It has long been stated that “beauty is in the eye of the beholder.”1 However, specific facial features are universally associated with attractiveness. Three components in facial esthetics that have been investigated through research in evolutionary psychology and that appear to represent cues for mate selection are symmetry, averageness, and secondary sexual characteristics.2 Cultural, social, and racial influences may affect one's judgment of attractiveness but they are secondary to these primary three characteristics.3,4
As with the other bilateral structures in the human body, symmetry in facial esthetics is evaluated in a right to left relationship. A slight asymmetry between the two facial halves is the norm; however, large asymmetries have been attributed in evolutionary psychology to signal lack of health and poor genetic makeup.2 Averageness, also referred to as prototype, is based on the concept that a computer-generated composite of select features from a group of many individuals will yield better esthetics than any single individual who is part of that group.5 In treatment planning in orthognathic surgery and orthodontics, the averageness concept is applied when any patient with a dentofacial deformity or malocclusion is compared to a norm. Through the use of cephalometrics, which examines the deviation in magnitude of specific dentofacial angles, lengths, and proportions, the patient is compared to individuals of the same age, gender, and ethnic group. Finally, secondary sexual characteristics are those that distinguish or define both sexes. A specific example is chin prominence in males and high cheekbones and short lower facial height in females.4,6
Symmetry, proportionality, and averageness are achievable goals in orthognathic surgery and serve as fundamental concepts that guide the treatment planning process in patients with dentofacial deformities. The esthetic outcomes obtained by following these goals likely result in an improvement in facial esthetics and appearance. Although facial esthetics is significantly affected with orthognathic surgery, other important functional aspects are also improved. Murphy et al.7 evaluated the quality of life of patients who had undergone orthognathic surgery and found moderate to high improvement in facial appearance (93%), masticatory function (64%), comfort (60%), and speech (32%).
Treatment Planning for Orthognathic Surgery
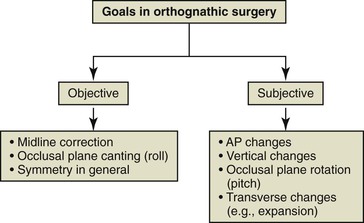
The treatment plan for patients with dentofacial anomalies must include specific goals, which can be divided into objective goals and subjective goals. Objective goals are those that can be measured exactly and, in general, are related to symmetry. It is clear that symmetry is measurable and has been regarded as one of the most important parameters in assessing facial esthetics.2–4 In orthognathic surgery planning, symmetry is mostly related to the transverse dimension; however, it can also be assessed in the vertical dimension (e.g., maxillary cant and ramus height differences). Objectives in the anteroposterior are more subjective, as they relate to averageness. The objectives in the vertical dimension are based on proportions and averageness and goals in this dimension are also prone to subjectivity (Fig. 21-1). Although the transverse dimension is mostly dictated by symmetry, averageness provided by normative values of different dental and skeletal dimensions could affect the surgical plan and therefore should also be included as a subjective goal.
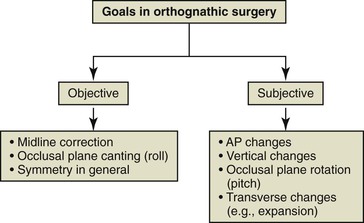
Figure 21-1 Objective and subjective goals in orthognathic surgery. AP, Anteroposterior.
Both objective and subjective goals guide the planning of orthognathic surgery. However, significant subjectivity influences the surgical plan. Although most surgeons and clinicians use cephalometrics as the basis for treatment planning for orthognathic surgery, disagreement can be common due to different clinicians' preferences as to what will constitute an ideal outcome. This is especially the case when patients and surgeons who have different ethnic backgrounds are considered. Lee et al.8 showed that there were discrepancies between American-trained and Asian-trained oral and maxillofacial surgeons regarding the type of treatment recommended for a group of Asian women with skeletal Class III profiles. While all of the Asian-trained surgeons preferred mandibular setback, approximately 40% of the American-trained surgeons preferred maxillary advancement.
During an orthognathic surgery case planning session it is not uncommon to encounter long discussions on the surgical movements that should be performed. Many complex questions can arise: How much should the maxilla be advanced (i.e., 3- or 5-mm)? Should the procedure include one or both jaws (especially in Class III malocclusions)? Is a genioplasty necessary? These questions arise because clinicians' preferences and biases affect these treatment decisions. Some clinicians prefer that the maxilla or mandible be projected more, or in some instances less, or that the incisor display at rest be a few millimeters more or less compared to other clinicians. This problem of disagreement is more relevant to the anteroposterior and vertical dimensions. However, such discrepancies are not present when symmetry is considered. This is why most clinicians and surgeons would consider a surgical plan with the maxillary midline off by 2-mm or more, a significant maxillary cant, or significant chin point deviation to be completely unacceptable.
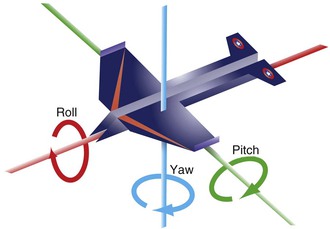
To meet the objective goals, new technology consisting of very precise three-dimensional (3D) planning software allows the virtual visualization of the craniofacial anatomy and aids in the surgical planning of patients with dentofacial deformities.9–11 This 3D planning software is very important in the clinician's ability to quantify with high precision the degree of asymmetry and plan with great detail the surgical movements. When planning occurs in three dimensions, aviation concepts become handy in describing the orientation and planning the surgical movement of a craniofacial structure within an orthogonal coordinate system. Rotational movements (pitch, yaw, and roll) along the three axes (x, y, and z) supplement the traditional two-dimensional movements along the different planes (sagittal, coronal, and axial) (Fig. 21-2).12 In essence, this 3D planning software allows visualization of the deformity and planning of the surgical movements in a virtual environment with six degrees of freedom.
