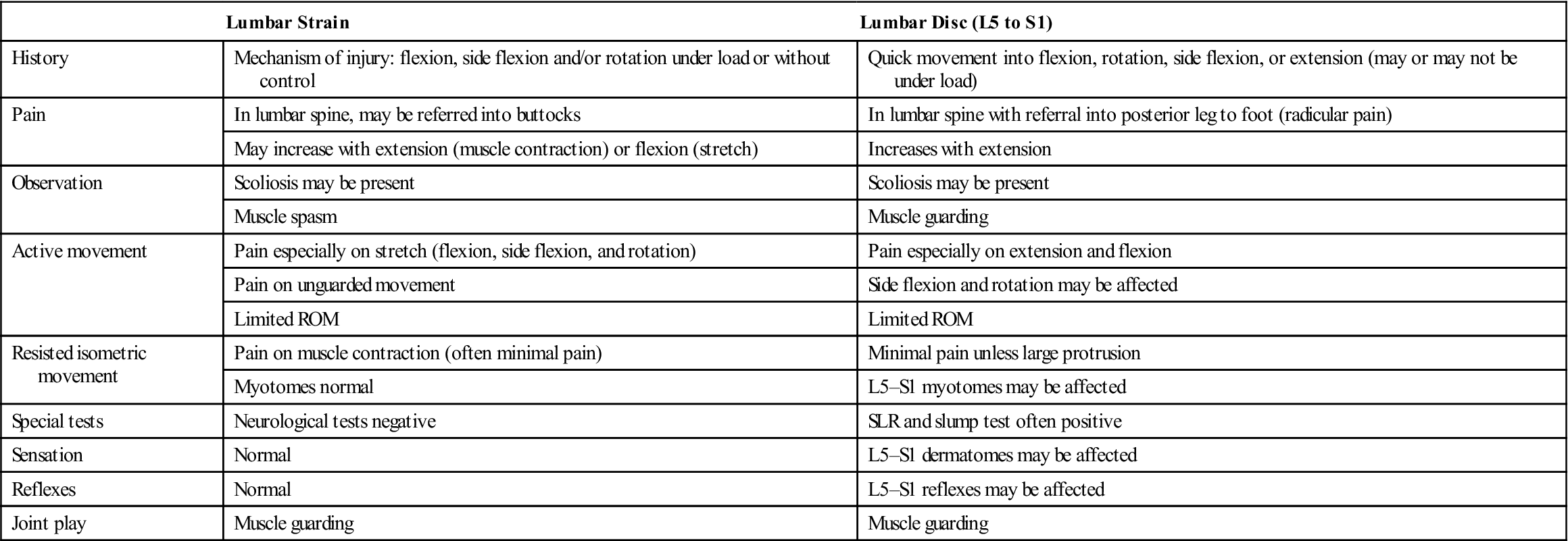
TABLE 9-14
Straight Leg Raising Test and Its Modifications
| SLR (Basic) | SLR2 | SLR3 | SLR4 | Cross (Well Leg) SLR5 | |
| Hip | Flexion and adduction | Flexion | Flexion | Flexion and medial rotation | Flexion |
| Knee | Extension | Extension | Extension | Extension | Extension |
| Ankle | Dorsiflexion | Dorsiflexion | Dorsiflexion | Plantar flexion | Dorsiflexion |
| Foot | — | Eversion | Inversion | Inversion | — |
| Toes | — | Extension | — | — | — |
| Nerve bias | Sciatic nerve and tibial nerve | Tibial nerve | Sural nerve | Common peroneal nerve | Nerve root (disc prolapse) |

Data from Butler, D.A.: Mobilisation of the nervous system. Melbourne, 1991, Churchill Livingstone.

A, Basic SLR and SLR2 (sciatic and tibial nerves). B, SLR3 (sural nerve). C, SLR4 (common peroneal nerve). D, SLR5 (intervertebral disc and nerve root). See Table 9-14 for movements at each joint.
The neck flexion movement has also been called Hyndman's sign, Brudzinski sign, Linder sign, and the Soto-Hall test. If the examiner desires, neck flexion may be done by itself as a passive movement (passive neck flexion). Tension in the cervicothoracic junction is normal and should not be considered a production of symptoms. If lumbar, leg, or arm symptoms are produced, the neurological tissue is involved. The ankle dorsiflexion movement has also been called the Bragard's test. Pain that increases with neck flexion, ankle dorsiflexion, or both indicates stretching of the dura mater of the spinal cord or a lesion within the spinal cord (e.g., disc herniation, tumor, meningitis). Pain that does not increase with neck flexion may indicate a lesion in the hamstring area (tight hamstrings) or in the lumbosacral or sacroiliac joints. Sicard's test involves straight leg raising and then extension of the big toe instead of foot dorsiflexion. Turyn's test involves only extension of the big toe.200
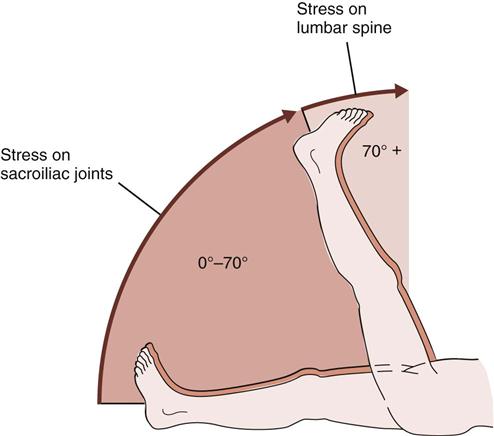
With unilateral straight leg raising, the nerve roots, primarily the L5, S1, and S2 nerve roots (sciatic nerve), are normally completely stretched at 70°, having an excursion of approximately 2 to 6 cm (0.8 to 2.4 inches).195 Pain after 70° is probably joint pain from the lumbar area (e.g., facet joints) or sacroiliac joints (Figure 9-66). However, if the examiner suspects hamstring tightness, the hamstrings must also be cleared by examination (see Chapter 11). The examiner should compare the two legs for any differences. Although the sciatic nerve roots are commonly stretched at 70° hip flexion, the ROM for straight leg raising and the stress placed on the neurological tissue vary greatly from person to person. For example, patients who are very hypermobile (e.g., gymnasts, synchronized swimmers) may not show a positive straight leg raising test until 110° to 120° of hip flexion, even in the presence of nerve root pathology. It is more important to compare left and right sides for symptoms before deciding whether a lesion is caused by stretching of the neurological tissue or arises from the joints or other soft tissues.
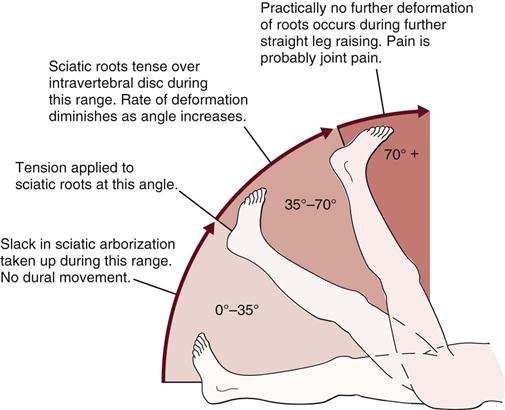
During the unilateral straight leg raising test, tension develops in a sequential manner. It first develops in the greater sciatic foramen, then over the ala of the sacrum, next in the area where the nerve crosses over the pedicle, and finally in the intervertebral foramen. The test causes traction on the sciatic nerve, lumbosacral nerve roots, and dura mater. Adhesions within these areas may result from herniation of the intervertebral disc or extradural or meningeal irritation. Pain comes from the dura mater, nerve root, adventitial sheath of the epidural veins, or synovial facet joints. The test is positive if pain extends from the back down into the leg in the sciatic nerve distribution.
A central protrusion of an intervertebral disc (L4 or L5 disc affecting nerve roots from L4 down to S3) leads to pain primarily in the back with the possibility of bowel and bladder symptoms; a protrusion in the intermediate area causes pain in the posterior aspect of the lower limb and low back; and a lateral protrusion causes pain primarily in the posterior leg with pain below the knee. Having said this, however, the examiner must realize that the intervertebral disc is only one cause of back pain.
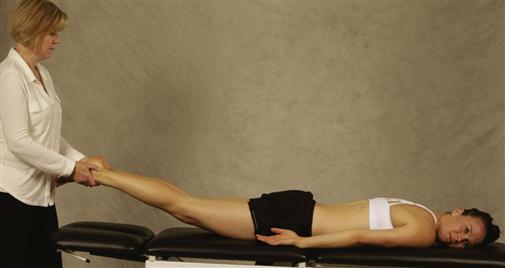
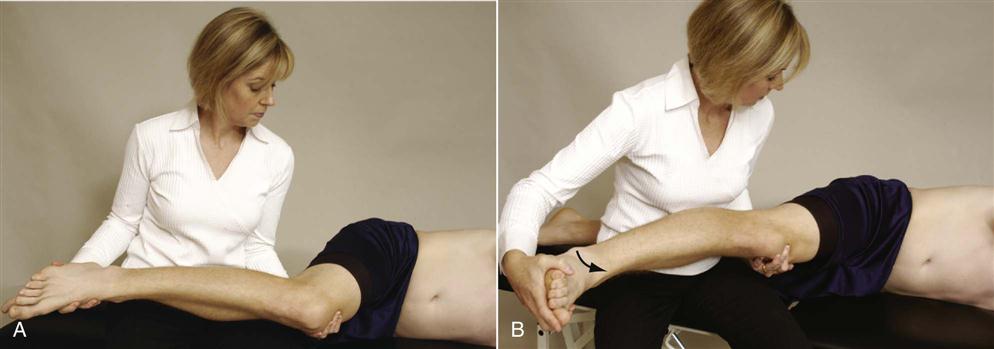
For patients who have difficulty lying supine, a modified straight leg raising test has been suggested.201 The patient is in a side lying position with the test leg uppermost and the hip and knee at 90°. The lumbosacral spine is in neutral but may be positioned in slight flexion or extension if this is more comfortable for the patient. The examiner then passively extends the patient's knee (Figure 9-67), noting pain, resistance, and reproduction of the patient's symptoms for a positive test. The knee position (amount of flexion remaining) on the affected side is compared with that on the good side.
