mandible associated with excessive condylar growth moves the pogonion forward, increases the facial angle, flattens the MP and tends to increase the overbite. In patients showing this type of growth pattern, it is difficult to correct the overbite and retain it. Therefore, molar height plays an important role in controlling the vertical position and, to some extent, the anteroposterior position of the chin.
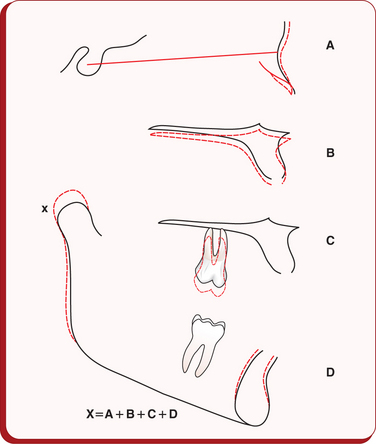
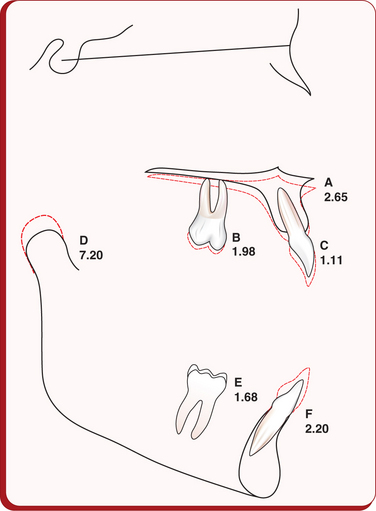
It is evident from the above discussion that the clinician must have deep understanding of these five principal growth increments – condylar growth, anteroposterior growth at nasion, the vertical growth of the corpus of the maxilla, vertical growth of the maxillary alveolar process and the vertical growth of the mandibular alveolar process –and the impact of their interaction on the chin position and outcome of the treatment. For the normal expression of the growth and the behaviour of the mandible, the condylar growth should equal the total of other four growth increments15 (Fig 1.11). The vertical growth of the anterior alveolar processes does not have a significant effect on facial height. However, it results in varying degrees of overbite. The vertical growth of the posterior alveolar process of the maxilla exceeds that of the mandible from age 8 to 14.16 Average growth (in millimetres) of maxilla, maxillary first molar, maxillary incisor, mandibular condyle, mandibular first molar and mandibular incisor in a 3-year period is shown in Figure 1.12.
Overbite changes
The growth of the jaws plays an important role in establishing varying degrees of overbite. The relationship between the condylar growth and the vertical growth of the posterior and anterior alveolar processes controls the amount of overbite. Therefore, to control deep bite or open bite, the clinician should control growth increments that determine this vertical relationship. Fred Schudy17 has called attention to the following growth increments that are relevant to the overbite relationship.
2. The body of the maxilla, having effect of lowering the palatal plane
3. Posterior alveolar process of the maxilla
4. Posterior alveolar process of the mandible
5. Vertical growth of the anterior alveolar process of the maxilla
As mentioned earlier, the vertical growth of the body of the maxilla and maxillary molars has the effect of pushing the mandible downward and backward through occlusal contact, influencing the overbite. The downward growth of the maxillary molars significantly exceeds the downward growth of maxillary incisors (by almost 2:1). Of all the six growth increments, the movement of maxillary incisors downward and away from the palatal pane is the smallest, while the mandibular incisor growth is perhaps the greatest and most variable.17 The vertical growth of the mandibular molars plays a minor role among these factors.
Facial soft tissue growth
Establishing optimal facial aesthetics is the primary goal of orthodontic treatment. As the position of the underlying hard tissues influences the morphology of the overlying facial soft tissues, it is essential for the clinician to have adequate knowledge of the soft tissue components of the face. In addition to this, the soft tissues of the face undergo significant changes throughout life due to growth, maturation and ageing; this information plays an important role in orthodontic diagnosis and treatment planning.
Nasal growth
Anatomical relationships and proportions of the nose, lips and chin largely determine the configuration of the face. The balance and harmony among these components is essential for the pleasing soft tissue facial profile. This is influenced by both growth and orthodontic treatment. In addition to understanding the changes that occur due to orthodontic treatment, the clinician should have knowledge about the amount and the direction of growth of the soft tissue elements of the face.
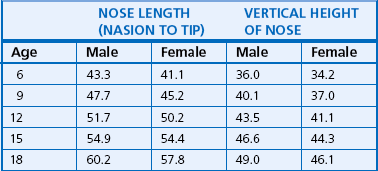
The projection of the ‘dorsal hump’ is increased due to the rotation of the upper nasal dorsum upward and forward (counterclockwise) between 6 and 14 years of age.18 The lower dorsum growth changes are related to vertical and horizontal skeletal patterns in the lower face, with clockwise rotation of the lower dorsum in vertically growing individuals. In females, the nasal projection remains virtually constant from 12 to 17 years of age, while in males, it shows a continued greater rate of growth with a resultant greater degree of nasal prominence at age 17.19 Several studies have pointed out that the nose grows downward and forward20,21(Fig 1.13). Both males and females experience proportionally more growth in the vertical dimension than the anteroposterior projection of the nose. In males, a spurt of growth occurs between 10 and 16 years of age with its peak from 13 to 14 years.20 The females show comparatively a steadier growth curve, with small percentage of subjects showing a nasal growth spurt around the age of 12 years. The majority of growth in length of the nasal bones takes place before the age of 10 years, but the soft tissues continue to grow downward and forward along with the maxillary complex.22 The growth changes in length and height of the nose are shown in Table 1.3.
Growth changes in the lip length and thickness
The upper lip rapidly increases in length from approximately 1 to 3 years of age, with a reduction in the rate of incremental growth between 3 and 6 years of age.20 From age 6 onward, a progressive increase in lip length continues till age 15. Most of the maxillary lip length is achieved by age 14 in females and by age 18 in males. The mandibular lip-length growth continues longer than the maxillary lip-length growth in females, which is complete by age 16.23 The incremental growth is greater in males than in females, which is not entirely complete by age 18. The changes in the lower anterior facial height due to vertical skeletal and dentoalveolar growth are usually concluded before completion of vertical lip growth, with comparatively more growth of the lower lip than the upper lip.24 Similar to many aspects of facial growth, the vertical growth of the lips is age and gender related.
The upper lip thickness increases in both males and females between 1 and 14 years of age, which continues in males beyond age 14.20 The upper lip thickness increases more in the vermillion region than in the part of the lip overlying point A. This change is proportional to the increase in length of the lip. In a similar manner, an increase in the thickness of the lower lip is greater in the vermillion region than at pogonion and point B. The upper lip thickness in females is at its maximum by 14 years of age and remains the same till age 16, with lip thinning afterward.23 In males, the upper lip thickness is at its maximum by 16 years of age, with lip thinning afterward. The lower lip thickness in both males and females is generally concluded by 15 years of age.23
The chin growth
The soft tissue chin thickness in females from 7 to 9 years of age is 11.7 mm, which increases by 1.6 mm up to age 17, whereas in males, it is 10.8 mm from age 7 to 9 and shows an increase of 2.4 mm up to age 17.19 This results in similar soft tissue chin thickness of 13.3 mm in both males and females at the age of 17 years.
Posttreatment craniofacial growth
In this chapter, the discussion on craniofacial growth so far has been related to actively growing individuals who constitute a large portion of the average orthodontic patient population. However, a portion of growth that usually occurs after orthodontic treatment can influence the long-term stability of a treated case. Therefore, for comprehensive and successful treatment of the growing child, every clinician should have knowledge about this ‘terminal growth’ of the craniofacial complex. George Schudy25 studied 74 orthodontically treated Caucasians to analyse the effects of post-treatment terminal growth on dentition and deeper basal structures (Fig 1.14). He suggested that the typical terminal growth is characterized by a decrease in SN-MP, SN-occlusal plane and the gonial angle. The mandible moves forward more than the maxilla, and the condylar growth proceeds in a predominantly vertical direction. The maxillary first molar moves forward more than the mandibular first molar. The upper incisors usually tip forward during the terminal phase of jaw growth. Posttreatment mandibular rotation, expressed by decreased SN-MP angle and lingual movement of lower incisor teeth, contribute to the overbite relapse and arch length reduction. The facial profile becomes progressively less convex primarily due to nasal growth and forward movement of the chin.
Ageing: skeletal and soft tissue changes
Knowledge on changes in the dentofacial complex as a result of ageing process is crucial to modern orthodontic diagnosis and treatment planning and should be of significant value to all orthodontists. The study by Behrents26 involving 113 untreated individuals from 17 to 83 years of age provided comprehensive data on the subject. In his study, the subjects from the age of 17–41 years (young adulthood) maintained their craniofacial patterns – Class II individuals grew as Class II individuals, and Class III individuals grew as Class III individuals. The subjects in the age group of 41–83 years showed vertical dimensional changes and became less protrusive. The males showed counterclockwise rotation of the mandible, and females tended to be more vertically growing. The percentage of change in the females was less than that in the males.
The soft tissue changes from age 17 to 83 included increased nasal projection and inferior movement of the nasal tip. The lips became less prominent and positioned inferiorly. Due to decreased lip prominence and lowering of the nasal tip, the nasolabial angle tended to become more acute. Dental changes included uprighting of the maxillary incisors and protrusion of the mandibular incisors in female group only. The mandibular molars uprighted in the males, and it moved forward in the females. The maxillary molars tipped mesially in the males, and it uprighted in the females.
Diagnostic information
The first step in the assessment of orthodontic patients is to generate relevant diagnostic information to establish accurate diagnosis and formulate a treatment plan. It is important to consider the improvement of patient's physical and emotional well-being as a part of a successful orthodontic treatment outcome. A sound knowledge of normal anatomy, growth and development is essential to recognize various dentofacial deformities. The goals of diagnostic and treatment planning process are threefold:
1. To identify various elements of malocclusion and their contribution to the development of a problem
2. To define the nature of the abnormality with an emphasis on exploring the possible aetiological factor
3. To formulate a treatment plan based on the specific needs and desires of the patient
Patient interview (Questionnaire)
The patient interview is often the first formal interaction between the patient and the orthodontist. Patient's general personal information and demographic data should be recorded to facilitate efficient communication between the patient and the office. The patient interview essentially consists of family history and patient history. The goal is to understand the development of the problem to institute appropriate therapeutic procedures and eliminate early causative factors. The author considers the patient's chief complaint or concern as the most important ingredient of patient interview process, as it provides valuable information on whether the patient is seeking functional improvement, aesthetic improvement or both. It also helps in designing a treatment strategy that should ideally incorporate the specific needs and desires of the patient.
A family (genetic) history is aimed at gathering some valuable information about certain malocclusions and other abnormalities present in members of the same family. A data pertaining to the history of orthodontic treatment for any siblings of the patient and either or both parents and the nature of their problems should be recorded. It should be noted that relatively a large number of craniofacial abnormalities are inherited and transmitted through a dominant gene, while in cases of cleft lip and palate, it is mostly through a recessive gene. During the course of interaction, it is common to have a patient or a parent respond that a close relative had a severe problem that required surgery.
Patient's history should include any postnatal trauma, the manner of feeding and nutritional disturbances. Inquiries should be made with respect to the child's general development like the initiation of walking and talking and the eruption of the first deciduous tooth. It is important to explore the possibility of having any abnormal habits like digit sucking and mouth breathing. Relevant information regarding allergies, medications, previous hospitalizations or traumatic injuries should be carefully recorded. While taking patient history, psychological aspects of orthodontic treatment should be discussed with the patient to determine motivation and attitude towards treatment, treatment result expectations, patient compliance etc. Such information is extremely useful to estimate future cooperation during treatment. Medical history of the patient forms an important part of the diagnostic information as it can indicate compromising factors that need special attention during treatment.
In patients with diabetes mellitus, it is essential to get blood glucose level under control prior to orthodontic treatment.27 Plaque control is critical in such patients as they are more prone to develop tooth decay and periodontal breakdown. Diabetes-related microangiopathy can occasionally occur in the periapical vascular supply, resulting in unexplained odontalgia, sensitivity on percussion, pulpitis or even a loss of vitality in sound teeth.28,29 The clinician should be alert to this phenomenon and should regularly check the vitality of teeth involved, especially when treatment is carried out for a prolonged duration. In adult patients with diabetes, it is important, prior to orthodontic treatment, to obtain a full-mouth periodontal examination including probing depth, plaque and gingivitis scores to determine the need for specific periodontal treatment. Deviations from appropriate diet and the scheduled insulin injections will result in distinct changes in the serum glucose level.30 Hypoglycemic reactions might occur more often in these patients. Type I diabetes mellitus is more often encountered in younger patients who frequently come for orthodontic treatment. For such patients, it is advisable to schedule long duration appointments in the morning hours, and the patient is advised to eat a usual meal and take required medication.
Orthodontic patients with bleeding disorders present two main challenges to the orthodontist: risk of viral infection (hepatitis and HIV) and risk of excessive bleeding. Treatment planning in such patients should incorporate reduction in the duration of treatment and nonextraction treatment whenever possible. Any gingival or mucosal irritation should be avoided; therefore, bonding of molar tubes is preferred over placing bands on the molars. In painful situations, it is better to prescribe acetaminophen with codeine if required and avoid aspirin. In case of gingival bleeding, 25% zinc chloride should be applied.
Patients with HIV infection are in an immunodeficient state and are more susceptible to infections. Therefore, necessary precautions should be taken to avoid cross-infections. Case history pertaining to the past and current medications should be obtained, and its relevance to the orthodontic treatment should be assessed. Low dosage of corticosteroids (1 mg/kg body wt) decreases tooth movement by suppressing osteoclastic activity.31 However, high dosage of corticosteroids (15 mg/kg body wt) increases osteoclastic activity, producing more rapid tooth movement and subsequent relapse.32 Therefore, it is advisable to avoid use of corticosteroids during orthodontic treatment.
As there are more and more adults seeking orthodontic treatment, it is important to know the impact of use of bisphosphonates, used in the treatment of osteoporosis and malignancies, on orthodontic treatment. Certain procedures like extractions and placement of miniscrews for skeletal anchorage should be avoided.33
Clinical examination
Orthodontic complications almost always arise from errors in diagnosis and not from failures in implementation of the proposed treatment plan. The clinical findings, therefore, become the basis of diagnostic procedures to establish accurate diagnosis. The goals of clinical examination are as follows:
1. To assess aesthetics, teeth and jaw relationships, hard and soft tissue pathology and jaw function
Natural head position
To record accurate clinical findings, the clinician should first determine the reference position of the patient in which the examination is carried out. For this purpose, it is appropriate to use the natural head position (NHP) in which the patient carries himself or herself in everyday life.34,35 In this position, the patient is instructed to sit upright and look straight ahead into the horizon or directly into a mirror mounted on the wall. This establishes a true horizontal line, parallel to the floor, where pupils of the eyes are centred in the middle of the eyes (Fig 1.15). It is based on the line of vision when the patient looks straight ahead, and it is related to the natural body posture and alignment with the cervical column.36 This position has shown reproducibility within the clinically acceptable variation of 4° as compared to the variability of 26° of FH plane and SN plane.35,37 NHP radiograph is obtained with the patient in the cephalostat looking straight ahead into a mirror and ear rods placed directly in front of the tragus with light contact with the skin to stabilize head in transverse plane. The patient should also be observed from the side to make sure that the pupil is in the middle of the eye. It should be noted that the lateral cephalostat ear rods alter the position of the head and neck during postural recordings.38 The patient should be comfortable and relaxed. The nose piece is then placed to establish third light contact with the skin, which secures the patient in NHP.
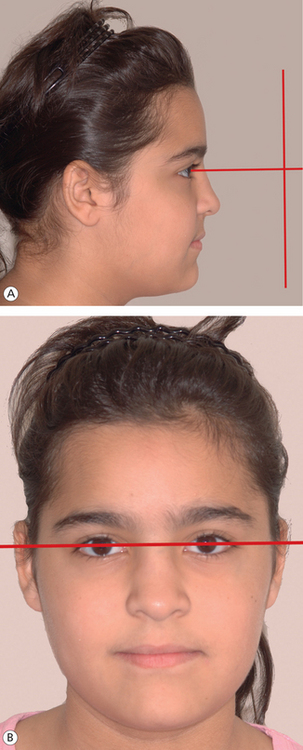
Figure 1.15 Natural head position. (A) The patient is looking straight ahead with the true horizontal coinciding with the line of vision and parallel to the floor. The pupils of the eyes are centred in the middle of the eyes. (B) The ‘true vertical’ is perpendicular to the floor and the ‘true horizontal’ (passing through the pupils).
Extraoral examination
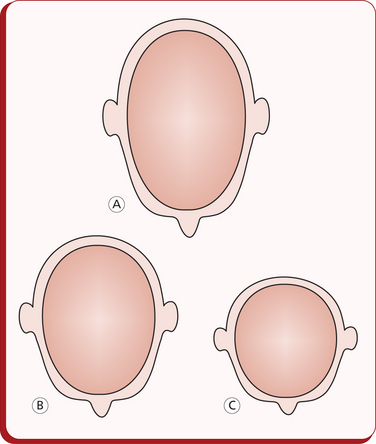
Cephalic and facial type: Extraoral examination should be carried with the patient in NHP. This essentially consists of an assessment of the facial structures and the shape of the head. The shape of the head can be determined by the measurements derived from the cephalic index (Fig 1.16). It is based on the anthropological measurements of the width and the length of the head.
