Management of Deep Overbite Malocclusion
Madhur Upadhyay, Ravindra Nanda
Deep overbite is perhaps the most common malocclusion and is also the most difficult to treat successfully. Excessive incisal overlap, which varies widely from patient to patient, is one of the primary manifestations of dental malocclusion.1 Before embarking on a detailed discussion of deep bite malocclusion it is imperative to understand the concept of overbite. One of the earliest definitions of overbite was put forward by Strang,2 who defined it as “the overlapping of the upper anterior teeth over the lowers in the vertical plane.” However, since the crown length of the upper and lower incisors varies significantly in individuals, a notation of overbite as a percentage is more descriptive and desirable. Therefore the same definition when put in terms of percentage defines overbite as “the amount and percentage of overlap of the lower incisors by the upper incisors.”
The ideal overbite in a normal occlusion may range between 2- and 4-mm or more appropriately between 5% and 25% (overlap of the mandibular incisors by the maxillary incisors) (Fig. 8-1). According to Nanda,3 even a range of 25% to 40% without any associated functional problems during various movements of the temporomandibular joint (TMJ) may be considered normal. However, overlaps greater than 40% should be considered “excessive” (deep bite), as they have the potential to cause deleterious effects on the overall dental health of the surrounding periodontal structures and the TMJ. At 5 to 6 years of age the percentage of overbite varies between 36.5% and 39.2%.4 Between 9 and 12 years of age the overbite usually increases, whereas in the period between 12 years and adulthood it decreases.5 Thereafter it remains largely unchanged, varying between 37.9% and 40.7% unless affected by other factors such as abrasion or loss of teeth, causing reduced vertical dimension. Severe deep bites (overbites >5-mm) are found in nearly 20% of children and 13% of adults, representing about 95.2% of vertical occlusal problems.
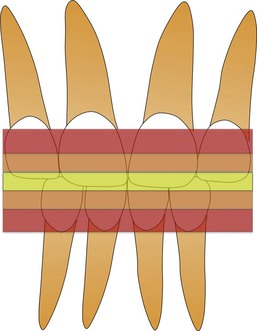
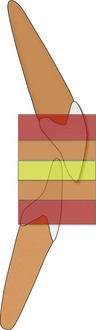
Figure 8-1 Zones of overbite: 5% to 25% is normal (yellow), 25% to 40% is increased overbite (orange), and >40% excessive (deep) overbite (red).
One of the most severe forms of excessive overbite is the cover bite6 (Fig. 8-2), which is most often associated with the Class II, Division 2 malocclusion. This condition was first recorded in 1912 in the German literature as Deckbiss.7 It is characterized by complete covering or concealment of the mandibular incisors' crowns due to excessive overbite and retroclination of the maxillary incisors. Another term that has been used previously to denote a severe form of deep bite is the closed bite8 (Fig. 8-3). This is mostly seen in adults and very rarely in young children and is characterized by excessive overbite resulting from loss of posterior teeth.

Figure 8-2 Example of cover bite malocclusion. Note that the lower incisors are completely concealed by the upper incisors.
Etiology
A deep bite malocclusion overlies a multitude of hidden skeletal or dental discrepancies. Accordingly, a deep bite should not be approached as a disease entity; instead, it is considered a clinical manifestation of an underlying skeletal or dental discrepancy.
From a developmental standpoint, skeletal or dental overbite is caused by either genetic or environmental factors, or a combination of both. Skeletal deep bites usually have a horizontal growth pattern and are characterized by (1) growth discrepancy of the maxillary and mandibular jawbones, (2) convergent rotation of the jaw bases, and/or (3) deficient mandibular ramus height. In such situations the anterior facial height is often short, particularly the lower facial third. On the other hand, dental deep bites show either supraocclusion (overeruption) of the incisors2,9 or infraocclusion (undereruption) of the molars,2,5,9,10 or a combination of the two. Other factors that can affect this condition include alteration in the tooth morphologies, premature loss of permanent teeth resulting in lingual collapse of the maxillary or mandibular anterior teeth, mesiodistal width of anterior teeth, and age-related natural deepening of the bite.
Deep bites primarily caused by environmental factors can also be classified as “acquired deep bites.” It is a well-known fact that there is a dynamic equilibrium of forces between the structures around the teeth, namely, the tongue, the buccinator, the mentalis and the orbicularis oris muscles, and the occlusal forces that assist in the balanced development and maintenance of the occlusion. Any environmental condition that disrupts this dynamic harmony can lead to a malocclusion. Some examples are:
1. A lateral tongue thrust or abnormal tongue posture causing infraocclusion of the posterior teeth
2. Wearing away of the occlusal surface or tooth abrasion
3. Anterior tipping of the posterior teeth into extraction sites
Hence deep bite etiology must be considered in detail in order to formulate a comprehensive diagnosis and treatment plan for each patient so that optimal skeletal, dental, and esthetic results can be attained.
