Chapter 9 Ethics and professional practice
Mastery of content will enable you to:
• Discuss the key terms listed and their relevance to guiding ethical professional conduct in nursing domains.
• Discuss the importance of ethics to, and in, the profession and practice of nursing.
• Critically examine what constitutes ethical professional practice.
• Discuss the notions of moral accountability and responsibility.
• Identify different moral theories that may guide ethical professional conduct.
• Examine the nature and authority of nursing codes of ethics.
• Outline 10 moral problems that may arise in nursing and healthcare contexts.
• Discuss how moral problems can be distinguished from non-moral problems.
• Discuss five steps that may be taken to identify and deal with moral problems arising in practice contexts.
• Apply one systematic model of moral decision making to a clinical situation.
• Discuss critically at least six ethical issues of importance to the nursing profession.
When people enter the nursing profession they are required to make a commitment to upholding exemplary standards of ethical conduct—that is, standards that are above what would normally be expected of the ‘ordinary person in the street’. The ethical standards that nurses are expected to uphold are prescribed in various codes of ethics, codes of conduct, and competency standards which have been developed and published by recognised professional nursing organisations. Some examples can be found in the codes of ethics and codes of conduct published respectively by the International Council of Nurses (ICN, 2006), the Nursing and Midwifery Board of Australia (NMBA) (Australian Nursing and Midwifery Council, 2008a, 2008b), the New Zealand Nurses Organisation (NZNO, 2010), the Nursing Council of New Zealand (NCNZ, 2009) and other similar bodies (Box 9-1).
BOX 9-1 WEBSITE ADDRESSES FOR LOCATING NURSING CODES OF ETHICS AND CODES OF CONDUCT
AHPRA NURSING AND MIDWIFERY BOARD OF AUSTRALIA (ANMC)
www.nursingmidwiferyboard.gov.au/codes-and-guidelines.aspx
ANMC (2008) Code of ethics for nurses in Australia
ANMC (2008) Code of professional conduct for nurses in Australia
ANMC (2006) National competency standards for the registered nurse
ANMC and NCNZ (2010) A nurse’s guide to professional boundaries
In addition to being expected to uphold exemplary standards of ethical professional conduct, nurses are required to also be able to identify and respond effectively to a wide range of ethical issues that may, and do, arise in nursing care and related healthcare contexts. How well nurses are able to respond to these requirements, however, will depend on their knowledge and understanding of what ethics is and how it can best be practised in a culturally, socially and geographically diverse world. Consider the case scenario in the clinical example below.
Both the Code of ethics for nurses in Australia (Australian Nursing and Midwifery Council, 2008a) and the NZNO (2010) Code of ethics explicitly require nurses to respect the needs, values, culture and vulnerability of people in the provision of nursing care and to ensure that the care provided to patients is culturally informed, safe and appropriate. However, the Codes also require nurses to ‘accept the rights of individuals to make informed choices in relation to their care’. In Mr G’s case it seems that these two requirements clash, raising the important question of what the right thing to do is in this and similar scenarios (see also Johnstone, 2011a). When, if ever, should a family’s pleas be taken into consideration in determining when (if at all), where, how and by whom a cancer diagnosis and poor prognosis should be disclosed to a client? How are nurses and other members of the healthcare team to decide these things? Moreover, do they have the cultural competence necessary to enable them to engage in moral decision-making processes in a safe and effective way? In the case of the NZNO Code of ethics another ethical dimension is added, since this Code also prescribes that nurses must recognise that many sociocultural groups ‘place the importance of the collective on a par with the needs and rights of the individual’ and that the rights of ‘both the individual and the collective must be respected’ (New Zealand Nurses Organisation, 2010:12).
THE CASE OF ‘MR G’
‘Mr G’, a 69-year-old Greek-born man who had migrated to Australia from rural Greece and who spoke little English, was admitted to a major metropolitan hospital for follow-up assessment and treatment of a cancer-related illness. Unfortunately, test results revealed that his condition had unexpectedly worsened, that his prognosis was poor and that palliative care was his best option. Upon learning of this bad news, Mr G’s family pleaded with the attending doctor not to tell their father that his medical condition had worsened and that his prognosis was poor. Mr G’s eldest daughter explained to the doctor that were he to tell Mr G that his cancer had spread, ‘this would destroy his hope and affect his quality of life’. She further explained that, in their Greek culture, ‘it was wrong to tell someone they had terminal cancer’. The doctor objected to the daughter’s request, however, arguing that the matter was ‘not about culture, but about ethics’ and that her father ‘had a right to know’. (Johnstone, 2009a, 2011a)
Being able to respond to this and other kinds of case scenarios in a morally just, responsible and competent way requires nurses to have at least a working knowledge and understanding of:
• key terms and concepts commonly used in discussions on ethical issues in nursing practice
• the importance of ethics to the profession and practice of nursing
• what constitutes ethical professional practice
• notions of moral accountability and responsibility
• reliable guides to ethical professional conduct
• key moral theories that are commonly used to guide ethical decision making and practice in nursing (including cross-cultural ethics)
• the nature and authority of nursing codes of ethics
• the kinds of moral problems that can and do arise in nursing and healthcare domains
• how moral problems can be distinguished from other kinds of problems (e.g. legal problems)
• processes for identifying and dealing with moral problems arising in practice contexts
• moral decision making in practice contexts
• bioethical issues of importance to the nursing profession.
Without the requisite knowledge and understanding of these things, it would be very easy for nurses to ‘rush to judgment’ when engaged in moral decision making and, as a consequence, make moral mistakes. If moral mistakes are made, this can result in morally significant harm to patients, their loved ones and also to healthcare providers. It is for this reason that nurses must make every effort, individually and collectively, to ensure that they are adequately prepared to deal with the moral complexities and quandaries that are likely to arise in their practice and places of work.
Terms and concepts
To be able to discuss ethical issues in nursing in a meaningful way, it is important to have an understanding of such key terms and concepts as ethics, morality, bioethics, nursing ethics, moral principles, moral rules, moral rights and moral duties.
Ethics and morality
Ethics (which may be used interchangeably with the term ‘moral’) is a general term used for referring to various ways of understanding and examining the ‘moral life’ (Beauchamp and Childress, 2009). More specifically, ethics involves thinking critically about and engaging in a systematic examination of what constitutes right and wrong/good and bad behaviour, and the bases upon which we might justify our judgments that an action or decision is ‘morally right or wrong’, all things considered. For example, a nurse may make the moral judgment that abortion is wrong and conscientiously object to assisting with an abortion procedure. Whether conscientious objection ought to be permitted, however, requires a critical examination of the bases on which the nurse has made that judgment, and the provision of sound (moral) justifications (reasons) for the action taken. Ethics, then, is concerned not just with giving values to certain things (e.g. abortion is right/wrong, good/bad), but also with justifying the bases on which judgments about these things might be made (Johnstone, 2009a; Kerridge and others, 2009; LaFollette, 2007).
It is important to clarify the use of the term ‘morality’ in discussions on ethics. In some nursing texts, the terms ‘ethics’ and ‘morality’ are treated as though they refer to different things. This use, however, is not correct. There is, in fact, no philosophically significant difference between the terms ‘ethics’ and ‘morality’, and hence they may be used interchangeably. The only distinction that may be drawn with validity between these two terms is that the word ‘ethics’ comes from the Greek ethikos (originally meaning custom or habit), and ‘morality’ from the Latin moralitas (also originally meaning custom or habit) (Johnstone, 2009a). Of course, today these terms refer to something much more sophisticated than merely custom or habit, as this chapter will show.
Bioethics
The term bioethics (from the Greek bios meaning life, and ethikos, ithiki meaning ethics)—literally, ethics in the realm of life—is a relatively new term that first found its way into public use in the early 1970s in the United States (Reich, 1994). Although the term was originally defined to include environmental concerns, as it is used today its main focus is on (Reich, 1995):
• the rights and duties of clients and healthcare professionals
• the rights and duties of research participants and researchers
• the formulation of public policy guidelines for clinical care and biomedical research.
Although originating in the United States, bioethics has developed as a discipline in its own right in countries around the world; it has also developed as a major international movement of popular interest to professionals and laypersons alike. Today, issues most commonly the subject of bioethics debate in professional journals, as well as in the mass circulation media, include:
• euthanasia and medically assisted suicide
• reproductive technology (including in vitro fertilisation, genetic engineering, surrogacy, embryonic and stem cell research)
• clients’ rights to privacy and confidentiality
• the economic rationalisation of healthcare
• research ethics (see Jecker and others, 2011; Jonsen and others, 2010).
Nursing ethics
Contemporary nursing ethics has been profoundly influenced by the modern bioethics movement and, in several respects, could even be described as a subcategory of bioethics; that is, nursing bioethics. Despite this modern influence, it is important to acknowledge that the nursing profession has its own rich and distinctive history of identifying and responding effectively to ethical issues in nursing and healthcare. In addition to having its own distinctive history of professional ethics, nursing can be said to have developed its own distinctive (nursing) ethics. This development not only has been necessary, but also was inevitable. It has been necessary because ‘a profession without its own distinctive moral convictions has nothing to profess’ and will be left vulnerable to the corrupting influences of whatever forces are more powerful (be they social, political, legal or other in nature) (Churchill, 1989). Furthermore, as Churchill (1989) has asserted in his classic article on the subject, ‘Professionals without an ethic are merely technicians who know how to perform work, but who have no capacity to say why their work has any larger meaning.’ Without meaning, there is little or no motivation to perform well.
What, then, is nursing ethics? Nursing ethics can be defined broadly as the examination of all kinds of ethical and bioethical issues from the perspective of nursing theory and practice, which in turn rest on the agreed core concepts of nursing, namely person, culture, care, health, healing, environment and nursing itself (or, more to the point, its end good), all of which have been comprehensively articulated in the nursing literature. In this regard, then, nursing ethics is not synonymous with, and indeed is greater than, an ethic of care, although an ethic of care has an important place in the general scheme of things encompassing nursing and nursing ethics.
Unlike other approaches to professional and healthcare ethics, nursing ethics recognises the ‘distinctive voices’ that are nurses, and emphasises the importance of collecting and recording nursing ‘stories from the field’. Like other approaches to ethics, however, nursing ethics recognises the importance of providing practical guidance on how to decide and act morally. Drawing on a variety of ethical considerations, nursing ethics, at its most basic, could thus also be described as a nursing practice discipline which aims to provide guidance to nurses on how to decide and act morally in the contexts in which they work.
Moral principles
General standards of conduct that make up an ethical system are known as moral principles. To say that a principle is moral is merely to assert that it is a behaviour guide that entails particular imperatives or obligations; that is, to do or to refrain from something that may have a morally significant outcome. It is generally accepted that moral principles function by specifying that some type of action or conduct is prohibited, required or permitted in certain circumstances (Beauchamp and Childress, 2009; Johnstone, 2009a). By this view, an action or behaviour is generally considered morally right or good if it accords with a given moral principle, and morally bad or wrong when it does not.