Dolichocephalic (long skull): less than 75.9
Brachycephalic (short skull): 81.0–85.4
An assessment of facial frontal and profile view is essential in order to have a comprehensive understanding of the patient's aesthetic characteristics.39 The facial type should be established from measurements derived from the proportional relationship of height and width of the face. The facial height and the width are determined by the distance between nasion and gnathion and bizygomatic width, respectively.
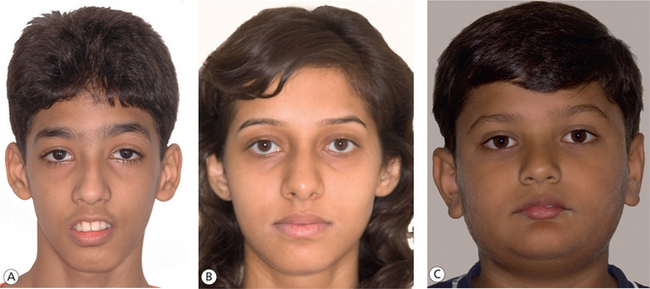
The average facial index in males is 88.5 ± 5.1, and in females, it is 86.2 ± 4.6. The facial index below normal is brachyfacial face type, indicating a broad and round face. The normal range facial index suggests that the face type is mesofacial, having average facial skeleton. If it is above normal, it is dolichofacial face type, indicating a long and narrow face due to high facial skeleton (Fig 1.17). This has a high significance in treatment planning as orthodontic treatment mechanics should be directed towards normalizing or at least maintaining the facial index. Also, it has been generally recognized that the form of the facial morphology has a certain relationship to the type of the archform. In a broader sense, expansion treatment modality is usually considered in borderline crowding cases of a broad facial type, while extractions are preferred in long face types.
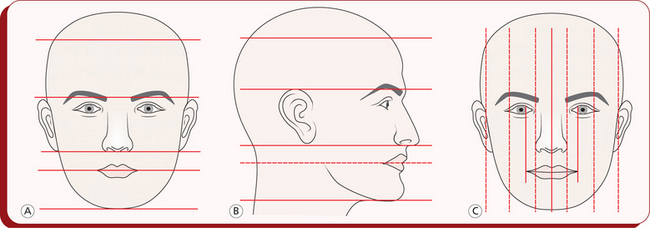
Frontal facial examination: Frontal view of the face is evaluated to determine vertical and horizontal proportions and symmetry, as any abnormality in proportion or asymmetry significantly contributes to the impaired facial aesthetics. In a patient with harmonious facial morphology, the height of the upper face determined by the distance between the hairline and the glabella (supraorbital ridges) should equal the height of the mid-face (measured between the supraorbital ridges to the base of the nose) and should also equal the height of the lower face (distance between the base of the nose and the chin)40 (Fig 1.18A). Within the lower one-third of the face, the distance between the base of the nose and the stomion should be half the distance from the stomion to the chin. Usually, the forehead is considered to be narrow or wide based on its relationship to the bizygomatic width.
In a bilateral symmetric face, the true vertical or the mid-line passes through the middle of the forehead, tip of the nose, the lips and the chin, perpendicular to the true horizontal (the line of vision) and divides the face into right and left equal halves (Fig 1.18C). Horizontally, the frontal face extending from left eye to right eye may be divided into three equal thirds: right and left eye widths and the nasal width. Also, the alar base (width of the base of the nose) should approximately equal the interinner canthal distance, and the width of the mouth should equal the distance between irises.40 At this stage of facial examination, it is important to evaluate facial and dental midlines for any deviation. A slight amount of facial asymmetry is common and may be considered ‘normal’. However, any gross facial asymmetry usually warrants further functional assessment for any deviations during various mandibular movements and also a skeletal examination with a posteroanterior cephalogram. Such evaluation provides fairly good information to the clinician for the overall facial appearance and proportionality.
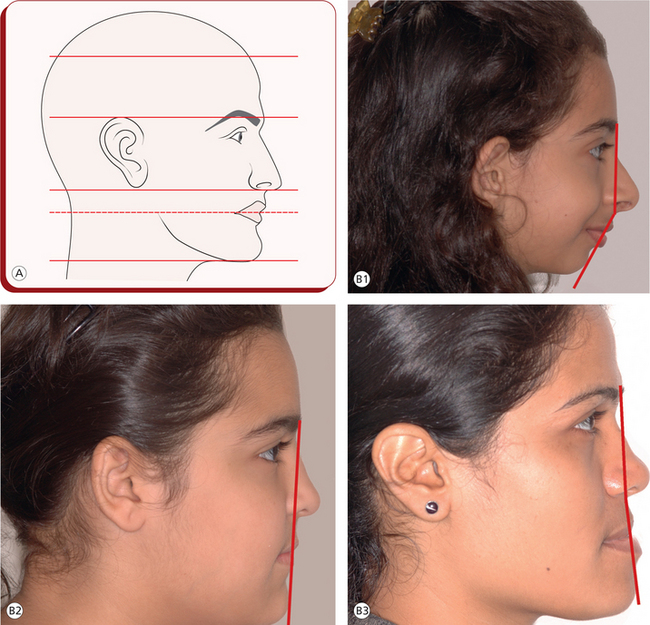
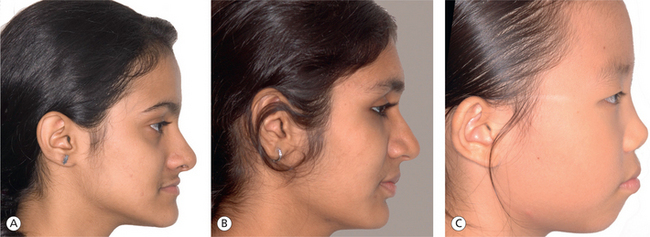
Profile facial examination: Examination of the facial profile of the patient is carried out to assess the jaw relationships and soft tissue drape, both anteroposteriorly and vertically. It is imperative that the patient is relaxed with the head oriented in the NHP. Variations in the configuration of the forehead have been observed according to age and gender and are genetically and ethnically determined. The lateral contour of the forehead can be flat, protruding or oblique. Patients with steep forehead generally tend to have more prognathic dental bases than those with flat forehead.
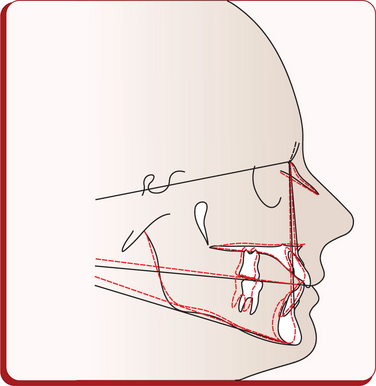
While assessing the facial profile, the clinician should consider vertical facial proportions (Fig 1.19A) and the relationship between two vertical lines – one from the glabella to the base of the upper lip and the other from the base of the upper lip to the most prominent point on the chin. This establishes whether the face is convex, straight or concave (Fig 1.19B). A convex angle indicates a Class II skeletal relationship, and a concave angle indicates a Class III skeletal relationship. The profile angle, however, only indicates the spatial relationship between the jaw bases relative to each other. Any deviation from the normal may be due to a disparity in absolute size, position or both. The facial divergence is determined by the inclination of the lower face relative to the forehead. Therefore, the possible line, normally straight and suggestive of an orthognathic profile, may slope anteriorly (anterior divergence) or posteriorly (posterior divergence). An inclination of MP should be clinically assessed by placing a scale or any instrument handle along the lower border of the mandible. A steep angulation indicates a high MP angle and usually a vertical growth direction. A nearly horizontal angulation indicates a low MP angle and generally a horizontal growth direction.
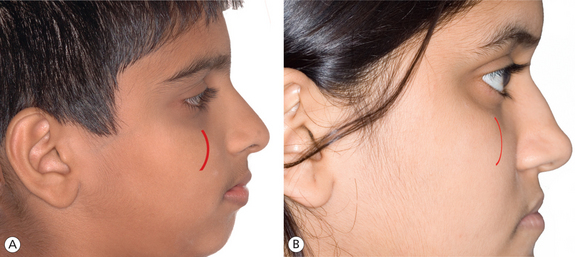
Malar sufficiency: The malar region should be observed for its optimal prominence. A direct quantification of the cheek bone prominence in millimetres is difficult. It needs to be assessed clinically as frontal and profile examination simultaneously. A prominent malar bone is a usual feature of an extreme case of horizontal grower (Fig 1.20A). Malar insufficiency is usually seen in an individual with maxillary retrognathism (Fig 1.20B).
Examination of nose: Morphological characteristics of the nose play an important role in the aesthetic appearance of the face (Fig 1.21A). To get an overall estimate of nasal proportion, the clinician should assess the ratio of the nasal width to the nasal height (GL-Sn), which should be 70%.41 Various anatomical parts of the nose, their analysis, interaction and role in nasal aesthetics and their contribution to an overall facial profile appearance may be evaluated with soft tissue cephalometric analysis. However, clinical examination should assess contour of the bridge and tip of the nose. The size, shape and width of the nostrils and position of the nasal septum should be assessed to determine an impairment of nasal breathing.
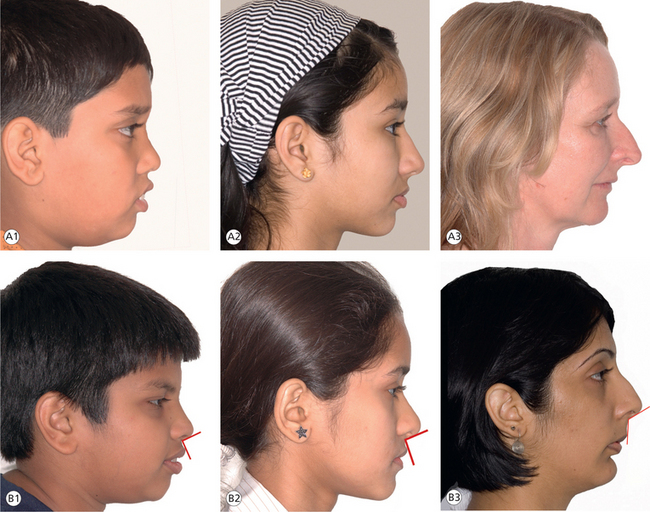
Figure 1.21 Examination of nose. (A) Nose size: (1) small nose, (2) average nose and (3) large nose. (B) Nasiolabial angle: (1) acute nasiolabial angle, (2) normal nasiolabial angle and (3) obtuse nasiolabial angle.
The nasolabial angle, formed by intersection of columella and upper lip tangent, should be in the range of 90°–120° (Fig 1.21B). Its morphology is a function of several anatomic features. An acute nasolabial angle is an indication of procumbency of maxilla, while obtuse nasolabial angle is produced by maxillary retrusion. When facial profiles are compared between males and females, female profiles with smaller noses are more aesthetically pleasing, and it is ideal for females to have less prominent noses and for males to have more prominent ones in relation to their chins.39
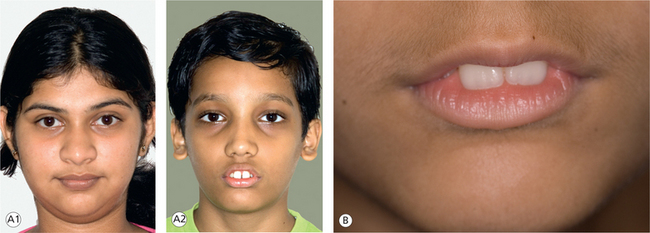
Examination of lips: The purpose of this clinical examination is to assess the configuration of the lips, which includes lip length, thickness, competence and posture. It is performed when the patient is in a relaxed position and the lips are in repose. The distance between the upper and lower lips when in repose should ideally be 2–3 mm. If this distance is increased, the lips are considered to be incompetent (Fig 1.22A). Under normal circumstances, the length of the upper lip measures one-third, and the lower lip and the chin measure two-thirds of the lower facial height. Incompetent lips could be due to either short upper lip or lips of normal length but everted as a result of incisor protrusion. The average upper lip length is 22 ± 2 in males and 20 ± 2 in females. A short upper lip results in incompetence of lips in the absence of incisor procumbancy. Ethnic characteristics do influence the lip protrusion. However, apart from this, lip protrusion is influenced by the configuration of underlying bony structures, thickness of the soft tissues, position of the anterior teeth and the tone of the orbicularis oris muscle. At rest, in patients with increased overjet, the lower lip is positioned behind the upper incisors. This situation causes lower lip dysfunction and is self-aggravating as the trapped lower lip pushes the upper teeth forward, increasing the overjet further (Fig 1.22B). The vertical position of the lips in relation to the upper incisors should be assessed when the patient is in repose (at rest) and on smiling. Ideally, the incisor display at rest should be 2–4 mm. On smiling, a gingival display of 1–3 mm is considered to be more aesthetic. It should be noted that with increasing age, the incisal display tends to reduce.
Examination of chin: The configuration of the chin plays an important role in facial aesthetics. It should be assessed in patient's NHP and relaxed facial musculature. The chin contour is evaluated with respect to the lower lip position and the configuration of the mentolabial fold (Fig 1.23). It is influenced by underlying bony structure and thickness and tone of the mentalis muscle. The chin position, both anteroposterior and vertical, is determined by the growth of the condyle, the displacement of the glenoid fossa and the vertical growth of the molar teeth.
The mentolabial sulcus in an average individual is shallow and follows a gradual S-shaped curve (Fig 1.24). A deep mentolabial sulcus is abnormal and is seen in case of reduced anterior facial height and lower anterior proclination. Abnormal muscle activity of the chin, observed clinically as puckering of skin over chin, golf ball chin, is suggestive of hyperactive mentalis. This may cause retroclination of mandibular incisors.
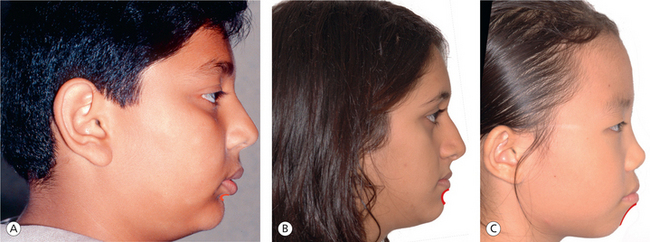
Figure 1.24 Mentolabial fold configuration. (A) Deep mentolabial sulcus. (B) Normal mentolabial sulcus. (C) Shallow mentolabial sulcus.
Another important factor that needs to be considered during an examination of facial profile is the determination of facial height. An increased or a decreased lower facial height, identified as long and short faces, presents the ultimate challenge to the orthodontist. The malocclusions that are associated with these distinct facial types are some of the most difficult treatment problems.
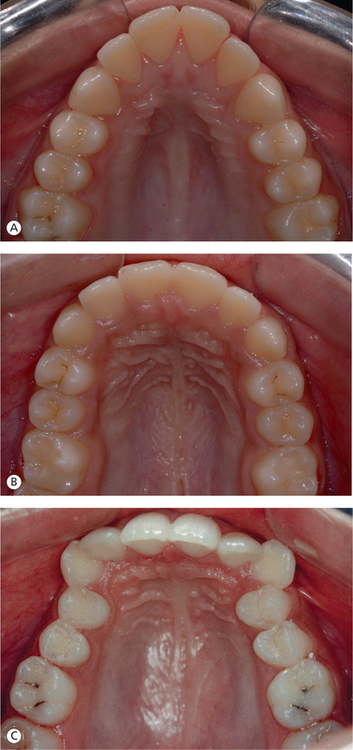
Intraoral examination
The findings of intraoral examination are the basis of diagnostic procedures. The goals of this part of clinical examination are (1) to recognize individual teeth malpositions, and intra-arch and interarch relationships (2) to detect any abnormality or pathology of soft tissue. Proper interpretation of various analyses at the time of establishing a diagnosis requires that these findings are accurately recorded, which serve as the foundation for treatment decisions. Intraoral clinical examination essentially consists of the examination of hard and soft tissues. Clinical examination of the dentition should consist of an assessment of the dental status and an accurate recording of dental and occlusal anomalies (Fig 1.25). It is important to determine the number of teeth present and the number of teeth missing and also the presence of supernumerary teeth. The maxillary and the mandibular dental arches are examined separately for archforms, symmetry, crowding of teeth, interproximal spacing, rotations, ectopic tooth positions, arch width and palatal depth (Fig 1.26).
Clinical examination of the occlusion should record molar and canine relationships, interincisal relationship, overjet, overbite, anterior and posterior crossbites etc. An important aspect of intraoral clinical examination is to reveal relevant information that cannot be obtained from the plaster models and lateral cephalogram. The soft tissue examination should consist of an assessment of tongue in relation to its size and posture; a gingival assessment pertaining to the gingival type like thick-fibrous, thin-fragile, anterior gingival architecture and mucogingival lesions; an assessment of frenal attachments and an examination of tonsils, adenoids etc. (Fig 1.27).