Diagnosis
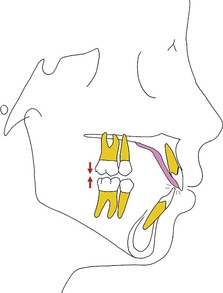
A deep overbite can be corrected either by extrusion of posterior teeth or by inhibition and genuine intrusion of anterior teeth, or by a combination of the two (Fig. 8-4). The choice of treatment is based in part on the etiology of deep bite, the amount of growth anticipated, the vertical dimension, the relationship of the teeth to the adjoining soft tissue structures, and the desired position of the occlusal plane.
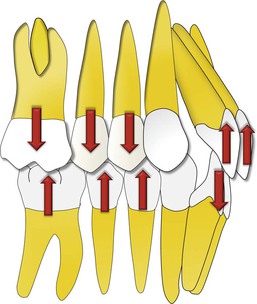
Figure 8-4 Deep bite malocclusion can be treated by either intrusion of incisors or extrusion of posterior teeth.
Growth Considerations
It is widely accepted that correction of deep bite is both easier to accomplish and more stable when it is performed on growing patients than when it is attempted on those with no appreciable growth remaining.11,12 Since growth tends to increase the vertical distance between the maxillae and the mandible, it is probably useful to treat such patients in a period of active mandibular growth. During the growth period, tooth eruption can be stimulated in the posterior segments and inhibited in the anterior because condylar growth allows for dentoalveolar growth. However, in adults such a movement is counteracted by the posterior occlusion, especially in a patient with a hypodivergent skeletal pattern. The stability of such a tooth movement, if performed, is highly questionable, as it leads to alterations in muscle physiology, thereby increasing the chances of relapse. In such malocclusions and others in which growth stimulation is no longer possible, fixed or removable mechanical appliances are needed to achieve optimal treatment results. In some patients a surgical procedure may be required. For example, in patients with vertical maxillary excess, a Le Fort I osteotomy with maxillary impaction might be required to achieve optimum dentofacial esthetics. A detailed discussion of this subject is beyond the scope of this chapter and can be found elsewhere.13
Assessment of the Vertical Dimension
Schudy14 advocated correction of deep bite with eruption of premolars and molars as the treatment of choice, while others3,15 have preferred intrusion of incisors to treat the majority of their patients. Instead of following anecdotal information it is important to carefully consider the influence of extrusive or intrusive mechanics on the vertical facial height of a patient, as this in turn may affect the anterior-posterior relationship of the maxilla and mandible.
In general, eruptive mechanics should not encroach on the freeway8 or interocclusal space, which is defined as the distance between the occlusal or incisal surfaces of the maxillary and mandibular teeth when the mandible is in the physiological rest position. The average is between 2- and 4-mm. When there is a larger than normal free space, greater opportunities exist for correction by guiding vertical alveolar development. For example, in a Class II, Division 2 patient with a hypodivergent facial pattern, redundant lips, and a flat mandibular plane angle, the deep bite can be corrected and facial esthetics improved by increasing the lower facial height or facial convexity. However, in most other Class II malocclusions it is not always desirable to increase the vertical dimension, since doing so would tend to accentuate the point A–point B discrepancy and increase an abnormally large lower face.
Soft Tissue Evaluation
In the present era, “soft tissue relationships” form an important diagnostic tool for deep bite correction. The clinician should always consider the maxillary incisor position relative to the lip position to determine whether to maintain, intrude, or extrude the maxillary incisors relative to the upper lip. With increased emphasis on smile esthetics and smile design, the use of dynamic smile analysis is gaining precedence over static photographs in diagnosing malocclusions and formulating appropriate treatment plans for their correction.16
Incisal exposure should be considered in three different clinical situations during initial examination: in relaxed lip position, while smiling, and during speech. In a relaxed lip position, 2- to 4-mm of incisor exposure, which includes the incisal edges, is considered acceptable. When smiling, the average incisor exposure is almost two-thirds that of the upper incisor, according to Maulik and Nanda.16 They also reported that in most pleasing smiles the upper lip in males does not show any gingiva; however, females can have 1- to 2-mm of gingival exposure. If this condition is met and a deep bite is still present, the treatment plan should focus on either posterior extrusion (if the vertical parameters permit) or lower incisor intrusion (Fig. 8-5). In contrast, an occlusal plane “significantly” below the ideal might show excessive gingiva, which might then require selective intrusion of the upper incisors (Fig. 8-6). Incisor exposure during speech may give additional information, as different facial muscles are involved.