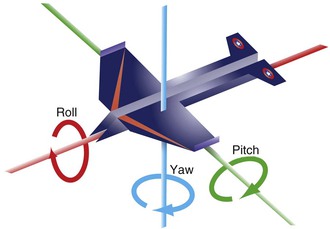
Figure 21-2 Concepts of roll, yaw, and pitch used in aviation and extrapolated to the planning of surgical movements in the three dimensions of space in orthognathic surgery.
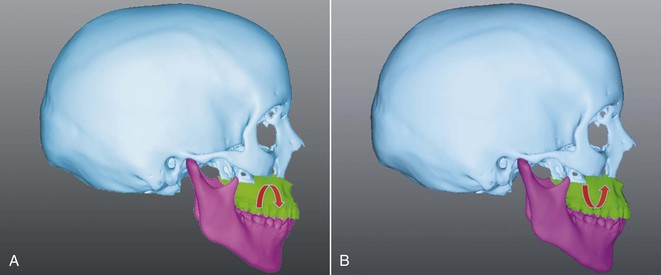
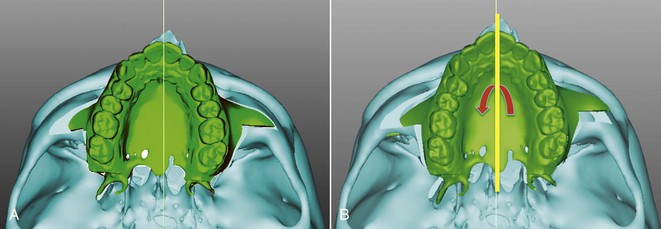
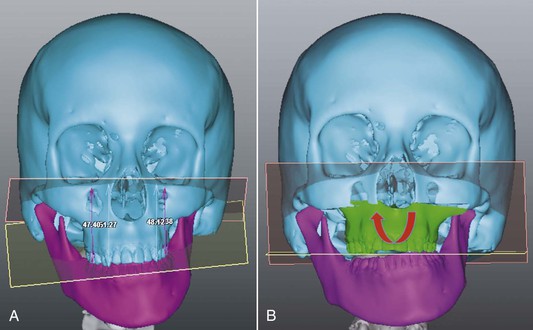
Pitch refers to rotational movements around a transverse or x axis; in aviation it refers to a situation in which an airplane makes a sudden maneuver to ascend or descend. In orthognathic surgery pitch refers to rotation of both jaws viewed from the sagittal plane, also known as clockwise or counterclockwise rotation (Fig. 21-3). Yaw refers to rotational movements around a vertical or y axis; in aviation it refers to sudden turns to the right or left. In orthognathic surgery yaw refers to the rotation of the maxilla in a lateral direction in order to surgically correct the midline (Fig. 21-4). It could further be described as the rotation of the axial plane around the y axis. Roll refers to rotational movements around an anteroposterior or z axis; in aviation it refers to the movement of an airplane when one wing swings upward and the other swings downward. In orthognathic surgery roll refers to the vertical movements made to correct canted occlusal planes evaluated from a frontal view by either descending or impacting one side (Fig. 21-5). In other words, roll is rotation of the coronal plane around the z axis.
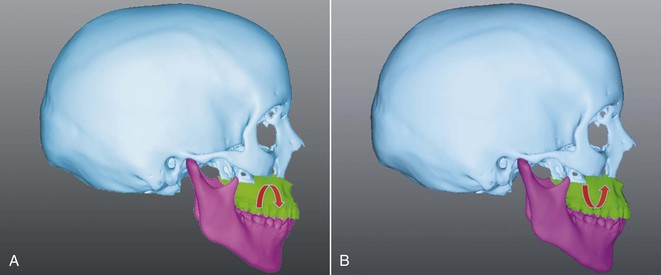
Figure 21-3 Pitch, or inclination movements of the maxilla and mandible in the sagittal plane. A, Clockwise rotation. B, Counterclockwise rotation.
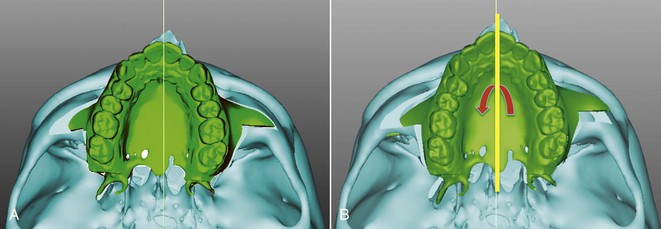
Figure 21-4 Yaw, or rotational movement of the maxilla around a vertical or y axis in order to correct the maxillary skeletal and dental midline. A, Maxillary skeletal deviation evaluated in the axial plane. B, Correction of the maxillary deviation by counterclockwise rotation in the axial plane.
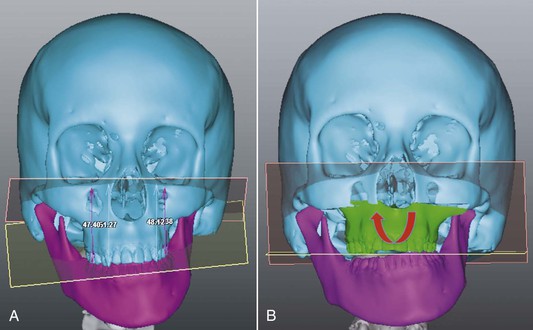
Figure 21-5 Roll, or rotational movements of the maxilla or the mandible around an anteroposterior axis or z axis to correct asymmetries in a vertical direction A, Significant occlusal cant evaluated in the coronal plane. B, Virtual osteotomy correcting the deformity by addressing the roll deviation.
