6 Role of available bone in dental implants
Introduction
Available bone is a quantitative assessment of the bone suitable for implant placement, which is available at an edentulous site. Bone availability describes “the external architecture and volume of bone in the edentulous area considered for ideal implant placement.” It is measured three-dimensionally in buccolingual width, vertical height, mesiodistal dimension of edentulous space, bone angulation, and crown height space for the future prosthesis. If the bone available is inadequate for prosthetically ideal implant insertion, the implant surgeon can perform bone grafting procedures to regenerate lost bone dimensions.
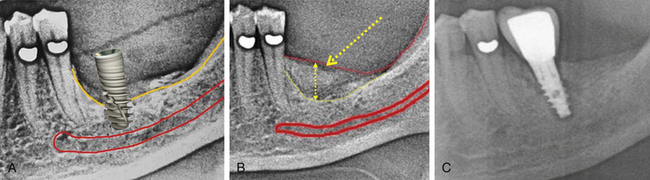
As described in previous chapters, implants are available in different diameters and lengths. The design of a root form implant may vary from one manufacturer to another. The crest module or implant platform of some implants may be wider than the body diameter. For example, the 3.3 mm diameter Adin implant has a 3.75 mm platform. The dentist should be aware that in most clinical situations, the ridge is found to be faciolingually thinnest at the crestal region, which may often make it difficult to place even the narrowest diameter implant without ridge modification. The bone at any edentulous site is considered to be adequate when the implant with adequate dimensions can be placed in such a way that it leaves minimum of 1.5–2 mm of three-dimensional bone all around the implant body and platform (facially, lingually, and apically from vital structures like the sinus floor, mandibular canal, etc.) (Fig 6.1A–D).
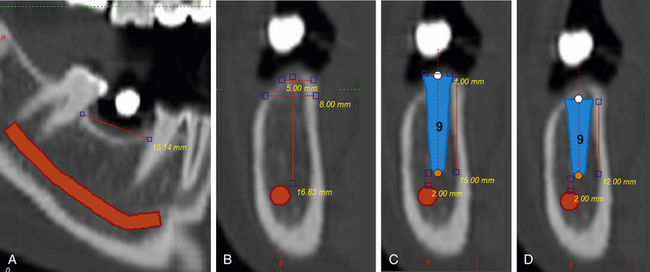
Fig 6.1 (A) Panoramic view of the edentulous mandibular molar site showing adequate bone length availability (15 mm) to place widest implant of any system (B) but the cross-sectional view of the same edentulous region shows inadequate bone availability at the ridge crest (5 mm), which cannot allow placement of even the narrowest implant of any system. The height of the bone above the mandibular canal is adequate (16.83 mm) to place an adequately long implant (14–15 mm long). (C) The implant with 4 mm x 15 mm dimensions can be placed with its platform at the crest level with simultaneous lateral bone augmentation to cover the facially exposed implant threads near the crest. (D) The shorter length (4 mm x 12 mm) implant is placed after 3 mm of osteoplasty, so that the implant platform can be placed at the level of wider subcrestal ridge.
Misch and Judy classification of bone availability
In 1985, Misch and Judy presented a classification of available bone for dental implant insertion, which is similar in both arches (Fig 6.2A–D). Bone modification procedures, grafting methods, and prosthodontic-related treatments were suggested for each category.
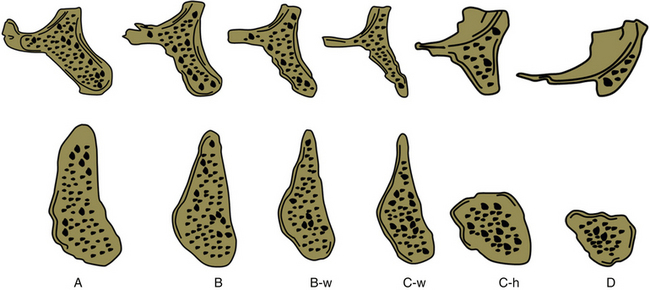
Fig 6.2 Misch and Judy classification of bone availability (Divisions A, B, C and D): Division A (abundant bone), Division B (barely sufficient bone), Division C (compromised bone), Division D (deficient bone), w (width), h (height).
