Cardiology
I. Websites
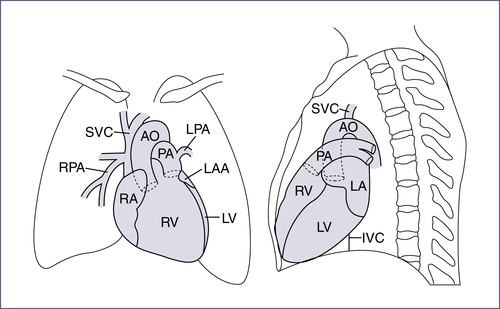
II. The Cardiac Cycle (Fig. 7-1)
III. Physical Examination
TABLE EC7-A
BLOOD PRESSURES AFTER 2 WEEKS OF AGE IN INFANTS FROM 26–44 WEEKS POSTCONCEPTIONAL AGE
| Postconceptional Age | 50th Percentile | 95th Percentile | 99th Percentile |
| 44 WEEKS | |||
| SBP | 88 | 105 | 110 |
| DBP | 50 | 68 | 73 |
| MAP | 63 | 80 | 85 |
| 42 WEEKS | |||
| SBP | 85 | 98 | 102 |
| DBP | 50 | 65 | 70 |
| MAP | 62 | 76 | 81 |
| 40 WEEKS | |||
| SBP | 80 | 95 | 100 |
| DBP | 50 | 65 | 70 |
| MAP | 60 | 75 | 80 |
| 38 WEEKS | |||
| SBP | 77 | 92 | 97 |
| DBP | 50 | 65 | 70 |
| MAP | 59 | 74 | 79 |
| 36 WEEKS | |||
| SBP | 72 | 87 | 92 |
| DBP | 50 | 65 | 70 |
| MAP | 57 | 72 | 71 |
| 34 WEEKS | |||
| SBP | 70 | 85 | 90 |
| DBP | 40 | 55 | 60 |
| MAP | 50 | 65 | 70 |
| 32 WEEKS | |||
| SBP | 68 | 83 | 88 |
| DBP | 40 | 55 | 60 |
| MAP | 48 | 62 | 69 |
| 30 WEEKS | |||
| SBP | 65 | 80 | 85 |
| DBP | 40 | 55 | 60 |
| MAP | 48 | 65 | 68 |
| 28 WEEKS | |||
| SBP | 60 | 75 | 80 |
| DBP | 38 | 50 | 54 |
| MAP | 45 | 58 | 63 |
| 26 WEEKS | |||
| SBP | 55 | 72 | 77 |
| DBP | 30 | 50 | 56 |
| MAP | 38 | 57 | 63 |

DBP, Diastolic blood pressure; MAP, mean arterial pressure; SBP, systolic blood pressure.
Data from Dionne J et al. Hypertension in infancy: diagnosis, management, and outcome. Pediatr Nephrol. 2012;27:17-32.
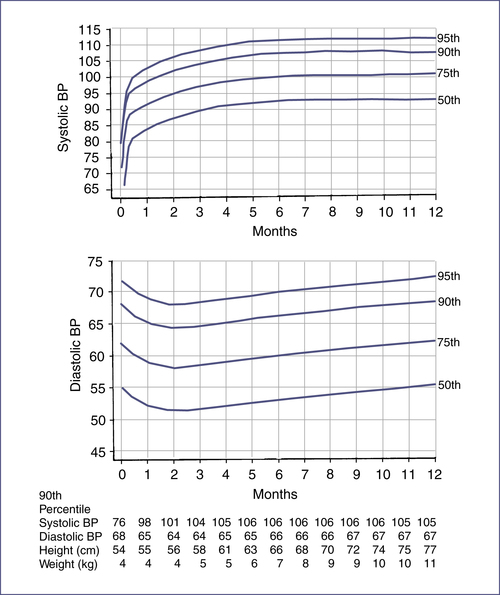
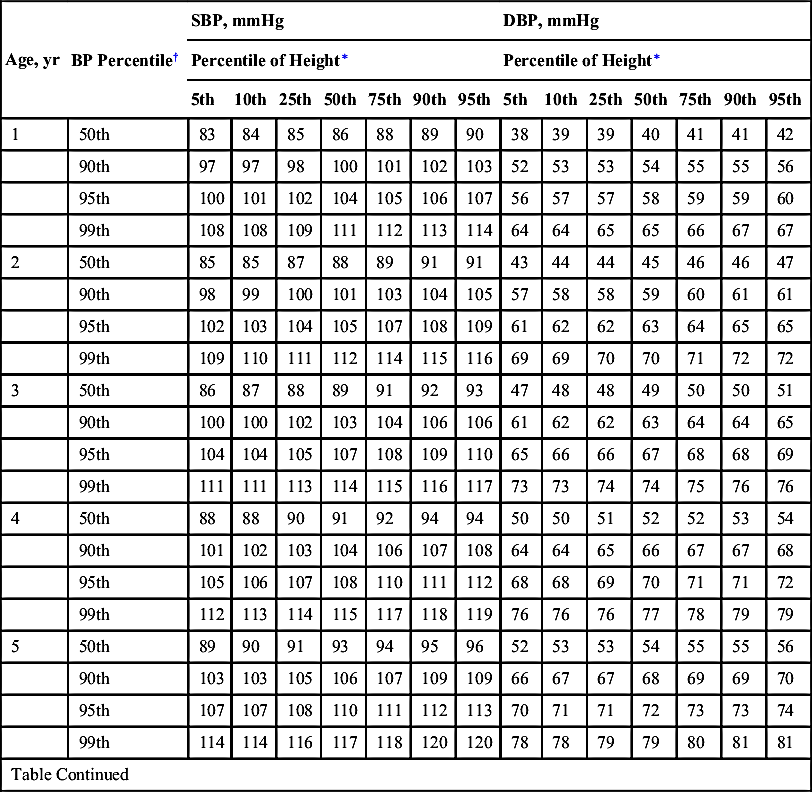
TABLE 7-1
BLOOD PRESSURE LEVELS FOR THE 50TH, 90TH, 95TH, AND 99TH PERCENTILES OF BLOOD PRESSURE FOR GIRLS AGE 1–17 YEARS BY PERCENTILES OF HEIGHT2
| Age, yr | BP Percentile† | SBP, mmHg | DBP, mmHg | ||||||||||||
| Percentile of Height∗ | Percentile of Height∗ | ||||||||||||||
| 5th | 10th | 25th | 50th | 75th | 90th | 95th | 5th | 10th | 25th | 50th | 75th | 90th | 95th | ||
| 1 | 50th | 83 | 84 | 85 | 86 | 88 | 89 | 90 | 38 | 39 | 39 | 40 | 41 | 41 | 42 |
| 90th | 97 | 97 | 98 | 100 | 101 | 102 | 103 | 52 | 53 | 53 | 54 | 55 | 55 | 56 | |
| 95th | 100 | 101 | 102 | 104 | 105 | 106 | 107 | 56 | 57 | 57 | 58 | 59 | 59 | 60 | |
| 99th | 108 | 108 | 109 | 111 | 112 | 113 | 114 | 64 | 64 | 65 | 65 | 66 | 67 | 67 | |
| 2 | 50th | 85 | 85 | 87 | 88 | 89 | 91 | 91 | 43 | 44 | 44 | 45 | 46 | 46 | 47 |
| 90th | 98 | 99 | 100 | 101 | 103 | 104 | 105 | 57 | 58 | 58 | 59 | 60 | 61 | 61 | |
| 95th | 102 | 103 | 104 | 105 | 107 | 108 | 109 | 61 | 62 | 62 | 63 | 64 | 65 | 65 | |
| 99th | 109 | 110 | 111 | 112 | 114 | 115 | 116 | 69 | 69 | 70 | 70 | 71 | 72 | 72 | |
| 3 | 50th | 86 | 87 | 88 | 89 | 91 | 92 | 93 | 47 | 48 | 48 | 49 | 50 | 50 | 51 |
| 90th | 100 | 100 | 102 | 103 | 104 | 106 | 106 | 61 | 62 | 62 | 63 | 64 | 64 | 65 | |
| 95th | 104 | 104 | 105 | 107 | 108 | 109 | 110 | 65 | 66 | 66 | 67 | 68 | 68 | 69 | |
| 99th | 111 | 111 | 113 | 114 | 115 | 116 | 117 | 73 | 73 | 74 | 74 | 75 | 76 | 76 | |
| 4 | 50th | 88 | 88 | 90 | 91 | 92 | 94 | 94 | 50 | 50 | 51 | 52 | 52 | 53 | 54 |
| 90th | 101 | 102 | 103 | 104 | 106 | 107 | 108 | 64 | 64 | 65 | 66 | 67 | 67 | 68 | |
| 95th | 105 | 106 | 107 | 108 | 110 | 111 | 112 | 68 | 68 | 69 | 70 | 71 | 71 | 72 | |
| 99th | 112 | 113 | 114 | 115 | 117 | 118 | 119 | 76 | 76 | 76 | 77 | 78 | 79 | 79 | |
| 5 | 50th | 89 | 90 | 91 | 93 | 94 | 95 | 96 | 52 | 53 | 53 | 54 | 55 | 55 | 56 |
| 90th | 103 | 103 | 105 | 106 | 107 | 109 | 109 | 66 | 67 | 67 | 68 | 69 | 69 | 70 | |
| 95th | 107 | 107 | 108 | 110 | 111 | 112 | 113 | 70 | 71 | 71 | 72 | 73 | 73 | 74 | |
| 99th | 114 | 114 | 116 | 117 | 118 | 120 | 120 | 78 | 78 | 79 | 79 | 80 | 81 | 81 | |
| Table Continued | |||||||||||||||
| Age, yr | BP Percentile† | SBP, mmHg | DBP, mmHg | ||||||||||||
| Percentile of Height∗ | Percentile of Height∗ | ||||||||||||||
| 5th | 10th | 25th | 50th | 75th | 90th | 95th | 5th | 10th | 25th | 50th | 75th | 90th | 95th | ||
| 6 | 50th | 91 | 92 | 93 | 94 | 96 | 97 | 98 | 54 | 54 | 55 | 56 | 56 | 57 | 58 |
| 90th | 104 | 105 | 106 | 108 | 109 | 110 | 111 | 68 | 68 | 69 | 70 | 70 | 71 | 72 | |
| 95th | 108 | 109 | 110 | 111 | 113 | 114 | 115 | 72 | 72 | 73 | 74 | 74 | 75 | 76 | |
| 99th | 115 | 116 | 117 | 119 | 120 | 121 | 122 | 80 | 80 | 80 | 81 | 82 | 83 | 83 | |
| 7 | 50th | 93 | 93 | 95 | 96 | 97 | 99 | 99 | 55 | 56 | 56 | 57 | 58 | 58 | 59 |
| 90th | 106 | 107 | 108 | 109 | 111 | 112 | 113 | 69 | 70 | 70 | 71 | 72 | 72 | 73 | |
| 95th | 110 | 111 | 112 | 113 | 115 | 116 | 116 | 73 | 74 | 74 | 75 | 76 | 76 | 77 | |
| 99th | 117 | 118 | 119 | 120 | 122 | 123 | 124 | 81 | 81 | 82 | 82 | 83 | 84 | 84 | |
| 8 | 50th | 95 | 95 | 96 | 98 | 99 | 100 | 101 | 57 | 57 | 57 | 58 | 59 | 60 | 60 |
| 90th | 108 | 109 | 110 | 111 | 113 | 114 | 114 | 71 | 71 | 71 | 72 | 73 | 74 | 74 | |
| 95th | 112 | 112 | 114 | 115 | 116 | 118 | 118 | 75 | 75 | 75 | 76 | 77 | 78 | 78 | |
| 99th | 119 | 120 | 121 | 122 | 123 | 125 | 125 | 82 | 82 | 83 | 83 | 84 | 85 | 86 | |
| 9 | 50th | 96 | 97 | 98 | 100 | 101 | 102 | 103 | 58 | 58 | 58 | 59 | 60 | 61 | 61 |
| 90th | 110 | 110 | 112 | 113 | 114 | 116 | 116 | 72 | 72 | 72 | 73 | 74 | 75 | 75 | |
| 95th | 114 | 114 | 115 | 117 | 118 | 119 | 120 | 76 | 76 | 76 | 77 | 78 | 79 | 79 | |
| 99th | 121 | 121 | 123 | 124 | 125 | 127 | 127 | 83 | 83 | 84 | 84 | 85 | 86 | 87 | |
| 10 | 50th | 98 | 99 | 100 | 102 | 103 | 104 | 105 | 59 | 59 | 59 | 60 | 61 | 62 | 62 |
