Chapter 2 Techniques and Geometry of Wound Repair
1 What are important considerations in surgical wound closure?
Surgical wound closure is performed in conjunction with biologic events such as fibroplasia, epithelialization, wound contraction, bacterial balance, and host defense mechanisms. All suture materials, including both absorbable and nonabsorbable monofilaments, should be considered as foreign bodies that evoke a tissue inflammatory reaction. This reaction may result in delayed wound healing, infection, or dehiscence. Selection of suture material should be based on the healing properties and requirements of the involved tissue, the biologic and physical properties of the suture material, the location of the wound on the body, and individualized patient considerations.
2 Why is the choice of suture material critical in the early stages of wound healing?
In the early stages of wound healing, the suture is primarily responsible for keeping the wound together. In the first 3 or 4 days after wound repair, the gain in tensile strength is related to the fibrin clot, which fills the wound cavity. Tensile strength is less than 5% of unwounded skin at 1 week, 10% at 2 weeks, 25% at 4 weeks, 40% at 6 weeks, and 80% at 8 to 10 weeks.
3 Which layer of a wound repair contributes the most to wound strength?
The dermal layer. Absorbable sutures placed in the dermis, such as poliglecaprone 25 (Monocryl), polyglactin 910 (Vicryl), polyglycolic acid (Dexon), or polyglyconate (Maxon), provide tensile strength over an extended period prior to suture resorption. Sutures placed in the epidermis, usually 5-0 or 6-0 nylon (depending on location), permit fine alignment of the skin edges only and should be removed within 5 days.
4 What are the basic principles of suturing skin wounds?
Skin edges should be débrided when necessary and always everted and approximated without tension. If simple stitches are not sufficient, horizontal or vertical mattress stitches may be necessary. After tying a knot, the suture appears pear-shaped in cross-section with raised borders. The everted skin edges gradually flatten to produce a level surface. It is important to place the suture so that the wound edges just touch each other. Postoperative edema creates additional tension with potential strangulation of tissue and resultant ischemia that may lead to necrosis.
5 What are the different methods of suturing skin wounds?
Simple interrupted sutures are placed so that the needle enters and exits the tissue at 90°, grasping identical amounts of tissue on each side to permit exact approximation of the wound margins. Of course, this principle applies only when the skin edges line up at exactly the same level. Occasionally, one side of the wound is higher and the other lower. To approximate the edges at the same level, it is necessary to grasp the tissue “high in the high” (closer to the epidermis) and “low in the low” (farther from the epidermis).
Vertical and horizontal mattress sutures are especially useful for everting stubborn wound edges. However, horizontal mattress sutures cause more ischemia than either simple interrupted or vertical mattress sutures.
Subcuticular or intradermal continuous sutures obviate the need for external skin sutures; thus, they avoid suture marks on the skin and result in the most favorable scar. These sutures should be left in place for 2 to 3 weeks. Prolene is often used because it produces little inflammatory reaction, maintains its tensile strength, and can easily be removed.
Half-buried mattress sutures (McGregor stitch or three-corner stitch) are especially useful for closing a V-shaped wound or approximating skin edges of different textures or thicknesses. This stitch usually prevents necrosis of the tip of the V, which is sometimes seen with simple interrupted sutures. By placing the buried portion of the suture within the dermis of the flap, ischemia and damage to the overlying skin are avoided.
Continuous over-and-over or running sutures are most often used for closure of scalp wounds because they can be performed rapidly and are hemostatic. Locking these stitches provides additional hemostasis. Nonlocking running stitches, using fine nylon, can be used in areas such as the face where the wound is uncomplicated and under no tension.
6 What is the role of immobilization in wound healing?
Immobilization of the wound is as important in soft tissue healing as it is in bone healing. By immobilizing the wound, tension across the skin edges is eliminated, yielding a more favorable scar. Immobilization can be achieved by using Steri-Strips, tapes, collodion, or even plaster splinting.
7 How are suture materials classified?
Suture materials are classified as natural or synthetic, absorbable or nonabsorbable, and braided or monofilament. Further classification takes into consideration the time until absorption occurs, extent of tissue reaction, and tensile strength.