Time: The Fourth Dimension in Orthognathic Surgery
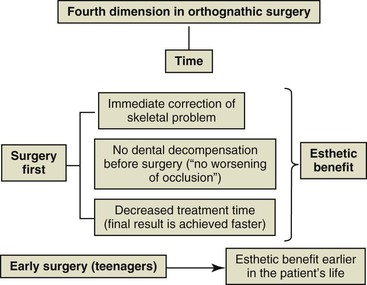
Time is another important aspect to consider in orthognathic surgery from two key perspectives. The first relates to the total treatment duration of the combined orthodontic and surgical interventions and the second relates to the appropriate time to execute the surgery. Total treatment time has been reduced with the “surgery first approach.”13,14 With this approach presurgical orthodontics is eliminated, thus reducing the total treatment time compared to the traditional three-phase approach: presurgical orthodontics, orthognathic surgery, and postsurgical orthodontics. In addition, there is immediate resolution of the dentofacial deformity and esthetics are not negatively affected by the dentoalveolar decompensation that accompanies the presurgical orthodontic phase (Fig. 21-6).
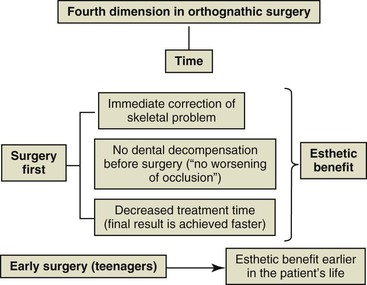
Figure 21-6 Time as the fourth dimension in orthognathic surgery.
The other aspect related to time is the age at which orthognathic surgery is performed, or surgical timing. Traditionally, orthognathic surgery was performed once maxillary and mandibular growth was complete. However, we can positively affect patients who have significant dentoalveolar deformities by performing early surgery (during adolescence). This allows for favorable facial change during a key stage of life in which the psychosocial aspect has great influence (see Fig. 21-6). In fact, early surgery or surgery during growth has been described by Wolford et al.15,16 as a viable option in different types of orthognathic surgical approaches if certain surgical considerations are followed.
Macroesthetics, Miniesthetics, and Microesthetics
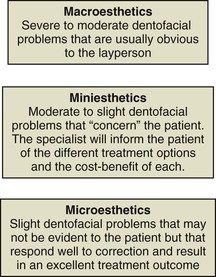
There are three major components that define esthetics in surgical cases: macroesthetics, miniesthetics, and microesthetics. These subgroups are based on the size and magnitude of deviation from the norm and should be considered carefully. Macroesthetics refers to the face, miniesthetics refers to the smile, and microesthetics refers to the esthetic characteristics of the teeth and gingival complex.17
Although this concept lays a good foundation for a classification system for facial esthetics, macroesthetics should include not only deviations from the norm of the face but also problems that affect the smile. In this line of thinking, macroesthetics is defined as the dentofacial problems that are usually identifiable by a layperson, orthodontist, or surgeon (Fig. 21-7). These problems include moderate to severe Class II or Class III skeletal anomalies, marked asymmetries, and vertical problems. The facial soft tissues would logically include labial or facial fissures and other visibly apparent anomalies that compromise facial esthetics. Intraorally, macroesthetics includes crowding, tooth malposition, missing teeth or teeth in poor condition (teeth with fractures, excessive wear, or discoloration), or severe gingival recession in the esthetic zone. The chief complaint also influences how to classify a problem in the macroesthetic, miniesthetic, and microesthetic categories.
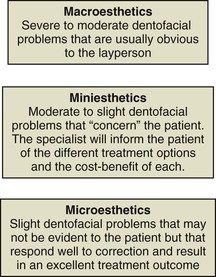
Figure 21-7 Definitions of macroesthetics, miniesthetics, and microesthetics.
Miniesthetics refers to slight to moderate facial or dental problems that are not so obvious that they can be pinpointed by the patient but that drive the patient to consult a clinician for an improvement in his or her smile. For example, patients consult for problems in the vertical dimension, such as slight or moderate gingival smile or slight to moderate skeletal Class II or Class III with dental compensations. Dentally, miniesthetics refers to tooth malposition, discoloration, diastemas or gingival recession, and other features that are not overtly evident.
Microesthetics refers to slight deviations from the norm that the patient has not identified but, if corrected, will enhance the smile esthetics. These details are what define the difference between a good result and an excellent one. Microesthetics would correspond to the correction of slight tooth malposition in the anterior esthetic zone, gingival recession or uneven gingival margins of more than 1-mm, and excessive tooth discoloration.
Case Reports
The following four cases illustrate the concepts of treatment planning; time as the fourth dimension; and macroesthetics, miniesthetics, and microesthetics in orthognathic surgery.
 Case Report 1
Case Report 1
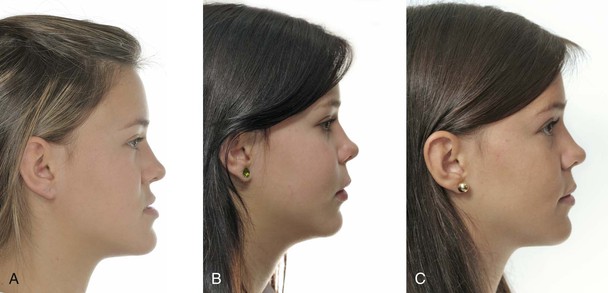
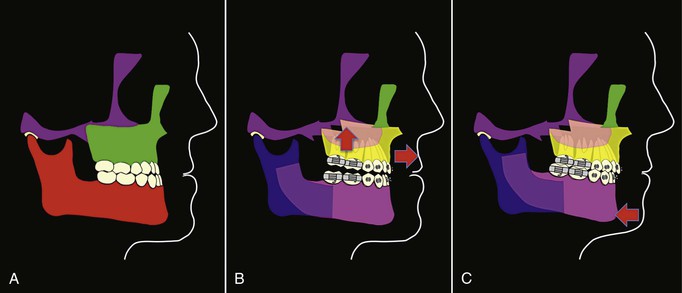
Figure 21-8 depicts the change in the facial profile and occlusion in a 17-year-old patient with a severe skeletal Class III malocclusion from pre-treatment (see Fig. 21-8, A) to 6 weeks after appliance insertion (see Fig. 21-8, B) to post-treatment after 8 months (see Fig. 21-8, C), when the orthodontic-surgical treatment was finished. The facial profile as well as the occlusion and dental appearance were clearly compromised in the initial photographs, which affected the macroesthetics. The patient had a maxillary advancement and mandibular setback with the benefits of the “surgery first approach,” namely (1) no dental decompensations prior to surgery, thereby preventing facial profile deterioration; (2) an immediate facial change after the patient decided to undergo surgery; and (3) completion of orthodontic-surgical treatment 8 months after surgery. Again, this illustrates a very short period of treatment compared to a conventional three-stage approach with presurgical orthodontics, orthognathic surgery, and postsurgical orthodontics treatment.
