Chapter 38 NURSING ASSESSMENT: gastrointestinal system
1. Describe the structures and functions of the organs of the gastrointestinal tract.
2. Describe the structures and functions of the liver, gall bladder, biliary tract and pancreas.
3. Explain the processes of ingestion, digestion, absorption and elimination.
4. Explain the processes of biliary metabolism, bile production and bile excretion.
5. Describe age-related changes in the gastrointestinal system and differences in assessment findings.
6. Identify the significant subjective and objective data related to the gastrointestinal system that should be obtained from a patient.
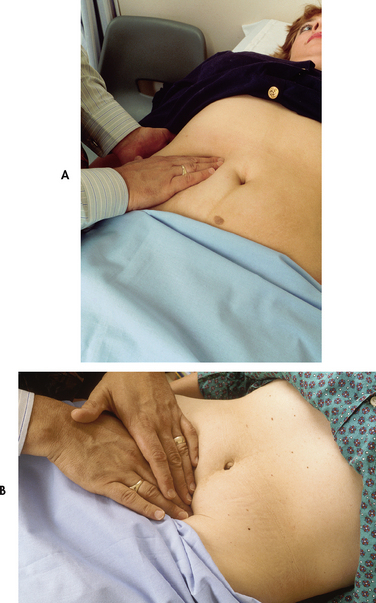
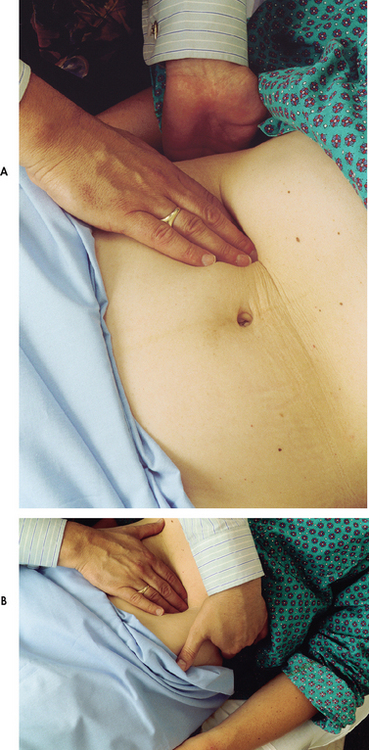
7. Describe the appropriate techniques used in the physical assessment of the gastrointestinal system.
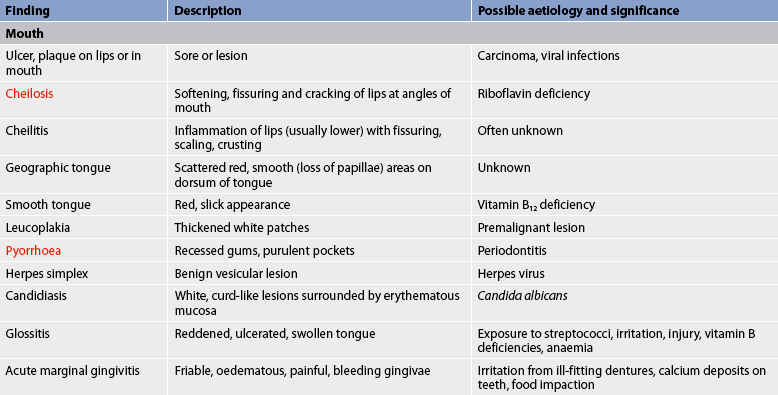
8. Differentiate between normal and common abnormal findings of a physical assessment of the gastrointestinal system.
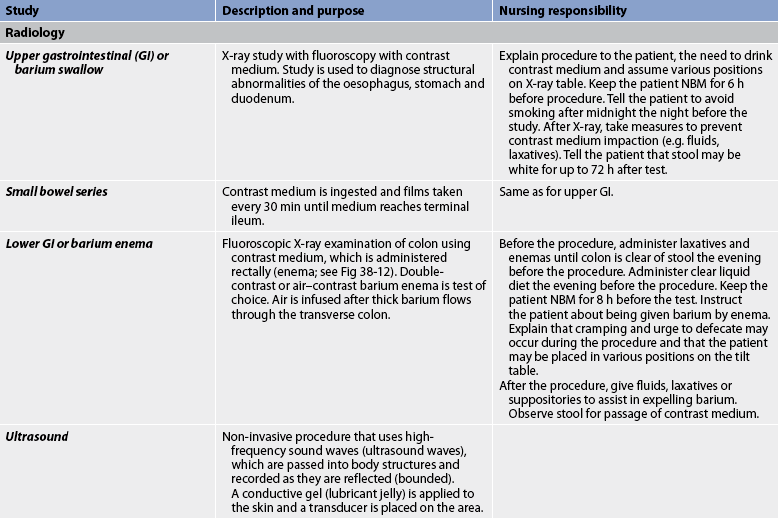
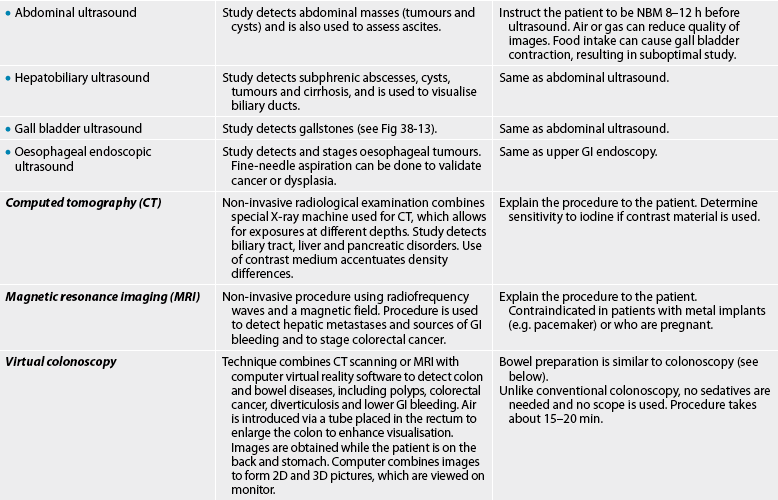
9. Describe the purpose, significance of results and nursing responsibilities related to diagnostic studies of the gastrointestinal system.
Structures and functions of the gastrointestinal system
The main function of the gastrointestinal (GI) system is to supply nutrients to body cells. This is accomplished through the processes of ingestion (taking in food), digestion (breakdown of food) and absorption (transfer of food products into circulation). Elimination is the process of excreting the waste products of digestion.