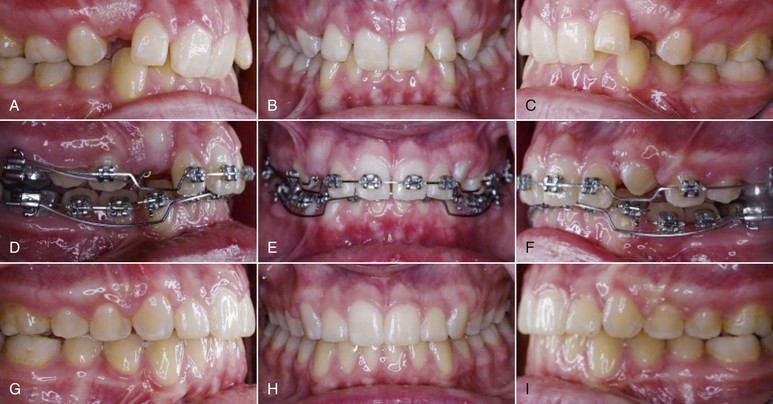
Figure 8-5 A–C, This adolescent female patient had the chief complaint of excessive overbite. On careful analysis it was observed that her upper incisor exposure was adequate both at rest and during smiling. D–F, The decision was made to intrude the lower incisors only so the deep bite malocclusion could be resolved without significantly affecting the patient's smile esthetics. Segmental intrusion of the lower incisors was carried out with an overlay intrusion arch. G–I, Treatment results.


Figure 8-6 A–F, Pretreatment photographs. G–P, Extremely light forces delivered through a Connecticut Intrusion Arch (CTA) were used to selectively intrude only the upper central incisors. Q–V, Treatment results show a significant improvement in the gingival exposure and the smile as well as the correction of the deep overbite.
Another important factor to consider is the “interlabial gap.” In patients exhibiting a large interlabial gap it might not be desirable to perform posterior extrusive mechanics, as this might further worsen the esthetics of the patient by increasing the interlabial gap. In fact, an increase in the interlabial gap may cause several other problems, such as inability to close the lips without strain and associated functional problems. Similarly, in individuals with redundant upper and lower lips or no interlabial gap but who show excessive overbite, posterior extrusive mechanics may be desirable.
Flaring (proclining) the incisors is yet another option that primarily camouflages deep bites. It is especially useful in patients who have retroclined incisors to begin with (e.g., Class II, Division 2 cases). However, rapid labial tipping of mandibular incisors must be avoided to minimize risk of root resorption, gingival recession, and bone dehiscence, especially on a narrow symphysis with questionable labio-lingual width of the alveolar bone.17 Another contraindication can be undesirable facial esthetics.
Treatment
Treatment mechanics for deep bite correction depend on a number of etiologic variables and the associated treatment plan. Nevertheless, as already mentioned, there are three ways to treat deep bite malocclusions: intrusion of the upper and lower incisors, extrusion of the upper and lower posterior teeth, or a combination of the two.
Intrusion of the Upper and Lower Incisors
Incisor intrusion is generally indicated in a patient with a vertical maxillary excess, a large interlabial gap, a long lower facial height, or a steep mandibular plane. Some of the appliances that can achieve “true incisor intrusion”18 are discussed below.
Intrusion Arch
An intrusion arch can be made from 0.016-inch × 0.022-inch or 0.017-inch × 0.025-inch CNA (Connecticut Nickel Titanium Archwires). Alternatively, preformed intrusion archwires—the Connecticut Intrusion Arch (CTA)19 (Ultimate Wireforms, Bristol, CT.) fabricated from a nickel-titanium (Ni-Ti) alloy that provides the advantages of shape memory, springback, and light continuous force distribution—can also be used (Fig. 8-7, A). The appliance setup includes two passive posterior (stabilizing) units and one active anterior unit (the intrusion arch). The passive units consist of stiff or rigid segmented wires (0.017-inch × 0.025-inch stainless steel or higher dimension wires) in the molars and premolars bilaterally. Inclusion of as many teeth as possible in the posterior segment minimizes side effects. The anterior segment, which includes either two or four incisors, is constructed with similar wires. Remember that the higher the dimension of the stainless steel wires, the more predictable the tooth movement is.
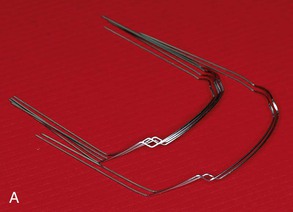
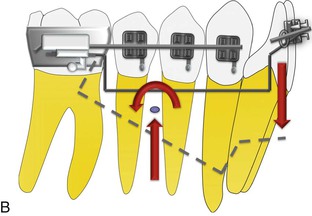
Figure 8-7 A, Preformed upper and lower Connecticut Intrusion Archwire (CTA) made from nickel-titanium (Ni-Ti) alloy. B, The biomechanical design of lower incisor intrusion with the CTA.
