Neuromuscular Junction
Structure of neuromuscular junction
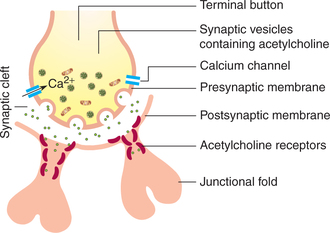
Neuromuscular junction refers to the intimate contact of the nerve endings with the muscle fibre to which they innervate. Characteristics of the nerve and muscle fibre at and near the neuromuscular junction are given as follows (Fig. 2.2-1).
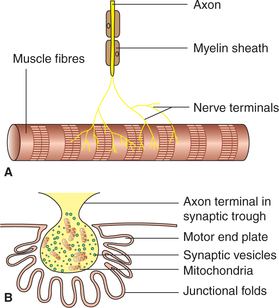
Fig. 2.2-1 Structure of neuromuscular junction: A, the axon of the neuron loses its myelin sheath and divides into fine branches and B, structure of terminal button and motor end plate.
Terminal button. The axon of a neuron supplying a skeletal muscle loses its myelin sheath and divides into a number of fine branches which end in small swellings (knobs) called terminal buttons or end feet which form a neuromuscular junction at the centre of muscle fibre (Fig. 2.2-1 A). The nerve terminal or the so-called synaptic knob contains a large number of vesicles (about three lakh) containing acetylcholine and mitochondria. The acetylcholine is synthesized by the mitochondria and is stored in the vesicles (Fig. 2.2-1B).
Presynaptic membrane. This refers to the axonal membrane lining the terminal buttons of the nerve endings.
Synaptic cleft. It is a 50-100nm wide space between the presynaptic and the postsynaptic membrane. It is filled by extracellular fluid with reticular fibres forming the matrix.
Postsynaptic membrane (Fig. 2.2-1 B). This is the name given to the muscle fibre membrane (sarcolemma) in the region of neuromuscular junction. The muscle membrane in this region is thickened and depressed to form the synaptic trough in which the terminal button fits. This thickened portion of the muscle membrane is also called motor end plate. Further, the postsynaptic membrane is thrown into large number of folds called subneural clefts or pallisades. These increase the surface area. The postsynaptic membrane near the junction folds contains receptor sites for acetylcholine called the nicotinic receptors. The matrix of subneural cleft contains the enzyme cholinesterase which can degrade acetylcholine.
Neuromuscular transmission
The skeletal muscle is stimulated only through its nerve. The neuromuscular junction transmits the impulses from the nerve to muscle. The sequence of events which causes transmission of impulse through the neuromuscular junction are:
• Release of acetylcholine by the nerve terminals,
• Effect of acetylcholine on the postsynaptic membrane,
• Development of end plate potential,
• Miniature end plate potential,
Release of acetylcholine by the nerve terminals
When the nerve impulse (action potential) travelling in the nerve fibre (axon) reaches the terminal buttons, the voltage-gated Ca2+ channels present on the presynaptic membrane open up, increasing its permeability to Ca2+ ions. Consequently the Ca2+ ions present in the extracellular fluid (ECF) of synaptic cleft enter the terminal buttons. The elevated Ca2+ levels in the cytosol of terminal buttons trigger a marked increase in exocytosis of vesicles, releasing acetylcholine in the synaptic cleft (Fig. 2.2-2).
Effect of acetylcholine on the postsynaptic membrane
The acetylcholine so released diffuses in the synaptic cleft and binds to the nicotinic-acetylcholine receptors located mainly on the junctional folds of the motor end plate (postsynaptic membrane).
Development of end plate potential
Due to opening of the acetylcholine-gated channels in the end plate membrane, a large number of Na+ ions from the ECF enter inside the muscle fibre following the electrochemical gradient.
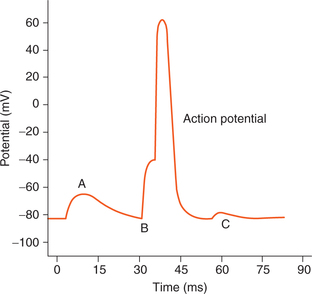
The resting membrane potential at the postsynaptic membrane is about -80 to -90 mV. When sodium ions carrying with them large numbers of positive charges enter inside, there occurs depolarization causing a local positive potential change inside the muscle fibre membrane called the end plate potential.
The end plate potential is non-propagative but when a critical level of -60 mV is reached, the end plate potential triggers the development of action potential in the muscle fibre (Fig. 2.2-3). The action potentials are generated on either side of the end plate and conducted away from the end plate in both the directions along the muscle fibres, thus causing muscle contraction.
Miniature end plate potential
Even at rest, small quanta of acetylcholine are released randomly from the nerve terminal. Each quantum of acetylcholine produces a weak end plate potential about 0.5mV in magnitude. This is called miniature end plate potential.
Removal of acetylcholine
The acetylcholine released in the synaptic cleft stays for a short period and is removed within 1 ms by two means as detailed below.
• Most of the acetylcholine is destroyed by the enzyme acetylcholinesterase, which is present in the matrix of synaptic cleft.
• A small amount of the acetylcholine diffuses out of the synaptic space and is then no longer available to act on the muscle fibre membrane.
It is important to note that the rapid removal of acetylcholine prevents the repeated excitation of muscle fibre.
Drugs affecting and disorders of neuromuscular junction
Drugs affecting neuromuscular junction
Neuromuscular blockers
Neuromuscular blockers are the drugs that block transmission at the neuromuscular junction. Some of the common neuromuscular blockers which are commonly used in clinical practice for producing muscle relaxation during surgery are given below
1. Curare. Curare prevents the neuromuscular transmission by competitive inhibition. The acetylcholine released thus cannot combine with the receptors and so end plate potential does not develop.
2. Bungarotoxin found in the venom of deadly snakes also blocks neuromuscular transmission by binding with the acetylcholine receptors.
3. Succinylcholine and carbamylcholine act like acetylcholine and cause depolarization of the postsynaptic membrane. But, these are not destroyed by cholinesterase and so the muscle remains in a depolarized state for a long time; thus, they block the myoneural junction by keeping the muscle in a depolarized state.
4. Botulinum toxin derived from the bacteria Clostridium botulinum blocks the transmission across the myoneural junction by preventing the release of acetylcholine from the terminal buttons of the nerve endings.
Disorder of neuromuscular junction
Myasthenia gravis
Myasthenia gravis is a disorder in which the myoneural junction is unable to transmit signals from the nerve fibre to muscle fibres, thereby causing paralysis of the involved muscles. Myasthenia is probably an autoimmune disease. In this disease the antibodies are produced against the acetylcholine-gated channels (receptors) present on the motor end plate, which destroy these channels. Thus, the acetylcholine released at the nerve terminal is not able to produce adequate end plate potential to excite the muscle fibre. If the disease is intense enough, the patient dies of paralysis, in particular, paralysis of respiratory muscles.
 Drugs affecting neuromuscular junction
Drugs affecting neuromuscular junction