| 90th | 112 | 112 | 114 | 115 | 116 | 118 | 118 | 73 | 73 | 73 | 74 | 75 | 76 | 76 | |
| 95th | 116 | 116 | 117 | 119 | 120 | 121 | 122 | 77 | 77 | 77 | 78 | 79 | 80 | 80 | |
| Table Continued | |||||||||||||||
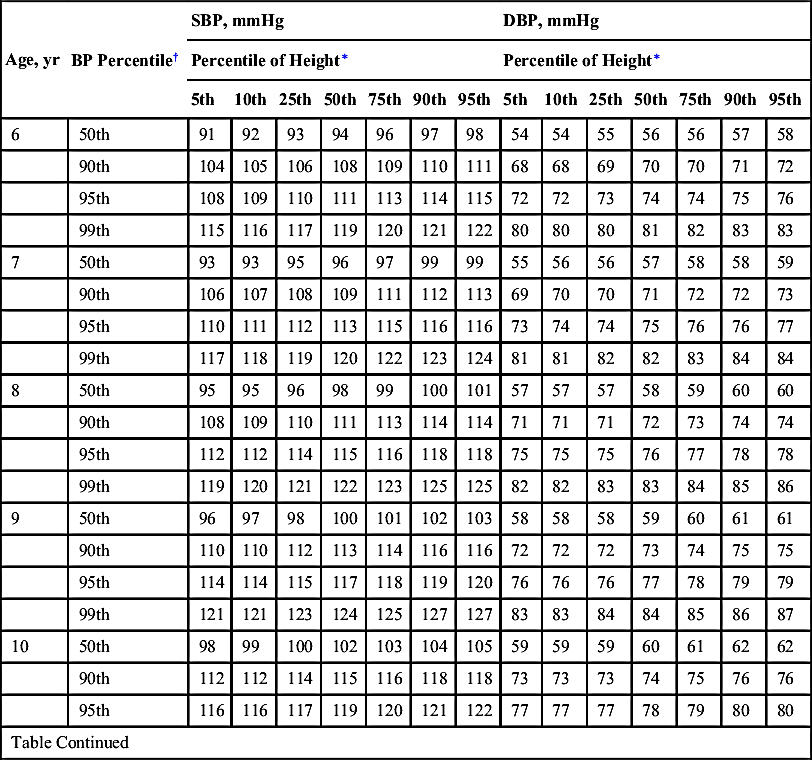
| Age, yr | BP Percentile† | SBP, mmHg | DBP, mmHg | ||||||||||||
| Percentile of Height∗ | Percentile of Height∗ | ||||||||||||||
| 5th | 10th | 25th | 50th | 75th | 90th | 95th | 5th | 10th | 25th | 50th | 75th | 90th | 95th | ||
| 99th | 123 | 123 | 125 | 126 | 127 | 129 | 129 | 84 | 84 | 85 | 86 | 86 | 87 | 88 | |
| 11 | 50th | 100 | 101 | 102 | 103 | 105 | 106 | 107 | 60 | 60 | 60 | 61 | 62 | 63 | 63 |
| 90th | 114 | 114 | 116 | 117 | 118 | 119 | 120 | 74 | 74 | 74 | 75 | 76 | 77 | 77 | |
| 95th | 118 | 118 | 119 | 121 | 122 | 123 | 124 | 78 | 78 | 78 | 79 | 80 | 81 | 81 | |
| 99th | 125 | 125 | 126 | 128 | 129 | 130 | 131 | 85 | 85 | 86 | 87 | 87 | 88 | 89 | |
| 12 | 50th | 102 | 103 | 104 | 105 | 107 | 108 | 109 | 61 | 61 | 61 | 62 | b3 | 64 | 64 |
| 90th | 116 | 116 | 117 | 119 | 120 | 121 | 122 | 75 | 75 | 75 | 76 | 77 | 78 | 78 | |
| 95th | 119 | 120 | 121 | 123 | 124 | 125 | 126 | 79 | 79 | 79 | 80 | 81 | 82 | 82 | |
| 99th | 127 | 127 | 128 | 130 | 131 | 132 | 133 | 86 | 86 | 87 | 88 | 88 | 89 | 90 | |
| 13 | 50th | 104 | 105 | 106 | 107 | 109 | 110 | 110 | 62 | 62 | 62 | 63 | 64 | 65 | 65 |
| 90th | 117 | 118 | 119 | 121 | 122 | 123 | 124 | 76 | 76 | 76 | 77 | 78 | 79 | 79 | |
| 95th | 121 | 122 | 123 | 124 | 126 | 127 | 128 | 80 | 80 | 80 | 81 | 82 | 83 | 83 | |
| 99th | 128 | 129 | 130 | 132 | 133 | 134 | 135 | 87 | 87 | 88 | 89 | 89 | 90 | 91 | |
| 14 | 50th | 106 | 106 | 107 | 109 | 110 | 111 | 112 | 63 | 63 | 63 | 64 | 65 | 66 | 66 |
| 90th | 119 | 120 | 121 | 122 | 124 | 125 | 125 | 77 | 77 | 77 | 78 | 79 | 80 | 80 | |
| 95th | 123 | 123 | 125 | 126 | 127 | 129 | 129 | 81 | 81 | 81 | 82 | 83 | 84 | 84 | |
| 99th | 130 | 131 | 132 | 133 | 135 | 136 | 136 | 88 | 88 | 89 | 90 | 90 | 91 | 92 | |
| 15 | 50th | 107 | 108 | 109 | 110 | 111 | 113 | 113 | 64 | 64 | 64 | 65 | 66 | 67 | 67 |
| 90th | 120 | 121 | 122 | 123 | 125 | 126 | 127 | 78 | 78 | 78 | 79 | 80 | 81 | 81 | |
| 95th | 124 | 125 | 126 | 127 | 129 | 130 | 131 | 82 | 82 | 82 | 83 | 84 | 85 | 85 | |
| Table Continued | |||||||||||||||
| Age, yr | BP Percentile† | SBP, mmHg | DBP, mmHg | ||||||||||||
| Percentile of Height∗ | Percentile of Height∗ | ||||||||||||||
| 5th | 10th | 25th | 50th | 75th | 90th | 95th | 5th | 10th | 25th | 50th | 75th | 90th | 95th | ||
| 99th | 131 | 132 | 133 | 134 | 136 | 137 | 138 | 89 | 89 | 90 | 91 | 91 | 92 | 93 | |
| 16 | 50th | 108 | 108 | 110 | 111 | 112 | 114 | 114 | 64 | 64 | 65 | 66 | 66 | 67 | 68 |
| 90th | 121 | 122 | 123 | 124 | 126 | 127 | 128 | 78 | 78 | 79 | 80 | 81 | 81 | 82 | |
| 95th | 125 | 126 | 127 | 128 | 130 | 131 | 132 | 82 | 82 | 83 | 84 | 85 | 85 | 86 | |
| 99th | 132 | 133 | 134 | 135 | 137 | 138 | 139 | 90 | 90 | 90 | 91 | 92 | 93 | 93 | |
| 17 | 50th | 108 | 109 | 110 | 111 | 113 | 114 | 115 | 64 | 65 | 65 | 66 | 67 | 67 | 68 |
| 90th | 122 | 122 | 123 | 125 | 126 | 127 | 128 | 78 | 79 | 79 | 80 | 81 | 81 | 82 | |
| 95th | 125 | 126 | 127 | 129 | 130 | 131 | 132 | 82 | 83 | 83 | 84 | 85 | 85 | 86 | |
| 99th | 133 | 133 | 134 | 136 | 137 | 138 | 139 | 90 | 90 | 91 | 91 | 92 | 93 | 93 | |
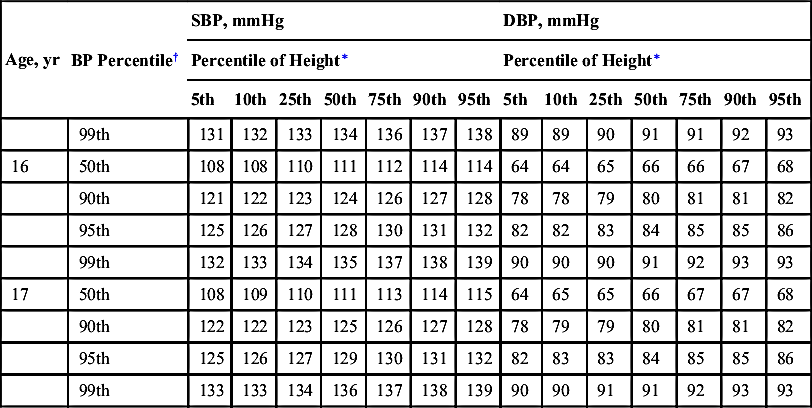
∗ Height percentile determined by standard growth curves.
† Blood pressure percentile determined by a single measurement.
Adapted from National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 Suppl):555-576.
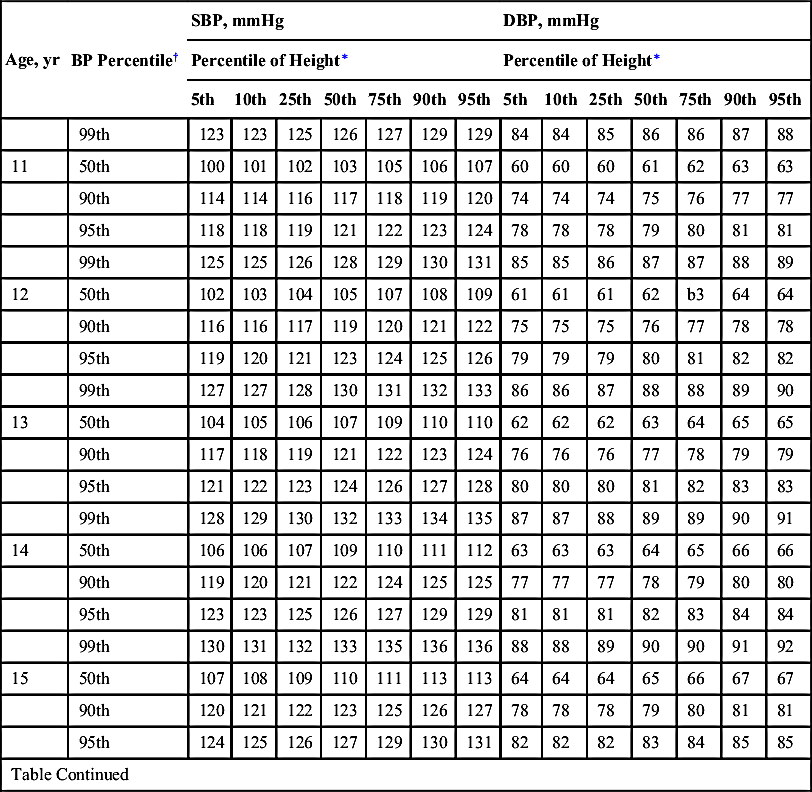
TABLE 7-2
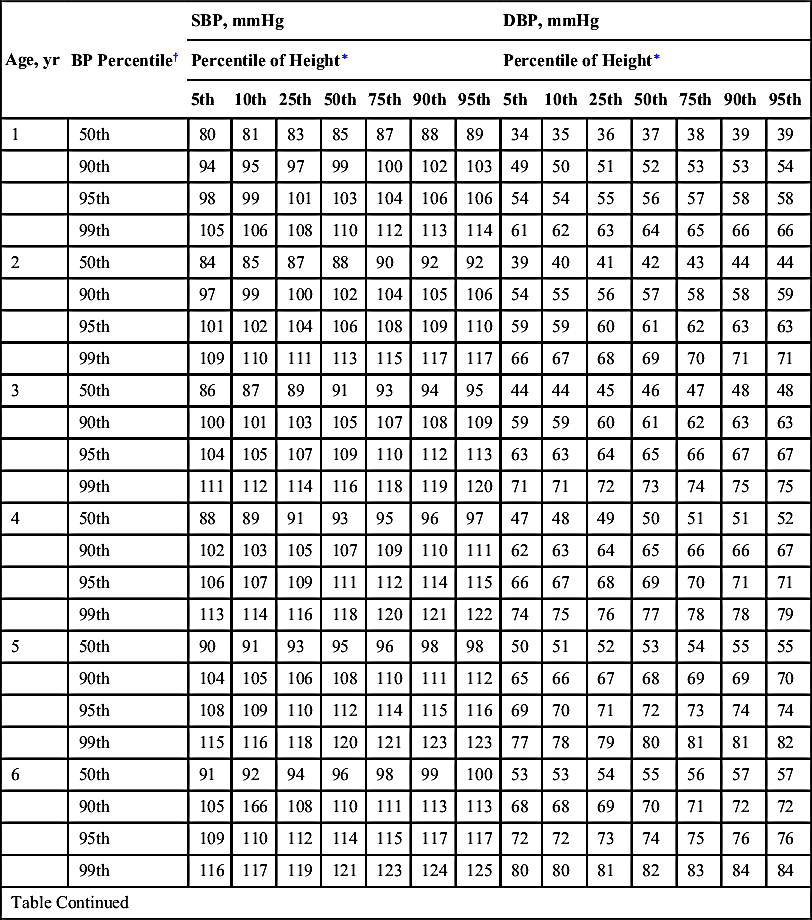
BLOOD PRESSURE LEVELS FOR THE 50TH, 90TH, 95TH, AND 99TH PERCENTILES OF BLOOD PRESSURE FOR BOYS AGE 1–17 YEARS BY PERCENTILES OF HEIGHT2
| Age, yr | BP Percentile† | SBP, mmHg | DBP, mmHg | ||||||||||||
| Percentile of Height∗ | Percentile of Height∗ | ||||||||||||||
| 5th | 10th | 25th | 50th | 75th | 90th | 95th | 5th | 10th | 25th | 50th | 75th | 90th | 95th | ||
| 1 | 50th | 80 | 81 | 83 | 85 | 87 | 88 | 89 | 34 | 35 | 36 | 37 | 38 | 39 | 39 |
| 90th | 94 | 95 | 97 | 99 | 100 | 102 | 103 | 49 | 50 | 51 | 52 | 53 | 53 | 54 | |
| 95th | 98 | 99 | 101 | 103 | 104 | 106 | 106 | 54 | 54 | 55 | 56 | 57 | 58 | 58 | |
| 99th | 105 | 106 | 108 | 110 | 112 | 113 | 114 | 61 | 62 | 63 | 64 | 65 | 66 | 66 | |
| 2 | 50th | 84 | 85 | 87 | 88 | 90 | 92 | 92 | 39 | 40 | 41 | 42 | 43 | 44 | 44 |
| 90th | 97 | 99 | 100 | 102 | 104 | 105 | 106 | 54 | 55 | 56 | 57 | 58 | 58 | 59 | |
| 95th | 101 | 102 | 104 | 106 | 108 | 109 | 110 | 59 | 59 | 60 | 61 | 62 | 63 | 63 | |
| 99th | 109 | 110 | 111 | 113 | 115 | 117 | 117 | 66 | 67 | 68 | 69 | 70 | 71 | 71 | |
| 3 | 50th | 86 | 87 | 89 | 91 | 93 | 94 | 95 | 44 | 44 | 45 | 46 | 47 | 48 | 48 |
| 90th | 100 | 101 | 103 | 105 | 107 | 108 | 109 | 59 | 59 | 60 | 61 | 62 | 63 | 63 | |
| 95th | 104 | 105 | 107 | 109 | 110 | 112 | 113 | 63 | 63 | 64 | 65 | 66 | 67 | 67 | |
| 99th | 111 | 112 | 114 | 116 | 118 | 119 | 120 | 71 | 71 | 72 | 73 | 74 | 75 | 75 | |
| 4 | 50th | 88 | 89 | 91 | 93 | 95 | 96 | 97 | 47 | 48 | 49 | 50 | 51 | 51 | 52 |
| 90th | 102 | 103 | 105 | 107 | 109 | 110 | 111 | 62 | 63 | 64 | 65 | 66 | 66 | 67 | |
| 95th | 106 | 107 | 109 | 111 | 112 | 114 | 115 | 66 | 67 | 68 | 69 | 70 | 71 | 71 | |