8 What are the differences among the various absorbable suture materials?
Catgut, derived from the submucosal layer of sheep intestine, evokes a moderate acute inflammatory reaction and is hydrolyzed by proteolytic enzymes within 60 days. Tensile strength is rapidly lost within 7 to 10 days. Chromization (chromic catgut suture) slightly prolongs these parameters compared with plain gut. The main indications for use of catgut suture include ligation of superficial vessels and closure of tissues that heal rapidly, such as oral mucosa. Catgut sutures also can be used in situations where one wishes to avoid suture removal, as in small children.
Vicryl and Dexon are synthetic materials that behave similarly. They produce minimal tissue reactivity and are completely absorbed within 90 days. Tensile strength is 60% to 75% at 2 weeks and lost at 1 month. Both are useful as intradermal sutures because of their low reactivity, but they should be used judiciously as buried sutures because of their tendency to “spit” with inflammation. Monocryl (a monofilament), on the other hand, can be used comparably as intradermal or buried sutures. Because the braided structure of Vicryl and Dexon may potentiate infection, neither should be used in wounds with potential bacterial contamination.
Polydioxanone (PDS), a synthetic absorbable monofilament, is minimally reactive. Absorption is essentially complete within 6 months, although little occurs before 90 days. Because of this slow absorption, “spitting” is a significant problem. As a monofilament suture, however, PDS is less prone to bacterial seeding. PDS sutures maintain their tensile strength considerably longer: 50% at 4 weeks and 25% at 6 weeks. Absorption is essentially complete at 6 months.
Maxon and Monocryl are absorbable monofilament sutures with qualities and advantages similar to those of PDS. However, they retain their tensile strength for only 3 or 4 weeks; absorption of Monocryl is essentially complete between 3 and 4 months.
9 What are the differences among the various nonabsorbable suture materials?
Nonabsorbable monofilament (Ethilon/nylon and Prolene) sutures incite minimal inflammatory reaction, slide well, and can be easily removed, thus providing ideal running intradermal stitches. Prolene appears to maintain its tensile strength longer than nylon, which loses approximately 15% to 20% per year. Nonabsorbable braided materials (Nurolon, Ethibond, and silk) elicit an acute inflammatory reaction that is followed by gradual encapsulation of the suture by fibrous connective tissue.
Staples cause less inflammatory reaction than sutures, have similar strength up to 21 days, and result in a similar final appearance when removed within 1 week postoperatively. Large wounds can be closed faster and more expeditiously with staples, which are useful for procedures such as abdominoplasty, reduction mammaplasty, and skin grafting.
10 What influences the permanent appearance of suture marks?
The key factors influencing scarring due to suture placement are (1) length of time that the skin suture remains in place, (2) tension on the wound edges, (3) region of the body, (4) presence of infection, and (5) tendency for hypertrophic scarring or keloid formation. The most critical factors in avoiding suture marks in the skin are tension-free closure and early removal. Sutures left in place for excessive periods result in severe scarring. Epithelial cells crawl along the path of the suture within the skin, resulting in sinus tract formation; cross-hatching occurs from prolonged compression of the suture on the epidermal surface. Wounds in which sutures are removed within 7 days usually produce a fine linear scar. Wound closure with a running dermal pull-out suture provides the optimal scar without interfering with the development of tensile strength. The finest sutures for any given wound should be used. The timing of removal depends on the region of the body in which the sutures have been placed and ranges from 3 to 5 days in the face to 10 to 14 days in the back and extremities.
11 What are Langer’s lines?
Elastic fibers within the dermis maintain the skin in a state of constant tension, as demonstrated by the gaping of wounds created by incising the dermis or by the immediate contraction of skin grafts as they are harvested. In 1861, Langer demonstrated that puncturing the skin of cadavers with a rounded sharp object resulted in elliptical holes produced by the tension of the skin. He stated that human skin was less distensible in the direction of the lines of tension than across them. Shortcomings of Langer’s lines are that (1) some tension lines were found to run across natural creases, wrinkles, and flexion lines; (2) they exist in excised skin; and (3) they do not correlate with the direction of dermal collagen fiber orientation. Nonetheless, Langer’s lines serve as a useful guide in the planning and design of skin incisions and excisions.