The examiner should then test both legs simultaneously (bilateral straight leg raising ![]() , Figure 9-68). This test must be done with care, because the examiner is lifting the weight of both lower limbs and thereby placing a large stress on the examiner's lumbar spine. With the patient relaxed in the supine position and knees extended, the examiner lifts both of the legs by flexing the patient's hips until the patient complains of pain or tightness. Because both legs are lifted the pelvis is not stabilized (as it would be by one leg in unilateral straight leg raise), so on hip flexion the pelvis is freer to rotate, thereby decreasing the stress on the neurological tissue. If the test causes pain before 70° of hip flexion, the lesion is probably in the sacroiliac joints; if the test causes pain after 70°, the lesion is probably in the lumbar spine area.
, Figure 9-68). This test must be done with care, because the examiner is lifting the weight of both lower limbs and thereby placing a large stress on the examiner's lumbar spine. With the patient relaxed in the supine position and knees extended, the examiner lifts both of the legs by flexing the patient's hips until the patient complains of pain or tightness. Because both legs are lifted the pelvis is not stabilized (as it would be by one leg in unilateral straight leg raise), so on hip flexion the pelvis is freer to rotate, thereby decreasing the stress on the neurological tissue. If the test causes pain before 70° of hip flexion, the lesion is probably in the sacroiliac joints; if the test causes pain after 70°, the lesion is probably in the lumbar spine area.
With the unilateral straight leg raising test, 80° to 90° of hip flexion is normal. If one leg is lifted and the patient complains of pain on the opposite side, it is an indication of a space-occupying lesion (e.g., a herniated disc, inflammatory swelling). This finding of pain when the examiner is testing the opposite (good) leg may be called the well leg raising test of Fajersztajn (Figure 9-69), a prostrate leg raising test, a sciatic phenomenon, Lhermitt's test, or the crossover sign ![]() .182,195,202 It is typically indicates a rather large intervertebral disc protrusion, usually medial to the nerve root (see Figure 9-69), and a poor prognosis for conservative treatment.197,203 The test causes stretching of the ipsilateral as well as the contralateral nerve root, pulling laterally on the dural sac. A positive Lasègue's and crossover sign can also indicate the degree of disc injury. For example, both are limited to a greater degree if sequestration of the disc occurs.86 If the examiner finds this test positive, careful questioning about bowel and bladder symptoms is a necessity. Many, but not all, patients with a central protrusion are candidates for surgery, especially if there are bowel and bladder symptoms.
.182,195,202 It is typically indicates a rather large intervertebral disc protrusion, usually medial to the nerve root (see Figure 9-69), and a poor prognosis for conservative treatment.197,203 The test causes stretching of the ipsilateral as well as the contralateral nerve root, pulling laterally on the dural sac. A positive Lasègue's and crossover sign can also indicate the degree of disc injury. For example, both are limited to a greater degree if sequestration of the disc occurs.86 If the examiner finds this test positive, careful questioning about bowel and bladder symptoms is a necessity. Many, but not all, patients with a central protrusion are candidates for surgery, especially if there are bowel and bladder symptoms.
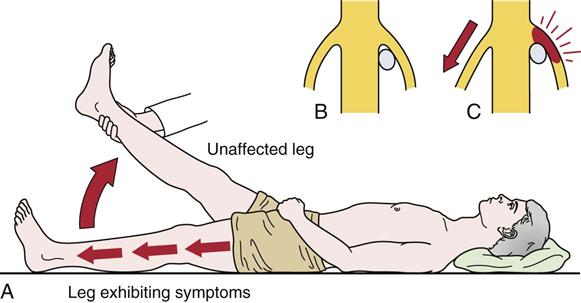
A, Movement of nerve roots occurs when the leg on the opposite side is raised. B, Position of disc and nerve root before opposite leg is lifted. C, When the leg is raised on the unaffected side, the roots on the opposite side slide slightly downward and toward the midline. In the presence of a disc lesion, this movement increases the root tension resulting in radicular signs in the affected leg, which remains on the table. (Modified from DePalma AF, Rothman RH: The intervertebral disc, Philadelphia, 1970, WB Saunders.)
 Valsalva Maneuver.
Valsalva Maneuver.
The seated patient is asked to take a breath, hold it, and then bear down as if evacuating the bowels (Figure 9-70). If pain increases, it indicates increased intrathecal pressure. The symptoms may be accentuated by having the patient first flex the hip to a position just short of that causing pain.195
Tests for Lumbar Instability
Lumbar instability implies that during movement, the patient loses the ability to control the movement for a brief time (milliseconds), or it may mean the segment is structurally unstable. The brief loss of control often results in a painful catch, apprehension, or an instability jog (sudden shift of movement in part of the ROM).87,204 Pope called this “loss of control in the neutral spine.”205 It commonly occurs with spondylosis owing to degeneration of the disc.205,206 Structural instability primarily results from spondylolisthesis, and the following tests are designed to test for structural instability.
 Farfan Torsion Test.32,38
Farfan Torsion Test.32,38
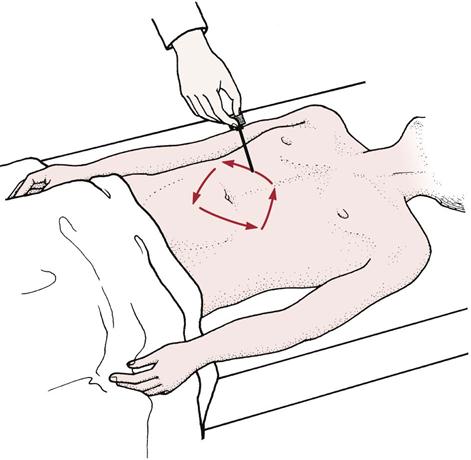
This nonspecific test stresses the facet joints, joint capsule, supraspinous and interspinous ligaments, neural arch, the longitudinal ligaments, and the disc. The patient lies prone. The examiner stabilizes the ribs and spine (at about T12) with one hand and places the other hand under the anterior aspect of the ilium. The examiner then pulls the ilium backward (Figure 9-71) causing the spine to be rotated on the opposite side producing torque on the opposite side. The test is said to be positive if it reproduces all or some of the patient's symptoms. The other side is tested for compression.
 H and I Stability Tests.75,92
H and I Stability Tests.75,92
This set of movements tests for muscle spasm and can be used to detect instability. The H and I monikers relate to the movements that occur (Figure 9-72).
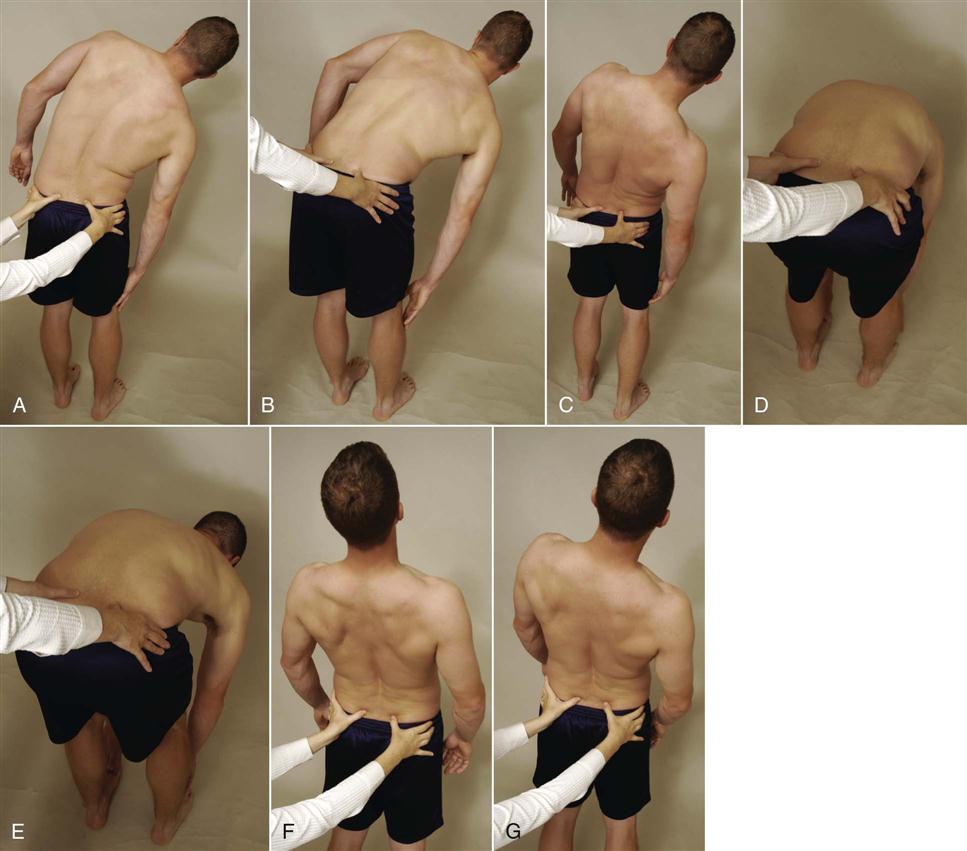
 Figure 9-72 H and I stability tests.
Figure 9-72 H and I stability tests.A, H test—side flexion. B, H test—side flexion followed by forward flexion. C, H test—side flexion followed by extension. D, I test—forward flexion. E, I test—forward flexion and side flexion. F, I test—extension. G, I test—extension and side flexion.
The first part of the test is the “H” movement. The patient stands in the normal resting position, which would be considered the center of the “ ”. The pain-free side is tested first. The patient is asked, with guidance from the clinician, to side flex as far as possible (the side of “
”. The pain-free side is tested first. The patient is asked, with guidance from the clinician, to side flex as far as possible (the side of “ ”). While in this position, the patient is then asked to flex (the front of the “
”). While in this position, the patient is then asked to flex (the front of the “ ”) and then move into extension (the back of the “
”) and then move into extension (the back of the “ ”). If flexion was more painful than extension, then extension would be done before flexion. The patient then returns to neutral and repeats the movements to the other side. The clinician may stabilize the pelvis with one hand and guide the movement with the other hand on the shoulder.
”). If flexion was more painful than extension, then extension would be done before flexion. The patient then returns to neutral and repeats the movements to the other side. The clinician may stabilize the pelvis with one hand and guide the movement with the other hand on the shoulder.
The second part of the test is the “I” movement. The patient stands in the normal resting position, which would be considered the center of the “ ”. Pain-free movement (flexion or extension) is tested first. With guidance from the clinician, the patient is asked to forward flex (or extend) the lumbar spine until the hips start to move (top part of “
”. Pain-free movement (flexion or extension) is tested first. With guidance from the clinician, the patient is asked to forward flex (or extend) the lumbar spine until the hips start to move (top part of “ ”). Once in flexion, the patient is guided into side bending (to the pain free side first “
”). Once in flexion, the patient is guided into side bending (to the pain free side first “ ”) followed by return to neutral and then side bending to the opposite side. The patient then returns to neutral standing and does the opposite movement (extension in this case) followed by side bending.