Moral principles commonly referred to in healthcare ethics include those of autonomy, non-maleficence, beneficence and justice (see section on moral theories, below). To illustrate how moral principles work, consider the principle of autonomy. The principle of autonomy demands respect for individuals as self-determining choosers and is widely accepted as a general standard of moral conduct. Given this principle, conduct which respects an individual’s self-determining choices (e.g. a client’s competent decision not to accept a recommended medical treatment) could be appraised as having accorded with the principle of autonomy and therefore as being morally ‘right’ and justified. Conversely, conduct which is disrespectful of an individual’s choices (e.g. a competent client’s decision to refuse medical treatment is rejected and overridden by a professional caregiver) could be appraised as having violated the principle of autonomy and therefore as being morally ‘wrong’. Moral principles thus not only guide conduct, but they can also be appealed to for justifying the conduct in question.
Moral rules
Like moral principles, moral rules also have a place in making up a system or scheme for guiding moral action. And like moral principles, moral rules also function by specifying that some type of conduct is prohibited, required or permitted (Beauchamp and Childress, 2009; Johnstone, 2009a). What distinguishes a moral rule from a moral principle, however, is its nature and force. Moral principles, for example, tend to be general in nature (e.g. do no harm; promote good). Moral rules, in contrast, are both derivative of, and justified by, parent principles and are very specific in their focus (e.g. do not kill others; do not tell a lie). It can be seen, then, that moral rules have a different force, sanctioning power, condition of existence, scope of application and level of concreteness from moral principles. In application, they are generally regarded as having less force than principles.
Rights
Common to discussions on nursing ethics is the notion of rights—including moral rights, human rights and clients’ rights. An understanding of these key terms is, therefore, warranted.
Moral rights
These are to be distinguished here from other kinds of rights, such as civil rights, legal rights, institutional rights and the like. Moral rights generally entail a claim about some special entitlement or interest which ought, for moral reasons, to be protected. For example, people commonly claim rights to such special interests as life, freedom, fair treatment, bodily integrity, health, and so on. The language used in asserting rights typically involves expressions like ‘I have a right to …’, ‘You have a right to …’, and so on.
Human rights
In contrast, human rights refer to a set of special interests that human beings (as opposed to non-human beings, such as animals) are entitled to claim by virtue of being human. Human rights can include moral rights, legal rights, civil rights and so on. A good example of human rights statements can be found in the United Nations (1948) Declaration of Human Rights. This declaration has influenced the development of nursing codes of ethics, not least the ICN’s (2006) revised Code of Ethics for Nurses, the NMBA’s Code of ethics for nurses in Australia (Australian Nursing and Midwifery Council, 2008a) and, to some extent, the NZNO’s (2010) Code of ethics, which although not overtly informed by a human rights framework, nonetheless contains statements that prescribe the protection of client rights (see Box 9-1).
Clients’ rights
These can be described as a subcategory of human rights. Statements of clients’ rights tend to entail statements about particular moral interests that a person might have in healthcare contexts and that require special protection when that person assumes the role of a client. Clients’ rights that might be commonly claimed include the right to healthcare, the right to make informed decisions, the right to confidentiality and the right to dignity and to be treated with respect.
Moral duties
A moral duty (to be distinguished from a legal duty, a civic duty and so on) is an action which a person is bound, for moral reasons, to perform. Language used in identifying duties typically involves expressions such as ‘I have a duty …’, ‘You have a duty …’, and so on. In a rights view of ethics, someone claiming a valid right supplies a moral reason for why another must act morally towards them. Indeed, moral duties are sometimes described as being correlative; that is, in relation to another’s rights claims. To put this in another way, if one person claims a right, this may entail another having a correlative duty to respect and respond to that right. For example, if a client claims the right to make an informed decision regarding nursing care, then an attending nurse could be said to have a correlative duty to respect and uphold that right. Moral reasons can also be supplied by an appeal to ethical principles. For example, adoption of the principle of autonomy would impose on decision makers a duty to uphold its prescriptions; namely, to respect people as self-determining choosers.
A critical task for decision makers is deciding just what their duties are in given situations. Making the correct decision depends on determining what counts as an overriding moral reason for doing something (bearing in mind that moral reasons are generally regarded as being stronger or more pressing than other kinds of reasons, such as personal preferences, civic duty and group membership). For example, in the case of a rights claim being made, whether or not another has a corresponding duty will depend on whether the right being claimed is genuine, whether the entity has moral rights at all and whether an agent does in fact have a duty correlative to the rights claim being made.
Sometimes people confuse rights with duties, and vice versa. A useful way to guide an understanding of the distinction between rights and duties is to consider that when people claim a right they are making a claim with respect to their own interests; in contrast, when people claim a duty they are making a claim with respect to the interests of another or others.
The importance of ethics
Nursing has a profound ethical dimension. Its practice never occurs in a moral vacuum and is never free of moral risk (Johnstone, 2009a). Even the smallest of nursing actions (e.g. giving an aspirin tablet) could, potentially, result in significant moral consequences—bad as well as good. Moreover, as long as nurses work with and care for other people, they will never be able to avoid the moral problems and issues that will invariably arise during the course of their practice.
During their everyday practice, nurses will often be confronted by such questions as: What should I do in this situation? How do I know I’m doing the right thing? What are my moral obligations in this case? The case of ‘Ms Winnow’, a competent patient with a health history of diabetes, obesity and large areas of skin breakdown who refused nursing care, helps to illustrate this point (Dudzinski and Shannon, 2006). The cares which Ms Winnow initially refused included being turned, having wound care for her decubitus ulcers and undergoing incontinence management. Ms Winnow’s refusals left attending nurses confronted with the dilemma of on the one hand wanting to respect her wishes and yet, on the other, knowing that respecting her wishes would place her at further risk of harm and suffering—including further breakdown of her ulcerated skin. In this case, provocative questions arise: What should her attending nurses do? What are their moral obligations to Ms Winnow? And how are they to know that, whatever they decide and do, they have done the right thing, all things considered?
When encountering an ethical problem in the workplace, nurses often worry about whether the moral decisions they make are ‘correct’; nurses are also known to experience moral perplexity and distress when—for various reasons—they did not ‘get it right’ or were unable to carry out what they had carefully and conscientiously thought was the right thing to do. It is for these kinds of reasons that ethics has assumed paramount importance in nursing.
Moral conduct in nursing
Nurses face many complex and varied moral problems during the course of their practice, which cannot be ignored. In fact, there are stated expectations in nursing standards of conduct that nurses not only must be able to identify and respond appropriately and effectively to a range of ethical problems and issues in nursing and healthcare contexts, but also must demonstrate moral competence in regard to these things.
Moral/ethical competence can be defined in terms analogous to clinical competence as the up-to-date knowledge and skills, and soundness of judgment, required of a profession as well as the demonstrated ability ‘to achieve desired outcomes through the performance of defined skills’ (Jormsri and others, 2005). In Australia, the specific moral competencies expected of registered nurses are outlined in the NMBA’s National competency standards for the registered nurse (Australian Nursing and Midwifery Council, 2006). This document makes clear that, in keeping with their ethical responsibilities as competent professionals, registered nurses must demonstrate ‘a satisfactory knowledge base’ as well as accountability for practice in regard to the protection of individual and group rights. The particular moral competencies expected of a registered nurse are listed under Standard 2: Practises within a professional and ethical nursing framework, and include:
• Practises in accordance with the nursing profession’s codes of ethics and conduct
• Practises in a way that acknowledges the dignity, culture, values, beliefs and rights of individuals/groups
• Advocates for individuals/groups and their rights for nursing and healthcare within organisational and management structures.
These competencies, in turn, are clarified to include the capabilities to:
• give due consideration to the nurse’s ethical responsibilities in all aspects of practice
• maintain an effective process of care when confronted by differing values, beliefs and biases
• recognise the rights of others and ensure that one’s own personal values and attitudes are not unjustly imposed on others
• provide care to individuals and groups that is informed about, sensitive to and respectful of their race, ethnicity, culture, language, religion, age, gender, sexuality, physical or mental status, and other distinguishing characteristics
• identify and adhere to strategies aimed at promoting the rights of individuals/groups in the healthcare setting
• act to ensure the rights of individuals/groups are not compromised
• protect the rights of individuals and groups in regard to informed decision making
• protect the rights of individuals and groups in regard to privacy and confidentiality
• question and/or clarify with members of the healthcare team any interventions that might seem inappropriate
• engage in morally responsible and accountable nursing practice.
In New Zealand, the specific moral competencies expected of registered nurses are outlined in the NCNZ’s (2009b) Competencies standards for registered nurses. These standards require registered nurses to be able to demonstrate knowledge and judgment and be ‘accountable for own actions and decisions, while promoting an environment that maximises client safety, independence, quality of life and health’. The particular moral competencies (and related indicators) expected of a registered nurse are variously listed under Domain 1: Professional responsibility and Domain 2: Management of nursing care, and include:
• Accepts responsibility for ensuring that his/her nursing practice and conduct meet the standards of the professional, ethical and relevant legislated requirements.
• Maintains clear, concise, timely, accurate and current client records within a legal and ethical framework.
• Discusses ethical issues related to health care/nursing practice (for example: informed consent, privacy, refusal of treatment and rights of formal and informal clients).
• Promotes a quality practice environment that supports nurses’ abilities to provide safe, effective and ethical nursing practice.
Moral accountability and responsibility
In identifying and responding effectively to moral problems in the workplace and, indeed, when practising in a professional capacity generally, nurses are morally accountable and responsible for their actions (Johnstone, 2009a). Thus, when a nurse breaches the agreed ethical standards of the nursing profession, there is an expectation that they will be made to account for and, ultimately, be held responsible for their conduct. Moral accountability and responsibility, however, do not reside only in individual nurses. The nursing profession as a whole, and those charged with the responsibility of regulating it, are also morally accountable and responsible for their actions. This is an important point, since it has a significant bearing on the kinds of strategies that might otherwise be used to respond effectively to situations in which the agreed ethical standards of the profession are at risk of being or have already been breached.
Understanding the nature and moral implications of professional accountability and responsibility in nursing requires a commensurate understanding of moral theories of accountability and responsibility. For instance, in the philosophical literature, accountability has classically been taken to mean:
[being] obliged to give satisfactory reasons for one’s actions, to be capable of giving an explanation for one’s actions, to be responsible for one’s conduct, to be made to pay for one’s conduct, or to reckon with the consequences of one’s actions. (Fry-Revere, 1992)
In turn, the notion of responsibility (of which accountability is a form) has been taken broadly to include not only one’s ‘intentional conduct’ (i.e. a person’s deliberate acts and omissions), but also:
anything with which one is seen to have a causal relationship (whether this perception is justified or not), including moral character, physical and psychological characteristics, salvation, and even unintentional effects on one’s own life or the lives of others. (Fry-Revere, 1992)
Drawing on both of the above accounts, moral theories of accountability hold that:
a person X, is accountable for his or her actions if X acted freely or intentionally and X’s action or inaction is causally related to the outcome for which X is being held accountable. (Fry-Revere, 1992)
Theories of moral accountability tend to emphasise accountability to oneself or to a superior entity. Either way, claims of moral accountability tend to assume that:
Human beings are free to act and cause events for which they are directly responsible and that some form of internal mechanism of accountability, whether based on conscience or belief, is essential to human interaction. (Fry-Revere, 1992)
As well, some form of external mechanism (e.g. an ethics complaints committee) is also essential to human interaction (Spencer and others, 2000).