| 99th | 113 | 114 | 116 | 118 | 120 | 121 | 122 | 74 | 75 | 76 | 77 | 78 | 78 | 79 | |
| 5 | 50th | 90 | 91 | 93 | 95 | 96 | 98 | 98 | 50 | 51 | 52 | 53 | 54 | 55 | 55 |
| 90th | 104 | 105 | 106 | 108 | 110 | 111 | 112 | 65 | 66 | 67 | 68 | 69 | 69 | 70 | |
| 95th | 108 | 109 | 110 | 112 | 114 | 115 | 116 | 69 | 70 | 71 | 72 | 73 | 74 | 74 | |
| 99th | 115 | 116 | 118 | 120 | 121 | 123 | 123 | 77 | 78 | 79 | 80 | 81 | 81 | 82 | |
| 6 | 50th | 91 | 92 | 94 | 96 | 98 | 99 | 100 | 53 | 53 | 54 | 55 | 56 | 57 | 57 |
| 90th | 105 | 166 | 108 | 110 | 111 | 113 | 113 | 68 | 68 | 69 | 70 | 71 | 72 | 72 | |
| 95th | 109 | 110 | 112 | 114 | 115 | 117 | 117 | 72 | 72 | 73 | 74 | 75 | 76 | 76 | |
| 99th | 116 | 117 | 119 | 121 | 123 | 124 | 125 | 80 | 80 | 81 | 82 | 83 | 84 | 84 | |
| Table Continued | |||||||||||||||
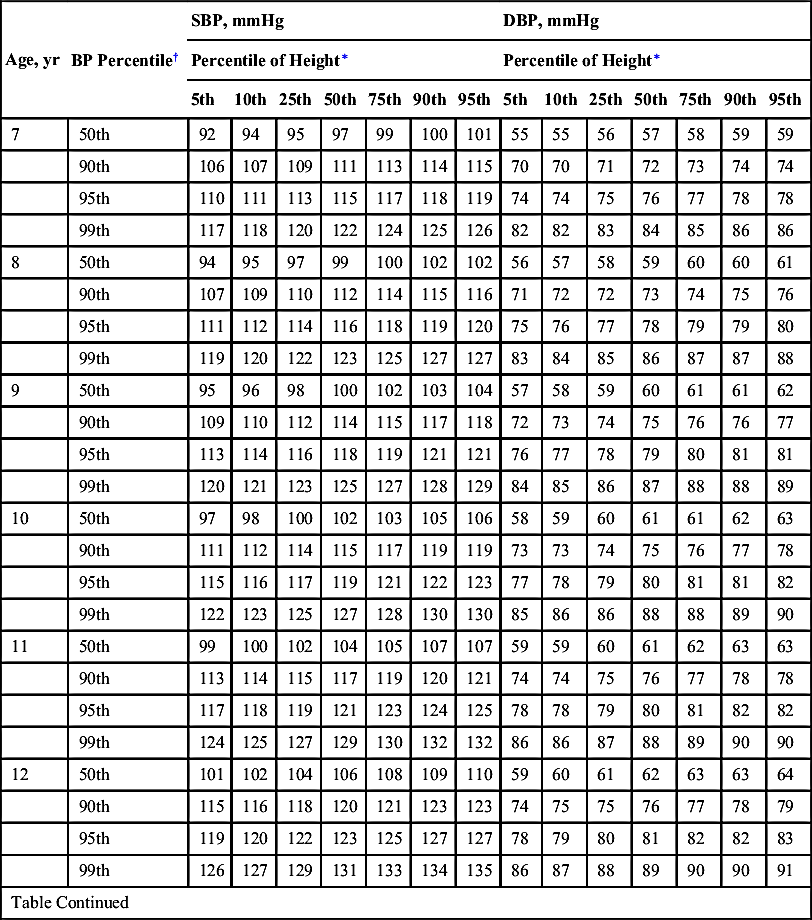
| Age, yr | BP Percentile† | SBP, mmHg | DBP, mmHg | ||||||||||||
| Percentile of Height∗ | Percentile of Height∗ | ||||||||||||||
| 5th | 10th | 25th | 50th | 75th | 90th | 95th | 5th | 10th | 25th | 50th | 75th | 90th | 95th | ||
| 7 | 50th | 92 | 94 | 95 | 97 | 99 | 100 | 101 | 55 | 55 | 56 | 57 | 58 | 59 | 59 |
| 90th | 106 | 107 | 109 | 111 | 113 | 114 | 115 | 70 | 70 | 71 | 72 | 73 | 74 | 74 | |
| 95th | 110 | 111 | 113 | 115 | 117 | 118 | 119 | 74 | 74 | 75 | 76 | 77 | 78 | 78 | |
| 99th | 117 | 118 | 120 | 122 | 124 | 125 | 126 | 82 | 82 | 83 | 84 | 85 | 86 | 86 | |
| 8 | 50th | 94 | 95 | 97 | 99 | 100 | 102 | 102 | 56 | 57 | 58 | 59 | 60 | 60 | 61 |
| 90th | 107 | 109 | 110 | 112 | 114 | 115 | 116 | 71 | 72 | 72 | 73 | 74 | 75 | 76 | |
| 95th | 111 | 112 | 114 | 116 | 118 | 119 | 120 | 75 | 76 | 77 | 78 | 79 | 79 | 80 | |
| 99th | 119 | 120 | 122 | 123 | 125 | 127 | 127 | 83 | 84 | 85 | 86 | 87 | 87 | 88 | |
| 9 | 50th | 95 | 96 | 98 | 100 | 102 | 103 | 104 | 57 | 58 | 59 | 60 | 61 | 61 | 62 |
| 90th | 109 | 110 | 112 | 114 | 115 | 117 | 118 | 72 | 73 | 74 | 75 | 76 | 76 | 77 | |
| 95th | 113 | 114 | 116 | 118 | 119 | 121 | 121 | 76 | 77 | 78 | 79 | 80 | 81 | 81 | |
| 99th | 120 | 121 | 123 | 125 | 127 | 128 | 129 | 84 | 85 | 86 | 87 | 88 | 88 | 89 | |
| 10 | 50th | 97 | 98 | 100 | 102 | 103 | 105 | 106 | 58 | 59 | 60 | 61 | 61 | 62 | 63 |
| 90th | 111 | 112 | 114 | 115 | 117 | 119 | 119 | 73 | 73 | 74 | 75 | 76 | 77 | 78 | |
| 95th | 115 | 116 | 117 | 119 | 121 | 122 | 123 | 77 | 78 | 79 | 80 | 81 | 81 | 82 | |
| 99th | 122 | 123 | 125 | 127 | 128 | 130 | 130 | 85 | 86 | 86 | 88 | 88 | 89 | 90 | |
| 11 | 50th | 99 | 100 | 102 | 104 | 105 | 107 | 107 | 59 | 59 | 60 | 61 | 62 | 63 | 63 |
| 90th | 113 | 114 | 115 | 117 | 119 | 120 | 121 | 74 | 74 | 75 | 76 | 77 | 78 | 78 | |
| 95th | 117 | 118 | 119 | 121 | 123 | 124 | 125 | 78 | 78 | 79 | 80 | 81 | 82 | 82 | |
| 99th | 124 | 125 | 127 | 129 | 130 | 132 | 132 | 86 | 86 | 87 | 88 | 89 | 90 | 90 | |
| 12 | 50th | 101 | 102 | 104 | 106 | 108 | 109 | 110 | 59 | 60 | 61 | 62 | 63 | 63 | 64 |
| 90th | 115 | 116 | 118 | 120 | 121 | 123 | 123 | 74 | 75 | 75 | 76 | 77 | 78 | 79 | |
| 95th | 119 | 120 | 122 | 123 | 125 | 127 | 127 | 78 | 79 | 80 | 81 | 82 | 82 | 83 | |
| 99th | 126 | 127 | 129 | 131 | 133 | 134 | 135 | 86 | 87 | 88 | 89 | 90 | 90 | 91 | |
| Table Continued | |||||||||||||||
| Age, yr | BP Percentile† | SBP, mmHg | DBP, mmHg | ||||||||||||
| Percentile of Height∗ | Percentile of Height∗ | ||||||||||||||
| 5th | 10th | 25th | 50th | 75th | 90th | 95th | 5th | 10th | 25th | 50th | 75th | 90th | 95th | ||
| 13 | 50th | 104 | 105 | 106 | 108 | 110 | 111 | 112 | 60 | 60 | 61 | 62 | 63 | 64 | 64 |
| 90th | 117 | 118 | 120 | 122 | 124 | 125 | 126 | 75 | 75 | 76 | 77 | 78 | 79 | 79 | |
| 95th | 121 | 122 | 124 | 126 | 128 | 129 | 130 | 79 | 79 | 80 | 81 | 82 | 83 | 83 | |
| 99th | 128 | 130 | 131 | 133 | 135 | 136 | 137 | 87 | 87 | 88 | 89 | 90 | 91 | 91 | |
| 14 | 50th | 106 | 107 | 109 | 111 | 113 | 114 | 115 | 60 | 61 | 62 | 63 | 64 | 65 | 65 |
| 90th | 120 | 121 | 123 | 125 | 126 | 128 | 128 | 75 | 76 | 77 | 78 | 79 | 79 | 80 | |
| 95th | 124 | 125 | 127 | 128 | 130 | 132 | 132 | 80 | 80 | 81 | 82 | 83 | 84 | 84 | |
| 99th | 131 | 132 | 134 | 136 | 138 | 139 | 140 | 87 | 88 | 89 | 90 | 91 | 92 | 92 | |
| 15 | 50th | 109 | 110 | 112 | 113 | 115 | 117 | 117 | 61 | 62 | 63 | 64 | 65 | 66 | 66 |
| 90th | 122 | 124 | 125 | 127 | 129 | 130 | 131 | 76 | 77 | 78 | 79 | 80 | 80 | 81 | |
| 95th | 126 | 127 | 129 | 131 | 133 | 134 | 135 | 81 | 81 | 82 | 83 | 84 | 85 | 85 | |
| 99th | 134 | 135 | 136 | 138 | 140 | 142 | 142 | 88 | 89 | 90 | 91 | 92 | 93 | 93 | |
| 16 | 50th | 111 | 112 | 114 | 116 | 118 | 119 | 120 | 63 | 63 | 64 | 65 | 66 | 67 | 67 |
| 90th | 125 | 126 | 128 | 130 | 131 | 133 | 134 | 78 | 78 | 79 | 80 | 81 | 82 | 82 | |
| 95th | 129 | 130 | 132 | 134 | 135 | 137 | 137 | 82 | 83 | 83 | 84 | 85 | 86 | 87 | |
| 99th | 136 | 137 | 139 | 141 | 143 | 144 | 145 | 90 | 90 | 91 | 92 | 93 | 94 | 94 | |
| 17 | 50th | 114 | 115 | 116 | 118 | 120 | 121 | 122 | 65 | 66 | 66 | 67 | 68 | 69 | 70 |
| 90th | 127 | 128 | 130 | 132 | 134 | 135 | 136 | 80 | 80 | 81 | 82 | 83 | 84 | 84 | |
| 95th | 131 | 232 | 134 | 136 | 138 | 139 | 140 | 84 | 85 | 86 | 87 | 87 | 88 | 89 | |
| 99th | 139 | 140 | 141 | 143 | 145 | 146 | 147 | 92 | 93 | 93 | 94 | 95 | 96 | 97 | |
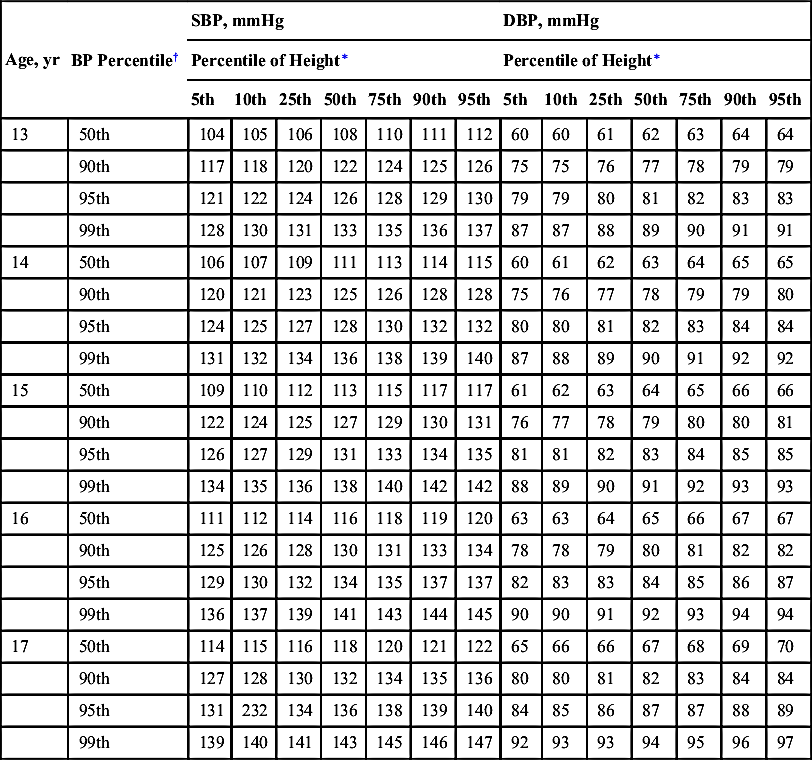
∗ Height percentile determined by standard growth curves.