Division A (abundant bone)
Division A bone is three-dimensionally abundant for the ideal implant insertion (Fig 6.3A and B). According to Misch, bone in this category should be:
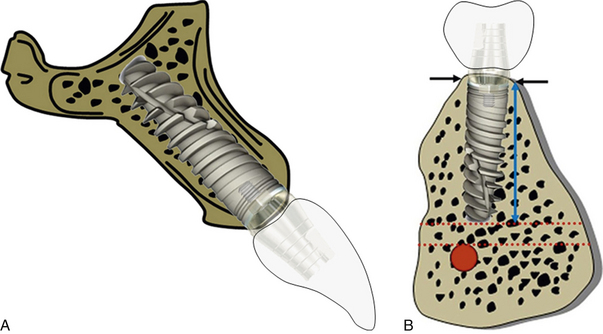
Fig 6.3 (A and B) Abundant bone in the maxilla and mandible suitable for inserting an implant with ideal dimensions.
Prosthetic options for Division A bone
a. is the best bone for any prosthetic option (Fig 6.4A–I).
b. may need osteoplasty for implant overdentures, to achieve more vertical height space and accommodate the implant suprastructures (ball/bar) under the denture.
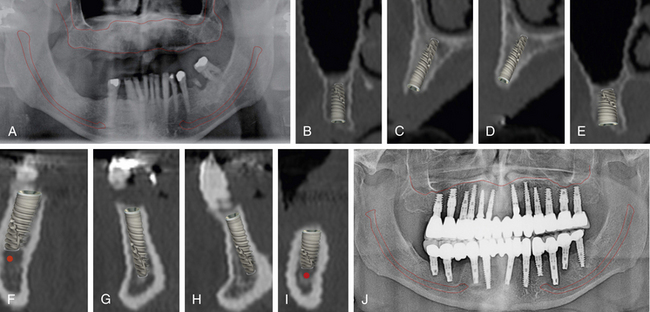
Fig 6.4 (A) Panoramic radiograph and (B–I) CT scan showing cross-sectional views of the maxilla and the mandible, showing the Division A bone (adequate bone) for implant placement without any ridge modification or grafting. (J) The implant-supported, full mouth fixed prosthesis can be seen in the radiograph.
Division B (barely adequate) bone
Bone in this category should be:
Prosthetic options for Division B bone
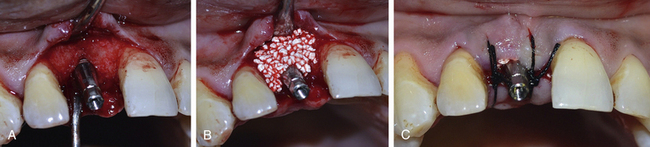
The bony ridge with Division B bone may be modified to division A bone by osteoplasty to achieve the wide ridge crest required to insert a regular diameter implant (Fig 6.5A–C). Lateral bone augmentation can also be performed before or with implant placement, especially in aesthetic areas where osteoplasty can elongate the clinical crown height (Fig 6.6A–C). This bone may be adequate for any prosthetic option in implant therapy.
Division C (compromised bone)
Bone in Division C category should be:
a. 0–2.5 mm in width (C-w bone)
b. Less than 12 mm in height (C-h bone)
Treatment options
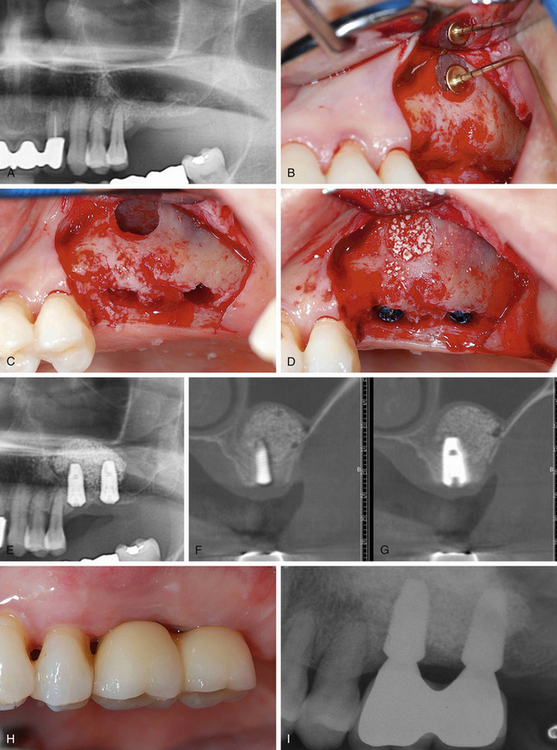
Osteoplasty can be done in C-w bone to achieve a wider platform to insert the implant, but the preferred option for the C-w bone is lateral bone augmentation before or at the time of implant insertion (Figs 6.7 and 6.8). Either short length root form implants or subperiosteal implants are used in C-h bone. Vertical bone augmentation (Fig 6.9A–C) or inferior alveolar nerve lateralization for posterior mandible and sinus elevation and grafting for posterior maxilla, may be the other options to achieve adequate ridge height for the insertion of long implants (Fig 6.10A–I).