”) followed by return to neutral and then side bending to the opposite side. The patient then returns to neutral standing and does the opposite movement (extension in this case) followed by side bending.
If a hypomobile segment is present, at least two of the movements (the movements into the same quadrant [for example, the top right of the “H” and “I”]) would be limited. If instability is present, one quadrant will again be affected, but only by one of the moves (i.e., by the “H” movement or the “I” movement—not both). For example, if the patient had spondylolisthesis instability in anterior shear (a component of forward flexion) and the “I” is attempted, the shear or slip occurs on forward flexion, and there is little movement during the attempted side bending or flexion. If the “H” is attempted, the side bending is normal, and the following forward flexion is full because the shear occurs in the second phase. So, in this case, the “I” movement is limited but not the “H” movement. This test is primarily for structural instability, but an instability jog may be evident during one of the movements if loss of control occurs. In this case, the end range is commonly normal, but loss of control occurs somewhere in the available ROM.
 Lateral Lumbar Spine Stability Test.92
Lateral Lumbar Spine Stability Test.92
The patient is placed in side lying with the lumbar spine in neutral. The examiner places the forearm over the side of the thorax at about the L3 level as an example. The examiner then applies a downward pressure to the transverse process of L3, which produces a shear to the side on which the patient is lying for vertebra below L3 and a relative lateral shear in the opposite direction to the segments above L3 (Figure 9-73). The production of the patient's symptoms indicates a positive test.
 Passive Lumbar Extension Test.207,208
Passive Lumbar Extension Test.207,208
The patient lies prone and relaxed. The examiner passively lifts and extends both extremities at the same time to about 1 foot (30 cm) from the bed. While maintaining the extension, the examiner gently pulls the legs (Figure 9-74). The test is considered positive if, in the extended position, the patient complains of strong pain in the lumbar region, very heavy feeling in the low back, or it feels like the low back is “coming off” and the pain disappears when the legs are lowered to the start position. Numbness or prickling sensation are not positive signs.
 Pheasant Test.
Pheasant Test.
The patient lies prone. With one hand, the examiner gently applies pressure to the posterior aspect of the lumbar spine. With the other hand, the examiner passively flexes the patient's knees until the heels touch the buttocks (Figure 9-75). If this hyperextension of the spine causes the patient to feel pain in the leg, the test is considered positive and indicates an unstable spinal segment.209
 Prone Segmental Instability Test.
Prone Segmental Instability Test.
The patient lies prone with the body on the examining table and the legs over the edge resting on the floor (Figure 9-76 ). The examiner applies pressure to the posterior aspect of the lumbar spine while the patient rests in this position. The patient then lifts the legs off the floor, and the examiner again applies posterior compression to the lumbar spine. If pain is elicited in the resting position only, the test is positive, because the muscle action masks the instability.210,211
 Specific Lumbar Spine Torsion Test.75,92
Specific Lumbar Spine Torsion Test.75,92
This test stresses specific levels of the lumbar spine. To do this, the specific level must be rotated and stressed. An example would be testing the integrity of left rotation on L5 S1. The patient is placed in a right side lying position with the lumbar spine in slight extension (slight lordosis). To achieve rotation and side bending, the examiner grasps the right arm and pulls it upward and forward at a 45° angle until movement is felt at the L5 spinous process. This “locks” all the vertebrae above L5. The examiner then stabilizes the L5 spinous process by holding the left shoulder back with the examiner's elbow while rotating the pelvis and sacrum forward until S1 starts to move (Figure 9-77) with the opposite hand. Minimal movement should occur, and a normal capsular tissue stretch should be felt when L5 S1 is stressed by carefully pushing the shoulder back with the elbow and rotating the pelvis forward with the other arm/hand. This test position is a common position used to manipulate the spine, so the examiner should take care not to overstress the rotation during assessment. In some cases, when doing the test, the examiner may hear a “click” or “pop.” This is the same “pop” or “click” that would be heard with a manipulation.
 Test of Anterior Lumbar Spine Instability.92
Test of Anterior Lumbar Spine Instability.92
The patient is placed in side lying with the hips flexed to 70° and knees flexed. The examiner palpates the desired spinous processes (e.g., L4 to L5). By pushing the patient's knees posteriorly with the body along the line of the femur, the examiner can feel the relative movement of the L5 spinous process on L4 (Figure 9-78). Normally, there should be little or no movement. Other levels of the spine may be tested in a similar fashion. A problem with the test is that the examiner should ensure that the posterior ligaments of the spine are relatively loose or relaxed. This can be controlled by altering the amount of hip flexion. With greater hip flexion, the posterior ligaments tighten more from the bottom (sacrum) up.
 Test of Posterior Lumbar Spine Instability.92
Test of Posterior Lumbar Spine Instability.92
The patient sits on the edge of the examining table. The examiner stands in front of the patient. The patient places the pronated arms with elbows bent on the anterior aspect of the examiner's shoulders. The examiner puts both hands around the patient so the fingers rest over the lumbar spine and with the heels of the hands gently pull the lumbar spine into full lordosis. To stress L5 on S1, the examiner stabilizes the sacrum with the fingers of both hands and asks the patient to push through the forearm while maintaining the lordotic posture (Figure 9-79). This produces a posterior shear of L5 on S1. Other levels of the spine may be tested in a similar fashion.
Tests for Joint Dysfunction
 McKenzie's Side Glide Test.
McKenzie's Side Glide Test.
The patient stands with the examiner standing to one side. The examiner grasps the patient's pelvis with both hands and places a shoulder against the patient's lower thorax. Using the shoulder as a block, the examiner pulls the pelvis toward the examiner's body (Figure 9-80). The position is held for 10 to 15 seconds, and then the test is repeated on the opposite side.39,184 If the patient has an evident scoliosis, the side to which the scoliosis curves should be tested first. A positive test is indicated by increased neurological symptoms on the affected side. It also indicates whether the symptoms are actually causing the scoliosis.
 Milgram's Test.
Milgram's Test.
The patient lies supine and actively lifts both legs simultaneously off the examining table 5 to 10 cm (2 to 4 inches), holding this position for 30 seconds. The test is positive if the limbs or affected limb cannot be held for 30 seconds or if symptoms are reproduced in the affected limb.183,184 This test should always be performed with caution because of the high stress load placed on the lumbar spine.
 One-Leg Standing (Stork Standing) Lumbar Extension Test.
One-Leg Standing (Stork Standing) Lumbar Extension Test.
The patient stands on one leg and extends the spine while balancing on the leg (Figure 9-81). The test is repeated with the patient standing on the opposite leg. A positive test is indicated by pain in the back and is associated with a pars interarticularis stress fracture (spondylolisthesis). If the stress fracture is unilateral, standing on the ipsilateral leg causes more pain.212–214 If rotation is combined with extension and pain results, this indicates possible facet joint pathology on the side to which rotation occurs.
 Quadrant (Extension Quadrant) Test.
Quadrant (Extension Quadrant) Test.
The patient stands with the examiner standing behind. The patient extends the spine while the examiner controls the movement by holding the patient's shoulders. The examiner may use his or her shoulders to hold the occiput and take the weight of the head. Overpressure is applied in extension while the patient side flexes and rotates to the side of pain. The movement is continued until the limit of range is reached or until symptoms are produced (Figure 9-82). The position causes maximum narrowing of the intervertebral foramen and stress on the facet joint to the side on which rotation occurs.215 The test is positive if symptoms are produced.216 Cipriano described a similar test as Kemp's test.200
 Schober Test.
Schober Test.
The Schober test may be used to measure the amount of flexion occurring in the lumbar spine. A point is marked midway between the two PSISs (“dimples of the pelvis”), which is the level of S2; then, points 5 cm (2 inches) below and 10 cm (4 inches) above that level are marked. The distance between the three points is measured, the patient is asked to flex forward, and the distance is remeasured. The difference between the two measurements indicates the amount of flexion occurring in the lumbar spine. Little reported a modification of the Schober test to measure extension as well.217 After completion of the flexion movement, the patient extends the spine, and the distance between the marks is noted. Little also advocated using four marking points (one below the dimples and three above) with 10 cm (4 inches) between them.
 Yeoman's Test.
Yeoman's Test.
The patient lies prone while the examiner stabilizes the pelvis and extends each of the patient's hips in turn with the knees extended. The examiner then extends each of the patient's legs in turn with the knee flexed. In both cases, the patient remains passive. A positive test is indicated by pain in the lumbar spine during both parts of the test.
Tests for Muscle Tightness
 90–90 Straight Leg Raising Test.
90–90 Straight Leg Raising Test.
See “Tests for Tight Hamstrings” in Chapter 11.
 Ober Test.
Ober Test.
See “Tests for Tight Tensor Fasciae Latae” in Chapter 11.
 Rectus Femoris Test.
Rectus Femoris Test.
See “Tests for Tight Rectus Femoris” in Chapter 11.
 Thomas Test.
Thomas Test.
See “Tests for Tight Iliopsoas” in Chapter 11.
Tests for Muscle Dysfunction
 Beevor Sign.
Beevor Sign.
The patient lies supine. The patient flexes the head against resistance, coughs, or attempts to sit up with the hands resting behind the head.183,218 The sign is positive if the umbilicus does not remain in a straight line when the abdominals contract, indicating pathology in the abdominal muscles (i.e., paralysis).
Tests for Intermittent Claudication
Intermittent claudication implies arterial insufficiency to the tissues. It is most commonly evident when activity occurs because of the increased vascular demand of the tissues. There are two types of intermittent claudication—vascular and neurogenic. The vascular type is most commonly the result of arteriosclerosis, arterial embolism, or thrombo-angiitis obliterans and commonly manifests itself with symptoms in the legs. The neurogenic type is sometimes called pseudoclaudication or cauda equina syndrome and is commonly associated with spinal stenosis and its effect on circulation to the spinal cord and cauda equina.219–224 The symptoms in this case may be manifested in the back or sciatic nerve distribution.
 Bicycle Test of van Gelderen.225
Bicycle Test of van Gelderen.225
The patient is seated on an exercise bicycle and is asked to pedal against resistance. The patient starts pedaling while leaning backward to accentuate the lumbar lordosis (Figure 9-83). If pain into the buttock and posterior thigh occurs, followed by tingling in the affected lower extremity, the first part of the test is positive. The patient is then asked to lean forward while continuing to pedal. If the pain subsides over a short period of time, the second part of the test is positive; if the patient sits upright again, the pain returns. The test determines whether the patient has neurogenic intermittent claudication.