It can be seen, then, that the issues of moral accountability and responsibility have important implications for nurses. For instance, an ongoing problem facing the nursing profession is that although nurses have enormous responsibilities as healthcare providers, they often lack the lawful authority they need in order to be able to fulfil these responsibilities in a safe and effective way (Johnstone, 1994, 2009a).
Guides to ethical professional conduct
As has previously been considered, when making moral judgments and decisions in nursing care domains, nurses are often faced with such perplexing questions as ‘What should I do and what is the right thing to do in such-and-such situation?’, ‘Are my judgments and decisions morally correct, all things considered?’, ‘How should I decide?’ and ‘Have I done (am I doing) the right thing?’ These and similar questions become even more pressing when considered against the backdrop of stringent moral accountabilities and responsibilities otherwise expected of registered nurses.
Possible answers to these and related questions can be sought by appealing to moral theories and/or nursing codes of conduct; noting, however, that neither of these is without some difficulties with respect to their moral authority and capacity to guide and justify particular actions in specific contexts. As Beauchamp and Childress (2009) explain, ‘Many practical questions would remain unanswered even if a fully satisfactory general ethical theory were available.’
Moral theories
It is generally accepted that moral theory is crucial, not just for the purposes of guiding moral decision makers in their thoughts and actions, but also for providing sound justifications for the decisions made and actions taken.
Moral problems arise frequently in healthcare contexts. This is not surprising given the culturally diverse range and complexity of the moral values that are operating and expressed in healthcare domains. Indeed, healthcare practice is profoundly value-laden in a morally significant sense, and hence it is inevitable that some moral conflicts and disagreements will arise. Further, given the complexity of the values that operate in healthcare domains, it is inevitable that sometimes the choices made (by nurses as well as others) will be problematic, insofar as they may express moral values, beliefs and evaluations which are not shared by others or with which others do not agree.
When experiencing situations involving moral problems and disagreement, it is tempting for decision makers to rely on their own ways of thinking and personal preferences to sustain the points of view they are advocating. Sometimes, however, a person’s ways of thinking and personal preferences may not be reliable or worthy action guides because these can result from prejudice, self-interest or ignorance. Thus, decision makers need to look elsewhere to justify their moral choices and actions. Ethical/moral theory is commonly regarded as a reliable source from which such justifications can be sought.
There are a number of different moral theories that can be appealed to for guiding and justifying moral decision making and conduct, all of which, to varying degrees, have both formed the basis of and influenced the development and practice of nursing ethics. Notable among these are deontological ethics, teleological or consequentialist ethics, ethical principlism, moral rights theory, virtue ethics and cross-cultural ethics. A brief summary of each of these theories is outlined below.
Deontological ethics
According to deontological ethics, duty is the basis of all moral action. Taken at its most basic, deontology asserts that some acts are obligatory (duty bound) regardless of their consequences. For example, a deontologist might assert that one has a duty to always tell the truth. By this view, the deontologist is duty bound to always tell the truth even when doing so might have horrible consequences. An important question to ask here is: How do we know what our duty is?
One possible answer to this question can be found in classical deontological theory that derives from religious ethics and what is otherwise known as ‘divine command theory’. According to this view, it is God’s command that determines our moral duties. If, for example, God commands ‘Thou shalt not kill’, ‘Thou shalt not steal’ and the like, then conduct that accords with (obeys) these commands is morally praiseworthy (right and justified). Conduct that contradicts God’s commands, in contrast, warrants condemnation (as wrong and unjustified). This is because and only because it is God’s command (Morriston, 2009; Wainwright, 2005).
There are many examples of deontological ethics influencing decision making in healthcare domains. For example, Jehovah’s Witnesses refuse life-saving blood transfusions on the grounds that to accept such treatment would be tantamount to violating God’s command that prohibits taking blood. Another example can be found in a deontological adherence by some doctors and surgeons to the preservation of ‘medically hopeless’ human life whatever the costs (read ‘consequences’), resulting in the administration of ‘futile’ medical treatment to clients sometimes even against their will (Schneiderman and Jecker, 2011).
Another answer can be found in what is otherwise known as ethical rationalism. This view dates back to the work of the 18th-century German philosopher Immanuel Kant, who held that the supreme principle of morality was reason, whose ultimate end is goodwill. According to a 1972 translation, Kant stated that reason is free (autonomous) to formulate moral law and to determine just what is to count as being an overriding moral duty. Kant held duty to be that which is done for its own sake, and ‘not for the results it attains or seeks to attain’ (Kant, 1972). Kant further believed that moral considerations (duties) were always overriding in nature—in other words, should take precedence over other considerations.
In terms of determining what one’s actual duty is, Kant suggested that this can be done by appealing to some formal (reasoned) principle or maxim. In choosing such a maxim, however, Kant warned that we must take care not to choose something that would privilege our interests over the interests of others. Kant’s solution to this problem was to establish a universally valid law called the ‘categorical imperative’. This law states: ‘Act only on that maxim through which you can at the same time will that it should become universal law’ (Kant, 1972). In other words, we should act only on maxims that we are prepared to accept as holding for everybody (including ourselves) throughout space and time. A variation of Kant’s law can be found in what is popularly known as the Golden Rule: ‘Do unto others as you would have them do unto you.’
Teleological ethics
According to teleological theory (also known as consequentialism), actions can be judged right and/or good only on the basis of the consequences they produce. In this respect, teleology denies everything that deontology asserts.
The most popularly known teleological theory of ethics is utilitarianism, which has as its central concern the general welfare of people as a whole, rather than of individuals. In short, utilitarianism views the world not in terms of certain individual rights which people may or may not claim, but in terms of the collective and overall welfare and interests of people generally (a consequentially ‘good outcome’). The perspective of utilitarianism is persuasive in that it promotes a universal point of view; namely, that one person’s interests cannot count as being superior to the interests of another just because they are personal interests (Rosen, 2003). To put this in another way, I cannot claim that my interests are more deserving than your interests are, just because they are my interests.
Classical utilitarianism, first advanced by the English philosopher Jeremy Bentham (1748–1832) and later modified by the work of the British philosopher John Stuart Mill (1806–73), holds roughly that moral agents have a duty to ‘maximise the greatest happiness/good for the greatest number’ (Bentham, 1962; Mill, 1962). This view has resulted in classical utilitarianism being dubbed the ‘greatest happiness principle’. Because of difficulties associated with calculating both individual and collective happiness and unhappiness, and the problem of individual interests being sacrificed for the collective whole, classical utilitarianism theory has been largely abandoned in favour of recent utilitarian theory. Of particular note is ‘preference utilitarianism’, which views the maximisation of individual preferences as being of intrinsic value rather than the maximisation of happiness per se. This is because, as Beauchamp and Childress (1989) have classically explained, ‘what is intrinsically valuable is what individuals prefer to obtain, and utility is thus translated into the satisfaction of those needs and desires that individuals choose to satisfy.’
Preference utilitarianism is also considered more plausible because it is relatively easy to calculate what people’s preferences are—all we have to do is to ask people what it is they prefer. And where their preferences are at odds with ethical conduct, we have no obligation to respect them. This position, however, rests on assumptions about the ‘use’ of utility and its supposed intrinsic value, which some contend it does not have (Millgram, 2000).
Ethical principlism
One of the most popular ethical theories used today when considering ethical issues in nursing and healthcare is the theory of ethical principlism. Ethical principlism is the view that ethical decision making and problem solving are best undertaken by appealing to sound moral principles (Beauchamp and Childress, 2009). The principles most commonly used are those of autonomy, non-maleficence, beneficence and justice.
Autonomy
As a concept, autonomy refers to a person’s self-contained and independent ability to decide. As a principle, autonomy prescribes that people ought to be respected as self-determining choosers and that it is wrong to violate a person’s considered and autonomous choices. This is so even if we do not agree with another’s choices and regard them as foolish, provided they do not interfere significantly with the moral interests of others. Applied in nursing and healthcare contexts, the principle of autonomy imposes on healthcare professionals a moral obligation to respect clients’ choices regarding recommended medical treatment and associated care. Further, this obligation holds even if attending healthcare professionals do not agree with the choices that clients make.
Non-maleficence
Maleficence refers to harm or hurt, so non-maleficence means to avoid harm or hurt. Simply stated, the principle of non-maleficence prescribes ‘do no harm’. Applied in nursing and healthcare contexts, the principle of non-maleficence would provide justification for condemning any act that unjustly injures a person or causes a person to suffer an otherwise avoidable harm. Harm, in this instance, may be broadly taken as involving the invasion, violation, thwarting or ‘setting back’ of a person’s significant welfare interests to the detriment of that person’s wellbeing (Beauchamp and Childress, 2009).
Beneficence
The principle of beneficence, similar in meaning to the word ‘benefit’, entails a positive obligation to ‘act for the benefit of others’; that is, to promote their welfare and wellbeing (Beauchamp and Childress, 2009). Thus it prescribes ‘do good’. Beneficent acts can include such virtuous actions as care, compassion, empathy, sympathy, altruism, kindness, mercy, love, friendship and charity (Johnstone, 2009), all of which stand to find ready application in nursing and healthcare contexts.
Justice
The principle of justice can be conceptualised in a variety of ways. For instance, justice can be interpreted as involving retribution (retributive justice, e.g. ‘an eye for an eye’), an equal distribution of benefits and burdens (distributive justice), justice as mercy, justice as harmony, justice as equality (‘equals must be treated equally, and unequals unequally’), justice as fairness, justice as what is deserved (‘just desserts’), and justice as inclusiveness, fellowship, compassion and respect (Beauchamp and Childress, 2009; Nussbaum, 2006; Sen, 2009). More recently, justice has also been conceptualised as a basic human need (Johnstone, 2011b; Taylor, 2006). The conceptualisations of justice most commonly used in healthcare are those of justice as fairness (an intuitive sense of justice) and as an equal distribution of benefits and burdens (a rationalistic sense of justice). For example, on the basis of both an intuitive and a rational appeal to the principle of justice, it might be concluded that it is manifestly unfair and disproportionately burdensome to withhold life-saving treatment (e.g. cardiac surgery) from those who cannot afford to pay for such treatment. Such an action stands as being burdensome since it places the poor in a disadvantaged position in relation to the rich—the poor stand to suffer a burden of compromised life expectancy (which the rich do not) on account of their inability to pay. At an intuitive level, such a situation does not feel right in that it feels ‘unfair’.
Although vulnerable to criticism on a variety of accounts, ethical principlism has increasingly come to replace more classical theoretical approaches to identifying and resolving moral problems in healthcare contexts. Since ethical principlism is widely appealed to in the healthcare and related ethics literature, it is important that nurses have at least a working knowledge and understanding of this approach. It is necessary for nurses to be aware, however, that principlism is not without its limitations. As the cases of ‘Mr G’ and ‘Ms Winnow’ considered earlier have demonstrated, applying these principles in practice can be very difficult.
Moral rights theory
Another popular and commonly used moral theory is that of moral rights theory, a form of deontological ethics. Moral rights have been particularly influential in the development of discourses on clients’ rights and the development of various codes and charters outlining clients’ rights in healthcare (Weller, 2006). As discussed earlier, a moral right is a special interest that a person may have and which ought to be protected and upheld for moral reasons.
There is no simple thesis of moral rights (Campbell, 2006; Dyck, 2005). Indeed, there are a number of bases on which an entity could validly claim moral rights, including natural law, common humanity, rationality and interests.