† Blood pressure percentile determined by a single measurement.
Adapted from National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents: The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004;114(2 Suppl):555–576.
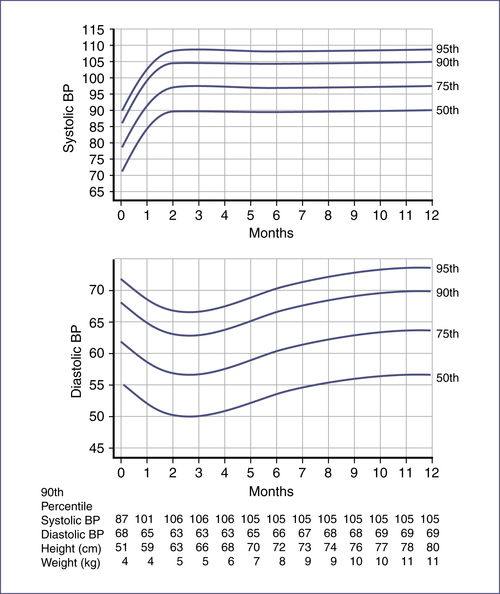
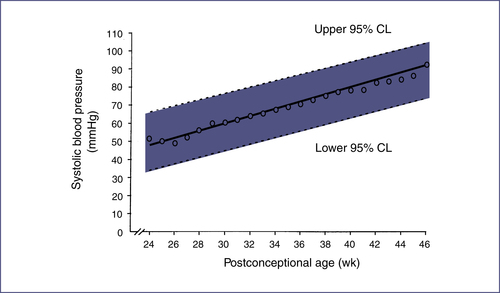
TABLE 7-3
| Type (Timing) | Description of Murmur | Age Group |
| Classic vibratory murmur (Still's murmur; systolic) | Maximal at LMSB or between LLSB and apex Grade 2–3/6 in intensity Low-frequency vibratory, twanging string, groaning, squeaking, or musical | 3–6 yr; occasionally in infancy |
| Pulmonary ejection murmur (systolic) | Maximal at LUSB Early to midsystolic Grade 1–3/6 in intensity Blowing in quality | 8–14 yr |
| Pulmonary flow murmur of newborn (systolic) | Maximal at LUSB Transmits well to left and right chest, axilla, and back Grade 1–2/6 in intensity | Premature and full-term newborns Usually disappears by 3–6 mo |
| Venous hum (continuous) | Maximal at right (or left) supraclavicular and infraclavicular areas Grade 1–3/6 in intensity Inaudible in supine position Intensity changes with rotation of head and disappears with compression of jugular vein. | 3–6 yr |
| Carotid bruit (systolic) | Right supraclavicular area over carotids Grade 2–3/6 in intensity Occasional thrill over carotid | Any age |
LLSB, Left lower sternal border; LMSB, left middle sternal border; LUSB, left upper sternal border.
From Park MK. Pediatric Cardiology for Practitioners. 5th ed. St Louis: Mosby; 2008:36.
IV. Electrocardiography
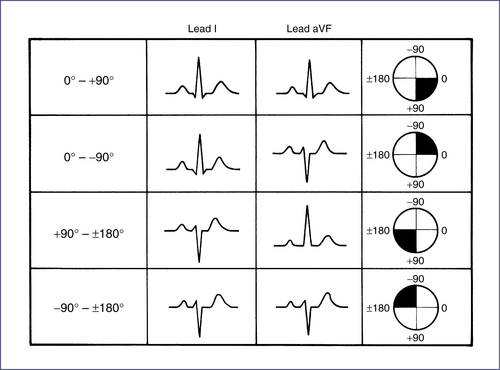
TABLE 7-4
NORMAL PEDIATRIC ELECTROCARDIOGRAM (ECG) PARAMETERS
| Age | Heart Rate (bpm) | QRS Axis∗ | PR Interval (sec)∗ | QRS Duration (sec)† | Lead V1 | Lead V6 | ||||
| R-Wave Amplitude (mm)† | S-Wave Amplitude (mm)† | R/S Ratio | R-Wave Amplitude (mm)† | S-Wave Amplitude (mm)† | R/S Ratio | |||||
| 0–7 days | 95–160 (125) | +30 to 180 (110) | 0.08–0.12 (0.10) | 0.05 (0.07) | 13.3 (25.5) | 7.7 (18.8) | 2.5 | 4.8 (11.8) | 3.2 (9.6) | 2.2 |
| 1–3 wk | 105–180 (145) | +30 to 180 (110) | 0.08–0.12 (0.10) | 0.05 (0.07) | 10.6 (20.8) | 4.2 (10.8) | 2.9 | 7.6 (16.4) | 3.4 (9.8) | 3.3 |
| 1–6 mo | 110–180 (145) | +10 to +125 (+70) | 0.08–0.13 (0.11) | 0.05 (0.07) | 9.7 (19) | 5.4 (15) | 2.3 | 12.4 (22) | 2.8 (8.3) | 5.6 |
| 6–12 mo | 110–170 (135) | +10 to +125 (+60) | 0.10–0.14 (0.12) | 0.05 (0.07) | 9.4 (20.3) | 6.4 (18.1) | 1.6 | 12.6 (22.7) | 2.1 (7.2) | 7.6 |
| 1–3 yr | 90–150 (120) | +10 to +125 (+60) | 0.10–0.14 (0.12) | 0.06 (0.07) | 8.5 (18) | 9 (21) | 1.2 | 14 (23.3) | 1.7 (6) | 10 |
| 4–5 yr | 65–135 (110) | 0 to +110 (+60) | 0.11–0.15 (0.13) | 0.07 (0.08) | 7.6 (16) | 11 (22.5) | 0.8 | 15.6 (25) | 1.4 (4.7) | 11.2 |
| 6–8 yr | 60–130 (100) | −15 to +110 (+60) | 0.12–0.16 (0.14) | 0.07 (0.08) | 6 (13) | 12 (24.5) | 0.6 | 16.3 (26) | 1.1 (3.9) | 13 |
| 9–11 yr | 60–110 (85) | −15 to +110 (+60) | 0.12–0.17 (0.14) | 0.07 (0.09) | 5.4 (12.1) | 11.9 (25.4) | 0.5 | 16.3 (25.4) | 1.0 (3.9) | 14.3 |
| 12–16 yr | 60–110 (85) | −15 to +110 (+60) | 0.12–0.17 (0.15) | 0.07 (0.10) | 4.1 (9.9) | 10.8 (21.2) | 0.5 | 14.3 (23) | 0.8 (3.7) | 14.7 |
| >16 yr | 60–100 (80) | −15 to +110 (+60) | 0.12–0.20 (0.15) | 0.08 (0.10) | 3 (9) | 10 (20) | 0.3 | 10 (20) | 0.8 (3.7) | 12 |
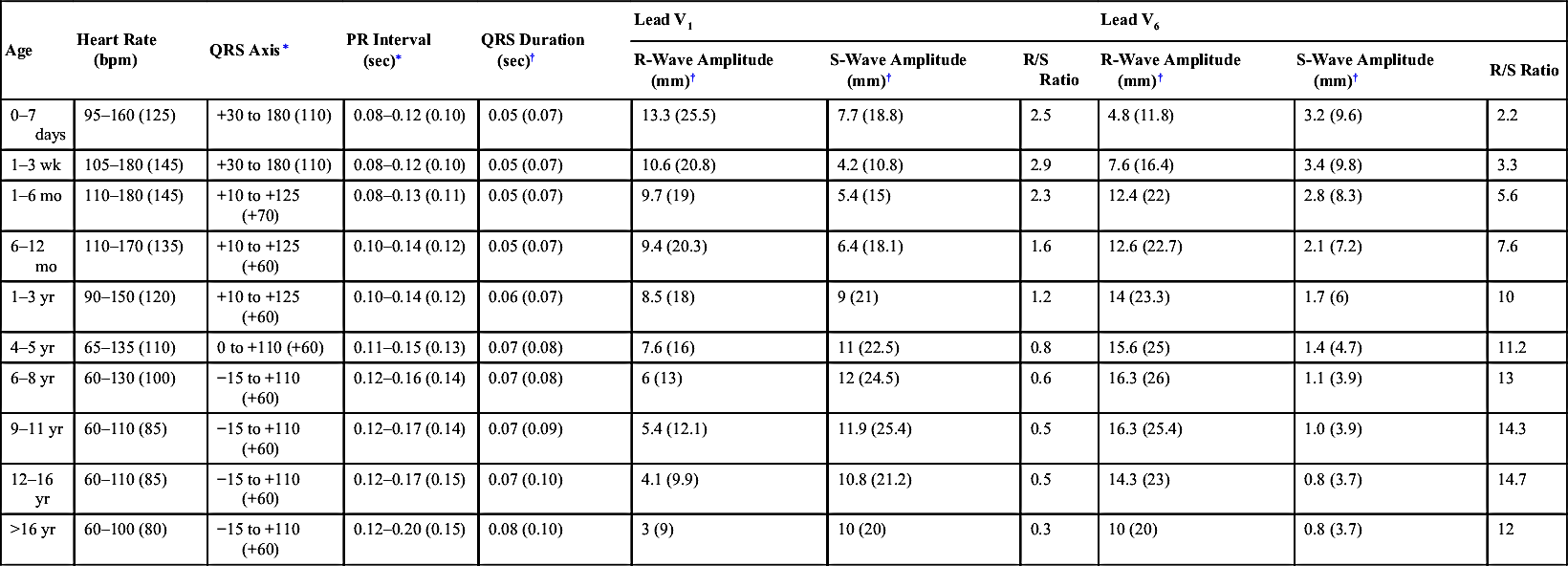
∗ Normal range and (mean).
† Mean and (98th percentile).
Adapted from Park MK. Pediatric Cardiology for Practitioners. 5th ed. St Louis: Mosby; 2008; and Davignon A et al. Normal ECG standards for infants and children. Pediatr Cardiol. 1979;1:123-131.