Evaluation of oral health
In addition to the evaluation of skeletal and dental anomalies, it is important to assess the health of oral hard and soft tissues. Orthodontic treatment should only be commenced following improved dental and oral health. A thorough dental caries or pulpal pathology evaluation is an important part of the orthodontic examination. Clinical examination of the periodontal structures should include gingival inflammation, the amount of attached gingiva, existing or potential mucogingival problems etc. (Fig 1.28).
Functional examination
Clinical examination of various components of the craniofacial complex in static relationship should be followed by the analysis of functional units of the masticatory system. The goals of this examination are directed towards the aeti-ologic evaluation of abnormality and the determination of type of orthodontic therapy. Modern orthodontic diagnosis and treatment planning should include three most important areas of functional analysis.42
1. Examination of the postural rest position of the mandible and the interposed freeway space
2. Examination of the temporomandibular joint (TMJ) function
Assessment of the postural rest position of the mandible
The primary goal of the functional analysis is to assess the mandibular position as determined by the musculature (Fig 1.29). The rest position of the mandible is influenced by the head and body posture. Therefore, it must be determined in an NHP, which can be reproduced easily. To determine this position, the patient is requested to repeat selected consonants. The letter ‘M’ or ‘C’ can be used, based on the fact that the mandible usually returns to postural rest. Alternatively, the patient can be requested to lick his or her lips first and then swallow to allow the mandible to return to the postural rest position. If the clinician is not been able to get the consistent postural rest position, another approach is to make careful observations as the patient talks or swallows as he or she has no idea of what is being examined.
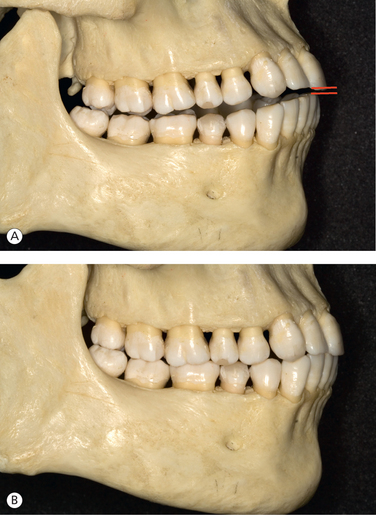
Figure 1.29 Functional examination. (A) Mandibular position at rest and interocclusal space. (B) Habitual occlusal position.
Once the postural rest position of the mandible is determined, it can be registered by different methods. Extraorally, it is possible to make direct caliper measurements on the patients profile. The distance between the two points, e.g. nasion and menton, is measured in both postural rest and habitual occlusion. The difference between the two measurements determines the interocclusal space. The cephalometric method is considered to be most reliable in providing successful results. It consists of obtaining three lateral cephalograms at three different positions: the first in the postural rest, the second in the initial contact of the teeth and the third in the habitual occlusion. The movement from the postural rest to the initial contact records the hinge movement of the condyle in the vertical plane, while the movement from the initial contact to the habitual occlusion is the sliding or translatory action in the sagittal plane.
In orthodontic diagnosis, the clinician should assess the path of closure of the mandible from postural rest to habitual occlusion in sagittal, vertical and transverse planes.
Assessment in the sagittal plane: In the sagittal plane, it is important to know whether the movement of the mandible from the rest position to occlusion is pure hinge movement, partly hinge with anterior sliding or partly hinge with posterior sliding component (Fig 1.30). This should be assessed in sagittal discrepancies like Class II and Class III malocclusions.
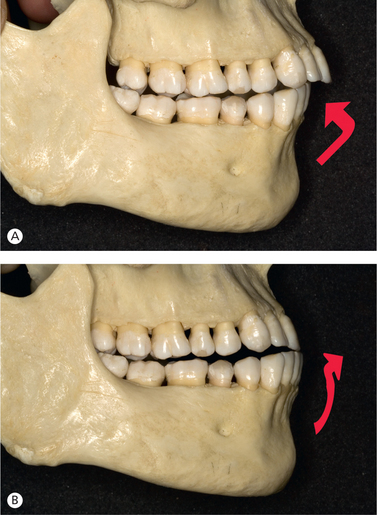
Figure 1.30 Mandibular path of closure. (A) Abnormal functional pattern with posterior sliding into the occlusal position. (B) Anterior sliding into the occlusal position.
a. Class II malocclusions without functional disturbance, therefore, exhibiting pure hinge movement of the condyle in the fossa, with path of closure of the mandible straight upward and forward from the postural rest to occlusion, are considered to be true Class II malocclusions.
b. The path of closure from the rest position to occlusion in some Class II malocclusions may be upward and backward – a posterior shift, indicating a combined rotary and sliding movement. This functional Class II appears to be more severe than it actually is.
c. Class II malocclusions with upward and forward displacement of the mandible upon closure appear to be less severe than they actually are.
a. A straight path of closure of the mandible with a hinge-type condylar movement is associated with a true Class III malocclusion without functional component.
b. In patients with severe mandibular prognathism, the path of closure may be upward and backward – an anterior postural resting position. The mandible slides posteriorly into the position of maximum intercuspation, masking the true sagittal dysplasia.
c. The path of closure of the mandible characterized by an anterior displacement with rotary and translatory action of the condyle from postural rest to habitual occlusion is associated with pseudo-Class III malocclusion.
Assessment in the vertical plane: This assessment is of significant value in determining therapeutic potential of functional appliances in the management of deep overbite cases. The amount of interocclusal clearance between the true deep overbite and the pseudo-deep overbite problems can be a distinguishing factor. The true deep overbite, associated with a large interocclusal clearance and caused by infraocclusion of the posterior segments, has good prognosis with functional appliance therapy. The pseudo-deep overbite problem, associated with a small or normal interocclusal clearance due to normal eruption of the posterior teeth, has poor prognosis with functional appliances. The discrepancy is mainly caused by overeruption of the incisors, which requires intrusive mechanics on the incisor teeth with fixed appliances.
Assessment in the transverse plane: The clinical examination of the transverse functional relationships is carried out by assessing the path of closure of the mandible from postural rest to habitual occlusion. This can be done by observing the position of mandibular midline as the mandible moves from the postural rest to occlusion.
In patients with pseudo-crossbite, the midline shift of the mandible is observed only in the occlusal position, while in postural rest, the midlines are coincident and well centred. This clinical situation is usually caused by tooth guidance. In patients with true-crossbite, due to a true asymmetric facial skeleton, the midline deviation is observed in both habitual occlusion and postural rest position.
This part of the functional examination provides valuable information related to the indications and contraindications for use of functional appliances and the prognosis.
Examination of the TMJ
The functional analysis must include the examination of TMJs and associated structures to assess normal or abnormal joint function; clicking, pain and dysfunction are characteristic features of pathologic TMJs. During the TMJ examination of the patient, the clinician should look for the following:
The key to understanding temporomandibular disorders is the differential diagnosis of the joint (internal derangement) as against the muscle pathology (myofascial pain) or the combination of the two.43,44
Any joint noises like clicking or crepitus may be diagnosed during anteroposterior or eccentric movements of the mandible with the use of a stethoscope or digital palpation. The joint clicking is differentiated as initial, intermediate, terminal and reciprocal clicking.42 Initial clicking is associated with retruded condyle position in relation to the disc. Intermediate clicking is observed in patients with uneven condylar and articular disc surfaces. Terminal clicking is a sign of the condyle being moved too far anteriorly, in relation to the disc, on maximum jaw opening. Reciprocal clicking is observed during opening and closing and is suggestive of incoordination between displacement of the condyle and disc. Any crepitus joint sound, observed as a cracking sound, indicates a rough condyle, disc or eminence surface. It occurs as a result of direct, long-term bone contacts between the fossa and the condyle.44
Palpation of the TMJ and the musculature should be performed for possible pain or sore muscles in the neck and mouth area. During opening and closing jaw movements, the TMJs may be palpated to reveal any pain on pressure. Palpation of muscles involved in mandibular movements is considered a significant part of the clinical examination. The lateral pterygoid and the masseter muscle should be palpated and examined bilaterally on every orthodontic patient, and any palpatory tenderness should be recorded.
The opening and closing movements of the mandible should be evaluated for any deviation or the extent of these movements. The mandible usually tends to deviate towards the side of an anteriorly dislocated disc. Uncoordinated zigzag movements occur as a result of asynchronic pattern of muscle contractions. Under normal circumstances, the patient should be able to open the mouth anywhere between 35 and 45 mm. Quite often, the patient cannot open the mouth, a situation called a closed lock, due to the displaced disk interfering with mouth opening. However, on some occasions, the patient cannot close the mouth – a situation called open lock – as the posteriorly displaced disk may not allow the condyle to return to its position in the fossa.45,46 If the joints demonstrate excessive mobility or hypermobility, it should be recorded in order to avoid overstretching the already compromised ligaments.44
The patient should also be examined for any signs of bruxism and clenching. It is usually night time clenching that, in many individuals, results in morning headaches. The patient's occlusion should be analyzed during various border excursions of the mandible for any prematuries or deflective contacts. This is because at the end of the orthodontic treatment, the patient should be left with a healthy masticatory musculature and good functional occlusion in centric, lateral excursive and protrusive movements.
Examination of orofacial function
A thorough analysis of all possible functions or dysfunctions of stomatognathic system is a part of modern orthodontic diagnosis and treatment planning. Any deviation in normal function may be a primary aetiologic factor in the development of a malocclusion. During the early stages of development, a child may develop unphysiologic reflex actions along with the normal physiologic reflex activities, which when prolonged may contribute to the development of a discrepancy. The resultant deformation of structures leads to the adaptive functional activity that may persist even after the disappearance of the original causative factor, e.g. thumb sucking habit. The functional examination to identify the abnormal functional aspects of stomatognathic system requires a detailed evaluation of the tongue, lips, swallowing, breathing etc.
Examination of the tongue: The examination should essentially include an assessment of the tongue function, posture, size etc. The abnormal tongue function like tongue thrust plays an important role in aetiopathogenesis of malocclusions (Fig 1.31). This can be either a primary causative factor as a result of retained infantile deglutitional pattern or other abnormal pressure habits or a secondary or an adaptive to an existing abnormal skeletal or dentoalveolar pattern. The tongue thrust may be present in the anterior region, usually associated with anterior open bite, and in the lateral region, associated with the development of lateral open bites, or it can be a complex in nature, where occlusion is supported only in the molar region.
The tongue posture should be examined clinically with the mandible in postural rest position. The posture and the shape can be narrow and long, protracted or retracted, spread laterally and shortened, flat or arched etc. The recognition of the type of tongue dysfunction is extremely important not only for determining its effect or associated deformity but also for generating useful information in designing the treatment strategy.
Deglutition: The functionally balanced or mature somatic swallow should take place without contracting the muscles of facial expression, the tongue inside the mouth and the teeth momentarily in contact. Abnormal swallowing is caused by retained infantile swallow or tongue thrust. The visceral or infantile swallow, found during the first few years of life, is gradually replaced by somatic or mature swallow as proprioception causes tongue postural and functional changes. Under normal developmental pattern, the functionally balanced or mature swallow is established between 2 and 4 years of age.
Examination of respiration: The clinical examination should incorporate an evaluation of respiration to determine the mode of breathing. An impaired nasal breathing represents a dysfunction of the orofacial musculature and interferes with the normal development of the dentition and orthodontic treatment. Patients with oronasal breathing typically present with constricted upper arch, deep palate, crossbite, poor oral hygiene and gingival hyperplasia. In patients with mouth breathing, the case history provides details regarding recurrent diseases of the upper air passages; the evaluation reveals low tongue posture and disturbed function, and the lip seal is usually inadequate.
Speech and malocclusion: Speech problems are quite often associated with severe malocclusion in some patients. The presence of certain abnormalities of teeth and jaws interferes with the normal production of certain sounds, thereby making the pronunciation of some words difficult or impossible (Table 1.4). Patients with impaired speech may require orthodontic treatment to correct abnormalities of teeth and jaws contributing to speech pathology, prior to effective speech therapy.
Table 1.4
Speech problems associated with malocclusion
| Speech sound | Problem | Related malocclusion |
| /S /, / Z / (sibilants) | Lisp | Anterior open bite, anterior large interproximal spaces |
| / t /, /d / (linguoalveolar stops) | Difficulty in production | Irregular incisors, especially lingual position of maxillary incisors |
| / f /, / v/(labiodental fricatives) | Distortion | Skeletal Class III |
| th, sh, ch (linguodental fricatives) (voiced or voiceless) | Distortion | Anterior open bite |
Source: Profitt WR. Contemporary orthodontics. 3rd ed. St. Louis: Mosby; 2000.
Diagnostic records and their analysis
It is essential to obtain high-quality, uncompromised diagnostic records for further evaluation of teeth and oral structures, occlusion and facial and jaw proportions. These records consist of study models and occlusal records, facial and intraoral photographs and radiographic records. The diagnostic records document the patient's pretreatment condition and provide additional information required to establish accurate diagnosis.
Study models
For the evaluation of the occlusion, a set of plaster study models should ideally display all teeth and alveolar processes. This requires that the impression is well extended into the labial/buccal and lingual sulci by producing maximum displacement of soft tissues. Also, for better visualization of asymmetries in the archform and tooth positions, models should be trimmed with a symmetric base. Poor quality study models do not offer adequate valuable diagnostic information.
It is important to obtain an occlusal record by registering the patient's wax-bite in habitual occlusion. The clinician should make sure that a gross discrepancy does not exist between this position and the retruded cuspal position. A sagittal discrepancy of 1–1.5 mm is of little significance; however, a discrepancy of greater magnitude or lateral shifts should be carefully recorded by obtaining centric relation (CR) bite registration.
Study model analysis is a three-dimensional evaluation of the maxillary and mandibular dental arches, the occlusion and the determination of the degree of malocclusion.
It must be correlated with other important diagnostic criteria like cephalometric analysis and radiographic analysis. Certain relationships between arch width, length and mesiodistal tooth material have been expressed by various indices of Pont, Linder, Harth and Korkhaus. In modern orthodontic diagnosis, these methods are generally considered to be of minimal diagnostic value; however, they are still widely used in most of the orthodontic practises and institutions.
1. The maxillary arch width in the premolar and molar regions should be assessed to determine if it is narrow, normal or broad. These values depend on the combined mesiodistal widths of the four upper incisors (SI).
for the arch width in premolar and molar regions, respectively.
The values thus obtained indicate the ideal values of premolar and molar widths. The actual measured values of the interpremolar (mesial occlusal pit of first premolars on either side) and intermolar (mesial occlusal pit of first molar on either side) widths are compared to the ideal values to conclude whether the arch is narrow, normal or broad.
2. To assess the adequacy of the arch perimeter from molar to molar, to accommodate an existing tooth material or to assess the degree of discrepancy, Carey's analysis for the mandibular arch and arch perimeter analysis for the maxillary arch are used.
The arch length mesial to the first molars is measured by using soft brass wire that is placed on the occlusal surfaces over the contact points and the incisal edges. This is the measured arch length. The total tooth material is calculated by adding the individual mesiodistal widths of the teeth mesial to the first molars.
When the measured arch length and the total tooth material are compared, if the discrepancy is less than 2.5 mm, the case should be treated nonextraction; if it is between 2.5 and 5 mm, second bicuspids should be extracted; and if the discrepancy is above 5 mm, first bicuspids are extracted.
3. To assess basal arch width and length of the maxilla and to determine the treatment modality, extraction or expansion, based on the degree of dental arch width, Ashley Howe's analysis is used.
where CFD is the canine fossa distance and TTM is the total tooth material.
If the ratio is less than 37%, extractions are required to resolve the discrepancy; if it is between 37% and 44%, the case is borderline; and if the ratio is more than 44%, no extractions are required.
Bolton's tooth ratio analysis: This is used to identify any occlusal misfit that is caused by interarch tooth-size incompatibility. By studying the ratios of total mandibular versus maxillary tooth size and anterior mandibular versus maxillary tooth size, one may estimate the overbite and overjet relationships likely to be obtained after treatment is finished. As the location and magnitude of tooth material excess is identified by this analysis, it helps guide the treatment planning to produce better posterior occlusion and incisal relationship.
An overall ratio of 91.3 ± 0.26 is considered ideal.
If the overall ratio is more than 91.3, then mandibular tooth material is excessive.
If overall ratio is less than 91.3, then maxillary tooth material is excessive.
Similarly, an anterior ratio is computed for the six anterior teeth in either arch.
An anterior ratio of 77.2 ± 0.22 is considered ideal.
If anterior ratio is more than 77.2, then mandibular anterior tooth material is excessive.
If anterior ratio is less than 77.2, then maxillary anterior tooth material is excessive.
Ideal ratio will give ideal overbite and overjet relationship, provided the angulations and the labiolingual thickness of the teeth are correct.
When planning treatment if there is maxillary anterior excess, proximal stripping of anteriors may be considered. If there is mandibular anterior excess, extraction of a lower incisor or proximal stripping may be considered.
Mixed dentition analysis: Mixed dentition analysis is useful to estimate the size of unerupted permanent teeth to calculate the space available. The information procured assists treatment planning in cases with intra-arch discrepancy (crowding, rotations etc.) and in those requiring interarch occlusal adjustments.