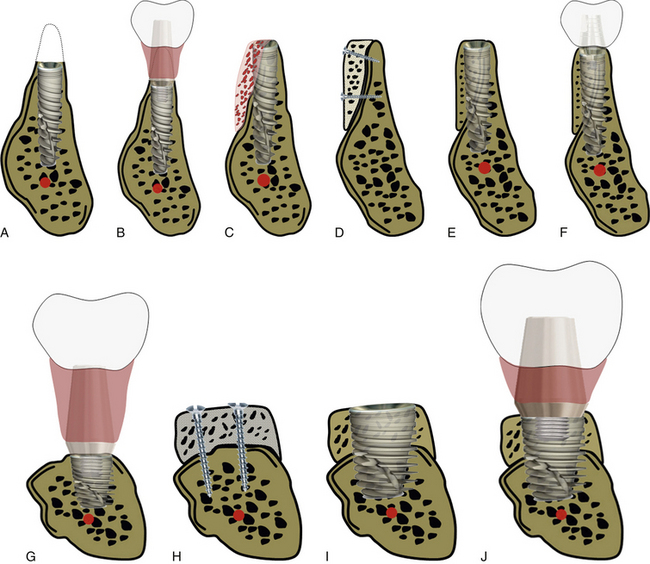
Fig 6.7 (A) Bony ridge in Division C-w bone category needs a large amount of vertical bone reduction to achieve an adequate ridge width for the placement of a narrow-to-regular diameter implant. (B) Osteoplasty not only increases the crown height but also results in increased thick, soft tissue height which may, over time, develop a deep soft tissue pocket that may harbour pathogens and lead to recurrent peri-implantitis. (C) The better option for the Division C-w bone is lateral bone augmentation either at the time of implant insertion or (D) before implant insertion (block grafting) to achieve the wide ridge crest for regular-diameter implant placement (E) for a prosthesis with an (F) ideal crown height. (G) For the Division C-h bone, either the short length implant is inserted or (H) vertical bone augmentation is performed to achieve adequate ridge height for the insertion of an (I) adequately long implant, which further reduces the crown: (J) implant height ratio.
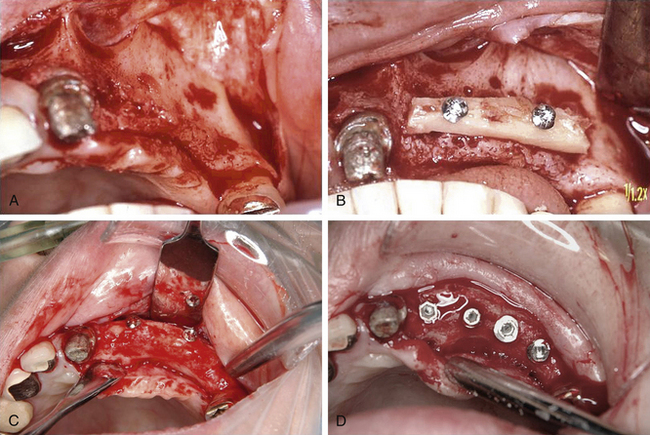
Fig 6.8 (A) Ridge with the C-w type of bone (compromised in width). (B) The lateral bone augmentation is performed using autogenous bone block. (C) Regeneration of new bone dimensions after the site is uncovered after 4 months. (D) Implants are inserted in the bone.
(Courtesy: Jun Shimada, Japan).
Division D bone (deficient bone)
This is the bone with severe atrophy, and it represents as basal bone loss, flat maxilla, and pencil-thin mandible, with more than 20 mm crown height.
Treatment options for the deficient ridge
Bone augmentation like vertical bone block grafting or nerve transpositioning, can be performed to insert adequately long implants in the mandible (Fig 6.11A and B). Vertical bone block grafting and/or sinus/nasal floor elevation and grafting is performed to insert implants in the maxilla, especially if a fixed, implant-supported prosthesis is planned.