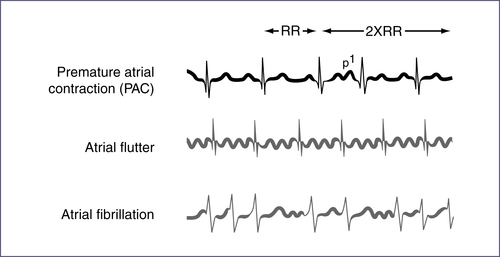
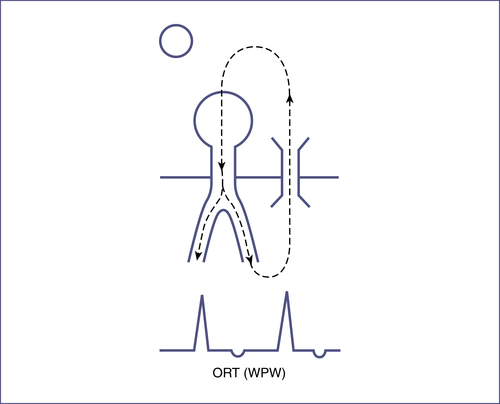
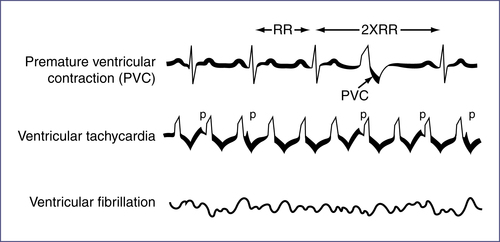
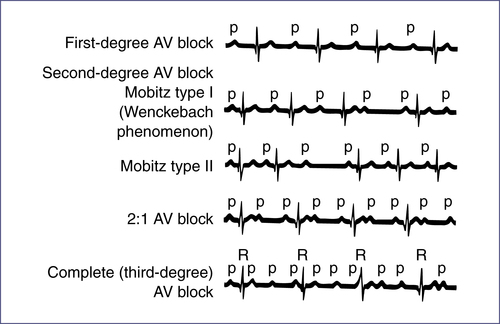
TABLE 7-6
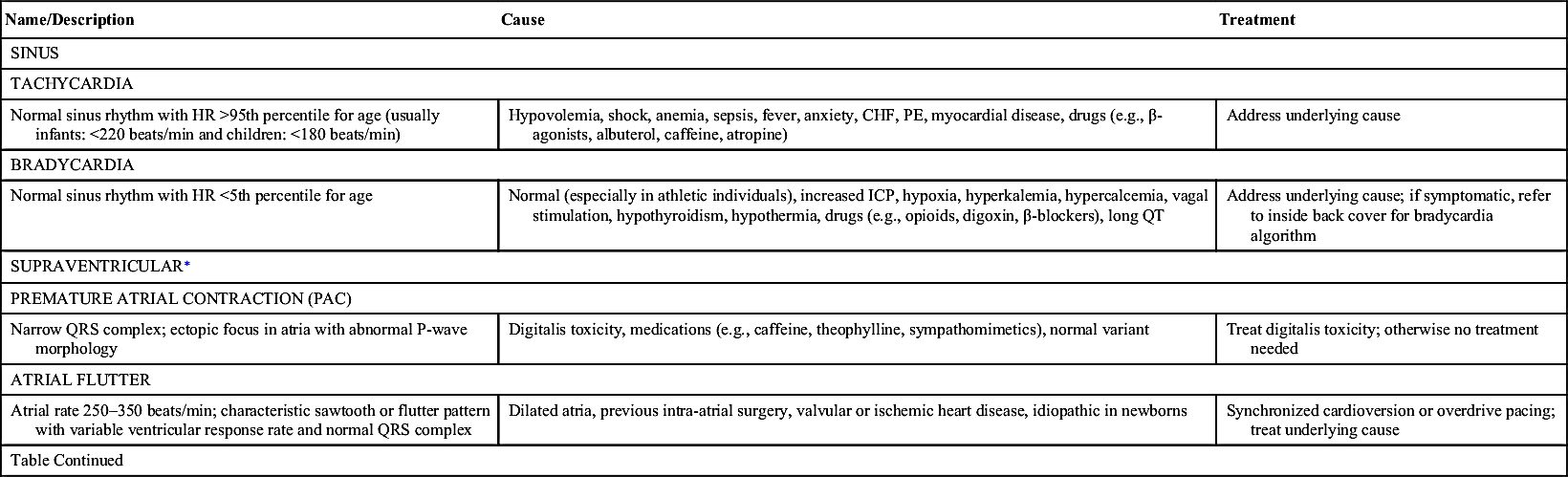
| Name/Description | Cause | Treatment |
| SINUS | ||
| TACHYCARDIA | ||
| Normal sinus rhythm with HR >95th percentile for age (usually infants: <220 beats/min and children: <180 beats/min) | Hypovolemia, shock, anemia, sepsis, fever, anxiety, CHF, PE, myocardial disease, drugs (e.g., β-agonists, albuterol, caffeine, atropine) | Address underlying cause |
| BRADYCARDIA | ||
| Normal sinus rhythm with HR <5th percentile for age | Normal (especially in athletic individuals), increased ICP, hypoxia, hyperkalemia, hypercalcemia, vagal stimulation, hypothyroidism, hypothermia, drugs (e.g., opioids, digoxin, β-blockers), long QT | Address underlying cause; if symptomatic, refer to inside back cover for bradycardia algorithm |
| SUPRAVENTRICULAR∗ | ||
| PREMATURE ATRIAL CONTRACTION (PAC) | ||
| Narrow QRS complex; ectopic focus in atria with abnormal P-wave morphology | Digitalis toxicity, medications (e.g., caffeine, theophylline, sympathomimetics), normal variant | Treat digitalis toxicity; otherwise no treatment needed |
| ATRIAL FLUTTER | ||
| Atrial rate 250–350 beats/min; characteristic sawtooth or flutter pattern with variable ventricular response rate and normal QRS complex | Dilated atria, previous intra-atrial surgery, valvular or ischemic heart disease, idiopathic in newborns | Synchronized cardioversion or overdrive pacing; treat underlying cause |
| Table Continued | ||
| Name/Description | Cause | Treatment |
| ATRIAL FIBRILLATION | ||
| Irregular; atrial rate 350–600 beats/min, yielding characteristic fibrillatory pattern (no discrete P waves) and irregular ventricular response rate of about 110–150 beats/min with normal QRS complex | Wolff-Parkinson-White syndrome and those listed previously for atrial flutter (except not idiopathic), alcohol exposure, familial | Synchronized cardioversion; then may need anticoagulation pretreatment |
| SVT | ||
| Sudden run of three or more consecutive premature supraventricular beats at >220 beats/min(infant) or >180 beats/min (child), with narrow QRS complex and absent/abnormal P wave; either sustained (>30 sec) or nonsustained | Most commonly idiopathic but may be seen in congenital heart disease (e.g., Ebstein anomaly, transposition) | Vagal maneuvers, adenosine; if unstable, need immediate synchronized cardioversion (0.5 J/kg up to 1 J/kg). Consult cardiologist. See “Tachycardia with Poor Perfusion” or “Tachycardia with Adequate Perfusion” algorithms in back of handbook. |
| I. AV Reentrant: Presence of accessory bypass pathway, in conjunction with AV node, establishes cyclic pattern of reentry independent of SA node; most common cause of nonsinus tachycardia in children (see Wolff-Parkinson-White syndrome, Table 7-9 and Fig. 7-10) | ||
| II. Junctional: Automatic focus; simultaneous depolarization of atria and ventricles yields invisible P wave or retrograde P wave | Cardiac surgery, idiopathic | Adjust for clinical situation; consult cardiology |
| III. Ectopic atrial tachycardia: Rapid firing of ectopic focus in atrium | Idiopathic | AV nodal blockade, ablation |
| NODAL ESCAPE/JUNCTIONAL RHYTHM | ||
| Abnormal rhythm driven by AV node impulse, giving normal QRS complex and invisible P wave (buried in preceding QRS or T wave) or retrograde P wave (negative in lead II, positive in aVR); seen in sinus bradycardia | Common after surgery of atria | Often requires no treatment. If rate is slow enough, may require pacemaker. |

AV, Atrioventricular; CHF, congestive heart failure; HR, heart rate; ICP, intracranial pressure; PE, pulmonary embolism; SA, sinoatrial; SVT, supraventricular tachycardia.
∗ Abnormal rhythm resulting from ectopic focus in atria or AV node, or from accessory conduction pathways. Characterized by different P-wave shape and abnormal P-wave axis. QRS morphology usually normal. See Figures 7-9, 7-10.6
TABLE 7-7
| Name/Description | Cause | Treatment |
| PREMATURE VENTRICULAR CONTRACTION (PVC) | ||
| Ectopic ventricular focus causing early depolarization. Abnormally wide QRS complex appears prematurely, usually with full compensatory pause. May be unifocal or multifocal. Bigeminy: Alternating normal and abnormal QRS complexes. Trigeminy: Two normal QRS complexes followed by an abnormal one. Couplet: Two consecutive PVCs. | Myocarditis, myocardial injury, cardiomyopathy, long QT, congenital and acquired heart disease, drugs (catecholamines, theophylline, caffeine, anesthetics), MVP, anxiety, hypokalemia, hypoxia, hypomagnesemia. Can be normal variant. | None. More worrisome if associated with underlying heart disease or syncope, if worse with activity, or if they are multiform (especially couplets). Address underlying cause, rule out structural heart disease. |
| VENTRICULAR TACHYCARDIA | ||
| Series of three or more PVCs at rapid rate (120–250 beats/min), with wide QRS complex and dissociated, retrograde, or no P wave | See causes of PVCs (70% have underlying cause). | See “Tachycardia with Poor Perfusion” and “Tachycardia with Adequate Perfusion” algorithms in back of handbook. |
| VENTRICULAR FIBRILLATION | ||
| Depolarization of ventricles in uncoordinated asynchronous pattern, yielding abnormal QRS complexes of varying size and morphology with irregular, rapid rate. Rare in children. | Myocarditis, MI, postoperative state, digitalis or quinidine toxicity, catecholamines, severe hypoxia, electrolyte disturbances, long QT | Requires immediate defibrillation. See algorithm for “Asystole and Pulseless Arrest” at back of book. |

TABLE 7-8
NONVENTRICULAR CONDUCTION DISTURBANCES
| Name/Description∗ | Cause | Treatment |
| FIRST-DEGREE HEART BLOCK | ||
| Abnormal but asymptomatic delay in conduction through AV node, yielding prolongation of PR interval | Acute rheumatic fever, tickborne (i.e., Lyme) disease, connective tissue disease, congenital heart disease, cardiomyopathy, digitalis toxicity, postoperative state, normal children | No specific treatment except address the underlying cause |
| SECOND-DEGREE HEART BLOCK: MOBITZ TYPE I (WENCKEBACH) | ||
| Progressive lengthening of PR interval until a QRS complex is not conducted. Common finding in asymptomatic teenagers. | Myocarditis, cardiomyopathy, congenital heart disease, postoperative state, MI, toxicity (digitalis, β-blocker), normal children, Lyme disease, lupus | Address underlying cause, or none needed |
| SECOND-DEGREE HEART BLOCK: MOBITZ TYPE II | ||
| Loss of conduction to ventricle without lengthening of the PR interval. May progress to complete heart block. | Same as for Mobitz type I | Address underlying cause; may need pacemaker |
| THIRD-DEGREE (COMPLETE) HEART BLOCK | ||
| Complete dissociation of atrial and ventricular conduction, with atrial rate faster than ventricular rate. P wave and PP interval regular; RR interval regular and much slower. | Congenital due to maternal lupus or other connective tissue disease | If bradycardic and symptomatic, consider pacing; see bradycardia algorithm at back of book. |
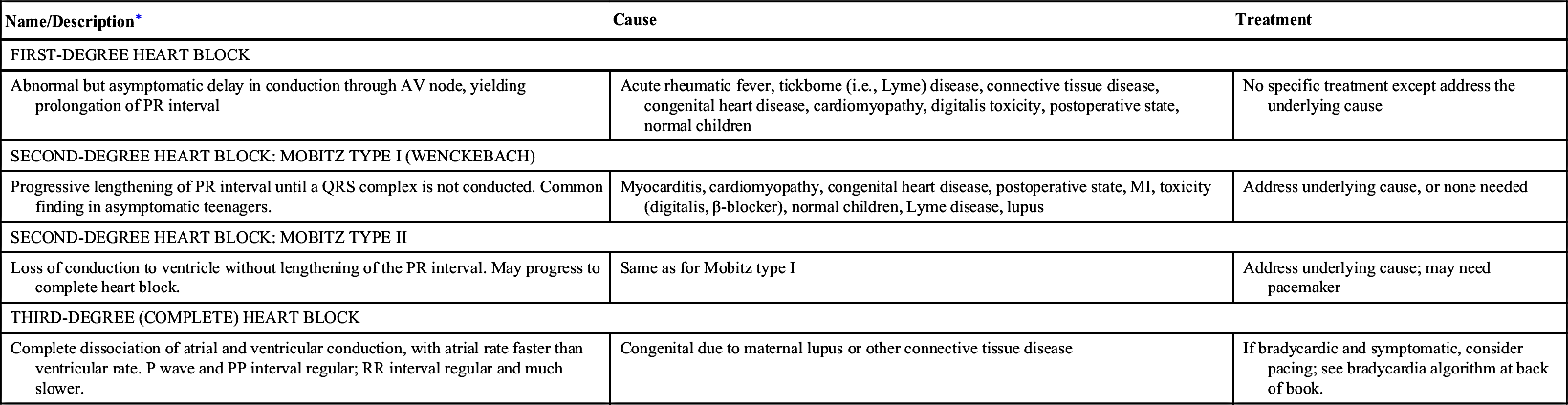
AV, Atrioventricular; MI, myocardial infarction.
∗ High-degree AV block: Conduction of atrial impulse at regular intervals, yielding 2:1 block (two atrial impulses for each ventricular response), 3:1 block, etc.
TABLE 7-9
VENTRICULAR CONDUCTION DISTURBANCES
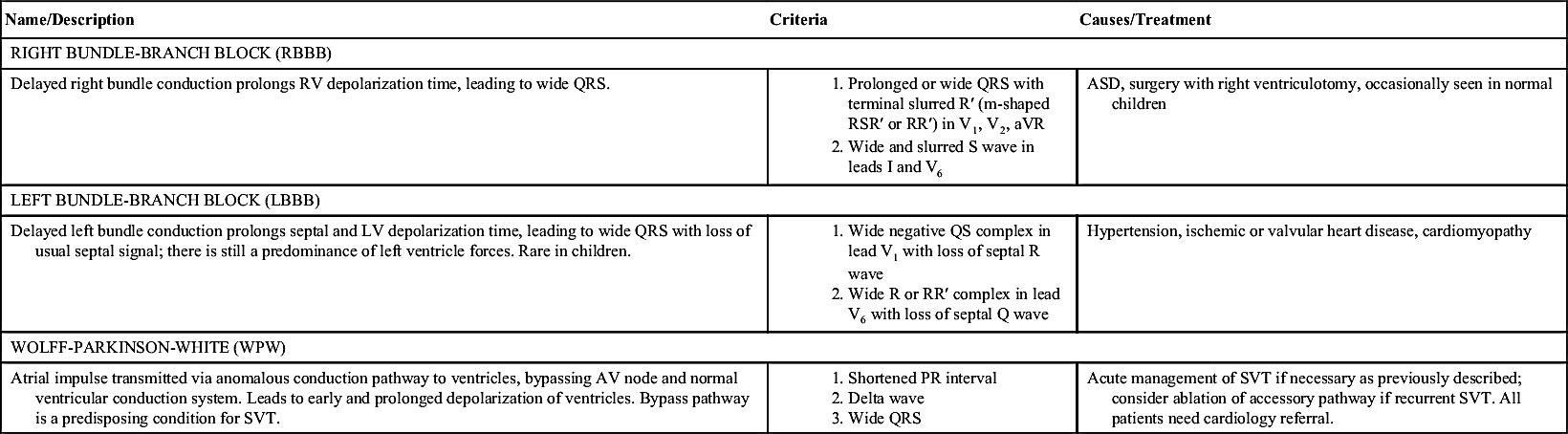
ASD, Atrial septal defect; LV, left ventricle; RV, right ventricle; SVT, supraventricular tachycardia.