Natural law
By this view, rights are the product of the laws of nature and apply equally to everybody; thus everybody is subject to them, just as they are to the laws of nature (e.g. gravity).
Common humanity
All human beings have rights equally, just by virtue of being human. This is because being human is not something over which human beings have control.
Rationality
Only people who are capable of rational, autonomous thought are entitled to claim rights. This means, controversially, that entities such as babies, unconscious people, people with severe brain injuries and the like are excluded from having rights.
Interests
In order to have rights, an entity must have interests; and in order to have interests, an entity must have the capacity to be benefited or harmed; which, in turn, presupposes sentience (the capacity to experience pleasure and/or pain) (Feinberg, 1979). This classic view is commonly seen as being among the most tenable theses of moral rights, since it is more inclusive than the other theories; for example, it includes both the rational and the non-rational, and other species besides human beings.
Virtue ethics
In recent times there has been a resurgence of virtue theory in ethics and a re-examination of the importance of ‘characterological excellence’ in determining ethical conduct (Oakley, 2006; Van Hooft, 2006). This is made manifest by the expression of such moral virtues as care, compassion, kindness, empathy, sympathy, altruism, generosity, respectfulness, trustworthiness, personal integrity, wisdom, courage and fairness. Virtue theorists claim that without the characterological excellence of virtue, ‘a person could, robot-like, obey every moral rule and lead the perfectly moral life’ but in doing so would be acting more like ‘a perfectly programmed computer’ than a morally responsible human being (Pence, 1991). There is a sense in which being moral involves much more than merely following rules; the missing link, claim virtue theorists, is character. On this point, Pence (1991) writes:
we need to know much more about the outer shell of behaviour to make such judgments, that is, we need to know what kind of person is involved, how the person thinks of other people, how he or she thinks of his or her own character, how the person feels about past actions, and also how the person feels about the actions not done.
Virtue ethics is particularly relevant to nursing and to nursing ethics since virtuous conduct is intricately linked to therapeutic healing behaviours and the promotion of human health and wellbeing.
The nursing profession’s well-articulated ethic of care (regarded by many influential nurse theorists as the moral foundation, essence, ideal and imperative of nursing) is consistent with a virtue theory of ethics (see the classic works of the following nurse theorists: Benner and Wrubel, 1989; Gaut, 1991; Gaut and Leininger, 1991; Leininger, 1988, 1990; Roach, 1987; Watson, 1985a, 1985b). Significantly, an ethic of care is enjoying a renaissance in the nursing ethics literature—particularly in regard to the issue of caring for vulnerable and marginalised groups of people at risk of being treated as ‘different’ and as ‘others’ by healthcare providers (Myhrvold, 2006; Nussbaum, 2006).
Cross-cultural ethics
As highlighted by the ‘Mr G’ case discussed in the opening paragraphs to this chapter, another perspective on ethics and bioethics that warrants consideration by nurses is cross-cultural ethics. The basic assumptions of cross-cultural ethics reflect the views that:
• ethics is very much a product of the culture, society and history from which it has emerged
• all cultures have a moral system, but what this system is and how it is applied will vary across, and sometimes even within, different cultures
• there is no such thing as a universal ethic; that is, one ultimate standard of moral conduct which applies to all people equally regardless of their individual circumstances, context and culture—in other words, a ‘one size fits all’ approach to ethics (Johnstone, 2009a, 2011a).
In any culturally diverse society it is imperative that a culturally informed, knowledgeable and sensitive approach to healthcare is taken (Fry and Johnstone, 2008; Johnstone, 2011a; Johnstone and Kanitsaki, 2008). One reason for this is that a failure to adopt such an approach can result in otherwise serious moral harm being caused to people. Cross-cultural ethics, therefore, goes far beyond merely considering and critiquing the nature and content of mainstream ethical theories; it also involves a systematic examination of the moral implications of cultural and linguistic diversity in healthcare domains, for example the extent to which clients of non-English-speaking and diverse cultural backgrounds suffer unnecessarily on account of the cultural and language differences between them and their professional carers (see, for example, Divi and others, 2007; Johnstone and Kanitsaki, 2006, 2009a).
Nurses and other healthcare workers have a stringent moral responsibility to avoid and/or prevent the otherwise avoidable moral harms that can result from a failure to take into account the language and cultural needs of their clientele (Johnstone and Kanitsaki, 2006, 2008, 2009a). The harmful aftermath of racism in healthcare is a particular example of this. Racism in nursing and healthcare is a problem that has not been formally recognised as an important ethical professional issue (Johnstone and Kanitsaki, 2009b, 2010). A cross-cultural approach to ethics would not only help identify the existence of racism in nursing and healthcare contexts, but also guide an effective response for dealing with it and, if not successful in eradicating it, at least minimise its harmful consequences to client health.
Nursing codes of ethics
Nursing codes of ethics have long featured as guides to ethical professional conduct in nursing. Just what they are, however, and how they function has not always been clearly understood.
As discussed extensively elsewhere (Johnstone, 2009a), a code may be defined as a conventional set of rules or expectations devised for a select purpose. By this view, a code of professional ethics could be described as a document laying out a set of moral rules and/or expectations devised for the purposes of guiding ethical professional conduct. Although codes of ethics are not fully developed systematic theories of ethics, they nevertheless tend to reflect a rich set of moral values that have been expressed and explained through a process of extensive consultation, debate, refinement, evaluation and review by practitioners over time.
Codes can be either prescriptive or aspirational in nature. In the case of prescriptive codes, provisions are ‘duty-directed, stating specific duties of members’ (Skene, 1996). In contrast, aspirational codes are ‘virtue-directed, stating desirable aims while acknowledging that in some circumstances conduct short of the ideal may be justified’ (Skene, 1996). Either way, codes of ethics have as their main concern directing ‘what professionals ought and ought not to do, how they ought to comport themselves, what they, or the profession as a whole, ought to aim at’ (Lichtenberg, 1996).
In Australia, for example, the NMBA’s Code of ethics for nurses in Australia (Australian Nursing and Midwifery Council, 2008a) and Code of professional conduct for nurses in Australia (Australian Nursing and Midwifery Council, 2008b) make explicit the ethical standards that Australian nurses are expected to uphold in the interests of promoting and protecting the moral interests and welfare of consumers, and the actions that must be taken against nurses if these agreed standards are breached; similarly, the NZNO’s (2010) Code of ethics and the NCNZ’s (2009) Code of conduct for nurses (see Box 9-1).
Historically, the professional–client relationship has been a special one in which certain privileges have been accorded to the attending professionals in return for the special (read ‘expert and often essential’) services they provide to their clients in the community at large. The professional–client relationship has also tended to be an unequal relationship, with the professional usually holding the balance of power. This imbalance of power has been implicated in both potential and actual vulnerability of clients when seeking and receiving professional services. Although the nature of the professional–client relationship has changed dramatically in recent decades, it nevertheless remains characterised by an imbalance of power involving, among other things, an imbalance of knowledge and legitimated authority to use knowledge.
This imbalance of power has helped to create a demand and given rise to an expectation among members of the community that professionals ought to, and will, submit to a system of rules imposing a greater constraint on their professional conduct than would otherwise be imposed on the conduct of ordinary (lay) people. All in all, there has emerged a general expectation that professionals will act in a supremely ethical manner when rendering services to clients.
Over the past several decades, recognition of the responsibility of professionals to act in an ethically exemplary manner has seen considerable attention being given to devising and agreeing to a system of rules to govern both personal and professional conduct (Coady and Bloch, 1996; Kerridge and others, 2009). A code of ethics serves this purpose by providing a clear and singular guide to conduct.
Codes of ethics serve a variety of functions. Key among them are to maintain ethical standards of conduct and to help the regulation of ethical professional conduct. These outcomes are thought to be achieved by the direct and the indirect value of codes in fostering and maintaining the standards of ethical professional conduct by cultivating moral character, by articulating certain characteristics and ideals of a profession, by facilitating the internalisation of these values and ideals by members of the professional group in question, and by prescribing and proscribing conduct that is otherwise not amenable to legislation, by specifying rules of conduct; for example, ‘Nurses will keep in confidence information gained in the professional–client relationship’ (Coady and Bloch, 1996; Johnstone, 2009a).
A characteristic feature of codes of ethics is their voluntariness. What this means is that persons subscribing to or upholding the terms of a given code of ethics do so free from any coercive or manipulative influences. In other words, compliance is and ought to be both autonomous and voluntary.
Like other moral action guides, however, codes are not without their limits. Problems include their having limited moral authority (being mostly a statement of rules, codes cannot override the demands of a more systematic and reflective system of moral principles and standards) and limited practical application (e.g. codes may offer very little practical guidance on how to make sound moral decisions when dealing with complex ethical issues and/or particular situations). The case of Mr G, referred to in the opening paragraphs of this chapter, underscores this point.
Despite these limits, codes of ethics and, of relevance to this discussion, nursing codes of ethics have an important role to play in regard to:
• advising the public of the values and ideals it can expect of nurses when delivering care to clients
• informing nurses of the values and ideals they are expected to uphold upon becoming members of the broader nursing profession
• providing standards against which nurses’ conduct can be measured and, if found to be in breach of these standards, censured via the lawful processes of disciplinary action.
Moral problems in nursing
When delivering nursing care to clients, nurses will encounter a range of moral problems. These problems range from the relatively simple to the extraordinarily complex, and can cause varying degrees of perplexity and distress in those who encounter them. Nurses, like other healthcare professionals, have a fundamental and unavoidable moral responsibility to be able to identify and respond effectively to the moral problems they encounter—which includes self-care (Johnstone, 2009a).
The ability of nurses to deal effectively with the problems they encounter will depend on a range of variables, including:
• their ability to correctly identify a given moral problem
• the level to which they are prepared educationally, psychologically and emotionally to be able to respond to various moral problems as they arise and are identified
• the extent to which institutional norms and practices are supportive of the moral authority and experience of nurses to deal with moral problems in the workplace
• the extent to which other legal processes recognise and are responsive to the moral authority of nurses and the ethical standards of the nursing profession generally.
Nursing point of view
When moral problems arise in healthcare contexts, the nurse’s observations and considered judgments (the ‘nursing point of view’) can play a vital role in the correct identification and mitigation of the problems at hand. Since nurses may be involved in very intimate physical acts with clients, such as bathing, feeding and special procedures, information that is not generally solicited by other attending healthcare workers, including doctors and social workers, is often revealed to nurses by clients and their families. Details about family life at home, information about coping styles or personal preferences and details about fears and insecurities may come out during nursing interventions. Such information can be vital to ensuring sound moral decision making concerning client care.
On the other hand, it is important for nurses to remember that care of any one client has become multidisciplinary and fragmented. The nursing point of view is part of a larger picture that is best built by all members of the healthcare team, including the client and family. Managers and administrators from different professional backgrounds may also contribute to ‘moral conversations’, as they are able to bring knowledge of systems, allocation of resources, financial possibilities or constraints to the decision-making process.
Wherever moral problems arise, the nursing point of view is valuable and often essential. It is both an obligation and a privilege for the professional nurse to accumulate information on the issues, examine personally held moral values and beliefs, and share knowledge with clients and with colleagues in an effort to overcome the difficult issues that often underlie and/or constitute moral problems in healthcare.
