Assessment for Sports Massage and Physical Rehabilitation Application
Outcome Goals and Care or Treatment Plans
Assessment Using Joint Movement
Kinetic Chain Assessment of Posture
Palpation of the Skin and Superficial Connective Tissue
Palpation of Superficial Connective Tissue Only
Palpation of Vessels and Lymph Nodes
Understanding Assessment Findings
After completing this chapter, the student will be able to perform the following:
1 Describe assessment for the sport and fitness population.
2 Apply a clinical reasoning process to treatment plan development.
3 Develop outcome goals that are quantifiable and qualifiable.
4 Adapt charting methods to the athletic population.
5 Complete a comprehensive history.
6 Complete a comprehensive physical assessment.
7 Perform postural assessment.
8 Perform basic orthopedic tests to assess for joint injury.
9 Analyze movement assessment findings.
10 Perform muscle strength assessment.
11 Describe and assess kinetic chain function.
13 Perform palpation assessment.
14 Integrate clinical reasoning into the treatment plan using assessment findings.
15 Relate assessment data to first-degree, second-degree, and third-degree dysfunction, and categorize the adaptation response to stage 1, 2, or 3 pathology.
16 Integrate ongoing assessment data channeled into appropriate massage treatment strategies.
Assessment
The massage therapist working with athletes, physical rehabilitation, and those involved with fitness has an expanded assessment responsibility. Assessment identifies the structures that need to be worked with, creates a clear intention about treatment goals, provides a baseline of objective information to measure the effectiveness of the treatment, and helps identify conditions that are contraindicated. When working with a client who is striving for optimal performance or who has pain, dysfunction, or disability, the massage therapist needs to gather information about both long-term and short-term treatment goals and relevant data about activities and training activity, as well as about pain or decreased function.
Information from the athletic trainer, coaches, or other professionals is important. The massage therapist must understand and apply assessment information provided by the trainer. If at any time you do not understand, ask clarifying questions. Information gathered by the massage therapist should be shared with the athletic trainer or other appropriate member of the sport and/or medical team in a concise and intelligent manner.
A massage treatment plan based on efficient biomechanical movement should focus on reestablishing or supporting effective movement patterns. Biomechanically efficient movement is smooth, bilaterally symmetric, and coordinated, with easy, effortless use of the body. Functional assessment measures the efficiency of coordinated movement. During assessment, noticeable variations need to be considered.
Once the treatment plan has been determined, the massage therapist needs to develop strategies for achieving the goals pertaining to the therapeutic massage. Teamwork is essential, with cooperation and consensus among the various professionals attending to the client. It is important for the massage therapist to maintain an appropriate scope of practice and not infringe on the professional responsibilities and expertise of others.
Clinical Reasoning Process
As the volume of knowledge pertaining to massage increases, and as soft tissue modalities such as massage are integrated into the areas of sport fitness and physical rehabilitation, it is becoming increasingly important to be able to think or reason through an intervention process and justify its effectiveness. Therapeutic massage practitioners must be able to gather information effectively, analyze that information to make decisions about the type and appropriateness of an intervention, and evaluate and justify the benefits derived from the intervention.
Effective assessment, analysis, and decision making are essential in meeting the needs of each client. Routine or a recipe-type application of therapeutic massage does not work for this population because each person’s set of presenting circumstances and outcome goals is different. An experienced sports massage professional possesses effective clinical reasoning skills targeted to this complex population.
Fact gathering is an initial part of the clinical reasoning process. Each unique client situation needs to be thoroughly researched. This text provides only a portion of the information needed. Additional research is almost always necessary.
Every massage professional who works with athletes needs to have a medical dictionary and comprehensive texts on athletic training, kinesiology, and pathology, as well as resources on the particular sport and references on medication and nutritional supplements. See the resource list in this text for recommendations. The Internet is also a vast resource.
Each sport has its ideal performance requirement and common injuries; however, a sprain in a football player, a soccer player, or a skate boarder is still a sprain. The sprain should be addressed according to the recommendations in this text. Understanding the demands of the sport is important. However, it is not necessary for the massage professional to be an expert in the sport activity. The sport activity is the context that the massage outcomes support.
Subjective and objective assessments are also sources of facts and are the major focus of this chapter. Analysis of factual data in the assessment leads to treatment plan development.
Outcome Goals and Care or Treatment Plans
Outcome goals need to be quantified. This means that they are measured in terms of objective criteria such as time, frequency, 1 to 10 scales, measurable increase or decrease in ability to perform an activity, and/or measurable increase or decrease in sensation, such as relaxation or pain.
Outcome goals also need to be qualified. How will we know when the goal is achieved? What will the client be able to do after the goal has been reached that he or she is not able to do now? For example, How fast will the client be able to run? What performance skills will the client be able to perform?
After the analysis of history and assessment data is complete and problems and goals have been identified, a decision needs to be made about the care or treatment plan. Depending on the situation, the massage treatment plan may need to be approved by appropriate supervising personnel.
Short-term goals typically support a session-by-session process and are dependent on the current status of the client. Long-term goals typically support recovery, performance, or rehabilitation. Long-term goals focus on what is being worked toward. Short-term goals focus on what currently is being worked on, as well as incremental steps toward achieving long-term goals. Short-term goals should not be in conflict with long-term goals.
For example, a golfer is involved in a conditioning program in preparation for going on tour. She has been working with the strength and conditioning coach on core strength and cardiovascular fitness. She has also been working with the golf coach on swing mechanics. Long-term goals for this client are to maintain range of motion (ROM) and manage a chronic tendency for low back pain. During this particular session, the client has indicated that she has a headache and delayed-onset muscle soreness. The focus of the current massage must consider both short-term and long-term goals. Short-term goals are to reduce headache pain and fluid retention as part of the existing long-term treatment plan.
How much time is allocated to each set goal depends on the adaptive capacity of the client. For example, massage targeting connective tissue application as part of the long-term goals plan may be reduced or eliminated in the areas where delayed-onset muscle soreness exists. Muscle energy application may require more effort than the client is willing to expend because of the headache.
It is this ever-changing dynamic of past history, current conditions, and future outcomes that makes any sort of massage routine useless. Each and every session is uniquely developed and applied on the basis of multiple factors. Many influencing factors must be considered when one is treating athletes or those in physical rehabilitation of any type. Assessment is the identification of all of these influences. Clinical reasoning is the sorting and developing of an appropriate treatment session.
Charting
As the treatment plan is implemented, it is recorded sequentially, session by session, in some form of charting process such as SOAP (subjective, objective, assessment [analysis], and plan). The plan is reevaluated and adjusted as necessary. This process should have been learned in entry level massage training.
Various charting methods are used in the sport and fitness realm. Regardless of the particular style, the basic SOAP plan is easily modified to other charting styles. Be very clear with supervisory personnel, usually the trainer, about the type and depth of information included on the client’s chart.
Good record keeping provides the therapist with the information necessary to communicate with health care and other personnel and furnishes accurate details about what treatment goals are specified, the methods of massage used, and the effectiveness of treatment.
Assessment Details
How extensive the assessment is depends on whether you are working under the direction of a doctor, a trainer, or another health care provider or are working independently. It is the responsibility of the primary care provider to take a thorough history, perform a complete examination, and inform the massage therapist regarding the client’s condition and desired outcomes for the massage. If you are working independently, it is your responsibility to perform the appropriate comprehensive assessment, especially to note contraindications and to clarify treatment goals.
This text assumes that the reader already has completed a comprehensive therapeutic massage course of study that included assessment procedures such as history taking, physical assessment, treatment plan development, and charting.1
The following procedures are recommended for targeting this specific population.
History
The history interview provides subjective information pertaining to the client’s health history, the reasons for massage, a history of the current condition, a history of past illness and health, and a history of any family illnesses that may be pertinent. It also contains an account of the client’s current health practices.
Targeting this information to the athlete or person in physical rehabilitation is the focus of this text. In addition to the general history, anyone who is working with an athlete or a person in physical rehabilitation needs to explore the following for each client:
• Surgery or medical procedures
• Therapeutic exercise activities
• Physical therapy intervention
• Training types such as strength and conditioning and agility
• Cognitive load (how much mental training required)
The client’s history may vary depending on whether the problem is the result of sudden trauma or is chronic. The following questions should be addressed if the athlete has an acute injury. Usually it is the doctor or trainer who performs the initial injury assessment:
• Has the client hurt the area before?
• How did the client hurt the area?
• What was heard when the injury occurred—a crack, snap, or pop?
• How bad was the pain and how long did it last?
• Is there any sense of muscle weakness?
• How disabling was the injury?
• Could the client move the area right away?
• Was the client able to bear weight for a period of time?
• Has a similar injury occurred before?
• Was there immediate swelling, or did the swelling occur later (or at all)?
For an athlete with a chronic condition, ask the following:
• What was the nature of the injury (trauma or repetitive use)?
• What is the nature of the pain—hot, pokey, sharp?
• When does the pain occur—when bearing weight or after activity?
• What injuries have occurred in the past?
• What first aid and therapy, if any, were given for these previous injuries?
Additional questions address when the client first noticed this condition to help to identify any previous incident or injury that occurred before the current condition:
Typically, a gradual onset suggests an overuse syndrome, postural stresses, or somatic manifestations of emotional or psychological stresses common in athletes.
Ask the client to point to as well as explain the area of complaint.
It is also important to know whether the client has had massage therapy before, whether it was helpful, and the type of massage application.
If the client has taken pain medication within 4 hours of assessment and treatment, the medication may be giving the client a false sense of comfort during assessment and during massage. Be aware of antiinflammatories, muscle relaxers, and so forth.
Is the client getting better, worse, or is the client in need of a referral?
Gestures
Pay attention to gestures used by the client. The general guidelines for gestures listed here are not written in stone. Professional experience indicates that those listed here are fairly dependable starting points when interpreting an individual’s body language.
It is the professional’s responsibility to understand what a gesture means for a particular individual.
The following are common gestures:
• A finger pointing to a specific area suggests an acupressure or motor point hyperactivity or a joint problem. What the pointing means depends on the area indicated.
• If the finger is pointed to a specific area and then the hand swipes in a certain direction, it may be a trigger point problem.
• If the area is grabbed, pulled, or held and is moved as if being stretched, this often indicates muscle or fascial shortening.
• If movement is needed to show the area of concern, the area may need muscle lengthening combined with muscle energy work to prepare for the stretch and reset of neuromuscular patterns.
• If the client moves into a position and then acts as if stuck, the area may need connective tissue stretching.
• If the client draws lines on his body, this may indicate nerve entrapment in the fascial planes or grooves.
Symptoms
It is important to determine how often the client notices the dysfunction or disability. Is it once a day, 2 or 3 days a week, once a week, or constant? Grade 1 and 2 sprains and strains to the muscles, tendons, and ligaments usually hurt when they are being used, and are relieved with rest. Constant pain may be associated with severe injury or underlying pathology. A client with constant pain should be referred to a physician.
The more serious the condition, the longer it will last.
Typical words used by the client to describe the symptoms are “stiff,” “achy,” “tight,” “stuck,” and “heavy.” These words are associated with muscles, tendons, ligaments, and joint capsules and their associated connective tissue and usually describe simple tension or mild overuse of the soft tissue or edema. If an ache is more than mild, is frequent, and lasts a long time, it is more serious and represents inflammation. A referral is required to rule out a more serious condition.
Typically, tight means an increase in neuromuscular activity. Achy and fat often indicate fluid retention or swelling. Stiff sensations often indicate a connective tissue pliability issue. Heavy sensation of the limbs indicates a firing pattern or gait reflex problem. Stuck sensations often mean a joint problem.
Other terms used to describe symptoms include the following:
Sharp, stabbing, tearing describes a more severe injury to the musculoskeletal system or a nerve root condition. This type of sensation is experienced with muscle or ligament tears, especially when the muscle or ligament is being used. The sensation is usually relieved at rest. A nerve root inflammation can elicit a sharp or stabbing pain, independent of movement.
Tingling, numbing, picky describes a nerve compression near the spine or in the extremities, or a circulation impairment.
Throbbing, hot is associated with acute injury inflammation and swelling, such as an abrasion puncture wound or an acute bursitis. Severe throbbing is a contraindication to massage.
Gripping, cramping is typically used to describe a serious condition, often a nerve root injury or a visceral condition. Gripping and cramping pain is a contraindication to massage and requires referral to a doctor.
The client can choose from the following descriptors:
Irritation or injury to the soft tissue can refer to the extremities, with diffuse pain and aching. Nerve entrapment and trigger point pain can radiate. Sharp well-localized pain in the extremities felt even at rest typically indicates a nerve root problem and requires a referral.
Ask the client to rate his or her pain on a 0 to 10 scale, with 10 being the worst pain ever experienced (incapacitating pain) and 0 being no pain. Moderate pain (5 to 9) interferes with a person’s ability to perform sport-related activities. Mild pain (1 to 4) does not interfere with a person’s activities of daily living but may interfere with sport performance.
The most simple strains and sprains of the musculoskeletal system are irritated by too much movement and are relieved by rest. When a condition hurts more with rest, this indicates either inflammation or pathology.
• What activities make the condition worse—moving, sitting, standing, walking, or resting?
• What sport movement is affected—running, jumping, cutting, swinging, acceleration, or deceleration?
As the soft tissue heals, it feels good to move the injured area. Stretching tight muscles, shortened ligaments, and joint capsules feels good, despite some mild discomfort. Acute injuries involving the soft tissue are painful with large movements and are relieved with rest. Muscle guarding makes stretching painful.
Pain caused by inflammation and tumors is worse at night. Constant, gripping pain that is worse at night requires immediate referral to a doctor. An area that hurts at night but is relieved with movement usually indicates inflammation. Joint pain and stiffness with fascial shortening are usually worse in the morning.
Clarifying assessment questions to ask include the following:
The client should demonstrate for the massage therapist. Trust the client’s impressions. They usually are right. Then translate what the client is saying into a massage application.
The client should draw a picture of his or her condition. When the client draws the picture, give as few directions as possible. Evaluate the drawing for location and intensity of the symptom. Does the client use hard zigzag lines or small or large circles? Then ask the client to explain.
All the history information should be consolidated and considered when treatment plans and session outcomes are documented.
![]() See the Evolve website that accompanies this book for an example of a history taking form.
See the Evolve website that accompanies this book for an example of a history taking form.
Physical Assessment
After the history is complete, the physical assessment is performed. The objective data are obtained during physical assessment.
Accurate assessment is best achieved using a sequence to ensure that all relevant information has been gathered. A major aspect of a massage session is palpation assessment.
In general, physical assessment includes the following:
Identify any scars or muscle atrophy. Scars may indicate prior surgery or prior injury and reveal that the area is compromised. Ask the client to describe how he or she received the scar.
An area of atrophy may have been deconditioned owing to lack of use, or this may indicate neurologic involvement. Simple atrophy can be a result of immobilization caused by prior fracture or lack of use due to pain.
Physical Assessment of Posture
Note the posture of the client in standing and seated positions, as well as the posture or position of the area of complaint. Look for areas of asymmetry. Asymmetry usually results when overly tense muscles or shortened connective tissue pulls the body out of alignment.
Direct trauma pushes joints out of alignment. Weak stabilizing mechanisms, such as overstretched ligaments or inhibited antagonist muscles, contribute to the problem. In these situations, a chiropractor, an osteopath, or another trained medical professional skilled in skeletal manipulation is needed. Often a multidisciplinary approach to client care is necessary.
First, observe the client during general movement as opposed to formal assessment to identify natural function. Then, perform the following structured standing assessment and compare the findings.
