Advanced Intravenous Calculations
Objectives
• Calculate milligrams per kilogram and micrograms per kilogram per minute and per hour.
• Calculate hourly drug dose and hourly flow rate for IV solutions.
• Estimate and calculate infusion rates and drug doses using ratio and proportion.
• Calculate time and dose intervals for direct IV push (bolus) medications administered by a syringe.
• Evaluate existing infusions for correct flow rate and/or drug dose, and obtain order to change if incorrect.
Introduction
This chapter builds on the mastery of the basic IV calculations learned in Chapter 6. Taking the time to work through each set of problems will facilitate the acquisition of the logic needed to solve complex IV solution calculations. When each step has been mastered, you will be able to identify and use basic safe calculation shortcuts.
Advanced IV Calculations
Advanced IV calculations are used to determine the amount of IV drug and flow rate per minute and/or per hour for HIGH-ALERT potent medications based on the patient’s weight, condition, and response to treatment. If an infusion device is not available, microdrip tubing should be used with a volume-control device (Figure 8-1 on page 182). High alert medications must be delivered on an IV pump.

The choice of administration and equipment depends not only on the orders and the patient’s condition but also on hospital policy, accrediting body policy, the current literature and pharmacy recommendations, and the equipment available.
The nurse must be able to evaluate orders and existing solutions for safe and correct dose/flow rates, preferred routes, and compatibilities with existing solutions. Table 8-1 provides the ISMP’s list of High-Alert medications.
Titrated Infusions
Dose/flow rate adjustments may be made, particularly with powerful solutions of medications, based on the patient’s condition, weight, and physiologic response to the medication. For example, an order may call for an IV to be titrated (adjusted) to maintain a certain blood pressure range. The most potent IV medications are administered and adjusted in micrograms per kilogram per minute or milligrams per kilogram per minute. For purposes of reducing errors and simplifying mathematics in flow rate calculations, many of these infusions now have a standardized total drug/total volume ratio of 1 : 1, 1 : 2, and 1 : 4 (e.g., 250 mg/250 mL [1 : 1]; 250 mg/500 mL [1 : 2], 250 mg/1000 mL [1 : 4]). If the patient requires fluid restriction, the physician may order a stronger concentration of drug to solution (4 : 1 or 2 : 1 drug in solution, such as 1 g : 250 mL [4 : 1] or 500 mg : 250 mL [2 : 1]).
 CLINICAL ALERT
CLINICAL ALERT
If you consult flow rate and compatibility charts, examine the source and the date published. If the publisher is a reputable source, such as the laboratory that furnishes the IV solutions in use, and if the chart is current, then take further care to examine the layout and content of the tables to ensure that the information needed is selected.
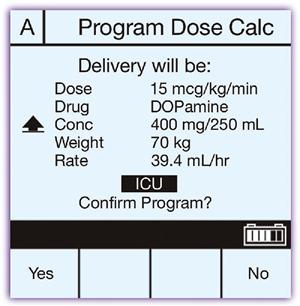
IV solutions that contain powerful medications are usually prepared by the pharmacy and administered by a volumetric infusion pump. There are several sophisticated devices on the market (Figure 8-1). The data to be entered can range from the traditional mL/hr to drug doses ordered per minute in mg/min or mcg/min, along with the patient’s weight, if necessary (mg/kg/min) (Figure 8-2).
New High Technology Infusion Devices Called “Smart Pumps”
A variety of infusion pump devices have been developed to reduce medication errors. Grave adverse drug events with powerful IV pump-infused drugs have occurred due to programming errors such as entering mL for mg, mg for mcg, or pounds for kg.* The smart pumps are preprogrammed with specific guidelines on kg weight-based dose limits, and usual doses for drugs used in specialized clinical areas such as adult and infant ICU areas, obstetrics, and so on. Hospital pharmacies often manage the multiple sources of preprogrammed software information including drug libraries and specific patient care area safe dose ranges.
The nurse selects the drug from the software on the pump, enters the drug concentration, the order, and the patient’s weight in kg to obtain the flow rate and is “alerted” if the data entered exceed safe dose limits for the target population. Some smart pumps also alert the nurse if the same drug is being infused on another line. All alerts are logged so that problems can be audited by the agency’s safety committees.
 CLINICAL ALERT
CLINICAL ALERT
Interpretation of drug concentrations on labels; awareness of differences among mcg, mg, mL, and units, and the difference between lb and kg; familiarity with safe dose ranges for the target population, pump equipment operation, and potential equipment flaws all are essential to safe administration. The nurse has a chance to confirm all the data before initiating the flow of the drug.
 CLINICAL ALERT
CLINICAL ALERT
Although these pumps can reduce errors, the nurse cannot be overly reliant on pump alerts. The alerts depend upon the accuracy and scope of preprogrammed information as well as the function of the pump.
Solving Titrated Infusion Problems
Hourly Drug and Flow Rate Formula for Titrated Infusions