TABLE 7-10
SYSTEMIC EFFECTS ON ELECTROCARDIOGRAM
| Short QT | Long QT-U | Prolonged QRS | ST-T Changes | Sinus Tachycardia | Sinus Bradycardia | AV Block | Ventricular Tachycardia | Miscellaneous | |
| CHEMISTRY | |||||||||
| Hyperkalemia | X | X | X | X | Low-voltage Ps; peaked Ts | ||||
| Hypokalemia | X | X | |||||||
| Hypercalcemia | X | X | X | X | |||||
| Hypocalcemia | X | X | X | ||||||
| Hypermagnesemia | X | ||||||||
| Hypomagnesemia | X | ||||||||
| DRUGS | |||||||||
| Digitalis | X | X | T | X | T | ||||
| Phenothiazines | T | T | |||||||
| Phenytoin | X | ||||||||
| Propranolol | X | X | X | ||||||
| Tricyclics | T | T | T | T | T | T | |||
| Verapamil | X | X | |||||||
| Table Continued | |||||||||
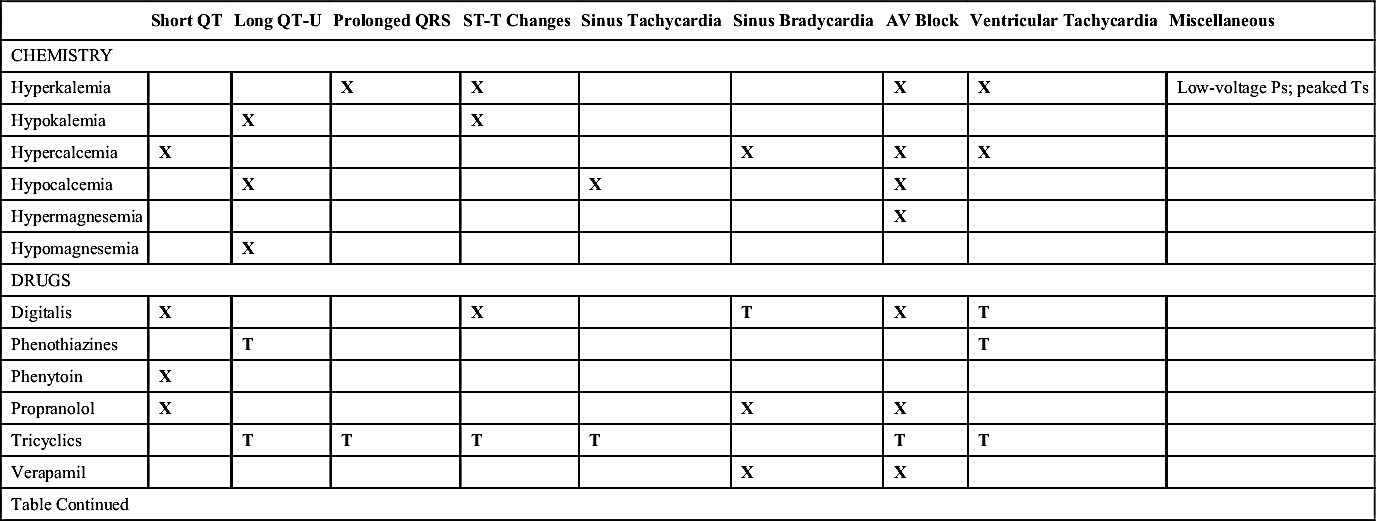
| Short QT | Long QT-U | Prolonged QRS | ST-T Changes | Sinus Tachycardia | Sinus Bradycardia | AV Block | Ventricular Tachycardia | Miscellaneous | |
| MISCELLANEOUS | |||||||||
| CNS injury | X | X | X | X | X | ||||
| Friedreich ataxia | X | X | Atrial flutter | ||||||
| Duchenne muscular dystrophy | X | X | Atrial flutter | ||||||
| Myotonic dystrophy | X | X | X | X | |||||
| Collagen vascular disease | X | X | X | ||||||
| Hypothyroidism | X | Low voltage | |||||||
| Hyperthyroidism | X | X | X | X | |||||
| Lyme disease | X | X | |||||||
| Holt-Oram, maternal lupus | X | ||||||||
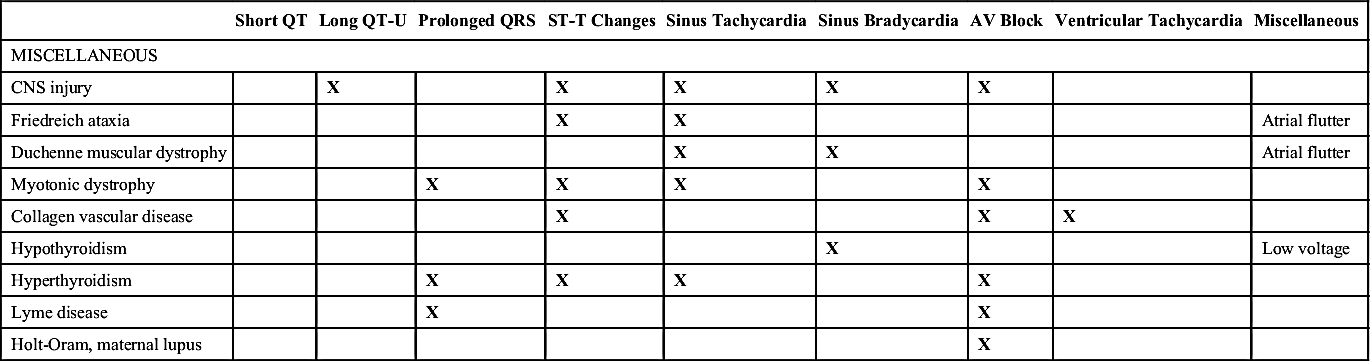
CNS, Central nervous system; T, present only with drug toxicity; X, present.
Adapted from Garson A Jr. The Electrocardiogram in Infants and Children: A Systematic Approach. Philadelphia: Lea & Febiger; 1983:172; and Walsh EP. Cardiac arrhythmias. In: Fyler DC, Nadas A,eds. Pediatric Cardiology. Philadelphia: Hanley & Belfus; 1992:141-143.
V. Imaging
VI. Congenital Heart Disease
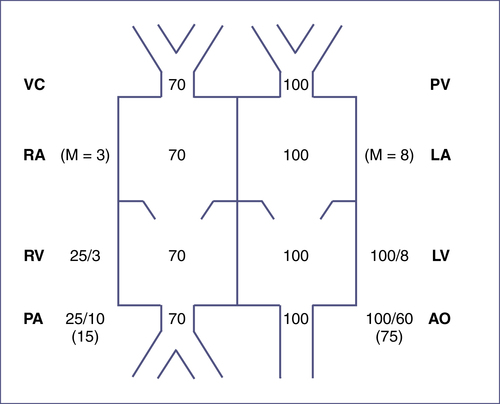
TABLE 7-11
MAJOR SYNDROMES ASSOCIATED WITH CARDIAC DEFECTS
| Syndrome | Dominant Cardiac Defect |
| CHARGE | TOF, truncus arteriosus, aortic arch abnormalities |
| DiGeorge | Aortic arch anomalies, TOF, truncus arteriosus, VSD, PDA |
| Trisomy 21 | Atrioventricular septal defect, VSD |
| Marfan | Aortic root dilation, mitral valve prolapse |
| Loeys-Dietz | Aortic root dilation with higher risk of rupture at smaller dimensions |
| Noonan | Supravalvular pulmonic stenosis, LVH |
| Turner | COA, bicuspid aortic valve, aortic root dilation as a teenager |
| Williams | Supravalvular aortic stenosis, pulmonary artery stenosis |
| FAS | Occasional: VSD, PDA, ASD, TOF |
| IDM | TGA, VSD, COA, cardiomyopathy |
| VATER/VACTERL | VSD |
| VCFS | Truncus arteriosus, TOF, pulmonary atresia with VSD, TGA, interrupted aortic arch |
ASD, Atrial septal defect; CHARGE, a syndrome of associated defects including Coloboma of the eye, Heart anomaly, choanal Atresia, Retardation, and Genital and Ear anomalies; COA, coarctation of aorta; FAS, fetal alcohol syndrome; IDM, infant of diabetic mother; LVH, left ventricular hypertrophy; PDA, patent ductus arteriosis; TGA, transposition of the great arteries; TOF, tetralogy of Fallot; VATER/VACTERL, association of Vertebral anomalies, Anal atresia, Cardiac anomalies, Tracheoesophageal fistula, Renal/radial anomalies, Limb defects; VCFS, velocardiofacial syndrome; VSD, ventricular septal defect.
Adapted from Park MK. Pediatric Cardiology for Practitioners. 5th ed. St Louis: Mosby; 2008:10-12.
TABLE EC 7-B
INTERPRETATION OF OXYGEN CHALLENGE TEST
| Condition | FIO2= 0.21 PaO2 (% Saturation) | FIO2= 1.00 PaO2 (% Saturation) | PaCO2 | |
| Normal | 70 (95) | >200 (100) | 35 | |
| Pulmonary disease | 50 (85) | >150 (100) | 50 | |
| Neurologic disease | 50 (85) | >150 (100) | 50 | |
| Methemoglobinemia | 70 (85) | >200 (85) | 35 | |
| Cardiac disease | ||||
| • Separate circulation∗ | <40 (<75) | <50 (<85) | 35 | |
| • Restricted PBF† | <40 (<75) | <50 (<85) | 35 | |
| • Complete mixing without restricted PBF‡ | 50 (85) | <150 (<100) | 35 | |
| Persistent pulmonary hypertension | Preductal | Postductal | ||
| PFO (no R–L shunt) | 70 (95) | <40 (<75) | Variable | 35–50 |
| PFO (with R–L shunt) | <40 (<75) | <40 (<75) | Variable | 35–50 |
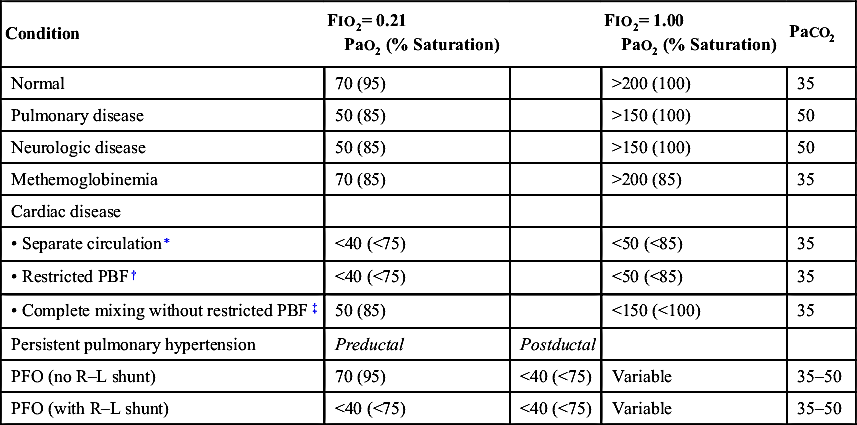
PBF, Pulmonary blood flow; PFO, patent foramen ovale.
∗ D-Transposition of the great arteries (D-TGA) with intact ventricular septum.
† Tricuspid atresia with pulmonary stenosis or atresia, pulmonary atresia or critical pulmonary stenosis with intact ventricular septum, or tetralogy of Fallot.
‡ Truncus, total anomalous pulmonary venous return, single ventricle, hypoplastic left heart, D-TGA with ventricular septal defect, tricuspid atresia without pulmonary stenosis or atresia.
Adapted from Lees MH. Cyanosis of the newborn infant: Recognition and clinical evaluation. J Pediatr. 1970;77:484; Kitterman JA. Cyanosis in the newborn infant. Pediatr Rev. 1982;4:13; and Jones RW, Baumer JH, Joseph MC, et al. Arterial oxygen tension and response to oxygen breathing in differential diagnosis of heart disease in infancy. Arch Dis Child. 1976;51:667-673.