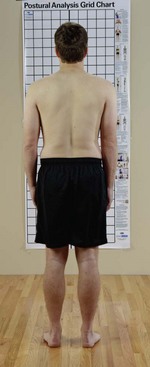
Standard Posture Front View
Standard Posture Back View
• Head: neutral position neither tilted nor rotated
• Shoulders: level, not elevated or depressed
• Scapulae: neutral position, medial borders essentially parallel and approximately 3 to 4 inches apart
• Thoracic and lumbar spines: straight
• Pelvis: level with both posterior superior iliac spines in same transverse plane
• Hip joints: neutral position neither adducted nor abducted or rotated (internal or external)
Standard Posture Side View
• Head: neutral position, not tilted forward or backward
• Cervical spine: normal curve, slightly convex to anterior
• Scapulae: flat against upper back
• Thoracic spine: normal curve, slightly convex to posterior
• Lumbar spine: normal curve, slightly convex to anterior
• Pelvis: neutral position, anterior superior iliac spine in same vertical plane as symphysis pubis
• Hip joints: neutral position, leg vertical at right angle in sole of foot
Note: An imaginary line should run slightly behind the lateral malleolus, through the middle of the femur, the center of the shoulder, and the middle of the ear.
Chart the findings and relate them to the client’s history (Figure 10-1).
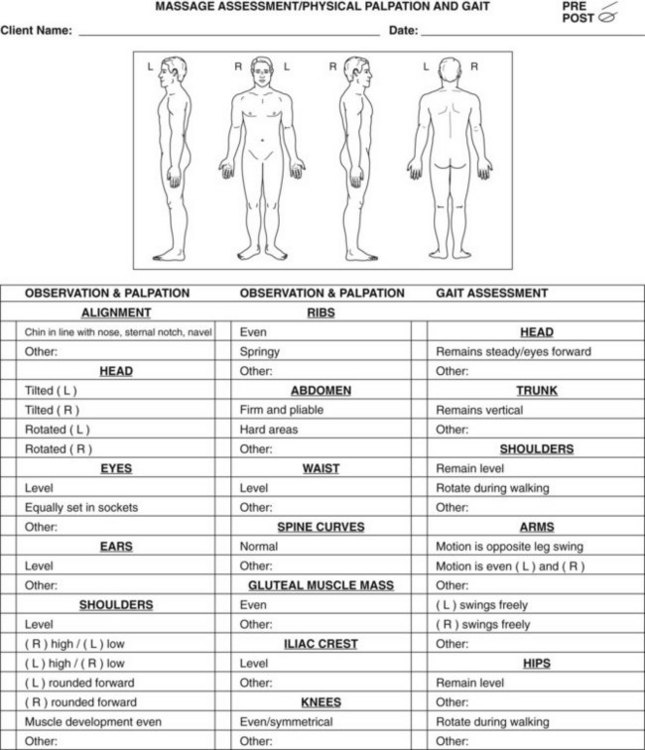
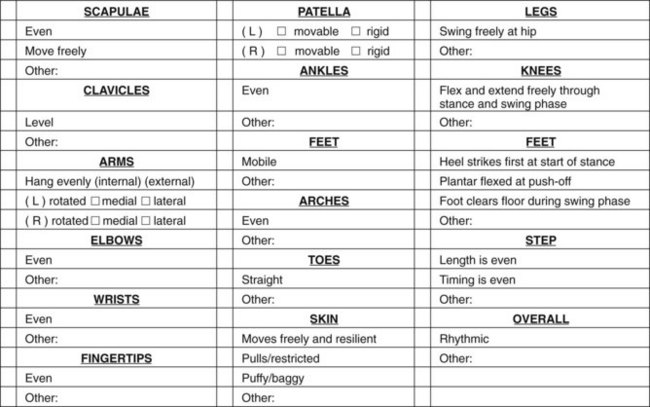
FIGURE 10-1 Physical assessment form. (Feel free to copy this form to use as an assessment tool.) (From Fritz S: Mosby’s fundamentals of therapeutic massage, ed 5, St Louis, 2013, Mosby.)
For the physical assessment, the main considerations are body balance, efficient function, and basic symmetry (Box 10-1).
The body is not perfectly symmetric, but the right and left halves of the body should be similar in shape, ROM, and ability to function. The greater the discrepancy in symmetry, the greater is the potential for soft tissue dysfunction.
Three major factors influence posture: heredity, disease, and habit. These factors must be considered when evaluating posture. The easiest influence to adjust is habit. By normalizing the soft tissue and teaching balancing exercises, the massage practitioner can play a beneficial role in helping clients overcome habitual postural distortion. Effects may arise from occupational habits (e.g., a shoulder rotation from golf) and recreational habits (e.g., a forward-shoulder position in a bike rider), or they may be sleep-related (long-term use of high pillows).
Clothing, sport equipment, shoes, and furniture affect the way a person uses his or her body. Tight clothing or equipment around the neck restricts breathing and contributes to neck and shoulder problems. Restrictive belts or tight pants also limit breathing and affect the neck, shoulders, and midback. Shoes with high heels and those that do not fit the feet comfortably interfere with postural muscles. Shoes with worn soles imprint the old postural pattern, and the client’s body assumes the dysfunctional pattern if he or she puts them back on after the massage. If postural changes are to be maintained, it is important to wear shoes that do not have worn soles.
Sleep positions can contribute to a wide range of problems. Furniture that does not support the back or that is too high or too low perpetuates muscular tension. Competing athletes travel and therefore change beds often. The seats in airplanes are seldom comfortable for athletes.
When assessing posture, it is important for the massage therapist to notice the complete postural pattern. Most compensatory patterns occur in response to external forces imposed on the body. However, if the client has had an injury, maintains a certain position for a prolonged period, or overuses a body area, the body may not be able to return to a normal dynamic balance efficiently. The balance of the body against the force of gravity is the fundamental determining factor in a person’s posture or upright position. Even subtle shifts in posture demand a whole body compensatory pattern (Figure 10-2).
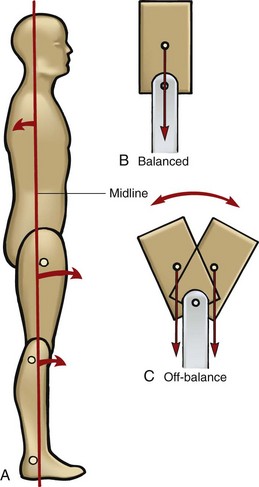
FIGURE 10-2 In normal relaxed standing (A), the leg and trunk tend to rotate slightly off the midline of the body but maintain a counterbalance force. Balance is achieved in B, but not in C. Whenever the trunk moves off this midline balance point, the body must compensate. (From Fritz S: Mosby’s fundamentals of therapeutic massage, ed 3, St Louis, 2004, Mosby.)
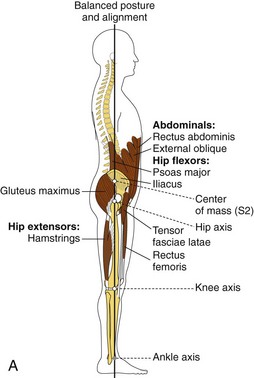
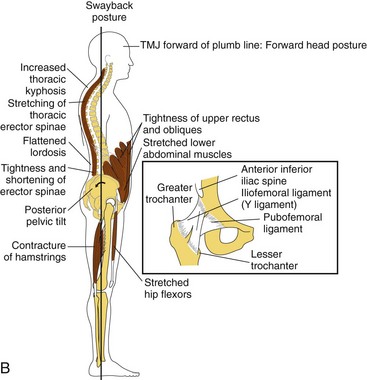
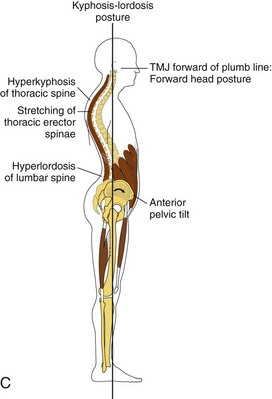
Cervical, thoracic, lumbar, and sacral curves develop because of the need to maintain an upright position against gravity (Figure 10-3).
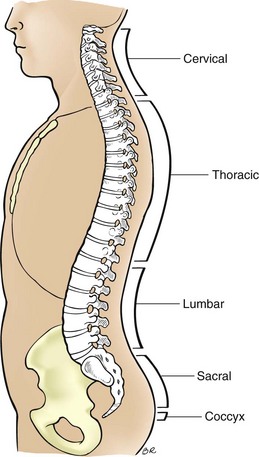
FIGURE 10-3 Normal spinal curves. (From Fritz S: Mosby’s fundamentals of therapeutic massage, ed 5, St Louis, 2013, Mosby.)
Standing posture requires various segments of the body to cooperate mechanically as a whole. Passive tension of ligaments, fascia, and connective tissue elements of the muscles supports the skeleton. Muscle activity plays a small but important role. Postural muscles maintain small amounts of contraction that stabilize the body upright in gravity by continually repositioning the body’s weight over the mechanical balance point.
In relaxed symmetric standing, both the hip and the knee joints assume a position of full extension to provide the most efficient weight-bearing position. The knee joint has an additional stabilizing element in its “screw home” mechanism. The femur rides backward on its medial condyle and rotates medially about its vertical axis to lock the joint for weight bearing. This happens only in the final phase of extension. The hamstrings are the major muscles that resist the force of gravity at the knees.
At the ankle joint, bones and ligaments do little to limit motion. Passive tension of the two-joint gastrocnemius muscle (i.e., the muscle crosses two joints) becomes an important factor. This stabilizing force is diminished if high-heeled shoes are worn. For example, rodeo riders wear cowboy boots. The heel of the shoe puts the gastrocnemius on a slack. If these heels are worn constantly, the muscle and the Achilles tendon shorten.
Posture is primarily determined by hereditary factors, such as bone structure and muscle type, and even by habitual movement patterns. These can create natural imbalances, but alone they do not normally lead to painful conditions until later in life. They can, however, combine with other stresses such as athletic activity, and together can lead to injury. Little can be done to change these hereditary factors, and regular exercise and soft tissue treatment are often the only ways of avoiding such symptoms.
Upright posture is maintained by a series of muscles running down the body. These muscles need to balance each other, in terms of strength and tension, and together must resist the forces of gravity. Any postural change will nearly always be in a downward and forward direction because fatigue or injury reduces the ability of postural muscles to combat gravity. This creates increased curvature in particular sections of the spine, which can be seen by the therapist when observing the client’s standing posture.
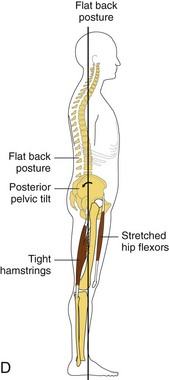
Postural dysfunction occurs in the three planes of movement (sagittal, frontal, and transverse), as well as in supination and pronation (Figures 10-4 and 10-5).
Assessment of Joint and Muscle Function
The more the fascia muscle tissue structure is researched, the more we understand that the concept of individual muscles is flawed. It is necessary to rethink the functional and structural aspect of contractile tissues—muscle tissue—as a continuum of function within spans of connective tissues such as fasciae, ligaments, and tendons. The idea of individual muscles and specific attachments is ingrained and it will take a long time to shift the paradigm. Throughout this text, the functional unit has been emphasized; however, knowledge of individual muscle names and locations remains valuable and will be used. Although the muscular system looks highly complicated, it is important to realize that the actual mechanics involved in movement are simple. A muscle can do only two things: it can contract and shorten, and it can relax and lengthen. The system is a complex pattern of movement composed of many simple levers and pulleys. Movement is created by muscle shortening, which pulls together bones that are connected at the joint.
Many muscles working in functional units provide the widest variety of movements and the ability to do them with stability, control, and efficiency. For example, the knee is basically a hinge joint capable of moving on only one plane, and so, theoretically, it should need only one pulley (muscle) to flex it and one to extend it. However for extension, there are the four quadriceps muscles, each of which pulls across the joint in a slightly different direction. During flexion, three hamstrings accomplish the same thing. This muscle interaction stabilizes the joint and enables it to adapt to variations in movement and to the random direction of forces from the outside environment. The whole of the muscular system works in unison to enable the body to cope with the stresses caused by gravity when movement takes place. It is important to see movement in terms of patterns of activity (movement strategies) taking place within a system rather than as the action of individual muscles. Almost all movement strategies involve the gait (walking) process.
Overuse problems develop in parts of a system that are put under greater stress, or repetitive use, compared with the rest of the system. The running action, for instance, does not involve just the leg muscles. Many muscles work to create a complicated pattern of rotation and spiral movements throughout the entire body. If this did not happen, and if movement is confined to the legs, then all the stress of impact and push-off will be absorbed by the ankle, knee, and hip joints, and the forces on these joints will cause damage. The spiraling movement up the body absorbs the stress and distributes the impact through many joints. Because no individual structure absorbs too much stress, the human body is able to function for many years.
Coordinated movement involves many muscles working together in a pattern to create the power and control needed to accomplish a task. Each muscle has a preferred function within a movement pattern; therefore, a particular movement will involve greater effort from certain individual muscles. For example, kicking a soccer ball involves a strong effort from the quadriceps muscles. Each of the four muscles within the group acts on the joint from a different angle; therefore, depending on the degree of rotation in the lower leg and the angle of force, one muscle may have to keep working slightly more than the rest.
The muscular system develops according to how the body is used. Each individual has unique patterns of muscle function adaptation, many of which are beneficial and are in harmony with the person’s activities and lifestyle, although some will be negative or excessive. Assessment provides information about beneficial or detrimental function.
For example, a midfield soccer player who often has to pass the ball with the inside of the foot will tend to use the vastus medialis, and the adductors may be involved. Therefore, the soccer player would naturally develop increased strength in the vastus medialis and adductors while training. Although this may appear to create an imbalance within the other quadriceps muscles, it could be natural for the individual; therefore, this may not be a situation requiring remedial treatment. The same imbalance found in a distance runner complaining of patellofemoral syndrome or groin pain would be a treatment priority.
Microtrauma
A muscle can suffer acute strain with its fibers being torn, if overused or overloaded. The same can occur on a microscopic level, even if just a few fibers are overused. When this breakdown occurs on a microscopic level, the pathologic changes that take place are the same as with any soft tissue tear: bleeding, swelling, muscle tension, guarding in surrounding tissues, and scar tissue formation. The delayed-onset muscle soreness experienced in muscles after hard exercise is due in part to this type of trauma (microtrauma).
Scar tissue can continue to build up gradually with repetitive activity. Adhesions can form, affecting the elasticity within that particular area of the muscle and making muscles vulnerable to further microtrauma. This process results in fibrotic changes in the muscle.
As function deteriorates in a small part of the muscle, it can create imbalance within a functional muscle unit (a group of muscles working together). As the condition builds up gradually, it may develop unnoticed in the early stages. Increased tension can then put excessive stress on adjoining structures such as the tendons, which can become more vulnerable to acute trauma. Biomechanical alterations develop as natural movement patterns compensate. In the long run, the overuse syndrome can lead to many problems, both locally and in other parts of the body. Several muscle dysfunctions can develop.
Massage is possibly the most effective way of identifying this type of problem. Palpation assessment identifies fibrotic changes in a muscle. This is the most important benefit of general preventive massage.
These areas should be treated in much the same way as any chronic muscle injury. Mechanical force is applied to break down scar tissue to improve flexibility and to realign tangled fibers.
Static positions, such as standing at attention in the military for long periods of time, put stress on specific tissues, causing microtrauma in a way similar to the active type of overuse, but from isometric overload instead of eccentric or concentric function. Lack of movement in the muscles also slows blood and lymph flow through the area, which can increase congestion and add to the problem.
