Chapter 20
Surface and Sectional Anatomy
Charles M. Washington
• Relate the importance and use of imaging modalities in radiation therapy.
• Compare and contrast aspects of anatomic positioning, anatomy features, and organ/tissue location used by the radiation oncology team for treatment planning and delivery.
• Understand the components and function of the lymphatic system and its role in treatment field design.
• Correlate superficial anatomic landmarks and cross-sectional perspectives to deeply seated internal anatomy.
Key Terms
Afferent lymphatic vessels
Anatomic position
Axillary lymphatic pathway
Body cavities
Body habitus
Compensatory vertebral curves
Efferent lymphatic vessels
Immunity
Internal mammary lymphatic pathway
Lymphatic system
Paranasal sinuses
Primary vertebral curves
Right lymphatic duct
Secondary vertebral curves
Spondylolisthesis
Suprasternal notch
Thoracic duct
Transpectoral lymphatic pathway
Radiation therapy practice requires that all team members have keen knowledge of human anatomy and physiology. Radiation therapists learn early in their education that they must have a comprehensive understanding of surface and cross-sectional anatomy. Knowledge of human anatomy is essential in simulation, treatment planning, and accurate daily treatment delivery. This chapter focuses on the surface and sectional anatomy used in simulation and treatment delivery performed by the radiation therapist. Surface anatomy is related to deep-seated structures within the human body. An overview of the diagnostic tools used to visualize internal structures is presented, along with a review of lymphatic physiology. This review is included because the lymphatics play a major role in treatment field design and disease management. A brief review of skeletal anatomy is presented to ensure a common basis for understanding important spatial relationships. Surface and sectional, as well as topographic, landmarks are presented in practical radiation therapy applications.
Perspective
The primary objective in management of cancer with radiation therapy is to deposit enough dose to a targeted area to result in cancer cell death while minimizing the effect on the surrounding healthy tissues. The challenge is to define a patient-specific therapy plan that localizes the tumor and surrounding dose-limiting tissues, such as the spinal cord, kidney, and eyes. In addition, the radiation therapist must maintain the integrity of the plan throughout its administration. Surface anatomy has changed very little in the past 50 years. Clinical application is essential in the understanding of a disease process on anatomic grounds, corresponding surface location of internal structures, and the appearance of internal imaged structures.
Visual, palpable, and imaged anatomy forms the basis of clinical examination in radiation therapy.1 Surface and sectional anatomy provides the foundation that the radiation therapist needs to be effective in simulation, treatment planning, and the daily administration of therapy treatments. Working without this foundation is like traveling from California to Maine for the first time without any planning: we know the general direction of where we want to go, but we do not know the most efficient way to get there. Sectional anatomy emphasizes the physical relationship between internal structures.2 The radiation therapist must have a complete understanding of imaging modalities that enable tumor visualization, identification of pertinent lymphatic anatomy, and the site-by-site relationship of surface and sectional anatomy. A systematic approach to this information allows the radiation therapist to link vital classroom information to its clinical application.
Related Imaging Modalities Used in Simulation and Tumor Localization
More than any other innovation, the ability to painlessly visualize the interior of the living human body has governed the practice of medicine during the twentieth century.3 In recent years, advancements in medical imaging techniques have allowed for effective ways to diagnose and localize pathologic disorders. The increased ability to image and localize the area of interest allows the treatment team to better target more exact treatment areas. Coupled with advanced immobilization, we can increase the dose delivered to the target while limiting dose to neighboring areas. The medical imaging modalities used in simulation and tumor localization fit into two categories: ionizing and nonionizing imaging studies. Ionizing imaging studies use ionizing radiation to produce images that primarily show anatomy. Examples of ionizing imaging studies include conventional radiography, computed tomography (CT), and nuclear medicine imaging, particularly positron emission tomography (PET) and the fusion of PET and CT. Nonionizing imaging studies use alternative means of imaging the body, such as magnetic fields in magnetic resonance imaging (MRI) and echoed sound waves in ultrasound scanning.
Conventional Radiography
A radiograph provides a two-dimensional image of the interior of the body. Computerized radiography (CR) and digital radiography (DR) can also be used to visualize internal anatomy without exposing a physical film. In either case, photostimulable plates or detectors capture the latent images for visualization on computer screens. The latent images produced show the differences in tissue densities of the body; however, x-rays do not always distinguish subtle differences in tissue density. Figure 20-1 shows a conventional chest radiograph produced with a radiation therapy simulator. The pertinent anatomy can be distinguished and outlined for practical application. Any anomaly, a variation from the standard, is recognizable on the image, as is any structure considered to be dose limiting.

Figure 20-1 Typical thorax conventional simulation film. Note how bony anatomy is distinguishable from cartilage and soft tissue.
Radiation therapy uses a considerable amount of diagnostic imaging tools in its daily practice. Fluoroscopic simulators use specialized diagnostic x-ray equipment to localize the treatment area and reproduce the geometry of the therapeutic beam before treatment. Radiographic localization, once the most commonly used method to localize tumor volumes, is still a viable way to capture treatment planning information.
Computed Tomography
In modern radiation therapy treatment planning and delivery, the use of CT imaging is the most common means of data capture. The translation of three-dimensional information is essential to the complex treatment delivery systems used today, such as intensity-modulated radiation therapy (IMRT), stereotactic radiosurgery (SRS), and all image-guided radiation therapies (IGRTs).
Computed tomography is an ionizing radiation–based technique in which x-rays interact with a scintillation crystal that is more sensitive than x-ray film.4 CT scanning combines x-ray principles and advanced computer technologies. The x-ray source moves in an arc around the body part being scanned and continually sends out beams of radiation. As the beams pass through the body, the tissues absorb small amounts of radiation, depending on their densities. The beams are converted to signals that are projected onto a computer screen. These images look like radiographs of slices through the body. They are typically perpendicular to the long axis of the patient’s body. The CT scan provides important anatomic and spatial relationships at a glance. A series of scans allows the examination of section after section of a patient’s anatomy.
The entire CT process takes only seconds for each slice and is completely painless. The detail of the images produced is approximately 10 to 20 times the detail of conventional radiography. Display of CT images reflects the differences among four basic densities: air (black), fat (dark/gray), water/blood (gray/light), and bone/metal (white).4 CT shows bone detail well. Radiation therapy treatment planning commonly uses CT images, particularly all conformal treatment plans and virtual simulation techniques.
Nuclear Medicine Imaging
The branch of medicine that uses radioisotopes in the diagnosis and treatment of disease is known as nuclear medicine. Nuclear medicine imaging uses ionizing radiation to provide information about physiology (function) and anatomic structure. This information is typically useful in noted abnormalities from tumor activity, specifically metastatic disease.5 Sensitive radiation detection devices display images of radioactive drugs taken through the body and their uptake in tissues. Although this imaging technique plays an important role in tumor imaging, it detects disease dissemination more than primary tumors. Bone and liver metastases are localized with nuclear medicine scans. These scans are relatively safe and can provide valuable information. The radionuclide bone scan is the procedure of choice for skeletal scanning. Figure 20-2 shows a bone scan. Areas of increased uptake, the dark spots, demonstrate high-activity areas that correspond to pathologic changes (uptake in the urinary bladder is normal). The radionuclide liver scan is the initial scan of choice for liver metastasis. Gallium scans localize areas of inflammation and tumor activity in patients with lymphoma. They are useful in monitoring changes in tumor size. Radiation safety procedures are important in nuclear medicine scanning. In both intravenous application and ingestion of radioactive isotopes, care in monitoring patient exposure to ionizing radiation is important. The elimination of isotopes that have run through the body (through urination) also necessitates careful monitoring and precautions.
Positron emission tomographic scanning uses short-lived radioisotopes such as carbon-11, nitrogen-13, and oxygen-15 in a solution commonly injected into a patient. The radioisotope circulates through the body and emits positively charged electrons, called positrons. These positrons collide with conventional electrons in body tissues and cause the release of gamma rays. These rays are detected and recorded. The computer creates a colored PET scan that shows function rather than structure. It can detect blood flow through organs such as the brain and heart, diagnose coronary artery disease, and identify the extent of stroke or heart attack damage. PET is useful in diagnosis of many different cancers. In that way, the physician can prescribe the appropriate treatment regimen early. In addition, PET images are used more and more to outline specific areas of anatomy and then correlated to other imaging studies such as CT and MR in treatment planning. The role of PET/CT is increasing, not only as an oncologic staging tool but also as an effective means of providing additional information for more effective treatment planning; more and more radiation oncology departments relay on PET/CT as an important tool in defining treatment areas. With both anatomic and physiologic information, the potential to visualize extension of disease not always seen on CT scan (because of size) can direct the radiation oncology team to ensure that the treatment field covers all diseased areas. This in itself can translate into better overall treatment results.
Magnetic Resonance Imaging
Magnetic resonance imaging is becoming increasingly important in radiation oncology. Technical advances in MRI allow departments to not only image targeted areas better for more accurate planning but also to aid in the daily delivery of treatment, particularly in adaptive radiation therapies. MRI records data that are based on the magnetic properties of the hydrogen nuclei, which can be thought of as tiny magnets spinning in random directions. These hydrogen nuclei (magnets) interact with neighboring atoms and with all applied magnetic fields.4 In this imaging modality, a strong uniform magnetic energy is applied to small magnetic fields that lie parallel to the direction of the external magnet. The patient is pulsed with radio waves, which cause the nuclei to send out a weak radio signal that is detected and reworked into a planar image of the body. The images, which indicate cellular activity, look similar to a CT scan. Figure 20-3 shows a sagittal MRI scan of the head.

Figure 20-3 Sagittal magnetic resonance image section through the head. (From Kelley LL, Peterson CM: Sectional anatomy for imaging professionals, ed 3, St. Louis, 2012, Mosby.)
MRI has a diagnostic advantage over CT in that it provides information about chemicals in an organ or tissue. Thus, MRI can be used in a noninvasive (one that does not involve puncture or incision of the skin or insertion of a foreign object into the body) biopsy on tumors. The disadvantages of MRI are the expensive magnetic shielding requirements, lower throughput (the number of patients an hour a machine can serve) when compared with CT, and increased cost in comparison with CT. MRI scans are commonly indexed, registered, and fused with CT scans and used in the treatment planning process. In these cases, the best of both imaging modalities are used to outline tumors for better conformal treatment planning.
Although MRI does not require the same precautions as needed with modalities that use ionizing radiation, stringent safety measures are necessary because of the strength of the magnets. The design of the MRI suite requires the identification of zoned safety areas. The team must pay close attention to maintaining an area that is ferrous-free (no iron) because the strength of the magnet can cause those items to forcefully fly into the bore of the unit. All items that are used for a patient in this area must be nonmagnetic. Maintaining a safe environment in the MRI suite is critical to providing safe patient care.
Ultrasound Scan
Ultrasound scan (US) uses high-frequency sound waves that are not heard by the human ear. These waves travel forward and continue to move until they make contact with an object; at that point, a certain amount of the sound bounces back. Submarines use this principle to find other underwater vessels and the depth of the ocean floor. US remains a less expensive and less hazardous alternative to the earlier studies.5 A transducer, a handheld instrument, generates high-frequency sound waves. It moves over the body part that is being examined. The transducer also picks up the returning sound waves. Normal and abnormal tissues exhibit varying densities that reflect sound differently. The resultant image is processed onto a screen and is called a sonogram. The images can be a still two-dimensional cross-sectioned image or a moving image, such as the heart of a fetus.
Ultrasound scan offers no exposure to ionizing radiation, is noninvasive and painless, and requires no contrast media. However, it does not effectively penetrate bone or air-filled spaces and therefore is not useful in imaging the skull, lungs, or intestines. In radiation therapy, the use of US continues to increase. It is very helpful in noninvasive determination of internal organ location, as evidenced in the increasing use of US to locate and guide brachytherapy implants, to locate tumors within the eye, and to increase positioning efficiency during conformal prostate treatment delivery with IMRT applications. Figure 20-4 shows a radiation therapist obtaining US localization information for a patient about to undergo treatment for prostate cancer.