TABLE 7-12
ACYANOTIC CONGENITAL HEART DISEASE
| Lesion Type | % of CHD/Examination Findings | CDG Findings | Chest Radiograph Findings |
| Ventricular septal defect (VSD) | 2–5/6 holosystolic murmur, loudest at the LLSB, ± systolic thrill ± apical diastolic rumble with large shunt With large VSD and pulmonary hypertension, S2 may be narrow | Small VSD: Normal Medium VSD: LVH ± LAE Large VSD: BVH ± LAE, pure RVH | May show cardiomegaly and increased PVMs, depending on amount of left-to-right shunting |
| Atrial septal defect (ASD) | Wide, fixed split S2 with grade 2–3/6 SEM at the LUSB May have mid-diastolic rumble at LLSB | Small ASD: Normal Large ASD: RAD and mild RVH or RBBB with RSR′ in V1 | May show cardiomegaly with increased PVMs if hemodynamically significant ASD |
| Patent ductus arteriosus (PDA) | 40%–60% in VLBW infants 1–4/6 continuous “machinery” murmur loudest at LUSB Wide pulse pressure | Small–moderate PDA: Normal or LVH Large PDA: BVH | May have cardiomegaly and increased PVMs, depending on size of shunt (see Chapter 18 Section IX.A for treatment) |
| Atrioventricular septal defects | Most occur in Down syndrome Hyperactive precordium with systolic thrill at LLSB and loud S2 ± grade 3–4/6 holosystolic regurgitant murmur along LLSB ± systolic murmur of MR at apex ± mid-diastolic rumble at LLSB or at apex ± gallop rhythm | Superior QRS axis RVH and LVH may be present | Cardiomegaly with increased PVMs |
| Pulmonary stenosis (PS) | Ejection click at LUSB with valvular PS—click intensity varies with respiration, decreasing with inspiration and increasing with expiration S2 may split widely with P2 diminished in intensity SEM (2–5/6) ± thrill at LUSB with radiation to back and sides | Mild PS: Normal Moderate PS: RAD and RVH Severe PS: RAE and RVH with strain | Normal heart size with normal to decreased PVMs |
| Aortic stenosis (AS) | Systolic thrill at RUSB, suprasternal notch, or over carotids Ejection click that does not vary with respiration if valvular AS Harsh SEM (2–4/6) at second RICS or third LICS, with radiation to neck and apex ± early diastolic decrescendo murmur due to AR Narrow pulse pressure if severe stenosis | Mild AS: Normal Moderate–severe AS: LVH ± strain | Usually normal |
| Table Continued | |||
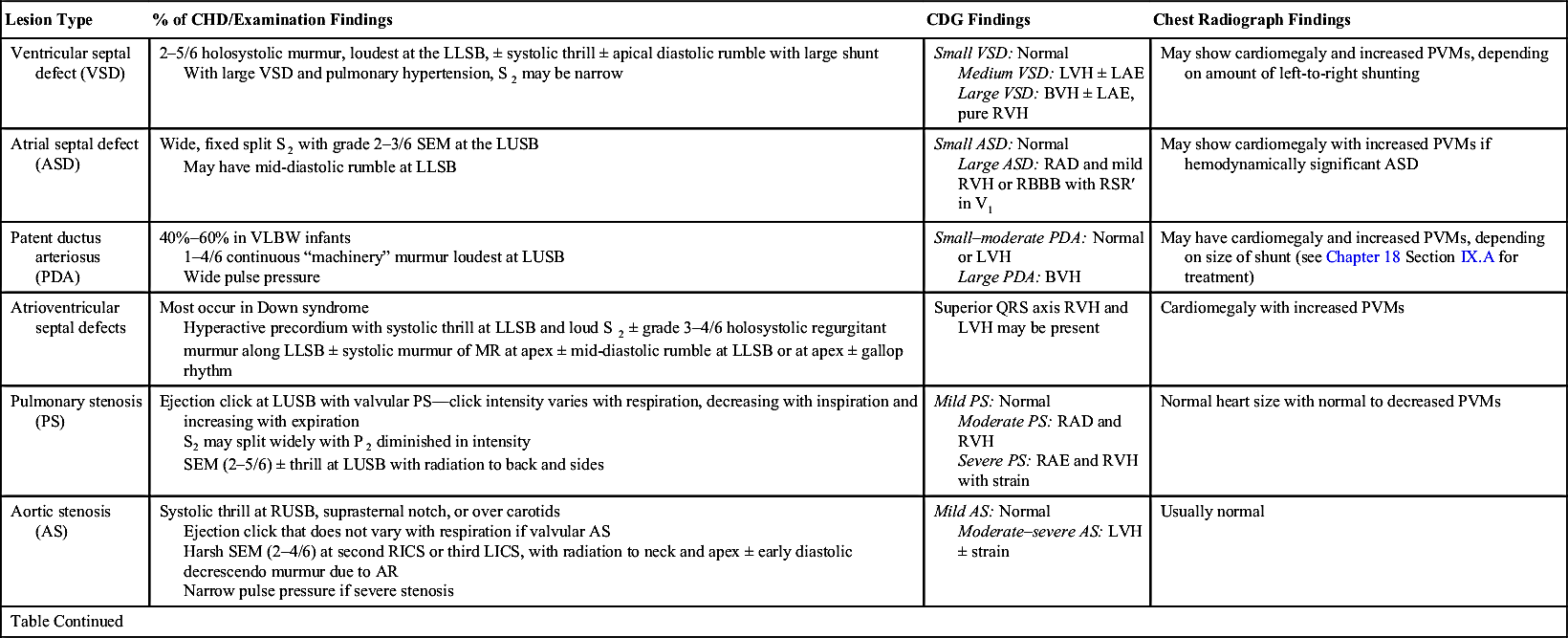
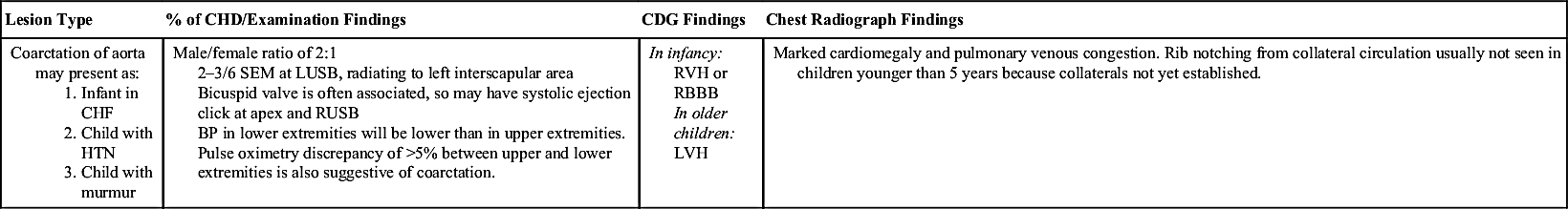
AR, Aortic regurgitation; ASD, atrial septal defect; BP, blood pressure; BVH, biventricular hypertrophy; CHD, congenital heart disease; CHF, congestive heart failure; HTN, hypertension; LAE, left atrial enlargement; LICS, left intercostal space; LLSB, left lower sternal border; LUSB, left upper sternal border; LVH, left ventricular hypertrophy; MR, mitral regurgitation; PVM, pulmonary vascular markings; RAD, right axis deviation; RAE, right atrial enlargement; RBBB, right bundle-branch block; RICS, right intercostal space; RUSB, right upper sternal border; RVH, right ventricular hypertrophy; SEM, systolic ejection murmur; VLBW, very low birth weight (i.e. <1500 g); VSD, ventricular septal defect.
TABLE 7-13
CYANOTIC CONGENITAL HEART DISEASE
| Lesion | Examination Findings | ECG Findings | Chest Radiograph Findings |
| Tetralogy of Fallot: 1. Large VSD 2. RVOT obstruction 3. RVH 4. Overriding aorta Degree of RVOT obstruction will determine whether there is clinical cyanosis. If PS is mild, there will be a left-to-right shunt, and child will be acyanotic. Increased obstruction leads to increased right-to-left shunting across VSD, and child will be cyanotic. | Loud SEM at LMSB and LUSB and a loud, single S2 ± thrill at LMSB and LLSB. Tet spells: Occur in young infants. As RVOT obstruction increases or systemic resistance decreases, right-to-left shunting across VSD occurs. May present with tachypnea, increasing cyanosis, and decreasing murmur. See Table 7-14 for treatment. | RAD and RVH | Boot-shaped heart with normal heart size ± decreased PVMs |
| Table Continued | |||
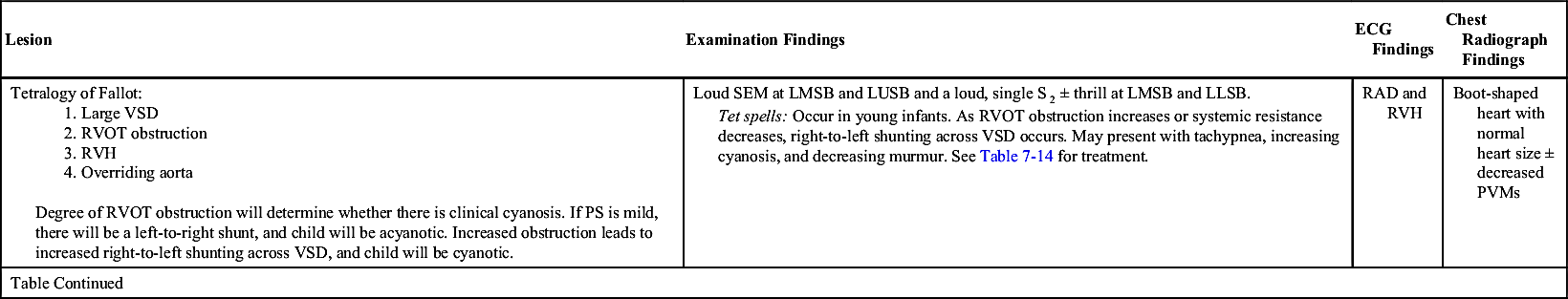
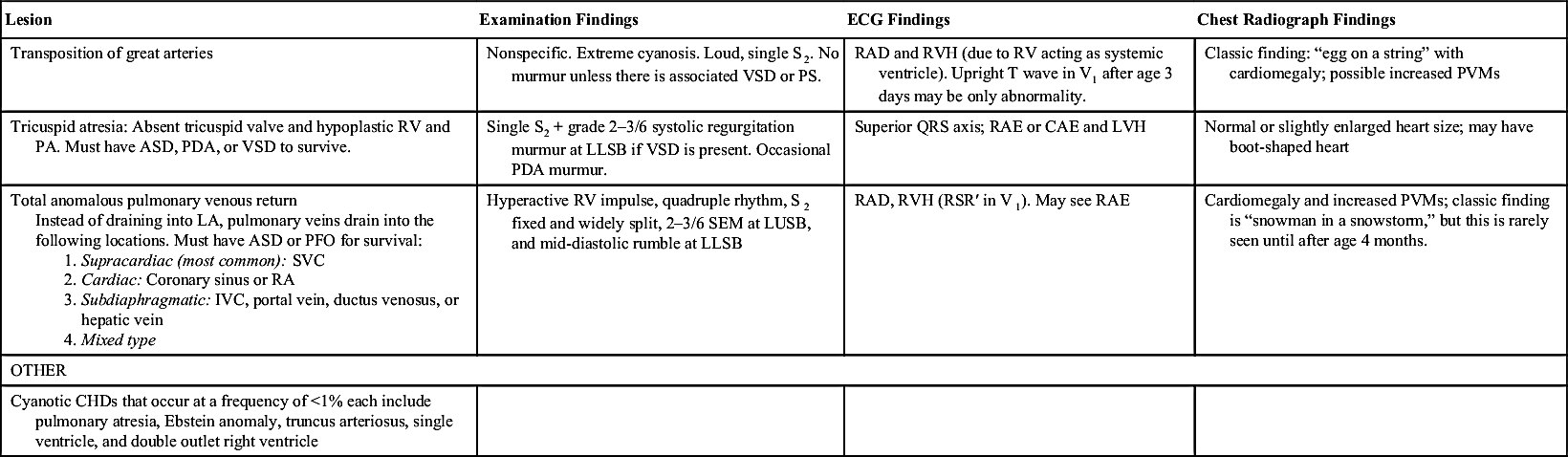
ASD, Atrial septal defect; CAE, common atrial enlargement; ECG, electrocardiogram; IVC, inferior vena cava; LA, left atrium; LLSB, left lower sternal border; LMSB, left mid-sternal border; LUSB, left upper sternal border; LVH, left ventricular hypertrophy; PA, pulmonary artery; PDA, patent ductus arteriosus; PFO, patent foramen ovale; PVM, pulmonary vascular markings; PS, pulmonary stenosis; RA, right atrium; RAD, right-axis deviation; RAE, right atrial enlargement; RV, right ventricle; RVH, right ventricular hypertrophy; RVOT, right ventricular outflow tract; SEM, systolic ejection murmur; SVC, superior vena cava; VSD, ventricular septal defect.