Active Movements
General understanding of biomechanics is especially important for the massage professional who works with athletes. The assessment question “What do you want your body to do?” will result in answers such as “run,” “ride,” “throw,” “catch,” “jump,” “bend,” “rotate,” “lift,” and “press.” The massage professional needs to break down the movements of the activity, assess for soft tissue changes that interfere with these movements, and then identify massage applications that can support these movements. For example, in response to the assessment question, “What do you need to do that you are having problems with?” I will often hear something like “run backward” or “swing.” Then I will ask the athlete to show me, and while I observe the movements, I can begin to target the specific outcomes.
Perhaps the athlete says, “I can’t stand on my left foot with the same balance as my right foot” (which is important for many sport activities). I ask the athlete to stand on the right foot, and I observe and palpate to determine the “normal” activity that he or she can perform. This is a general assessment and treatment principle. The least affected movement pattern or structure becomes “normal” for evaluation and comparison purposes. Regardless of the situation, in practical application this works. I then ask the athlete to stand on the left foot, where the problem exists, and I compare it with the more normal function. Then I assess for the difference between the two—tissue texture and pliability, ROM, and firing patterns. Choices about what treatments to use are based on the assessment information.
The next part of the examination is divided into two sections. In active movement assessment, the massage therapist asks the client to perform movements in specific directions in all planes of movement. The squat assessment is particularly beneficial. In passive movement assessment, the massage therapist moves the client.
Injuries and dysfunctions of the musculoskeletal system are symptomatic when the injured area is actively moved. More complex conditions such as inflammation of the nervous system, systemic conditions such as heart disease, and pathologies such as tumors are not significantly affected by movement. If an area does not hurt at rest, but it does hurt with movement, soft tissue dysfunctions are indicated.
Remember that each individual joint movement pattern is part of an interconnected aspect of the neurologic and fascial coordination pattern of muscle movement called the kinetic chain. The support system involves the tensegric nature of the body’s connective design. Posture and movement dysfunctions identified in an individual joint pattern must be assessed and treated in broader terms of kinetic chain interactions, muscle tension/length relationships, and the effects of stress and strain on the entire system.
![]() Log on to your Evolve website to watch Video 10-1: Multiplanar Assessment (Functional Assessment).
Log on to your Evolve website to watch Video 10-1: Multiplanar Assessment (Functional Assessment).
Range of Motion
Remember that each person is unique, and many factors influence available range of motion. Just because a joint does not have the textbook range of motion (ROM) does not mean that what is displayed is abnormal. Abnormality is indicated by nonoptimal function. This can be seen as a limitation or an exaggeration in the “textbook normal” range of motion (Box 10-2).
ROM is measured in degrees. Joint movement is measured from the neutral line of anatomic position. Movement of a joint in the sagittal, frontal, or transverse plane is described as the number of degrees of flexion, extension, adduction, abduction, and internal and external rotation (Figure 10-6). For example, the elbow has approximately 150 degrees of flexion at the end range and 180 degrees of extension. Anything less than this is hypomobility, and anything more is considered hypermobility. Massage therapists typically estimate degrees of movement, and other professionals use specific equipment to obtain precise information. The normal ROM of joints is found in anatomy texts such as Mosby’s Essential Sciences for Therapeutic Massage.
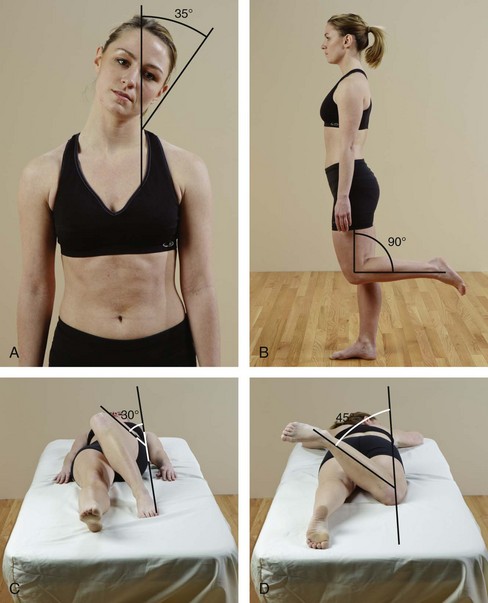
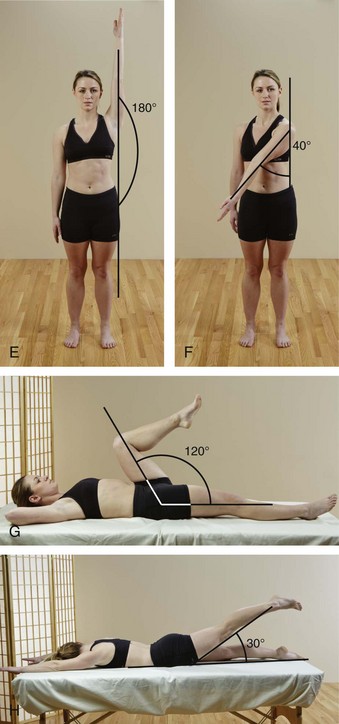
FIGURE 10-6 Examples of approximate degrees of movement. A, 35 degrees of lateral flexion. B, 90 degrees of knee flexion. C, 30 degrees of internal hip rotation. D, 45 degrees of external hip rotation.
E, 180 degrees of shoulder abduction. F, 40 degrees of horizontal shoulder adduction. G, 120 degrees of hip flexion. H, 30 degrees of hip hyperextension.
Each movement pattern (e.g., flexion and extension of the elbow and knee, circumduction and rotation of the shoulder and hip, movement of the trunk and neck) is assessed in sequential positioning in each area of all available movement patterns, testing for strength, range, and ease of movement. Functional assessment is the combination of all previously described assessments.
Range of motion is assessed through joint movement.
When active joint movement is performed, the client moves the joint through the planes of motion that are normal for that joint. Any pain, crepitus, or limitation that is present during the action should be reported. This assessment identifies what the client is willing or able to do.
Passive joint movement is performed when the massage therapist moves the joint passively through the planes of motion that are normal for the joint. The assessment identifies limited (hypomobility) or excessive movement (hypermobility) of the joint.
Passive joint movement is done carefully and gently to allow the client to fully relax the muscles while the assessment is performed. The client reports the point at which pain or bind, if present, occurs. The massage therapist stops the motion at the point of pain or bind, unless assessing for joint end-feel. Then a tiny increase in resistance is used to assess the quality of movement just past the bind. Passive joint movement assessment provides information about the joint capsule and ligaments and other restricting mechanisms, such as myofascial soft tissue.
![]() Log on to your Evolve website to watch Video 10-2: Passive Joint Movement (Range of Motion).
Log on to your Evolve website to watch Video 10-2: Passive Joint Movement (Range of Motion).
Basic Orthopedic Tests
The main reason for orthopedic tests is to assess for bone, joint, ligament, and tendon injury. Orthopedic tests also identify impingement areas. The most common structures impinged are nerves, blood vessels, and tendons, and occasionally muscles. Performing orthopedic tests can determine whether or not a referral is necessary. Even if you do not perform orthopedic assessment as part of the massage assessment process, it is likely that a client will tell you that he or she had a positive result when assessed by another health professional such as an athletic trainer, physical therapist, chiropractic physician, or medical or osteopathic doctor.
Most orthopedic tests assess stress areas to be evaluated in an effort to evaluate pain, joint play, and muscle extensibility. Because of the strain involved during some orthopedic tests, care must be taken to avoid further injury. Before any orthopedic tests are conducted, an area must be free from fracture or neoplasm (an abnormal growth). Furthermore, any client with characteristics such as severe spasm, pain with unknown etiology (cause), or pain that wakes him or her up at night, should not be evaluated with orthopedic tests until a full medical evaluation can be completed to address these unexplained symptoms.
A positive test will reproduce the client’s symptoms. If the client does not want you to perform the test, this is called an apprehension sign. Additional positive signs are change in stability of the joint and changes in pulses.
Assessment Using Joint Movement
The ROM of a joint is measured in degrees. A full circle is 360 degrees. A flat horizontal line is 180 degrees. Two perpendicular lines (as in the shape of a capital “L”) create a 90-degree angle. When the ROM of a joint allows 0 to 90 degrees of flexion, anything less is hypomobile and anything more is hypermobile. A great degree of variability exists among individuals as to actual normal ROM. The degrees provided are general guidelines. ROM is measured from the anatomic position. Anatomic position is considered 0 degrees of motion, regardless of whether the client is standing, supine, or side-lying.
Decreased ROM may result from pain or changes in joint position, or from soft tissue bind. If loss of motion is not a result of pain, more information is needed to determine whether lack of motion is caused by adhesions in the joint capsule, muscle guarding, joint degeneration, or other factors.
Increased ROM that is significantly different from the other side indicates moderate to severe injury to the ligaments, joint capsule, or both. Increased ROM on both sides compared with normal anatomic ROM suggests a generalized hypermobility syndrome and potential instability in the joints.
During actual movement assessment, the following categories are noted by the massage therapist:
Range of motion (ROM). Is the motion normal, decreased, increased? Determining normal ROM is more complex than it might seem. You need to consider the client’s age and sex, sport type, and muscle texture. ROM is lessened as we age. Women typically have greater ROM than men. If the complaint is in the extremities, begin with the noninvolved side, and always compare both sides. The less involved side becomes the “normal side” for comparison.
Limits to joint movement. Joints have various degrees of ROM. Anatomic, physiologic, and pathologic barriers to motion exist. Anatomic barriers are determined by the shape and fit of bones at the joint. The anatomic barrier is seldom reached because the possibility of injury is greatest in this position. Instead the body protects the joint by establishing physiologic barriers.
Physiologic barriers are the result of limits in ROM imposed by protective nerve and sensory function to support optimal function. An adaptation in the physiologic barrier so that the protective function limits instead of supports optimal functioning is called a pathologic barrier. Pathologic barriers often are manifested as stiffness, pain, or a “catch.”
When using joint movement techniques, remain within the physiologic barriers. If a pathologic barrier limits motion, use massage techniques to gently and slowly encourage the joint to increase the limits of ROM to the physiologic barrier.
The stretch on the soft tissues, such as muscles, tendons, fasciae, and ligaments, and the arrangement of the joint surfaces determine the ROM of the joint and therefore the joint’s normal end-feel.
Overpressure is the term used when the massage therapist gradually applies more pressure when the end of the available passive range of joint motion has been reached. The sensation transmitted to the therapist’s hands by tissue resistance at the end of the available range is the end-feel of a joint.
Types of End-Feel
Soft tissue approximation end-feel occurs when the full ROM of the joint is restricted by normal muscle bulk; it is painless and has a feeling of soft compression. Muscular/ tissue stretch end-feel occurs at the extremes of muscle stretch, as in the hamstrings during a straight leg raise; it has a feeling of increasing tension, springiness, or elasticity. Capsular stretch, or leathery, end-feel occurs when the joint capsule is stretched at the end of its normal range, such as with external rotation of the glenohumeral joint; it is painless and has the sensation of stretching a piece of leather. Bony, or hard, end-feel occurs when bone contacts bone at the end of normal range, as in extension of the elbow; it is abrupt and hard.
Abnormal End-Feel
Many types of abnormal end-feel have been identified. Empty end-feel occurs when there is no physical restriction to movement except the pain expressed by the client. Muscle spasm end-feel occurs when passive movement stops abruptly because of pain; there may be a springy rebound from reflexive muscle spasm. Boggy end-feel occurs when edema is present; it has a mushy, soft quality. Springy block, or internal derangement, end-feel is a springy or rebounding sensation in a noncapsular pattern; this indicates loose cartilage or meniscal tissue within the joint. Capsular stretch (leathery) end-feel that occurs before normal range indicates capsular fibrosis with no inflammation. Bony (hard) end-feel that occurs before normal range indicates bony changes or degenerative joint disease or malunion of a joint after a fracture.
An empty end-feel with no bind or stability indicates a seriously damaged joint, and referral is required.
Analysis of Active Movement
If active movement is painful, ask the client to describe its location, quality, and severity. The three stages of healing that elicit pain at different ranges of the movement are as follows:
1. Acute conditions yield pain before the normal ROM.
2. Subacute conditions give pain at the end of the normal range.
3. Chronic conditions may elicit pain with slight overpressure at the end of active or passive motion.
Pain with passive motion at different ranges of the movement indicates a stage of healing that is the same as for active motion.
Active and passive ROM can identify limits of movement. If an empty capsular or hard end-feel is identified, the joint is damaged. Referral is needed for acute conditions. ROM limited by muscle contraction may indicate an underlying problem with joint laxity, and caution is indicated before muscle guarding is reduced. Proceed slowly until a balance between increased ROM and maintenance of joint stability is achieved. If joint stability is reduced, the client usually experiences pain in the joint for a day or two after the massage. Simple edema around a joint is managed with lymphatic drain. Any unexplained edema should be referred for diagnosis.
ROM should improve as the client’s tissues normalize with general massage. Progressive mobilization in ROM is an indication of improved function. Never force an increase in ROM. Instead, allow it to be a natural outcome of effective massage application.
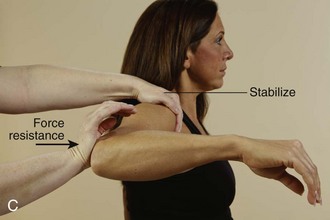
Muscle Strength Assessment
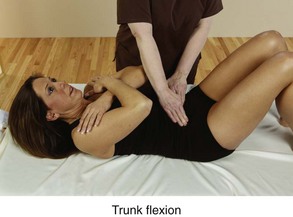
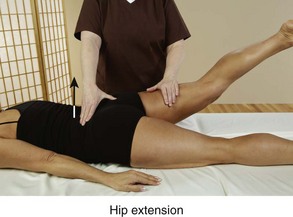
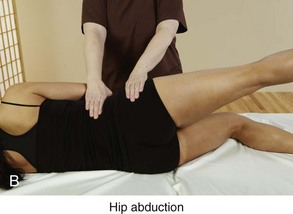
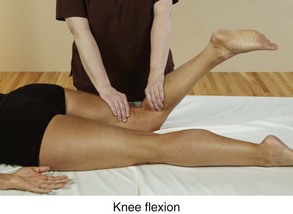
Muscle strength assessment is performed by applying resistance to a specific group of muscles. Resistance (pressure against) applied to the muscles is focused at the end of the lever system (Figure 10-7).
For example, when the function of the shoulder is assessed, resistance is focused at the distal end of the humerus, not at the wrist. When extension of the hip is assessed, resistance is applied at the end of the femur. When flexion of the knee is assessed, resistance is applied at the distal end of the tibia.
Resistance is applied slowly, smoothly, and firmly at an appropriate intensity as determined by the size of the muscle mass. Stabilization is essential to assess movement patterns accurately. Only the area assessed is allowed to move. Movement in any other part of the body must be stabilized. A stabilizing force is usually applied by the massage therapist. As one hand applies resistance, the other provides stabilization. Sometimes the client can provide stabilization by holding onto the massage table. Some methods use straps to provide stabilization. The easiest way to identify the area to be stabilized is to move the area to be assessed through the ROM. At the end of the range, some other part of the body begins to move; this is the area of stabilization. Return the body to a neutral position. Provide appropriate stabilization to the area identified and begin the assessment procedure (Figure 10-8).
During assessments, muscles should be able to hold against appropriate resistance without strain or pain from the pressure, and without recruiting or using other muscles. Appropriate resistance is applied slowly and steadily and with just enough force to induce muscles to respond to the stimulus. Large muscle groups require greater force than small ones. The position should be easy to assume and comfortable to maintain for 10 to 30 seconds. Contraindications to this type of assessment include joint and disk dysfunction, acute pain, recent trauma, and inflammation.
