Physiological Activities in Mouth, Pharynx and Oesophagus
Introduction
The functioning of digestive system starts from the mouth (oral cavity) and ends at the anus.
ingestion of food involves following processes:
• Placing of food into the mouth,
• Mastication, i.e. chewing the food into smaller pieces,
The above mentioned physiological activities which take place in the mouth, pharynx and oesophagus are discussed in this chapter.
Mastication
Mastication or chewing refers to the process by which the food placed in the mouth is cut and grounded into smaller pieces. It involves:
• Action of teeth—the incisors provide a strong cutting action, whereas the molars have a grinding action and
• Co-ordinated movements of the tongue and muscles of the oral cavity.
Chewing reflex
Mastication or chewing, though a voluntary act, is coordinated by a chewing reflex that facilitates the opening and closing of the jaw. The chewing reflex operates as follows:
• When the mouth is opened to place the food inside it, the muscles of jaw are stretched which leads to their contraction due to stretch reflex, thereby raising the jaw to cause closure of the mouth.
• When the mouth is closed, the food comes into contact with buccal receptors which cause reflex inhibition of the muscles of mastication and also initiate a reflex contraction of the digastric and lateral pterygoid muscles, causing the mouth to open.
• This cycle of opening and closing the jaw leads to mastication. The tongue contributes to the grinding process by positioning the food between the upper and lower teeth.
Muscles of mastication
Muscles of mastication include masseter, temporalis, and internal and external pterygoids. Buccinator is an accessory muscle of mastication which prevents accumulation of food between the cheek and teeth.
Net effect of mastication. The bolus of food becomes a homogenized mixture of small food particles, saliva and mucus, which is easy to swallow and digest.
Lubrication of food by saliva
Salivary glands
In addition to the chewing, another important physiological activity which takes place in the mouth is lubrication of food by saliva. The saliva is secreted by three pairs of major salivary glands.
1 Parotid glands
Location. Parotid glands are the largest salivary glands (each weighing 20–30 g) located near the angles of jaw.
Acini. The parotid glands are purely serous glands (Fig. 7.2-1) which secrete watery saliva containing more than 90% water. Parotid glands secrete 25% of the total salivary secretion (which is about 1500 mL/day).
Ducts. Ducts of the parotid glands open on the inner side of the right and left cheek, and pour their secretions in the vestibule.
2 Sublingual glands
Location. The sublingual gland is the smallest of the three main salivary glands. It lies just below the mucosa on the floor of mouth. Each gland raises a ridge of mucosa which starts at the sublingual papilla and runs laterally and backwards. The ridge is called the sublingual fold.
Acini. The sublingual gland contains both serous and mucous acini (Fig. 7.2-1), the latter predominating.
Ducts. Ducts of sublingual gland are 8–20 in number. Most open into the mouth on the summit of the sublingual fold but a few may open into the submandibular duct.
3 Submandibular glands
Location. The submandibular glands are the large salivary glands which lie (one on each side) partly under cover of the body of the mandible.
Acini. The submandibular gland is composed of a mixture of serous and mucous acini, the former predominating (Fig. 7.2-1).
Ducts. S-shaped duct of each submandibular gland opens on the sublingual papilla located just lateral to the frenulum lingua.
Note. The sublingual and the submandibular glands secrete a fluid that contains a higher concentration of proteins and so is more viscus as compared to the watery secretion of parotid glands.
Saliva
Secretion and composition
Amount. Under normal circumstances the salivary glands secrete about 500–1500 mL of saliva every day. pH of saliva varies from 6 to 7.4.
Composition. Saliva is composed of 99% water and 1% solids, which include:
• Organic substances, such as L-amylase (ptyalin), lingual lipase, kallikrein, lysozyme, small amounts of urea, uric acid, cholesterol and mucin.
Note. Composition of saliva varies with the salivary flow rate.
Mechanism of formation of saliva
Mechanism of formation of saliva involves two processes.