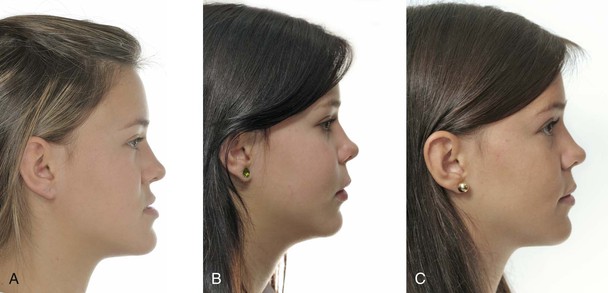
Figure 21-8 A, Profile maxillomandibular relationship revealing a severe Class III skeletal dentofacial deformity at pre-treatment. B, Correction of the skeletal and dental aspects with a “surgery first approach” (6 weeks after surgery). C, Final profile and occlusal outcome after 8 months of treatment.
The anteroposterior and vertical position of the maxillary incisors at rest is one of the most important clinical aspects to evaluate in surgical treatment planning. The determination of the maxillary incisor position in space is the cornerstone used to sequentially position the other structures of the dentofacial complex. It could be regarded as the reference landmark used to plan the key dental and osseous movements. An adequate incisor position at rest in the vertical dimension, approximately 2- to 3-mm of incisor display, will most likely result in a good esthetic outcome in the middle facial third and the smile line.
An important consideration in the determination of the vertical position of the incisors, based on the amount of display on smile, is the evaluation of lip mobility. Patients who have labial hypermobility will most likely have increased gingival display on smiling, regardless of an adequate exposure of the upper incisors at rest. If the maxilla is impacted in such patients, the smile vertical display may be corrected but this will occur at the expense of no display of the incisors during speech, which gives an inadequate appearance of edentulism, a significant negative impact in facial esthetics. Therefore it is very important to evaluate the patient both at rest and on smiling and it is recommended that the final vertical position of the incisors should err in the direction of slightly excessive gingival display on smiling rather than an outcome with no incisor display at rest.
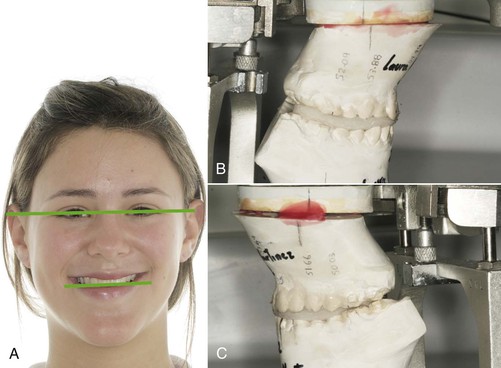
After considering the maxillary incisor position in a vertical dimension, the vertical position of the maxillary buccal segments should follow. Any deviation of the yaw of the maxilla should be appraised and corrected if indicated. The proper positioning of these buccal segments in combination with the adequate display of the maxillary anterior segment will yield optimal smile esthetics from a frontal view (Fig. 21-9). Figure 21-10 shows the inclination or cant of the upper occlusal plane with respect to the bipupilar line. The occlusal plane was more caudal on the right side and more coronal on the left side. Three options were available to level the occlusal cant: (1) impaction of the right buccal segment, (2) inferior repositioning of the left segment, or (3) a combination of both by means of a slight ascent of the right side and a slight descent of the left side. Since the amount of incisor display was reduced on both rest and smile, an inferior repositioning of the left side by 2-mm combined with rotation around the crowns of the right buccal segment was performed (see Figs. 21-10, B and C).

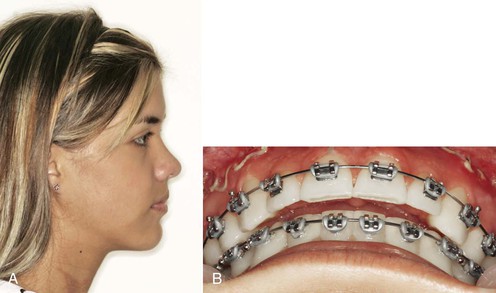
Figure 21-9 A, Frontal presurgical and (B) postsurgical result showing the macroesthetics and miniesthetics outcomes after an adequate treatment plan and surgical intervention.
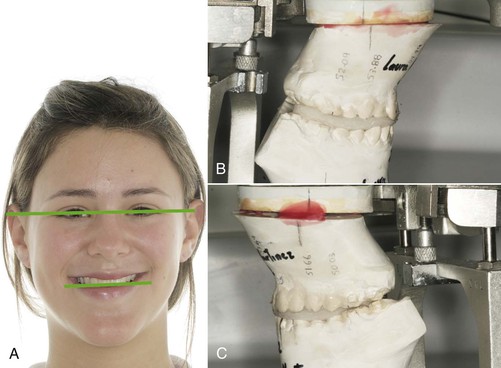
Figure 21-10 A, Occlusal cant in relation to the bipupilar line. B, No vertical repositioning of the maxilla on the right side for the cant correction. C, Inferior repositioning of the left side of the maxilla to improve the tooth display on that side and correct the occlusal cant (roll).