The intrusion arch is activated by placing a 30-degree gingival bend 2- to 3-mm mesial to the molar tubes so that the wire lies passively in the vestibular sulcus. Activation is accomplished by bringing it occlusal and tying it to the anterior segment as a point contact, as opposed to placing it directly into the bracket slots as is done with the utility arch.20,21 The intrusion arch uses a one-couple force system, which makes the appliance statically determinant (i.e., the various forces and moments in this setup can be quantified to an appreciable degree of accuracy). The intrusion arch can also be tied back or cinched to prevent flaring of the incisors if the intrusive force is being applied anterior to the center of resistance (CRES) of the incisors. The reciprocal action of the intrusion arch on the molars or the buccal segments is the extrusion and/or distal tip back of the crowns and the mesial movement of the roots (Fig. 8-7, B). This can be very helpful in a Class II, Division 1 patient who requires correction of the molar relation to a Class I. In such patients a buccal segment is often not needed, as it may prevent distal tip back of molars. However, in Class I malocclusions with deep bite, a tip back may cause steepening of the occlusal plane. Increasing the number of teeth in the anchor unit is one way to minimize such side effects. Another method is to use relatively low forces to the order of 40 g for the upper four incisors and 30 g for the lower incisors. As a general guideline, 10 to 15 g of force per incisor is acceptable to prevent posterior side effects.22 Recent evidence has shown that the intrusive forces can be made so light that reactive forces on the anchor teeth remain well below the force levels needed for extrusion and tipping.22 Therefore the use of a headgear to prevent side effects is completely avoidable. Additionally, low forces help to minimize root resorption. On average, after the initial activation period of 3 to 4 weeks the base arch should intrude 0.4- to 0.6-mm per month.23
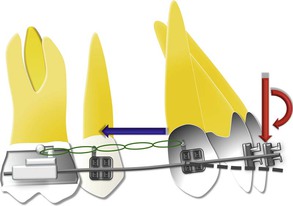
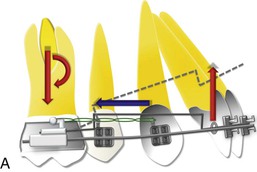
Another useful clinical application of intrusion arch, besides its other uses,19 is in preventing the side effects associated with canine retraction. A popular method of canine retraction is “frictional mechanics” employing a continuous arch system. The obvious advantages of this system (compared to frictionless mechanics) are reduced possibility of unpredicted canine movement (e.g., rotation, flaring, and extrusion of the canine) and minimal wire bending. However, when an archwire with a low load-deflection rate is used it tends to deform, leading to undesirable side effects on the anterior teeth in the form of extrusion of the incisors or deepening of the bite.24 This type of deep bite can also be termed “iatrogenic deep bite,” which in the present context means deep bite induced inadvertently by the clinician (Fig. 8-8). With larger or rigid archwires the system might develop excessive friction leading to delayed tooth movement, anchorage loss, or maybe even cessation of canine retraction. Therefore the use of a 0.016-inch × 0.022-inch CTA as an overlay archwire to optimize the biomechanical system for canine retraction, as shown in Figure 8-9, is recommended. The counterclockwise moment (if tied anterior to the CRES of the anterior teeth) and the intrusive force on the incisors ensure the stability of the incisors by counteracting the iatrogenic forces generated by canine retraction. Additionally, molar anchorage is reinforced due to a tip-back moment on the posterior segment.
Utility Arch
The utility arch (Fig. 8-10) is similar in design to the CTA. It is stepped down at the molars, passes through the buccal vestibule, and is stepped up at the incisors to avoid distortion from occlusal forces. The difference is that for intrusion the utility arch is tied into the incisor brackets, which create a two-couple force system the moment of which tends to tip the incisor crowns facially and the molar distally. Although the facial tipping of incisors can be avoided by cinching or tying back the intrusion utility arch, any force that tends to bring the anchor teeth mesially is undesirable. Incorporating a “twist” or “torque bend” in the incisor segment is another way of controlling the tendency of the teeth to tip facially; however, this will increase the intrusive force on the incisor segment and the extrusive force on the molar. It is well known that heavier forces do not increase the amount or rate of intrusion.25,26 Another problem is that, unlike the CTA, this being a two-couple system means that it is impossible to accurately determine the magnitude of the reactive forces (statically indeterminate), which makes it rather impossible to adjust the archwire to prevent side effects. Therefore in our clinical practice we prefer to use the CTA. Also, considerable chair time is saved as the CTA involves no wire bending and needs minimal adjustment.
Three-Piece Intrusion Arch
Labial tipping of incisors gives the clinical impression of deep bite correction because it influences the vertical incisal edge position. Similarly, during extensive retraction of incisors development of a deep bite (iatrogenic) is common due to uprighting of the incisors (Fig. 8-11). It is therefore important to control the labio-lingual inclination of the anterior teeth as they are intruded and retracted, especially if they are flared to begin with.
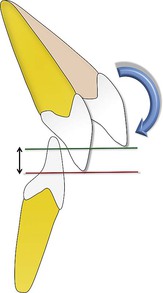
Figure 8-11 Uprighting (or retraction) of proclined incisors during orthodontic treatment might lead to development of deep bite (iatrogenic in nature).
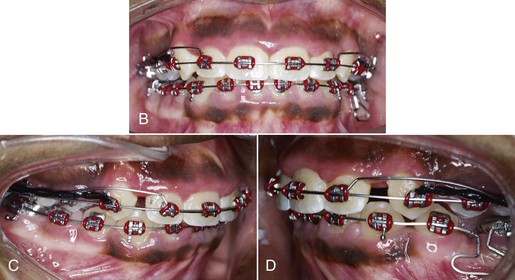
A three-piece intrusion arch27 uses segmental mechanics to simultaneously intrude and retract incisor teeth in a highly predictive manner. The passive units, with some modifications, are constructed in the same way as described previously for intrusion arch (Fig. 8-12). The active units consist of two segmented springs made from 0.016-inch × 0.022-inch or 0.017-inch × 0.025-inch CNA wires activated by placing a 30-degree gingival bend 2 to 3 mm mesial to the molar tubes. The gingival bend can be increased or decreased based on the desired amount of intrusive force. The wires are hooked to the distal extensions on the anterior segmented wire at a point close to the estimated CRES of the incisors. Application of a light, distal force delivered by a Class I elastic or a power chain to the anterior segment helps to alter the direction of the intrusive force on the anterior segment, so that the forces are directed in an upward and backward direction through the CRES of the anterior teeth or as required in a particular case (Fig. 8-13).
