Blood Pressure Monitoring
Overview
The frequent measurement of blood pressure during anesthetic administration is a standard practice throughout the world. Because of significant intraoperative blood pressure variance—combined with the presumed value of accurate, frequent, repeatable determinations in predicting certain intraoperative and postoperative problems—the trend in recent years in developed countries has been almost completely toward the use of automatic, digital, electromechanical instrumentation. Many of these devices function quite well and require minimal effort and limited special training. This chapter discusses the most common instrumentation and methods for measuring blood pressure currently in clinical use. This includes principles of operation, perceived advantages and disadvantages, relative accuracy, and factors that may affect operation. It is assumed that the reader is aware of recommended and normal limits for blood pressure and the medical implications of abnormal values.
History of Blood Pressure Measurement
Nearly every practicing physician is familiar with the originally reported measurement of blood pressure obtained by the Reverend Stephen Hales, who cannulated the femoral artery of a horse and measured the average height of the blood column at approximately 9 feet, corresponding to 200 millimeters of mercury (mm Hg) or 27 kilopascals (kPa). Hales also described respiratory variation and pulsatile pressure, a remarkable achievement in the eighteenth century. Further work was limited until the late nineteenth century, when numerous investigators described noninvasive blood pressure determinations. The auscultatory method of Korotkoff (1905) has been the most common method for blood pressure determination for the past 100 years. However, the oscillometric technique originally described by Roy and Adami in 1890 rapidly gained popularity in the late twentieth century and is the theoretical basis for most automated, noninvasive, blood pressure–measuring equipment manufactured today.
Definitions of Blood Pressure
Accompanying the development of various methods of blood pressure determination was controversy over the actual definition of systolic, diastolic, and mean blood pressures. For invasive methods that produce a pulsatile waveform, the definitions are simple: systolic pressure is the maximum instantaneous pressure, diastolic pressure is the minimum instantaneous pressure, and mean pressure is the area under the waveform-time curve divided by the time interval for one or more beats, a quantity easily determined with simple software.
Blood pressure determinations are highly dependent on the anatomic site being measured.1 Usually there is an increase in systolic values and a decrease in diastolic values as blood pressure is measured more peripherally in the vascular tree of healthy subjects. Because of the opposite changes of the systolic and diastolic values, mean blood pressure normally remains relatively constant as the measurement site changes. In patients with vascular disease and resultant restricted arterial flow, further errors are introduced that usually produce decreases in systolic, diastolic, and mean flow at more distal locations. Despite these well-known predictable errors, the radial arterial pressure—determined by a small cannula inserted near the wrist, combined with an electronic transducer and digital display system—has become the de facto clinical standard of comparison for human blood pressure determinations. Nearly all published methodology comparisons and so-called accuracy studies use the radial arterial pressure as the reference standard. This is done despite the fact that the choice of the radial artery is more one of safety and convenience than of scientific validity. Much less affected by arterial system variables is the central aortic root pressure, probably a much more reliable standard, although measurement of aortic root pressure in humans generally involves unacceptable risk.
Instrumentation and Units of Measure
Several different types and models of automated noninvasive blood pressure instrumentation have become available in the United States in recent years, and their use has become ubiquitous in anesthesia over much of the world. Each approach measures different physical quantities, from which values for systolic, diastolic, and mean blood pressure are derived. Noninvasive blood pressure readings never correlate exactly with measured invasive radial arterial blood pressure, irrespective of construction and calibration precision. It is always hoped, however, that the accuracy of any method is such that differences between readings are of little clinical significance. In general, this is true for most commercial oscillometric instruments, although other noninvasive methods do not consistently perform as well in all situations. Reliability of modern automated noninvasive oscillometric equipment has reached the point where it is unnecessary to validate the automated unit with an older method, such as auscultation, because the manual approach is less reliable and more subjective than the automated method and most often represents a step down in accuracy.
The standard unit of measure for blood pressure in the United States is millimeters of mercury (mm Hg), or torr, in which 760 mm Hg equals 1 standard atmosphere of pressure at sea level. Elsewhere in the world, the kilopascal (kPa) often is the standard unit of pressure measurement (1 kPa = 7.5 mm Hg). Most commercial digital blood pressure instrumentation provides a readout to within 1 mm Hg, although this implied significance considerably exceeds the actual precision and repeatability of even the best invasive units and certainly does not provide meaningful additional clinical information. The actual precision of the best noninvasive devices is approximately 5 to 10 mm Hg. Calibration accuracy of noninvasive blood pressure devices is most often measured and adjusted by the manufacturer through comparison with radial arterial blood pressure in healthy human subjects. This method obviously involves limitations, not the least of which is using average values without adjustment for anatomic differences, such as body habitus.
As mentioned, radial arterial pressure correlates well with central aortic pressure in healthy subjects,1 but the two values may disagree by a considerable amount, especially in hypertensive and hyperdynamic patients and in patients with peripheral vasoconstriction or vascular disease.2 In addition, every noninvasive method measures blood pressure indirectly, by inference from measured physical quantities,3 such as cuff air-pressure oscillations; the correlation with invasive pressure is never perfect, even under the best of circumstances. This should be kept in mind when interpreting noninvasive blood pressure readings.