It is very important to keep in mind the effect of sagittal maxillary movements on incisor display. Although the 2-mm of maxillary descent on the left side adequately leveled the occlusal plane, it did not provide sufficient incisor display at rest. However, an important consideration was that the maxilla was to be advanced in order to project the middle third forward. The result of this anterior repositioning of the maxilla is an increase in incisor display, both at rest and on smiling. This effect of the anteroposterior surgical movement of the maxilla on the vertical display of the incisors is important to consider in the planning of the maxillary position in space.
Concurrent with the maxillary positioning of the buccal segments, it is important to evaluate the pitch from a sagittal perspective. Although not very commonly appraised, this inclination has important consequences on the consonance of the smile line with the lower lip. That is, the flatter the plane in reference to the anterior cranial base plane, the more difficult it is to achieve a consonant smile and the increased chance of a flat or reverse smile arc. Finally, once the maxilla has been positioned correctly in space, the mandible is guided to its correct position based on the maxillary midline and the buccal occlusal relationship. Refinement of the esthetics in all three dimensions can be obtained by means of a genioplasty when indicated.
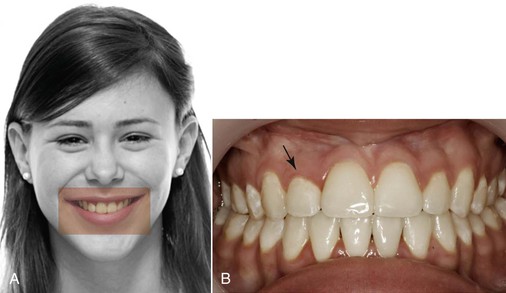
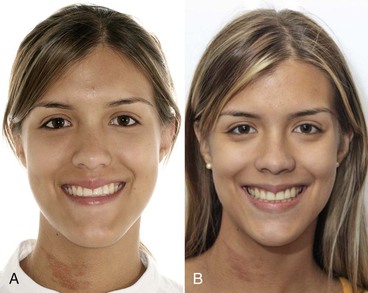
Once the surgical procedure is completed, treatment continues with the postsurgical orthodontics phase. At the end of orthodontic treatment, minor surgical procedures in gingival contouring further refine the esthetic result. Figure 21-9 shows the changes in microesthetics in the smile after completion of the orthodontic treatment. The patient showed a low smile line without exposure of the upper incisors, which was corrected with surgery, thereby improving her miniesthetics. Although the postsurgical improvements to her smile line were very adequate, the fact that the upper right lateral incisor was shorter than the left made the asymmetry of the gingival margins more noticeable, thereby compromising the microesthetics (Fig. 21-11). Figure 21-12 depicts a minimally invasive periodontal surgery performed in order to displace the gingival margin apically by 1.5-mm in the upper right lateral incisor. In addition, the patient had tooth whitening, which complemented the microesthetics. Figure 21-13 shows the impact of these procedures, which addressed the microesthetics in the final esthetic outcome.
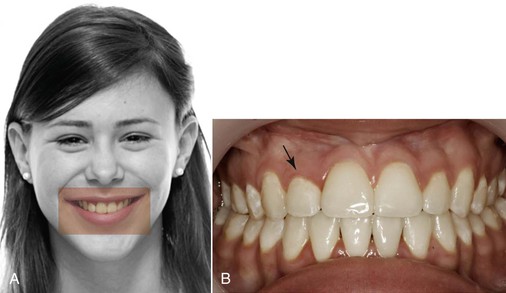
Figure 21-11 A, Microesthetics problem noticeable in the smile. B, Intraoral photograph showing the asymmetrical maxillary gingival margin of the right lateral incisor with reduced crown length.

Figure 21-12 Crown lengthening procedure on the right maxillary lateral incisor to match the gingival margin of the maxillary left lateral incisor. A, Flap showing the crestal bone level. B, Removal of the crestal bone to establish adequate biological width. C, Final result showing the improvement in the symmetry and proportion of the anterior teeth in the esthetic zone.

Figure 21-13 Difference in the smile esthetics of the patient (A) before and (B) after two procedures related to microesthetics (crown lengthening and tooth whitening). These two microesthetic details mark the difference between a good result and an excellent one. (Case from Uribe F, Villegas C, Nanda R. Surgically enhancing the speed of tooth movement: Can we alter the biology? In: McNamara JA Jr, Kapila SD, eds. Surgical Enhancement of Orthodontic Treatment. Ann Arbor, MI: The University of Michigan, 2010:323–344.)
 Case Report 2
Case Report 2
Figure 21-14 shows a 12-year-old female patient who presented with a significant dentofacial deformity involving severe crowding in the maxillary arch, lip incompetence, and excessive and asymmetrical gingival display due to vertical excess of the maxilla. Additionally, mandibular retrognathism due to posterior mandibular rotation was present, compromising her dental and facial macroesthetics.

Figure 21-14 Patient with significant dentofacial deformity. A, Frontal view depicting the long lower facial height and increased interlabial gap. B, Excessive asymmetrical gingival display with incisal cant and maxillary lateral incisor not visible due to excessive crowding (macroesthetic problems). C, Profile view displaying an acute nasolabial angle, long lower facial height, increased interlabial gap, and retrognathic mandible. D, Frontal intraoral view illustrating excessive crowding, anterior open bite, canted incisal plane, and significant midline discrepancy. E, Occlusal view showing the maxillary crowding and blocked-out right lateral incisor.