12 What are relaxed skin tension lines?
Relaxed skin tension lines (RSTLs), also known as wrinkle lines, natural skin lines, lines of facial expression, or lines of minimal tension, lie perpendicular to the long axis of the underlying facial muscles. They are accentuated by contraction of the facial muscles, as occurs with smiling, frowning, grimacing, puckering the lips, or closing the eyes tightly. An example is the frontalis muscle, which runs vertically straight up the forehead; RSTLs on the forehead run transversely or perpendicular to the underlying frontalis muscle.
13 What is the optimal scar?
The optimal scar is a fine, flat, concealed linear scar lying within or parallel to a skin wrinkle or natural skin line, contour junction, or RSTL. There should be no contour irregularity, distortion of adjacent anatomic or aesthetic units or landmarks, or pigmentation changes.
14 What causes “stretch” marks?
Significant stretch may result in disruption of the dermis with loss of continuity of the elastic fibers. Once this occurs, elastic recoil and skin tension in the involved area are lost—the result is a stretch mark.
15 Which excisional methods can be used for removal of skin lesions?
Skin lesions can be removed by elliptical, wedge, or circular excisions. Most skin lesions are removed by simple elliptical excision with the long axis of the ellipse on, or paralleling, a wrinkle, contour line, or RSTL. The ellipse may be lenticular in shape with angular edges or have rounded edges. Ideally, the long axis should be four times longer than the short axis. Wedge excisions are performed primarily for lesions on the free margins of the ears, lips, eyelids, or nostrils. Lip lesions can be excised as either triangular or pentagonal wedges. Pentagonal rather than triangular excision often leads to less contracture and shortening along the longitudinal axis of the incision with a more favorable scar. Closure of circular defects can be performed by a purse string suture, a skin graft, or a local flap.
16 What is the purpose of serial excisions?
Large lesions, such as giant nevi, can be removed by serial excisions. This approach takes advantage of the viscoelastic properties of skin and the creep and stress–relaxation phenomenon. It has been especially useful for improvement of male pattern baldness by excision of non–hair-bearing areas of the scalp. However, with the introduction of soft tissue expansion, the technique of serial excision has become less popular.
17 What are the differences among rotation, transposition, and interpolation flaps?
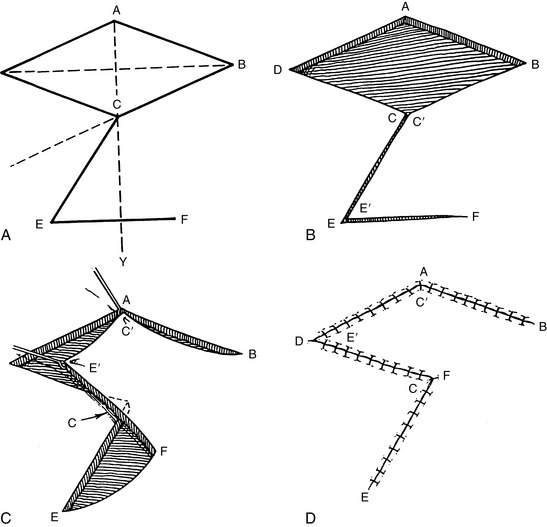
Each of these flaps has a specific pivot point and an arc through which the flap is rotated. The line of greatest tension of the flap is the radius of that arc. The rotation flap is a semicircular flap, whereas the transposition flap is a rectangular flap, consisting of skin and subcutaneous tissue that rotates about a pivot point into an immediately adjacent defect. The flap donor site can be closed by direct suturing or with a skin graft. A small back-cut from the pivot point along the base of the flap can be made to release a flap that is under too much tension. Because a skin flap rotated about a pivot point becomes shorter in length the farther it is rotated, the transposition flap usually is designed to extend beyond the defect. A sufficient flap design is verified with a cloth template (Fig. 2-1). An interpolation flap, although similar in design to the rotation and transposition flaps, is rotated into a nearby but not immediately adjacent defect. The pedicle of this flap, therefore, must pass over or under the intervening tissue.
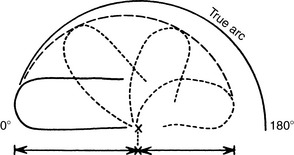
Figure 2-1 A skin flap rotated about a pivot point becomes shorter in effective length the farther it is rotated. Therefore a flap should be designed to extend beyond the defect.
