Physiology of Pregnancy and Parturition
Physiology of pregnancy
Physiology of pregnancy is mainly concerned with maternal adaptations to provide ideal atmosphere for fertilization, nutrition to the growing fetus and safe child birth. The physiology of pregnancy can be discussed under following headings:
• Fertilization and implantation,
• Formation of placenta and its functions,
Fertilization and implantation
Fertilization
Fertilization refers to the fusion of male and female gametes (i.e. spermatozoon and ovum). It takes place in the middle segment (ampulla) of the fallopian tube. It involves following events:
1 Transport of gametes
Before fertilization, the ovum and sperms reach the ampulla for fertilization.
Transport of ovum. At the time of ovulation the ovum is directly expelled into the peritoneal cavity and then enters into the fallopian tube. The contractions of smooth muscle fibres present in the wall of fallopian tube also help in transport of the ovum.
Transport of sperms in the female genital tract. After ejaculation, several million sperms (average–200 million sperms per ejaculation) get deposited in the vagina. After ejaculation, normal sperm shows flagellar movements in the fluid medium at a rate of 1–4 mm/min. Therefore, in 30–60 min, they are able to reach the fallopian tube.
2 Sperm capacitation
Sperm capacitation refers to the process that makes a sperm to fertilize an ovum. Immediately after ejaculation in female genital tract the sperm undergoes certain changes, which enable it to fertilize an ovum. It takes about 1–10 h (capacitation period).
3 Fusion of gametes
The fusion of ovum and sperm involves the following steps (Fig. 9.4-1):
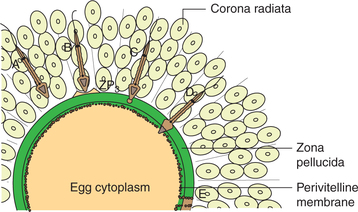
Fig. 9.4-1 Sequential events of fertilization of an ovum by the sperm: A, penetration of corona radiata; B, binding of sperm to zona pellucida; C, acrosomal reaction; D, fusion of sperm with oocyte and E, discharge of cortical granules into the perivitelline space producing vitelline block to polyspermy.
Chemoattraction. Chemoattraction of the sperms to ovum occurs by substances produced by the ovum.
Penetration of sperm through ovum coverings. It is made possible by the release of enzyme hyaluronidase and other proteolytic enzymes present on the acrosome of the sperm. The binding of sperm to zona pellucida glycoprotein (ZP3) triggers acrosomal reaction.
Acrosomal reaction (Fig. 9.4-1C). It involves release of acrosin (protease enzyme) from anterior membrane of acrosome of the sperm.
Only one sperm can enter into the oocyte, and further entry of sperms is prevented by the activation of ovum.
Implantation
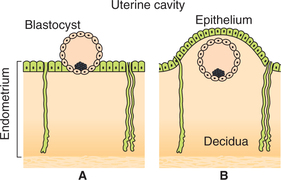
Implantation of a fertilized ovum involves following steps.
1. Formation of blastocyst. The fertilized ovum starts dividing immediately and is called morula (16-cell stage) and blastocyst (100-cell stage).
2. Transportation of blastocyst in uterine cavity. In next 3–4 days, blastocyst is transported into the cavity of the uterus.
3. Implantation of blastocyst in the endometrium. The blastocyst then erodes and burrows into the endometrium (Fig. 9.4-2).
The blastocyst goes deeper and deeper into the uterine mucosa till whole of it lies within the endometrium.
4. Decidual reaction. After implantation, the endometrium is called decidua. The stroma cells of the endometrium get enlarged, become vacuolated and get filled with glycogen and lipids. These cells are called decidual cells. The stored glycogen and lipids are the source of nutrition for the embryo till placenta takes up this function. Therefore, this change in stroma cell is called decidual reaction.
Placenta and pregnancy tests
Placenta
Placenta is a temporary organ formed during pregnancy. It is an important link between the mother and the fetus.
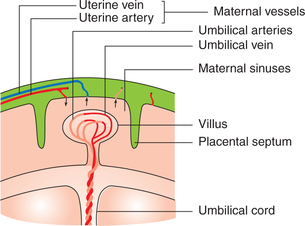
• When fully formed, the placenta (Fig. 9.4-3) is a discshaped structure, has a diameter of 15–20 cm and weighs about 500 gm.
• After birth of the baby, the placenta is shed off along with the decidua.