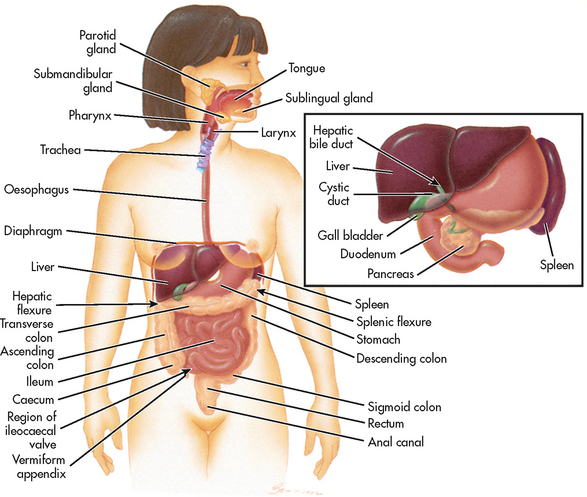
The GI system (also called the digestive system) consists of the GI tract and its associated organs and glands. Included in the GI tract are the mouth, oesophagus, stomach, small intestine, large intestine, rectum and anus. The associated organs are the liver, pancreas and gall bladder (see Fig 38-1).
Factors outside the GI tract can influence its functioning. Both psychological and emotional factors, such as stress and anxiety, influence GI functioning in many people. Stress may be manifested as anorexia, epigastric and abdominal pain, or diarrhoea or constipation. However, GI problems should never be attributed solely to psychological factors. Organic and psychologically based problems can exist independently or concurrently. Physical factors, such as dietary intake, ingestion of alcohol and caffeine-containing products, cigarette smoking, poor sleep, fatigue, mobility and exercise may also affect GI function. Some organic diseases of the GI system, such as peptic ulcer disease and ulcerative colitis, may be aggravated by stress.
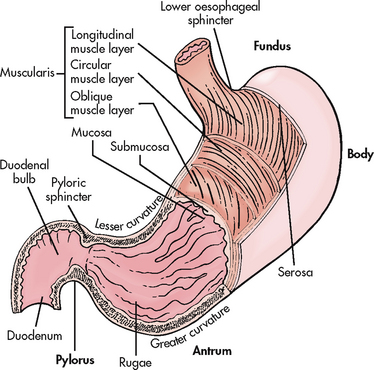
The GI tract is a tube approximately 9 m long extending from the mouth to the anus. The entire tract is composed of four common layers. From the inside to the outside, these layers are: (1) mucosa; (2) submucosa; (3) muscularis; and (4) serosa (see Fig 38-2). In the oesophagus the outer coat is fibrous tissue rather than serosa. The muscular coat of the GI tract usually consists of two layers: the longitudinal (outer) layer and the circular (inner) layer, but within the proximal stomach there is an additional inner coat of oblique muscle.
The GI tract is innervated by the parasympathetic and the sympathetic branches of the autonomic nervous system. The parasympathetic system is mainly excitatory and the sympathetic system is mainly inhibitory. For example, peristalsis is increased by parasympathetic stimulation and decreased by sympathetic stimulation. Sensory information is relayed via both sympathetic and parasympathetic afferent fibres.
The GI tract also has its own nervous system: the enteric, or intrinsic, nervous system. The enteric nervous system is composed of two nerve layers that lie between the mucosa and the circular muscle layer and the circular and longitudinal muscle layers. These neurons contribute to the coordination of GI motor and secretory activities. The enteric nervous system is also known as the ‘gut brain’. It contains numerous neurons (about as many as the spinal cord) and has the ability to control movement and secretion of the GI tract.
The GI tract and accessory organs receive approximately 25–30% of the cardiac output. Circulation in the GI system is unique in that venous blood draining the GI tract organs empties into the portal vein, which then perfuses the liver. The upper portion of the GI tract receives its blood supply from the splanchnic artery. The small intestine receives its blood supply from branches of the hepatic and superior mesenteric arteries. The large intestine receives its blood supply mainly from the superior and inferior mesenteric arteries. Because such a large percentage of the cardiac output perfuses these organs, the GI tract is a major source from which blood flow can be diverted during exercise or stress.
The two types of movement of the GI tract are mixing (segmentation) and propulsion (peristalsis). The secretions of the GI system consist of enzymes and hormones for digestion, mucus to provide protection and lubrication, and water and electrolytes.
The abdominal organs are almost completely covered by the peritoneum. The two layers of the peritoneum are the parietal, which lines the abdominal cavity wall, and the visceral, which covers the abdominal organs. The peritoneal cavity is the potential space between the parietal and visceral layers. The two folds of the peritoneum are the mesentery and the omentum. The mesentery attaches the small intestine and part of the large intestine to the posterior abdominal wall and contains blood and lymph vessels. The lesser omentum goes from the lesser curvature of the stomach and upper duodenum to the liver, and the greater omentum hangs from the stomach over the intestines like an apron. The omentum contains fat and lymph nodes.
The primary functions of the GI system are: (1) ingestion and propulsion (movement) of food; (2) digestion; (3) absorption; and (4) elimination. Each part of the GI system performs different activities to accomplish these functions.
INGESTION AND PROPULSION OF FOOD
Ingestion is the intake of food. A person’s appetite or desire to ingest food is a significant factor in how much food is eaten. Multiple factors are involved in the control of appetite. An appetite centre is located in the hypothalamus. It is directly or indirectly stimulated by hypoglycaemia, an empty stomach, a decrease in body temperature and input from higher brain centres. The hormone ghrelin released from the stomach mucosa plays a role in appetite stimulation. Another hormone, leptin, is involved in appetite suppression. The sight, smell and taste of food frequently stimulate appetite. Appetite may be inhibited by stomach distension, illness (especially accompanied by fever), hyperglycaemia, nausea and vomiting, certain drugs (e.g. amphetamines) and medical conditions, such as hiatus hernia and achalasia.
Deglutition (swallowing) is the mechanical component of ingestion. The organs involved in the deglutition of food are the mouth, pharynx and oesophagus.
Mouth
The mouth consists of the lips and oral (buccal) cavity. The lips surround the orifice of the mouth and function in speech. The roof of the oral cavity is formed by the hard and soft palates. The oral cavity contains the teeth, used in mastication (chewing), and the tongue. The tongue is a solid muscle mass that assists in mastication by keeping food between the teeth during chewing and moving the food to the back of the throat for swallowing (deglutition). Taste receptors are found on the sides and tip of the tongue. The tongue is also important in speech.
Within the oral cavity are three pairs of salivary glands: the parotid, submaxillary and sublingual. These glands produce saliva, which consists of water, protein, mucin, inorganic salts and salivary amylase. Approximately 1 L of saliva is produced each day. Saliva serves many roles, including the lubrication of food and the prevention of bacterial overgrowth in the oral cavity.
Pharynx
The pharynx is a musculomembranous tube that may be divided into the nasopharynx, oropharynx and laryngeal pharynx. The mucous membrane of the pharynx is continuous with the nasal cavity, mouth, auditory tubes and larynx. The oropharynx secretes mucus, which aids in swallowing. The epiglottis is a lid of fibrocartilage that closes over the larynx during swallowing. During ingestion the oropharynx provides a route for food from the mouth to the oesophagus. When receptors in the oropharynx are stimulated by food or liquid, the swallowing reflex is initiated.
Oesophagus
The oesophagus is a hollow, muscular tube that receives food from the pharynx and moves it to the stomach by peristaltic contractions. It is 23–25 cm long and 2 cm in diameter. The oesophagus is located in the thoracic cavity and starts behind the trachea at the lower end of the pharynx and extends to the stomach. The upper one-third of the oesophagus is composed of striated skeletal muscle and the distal two-thirds are composed of smooth muscle.