 Stoop Test.
Stoop Test.
The stoop test is performed to assess neurogenic intermittent claudication to determine whether a relation exists among neurogenic symptoms, posture, and walking.226 When the patient with neurogenic intermittent claudication walks briskly, pain ensues in the buttock and lower limb within a distance of 50 m (165 feet). To relieve the pain, the patient flexes forward. These symptoms may also be relieved when the patient is sitting and forward flexing. If flexion does not relieve the symptoms, the test is negative. Extension may also be used to bring the symptoms back.
 Treadmill Test.227,228
Treadmill Test.227,228
This test may also be used to determine if the patient has intermittent claudication. Two trials are conducted—one at 1.2 mph and one at the patient's preferred walking speed. The patient walks upright (no leaning forward or holding hand rails is allowed) on the treadmill for 15 minutes or until the onset of severe symptoms (symptoms that would make patient stop walking in usual life situations). Time to first symptoms, total ambulatory time, and precipitating symptoms are recorded.
Tests for Malingering
 Burns Test.
Burns Test.
The patient is asked to kneel on a chair and then bend forward to touch the floor with the fingers (Figure 9-84). The test is positive for malingering if the patient is unable to perform the test or the patient overbalances.184
 Hoover Test.
Hoover Test.
The patient lies supine. The examiner places one hand under each calcaneus while the patient's legs remain relaxed on the examining table (Figure 9-85).229–231 The patient is then asked to lift one leg off the table, keeping the knees straight, as for active straight leg raising. If the patient does not lift the leg or the examiner does not feel pressure under the opposite heel, the patient is probably not really trying or may be a malingerer. If the lifted limb is weaker, however, pressure under the normal heel increases, because of the increased effort to lift the weak leg. The two sides are compared for differences.
Other Tests
 Sign of the Buttock.
Sign of the Buttock.
The patient lies supine,148 and the examiner performs a passive unilateral straight leg raising test. If there is unilateral restriction, the examiner then flexes the knee to see whether hip flexion increases. If the problem is in the lumbar spine or hamstrings, hip flexion increases when the knee is flexed. This finding indicates a negative sign of the buttock test. If hip flexion does not increase when the knee is flexed, it is a positive sign of the buttock test and indicates pathology in the buttock behind the hip joint, such as a bursitis, tumor, or abscess.232 The patient should also exhibit a noncapsular pattern of the hip.
Reflexes and Cutaneous Distribution
After the special tests, the reflexes should be checked for differences between the two sides (Figure 9-86) if one suspects neurological involvement in the patient's problem.

A, Patellar (L3) in sitting position. B, Patellar (L3) in lying position. C, Medial hamstrings (L5) in supine lying position. D, Lateral hamstrings (S1, S2) in prone lying position. E, Achilles (S1) in sitting position. F, Achilles (S1) in kneeling position. G, Posterior tibial (L4, L5) in prone lying position.
The deep tendon reflexes are tested with a reflex hammer with the patient's muscles and tendons relaxed. The patellar reflex may be performed with the patient sitting or lying, and the hammer strikes the tendon directly. To test the patellar reflex (C3 to C4), the knee is flexed to 30° (supine lying) or 90° (sitting). The Achilles reflex (S1 to S2) may be tested in prone, sitting, or kneeling position. To test the Achilles reflex, the ankle is at 90° or slightly dorsiflexed. The examiner must ensure that the patient's dorsiflexors are relaxed before doing the test; otherwise, the test will not work. This is done by passively dorsiflexing the foot and feeling for the “springing back” of the foot into plantar flexion. If this does not occur, the dorsiflexors are not relaxed. To test the hamstring reflex (semimembrinosus: L5, S1, and biceps femoris: S1 to S2), the examiner places the thumb over the appropriate tendon and taps the thumbnail to elicit the reflex. Again, the knee should be slightly flexed with the hamstrings relaxed to perform the test.
Neurogenic intermittent claudication may cause the reflexes to be absent soon after exercise (Table 9-15).233,234 If neurogenic intermittent claudication is suspected, it is necessary to test the reflexes immediately, because reflexes may return within 1 to 3 minutes after stopping the activity.
TABLE 9-15
Differential Diagnosis of Intermittent Claudication
| Vascular | Neurogenic | |
| Pain | Related to exercise; occurs at various sites simultaneously | Related to exercise; sensations spread from area to area |
| Pulse | Absent after exercise | Present after exercise |
| Protein content of cerebrospinal fluid | Normal | Raised |
| Sensory change | Variable | Follows more specific dermatomes |
| Reflexes | Normal | Decreased but returns quickly |
Another reflex that may be tested is the superficial cremasteric reflex, which occurs in males only (Figure 9-87). The patient lies supine while the examiner strokes the inner side of the upper thigh with a pointed object. The test is negative if the scrotal sac on the tested side pulls up. Absence or reduction of the reflex bilaterally suggests an upper motor neuron lesion. A unilateral absence suggests a lower motor neuron lesion between L1 and L2. Absences have increased significance if they are associated with increased deep tendon reflexes.235
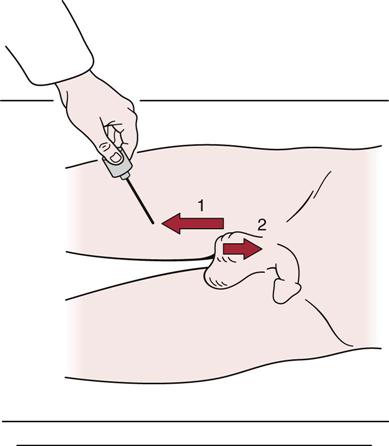
1, The examiner runs a sharp object along the inner thigh. 2, A negative reflex is indicated by the scrotum's rising on that side.
Two other superficial reflexes are the superficial abdominal reflex (Figure 9-88) and the superficial anal reflex. To test the superficial abdominal reflex, the examiner uses a pointed object to stroke each quadrant of the abdomen of the supine patient in a triangular fashion around the umbilicus. Absence of the reflex (reflex movement of the skin) indicates an upper motor neuron lesion; unilateral absence indicates a lower motor neuron lesion from T7 to L2, depending on where the absence is noted, as a result of the segmental innervation. The examiner tests the superficial anal reflex by touching the perianal skin. A normal result is shown by contraction of the anal sphincter muscles (S2 to S4).
Finally, the examiner should perform one or more of the pathological reflex tests (see Table 1-33) used to determine upper motor lesions or pyramidal tract disease, such as the Babinski or Oppenheim tests (see “Special Tests”). The presence of these reflexes indicates the possible presence of disease or upper motor neuron lesion, whereas their absence reflects the normal situation.
If neurological symptoms are found, the examiner must check the dermatome patterns of the nerve roots as well as the peripheral sensory distribution of the peripheral nerves (Table 9-16 and Figure 9-89). Remember that dermatomes vary from person to person, and the accompanying representations are estimations only. The examiner tests for sensation by running relaxed hands over the back, abdomen, and lower limbs (front, sides, and back), being sure to cover all aspects of the leg and foot. If any difference between the sides is noted during this sensation scan, the examiner may then use a pinwheel, pin, cotton ball, or brush to map out the exact area of sensory difference and determine the peripheral nerve or nerve root affected.
TABLE 9-16
| Nerve (Root Derivation) | Sensory Supply | Sensory Loss | Motor Loss | Reflex Change | Lesion |
| Lateral cutaneous nerve of thigh (L2–L3) | Lateral thigh | Lateral thigh; often intermittent | None | None | Lateral inguinal entrapment |
| Posterior cutaneous nerve of thigh (S1–S2) | Posterior thigh | Posterior thigh | None (note: Sciatic nerve often involved, too) | None (note: Sciatic nerve often involved, too) | Local (buttock) trauma Pelvic mass Hip fracture |
| Obturator nerve (L2–L4) | Medial thigh | Often none ± medial thigh | Thigh adduction | None | Pelvic mass |
| Femoral nerve (L2–L4) | Anteromedial thigh and leg | Anteromedial thigh and leg | Knee extension ± hip flexion | Diminished knee jerk | Retroperitoneal or pelvic mass Femoral artery aneurysm (or puncture) Diabetic mononeuritis |
| Saphenous branch of femoral nerve (L2–L4) | Anteromedial knee and medial leg | Medial leg | None (note: Positive Tinel sign 5 to 10 cm above medial femoral epicondyle of knee) | None (note: Positive Tinel sign 5 to 10 cm above medial femoral epicondyle of knee) | Local trauma Entrapment above medial femoral condyle |
| Sciatic nerve (L4–L5, S1) | Anterior and posterior leg Sole and dorsum of foot |
Entire foot | Foot dorsiflexion Foot inversion ± plantar flexion ± knee flexion |
Diminished ankle jerk | Pelvic mass Hip fracture Piriformis entrapment Misplaced buttock injection |
| Common peroneal nerve (division of sciatic nerve) | Anterior leg, dorsum of foot | None or dorsal foot | Foot dorsiflexion, inversion, and eversion (note: Positive Tinel sign at lateral fibular neck) | None (note: Positive Tinel sign at lateral fibular neck) | Entrapment pressure at neck of fibula Rarely, diabetes, vasculitis, leprosy |

From Reilly BM: Practical strategies in outpatient medicine, Philadelphia, 1991, WB Saunders, p. 928.
Pain may be referred from the lumbar spine to the sacroiliac joint and down the leg as far as the foot. Seldom is pain referred up the spine (Figure 9-90). Pain may be referred to the lumbar spine from the abdominal organs, the lower thoracic spine, and the sacroiliac joints. Muscles may also refer pain to the lumbar area (Table 9-17).236
TABLE 9-17
Lumbar Muscles and Referral of Pain
| Muscle | Referral Pattern |
| Ilicostalis lumborum | Below T12 ribs lateral to spine down to buttock |
| Longissimus | Beside spine down to gluteal fold |
| Multifidus | Lateral to spine, sacrum to gluteal cleft, posterior leg, and lower abdomen |
| Abdominals | Below xiphisternum and along anterior rib cage down along inguinal ligament to genitals |
| Serratus posterior inferior | Lateral to spine in T9–T12 posterior rib area |
Data from Travell JG, Simons DG: Myofascial pain and dysfunction: the trigger point manual, Baltimore, 1983, Williams & Wilkins.