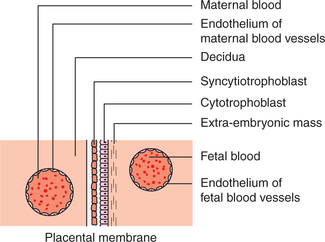
The placental membrane
The maternal and the fetal blood do not mix with each other. They are separated by a placental membrane and made up of the layers of the wall of the villus. From the fetal side, these are (Fig. 9.4-4):
• Endothelium of fetal blood vessels and its basement membrane,
• Surrounding mesenchymal tissue (connective tissue),
The total area of the membrane varies from 4 to 14 m2. Its thickness is 0.025 mm in the beginning and it is reduced to 0.002 mm in the later part of pregnancy.
Functions of placenta
The fully functional placenta develops by the end of third month (12 weeks) of pregnancy. Placenta serves mainly three functions:
• Hormone secretion (endocrinal functions of placenta),
The syncytiotrophoblast of the placenta serves as an endocrine gland. The hormones secreted by the placenta are:
• Human chorionic gonadotropins (HCG),
• Human chorionic somatomammotropins (HCS),
1. Human chorionic gonadotropins. Human chorionic gonadotropin is a polypeptide (largest active peptide). It is secreted by syncytiotrophoblast; soon after fertilization it is detected in the maternal blood as early as 6–8 days after conception, and reaches its peak between 60 and 90 days of gestation. After this the concentration falls to a very low level, and just before labour its level falls to zero (Fig. 9.4-5A). Its approximate peak value in human maternal blood during normal pregnancy is 5 mg/mL.
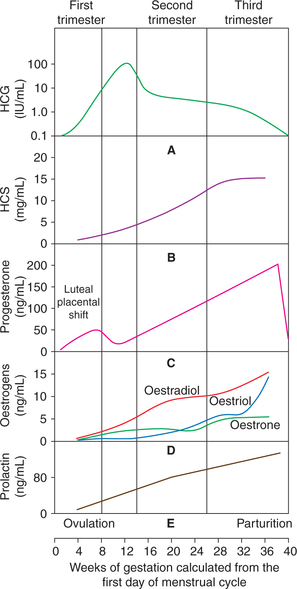
Fig. 9.4-5 Profile of plasma concentration of hormones during normal pregnancy: A, human chorionic gonadotropin (HCG); B, human chorionic somatomammotropin (HCS); C, progesterone; D, oestrogens and E, prolactin.
Physiological effects of HCG are:
• HCG is a luteotropic hormone. Its actions are similar to LH of anterior pituitary, hence are also called second luteotropic hormone. It maintains the functions of the corpus luteum up to 7 weeks after conception until fetoplacental unit is able to synthesize its own oestrogen and progesterone.
• HCG stimulates fetal testes in male fetus to secrete testosterone prior to fetal pituitary LH secretion. This testosterone and Mullerian regression factor secreted by the fetal testes is responsible for development of male genital organs and descent of testes during intrauterine life.
2. Human chorionic somatomammotropin. The syncytiotrophoblast cells of placenta also secrete a large amount of HCS. HCS is protein in nature and structurally resembles to growth hormone.
Plasma concentration. The secretion of HCS begins at fifth week of pregnancy. It increases gradually throughout pregnancy. Its peak reaches at term and peak value is 15 μg/mL (Fig. 9.4-5B).
It functions as maternal growth hormone of pregnancy, causes deposition of protein in the tissues and brings about nitrogen, calcium and potassium retention.
3. Human chorionic thyrotropin. Human chorionic thyrotropin (HCT) secreted by the placenta has properties quite similar to that of thyroid stimulating hormone (TSH). The physiological role of this substance is not very clear.