Reference Points
If the aortic root is taken as the desired reference point for blood pressure, all measurement techniques must take into account the effect of gravity and the water column hydrostatic pressure that results from a difference of height between the aortic root and the location of the transducer. This amounts to a difference of approximately 7.5 mm Hg for every 10-cm difference in vertical height from the aortic root. The effect is small for a brachial cuff, but it can be large (>50 mm Hg) if, for example, the pressure transducer is accidentally positioned improperly, or if an ankle cuff is used on an individual in a sitting position. Under these circumstances, an accurate pressure can still be obtained, but the operator must add or subtract a fixed amount to the measured blood pressure. This applies to both noninvasive and invasive instruments. Some novel and practical methods have been suggested to accomplish this compensation in everyday clinical situations,4 but the general rule that 10 cm equals 7.5 mm Hg or 1 kPa always works.
Manual (Riva-Rocci) Measurement Technique
The measurement of blood pressure with an air-inflatable cuff placed on the proximal arm, listening with a stethoscope over the brachial artery for Korotkoff sounds as cuff pressure is slowly decreased, remains the most common and inexpensive method of blood pressure determination. This method was originally described by Scipione Riva-Rocci in the mid-nineteenth century. Five distinct sound phases are heard as pressure decreases from above systolic to below diastolic: in phase I, clear tapping sounds are heard; in phase II, sounds become softer and longer; in phase III, they become crisper and louder; in phase IV, sounds become muffled and softer; and in phase V, sounds completely disappear.5 Systolic blood pressure is measured as the onset of phase I, and diastolic is measured at the onset of phase V. Mean blood pressure (BP) is not specifically measured, but it often is approximated as follows:
where DP is diastolic pressure and SP is systolic pressure. The advantages of the Riva-Rocci (auscultatory) technique are numerous and include low cost, simplicity, lack of dependence on electricity, and ruggedness. This method suffers from imperfect correlation with invasive measurement of blood pressure because of numerous factors, such as ambient noise, auditory acuity of the clinician, atherosclerotic vascular changes, obesity, and cuff size in relation to the limb.6 In healthy patients, however, the clinical accuracy is high. Riva-Rocci blood pressure is generally biased low (10 to 30 mm Hg) for systolic blood pressure and high (5 to 25 mm Hg) for diastolic pressure, especially in hypertensive patients.7 The precision (scatter) is approximately ±20 mm Hg compared with invasive radial arterial pressure.8 The errors are exacerbated by obesity, edema, and vascular disease. In critically ill hypotensive patients, it is often impossible to obtain a reliable auscultatory blood pressure without resorting to Doppler flow-sensing devices to detect the arterial blood flow. With the increased use of pulse oximetry, systolic pressure can be reliably measured with a much improved sensitivity over manual palpation or Korotkoff sounds by noting the point of occlusion of pulsatile flow in the finger through the observation of the corresponding pulse waveform on the oximeter display.9 Despite a lack of accuracy and subjectivity compared with automated and invasive methods, manual auscultatory measurement of blood pressure is commonly used for healthy, nonsurgical patients because of the low cost and the unimportance of small errors in the healthy population.
Multiple techniques exist for the physical measurement of cuff pressure throughout deflation. Mercury sphygmomanometers are the more traditional approach, but aneroid and hybrid devices have been consistently increasing in popularity. Actual mercury manometers have mostly disappeared from developed countries because of environmental concerns with liquid mercury. Hybrid devices generally use an electronic pressure gauge that is digitally displayed, replacing the mercury column and circular scale of Bourdon tube mechanical gauges. Hybrid devices usually have the option for the displayed pressure to stop decreasing when significant systolic, diastolic, and mean pressure levels are reached. All pressure techniques are comparable when used properly, although more modern devices are easier to use.
During the 1970s, several automated devices were introduced, such as the Roche Arteriosonde (Roche Diagnostics, Indianapolis, IN), which used the Riva-Rocci technique to measure blood pressure automatically and noninvasively. These devices incorporated either a small microphone or a Doppler transducer built into the cuff, which was placed over the brachial artery, and the cuff was inflated automatically by an air pump. These devices proved to be more technically complicated than oscillometric devices introduced later; they have gradually disappeared from clinical use and are no longer manufactured.
Oscillometric Blood Pressure Devices
It is common to observe pulsatile pressure variation in the air pressure gauge during manual measurement of blood pressure using auscultation. Oscillometric cuff blood pressure measurement methods take advantage of this pulsatile variation to allow the extrapolation of arterial blood pressure. The simplest manual technique is to deflate the cuff slowly from a pressure above the expected systolic value. At a pressure roughly corresponding to systolic arterial pressure, the needle of the pressure gauge begins to oscillate slightly (1 to 5 mm Hg) with each cardiac contraction (Fig. 12-1). This value is assumed to be the systolic pressure, and for many years this was the standard method of measuring blood pressure in children, in whom Korotkoff sounds are difficult to hear. An enhancement of this technique was the oscillotonometer, an obsolete mechanical device equipped with two cuffs and a sensitive gauge designed to greatly amplify the observed oscillations and thus increase the sensitivity. The mean pressure is usually assumed to be the cuff pressure that produces the maximum amplitude of oscillations. The diastolic pressure is difficult to measure directly by oscillometric methods, because the oscillations decrease gradually as cuff pressure decreases below the actual diastolic arterial value. The mechanical oscillotonometer lost popularity with the development of automated devices.