Figure 20-4 Therapist obtaining ultrasound information for intensity-modulated radiation therapy (IMRT) treatment.
Modern imaging modalities provide important information to the radiation therapy team for tumor localization and for bladder volume verification. Cross-sectional images are very valuable. They provide views within the patient and display organs with their normal shape and orientation, typically in treatment position. The direct relationships allow for accurate treatment planning. The patient’s surface anatomy can be related to the inner structure. In addition to organs displayed with their normal living shape, normal anatomic relationships can be observed. In particular, the study of sectional images allows the radiation therapy practitioner to develop an excellent three-dimensional concept of anatomy.2 These modalities provide the basic information necessary for development of critical thinking skills in surface and sectional anatomy that is essential in the role of the radiation therapist.
Anatomic Positioning
Radiation therapy requires daily reproducible positioning for effective treatment delivery. The radiation therapist uses various terms to describe the relationship of anatomic parts, planes, and sections that serve as the foundation in understanding of the body’s structural plan.
Definition of Terms
With terms that reference human body position, the body is assumed to be in the anatomic position to allow for clear reference of directional relationships. The anatomic position is one in which the subject stands upright, with feet together flat on the floor, toes pointed forward, arms straight down by the sides of the body with palms facing forward, fingers extended, and thumbs pointing away from the body.1 Figure 20-5 shows this position.
Directional terms explain the location of various body structures in relation to each other. These terms are precise and avoid the use of unnecessary words and paint a clear picture for the radiation therapist. Superior means toward the head; inferior, toward the feet; medial, toward the midline of the body; and lateral, toward one side or the other. Anterior relates to anatomy nearer to the front of the body; posterior is nearer to or at the back of the body. Ipsilateral refers to a body component on the same side of the body, whereas contralateral refers to the opposite side of the body. Supine means lying face up; prone means lying face down. Table 20-1 outlines the directional terms commonly used by the radiation therapy team.
Planes and Sections
The human body may also be examined with respect to planes, which are imaginary flat surfaces that pass through it. Figure 20-6 illustrates the standard anatomic planes. The sagittal plane divides the body vertically into right or left sides. The median sagittal plane, also called the midsagittal plane, divides the body into two symmetric right and left sides. There is only one median sagittal plane. A parasagittal plane is a vertical plane that is parallel to the median sagittal plane and divides the body into unequal components, both right and left. A coronal or frontal plane is perpendicular (at right angles) to the sagittal plane and vertically divides the body into anterior and posterior sections. A horizontal or transverse plane is perpendicular to the midsagittal, parasagittal, and coronal planes and divides the human body into superior and inferior parts. When a healthcare professional views a body structure, that structure is often seen in a sectional view. A sectional view looks at a flat surface that results from a cut made through the three-dimensional structure.

Figure 20-5 Anatomic position and bilateral symmetry. In the anatomic position, the body is in an erect, or standing, posture with the arms at the sides and palms forward. The head and feet also point forward. The dotted line shows the body’s bilateral symmetry. As a result of this organizational feature, the right and left sides of the body are mirror images of each other. (From The body as a whole. In Thibodeau GA, Patton KT, editors: Anatomy and physiology, ed 6, St. Louis, 2007, Mosby.)
Surface and cross-sectional anatomies in radiation therapy are not solely a set of definitions or a listing of body parts. The practitioner must relate the body’s physical perspective to its overall function. The standardized anatomic terms presented assist in accurate realization of those relationships.
Body Cavities
The spaces within the body that contain internal organs are called body cavities (Figure 20-7). The two main cavities are the posterior, or dorsal, and the anterior, or ventral, cavities. The dorsal cavity can be further divided into: (1) the spinal or vertebral cavity, protected by the vertebrae, which contains the spinal cord; and (2) the cranial cavity, which contains the brain.
The anterior cavity is subdivided by a horizontal muscle, called the diaphragm, into the thoracic cavity and the abdominopelvic cavity. The thoracic cavity is further divided into a pericardial cavity, which contains the heart and two pleural cavities, including the right and left lungs.
The abdominopelvic cavity has two sections: the upper abdominal cavity and the lower pelvic cavity. No intervening partition exists between the two. The principal structures located in the abdominal cavity are the peritoneum, liver, gallbladder, pancreas, spleen, stomach, and most of the large and small intestines. The pelvic section contains the rest of the large intestine and the rectum, urinary bladder, and internal reproductive system.

Figure 20-6 Directions and planes of the body. These planes provide a standardized reference for the radiation therapist. (From Organization of the body. In Thibodeau GA, Patton KT, editors: Anatomy and physiology, ed 6, St. Louis, 2007, Mosby.)

Figure 20-7 Major body cavities. A, Sagittal view. B, Anterior view. (From Kelley LL, Peterson CM: Sectional anatomy for imaging professionals, ed 3, St. Louis, 2012, Mosby.)

Figure 20-8 Abdomen. A, Division of the abdomen into four quadrants. Diagram shows relationship of internal organs to the abdominopelvic quadrants. B, Nine abdominopelvic regions showing the most superficial organs. (From Kelley LL, Peterson CM: Sectional anatomy for imaging professionals, ed 3, St. Louis, 2012, Mosby.)
TABLE 20-1
Anatomic and directional terms
| TERM | DEFINITION | EXAMPLE |
| Superior | Toward the top of the body | The manubrium is superior to the body of the sternum. |
| Inferior | Toward the bottom of the body | The stomach is inferior to the lung. |
| Anterior | Toward the front of the body | The trachea is anterior to the esophagus, which is anterior to the spinal cord. |
| Posterior | Nearer to the back (rear) | The esophagus is posterior to the trachea. |
| Medial | Nearer to the midline; away from the side | The ulna is on the medial side of the forearm. |
| Lateral | Farther from the midline or to the side | The pleural cavities are lateral to the pericardial cavity. |
| Ipsilateral | On the same side (of the body) | The ascending colon and appendix are ipsilateral. |
| Contralateral | On the opposite side (of the body) | The ascending colon and descending colon are contralateral. |
| Proximal | Nearer to the point of origin or attachment | The humerus is proximal to the radius. |
| Distal | Away from the point of origin or attachment | The phalanges are distal to the carpals. |
| Superficial | On or near the body surface | The skin is superficial to the thoracic viscera. |
| Deep | Away from the body surface | The ribs are deep to the skin of the chest. |
Modified from Thibodeau GA, Patton KT: Anatomy and physiology, ed 6, St. Louis, 2007, Mosby.
The abdominopelvic cavity is large and is divided into four quadrants with a transverse plane placed across the midsagittal plane at the point of the umbilicus (navel). The four quadrants are the right upper, left upper, right lower, and left lower. The abdominal cavity can also be sectioned into a number of regions. Figure 20-8 shows the quadrants and regions of the abdomen and pelvis. Table 20-2 outlines the regions of the abdominal cavity.
TABLE 20-2
Regions of the abdominal cavity
| REGION | DESCRIPTION |
| Umbilical | Centrally located around the navel |
| Lumbar | Regions to the right and left of the navel; lumbar refers to the lower back, which is located here |
| Epigastric | Central region superior to the umbilical region |
| Hypochondriac | Regions to the right and left of the epigastric region and inferior to the cartilage of the rib cage |
| Hypogastric | Central region inferior to the umbilical region |
| Iliac | Regions to the right and left of the hypogastric region; iliac refers to the hip bones, which are located here |
The surface markings and locations of all structures are approximations and generalizations.2 However, knowledge of the varying body types provides the radiation therapist with practical information. If therapists have an idea of where the internal structures are, especially during a simulation, they can locate the placement of the treatment reference points sooner and more accurately. This equates to less time on the simulation table and faster capture of CT scout images for the patient.
Body Habitus
Roentgen’s discovery of the x-ray allowed scientists at the turn of the nineteenth century to revolutionize the medical field, both diagnostically and therapeutically.3 These early radiographs showed differences in the location of internal anatomy from one person to the next. Although everyone had the same organs, the organs were not necessarily in the exact same place. It was agreed that humans are a variable species with regard to structural characteristics, and it is evident that variety in general physique corresponds to great variation in visceral form, position, and motility. Consistency exists between certain physiques and certain types of visceral form and arrangement. A thorax of certain dimensions obviously can house lungs of only a certain form. The same is true for the abdomen. Knowledge of this can greatly assist the radiation therapist in relating internal anatomy to varying body types.
The physique, or body habitus, of an individual can be classified into four groups. The hypersthenic habitus represents about 5% of the population. This body type exhibits a short wide trunk, great body weight, and a heavy skeletal framework. The abdomen is long with great capacity, the alimentary tract is high, and the stomach is almost thoracic. The pelvic cavity is small. When a chest film of this body type is taken, the cassette may need to be turned crosswise to image the entire chest.
The sthenic habitus is similar to the hypersthenic habitus and represents most well-built individuals. Sthenic habitus has the highest rate of occurrence and accounts for about half of the population. These persons are of considerable weight with a heavy skeletal framework when compared with hypersthenic individuals. Like the hypersthenic, the alimentary tract is high but with the stomach located slightly lower in the trunk.
The hyposthenic habitus, which represents approximately 35% of the population, has an average physique. This habitus has many of the sthenic characteristics and may be difficult to identify. The abdominal cavity falls between the sthenic and the asthenic.
The asthenic habitus has a more slender physique, light body weight, and a lighter skeletal framework. It is found in 10% of the population. The thorax has long narrow lung fields, with its widest portion in the upper zones. The heart seems to “hang” in the thoracic cavity, almost like a pendant. The asthenic body has an abdomen longer than the hypersthenic and is typically accompanied by a pelvis with great capacity. The alimentary tract is lowest of all types mentioned. Figure 20-9 compares the various body habitus. Although the internal components are the same in all body types, the locations do vary. These categories can help standardize the variances seen from person to person.
Lymphatic System
Knowledge of the lymphatic system is important in radiation therapy. For local and regional control of malignant disease processes to be achieved, the anatomy of the lymphatic system must be considered. Many tumors spread through this system; often areas of tumor spread are predicted based solely on that knowledge. For example, in a head and neck treatment plan, the supraclavicular fossa (SCF) is commonly treated even without clinical evidence of tumor present (prophylactic treatment). This treatment is important because the lymphatic drainage of the head and neck eventually drains to that area, which is the location of the right and left lymphatic ducts. This increases the potential for dissemination of disease to other parts of the body. In any examination of surface and cross-sectional anatomy specific to radiation therapy, the lymphatic system is important.
The lymphatic system consists of lymphatic vessels, lymphatic organs, and the fluid that circulates through it, called lymph. The system is closely associated with the cardiovascular system and is composed of specialized connective tissue that contains a large quantity of lymphocytes. Lymphatic tissue is found throughout the body.
The lymphatic system has three main functions. First, lymphatic vessels drain tissue spaces of interstitial fluid that escapes from blood capillaries and loose connective tissues, filters it, and returns it to the bloodstream, an essential part of maintaining the overall fluid levels in the body. This function of draining and transporting interstitial fluid is the most important system role.6 Second, the lymphatic system absorbs fats and transports them to the bloodstream. Third, this intricate system plays a major role in the body’s defense and immunity. Immunity is the ability of the body to defend itself against infectious organisms and foreign bodies. Specifically, lymphocytes and macrophages protect the body by recognizing and responding to the foreign matter.
Lymphatic Vessels
Lymphatic vessels contain lymph. Lymph is excessive tissue fluid that consists mostly of water and plasma proteins from capillaries. It differs from blood by the absence of formed elements. Lymphatic vessels start in spaces between cells; at that point, they are referred to as lymphatic capillaries. These lymphatic vessels are extensive. Virtually every region of the body that has a blood supply is richly supplied with these capillaries. It stands to reason that those areas that are avascular do not have the same number of vessels. Examples of these avascular areas are the central nervous system and bone marrow. These lymphatic capillaries are more permeable for substances to enter than are associated blood capillaries. Cellular debris, sloughed off cells, and foreign substances that occur in the intercellular spaces are more readily collected through these lymphatic pathways and transported away for filtration. They start blindly in the interstitial spaces and flow in only one direction.
The lymphatic capillaries join to form larger lymphatic vessels. Lymphatic vessels resemble veins in structure but have thinner walls and more valves that promote the one-way flow. These larger vessels follow veins and arteries and eventually empty into one of two ducts in the upper thorax—the thoracic duct or the right lymphatic duct—which then flow into the subclavian veins.