When a movement pattern is evaluated, two types of information are obtained in one functional assessment.
First, when a jointed area moves into flexion and the joint angle is decreased, the prime mover and synergists concentrically contract, the antagonists eccentrically function while lengthening, and the fixators isometrically contract and stabilize. Body-wide stabilization patterns also come into play to assist in allowing the motion. During assessment, resistance can be applied to load the prime mover groups, and synergists to assess for neurologic function of strength and, to a lesser degree, endurance, as the contraction is held for a period of time. At the same time, the antagonist pattern of the tissues that are lengthened during positioning for the functional assessment can be assessed for increased tension patterns or connective tissue shortening. Dysfunction shows itself in limited ROM by restricting the movement pattern. Therefore, when a jointed area is placed into flexion, the extensors are assessed for increased tension or shortening. When the jointed area moves into extension, the opposite becomes the case. The same holds for adduction and abduction, internal and external rotation, plantar flexion and dorsiflexion, and so on.
![]() For a comprehensive strength testing sequence, see the Evolve website.
For a comprehensive strength testing sequence, see the Evolve website.
Interpreting Muscle-Specific Testing Findings
Muscle strength testing determines a muscle’s force of concentric contraction. The preferred method is to isolate the muscle or muscle group by positioning the muscle with its attachment points as close together as possible. The muscle or muscle group being tested should be isolated as specifically as possible.
The client holds or maintains the contracted position of the muscle isolation while the therapist slowly and evenly applies counterpressure to pull or push the muscle out of its isolated position. The massage therapist must use sufficient force to recruit a full response by the muscles being tested but not enough to recruit other muscles in the body. The client should not hold his or her breath during assessment. If strength testing is done this way, there is little chance that the therapist will injure the client. As with all assessment, it is necessary to compare the muscle tested with a similar area—usually the same muscle group on the opposite side.
Another muscle testing method is to compare a muscle group’s strength with its antagonist pattern. The body is designed so that the flexor, internal rotator, and adductor muscles are about 25% to 30% stronger than the extensor, external rotator, and abductor muscles. It is also designed so that flexors and adductors usually work against gravity to move a joint. The main purposes of extensors and abductors are to restrain and control the movement of flexor and adductor muscles and to return the joint to a neutral position. Less strength is required because gravity is assisting the function. A third form is strength testing to assess for facilitator and inhibitor patterns during gait function. ![]()
Strength testing should reveal a difference in the pattern between flexors, internal rotators, and adductors, and between extensors, external rotators, and abductors in an agonist/antagonist pattern. These groups should not be equally strong. Flexors, internal rotators, and adductors should show greater muscle strength than extensors, external rotators, and abductors (Box 10-3).
Muscle strength testing indicates the following possible findings:
• A strong and painless contraction indicates a normal structure.
• A painful but strong contraction indicates an injury or dysfunction in the tested muscle-tendon-periosteal unit.
• A weak and painless contraction may be caused by one or more of the following situations:
• The muscle is inhibited owing to a hypertonic antagonist pattern.
• The muscle is inhibited owing to dysfunction or injury to adjacent joint structures.
• A spinal nerve condition is causing impingement on or irritation of the motor nerve and weakness in the muscles innervated by that nerve.
• The muscle is deconditioned owing to disuse as a result of previous injury or disease.
• The length-tension relationship is long.
Postural and Phasic Muscles
Postural (stabilizer) and phasic (mover) muscles are made up of different kinds of muscle fibers. Postural muscles have a higher percentage of slow-twitch red fibers, which can hold a contraction for a long time before fatiguing. Phasic muscles have a higher percentage of fast-twitch white fibers, which contract quickly but tire easily. These two types of muscle develop different types of dysfunction and are tested differently.
Postural Muscles
Postural (stabilizer) muscles are relatively slow to respond compared with phasic muscles. They do not produce bursts of strength if asked to respond quickly, and they may cramp. They are the deliberate, slow, steady muscles that require time to respond. Using the analogy of the tortoise and the hare, these muscles are the tortoise. Inefficient neurologic patterns, muscle tension, reorganization of connective tissue with fibrotic changes, and trigger points are common in postural muscles.
If posture is not balanced, postural muscles must function more like ligaments and bones. When this happens, additional connective tissue develops in the muscle to provide the ability to stabilize the body in gravity. The problem is that the connective tissue freezes the body in the position because, unlike muscle, which can actively contract and lengthen, connective tissue is static.
Postural muscles tend to shorten and increase in tension when under a strain-tension-length relationship. This information is important when attempting to assess which muscles are tense and short, and therefore in need of lengthening, and which groups of muscle are apt to develop connective tissue changes and require stretching. Connective tissue shortening is dealt with mechanically through forms of stretch. Hypertension of concentric contraction muscles is dealt with through muscle energy methods and reflexive lengthening procedures.
Phasic Muscles
Phasic (mover) muscles jump into action quickly and tire quickly. It is more common to find musculotendinous junction problems in phasic muscles. The four most common problems are microtearing of muscle fibers at the tendon, inflamed tendons (tendonitis), tendons adhering to underlying tissue, and bursitis.
Phasic muscles usually weaken in response to postural muscle shortening. Sometimes the weakened muscles also shorten. This shortening allows the weak muscle to retain the same contraction power on the joint. It is important not to confuse this condition with hypertense muscles. These muscles are inhibited and weak.
Phasic muscles occasionally become overly tense and short. This almost always results from some sort of repetitive behavior and is a common problem in athletes. Phasic muscles also become short in response to a sudden posture change that causes the muscles to assist the postural muscles in maintaining balance. These common, inappropriate muscle patterns often result from an unexpected fall or near-fall, an automobile accident, or some other trauma. Basic massage methods discussed in this text can be used to reset and retrain out-of-sync muscles.
Kinetic Chain Assessment of Posture
Consider the body as a circular form divided into four quadrants: a front, a back, a right side, and a left side, with divisions on the sagittal and frontal planes; the body must be balanced in three dimensions to withstand the forces of gravity.
The body moves and is balanced in gravity in the following transverse plane areas that easily allow movement: atlas; C6 and C7 vertebrae; T12 and L1 vertebrae (the thoracolumbar junction); L4, L5, and S1 vertebrae (the sacrolumbar junction); and hips, knees, and ankles (Figure 10-9). If a postural distortion exists in any of the four quadrants or within one of the jointed areas, the entire balance mechanism must be adjusted. This occurs as a pinball-like effect that jumps front to back and side to side in the soft tissue between the movement lines (see Figure 10-9).
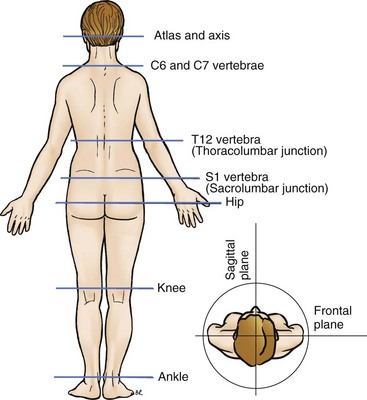
FIGURE 10-9 Quadrants and movement segments. (From Fritz S: Mosby’s fundamentals of therapeutic massage, ed 3, St Louis, 2004, Mosby.)
To gain an understanding of postural balance, use a pole of some type (a broom handle without the broom portion will work). Tie a string around the pole. Now, try to balance the pole on its end with the string. Note that you work opposite the pattern when trying to counter the fall pattern of the pole. If the pole tends to fall forward and to the left, you apply a counterforce back and to the right.
This is also what the body does if part of it moves off the balance line. The body is made up of many different poles stacked on top of one another. The poles stack at each of the movement segments. Muscles between the movement segments must be three-dimensionally balanced in all four quadrants to support the pole in that area. Each area needs to be balanced. If one pole area tips a bit to the right, the body compensates by tipping the adjacent pole areas (above and/or below) to the left. If a pole area is tipped forward, adjacent poles are tipped back. A chain reaction occurs, such that when compensating poles tip back, their adjacent areas must counterbalance the action by tipping forward. This is how body-wide compensation patterns occur.
Whether the pole areas sit nicely on top of each other with evenly distributed muscle action or whether they are tipped in various positions and counterbalanced by compensatory muscle actions, the body remains balanced in gravity. However, the “tippy pole” pattern is much more inefficient than the “balanced pole pattern” (Figure 10-10).
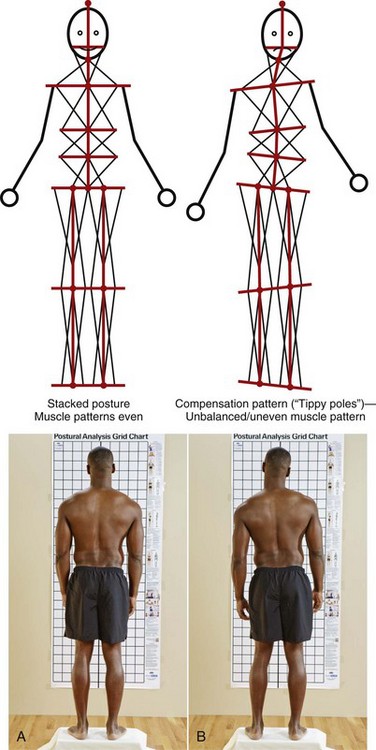
FIGURE 10-10 Posture balance and imbalance. Stacked poles (A) versus tippy pole (B) postural influences on the body. (From Fritz S: Mosby’s fundamentals of therapeutic massage, ed 3, St Louis, 2004, Mosby.)
Intervention plans attempt to normalize the balance process by relaxing the tension pattern in overly tight and short areas, strengthening muscles in corresponding taut and long but weak areas, and allowing the poles to straighten out. If a pole is permanently tippy, as with scoliosis or kyphosis, intervention plans attempt to support appropriate compensation patterns and prevent them from increasing beyond what is necessary for postural balance.
Muscle imbalance, discovered by observation, by palpation, and through muscle testing procedures, often indicates how the body is compensating for postural and movement imbalances. Muscle testing also can locate the main muscle problems. When the primary dysfunctional group of muscles is concentrically contracted against resistance, the main compensatory patterns are activated, and the other body compensation patterns are activated and exaggerated. The massage professional must then become a detective, looking for clues to unwind the pattern by concentrating on methods that restore symmetry of function.
A major muscle problem is overly tense muscles. If these muscles can be relaxed, lengthened, and, if necessary, stretched to activate connective tissue changes, the rest of the dysfunctional pattern often resolves.
If the extensors and abductors are stronger than the flexors and adductors, major postural imbalance and postural distortion result. Similarly, if the extensors and abductors are too weak to balance the other movement patterns, the body curls into itself, and nothing works properly.
If gait and kinetic chain patterns are inefficient, more energy is required for movement, and fatigue and pain can result.
Shortened postural (stabilizer) muscles must be lengthened and then stretched. This takes time and uses all the massage practitioner’s technical skills. Because of the fiber configuration of the muscle tissue (slow-twitch red fibers or fast-twitch white fibers), techniques must be sufficiently intense and must be applied long enough to allow the muscle to respond.
Shortened and weak phasic muscles must first be lengthened and stretched. Eventually, strengthening techniques and exercises will be needed. Long and weak muscles need therapeutic exercise. If the hypertense phasic muscle pattern is caused by repetitive use, the muscles can be normalized with muscle energy techniques and then lengthened. Overly tense muscles often increase in size (hypertrophy). Muscle tissue that has undergone hypertrophy begins to return to normal if it is not used for the activity. The client must reduce the activity of that muscle group until balance is restored, which usually takes about 4 weeks. Athletes often display this pattern and very likely will resist complete inactivity. A reduced activity level and a more balanced exercise program, combined with flexibility training, can be beneficial for them. Refer these individuals to appropriate training and coaching professionals, if indicated.
People usually complain of problems in the tight but long eccentrically functioning and inhibited muscle areas. Massage in these areas makes the symptoms worse because massage further lengthens the area. Instead, identify the shortened tissues and apply massage to lengthen and stretch tense areas. Assessment must identify the concentrically contracted shortened areas so that correction can be applied.
Muscle Firing Patterns
![]() Log on to your Evolve website to watch Video 10-3: Muscle Activation Sequences (Muscle Firing Patterns).
Log on to your Evolve website to watch Video 10-3: Muscle Activation Sequences (Muscle Firing Patterns).
A muscle firing pattern (or muscle activation sequence) is the sequence of muscle contraction involvement with agonist and synergist that best produces joint motion. Muscles also contract, or fire, in a neurologic sequence to produce coordinated movement. If the muscle firing pattern is disrupted, and if muscles fire out of sequence or do not contract when they are supposed to, labored movement and postural strain result. Firing patterns can be assessed by initiating a particular sequence of joint movements and palpating for muscle activity to determine which muscle is responding to the movement.
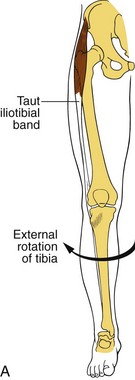
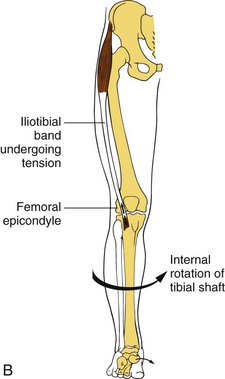
The central nervous system recruits appropriate muscles in specific muscle activation sequences to generate the appropriate muscle function of acceleration, deceleration, or stability. If these firing patterns are abnormal, with the synergist becoming dominant, efficient movement is compromised and the joint position is strained. The general activation sequence is (1) prime mover, (2) stabilizer, and (3) synergist. If the stabilizer has to also move the area (acceleration) or control movement (deceleration), it typically becomes short and tight. If the synergist fires before the prime mover, the movement is awkward and labored.
If one muscle is tight and short, reciprocal inhibition occurs. Reciprocal inhibition exists when a tight muscle decreases nervous stimulation of its functional antagonist, causing it to reduce activity. For example, a tight and short psoas decreases (inhibits) the function of the gluteus maximus. The activation and force production of the prime mover (gluteus maximus) are decreased, leading to compensation and substitution by the synergists (hamstrings) and stabilizers (erector spinae), creating an altered firing pattern.
The most common firing pattern dysfunction is synergistic dominance, in which a synergist compensates for a prime mover to produce the movement. For example, if a client has a weak gluteus medius, then synergists (the tensor fascia lata, adductor complex, and quadratus lumborum) become dominant to compensate for the weakness. This alters normal joint alignment, which further alters the normal length-tension relationships of the muscles around the joint. See Box 10-4 for the most commonly used assessment procedures and interventions for altered firing patterns.
Each jointed area has a movement muscle activation sequence. The movement is a product of the entire mechanism, including the following:
• Bones, joints, and ligaments
• Capsular components and design
• Tendons, muscle shapes, and fiber types
• Interlinked fascial networks, nerve distribution, and myotatic units of prime movers
• Antagonists, synergists, and fixators
• Neurologic kinetic chain interactions
• Body-wide influence of reflexes, including positional and righting reflexes of vision and the inner ear and gait reflex
Assessment of a movement pattern as normal indicates that all parts are functioning in a well-orchestrated manner. When a dysfunction is identified, causal factors can arise from any one or a combination of these elements. Often a multidisciplinary diagnosis is necessary to identify clearly the interconnected nature of the pathologic condition.
Inappropriate firing patterns can be addressed by inhibiting the muscles that are contracting out of sequence and stimulating the appropriate muscles to fire. Compression to the muscle belly effectively inhibits a muscle. Tapotement is a good technique for stimulating muscles. If the problem does not normalize easily, referral to an exercise professional may be indicated.