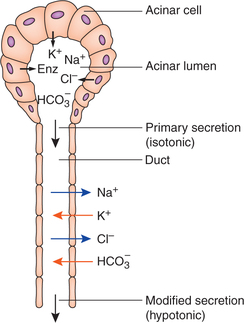
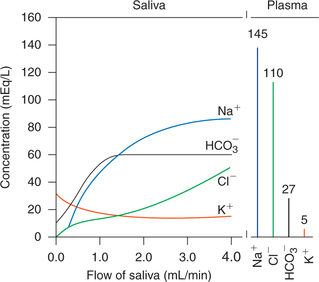
1. Primary secretion of saliva. The acinar cells of salivary glands secrete the initial saliva into the salivary ducts. The initial saliva is isotonic, i.e. has the same Na+, Cl−, K+ and  concentrations as plasma (Fig. 7.2-2). However, the initial saliva is soon modified by the salivary ducts.
concentrations as plasma (Fig. 7.2-2). However, the initial saliva is soon modified by the salivary ducts.
2. Modification of saliva. The ductal cells that line the tubular portions of the salivary ducts change the composition of initial saliva by following processes (Fig. 7.2-2):
• Reabsorption of Na+ and Cl− occurs in the ductal cells, therefore, the concentration of these ions is lower than their plasma concentration.
• Secretion of K+ and  is caused by the ductal cells, therefore, the concentrations of these ions are higher than their plasma concentrations.
is caused by the ductal cells, therefore, the concentrations of these ions are higher than their plasma concentrations.
• Modified saliva becomes hypotonic in the ducts because the ducts are relatively impermeable to water.
Note. Aldosterone acts on the ductal cells to increase the reabsorption of Na+ and Cl− from the salivary ducts (analogous to its actions on renal tubule). Thus a high Na+/Cl− ratio is seen when aldosterone is deficient in Addison's disease, and in presence of excess aldosterone the concentration of sodium chloride in saliva falls almost to zero and increases K+ concentration.
Effects of flow rate on the composition of saliva
1. At high flow rates, there is less time for reabsorption and secretion, and therefore the saliva is most like the initial secretion by the acinar cells. Thus, with the increase in flow rate the concentration of ions changes (Fig. 7.2-3):
• Sodium ion (Na+) concentration increases progressively to a plateau value of 80–90 mEq/L.
• Chloride ions (Cl−) concentration increase to about 50 mEq/L.
Note. Na+ and Cl− concentrations of saliva are always lower than that in the plasma.
• Potassium ion (K+) concentration decreases to 15–20 mEq/L.
• Bicarbonate ion  concentration increases when salivary flow rate increases (up to 50–70 mEq/L).
concentration increases when salivary flow rate increases (up to 50–70 mEq/L).
2. At low flow rates, there is more time for reabsorption and secretion, therefore, the modified saliva under resting conditions contains:
Phases of salivary secretion
1. Cephalic phase refers to the secretion of saliva before entering of food into the mouth. It is caused by a conditioned reflex initiated by the mere sight or smell of food.
2. Buccal phase refers to the secretion of saliva caused by stimulation of buccal receptors by the presence of food in the mouth. It is an unconditioned reflex, partially regulated by the appetite area of the brain.
3. Oesophageal phase occurs due to the stimulation of salivary glands to a slight degree by the food passing through oesophagus.
4. Gastric phase refers to the secretion of saliva by the presence of food in the stomach. It specially occurs when irritant food is present in the stomach (e.g. increased salivation before vomiting).
5. Intestinal phase refers to a salivary secretion caused by the presence of irritant food in the upper intestine.
Control of salivary secretion
• Salivary secretion is controlled entirely by the autonomic nervous system (ANS) reflexes.
• Salivary secretion production is increased by both parasympathetic and sympathetic activity; however the activity of former is more important.