Peripheral Nerve Injuries of the Lumbar Spine
Lumbosacral Tunnel Syndrome.
This syndrome involves compression of the L5 nerve root as it passes under the iliolumbar ligament in the iliolumbar canal (Figure 9-91). The usual cause of compression is trauma (inflammation), osteophytes, or a tumor. Symptoms are primarily sensory (L5 dermatome) and pain. There is minimal or no effect on the L5 myotome.237
Joint Play Movements
The joint play movements have special importance in the lumbar spine, because they are used to determine the end feel of joint movement as well as the presence of joint play. They are often used to replace passive movements in the lumbar spine, which are difficult to perform because of the need to move the heavy trunk or lower limbs. As the joint play movements are performed, the examiner should note any decreased ROM, pain, or difference in end feel.238
Flexion, Extension, and Side Flexion
The movements tested during these motions are sometimes called passive intervertebral movements (PIVMs).239 Flexion is accomplished with the patient in the side lying position. The examiner flexes both of the patient's bent knees toward the chest by flexing the hips (Figure 9-92, A). While palpating between the spinous processes of the lumbar vertebrae with one hand (one finger on the spinous process, one finger above, and one finger below the process), the examiner passively flexes and releases the patient's hips; the examiner's body weight is used to cause the movement. The examiner should feel the spinous processes gap or move apart on flexion. If this gapping does not occur between two spinous processes, or if it is excessive in relation to the other gapping movements, the segment is hypomobile or hypermobile, respectively. The results, however, will depend on the skill of the examiner as interrater reliability studies have shown only average reliability.239

 Figure 9-92 Joint play movements of the lumbar spine.
Figure 9-92 Joint play movements of the lumbar spine.A, Flexion. B, Extension. C, Side flexion. D, Posteroanterior central vertebral pressure (PACVP). E, Posteroanterior unilateral vertebral pressure (PAUVP). F, Transverse vertebral pressure (TVP).
Extension (Figure 9-92, B) and side flexion (Figure 9-92, C) are tested in a similar fashion, except that the movement is passive extension or passive side flexion rather than passive flexion. Side flexion is most easily accomplished by grasping the patient's uppermost leg and rotating the leg upward, which causes side flexion in the lumbar spine by tilting the pelvis. Hip pathology must be ruled out before this is performed.
Central, Unilateral, and Transverse Vertebral Pressure
These movements are sometimes called passive accessory intervertebral movements (PAIVMs). To perform the last three joint play movements, the patient lies prone.240 The lumbar spinous processes are palpated beginning at L5 and working up to L1. If the examiner plans to test end feel over several occasions, the same examining table should be used to improve reliability.241 Likewise, the patient should be positioned the same way each time. The greatest movement occurs with the spine in neutral.242 Interrater reliability of these techniques is often low.243
The examiner positions the hands, fingers, and thumbs as shown in Figure 9-92, D, to perform posteroanterior central vertebral pressure (PACVP). Pressure is applied through the thumbs, with the vertebrae being pushed anteriorly (see Figure 8-39). The examiner must apply the pressure slowly and carefully so that the feel of the movement can be recognized. In reality, the movement is minimal. This springing test may be repeated several times to determine the quality of the movement through the range available, and the end feel.
To perform posteroanterior unilateral vertebral pressure (PAUVP), the examiner moves the fingers laterally away from the tip of the spinous process about 2.5 to 4.0 cm (1.0 to 1.5 inches) so that the thumbs rest on the muscles overlying the lamina or the transverse process of the lumbar vertebra (Figure 9-92, E). The same anterior springing pressure is applied as in the central pressure technique. This springing pressure causes a slight rotation of the vertebra in the opposite direction, which can be confirmed by palpating the spinous process while doing the technique. The two sides should be evaluated and compared.
To perform transverse vertebral pressure (TVP), the examiner's fingers are placed along the side of the spinous process of the lumbar spine (Figure 9-92, F). The examiner then applies a transverse springing pressure to the side of the spinous process, which causes the vertebra to rotate in the direction of the pressure, feeling for the quality of movement. Pressure should be applied to both sides of the spinous process to compare the quality of movement through the range available and the end feel.
Palpation
If the examiner, having completed the examination of the lumbar spine, decides that the problem is in another joint, palpation should not be done until that joint is completely examined. However, when palpating the lumbar spine, any tenderness, altered temperature, muscle spasm, or other signs and symptoms that may indicate the source of pathology should be noted. If the problem is suspected to be in the lumbar spine area, palpation should be carried out in a systematic fashion, starting on the anterior aspect and working around to the posterior aspect.
Anterior Aspect
With the patient lying supine, the following structures are palpated anteriorly (Figure 9-93).
Umbilicus.
The umbilicus lies at the level of the L3–L4 disc space and is the point of intersection of the abdominal quadrants. It is also the point at which the aorta divides into the common iliac arteries. With some patients, the examiner may be able to palpate the anterior aspects of the L4, L5, and S1 vertebrae along with the discs and anterior longitudinal ligament with careful deep palpation. The abdomen may also be carefully palpated for symptoms (e.g., pain, muscle spasm) arising from internal organs. For example, the appendix is palpated in the right lower quadrant and the liver in the right upper quadrant; the kidneys are located in the left and right upper quadrants, and the spleen is found in the left upper quadrant.
Inguinal Area.
The inguinal area is located between the ASIS and the symphysis pubis. The examiner should carefully palpate for symptoms of a hernia, abscess, infection (lymph nodes), or other pathological conditions in the area.
Iliac Crest.
The examiner palpates the iliac crest from the ASIS, moving posteriorly and looking for any symptoms (e.g., hip pointer or apophysitis).
Symphysis Pubis.
The examiner uses both thumbs to palpate the symphysis pubis. Standing at the patient's side, the examiner pushes both thumbs down onto the symphysis pubis so that the thumbs rest on the superior aspect of the pubic bones (see Figure 10-15). In this way, one can ensure that the two pubic bones are level. The symphysis pubis and pubic bones may also be carefully palpated for any tenderness (e.g., osteitis pubis).
Posterior Aspect
The patient is then asked to lie prone, and the following structures are palpated posteriorly (Figure 9-94).
Spinous Processes of the Lumbar Spine.
The examiner palpates a point in the midline, which is on a line joining the high point of the two iliac crests. This point is the L4–L5 interspace. After moving down to the first hard mass, the fingers will be resting on the spinous process of L5. Moving toward the head, the interspaces and spinous processes of the remaining lumbar vertebrae can be palpated. In addition to looking for tenderness, muscle spasm, and other signs of pathology, the examiner should watch for signs of a spondylolisthesis, which is most likely to occur at L4–L5 or L5–S1. A visible or palpable dip or protrusion from one spinous process to another may be evident, depending on the type of spondylolisthesis present. In addition, absence of a spinous process may be seen in a spina bifida. If the examiner moves laterally 2 to 3 cm (0.8 to 1.2 inches) from the spinous processes, the fingers will be resting over the lumbar facet joints. These joints should also be palpated for signs of pathology. Because of the depth of these joints, the examiner may have difficulty palpating them. However, pathology in this area results in spasm of the overlying paraspinal muscles, which can be palpated.
Sacrum, Sacral Hiatus, and Coccyx.
If the examiner returns to the spinous process of L5 and moves caudally, the fingers will be resting on the sacrum. Like the lumbar spine, the sacrum has spinous processes, but they are much harder to distinguish because there are no interposing soft-tissue spaces between them. The S2 spinous process is at the level of a line joining the two PSISs (“posterior dimples”). Moving distally, the examiner's fingers may palpate the sacral hiatus, which is the caudal portion of the sacral canal. It has an inverted U shape and lies approximately 5 cm (2 inches) above the tip of the coccyx. The two bony prominences on each side of the hiatus are called the sacral cornua (see Figure 10-67). As the examiner's fingers move farther distally, they eventually rest on the posterior aspect of the coccyx. Proper palpation of the coccyx requires a rectal examination using a surgical rubber glove (Figure 9-95). The index finger is lubricated and inserted into the anus while the patient's sphincter muscles are relaxed. The finger is inserted as far as possible and then rotated so that the pulpy surface rests against the anterior surface of the coccyx. The examiner then places the thumb of the same hand against the posterior aspect of the sacrum. In this way, the coccyx can be moved back and forth. Any major tenderness (e.g., coccyodynia) should be noted.
Iliac Crest, Ischial Tuberosity, and Sciatic Nerve.
Beginning at the PSISs, the examiner moves along the iliac crest, palpating for signs of pathology. Then, moving slightly distally, the examiner palpates the gluteal muscles for spasm, tenderness, or the presence of abnormal nodules. Just under the gluteal folds, the examiner should palpate the ischial tuberosities on both sides for any abnormality. As the examiner moves laterally, the greater trochanter of the femur is palpated. It is often easier to palpate if the hip is flexed to 90°. Midway between the ischial tuberosity and the greater trochanter, the examiner may be able to palpate the path of the sciatic nerve. The nerve itself is not usually palpable. Deep to the gluteal muscles, the piriformis muscle should also be palpated for potential pathology. This muscle is in a line dividing the PSIS of the pelvis and greater trochanter of the femur from the ASIS and ischial tuberosity of the pelvis.
Diagnostic Imaging244–254
It is imperative when using diagnostic imaging, to correlate clinical findings with imaging findings, because many anomalies, congenital abnormalities, and aging changes may be present that are not related to the patient's problems and may be seen in asymptomatic individuals.255,256
Plain Film Radiography
Routine plane lumbosacral x-rays are most appropriate when risk factors of a vertebral fracture are present or if patient has not improved after a course of conservative treatment (about 1 month).256 In adults under 50 years of age with no signs or symptoms of systemic disease, imaging is not required.257 For patients over 50 years of age, plain x-rays and laboratory tests can rule out most systemic diseases.257
Normally, anteroposterior and lateral views are taken.258 In some cases, two lateral views may be taken, one that shows the whole lumbar spine, and one that focuses on the lower two segments. Oblique views are taken if spondylolysis or spondylolisthesis is suspected.123
Anteroposterior View.
With this view (Figure 9-96), the examiner should note the following:
2. Any wedging of the vertebrae, possibly resulting from fracture (Figure 9-99).
3. Disc spaces. Do they appear normal, or are there height decreases, as occurs in spondylosis?
4. Any vertebral deformity, such as a hemivertebra or other anomalies (Figures 9-100 through 9-103).
5. The presence of a bamboo spine, as seen in ankylosing spondylitis.
6. Any evidence of lumbarization of S1, making S1–S2 the first mobile segment rather than L5–S1. Lumbarization occurs in 2% to 8% of the population (Figure 9-104).