Gait Assessment
![]() Log on to your Evolve website to watch Video 10-4: Gait Assessment.
Log on to your Evolve website to watch Video 10-4: Gait Assessment.
Understanding the basic body movements of walking helps the massage therapist recognize dysfunctional and inefficient gait patterns.
Disruption of gait reflexes creates the potential for many problems. Common gait problems include a functional short leg caused by muscle shortening, tight neck and shoulder muscles, aching feet, and fatigue. The massage therapist must understand biomechanics, including posture, interaction of joint functions, and gait, and must expand that knowledge to the demands of sport performance.
This is especially important in rehabilitation progress in which walking is the goal or part of the program. It is important to observe the client from front, back, and both sides. To begin, the massage practitioner should watch the client walk, noticing the heel-to-toe foot placement. The toes should point directly forward with each step.
Observe the upper body. It should be relaxed and fairly symmetric. The head should face forward with the eyes level with the horizontal plane. There is a natural arm swing that is opposite to the leg swing. The arm swing begins at the shoulder joint. On each step, the left arm moves forward as the right leg moves forward and then vice versa. This pattern provides balance. The rhythm and pace of the arm and leg swing should be similar. Increased walking speed increases the speed of the arm swing. The length of the stride determines the arc of the arm swing.
Observe the client walking, and note his or her general appearance. The optimal walking pattern is as follows:
1. Head and trunk are vertical, with the eyes easily maintaining forward position and level with the horizontal plane; shoulders are level.
2. Arms swing freely opposite the leg swing, allowing the shoulder girdle to rotate opposite the pelvic girdle.
3. Step length and step timing are even.
4. The body oscillates vertically with each step.
5. The entire body moves rhythmically with each step.
6. At the heel strike, the foot is approximately at a right angle to the leg.
7. The knee is extended but not locked.
8. The body weight is shifted forward into the stance phase.
9. At push-off, the foot is strongly plantar-flexed, with defined hyperextension of the metatarsophalangeal joints of the toes.
10. During the leg swing, the foot easily clears the floor with good alignment, and the rhythm of movement remains unchanged.
11. The heel contacts the floor first.
12. The weight then rolls to the outside of the arch.
13. The arch flattens slightly in response to the weight load.
14. The weight then is shifted to the ball of the foot in preparation for the spring-off from the toes and shifting of weight to the other foot.
During walking, the pelvis moves slightly in a side-lying figure-eight pattern. Movements that make up this sequence are transverse, medial, and lateral rotation. The stability and mobility of the sacroiliac joints play very important roles in this alternating side figure-eight movement. If these joints are not functioning properly, the entire gait is disrupted. The sacroiliac joint is one of the few joints in the body that is not directly affected by muscles that cross the joint. It is a large joint, and bony contact between sacrum and ilium is broad. It is common for the rocking of this joint to be disrupted (Figure 10-11).
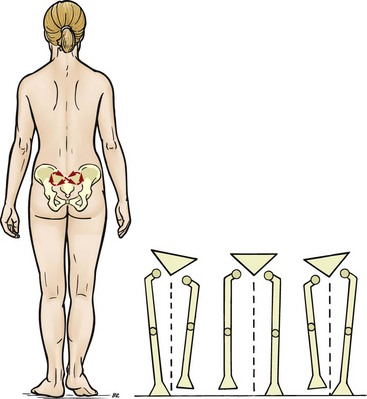
FIGURE 10-11 The mechanism of the slight rocking movement of the sacroiliac joint. (From Fritz S: Mosby’s fundamentals of therapeutic massage, ed 5, St Louis, 2013, Mosby.)
The hips rotate in a slightly oval pattern, beginning with a medial rotation during the leg swing and heel strike, followed by a lateral rotation through the push-off. The knees move in a flexion and extension pattern opposite each other. The extension phase never reaches enough extension to initiate the normal knee lock pattern that is used in standing. The ankles rotate in an arc around the heel at heel strike and around a center in the forefoot at push-off. Maximal dorsiflexion at the end of the stance phase and maximal plantar flexion at the end of push-off are necessary.
When assessing gait, observing for areas of the body that do not move efficiently during walking is a good means of detecting dysfunctional areas. Pain causes the body to tighten and alters the normal relaxed flow of walking. Muscle weakness and shortening interfere with neurologic control of agonist (prime mover) and antagonist muscle action. Hypomobility (limitation of joint movement) and hypermobility (laxity) result in protective muscle contraction.
If the situation becomes chronic, both muscle shortening and muscle weakness result. Changes in the soft tissue, including all connective tissue elements of the tendons, ligaments, and fascial sheaths, restrict the normal action of muscles. Connective tissue usually shortens and becomes less pliable.
Amputation disrupts the body’s normal diagonal balance. Obviously, any amputation of the lower limb disturbs the walking pattern. What is not so obvious is that amputation of any part of the upper limb affects the counterbalance movement of the arm swing during walking. The rest of the body must compensate for the loss. Loss of any of the toes greatly affects the postural information sent to the brain from the feet.
It is possible to have soft tissue dysfunction without joint involvement. Any change in the tissue around a joint has a direct effect on joint function. Changes in joint function eventually cause problems with the joint. Any dysfunction of the joint immediately involves the surrounding muscles and other soft tissue.
Disruption of gait demands that the body compensate by shifting movement patterns and posture. Because of this, all dysfunctional patterns are whole body phenomena. Working only on the symptomatic area is ineffective and offers only limited relief. Therapeutic massage with a whole body focus is extremely valuable in dealing with gait dysfunction. Corrective measures include normalizing muscle firing patterns and gait reflex patterns (see Box 10-4).
![]() The Evolve website provides step-by-step visual instructions for performing gait testing assessments, findings, and intervention suggestions.
The Evolve website provides step-by-step visual instructions for performing gait testing assessments, findings, and intervention suggestions.
Interpreting Gait Assessment Findings
When interpreting the information gathered from gait assessment, the massage practitioner should focus on areas that do not move easily when the client walks and areas that move too much. Areas that do not move are restricted; areas that move too much are compensating for inefficient function. By releasing the restrictions through massage and reeducating the reflexes through neuromuscular work and exercise, the practitioner can help the client improve the gait pattern.
The techniques followed are similar to those for postural corrections. The shortened and restricted areas are softened with massage, and then the neuromuscular mechanism is reset with muscle energy techniques, muscle lengthening, stretching, and normalizing of firing patterns.
The client should be taught slow lengthening and stretching procedures. After stimulating the muscles in weakened areas, the practitioner can refer the client for strengthening exercises. The therapist must be sure that the adaptation methods are built into the context of a complete massage rather than spot work on isolated parts of the body. Suggestions can be made to the client to evaluate factors that may contribute to these adaptations, such as posture, footwear, chairs, tables, beds, clothing, workstations, physical tasks (e.g., shoveling), and repetitive exercise patterns.
Sacroiliac Joint Function
![]() Log on to your Evolve website to watch Video 10-5: Correction Methods for Gait Assessment and/or Muscle Firing Patterns.
Log on to your Evolve website to watch Video 10-5: Correction Methods for Gait Assessment and/or Muscle Firing Patterns.
Proper functioning of the sacroiliac (SI) joint is an important factor in walking patterns. Because sacroiliac joint movement has no direct muscular component, it is difficult to use any kind of muscle energy lengthening when working with this joint. The SI joint is embedded deep in supporting ligaments. To keep surrounding ligaments pliable, direct and specific, connective tissue techniques are indicated unless the joint is hypermobile. If that is the case, external bracing combined with rehabilitative movement may be indicated. Sometimes the ligaments restabilize the area. Stabilization of the jointed area should be interspersed with massage and gentle stretching to ensure that the ligaments remain pliable and do not adhere to each other. This process takes time.
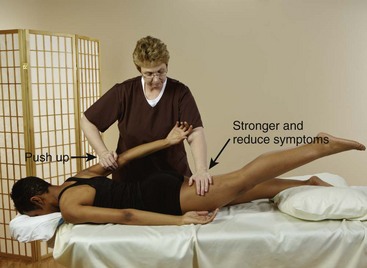
To assess for possible SI joint involvement, apply deep broad-based compression over the joint (Figure 10-12). If symptoms increase, SI joint dysfunction is indicated. Another assessment is to have the client stand on one foot and then extend the trunk. This loads the SI joint and would increase symptoms of SI joint dysfunction. Have the client lie prone and extend the hip. Then apply resistance to the opposite arm and have the client push against the resistance by extending the shoulder and arm (Figure 10-13), and then, while doing this, also extend the contralateral hip. If it is easier to lift and symptoms are relieved, SI joint function can be improved by exercise and massage, because force closure mechanisms are able to be addressed. If no improvement is noted, external bracing may help.
The diagnosis of specific joint problems and fitting for external bracing are outside the scope of practice for therapeutic massage, and the client must be referred to the appropriate professional.
Analysis of Muscle Testing and Gait Patterns
![]() Log on to your Evolve website to watch Video 10-6: Low Back Pain Assessment.
Log on to your Evolve website to watch Video 10-6: Low Back Pain Assessment.
It is important to consider the pattern of muscle interactions that occurs with walking. Remember that gait has a certain pattern for efficient movement. For example, if the left leg is extended for the heel strike, the right arm also is extended. This results in activation of flexors of both the arm and the leg and inhibition of the extensors. It is common to find a strength imbalance in this gait pattern. One muscle out of sequence with the others can set up tense (too strong) or inhibited (weak) muscle imbalances. Whenever a muscle contracts with too much force, it overpowers the antagonist group, resulting in inhibited muscle function. Imbalances can occur anywhere in the pattern.
Strength muscle testing should reveal that the flexor and adductor muscles of the right arm activate, facilitate, and coordinate with the flexors and adductors of the left leg. The opposite is also true: left arm flexors and adductors activate, facilitate, and coordinate with the right leg flexors and adductors. Extensors and abductors in the limbs coordinate in a similar fashion.
If the flexors of the left leg are activated, as occurs during strength testing, the flexors and adductors of the right arm should be facilitated and should be strong in strength testing. The flexors and adductors of the right leg and left arm should be inhibited and should be weak in strength testing. Also, the extensors and abductors in the right arm and left leg should be inhibited. All associated patterns follow suit (i.e., activation of the right arm flexor pattern facilitates the left leg flexor pattern and inhibits left arm and right leg flexor muscles while facilitating extensors and abductors). In a similar way, activation of the adductors of the right leg facilitates the adductors of the left arm and inhibits the abductors of the left leg and right arm. The other adductor/abductor patterns follow the same interaction pattern.
All these patterns are associated with gait mechanisms and reflexes. If any pattern is out of sync, gait, posture, and efficient function are disrupted. ![]()
Gait Muscle Testing as an Intervention Tool
An understanding of gait provides a powerful intervention tool. For example, a person trips and strains the left hip extensor muscles. Gait muscle testing reveals an imbalanced pattern by showing that the left hip extensor muscles are weak, whereas the flexors in the left hip and the right arm/shoulder are overly tense. The hip and the leg are sore and cannot be used for work, but the arm muscles are fine. By activating the extensors in the right shoulder and arm, movement of the left hip extensor muscles can be facilitated. By activating the flexors of the left arm, the flexors of the left hip are inhibited. This process may restore balance in the gait pattern. Many combinations are possible based on gait pattern and reflexes. Gait muscle testing provides the means of identifying these interactions.
Palpation Assessment
Palpation assessment is a major aspect of the massage. In any given massage, about 90% of the touching is also assessment developed as part of gliding, kneading, or joint movement. Palpation assessment makes contact with tissue but does not override it or encourage it to change. Palpation assessment is used to identify normal tissue and movement with deviations from the norm. The least affected area is the norm for comparison. The tissues the massage therapist should be able to distinguish are skin, superficial fascia, fascial sheaths, tendons, ligaments, blood vessels, muscle layers, and bone. Palpation also includes assessment for hot and cold and for various body rhythms, including breathing patterns and pulses.
Using palpation assessment, the massage therapist is able to:
• Differentiate between different types of tissue
• Distinguish differences of tissue texture and density in the same tissue types
• Palpate through the various tissue layers from superficial to deep
The acronym STAR or TART is used in osteopathic medicine to describe changes in tissue and movement that are assessable when dysfunction occurs (Chaitow, 2010):
If a client experiences pain during palpation, it is important to first check technique to make sure that palpation is not the cause of the pain. Pain in a particular area does not necessarily mean that there is a problem. Some areas of the body are naturally a little painful when deeply palpated. These points will be located on both sides of the body in the same area and are typically the locations of nerves. If tissues feel normal to the massage therapist but cause pain when palpated, compare them with the same areas on the other side of the body. If there is a difference, then there may be a problem; if they feel the same, there is no problem and the feeling is normal.
The American College of Rheumatology has developed a quantifiable method of assessing tissue tenderness. The response to palpatory stimulus is determined by observing pain behaviors, such as facial grimacing and signs of withdrawal. By comparing the painful sites with uninvolved body areas, it is possible to determine whether the response is due to increased physiologic activity. This same assessment process can be used to detect a change in pain perception at the same pressure. Instruments for gauging pressure, called algometers, can further objectify the assessment. A baseline of 4 kg of pressure is used (enough to blanch the tip of a thumbnail pressed on a table), and results are rated as follows:
• Grade I—Tenderness with no physical or verbal response
• Grade II—Tenderness with grimacing or flinching or both
There is no benefit in applying deep pressure to a small area because this shows only what those particular tissues feel like and gives no information about how they compare with surrounding tissues. Instead, it is necessary to palpate all tissues in the area to feel any textural changes. Damage can occur in soft tissue at any level. One mistake sometimes made during palpation assessment is to explore deeper and deeper into the tissues in an effort to find the problem, only to miss it because it is located more superficially. It is therefore necessary to vary the degree of pressure used, from fairly light to very deep, to assess all the different tissue layers. When palpating tissues around a joint, move the joint into different positions to access different surfaces of bones and soft tissues. Pressing into tissue and removing all the slack puts the tissue in tension. Normally, there is no pain with pressing into the soft tissue—only a sense of pressure.
• Normal: The soft tissue feels resilient and pliable, blanches when compressed, and then quickly returns to normal color. There is no abnormal movement or pain.
• Acute injury: The soft tissue feels boggy, warm, or hot. The client feels pain before tissue is palpated and can often point to the most painful area.
• Chronic condition: The soft tissue feels fibrous, thickened, stiff, and tight. Pain sensations are more dull and occur over a larger area.
The recommended sequence of applications of palpation is as follows:
Near-Touch Palpation
The first application of palpation does not involve touching the body. Near-touch palpation detects hot and cold areas and is best performed just off the skin using the back of the hand, because the back of the hand is very sensitive to heat. The general temperature of the area and any variations should be noted. Very sensitive cutaneous (skin) sensory receptors detect changes in air pressure and currents and movement of air. Being able to consciously detect these subtle sensations is an invaluable assessment tool.
Hot areas may be caused by inflammation, muscle spasm, hyperactivity, or increased surface circulation. When the focus of intervention is to cool down hot areas, one method is application of ice (see section on hydrotherapy). Another way to cool an area is to reduce muscle spasm and encourage more efficient blood flow in the surrounding areas.
Cold areas often are areas of diminished blood flow, increased connective tissue formation, or muscle flaccidity. Cold areas may have heat applied to them. Stimulation massage techniques increase muscle activity, thus heating up the area. Connective tissue approaches soften connective tissue, help restore space around the capillaries, and release histamine, a vasodilator, to increase circulation. These approaches can warm a cold area.