remember
IV orders may necessitate converting mcg or mg/min to mg/hr.
 Example
Example
Ordered: 3 mcg/kg/min of Intropin (dopamine HCl) for a new patient with heart failure. Available: 400 mg dissolved in 500 mL D5W. The literature recommends an initial dose of 2 to 5 mcg/kg/min, (not to exceed a total of 50 mcg/kg/min). The dose is to be titrated to the patient’s systolic blood pressure at the level ordered by the physician. This patient weighs 242 lb. What flow rate should be set?
Step 1
Step 2
Compare the SDR recommended in the literature with the order:
 CLINICAL ALERT
CLINICAL ALERT
Titrated infusions seldom require a high flow rate. It is essential that the flow rates be correct. Speeding up or slowing down an IV without a physician’s order, to compensate for incorrect flow rate, is hazardous. Be aware that abrupt changes in the flow rates of IV fluids and therefore in medication levels can cause serious side effects.
Step 3
a. Calculate the ordered hourly drug dose in milligrams (same terms as drug [400 mg] on hand) using a calculator (recalling that 1000 mcg 5 1 mg).
3 mcg 3 110 kg 3 60 min 4 1000 5 19.8 mg/hr, rounded to 20 mg/hr.
b. Calculate the hourly flow rate (HV) after reducing the total drug/total volume ratio to lowest terms.

Set the flow rate on the IV infusion device to 25 mL/hr.
Alternative Step 3
If the hourly volume is known but the hourly drug dose is not, just place the unknown (x) under the hourly drug dose and fill in the hourly volume ordered in this equation. Check the answer with the literature for the SDR (e.g., the order was for 25 mL/hr or is infusing at 25 mL/hr when you arrive; how much drug is the patient receiving per hour and per minute so that the SDR can be checked?).
Use the same formula. Read the total drug, total volume, and hourly volume on the IV devices in the patient’s room:

The SDR states 2 to 5 mcg/kg/min. Now you know that the order was followed properly, and that the flow rate is correct and within the SDR. The next few worksheets provide the necessary basic skills practice to understand and perform these calculations rapidly.
Example
Example
Example
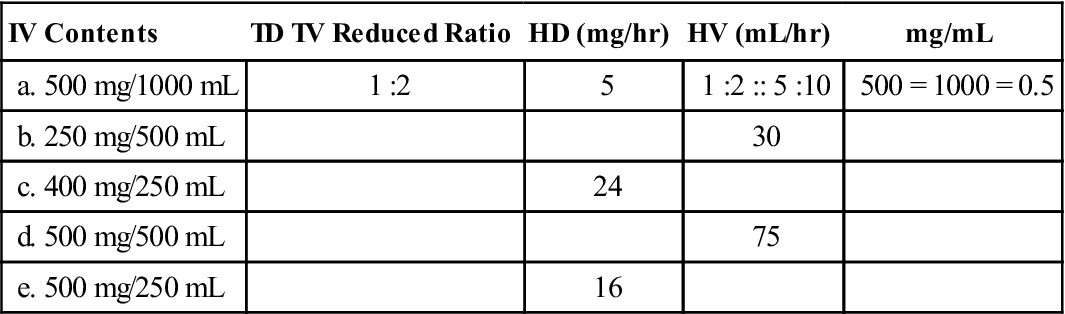
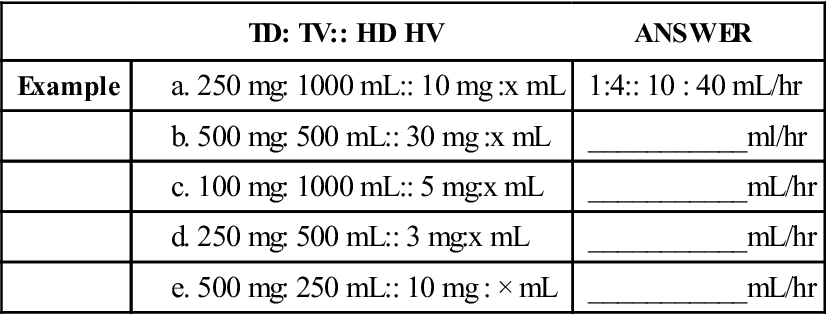
| TD: TV:: HD HV | ANSWER | |
| Example | 1:4:: 10 : 40 mL/hr | |
| ___________ml/hr | ||
| ___________mL/hr | ||
| ___________mL/hr | ||
| ___________mL/hr |
4. If you came on duty and evaluated these IV solutions and rates in a patient-care setting, you would estimate the hourly drug after first reducing the total drug/total volume ratio and then examining the rate set on the infusion device.
Estimate the hourly drug (x).
Example
Example
| TD: TV:: HD:HV | ANSWER | |
| Example | 1:4:: 4: 16 ml/hr | |
| ____________ml/hr | ||
| ____________ml/hr | ||
| ____________ml/hr | ||
| ____________ml/hr |