With swallowing, the upper oesophageal sphincter (cricopharyngeal muscle) relaxes and a peristaltic wave moves the bolus (masticated food) into the oesophagus. The muscular layers contract (peristalsis) and propel the food to the stomach. The lower oesophageal sphincter (LOS) at the distal end of the oesophagus remains contracted except during swallowing, belching or vomiting. The LOS is an important barrier that prevents reflux of acidic gastric contents into the oesophagus.
DIGESTION AND ABSORPTION
Mouth
Digestion begins in the mouth and involves both mechanical (mastication) and chemical digestion. Saliva is the first secretion involved in digestion and its main function is to lubricate and soften the food mass, thus facilitating swallowing. Saliva contains amylase (ptyalin), which hydrolyses starches to maltose. However, salivary amylase is not necessary for the digestion of carbohydrates. (See Fig 38-3, which illustrates the absorption sites of different substances in the digestive tract.)
Stomach
The functions of the stomach are to store food, mix the food with gastric secretions and empty the contents into the small intestine at a rate at which digestion can occur. The stomach absorbs only small amounts of water, alcohol, electrolytes and certain drugs.
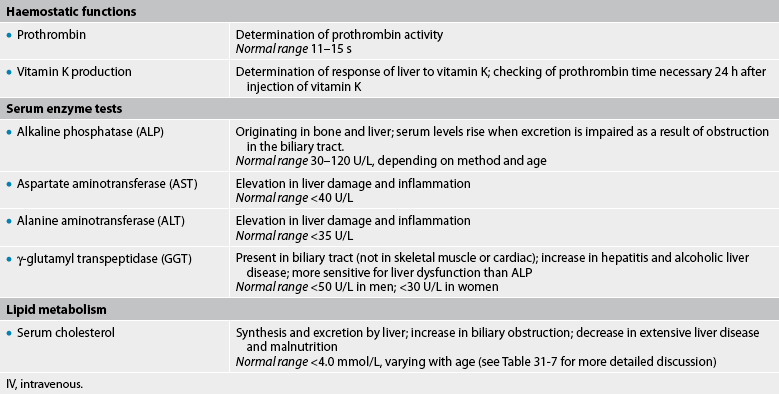
The stomach lies obliquely in the epigastric, umbilical and left hypochondriac regions of the abdomen (see Fig 38-8). The shape and position of the stomach change depending on the degree of gastric distension. It always contains gastric fluid and mucus. The three main parts of the stomach are the fundus, the body and the antrum (see Fig 38-2). The pylorus is a small portion of the antrum that lies proximal to the pyloric sphincter. Sphincter muscles (the LOS and the pyloric sphincter) guard the entrance to, and exit from, the stomach. The cardiac orifice is the opening between the oesophagus and the stomach.
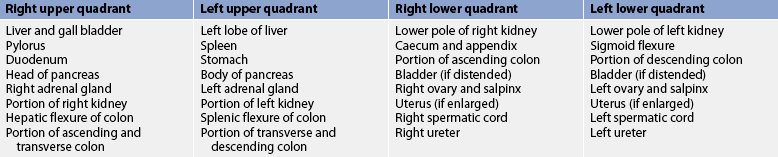
Figure 38-8 A, Abdominal quadrants. B, Abdominal regions. LLQ, left lower quadrant; LUQ, left upper quadrant; RLQ, right lower quadrant; RUQ, right upper quadrant.
The serosa (outer layer) of the stomach is formed by the peritoneum. The muscular layer consists of the longitudinal (outer) layer, circular (middle) layer and oblique (inner) layer. The mucosal layer forms folds called rugae that contain many small glands. In response to nutrient intake, these glands work to secrete most of the gastric juice and to control the rate of passage of food to the duodenum. In the fundus the glands contain chief cells, which secrete pepsinogen, and parietal cells, which secrete hydrochloric acid (HCl), water and intrinsic factor. The secretion of HCl makes gastric juice acidic in comparison to other body fluids. This acidic pH aids in the protection against ingested organisms. Intrinsic factor promotes vitamin B12 absorption in the small intestine. Mucus is secreted by glands in the cardiac and pyloric areas.
Small intestine
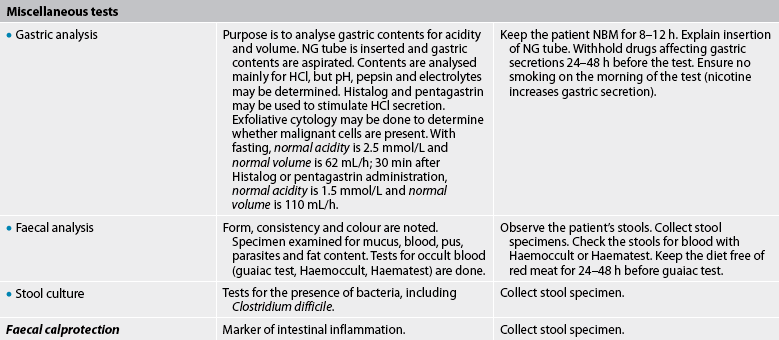
The two primary functions of the small intestine are digestion and absorption (uptake of nutrients from the gut lumen to the bloodstream). The small intestine is a coiled tube approximately 7 m in length and 2.5–2.8 cm in diameter, diminishing in diameter at the lower end. It extends from the pylorus to the ileocaecal valve. The small intestine is composed of the duodenum, the jejunum and the ileum. The ileocaecal valve, which separates the small intestine from the large intestine, prevents reflux of large intestine contents into the small intestine.
The serosa of the small intestine is formed by the peritoneum. The mucosa is thick, vascular and glandular. The circular folds in the mucosal and submucosal layers provide a greater surface area for digestion and absorption.
The functional units of the small intestine are the villi. They are present in the entire small intestine. Villi are minute, finger-like projections of the mucous membrane. They contain goblet cells, which secrete mucus, and epithelial cells, which produce intestinal digestive enzymes. The epithelial cells also have microvilli, which compose the brush border. There are, on average, 4–5 million villi present in the normal small bowel. Thus, the presence of villi and microvilli increases the absorptive capacity of the small bowel approximately 600-fold.
The digestive enzymes on the brush border of the microvilli chemically break down nutrients so that they can be absorbed. The villi are surrounded by the crypts of Lieberkühn, which contain the base columnar cells that are the stem cells for the other epithelial cell types. Brunner’s glands in the submucosa of the duodenum secrete mucus.