Figure 20-9 Comparison of the four body habitus. Note that all feature the same structures. However, the internal viscera vary in position from one physique to another.
Fluid movement in the lymphatic system depends on hydrostatic and osmotic pressures that increase through skeletal muscle contraction. As the muscles around the vessels contract, the lymph is moved past a one-way valve that closes, which prevents the lymph from flowing backward. Respiratory movements create a pressure gradient between two ends of the lymphatic system. Fluid flows from high-pressure areas, such as the abdomen, to low-pressure areas, such as the thorax, where pressure falls as each inhalation occurs.
Lymph Nodes
Along the paths of the lymph vessels are lymph nodes. These nodes vary in size from 2 to 30 mm in length, and they often occur in groups.6 A lymph node contains both afferent and efferent lymphatic vessels. Afferent lymphatic vessels enter the lymph node at several points along the convex surface. They contain one-way valves that open into the node, bringing the lymph into it. On the other side of the node are efferent vessels. The efferent lymphatic vessels are overall smaller in diameter than the afferent vessels; their valves open away from the node, again facilitating one-way flow.6 More afferent vessels come into a node than efferent vessels come out of it, which slows the flow through the nodes. This is similar to driving along a four-lane highway during rush hour and getting to a point of road construction that restricts traffic flow to one lane. You can go in only one direction and must wait your turn to move through the area. This slowing of the lymph through the node permits the nodes to effectively filter the lymph, and, through phagocytosis, the endothelial cells of the node engulf, devitalize, and remove contaminants. Figure 20-10 shows the components of a typical lymph node. The substances can be trapped inside the reticular fibers and pathways throughout the node, which causes edema. Edema is an excessive accumulation of fluid in a tissue that produces swelling. Edema can occur when excessive foreign bodies, lymph, and debris are engulfed in the node. This condition is evident when a person has a cold or the flu. The subdigastric nodes, located in the neck just below the angle of the mandible, become swollen and tender because of the heightened phagocytic activity in that area to rid the body of the trapped contaminants. The swelling goes down as the pathogen is devitalized. Edema also occurs when altered lymphatic pathways cause more than normal amounts of lymph filtration. This condition is commonly seen after mastectomy. The arm on the side of the surgery is often swollen because of the altered natural lymphatic pathways after the operation. The same amount of lymph is redirected through alternate routes, which causes the slowdown of lymphatic flow.

Figure 20-10 Lymph node. Arrows indicate the direction of lymph flow. The germinal centers are sites of lymphocyte production. As lymph moves through the lymph sinuses, macrophages remove foreign substances. (See color plate 11.) (From Lymphatic system. In Thibodeau GA, Patton KT, editors: Anatomy and physiology, ed 6, St Louis, 2007, Mosby.)
Lymphatic Organs
The spleen is the largest mass of lymphatic tissue in the body at roughly 12 cm in length. It is located posterior to and to the left of the stomach in the abdominal cavity, between the fundus of the stomach and the diaphragm. The spleen actively filters blood, removes old red blood cells, manufactures lymphocytes (particularly B cells, which develop into antibody-producing plasma cells) for immunity surveillance, and stores blood. Because the spleen has no afferent lymphatic vessels, it does not filter lymph. However, the spleen is often thought of as a large lymph node for the blood. During a laparotomy, which is surgical inspection of the abdominal cavity, in patients with lymphoma, this organ is often removed for biopsy and staging purposes. In this case, the bone marrow and liver then assume the functions of the spleen.
The thymus is located along the trachea superior to the heart and posterior to the sternum in the upper thorax. This gland is larger in children than in adults and is more active in pediatric immunity. The gland serves as a site where T lymphocytes can mature.
The tonsils are series of lymphatic nodules embedded in a mucous membrane. They are located at the junction of the oral cavity and pharynx. These collections of lymphoid tissue protect against foreign body infiltration by producing lymphocytes. The pharyngeal tonsils, or adenoids, are in the nasopharynx; the palatine tonsils are in the posterior lateral wall of the oropharynx; and the lingual tonsils are at the base of the tongue in the oropharynx.
The thoracic duct is on the left side of the body and is typically larger than the right lymphatic duct. It serves the lower extremities, abdomen, left arm, and left side of the head and neck and drains into the left subclavian vein. This duct is approximately 35 to 45 cm in length and begins in front of the second lumbar vertebra (L2) where it is called the cisterna chyli. As lymph travels through the lower extremities to the cisterna chyli, it continues its upward trek to the thoracic duct. As it passes through the mediastinum, it bypasses many of the mediastinal node stations. Because of this anatomic fact, pedal lymphangiography, a technique used for visualization of nodal status with injection of dye into lymphatic outlets in the feet, cannot be used to visualize mediastinal disease. The right lymphatic duct serves only the right arm and right side of the head and neck and drains into the right subclavian vein. This duct is approximately 1 to 2 cm in length. These ducts drain into the right and left subclavian veins, which in turn drain to the heart by way of the superior vena cava. Box 20-1 reviews the flow of lymph through the lymphatic system.
Knowledge of the location of the lymph nodes and direction of lymph flow is important in the diagnosis and prognosis of the spread of metastatic disease. Cancer cells, especially carcinomas from epithelial tissues, often spread through the lymphatic system. Metastatic disease sites are predictable by their lymphatic flow from the primary site.7 Inadequate knowledge of the lymphatic system may translate into ineffective treatment delivery.
Axial Skeleton: Skull, Vertebral Column, and Thorax
Most imaging modalities provide valuable information through visualization of differences in anatomic densities. The denser a component, the whiter it appears on a radiographic image. The axial skeleton provides the radiation therapist with a wealth of information used to reference the location of internal anatomy. The following sections briefly review axial skeleton anatomy and provide the reader with a reference necessary in relating internal structures to surface anatomy.
Skull
The skull has approximately 29 bones, and these are mostly joined by sutures, joints held together by connective tissue, which limit movement. The mandible and ossicles, which are bones in the middle ear, are the only bones in the skull not joined by sutures.
The frontal, parietal, temporal, sphenoid, and occipital bones all form the lateral aspect of the skull vault. The first two meet in the midline at the bregma, the roof of the skull, often referred to as the “soft spot,” and the last two meet at the lambda. The facial skeleton, or visceral cranium, includes the 14 bones of the face. It consists of two maxillary bones, two zygomatic bones, two nasal bones, two lacrimal bones, two palatine bones, two inferior conchae, and one mandible.
Sutures
The four prominent sutures in the skull, or fibrous joints, allow little or no movement between them, which makes the transitions between bones of the skull smooth and stable. The coronal suture lies between the frontal bone and the two parietal bones. On either side of the skull, it begins at the bregma and ends at the temporal bone. The sagittal suture lies between the two parietal bones and runs from the bregma to the lambda. The lambdoidal suture is in the posterior portion of the skull and lies between the parietal and occipital bones. Finally, the squamosal sutures, one on each side of the skull, are located near the ears and lie between the parietal and temporal bones. Identification of these sutures radiographically can assist the radiation therapist in locating corresponding underlying structures. Figure 20-11 shows the bones of the skull and sutures.
Paranasal Sinuses
The bones of the skull and face contain the paranasal sinuses, which are air spaces lined by mucous membranes that reduce the weight of the skull and give a resonant sound to the voice. When a person has sinusitis, an inflammation and blockage of the sinus cavities, the voice often has a “stuffed up” tone (loss of resonance). The paired sinuses are air-filled spaces within the frontal, maxillary, sphenoid, and ethmoid bones. They are lined with mucous membranes and are relatively small at birth. They enlarge during development of the permanent teeth and reach adult size shortly after puberty.2 The paranasal sinuses are easily seen on plain x-ray, CT, and MRI. Cross sections are an excellent tool to study the surface relations in these areas.7 Figure 20-12 shows the paranasal sinuses in cross section.
The maxillary sinus is a pyramid-shaped cavity that is enclosed in the maxilla. It is the largest of the paranasal sinuses. The roof of the sinus forms the floor of the orbit. The frontal sinus lies in the frontal bone above the orbit. It may be located on the surface with a triangle between the following three points: the nasion, a point 3 cm above the nasion, and the junction of the medial and middle thirds of the superior orbital margin (SOM). The sphenoid sinus lies posterior and superior to the nasopharynx, enclosed in the body of the sphenoid bone at the level of the zygomatic arch. Superiorly the sinus is related to the sella turcica (which is approximately 2 cm anterior and 2 cm superior to the external auditory meatus) and the pituitary. The pituitary may be surgically removed through a transsphenoidal approach, one that goes through the nasal cavity; in diseases in which the transsphenoidal approach in not a viable option, a transcranial methodology may be used. The ethmoid sinus is bilateral but consists of a honeycomb of air cells that lie between the middle wall of the orbit and the upper lateral wall of the nose.
Vertebral Column
The vertebral column, located in the midsagittal plane of the posterior cavity, extends from the skull to the pelvis. It consists of separate bones, the vertebrae, which appear as rectangular densities on radiographs.2 The 33 bones in the adult vertebral column are shown in Figure 20-13, which also indicates the number of bones in each section. There are 7 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 4 coccygeal vertebrae. At the inferior aspect of the column, the sacrum has five fused bones, whereas the coccyx is composed of four fused bones.