Despite numerous suggested methods, they basically fall into two types:
1. Methods involving measurements from radiographic images
2. Methods involving use of prediction tables, for example, Moyers' prediction tables and Staley-Kreber graph.
Each method has its disadvantages and advantages. Accuracy, ethnic variations and ease of application need to be prime considerations while selecting a method. The author finds the following two methods to be reasonably accurate, easy and clinically useful.
1. Measurement of teeth on radiograph: a good quality, undistorted periapical radiograph is essential. The magnification on the radiograph can be accounted for by simply measuring another erupted tooth and applying the following proportionality equation:
This method can be used in either arches and in all ethnic groups.
2. Tanaka and Johnston method: the width of the lower incisors is used to estimate the width of the unerupted canines and premolars. The method has a slight bias towards overestimating the unerupted tooth sizes.
Radiographic records
Radiographic records and their analysis form an integral part of orthodontic diagnosis. A routine clinical examination should be followed by obtaining necessary radiographs to confirm certain clinical findings and to generate additional information to establish an accurate diagnosis. As a part of routine examination, two types of radiographic records are required: panoramic, periapical and occlusal views to provide information regarding the condition of the teeth, bony structures, abnormal position of teeth etc. and cephalometric radiographs to evaluate malocclusion with respect to facial proportions, components involved and their interrelationships (Fig 1.32).
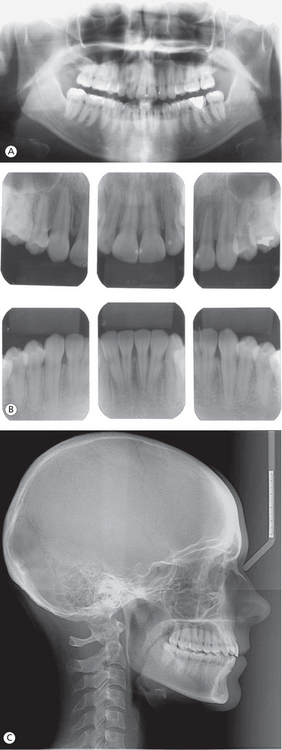
Figure 1.32 Radiographic records. (A) Orthopantomogram. (B) Intraoral periapical radiographs. (C) Lateral cephalogram.
Radiologic examination: A panoramic radiograph is valuable for orthodontic evaluation at any age. It provides a broader spectrum of views sufficient enough to show any pathologic lesions and supernumerary or impacted teeth. Trabecular pattern, bone loss, caries, developmental status of the teeth etc. can be easily assessed, and the areas that require a detailed view with intraoral periapical radiographs can be identified. It is certainly a valuable tool for the screening examination to generate adequate information for the clinician to make crucial initial decisions. A series of intraoral periapical radiographs is essential for an adult patient with periodontal disease. For patients with impacted teeth or malposed unerupted teeth, intraoral occlusal radiograph is indicated to determine their exact location. For children and adolescents, bitewing radiographs may be required for a thorough assessment of interproximal caries. The basic principle of radiologic examination is to obtain maximum information with a minimum radiation exposure.
Cephalometric analysis
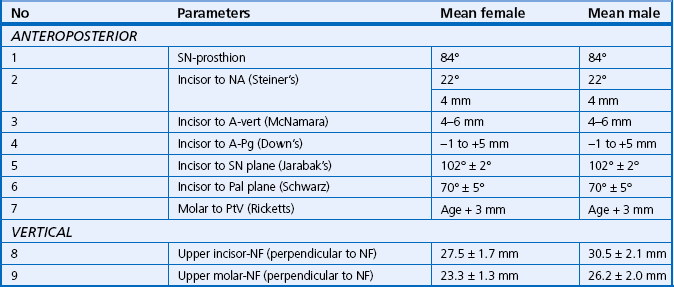
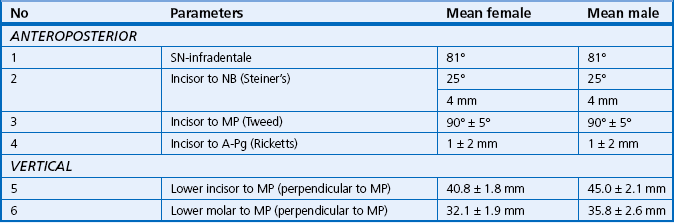
An analysis of the lateral cephalometric radiograph is one of the valuable tools used in orthodontic diagnosis and cranio-facial research. With the help of various linear and angular measurements, both sagittaly and vertically, it is possible to localize the malocclusion, assess the configuration of the facial skeleton, ascertain the extent of jaw bases and their interrelationship, assess the soft tissue morphology, identify the growth pattern and direction, evaluate the axial inclination of incisors, analyze the posttreatment changes and define the treatment possibilities and limitations. As a clinician, it is important not to establish the diagnosis solely based on the lateral cephalometric analysis as it lacks information on certain important criteria like transverse discrepancies, functional relationships and soft tissue dynamics.
Clinical examination is useful in assessing the facial proportions and jaw relations along with the soft tissue drape in all three planes of space. However, accurate quantification of size, position and orientation of the jaws, teeth and the soft tissues is possible only with cephalometric assessment. The information generated from cephalometric analysis helps in pinpointing the problem areas, which is essential in arriving at accurate diagnosis and establishing a detailed treatment plan. In fact, the data, on numerous occasions, also helps predict the prognosis for a case.
The basic cephalometric points required to analyze various components of the craniofacial complex are shown in Figure 1.33.
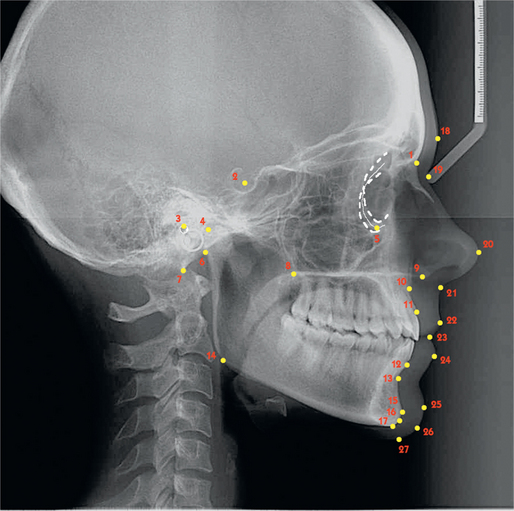
Figure 1.33 Cephalometric points. 1. N, hard tissue nasion; 2. S, sella; 3. Po, porion; 4. Co, condylion; 5. Or, orbitale; 6. Ar, articulare; 7. Ba, basion; 8. PNS, posterior nasal spine; 9. ANS, anterior nasal spine; 10. A, point A; 11. Pr, prosthion; 12. In, infradentale; 13. B, point B; 14. Go, gonion; 15. Pg, hard tissue pogonion; 16. Gn, hard tissue gnathion; 17. Me, hard tissue menton; 18. G, glabella; 19. N', soft tissue nasion; 20. P, pronasale; 21. Sn, subnasale; 22. Ls, labrale superior; 23. St, stomion; 24. Li, labrale inferius; 25. Pg', soft tissue pogonion; 26. Gn', soft tissue gnathion; 27. Me', soft tissue menton.
Systematic approach to cephalometric analysis should include assessment of
Cranial base assessment
Growth of the cranial base, though appears to be remote from the orthodontist's primary concern, influences the height and depth of the upper face and position of the upper teeth during orthodontic treatment (Fig 1.34, Table 1.5). It is essential to assess the anterior and middle cranial fossa length (1,2) and flexure (3,4). Since the anterior and middle cranial fossae are related to the maxilla and the mandibular ramus, respectively, when they are of average length, an average length of the maxilla and the mandibular ramus is normal and expected. When the cranial fossae are shorter or longer, a corresponding change in the maxilla or ramus height may be considered normal. A greater flexure of the cranial base or smaller saddle angle will lead to an increased predisposition to skeletal Class III relationship despite normal-sized maxilla and mandible. Similarly, a decreased cranial base flexure or larger saddle angle will lead to greater probability of a Class II jaw relationship even if the jaws are of normal size.
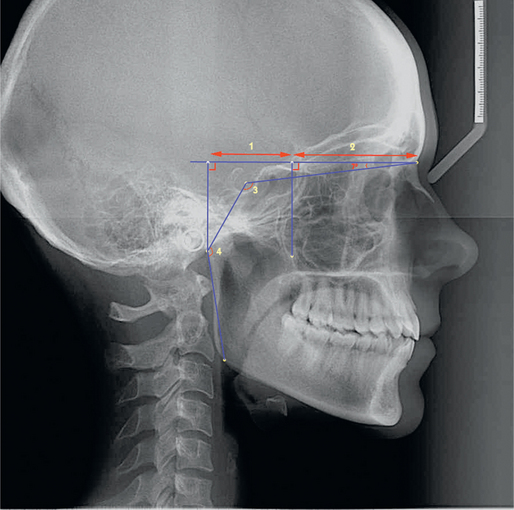
Figure 1.34 Cranial base. 1. Effective length of middle cranial fossa (distance between Ar and Ptm when projected on the HP), 2. Effective length of the anterior cranial fossa (distance between Ptm and N along the HP), 3. Saddle angle (N-S-Ar), 4. Articular angle (S-Ar-Go). The HP is a constructed horizontal plane at 7° to the SN plane.
Maxillary skeletal assessment
The skeletal component of the maxilla should be carefully assessed in relation to its length, sagittal and vertical positions and rotational pattern (Fig 1.35, Table 1.6). After determining the effective maxillary length (3,4), the clinician should evaluate its sagittal position relative to the cranium (1,2), as even a normal-sized jaw may be protrusive or retrusive if it is positioned anteriorly or posteriorly. The cephalometric assessment should include the identification of vertical component contributing to the malocclusion, as it influences the sagittal jaw position. Therefore, the vertical position of the maxilla (5,6) and the inclination of the palatal plane (7) should be evaluated.
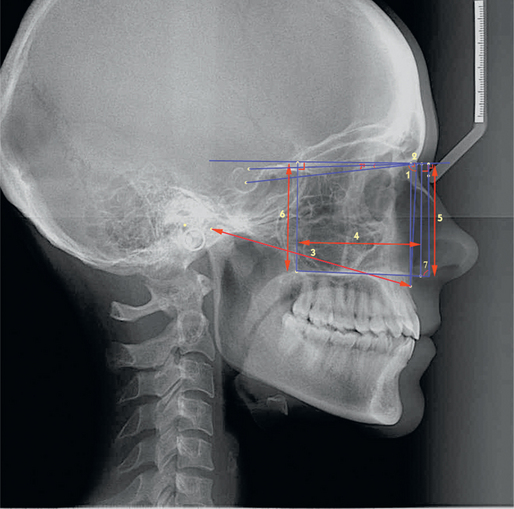
Figure 1.35 Maxillary skeletal. 1. SN-A, 2. Horizontal distance from N to A (parallel to the HP), 3. Effective maxillary length (Co-point A), 4. Effective length of palate (distance between PNS-ANS parallel to the HP), 5. Distance between N and ANS (perpendicular to HP), 6. Distance between N and PNS (perpendicular to HP), 7. J angle-angle between palatal plane and perpendicular to N-Se passing through N'.
Maxillary dentoalveolar assessment
The inclination and position of the dental units in each jaw should be assessed relative to the facial plane and the jaw base itself (Fig 1.36, Table 1.7). The anteroposterior extent of the maxillary alveolar process relative to the cranial base should be determined (1). To differentiate a skeletal problem from a dental problem, it is critical to assess the inclination and sagittal position of the maxillary incisors relative to both the maxillary skeletal base and the cranium (2–5). The vertical position of the incisal edge and the first molar cusp tip relative to the nasal floor should be assessed to identify any dentoalveolar excess or deficiency (8,9). An assessment of the dental arch length posterior to the maxillary first molar is done to evaluate the amount of alveolar arch length available for molar distalization mechanics. This analysis is done relative to the pterygomaxillary fissure (7) and is useful when contemplating maxillary molar distalization.
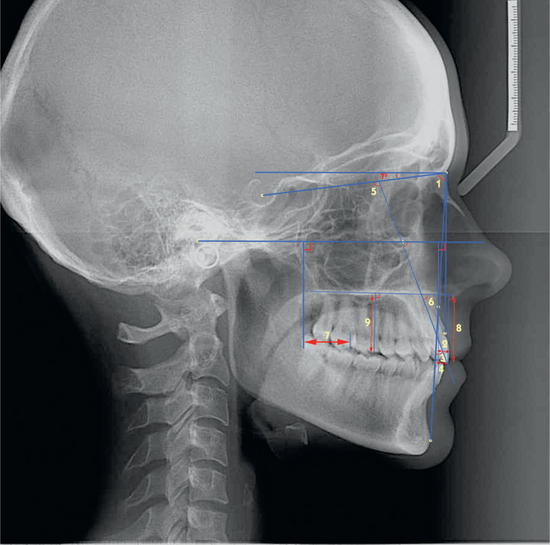
Figure 1.36 Maxillary dentoalveolar. 1. SN-prosthion, 2. Upper incisor axis to NA (inclination) and horizontal distance from most labial aspect of upper incisor to NA, 3. Horizontal distance from upper incisor to A-vertical (perpendicular from FH through point A), 4. Horizontal distance from upper incisor edge to A-Pog line, 5. Angle between upper incisor axis and SN plane (inner angle), 6. Angle between upper incisor axis and palatal plane, 7. Horizontal distance between Ptv (perpendicular to FH through distal most point on pterygomaxillary fissure) to distal aspect of upper first molar, 8. Upper incisor edge to nasal floor (NF) (perpendicular distance to NF), 9. Upper first molar mesiobuccal cusp tip to NF (perpendicular distance to NF).
Mandibular dentoalveolar assessment
The clinician should determine the anteroposterior extent of the mandibular alveolar process in relation to the cranium (Fig 1.37, Table 1.8) (1). The inclination and horizontal position of the mandibular incisors are analyzed with respect to jaw base and facial plane (A-Pog) (2–4). The vertical position of the incisors and molars is evaluated relative to the MP to ascertain dentoalveolar excess or deficiency (5,6). The proper assessment of mandibular dentoalveolar segment is of significant value to determine its role in development of a problem and to identify associated dental compensations.
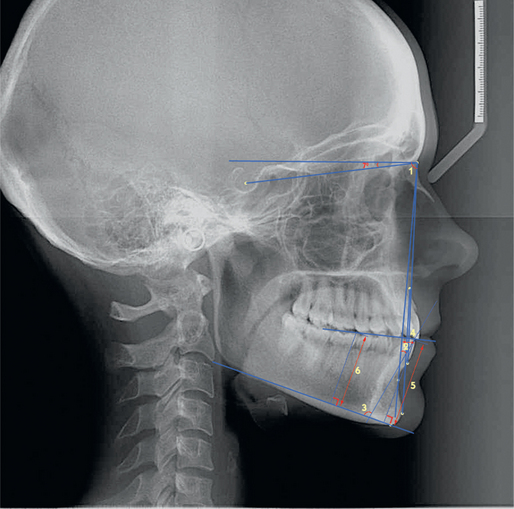
Figure 1.37 Mandibular dentoalveolar. 1. SN-infradentale, 2. Lower incisor axis to NB (angle) and horizontal distance from most labial aspect of lower incisor to NB, 3. Angle between lower incisor axis and mandibular plane (MP), 4. Horizontal distance from lower incisor edge to A-Pg plane, 5. Lower incisor edge to MP (perpendicular distance to MP), 6. Lower first molar mesiobuccal cusp tip to MP (perpendicular distance to MP).
Mandibular skeletal assessment
A cephalometric evaluation of the mandible should involve the analysis of its morphologic and positional variations (Fig 1.38, Table 1.9), in addition to the evaluation of the effective length of the body (3,4), chin (5) and vertical ramus (9); the sagittal mandibular position should be assessed relative to the cranium (N) (1) and the facial plane (N-Pg) (2). The gonial angle configuration (10) is another important parameter that gives a fair indication of morphologic growth pattern of the mandible. The assessment of the inclination of the mandibular base relative to the cranium is done using various reference planes (6–8).
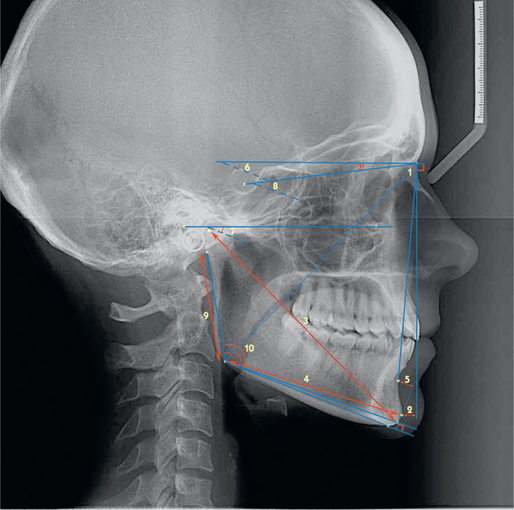
Figure 1.38 Mandibular skeletal. 1. SN-B, 2. Horizontal distance from N to Pg (parallel to HP), 3. Effective mandibular length (Co-Gn), 4. Length of mandibular body (Go-Pg), 5. Horizontal distance from point B to Pg (parallel to MP), 6. MP-HP (angle), 7. Angle between FH and MP, 8. Angle between SN plane and Go-Gn, 9. Length of mandibular ramus (Ar-Go), 10. Gonial angle – upper gonial angle (Ar-Go-N), lower gonial angle (N-Go-Gn), total gonial angle (Ar-Go-Gn).