Physiology of digestion
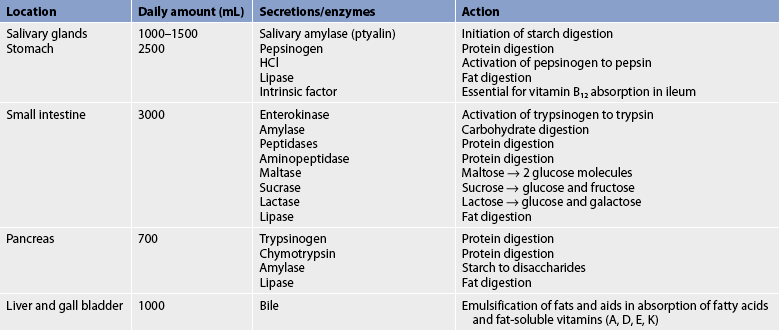
Digestion is the physical and chemical breakdown of food into absorbable substances. Digestion in the GI tract is facilitated by the timely movement of food through the various organs and the secretion of specific enzymes. These enzymes break down foodstuffs to appropriately sized particles for absorption (see Table 38-1).
The process of digestion begins in the mouth, where the food is chewed, mechanically broken down and mixed with saliva. The saliva lubricates the food. In addition, salivary amylase begins the breakdown of starch. Salivary gland secretion is stimulated by chewing movements and the sight, smell, thought and taste of food. The food is swallowed and passes into the oesophagus, where peristaltic waves propel it to the stomach. No digestion or absorption occurs in the oesophagus.
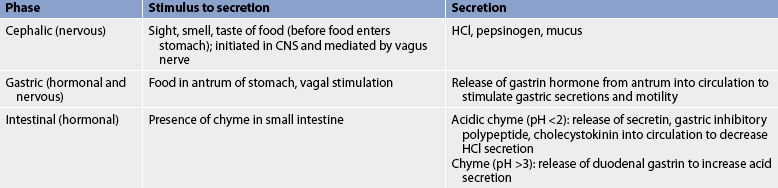
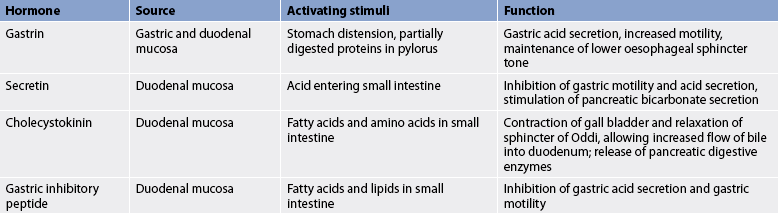
In the stomach the digestion of proteins begins with the release of pepsinogen from chief cells. The acidic environment of the stomach results in the conversion of pepsinogen to its active form, pepsin. Pepsin begins the initial breakdown of proteins. In the stomach there is minimal digestion of starches and fats. The food is mixed with gastric secretions, which are under neural and hormonal control (see Tables 38-2 and 38-3). The stomach also serves as a reservoir for food, which is slowly expelled into the small intestine. The length of time that food remains in the stomach depends on the composition of the food but average meals remain from 3 to 4 hours.
Digestion is completed in the small intestine, where carbohydrates are hydrolysed to monosaccharides, fats to glycerol and fatty acids, and proteins to amino acids. The physical presence of chyme (food mixed with gastric secretions), along with its chemical nature in the small intestine, stimulates motility and secretion. Secretions involved in digestion include enzymes from the pancreas, bile from the liver (see Table 38-1) and intestinal secretions from glands in the small intestine. Both secretion and motility are under neural and hormonal control.
When food enters the stomach and small intestine, hormones are released into the bloodstream (see Table 38-3). The hormone secretin stimulates the pancreas to secrete fluid with a high concentration of bicarbonate. This alkaline secretion enters the duodenum and neutralises acid in the chyme. The duodenal mucosa also secretes mucus to protect against the HCl. In response to the presence of chyme, the hormone cholecystokinin (CCK), produced by the duodenal mucosa, enters the bloodstream and stimulates contraction of the gall bladder and relaxation of the sphincter of Oddi. These actions permit bile to flow from the common bile duct into the duodenum. Bile is necessary for the digestion of fats. CCK also stimulates the pancreas to synthesise and secrete enzymes for enzymatic digestion of carbohydrates, fats and proteins.
Enzymes present on the brush border of the microvilli complete the digestion process. These enzymes hydrolyse disaccharides to monosaccharides and peptides to amino acids for absorption.
Absorption is the transfer of the end products of digestion across the intestinal wall to the circulation. Most absorption occurs in the small intestine. The surface area of the small intestine is greatly increased by its circular folds, villi and microvilli. The movement of the villi enables the end products of digestion to come in contact with the absorbing membrane. Monosaccharides (from carbohydrates), fatty acids (from fats), amino acids (from proteins), water, electrolytes and vitamins are absorbed.
ELIMINATION
Large intestine
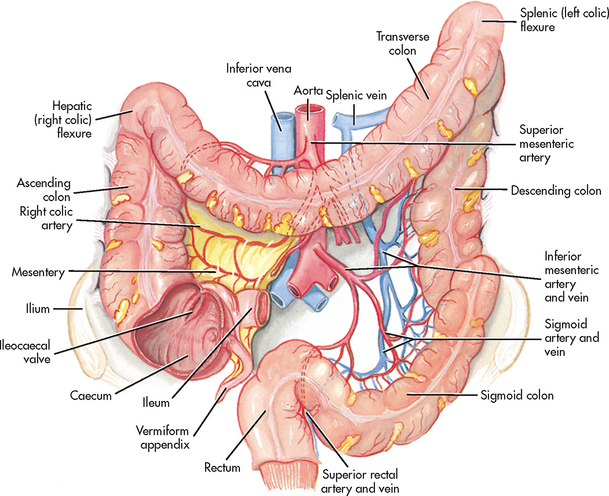
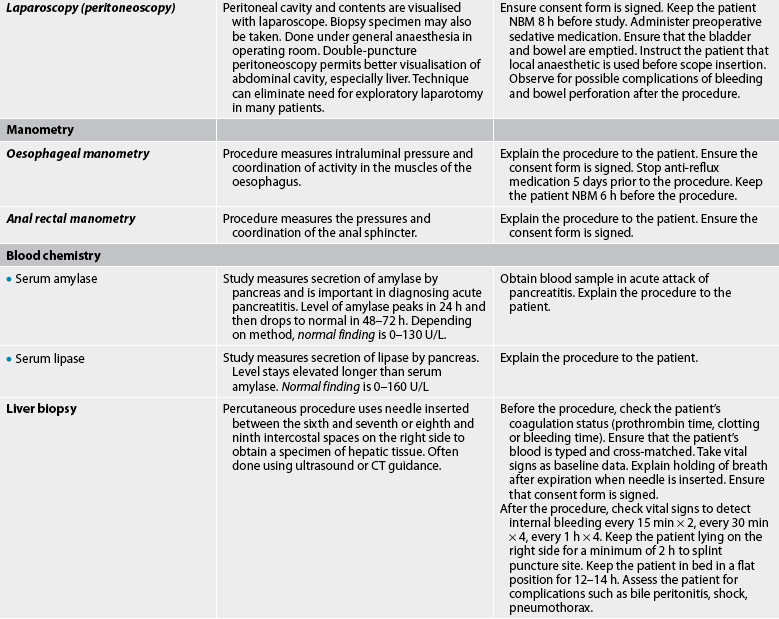
The large intestine is a hollow, muscular tube approximately 1.5–2 m long and 5 cm in diameter. The four parts of the large intestine are: (1) the caecum and the appendix, a narrow tube at the end of the caecum; (2) the colon (ascending colon on the right side, transverse colon across the abdomen, descending colon on the left side, and sigmoid colon); (3) the rectum; and (4) the anus, the terminal portion of the large intestine (see Fig 38-4).