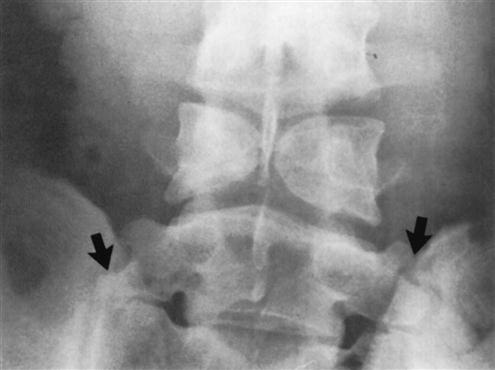
7. Any evidence of sacralization of L5, making the L4–L5 level the first mobile segment rather than L5–S1. This anomaly occurs in 3% to 6% of the population (Figure 9-105).
8. Any evidence of spina bifida occulta, which occurs in 6% to 10% of the population (see Figure 9-102).
Some wedging may also be seen in the vertebra above.
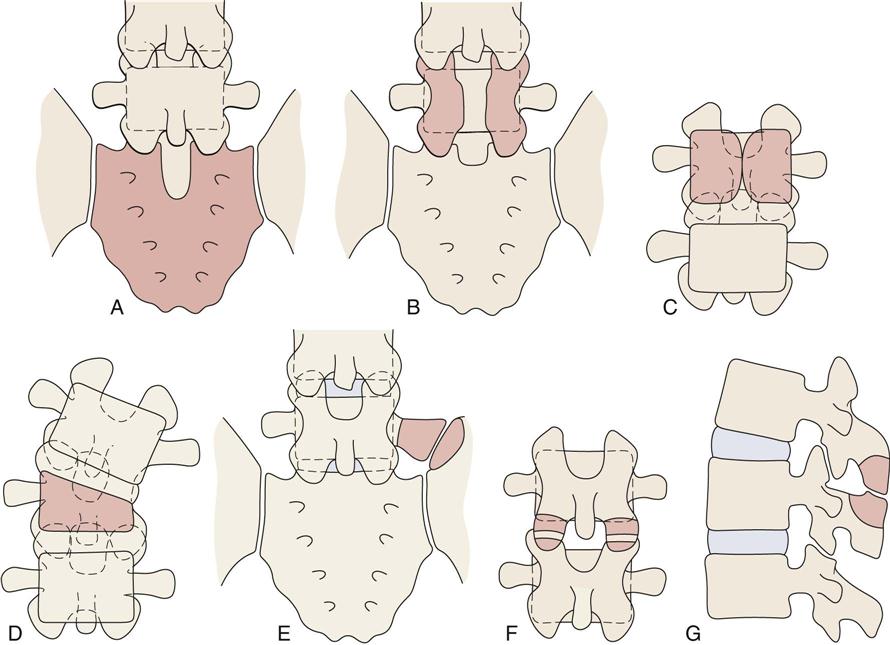
A, Spina bifida occulta, S1. B, Spina bifida, L5. C, Anterior spina bifida (“butterfly vertebra”). D, Hemivertebra. E, Iliotransverse joint (transitional segments). F, Ossicles of Oppenheimer. These are free ossicles seen at the tip of the inferior articular facets and are usually found at the level of L3. G, “Kissing” spinous processes. (Redrawn from MacNab I: Backache, Baltimore, 1977, Williams & Wilkins, pp. 14–15.)
Also note transitional segments (large arrows). (Modified from Jaeger SA: Atlas of radiographic positioning: normal anatomy and developmental variants, Norwalk, CT, 1988, Appleton & Lange, p. 333.)

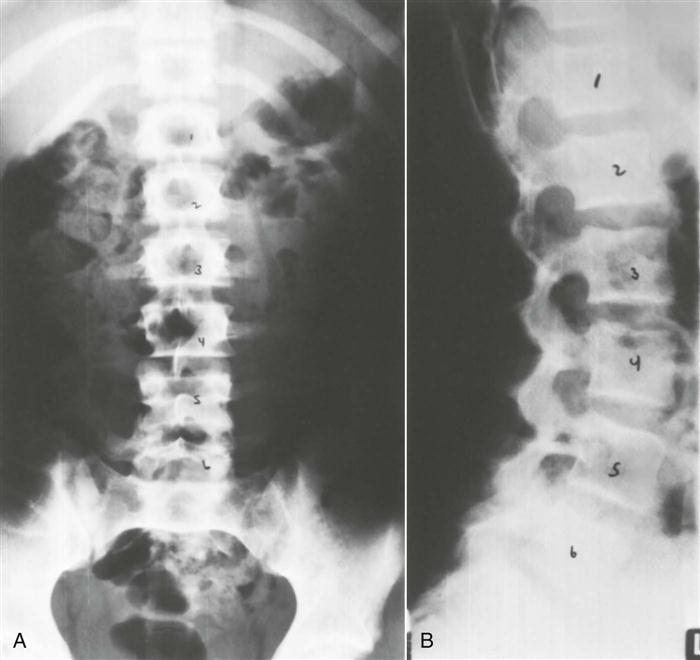
A, Note the massive formation of sacral ala on the left side with a relatively normal transverse process on the right (anteroposterior view). B, Lateral view showing the narrow disc space and the massive arches. (From O'Donoghue DH: Treatment of injuries to athletes, ed 4, Philadelphia, 1984, WB Saunders, p. 403.)
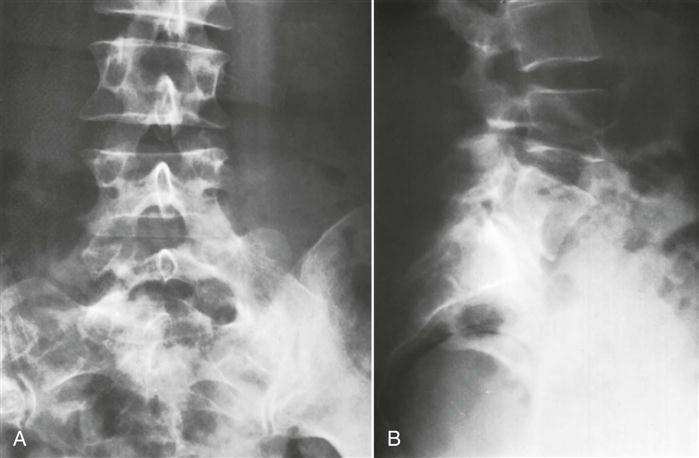
Lateral View.
With this view (Figure 9-106), the examiner should note the following:
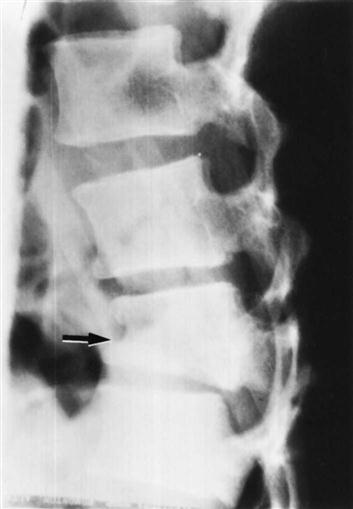
1. Any evidence of spondylosis or spondylolisthesis, which occurs in 2% to 4% of the population (Figure 9-107). The degree of slipping can be graded as shown in Figure 9-108.259 New grading or classification system involving lateral sacropelvic and spinopelvic balance have also been suggested.260
2. A normal lordosis. Do the intervertebral foramina appear normal?
3. Any wedging of the vertebrae.
5. Alignment of the vertebrae should be noted. Disruption of the curve may indicate spinal instability.
6. Any osteophyte formation or traction spurs (Figure 9-109).251,261 Traction spurs indicate an unstable lumbar intervertebral segment. A traction spur occurs approximately 1 mm from the disc border; an osteophyte occurs at the disc border with the vertebral body.

A, Film tracing. B, Radiograph. (From Finneson BE: Low back pain, Philadelphia, 1973, JB Lippincott, pp. 54–55.)
A, Grade 1: Arch defect in L5 with mild forward displacement of L5 on S1; backache but no gross disability. B, Grade 2: More forward slipping between L4 and L5 with collapse of the intervertebral disc; definite symptomatic back with restriction of motion, muscle spasm, and curtailment of activities. C, Grade 3: More extensive slipping combined with a wide separation at the arch defect and degenerative changes of the disc; grossly symptomatic. D, Grade 4: Vertebrae slipped forward more than halfway; severe disability. (From O'Donoghue DH: Treatment of injuries to athletes, ed 4, Philadelphia, 1984, WB Saunders, p. 402.)
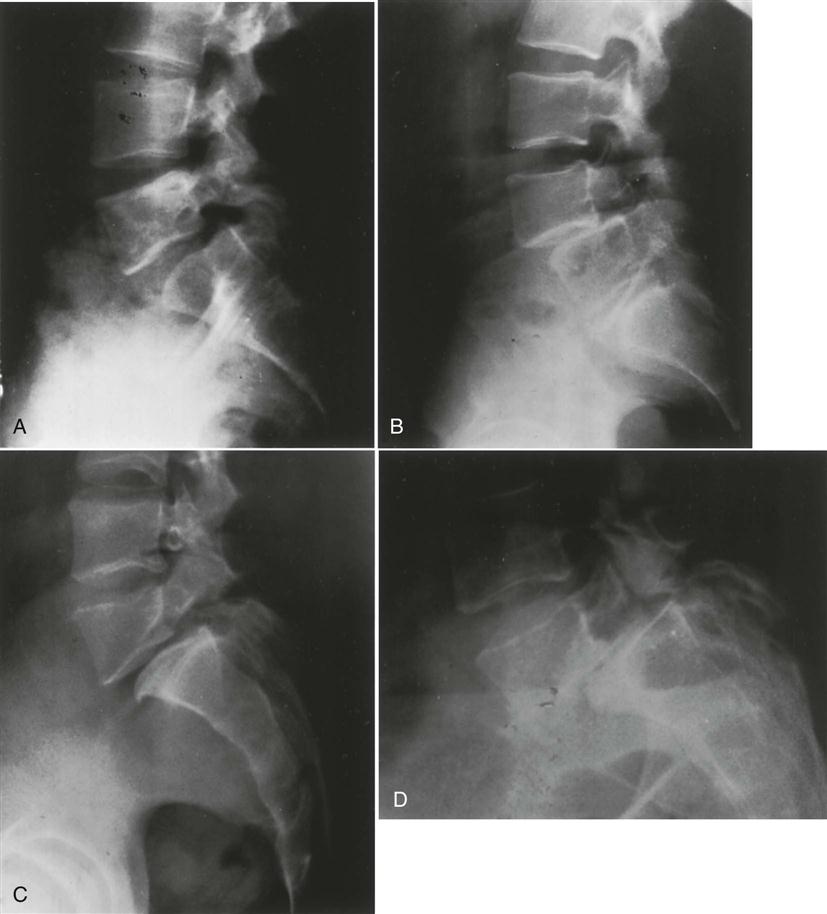
Oblique View.