Figure 20-11 Skull. A, Anterior view of the skull. B, Skull viewed from the left side. (From Kelley LL, Petersen CM: Sectional anatomy for imaging professionals, ed 2, St. Louis, 2007, Mosby.)
The sacrum supports the rest of the vertebral column and thus provides the support necessary for the human body’s erectness. The vertebrae are separated by radiolucent fibrocartilage called intervertebral disks. In the cervical and thoracic spine, the disks are of similar thickness. In the lumbar spine, the height increases progressively down the column.2
The vertebral column is also very flexible. Although limited motion exists between any two neighboring vertebrae, the vertebral column is capable of substantial motion. The column also protects the spinal cord and provides points of attachment for the skull, thorax, and extremities.
Vertebral Characteristics
Most vertebrae share several common characteristics. They have a body that is attached to a posterior vertebral arch. These two components border the vertebral foramen, the passage through which the spinal cord passes. The spinous and transverse processes allow for muscle attachments. The spinou s process is posterior and forms where two laminae meet. These laminae are often palpated in aligning spinal treatment fields. The transverse processes are lateral projections where a pedicle joins a lamina. Figure 20-14 shows a typical vertebra with its prominent features labeled.
The first two vertebrae, C1 and C2, are atypical from all others. C1, the atlas, serves the specialized function of supporting the skull and allowing the head to tilt in the “yes” motion. It has no vertebral body. C2, the axis, has an odontoid process that extends into the ring of the atlas. When the head turns from side to side, it pivots on this process. These two vertebrae are shown in Figure 20-15.

Figure 20-12 The paranasal sinuses. A, Lateral view. B, Frontal view. The inset image is a projection radiograph that shows the outlines of the facial bones and some of the paranasal sinuses. (From Skeletal system. In Thibodeau GA, Patton KT, editors: Anatomy and physiology, ed 6, St. Louis, 2007, Mosby.)

Figure 20-13 Right lateral view, anterior view, and posterior view of the vertebral column. The image inset shows a midsagittal magnetic resonance image of the vertebral column from the left side. (From Support and movement. In Thibodeau GA, Patton KT, editors: Anatomy and physiology, ed 6, St. Louis, 2001, Mosby.)

Figure 20-14 Lumbar vertebrae. Lateral and superior views of L3. (From The skeletal system. In Thibodeau GA, Patton KT, editors: Anatomy and physiology, ed 6, St. Louis, 2007, Mosby.)
Vertebral Column Curvatures
The vertebral column demonstrates several curvatures that develop at different levels.2 These curvatures can be classified as either primary or compensatory (secondary) curvatures. Primary vertebral curves are developed in utero as the fetus develops in the C-shaped fetal position, and they are present at birth. Compensatory vertebral curves or secondary vertebral curves develop after birth as the child learns to sit up and walk. Muscular development and coordination influence the rate of secondary curvature development.
The cervical curve extends from the first cervical to the second thoracic vertebrae (C1 to T2). It is convex anteriorly and develops as children learn to hold their head up and sit alone at approximately 4 months of age. This curve is a secondary curvature. The thoracic curve extends from T2 to T12 and is concave anteriorly. This is one of the primary curves of the vertebral column. The lumbar curve runs from T12 to the anterior surface of L5. This convex forward curve develops when a child learns to walk at approximately 1 year of age. The pelvic curve is concave anteriorly and inferiorly and extends from the anterior surfaces of the sacrum and coccyx. This is the other primary curve. The thorax can also have a slightly right or left lateral curve that is influenced by a child’s predominate use of the right or left hand during childhood and adolescence.
The cervical, thoracic, lumbar, and pelvic curves are found in the normal human vertebral column. Three abnormal curvatures also are present both clinically and radiographically. Kyphosis is an excessive curvature of the vertebral column that is convex posteriorly. This curve can develop with degenerative vertebral changes. Scoliosis is an abnormal lateral curvature of the vertebral column with excessive right or left curvature in the thoracic region. This abnormal curvature can develop if only one side (half) of the vertebral bodies are irradiated in pediatric patients, as in the case of patients treated for Wilms’ tumor. The radiation slows vertebral body growth on one side and the contralateral side grows at a normal rate, thus creating scoliotic changes. Lordosis is an excessive convexity of the lumbar curve of the spine. Spondylolisthesis occurs when one of the spine’s vertebrae (bones) slips forward over the vertebra beneath it. Spondylolisthesis occurs most often in the lumbar spine (low back). Figure 20-16 shows these abnormal spine curvatures.
Thorax
The illustration in Figure 20-17 shows the full thorax made up of the bony cage formed by the sternum, costal cartilage, ribs, and thoracic vertebrae to which they are attached.1,8 The thorax encloses and protects the organs in the thoracic cavity and upper abdomen. It also provides support for the pectoral girdle and upper extremities.
Sternum and Ribs
The sternum, or breastbone, comprises three parts: the manubrium, which is the superior portion; the body, the middle and largest portion; and the xiphoid process, which is the inferior projection that serves as ligament and muscle attachments. The manubrium has a depression called the suprasternal notch (SSN), which occurs at the level of T2 and articulates with the medial ends of the clavicles. This point may be used in measuring the angle of chin tilt in patients with head and neck cancer when thermoplastic immobilization masks are not used. It also serves as a palpable landmark when setting up a SCF field. The manubrium also articulates with the first two ribs. The junction of the manubrium and the body form the sternal angle, also called the angle of Louis; it occurs at the level of T4.
The body of the sternum articulates with the 2nd through 10th ribs. Of the 12 pairs of ribs, the superior 7 pairs are considered true ribs. They are easily seen in the asthenic body habitus and are palpable in most others.9 They articulate posteriorly with the vertebrae and anteriorly with the sternum directly through a cartilaginous joint. These are known as the vertebrosternal ribs. The next three pairs join with the vertebrae posteriorly and anteriorly with the cartilage of the immediately anterior rib. These ribs are classified as vertebrochondral ribs. The next (last) pairs articulate only with the vertebrae and do not connect with the sternum in any way; they are called floating ribs.

Figure 20-17 The bony framework of the thorax provides many useful landmarks. (From Skeletal system. In Thibodeau GA, Patton KT, editors: Anatomy and physiology, ed 6, St. Louis, 2007, Mosby.)
The axial skeleton is easily seen with most imaging techniques used in radiation therapy. A thorough working knowledge of these components serves the radiation therapist in overall daily operations. This information is used in relating the surface and cross-sectional anatomy and the palpable bony landmarks that are used in field placement and treatment planning.
Surface and Sectional Anatomy and Landmarks of the Head and Neck
The human head has various anatomic features that are both interesting and useful to the radiation therapist. These structures are rich in bony moveable soft tissue landmarks and lymphatics commonly used in field placement, position locations, and so forth. The bony landmarks are stable and are typically used as reference points, as in locating a positioning or central axis tattoo. Soft tissue landmarks can also be extremely useful. However, they tend to be more mobile and provide a less reliable reference than the bony landmarks.
Bony Landmarks: Anterior and Lateral Skull
Figures 20-18 and 20-19 outline the locations of the following anterior and lateral bony structures.

Figure 20-18 Bony landmarks of the anterior skull: 1, Frontal bone; 2, superciliary arch; 3, glabella; 4, nasion; 5, superior orbital margin; 6, maxilla; 7, zygomatic bone; 8, angle of mandible; 9, sphenoid bone (greater wing); 10, temporal bone; 11, parietal bone.