The most important function of the large intestine is the absorption of water and electrolytes. It also forms faeces and serves as a reservoir for the faecal mass until defecation occurs. Faeces are composed of water (75%), bacteria, unabsorbed minerals, undigested foodstuffs, bile pigments and desquamated epithelial cells. The large intestine secretes mucus, which acts as a lubricant and protects the mucosa.
Microorganisms in the colon are responsible for the breakdown of proteins that are not digested or absorbed in the small intestine. These amino acids are deaminated by the bacteria, leaving ammonia, which is carried to the liver and converted to urea. Bacteria in the colon synthesise vitamin K and some of the B vitamins. Bacteria also play a part in the production of flatus.
The movements of the large intestine are usually slow. When the circular muscles contract, they produce a kneading action termed haustral churning. Propulsive (mass movement) peristalsis also occurs. When food enters the stomach and duodenum, the gastrocolic and duodenocolic reflexes are initiated, resulting in peristalsis in the colon. These reflexes are more active after the first daily meal and frequently result in bowel evacuation.
Defecation is a reflex action involving voluntary and involuntary control. Faeces in the rectum stimulate sensory nerve endings that produce the desire to defecate. The reflex centre for defecation is in the sacral portion of the spinal cord (parasympathetic nerve fibres). These fibres produce contraction of the rectum and relaxation of the internal anal sphincter. Defecation is controlled voluntarily by relaxing the external anal sphincter when the desire to defecate is felt. An acceptable environment for defecation is usually necessary or the urge to defecate will be ignored. If defecation is suppressed over long periods, problems can occur, such as constipation or stool impaction.
Defecation can be facilitated by the Valsalva manoeuvre. This manoeuvre involves contraction of the chest muscles on a closed glottis with simultaneous contraction of the abdominal muscles. These actions result in increased intraabdominal pressure. The Valsalva manoeuvre may be contraindicated in the patient with a head injury, eye surgery, cardiac problems, haemorrhoids, abdominal surgery or liver cirrhosis with portal hypertension.
Constipation is common in older adults and is caused by many factors, including slower peristalsis, inactivity, decreased dietary fibre, decreased fluids, depression, constipating medications and laxative abuse.1,2 (Constipation is discussed in Ch 42.)
LIVER, BILIARY TRACT AND PANCREAS
Liver
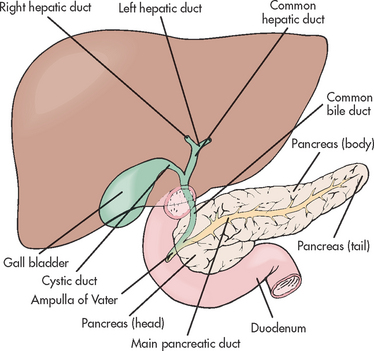
The liver is the largest internal organ in the body, weighing approximately 1.37 kg in the adult. It lies in the right hypochondriac and epigastric regions (see Fig 38-8). Most of the liver is enclosed in peritoneum. It has a fibrous capsule that divides it into right and left lobes (see Fig 38-5).
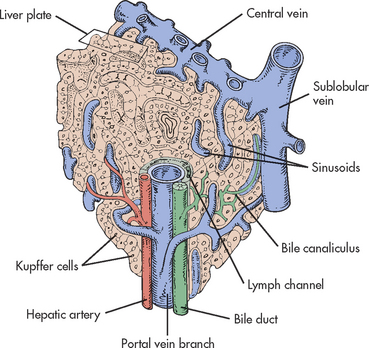
The functional units of the liver are lobules (see Fig 38-6). Lobules consist of rows of hepatic cells, hepatocytes, arranged around a central vein. The capillaries (sinusoids) are located between the rows of hepatocytes and are lined with Kupffer cells, which carry out phagocytic activity (removal of bacteria and toxins from the blood). Interlobular bile ducts form from bile capillaries (canaliculi). The hepatic cells secrete bile into the canaliculi.
The nerve supply to the liver is from the left vagus and sympathetic coeliac plexus. About one-third of the blood supply comes from the hepatic artery (branch of the coeliac artery) and two-thirds comes from the portal vein. The portal circulatory system (enterohepatic) brings blood to the liver from the stomach, intestines, spleen and pancreas. This blood enters the liver through the portal vein. The portal vein carries absorbed products of digestion directly to the liver. In the liver the portal vein branches and comes in contact with each lobule. The blood in the sinusoids is a mixture of arterial and venous blood.
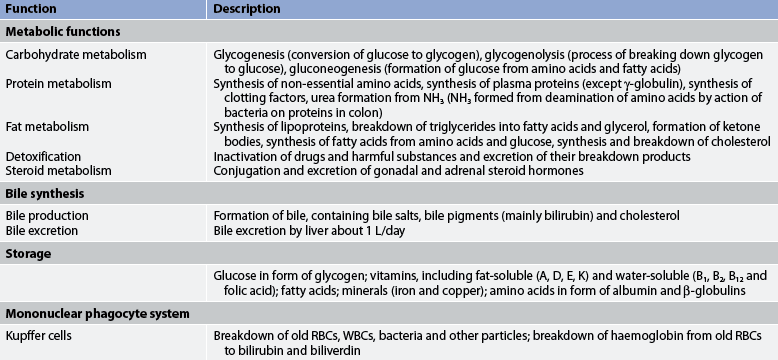
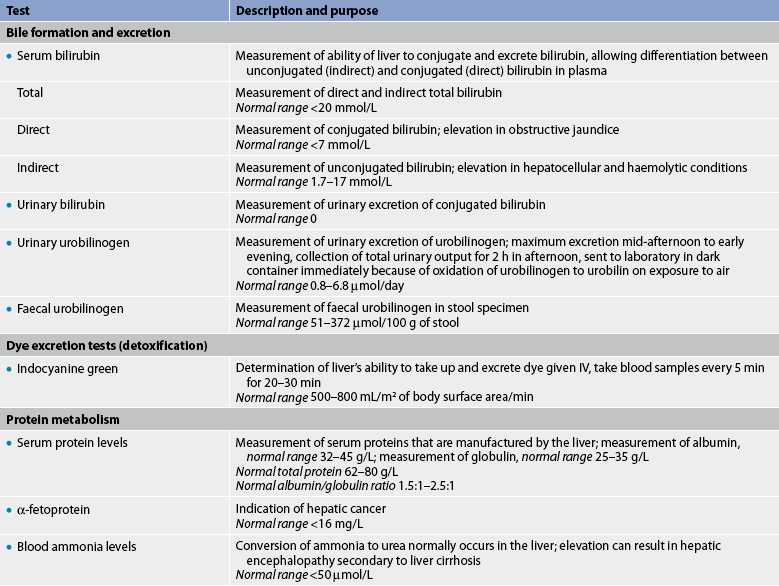
The liver is essential for life. It functions in the manufacture, storage, transformation and excretion of a number of substances involved in metabolism. The functions of the liver are numerous but can be classified into four main areas, which are summarised in Table 38-4.