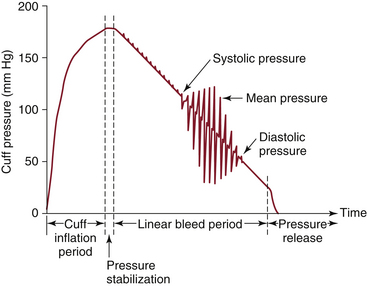
FIGURE 12-1 Observed oscillations in cuff pressure during deflation. The amplitude of oscillations is greatly exaggerated.
Many different electronic oscillometric devices have been developed and commercially introduced and have subsequently become very widely used. Although the specific algorithms used to determine systolic, diastolic, and mean blood pressure values are often proprietary with the manufacturer, it is likely that all of the devices function in a manner similar to the manual oscillometric techniques described above. Cuff pressure is first increased above the expected systolic blood pressure value and then is slowly and gradually decreased, while the pressure oscillations in the cuff are measured electronically. Computation of the diastolic blood pressure is inferred mathematically from the mean value (peak of oscillation strength), the systolic value, and from the characteristics of the “tail” as oscillations decrease at low pressures. Models manufactured since the mid-1980s use high-performance microprocessors and perform remarkably well.10 They generally incorporate automatic repeated measurement at predetermined time intervals, automatic recording, serial data outputs, and sophisticated alarms.
Automatic oscillometric blood pressure devices offer multiple advantages over manual devices. They eliminate clinician subjectivity and, for a noninvasive monitor, introduce an unprecedented degree of repeatability in regard to subsequent readings. In addition to improved quality and accuracy, automatic devices have been shown to decrease the incidence of “white coat hypertension,” the increase in patient blood pressure as a result of being in a medical setting.11 Larger differences between automatic and auscultatory approaches have been shown to occur more frequently when recorded inconsistencies are apparent in the pressure waveforms.12 The automated algorithms are presumably optimized to correlate well with invasive blood pressure readings in the average healthy subject. Values have been shown to be algorithm dependent, which indicates a need for a standardized approach.13 Even so, the precision and bias of well-designed units are generally less than 10 mm Hg.10
The oscillometric cuff is the same as the one used for manual auscultatory methods, and problems related to this method remain. In particular, atherosclerosis, edema, obesity, and chronic hypertension introduce errors in systolic (measures too low) and diastolic (measures too high) oscillometric blood pressures when the cuff is used compared with invasive arterial pressure measurements.14 Using the improper cuff size also introduces significant errors6: cuffs that are larger than needed produce erroneously low oscillometric readings, and cuffs that are too small produce higher readings. The proper cuff width has been found to be approximately 46% of arm circumference.15 Intermittent automated blood pressure monitoring also interferes with ipsilateral intravenous (IV) access and pulse oximetry.
Assuming a properly sized cuff, oscillometric units usually function adequately for obese patients and for children, for whom auscultatory methods fail. Oscillometric cuffs also work well on the calf, ankle, or thigh, a fact often overlooked by the clinician. Finally, the accuracy of an infant cuff used on the adult thumb seems to also be acceptable when brachial or lower extremity cuffs are precluded.16
Invasive Blood Pressure Monitoring
Invasive blood pressure monitoring often is the clinical method of choice if large hemodynamic changes are expected or encountered, frequent blood sampling is anticipated, or there is a need for continuous, accurate, beat-to-beat blood pressure determination.17 The majority of continuous electrocardiograph monitoring units sold in the United States also have the capability to simultaneously measure invasive and noninvasive blood pressure. Besides the obvious advantage of allowing arterial blood sampling, the invasive method provides unsurpassed reliability and accuracy, especially when extremes of blood pressure are expected.
The usual method of invasive blood pressure monitoring consists of the percutaneous insertion of a small-bore (18- to 22-gauge) plastic catheter into a peripheral artery. The catheter is physically connected via high-pressure plastic tubing to an electronic pressure transducer and display unit. The transducer is a sterile, miniature, self-contained assembly that contains the electromechanical components within a clear plastic case. Most transducers incorporate an integral mechanism for providing a continuous, slow flush of sterile solution through the tubing and catheter to prevent clotting. In addition, a mechanism for rapid manual flushing is provided. The entire assembly is designed for single-patient use at a cost of approximately $15 per patient. The use of solid-state, individually calibrated instruments has greatly improved the accuracy over older, partially disposable systems.18 In general, an absolute accuracy of 5 mm Hg or better throughout the measurement range can be expected. Identical redundant transducer systems typically are used if central venous or pulmonary arterial pressures are simultaneously monitored.
Invasive arterial blood pressure monitoring is not without risk. Potential problems include symptomatic or asymptomatic arterial thrombosis, infection, accidental injection of IV drugs, nerve damage from trauma or hematoma during placement, and exsanguination from accidental disconnection. All these problems have been reported to occur infrequently. Slogoff and colleagues19 studied arterial cannulation in a large series of surgical patients and concluded that the risks of radial artery cannulation often are exaggerated and that serious morbidity in adults is rare. They also found no evidence to support the long-held beliefs that the shape, size, and material of the catheter and duration of insertion are important predictors of complications. In addition, their study found no objective evidence that noninvasive determination of collateral flow before the catheter is inserted, such as the Allen test, was of any value in predicting morbidity. Furthermore, no evidence suggested that one cannulation site—radial, ulnar, brachial, axillary, femoral, or dorsalis pedis—was safer than another, except perhaps from an infectious disease viewpoint. It is uncertain whether these conclusions can be extended to children and neonates, although the available evidence indicates that arterial cannulation in this population is a reasonably safe procedure.20
Arterial cannulation often is painful, and liberal local anesthesia combined with anxiolytic medication is highly recommended for insertion. Although many different insertion techniques have been described—including the guidewire Seldinger technique, transfixion, or direct insertion—most of these methods are successful in trained hands, and there is little reason to suggest that any technique is consistently safer or better than another. Severe hypotension, vascular disease, or previous cannulation can make insertion difficult or impossible. In these cases, direct exposure of the artery via a surgical cutdown may be the only method to cannulate the artery successfully, although infectious complications are much more common with a surgical incision.21 Also, the use of ultrasound guidance may be useful in these difficult situations.