Figure 20-19 Bony landmarks of the lateral skull: 1, Frontal bone; 2, superciliary arch; 3, glabella; 4, nasion; 5, superior orbital margin; 6, maxilla; 7, zygomatic bone; 8, lateral canthus; 9, midzygoma point; 10, external acoustic meatus; 11, mastoid process; 12, angle of mandible; 13, external occipital protuberance or inion; 14, greater wing of sphenoid; 15, temporal bone; 16, parietal bone; 17, parietal eminence; 18, sternocleidomastoid muscle; 19, trapezius muscle; 20, clavicle.
The glabella is the slight elevation directly between the two orbits in the frontal bone. It is just above the base of the nose. This palpable landmark is more prominent in some individuals than in others.
The nasion is the central depression at the base of the nose. It is formed by the point at which the frontal and nasal bones join.
The superciliary arch starts at the glabella and moves superiorly and laterally above the central portion of the eyebrow. The central part lies superficially to the frontal sinuses on either side and forms the brow of the skull.
The superior orbital margin (SOM) rests just inferior to the eyebrow and is more pronounced on its lateral aspect. The SOM forms the roof of the orbit and serves as one of the points used to delineate the inferior border of whole brain fields (along with the tragus and mastoid tip). When that part of the SOM is in the treatment field, the frontal part of the brain is also in the field.
The maxilla is the bone between the ala (lateral soft tissue prominence) of the nose and the prominence of the cheek. This bone houses the largest of the paranasal sinuses. The inferior alveolar ridge of the maxilla houses the teeth sockets.
The zygomatic bone forms part of the lateral aspect of the orbit and the prominence of the cheek. The articulation between the frontal process of the zygomatic bone and the zygomatic process of the frontal bone can be palpated in the lateral orbital margin (LOM). The midzygoma point, a point midway between the external auditory meatus (EAM) and the lateral canthus, lies roughly at the floor of the sphenoid sinus and the roof of the nasopharynx. One centimeter superior to that point corresponds to the floor of the sella turcica, and 1.5 cm superior to the point corresponds to the pituitary gland.
The mastoid process is an extension of the mastoid portion of the temporal bone at the level of the ear lobe. It is commonly used to delineate the posterior point of the inferior whole brain border (imaginary line that extends from the SOM to the mastoid tip, commonly through the tragus of the ear).
The external occipital protuberance (EOP; or inion) is the prominence in the posterolateral aspect of the occipital bone of the skull.
The angle of the mandible is the point at which the muscles used for chewing are attached. In addition, several lymph node groups are located inferior and medial to that point. It is also a classic landmark for the tonsils.
Landmarks around the Eye
Whenever practical, the landmarks used around the eye should be the bony landmarks. They are radiographically visible and are easily checked if a second course of treatment is necessary in the same or neighboring area. The soft tissue landmarks often vary with age, weight, and surgical changes. They are open to variable interpretation and misinterpretation because of the extreme flexibility of the skin. Figure 20-20 illustrates these landmarks. The following outlines the important landmarks around the eye.
The superior orbital margin forms the upper border of the orbit.
The inferior orbital margin (IOM) forms the lower border of the bony orbit.
The lateral orbital margin is a bony landmark that forms the lateral border of the bony orbit.
The medial orbital margin is extremely difficult to palpate and therefore is not clinically useful as an anatomic landmark. It does have some usefulness radiographically.
The inner canthus (IC) is a soft tissue landmark that is formed at the junction of the upper and lower eyelids at the medial aspect of the eye.
The outer canthus (OC) is a soft tissue landmark that is formed at the junction of the upper and lower eyelid at the lateral aspect of the eye.
The punctum lacrimae is a soft tissue landmark that can be used as a point of reference in the surface anatomy of the eye. This white-appearing section of the eye lies just next to the IC on the lower eyelid. Tears are drained through this duct into the lacrimal duct. This opening can become blocked by fibrotic changes from ionizing radiation administered to the area, which causes constant tearing. Extreme caution should be exercised to avoid this occurrence, particularly with treatment of the anterior maxillary sinus field arrangement.
Landmarks around the Nose
As in the case of the eye, the landmarks used around the nose should be the bony landmarks. Soft tissue landmarks often vary with age, weight, and surgical changes and are open to variable interpretation and misinterpretation because of the extreme flexibility of the skin. Figure 20-21 illustrates these landmarks. The following outlines the landmarks around the nose; some are reiterated from previous sections.
The lateral ala nasi (LAN) is a soft tissue landmark formed by the lateral attachment of the ala nasi with the cheek. The inferior ala nasi (IAN) is a soft tissue landmark formed by the inferior attachment of the ala nasi with the cheek. Both are prominent in most people and can be useful landmarks with measurements in any direction, such as superior to inferior, medial to lateral, and anterior to posterior.
The nasion is the depression of the nose where it joins the forehead at the level of the SOM. It is a useful landmark if it is deep and pronounced and coincides with the crease of the nose. If it is shallow, it is more open to variable interpretation.
The glabella is the bony prominence in the forehead at the level just superior to the SOM. As with the nasion, it is useful if it is prominent and sharp. It is not useful if it is flat or extremely curved, where it, too, is open to misinterpretation.
The ala nasi, dorsum of the nose, and external nares are useful as checkpoints in the surface anatomy of the nose and useful in the positioning of radiation treatment portals.
Landmarks around the Mouth
Landmarks around the mouth are generally not very accurate because of the extreme flexibility in the area. Every effort should be made to document these landmarks with reference to more stable anatomic points, if possible. If these landmarks are used, the position of the mouth is important to note, as well as any positioning or immobilization devices used, such as a cork, oral stent, or similar devices. Figure 20-22 illustrates the landmarks around the mouth.
The commissure of the mouth is formed at the junction of the upper and lower lip. This landmark is extremely mobile.
The mucocutaneous junction (MCJ) is located at the junction of the vermilion border of the lip with the skin of the face.
The columella is located at the junction of the skin of the nose with the skin of the face at the superior end of the philtrum.
Landmarks around the Ear
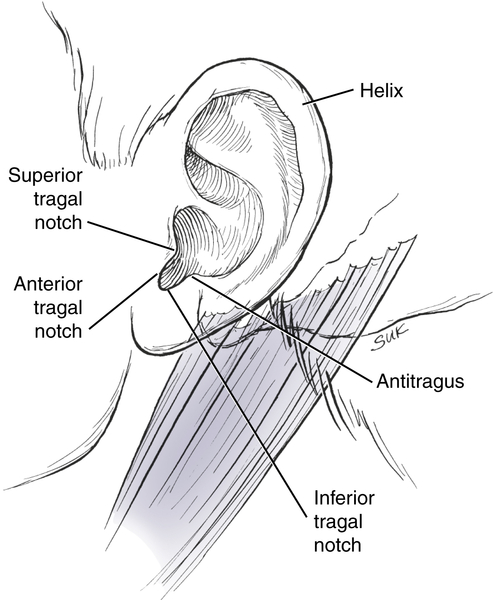
The external ear consists of the auricle or pinna, which is formed from a number of irregularly shaped pieces of fibrocartilage covered by skin. It has a dependent lobule, or ear lobe, and an anterior tragus, commonly used as anatomic references.1,5,10 Parts of the ear are labeled in Figure 20-23.
The tragus is made up of a fairly stable cartilage that partially covers the external auditory meatus in the external ear and is often used in radiation therapy during initial positioning. A pair of optical lasers, coincident with each other, can be focused on the tragus on both sides of the patient. This places the patient’s head in a relatively nontilted position because their locations are typically symmetrical. Just anterior to the tragus corresponds to the posterior wall of the nasopharynx. The posterior limit of many head and neck off-cord fields lies at this point.
The tragal notch is the semicircular notch in the ear immediately inferior to the tragus. The superior tragal notch (STN) makes up the superior margin of the tragal notch. The inferior tragal notch (ITN) defines the inferior margin of the tragal notch. The anterior tragal notch (ATN) makes up the anterior margin of the tragal notch.
Landmarks and Anatomy around the Neck
The boundaries of the anterior aspect of the neck are the body and angles of the mandible superiorly and the superior border and SSN of the sternum and the clavicles. The posterior aspect of the neck is bound superiorly by the EOP and laterally by the mastoid processes. The posterior inferior border ends at approximately the level of the seventh cervical vertebra to the first thoracic vertebra (C7-T1).2 Figure 20-24 illustrates the features of the neck anatomy.
The upper cervical vertebrae are not easily palpated; the last cervical and first thoracic vertebrae are the most obvious. The hyoid bone lies opposite the superior border of C4. When the head is in the anatomic position, the hyoid bone may be moved from side to side between the thumb and middle finger, approximately 1 cm below the level of the angle of the mandible, C2-C3. Table 20-3 relates the location of the cervical bony landmarks to other associated anatomic features.
Pharynx
The pharynx is a membranous tube that extends from the base of the skull to the esophagus. It connects the nasal and oral cavities with the larynx and esophagus. It is divided into the nasopharynx, oropharynx, and laryngopharynx, shown in Figure 20-25. Note that in a sectional view of the low neck, the therapist can easily remember how to distinguish the order of the spinal cord, esophagus, and trachea. From a posterior to anterior perspective, the order is always SET up: S, spinal cord; E, esophagus; and T, trachea.

Figure 20-24 The neck has many useful anatomic landmarks that can assist the radiation therapist. Relating surface structures to deeper anatomy is essential in the practice of radiation therapy. 1, Body of mandible; 2, angle of mandible; 3, hyoid bone; 4, thyroid cartilage; 5, cricoid cartilage; 6, mastoid process; 7, external occipital protuberance (EOP); 8, atlas; 9, axis; 10, suprasternal notch; 11, clavicle; 12, sternocleidomastoid muscle; 13, trapezius muscle.
TABLE 20-3
Cervical neck landmarks and associated anatomy
| CERVICAL SPINE | ASSOCIATED ANATOMY |
| C1 | Transverse process lies just inferior to the mastoid process; may be palpated in the hollow inferior to the ear |
| C2-C3 | Level with the angle of the mandible; lies 5 to 7 cm below the external occipital protuberance |
| C4 | Located just superior to the hyoid bone of the neck; serves as a point of muscle attachment |
| C4 | Level with the superior portion of the thyroid cartilage and marks the beginning of the larynx |
| C6 | Level with the cricoid cartilage; location of the junction of the larynx to trachea and pharynx to esophagus |
| C7 | First prominent spinous process in the posterior neck |

Figure 20-25 Nasal cavity and pharynx. A, Sagittal section through the nasal cavity and pharynx viewed from the medial side. B, Photograph of a sagittal section of the nasal cavity. (A, From Symonds P, et al: Walter and Miller’s textbook of radiotherapy, ed 7, St. Louis, 2012, Churchill Livingstone. B, From The lymphatic system and immunity. In Seeley RR, Stephens TD, Tate P, editors: Essentials of anatomy and physiology, St. Louis, 1991, Mosby.)
1. The nasopharynx, or epipharynx, communicates with the nasal cavity and provides a passageway for air during breathing.
2. The oropharynx, or mesopharynx, opens behind the soft palate into the nasopharynx and functions as a passageway for food moving down from the mouth and for air moving in and out of the nasal cavity.
3. The laryngopharynx, or hypopharynx, is located inferior to the oropharynx and opens into the larynx and esophagus.
Larynx
The larynx connects to the lower portion of the pharynx above it and to the trachea below it. It extends from the tip of the epiglottis at the level of the junction of C3 and C4 to the lower portion of the cricoid cartilage at the level of the C6 vertebra.10 The larynx is subdivided into three anatomic regions: the supraglottis, glottis, and subglottis. Figure 20-26 illustrates sectional views of the larynx. The larynx is actually an enlargement in the airway at the top of the trachea and below the pharynx. It serves as a passageway for air moving in and out of the trachea and functions to prevent foreign objects from entering the trachea.
The thyroid cartilage forms a midline prominence, the laryngeal prominence or Adam’s apple, which is more obvious in the adult male. The vocal cords are attached to the posterior part of this prominence. The cricoid cartilage serves as the lower border of the larynx and is the only complete ring of cartilage in the respiratory passage; the others are open posteriorly. It is palpable as a narrow horizontal bar inferior to the thyroid cartilage and is at the level of the C6 vertebra.
Nasal and Oral Cavities
The nasal cavity opens to the external environment through the nostrils. Posteriorly the nostrils are continuous with the nasopharynx and are lined with a ciliated mucous membrane. The oral cavity has a vestibule, which is the space between the cheeks and teeth and the oral cavity proper that opens posteriorly into the oropharynx and houses the soft palate, hard palate, uvula, anterior tongue, and floor of the mouth.
Surface Anatomy of the Neck
Anatomic landmarks around the neck are mainly used as checkpoints and reference points that can establish the patient’s position or the anatomic position of the treatment field. The most commonly used landmarks of the neck are:
1. Skin profile
2. Sternocleidomastoid muscle, which is attached to the mastoid and occipital bones superiorly and sternal and clavicular heads inferiorly. These muscles form the V shape in the neck and are associated with a great number of lymph nodes.
3. Clavicle
4. Thyroid notch
5. Mastoid tip
6. EOP
7. Spinous processes
These surface neck landmarks assist the radiation therapist in referencing locations of treatment fields and dose-limiting structures. They are illustrated in Figure 20-27.
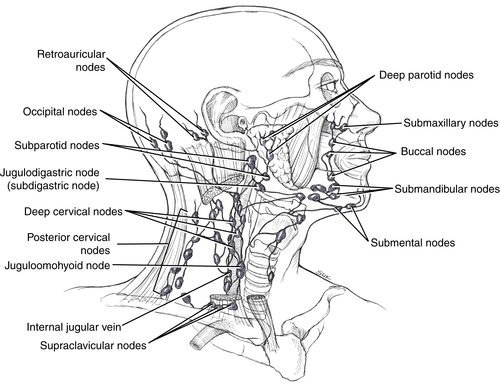
Lymphatic Drainage of the Head and Neck
The lymphatic drainage of the head and neck is through deep and superficial lymphatic channels, around the base of the skull, and deep and superficial lymph chains. The head and neck area is rich in lymphatics. Enlarged cervical lymph nodes are the most common adenopathy seen in clinical practice.1 They are typically associated with upper respiratory tract infections but may also be the site of metastatic disease from the head and neck, lungs, or breast or of primary lymphoreticular disease such as Hodgkin disease. The lymph nodes of the head and neck are outlined in the following section. Figures 20-28 and 20-29 show the lymphatic chains and nodes in the head and neck.