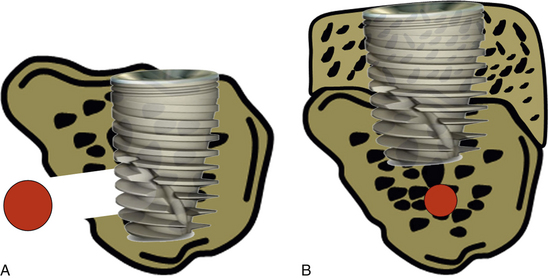
Fig 6.11 (A) With advancements in implant therapy, deficient (Division D) bone has been successfully used for implant placement with multiple approaches like nerve lateralization, sinus grafting, nasal floor grafting, etc. for implant placement; (B) but vertical bone augmentation not only facilitates the placement of adequately long implants but also reduces the long crown height.
Prosthetic options for Division D bone
Implant overdentures should be the treatment of choice for the deficient ridge (Fig 6.12A–D), because implant-supported, fixed prosthesis may need multiple invasive bone grafting procedures like sinus grafting, block grafting, nerve transpositioning, etc. (Fig 6.13A and B). Subperiosteal implants are preferred over endosseous root form implants to avoid problems, such as mandibular fracture in Division D ridge (Fig 6.14A–D).
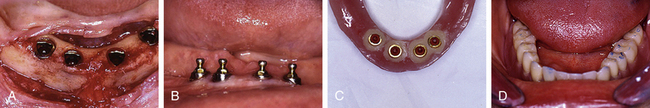
Fig 6.12 Deficient (Division D) mandibular bone with the only basal bone left. (A–D) Four short length implants are placed and an implant overdenture is delivered with ball abutment ‘O’ ring attachments
(Courtesy: Saad Zemmouri).
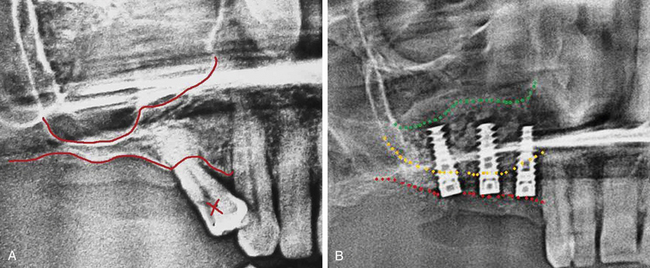
Fig 6.13 (A) Deficient (Division-D) bone in the posterior maxilla caused by vertical ridge resorption and maxillary sinus pneumatization, (B) The sinus elevation and grafting is performed for the insertion of adequately long implants.
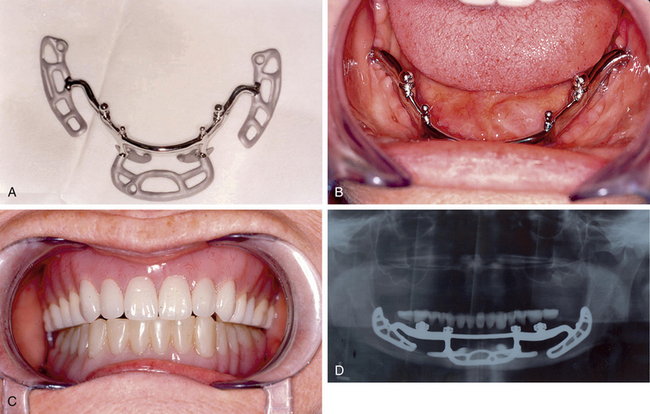
Fig 6.14 The subperiosteal implant can be preferred over the endosseous root form implant to avoid problems such as mandibular fracture in the Division D ridge. (A) Subperiosteal implant (B) placed on the deficient mandibular ridge (C) to support denture. (D) Post-loading radiograph
(Courtesy: Terry D Whitten, DDS).
Summary
In implant dentistry, the prosthesis is planned before implant insertion and the dimensions, positions, and angulations of implants are decided according to the requirements of the future prosthesis. Considering the various parameters like stress factors, cantilevers etc., and the bone available for the implant insertion plays a key role in the overall implant treatment success. Three-dimensional bone volumes, external architecture, and angulation in relation to the ideal implant axis, are the major factors which should be considered during treatment planning.
The edentulous jawbone available for implant placement has been divided in four types by Carl E Misch, to make it easy to assess patient requirements, plan implant placement, and choose the best prosthesis for long-term success. The Division A type ridge offers adequate bone for the ideal implant insertion to support a prosthesis, with appearance and function approximately similar to the natural tooth. The fixed implant prosthesis is usually preferred for the Division A ridge.