To minimize possible complications, common sense dictates that arterial catheters should be removed as soon as they are no longer needed.21 Continuous flushing with heparinized saline at a rate of 5 to 10 mL/h to prevent clotting used to be standard practice. However, because of concerns about heparin-induced thrombocytopenia (HIT, as well as lack of evidence that heparin-containing solutions are superior to plain saline flushing, heparin has been removed from the flush solution. The capability to flush the system automatically has been incorporated into virtually all modern disposable transducer sets. In the intensive care unit (ICU), arterial catheters tend to stop functioning after 1 to 2 weeks because of a combination of arterial inflammation, occlusion, and clot formation. This necessitates removal of the catheter and a change to an alternate site.
Ideally, an invasive blood pressure transducer should be small, reliable, incorporated into the catheter itself, free from nonlinearity and distortion, and inexpensive. Devices approaching this complete ideal are still experimental, but current disposable transducers provide a technology with generally acceptable consistent performance in a reasonably sized package (Fig. 12-2). Many factors influence the accuracy of modern invasive arterial monitoring equipment, not the least of which is the ambiguity and disagreement over the exact quantitative definition of blood pressure.3 Aortic root pressure is the accepted physiologic standard, but safety considerations preclude routine measurement outside the laboratory. Radial arterial pressure reflects aortic pressure well in healthy, young individuals, but this is seldom the condition of patients who require invasive monitoring. As previously mentioned, as the location of the catheter becomes more peripheral, measured systolic pressure tends to increase and diastolic pressure tends to decrease as a result of resonance effects in the arterial tree. Because of the opposing changes of systolic and diastolic blood pressure readings, mean pressure decreases only slightly. Vascular disease and vasoconstriction predictably decrease both systolic and diastolic measurements in proportion to the severity of the condition, and it is fairly common to note an error of 50 mm Hg or more in the cold, severely vasoconstricted patient.2 In this situation, femoral invasive or brachial noninvasive oscillometric blood pressure readings may more accurately reflect aortic pressure than do radial invasive readings. It should be noted that noninvasive oscillometric blood pressure readings also have been shown to underestimate systolic pressure and overestimate diastolic pressure in first-time stroke patients.22
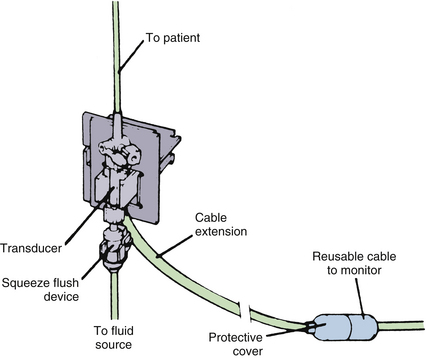
FIGURE 12-2 Typical disposable hemodynamic pressure transducer. (Courtesy Abbott Critical Care Systems, North Chicago, IL.)
Modern electronic monitors are designed to interface reliably with electromechanical transducer systems without the need for extensive training. A provision for static “zeroing” of the system, eliminating a fixed error, is built into the monitor; after the zeroing procedure is accomplished, the system is ready for operation. As previously mentioned, it is important to position the transducer with the reference point at the approximate level of the aortic root to eliminate the effect of the fluid column height difference. Most monitors display a waveform, preferably with a calibrated scale and a digital numeric display of systolic, diastolic, and mean pressures. Each manufacturer produces an electronic instrument with slightly different, often proprietary, frequency response and filtering algorithms. The various techniques for extracting digital quantities vary from simple peak-and-valley detection to sophisticated algorithms that incorporate digital noise filtering and compensation for artifacts and ringing. Thus it is difficult for two different monitors to read exactly the same numerical blood pressure, although the differences are likely to be clinically insignificant, especially with regard to the mean blood pressure value.
Visualization of the pressure waveform, an important step in assuring the accuracy of digital readings, can be quite useful in qualitatively inferring the inotropic and volume status of the patient. In general, a crisp upstroke implies a more hyperdynamic situation, and a broad peak or plateau of the blood pressure waveform implies adequate diastolic filling and venous volume.3 Severely hypovolemic patients often demonstrate a sharp upstroke followed by an equally sharp descent nearly to baseline and a secondary, dicrotic wave approximately half the height of the systolic ejection wave. Marked variation of pulse pressure volume (PPV) as a result of the ventilation cycle is often a sign of hypovolemia or tamponade.23 This can be calculated and displayed in real time using commercially available monitors (Vigileo, LiDCO; Edwards Lifesciences, Irvine, CA) and is increasing in popularity because of the shortage of reliable parameters of fluid status. A marked decrease in the systolic-diastolic difference with a normal mean pressure reading usually indicates a failing catheter or flush system or severe peripheral vasoconstriction.