I Parasympathetic control
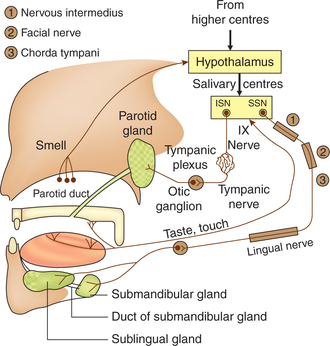
Parasympathetic nerve supply (Fig. 7.2-4)
Parotid glands are supplied by the parasympathetic fibres (preganglionic), which arise from the inferior salivary nucleus (dorsal nucleus of IXth nerve) of medulla.
• Preganglionic fibres run via tympanic nerve and small superficial petrosal nerve to otic ganglion.
• Postganglionic fibres from the otic ganglion join auriculotemporal nerve to reach parotid gland where fibres are supplied along with blood vessels of gland.
Submandibular and sublingual glands are supplied by the parasympathetic fibres originating from superior salivary nucleus (dorsal nucleus of VIIth nerve).
• Preganglionic fibres run in the nervous intermedius (sensory division of VIIth nerve), join the facial nerve and leave by its chorda tympani branch to join lingual nerve. They synapse in the ganglia present near the glands.
• Postganglionic fibres arising from the ganglia present near the glands are supplied to the glands along with the blood vessels.
Parasympathetic nerves are secretomotor to the salivary glands and control their secretion via following reflexes.
1. Conditioned reflexes. Sight, smell or even thought of palatable food increases the salivary secretion by the conditioned reflexes. In conditioned reflexes, the parasympathetics supplying the salivary glands are stimulated by impulses coming from higher centres of brain.
2. Unconditioned reflexes are initiated by the stimulation of receptors in the buccal cavity. Receptors and afferents, and efferents of unconditioned reflexes are discussed below.
• Mechanoreceptors which are excited by tactile stimulation from the tongue, mouth and pharynx.
• Afferent path of tactile stimulation reflexes run in trigeminal nerve branches (such as lingual, buccal and palatine nerves), pharyngeal branches of vagus and glossopharyngeal nerve.
• Chemoreceptors, i.e. tastebuds are stimulated by the sensation of taste and chemicals in the food. Afferents for taste sensation from:
– Posterior one-third of tongue pass via glossopharyngeal nerve to end in inferior salivary nucleus (dorsal nucleus of IXth nerve), and
– Anterior two-third of tongue pass via nervous intermedius (branch of VIIth nerve) to end in superior salivary nucleus (dorsal nucleus of VIIth nerve).
• Salivary centre is thus constituted by superior and inferior salivary nuclei.
• Efferents from superior salivary nucleus stimulate the submandibular and sublingual salivary glands, while those from the inferior salivary nucleus stimulate the parotid glands.
Effects of parasympathetic stimulation
Parasympathetic nerve stimulation causes the salivary gland cells to secrete a large volume of watery fluid that is high in electrolytes but low in proteins.
Stimulation of parasympathetic nerves liberate a proteolytic enzyme kallikrein from the gland cells, which acts on α2-globulin in interstitial fluid to form bradykinin. It also causes local release of VIP (vasoactive intestinal peptide). These increase the saliva production by causing vasodilatation of blood vessels of salivary gland.
II Sympathetic control
• Preganglionic fibres originate from the lateral horn cells of T1 and T2 segments of spinal cord and enter paravertebral sympathetic chain via ventral roots to synapse with the cells in superior cervical ganglion.
• Postganglionic fibres run along the carotid artery branches and are supplied to the three pairs of salivary glands along with their blood supply.
Functions of saliva
1 Protective function
• Dilutes hot and irritant food substances, thus preventing injury to buccal mucosa.
• Washes away food particles that remain in the oral cavity at the end of meal and thus cleans the oral cavity, i.e. helps in maintaining oral hygiene. In this way, growth of several harmful bacteria in the oral cavity is prevented.