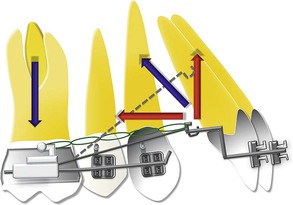
Figure 8-12 A sketch of the biomechanics involved when using a three-piece intrusion arch for simultaneous intrusion and retraction of maxillary incisors.

Figure 8-13 Adult patient showing a severe deep bite due to supraeruption of the incisors. A–C, Pre-treatment intraoral views. D–I, Three-piece intrusion arches were placed in both the upper and the lower arches for deep bite correction. J–L, Optimum overbite and overjet were established at the end of treatment.
Extrusion of Upper and Lower Posterior Teeth
Biteplates
Currently, biteplates are the most popular appliances to correct deep bites by molar extrusion (Fig. 8-14). These appliances load the incisors for an intrusive effect but leave the posterior teeth free to erupt, thereby leveling the curve of Spee primarily by posterior extrusion, as the intrusive effect on the incisors at best is minimal. Sleichter28 studied the vertical changes of molars and incisors with biteplate treatment. He found that alveolar height in the molar region increased while there was minimal change in the incisal area.
Two types of biteplates can be used: removable or fixed.
• Removable biteplates consist of an acrylic platform anchored to the maxillary dentition with arrowhead, Adams, or crib clasps. Anteriorly there is a labial bow, which helps to stabilize the biteplate and contact the teeth at the incisal one-third. By acting as a premature incisal stop, usually within the confines of the interocclusal space (freeway space), the block forces the posterior teeth from occlusal contact and allows them to erupt. It is advisable not to disocclude the posterior teeth by more than 2-mm, as this allows for close supervision of the follow-up and progress of the patient's treatment and also prevents any sudden TMJ or myofunctional change.
• Fixed or bonded biteplates consist of blocks of composite or glass ionomer cement that can be bonded on the lingual surface of maxillary incisors to disocclude the posterior teeth. Their advantages over removable biteplates are that they can be integrated with fixed appliance mechanotherapy, there is no need for patient cooperation, and the appliance itself is considerably less bulky.
Functional Appliances
Functional appliances can also be used to achieve posterior extrusion to correct deep bites, especially in low angle Class II malocclusions. Functional appliances help in positioning the lower jaw forward to an edge-to-edge relationship, thereby disoccluding the posterior teeth, which are then free to erupt. Eruption can be augmented by using elastics during fixed appliance mechanotherapy. However, for treatment to succeed, the appliance must be worn nearly full-time. Unfortunately, a significant number of patients do not cooperate fully and appliances are often worn only part-time and lost or broken while out of the mouth. Many of these problems can be overcome by using fixed functional appliances, such as the Twin Force bite corrector (Fig. 8-15).
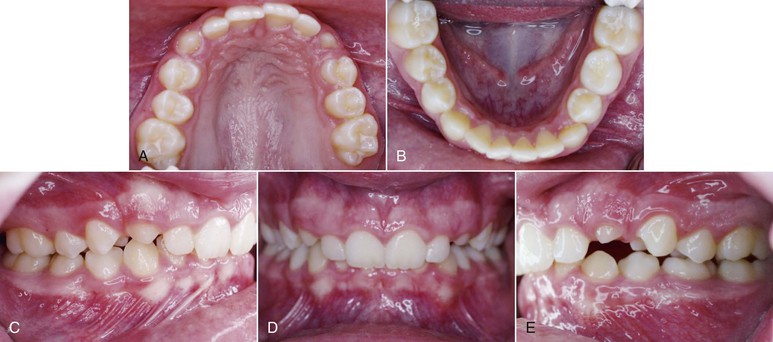
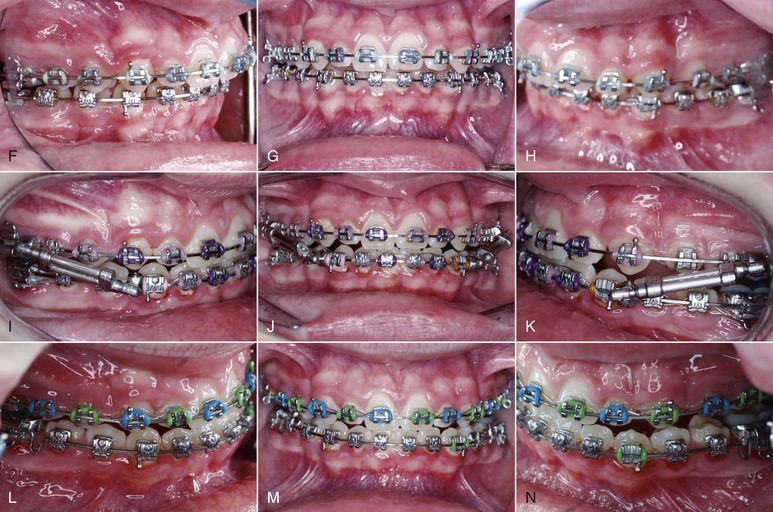
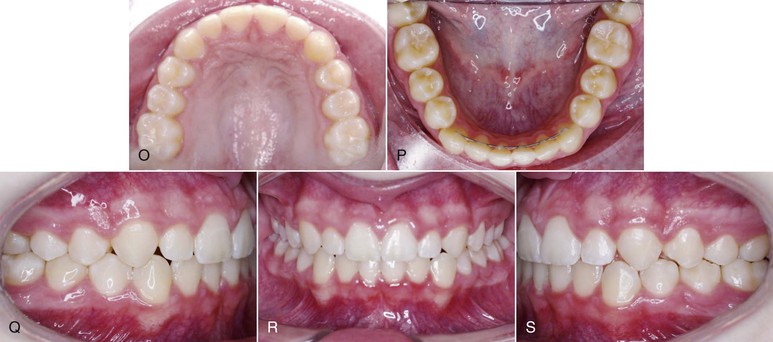