As blood pressure does not directly correlate well with cardiac output, pulse waveform analysis on invasive arterial pressure waveforms has become a popular approach for minimally invasive cardiac output determinations. This technology has been shown to be reasonably accurate and clinically acceptable, although minimal algorithmic improvements are still necessary.24 Because of the extreme clinical importance of accurate cardiac output measurement, strong future growth in this field is likely.
The electromechanical assembly of catheter, transducer, and connecting tubing forms a less than ideal measuring system (Fig. 12-3) with the introduction of resonances and waveform distortion and resultant predictable errors in blood pressure determination.25 Scaling errors have been all but eliminated with the introduction of disposable, individually calibrated transducers, but older systems require static calibration and comparison with a reference manometer before use.18 The inherent frequency response of the transducer itself is seldom a limiting factor with modern disposable units, but underdamping and ringing at a characteristic high frequency is the rule.26 Underdamping increases systolic readings and simultaneously decreases diastolic readings, with little effect on the mean pressure (Fig. 12-4), generally exaggerating the effects of the vascular tree.1 The fact that the catheter faces into the bloodstream likewise distorts the waveform, produces a pitot-tube effect similar to an airspeed measurement, and exaggerates systolic pressure readings. These errors are especially noticeable in the tachycardic hyperdynamic patient. In practice, resonance errors are usually ignored, in which case mean pressure should be regarded as the value on the basis of which clinical decisions are made. Inexpensive, adjustable, disposable damping devices are available to eliminate the problem of ringing and overshoot and to enable the user to achieve adequate damping (see Fig. 12-4). The use of the shortest possible connecting tubing and careful attention to eliminating air bubbles throughout the system are also essential to ensure accuracy.26
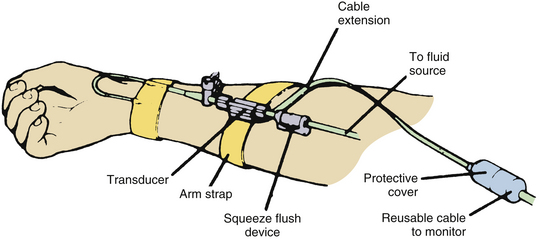
FIGURE 12-3 Recommended setup for invasive, disposable, radial arterial transducer, including short length of connecting tubing.
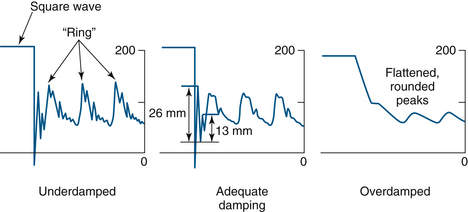
FIGURE 12-4 Effect of damping coefficient on arterial wave morphology. Note the differences in systolic (peak) pressure.
In summary, peripheral invasive blood pressure monitoring has become a standard technique in widespread clinical use when continuous, reliable blood pressure monitoring combined with the ability for convenient blood sampling is required. Modern disposable systems enable reasonable accuracy with a minimum of inconvenience. Arterial cannulation in the adult is a reasonably safe procedure to the best of our current knowledge, but it should nevertheless be used only when clinically indicated and appropriate.
Continuous Noninvasive Blood Pressure Monitoring
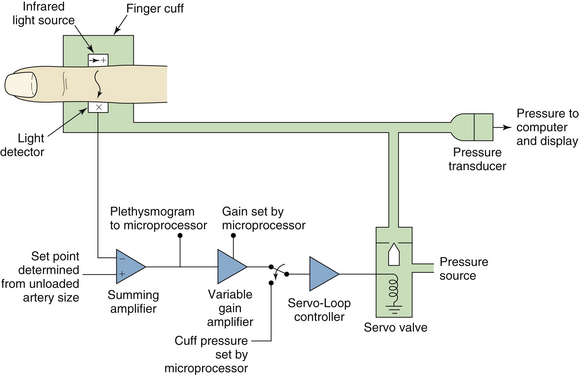
The continuous, beat-to-beat measurement of blood pressure is accurately accomplished using an invasive catheter, but this technique involves discomfort and risk for the patient and is not appropriate for use in healthy subjects on a routine basis. Nevertheless, it is desirable to measure blood pressure continuously and noninvasively under many circumstances. This elusive goal was first reached in a practical form and was reported by Peñaz27 in 1973. The actual measuring element consists of a small air cuff designed to fit around the middle phalanx of the adult finger. The inner surface of the cuff contains a built-in light source that directs an infrared (IR) beam transversely through both digital arteries (Fig. 12-5). An IR receiver on the opposite side of the finger then generates a signal proportional to the blood volume of the finger. The signal is used as a control signal in a feedback loop that causes rapid inflation or deflation of the cuff. Ideally, the feedback system instantaneously tracks pulsatile changes in the finger and inflates the cuff synchronously to maintain a constant IR light absorbance (Fig. 12-6). This condition, known as volume clamping, produces an instantaneous cuff pressure very similar to the instantaneous arterial pressure in the finger. The cuff pressure is then sent to an amplifier and display system similar to that used for invasive pressure measurement. This technology is used in the Finapres blood pressure–monitoring system (Finapres Medical Systems, Amsterdam).28 Three devices that use this technology are the Nexfin (BMEYE, Amsterdam), the Finometer MIDI (second generation of the Finapres), and CNAP (CNSystems, Graz, Austria).