With the oblique view (Figure 9-110), the examiner should look for any evidence of spondylolisthesis (sometimes referred to as a “Scottie dog decapitated”) or spondylolysis (sometimes referred to as a “Scottie dog with a collar;” Figure 9-111).
Motion Views.
In some cases, motion views may be used to demonstrate abnormal spinal motion or structural abnormalities. These are usually lateral views showing flexion and extension to demonstrate instability or spondylolisthesis (Figure 9-112), but they may also include anteroposterior views with side bending.166,262,263
Myelography
A myelogram, although seldom used today because of its complications and replacement by computed tomography (CT) scans and magnetic resonance imaging (MRI), can confirm the presence of a protruding intervertebral disc, osteophytes, a tumor, or spinal stenosis (Figures 9-113 through 9-115). The examiner must be careful of the side effects of myelograms, which include headache, stiffness, low back pain, cramps, and paresthesia in the lower limbs. Although side effects do occur, no permanent injuries have been noted.
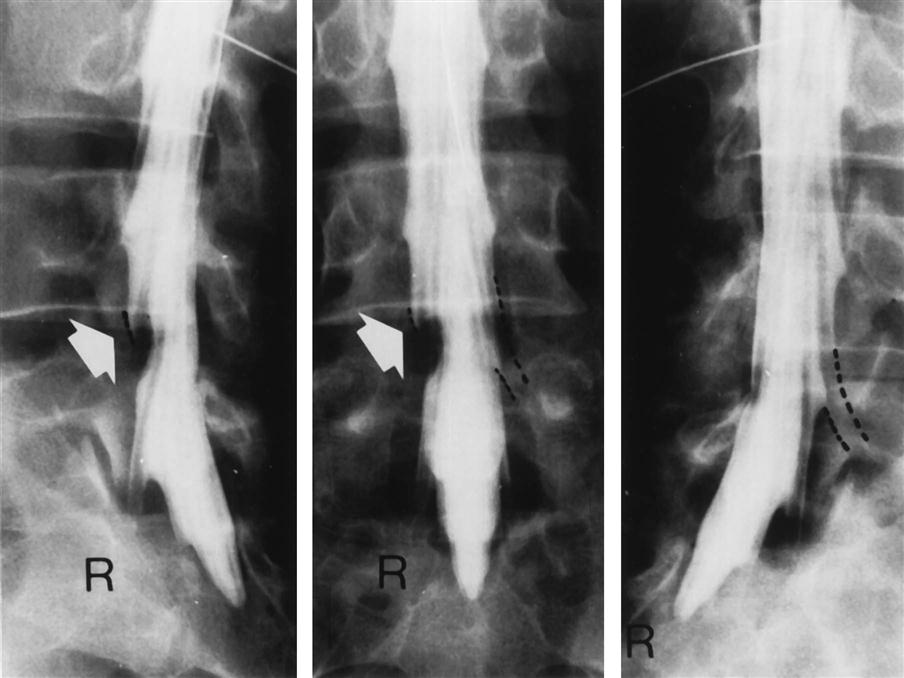
Note lack of filling of the nerve root sleeve and indentation (arrow) of the dural sac. (From Rothman RH, Simeone FA: The spine, Philadelphia, 1982, WB Saunders, p. 550.)


Radionuclide Imaging (Bone Scans)
Bone scans are useful for detecting active bone disease processes and areas of high bone turnover. In children, the epiphyseal and metaphyseal areas of the long bones show increased uptake. In adults, only the metaphyseal area is so affected. Traumatic bone injuries, tumors, metabolic abnormalities (e.g., Paget disease), infection, and arthritis may be detected on bone scan.124
Computed Tomography
A CT scan may be used to delineate a fracture or to show the presence of spinal stenosis caused by protrusion or a tumor, or if a bony abnormality is suspected256 (Figures 9-116 through 9-119). As with plain x-rays, results must be correlated with clinical findings, because the anatomical changes seen are often unassociated with the patient's symptoms.255,264,265 This technique provides an axial projection of the spine, showing the anatomy of not only the spine but also the paravertebral muscles, vascular structures, and organs of the body cavity. In doing so, it shows more precisely the relation among the intervertebral discs, spinal canal, facet joints, and intervertebral foramina. It may be used to evaluate spinal stenosis, the shape of the spinal canal, epidural scarring (after surgery), facet joint arthritis, tumors, and trauma.124,266,267 It may be used in conjunction with a water-soluble contrast medium (computer-assisted myelography) to further delineate the structures.
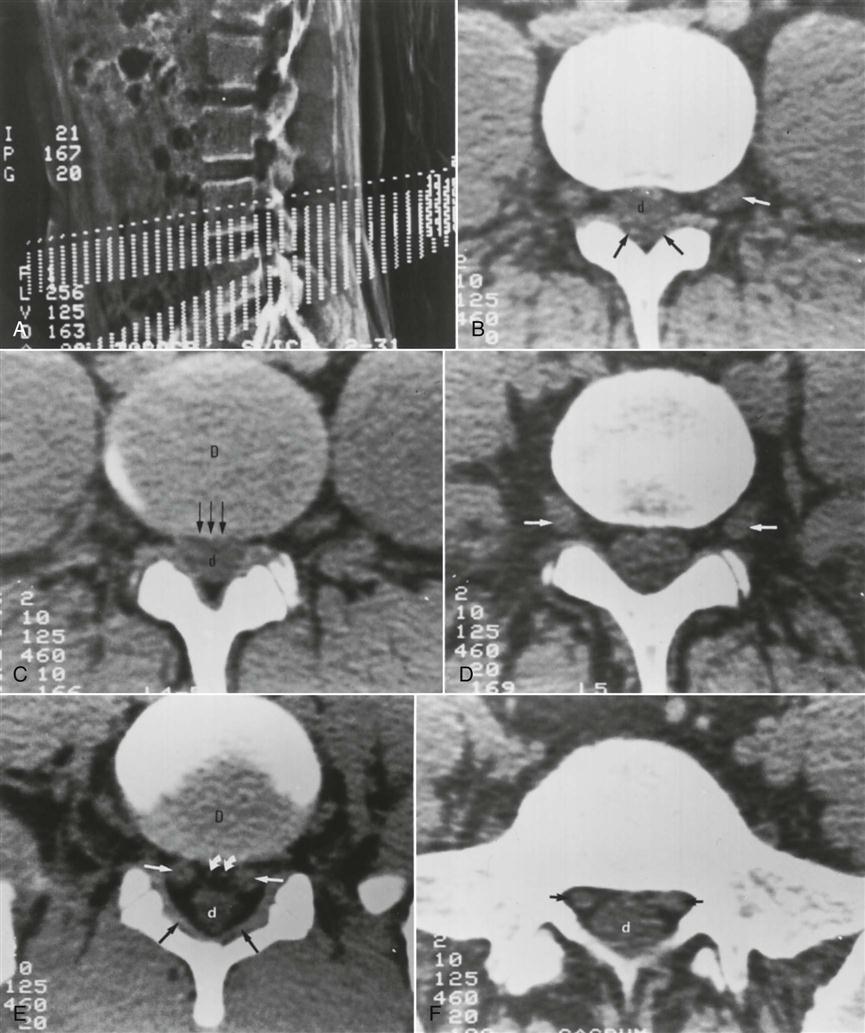
A, Scout view. The chosen sections (dashed lines) can be planned and angled along the planes of the discs. B, CT scan through the L4 vertebral body shows the neural foramina and the L4 nerve root ganglia (white arrow indicates left ganglion). The dural sac (d) and ligamenta flava (black arrows) are shown. C, CT scan through the L4–L5 disc (labeled D) shows very little fat between the posterior margin of the disc (arrows) and the dural sac (d). The nerve roots are not clearly shown. D, CT scan through the L5 vertebral body and foramina shows the L5 nerve root ganglia (arrows). E, CT scan through the L5–S1 disc space (labeled D) shows the L5 nerve roots (straight white arrows), the dural sac (d), and the ligamenta flava (black arrows). Small epidural veins are noted (curved arrows). F, At the S1 level, the S1 nerve roots (arrows) and dural sac (d) are clearly visualized. (From Weissman BNW, Sledge CB: Orthopedic radiology, Philadelphia, 1986, WB Saunders, p. 306.)