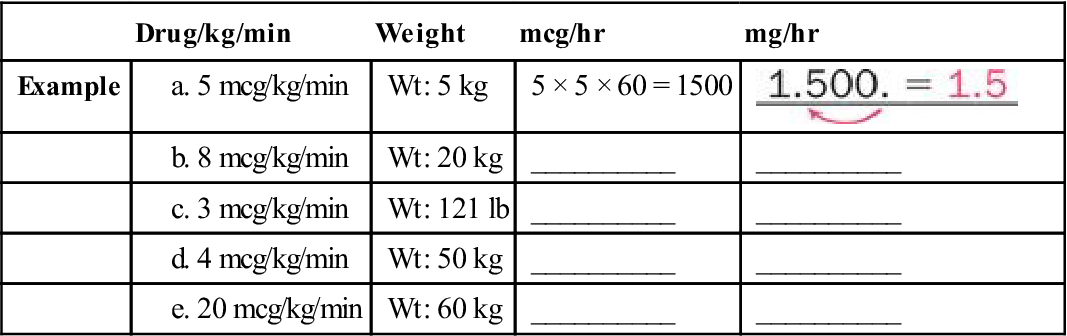
Tip: Being able to convert drug, weight, time, and volume parameters within the metric system with ease facilitates advanced IV calculations.
 CLINICAL ALERT
CLINICAL ALERT
Remember that the difference between a microgram (mcg) and a milligram (mg) is “3 1000.” The difference between drug per minute and hourly drug is “3 60.”
The difference between mcg/kg/min and mcg/min is equal to “3 the weight in kilograms.” Manipulating these differences is critical for safe medication administration.
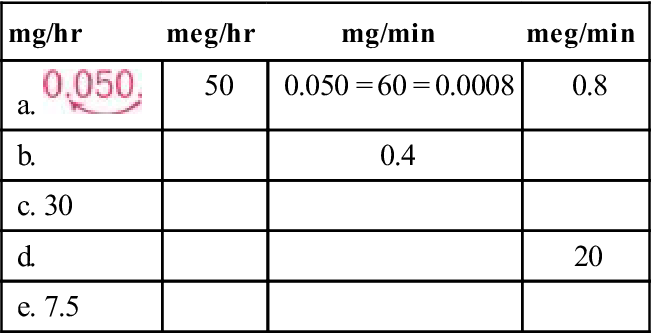
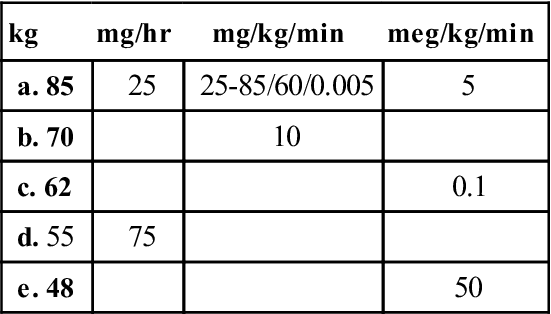
It is often necessary to verify the amount of drug being delivered in an existing solution. The amount of drug in the IV solution is frequently a milligram dose, whereas the amount of drug the patient is receiving is a microgram dose or a microgram/kilogram dose.
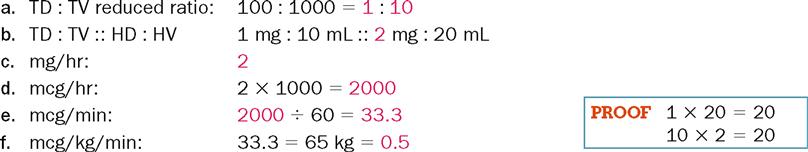
Note the example in Problem 1 and do the following in the remaining problems:
• Set up your TD : TV :: HD : HV ratio and determine mg/hr. Prove your answer.
• Move decimals to change milligrams to micrograms (31000).
• Use a calculator to change hourly drug (HD) to drug/minute (divide by 60).
• Use a calculator to determine kilograms, and divide micrograms by kilogram weight to obtain mcg/kg/min. Enter all calculator data twice for verification.
Example
1. An IV of Drug Y 100 mg in 1000 mL is infusing at 20 mL/hr. The physician asks, “How many mg/hr is the patient receiving? How many mcg/min? How many mcg/kg/min?” The patient weighs 143 lb today.
2. An IV of Drug Y 250 mg in 500 mL is infusing at 15 mL/hr. The patient weighs 110 lb today.
a. TD : TV :: HD : HV reduced ratio:

3. An IV of Drug Y 400 mg in 1000 mL is infusing at 5 mL/hr. The patient weighs 121 lb today.
a. TD : TV :: HD : HV reduced ratio:

4. An IV of Drug Y 1000 mg in 250 mL is infusing at 10 mL/hr. The patient weighs 132 lb today.
a. TD : TV :: HD : HV reduced ratio:

5.  An IV of Drug Y 500 mg in 250 mL is infusing at 8 mL/hr. The patient weighs 175 lb today. (Calculate kilograms to nearest tenth.)
An IV of Drug Y 500 mg in 250 mL is infusing at 8 mL/hr. The patient weighs 175 lb today. (Calculate kilograms to nearest tenth.)
a. TD : TV :: HD : HV reduced ratio:

Perform the requested calculations. Use a calculator for long division or multiplication. Evaluate flow rates.
 Example
Example
1. Nitroprusside sodium infusion is ordered at 0.3 mcg per kg per minute IV and is being infused on a patient with hypertension in a pharmacy prepared solution of 50 mg in 500 mL of D5W. Pharmacy directions instruct to set a flow rate of 12.6 mL an hr for this patient and administer on an IV pump. The patient’s weight is 70 kg.
2. Azithromycin 500 mg IV is ordered for a patient with pelvic inflammatory disease. Directions state that each 500 mg vial must be reconstituted first with 4.8 mL SW to give 100 mg per mL. Further dilute each 500 mg to 250 mL with D5W or other compatible solutions. For 2 mg per mL dilution, give over 1 hr. The nurse you are replacing on shift states that IV rate should be 500 mL per hour.
3. Cefepime HCl 1 g is ordered IV q12h for a patient with severe pneumonia. Supplied is an ADD Vantage vial. 1 g vial to be diluted to 50 mL with NS in an ADD Vantage infusion container. Dose concentrations between 1 mg per mL and 40 mg per mL are acceptable. Current IV drug reference text for intermittent infusions states, “Infuse over 30 minutes.”
a. Mg per mL concentration after dilution:
b. Is the concentration safe to administer?
c. Flow rate to administer over 30 minutes:
4. Pantroprazole sodium 40 mg IV infusion once daily for 10 days is ordered for a patient with severe gastroesophageal reflux disease (GERD). A 40 mg dose is reconstituted first with 10 mL NS and further diluted to total volume of 100 mL with D5W and infused over at least 15 minutes, per label instructions. The IV is programmed when you come on duty for 6.7 mL per minute on a pump.
a. Mg per mL after first dilution:
b. Mg per mL after final dilution:
c. Is the IV program approximately correct?
d. IV flow rate per hr: (to the nearest tenth of a mL)
5.  Cytoxan 5 mg per kg IV two times a week is ordered for an adult patient with malignant disease. The patient’s weight is 50 kg. The pharmacy has sent a diluted solution of 250 mg in 250 mL NS. Directions in current pharmacy reference say to infuse over at least 60 minutes. This order is to infuse over 90 minutes. When you arrive on duty, the IV is infusing at 100 mL per hr.
Cytoxan 5 mg per kg IV two times a week is ordered for an adult patient with malignant disease. The patient’s weight is 50 kg. The pharmacy has sent a diluted solution of 250 mg in 250 mL NS. Directions in current pharmacy reference say to infuse over at least 60 minutes. This order is to infuse over 90 minutes. When you arrive on duty, the IV is infusing at 100 mL per hr.
 CLINICAL ALERT
CLINICAL ALERT
Patient Safety Issue: Each nurse needs to refer to manufacturer instructions, current drug references, and personal calculations to protect the patient from prescriber, pharmacy, and prior caretaker IV drug, dosage, and/or flow rate errors and ADE or sentinel events.
High-risk drugs and powerful drugs are administered on an IV pump. Beware of prescribing, programming, and mechanical errors.
Evaluate the following orders and infusions for safety. Use a calculator to determine kilogram weights to the nearest tenth. Change micrograms to milligrams, when applicable, by moving decimals. Use a calculator to determine the SDR when needed. Double check and label all calculations. Prove the hourly flow rate calculation. If requested, decide whether the order/infusion is:
 Example
Example
1. Ordered: Dopamine HCl (Intropin) 4 mcg/kg/min IV for a 110-lb patient. The literature states that the usual dose is 2 to 5 mcg/kg/min. Available: Dopamine 200 mg in 250 mL D5W.

2.  Ordered: Dobutamine HCl (Dobutrex) 5 mcg/kg/min IV for a 132-lb patient. Available: Dobutamine 250 mg in 250 mL D5W. The flow rate is currently infusing at 36 mL/hr.
Ordered: Dobutamine HCl (Dobutrex) 5 mcg/kg/min IV for a 132-lb patient. Available: Dobutamine 250 mg in 250 mL D5W. The flow rate is currently infusing at 36 mL/hr.
c. Hourly drug order in mg*:
e. Hourly flow rate to be set on infusion device:
f. Is current infusion correct?

3.  Ordered: Lidocaine 4 mg/min. Available: 1 g of lidocaine in 500 mL of D5W.
Ordered: Lidocaine 4 mg/min. Available: 1 g of lidocaine in 500 mL of D5W.
a. TD : TV reduced ratio (mg : mL):
c. Hourly flow rate to be set on infusion device:

4.  Ordered: Isuprel (isoproterenol hydrochloride) 5 mcg/min. Available: Isoproterenol hydrochloride 1 mg in 250 mL D5W.
Ordered: Isuprel (isoproterenol hydrochloride) 5 mcg/min. Available: Isoproterenol hydrochloride 1 mg in 250 mL D5W.
b. Hourly drug ordered in mcg and in mg:
d. Hourly flow rate to be set on infusion device:

5.  Ordered: Initial infusion of norepinephrine at 50 mL/hr. Available: Norepinephrine 1 mg in 250 mL normal saline (NS). The SDR is 8 to 12 mcg/min initially.
Ordered: Initial infusion of norepinephrine at 50 mL/hr. Available: Norepinephrine 1 mg in 250 mL normal saline (NS). The SDR is 8 to 12 mcg/min initially.
b. Hourly drug being infused in mg:
c. Hourly drug order in mcg/hr:
d. Hourly drug order in mcg/min:

 CLINICAL ALERT
CLINICAL ALERT
Document IVs carefully according to hospital policies. Consult the prescriber if the flow rate needs adjustment.
Calculate and evaluate the following orders. Remember that the terms must be the same in your TD : TV :: HD : HV ratio and proportion.
 Example
Example
1. Ordered: Magnesium sulfate 2 g/hr IV. Available: Magnesium sulfate 40 g/250 mL Ringer’s lactate solution on an infusion device infusing at 13 mL/hr.