Palpation of the Skin Surface
The second application of palpation is very light stroking of the skin surface (Figure 10-14). First, determine whether the skin is dry or damp. Damp areas feel a little sticky, or the fingers drag. This light stroking causes the root hair plexus that senses light touch to respond. It is important to notice whether an area reacts with more “goose bumps” than other areas (pilomotor reflex). This is a good time to observe for color, especially blue or yellow coloration. The practitioner also should note and keep track of all moles and surface skin growths, pay attention to the quality and texture of the hair, and observe the shape and condition of the nails.
Palpation of the Skin Itself
Palpation of the skin itself is done through gentle, slight stretching of the skin in all directions, comparing the elasticity of these areas (Figure 10-15). The skin also can be palpated for surface texture. By applying light pressure to the skin surface, roughness or smoothness can be felt.


FIGURE 10-15 A, Skin stretching used to assess for elasticity. B, Skin that seems tight compared with surrounding skin may indicate dysfunctional areas.
Skin should be contained, hydrated, resilient, and elastic, and should have even and rich coloration. Skin that does not spring back into its original position after a slight pinch may be a sign of dehydration. The skin should have no blue, yellow, or red tinges. Blue coloration suggests lack of oxygen; yellow indicates liver problems, such as jaundice; and redness suggests fever, alcohol intake, trauma, or inflammation. Color changes are most noticeable in the lips, around the eyes, and under the nails.
Bruises must be noted and avoided during massage. If a client displays any hot red areas or red streaking, he or she should be referred to a physician immediately. This is especially important when symptoms are present in the lower leg because of the possibility of deep vein thrombosis (blood clot).
The skin should be watched carefully for changes in any moles or lumps. As massage professionals, we often spend more time touching and observing a person’s skin than anyone else, including the person being massaged. If we keep a keen eye out for changes and refer clients to physicians early, many skin problems can be treated before they become serious.
Depending on the area, the skin may be thick or thin. The skin of the face is thinner than the skin of the lower back. The appearance of the skin in each particular area, however, should be consistent. The skin loses its resilience and elasticity over areas of dysfunction. It is important to be able to recognize visceral referred pain areas in the skin (Figure 10-16). If changes occur to the skin in these areas, refer the client to a physician.
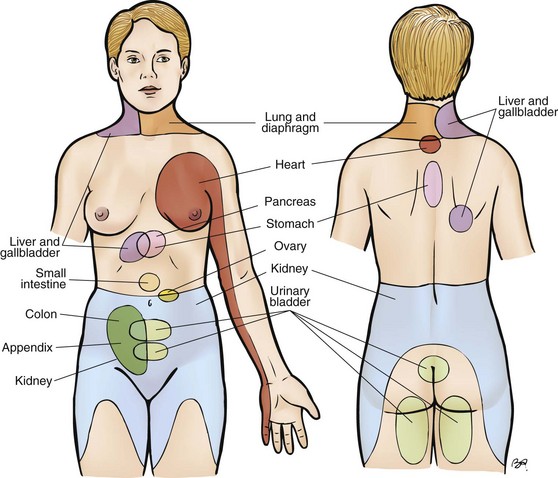
FIGURE 10-16 Referred pain. The diagram indicates cutaneous areas to which visceral pains may be referred. The massage professional encountering pain in these areas needs to refer the client to a physician for diagnosis to rule out visceral dysfunction. (From Fritz S: Mosby’s fundamentals of therapeutic massage, ed 5, St Louis, 2013, Mosby.)
The skin is a blood reservoir. At any given time it can hold 10% of available blood in the body. The connective tissue in the skin must be soft to allow the capillary system to expand to hold the blood. Histamine, which is released from mast cells found in the connective tissue of the superficial fascial layer, dilates the blood vessels. Histamine is also responsible for the sense of “warming and itching” in an area that has been massaged.
Damp areas on the skin are indications that the nervous system has been activated in that area. This small amount of perspiration is part of a sympathetic activation called a facilitated segment. Surface stroking with enough pressure to drag over the skin elicits a red response over the area of a hyperactive muscle. Deeper palpation of the area usually elicits a tender response. The small erector pili muscles attached to each hair are under the control of the sympathetic autonomic nervous system. Light fingertip stroking produces goose bumps over areas of nerve hyperactivity. All of these responses can indicate potential activity, such as trigger points in the layers of muscle under the indicated area.
The hair and nails are part of the integumentary system and reflect health conditions. The hair should be resilient and secure; hair loss should not be excessive when the scalp is massaged.
The nails should be smooth. Vertical ridges may indicate nutritional difficulties, and horizontal ridges may be signs of stress caused by changes in circulation that affect nail growth. Clubbed nails may also indicate circulation problems. The skin around the nails should be soft and free of hangnails.
It is important to continuously monitor the skin and associated structures. During times of stress, the epithelial tissues are affected first. Signs of prolonged stress, medication side effects, and pathologic conditions include hangnails, split skin around the lips and nails, mouth sores, hair loss, dry scaly skin, and excessively oily skin. This area is one of the best for assessing adaptive capacity. For example, slow wound healing would indicate strain in the system.
Palpation of the Skin and Superficial Connective Tissue
In palpation of both the skin and superficial connective tissue, a method such as skin rolling is used to further assess the texture of the skin by lifting it from the underlying fascial sheath (Figure 10-17) and measuring the skin fold, or comparing the two sides for symmetry (Figure 10-18). The skin should move evenly and should glide on the underlying tissues. Areas that are stuck, restricted, or too loose should be noted, as should any areas of the skin that become redder than surrounding areas.
Palpation of Superficial Connective Tissue Only
The fifth application of palpation is the superficial connective tissue, which separates and connects the skin and muscle tissue. It allows the skin to glide over the muscles during movement. This layer of tissue is found by applying compression until the fibers of the underlying muscle are felt. The pressure then should be lightened so that the muscle cannot be felt, but if the hand is moved, the skin also moves. This area feels a little like a very thin water balloon. The tissue should feel resilient and springy, like gelatin. Superficial fascia holds fluid. If surface edema is present, it is found in the superficial fascia. This water-binding quality gives this area the feel of a water balloon, but it should not feel boggy or soggy or show pitting edema (i.e., the dent from the pressure remains in the skin).
Methods of palpation that lift the skin, such as kneading and skin rolling, provide much information. Depending on the area of the body and the concentration of underlying connective tissue, the skin should lift and roll easily (Figure 10-19). Loosening of these areas is very beneficial, and the practitioner can achieve this by applying assessment methods (kneading and skin rolling) slowly and deliberately, allowing a shift in the tissues. A constant drag should be kept on the tissues, because both skin and superficial connective tissue are affected.

FIGURE 10-19 Use of kneading to assess the skin and superficial connective tissues by lifting of the tissues.
Any area that becomes redder than the surrounding tissue or that stays red longer than other areas is suspect for connective tissue changes (Figure 10-20). Usually, lifting and stretching (bend, shear, and torsion forces) of the reddened tissue or use of myofascial approaches (tension forces) will normalize these areas.
Palpation of Vessels and Lymph Nodes
The sixth application of palpation involves circulatory vessels and lymph nodes. Just above the muscle and still in the superficial connective tissue lie the more superficial blood vessels. These vessels are distinct and feel like soft tubes. Pulses can be palpated, but if pressure is too intense, the feel of the pulse is lost (Figure 10-21). Palpating for pulses helps detect this layer of tissue.
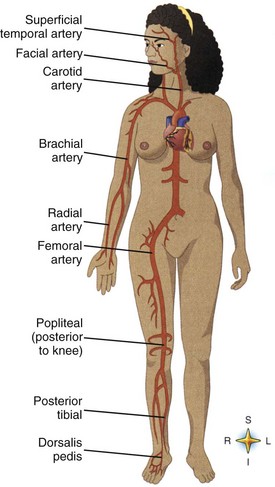
FIGURE 10-21 Pulse points. Each pulse point is named after the artery with which it is associated. (From Thibodeau GA, Patton KT: Anatomy and physiology, ed 5, St Louis, 2003, Mosby.)
In this same area are the more superficial lymph vessels and lymph nodes. Lymph nodes usually are located in joint areas and feel like small, soft “gelcaps.” The compression of the joint action assists in lymphatic flow. A client with enlarged lymph nodes should be referred to a medical professional for diagnosis. Very light, gentle palpation of lymph nodes and vessels is indicated in this circumstance.
Vessels should feel firm but pliable and supported. If bulging, mushiness, or constriction is noted in any areas, the massage therapist should refer the client to a physician.
Pulses should be compared by feeling for a strong, even, full-pumping action on both sides of the body. If differences are perceived, the massage practitioner should refer the client to a physician. Sometimes the differences in pulses can be attributed to soft tissue restriction of the artery or to a more serious condition that can be diagnosed by the physician. Refill of capillaries in nail beds after compression of the nail should take approximately 3 to 5 seconds and should be equal in all fingers.
Enlarged lymph nodes may indicate local or systemic infection or a more serious condition. The client should be referred to a physician immediately.
Palpation of Skeletal Muscles
The seventh application of palpation is skeletal muscle. Muscle is made up of contractile fibers embedded in connective tissue. Muscle has a distinct fiber direction. Its texture feels somewhat like corded fabric or fine rope. The area of the muscle that becomes the largest when the muscle is concentrically contracted is in the belly of the muscle. Where the muscle fibers end and the connective tissue continues, the tendon develops; this is called the musculotendinous junction.
It is a good practice activity to locate both of these areas for all surface muscles and for as many underlying ones as possible. Almost all muscular dysfunctions, such as trigger points or microscarring from minute muscle tears, are found at the musculotendinous junction or in the belly of the muscle. Most acupressure points, often classified as motor points, also are located in these areas.
Often three or more layers of muscle are present in an area. These layers are separated by fascia, and each muscle layer should slide over the one beneath it (Figure 10-22).




FIGURE 10-22 Sliding of muscle layers. A and B, Sliding rectus femoris. C and D, Sliding hamstrings.
Muscle tends to push up against palpating pressure when it is concentrically contracting. Having the client slowly move the joint that is affected can help in identifying the proper locations of muscles being assessed (Figure 10-23).


FIGURE 10-23 Specific palpation of a muscle. A, Place hand on target muscle belly (biceps brachii) and have client contract against resistance to initiate concentric action, making the tissues push up and feel hard. B, Example of specific palpation of hamstrings.
In palpation of the muscles, compressing systematically through each layer until the bone is felt is important (Figure 10-24). Pressure used to reach and palpate the deeper layers of muscle must travel from the superficial layers down to the deeper layers. To accomplish this, the compressive force must be even, broad-based, and slow. There should be no “poking” quality to the touch or abrupt pressure pushing through muscle layers, because the surface layers of muscle will tense up and guard, preventing access to deeper layers.




FIGURE 10-24 Massage applications systematically generate force through each tissue layer. This figure provides a graphic representation of force applied, which would begin with light superficial applications, progressing with increased pressure to the deepest layer. A, Surface. B, First muscle layer. C, Second muscle layer. D, Third muscle layer.
Palpation of each specific muscle area involves sliding each layer of muscle back and forth over the underlying layer to make sure there is no adherence between muscle layers.
Muscle layers usually run cross-grain to each other. The best example of this is the abdominal muscle group. Even in the arm and leg, where all muscles seem to run in the same direction, a diagonal crossing and spiraling of the muscle groups is evident.
Interpreting Skeletal Muscle Assessment Findings
Muscles can feel tense and ropy in both concentric (short) and eccentric (long) patterns. Therefore think of muscle functioning as short and tight, and long and tight.
Skeletal muscle is assessed both for texture and for function. It should be firm and pliable. Soft, spongy muscle or hard, dense muscle indicates connective tissue dysfunction. Muscle atrophy results in a muscle that feels smaller than normal. Hypertrophy results in a muscle that feels larger than normal. Application of appropriate techniques can normalize the connective tissue component of the muscle. Excessively strong or weak muscles can be caused by problems with neuromuscular control or imbalanced work or exercise demand. Weak muscles can be a result of wasting (atrophy) of the muscle fibers.
Tension can be felt in muscles that are concentrically short or eccentrically long. Tension that manifests in short muscles that are concentrically contracted results in tissue that feels hard and bunched. When muscles are tense from being pulled into an extension pattern, they feel like long, taut bundles with some contraction and shortened muscle fiber groups. Usually, flexors, adductors, and internal rotators become short, whereas extensors, abductors, and external rotators palpate tense but are long and have eccentric contraction patterns. Massage treatment most often first addresses the short concentrically contracted muscles to lengthen them, rather than the long muscles, because massage methods usually result in longer tissues, which would ultimately worsen the problem. Therapeutic exercise is necessary to restore normal tone to the “long muscles.”
Spot work on isolated areas is seldom effective. Neurologic muscle imbalances are kinetic chain interactions linked by reflex patterns, most notably gait reflexes and the interaction between postural and phasic muscles.
Important areas are the musculotendinous junction and the muscle belly, where the nerve usually enters the muscle. As was pointed out earlier, motor points cause a muscle contraction with a small stimulus. Disruption of sensory signals at the motor point causes many problems, including trigger points and referred pain, hypersensitive acupressure points, and restricted movement patterns caused by an increase in the physiologic barrier and the development of pathologic barriers.
Palpation of Tendons
The eighth application of palpation is the tendons. Tendons have a higher concentration of collagen fibers and feel more pliable and less ribbed than muscle. Tendons feel like duct tape. Under many tendons is a cushion of fluid-filled bursae that assists the movement of the bone under the tendon.
Tendons should feel elastic and mobile. Tendon pathology is called tendinopathy. If a tendon has been torn, it may adhere to the underlying bone during the healing process. Some tendons, such as those of the fingers and toes, are enclosed in a sheath and must be able to glide within the sheath. If they cannot glide, inflammation builds up, and the result is tenosynovitis. Overuse also can cause inflammation. Inflammation signals the formation of connective tissue, which can interfere with movement and cause the tendons to adhere to surrounding tissue. In tendons without a sheath, this condition is called tendonitis. Frictioning techniques help these conditions. Usually, tight tendon structures are normalized when the resting length of the muscle is normalized.
Palpation of Fascial Sheaths
The ninth application of palpation is fascial sheaths. Fascial sheaths feel like sheets of plastic wrap. They separate muscles and expand the connective tissue area of bone for muscular attachment. Some, such as the lumbodorsal fascia, the abdominal fascia, and the iliotibial band, run on the surface of the body and are thick, like a tarp. Others, such as the linea alba and the nuchal ligament, run perpendicular to the surfaces of the body and the bone like a rope. Still others run horizontally through the body. The horizontal pattern occurs at joints (Figure 10-25), the diaphragm muscle (which is mostly connective tissue), and the pelvic floor. Fascial sheaths separate muscle groups. They provide a continuous, interconnected framework for the body that follows the principles of tensegrity. Fascial sheaths are kept taut by the design of the cross-pattern and the action of muscles that lie between the sheaths, such as the gluteus maximus, which lies between the iliotibial band and the lumbodorsal fascia.
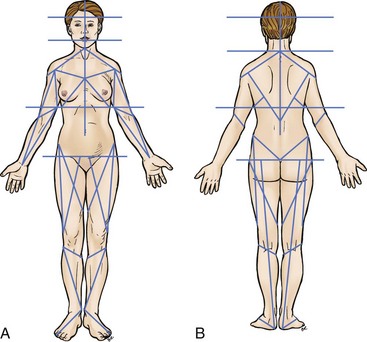
FIGURE 10-25 Fascial sheaths. A, Anterior view. B, Posterior view. (From Fritz S: Mosby’s fundamentals of therapeutic massage, ed 5, St Louis, 2013, Mosby.)