• Destroys harmful bacteria in the mouth and thus minimizes the risk of buccal infection and dental caries because of its following constituents:
– Lysozymes, which have bactericidal action;
– IgA, which provides immunological defence against bacteria and viruses; and
– Lactoferrin, which has bacteriostatic action, i.e. prevents multiplication of bacteria.
• Dilutes any hydrochloric acid (HCl) and bile, which regurgitate into oesophagus and mouth.
4 Role in taste sensation
Saliva acts as a solvent for various foodstuffs. As taste is a chemical sense, the taste receptors respond only to the dissolved substances.
5 Role in speech
Salivary mucus lubricates the oral mucosa and thus aids speech by the facilitating movements of lips and tongue.
Deglutition (swallowing)
Phases of swallowing
Deglutition or swallowing refers to the passage of food from the oral cavity into the stomach. It comprises three phases:
Oral phase
• Oral phase or the first stage of swallowing is a voluntary phase.
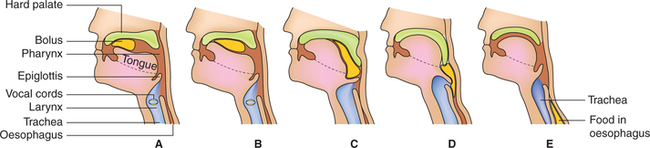
• During this phase the bolus of food formed after mastication is put over the dorsum of tongue. The tongue forces the bolus into the oropharynx by pushing up and back against the hard palate (Fig. 7.2-5A).
Pharyngeal phase
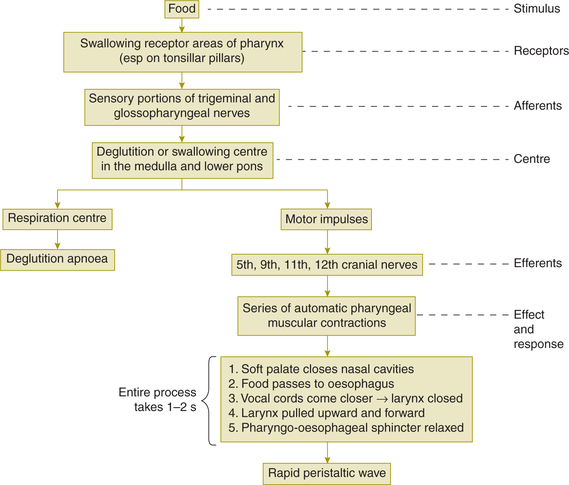
Pharyngeal phase or second stage of swallowing is an involuntary phase caused by a swallowing reflex.
Deglutition centre co-ordinating the reflex activity is located in the medulla oblongata and lower pons, i.e. in the nucleus of the tractus solitarius (NTS) and the nucleus ambigus (Fig. 7.2-6).
Events during pharyngeal phase
Events which take place during movement of bolus from the pharynx into the oesophagus occur in following sequence (Fig. 7.2-5B, (C and D):
• Oral cavity is shut off from the pharynx by the approximation of posterior pillars of the fauces.
• Nasopharynx is closed by the upward movement of soft palate, preventing regurgitation of food into the nasal cavities.
• Palatopharyngeal folds are pulled medially to make a slitlike opening for food, allowing only properly masticated food to pass through (selective action).
• Vocal cords strongly approximate stopping the breathing temporarily (deglutition apnoea). Larynx is pulled upward and anteriorly by neck muscles enlarging the opening of oesophagus, which is normally a slit and epiglottis swings backwards to close laryngeal opening. All this guides the food towards the oesophagus and prevent its entry into the trachea.
• Upper oesophageal sphincter (UES) which normally remains contracted tonically opens up and allows the bolus of food to be pushed into the upper part of oesophagus by the rapid peristaltic contraction wave of pharynx, which also continues in the oesophagus.