Biliary tract
The biliary tract consists of the gall bladder and the duct system. The gall bladder is a pear-shaped sac that is located below the liver. The function of the gall bladder is to concentrate and store bile. It can hold approximately 45 mL of bile.
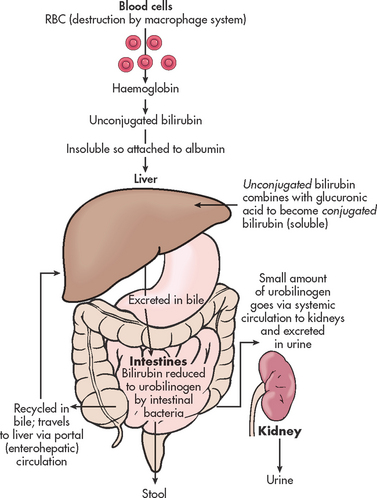
Bile is produced by the hepatic cells and secreted into the biliary canaliculi of the lobules. Bile then drains into the interlobular bile ducts, which unite into the two main left and right hepatic ducts. The hepatic ducts merge with the cystic duct from the gall bladder to form the common bile duct (see Fig 38-5). Most bile is stored and concentrated in the gall bladder. It is then released into the cystic duct and moves down the common bile duct to enter the duodenum at the ampulla of Vater. In the intestines, most of the bilirubin is reduced to stercobilinogen and urobilinogen by bacterial action. Stercobilinogen accounts for the brown colour of stool. A small amount of conjugated bilirubin is reabsorbed by the blood. Some urobilinogen is reabsorbed by the blood and returned to the liver through the portal circulation (enterohepatic) and excreted in the bile. An insignificant amount of urobilinogen is excreted in the urine.3 The sphincter of Oddi keeps the ampulla closed except when stimulated by the presence of food in the GI tract.
Bilirubin metabolism
Bilirubin, a pigment derived from the breakdown of haemoglobin, is constantly produced (see Fig 38-7). Because it is insoluble in water, it is bound to albumin for its transport to the liver. This form of bilirubin is referred to as unconjugated. In the liver bilirubin is conjugated with glucuronic acid. Conjugated bilirubin is soluble and is excreted in bile. Bile also consists of water, cholesterol, bile salts, electrolytes and phospholipids. Bile salts are needed for fat emulsification and digestion.
Pancreas
The pancreas is a long, slender gland lying behind the stomach and in front of the first and second lumbar vertebrae. It consists of a head, body and tail. The anterior surface is covered by peritoneum. The pancreas contains lobes and lobules. The pancreatic duct extends along the gland and enters the duodenum through the common bile duct (see Fig 38-5). The pancreas has both exocrine and endocrine functions. The exocrine function of the pancreas contributes to the process of digestion. Exocrine cells in the pancreas secrete pancreatic enzymes (see Table 38-1). The endocrine function occurs in the islets of Langerhans, in which beta cells secrete insulin, alpha cells secrete glucagon, delta cells secrete somatostatin and F cells secrete pancreatic polypeptide.
Assessment of the gastrointestinal system
SUBJECTIVE DATA
Subjective data are obtained from the patient through direct questioning about symptoms or as the patient is explaining to the nurse why they are seeking treatment.
Important health information
Past health history
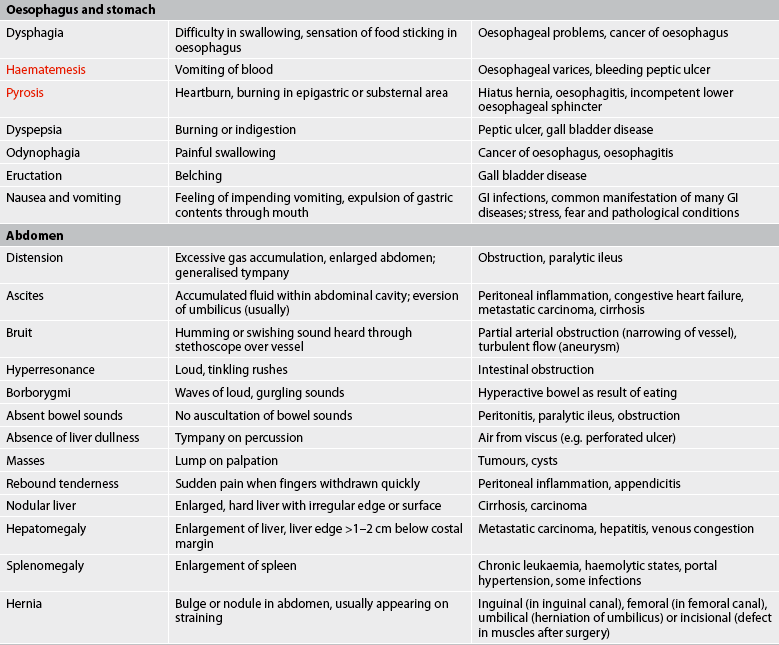
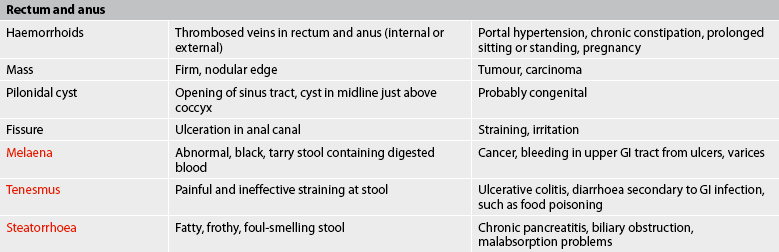
Information should be gathered from the patient about the history or existence of the following problems related to GI functioning: abdominal pain, nausea and vomiting, diarrhoea, constipation, abdominal distension, jaundice, anaemia, heartburn, dyspepsia, changes in appetite, haematemesis, food intolerance or allergies, indigestion, excessive gas, bloating, melaena, haemorrhoids and rectal bleeding. In addition, the patient should be asked about a history or existence of diseases such as gastritis, hepatitis, colitis, gall bladder disease, peptic ulcer, cancer or hernias, especially hiatus hernia.