The larger nerves and blood vessels lie in grooves created by the fascial separations. Careful comparison reveals that the location of the traditional acupuncture meridians corresponds to these nerve and blood vessel tracts. The fascial separations can be made more distinct and more pliable by palpating with the fingers. With sufficient pressure, the fingers tend to fall into these grooves, which can then be followed. These areas need to be resilient and pliable but distinct, because they serve as both stabilizers and separators.
Fascial sheaths should be pliable, but because they are stabilizers, they may be denser than tendons in some areas. Problems arise if the tissues these sheaths separate or stabilize become stuck to the sheath, or if the fascial sheath becomes less pliable.
Myofascial approaches are best suited to dealing with the fascial sheaths. Mechanical work, such as slow, sustained stretching, and methods that pull and drag on the tissue are used to soften the sheaths. Because it often is uncomfortable, creating a burning, pulling sensation, the work should not be done unless the client is committed to regular appointments until the area is normalized. This may take 6 months to 1 year.
Chronic health conditions almost always show dysfunction of the connective tissue and fascial sheaths. Any techniques categorized as connective tissue approaches are effective as long as the practitioner proceeds slowly and follows the tissue pattern. The massage therapist should not override the tissue or force the tissue into a corrective pattern. Instead, the tissue must be untangled or unwound gradually, following ease and bend directions.
Fascial separations between muscles create pathways for the nerves and blood vessels. When palpated, these pathways feel like grooves running between muscles. If these areas become narrow or restricted, blood vessels may be constricted and nerves impinged. A slow, specific, stripping gliding along these pathways can be beneficial (Figure 10-26). The nerves run in these fascial pathways, and the nerve trunks correlate with the traditional meridian system. Therefore, most meridian and acupressure work takes place along these fascial grooves (Figure 10-27). Muscle layers are also separated by fascia, and because muscles must be able to slide over each other, it is necessary to make sure that there is no adherence between muscles. This situation often occurs in the legs. If assessment indicates that the muscles are stuck to each other, kneading and gliding can be used to slide one muscle layer over the other.
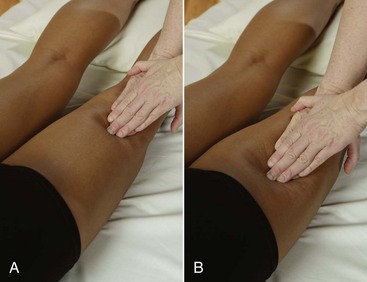
FIGURE 10-26 Gliding in fascial grooves. A, Identify the separation between muscle compartments. B, Glide slowly, assessing for adherence and binding.
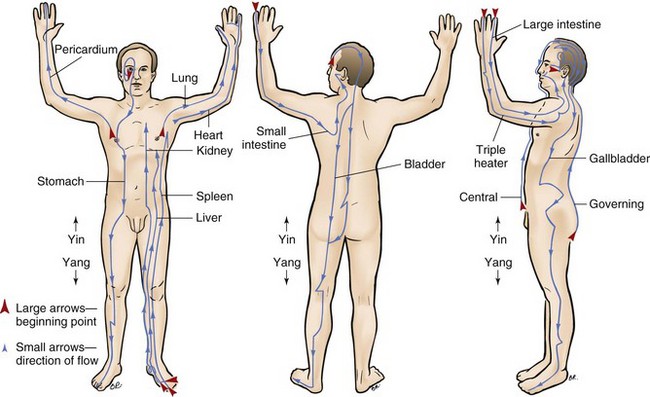
FIGURE 10-27 Typical location of meridians. Meridians tend to follow nerves and grooves. Yin and yang meridians are paired as follows: (From Fritz S: Mosby’s fundamentals of therapeutic massage, ed 3, St Louis, 2004, Mosby.)
| Yin Meridian | Yang Meridian |
| Pericardium | Triple heater |
| Liver | Gallbladder |
| Kidney | Bladder |
| Heart | Small intestine |
| Spleen | Stomach |
| Lung | Large intestine |
Water is an important element of connective tissue. To keep connective tissue soft, the client must remain hydrated.
Palpation of Ligaments
Ligaments feel like bungee cords, and some are flat when palpated. Ligaments should be flexible enough to allow the joint to move, yet stable enough to restrict movement. It is important to be able to recognize a ligament and not mistake it for a tendon. With the joint in a neutral position, if muscles are isometrically contracted, the tendon moves but the ligament does not. If ligaments are not pliable or are tender, shear force is used to normalize the tissue.
Palpation of Joints
The eleventh application of palpation is the joints. Careful palpation should reveal the space between synovial joint ends. Joints often feel like hinges. Most assessment is of active and passive joint movements. An added source of information is palpation of a joint while it is in motion. There should be a stable, supported, resilient, and unrestricted range of motion.
![]() Log on to your Evolve website for a summary of joint function.
Log on to your Evolve website for a summary of joint function.
When palpating joints, it is important to assess for end-feel, as previously discussed. Simply put, end-feel is the perception of the joint at the limit of its ROM, and it may be soft or hard. In most joints, it should feel soft. This means that the body is unable to move any more through muscular contraction, but a small additional move by the therapist still produces some give. A hard end-feel is what bony stabilization of the elbow feels like on extension. No more active movement is possible, and passive movement is restricted by bone.
For the massage practitioner, it is important to be able to palpate the bony landmarks that indicate tendinous attachment points of the muscles and to trace the shape of the bone.
Movement of the joints through a comfortable ROM can be used as an evaluation method. Comparison of the symmetry of ROM (e.g., comparing the circumduction pattern of one arm with that of the other) is effective for detecting limitations of a particular movement. Muscle energy methods, as well as all massage manipulations, can be used to support symmetric ROM functions.
All these tissues and structures are supported by general massage applications, which result in increased circulation, increased pliability of soft tissue, and normalized neuromuscular patterns.
Massage can positively affect the normal limits of the physiologic barrier. When joints are traumatized, the surrounding tissue becomes “scared,” almost as if saying, “This joint will never get in that position again.” When this happens, all proprioceptive mechanisms reset to limit ROM, setting up a pathologic barrier. Massage and appropriate muscle lengthening and general stretching, combined with muscle energy techniques and self-help, can have a beneficial effect on ligaments and joint function. Ligaments are relatively slow to regenerate, and it takes time to notice improvement.
Palpation of Bones
The twelfth application of palpation is the bones. Those who have developed their palpation skills find a firm but detectable pliability when palpating bone. Bones feel like young sapling tree trunks and branches.
Palpation of Abdominal Viscera
The thirteenth application of palpation is the viscera. The abdomen contains the viscera, or internal organs of the body. It is important for the massage professional to be able to locate and to know the positioning of the organs in the abdominal cavity (Figure 10-28). The massage therapist should be able to palpate the distinct firmness of the liver and the location of the large intestine.
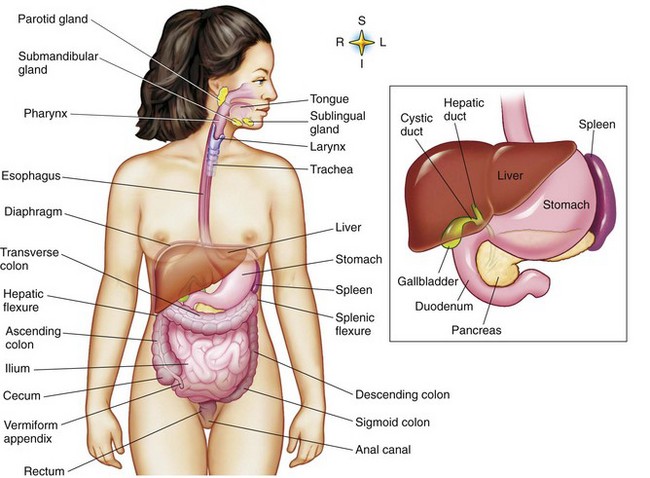
FIGURE 10-28 Location of digestive organs. (From Thibodeau GA, Patton KT: The human body in health and disease, ed 5, St Louis, 2010, Mosby.)
Refer the client to a physician if any hard, rigid, stiff, or tense areas are noted in the abdomen, or if pain is increased when palpation pressure ceases. Close attention must be paid to visceral referred pain areas. If tissue changes are noted in these areas, the practitioner must refer the client to a physician.
The skin often is tighter in areas of visceral referred pain. As a result of cutaneous/visceral reflexes, benefit may be obtained by stretching the skin in these areas. There is some indication that normalizing the skin over these areas has a positive effect on functioning of the organ. If nothing else, circulation is increased and peristalsis (intestinal movement) may be stimulated.
In accordance with the recommendations for colon massage, repetitive stroking in the proper directions may stimulate smooth muscle contraction and can improve elimination problems and intestinal gas (Figure 10-29). Psoas work is often done through the abdomen.
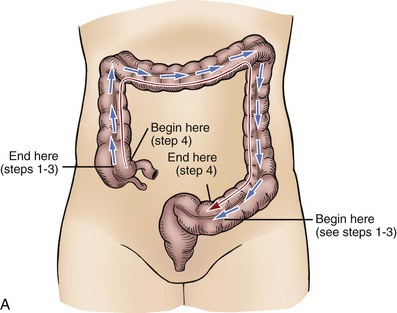




FIGURE 10-29 A, Colon with flow pattern arrows. All massage manipulations are directed in a clockwise fashion. Manipulations begin in the lower left-hand quadrant (on the left side as one views the illustration) at the sigmoid colon. The methods progressively contact all of the large intestine as they eventually end up encompassing the entire colon area. B, Abdominal sequence. The direction of flow for emptying of the large intestine and colon is as follows: 1, Massage down the left side of the descending colon using short strokes directed to the sigmoid colon. 2, Massage across the transverse colon to the left side using short strokes directed to the sigmoid colon. 3, Massage up the ascending colon on the right side of the body using short strokes directed to the sigmoid colon. End at the right side of the ileocecal valve located in the lower right-hand quadrant of the abdomen. 4, Massage entire flow pattern using long, light to moderate strokes from the ileocecal valve to the sigmoid colon. Repeat sequence. (Modified from Fritz S: Mosby’s fundamentals of therapeutic massage, ed 5, St Louis, 2013, Mosby.)
Palpation of Body Rhythms
The fourteenth application of palpation is the body rhythms. Body rhythms are felt as even pulsations or undulations. Body rhythms are designed to operate in a coordinated, balanced, and synchronized manner. In the body, all rhythms are entrained. When palpating body rhythms, the practitioner should get a sense of this harmony. Although the trained hand can pick out some of the individual rhythms, just as one can hear individual notes in a song, it is the whole connected effect that is important. When a person feels “off” or “out of sync,” often he or she is speaking of disruption in the entrainment process of body rhythms.
Respiration
The breathing rhythm is easy to feel. It should be even and should follow good principles of inhalation and exhalation. To palpate the breath, while the client goes through three or more breathing cycles, the practitioner places his or her hands over the client’s ribs and evaluates the evenness and fullness of the breaths. Relaxed breathing should result in slight rounding of the upper abdomen and lateral movement of the lower ribs during inhalation. Movement in the shoulders or upper chest indicates potential difficulties with the breathing mechanism.
Improved breathing function helps the entire body. The muscular mechanism for inhalation and exhalation of air is like a simple bellows system and depends on unrestricted movement of the musculoskeletal components of the thorax. Muscles of respiration include scalenes, intercostals, anterior serratus, diaphragm, abdominals, and pelvic floor muscles. If a breathing pattern disorder is a factor and the person is prone to anxiety, intervention softens and normalizes the upper body and supports the mechanism of breathing.
Because of the whole body interplay between muscle groups in all actions, including breathing, it is not uncommon to find tight lower leg and foot muscles interfering with breathing. Disruption of function in any of these muscle groups inhibits full and easy breathing.
General relaxation massage and stress reduction methods seem to help breathing the most. The client can be taught slow lengthening and stretching methods and the breathing retraining pattern. The client also can be advised to not wear restrictive clothing and not to hold in the stomach. (See specific protocol for breathing dysfunction.)
Circulation
The movement, or circulation, of the blood is felt at the major pulse points. The pulses should be balanced on both sides of the body. Basic palpation of the movement of blood is done by placing the fingertips over pulse points on both sides of the body and comparing for evenness.
The vascular refill rate is another means of assessing the efficiency and rhythm of the circulation. To assess this rate, press the nail beds until they blanch (push blood out), then let go and count the seconds until color returns. A normal rate is 3 to 5 seconds.
Assessment of Subtle Body Rhythms
Many other biological oscillators function in a rhythmic pattern, but they are more difficult to palpate. Body rhythms are assessed before and after massage. Improvement in rate and evenness should be noted after the massage. Massage offered by a centered practitioner with a focused, rhythmic intent provides patterns for the client’s body to use to entrain its own rhythms. The massage practitioner must remain focused on the natural rhythms of the client. Although the entrainment pattern of the practitioner and the massage provides a pattern for the client, it should not superimpose an unnatural rhythm on the client. Any foreign patterns ultimately will be rejected by the client’s body. Instead, the practitioner should support the client in reestablishing his or her innate entrainment rhythm. Supported by rocking methods and a rhythmic approach to the massage and the appropriate use of music, the body can reestablish synchronized rhythmic function.
Understanding Assessment Findings
14. Integrate clinical reasoning into the treatment plan using assessment findings.
15. Relate assessment data to first-degree, second-degree, and third-degree dysfunction, and categorize the adaptation response to stage 1, 2, or 3 pathology.
Functional biomechanical assessment defines mobility based on active and passive movements of the body through the use of palpation and observation to detect distortion in these movements. Muscle testing and identification of the functional relationships of muscles also are performed.
Typical dysfunction includes the following:
Any one or a combination of these conditions can lead to changes in motor function and can be accompanied by temporary or chronic joint, muscular, and nervous system disorders. The results of an assessment identify appropriate function or dysfunction in each area. When all assessments have been completed, the overall result is described as normal or as stage 1, stage 2, or stage 3 dysfunction. Typical dysfunction includes local functional block, local hypermobility or hypomobility, altered firing patterns, and postural imbalance, all of which lead to changes in motor function and are accompanied by temporary or chronic disorders of the joints, muscles, and nervous system.
Functional assessment defines mobility through active and passive movements of the body and by palpation and observation of distortion in these movements. Muscle testing and definition of the functional relationships of muscles are also performed.
Distortions in functioning are often measured and categorized in the following manner:
First-degree distortion—Shortening or weakening of some muscles or the formation of local changes in tension or connective tissue in these muscles. For usual and simple movements, a person has to use additional muscles from different parts of the body. As a result, movement becomes uneconomical and labored.
Second-degree distortion—Moderately expressed shortening of postural muscles and weakening of antagonist muscles. Moderately peculiar postures and movements of some parts of the body are evident. Postural and movement distortions, such as altered firing patterns, begin to occur.
Third-degree distortion—Clearly expressed shortening of postural muscles and weakening of antagonist muscles, with the appearance of specific, nonoptimal movement. Significantly expressed peculiarity in postures and movement occurs. Increased postural and movement distortions result.
It is important to define which muscles are shortened and which are inhibited and likely long and taut, to determine the appropriate therapeutic intervention.
Based on the three levels of distorted function, three stages apparently occur in the development of postural and movement pathology:
Stage 1 Dysfunction (Functional Tension). At stage 1 dysfunction (functional tension), a person tires more quickly than normal. This fatigue is accompanied by the first- or second-degree limitation of mobility, painless local myodystonia (changes in muscle length-tension relationship and motor tone), postural imbalance of the first or second degree, and nonoptimal motor function of the first degree.