Figure 20-29 Sagittal view of deep lymph nodes in the head and neck in relation to underlying structures.
The occipital lymph nodes, typically one to three in number, are located on the back of the head, close to the margin of the trapezius muscle attachment on the occipital bone. These nodes provide efferent flow to the superior deep cervical nodes.
The retroauricular lymph nodes, usually two in number, are situated on the mastoid insertion of the sternocleidomastoid muscle deep to the posterior auricular muscle. They drain the posterior temporo-occipital region of the scalp, auricle, and external auditory meatus. They provide efferent drainage to the superior deep cervical nodes.
The deep parotid lymph nodes are arranged into two groups. The first group is embedded in the parotid gland, whose superior border is the temporomandibular joint (TMJ); posterior border, the mastoid process; inferior border, the angle of the mandible; and anterior border, the anterior ramus. The second group—the subparotid nodes—are located deep to the gland and lie on the lateral wall of the pharynx. Both drain the nose, eyelid, frontotemporal scalp, EAM, and palate. They provide efferent flow to the superior deep cervical nodes.
The submaxillary lymph nodes are facial nodes that are scattered over the infraorbital region. They span from the groove between the nose and cheek to the zygomatic arch. The buccal lymph nodes are scattered over the buccinator muscle. These nodes drain the eyelids, nose, and cheek and supply efferent flow to the submandibular nodes. The submandibular lymph nodes lie on the outer surface of the mandible. They drain the scalp, nose, cheek, floor of the mouth, anterior two thirds of the tongue, gums, teeth, lips, and frontal, ethmoid, and maxillary sinuses. They provide efferent drainage to the superior deep cervical nodes.
The retropharyngeal lymph nodes, one to three in number, lie in the buccopharyngeal fossa, behind the upper part of the pharynx and anterior to the arch of the atlas. These nodes are commonly involved in nasopharyngeal tumors and subsequently are included in the treatment fields.
The submental lymph nodes are found in the submental triangle of the digastric muscles, lower gums and lips, tongue, central floor of the mouth, and skin of the chin. These nodes provide efferent drainage to the submandibular nodes.
The superficial cervical lymph nodes form a group of nodes located below the hyoid bone and in front of the larynx, trachea, and thyroid gland.
The deep cervical lymph nodes form a chain of 20 to 30 nodes along the carotid sheath and around the internal jugular chain along the sternocleidomastoid muscle. The jugulodigastric lymph node, at times called the subdigastric node, is typically located superior to the angle of the mandible and drains the tonsils and the tongue. Inferiorly, the chain spreads out into the subclavian triangle. One of the nodes in this group lies in the omohyoid tendon and is known as the juguloomohyoid lymph node.1,2 When these two nodes are enlarged, carcinoma of the tongue may be indicated because enlarged neck nodes may be the only sign of the disease. These vessels supply efferent flow to form the jugular trunk, which drains to the thoracic or right lymphatic duct, both in the SCF. The cervical lymph nodes are typically included in the treatment fields of most head and neck cancers that spread through the lymphatics, which include most of these cancers. The fields that encompass the group are commonly called posterior cervical strips.
Surface and Sectional Anatomy and Landmarks of the Thorax and Breast
Various malignant diseases manifest themselves in the human thorax. Cancers of the lung, breast, and mediastinal lymphatics require the radiation therapist to have a working knowledge of the surface and sectional anatomy of the thorax. The human thorax has various anatomic features that are commonly used in field placement, position locations, and so forth. The thorax extends from the clavicles superiorly to the costal margin inferiorly.

Figure 20-30 Surface anatomy of the female breast. This gland is teardrop-shaped with a portion that extends from the anterior chest wall into the axilla.
Anterior Thoracic Landmarks
The clavicles are visible throughout their entire length in the anterior thorax, especially in the asthenic body habitus. The clavicles are easily palpable. The radiation therapist uses the clavicles when outlining a field to treat the lower neck and upper chest lymphatics. The supraclavicular lymph nodes are located superior to the clavicles; they are often treated prophylactically in head and neck and lung cancers. In addition, the brachial plexus, a network of nerves located at the medial section of the clavicle and often involved in superior sulcus (Pancoast) tumors of the lung, can be referenced to this point.
The musculature of the anterior chest wall includes the pectoralis major, pectoralis minor, and deltoid. The pectoralis major is medially attached to the clavicle and superior five costal cartilages. It passes laterally to the axilla. The inferior border of the muscle is not as visible in the female adult because it is covered by the breast.1,2 The pectoralis minor is overlapped by the pectoralis major. The deltoid muscle forms the rounded portion of the shoulder.
The Breast and Its Landmarks
The male breast remains poorly developed throughout life, whereas the female breast develops to a variable degree during puberty. Although the sizes of the female breasts vary, they typically lie between the second rib superiorly and the sixth rib inferiorly. The female breast is shown in Figure 20-30. The medial border is the lateral aspect of the sternum, and the lateral border corresponds to the midaxilla. The breast tissue is teardrop shaped; the round, drop portion is situated medially, and the upper outer portion, called the tail of Spence, extends into the axilla. The upper limits of tangential treatment fields are typically high near the SSN, to include the entire breast and tail of Spence when the SCF is not treated.

Figure 20-31 Computed tomographic scan view of the female breast and thorax. The contours of the breast and chest wall from images like this greatly enhance accuracy of treatment planning. Note how tumor volume can easily be related to other internal anatomy.
The breast can be divided into quadrants: upper outer, upper inner, lower outer, and lower inner. Most tumors are located in the upper outer quadrant of the breast. Tumor location is important in associating the tumor spread patterns. If the breast tumor is located in an inner quadrant, the medially located nodes, such as the internal mammary nodes, may be involved. If the tumor is located in an outer quadrant, the axillary nodes need to be examined for possible involvement. This information is particularly important to the therapist because tumor location and extension dictate field parameters.
Other surface anatomy of the breast includes the nipple, areola, and inframammary sulcus. The nipple projects just below the center of the breast. In the male, the nipple lies over the fourth intercostal space; the location varies in the female. The areola is the area that surrounds the nipple. Its coloration changes with varying hormonal levels, as seen in pregnancy. The inframammary sulcus, the inferior point of breast attachment, varies from person to person. In females with large breasts, the breast overhangs this point of attachment and causes considerable concern during its external beam treatment because the breast can bolus itself in these cases.
Radiographically, the breast produces shadows that are easily seen on conventional radiographs. Figure 20-31 shows a CT scan slice through a section of the thorax and breast. Note how the patient’s internal anatomy can be related to the contour of the breast. This information is useful in treatment planning.
Posterior Thoracic Landmarks
The posterior thorax is formed by the structures commonly referred to as the back. On initial inspection, the back is made up of various muscles and bony landmarks. The major musculature includes the trapezius, teres major, and latissimus dorsi. The trapezius muscle is a flat triangular muscle that produces a trapezoid shape with the lateral angles at the shoulders and the superior angle at the EOP. The inferior angle is at the level of T12. The teres major is a band of muscle between the inferior angle of the scapula and the humerus; it forms the posterior wall of the axilla. The latissimus dorsi is the broad muscle on either side of the back that spans from the iliac crest of the pelvic bones to the posterior axilla.1,2,11,12 Figure 20-32 shows the surface anatomy of the posterior thorax.
The spines of the thoracic vertebrae slope inferiorly; the tips lie more inferior than the corresponding vertebral bodies and are easily palpable. The scapula, the large posterior bone associated with the pectoral girdle, is easily palpated on the back. The spine of the scapula is located at the level of T3. The inferior angle of the scapula is located at the level of T7.
The lower back has a few bony landmarks that serve the radiation therapist well. The crest of the ilium is located at the level of L4. This point is important in locating the subarachnoid space, the point at which lumbar punctures are commonly made. The posterosuperior iliac spine (PSIS) is approximately 5 cm from midline, is easily palpable, and lies at the level of S2.
Internal and Sectional Anatomy of the Thorax
Bone detail can easily be visualized with CT scan sections. MRI shows soft tissue anatomy not clearly seen with conventional x-ray equipment. Fascial planes are identified, which allows separation of organ systems, vascular supply, muscles, bone, and lymphatic system.4,13,14 The thorax provides much anatomic information that the radiation therapist uses in the daily administration of ionizing radiation.
The trachea is the part of the airway that begins at the inferior cricoid cartilage, at the level of C6. It is approximately 10 cm long and extends to a point of bifurcation, called the carina, at the level of T4-T5. Topically, it corresponds to the angle of Louis (Figure 20-33). The bifurcation forms the beginning of the right and left main bronchi, which can assist the therapist in locating the initial location of treatment field borders, especially lung cancer fields whose inferior border commonly lies a few centimeters below this anatomic reference point.
The diaphragm is the dome-shaped muscle that separates the thorax and abdomen. It is important in respiration and lies between T10 and T11. The esophagus and inferior vena cava pass through the diaphragm at the level of T8-T9, whereas the descending aorta goes through at the level of T11-T12. These features are shown in cross section in Figure 20-34.
The pleural cavity extends superiorly 3 cm above the middle third of the clavicle. The anterior border of the pleural cavity reaches the midline of the sternal angle. The pleura are more extensive in the peripheral regions around the outer chest wall. The diaphragm bulges up into each pleural cavity from below. The pleura mark the limit of expansion of the lungs.1,2
The lungs correspond closely with the pleura, except in the inferior aspect, where they do not extend down into the lateral recesses. The anterior border of the right lung corresponds to the right junction of the costal and mediastinal pleura down to the level of the sixth chondrosternal joint. The anterior border of the left lung curves away laterally from the line of pleural reflection. The surface projection of the lung and pleura is noted in Figure 20-35.