A surgical plan involving conventional orthognathic surgery was established. In the maxillary arch, presurgical orthodontics without extractions was completed through distalization of the molars using a bone-supported dual-force distalizer (DFD) (Fig. 21-15).18 Some of the dental macroesthetic problems, such as excessive crowding in the anterior segment and an incisal cant, were resolved in this presurgical orthodontic phase (Fig. 21-16, A). However, the facial macroesthetics involving the excessive gingival display and long vertical proportions with poor chin projection remained unresolved (Fig. 21-16, B).

Figure 21-15 Distalization by means of the dual-force distalizer (DFD) to address the crowding.
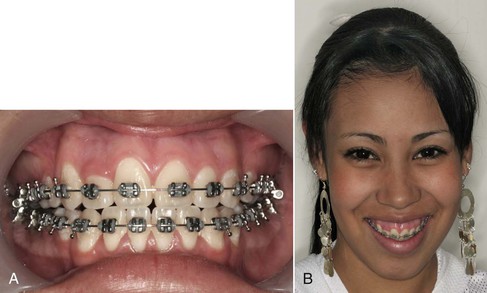
Figure 21-16 A, Good arch alignment with incisal cant resolved and maxillary right lateral incisor incorporated in the arch. B, Excessive gingival display compromising macroesthetics.
Early bimaxillary orthognathic surgery and mentoplasty were performed at age 13 years, 6 months to address these macroesthetic concerns, which were having a psychosocial impact on the patient at that stage. A Le Fort I osteotomy was performed to impact the maxilla by 7-mm. Bilateral sagittal split osteotomy (BSSO) of the mandible was also performed to align the occlusion, obtaining a Class I molar relationship. In addition, an 8-mm advancing genioplasty was performed to project the chin point anteriorly and superiorly (Fig. 21-17).
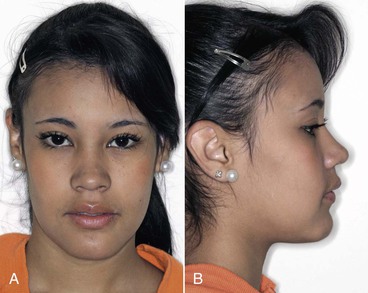
Figure 21-17 Postsurgical result with significant reduction in the interlabial gap and nasolabial angle and improvement in facial proportions and chin projection. A, Frontal view. B, Profile view.
The surgery corrected the facial macroesthetic problems of excessive gingival display at rest and smile, excessive interlabial gap, a convex profile, and poor chin projection. This patient was treated with the traditional sequence of presurgical orthodontics, orthognathic surgery, and postsurgical orthodontics. Total treatment time was 30 months; therefore there was no real benefit regarding treatment time. We did observe that by doing the surgery early (13 years, 6 months), the patient benefited by having her dentofacial esthetic problem corrected without having to wait until age 16 or 18 years to obtain this favorable change.
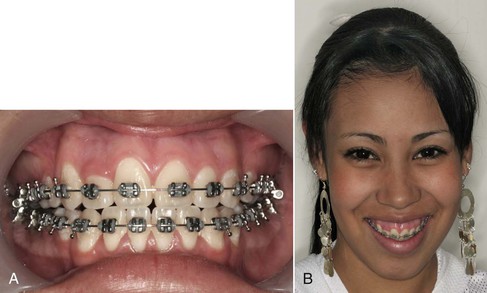
The macroesthetics and miniesthetics were addressed with the combined surgical-orthodontic plan. However, the microesthetic component of the smile needed additional refinement. Figure 21-18 shows the right maxillary lateral incisor with a shorter clinical crown compared to the contralateral side and not matching the normal maxillary anterior gingival height architecture of the adjacent teeth. This discrepancy was noticeable on smiling; however, the patient had not noticed this issue. Figure 21-19 shows the significant improvement in the smile and overall esthetics that was obtained once gingivectomy was performed to elongate the crown of the right lateral incisor.

Figure 21-18 Postsurgical result from the frontal view. A, Adequate occlusal outcome; however, the microesthetics are still not perfect, with a gingival discrepancy between lateral incisors. B, Smile highlighting the microesthetics problem observed in the difference in symmetry and proportions of the maxillary right lateral incisor and the adjacent teeth.

Figure 21-19 A, Microesthetics addressed with a gingivectomy of the maxillary right lateral incisor. B, Microesthetic detail affecting the overall esthetic outcome.
 Case Report 3
Case Report 3
Figure 21-20 shows an 18-year-old patient with the chief complaint of excessive wear of the anterior teeth. The patient related having completed orthodontic treatment with extractions of all first premolars 2 years prior but over time the bite had reached an anterior edge-to-edge relationship (see Fig. 21-20, A). Facially, the patient presented with a slightly concave profile (see Fig. 21-20, B), with a desire to improve her facial esthetics only if the treatment was not “long and traumatic.” The patient had consulted several other orthodontists, who had said that the correction of the dental problem was very risky because of the magnitude of root resorption from the previous orthodontic treatment, mainly in the upper lateral incisors and the upper left second premolar (Fig. 21-21).

Figure 21-20 A, Patient with a Class III malocclusion treated with orthodontics 2 years prior to her consultation. Wear of the incisors was evident, with an edge-to-edge incisor relationship that was not favorable for the integrity of the dentition in the long-term. B, Moderate Class III skeletal relationship with obvious midface deficiency.

Figure 21-21 Panoramic radiograph depicting the significant root resorption noticed in the maxillary left second premolar and lateral incisors.
A surgical orthodontic treatment with a “surgery first approach” was presented to the patient in order to address the occlusal and esthetics issues, minimizing the time with orthodontic appliances and thus reducing the chances of further root resorption. This treatment plan included a clockwise rotation of the maxillomandibular complex. To accomplish this, a high Le Fort I osteotomy was planned to impact the maxilla 3-mm posteriorly and advance it by 3-mm to project the paranasal region and the upper lip forward (Fig. 21-22, A and B). In addition, a bilateral sagittal osteotomy of the mandible to set back the chin point by 3-mm was planned. This resulted in an orthognathic profile with slightly less chin projection (Fig. 21-22, C).