Stage 2 Dysfunction (Functional Stress). Stage 2 dysfunction (functional stress) is characterized by a feeling of fatigue following moderate activity, discomfort, slight pain, and the appearance of one or more degrees of limited mobility that is painless or that results in first-degree pain. It may be accompanied by local hypermobility or hypomobility. Functional stress is also characterized by reflex vertebral-sensory dysfunction, fascial/connective tissue changes, and regional postural imbalance. It is accompanied by distortion of motor function of the first- or second-degree increase in motor tone and firing pattern alterations.
Stage 3 Dysfunction (Connective Tissue Changes in the Musculoskeletal System). Reasons for connective tissue changes include overloading, disturbances of tissue nutrition, microtrauma, microhemorrhage, unresolved edema, and other endogenous (inside the body) and exogenous (outside the body) factors. Hereditary predisposition is also a consideration. In stage 3 dysfunction, changes in the spine and weight-bearing joints may appear, with areas of local hypermobility and instability of several vertebral motion segments, hypomobility, widespread painful muscle tension, fascial and connective tissue changes in the muscles, regional postural imbalance of the second or third degree in many joints, and temporary nonoptimal motor function with second- or third-degree distortion. Visceral disturbances may be present.
Implications for Massage Treatment
Functional tension can often be managed effectively by massage methods applied by practitioners with training equivalent to 500 to 1000 hours that includes an understanding of the information presented in this text and technical training in the chosen method. Working with stages 2 and 3 (functional stress and connective tissue changes) usually requires more training and proper supervision within a multidisciplinary approach.
Assessment also identifies areas of resourceful and successful compensation. These compensation patterns occur when the body has been required to adapt to some sort of trauma or repetitive use pattern. Permanent adaptive changes, although not as efficient as optimal functioning, are the best pattern that the body can develop in response to an irreversible change in the system. Resourceful compensation is not to be eliminated but supported.
Years of clinical experience have taught many therapists that most symptoms and dysfunctional patterns are compensatory patterns. Some problems are recent, and others qualify for archaeologic exploration, having developed in early life and having been compounded through time. Compensatory patterns often are complex, but the client’s body frequently can show us the way if we can listen to the story it tells.
There are many instances of resourceful compensation, a term used for the adjustments the body makes to manage a permanent or chronic dysfunction. Protective muscle spasm (guarding) around a compressed disk is an example. The splinting action of the spasms protects the nerves and provides additional stability in the area.
Decisions must be made regarding how and to what degree the compensatory pattern should be altered. It seems prudent to assume that the body knows what it is doing. The wise therapist spends time learning to understand the reasons for the compensatory patterns presented by the body. When resourceful compensation is present, therapeutic massage methods are used to support the altered pattern and prevent any further increase in postural distortion over what is necessary to support the body change.
Some compensatory patterns are set up for short-term situations that do not require permanent adaptation. Having a leg in a cast and walking on crutches for a period of time is a classic example. The body catching itself during an “almost” fall is another classic setup pattern. Unfortunately, the body often habituates these patterns and maintains them well beyond their usefulness. As a result, over time the body begins to show symptoms of pain or inefficient function, or both.
Many compensatory patterns develop to maintain a balanced posture, and even though the posture becomes distorted during compensation, the overall result is a balanced body in a gravitational line. It also is important to consider the pattern of muscle interactions, such as the ones that occur when walking, and to recognize that gait has a certain pattern for the most efficient movement that the body can manage.
There is no set system for figuring out compensatory patterns. All these factors must be considered in devising a plan that best serves the client.
Remember, as indicated earlier, first-degree and stage 1 dysfunction can usually be managed by general massage application. Stage 2 and stage 3 dysfunction should be referred to the appropriate health care professional, and cooperative multidisciplinary treatment plans should be developed. Keeping this in mind, the massage therapist honors the limits of their scope of practice.
If the massage therapist is working in a sports team environment, the athletic trainer in conjunction with the team doctor and the physical therapist would do most of the assessment. These professionals would also provide the treatment plan and outcome goals to be carried out by the massage therapist. This does not mean that the massage therapist does not also do an assessment to identify the focus for massage application. Findings are submitted to the trainer.
Organizing Assessment Information Into Treatment Strategies
The body is an interrelated, relatively symmetric functional form. For both assessment purposes and treatment approaches, it is helpful to consider these interrelationships. Science does not totally explain how our molecules stay together, let alone how the body constantly adapts second by second to internal and external environmental demands. Yet natural design is usually very simple and is set up in repeating patterns that function together for efficiency.
Sympathetic/Parasympathetic Balance
In general, excessive sympathetic activation should be balanced by a relaxing massage, and excessive parasympathetic activation should be balanced by a stimulating massage. However, it is not quite that easy. To establish rapport and ultimately entrainment, it is recommended that the practitioner work with the client by addressing the client’s current state. This is also very true when deciding whether the general massage approach will be stimulation or relaxation.
If the client is functioning from sympathetic nervous system dominance, and relaxation methods such as rocking and slow gliding are used initially, the work often seems irritating to the client. If the session is begun with a more stimulating approach, using such strokes as rapid compression, muscle energy methods, lengthening, and tapotement, the design of the massage fits the physiologic level of the client. After some of the nervous energy has been discharged, the client is ready for the more relaxing methods.
The same is true with parasympathetic dominance patterns. If the client is feeling “down,” beginning with a stimulating approach may feel like an attack. It is better to begin with more subtle relaxation methods and progress slowly into stimulating approaches to encourage balance.
If the client seems “out of sorts,” operating more as a collection of parts than the sum of the parts, entrainment processes may be off. The centered, coordinated presence of the professional providing a harmonized approach to the massage is beneficial.
Body Symmetry
Body symmetry interrelationships can be seen in the nervous system, especially various reflexes—oculopelvic, crossed-extensor, withdrawal, gait, and other such patterns. Observation of the body reveals structural similarity in the design of the shoulder and pelvic girdles and of the upper and lower limbs. It is logical to assume that similarly shaped areas function in similar ways.
The axial skeleton does not seem to show a design similar to that of the appendicular skeleton; however, with a bit of imagination, one can see that it is there. Consider the rib cage as the central point: above it you have the cervical vertebrae and the head; below it, the lumbar vertebrae, sacrum, and coccyx (what is left of a tail). Most biological forms have a head at one end and a tail at the other. Imagine if we removed the head or added a tail, and there you go—symmetry.
The principles of postural balance and mobility factor in. The axial skeleton displays a mirror image as a top/bottom with the midpoint about the navel. Therefore, the imaginary tail pairs with the real head, the coccyx pairs with the atlas, and the axis with the sacrum; the lumbar and cervical areas pair together. This mirror image can be considered functional for posture and stability. The muscles pair as follows: occipital base and suprahyoids with pelvic floor, sternocleidomastoid and longus coli with the psoas and rectus abdominis, scalenes with quadratus lumborum, internal and external intercostals with internal and external obliques, and transversus thoracis with transversus abdominis. On the dorsal aspect of the thorax, you find the posterior serratus superior and inferior paired. Muscles that are oriented more vertically, such as the rectus abdominis and erector spinae group, pair on the dorsal and ventral aspects. If the pairs are also agonist/antagonists, then a reciprocal inhibition pattern can occur, or a co-contraction situation is noted.
Therefore, if a client has a short psoas, the sternocleidomastoid and the longus colli may also be short. If the scalenes are short, the quadratus lumborum may show reflex shortening. Dysfunction in the occipital base may also involve pelvic floor dysfunction.
The girdles and limbs that attach to the axial skeleton move in contralateral patterns—the left lower with right upper, and so forth. The scapula and the clavicle pair with the pelvis. The sacroiliac joints pair with both sternoclavicular joints. Other pairs include humerus and femur, tibia/fibula and radius/ulna, carpals and tarsals, metacarpals and metatarsals, phalanges and corresponding phalanges, hip and shoulder joints, elbow and knee, ankle and wrist, and foot and hand.
A corresponding symmetry is evident in the functional aspects of the axial soft tissue: the rotator cuff muscles with the deep lateral hip rotators, the deltoid with the gluteal group, the pectoralis minor and coracobrachialis with the pectineus, the pectoralis major and latissimus dorsi with the adductors, the quadriceps with the triceps and anconeus, the hamstrings with the biceps brachii, the brachialis with the popliteus, the wrist and finger flexors with the ankle plantar flexors, the wrist and finger extensors with the dorsiflexors, the supinators with the inverters, the pronators with the everters, and finally, the palm of the hand with the sole of the foot. These relationships should be easy to conceptualize.
Remember that in the appendicular skeleton, a counterbalancing crossed pattern exists, so again the left arm pairs with the right leg, and the right arm with the left leg. Thus, if a client has a short hamstring on the left, he or she may also have a short biceps brachii on the right. A bruise on the right quadriceps may result in reflex guarding in the left triceps. A sprain of the great toe on the right foot may result in reflexive guarding in the left thumb. A short gastrocnemius bilateral may also reflexively include short wrist flexors bilaterally. Guarding patterns for a knee injury may occur reflexively around the opposite elbow. Right sacroiliac pain may be paired with left sternoclavicular joint dysfunction. Short deep lateral hip rotators on the left may involve reflexive guarding in the right rotator cuff, with changes in movement of the shoulder. Restricted shoulder/arm movement on the right may be a lingering response to a previous adductor/groin injury on the left. The possible interactions are countless.
These potential patterns may be used in analysis of assessment and development of massage application (Figure 10-30).
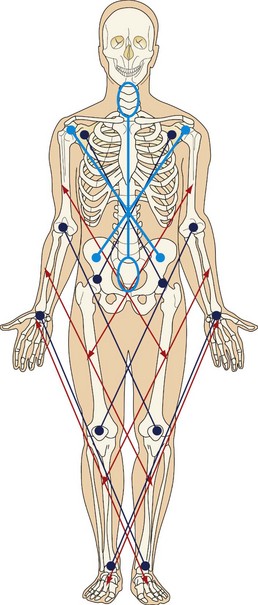
FIGURE 10-30 Areas of symmetry. Arm—Thigh; Forearm—Leg; Hand—Foot; Shoulder—Hip; Elbow—Knee; Wrist—Ankle; Cervical—Sacrum; Shoulder Girdle—Pelvic Girdle.
For example, if a baseball pitcher has restricted ROM in the pitching arm (right arm) that has appeared over time and seems unrelated to the common strain in the arm, ask whether there was a previous groin injury or increased groin tightness on the left. For treatment, first address the adductors of the leg and the deep lateral hip rotators on the left while the client moves the right arm slowly through ROM. Continually palpate for areas in the thigh and hip muscles that seem to overrespond to the arm movement, and focus inhibition methods (usually compression in the muscle belly but sometimes in the attachments) in these areas. Then reassess the shoulder and arm for change. Finally, address the remaining arm symptoms.
Another example: A client has quadratus/psoas shortening related to low back pain. Ask whether he is also experiencing any symptoms in the neck. Assess the ROM of the neck and palpate for especially tender areas. Before addressing the low back pain, make sure that the scalenes and the sternocleidomastoid muscles are normal, and treat dysfunction with muscle energy methods or direct inhibition while the client rotates the pelvis in various directions. As in the previous example, continue to assess for areas that overrespond to activation of the quadratus lumborum and psoas movement. Focus on those areas and reassess the low back pain. Treat the remaining symptoms of low back pain. While addressing the quadratus lumborum and the psoas, have the client rotate the head in slow large circles to activate the pattern and facilitate the release.
Another example: A soccer player has a thigh bruise, and it cannot be directly massaged other than by lymphatic drain. To create a reduction in reflexive guarding and pain, massage is applied to the opposite triceps group. A surprisingly sore area may correspond to the location of the bruise.
When working with these patterns, remember the focus of the massage. If the goal of the massage is to increase mobility of the left ankle, it may be helpful for the client to slowly move the right wrist in circles; the intent is not to treat the wrist, but to influence the dysfunctional ankle. If the goal of the massage is to manage short hamstrings, the biceps muscle of the arm will be part of the treatment approach. Although the client may notice changes in the arm when massage is being applied, the client should be moving the knees back and forth so that the hamstrings are affected because this is the goal of the massage. A client with a groin pull will likely benefit from massage of the arm adductors and abductors, but the intent of the massage of this area is to influence the groin.
The general protocol and many of the other specific recommendations for massage incorporate these concepts. It is prudent for the massage therapist to become proficient with this strategy for organizing and understanding injury and training adaptation. Seemingly unrelated symptoms are indeed part of the same process.
Additional guidelines for analyzing problems found through the functional biomechanical assessment include the following:
• If an area is hypomobile, consider tension or shortening in the antagonist pattern as a possible cause.
• If an area is hypermobile, consider instability of the joint structure or muscle weakness in the fixation pattern or problems with antagonist/agonist co-contraction function.
• If an area cannot hold against resistance, consider weakness from reciprocal inhibition of the muscles of the prime mover and synergist pattern, and tension in the antagonist pattern as possible causes.
• If pain or heaviness occurs on passive movement, consider joint capsule dysfunction and nerve entrapment syndrome as possible causes.
• If pain occurs on active movement, consider muscle firing patterns with fascial involvement as a possible cause.
• Always consider as possible causes body-wide reflexive patterns, as discussed in the sections on posture, gait assessment, and kinetic chain assessment.
• The following guidelines also are important:
• During muscle testing, the ability to easily resist applied force should be the same or very similar bilaterally.
• Opposite movement patterns should be easy to assume.
• Bilateral asymmetry, pain, weakness, inability to assume the isolation position or to move into the opposite position, fatigue, or a heavy sensation may indicate dysfunction.
• Intervention or referral depends on the severity of the condition (stage 1, 2, or 3) and whether the dysfunction is joint-related, neuromuscular-related, or myofascial-related.
![]() Log on to your Evolve website to view an assessment sequence for an 80-year-old marathon runner.
Log on to your Evolve website to view an assessment sequence for an 80-year-old marathon runner.
Summary
The main purpose of intervention is to help the body regain symmetry and ease of movement. Therefore, when observing gait or posture, the practitioner notes areas that seem pulled, twisted, or dropped. The massage practitioner’s job is to use massage methods to lengthen shortened areas, untwist twisted areas, raise dropped areas, drop raised areas, soften hard areas, harden soft areas, warm cold areas, and cool hot areas.
During assessment, careful attention should be paid to the order of priority in which the client relays the information. If the headache is mentioned first, the knee ache second, and the tight elbow last, the areas should be dealt with in that order, if possible, in the massage flow.
The importance of listening to understand is paramount. Many experienced professionals have learned that if we listen to our clients, they will tell us what is wrong and how to help them restore balance. Athletes are especially attuned to their body function. Slow down, do not jump to conclusions, pay attention, and let the information unfold. Realize that each client is the expert about himself or herself. Clients are your teachers about themselves, and in teaching you, they often begin to understand themselves better. In every session, approach each client with fascination about what you will learn from him or her. No textbook, class, or instructor can equal the teaching provided by careful attention to the client.
Visit the Evolve website to download and complete the following exercises.
Note: This chapter does not adapt well to written question responses. The information is skill-based; therefore, the following exercises are recommended.
1. Develop a checklist of all history components covered.
2. Develop a checklist of all physical assessment components covered.
3. Complete ten comprehensive assessments using all methods covered in this chapter and your checklists.
4. Develop a treatment plan based on each assessment.
5. Implement the treatment plan and reassess after ten sessions. Chart each.
6. Write a post-assessment narrative describing the outcomes achieved or not achieved by the client.
1For more in-depth information, see Fritz S: Mosby’s fundamentals of therapeutic massage, ed 5, St Louis, 2013, Mosby; and Fritz S: Mosby’s essential sciences for therapeutic massage, ed 4, St Louis, 2013, Mosby.