(From Place MJ, Herber SC, Hardesty RA: Basic techniques and principles in plastic surgery. In Aston SJ, Beasley RW, Thorne CHM [eds]: Grabb and Smith’s Plastic Surgery, 5th ed. Philadelphia, Lippincott-Raven, 1997, p 22, with permission.)
18 What is a bilobed flap?
A bilobed flap is a transposition flap that consists of two flaps often designed at right angles to each other. The primary flap is transposed into the defect, whereas the secondary flap, usually half the diameter of the primary flap, is used to close the donor site (Fig. 2-2).
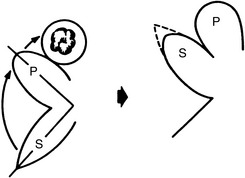
Figure 2-2 Bilobed flap. After excision of the lesion, the primary flap (P) is transposed into the resultant defect. The secondary flap (S) is then transposed to close the donor site defect.
(From Place MJ, Herber SC, Hardesty RA: Basic techniques and principles in plastic surgery. In Aston SJ, Beasley RW, Thorne CHM [eds]: Grabb and Smith’s Plastic Surgery, 5th ed. Philadelphia, Lippincott-Raven, 1997, p 23, with permission.)
19 What is a “dog ear”? How can it be eliminated?
In excising a lesion in elliptical fashion, the long axis should be four times the length of the short axis. Dog ears form at the ends of a closed wound when either the ellipse is made too short or one side of the ellipse is longer than the other. Dog ears may flatten over time, but primary correction is best. If the elliptical excision is too short, the ellipse can be lengthened to include the excessive tissue or the redundant tissue excised as two small triangles. If one side of the incision is longer than the other, the dog ear can be corrected by making a short right-angle or 45° incision at the end of the ellipse with removal of the redundant tissue.
20 When should scar revision be performed? What are the goals?
Scar revision should be performed once the scar has matured—usually 9 months to 2 years after the original procedure. The goals of scar revision are to reorient the scar, divide it into smaller segments, and make it level with adjacent tissue.
21 What is a Z-plasty?
Referred to by Limberg as “converging triangular flaps,” the Z-plasty is a technique in which two triangular flaps are interdigitated without tension, producing a gain in length along the direction of the common limb of the Z (useful in the management of scar contractures) as well as a change in the direction of the common limb of the Z (useful in the management of facial scars).
22 How is a Z-plasty designed?
A Z-plasty consists of a central limb, usually placed along the scar or line of contracture, and two limbs positioned to resemble a Z or reverse Z. The limbs must be equal in length to permit the skin flaps to fit together after transposition. The angles of the Z vary from 30° to 90°. The central limb, oriented along the line of contracture, usually is under considerable tension. After release or division of this contracture, the shape of the parallelogram immediately changes with spontaneous flap transposition and lengthening along the line of the central limb. Lengthening is related to the difference between the long and short axes of the parallelogram formed by the Z. The wider the angles of the triangular flaps, the greater the difference between the long and short diagonals and thus the greater the lengthening. In designing a Z-plasty, sufficient laxity must be available transversely to achieve the appropriate lengthening perpendicular to it. The limbs of the Z-plasty should follow the RSTLs (Fig. 2-3).
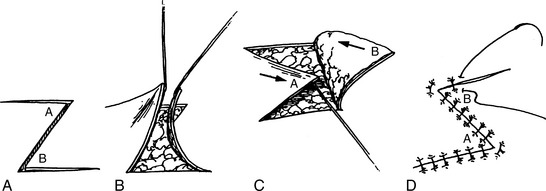
Figure 2-3 Classic Z-plasty using 60° angles. A, B, Flap design and elevation. C, D, Flap transposition and suture without tension.
(From Weinzweig N, Weinzweig J: Basic principles and techniques in plastic surgery. In Cohen M [ed]: Mastery of Plastic and Reconstructive Surgery. Boston, Little, Brown, 1994, p 26, with permission.)
23 Why are angle size and limb length important in performing a Z-plasty?
The angle size determines the percentage increase in length. The original limb length controls the absolute increase in final limb length. As the angle size increases, the degree of lengthening increases. A 30° angle produces a 25% increase in length; a 45° angle, a 50% increase; a 60° angle, a 75% increase; a 75° angle, a 100% increase; and a 90° angle, a 120% increase. Although the length increase values are only theoretical, they provide a good approximation of the actual lengthening. In general, the actual increase in length is slightly less than the theoretical increase.