Gerontological considerations: effects of ageing on the gastrointestinal system
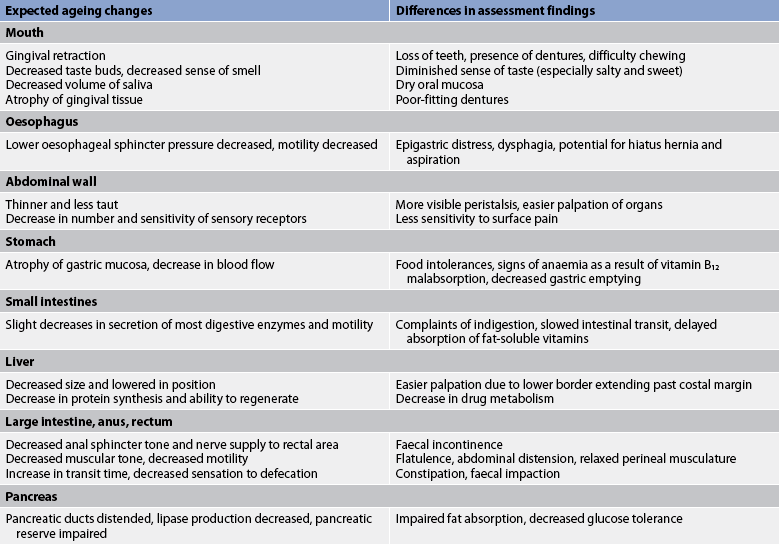
The process of ageing causes changes in the functional ability of the GI system, although less than in other organ systems (see Table 38-5). Tooth enamel and dentine wear down and make the teeth susceptible to cavities. Periodontal disease can lead to loss of teeth. Xerostomia (dry mouth from decreased saliva production) affects many older adults and may be associated with difficulty swallowing (dysphagia).3 Taste buds decrease, the sense of smell diminishes and salivary secretions diminish, all of which can lead to a decrease in appetite and make eating less pleasurable.
Age-related changes in the oesophagus include delayed emptying as a result of smooth muscle weakness and an incompetent LOS.1 Decreased oesophageal clearance of acid may put the older patient at risk of gastro-oesophageal reflux disease (GORD).3 Motility of the GI system decreases with age, but secretion and absorption are affected to a lesser extent. The elderly patient often experiences a decrease in HCl secretion (hypochlorhydria), delayed gastric emptying and constipation. With chronic atrophic gastritis there is a decrease in the number of parietal cells and a subsequent reduction in the amount of acid and intrinsic factor secreted. Although constipation is a common complaint of elderly patients, age-related changes in colonic secretion or motility have not been consistently shown.2
The liver decreases in size after 50 years of age, but the results of liver function tests remain within normal ranges. Enzyme changes in the liver that are age-related decrease the ability of the liver to metabolise drugs and hormones. The size of the pancreas is unaffected by ageing but it does undergo structural changes, such as fibrosis, fatty acid deposits and atrophy. Ageing does not cause changes in the structure and function of the gall bladder and bile ducts. However, with ageing there is an increase in the incidence of gallstones.3
Older adults, especially those over 85, are at risk of decreased food intake.2,3 Economic constraints may reduce the ability to purchase food supplies, which may affect nutritional intake, as well as reducing the number of fresh fruits and vegetables consumed and thus the amount of fibre. A reduction in dietary fibre, along with reduced fluid intake and decreased physical activity, contributes to constipation. Approximately 35% of individuals over 65 are obese.2 Age-related changes in the GI system and differences in assessment findings are presented in Table 38-5.
The patient should be questioned about weight history. Any unexplained or unplanned weight loss or weight gain within the past 12 months should be explored. A history of chronic dieting and repeated weight loss and gain should be documented.
Medications
The health history should include an assessment of the patient’s past and current use of medications. The names of all drugs along with their frequency of use and duration are important. Many medications may have an effect on the GI system. This is an important part of the assessment, particularly in relation to liver problems. It should include over-the-counter drugs, prescription drugs, herbal products and nutritional supplements. The use of prescription or over-the-counter appetite suppressants should be noted. Many chemicals and drugs are potentially hepatotoxic (see Box 38-1), and any use of illicit drugs should be documented. Antibiotics can cause changes in the normal bacterial composition in the GI tract, resulting in diarrhoea. The nurse should ask the patient if laxatives or antacids are taken, including the kind and frequency.
The nurse should also assess the patient’s use of over-the-counter pain medications. Chronic high doses of paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs) can be hepatotoxic. Chronic NSAID use can also predispose a person to upper GI bleeding.
Surgery or other treatment
Information should be obtained about hospitalisations for any problems related to the GI system. Data should also be obtained related to any abdominal or rectal surgery, including the year, reason for surgery, postoperative course and possible blood transfusions. Terms related to surgery of the GI system are presented in Table 38-6.
TABLE 38-6 Surgical procedures of the gastrointestinal system
| Surgical procedure | Description |
|---|---|
| Antrectomy | Removal of antrum portion of the stomach |
| Appendicectomy | Removal of the appendix |
| Caecostomy | Opening into caecum |
| Cholecystectomy | Removal of gall bladder |
| Cholecystostomy | Opening into gall bladder |
| Choledochojejunostomy | Opening between common bile duct and jejunum |
| Choledocholithotomy | Opening into common bile duct for removal of stones |
| Colectomy | Removal of the colon |
| Colostomy | Opening into colon |
| Gastrectomy | Removal of the stomach |
| Gastrostomy | Opening into stomach |
| Glossectomy | Removal of the tongue |
| Hemiglossectomy | Removal of half of the tongue |
| Herniorrhaphy | Removal of a hernia |
| Ileostomy | Opening into ileum |
| Mandibulectomy | Removal of the mandible |
| Oesophagoenterostomy | Removal of portion of the oesophagus with segment of colon attached to remaining portion |
| Oesophagogastrostomy | Removal of oesophagus and anastomosis of remaining portion to stomach |
| Pyloroplasty | Enlargement and repair of pyloric sphincter area |
| Vagotomy | Resection of branch of vagus nerve |
Functional health patterns
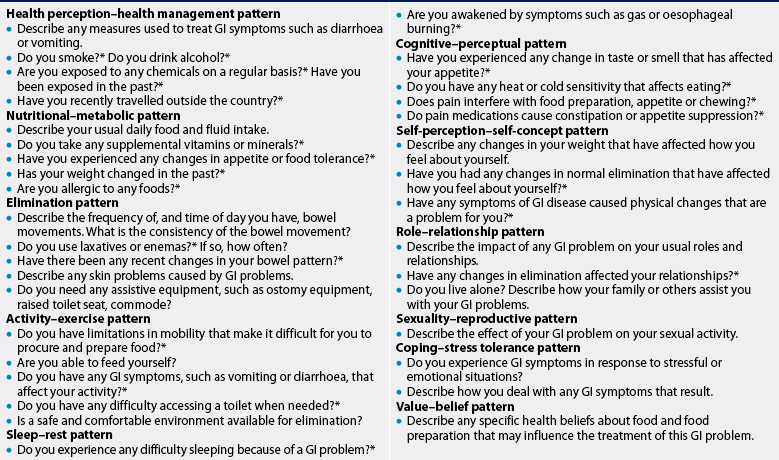
Key questions to ask a patient with a GI problem are presented in Table 38-7.
Health perception–health management pattern
The nurse should ask about the patient’s health practices related to the GI system, such as maintenance of normal body weight, attention to proper dental care, maintenance of adequate nutrition and effective elimination habits.
The patient should be asked about recent foreign travel with possible exposure to hepatitis, parasitic or bacterial infestation. A past history of receiving hepatitis A and/or hepatitis B vaccinations should be documented.