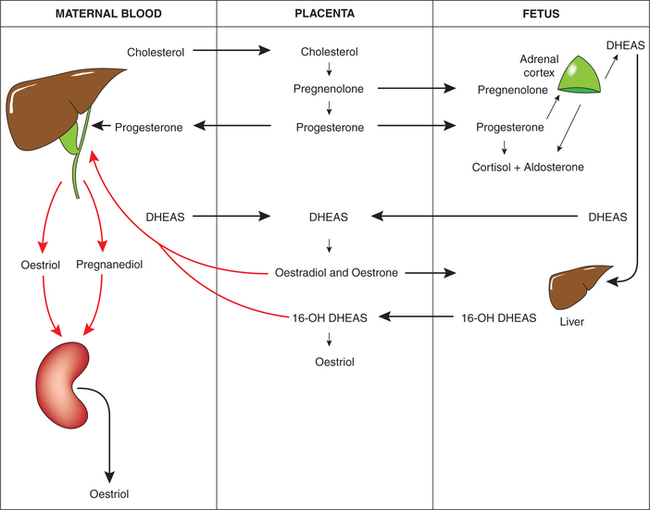
4. Placental progesterone. Progesterone is C-21 steroid hormone.
Synthesis. During early pregnancy, it is synthesized by corpus luteum of pregnancy and then by syncytiotrophoblasts of placenta (85% of total contribution).
• Placental syncytiotrophoblasts do not synthesize cholesterol. Therefore, cholesterol is mainly derived from maternal circulation and very little is contributed by the fetus.
• The fetus, placenta and mother—though they are independent, but constitute a functional unit called fetoplacental maternal unit (Fig. 9.4-6).
Plasma concentration. During pregnancy plasma concentration of progesterone rises steadily throughout gestation (Fig. 9.4-5C) reaching a maximum plateau at 30–40 weeks of gestation, and its level does not fall to zero like other placental hormones. Just before the onset of labour its level decreases.
Physiological effects of placental progesterone are:
(i) It helps to preserve the pregnancy by promoting the growth of endometrium. It converts secretory endometrium of luteal phase of menstrual cycle to decidual during pregnancy.
(ii) Progesterone has a marked inhibitory effect on the contractions of uterus.
(iii) It causes development of alveolar system of mother's breast. Its synergic action with oestrogen prepares the breast for lactation after the birth of the baby.
5. Placental oestrogens. Placental oestrogens are C-21 steroid hormones; quantitatively oestriol is the major oestrogen of pregnancy with smaller amount of oestradiol and oestrone.
Plasma concentration. Like progesterone, plasma oestrogen (oestriol) concentration rises throughout the gestation. Its peak value (14 ng/mL) and secretory curve parallels as that of the progesterone, and maximum plateau is reached at 30–40 weeks of gestation.
The plasma concentration of oestriol reflects the functional status of fetoplacental maternal unit activity.
B Transport of substances between the mother and the fetus
1. Transport of nutrients. The major function of placenta is to provide foodstuffs from mother's blood into the fetus.
By the fourth week of pregnancy, the placenta takes up the nutritive functions. The nutritive materials which are transported from mother's blood into the fetus are:
• Calcium and inorganic phosphates.
• Potassium, sodium and chloride ions, and substances with molecular weight less than 1000 can cross readily by simple diffusion.
2. Excretion of waste products through placenta. Excre tory products, especially urea, uric acid and creatinines, etc. formed in the fetus are transported into the mother's blood and then excreted by mother's kidneys. Thus placenta also acts as a fetal kidney.
3. Diffusion of respiratory gases
(i) Oxygen transport. Dissolved oxygen from the maternal sinuses of placenta diffuses into the fetal blood along the pressure gradient (mean pO2 in mother's blood is 50 mm Hg, whereas in fetal blood mean pO2 is 30 mm Hg).
(ii) Transport of CO2. Transport of CO2 from fetus occurs by diffusion along the pressure gradient. The pCO2 of fetal blood is 2–3 mm Hg higher than that of the maternal blood (as CO2 is continuously being formed in the fetus and eliminated only through placenta). Thus placenta acts as fetal lungs.
4. Transport of antibodies. Maternal immunoglobulins are transferred into the fetus and are responsible for innate immunity.
Rh agglutinins are easily transported as compared to ABO agglutinins, that is why the effects of Rh incompatibility are more severe.
5. Transport of harmful substances. Certain viruses and many drugs (like nicotine and barbiturates) can easily cross the placental barrier and may produce harmful effect on the fetus. Therefore, as far as possible one should avoid these drugs and smoking during pregnancy.
Pregnancy tests
In an adult healthy woman, amenorrhoea is the first sign of pregnancy, but it occurs in many other conditions as well. Therefore, detection of early pregnancy is made possible by certain pregnancy tests. The pregnancy detection tests are based on presence of HCG in the urine of pregnant lady.
Gravindex test
Immunological pregnancy tests are based on the antigenic properties of HCG.
The kit for this test consists of:
• Gravindex antigen (latex particles coated with HCG), Gravindex antibodies (serum containing antibodies against HCG) and a dark coloured slide.