Figure 8-15 A–E, Pre-treatment clinical views of a Class II, Division 1 patient with severe deep bite. F–N, Patient was treated with a Twin Force bite corrector (fixed functional appliance). Note how the anterior positioning of the mandibular teeth in an edge-to-edge relationship with the maxillary incisors disoccludes the posterior teeth, which are then free to erupt. Alternatively, elastics can be used to augment their eruption. O–S, Results of treatment.
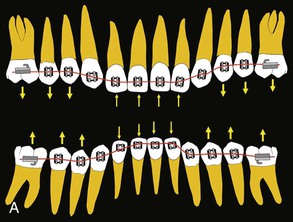
Combination of Intrusion and Extrusion
By positioning anterior brackets occlusally and posterior brackets gingivally or by using reverse curve archwires, simultaneous intrusion of anterior teeth and extrusion of posterior teeth can be attained (Fig. 8-16). However, there is no definite control over such mechanics. Changes in the axial inclination of the buccal teeth and flaring of incisors due to an intrusive force anterior to the CRES are some of the drawbacks that need to be addressed. Also, since extrusion is more easily accomplished than intrusion a reverse curve of Spee wire will extrude posterior teeth while obtaining minimal, if any, anterior intrusion.29
Implants for Deep Bite Correction
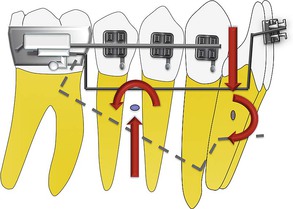
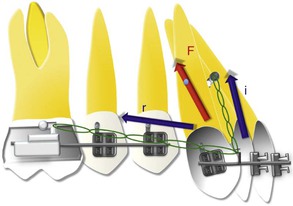
Anchorage control, especially in the vertical dimension, is of paramount importance if bite opening must be achieved by genuine intrusion of the anterior teeth. Additionally, if intrusion of all six anterior teeth (including the canines) is desired (instead of only four incisors), as in a “cover bite” malocclusion, extraoral appliances become a prerequisite in order to withstand the additional burden of anchorage. According to Burstone,15 it is not possible to intrude all six anterior teeth at one time without producing undesirable axial inclination change in the posterior segment. An additional 20 to 30 g of force would be required on each side to intrude the canine, taking into account the root size and the dense surrounding bone. Although efficient, extraoral appliances require extensive patient cooperation. Recently it has also been shown that the chances of root resorption are greater with these appliances, possibly due to the “jiggling effect.”30 Esthetics and social issues are also of concern. In the past decade, skeletal anchorage systems such as mini-plates, palatal implants, mini-implants, and screws have revolutionized orthodontic anchorage and biomechanics by making anchorage more stable.31–35 Mini-implants can be used effectively for en masse intrusion of anterior teeth36 (Fig. 8-17).

Figure 8-17 A–C, Sixteen-year-old postpubertal male patient presenting with a severe Class II, Division 2 malocclusion with 100% deep bite. D and E, In the first phase of treatment a Jones jig molar distalization appliance was used to distalize the maxillary molars by more than 6 mm, to achieve a Class I molar relation. F and G, In the second phase of treatment mini-implants were inserted between the roots of the maxillary lateral incisor and canine to intrude all maxillary anterior teeth en masse in a single step. More than 4-mm of intrusion was achieved without any posterior teeth extrusion. The implants remained stable throughout treatment. In the mandibular arch the incisors were proclined to alleviate the severe crowding. H–J, Good overjet and overbite were achieved after completion of active orthodontic treatment.