Distinguishing moral problems from other kinds of problems
Being able to identify and respond effectively to moral problems in professional practice requires an understanding of what a moral problem is and how it might be distinguished from other kinds of problems, for example a legal problem or a clinical problem.
It is generally accepted that a moral problem has as its central concerns:
• the promotion and protection of people’s genuine wellbeing and welfare, including their interests in not suffering unnecessarily
• responding justly to the genuine needs and significant moral interests of different people
• determining and justifying what constitutes right and wrong conduct in a given situation (Beauchamp and Childress, 2009; Johnstone, 2009a; Kerridge and others, 2009).
Nurses are fundamentally involved with promoting and protecting people’s genuine wellbeing and welfare and, in achieving these ends, responding justly to the genuine needs and interests of different people. And so long as nurses work and interact with people in a professional capacity, they will continue to be involved in the promotion and achievement of these moral ends.
Moral problems (also called ethical issues) fall roughly into three categories:
1. those that involve procedural difficulties associated with the actual identification and satisfactory resolution of moral problems in nursing and healthcare contexts, such as unethical conduct, moral impairment, moral incompetence, moral disagreement and ethical dilemmas
2. those that involve everyday ethical issues that arise in face-to-face ‘hands-on’ encounters with clients and co-workers
3. the more ‘exotic’ issues of applied ethics involving a range of bioethical issues, such as clients’ rights to informed consent, confidentiality or euthanasia/assisted suicide.
Identifying and responding effectively to moral problems in nursing
All nurses are expected to be able to identify correctly and respond effectively to moral problems in the workplace. The kinds of problems that may be encountered are summarised below.
Moral unpreparedness
A person is not adequately prepared educationally, psychologically or emotionally to deal with a presenting moral problem. When faced with a moral problem, a morally unprepared nurse may not take appropriate action to remedy a troubling situation on the grounds of ‘I did not know what to do’.
Moral blindness
A nurse (or other member of the healthcare team) is blind to the ethical dimensions of a presenting problem; for example, they may wrongly regard the problem at hand as a clinical or technical problem requiring only a clinical solution, not a moral one. By analogy, like a colour-blind person who cannot see certain colours, a morally blind person cannot see the moral dimensions of a given situation or problem. Take, for example, a medical decision not to resuscitate a client. This may be construed as simply ‘good medical practice’ and, as such, outside the concerns of ethics, regardless of the fact that such a decision may have been based firmly on quality-of-life considerations and made without the client’s knowledge or consent.
Moral indifference
A nurse (or other member of the healthcare team) is largely unconcerned about the demands of ethical professional conduct. A nurse who is morally indifferent may, for example, demonstrate a lack of interest in or concern about a client’s wellbeing and/or welfare. The morally indifferent nurse might refrain from engaging in any discussions or activities aimed at client advocacy, or disregard a client’s pain and discomfort.
Amorality
A nurse or other member of the healthcare team literally has no morality. As the word itself suggests, there is an absence of morality in these people.
Immorality/unethical conduct
A nurse or other member of the healthcare team accepts ethical standards of conduct, but nevertheless deliberately violates them. An example is the case of a nurse who steals money from an elderly client or fraudulently uses her credit card.
Moral complacency
A nurse or other member of the healthcare team is unwilling to accept that their moral beliefs and viewpoints may be mistaken. Such a nurse is reluctant to accept that their point of view is often just one among many that deserves to be considered, compared and contrasted. For example, a morally complacent nurse may hold firmly to the view that it is morally wrong to perform resuscitation on people over the age of 75 (regardless of the person’s wishes to the contrary), since they are already old, at the end of their lives and should not be troubled by having to decide such burdensome issues.
Moral fanaticism
A nurse or other member of the healthcare team uncritically holds extreme moral views. For example, a nurse might uncritically and fanatically uphold the view that, irrespective of their stated cultural values and beliefs and expressed wishes, people diagnosed with cancer should be told their cancer diagnosis by an attending doctor. Moreover, such information should be communicated ‘directly’ and ‘frankly’ to the person by the doctor, regardless of the person’s or the family’s wishes in regard to what information should be given, when, where, how and by whom. Such a nurse might further hold the view that ‘Even if this information may result in causing the patient otherwise preventable distress, they should still be told directly whether they wish it or not, whether the family is there or not, because “they have a right to know”. And this is just the way it should be’.
Moral disagreement
Nurses or other members of the healthcare team may disagree about the morally correct course of action to take in a given case. Disputing parties may share and subscribe to common moral standards, but disagree as to:
• when one set of standards should override another set, for example whether the principle of autonomy is stronger than the principle of non-maleficence in a situation involving the disclosure of a poor diagnosis to a client
• what should count as acceptable exceptions and limitations to applying the standards in question, for example a nurse might be willing to act as a client’s advocate but only so long as their own significant moral interests are not compromised; another nurse might not subscribe to this limitation
• whether a given set of standards should be chosen at all, for example two nurses might disagree that the moral principle of autonomy ought to be given consideration in the euthanasia debate.
Moral disagreement may also arise when disputing parties do not agree on any ethical standards at all.
Moral dilemmas
Nurses or other members of the healthcare team may find themselves between what is colloquially referred to as ‘a rock and a hard place’. Broadly speaking, a moral dilemma may be described as a situation involving choice between what seem to be two equally undesirable alternatives. Moral dilemmas commonly take one of three forms:
1. Where there exists a logical incompatibility between two or more moral principles; for example, in the context of informed decision making, where the information being disclosed is potentially harmful it may not be possible to uphold both the principle of autonomy (i.e. respect a client as a self-determining chooser) and the principle of non-maleficence (i.e. protect the client from otherwise avoidable harm) (refer to the case of Ms Winnow, discussed earlier).
2. When competing moral duties exist and a nurse cannot fulfil both, they must choose which duty to fulfil; for example, in a life-and-death situation, a nurse might feel duty bound to protect both a client and the chosen carers from the harm of suffering associated with the crisis at issue. That might not be possible and no matter what strategies the nurse uses, someone is going to suffer. Here the nurse might ask: ‘Which duty ought I to fulfil?’
3. When competing and conflicting interests exist; for example, two clients may have equally deserving rights claims and a nurse may be in a position to respond to only one of these claims at a time. Abortion is a good example here, especially in cases where the rights of the mother might compete with the rights of a fetus and/or the father. Here the nurse might ask: ‘Whose interests ought I to uphold?’
Moral stress, distress and moral perplexity
A nurse or other member of the healthcare team may suffer stress, distress and perplexity on account of having identified a given moral problem but been largely unsuccessful in resolving it. These states can manifest as emotional turbulence, indignation, incredulity, rage and outrage, anger, despair and an overwhelming and paralysing sense of hopelessness. If not resolved, this problem can lead to burnout and nurses resigning from their jobs.
Processes of moral decision making
Moral problems, like other kinds of problems, can be approached using a systematic decision-making process. Like the nursing process, identifying and resolving moral problems in healthcare contexts involves at least five steps:
1. Assessing the situation. Every effort is made to obtain all the relevant information pertaining to the case to enable a proper assessment of the nature of the problem and whether, indeed, it is a moral problem at all. Sometimes what seems like a moral problem may, in reality, be a legal problem or a clinical problem or a problem of some other practical non-moral nature.
2. Diagnosing or identifying the moral problem. The information collected is appraised and a judgment made on the nature of the problem at hand. It might be concluded on the basis of the information collected that the moral problem at hand involves a case of, for example, unethical conduct or a full-blown ethical dilemma; conversely, the problem at hand may be shown to involve little more than a breakdown in communication, hence not requiring a moral remedy per se.
3. Setting moral goals and planning an appropriate course of action. A specific plan of action is devised to resolve the moral problem(s) identified. If the problem involves a moral dilemma or a moral disagreement, then the plan of action will have as its focus, for example, an attempt to resolve the impasse that has arisen and to find a satisfactory solution; that is, one that has just and defensible moral outcomes.
4. Implementing the plan of action. The decision maker engages in the implementation of the plan of action; that is, sets the wheels in motion, as it were. Depending on the problem(s) identified, this could involve a range of actions, including reporting the matter to a supervisor or manager, and even seeking the involvement of an institutional ethics committee for advice.
5. Evaluation of moral outcomes of the actions taken. An assessment is made with respect to whether the desired moral outcomes of the actions taken were achieved. If the evaluation proves negative, then the whole situation needs to be reappraised using the same systematic process.
This model of moral decision making (see Figure 9-1) is by no means the only model that might be used to approach moral problems. Nevertheless, it is a very useful model and one that is relatively easy to use. It does, however, presuppose that decision makers have at least a working knowledge and understanding of ethics and the ability to think critically when applying ethics to and in professional practice. It would be useful at this point to briefly demonstrate how the model might be used (see Box 9-2, then read the clinical example overleaf before studying steps 1 to 5 of the discussion; consider also applying this process to the cases of Mr G and Ms Winnow, presented earlier in this chapter).
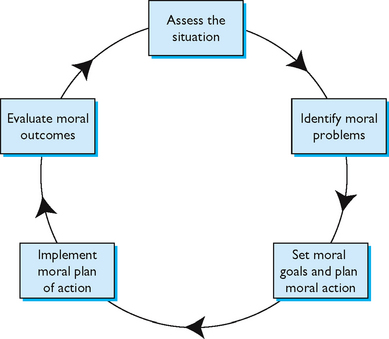
FIGURE 9-1 Moral decision making.
From Johnstone M-J 2009 Bioethics: a nursing perspective, ed 5. Sydney, Churchill Livingstone.
BOX 9-2 HOW TO PROCESS A MORAL PROBLEM
Step 1. Assess the situation and gather all the information relevant to the case; ask: What are the relevant facts of the case?
Step 2. Diagnose the moral problem; ask: What is the nature of the problem in this case?
Step 3. Set moral goals and plan a course of action aimed at achieving a morally just outcome; ask: How best can the client’s best interests (wellbeing and welfare) be maximised in this case?
Step 4. Implement the plan of action.
Step 5. Evaluate the outcome of the plan of action implemented; ask: Has the desired moral outcome been achieved in this case?
On your ward, a 35-year-old woman has been hospitalised in the final stages of a struggle with brain cancer. She is a single mother, with two young children at home. Despite treatment, the tumour continues to grow and the medical team has agreed that further treatment would be futile. You have cared for this client during past admissions, and during one especially open discussion, she expressed wishes to explore ‘do not resuscitate’ (DNR) directives. During the current admission, her medical consultant is out of town. The attending on-call doctor does not know the client personally, but he has spent some time with her. He has reviewed the clinical data and agrees that the client is entering advanced stages of her disease. In his opinion, however, the client is not ready to discuss end-of-life issues. In fact, he states that on being offered the option to discuss DNR, the client declined. You have asked him to convene a family conference to discuss DNR directives but he refuses to do so.
Clinical example discussion
STEP 1—ASSESS THE SITUATION AND ASK: WHAT ARE THE RELEVANT FACTS OF THIS CASE?
What may at first appear to be a question of ethics may not be such at all, and may be resolved by clarifying one’s knowledge base about clinical facts and reviewing policy and procedure, standards of care and so on. When it can be shown, however, that perplexing questions remain about the client’s genuine wellbeing and welfare (including her interests in not suffering unnecessarily), that the genuine needs and significant moral interests of different people are at stake and in need of protection, and that assistance is required in determining and justifying what constitutes right and wrong conduct in the situation at hand, then it is evident that a moral problem exists. The next step is to ascertain what kind of moral problem exists. This is crucial to the moral decision-making process, since unless the type of moral problem is diagnosed, any plan of action implemented risks failing to achieve a satisfactory moral outcome.