24 What is the optimal angle for Z-plasty design?
The optimal angle is 60°. Angles significantly less than 60° do not achieve sufficient lengthening, defeating the purpose of the Z-plasty and resulting in flap narrowing and vascular compromise. Angles much greater than 60° produce significant tension in the adjacent tissue, preventing transposition of the flaps.
25 What are the indications for multiple Z-plasties?
A similar degree of lengthening can be produced by a single Z-plasty and multiple Z-plasties, because the total length of the central limbs of multiple Z-plasties can equal the length of the single Z-plasty. Multiple Z-plasties, however, produce less transverse shortening. Lateral tension is reduced and more equally distributed over the entire length of the central limbs. Multiple Z-plasties are useful when insufficient tissue is available for a large single Z-plasty. In addition, multiple Z-plasties of facial scars often produce cosmetically superior results.
26 What is a four-flap Z-plasty?
A four-flap Z-plasty is an effective technique to correct thumb–index web space and axillary contractures. A 90°/90° angle or 120°/120° angle Z-plasty is designed. The two-flap Z-plasty is then converted to a four-flap Z-plasty by bisecting the angles, creating flaps that are 45° or 60°. This technique produces greater lengthening (124%) with less tension on the flaps.
27 What is a double-opposing Z-plasty?
Also known as the combination five-flap Y-V advancement and Z-plasty, the double-opposing Z-plasty is particularly useful for releasing contractures of concave regions of the body, such as the dorsum of the interdigital web spaces and the medial canthal region. The central flap is advanced in Y-V fashion while the flaps of the two Z-plasties on each side of the central flap are transposed (Fig. 2-4).
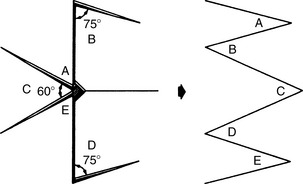
Figure 2-4 Five-flap Y-V advancement and Z-plasty. The central flap (C) is advanced in a Y-V fashion. The flaps of the two Z-plasties on each side of the central flap are transposed.
(From Jankauskas S, Cohen IK, Grabb WC: Basic techniques in plastic surgery. In Smith JW, Aston SJ [eds]: Grabb and Smith’s Plastic Surgery, 4th ed. Boston, Little, Brown, 1991, p 76, with permission.)
28 What is a W-plasty?
A W-plasty is another technique for reorienting the direction of a linear scar. Triangles of equal size are outlined on either side of the scar with the tip of the triangle on one side placed at the midpoint of the base of the triangle on the opposite side. At the ends of the scar, the excised triangles should be smaller, with the limbs of the W tapered. The tips of the triangles should be sutured with three-corner stitches to prevent necrosis of the flap tips.
29 What is the main disadvantage of a W-plasty?
A W-plasty does not lengthen a contracted linear scar; a Z-plasty should be used for this purpose. A W-plasty increases rather than decreases tension in the area of the scar because of the necessary sacrifice of tissue and should be used only when there is an abundance of tissue adjacent to the scar.
30 What is the V-Y advancement technique?
The V-Y advancement technique allows forward advancement of a triangular flap (V) without rotation or lateral movement and closure of the resulting defect in a Y fashion. The skin that is actually advanced is on either side of the V (Fig. 2-5).
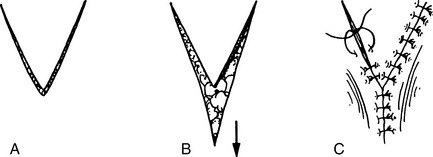
Figure 2-5 V-Y advancement technique. The central V is advanced forward and the defect is closed in a Y configuration.
(From Weinzweig N, Weinzweig J: Basic principles and techniques in plastic surgery. In Cohen M [ed]: Mastery of Plastic and Reconstructive Surgery. Boston, Little, Brown, 1994, p 26, with permission.)
31 When is a V-Y advancement flap used?
This technique is extremely useful for lengthening the nasal columella, correcting the whistle deformity of the lip, and closure of selected soft tissue defects. It also can be used in various other skin and mucosal flaps.