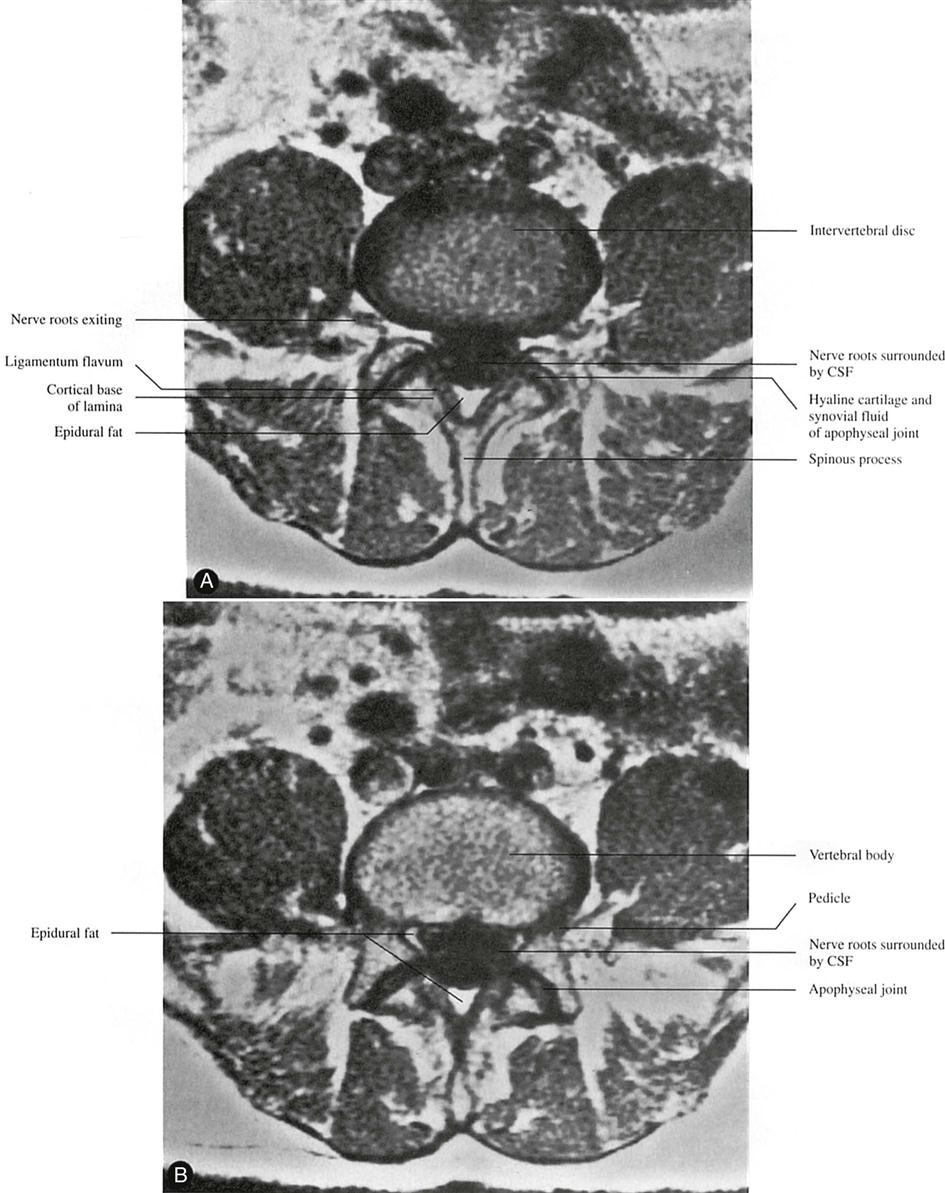
A, Lateral digital scout view obtained through the lumbosacral spine. The upper and lower scan limits through the L4–L5 region are designated with an electronic cursor. Scan collimation is 5 mm thick; incrementation is 3 mm (2-mm overlap). B, Axial CT section of L4. The L4 root ganglia and spinal nerves are seen within the intervertebral foramina (white arrowheads) surrounded by abundant epidural fat (e). The thecal sac (t) is bounded anterolaterally by fat in the lateral recess. The posterior arch of L4 consists of inferior facets (if), laminae (l), and spinous process (s). The superior facet of L5 (sf) is just visible. C, The next lower axial section demonstrates the L4–L5 facet articulations. The ligamentum flavum (lf) is contiguous with the facet joint capsule. Again, the thecal sac (t) is readily apparent; it is slightly higher in density than the adjacent epidural fat. Note that without subarachnoid contrast media, the intrathecal contents cannot be discerned. D, Axial CT section of the L4–L5 disc space. The disc (multiple black arrowheads) is a region of central hypodensity surrounded by the cortical margin of L4. The posterior arch of L4 projects below the disc level. The intervertebral foramina (ivf) have begun to close. The cartilaginous articular surfaces (white arrowhead) between superior (sf) and inferior (if) facets are poorly demonstrated with these window settings. The ligamentum flavum (double black arrowheads) is noted medial to the facet joints. s, Spinous process; t, thecal sac. E, The next inferior CT section demonstrates the disc (multiple arrowheads) positioned somewhat more anteriorly, marginated posteriorly at this level by the posterosuperior cortical rim of the L5 body. The ligamentum flavum (double arrowheads) normally maintains a flat medial surface adjacent to the thecal sac (t). The posterior arch of L4 and its spinous process (s) are still in view. F, Axial CT section through the L5 body at the level of the pedicles (p). The canal now completely encloses the thecal sac (t). G, Immediately below, only the spinous process (s) of the posterior arch of L4 is visible. The transverse process (tp) of L5 is noted. t, Thecal sac. H, At the level of the iliac crest (IC), the posterior arch of L5 (small arrowheads) has just begun to form. The transverse processes (tp) are quite large at this level. t, Thecal sac. (From LeMasters DL, Dowart RL: High-resolution, cross-sectional computed tomography of the normal spine. Orthop Clin North Am 16:359, 1985.)

A, Lateral view during metrizamide myelography showing indentations on the anterior aspect of the contrast column (arrows) at L3–L4 and L4–L5 resulting from bulging intervertebral discs. The levels for subsequent CT sections B and D are marked. B, CT section through the L4 vertebra and L4–L5 foramina 1 hour after a metrizamide myelogram. Contrast agent fills the left axillary pouch (white arrow) and the right nerve root sleeve. Small arrows indicate the filling defects produced by the remaining nerve roots. C, CT section slightly more distal than B shows the L4 nerve root ganglia (left ganglion is indicated by arrow). D, Section through the L4–L5 disc and the posterior inferior body of L4 shows an abnormally bulging disc without compression of the subarachnoid space. The ligamentum flavum on the left (arrow), the superior facet of L5 (sf-5), and the inferior facet of L4 (if-4) are indicated. (From Weissman BNW, Sledge CB: Orthopedic radiology, Philadelphia, 1986, WB Saunders, p. 284.)

Sagittal reformatted image derived from transverse CT scans of the lumbar spine shows degeneration at the L4–L5 level with a vacuum phenomenon. A grade II spondylolisthesis at the L4–L5 level results from osteoarthritis of the facet joints. (From Resnick D, Kransdorf MJ: Bone and joint imaging, Philadelphia, 2005, WB Saunders, p. 146.)
Magnetic Resonance Imaging
MRI is a noninvasive technique that can be used in several planes (transaxial, coronal, or sagittal) to delineate bony and soft tissues. This technique is commonly used to diagnose tumors, to view the spinal cord within the spinal canal, and to assess for syringomyelia, cord infarction, or traumatic injury.124,268 The delineation of soft tissues is much greater with MRI than with CT.269 For example, with MRI, the nucleus pulposus and the annulus fibrosis are easier to differentiate because of their different water contents, making it the preferred imaging modality for disc disease and radiculopathy (Figures 9-120 through 9-124).23,256,270,271 As with other diagnostic imaging techniques, clinical findings must support what is seen before the structural abnormalities can be considered the source of the problem.255,264,272–274 Up to 30% of asymptomatic patients with no history of low back pain show disc abnormalities.23,275 Things to look for on MRI are disc height, presence or absence of annular tears, degenerative signs, and end plate changes.23
A, Level of neural canal. B, Level of pedicle. CSF, Cerebrospinal fluid. (From Bassett LW, Gold RH, Seeger LL: MRI atlas of the musculoskeletal system, London, 1989, Martin Dunitz, p. 40.)


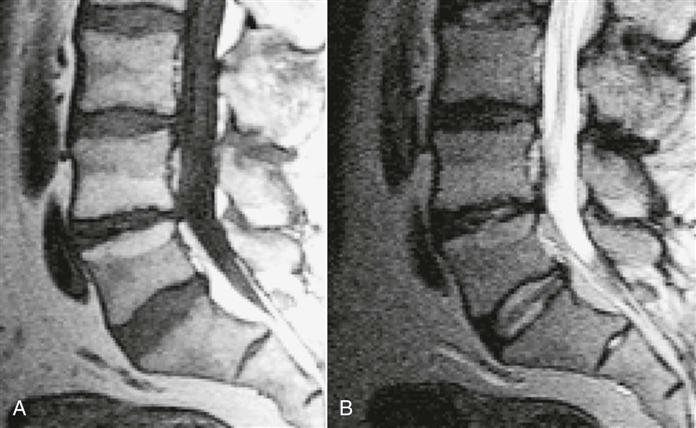
Sagittal T1-weighted (A) and T2-weighted (B) spin echo magnetic resonance (MR) images of the lumbar spine show signal intensity changes at the L4–L5 level that are typical of a type II end plate. The signal intensity of subchondral bone at this level is identical to that of fat. There is also evidence of degeneration of the intervertebral disc at this level, with a decrease in disc space height and loss of disc signal on the T2-weighted image. (From Resnick D, Kransdorf MJ: Bone and joint imaging, Philadelphia, 2005, WB Saunders, p. 144.)

Discography276
For discography, radiopaque dye is injected into the nucleus pulposus. It is not a commonly used technique but may be used to see whether injection of dye reproduces the patient's symptoms, making it diagnostic (Figure 9-125).
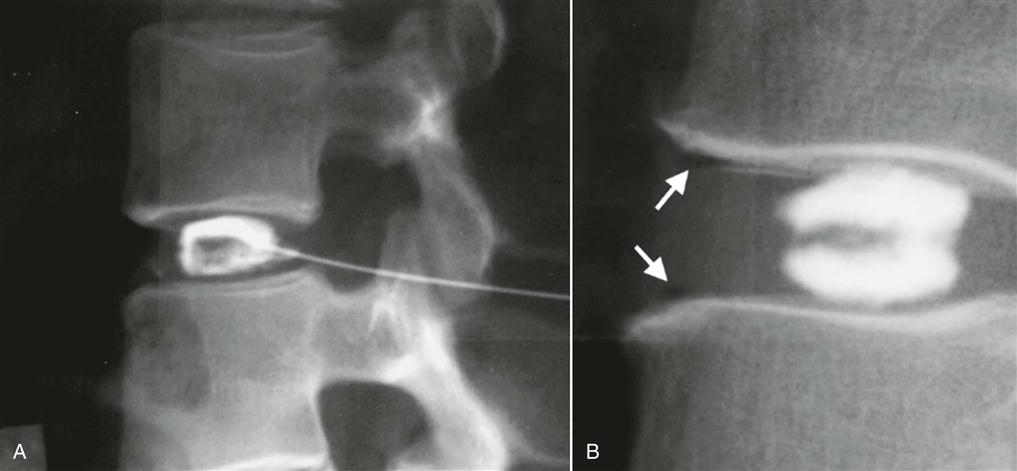
A, Lateral lumbar spine with discographic needle entry low in the posterior disc margin. Note the normal unilocular appearance of the nucleogram. B, Normal bilocular appearance of the nucleogram. The anterior arrows identify anterior vacuum phenomena in the anulus fibrosus, consistent with peripheral annular tears that were asymptomatic at discography. (From Resnick D, Kransdorf MJ: Bone and joint imaging, Philadelphia, 2005, WB Saunders, p. 164.)