2.  Ordered: Pitocin (oxytocin) 20 milliunits/min. Available: 1000 mL D5NS with 10 units of Pitocin (1000 milliunits = 14; 1 unit). The IV is infusing at 100 mL/hr. (Hint: Change units to milliunits to obtain the total drug equivalent for the equation.)
Ordered: Pitocin (oxytocin) 20 milliunits/min. Available: 1000 mL D5NS with 10 units of Pitocin (1000 milliunits = 14; 1 unit). The IV is infusing at 100 mL/hr. (Hint: Change units to milliunits to obtain the total drug equivalent for the equation.)
b. TD (milliunits) : TV :: HD (milliunits) : HV ordered:

3.  Ordered: Terbutaline 10 mcg/min for 30 min. Available: Terbutaline 5 mg in 500 mL/D5W.
Ordered: Terbutaline 10 mcg/min for 30 min. Available: Terbutaline 5 mg in 500 mL/D5W.
b. Hourly drug ordered in mcg:
e. Hourly flow rate to be set on infusion device:

4.  Ordered: Magnesium sulfate 25 mL/hr. Call the doctor when 2 g have been infused. Available: 500 mL D5W with 20 g of magnesium sulfate on infusion device.
Ordered: Magnesium sulfate 25 mL/hr. Call the doctor when 2 g have been infused. Available: 500 mL D5W with 20 g of magnesium sulfate on infusion device.
a. TD (g) : TV reduced ratio in infusion:
b. TD : TV :: HD : HV (existing infusion):
d. Length of time 2 g to be infused:

5.  Ordered: Pitocin (oxytocin) 2 milliunits/min. Available: 10 units Pitocin in 1000 mL of D5NS.
Ordered: Pitocin (oxytocin) 2 milliunits/min. Available: 10 units Pitocin in 1000 mL of D5NS.
a. milliunits/mL of Pitocin in IV container:
e. Flow rate on infusion device to be set:

Calculate and evaluate the following infusion problems.
1.  Ordered: Esmolol hydrochloride at 39 mL/hr. Available: 5 g in 500 mL 5% D Ringer’s lactated solution. The patient weighs 143 lb. The SDR is 50 to 200 mcg/kg/min.
Ordered: Esmolol hydrochloride at 39 mL/hr. Available: 5 g in 500 mL 5% D Ringer’s lactated solution. The patient weighs 143 lb. The SDR is 50 to 200 mcg/kg/min.
b. SDR for this patient in mcg/min:
d. TD : TV :: HD : HV ratio ordered:
e. Hourly drug delivered in mg:
2.  Ordered: Nitroglycerin IV at 10 mcg/min. Available: Nitroglycerin IV 50 mg in 500 mL D5W. The infusion is flowing at 6 mL/hr.
Ordered: Nitroglycerin IV at 10 mcg/min. Available: Nitroglycerin IV 50 mg in 500 mL D5W. The infusion is flowing at 6 mL/hr.
a. TD : TV :: HD : HV ratio ordered:
c. TD : TV :: HD : HV infusing
3.  Ordered: Pronestyl (procainamide hydrochloride) at 50 mL/hr. Available: 1 g in 500 mL D5W. The SDR for maintenance is 1 to 6 mg/min.
Ordered: Pronestyl (procainamide hydrochloride) at 50 mL/hr. Available: 1 g in 500 mL D5W. The SDR for maintenance is 1 to 6 mg/min.
b. Hourly drug delivered in mg:
4.  Ordered: Nipride (sodium nitroprusside) at 0.3 mcg/kg/min. Available: 50 mg sodium nitroprusside in 250 mL NS. The infusion is flowing at 15 mL/hr. The patient weighs 220 lb.
Ordered: Nipride (sodium nitroprusside) at 0.3 mcg/kg/min. Available: 50 mg sodium nitroprusside in 250 mL NS. The infusion is flowing at 15 mL/hr. The patient weighs 220 lb.
c. TD : TV :: HD : HV ratio ordered:
d. TD : TV :: HD : HV ratio infusing:
e. Hourly drug infusing in mg:
5. Ordered: Cardizem (diltiazem hydrochloride) at 15 mg/hr. Available: Diltiazem hydrochloride 125 mg in 25 mL diluent to be added to 100 mL D5W. Infusion is flowing at 15 mL/hr.
Direct IV (Bolus) Administration with a Syringe
Direct IV administration (IV push) is used to administer small amounts of diluted or undiluted medication over a brief period (seconds or minutes), preferably into a vascular access device.
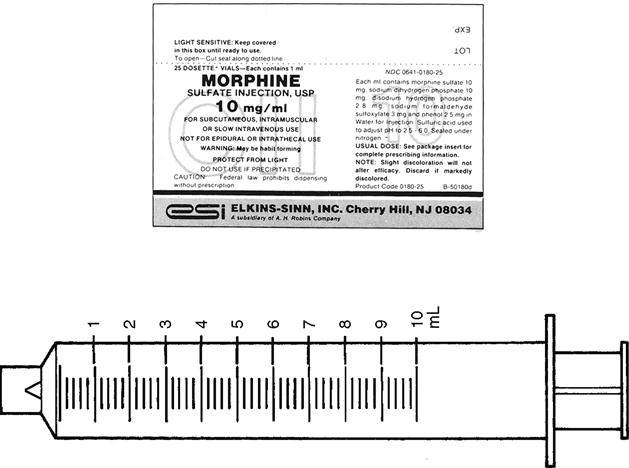
Medications such as morphine, Dilantin, or furosemide may be prepared in a syringe and then delivered directly via an intermittent IV med-lock or the proximal port of an existing continuous IV.
 CLINICAL ALERT
CLINICAL ALERT
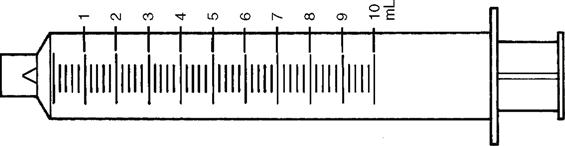
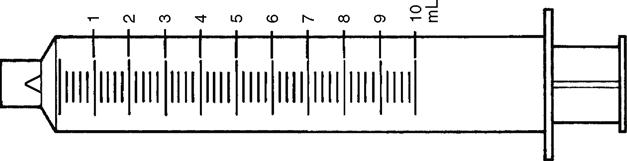
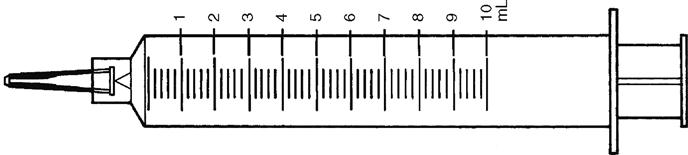
Many of the medications that are administered in this manner must be diluted. A wide barrel (diameter) syringe such as a 10-mL syringe is preferred in order to reduce pressure during administration. Check agency policies for flushes and other direct IV push medications.
It is crucial that the literature be consulted for safe-dose limits, rates of flow, dilutions, compatible solutions, and routes, and that the patient’s response be closely monitored during the administration and afterwards.
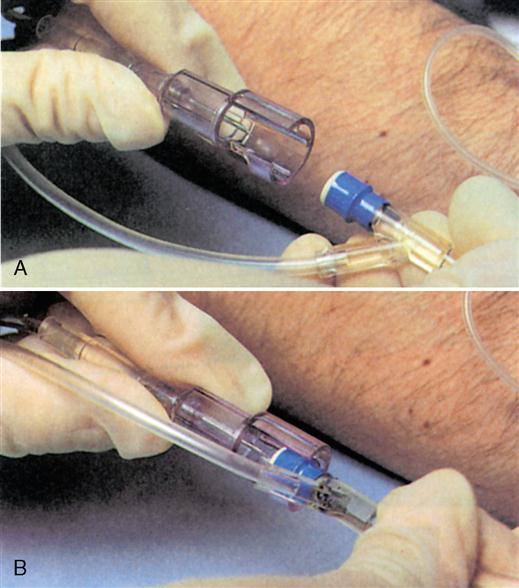
To reduce needlestick injuries, the trend is to use infusion systems with safety features (Figure 8-3).
There are two ways to time IV push medications for direct administration of medication through a syringe. Regardless of the method you select, the first step is always to calculate and prepare the correct volume.
Timing IV Push Medications—Method 1 (mL per Minute)
This method calculates the amount in milliliters to be slowly and gradually pushed over each minute.
Formula