Procedure. This test is performed on the control and test samples of urine.
Control sample. A drop of urine sample from non-pregnant subject (containing no HCG) is mixed with a drop of antiserum containing HCG antibodies. Then it is mixed with HCG coated latex particles. There will be agglutination because urine of non-pregnant subject does not contain antigen; therefore, antibodies are not neutralized. Thus occurrence of agglutination indicates no pregnancy or pregnancy test is negative.
Test sample. A drop of urine of suspected pregnant lady (containing HCG) is mixed with a drop of anti-serum (containing HCG antibodies). Then it is mixed with HCGcoated latex particles. There will be no agglutination because antibodies have been neutralised by the HCG present in the urine. Therefore, occurrence of no agglutination means positive pregnancy test.
Physiological changes in mother during pregnancy
The normal average duration of pregnancy in human beings is 280 days (40 weeks) and is calculated from the first day of the last menstrual period or 256–270 days from the time of ovulation. As the pregnancy progresses, various types of extra demands are imposed on the mother's body by the growing fetus, which are met with by certain adaptations in almost all the organ systems of the body. These physiological changes include.
I Changes in genital organs
1. Uterus. To accommodate the growing fetus marked increase in the size of uterus takes place. The enlargement is mainly due to hypertrophy and to some extent hyperplasia of the myometrial smooth muscle fibres.
2. Ovaries. The follicular changes and ovulation do not occur because FSH and LH of anterior pituitary are inhibited.
3. Cervix. Endocervix gets hypertrophied, the cervical glands increase in number and their secretions form a plug that closes the cervical canal, and the tough cervix becomes soft.
4. Mammary glands. Under the influence of various hormones breast enlarges in early pregnancy. Hyperplasia of ductal and alveolar tissue occurs, the areola becomes pigmented and many sebaceous glands become prominent in the areola. Nipples also become larger and pigmented.
II Weight gain
A woman may gain total of 10–12 kg of weight during normal pregnancy, which is contributed by:
III Haematological changes
1. Blood volume. The total blood volume increases by 30%. The plasma volume increases relatively more than that of the red cell volume, which causes haemodilution; thus there is physiological anaemia of pregnancy.
2. The haematological indices show following changes:
3. Plasma proteins. The total concentration of plasma proteins decreases from 7.5 to 6 gm% due to haemodilution. The fibrinogen level increases, but serum albumin level markedly decreases.
4. Leucocytes. Total leucocyte count (TLC) increases and may reach up to 20,000/mm3.
5. Platelets. There occurs a slight decrease in the platelet count.
6. Coagulation factors. Pregnancy seems to be a hypercoagulable state due to an increase in following: fibrinogen, and factors VII, VIII, IX and X. The hypercoagulability of the blood plays a significant role of haemostasis at the time of separation of placenta during delivery.
IV Cardiovascular system changes
1. Position of heart. The gravid uterus pushes the diaphragm upwards resulting change in the position of heart.
2. Heart rate. Heart rate also increases by 10–12 beats/min.
3. Cardiac output. Cardiac output (CO) increases from 5 L/min to 7 L/min at 20 weeks of gestation.
4. Blood pressure may show following changes:
• Systolic blood pressure. In normal pregnancy, there is either no change in systolic pressure or some fall may occur.
• Diastolic pressure decreases and by 16–20 weeks of pregnancy its value is lowest. Then it starts rising and comes back to normal.
5. Blood flow. Blood flow to skin, uterus and kidneys increases to meet the demands.
6. Venous pressure. The gravid uterus exerts pressure on the pelvic veins, abdominal veins and femoral veins, thus increasing the venous pressure. The rise in femoral venous pressure results in oedema in feet (common occurrence).
V Respiratory system changes
1. Hyperventilation. High levels of plasma progesterone during pregnancy increase the sensitivity of respiratory neurons to CO2 resulting in hyperventilation.
2. Gas exchange. Gas exchange across the alveoli is greatly enhanced due to a marked increase in the pulmonary blood flow.
3. Oxygen consumption. Oxygen consumption of body increases by 15% to meet the demands of growing fetus and for the extra work of heart, uterus and other tissue.
VI Urinary system changes
Kidney functions show following changes.
1. Renal blood flow. There is a marked increase in renal blood flow due to increase in the cardiac output and vasodilatation.