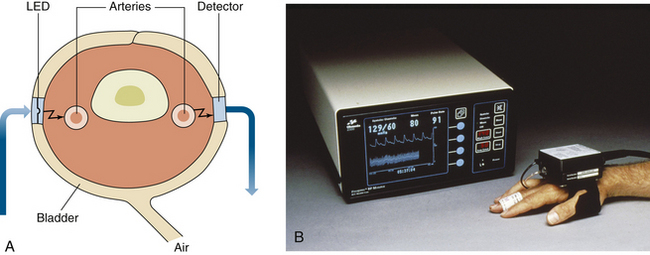
FIGURE 12-5 A, The Finapres blood pressure cuff. LED, light-emitting diode. B, The finger cuff, transducer, and monitor. (B, Courtesy Finapres Medical Systems, Amsterdam.)
The Peñaz method has several obvious limitations.29 Low peripheral perfusion states reduce the useful signal to a point at which oscillation of the feedback system is difficult to prevent, negatively affecting accuracy. When functioning perfectly, the Peñaz method accurately measures the blood pressure in the finger, which may or may not correlate with central arterial pressure. Calibration time has been shown to affect the accuracy compared with intraaortic measurements of blood pressure.30 In the case of vascular disease or physiologic vasoconstriction, such as in hypothermia, blood pressure in the finger can be very low or even essentially absent, whereas the patient may be centrally hypertensive. Perfusion of the finger during continuous use is marginal, although not apparently to a harmful extent, but fingertip cyanosis often is present.31 Prolonged use in a conscious patient is sometimes accompanied by reports of pain, although this issue has been improved with most modern devices. One example is the introduction of a “rest period,” although the Peñaz device is still probably contraindicated in such conditions as Raynaud disease and sickle cell anemia.
Despite these problems, the Peñaz method is arguably the most successful implementation of beat-to-beat noninvasive blood pressure measurement, and it displays clinical accuracy in healthy subjects similar to that of the best oscillometric devices.10 The pressure tracings produced by the Finapres method often strikingly resemble those produced by simultaneous invasive radial artery catheters used during comparison studies, including even the dicrotic notch.28 The Finapres method has also been shown to adequately correlate with arterial blood pressure in determinations of cerebrovascular pressure reactivity.32 The device has proven useful where measurement of rapid blood pressure transients is desirable without the risk, discomfort, and expense of invasive arterial catheterization. By comparison, even the best oscillometric devices offer a blood pressure reading only approximately every 30 seconds.33 In addition, confining the transducer system to one finger eliminates interference with IV infusions and pulse oximetry, which is often problematic with oscillometric monitors.
The CNAP Monitor 500 system (CNSystems Medizintechnik AG, Graz, Austria) uses a double-finger sensor to obtain a continuous noninvasive blood pressure measurement (Fig 12-7). This double-finger sensor produces a continuous blood pressure signal that is calibrated to an initial oscillometric value by a special transfer function. The CNAP uses a vascular unloading technique for measuring blood pressure rhythms and pulse waves. Older methods used only a single control loop, which had to manage fast pressure increases and release in the cuff as well as the tracking of blood pressure changes for the stability of the system. The CNAP overcomes the drawbacks of the single-loop system by using a number of interlocking control loops.

FIGURE 12-7 A, The CNAP Monitor 500 with arm and finger blood pressure cuffs. B, The CNAP monitor double finger cuff and transducer. (Courtesy CNSystems Medizintechnik AG, Graz, Austria.)
The CNAP sensor consists of two semirigid cylinders, one for each finger. Inflatable cuffs, sensors, and electronics are placed inside the semirigid tubes. Three different sizes cover finger diameters from 10 to 30 mm (Fig. 12-8). The device appears to have good correlation with both invasive and oscillometric blood pressure measurements.34-35
Arterial Tonometry
In this context, arterial tonometry (AT) is the external application of a pressure transducer over an artery to discern blood pressure changes from changes in the amplitude of the transduced signal. This method is the oldest proposed method for measurement of beat-to-beat blood pressure, but it has been beset by the lack of a reliable transducer and support system and unacceptable sensitivity to uncompensated changes in dynamic arterial wall tension. Devices using this technology are not common and are considered less clinically useful than oscillometric and invasive measurements.34 The Vasotrac device (Medwave, Arden Hills, MN) was one of the early tonometers, but it is no longer being produced. It was not a continuous monitor; rather it measured blood pressure three to four times a minute. Studies found reasonable correlation with invasive arterial pressure, but the device was not considered accurate enough for use in liver transplantation.37-39 The T-Line Tensymeter TL-200 (Tensys Medical, San Diego, CA) is a newer tonometry device that gives continuous blood pressure measurements. A study by Janelle and colleagues40 found good correlation with simultaneous arterial measurements. AT is more commonly used for the measurement of pulse wave velocity, considered to be the most robust and reproducible measure of arterial stiffness.
Limited development of AT blood pressure devices is still occurring and will no doubt lead to possible future applications. This is due to some unique advantages of AT compared with the Peñaz method for continuous blood pressure recording. AT is theoretically less sensitive than the Peñaz method because of inaccuracies caused by vascular disease and vasoconstriction because the radial artery is so much larger than blood supplies to the finger. Also, discomfort in the awake individual seems to be minimal and cyanosis is not observed. However, future innovations are still needed to improve and expand this technology.