Availability of sufficient interdental bone, less soft tissue irritation, and a larger anterior segment (if all six anterior teeth are included) that requires greater control are some of the factors that must be considered when placing mini-implants for intrusion of anterior teeth. We have found the interdental bone between the roots of the canine and lateral incisors, bilaterally, as an appropriate location for placement of mini-implants. The selection of the point of application of the intrusive force with respect to the CRES of the anterior segment is also an important consideration in the placement of the implants, so that the nature of the tooth movement that will occur can be predicted more accurately. The CRES of the six anterior teeth has been estimated to be halfway between the CRES of the four incisors and canines.36 True intrusion without axial inclination change can be obtained only by directing the intrusive force through the CRES of the anterior teeth. In the patient described in Figure 8-17, a light distal force (r) was delivered by an elastic chain to the anterior segment to alter the direction of the intrusive force (i) so that true intrusion of the anterior teeth could be achieved along their long axes (Fig. 8-18). The distal force used was of very low magnitude, primarily to redirect the line action of the intrusive force.
Retention and Stability
As discussed, correction of deep bite malocclusion can be attained by a variety of methods with fairly predictable results. However, the real challenge is maintaining the overbite over an appreciable period. The results of most studies concerning the stability of overbite correction suggest a decrease in the overbite during treatment followed by an increase in the overbite after appliance removal, although at the clinical level this increase might not be significant.37 The following are some factors that must be kept in mind when planning retention for deep overbite correction:
1. Age: Deep bite correction is usually achieved by the simultaneous intrusion of incisors and extrusion of the posterior teeth. Growing patients benefit the most with this approach because active vertical growth during deep bite correction ensures greater stability. Because growth tends to increase the vertical distance between the jaw bases, performing treatment during this period is most advantageous.
2. Facial type: Certain facial types have a greater potential for permanent correction than others. Hyperdivergent facial types usually exhibit a more favorable reaction to overbite correction when compared to hypodivergent facial types. This can be attributed to the growth rate in the vertical direction, which is highest and lasts the longest in high angle patients.
3. Molar extrusion and incisor intrusion: The stability of molar extrusion in growing patients has been examined in previous studies, which suggest that this is a fairly stable procedure if the interocclusal space is not violated. Any eruptive movement beyond the interocclusal space might not be stable due to strong posterior occlusion or muscle stretching, especially in low angle individuals. For the same reason, in adults incisor intrusion is regarded as more stable. Other factors that can lead to relapse of incisor intrusion include continued lower incisor eruption, canting of the occlusal plane, incomplete leveling of the curve of Spee, and forward rotation of the mandible.
4. Inter-incisal angle: Riedel38 has suggested that a large inter-incisal angle at the end of treatment is associated with relapse of deep overbite. This might be because a large inter-incisal angle tends to force the crowns of the mandibular incisors lingually and the apex of the maxillary incisors labially.12 A study by Burzin and Nanda37 showed that the axial inclination of the incisors did not change significantly during a 2-year post-treatment observation period. They suggested that ideal axial inclination of the incisors at the end of treatment could be a factor in overbite stability. Therefore maintaining optimum inter-incisal angle, incisal stops, and guidance between the maxillary and mandibular incisors is essential for maintaining overbite correction. The inter-incisal angle can be higher for dolichofacial patterns and less for brachyfacial patterns; however, in general an angle of 125 to 135 degrees ensures good stability for deep bite correction.
Summary
Deep overbite is a common component of malocclusion in adults and children. Although a number of treatment modalities were discussed in this chapter, the importance of accurate diagnosis, which entails the precise estimation of the etiologic factors, cannot be undermined because effective treatment of deep bite and its retention in the long-term critically depend on it. Esthetic considerations such as maxillary incisor to lip relationship and gingival exposure on smiling are also important diagnostic features that must be considered in the treatment plan.
References
1. Goldstein MS, Stanton FL. Various types of occlusion and amounts of overbite in normal and abnormal occlusion between two and twelve years. Int J Orthod Oral Surg. 1936;22:549–569.
2. Strang RHW. A Textbook of Orthodontia. Lea & Febiger: Philadelphia, PA; 1950.
3. Nanda R. The differential diagnosis and treatment of excessive overbite. Dent Clin North Am. 1981;25:69–84.
4. Dermaut LR, Pauw GD. Biomechanical aspects of Class II mechanics with special emphasis on deep bite correction as a part of the treatment goal. Nanda R. Biomechanics in Clinical Orthodontics. WB Saunders: Philadelphia, PA; 1997:86–89.
5. Flemming HB. Investigation of the vertical overbite during the eruption of the permanent dentition. Angle Orthod. 1961;31:53–62.
6. Peck S, Peck L, Kataja M. Class II Div 2 malocclusion: a heritable pattern of small teeth in well-developed jaws. Angle Orthod. 1998;68:9–17.