2. Glomerular filtration rate (GFR) increases by 50% due to an increase in renal blood flow and solute load.
3. Renal tubular absorptive capacity for sodium and chloride ions also increases by 50% due to high level of steroid hormones secreted by the placenta and the adrenal cortex.
4. Glycosuria is a common physiological phenomenon during pregnancy.
5. Proteinuria occurs due to increase in excretion of proteins.
6. Water balance. During later months of pregnancy, excess of water is retained due to:
7. Acid–base balance. Hyperventilation during pregnancy results in respiratory alkalosis. Kidneys, therefore, compensate for it by excreting more  ions in the urine.
ions in the urine.
VII Gastrointestinal system changes
1. GIT secretions. Hypochlorhydria is very common due to decreased gastric secretion.
2. GIT motility decreases under the influence of hormones resulting in delayed gastric emptying.
3. Gall bladder functions. Gall bladder increases in size and empties its contents at a very slow rate.
4. Liver functions are also altered during pregnancy. The fibrinogen synthesis increases and albumin decreases; thus plasma A:G ratio is also altered.
5. Morning sickness. Anorexia, nausea and vomiting are very common in early pregnancy (first trimester) especially in the morning hours, hence is known as morning sickness. The cause for the morning sickness is not known.
VIII Metabolic changes
1. The basal metabolic rate (BMR) of the pregnant woman increases by about 15% during later half of the pregnancy.
2. Protein metabolism. When the diet is balanced and adequate then there is nitrogen retention and positive nitrogen balance. The proteins are deposited in the uterus, breast, fetus and placenta.
3. Carbohydrate metabolism shows following changes:
• Blood glucose level increases due to rapid absorption from the gut.
• Glycosuria is of common occurrence due to the increase in GFR and decrease in renal threshold for glucose.
4. Fat metabolism. About 3–4 kg of fat is deposited in the body during pregnancy. There occurs an increase in plasma concentration of cholesterol, phospholipids and triglycerides.
IX Endocrine system changes
Almost all the endocrine glands of the mother react substantially during pregnancy. Firstly, due to increased metabolic load on the mother and secondly in response to the hormones produced by the placenta and fetus.
X Changes in the skin
1. Hyperpigmentation occurs on the face (butterfly pattern known as chloasma), areola, nipple and midline of abdomen (linea alba) extending from pubic symphysis to xiphisternum. The hyperpigmentation is related to increased secretion of ACTH and MSH during pregnancy.
2. Stria gravidarum. These are linear scars present on the lower abdomen due to stretching of skin.
Physiology of parturition
Parturition is the process by which baby is born. It involves preparation for child birth, act of child birth and recovery from child birth. It is difficult to predict the exact date of onset of labour. It may occur any time between 37th and 40th weeks of gestation. The uterine myometrium and cervix play an important role for this process.
Mechanics of parturition
From the functional point of view, mechanics of parturition mainly involves:
Control of parturition
The mechanisms responsible for onset of labour in human are still not understood exactly. The control of parturition includes the role of:
A Hormonal factors
The hormonal changes that initiate the parturition and cause increased excitability of uterine musculature are given below.
1. Activation of fetal hypothalamic–pituitary–adrenal axis. Recently, it has been hypothesized that the initial signals for the onset of labour comes from the fetus only, and due to some unknown factors, corticotropin-releasing hormone (CRH) secretion in the fetus results in an increase in ACTH secretion few days before parturition. ACTH causes fetal adrenal cortex to secrete large amount of androgens.
The above changes lead to an altered oestrogen–progesterone ratio.
2. Role of altered oestrogen–progesterone ratio. The altered oestrogen–progesterone ratio also causes:
B Mechanical factors
Mechanical factors that increase the contractility of uterus include the following.
1. Stretch of uterine musculature usually increases its own contractility (myogenic theory). As the pregnancy advances with growing fetus, the stretch increases leading on to uterine contractility.
2. Positive feedback effect. Stretching and irritation of cervix is particularly important because this positive feedback effect leads to further reflex increase in uterine contractility.
The positive feedback mechanism continues until the baby is expelled.
3. Role of Ferguson reflex. Once labour is started, the uterine contractions dilate the ripened cervix. The cervical dilatation in turn sets of signals in afferent nerves that increase oxytocin secretion from the posterior pituitary. This is called Ferguson reflex.
 Fertilization and implantation
Fertilization and implantation Transportation of ovum
Transportation of ovum