Maxillomandibular relation
After the maxilla and mandible have been assessed individually, it is critical to evaluate their relationship to each other (Fig 1.39, Table 1.10) (1–3,8,10,11). It is the relative position of the jaws to each other that determines a Class I, Class II or Class III malocclusion and facial types. The lower anterior face height (4) is a representation of the sum of the anterior dentoalveolar heights of the two jaws and skeletal base inclination. The facial convexity (5) is determined by the relative position of the cranium (N), maxilla and mandible to each other. To predict the probable direction and pattern of future facial growth, the growth axis (Y-axis) (6) and facial pattern (Jarabak's ratio) (7) should be assessed. The cranial base flexure, glenoid fossa inclination and gonial angle of the mandible together provide valuable information in the prediction of the growth pattern, horizontal or vertical, of the jaws (9).
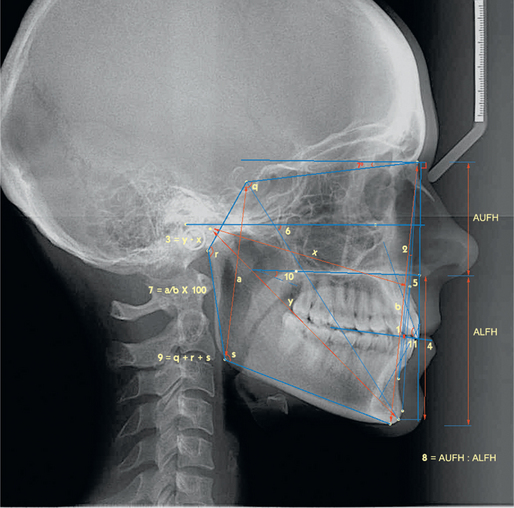
Figure 1.39 Maxillomandibular relation. 1. Distance between point A perpendicular (AO) and point B perpendicular (BO) on occlusal plane, 2. A-N-B, 3. y (Co-Gn) - x (Co-point A), 4. Distance between ANS and Gn (perpendicular to HP), 5. N-A-Pg (angle), 6. Angle between FH plane and S-Gn, 7. Posterior facial height (S-Go)/anterior facial height (N-Me) × 100, 8. Anterior upper facial height (vertical distance from N to ANS): anterior lower facial height (vertical distance from ANS to Me), 9. Saddle angle (N-S-Ar) + articular angle (S-Ar-Go) + gonial angle (Ar-Go-Gn) = Björk's sum, 10. Angle between palatal plane (ANS-PNS) and mandibular plane, 11. Inner angle between long axes of upper and lower incisors.
Soft tissue analysis
As the orthodontic treatment influences the position of teeth and jaws, which in turn influences the morphology of the overlying facial soft tissues, the evaluation of the soft tissue components of the face plays an important role in diagnosis and treatment planning (Figs 1.40 and 1.41, Table 1.11).
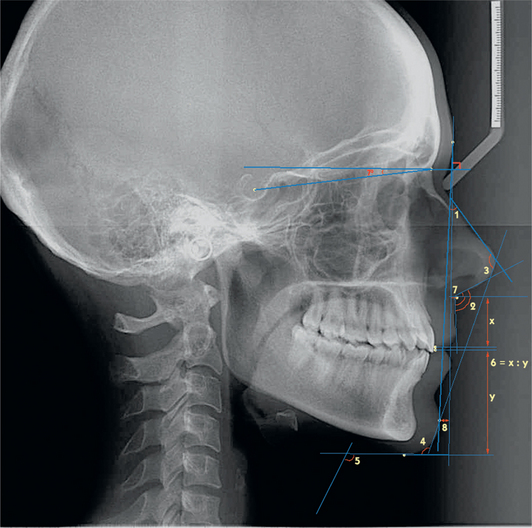
Figure 1.40 Soft tissue assessment 1. 1. Angle between G-Pg' and line along axis of radix of nose, 2. Nasolabial angle – angle between columella tangent and upper lip tangent at subnasale. It is divided into two by a postural horizontal line passing through subnasale. 3. Nasomental angle – angle between E-line and line along axis of radix of nose. 4. Mentocervical angle – angle between E-line and tangent to submental area. 5. Angle between tangent to submental area and neck tangent. 6. Upper lip length (x) (subnasale to stomion superior): lower lip length (y) (stomion inferior to soft tissue menton). 7. Horizontal distance from G perpendicular (perpendicular to HP through glabella) to subnasale. 8. Horizontal distance from G perpendicular to soft tissue pogonion.
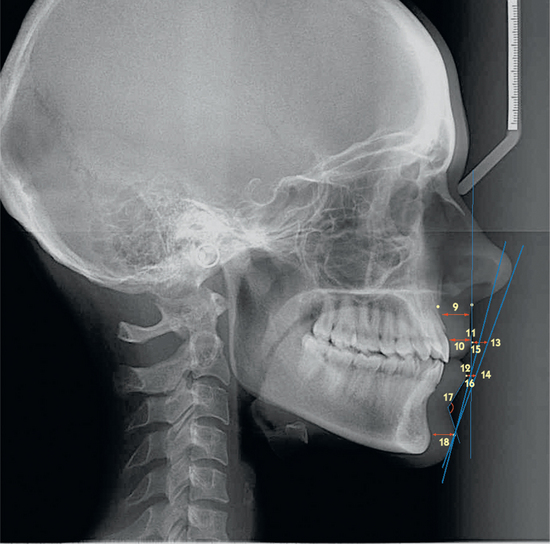
Figure 1.41 Soft tissue assessment 2.9. Upper lip thickness – horizontal distance from a point on the outer alveolar plate 2 mm below point A on to the outer border of the upper lip, 10. Upper lip strain – horizontal distance from vermilion border of the upper lip to the labial surface of the maxillary central incisor (this measurement should be within 1 mm of the upper lip thickness. If it is lesser, the lips are considered to be strained), 11. Upper lip prominence – horizontal distance from labrale superior to Sn-vertical (true vertical passing through Sn), 12. Lower lip prominence – horizontal distance from labrale inferius to Sn-vertical, 13. Horizontal distance from E-line to upper lip, 14. Horizontal distance from E-line to lower lip, 15. S-line to upper lip, 16. S-line to lower lip, 17. Mentolabial angle – angle between lower lip tangent and chin tangent at deepest point in soft tissue mentolabial sulcus, 18. Soft tissue chin thickness – distance between the bony and soft tissue facial planes (i.e. Pg to Pg′).
1. The nose morphology, position and size, though cannot be directly influenced by orthodontic or orthopaedic intervention, have a significant bearing on the overall facial appearance. Hence, its various parameters demand careful evaluation (1,3).
2. The nasolabial angle (2) is determined by the tip of the nose and the prominence of the upper lip. The assessment of a deviation from normal nasolabial angle should be done by individual evaluation of either factors by drawing a true horizontal line through subnasale. Nasolabial angle helps determine prominence of the upper dental units and upper lip and is an important factor to be considered when contemplating amount of anterior dental retraction.
3. The length of the lips (6) influences the incisal show at rest and during function (smiling). This is a very critical factor in designing anterior intrusion and retraction mechanics.
4. The assessment of the overall maxillary and mandibular prominence (jaws, teeth and soft tissue drape) plays an important role in planning sagittal orthodontic or orthopaedic correction (7,8).
5. The upper lip thickness and strain factor, if any, should be calculated (9,10). Thicker lips follow tooth movement less closely as compared to thin lips. The upper lip strain needs to be eliminated by equivalent incisal retraction for the lips to assume normal form and thickness.
6. The prominence of the lips is assessed relative to various reference lines (11–16). Appropriate lip prominence is essential for good facial balance.
Diagnostic process
The entire process of orthodontic diagnosis and treatment planning involves recognition of the various characteristics of malocclusion, defining the nature of the problem and its aetiology and designing a treatment strategy based on the needs and desires of the individual patient. The diagnostic procedure begins with the patient interview and the initial examination; however, the diagnostic process is focused on the synthesis of relevant diagnostic information and its proper interpretation to establish an accurate diagnosis. The patient interview and the initial examination quickly capture the attention of the clinician to formulate an initial diagnosis, which then guides the practitioner to carry out relevant detailed examination and analysis of records to establish a final diagnosis (Fig 1.42).
The goal of the diagnostic process is to synthesize the relevant diagnostic information and its proper interpretation to produce a comprehensive but concise list of patient's problems. This should ultimately help the clinician to design a rational treatment plan that maximizes benefit to the patient. It is important to derive a problem list from the diagnostic information and prioritize it according to the patient's needs and desires. The patient's concern and the chief complaint are essential components of this process.
Defining treatment goals
Malocclusion or abnormalities of the teeth is not a disease; therefore, patient's problems do not result from disease but rather from abnormal growth and development. This has a potential influence on patient's physical and mental health. Orthodontic treatment should now be viewed more clearly as a health service dedicated to improve the patient's life by enhancing dental and jaw functions and dentofacial aesthetics. Once patient's diagnostic information is synthesized into dental, skeletal, functional and soft tissue profile, the orthodontic treatment goals should be clearly defined. A common mistake made by the clinician at this stage is to establish treatment goals based on a specific treatment mechanics or the appliance system. This approach diminishes the scope of available solutions for patient's individual problems. The diagnostic information, especially the clinical examination, must reveal what the patient desires to gain from the treatment, and it must be included in the treatment goals and in the final treatment plan. In order to provide a high-quality orthodontic care to our patients, it is essential to define treatment goals comprehensively as follows47–49:
1. Static occlusal relationships
2. Dynamic occlusal relationships – functional occlusion goals
Static occlusal goals
Achieving proper occlusal relationship of maxillary and mandibular teeth at the conclusion of orthodontic treatment has been a fundamental goal of any treatment plan. Angle50 proposed his most famous key to occlusion as a guide to orthodontic diagnosis and treatment planning. It was based on the sagittal relationship of the maxillary permanent first molar to the mandibular permanent first molar. Since the occlusal problems exist in all three planes of space – sagittal, transverse and vertical – the contemporary orthodontic diagnosis must include a three-dimensional assessment of these abnormalities and establishment of goals accordingly. Andrew's51 six keys to occlusion, which he developed by studying untreated ideal occlusions, constitute a well-defined goals for static dental alignment. It is important to establish treatment goals for each individual tooth with respect to its best-fit, both anatomically and functionally, and achieve them with appropriate treatment mechanics. Proper alignment of maxillary and mandibular teeth, a well-coordinated archforms, levelled marginal ridges, proper position of contact points, three-dimensional position of individual teeth and the maximum intercuspation of posterior teeth are some of the important static occlusal goals.
Dynamic occlusal relationships
In addition to the above-mentioned static occlusal relationships that at least partially contribute to the stability of a treated case, the clinician should expand the scope of these goals to include the neuromuscular and bony structures of the temporomandibular joint (TMJ). This requires a careful consideration of mainly three areas of functional occlusion: centric relation (CR), anterior guidance and stability of posterior tooth arrangement. CR of the mandible is a superior limit position of the condyles in the fossae, with the mandible centred and at its most closed position.48 The essence of optimal TMJ form and function is considered the ‘seated condylar position’, which is defined as superior, anterior and midsagittal (centred transversely).52 This should represent an idealized treatment goal. It is important to achieve stable CR of the mandible with maximum intercuspation of the teeth at this position. In the intercuspal position and retruded contact position, the mandible should be situated in the same sagittal plane; the distance between the two positions being less than 1 mm. When the mandible is in CR, all the teeth must occlude in maximum intercuspation. The occlusal scheme that is most successful in preventing occlusal problems in patients over a long period of time is the mutually protected occlusion.53 In the absence of other problems, mere presence of centric occlusion – centric relation (CO-CR) discrepancy by itself is not an indication for treatment. However, if there is sufficient cause to treat, the treatment goal should be to achieve the physiologic position of the condyles as determined by the musculature in a superior-anterior fossa position, with the maximum inter-cuspation of the teeth taking place in this position.
As soon as the mandible moves out of centric closure, the maxillary and mandibular anterior teeth should work against each other to separate or disclude the posterior teeth. This anterior guidance is determined by the position of the maxillary and mandibular anterior teeth and their relationship to each other. The lingual surfaces of the upper anteriors should provide harmonious glide path to disclude posteriors during the protrusive excursion of the mandible.
During the mandibular lateral excursions, the maxillary and mandibular canines work against each other and form the main gliding inclines to provide gentle lateral lift, with no lateral interferences on the balancing side. Under certain situations when maxillary cuspid is missing, the mandibular cuspid can be made to work satisfactorily with a maxillary bicuspid. If more teeth than the cuspids on working side are allowed to contact in lateral excursions, uneven wear is likely to occur because each tooth is at a different distance from the rotating condyle and therefore moves on a different arc.54 Therefore, in order to achieve the optimal functional occlusion, the following criteria should be carefully observed.
1. Stable CR – condyles in a seated position
2. Maximum intercuspation of teeth in CR position
3. Relaxed healthy musculature
4. When molars are in occlusion, the anteriors are in a very close approximation but do not touch
5. The mandibular anteriors engage the lingual surfaces of the opposing maxillary anteriors immediately with the protrusive mandibular movement
6. During the lateral mandibular excursive movements, cuspids are in the best position to provide the main gliding inclines, with no interferences on the balancing side.
Acceptable goals for centric occlusion (CO)–CR discrepancy for orthodontic cases are as follows:
Occlusal disharmonies cannot be studied in the functioning mouth because the muscles and nerve reflexes, often called neuromuscular avoidance mechanism, protect the teeth by overriding the joint's guidance.55 Records taken in the seated condylar position and mounted on the articulator allow the joint and tooth relationships to be evaluated without interferences from the neuromuscular avoidance mechanism. In the process of diagnosis, in order for the clinician to recognize the potential or existing problem cases, it is necessary to know the signs and symptoms of occlusal disharmony. Some of the signs and symptoms of occlusal interferences include48 the following:
Orofacial functional goals
The traditional approach to orthodontic treatment planning has been directed towards the achievement of hard tissue goals, while contemporary principles of treatment planning place an emphasis on the soft tissue assessment and management. However, when it comes to defining orthodontic treatment goals, the focus has been on planning tooth movements to achieve ideal occlusal relationships and aesthetics, almost ignoring the goals for stomatognathic function. It is important to understand a relationship between anatomic form and physiologic function and the effects of abnormal functional influences on dentofacial structures and growth.
The clinician should define goals related to the functional criteria that exist in the soft tissue relationships to the teeth. This includes the ability of the patient to achieve adequate lip closure after orthodontic treatment.56 The assessment of lip dysfunctions should be done in relation to the configuration and functioning of the lips, and if present, appropriate measures should be taken to eliminate nonnutritive sucking habits, including the visual evidence of mentalis muscle hyperactivity.
The abnormal pressure habit like thumb sucking generally interferes with normal eruption of incisors and promotes excessive eruption of posterior teeth. This habit should be corrected prior to the initiation of orthodontic therapy to make sure that there are no abnormal influences that bring about displacement of teeth. Restoration of normal tongue function and teeth-together swallowing pattern should be the integral parts of treatment goals. As the chronically impeded nasal breathing represents a dysfunction of the orofacial musculature, the patient should be examined carefully to identify the mode of respiration. If abnormal function is detected, a suitable plan should be instituted to encourage nasal breathing to promote normal development of the dentition and efficient orthodontic treatment.
Optimal facial aesthetics
Achievement of optimal facial aesthetics is the primary goal of orthodontic treatment. The aesthetic benefits of orthodontic treatment are the most universally recognized by both patients and practitioners.57,58 Orthodontic diagnosis and treatment planning have become more sophisticated and scientific, and the emphasis should be placed on soft tissue analysis and its influence on treatment planning. This information should help the clinician to define treatment goals for a well-proportioned, balanced and harmonious soft tissue profile at the conclusion of treatment. The relationships of nose, lips, chin and facial soft tissue dynamics are important considerations. A comprehensive soft tissue evaluation of the patient's facial frontal and profile view should provide valuable information for better understanding of the patient's aesthetic characteristics. This ensures that the patients are treated to their soft tissue/facial aesthetic goals and not just to the cephalometric norms. It should be emphasized that the facial aesthetic goals are not compromised for a good occlusion. The patient's facial aesthetic is determined by the interrelationships and proportions of nose, upper and lower lips and the chin. Those goals can be outlined as follows:
• Establishing normal configuration of the lips, which is assessed by lip length, width and curvature
• Normal lip protrusion, which is influenced by the soft tissue thickness, position of the anterior teeth and the underlying bony structures
• Establishing normal configuration of the soft tissue chin, which is influenced by the thickness and tone of the mentalis muscle
• Normal chin position is also determined by the morphology and the craniofacial relationship of the mandible
One of the most important aesthetic goals of orthodontic treatment pertaining to the soft tissue dynamics of face is to achieve a ‘balanced smile’. There is no universal ideal smile. The orthodontic treatment should be aimed at achieving the perfect smile that is characterized by the maxillary anterior dentition following the curvature of the lower lip, the corners of the lips that are elevated to the same height (symmetrical), the bilateral negative spaces that separate the teeth from the corners of the lips and displaying appropriate position of the teeth and normal gingival architecture.59,60
The ideal facial aesthetics require the following:
1. Nasolabial angle of 90°–110°
2. Strong chin − 90° soft tissue facial plane
4. Lower facial height of 55% of total face height from nasion to menton
Other desirable features include the following:
1. Vermilion border of upper lip showing one-third of upper central incisor crown
2. Full smile showing entire upper central incisor and 1–2 mm of attached gingiva
3. Lips should be contained within the nose-chin line (Ricketts)
For attractive faces, a range for facial profile analysis (Powell) is as follows:
Periodontal health
One of the prime goals of orthodontic treatment is to achieve optimal periodontal health. This includes the preservation and minimum treatment–induced deterioration of hard and soft tissues of the periodontal apparatus. In postorthodontic treatment, the patient should not show signs of gingival recession, fenestration, dehiscence, periodontal pockets, root resorption or unusual pattern of attrition or crown wear facets. The orthodontist should make a careful assessment of patient's existing periodontal condition and the potential for bone loss or gingival recession during orthodontic tooth movement. An evaluation of the periodontal soft tissues should include an assessment of oral hygiene, areas of mucogingival tension, frenum pulls, amount of attached gingiva etc. Of paramount importance is the amount of attached gingiva – both height and labiolingual thickness.