7. Mayrhofer B. Lehrbuch der Zahnkrankheiten. Gustav Fischer Verlag: Jena, Germany; 1912.
8. Moyers RE. Handbook of Orthodontics. 4th ed. IL: Year Book Medical Publishers: Chicago; 1998.
9. Prakash P, Margolis HI. Dento-cranofacial relations in varying degrees of overbite. Am J Orthod. 1952;38:657–673.
10. Wylie WL. The relationship between ramus height, dental height and overbite. Am J Orthod Oral Surg. 1946;32:57–67.
11. Bell W, Jacobs J, Legan H. Treatment of Class II deep bite by orthodontic and surgical means. Am J Orthod. 1984;85:1–19.
12. Simons M, Joondeph D. Change in overbite: a ten-year post-retention study. Am J Orthod. 1973;64:349–367.
13. Proffit WR, White RP, Sarver DM. Long face problems. Proffit WR, White RP Jr, Sarver DM. Contemporary Treatment of Dentofacial Deformity. Mosby: St. Louis, MO; 2003:464–506.
14. Schudy FF. The control of vertical overbite in clinical orthodontics. Angle Orthod. 1968;38:19–38.
15. Burstone CR. Deep overbite correction by intrusion. Am J Orthod. 1977;72:1–22.
16. Maulik C, Nanda R. Dynamic smile analysis in young adults. Am J Orthod Dentofacial Orthop. 2007;132:307–315.
17. Wehrbein H, Bauer W, Diedrich P. Mandibular incisors, alveolar bone, and symphysis after orthodontic treatment: a retrospective study. Am J Orthod Dentofacial Orthop. 1996;110:239–246.
18. Ng J, Major PW, Heo G, Flore-Mir C. True incisor intrusion attained during orthodontic treatment: a systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2005;128:212–219.
19. Nanda R, Marzban R, Kulhberg A. The Connecticut intrusion arch. J Clin Orthod. 1998;32:708–715.
20. Ricketts RM. Bioprogressive therapy as an answer to orthodontic needs: part I. Am J Orthod. 1976;70:241–268.
21. Ricketts RM. Bioprogressive therapy as an answer to orthodontic needs: part II. Am J Orthod. 1976;70:359–397.
22. Steevenbergen EV, Burstone CJ, Prahl-Andersen B, Aartman IHA. The influence of force magnitude on intrusion of the maxillary segment. Angle Orthod. 2005;75:723–729.
23. Faber ZT. The Relationship of Tooth Movement to Measured Force Systems: A Prospective Analysis of the Treatment Effects of Orthodontic Intrusion Arches [master's thesis]. Division of Orthodontics, University of Connecticut: Storrs, CT; 1994.
24. Nanda RS, Ghosh J. Biomechanical considerations ion sliding mechanics. Nanda R. Biomechanics in Clinical Orthodontics. WB Saunders: Philadelphia, PA; 1997:188–217.
25. Dellinger EL. A histologic and cephalometric investigation of premolar intrusion in the Macaca speciosa monkey. Am J Orthod. 1967;53:325–355.
26. Reitan K. Initial tissue behavior during apical root resorption. Angle Orthod. 1974;44:68–82.
27. Shroff B, Nanda R. Biomechanics of class II correction. Nanda R. Biomechanics in Clinical Orthodontics. WB Saunders: Philadelphia, PA; 1997:143–155.
28. Sleichter CG. Effects of maxillary bite plane therapy in orthodontics. Am J Orthod. 1954;40:850–870.
29. Woods MG. The mechanics of lower incisor intrusion: experiments in non-growing baboons. Am J Orthod. 1988;93:186–195.
30. Deguchi T, Murakami T, Kuroda S, Yabuuchi T, Kamioka H, Yamamoto TT. Comparison of the intrusion effects on the maxillary incisors between implant anchorage and J-hook headgear. Am J Orthod Dentofacial Orthop. 2008;133:654–660.
31. Nanda R, Uribe FA. Temporary Anchorage Devices in Orthodontics. Mosby Elsevier: St. Louis, MO; 2009.
32. Upadhyay M, Yadav S, Nagaraj K, Patil S. Treatment effects of mini-implants for en-masse retraction of anterior teeth in bialveolar dental protrusion patients: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2008;134:18–29.
33. Nagaraj K, Upadhyay M, Yadav S. Mini-implant anchorage for a skeletal class II malocclusion with missing mandibular incisors: a case report. World J Orthod. 2008;9(2):155–166.
34. Upadhyay M, Yadav S. Mini-implants for retraction, intrusion and protraction in a Class II division 1 patient. J Orthod. 2007;34(3):158–167.
35. Upadhyay M, Nagaraj K, Yadav S, Saxena R. Mini-implants for en masse intrusion of maxillary anterior teeth in a severe Class II division 2 malocclusion. J Orthod. 2008;35:79–89.
36. Melsen B, Fotish V, Burstone CJ. Vertical force considerations in differential space closure. J Clin Orthod. 1990;24:678–683.
37. Burzin J, Nanda R. The stability of deep overbite correction. Nanda R, Burstone CJ. Retention and Stability in Orthodontics. WB Saunders: Philadelphia, PA; 1993:61–79.
38. Riedel RA. A review of the retention problem. Angle Orthod. 1960;30:179–194.