The Division B ridge may provide adequate bone width for narrow diameter implants, but additional implants should be inserted for the multiple unit or full-arch fixed prosthesis. The Division B ridge can be changed to the Division A ridge type with either vertical osteoplasty or lateral bone augmentation to make it adequate in width for regular diameter implant placement. The lateral bone augmentation should be preferred over osteoplasty in the anterior maxilla to deliver aesthetic results. Osteoplasty can be preferred in the anterior mandible as adequate bone height is available to insert long implants and there is not much aesthetic concern. The Division B posterior mandible also usually shows adequate bone height and high density to stabilize short length implants, and thus, osteoplasty can be done in the posterior mandible with Division B ridge. Because of poor bone density and higher stress factors, bone augmentation is preferred over osteoplasty in the posterior maxilla.
Regardless of the location, the Division C-w ridge (ridge compromised in width) should be managed with lateral bone augmentation. While short length implants can be inserted into the Division C-h ridge (ridge compromised in height), vertical bone augmentation is performed to place implants with adequate length.
Deficient bone (Division D) in the mandible can be used to insert multiple short length implants to retain the overdenture, but vertical bone augmentation is required in the deficient maxilla.
Gruber H., Solar P., Ulm C. Maxillomandibular anatomy and pattern of resorption during atrophy. In: Watzek G., ed. Endosseous implants: scientific and clinical aspects. Chicago: Quintessence, 1996.
Tatum H.O. Maxillary and sinus implant reconstructions. Dent Clin North Am. 1980;30:207–229.
Mason M.E., Triplett R.G., Van Sickels J.E., et al. Mandibular fractures through endosseous cylinder implants: report of cases and review. J Oral Maxillofac Surg. 1990;48:311–317.
Misch C.E. Short dental implants: a literature review and rationale for use. Dent Today. 2005;24:64–68.
Jemt T., Lekholm U. Implant treatment in edentulous maxillae: a 5-year follow-up report on patients with different degrees of jaw resorption. Int J Oral Maxillofac Implants. 1995;10:303–311.
Curtis T.A., Ware W.H., Beirne O.R., et al. Autogenous bone grafts for atrophic edentulous mandibles: a final report. J Prosthet Dent. 1987;57:73–78.
Misch C.E., Wang H.L. The procedures, limitations and indications for small diameter implants and a case report. Oral Health. August 2004;94:16–26.
Misch C.M. Ridge augmentation using mandibular ramus bone graft for the placement of dental implants: presentation of a technique. Pract Perio Aesth Dent. 1996:127–135.
Scortecci G.M. Immediate function of cortically anchored disk design implants without bone augmentation in moderately to severely resorbed completely edentulous maxillae. J Oral Implant. 1999;25:70–79.
Judy K.W., Misch C.E. Evolution of the mandibular subperiosteal implant. N Y Dent J. 1983;53:9–11.
Razavi R., Zena R.V., Khan Z., et al. Anatomic site evaluation of edentulous maxillae for dental implant placement. J Prosthet Dent. 1995;4:90–94.
Lam R.V. Contour changes of the alveolar process following extraction. J Prosthet Dent. 1960;10:25–32.
Tallgren A. The continuing reduction of the residual alveolar ridges in complete denture wearers. A mixed longitudinal study covering 25 years. J Prosthet Dent. 1972;27:120–132.
Misch C.E. Divisions of available bone in implant dentistry. Int J Oral Implants. 1990;7:9–17.
Misch C.E., Judy K.W.M. Classification of partially edentulous arches for implant dentistry. Int J Oral Implants. 1987;4:7–12.
Misch C.E. Classification and treatment options of the completely edentulous arches in implant dentistry. Dent Today. October 1990:26–30.
Weiss C.M., Judy K.W.M. Severe mandibular atrophy: biological considerations of routine treatments with complete subperiosteal implants. Int J Oral Implants. 1974;4:431–469.
Misch C.E. Available bone influences prosthodontic treatment. Dent Today. February 1988:44–75.
Karagaclioglu L., Ozkan P. Changes in mandibular ridge height in relation to aging and length of edentulism period. Int J Prosthodont. 1994;7:368–371.
Misch C.E. Bone classification, training keys to implant success. Dent Today. May 1989:39–44.