The patient should be assessed in relation to certain habits that directly affect GI functioning. The consumption of alcohol in large quantities has detrimental effects on the mucosa of the stomach and also increases the secretion of HCl and pepsinogen. Chronic alcohol exposure causes fatty infiltration of the liver and can cause damage leading to cirrhosis. The nurse should obtain a history of cigarette smoking. Nicotine is irritating to the entire GI tract mucosa. Cigarette smoking is related to various GI cancers (especially mouth and oesophageal cancers), oesophagitis and ulcers. Smoking will also delay the healing of ulcers.
Nutritional–metabolic pattern
A thorough nutritional assessment is essential. A dietary history should be taken and compared with the food pyramid (see Fig 39-1 and Table 39-1). The nurse should ask open-ended questions that will allow the patient to express their beliefs and feelings about their diet. It may be necessary to ask the patient for a 24-hour dietary recall to analyse the adequacy of the diet. The nurse should assist the patient in recalling the preceding day’s food intake, including early morning and night-time intake. The nurse should find out about the intake of snacks, liquids and vitamin supplements. The diet must then be evaluated in terms of the recommended groups and servings on the food pyramid. If weekend eating habits vary greatly, the nurse should obtain a separate weekend diet history and assess the patient’s intake for both quality and quantity of food.
The nurse should ask the patient about the use of sugar and salt substitutes, use of caffeine, and amount of fluid and fibre intake. (Fluid management is discussed in Ch 16.) The patient should be questioned about any changes in appetite, food tolerance and weight. Anorexia and weight loss may indicate the presence of cancer. The nurse should ask the patient about any food allergies and determine what GI symptoms such allergic responses cause, and ascertain any dietary intolerances, including lactose and gluten.
Elimination pattern
A detailed account of the patient’s bowel elimination pattern should be elicited. The frequency, time of day and usual consistency of stool should be noted. The use of laxatives and enemas, including type, frequency and results, should be documented. Any recent change in bowel patterns should be investigated.
The amount and type of fluid and fibre intake should be determined because they have an important effect on the frequency and consistency of stools. Inadequate intake of fibre can be associated with constipation. Analysis of fluid intake and output could indicate the presence of a urinary problem and the possibility of fluid retention.
Food allergies can cause lesions, pruritus and oedema. Diarrhoea can result in redness, irritation and pain in the perianal area. External drainage systems, such as an ileostomy or ileal conduit, can cause local skin irritation. The possible association between a skin problem and a GI problem should be investigated.
Activity–exercise pattern
The patient’s ambulatory status should be assessed to determine whether the patient is capable of securing and preparing food. If the patient is unable to manage these tasks, the nurse should determine whether family or an outside agency is meeting this need. Any limitation in the patient’s ability to feed themselves independently should be noted. Any difficulty accessing a safe environment for elimination should be assessed. Use of, and access to, elimination supplies should be assessed, such as a commode or ostomy supplies. Activity and exercise may affect GI motility. Immobility is a risk factor for constipation.
Sleep–rest pattern
Many food-related events can interrupt and interfere with the quality of sleep. Nausea, vomiting, diarrhoea, indigestion, bloating and hunger can produce sleep problems and should be investigated. The patient should be asked if GI symptoms affect sleep or rest. For example, a patient with a hiatus hernia may be awakened because of burning pain; sleep may be improved by elevating the head of the bed for this patient.
Patients often have a bedtime ritual that involves the use of a particular food or beverage. Milk is known to induce sleep through the effect of the serotonin precursor L-tryptophan. Herbal teas and melatonin are often sleep-inducing. Individual routines should be noted and complied with whenever possible to avoid sleeplessness. Hunger can prevent sleep and should be relieved by a light, easily digested snack unless contraindicated.
Cognitive–perceptual pattern
Decreases in sensory adequacy can result in problems related to the acquisition, preparation and ingestion of food. Changes in taste or smell can affect appetite and eating pleasure. Vertigo can make shopping and standing at a stove difficult and dangerous. Heat or cold sensitivity could make certain foods painful to eat. Problems in expressive communication could make it difficult and frustrating for the patient to make personal desires and preferences known. The nurse should assess the patient in this pattern to judge the effect of deficiencies on adequate nutritional intake. If the patient has been diagnosed as having a GI disorder, the nurse should ask questions to determine the patient’s understanding of the illness and its treatment.
Pain is another area that requires careful assessment related to its effect on the GI system and nutrition. Relevant behaviours associated with chronic pain include avoidance of activity, fatigue and disruption of eating patterns. The possible effects of narcotic pain medication related to constipation, nausea, sedation and appetite suppression should be assessed.
Self-perception–self-concept pattern
Many GI and nutritional problems can have serious effects on the patient’s self-perception. Overweight and underweight people often have problems related to self-esteem and body image. Repeated attempts to achieve a personally acceptable weight can be discouraging and depressing for the patient. The manner in which the patient recounts a weight history can alert the nurse to potential problems in this area.
Another potentially problematic area is the need for external devices to manage elimination, such as a colostomy or an ileostomy. The patient’s willingness to engage in self-care and to discuss this situation should provide the nurse with valuable information related to body image and self-esteem.
The physical changes often associated with advanced liver disease can be problematic for the patient. Jaundice and ascites cause significant changes in external appearance. The patient’s attitude towards these changes should be assessed.
Role–relationship pattern
Problems related to the GI system such as cirrhosis, alcoholism, hepatitis, ostomies, obesity and carcinoma can have a major impact on the patient’s ability to maintain usual roles and relationships. A chronic illness may necessitate leaving a job or reducing the number of hours worked. Changes in body image and self-esteem can affect relationships. The availability of, and satisfaction with, support should be determined. It is important that the nurse be aware of these possible consequences and assess for their presence.
Sexuality–reproductive pattern
Changes related to sexuality and reproductive status can result from problems of the GI system. For example, obesity, jaundice, anorexia and ascites could decrease the acceptance of a potential sexual partner. The presence of an ostomy could affect the patient’s confidence related to sexual activity. Chronic alcoholism could discourage a meaningful relationship that could develop into a sexual relationship. Sensitive questioning by the nurse may determine the presence of potential problems.
Anorexia can affect the reproductive status of a female patient. Alcoholism can affect the reproductive status of both men and women. A poor nutritional intake before and during pregnancy can result in a low-birth-weight infant.
Coping–stress tolerance pattern
The nurse should try to determine what stressors affect the patient and what coping mechanisms the patient uses to function with these stressors. GI symptoms such as epigastric pain, nausea and diarrhoea develop in many people in response to stressful or emotional situations. Some GI problems, such as peptic ulcers and irritable bowel syndrome, are aggravated by stress.
Value–belief pattern
The patient’s spiritual and cultural beliefs regarding food and food preparation should be assessed. As far as possible, these preferences should be respected by the healthcare provider. In addition, the nurse should determine whether any value or belief could interfere with planned interventions. For example, if the patient with anaemia is a vegetarian, the suggestion of adding liver to the diet is obviously inappropriate. Thoughtful assessment and consideration of the patient’s beliefs and values will usually increase patient compliance and satisfaction.