Further review of scientific data will probably not contribute to a resolution of the problem, but it is important to review the data carefully to make this determination. It is evident that there is disagreement, but this does not revolve around whether the client is in a seriously ill state, so further clinical information will not change the basic question: Should the client have an opportunity to discuss the ‘do not resuscitate’ (DNR) directive at this time? The question is perplexing. Basically, two professional team members disagree on an assessment of a client’s readiness to confront the very difficult issues around dying. The answer to the question concerning the client’s readiness has important implications for her wellbeing and welfare. If she is not ready, then raising the issues may cause anguish and fear in the client and her family. If she is ready, and the team avoids discussion, she may suffer unnecessarily in silence. If she is very close to death, then the lack of a DNR directive will necessitate the application of cardiopulmonary resuscitation (CPR) that could also result in harmful moral consequences. Knowing that CPR can cause pain and can carry devastating risks, not least the accidental rupture of internal organs, its application in a situation where further life is unlikely could prolong suffering and reduce dignity.
In assessing the situation at hand, it is necessary for the nurse to gather as much relevant information as possible. Since resolution of moral problems may arise from unlikely sources, it is helpful to incorporate as much knowledge as possible at every step of the process. At this point, the information could include looking at laboratory and test results, the clinical state of the client in question and perhaps current literature about the diagnosis or condition of the client. It may include careful investigation of the psychosocial concerns of the client and of the client’s significant others. A client’s cultural, religious and family orientation is part of the nurse’s assessment.
In this scenario, all the clinical information pertinent to the case would be obtained. It might be helpful to determine if the client retains most cognitive functions, even though her brain tumour is aggressive. A review with the attending medical consultant might result in agreement that she is fully competent, but definitely afraid and overwhelmed by the prognosis. Since the problem seems to exist because two professionals do not agree on a client’s state of mind, it may be helpful to reassess the client, or even to request that an independent person assess the client’s readiness to discuss end-of-life issues. Sometimes, family members or significant other people in the client’s life will hold important clues to a client’s state of mind and also how best to approach a given situation in a culturally informed and appropriate manner. In addition to this, the moral standards that are guiding the decision making should be clarified. What might be at issue in this case is a moral disagreement about the appropriateness of appealing to and applying the respective moral principles of autonomy and non-maleficence. Thus, what might initially look like a disagreement in professional opinion may in fact be much more than that—it may also involve a fundamental disagreement in moral viewpoint, or moral disagreement.
STEP 2—DIAGNOSE THE MORAL PROBLEM
Once the nurse is satisfied that the problem is a moral problem rather than some other kind of problem, for example a disagreement about the client’s health status which could be clarified by appeal to the clinical facts of the case, then it becomes necessary to make a more definitive moral diagnosis. The possibilities, as have been shown above, can include one or more of the following:
The clinical example meets the criteria for a moral problem. However, a more definitive moral diagnosis is needed. One possibility is that this case exemplifies a moral disagreement, since both doctor and nurse share a common moral commitment to preventing harm to the client but disagree on how this harm-prevention might be achieved—the doctor believes that imposing unwanted information (though crucial to informed decision making) on the client could result in her being caused unnecessary harm, whereas the nurse believes that withholding the information could likewise result in her being caused unnecessary harm. This situation could also be said to pose an ethical dilemma, since both doctor and nurse are situated between ‘a rock and a hard place’ and confronted by the question, ‘What ought I to do?’ Further information about the case might result in still other moral diagnoses being made.
STEP 3—SETTING MORAL GOALS AND PLANNING ACTION
Once all the relevant information has been gathered and a correct moral diagnosis made, attention can then shift to more specific questions such as: Should this client discuss the DNR directive at this time? What are the benefits and what constitute the risks of a DNR order at this time? An important question also seems to involve the client’s current state of mind: Is she afraid to speak? Is she feeling cut off from her normal network, including her medical consultant? Are these feelings contributing to confusion about DNR decisions? Has she been approached in a culturally informed and appropriate (culturally competent) manner?
Once these and similar questions are raised, it becomes easier to consider possible courses of action. What action is, in fact, planned will depend on still further questions being asked.
Other questions and possible courses of action could include: Should you initiate a discussion with the client independently of the doctor? Would you be outside your professional domain if you facilitated a DNR directive? What if your assessment was incorrect: would you contribute not to the dignity but to the distress of the client? The answers to these questions may be elusive, since they depend on an understanding of the client’s views and wishes that are not necessarily obvious. Even if legally the nurse cannot actually write a DNR directive, this fact does not relieve the nurse of moral questions since the ability to influence an attending doctor’s or a client’s decision regarding DNR remains. On considering these and similar questions, you might set the following goal and strategies:
• Goal: to achieve an outcome that genuinely maximises the client’s best interests (wellbeing and welfare) and prevent otherwise avoidable harmful moral consequences.
• Strategies: seek a meeting of the healthcare team to discuss the case and to work collaboratively to achieve a ‘best outcome’. This step represents the most important and delicate part of the process. Team members could be approached informally on a one-to-one basis within the ward setting and invited to attend. Team members might also be requested by a manager to attend a meeting. Whatever meeting takes place, the nurse has an obligation to articulate and justify the moral stance he/she is taking.
Alternatively, if efforts at the ward level fail to achieve a resolution, it may be necessary to refer the case to a unit or institutional ethics committee for guidance on how best to deal with the problem. If an ethics committee meeting is convened, the discussion will usually be multidisciplinary in focus. A facilitator or chairperson will ensure that all points of view are examined, and that all pertinent issues are identified. A decision or recommendation is the usual outcome of discussion. In the best of circumstances, participants discover a course of action that meets criteria for acceptance by all. Occasionally, however, participants may leave the discussion disappointed or even opposed to the decision. But in a successful discussion, all members will have agreed on an action or decision that can be implemented.
STEP 4—IMPLEMENT PLAN OF ACTION
Once the nurse has formulated a plan of action, it is then possible to implement it. In this case, the nurse may embark on discussions with members of the healthcare team. In other words, the nurse engages in the moral actions that have been planned.
The discussion focuses on the disagreement between the nurse’s assessment and the doctor’s regarding the client’s readiness to discuss end-of-life issues. The approach to moral decision making might include a discussion of the principles of autonomy, beneficence and non-maleficence: Does the client want something different from what she is expressing? Is the team approaching the client in a culturally appropriate manner? Which plan would provide the most good for this client, a DNR directive or no directive? Would a direct discussion with the client promote wellbeing or anguish? Should the discussion be held with her family first?
With several members of the healthcare team present, the discussion proceeds. In the end, the team proposes a formal meeting with the client, where you, the nurse, the attending doctor and a supportive family member are all present. This proposed course of action will maximise the support of the client’s existing network. In a trusting environment, the client is most likely to express her fears, insecurities and wishes most accurately. Team members agree to keep the discussion open-ended and exploratory. Rather than asking if the client wants a DNR directive written, perhaps the team could wait for her to bring up the issue. In this way, the team could be assured of her consent and willingness to participate in the discussion.
STEP 5—EVALUATE THE MORAL OUTCOMES OF THE ACTION TAKEN
After implementing the planned moral course of action, the nurse should evaluate whether the projected moral goals and the desired moral outcomes were achieved.
At the meeting, the client in fact opens up. She expresses relief at the chance to explore her options and feelings. Pain management issues are clarified. She wants to discuss a DNR directive, but requests a visit from her priest before making a final decision. The goal of maximising the client’s best interests have been achieved. The possibility of harmful moral consequences to the client have, it seems, been averted.
If the moral goals of action have not been achieved, then the process will need to begin again with questions asked as to why a desired moral outcome was not achieved. For example, it may transpire that not all the relevant facts of the matter were obtained and consequently the problem was misdiagnosed.
Bioethical issues in nursing
Since the inception of bioethics as a discipline in the early 1970s, a number of bioethical issues have emerged that are of particular relevance to nurses. Key among these are the issues of informed consent, confidentiality, quality of life, DNR directives, euthanasia/assisted suicide and resource allocation in healthcare. New and emerging ethical issues include the problems of equity and social justice associated with the health impacts of climate change, peak oil and pandemic influenza.
Informed consent
The main aims of informed consent processes are to promote and protect the client’s right to self-determination, and to remind healthcare practitioners of their duty to provide clients with the information necessary to make intelligent choices about whether to accept recommended care and treatment (Faden and Beauchamp, 1986; Manson and O’Neill, 2007). The main way of meeting these goals has been to share knowledge about clinical findings and management plans as they are implemented. In certain well-defined situations, the client must provide written evidence of consent, such as consent to a surgical procedure or consent to participate in an experimental regimen.
The practice of informed consent has gained increasing acceptance and respect in Australia and New Zealand. Healthcare providers now go to great lengths to share information that promotes informed decision making. Institutional policies and civil law protect the client’s right to informed consent. Its practice represents a clear effort to respect the autonomy of clients, and in this way also represents a fundamental shift from the medical paternalism (‘doctor knows best’) that was once characteristic of healthcare practice.
A commitment to the concept of informed consent does not ensure a lack of controversy. The concept depends on a certain level of competence on the part of the provider to communicate well, and also depends on a level of competence on the part of the client to understand. It is not always easy to secure these competencies. Furthermore, studies on communication skills demonstrate that healthcare providers are more likely to share information with clients who have similar cultural backgrounds to the provider. Providers may be more likely to give directives or advice than truly to share knowledge with clients whom they perceive to be less educated or less intelligent and, in the case of clients who do not speak English or do not speak it proficiently, may even fail to communicate relevant information at all (Johnstone and Kanitsaki, 2006, 2009b).
For consent to be properly informed it must satisfy the following criteria:
• The client was given relevant information to enable an intelligent choice to be made. Relevant information may be taken as referring to any information that would make a material difference to the choices being made.
• The client understood the information disclosed.
• The client’s consent was given voluntarily; that is, it was provided in a context that was free of coercive and/or manipulative influences.
• The client was competent to exercise the choices made.
• The client gave consent and understood the implications of doing so; that is, in consenting, the client was consenting to something (e.g. a medical procedure) being done to them (Beauchamp and Childress, 2009; Faden and Beauchamp, 1986; Kerridge and others, 2009).
Confidentiality
It is generally accepted that nurses, like other members of the healthcare team, have a stringent moral duty to keep secret any private information gained in the professional–client relationship. Nursing codes of ethics make explicit the nurse’s duty in this regard, and make it clear that nurses must exercise critical judgment if and when disclosing otherwise confidential information to a third party. The main aim of the rule of confidentiality is to protect clients against the morally harmful consequences that can occur when unconsented disclosures are made. An unconsented disclosure of, for example, a client’s newly diagnosed HIV-positive status could result in the client being rejected by family and friends and hence left without social support at a time when it is most needed. It might also result in the client losing his/her job, which although illegal still happens, compounding their loss of social support.