Pulse Transit Time: Photometric Method
The relationship between pulse wave velocity and blood pressure was first described in 1922 by Bramwell and Hill. Pulse transit times (PTTs) are measured by pulse transducers placed at two or more sites on the body. The transducers, located at different distances from the central circulation, measure the delay time between the sites (Fig. 12-9). Alternatively, the time can be calculated as the time delay from the initiation of the cardiac contraction (measure from electrocardiogram) to the photoplethysmograph waveform. PTT has been used in psychiatric studies as a nonspecific index of cardiovascular activity, and it has long been noted that PTT bears a roughly inverse relationship to systolic arterial blood pressure.41 The relation to diastolic and mean pressure does not seem to be as clear. Calibration is commonly accomplished via a separate oscillometric monitor and brachial cuff placed on the arm. Changes in blood pulse transit time are transformed into blood pressure measurements using a proprietary algorithm.
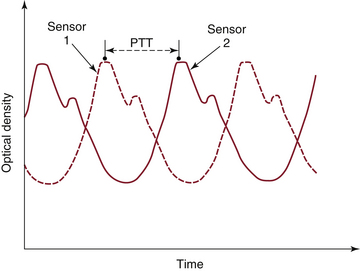
FIGURE 12-9 Definition of pulse transit time (PTT) as measured by two optical sensors. (Courtesy GE Healthcare, Waukesha, WI.)
The accuracy of these devices has not been adequately evaluated in an objective fashion and depends to a large extent on the presumption of a relationship between blood pressure and transit time. Recent preliminary data have shown a strong correlation to invasive blood pressure measurements.42 This technology theoretically eliminates most of the problems associated with the Peñaz and tonometric methods discussed above. If this methodology continues to demonstrate accurate readings, it will offer a beat-to-beat blood pressure technology only slightly more cumbersome than the now-standard oscillometric unit combined with the similarly standard pulse oximetry.
As mentioned, several methods of noninvasively measuring blood pressure have been developed into practical working devices. Although fast approaching, none of the continuous methods discussed has consistently demonstrated the reliability and ease of use that have been realized by the oscillometric units. In addition, the expense of these alternative technologies has largely limited their use to experimental protocols rather than routine use.
In summary, invasive measurement of blood pressure via a peripherally placed intraarterial cannula remains the method of choice when beat-to-beat blood pressure measurement is required for clinical care. Invasive monitoring is not without risk, but where continuous pressure monitoring and/or frequent blood sampling is required, the morbidity is quite acceptable.
References
1. Hamilton W.F., Dow P. An experimental study of the standing waves in the pulse propagated through the aorta, Am J Physiol. 1939;(125):48–49.
2. Pauca A.L., Hudspeth A.S., Wallenhaupt S.L., et al. Radial artery-to-aorta pressure difference after discontinuation of cardiopulmonary bypass. Anesthesiology. 1989;70(6):935–941.
3. Bruner J.M.R. Handbook of blood pressure monitoring. Littleton, MA: PSG Publishing; 1978.
4. Pennington L.A., Smith C. Leveling when monitoring central blood pressures: an alternative method. Heart Lung. 1980;9(6):1053–1059.
5. Pickering T.G., Hall J.E., Appel L.J., et al. Recommendations for blood pressure measurement in humans and experimental animals. Part 1: Blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005;45(1):142–161.
6. Manning D.M., Kuchirka C., Kaminski J. Miscuffing: inappropriate blood pressure cuff application. Circulation. 1983;68(4):763–766.
7. Finnie K.J., Watts D.G., Armstrong P.W. Biases in the measurement of arterial pressure. Crit Care Med. 1984;12(11):965–968.
8. Rutten A.J., Ilsley A.H., Skowronski G.A., Runciman W.B. A comparative study of the measurement of mean arterial blood pressure using automatic oscillometers, arterial cannulation and auscultation. Anaesth Intensive Care. 1986;14(1):58–65.
9. Talke P., Nichols R.J., Jr., Traber D.L. Does measurement of systolic blood pressure with a pulse oximeter correlate with conventional methods? J Clin Monit. 1990;6(1):5–9.
10. Gorback M.S., Quill T.J., Lavine M.L. The relative accuracies of two automated noninvasive arterial pressure measurement devices. J Clin Monit. 1991;7(1):13–22.
11. Myers M.G., Gowin M., Dawes M., et al. Conventional versus automated measurement of blood pressure in primary care patients with systolic hypertension: randomised parallel design controlled trial. Br Med J. 2011;342:d286.
12. Amoore J.N., Lemesre Y., Murray I.C., et al. Automatic blood pressure measurement: the oscillometric waveform shape is a potential contributor to differences between oscillometric and auscultatory pressure measurements. J Hypertens. 2008;26(1):35–43.
13. Alpert B.S. Oscillometric blood pressure values are algorithm-specific. Am J Cardiol. 2010;106(10):1524. author reply 1524–1525
14. Loubser P.G. Comparison of intra-arterial and automated oscillometric blood pressure measurement methods in postoperative hypertensive patients. Med Instrum. 1986;20(5):255–259.
15. Marks L.A., Groch A. Optimizing cuff width for noninvasive measurement of blood pressure. Blood Press Monit. 2000;5(3):153–158.