Example
Ordered: Digoxin 0.5 mg IV over 5 min. Dilute to 4 mL sterile water for injection.
4 mL : 5 min :: mL : 1 min

Schedule
| Schedule | 1600: 00 | 4 mL in syringe |
| 1601 | 3.2 mL remaining | |
| 1602 | 2.4 mL remaining | |
| 1603 | 1.6 mL remaining | |
| 1604 | 0.8 mL remaining | |
| 1605 | 0 remaining |

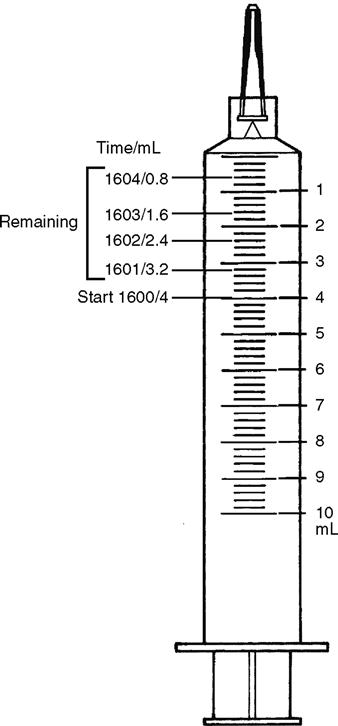
The schedule above reflects a start time of 1600 hours. It is helpful to write your start time and a schedule of “markers” (increments of time and volume) when you need to push over several minutes. Write this before beginning to inject and have it in front of you to avoid errors caused by distraction.
Safety syringes and needleless syringes are being used to reduce needlestick injuries (Figure 8-4).
Timing IV Push Medications—Method 2 (Seconds per Calibration)
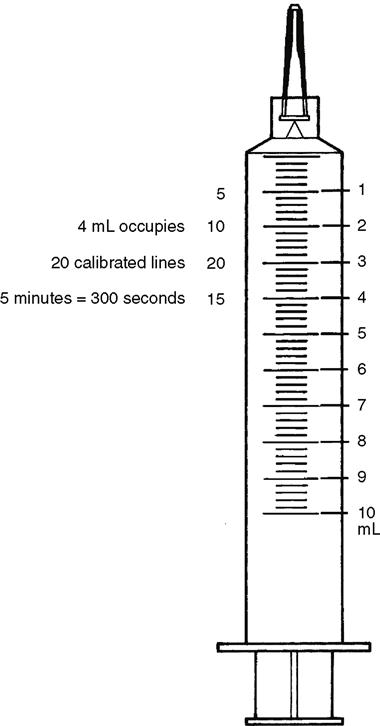
Many IV push medications have dilutions that permit 1 mL/min so that the timing is easy to maintain. Occasionally, when the timing is to be very slow and is not 1 mL/min, counting seconds per calibration permits more precise timing of the injection.
RULE
Divide the number of seconds of total time of administration by the number of calibrated increments in a syringe prepared with medication (lines on the syringe within each milliliter). This will yield the seconds per increment to be pushed.
Formula