Confidentiality is not, however, an absolute principle. What this means is that although, as a general rule, we ought to keep information gained in the professional–client relationship secret, there may be times when disclosing such information is morally warranted. Indeed, it is generally recognised and accepted that sometimes there may be overriding moral reasons that disclosures should be made, for example where such disclosures could otherwise help prevent harm to innocent others. If a client disclosed that, for example, he intended to act out a revenge fantasy and kill someone he disliked, then the duty to keep this information confidential could be overridden by a stronger duty to warn the intended victim. In cases involving known or suspected cases of child abuse or elder abuse, disclosures might not only be morally warranted but legally mandated as well.
Quality of life
It is difficult to imagine a concept with a more personal, or more elusive, definition than quality of life. For each individual, quality of life is something that is intensely personal and particular. Yet society uses quality-of-life measures to help determine the benefits of medical intervention and, as a result, discussions about quality of life abound (Jecker and others, 2011; Kerridge and others, 2009). Some social scientists have proposed formulas or other objective measuring devices that can be applied to individual and group situations, and to whole populations (Rapley, 2003). These formulas might take into account the age of the client, ability to live independently and ability to contribute to society in a gainful way. Such a formula might help a committee determine, for example, the relative merits of giving an organ to one recipient over another. Or, a quality-of-life measure could help a client and family decide on the merits of a certain risky intervention, such as organ transplant or experimental drug management. The question of quality of life is paramount to discussions about futile care, euthanasia/medically assisted suicide, and DNR directives.
Given the diverse ways in which the notion of quality of life can be defined, it is important that nurses are clear about what they mean by this concept and that they ensure they do not inadvertently impose their views about what quality of life is on the client (Johnstone, 2009a).
Do not resuscitate (DNR) directives
At some stage during their practice, nurses will encounter clients who have been made the subject of a ‘do not resuscitate’ or DNR directive. A DNR directive (also sometimes written as a ‘do not attempt resuscitation’ (DNAR) or ‘not for resuscitation’ (NFR) directive) is made by an attending medical officer, and typically prescribes that in the event of a cardiac or respiratory arrest, no emergency resuscitation or life-supporting measures will be initiated. In other words, were the client to suffer a cardiac or respiratory arrest, CPR would not be performed. The issue of DNR has long been a controversial bioethical issue for nurses, as discussed elsewhere (Johnstone, 2009a). One reason for this has been that, at least in the past, it was not uncommon for DNR directives to be given without the client’s knowledge or consent. This was often justified on the questionable grounds that such knowledge would only cause the client unnecessary distress. Other problems related to:
• lack of institutional policies and guidelines for prescribing DNR
• the use of vague criteria for deciding whether a client ought to be made the subject of a DNR directive
• poor communication of medical decisions surrounding DNR practices
• poor documentation processes; for example, in the past, a DNR directive was commonly communicated via the use of coloured dots (usually black ones) being placed on the client’s chart or against their names on the ward admission board
• nurses being left to carry a disproportionate burden of responsibility with respect to the execution of such directives (Johnstone, 2009a:173).
Today, the issue of DNR is discussed much more openly with clients and their chosen carers as well as with members of the healthcare team. Nevertheless, the issue remains problematic and continues to invite debate in both the bioethics and the nursing ethics literature. Even though there have been notable improvements in the development and operationalisation of DNR policies and practices in local healthcare institutions, research has shown that wide variations continue to exist (Sidhu and others, 2007).
Euthanasia/medically assisted suicide
Euthanasia/medically assisted suicide involves the deliberate administration of a lethal substance to end a patient’s life, usually in a clinical context (Johnstone, 2009a). Some people request euthanasia in instances where they have come to view their life or suffering as ‘unbearable’. More recently, supporters of euthanasia have advocated advance euthanasia directives (also called ‘preemptive euthanasia’) whereby requests for euthanasia are made in advance of an anticipated state of suffering (mental or physical) being experienced (Hertogh, 2009). Nurses, like others in the community, hold diverse values, opinions and beliefs about the moral permissibility of euthanasia/medically assisted suicide and whether it should be legalised. Of particular concern to nurses in Australia and New Zealand (where euthanasia is illegal) is the confronting question of whether the nursing profession should formally and publicly support calls for the legalisation of euthanasia/medically assisted suicide and whether nursing organisations should adopt a formal policy position to this effect (Johnstone, 2010a). Also confronting is the question of whether nurses should themselves assist with performing euthanasia in the event of it being made legal. Nurses and professional nursing organisations have an obvious stake in the outcome of the euthanasia/medically assisted suicide debate (Johnstone, 2010a). Accordingly, nurses have a moral and professional responsibility to ensure that they are kept well informed about the issues in question and keep abreast of developments discussed critically in the legal and bioethics literature. This includes questioning and calling into question public opinion, which indicates nothing more than a certain percentage of the population holding a particular opinion on the matter. Whether public opinion (which currently favours the legalisation of euthanasia) has the authority to prescribe a society’s moral values is another matter entirely (Johnstone, 2009a).
Access and equity in healthcare
Access and equity in healthcare are poised to become the most pressing ethical issues in the 21st century. This is because over the next 40 years, population ageing, the increasing burden of chronic disease, the possible health consequences of climate change and the depletion of the world’s non-renewable resources (e.g. petroleum) will all place unprecedented and overwhelming demands on the healthcare system and the individuals comprising it. In the case of population ageing, people over the age of 65 years are expected to become frequent users of the public health system and that ‘real health spending’ during the period 2010 to 2050 will increase exponentially for this population group (Johnstone, 2010b; Johnstone and Kanitsaki, 2009c). Critics contend that the costs associated with an ageing population and associated burden of chronic disease will be so high that the level of healthcare currently being provided will not be sustainable. The future will therefore be one in which ‘tough moral choices’ will have to be made.
Adding to the problem of future access to and equity in healthcare is the potential negative impact of climate change. Experts predict that climate change will see a significant increase in illness and deaths from frequent and severe heat-waves, vector-borne diseases, and other extreme weather events (McMichael and others, 2006). Peak petroleum (the point at which the world’s oil reserves begin to decline, which some say may already have been reached) will also affect healthcare delivery in deleterious ways (Frumkin and others, 2007, 2009; Hess and others, 2011; Schwartz and others, 2011). This is because healthcare services are utterly dependent on petroleum products (e.g. medical supplies and equipment, pharmaceuticals, transportation and service delivery, and energy) without which they will come to a halt (Johnstone, 2011c).
In order to mitigate the negative impact of these developments, authorities have increasingly emphasised the need for healthcare reform and a more responsive and better coordinated healthcare system. Healthcare reform, in this instance, has been clarified to include making adjustments to healthcare spending in order to obtain ‘better value for money’. Some argue, however, that healthcare reform is not just a matter of making the system ‘work better’. Callahan suggests, for example, that if the common good is to be achieved, we need to rethink some of our fundamental values about health and healthcare. This, he suggests, is going to require a ‘cultural revolution’ in our thinking about medical technology, progress, dying, death and ageing, because the brutal reality is that ‘there are no reliable or seriously envisioned practical and politically accepted means of managing costs anywhere near the extent that is necessary’ (Callahan, 2009). He further argues that when the costs of the benefits of medical technology begin to exceed what a community or nation can afford, then questions need to be raised about when ‘enough is enough’ and how the point of ‘enough’ might be determined (Callahan, 2009).
The complex of population ageing, the increasing burden of chronic disease, climate change and the depletion of the world’s non-renewable resources raises critical questions about how prepared the nursing profession is to respond to what have been termed the ‘three Rs’ (Wynia, 2007) when faced with ‘extreme events’, that is: rationing (e.g. of medications), restrictions (e.g. on people’s access to and from healthcare services) and responsibilities (of healthcare professionals to continue providing care and treatment when resources are scarce or depleted).
The ethical consequences of these evolving scenarios are likely to be incremental, rather than sudden. Even so, without forward planning encompassing a comprehensive vulnerability analysis, nurses will not be well placed to prepare for or mitigate the tough ethical challenges and choices that lay ahead.
Being ethical in extreme situations can be particularly challenging because it may not be clear what the right thing to do is. Considering ethical quandaries in advance will help mitigate this difficulty. In the meantime, it is timely for attention to be given to the following questions:
• What steps need to be taken now to ensure the development of a viable and sustainable healthcare system that is responsive and well coordinated to meet the needs of future generations?
• Will the solutions proposed be effective and just?
• What processes does the nursing profession need to engage in if it is to contribute meaningfully to public policy debate and agenda setting for achieving a sustainable and just healthcare system for all people across the lifespan?
‘Everyday’ ethical issues in nursing
As well as having to deal with the procedural issues of ethics—that is, identifying ethical issues and responding to them effectively—and the ‘life and death’ issues commonly associated with the discipline of bioethics, nurses have to grapple with ‘everyday’ ethics. Everyday ethics in nursing derives from the experiences of nurses (and their clients) in day-to-day ‘hands-on’ practice. Unlike the more ‘exotic’ issues of bioethics (discussed above), everyday ethics in nursing concern such things as:
• catalysts to moral action (e.g. the look of suffering in a patient’s eyes)
• operating moral values (e.g. sympathy, empathy, compassion)
• ethical decision-making processes in nursing and healthcare contexts
• barriers to ethical practice
When nurses talk about everyday ethical issues, their conversations are not about the so-called paramount or exotic issues of bioethics (such as euthanasia, abortion and IVF), but about the more fundamental issues of (Johnstone, 2009b):
• how to help a patient in distress in the ‘here and now’
• how to stop ‘things going bad for a patient’
• how to best support a relative or chosen carer during times of distress and when the ‘system’ appears to be against them
• how to make things ‘less traumatic’ for someone who is suffering
• how to reduce the anxiety and vulnerability of the people being cared for
• where nurses can get help for their own moral distress
• how to make a difference in contexts where indifference to the moral interests of others is manifest.
The moral responsibility of nurses to engage in ‘self-care’ (see Value statement 4 of the Code of ethics for nurses in Australia (Australian Nursing and Midwifery Council, 2008a)) is another ‘everyday’ issue that is finding its way into the conversation of nurses.
The above concerns are just as worthy of attention by nurses and others as are the more ‘exotic’ issues of bioethics. The everyday ethical issues identified constitute an important component of nursing ethics and warrant in-depth consideration in the interests of promoting ethical practice in nursing and related care contexts.
Conclusion
The courage and intelligence to act, both as an advocate for clients and as a professional member of the healthcare team, comes only after a committed effort to learn and to understand ethical issues in nursing and healthcare. The professional nurse has an important point of view regarding clients, the healthcare system that supports clients and the institutions that constitute the healthcare system. The nurse both owes a duty and enjoys a privilege to articulate that point of view. Learning the language of ethics is a part of the skill necessary to exercise this duty and privilege. In addition, review and contemplation of various ethical constructions of different issues assists nurses in the formulation of considered ethical professional points of view, a necessary ingredient in the negotiation of difficult ethical situations.
KEY CONCEPTS
• Ethics involves thinking critically about and engaging in a systematic examination of what constitutes right and wrong/good and bad behaviour, and the bases upon which we might justify our judgments about the ideals of right and wrong behaviour.
• Bioethics refers specifically to ethical issues that arise in the context of biomedical research and healthcare service delivery.
• Nursing ethics involves the examination of all sorts of ethical issues from the perspective of nursing theory and practice.
• A code of ethics is a conventionalised set of rules of expectations devised for the purposes of guiding ethical professional conduct.