TABLE 7-14
TREATMENT OPTIONS FOR TET SPELLS
| Treatment | Rationale |
| INITIAL OPTIONS | |
| Calm child | Decreases PVR |
| Encourage knee-chest position | Decreases venous return and increases SVR |
| Oxygen | Reduces hypoxemia, decreases PVR |
| Intravenous fluids | Provides volume resuscitation |
| Morphine (morphine sulfate 0.1–0.2 mg/kg SQ or IM) | Decreases venous return, decreases PVR, relaxes infundibulum. Do not try to establish IV access initially; use SQ route. |
| IF THERE IS NO RESPONSE TO INITIAL MEASURES | |
| Phenylephrine (0.02 mg/kg IV) | Increases SVR |
| Propranolol (0.01–0.25 mg/kg slow IV push) | Has negative inotropic effect on infundibular myocardium; may block drop in SVR |
| Ketamine 1–3 mg/kg | Increases SVR and sedates |
| OTHER | |
| Correct anemia | Increases delivery of oxygen to tissues |
| Correct pathologic tachyarrhythmias | May abort hypoxic spell |
| Infuse glucose | Avoids hypoglycemia from increased utilization and depletion of glycogen stores |
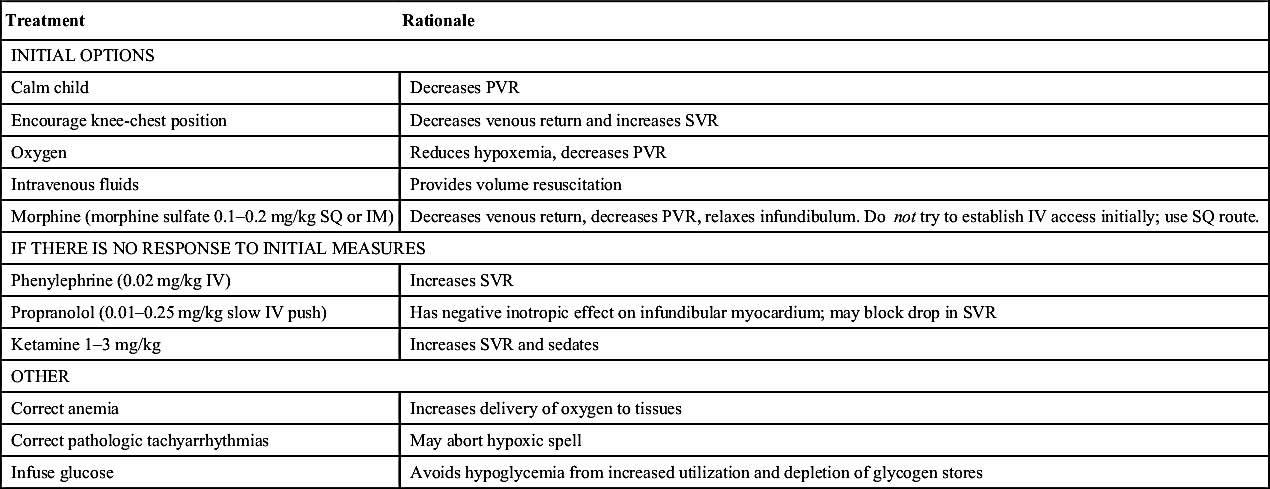
IM, Intramuscular; IV, intravenous; PVR, peripheral venous resistance; SQ, subcutaneous; SVR, systemic vascular resistance.
From Park MK. Pediatric Cardiology for Practitioners. 5th ed. St Louis: Mosby; 2008:239.
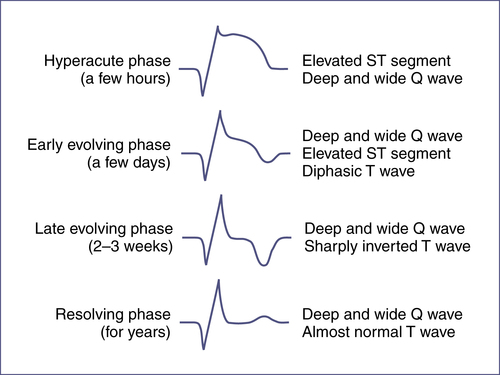
VII. Acquired Heart Disease
TABLE 7-15
PROPHYLACTIC REGIMENS FOR DENTAL AND RESPIRATORY TRACT PROCEDURES
| Drug | Dosing∗ (not to exceed adult dose) |
| Amoxicillin† | Adult: 2 g; Child: 50 mg/kg PO |
| Ampicillin | Adult: 2 g; Child: 50 mg/kg IM/IV |
| Cefazolin or ceftriaxone‡ | Adult: 1 g; Child: 50 mg/kg IM/IV |
| Cephalexin‡ | Adult: 2 g; Child: 50 mg/kg PO |
| Clindamycin | Adult: 600 mg; Child: 20 mg/kg PO/IM/IV |
| Azithromycin/clarithromycin | Adult: 500 mg; Child:15 mg/kg PO |
∗ Oral (PO) medications should be given 1 hour before procedure; intramuscular/intravenous (IM/IV) medications should be given within 30 min prior to procedure.
† Standard general prophylaxis.
‡ Cephalosporins should not be used in persons with intermediate-type hypersensitivity reaction to penicillins or ampicillin.
Adapted from Wilson W, Taubert KA, Gewitz M, et al. Prevention of infectiveendocarditis: Guidelines from the American Heart Association: A guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2007;116:1736-1754.
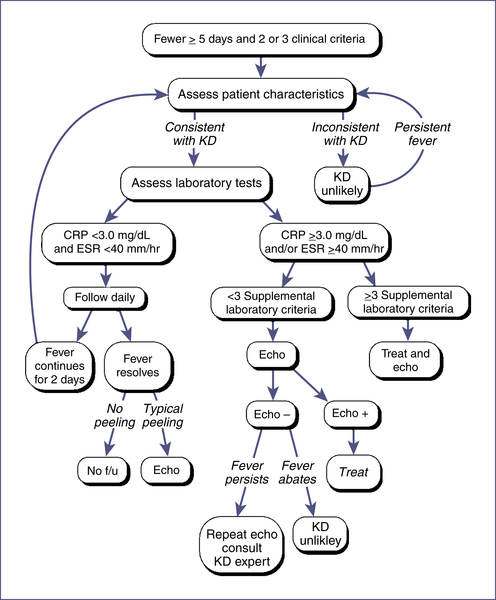
TABLE EC 7-C
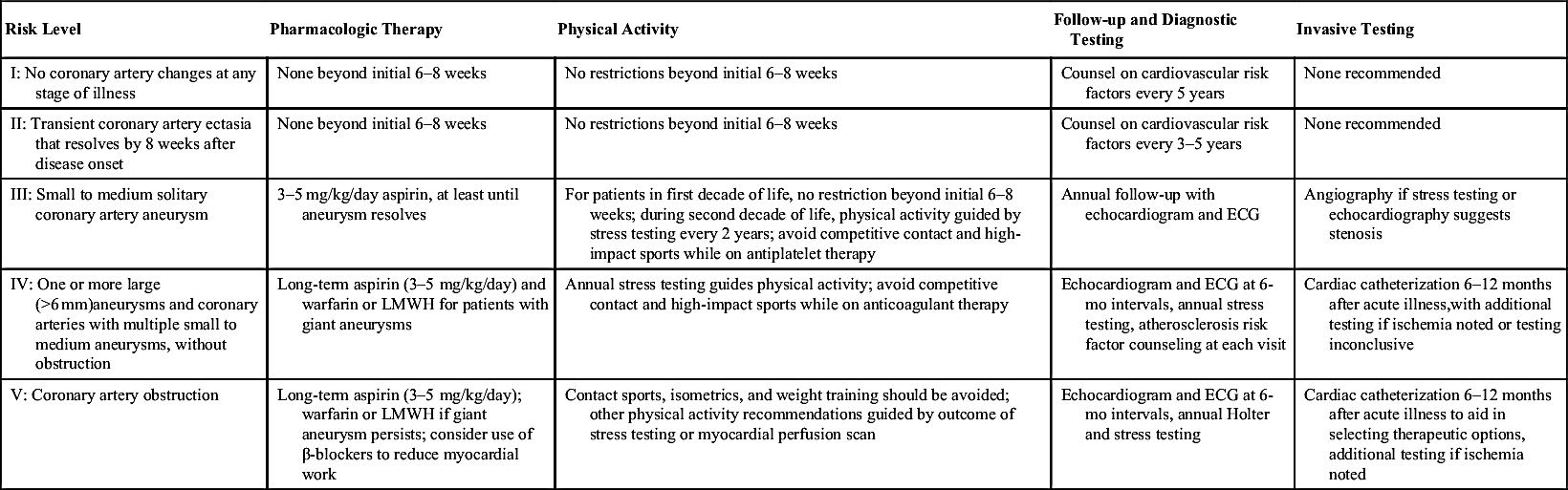
GUIDELINES FOR TREATMENT AND FOLLOW-UP OF CHILDREN WITH KAWASAKI DISEASE
| Risk Level | Pharmacologic Therapy | Physical Activity | Follow-up and Diagnostic Testing | Invasive Testing |
| I: No coronary artery changes at any stage of illness | None beyond initial 6–8 weeks | No restrictions beyond initial 6–8 weeks | Counsel on cardiovascular risk factors every 5 years | None recommended |
| II: Transient coronary artery ectasia that resolves by 8 weeks after disease onset | None beyond initial 6–8 weeks | No restrictions beyond initial 6–8 weeks | Counsel on cardiovascular risk factors every 3–5 years | None recommended |
| III: Small to medium solitary coronary artery aneurysm | 3–5 mg/kg/day aspirin, at least until aneurysm resolves | For patients in first decade of life, no restriction beyond initial 6–8 weeks; during second decade of life, physical activity guided by stress testing every 2 years; avoid competitive contact and high-impact sports while on antiplatelet therapy | Annual follow-up with echocardiogram and ECG | Angiography if stress testing or echocardiography suggests stenosis |
| IV: One or more large (>6 mm)aneurysms and coronary arteries with multiple small to medium aneurysms, without obstruction | Long-term aspirin (3–5 mg/kg/day) and warfarin or LMWH for patients with giant aneurysms | Annual stress testing guides physical activity; avoid competitive contact and high-impact sports while on anticoagulant therapy | Echocardiogram and ECG at 6-mo intervals, annual stress testing, atherosclerosis risk factor counseling at each visit | Cardiac catheterization 6–12 months after acute illness,with additional testing if ischemia noted or testing inconclusive |
| V: Coronary artery obstruction | Long-term aspirin (3–5 mg/kg/day); warfarin or LMWH if giant aneurysm persists; consider use of β-blockers to reduce myocardial work | Contact sports, isometrics, and weight training should be avoided; other physical activity recommendations guided by outcome of stress testing or myocardial perfusion scan | Echocardiogram and ECG at 6-mo intervals, annual Holter and stress testing | Cardiac catheterization 6–12 months after acute illness to aid in selecting therapeutic options, additional testing if ischemia noted |
VIII. Exercise Recommendations for Congenital Heart Disease
IX. Lipid Monitoring Recommendations
TABLE EC 7-D
EXERCISE RECOMMENDATIONS FOR CONGENITAL HEART DISEASE AND SPORTS ALLOWED FOR SOME SPECIFIC CARDIAC LESIONS15
| Diagnosis | Sports Allowed |
| Small ASD or VSD | All |
| Mild aortic stenosis | All |
| MVP (without other risk factors) | All |
| Moderate aortic stenosis | IA, IB, IIA |
| Mild LV dysfunction | IA, IB, IC |
| Moderate LV dysfunction | IA only |
| Long QT syndrome | IA only |
| Hypertrophic cardiomyopathy | None (or IA only) |
| Severe aortic stenosis | None |
| Sports Classification | Low Dynamic (A) | Moderate Dynamic (B) | High Dynamic (C) |
| I. Low static | Billiards Bowling Golf Riflery | Baseball/softball Table tennis Volleyball Fencing | Racket sports Cross-country skiing Field hockey∗ Race walking Running (long distance) Soccer∗ |
| II. Moderate static | Archery Auto racing∗,† Diving∗,† Equestrian∗,† Motorcycling∗,† | Fencing Field events (jumping) Figure skating∗ Football (American)∗ Surfing Rugby∗ Running (sprint) Synchronized swim† | Basketball∗ Ice hockey∗ Cross-country skiing (skating technique) Swimming Lacrosse∗ Running (middle distance) Team handball |
| III. High static | Bobsledding Field events Gymnastics∗,† Rock climbing Sailing Windsurfing∗,† Waterskiing∗,† Weight lifting∗,† | Body building∗,† Downhill skiing∗,† Skateboarding∗,† | Boxing/wrestling∗ Martial arts∗ Rowing Speed skating Cycling∗,† |
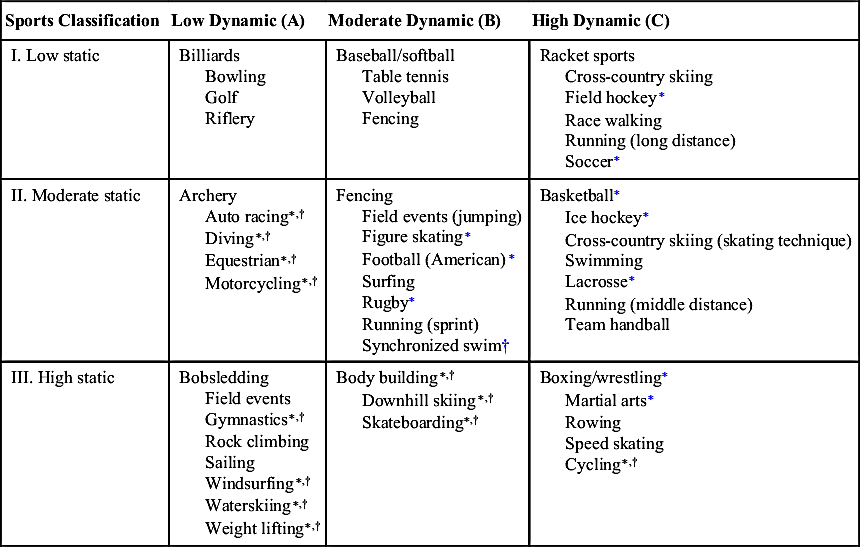
ASD, Atrial septal defect; LV, left ventricular; MVP, mitral valve prolapse; VSD, ventricular septal defect.
∗ Danger of bodily collision.
† Increased risk if syncope occurs.
Adapted from Maron BJ, Zipes DP. 36th Bethesda Conference: Eligibility recommendations for competitive athletes with cardiovascular abnormalities. J Am Coll Cardiol. 2005;45:1313-1375; and Committee on Sports Medicine and Fitness, American Academy of Pediatrics. Medical conditions affecting sports participation. Pediatrics. 2001;107:1205-1209.