• Once the bolus of food has passed into the oesophagus, cricopharyngeus contracts, vocal cords open up allowing normal breathing to be resumed and the UES once again goes into tonic contraction.
The entire process of pharyngeal phase is completed in 1–2 s.
Oesophageal phase
During oesophageal phase, the food bolus is propelled from the upper part of oesophagus to the stomach by the oesophageal peristalsis and aided by gravity. Before describing the features of oesophageal peristalsis, it will be worthwhile to discuss briefly the applied anatomy of oesophagus.
Applied anatomy of oesophagus
Oesophagus is a fibromuscular tube about 25-cm long. It is separated from the pharynx by the UES and from the stomach by the lower oesophageal sphincter (LES).
Upper oesophageal sphincter. UES is a true sphincter that is normally contracted tonically, and serves to prevent the entry of air into the oesophagus during normal respiration. Its tone is maintained by the continual firing of vagal fibres.
The UES opens during swallowing when a rapid peristaltic wave starting in the pharyngeal muscles passes on to oesophagus.
Lower oesophageal sphincter. LES also known as cardiac sphincter refers to distal 2 cm of oesophagus. Its contractile characteristics are quite different from the rest of oesophageal smooth muscle (that is why it is called physiological sphincter).
The principal function of LES is to prevent regurgitation of gastric contents (food, gastric juice and air) into the oesophagus. The local hormone, gastrin, increases the tone of LES and helps to keep the sphincter more tightly closed during digestion.
Oesophageal peristalsis
• The oesophageal phase of deglutition (Fig. 7.2-5E) is completed by two types of oesophageal peristalsis, primary and secondary.
Primary oesophageal peristalsis
• Primary oesophageal peristalsis is initiated by swallowing. As soon as the food bolus enters the oesophagus from pharynx, the UES contracts to prevent regurgitation of food into the mouth and primary oesophageal peristalsis begins, which propels the food downwards.
• The LES (which normally remains tonically contracted) relaxes as the peristaltic wave approaches the sphincter and allows the bolus of food to enter the stomach without causing any resistance.
Secondary oesophageal peristalsis
• When the primary oesophageal peristalsis is not able to push a bolus of solid food all the way down the oesophagus, the food remaining in the oesophagus stretches mechanical receptors and initiates another peristaltic wave called the secondary oesophageal peristalsis.
• Secondary oesophageal peristalsis is co-ordinated by the intrinsic nervous system of the oesophagus.
Note. After the food enters the stomach, the LES contracts to prevent regurgitation of food into the oesophagus. With this the oesophageal phase of deglutition is completed.
Disorders of swallowing
1 Abolition of deglutition reflex
Abolition of deglutition reflex causes regurgitation of food into the nose or aspiration into the larynx and trachea. It may occur:
2 Aerophagia
• Aerophagia refers to the unavoidable swallowing of air along with the swallowing of food bolus and liquids.
• It usually occurs in nervous individuals having low tone of the UES.
• Some of the gases present in the air swallowed are absorbed, partly the air is regurgitated into the oral cavity and out in the atmosphere (belching) and majority of it passes on the colon and is then expelled as flatus through the anus.
4 Cardiac achalasia
Cardiac achalasia is a neuromuscular disorder of the lower two-thirds of oesophagus, characterized by absence of oesophageal peristalsis and failure of the LES to relax during swallowing.
5 Gastroesophageal reflux disease
Gastroesophageal reflux disease refers to a condition in which incompetence of the LES causes reflux of acidic gastric contents into the oesophagus. Reflux of stomach acid causes oesophageal pain (heartburn) and may lead to irritation of oesophagus or bronchioles (due to aspiration).
 Salivary glands
Salivary glands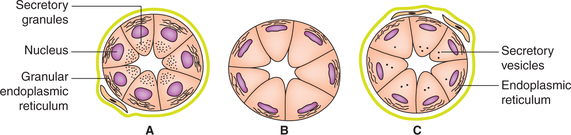
 Important note
Important note