• The study of ethics, bioethics and nursing ethics is of fundamental importance for members of the nursing profession.
• Nurses are morally accountable and morally responsible for their actions.
• Nurses maintain ethical competence in practice and assume responsibility for nursing judgments.
• Nurses have a professional ethical responsibility to clients, the profession and society to provide high-quality healthcare and to maximise client wellbeing and welfare.
• Common ethical principles used to guide decision making and conduct in healthcare are autonomy, beneficence, non-maleficence and justice; they are not, however, the only guides to moral conduct and may even be inappropriate for guiding decision making in some cultural contexts.
• Rights and duties are also important considerations in guiding moral decision making and conduct in healthcare settings.
• Ethics is the product of the culture from which it has arisen and is fundamentally concerned with the promotion of human wellbeing and welfare.
• Moral problems can arise when practitioners lack educational preparation for dealing with ethical issues in the workplace. These include differences in moral values, beliefs and attitudes and commitment with respect to performing one’s moral duty. Professional role change, technological advances and social issues also challenge unthinking perspectives about what constitutes the moral life.
• Moral problems can be resolved by using a systematic process for moral decision making and action. Critical thinking is an important part of this process.
• Moral problems may occur in any segment of the healthcare delivery system.
• Moral mistakes can be made when nurses and allied health workers ‘rush to judgment’ and rely on personal opinion, values and beliefs rather than evidence and sound moral theory to guide their moral decision making and actions.
• The nurse’s observations and considered judgments (the ‘nursing point of view’) can play a vital role in the correct identification and resolution of moral problems.
Australian Nursing and Midwifery Council (ANMC). National competency standards for the registered nurse. Canberra: ANMC, 2006. Online Available at www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/Codes-Guidelines.aspx 24 Apr 2012.
Australian Nursing and Midwifery Council (ANMC). Code of ethics for nurses in Australia. Canberra: ANMC, 2008. Online Available at www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/Codes-Guidelines.aspx 24 Apr 2012.
Australian Nursing and Midwifery Council (ANMC). Code of professional conduct for nurses in Australia. Canberra: ANMC, 2008. Online Available at www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/Codes-Guidelines.aspx 24 Apr 2012.
Beauchamp T, Childress J. Principles of biomedical ethics, ed 3. New York: Oxford University Press, 1989.
Beauchamp T, Childress J. Principles of biomedical ethics, ed 6. New York: Oxford University Press, 2009.
Benner P, Wrubel J. The primacy of caring. Menlo Park, CA: Addison-Wesley, Nursing Division, 1989.
Bentham J. An introduction to the principles of morals and legislation (reprinted from 1789 ed). Utilitarianism (reprinted from 1859 ed). In: Warnock M, ed. Utilitarianism. London: Fontana Library/Collins, 1962.
Callahan D. Taming the beloved beast: how medical technology costs are destroying our health care system. Princeton: Princeton University Press, 2009.
Campbell T. Rights: a critical introduction. London: Routledge, 2006.
Churchill L. Reviving a distinctive medical ethic. Hastings Center Report. 1989;19(3):28.
Coady M, Bloch S, eds. Codes of ethics and the professions. Melbourne: Melbourne University Press, 1996.
Divi C, et al. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. 2007;19(2):60.
Dudzinski D, Shannon E. Competent patients’ refusal of nursing care. Nursing Ethics. 2006;13(6):608–621.
Dyck A. Rethinking rights and responsibilities: the moral bonds of community. Washington DC: Georgetown University Press, 2005.
Faden RR, Beauchamp TL. A history and theory of informed consent. New York: Oxford University Press, 1986.
Feinberg J. The rights of animals and unborn generations. In: Wasserstrom RA, ed. Today’s moral problems. New York: Macmillan, 1979.
Frumkin H, et al. Peak petroleum and public health. JAMA. 2007;298(14):1688–1690.
Frumkin H, et al. Energy and public health: the challenges of peak petroleum. Public Health Rep. 2009;124:5–19.
Fry S, Johnstone M. Ethics in nursing practice: a guide to ethical decision making, ed 3. Geneva: International Council of Nursing/Oxford, Blackwell, 2008.
Fry-Revere S. The accountability of bioethics committees and consultants. Frederick: University Publishing Group, 1992.
Gaut D. The presence of caring in nursing. New York: National League for Nursing Press, 1991.
Gaut D, Leininger M. Caring: the compassionate healer. New York: National League for Nursing Press, 1991.
Hertogh C. The role of advance euthanasia directives as an aid to communication and shared decision-making in dementia. J Med Ethics. 2009;35(2):100–103.
Hess J, et al. Petroleum and health care; evaluating and managing health care’s vulnerability to petroleum supply shifts. Am J Public Health. 2011;101(9):1568–1579.
International Council of Nurses (ICN). The ICN code of ethics for nurses. Geneva: ICN, 2006.
Jecker N, et al. Bioethics: an introduction to the history, methods, and practice, ed 3. Sudbury MA: Jones & Bartlett, 2011.
Johnstone M. Nursing and the injustices of the law. Sydney: WB Saunders/Baillière Tindall, 1994.
Johnstone M. Bioethics: a nursing perspective, ed 5. Sydney: Churchill Livingstone, 2009.
Johnstone M. Ethics in nursing. In Daly J, Speedy S, Jackson D, eds.: Contexts of nursing, ed 3, Sydney: Churchill Livingstone, 2009.
Johnstone M. Position statements on euthanasia. Austral Nurs J. 2010;18(6):24.
Johnstone M. Health care justice for the ageing. Austral Nurs J. 2010;17(9):29.
Johnstone M. Ethics, cancer and truth telling. Aust Nurs J. 2011;18(8):21.
Johnstone M. Nursing and justice as a basic human need. Nurs Philosophy. 2011;12:34–44.
Johnstone M. Peak oil and health care without plastic. Austral Nurs J. 2011;18(10):29.
Johnstone M, Kanitsaki O. Culture, language and patient safety: making the link. Int J Qual Health Care. 2006;18(5):383.
Johnstone M, Kanitsaki O. Cultural diversity and the Australian healthcare system. In: Barrowclough S, Gardner H, eds. Analysing Australian health policy: a problem orientated approach. Sydney: Elsevier, 2008.
Johnstone M, Kanitsaki O. Ethics and advance care planning in a culturally diverse society. J Transcultural Nurs. 2009;20(4):405–416.
Johnstone M, Kanitsaki O. The spectrum of ‘new racism’ and discrimination in health care: a reappraisal. Collegian. 2009;16(2):63–69.
Johnstone M, Kanitsaki O. Population ageing and the politics of demographic alarmism: implications for the nursing profession. Austral J Adv Nurs. 2009;26(3):86–92.
Johnstone M, Kanitsaki O. The neglect of racism as an ethical issue in health care. J Immigrant Minority Health. 2010;12:489–495.
Jonsen A, et al. Clinical ethics: a practical approach to ethical decisions in clinical medicine. New York: McGraw-Hill Medical, 2010.
Jormsri P, et al. Moral competence in nursing practice. Nurs Ethics. 2005;12(6):582–594.
Kant I. The moral law (translated by Paton HJ). London: Hutchinson University Library, 1972.
Kerridge I, et al. Ethics and law for the health professions, ed 3. Sydney: Federation Press, 2009.
LaFollette H, ed. Ethics in practice, ed 3, Malden MA: Blackwell, 2007.
Leininger M. Care: the essence of nursing and health. Detroit: Wayne State University Press, 1988.
Leininger M. Ethical and moral dimensions of care. Detroit: Wayne State University Press, 1990.
Lichtenberg J. What are codes of ethics for? In: Coady M, Bloch S, eds. Codes of ethics and the professions. Melbourne: Melbourne University Press, 1996.
McMichael AJ, et al. Climate change and human health: present and future risks. Lancet. 2006;367(9513):859–869.
Manson NC, O’Neill O. Rethinking informed consent in bioethics. Cambridge: Cambridge University Press, 2007.
Mill JS. Utilitarianism (reprinted from 1859 ed). In: Warnock M, ed. Utilitarianism. London: Fontana Library/Collins, 1962.
Millgram E. What’s the use of utility? Philosophy Public Affairs. 2000;29(2):113–136.
Morriston W. What if God commanded something terrible? A worry for divine-command meta-ethics. Religious Stud. 2009;45:249–267.
Myhrvold T. The different other—towards an including ethics of care. Nurs Philosophy. 2006;7(3):125.
New Zealand Nurses Organisation (NZNO). Code of ethics. Wellington: NZNO, 2010.
Nursing Council of New Zealand (NCNZ). Code of conduct for nurses. Wellington: NCNZ, 2009.
Nursing Council of New Zealand (NCNZ). Competencies standards for registered nurses. Wellington: NCNZ, 2009.
Nussbaum M. Frontiers of justice: disability, nationality, species membership. Cambridge MA: The Belknap Press of Harvard University Press, 2006.
Oakley J. Virtue ethics and professional roles. Cambridge: Cambridge University Press, 2006.
Pence G. Virtue theory. In: Singer P, ed. A companion to ethics. Oxford: Wiley-Blackwell, 1991.
Rapley M. Quality of life research: a critical introduction. London: Sage Publications, 2003.
Reich W. The word ‘bioethics’: its birth and the legacies of those who shaped it. Kennedy Inst Ethics J. 1994;4(4):319.
Reich W. The word ‘bioethics’: the struggle over its earliest meanings. Kennedy Inst Ethics J. 1995;5(1):19.
Roach MS. The human act of caring: a blueprint for the health professions. Ottawa: Canadian Hospital Association, 1987.
Rosen F. Classical utilitarianism from Hume to Mill. London: Routledge, 2003.
Schneiderman L, Jecker N. Wrong medicine: doctors, patients and futile treatment, ed 2. Baltimore/London: Johns Hopkins University Press, 2011.
Schwartz BS, et al. Public health and medicine in an age of energy scarcity: the case of petroleum. Am J Public Health. 2011;101(9):1560–1567.
Sen A. The idea of justice. London: Allen Lane, 2009.
Sidhu NS, et al. ‘Not-for-resuscitation’ orders in Australian public hospitals: policies, standardised order forms and patient information leaflets. Med J Austral. 2007;186(2):72–75.
Skene L. A legal perspective on codes of ethics. In: Coady M, Bloch S, eds. Codes of ethics and the professions. Melbourne: Melbourne University Press, 1996.
Spencer E, et al. Organization ethics in healthcare. New York: Oxford University Press, 2000.
Taylor A, ed. Justice as a basic human need. New York: Nova Science Publishers, 2006.
United Nations. The United Nations declaration of human rights. New York: United Nations, 1948.
Wainwright WJ. Religion and morality. Aldershot: Ashgate, 2005.
Van Hooft S. Understanding virtue ethics. Chesham, UK: Acumen Publishing, 2006.
Watson J. Nursing: the philosophy and science of caring. Boulder: Colorado Associated University Press, 1985.
Watson J. Nursing: human science and human care: a theory of nursing. Norwalk: Appleton-Century-Crofts, 1985.
Weller P. Human rights, health rights and the jurisprudence of public health law. In: Freckelton I, Petersen K, eds. Disputes and dilemmas in health law. Sydney: The Federation Press, 2006.
Wynia M. Ethics and public health emergencies: encouraging responsibility. Am J Bioethics. 2007;7(4):1–4.