32 What is a rhombic flap?
The rhombic flap, originally described by Limberg and often referred to as the Limberg flap, is a combination of rotation and transposition flaps that borrows adjacent loose skin for coverage of a rhombic defect. A rhombus is an equilateral parallelogram with (1) acute angles of 60° and obtuse angles of 120°, (2) long and short diagonals perpendicular to each other, and (3) a short diagonal equal in length to each side of the rhombus. The flap is designed as an extension of the short diagonal opposite either of the two 120° angles of the rhombus. The short diagonal is extended by a distance equal to its length. From this point, a line of equal length is drawn at 60° parallel to either side of the rhombus. Therefore four Limberg flaps are possible for any given rhombic defect (Fig. 2-6).
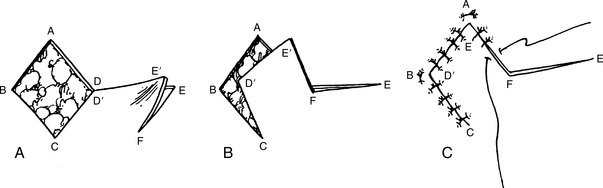
Figure 2-6 Rhombic flap. A, Flap design. B, Elevation of flap with wide undermining of the base to allow transposition. C, Suture of the flap without tension.
(From Weinzweig N, Weinzweig J: Basic principles and techniques in plastic surgery. In Cohen M [ed]: Mastery of Plastic and Reconstructive Surgery. Boston, Little, Brown, 1994, p 26, with permission.)
33 Should lesions be excised to create rhombic defects?
No. Lesions should be excised as circular defects or as necessary to permit adequate excision. A rhombus encompassing the defect and the four possible rhombic flaps can then be drawn. The selected flap is incised and elevated. Wide undermining beneath the base of the flap is necessary to allow the flap to fall into position in the rhombic defect without tension. The initial sutures are placed in the four corners of the defect.
34 What is the Dufourmental flap?
The Dufourmental flap is a variation of the rhombic flap in which the angles differ from the standard 60° and 120° angles in the Limberg flap. Although angles of 30° and 150° usually are used, angles up to 90° are possible. This versatile flap is useful for coverage of a defect in the shape of a rhomboid rather than a rhombus. Although the two terms are often used interchangeably, a rhomboid differs from a rhombus in several important respects: (1) it has acute angles of various degrees, (2) only opposite sides are equal in length, (3) diagonals are not perpendicular, (4) diagonals are not equal in length, and (5) diagonals are not necessarily equal in length to the sides of the parallelogram. Planning is more complex than for the Limberg flap, and it is often easier simply to convert the defect into a rhombus with angles of 60° and 120° (Fig. 2-7).
Borges A.F. Elective Incisions and Scar Revision. Boston: Little, Brown, 1973.
Borges A.F. Choosing the correct Limberg flap. Plast Reconstr Surg. 1978;62:542-545.
Borges A.F. W-plasty. Ann Plast Surg. 1979;3:153-159.
Jackson I.T. Local Flaps in Head and Neck Reconstruction. St. Louis: Mosby, 1995.
Limberg A.A. The Planning of Local Plastic Surgical Operations. Lexington, MA: Collamore Press, 1984. [translated by SA Wolfe]
McGregor I.A. The Z-plasty. Br J Plast Surg. 1966;19:82-87.
McGregor I.A. Fundamental Techniques in Plastic Surgery and Their Surgical Applications, 7th ed. Edinburgh: Churchill Livingstone, 1980.
Jankauskas S., Cohen I.K., Grabb W.C. Basic technique of plastic surgery. In: Smith J.W., Aston S.J., editors. Grabb and Smith’s Plastic Surgery. 4th ed. Boston: Little, Brown and Company; 1991:3-90.
Weinzweig J., Weinzweig N. Plastic surgery techniques. In: Guyuron M., Eriksson E., Persing J., et al, editors. Plastic Surgery. Philadelphia: Elsevier, 2008, pp 1013–1032.
Weinzweig N., Weinzweig J. Basic principles and techniques in plastic surgery. In: Cohen M., editor. Mastery of Plastic and Reconstructive Surgery. Boston: Little, Brown, 1994, pp 14–33.