Example
Give 0.5 mg digoxin IV over 5 min. Directions say to dilute to 4 mL of sterile water for injection. There are 20 calibrations in 4 mL on this syringe.

Use the second hand on your watch and/or count each cycle (1 to 15) as you administer the medication, 1 calibration (0.2 mL) every 15 seconds.
Tip: start count when the second hand is on 12.
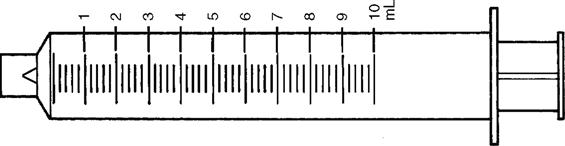
Solve the following problems using the syringes shown to calculate the seconds per calibration, if applicable, and mL/min to be administered.
1. Ordered: 10% calcium chloride (10 mL) over 5 min.
a. For how many seconds will you administer each calibration?
b. How many mL/min will be injected?
2. Ordered: Digoxin 0.5 mg IV over 10 min. (The literature specifies a minimum of 5 min for administration.) Available: Digoxin 250 mcg/mL.
b. Total seconds for injection:
3. Ordered: Phenytoin sodium IV loading dose of 900 mg at 50 mg/min on an infusion device (Figure 8-5). Available: Phenytoin 100 mg/mL.
4. Ordered: Furosemide 20 mg IV undiluted over 2 min. Available: Furosemide 10 mg/mL.
5.  Ordered: Morphine Sulfate 4 mg IV injection. The literature states that a single dose should be administered over 4 to 5 min and that the dose may be diluted in 4 to 5 mL with sterile water or normal saline for injection. The nurse dilutes it to 5 (mL) with NS.
Ordered: Morphine Sulfate 4 mg IV injection. The literature states that a single dose should be administered over 4 to 5 min and that the dose may be diluted in 4 to 5 mL with sterile water or normal saline for injection. The nurse dilutes it to 5 (mL) with NS.