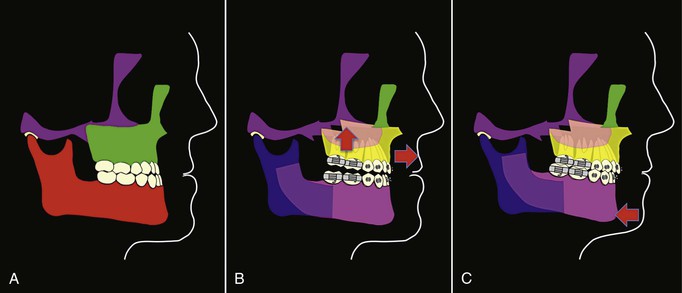
Figure 21-22 Cartoons depicting the surgical movements. A, Presurgery. B, Maxillary advancement and posterior impaction resulting in clockwise occlusal plane rotation. C, Mandibular setback and occlusal plane rotation to match the maxilla.
These procedures evidently produced an orthognathic profile (Fig. 21-23, A) where the middle third was projected forward and the mandible was displaced slightly down and back with a slightly increased postsurgical overjet (Fig. 21-23, B) that was corrected during the postsurgical orthodontic treatment. Figure 21-24 shows the final result after the orthodontic postsurgical phase, which lasted 2 months and 28 days. Once again it can be observed that the “surgery first approach” sequence helps to streamline a treatment that traditionally would have been longer and possibly had a higher biological cost for the teeth that presented root resorption.
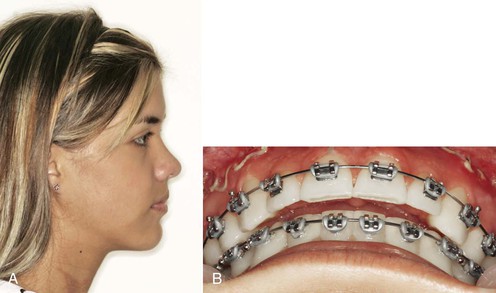
Figure 21-23 A, Postsurgical orthognathic profile. B, Slightly increased overjet left to decompensate the lower incisors. This is a common practice in the “surgery first approach.”

Figure 21-24 Postsurgical occlusion 2 months and 28 days after surgery at debonding. A, Adequate overbite, midline relationship, and occlusion. B, Note the final overjet.
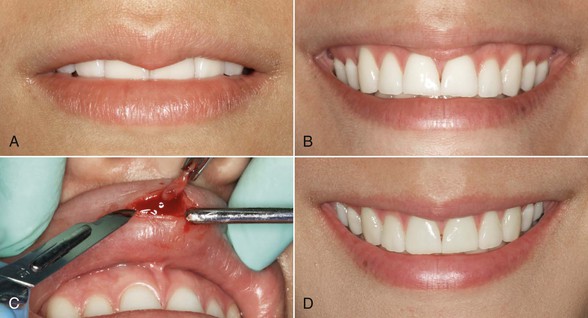
Figure 21-25 shows the change in the smile with the combined surgical-orthodontic treatment. The clockwise rotation of the maxilla around the upper central incisors edge had a significant effect on the smile esthetics by steepening the flat presurgical occlusal plane. This steepening aided in developing a consonant smile arc from the presurgical flat smile arc without affecting vertically the incisor display. Also, by impacting the maxilla posteriorly, the gingival display in the buccal segments was reduced. However, when the microesthetics of the maxillary lip was evaluated at rest and on smiling (Fig. 21-26, A and B), a lip eversion with redundant tissue noticeably compromised the esthetics of the smile. To correct this microesthetic issue, an elliptical excision of a portion of the labial mucosa was performed (Fig. 21-26, C). Although the patient was unaware that the mucosa everted when she smiled, she was pleased that it could be corrected through a simple procedure and had a dramatic improvement in the smile microesthetics (Fig. 21-26, D). This example clearly illustrates that, as clinicians, we are responsible for detecting small microesthetic deviations and advising patients on the viability and complexity of their correction.
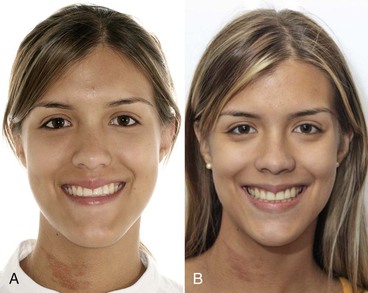
Figure 21-25 A, Pre-treatment and (B) post-treatment esthetics. Note the difference in macroesthetics and miniesthetics. Positive results are observed in the face and the smile. Notably, the occlusal plane clockwise rotation facilitated the possibility of obtaining a consonant smile and reducing the posterior gingival display.
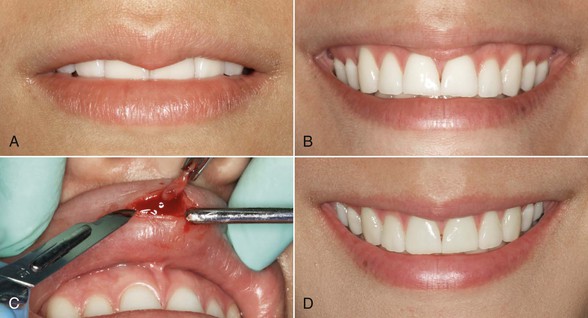
Figure 21-26 Microesthetics in the lip soft tissue are addressed. A, Small redundant tissue in the lip philtrum at rest. B, Redundant tissue more evident on smile. C, Minor excision of the redundant lip tissue. D, Improvement in the microesthetics after minimally invasive lip procedure. (Case from Villegas C, Janakiraman N, Uribe F, Nanda R. Rotation of the maxillo-mandibular complex to enhance esthetics using the Surgery First Approach. J Clin Orthod. 2012;46[2]:85–91.)