The following procedures, directly or indirectly, promote better periodontal health:
• Proper alignment of teeth to facilitate oral hygiene maintenance
• Proper proximal contacts to prevent food lodgment and impaction
• Parallelism of roots that promotes sufficient bone between the roots, which is generally considered to provide greater resistance to periodontal bone loss if patient develops periodontal disease in the future
• No premature contacts in maximum intercuspation and during various mandibular excursions to prevent tooth mobility, periodontal damage etc.
• Proper positioning of teeth in the cancellous bone between labial and lingual cortical plates to prevent gingival recession
• Normal interincisal relationship to prevent redevelopment of deep bite and subsequent stripping of gingival tissue either from the palatal aspect of maxillary incisors or from the labial aspect of mandibular incisors
• Controlling the magnitude of orthodontic force levels, as the application of heavy forces over a period of long time contributes to the external root resorption
• Elimination of pretreatment bony defects by controlled force eruption or uprighting of teeth
• Effective oral hygiene maintenance protocol by the patient
Posttreatment long-term stability
Long-term stability of tooth positions achieved after orthodontic treatment should be the primary goal of every orthodontic treatment plan. It is an area of great concern to the orthodontic profession and greatly influences the treatment plan. Many of the posttreatment changes in the dentition like deepening of overbite, increased overjet, relapse of treated Class II relationship and crowding of the maxillary and the mandibular incisors are being considered mainly due to posttreatment growth changes. The posttreatment growth significantly contributes to the lingual movement of mandibular incisors leading to deepening of overbite, loss of arch length and lower incisor crowding.25 Other post-treatment changes like anterior open bite and interdental spacing and changes in a single rotated tooth are considered primarily due to local factors such as persistent habits, inability of the periodontal fibres to reorganize and lack of adaptability of the soft tissues.
As mentioned earlier, achievement of static and dynamic occlusal goals, optimal periodontal health and bone support as guidelines to finish orthodontic cases to the highest standards at least partially contribute to the stability. In addition to this, the clinician should consider anticipated posttreatment growth and local factors in the planning of active treatment and retention protocol to enhance long-term stability.
Orthodontic treatment planning
Proper treatment planning depends on accurate diagnosis, which in turn requires objective, relevant and accurate information, patient data and an analysis of various records. It is important to understand that both the treatment planning process and the delivery of orthodontic care involve much more than the simple process of bonding brackets to the teeth and following a predetermined sequence of archwires. The treatment must be dictated by the individual patient's problem and diagnosis.61 Orthodontic treatment planning process is illustrated in Figure 1.43. The goal-based treatment planning provides a guide for the techniques and mechanics used in the delivery of orthodontic care. The entire process of treatment planning is influenced by many factors.
Factors influencing treatment planning
Presence or absence of the growth is frequently a significant factor in selection of a treatment plan. Facial growth occurs in a downward and forward direction, and its presence is usually a positive factor in resolution of many adolescent malocclusions. Several treatment modalities like headgear or functional appliances rely on this growth as a part of orthopaedic treatment for stable correction of skeletal discrepancies. Orthodontic treatment mechanisms influenced by growth are not available for the adult patient. The natural eruption of teeth along with the vertical growth of the alveolar bone provides many treatment options to the clinician, as controlling the vertical dimension significantly contributes to occlusal correction. The growing patients present with significant potential for adaptability of stomatognathic system, which allows a variety of biomechanical choices like the use of Class II elastics. The ageing process appears to result in changes in the biologic system of the teeth and alveolar process.62 It alters the ability of the fibroblast to produce collagen.63 Since there is minimal skeletal adaptability and no growth in adult patients, orthodontic treatment is dependent on tooth movement to achieve entirely desired results unless surgical procedures are used for the underlying skeletal disharmonies. In planning a tooth movement, the clinician must recognize that the growing patients exhibit predictable and rapid rate of tooth movement, especially during eruptive stages when permanent root development is not yet completed.64 Adult orthodontic patients are at no greater risk for orthodontically induced root resorption on the average; however, they exhibit more severe root resorption than in adolescent patients.65
Location of discrepancy
One of the key factors influencing the treatment planning process is the location of the problem within the dentofacial complex. Since orthodontic treatment affects many structures of the craniofacial complex like teeth, supporting structures, maxillary and mandibular basal bones, TMJs and facial structures, the clinician must define treatment goals for these areas in order to establish an effective treatment plan.
• If there is only occlusal problem, this can be addressed by orthodontic tooth movement alone, at any time, or by occlusal equilibration.
• If the problem is dentoalveolar in nature, effective measures may be taken even after cessation of growth. Treatment procedures in this area are indicated if compensation of the underlying skeletal discrepancy is required.
• If the discrepancy is confined to the skeletal bases (skeletal malocclusion), the treatment should influence the facial sutures and TMJs, and it is possible only during the periods of active growth. In nongrowing patients, changes in the abnormal skeletal relationships can be achieved with surgical intervention.
Existing discrepancy
Proper assessment of various elements contributing to the existing discrepancy to determine the complexity of a problem is essential for treatment planning. There are many clinical entities that contribute to the complexity of a problem and its management, and it is not possible to include every clinical entity to determine the severity of discrepancy. The American Board of Orthodontics developed the discrepancy index (DI) based on those disorders that represent most conditions that orthodontists treat.66 The target disorder elements chosen to make up the DI are measurements of overjet, overbite, anterior open bite, lateral open bite, crowding, occlusion, lingual posterior crossbite, buccal posterior crossbite, ANB angle, IMPA and SN-GoGn angle. Other conditions that influence the treatment complexity are missing or supernumerary teeth, ectopic eruption, transposition, anomalies of tooth size and shape, CO-CR discrepancies, skeletal asymmetry and excess curve of Wilson. It has been generally recognized that more severe the case, the more complex the treatment and more difficult to treat. However, the degree of difficulty is somewhat subjective and a matter of perception. Some clinical situations that are considered difficult by some clinicians might be perceived as relatively easy to treat by others. This is usually due to differences in diagnostic approach, appliances used, overall approach to treatment and training.
Functional assessment
The importance of functional analysis in the examination of different clinical situations has been universally recognized. Equally important is the understanding of its significance in treatment planning. The movement of the mandible is hinge like as it changes from the rest to the occlusal position. The postural rest position of the mandible can be either anterior or posterior to the habitual occlusal position. The functional disorder is more serious than the findings of the occlusal examination. Any abnormality in mandibular position resulting in transposition should be eliminated in order to assess the full extent of the discrepancy. The path of closure of the mandible and condylar position in the fossa should be evaluated properly. Intermaxillary relationships and the rest position can only be changed during active growth with functional appliances.
The assessment of lip configuration in relation to incisor relationship and angulation plays an important role in treatment planning. For example, lip dysfunction in patients with skeletal Class II relationship will have much more serious consequences due to the presence of unfavourable relationship of the maxillary and mandibular skeletal bases. The abnormal outcome of the assessment of tongue position and function should be considered in the final treatment plan. The elimination of tongue dysfunction determines the treatment outcome and its potential stability. The clinician must assess the upper airway patency to determine the mode of breathing. Enlarged adenoids that may be distinguished in the radiograph often lead to reduced patency of upper respiratory passages and oral breathing. The final treatment plan should incorporate the necessary measures to establish nasal breathing and teeth–together swallowing pattern.
Aetiological assessment
Once the abnormality has been located in the dentofacial complex based on the clinical examination and analysis of diagnostic records, and functional relationships have been determined, the orthodontist should draw some conclusions to the cause of the problem. The orthodontic treatment plan for any malocclusion must include the elimination of the aetiological factor. There are many causative factors that contribute to the development of malocclusion and dentofacial deformity. In some patients, the aetiology of some characteristic malocclusions appears to be almost genetic in nature, while in others, it is a result of some environmental influences. Certain malocclusions are developed as a result of disturbances of dental development like congenitally missing teeth, malformed and supernumerary teeth, interference with tooth eruption due to sclerotic bone or heavy fibrous gingiva and ectopic eruption. Sometimes, improper guidance of eruption either due to early loss of primary teeth or due to functional shifts of the mandible while permanent teeth are erupting leads to the development of a problem.
Some kind of a trauma to the teeth in children during their formative years and childhood jaw fractures due to falls and impacts cause severe mandibular deficiency requiring surgical correction in about 5% of affected patients.67 It is also interesting to note that about 75% of children with early condylar process fractures have normal mandibular growth and therefore do not contribute to the development of malocclusion.68 The functional influences like thumb sucking, tongue-thrusting and mouth-breathing habits affect dentofacial development leading to a deformity. Whatever may be the aetiological factor, the diagnostic process should guide the clinician to identify it, and its elimination should become an integral part of a well thought-out treatment plan.
Patient compliance
Patient compliance is one of the determinants of the use of various treatment options that are available in modern orthodontic practise. Lack of compliance in the present orthodontic patient population has been a major concern for the orthodontists. Over the few years, the percentage of patients exhibiting poor compliance has been increased tremendously, with only about 10% demonstrating excellent compliance.69 It is the author's experience that both patients and their families misrepresent – generally overestimate the extent of compliance. The clinician must be aware of the fact that the patient compliance usually decreases when longer duration treatment is required.70 Therefore, patient compliance should be given due importance in the treatment planning process, and appropriate measures should be designed and explained at the time of case presentation.
Patient compliance may be improved by many ways:
1. Patient motivation: the ability to motivate a patient to comply is an essential ingredient of successful outcome of orthodontic therapy.
2. Reduction of treatment duration: a well-defined treatment goal must be defined before the execution of treatment plan to prevent unnecessary, prolonged treatment that may ‘burn out’ the patient subsequently.
3. Involvement of patient and parent in treatment decision: the orthodontist must make every effort to involve the patient and the parent in the treatment decision and emphasize the importance of high levels of patient cooperation as per the specific needs of the patient.
4. Lastly, it would be prudent for the clinician to consider that the patient will demonstrate diminished compliance over a period of time and therefore, design treatment plans and mechanics that minimize the need for compliance.
Dentofacial aesthetics
The aesthetic benefits of orthodontic treatment have been universally recognized by both patients and orthodontists. In majority of cases, patients seek orthodontic treatment primarily because of aesthetic concerns, and the influence of orthodontic treatment in attaining aesthetic improvements should neither be understated nor be overemphasised during the treatment planning process. This is because any discrepancy in aesthetic treatment outcome and patient expectations leads to patient dissatisfaction. In patients with significant anterior teeth crowding due to severe maxillary and mandibular arch length discrepancies, alignment of teeth with orthodontic treatment plays an important role in achieving an attractive smile. This can be accomplished by
• Nonextraction treatment approach
Bicuspids are extracted to gain adequate space. Another commonly featured aesthetic problem is excessive teeth and gingival display upon smile.71 The treatment considerations for excessive incisor show depend on the aetiological reasons. The maxillary incisors may be intruded with intraoral intrusion arches. The detorqued maxillary incisors should be adequately torqued or advanced. If it is due to soft tissue defect, short philtrum, V-Y cheiloplasty may be performed. In adults if it is associated with vertical maxillary excess, surgical impaction of the maxilla using LeFort I osteotomy is useful. On the other hand, patients also express their concern over inadequate incisor show. Orthodontic torquering, or retraction of flared maxillary incisors, increase in adequate crown length by various dental procedures, soft tissue surgical procedure (direct or indirect lip lift) for long philtrum, and maxillary downgraft using LeFort I osteotomy for vertical maxillary deficiency are some of the treatment options to deal with this problem.
The lip position is influenced by the relative protrusion or retrusion of incisors and is considered to be the determinant of extraction or nonextraction treatment decision.72 It is important to consider that the increase in size of nose and chin is usually more than the soft tissue lip thickness changes over a period of time.73 Lip projection is a function of (a) protrusion or retrusion of teeth, which can be resolved by incisor retraction or advancement, (b) maxillo-mandibular protrusion or retrusion, which can be addressed by orthopaedic correction at early age or surgical intervention in adults and (c) lip thickness, which is influenced by patient age, ethnicity etc.
Patient motivation and expectations
Patients seeking orthodontic treatment show different motivation levels at different age groups.74 Since adult patients themselves make their decision to undergo orthodontic treatment, they may be considered internally motivated.75 These highly motivated patients may be more compliant during the course of treatment contributing to the success of treatment outcome. The areas of patient satisfaction and happiness are highly sensitive and extremely important in orthodontic practise. The practising orthodontist must be prepared to assess certain influencing factors like patient expectations and psychological well-being of the patient. Aesthetic benefits of orthodontic treatment have been universally recognized. Even for those patients who choose to undergo orthodontic treatment primarily for the improvement of function, aesthetic concerns play a major role. The successful correction of patient's abnormal clinical entities along with the achievement of functional goals does not always ensure patient satisfaction if it has compromised aesthetic relationships. The clinician should identify the reasons for seeking orthodontic treatment as unrealistic patient expectations may lead to poor satisfaction with the final outcome. The key factor here is to make sure that the treatment results are aligned with the patient expectations, which need to be incorporated into treatment planning process.
Periodontal condition
Orthodontic treatment involves the use of light, continuous forces to bring about a controlled tooth movement in a predetermined direction. During this period, it is a basic requirement to maintain an optimal periodontal health to avoid any unfavourable response from the supporting structures of the teeth. During the treatment planning process, abnormal findings pertaining to the periodontal health revealed during the careful clinical examination should guide the clinician to incorporate appropriate measures in the final treatment plan to restore its normal health. It is critical to assess the potential impact of planned tooth movement on the tooth-supporting tissues. If the patient has experienced bone and attachment loss leading to tooth migration or extrusion, orthodontic treatment is recommended to improve the prognosis of such periodontally compromised teeth.76 Reduced periodontal attachment consequent to disease requires that the orthodontic force systems are modified to produce desired force magnitudes to induce predictable tooth movement without any damage to the periodontium. As a result of an attachment loss, the centre of resistance of a tooth also shifts apically causing a great tendency for the tooth to tip.77 It must be recognized that in the absence of plaque, orthodontic tooth movements do not induce gingivitis; however, in the presence of plaque, the same may produce marginal bone loss.
Another important aspect to be considered in the treatment plan is the type of bone through which the tooth is moved. An excessive tooth movement, especially in a labiolingual direction that displaces the root through the cortical bone, results in a fenestration. Therefore, the clinician has to be more careful in planning torque movements, especially in the incisor and canine region and in the maxillary premolars and molars where the labial cortical bone plate is considered thinner than at the lingual aspect. The bone fenestration effect is seen in the region of the apical part of the root, while the bone dehiscence involves marginal bone loss on the facial aspect of the root.
Rapid maxillary expansion (RME) produces most favourable outcome if carried out at young ages when sutures are not closed. Research studies on palatal suture closure have shown large individual variations with age.78 RME used in patients with fully or partially closed sutures or orthodontic overexpansion usually results in tipping of buccal segment teeth leading to a marginal bone resorption.
Retention and stability considerations
Retention and stability of an orthodontically treated case has been the area of great concern to the profession since the inception of this specialty. Ideally, retention planning to ensure better stability should begin with diagnosis and treatment planning. During the treatment planning process, the practising clinician should identify the areas of potential relapse, define goals for tooth positions for better stability, design appropriate treatment mechanics to achieve these goals and establish individualized retention protocol. It is important to distinguish physiologic recovery and relapse as two separate entities. Orthodontically treated patient typically shows posttreatment changes that are related to the treatment and those that are considered to be normal developmental changes as part of the ageing. Elimination of causative factors for the development of malocclusion plays an important role in preventing recurrence. Tooth-supporting structures – both hard and soft tissues – must be given sufficient time to reorganize around newly positioned teeth. Occlusal goals must be defined and achieved with proper finishing procedures, as the proper occlusion with good intercuspation is a potent factor in holding the teeth in their corrected position.79 The archform, particularly in the lower arch, should not be permanently altered. Root parallelism at the extraction sites should be achieved and verified radiographically before appliance removal. As the time for formation of mineralized bone increases with advancing age, it is important to consolidate teeth after movement and prolong the retention period. Periodontal considerations, extraction decisions and retention regimens play a vital role in the achievement and maintenance of an optimal result.80
Therefore, the secret of successful planning of retention and long-term stability lies in the consideration of malocclusion-specific, treatment-specific and adult-specific principles in the treatment planning process.