Use a calculator. Estimate your answers for each applicable step in the mathematics. Establish the reduced total drug/total volume ratio for the infusions, move decimals to convert between micrograms and milligrams, and use logical shortcuts such as multiplying by 60 to change minutes to hours where applicable.
1.  Ordered: Isoproterenol HCl IV at 5 mcg/min. How many mg/hr would be infused?
Ordered: Isoproterenol HCl IV at 5 mcg/min. How many mg/hr would be infused?
2.  Available: Aminophylline 250 mg in 1000 mL of D5W. How many milligrams are in each milliliter of the IV solution (mg/mL)?
Available: Aminophylline 250 mg in 1000 mL of D5W. How many milligrams are in each milliliter of the IV solution (mg/mL)?
3.  Available: 1 g of lidocaine in 500 mL of D5W. What is the total drug ratio in mg to the total volume of IV solution?
Available: 1 g of lidocaine in 500 mL of D5W. What is the total drug ratio in mg to the total volume of IV solution?
4.  Available: Norepinephrine 1 mg in 250 mL of NS. The SDR is 8 to 12 mcg/min initially. What is the minimum flow rate recommendation in mL/hr? Hint: Change the SDR to milligrams after you obtain the SDR in mcg/hr so that you can compare milligrams to milligrams.
Available: Norepinephrine 1 mg in 250 mL of NS. The SDR is 8 to 12 mcg/min initially. What is the minimum flow rate recommendation in mL/hr? Hint: Change the SDR to milligrams after you obtain the SDR in mcg/hr so that you can compare milligrams to milligrams.
5. Ordered: Furosemide 30 mg IV push over 2 min. Available: Furosemide 10 mg/mL. How many mL/min are to be administered?
6.  Ordered: Lanoxin IV push 0.5 mg over 5 min. Available: Lanoxin 250 mcg/mL. How many mL/min will be injected?
Ordered: Lanoxin IV push 0.5 mg over 5 min. Available: Lanoxin 250 mcg/mL. How many mL/min will be injected?
7.  Procainamide hydrochloride is infusing at 40 mL/hr (per the prescriber order) for maintenance in an adult with an arrhythmia. Available: 1 g in 500 mL D5W. The SDR for maintenance is 1 to 6 mg/min. What decision will the nurse make?
Procainamide hydrochloride is infusing at 40 mL/hr (per the prescriber order) for maintenance in an adult with an arrhythmia. Available: 1 g in 500 mL D5W. The SDR for maintenance is 1 to 6 mg/min. What decision will the nurse make?
a. The order is within SDR. Proceed with the IV.
b. The order is above the SDR. Hold the infusion and clarify with the physician.
c. The order is below SDR. Start the infusion and consult with the physician.
d. The order is unclear. Consult with a knowledgable colleague.
8.  Ordered: Procainamide hydrochloride at 60 mg/hr on an infusion device. Available: 1 g in 1000 mL D5W. What flow rate in mL/hr will the nurse set?
Ordered: Procainamide hydrochloride at 60 mg/hr on an infusion device. Available: 1 g in 1000 mL D5W. What flow rate in mL/hr will the nurse set?
9.  Ordered: Magnesium sulfate 30 mL/hr. Call the physician when 3 g have been infused. Available: 500 mL D5W with 20 g of magnesium sulfate on an infusion device. In how much time will you expect to call the physician at this flow rate? Hint: Determine how much drug per hour is infusing.
Ordered: Magnesium sulfate 30 mL/hr. Call the physician when 3 g have been infused. Available: 500 mL D5W with 20 g of magnesium sulfate on an infusion device. In how much time will you expect to call the physician at this flow rate? Hint: Determine how much drug per hour is infusing.
10.  Ordered: Dobutamine HCl 2.5 mcg/kg/min for a 70-kg patient. Available: Dobutamine HCl IV concentration 500 mcg/mL. What flow rate will you set in mL/hr?
Ordered: Dobutamine HCl 2.5 mcg/kg/min for a 70-kg patient. Available: Dobutamine HCl IV concentration 500 mcg/mL. What flow rate will you set in mL/hr?
Solve the following problems using a calculator, moving decimals, reducing ratios, and labeling your answers. Prove your work.
1.  Ordered: Dobutamine HCl 5 mcg/kg/min. Available: Dobutamine HCl 2000 mcg/mL in an infusion device. Patient’s weight is 50 kg.
Ordered: Dobutamine HCl 5 mcg/kg/min. Available: Dobutamine HCl 2000 mcg/mL in an infusion device. Patient’s weight is 50 kg.
b. Flow rate to be set on IV infusion device: ________ hr
2.  Ordered: Potassium chloride 10 mEq to be administered to a 44-lb child with hypokalemia. Administer over 4 hr. Dilute in 100 mL of D5W. The literature states that the rate should not exceed 3 mEq/kg/24 hr for a child.
Ordered: Potassium chloride 10 mEq to be administered to a 44-lb child with hypokalemia. Administer over 4 hr. Dilute in 100 mL of D5W. The literature states that the rate should not exceed 3 mEq/kg/24 hr for a child.
b. SDR for this child per 24 hr:
e. Amount of drug in mL to be added to IV (refer to label for mEq/mL):
f. Hourly flow rate on infusion device in mL:

3.  Ordered: Dopamine HCl at 2 mcg/kg/min. Infusing when you enter the room: Dopamine HCl at 15 mL/hr. Available: Dopamine HCl 400 mg/500 mL. Patient’s weight is 80 kg.
Ordered: Dopamine HCl at 2 mcg/kg/min. Infusing when you enter the room: Dopamine HCl at 15 mL/hr. Available: Dopamine HCl 400 mg/500 mL. Patient’s weight is 80 kg.
e. Decision (correct or needs order for change):
4.  Ordered: Dopamine IV at 4 mcg/kg/min for a patient in septic shock who weighs 110 lb today. The SDR is 2 to 10 mcg/kg/min. The IV solution contains 200 mg in 250 mL of solution. The IV is flowing at 15 mL/hr when you enter the room.
Ordered: Dopamine IV at 4 mcg/kg/min for a patient in septic shock who weighs 110 lb today. The SDR is 2 to 10 mcg/kg/min. The IV solution contains 200 mg in 250 mL of solution. The IV is flowing at 15 mL/hr when you enter the room.
h. Decision (correct or needs order for change):

5.  Ordered: Dilaudid (hydromorphone HCl) 3 mg direct IV for a patient with severe pain. Directions state it may be given undiluted slowly or diluted up to 5 mL with SW or NS to facilitate titration. It may be administered over 2 to 5 minutes slowly. The nurse dilutes it to 3 mL and plans to administer it over 3 minutes.*
Ordered: Dilaudid (hydromorphone HCl) 3 mg direct IV for a patient with severe pain. Directions state it may be given undiluted slowly or diluted up to 5 mL with SW or NS to facilitate titration. It may be administered over 2 to 5 minutes slowly. The nurse dilutes it to 3 mL and plans to administer it over 3 minutes.*

a. Total amount of Dilaudid to be prepared (in mL, round to nearest tenth):
b. Total amount of diluted volume to be administered in mL:
 CLINICAL ALERT
CLINICAL ALERT
*When small amounts of medication are ordered, dilution makes it easier to control the rate of injection. This nurse wants to administer 1 mL per minute for ease of administration. There were other options. Always read the directions for dilution and rate of administration. If the patient begins to have side effects, the medication will be withdrawn. It is safer and always preferable to inject into an existing IV port or line so that side effects can be countered quickly when necessary.