Figure 20-33 This x-ray image shows the trachea and its distal bifurcation, the carina. The branching typically occurs at T3-T4.
The heart rests directly on the diaphragm in the pericardial cavity and is covered anteriorly by the body of the sternum. The base of the heart lies at the level of T4. A cardiac shadow can clearly be seen in a radiograph of the chest.
Associated with the thorax and heart are an abundance of arteries and veins—the great vessels. The aorta has ascending and descending components. The ascending aorta runs from the aortic orifice at the medial end of the third left intercostal space up to the second right chondrosternal joint. This arch continues above the right side of the sternal angle and then turns down behind the second left costal cartilage. The descending aorta runs down behind this cartilage, gradually moving across to reach a point just to the left of midline, approximately 9 cm below the xiphisternal joint where it enters the abdomen. The innominate left common carotid and left subclavian arteries extend from this aortic arch. The superior vena cava is located at the level of T4. It runs down through the pericardium, where it enters the heart. The inferior vena cava does not extend a great distance in the thorax; it lies in the right cardiodiaphragmatic angle and enters the heart behind the sixth right costal cartilage.
Lymphatics of the Breast and Thorax
The lymphatic drainage of the thorax and breast is important to the radiation therapist. The thorax is rich in lymphatic vessels. The lymphatics of the axilla, SCF, and mediastinum play a major role in radiation therapy field arrangement of breast, head and neck, lung, and lymphatic cancers. The lymph nodes of the thorax are divided into nodes that drain the thoracic wall and breast and those that drain the thoracic viscera.
Breast Lymphatics
Three lymphatic pathways are associated with the breast: the axillary, transpectoral, and internal mammary pathways. These pathways are the major routes of lymphatic drainage for the breast. Specific lymph node groups are associated with each pathway and are shown in Figure 20-36.
The axillary lymphatic pathway comes from trunks of the upper and lower half of the breast. Lymph is collected in lobules that follow ducts, which anastomose behind the areola of the breast; from that point, they drain to the axilla. This pathway is also referred to as the principal pathway. The nodes of this pathway drain the lateral half of the breast. These nodes are important to note in invasive breast cancers: axillary nodes are commonly biopsied for assessment of disease spread. The axillary lymph nodes are commonly at the level of the second to third intercostal spaces and can be divided into low, mid, and apical axillary nodes.
The transpectoral lymphatic pathway passes through the pectoralis major muscle and provides efferent drainage to the supraclavicular and infraclavicular fossa nodes. One of the intermediate nodes in the infraclavicular fossa worth noting is Rotter’s node. Nodes of the SCF and low neck, generally 1 to 3 cm deep, are often treated when there is involvement of the transpectoral pathway. The scalene node, found in the low neck/SCF, is often biopsied to note disease spread.
The internal mammary lymphatic pathway runs toward the midline and passes through the pectoralis major and intercostal muscles close to the body of the sternum (T4 to T9). Associated with this pathway are the internal mammary nodes. These nodes are more commonly involved with primary breast cancers that are located in the inner breast quadrants and with positive axillary nodes. These nodes are generally 2.5 cm from midline (with variations from 0 to 5 cm) and are approximately 2.5 cm deep (with variations from 1 to 5 cm). CT scans are extremely helpful to the radiation oncology team in assessment of the location of these nodes. The lateral location and depth assist in determination of the field width and treatment energy, respectively.
Breast lymphatic flow is also important from a surgical standpoint. With radical breast surgery, lymphatic flow is often compromised. Because the channels of flow are altered with surgical intervention, the lymph has fewer drainage paths back to the cardiovascular system. This slowed drainage causes edema that is sometimes seen in the arms of patients who have received radical breast surgery. Exercise and elevation of the limb help drain stagnant lymph. This complication has led the cancer management team to use less radical surgery when possible, along with other modalities.
Thoracic Lymphatics
The mediastinum has a rich intercommunicating network of lymphatics. The most important nodes to note are the lymphatics of the thoracic viscera and pulmonary veins. They are commonly involved in Hodgkin disease and in lung cancers, in which they can be radiographically seen as a widened mediastinum. The lymphatics of the lung and mediastinum are shown in Figure 20-37.
The superior mediastinal nodes are located in the superior mediastinum. They lie anterior to the brachiocephalic veins, the aortic arch, and the large arterial trunks that arise from the aorta. They receive lymphatic vessels from the thymus, heart, pericardium, mediastinal pleura, and anterior hilum. The tracheal nodes extend along both sides of the thoracic trachea and are also called the paratracheal nodes. The superior tracheobronchial nodes are located on each side of the trachea. They are superior and lateral to the angle at which the trachea bifurcates into the two primary bronchi.

Figure 20-36 The lymphatic pathways associated with the breast: axillary, transpectoral, and internal mammary.
The inferior mediastinal nodes are located in the inferior mediastinum. The inferior tracheobronchial nodes lie in the angle below the bifurcation of the trachea. They are also called the carinal nodes. The bronchopulmonary nodes, often called the hilar nodes, are found at the hilus of each lung, at the site of the division of the main bronchi and pulmonary vessels into the lobular bronchi and vessels. These nodes are involved in most lung cancer cases. The pulmonary nodes, also known as the intrapulmonary nodes, are found in the lung parenchyma along the secondary and tertiary bronchi.
In the right lung, all three lobes drain to the intrapulmonary and hilar nodes. They then flow to the carinal nodes and then to the paratracheal nodes before they reach the brachiocephalic vein through the scalene node and right lymphatic duct. In the left lung, the upper lobe drains to the pulmonary and hilar nodes, carinal nodes, left superior paratracheal nodes, and then the brachiocephalic vein through the thoracic duct. The left lower lobe drains to the pulmonary and hilar nodes, then to the right paratracheal nodes, where it follows the path outlined for the right lung. This is important when designing the treatment field of a patient with lung cancer.
Surface and Sectional Anatomy and Landmarks of the Abdomen and Pelvis
The abdomen and pelvis house many organs that are treated for malignant disease. Management presents treatment planning challenges for the radiation therapist and medical dosimetrist because of the abundance of radiosensitive structures within the abdominal and pelvic cavities. Treatment of a colorectal cancer to a dose of 60 Gy or more can be difficult when the neighboring anatomy tolerates much less. Knowledge of surface and cross-sectional anatomy of the abdomen and pelvis is essential in radiation therapy. The radiation therapist must be able to bridge knowledge of surface and sectional anatomy with various body habitus to visualize internal anatomy. However, relating internal structures to the topography of the area is not without certain challenges, particularly in the anterior abdomen. When compared with the head, neck, and thorax, the anterior abdomen does not have as many bony landmarks to reference. However, some stable bony landmarks in the pelvis are commonly referenced.