Growth prediction
The ability to forecast or predict dentofacial growth is perhaps the most essential and integral part of contemporary clinical orthodontics. There are several elements the clinician has to deal with in the prediction of craniofacial changes: the direction, the magnitude, the timing, the rate of change and the effects of treatment.9 The growth changes in the face are complex and demonstrate a great degree of individual variations, but how predictable are these variations that are considered to be normal, in the growth of the face?
In a broader perspective, the growth prediction can be accomplished by three basic methods: longitudinal, metric and structural.10
Longitudinal method of growth prediction
This method evaluates an individual over a period of time to determine the pattern of growth and age-related individual peculiarities. Tweed81 used this approach on his growing patients by advocating two lateral cephalograms, 12–18 months apart, to assess the skeletal facial changes. The limitation of this approach to growth prediction is that it is accurate only when it is performed retrospectively and not prospectively. Also, the growth pattern is not constant, and the pattern of growth recorded at a juvenile age may well have changed by adolescence. Therefore, it should not be considered an accurate method of predicting future dentofacial changes.
Metric approach to growth prediction
This method of growth prediction uses a single radiograph to measure different structures that are then related to future growth changes. It is based on statistical information on average growth increments derived from a normative sample to be added to the recorded actual facial dimensions of the patient. The goal is to estimate the statistically probable future facial dimensions of the patient.
Structural approach to growth prediction
Björk82 developed a structural method for the prediction of mandibular growth direction by using metallic implants. This method involves the recognition of specific structural morphological features in the mandible that would help to identify future growth trends. Björk83 considered seven areas on a single cephalogram to predict mandibular rotation:
1. The inclination of the condyle (with vertical condylar growth, the mandibular rotates forward)
2. The curvature of the mandibular canal (the more curved the canal is, the more forward mandibular rotation will be)
3. Inclination of the symphysis (if it is inclined lingually, the mandible will rotate forward)
4. Shape of the lower border of the mandible (the forward rotator has concave lower border as against the convex, or notched, lower border of the backward rotator)
5. The interincisal angle (more acute in forward rotators)
Later, Skieller et al84 found that, of these original signs, four of the variables – mandibular inclination, intermolar angle, the shape of the lower border and inclination of symphysis – when combined gave the best prognostic estimate of 86% of mandibular growth rotation.
Treatment options
In designing a treatment plan, it is an important step to select the appropriate treatment strategy to resolve the discrepancy. There are several general treatment options available, which need to be carefully explored and evaluated before finalising on the modality of choice. As stated earlier, the treatment plan should be individualized – tailored to individual patient needs. This guides the clinician to make sure that the potential treatment option is carefully assessed and fits with the general treatment goals. One of the common mistakes made by the orthodontist is to design a treatment strategy instinctively based on a quick impression of whether the patient needs extractions or not. It requires a great deal of flexibility on part of the clinician to examine all the rational possibilities to formulate the successful treatment plan.
Early treatment
The optimal timing of treatment of the various problems in growing patients remains a controversial issue. In author's opinion, the two-phase treatment – an interceptive phase carried out during the mixed dentition and corrective phase in the permanent dentition – should not only optimize oral health, function, aesthetics and stability but also justify the time, cost and resources involved. The variability in initial clinical conditions and treatment response and differences among the orthodontic professionals concerning treatment beliefs, goals and even skills significantly contribute to the complexity in determining the relative merits of these two treatment approaches. The early treatment approach provides the clinician with more treatment options, better use of growth potential and less need for en masse tooth movement, torque and dental compensations in the second phase of treatment.
The leeway space can provide adequate space to align and accommodate crowded teeth in majority of patients.85 The combined mesiodistal widths of the deciduous canine and first molar are the same as the combined mesiodistal diameters of the permanent canine and first premolar, and the space gain represents only the ‘E’ space.86 The ‘E’ space can be accomplished by using passive appliances such as holding arches in the late mixed dentition stage. The transplatal arch is used in the mixed dentition to produce molar rotations, changes in root torque, transverse molar changes etc.
Early arch development can be achieved by the use of lip bumper and rapid palatal expansion (RPE) treatments to induce spontaneous expansion of dental arches. It has been reported that both arch length and width are increased with lip bumper therapy.87,88 Interestingly, the largest amount of postretention irregularity was observed in a group of mixed dentition patients whose treatment involved more than 1 mm of arch length expansion.89 It then guides the clinician to limit the lip bumper therapy to a 1-mm increase in arch length. This can be fairly established after 3–6 months of use of lip bumper.88
Orthodontic expansion, produced by removable expansion appliances or fixed appliances, is primarily a dentoalveolar in nature due to buccal movements of posterior teeth. An excessive expansion leads to a buccal tipping of crowns and a lingual tipping of the roots of the posterior teeth. This occlusal change along with the presence of the cheek musculature forces provides instability to the achieved expansion. On the other hand, RME produces orthopaedic expansion, affecting the underlying skeletal components rather than by the movement of teeth through alveolar bone. This method separates the midpalatal suture where new bone is deposited to establish the integrity of the midpalatal suture in 3–6 months.90
In the management of Class II malocclusions, the use of extraoral appliances produces an orthopaedic effect that is important for patients with maxillary prognathism. The results of extraoral appliance use, when compared between patients in the early and late mixed dentition stage, showed a 1 mm greater orthopaedic effect in the younger group.91
The use of functional appliances in patients with Class II malocclusions characterized by mandibular retrognathism, with the intent to stimulate mandibular growth, has been advocated. The use of Functional Regulator (FR-II) appliance demonstrated an age-dependent mandibular growth response, showing more mandibular growth in patients older than 10.5 years (4.0 mm/year) than that observed in younger group (less than 10.5 years, exhibiting a mandibular growth of 3.2 mm/year).92
The appropriate time for the optimal use of space maintaining (holding arches) and various functional appliances is not clear. However, it is author's experience that treatment goals can be accomplished in majority of the patients when treatment is initiated in the late mixed dentition stage of development. This treatment approach also reduces the prolonged duration of treatment and the increased cost associated with the treatment that is started in the early mixed dentition stage.
Treatment modalities that are commonly used in the early intervention of Class III malocclusion include the reverse pull headgear along with RPE and chin cup therapy. The face mask therapy is very effective in patients with maxillary deficiency. It is important for the clinician to know that the face mask therapy does not normalize growth; treated patients resuming a Class III growth pattern characterized by deficient maxillary growth is considered to be the main cause for posttreatment relapse.93 In patients with Class III malocclusion characterized by excessive mandibular growth, the use of chin cup is believed to alter the mandibular form and retardation of condylar growth. It has been suggested that the chin cup must be worn by the patient till growth is complete if meaningful results are to be expected.
Early orthodontic treatment specifically designed to reduce overjet can affect the incidence of maxillary incisor trauma in children. Early intervention is of significant value for the management of tooth eruption disturbances in patients with ectopic eruption, presence of mesiodens, canine impactions etc. It also has psychological benefits, and there is strong evidence to suggest that children who received early orthodontic treatment have higher self-esteem and more positive childhood experience than those who did not receive it.
Extraction and nonextraction
Extraction of teeth has been a most reliable and widely practised method of gaining space to resolve intra-arch discrepancy. However, the introduction of other methods of gaining space, early treatment, growth modification therapy, better anchorage control and changing aesthetic standards for a fuller face and profile have all contributed to the non-extraction approach. The decision of extraction or nonextraction can be difficult in many circumstances, and there are several factors that govern the decision-making process.
The degree of intra-arch crowding is one of the parameters to determine the need for extractions. Equally important is to predict the effect of subsequent treatment on lipprotrusion and soft tissue profile. In a general sense, the more severe pretreatment crowding, the more likely that extractions are required to gain adequate space to resolve discrepancy. The modern orthodontic treatment planning should be individualized since every patient varies morphologically and functionally. Therefore, the specific amount of crowding may require extractions in one patient; however, the same may not warrant extractions in another. The author considers nasolabial angle as one of the determinants of extraction therapy. If a patient has obtuse nasolabial angle, it is not appropriate to retract the lip further. Extractions are required if the teeth are severely proclined, which does not allow the patient to achieve adequate lip seal during swallowing. The impact of sagittal movement of incisors on the lip position is also influenced by the morphology of lips. It should be noted that thinner, incompetent lips respond more dramatically to incisor position change than do thicker and competent lips.
If mandibular incisors are likely to be advanced as a part of nonextraction treatment plan, the periodontal condition, especially the width and thickness of attached gingiva, should be considered. In a patient with signs of gingival recession, or thin or deficient attached gingiva associated with mandibular anterior teeth, the labial positioning of such teeth is likely to cause progression of the condition.94 It may be advisable to reconsider extraction therapy or place a gingival graft prior to treatment in such cases. The resolution of moderate crowding in patients with deep overbite, upright incisors and a convergent skeletal profile should be managed with nonextraction treatment approach as the extraction therapy will require retraction of already upright teeth and greater movements of roots to achieve normal tooth angulations.
Surgical and nonsurgical treatment
The presence or absence of skeletal components contributing to the malocclusion and the amount of growth remaining for a given patient influence the surgical or nonsurgical treatment decision. In a growing patient, there are many nonsurgical treatment options available to achieve desirable treatment goals. Several orthopaedic appliances are used to resolve skeletal discrepancies in Class II and Class III malocclusions. Obviously for adult patients, these nonsurgical, orthopaedic treatment options are not possible due to the absence of growth potential.
If surgical intervention is the treatment of choice, when should it be performed? Is it before or after the completion of growth? Surgical correction before the completion of growth is certainly a controversial issue. There is no scientific evidence to support that surgery performed at an early age creates a normal environment to promote favourable growth.95 Surgical correction of abnormal skeletal bases, carried out at an early stage of development, does not contribute to the improvement of abnormal growth pattern.95,96
In a mild to moderate Class II patient, it is possible to achieve normal occlusal relationships with a combination of favourable growth and well-designed treatment mechanics. However, it is unlikely that a patient with very severe skeletal abnormalities and unfavourable growth pattern will suddenly grow normally and establish normal relationships of various components involved. Most believe that surgery should not be attempted before the completion of growth.
Dentofacial aesthetics is probably one of the common reasons why patients opt for surgical intervention. Surgical treatment produces dramatic facial changes in patients with certain sagittal discrepancies, like increased facial convexity, and vertical discrepancies, like increased lower facial height, which are not possible through orthodontic tooth movement alone.97,98
Therefore, when it comes to making a treatment option decision, the clinician should fully explore the best surgical and nonsurgical options and weigh advantages and disadvantages of each procedure and its impact on aesthetics, function and stability.
Orthopaedic and orthodontic treatment
It has been universally recognized that abnormal growth is responsible for a high percentage of malocclusions, both sagittaly and vertically. The goal of orthopaedic treatment is to correct existing or developing skeletal imbalances to improve the orofacial environment at an early stage of development. Therapeutically-induced neuromuscular and skeletal adaptations in the craniofacial complex initiated during the mixed dentition stage can be achieved using variety of functional appliances. Quite often, the differential growth between the maxilla and the mandible – mandible growing faster than maxilla – contributes significantly to the improvement of occlusal relationships in Class II malocclusion. Does this mean that Class II malocclusions in growing patients are self-correcting? It is author's experience that in spite of this differential growth, the occlusion still remains the same as a result of maxillary teeth compensation by downward and forward movements. The key to control and correct this discrepancy is to hold the maxillary teeth and prevent them from displacing downward and forward by using headgears or orthopaedic appliances. Also, in growing Class II individuals, mandibular growth can be enhanced; however, there is little evidence to support that the growth of the mandible can be restrained by using chin cup in growing Class III individuals.99
Class III malocclusion is one of the most difficult malocclusions to treat in mixed dentition stage. Early treatment with orthopaedic facial mask, ideally initiated at the time of eruption of maxillary central incisors, produces the most dramatic results in the shortest period of time. The early intervention of Class III malocclusion does not necessarily eliminate the need for orthognathic surgery, especially in patients with significant skeletal imbalances and a family history of Class III malocclusion.
Treatment sequencing
Establishing a ‘sequenced-treatment mechanics plan’ based on the specific tooth movement goals is essential for a smooth and efficient treatment progress. After the formulation of final treatment plan, the practitioners must be precise in outlining the steps of treatment and the rationale for these steps. In most patients, the treatment mechanics used to achieve a particular goal will also help in the correction of another problem.100
In a routine orthodontic treatment, the posterior cross-bites should be corrected first prior to addressing other problems. The gross correction of asymmetries may be accomplished easily before the complete bonding is done. However, in some cases, it is mandatory to achieve intra-arch alignment of teeth to facilitate correction in both the maxillary and mandibular arches, especially if elastics are going to be used. Typical treatment sequencing in patients with deep overbite involves initial alignment of teeth followed by intrusion of incisors. Overbite correction usually precedes the closure of extraction spaces; however, in some cases, simultaneous intrusion and retraction of incisors can be accomplished. In nonextraction treatment approach, the maxillary molars can be distalized using fixed distalizing modules to gain adequate space and accomplish molar correction. This will be followed by the stabilization of molars in their new positions, intrusion of incisors, distal drifting of bicuspids, bonding of mandibular arch and progressing to finishing and detailing (Fig 1.44). The above-mentioned couple of examples demonstrate the fact that the treatment sequencing should be individualized, should not follow a set pattern and should be based on the specific tooth movement goals.

Figure 1.44 Treatment sequencing. Intraoral photographs of a 28-year-old male patient show (A) maxillary and mandibular anterior crowding, (B) bilateral posterior crossbite and (C) labially placed maxillary canines. The proposed treatment sequencing for this patient is correction of bilateral posterior crossbite; bilateral distalization of maxillary molars; stabilization of maxillary molars in their new positions, while simultaneous differential retraction of bicuspids (also to address evident anterior midline shift) and intrusion of incisors; mandibular arch bonding; alignment and levelling; finishing and detailing of dentition and placement of retainers.
The concept of treatment sequencing in the management of patients with interdisciplinary treatment approach is little different and more complex. An interdisciplinary dentofacial therapy is the ultimate utilization of the expertise and skills in the various disciplines of dentistry.101 It involves a team of various specialists like orthodontist, prosthodontist and periodontist with active communication among themselves throughout treatment, from the diagnosis and treatment planning stages through to the completion of active treatment and into the retention phase. The primary goal of treatment sequencing here is to organize the sequence of various treatment procedures provided by different specialists into a logical order so that each intervention performed by one of the specialists from the interdisciplinary team facilitates the next in order.102 Interdisciplinary treatment typically involves a sequence of disease control (periodontal, periapical infections), correction of structural malrelationships, correction of periodontal defects, restorative therapy and maintenance of optimal oral health.
Evaluation of treatment progress
After the execution of final treatment plan, it is an important step to closely monitor the treatment progress. Active orthodontic treatment phase, the duration of which is estimated and defined at the beginning of treatment and the same is communicated to the patient, involves a series of procedures and events; the goal of every practitioner is to make sure that it proceeds smoothly and efficiently. This is often influenced by many factors like efficiency of orthodontic appliances and their clinical management by the doctor, keeping regular appointments by the patient and reinforcement of oral hygiene protocol by the orthodontic office. It is a good practise to continue to focus on certain specific treatment goals like planned tooth movements or skeletal movements and roughly estimate the time frame by which these goals are expected to be met in order to have total control of progress throughout treatment.
If, for example, maxillary molar distalization therapy with fixed distalizing module has been implemented to gain space in the maxillary arch, its progress should be monitored to check if the molar is being moved distally in a predetermined direction. Certain associated untoward movements like palatal movement of molars should be detected early and the force direction should be altered promptly to avoid unnecessary delays. Quite often, in spite of careful formulation of treatment plan, treatment does not always proceed as planned, especially for patients in whom growth or cooperation is expected. Decalcification of the enamel surface mainly due to poor patient compliance is associated with fixed orthodontic appliance therapy.103,104 Therefore, appropriate measures should be instituted to prevent the development of white spot lesions and ensure proper treatment progress. An initial inaccurate diagnosis may sometimes lead to the changes in treatment direction. These unexpected revisions of treatment plan are generally expected by the patient if the possibilities are defined and explained at the beginning of treatment. The goal of any good orthodontic treatment plan is to make sure that the decision-making process is complete before the treatment is executed. Progressive evaluation and reevaluation of treatment progress will only help the clinician intercept and reverse untoward events, if any, as they appear rather than allowing them to become big problems leading to a significant extension of overall treatment time. This will also ensure good patient experience and higher levels of patient satisfaction.
Conclusion
Diagnosis in orthodontics, like in other disciplines of dentistry and medicine, is the recognition of abnormal conditions, the practical synthesis of the diagnostic information that helps the clinician to plan an appropriate treatment strategy. It is essential to have a sound knowledge of normal anatomy and craniofacial growth to recognize various dentofacial deformities; and high-quality, uncompromised diagnostic records for further evaluation of teeth and oral structures, occlusion and facial and jaw proportions.