16. Gorback M.S., Quill T.J., Bloch E.C., Graubert D.A. Oscillometric blood pressure determination from the adult thumb using an infant cuff. Anesth Analg. 1989;69(5):668–670.
17. Yocum G.T., Gaudet J.G., Teverbaugh L.A., et al. Neurocognitive performance in hypertensive patients after spine surgery. Anesthesiology. 2009;110(2):254–261.
18. Philip J.H., Philip B.K., Lehr J.L. Accuracy of hydrostatic pressure measurement with a disposable dome transducer system. Med Instrum. 1985;19(6):273–274.
19. Slogoff S., Keats A.S., Arlund C. On the safety of radial artery cannulation. Anesthesiology. 1983;59(1):42–47.
20. Selldén H., Nilsson K., Larsson L.E., Ekström-Jodal B. Radial arterial catheters in children and neonates: a prospective study. Crit Care Med. 1987;15(12):1106–1109.
21. Maki D.G., Kluger D.M., Crnich C.J. The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc. 2006;81(9):1159–1171.
22. Manios E., Vemmos K., Tsivgoulis G., et al. Comparison of noninvasive oscillometric and intra-arterial blood pressure measurements in hyperacute stroke. Blood Press Monit. 2007;12(3):149–156.
23. Cannesson M., Aboy M., Hofer C.K., Rehman M. Pulse pressure variation: where are we today? J Clin Monit Comput. 2011;25(1):45–56.
24. Della Rocca G., Costa M.G., Chiarandini P., et al. Arterial pulse cardiac output agreement with thermodilution in patients in hyperdynamic conditions. J Cardiothorac Vasc Anesth. 2008;22(5):681–687.
25. Gardner R.M. Direct blood pressure measurement: dynamic response requirements. Anesthesiology. 1981;54(3):227–236.
26. Hunziker P. Accuracy and dynamic response of disposable pressure transducer-tubing systems. Can J Anaesth. 1987;34(4):409–414.
27. Peñaz J.: Photoelectric measurement of blood pressure, volume, and flow in the finger. In Albert A., Vogt W., Hellig W., editors: Digest of the Tenth International Conference on Medical and Biological Engineering, Dresden, 104, 1973
28. Boehmer R.D. Continuous, real-time, noninvasive monitor of blood pressure: Peñaz methodology applied to the finger. J Clin Monit. 1987;3(4):282–287.
29. Kurki T., Smith N.T., Head N., Dec-Silver H., Quinn A. Noninvasive continuous blood pressure measurement from the finger: optimal measurement conditions and factors affecting reliability. J Clin Monit. 1987;3(1):6–13.
30. Panerai R.B., Sammons E.L., Smith S.M., et al. Transient drifts between Finapres and continuous intra-aortic measurements of blood pressure. Blood Press Monit. 2007;12(6):369–376.
31. Gravenstein J.S., Paulus D.A., Feldman J., McLaughlin G. Tissue hypoxia distal to a Peñaz finger blood pressure cuff. J Clin Monit. 1985;1(2):120–125.
32. Kasprowicz M., Schmidt E., Kim D.J., et al. Evaluation of the cerebrovascular pressure reactivity index using non-invasive Finapres arterial blood pressure. Physiol Meas. 2010;31(9):1217–1228.
33. Gorback M.S., Quill T.J., Graubert D.A. The accuracy of rapid oscillometric blood pressure determination. Biomed Instrum Technol. 1990;24(5):371–374.
34. Jagadeesh A.M., Singh N.G., Mahankali S. A comparison of a continuous noninvasive arterial pressure (CNAP) monitor with an invasive arterial blood pressure monitor in the cardiac surgical ICU. Ann Cardiac Anaesth. 2012;15:180–184.
35. Ilies C., Kiskalt H., Siedenhans D., et al. Detection of hypotension during caesarean section with continuous non-invasive arterial pressure device or intermittent oscillometric arterial pressure measurement. Br J Anaesth. 2012;109:413–419.
36. Hansen S., Staber M. Oscillometric blood pressure measurement used for calibration of the arterial tonometry method contributes significantly to error. Eur J Anaesthesiol. 2006;23(9):781–787.
37. Belani K., Ozaki M., Hynson J., et al. A new noninvasine method to measure blood pressure: results of a multicenter trial. Anesthesiology. 1999;91:686–692.
38. Thomas S.H., Winsor G.R., Pang P.S., et al. Use of a radial artery compression device for noninvasive, near-continuous blood pressure monitoring in the ED. Am J Emerg Med. 2004;22:474–478.
39. Findlay J.Y., Gali B., Keegan M.T., et al. Vasotrac arterial blood pressure and direct arterial blood pressure monitoring during liver transplantation. Anesth Analg. 2006;102:690–693.
40. Janelle G.M., Gravenstein N. An accuracy evaluation of the T-Line Tensymeter (continuous noninvasive blood pressure management device) versus conventional invasive radial artery monitoring in surgical patients. Anesth Analg. 2006;102:484–490.
41. Lane J.D., Greenstadt L., Shapiro D., Rubinstein E. Pulse transit time and blood pressure: an intensive analysis. Psychophysiology. 1983;20(1):45–49.
42. Bartsch S., Ostojic D., Schmalgemeier H., et al. Validation of continuous blood pressure measurements by pulse transit time: a comparison with invasive measurements in a cardiac intensive care unit [in German]. Dtsch Med Wochenschr. 2010;135(48):2406–2412.