Figure 20-38 The muscles of the anterior and lateral abdominal wall work in unison to provide structure and stability to the torso.
Anterior Abdominal Wall
The anterior abdominal wall is bordered superiorly by the inferior costal margin and inferiorly by the symphysis pubis, inguinal ligament, anterosuperior iliac spine (ASIS), and iliac crest. The anterior aspect of the wall is formed by sheets of interlacing muscles that provide stability and form to the abdomen. The major muscles that help form the anterior abdominal wall include the rectus abdominis, transverse abdominis, internal oblique, and external oblique.
The external oblique muscle extends from the lower eight ribs to an insertion point that spans from the iliac crest to the midline aponeurosis, a sheet-like tendon that joins one muscle to another. It extends from the outer lateral body to the midline.
The internal oblique muscle spans from the iliac crest and inguinal ligament to the cartilage of the last four ribs. It runs in a midline to an outer lateral perspective.
The transverse abdominis muscle runs from the iliac crest, inguinal ligament, and last six rib cartilages to the xiphoid process, linea alba (a tough fibrous band that extends from the xiphoid process to the symphysis pubis), and pubis on both sides. Thus, this muscle runs from side to side.
The rectus abdominis muscle is commonly called the “six pack” by sports buffs. This muscle runs from the symphysis pubis to the xiphoid process and has three transverse fibrous bands that separate the muscle into six sections that are prominent in individuals with pronounced muscular tone.
These muscles work together in providing structure to the anterior abdominal wall. Figure 20-38 shows the interrelated nature of these muscles.
A number of structures can be palpated in the abdomen. The xiphoid process lies in the epigastric region at the level of T9. This bony landmark is very stable. The radiation therapist typically uses this structure and the SSN to ensure that a patient is lying straight on the treatment couch. If both landmarks are in line with the projection of a sagittal laser, the thorax is usually straight. The xiphoid can also be used in conjunction with the symphysis pubis or associated soft tissue landmarks to ensure that the lower body is straight. The cartilages of the 7th to 10th ribs form the costal margin, which forms the inferior border of the rib cage. The umbilicus, also known as the navel or belly button, is an inconsistent, mobile landmark on the anterior abdomen. It is typically at the level of L4 when an individual is in a recumbent position. When standing, in the infant, and in the pendulous abdomen, it lies at a lower level.
Posterior Abdominal Wall (Trunk)
In the posterior wall, the lower ribs, lumbar spines, PSIS, and iliac crest are palpable. A line, called the intercristal line, can be drawn between the iliac crests.1 This line typically passes between the spines of the third and fourth lumbar vertebrae, a location important in lumbar punctures.
Landmarks of the Anterior Pelvis
The anterior pelvis has several bony and soft tissue landmarks that are useful to the radiation therapist. They are outlined in the following section and shown in Figure 20-39.
The iliac crest extends from the ASIS to the PSIS. The ASIS is palpable, and measurements may be taken from it in the superoinferior or mediolateral direction. It is often used in referencing the location of the femur. The lateral iliac crest is also easily palpable and, being on the lateral pelvic wall, may be used as a transverse level on either the anterior or the posterior pelvis. The lateral iliac crest level is the line that joins the right and left lateral iliac crests. These crests are the most superior margin of the ilium on the lateral pelvic wall. Measurements may be taken from this level in the superoinferior direction.
The head of the femur and greater trochanter, although not direct components of the true pelvis, are important to note when considering the lateral pelvic anatomy. The head of the femur articulates with the hip at the acetabulum. If this is irradiated beyond tolerance, fibrotic changes can occur and cause painful or limited motion of the joint. Usually this joint is shielded in moderate to large pelvic portals to limit this occurrence. The greater trochanter is the only part of the proximal femur that can be palpated; therefore, its relationship to bony points of the hip bone is important.6 The radiation therapist uses the greater trochanter when aligning patients during simulation to alleviate pelvis rotation. The patient should be horizontally level when the greater trochanters are at the same height from the tabletop. The radiation therapist can measure this with a ruler and optical lasers.
The symphysis pubis appears as the 5-mm midline gap between the inferior parts of the pelvic bones.2 The upper border pubis is the palpable upper border of the midline pubic bone. It is fairly easy to palpate, except in extremely obese patients. When it is palpated, care should be taken to allow for overlying tissue. The lower border pubis is the palpable lower border of the pubic bone in midline. It is not as easily palpable as the upper border pubis because it lies more inferiorly and posteriorly. All of these can be accurately located radiographically. The radiation therapist uses these components when setting the anterior border of lateral prostate fields (the prostate lies immediately posterior to the symphysis pubis).
The ischial tuberosities are located in the inferior portion of the pelvis. This corresponds to the lower region of the buttock. When a person sits down, the ischial tuberosities bear the weight of the body. Many radiation oncologists use the ischial tuberosities as the inferior border of the anterior and posterior prostate treatment portals.
When pelvic irradiation is indicated, the radiation therapist can use the anatomy of the perineum, the diamond-shaped area bounded laterally by the ischial tuberosities, anteriorly by the symphysis pubis, and posteriorly by the coccyx, to assist in portal location. Treatment lines in these areas commonly fade because of perspiration and garment rubbing.6 Knowledge of the area can thus provide a practical means of field verification. Both male and female anatomies have useful landmarks.
The anterior commissure of the labia majora is easily distinguishable in the female. It is an important soft tissue landmark because it is used as a reference point from which the upper or lower border pubis is measured. Thus, checking back to this soft tissue landmark may eliminate variations in the palpation of the pubic bone.
The base of the penis is taken as the line that joins the anterior skin of the penis with the skin of the anterior pelvic wall. This level is used as a reference point from which the upper or lower border pubis is measured in the male. A therapist may measure changes in the lateral position of prostate fields by referencing appropriate measurements from the base of the penis.
Landmarks of the Posterior Pelvis
The most commonly used bony surface landmarks of the posterior pelvis are the PSISs, the coccyx, the iliac crests, and the lateral iliac crests. Because the latter two were also mentioned in the previous section, only the PSIS and coccyx are discussed here. The PSISs are indicated by dimples above and medial to the buttock, approximately 5 to 6 cm from the midline. They are palpable, and measurements may be taken in the superoinferior or mediolateral direction. The coccyx lies deep to the natal cleft with its inferior end approximately 1 cm from the anus.
Abdominopelvic Viscera
The organs of the abdomen and pelvis can be visualized with various means. Radiographs, CT, MRI, and US are commonly used to provide information concerning organ location. Note that the location of any organ in the abdomen and pelvis can vary with respiration, anatomic position, and level of fullness, which is why placement of radiation therapy patients in a reproducible position that limits movement daily is extremely important. As observed previously, body habitus affects the location of internal organs. This holds true for the abdomen and pelvis as well. This section examines the location of the abdominal and pelvic viscera.
Location of the Alimentary Organs
The esophagus begins at the lower border of the cricoid cartilage in the neck and travels through the diaphragm to the cardiac sphincter, the entrance to the stomach, at the level of T10 approximately 2 to 3 cm to the left of midline. For radiographic visualization of the esophagus, the patient commonly is instructed to swallow a radiopaque substance such as barium before examination.
The duodenum, a C-shaped section of the small bowel approximately 25 cm in length, starts to the right of midline at the edge of the epigastric region. The stomach lies between the duodenum and the distal esophagus and is of variable size and location, partly covered by the left rib cage and filling the epigastric region. The root of the small gut mesentery, made up of sections called the jejunum and ileum, extends from the duodenum to the inlet to the large bowel.1,2
The start of the large bowel is the cecum. It lies in the right iliac region at the level of L4. The ascending colon (15 cm in length) and hepatic flexure of the colon on the right side and the splenic flexure and descending colon (25 cm in length) on the left side are largely retroperitoneal structures, whereas the transverse and sigmoid colon have a mesentery and vary in their position from one person to the next.1,2 However, similarities are found within common body habitus. The rectum starts at the level of S3 and ends approximately 4 cm from the anus. It is one of the dose-limiting structures when prostate treatment fields are outlined. Rectal visualization is thus important during the simulation process.
Figure 20-40 delineates the surface projections of the alimentary tract in the abdomen and pelvis.
Location of Nonalimentary Organs
The radiation therapist benefits from a working knowledge of the nonalimentary organs of the abdomen and pelvis. Many times these organs are involved in malignant processes and must be included in the patient’s treatment scheme. Figure 20-41 shows the surface projections of the organs outlined here.
The liver is an irregularly shaped organ located in the right hypochondriac region of the abdomen above the costal margin. The superior margin of the liver, which bulges into the diaphragm, is at the level of T7-T8. The liver is commonly imaged with CT scan, US, and nuclear medicine studies.
The gallbladder is located below the lower border of the liver and contacts the anterior abdominal wall where the right lateral border of the rectus abdominis crosses the ninth costal cartilage. This location is called the transpyloric plane. Again, US is useful in distinguishing biliary obstructions and gallstones.
The spleen, mentioned previously as a lymph node for the blood, is located posteriorly approximately 5 cm to the left of midline at the level of T10-T11. The healthy organ lies beneath the 9th through 11th ribs on the left side of the body. This organ is often examined surgically in patients with lymphoma to determine disease extension. If the organ is removed for biopsy, the splenic pedicle, the point of attachment of the organ to its vascular and lymphatic connections, is included in the abdominal treatment field for Hodgkin disease.
Three components, the head, body, and tail, compose the pancreas. The head of the pancreas is located in the C section of the duodenum. The body extends slightly superiorly to the left across midline, at the level of L1. The tail of the pancreas passes into the hilum, a concave point of an organ that has vascular inlets and outlets, of the spleen.
Location of the Urinary Tract Organs
The kidneys lie on the posterior abdominal wall in the retroperitoneal space. The hilum of the right kidney is at the level of L2, whereas the hilum of the left is at the level of L1. The right kidney lies lower than the left because of the presence of the adjacent liver. Superior and medial to each kidney are the adrenal glands. The kidneys are generally not fixed to the abdominal wall; they can move as much as 2 cm with respiration. When the radiation therapist outlines the location of these radiation-sensitive structures, this movement is important to take into account.
The ureters are tubular structures that transport urine from the kidneys to the urinary bladder. They run anterior to the psoas muscles and enter the pelvis lateral to the sacroiliac (SI) joint. The ureters, as well as the kidneys, are commonly imaged with CT scan, US, and intravenous and retrograde studies.
The urinary bladder is located in the pelvis. The neck of the bladder lies posterior to the symphysis pubis and anterior to the rectum. This organ also lies immediately superior to the prostate in the male. The urinary bladder is a dose-limiting structure in the treatment of prostatic cancer. It is commonly visualized with contrast agents during the simulation process.
The topographic relations of the urinary tract organs are shown in Figure 20-42.
Lymphatics of the Abdomen and Pelvis
The lymphatic drainage routes for the abdomen and pelvis are important to the radiation therapist. An abundance of lymphatic vessels is found in this section of the body. Those of the retroperitoneum and pelvis play a major role in radiation therapy field arrangement of gynecologic, genitourinary, and lymphatic cancers. Figures 20-43 and 20-44 show the nodes and nodal groups outlined here.
The lymphatic pathways and nodes of the abdomen are often referred to as the visceral nodes because they are closely associated with the abdominal organs. The three principal groups of nodes of the abdomen that drain the corresponding viscera before entering the cisterna chyli or the thoracic duct are the celiac, superior mesenteric, and inferior mesenteric groups, also called the preaortic nodes.
The celiac nodes include the nodes that drain the stomach, greater omentum, liver, gallbladder, and spleen and most of the lymph from the pancreas and duodenum. The superior mesenteric nodes drain part of the head of the pancreas; a portion of the duodenum; the entire jejunum, ileum, appendix, cecum, and ascending colon; and most of the transverse colon. The inferior mesenteric nodes drain the descending colon, the left side of the mesentery, the sigmoid colon, and the rectum.
The posterior abdominal wall has a rich network of lymphatic vessels. The para-aortic nodes provide efferent drainage to the cisterna chyli, which is the beginning of the thoracic duct. These nodes run adjacent to the abdominal aorta from T12 to L4. This major section of the lymphatic system eventually receives lymph from most of the lower regions of the body. The para-aortics directly drain the uterus, ovary, kidneys, and testicles. An interesting note is that embryonically the testes develop near the kidneys and descend into the scrotum after birth. As they descend, they take the vascular and lymphatic vessels with them as direct means for blood and lymph flow.
The common iliac nodes lie at the bifurcation of the abdominal aorta at the level of L4. These nodes directly drain the urinary bladder, prostate, cervix, and vagina. This chain moves laterally and breaks up into the external and internal iliac nodes. The external iliac nodes drain the urinary bladder, prostate, cervix, testes, vagina, and ovaries. The internal iliac nodes, also known as the hypogastric nodes, drain the vagina, cervix, prostate, and urinary bladder. These nodes are more medial and posterior to the external iliac nodes previously mentioned.
The inguinal nodes are more superficial than the previously mentioned nodes. These nodes directly drain the vulva, uterus, ovaries, and vagina. These nodes are commonly treated with electrons because of their superficial location.
Applied Technology
Practical application of the material presented in this chapter is important. To enhance the comprehensive understanding of the relationships presented, the last section of this chapter presents diagrams that relate structures to vertebral body levels and CT scans through the head, neck, thorax, abdomen, and pelvis. The appropriate structures pertinent to the radiation oncology practitioner are shown. Figures 20-45 through 20-49 show these diagrams and scans.

Figure 20-46 Major lymph nodes of the abdomen and pelvis: 1, Preauricular; 2, mastoid; 3, occipital; 4, upper cervical; 5, parotid; 6, submaxillary; 7, submental; 8, jugulodigastric; 9, upper deep cervical; 10, spinal accessory chain; 11, infrahyoid; 12, pretracheal; 13, jugulo-omohyoid; 14, lower deep cervical; 15, supraclavicular; 16, mediastinal; 17, interlobar; 18, intertracheal; 19, posterior mediastinal; 20, lateral pericardial; 21, diaphragmatic; 22, mesenteric; 23, para-aortic; 24, common iliac; 25, lateral sacral; 26, external iliac; 27, hypogastric; 28, inguinal; 29, interpectoral; 30, axillary apex; 31, axillary; 32, cisterna chyli; 33, splenic; 34, femoral; 35, epitrochlear.

Figure 20-47 A, Sectional computed tomographic scan views of the thorax with labeled anatomy (B). ACA, Ascending aorta; A/C art, acromial clavicular articulation; CA, carotid artery; CL, clavicle; C/M art, clavicular macrobial articular; DCA, descending aorta; E, esophagus; GF, glenoid fossa; HH, humeral head; LCCA, left common carotid artery; LSA, left subclavian artery; RBA, right bronchocephalic artery; Rib/V art, rib/vertebral artery; SC, scapula; SP, spinous; ST, sternum; T, trachea; V, vein; VB, vertebral body.

Figure 20-48 A, Sectional computed tomographic scan views of the abdomen with labeled anatomy (B). A, Aorta; DCA, descending aorta; GB, gallbladder; K, kidney; L, liver; S, splecen; SB, small bowel; SC, spinal cord; SP, spinous process; VB, vertebral body.


Figure 20-49 A, Sectional computed tomographic scan view of the male pelvis with labeled anatomy (B). A, Acetabulum; AS, axial sphincter; AV, anal verge; B, bladder; C, coccyx; FH, femoral head; FN, femoral neck; FS, femoral shaft; GT, greater tuberosity; I, ischium; P, prostate; R, rectum; S, sacrum; SB, small bowel; SP, symphysis pubis; SV, seminal vesicles. C, Sectional CT scan view of the female pelvis with labeled anatomy (D). A, Acetabulum; B, bladder; C, cervix; CX, coccyx; DS, descending sigmoid; EL, external iliac; FA, femoral artery; FH, femoral head; FN, femoral neck; FS, femoral shaft; GT, greater tuberosity; I, ilium; IL, internal iliac; ISH, ischium; P, pubis; R, rectum; SM, small intestine; SP, symphysis pubis; U, uterus; V, vagina.
Summary
• Radiation therapy requires its practitioners to have a keen knowledge and understanding of surface and sectional anatomy.
• The complex simulation procedures and planning used in patient treatment mandate strict attention to detail.
• The radiation therapist must use information provided by several imaging modalities to achieve the ultimate goal: administration of a tumoricidal dose of radiation to the tumor and tumor bed with as much normal tissue spared as possible.
• The lymphatic vessels play a major role in treatment field delineation and disease management.
• The complexity of radiation therapy requires the radiation therapist to use all available means to function effectively. All therapists should review their practical skills in surface and sectional anatomy because they are crucial for accurate treatment planning and delivery.
• For patients to completely benefit from the new technology in radiation therapy, the radiation therapist must have a strong anatomic base that allows effective treatment delivery.
• Medical imaging greatly assists not only in targeting but also in promoting greater treatment delivery options through more precise and exacting means.
• Body habitus knowledge helps the radiation therapist quickly locate treatment areas and relate internal structure location as related to body type. Knowledge of how the human body varies is essential to effective practice.
• The lymphatic system and its related components depict possible routes of tumor spread. The system’s one-way flow makes the spread patterns predictable. Closely associated with neighboring structures and the cardiovascular system, the lymphatic channels and extent of their involvement in a cancer diagnosis are essential in the radiation treatment field design and delivery.
• Anatomic landmarks are important tools in locating and recalling treatment areas. Two types of landmarks should be considered: bony and soft tissue. Although all provide useful information, the bony landmarks are more stable and more predictably referenced. Soft tissue landmarks are useful in locating general areas but may not be as exact in comparison.