The entire process of orthodontic diagnosis and treatment planning involves recognition of the various characteristics of malocclusion, defining the nature of the problem and its aetiology and designing a treatment strategy based on the needs and desires of the individual patient. Once patient's diagnostic information is synthesized into dental, skeletal, functional and soft tissue profile, the orthodontic treatment goals should be clearly defined. Proper treatment planning depends on accurate diagnosis, which in turn requires objective, relevant and accurate information, patient data and an analysis of various records. Establishing a ‘sequenced-treatment mechanics plan’ based on the specific tooth movement goals is essential for a smooth and efficient treatment progress and treatment outcome.
References
1. Knott, V.B. Changes in the cranial base measures of human males and females from age 6 years to early adulthood. Growth. 1971;35:145–158.
2. Hight, J.R. The correlation of spheno-occipital synchondrosis fusion to hand-wrist maturation. Am J Orthod. 1981;79:464–465.
3. Björk, A. Cranial base development. Am J Orthod. 1955;41:198–225.
4. Baumrind, S., Korn, E.L., Isaacson, R.J., et al. Superimpositional assessment of treatment-associated changes in the temporoman-dibular joint and the mandibular symphysis. Am J Orthod. 1983;84:443–465.
5. Buschang, P.H., Santos-Pinto, A. Condylar growth and glenoid fossa displacement during childhood and adolescence. Am J Orthod Dentofacial Orthop. 1998;113:437–442.
6. Enlow, D.H. Facial growth, 3rd, Philadelphia: WB Saunders, 1990.
7. Björk, A. Sutural growth of the upper face studied by the implant method. Acta Odontol Scand. 1966;24(2):109–127.
8. Schudy, F.F. Vertical growth versus anteroposterior growth as related to function and treatment. Angle Orthod. 1964;34(2):75–93.
9. Ricketts, R.M. The influence of orthodontic treatment on facial growth and development. Angle Orthod. 1960;30:103–133.
10. Björk, A. Variations in the growth of the human mandible. Longitudinal radiographic study by the implant method. J Dent Res. 1963;42(suppl 1):400–411.
11. Baumrind, S., Ben-Bassat, Y., Korn, E.L., et al. Mandibular remodeling measured on cephalograms I. Osseous changes relative to superimposition on metallic implants. Am J Orthod Dentofacial Orthop. 1992;102:134–142.
12. Riolo, M.L., Moyers, R.E., McNamara, J.A., Jr., et al. An atlas of craniofacial growth. Ann Arbor: University of Michigan, Center for human growth and development, 1974.
13. Björk, A., Skieller, V. Normal and abnormal growth of the mandible: a synthesis of longitudinal cephalometric implant studies over a period of 25 years. Eur J Orthod. 1983;5:1–46.
14. Bishara, S.E., Jakobsen, J.R., Treder, J., et al. Arch width changes from 6 weeks to 45 years of age. Am J Orthod Dentofacial Orthop. 1997;111:401–409.
15. Schudy, F.F. The rotation of the mandible resulting from growth: its implications in Orthodontic treatment. Angle Orthod. 1965;35(1):36–50.
16. Schudy, F.F. Vertical growth versus anteroposterior growth as related to function and treatment. Angle Orthod. 1964;34(3):75–93.
17. Schudy, F.F. The control of vertical overbite in clinical orthodontics. Angle Orthod. 1968;38(1):19–39.
18. Buschang, P.H., Ronald De La Cruz, Anthony, D., Viazis, Arto Demirjian, et al. Longitudinal shape changes of the nasal dorsum. Am J Orthod Dentofacial Orthop. 1993;103:539–543.
19. Genecov, J.S., Sinclair, P.M., Dechow, P.C. Development of the nose and soft tissue profile. Angle Orthod. 1990;60(3):191–198.
20. Subtelny, J.D. Longitudinal study of soft tissue facial structures and their profile characteristics, defined in relation to underlying skeletal structure. Am J Orthod. 1959;45:481–507.
21. Chaconas, S.J. A statistical evaluation of nasal growth. Am J Orthod. 1969;56:403–414.
22. Manera, J.F., Subtelny, M.D. A cephalometric study of the growth of the nose. Am J Orthod. 1961;47:703–705.
23. Mamandras, A.H. Linear changes of the maxillary and mandibular lips. Am J Orthod. 1988;94:405–410.
24. Vig, P.S., Cohen, A.M. Vertical growth of the lips: a serial cephalometric study. Am J Orthod. 1979;75:405–415.
25. Schudy, G.F. Posttreatment craniofacial growth: its implications in orthodontic treatment. Am J Orthod. 1974;65(1):39–57.
26. Behrents, R.G. Growth in the aging craniofacial skeleton: craniofacial growth series. Ann Arbor: University of Michigan, 1985.
27. Bensch, L., Braem, M., Van Acker, K., et al. Orthodontic treatment considerations in patients with diabetes mellitus. Am J Orthod Dentofacial Orthop. 2003;123:74–78.
28. Firkin, D., Ferguson, J. Diabetes mellitus and the dental patient. NZ Dent J. 1985;81:7–11.
29. Geza, T., Rose, L. Dental correlations for diabetes mellitus. In: Rose L.F., Kaye D., eds. Internal medicine for dentistry. 2nd. St. Louis: C.V. Mosby; 1990:1153.
30. Van Venrooy, J.R., Proffit, W.R. Orthodontic care for compromised patients: possibilities and limitations. J Am Dent Assoc. 1985;111:262–266.
31. Ong, C.K., Walsh, L.J., Harbrow, D., et al. Orthodontic tooth movement in the prednisolone – treated rat. Angle Orthod. 2000;70(2):118–125.
32. Ashcraft, M.B., Southard, K.A., Tolley, E.A. The effect of corticosteroid induced osteoporosis on orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 1992;102:310–319.
33. Graham, J.W. Bisphosphonates and orthodontics. J Clin Orthod. 2006;40(7):425–428.
34. Moorrees, C.F.A., Kean, M.R. Natural head position, a basic consideration in the interpretation of cephalometric radiographs. Am J Phys Anthropol. 1956;16:213–234.
35. Viazis, A.D. A cephalometric analysis based on natural head position. J Clin Orthod. 1991;25:172–182.
36. Solow, B., Tallgren, A. Head posture and craniofacial morphology. Am J Phys Anthropol. 1976;44:417–436.
37. Solow, B., Siersbaek-Nielsen, S., Greve, E. Airway adequacy, head posture, and craniofacial morphology. Am J Orthod. 1983;86:495–500.
38. Greenfield, B., Kraus, S., Lawrence, E., et al. The influence of cephalostatic ear rods on the positions of the head and neck during a postural recordings. Am J Orthod Dentofacial Orthop. 1989;95:312–318.
39. Lines, P.A., Lines, R.R., Lines, C.A. Profile metrics and facial esthetics. Am J Orthod. 1978;73:648–657.
40. Proffit, W.R. Orthodontic diagnosis: the development of a problem list. In: Proffit W., ed. Henry fields. Contemporary orthodontics. St. Louis: C.V. Mosby; 1986:123–167.
41. Stella, J.P., Epker, B.N. Systematic esthetic evaluation of the nose for cosmetic surgery. Oral Maxillofac Surg Clin North Am. 1990;2:273–287.
42. Graber, T.M., Rakosi, T., Petrovic, A. Functional analysis. In: Graber T.M., Rakosi T., Petrovic A., eds. Dentofacial orthopedics with functional appliances. St. Louis: The C.V. Mosby; 1985:111–149.
43. Williamson, E.H. Occlusion and TMJ dysfunction. J Clin Orthod. 1981;15:393–410.
44. Okeson, J.P. Management of temporomandibular disorders and occlusion, 2nd, St. Louis: The C.V. Mosby, 1989.
45. Williamson, E.H. Occlusion and TMJ dysfunction. J Clin Orthod. 1981;15:333–350.
46. Williamson, E.H. Occlusion: understanding or misunderstanding. Angle Orthod. 1976;46:86–93.
47. Karad, A. Excellence in finishing: current concepts, goals and mechanics. J Indian Orthod Soc. 2006;39:126–138.
48. Roth, R.H. Functional occlusion for the orthodontist. J Clin Orthod. 1981;1:32–50.
49. Mclaughlin, R.P., Bennett, J.C. Finishing with the preadjusted orthodontic appliance. Semin Orthod. 2003;9:165–183.
50. Angle, E.H. Malocclusion of the teeth, 7th, Philadelphia: S.S. White, 1907.
51. Andrews, L.F. The six keys to normal occlusion. Am J Orthod. 1972;63:296–309.
52. Okeson, J.P. Management of temporomandibular disorders and occlusion, 3rd, St. Louis: C.V. Mosby, 1993.
53. Stallard, H. Organic occlusion. In: Parone B.W., ed. Oral rehabilitation and occlusion, section II, topic 9. San Francisco: University California, 1972.
54. Huffman, R.W., Regenos, T.W. Principles of occlusion. London: H and R press, 1973.
55. Roth, R.H. The maintenance system and occlusal dynamics. Dent Clin North Am. 1976;20:761–788.
56. Burstone, C.J. Lip posture and its significance in treatment planning. Am J Orthod. 1967;53:262–284.
57. Breece, G.L., Nieberg, L.G. Motivations for adult orthodontic treatment. J Clin Orthod. 1986;20:166–171.
58. Shaw, W.C., Rees, G., Dawe, M., et al. The influence of dentofacial appearance on the social attractiveness of young adults. Am J Orthod. 1985;87:21–26.
59. Ahmad, I. Geometric considerations in anterior dental esthetics: restorative principles. Pract Periodont Aesthet Dent. 1998;10(7):813–822.
60. Janzen, E. A balanced smile: a most important treatment objective. Am J Orthod. 1977;72:359–372.
61. Chaconas, S.J. Orthodontic diagnosis and treatment planning. J Oral Rehabil. 1991;18:531–545.
62. Norton, L.A. The effect of aging cellular mechanisms on tooth movement. Dent Clin North Am. 1988;32:437–446.
63. Sodek, J. A comparison of the rates of synthesis and turnover of collagen proteins in adult rat periodontal tissues and skin using microassay. Arch Oral Biol. 1977;22:655–665.
64. Musich, D.R. Assessment and description of the treatment needs of adult patients evaluated for orthodontic therapy. Part I, II, III. Int J Adult Orthodon Orthognath Surg. 1986;1(1):55–67. [1(2):101–107,1(4):251–274].
65. Mirabella, A.D. Risk factors for apical root resorption of maxillary anterior teeth in adult orthodontic patients. Am J Orthod Dentofacial Orthop. 1995;108:48–55.
66. Cangialosi, T.J., Riolo, M.L., Owens, S.E., Jr., et al. The ABO discrepancy index: a measure of case complexity. Am J Orthod Dentofacial Orthop. 2004;125:270–278.
67. Proffit, W.R., Vig, K.W., Turvey, T.A. Early fracture of the mandibular condyles: frequently an unsuspected cause of growth disturbances. Am J Orthod. 1980;78:1–24.
68. Lund, K. Mandibular growth and remodeling process after mandibular fractures. Acta Odontol Scand. 32(suppl 64), 1974.
69. Michaud, P.A., Frappier, J.U., Pless, I.B. Compliance in adolescents with chronic disease. Arch Fr Pediatr. 1991;48:329–336.
70. Blowey, D.L., Hébert, D., Arbus, G.S., et al. Compliance with cyclosporine in adolescent renal transplant recipients. Pediatr Nephrol. 1997;11:547–551.
71. Peck, S., Peck, L., Kataja, M. The gingival smile line. Angle Orthod. 1992;62:91–100.
72. Drobocky, O.B., Smith, R.J. Changes in facial profile during orthodontic treatment with extraction of four first premolars. Am J Orthod Dentofacial Orthop. 1989;95:220–230.
73. Nanda, R.S., Meng, H., Kapila, S., et al. Growth changes in the soft tissue facial profile. Angle Orthod. 1990;60:177–190.
74. Varela, M. Impact of orthodontics on the psychologic profile of adult patients: a prospective study. Am J Orthod Dentofacial Orthop. 1995;108:142–148.
75. Breece, G.L., Nieberg, L.G. Motivation for adult orthodontic treatment. J Clin Orthod. 1986;20:166–171.
76. Melsen, B. Adult orthodontics: factors differentiating the selection of biomechanics in growing and adult individuals. Int J Adult Orthodon Orthognath Surg. 1988;3:167–177.
77. Haskell, B.S., Spencer, W.A., Day, M. Auxiliary springs in continuous arch treatment: part 1. An analytical study employing the finite-element method. Am J Orthod Dentofacial Orthop. 1990;98:387–397.
78. Persson, M., Thilander, B. Palatal suture closure in man from 15 to 35 years of age. Am J Orthod. 1977;72:42–52.
79. Kahl-Nieke, B., Fischbach, H., Schwarze, C.W. Postretention crowding and incisor irregularity – a long-term follow-up evaluation of stability and relapse. Br J Orthod. 1995;22:249–257.
80. Melsen, B., Agerbaek, N., Markenstam, G. Intrusion of incisors in adult patients with marginal bone loss. Am J Orthod Dentofacial Orthop. 1989;96:232–241.
81. Tweed, C. Clinical orthodontics, 1. C.V. Mosby: St. Louis, 1966:13–29.
82. Björk, A. The face in profile. Sven Tandlak Tidskr. 40, 1947.
83. Björk, A. Prediction of mandibular growth rotation. Am J Orthod. 1969;55:585–599.
84. Skieller, V., Björk, A., Linde-Hansen, T. Prediction of mandibular growth rotation evaluated form a longitudinal implant sample. Am J Orthod. 1984;86:359–370.
85. Arnold, S. Analysis of leeway space in the mixed dentition, Master's thesis. Boston: Boston University, 1991.
86. Moyers, R.E., van der Linden, F.P.G.M., Riolo, M.L., et al. Standards of human occlusal development. In: Monograph 5. Craniofacial Growth Series. Ann Arbor: Center of Human Development, The University of Michigan; 1976.
87. Osborn, W.S., Nanda, R.S., Currier, G.F. Mandibular arch perimeter changes with lip bumper treatment. Am J Orthod Dentofacial Orthop. 1991;99:527–532.
88. Bergersen, E.O. A cephalometric study of the clinical use of the mandibular labial bumper. Am J Orthod. 1972;61:578–602.
89. Little, R.M., Reidel, R.A., Stein, A. Mandibular arch length increase during the mixed dentition: postretention evaluation of stability and relapse. Am J Orthod Dentofacial Orthop. 1990;97:393–404.
90. Haas, A.J. The treatment of maxillary deficiency by opening the mid-palatal suture. Angle Orthod. 1965;65:200–217.
91. Wieslander, L. Early or late cervical traction therapy of Class II malocclusions in the mixed dentition. Am J Orthod. 1975;67:432–439.
92. McNamara, J.A., Jr., Bookstein, F.L., Shaughnessy, T.G. Skeletal and dental relationships following functional regulator therapy on Class II patients. Am J Orthod. 1985;88:91–109.
93. Turley, P. Managing the developing Class III malocclusion with palatal expansion and face mask therapy. Am J Orthod Dentofacial Orthop. 2002;122(4):349–352.
94. Artun, J., Krogstad, O. Periodontal status of mandibular incisors following excessive proclination. Am J Orthod Dentofacial Orthop. 1987;91:225–232.
95. Washburn, M.C., Schendel, S.A., Epker, B.N. Superior repositioning of the maxilla during growth. J Oral Maxillofacial Surg. 1982;40:142–149.
96. Huang, C.S., Ross, R.B. Surgical advancement of the retrognathic mandible in growing children. Am J Orthod. 1982;82:89–103.
97. McNeil, R.W., West, R.A. Severe mandibular prognathism: orthodontic versus surgical orthodontic treatment. Am J Orthod. 1977;72:176–182.
98. Sinclair, P.M. Orthodontic consideration in adult surgical orthodontic cases. Dent Clin North Am. 1988;32:509–528.
99. Sugawara, J., Asano, T., Endo, N., et al. Long-term effects of chin cap therapy on skeletal profile in mandibular prognathism. Am J Orthod Dentofacial Orthop. 1990;98:127–133.
100. Lindauer, S.J. Orthodontic treatment planning. In: Nanda R., Kuhlberg A., eds. Biomechanics in clinical orthodontics. Philadelphia: WB Saunders; 1996:23–49.
101. Roblee, R.D. Interdisciplinary dentofacial therapy. In: Roblee R.D., ed. Interdisciplinary dentofacial therapy – a comprehensive approach to optimal patient care. Singapore: Quintessence publishing; 1994:17–43.
102. Spear, F.M., Kokich, V.G., Mathews, D.P. Interdisciplinary management of a patient with a skeletal deformity. Adv Esthet Interdiscip Dent. 2005;1(2):12–18.
103. Årtun, J., Brobakken, B.O. Prevalence of carious white spots after orthodontic treatment with multibonded appliances. Eur J Orthod. 1986;8:229–234.
104. Øgaard, B. Prevalence of white spots lesions in 19 year olds: a study on untreated and orthodontically treated persons 5 years after treatment. Am J Orthod Dentofacial Orthop. 1989;96:423–427.