 Case Report 4
Case Report 4
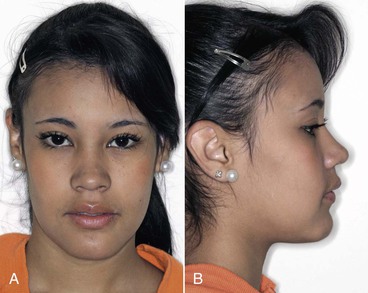
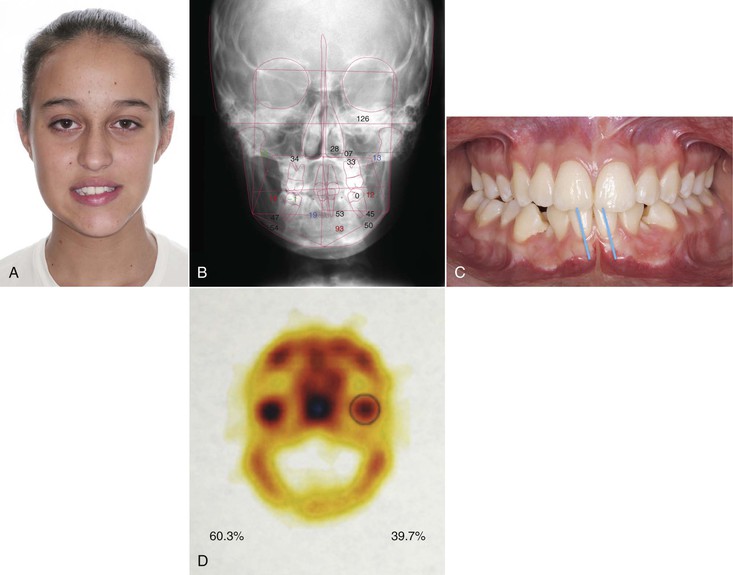
An 11.2-year-old female patient consulted for a facial asymmetry that had progressed during the last year. The physical exam revealed deviation of the chin toward the left side. An occlusal plane cant was observed as a result of increased vertical growth of the right side (Fig. 21-27, A and B). Deviation of the lower dental midline was not notable since the lower incisors had compensated with their axial inclination for the present mandibular asymmetry (Fig. 21-27, C). A comparative scintigraphy of the mandibular condyles revealed the presence of 60.3% of the contrast media on the right condyle and 39.7% on the left condyle; this confirmed the diagnosis of active hyperplasia of the right condyle (Fig. 21-27, D).19
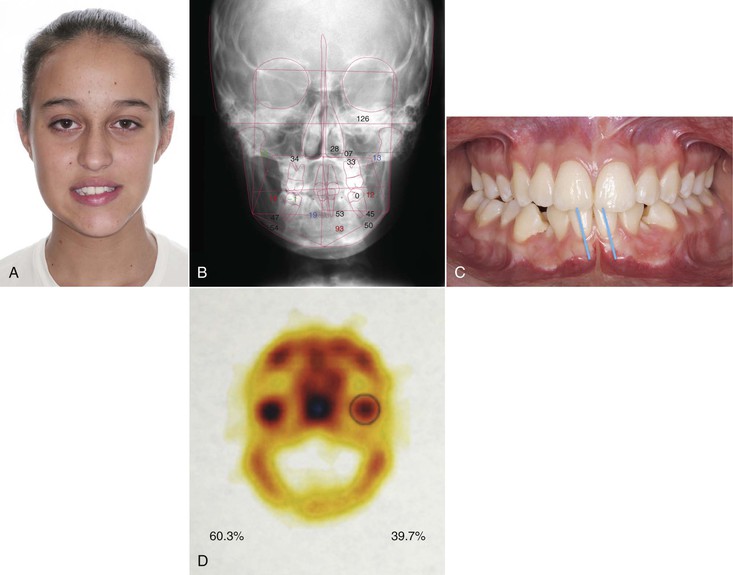
Figure 21-27 A, Patient with gross asymmetry noticed during growth. B, Posteroanterior cephalogram showing the significant maxillary and mandibular asymmetry. C, Lower incisor inclination trying to compensate for the facial asymmetry showing no midline deviation in relation to the maxilla at the incisal edge. D, Bone scan reflecting abnormal uptake of the radioactive marker on the right condyle.
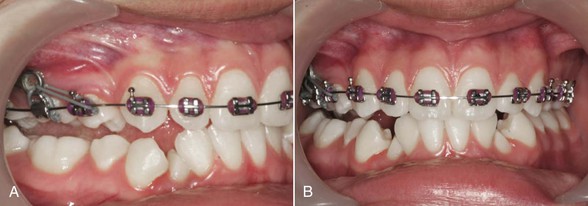
Based on this diagnosis, a high intracapsular condylectomy of the right condyle was performed and an infrazygomatic mini-plate was placed on the right side. In addition, mini-screws were placed in the palate to serve as skeletal anchorage in conjunction with the mini-plate in order to level the occlusal plane without tipping by intruding the teeth on the right side. Figure 21-28 shows the posterior open bite obtained in the right side after the intrusion and the deviation of the lower midline toward the right side after the condylectomy.
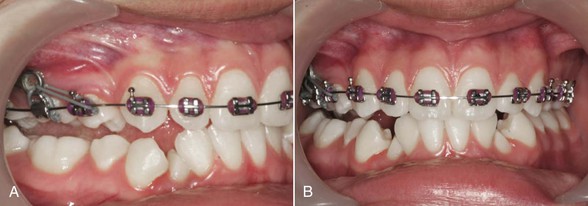
Figure 21-28 A, Force from right buccal mini-plate to intrude the buccal segment and correct the occlusal cant. B, Intentional lateral open bite created by the intrusion of the right maxillary buccal segment.
Orthodontic treatment with extraction of the first lower premolars was then performed. The patient had extractions of the maxillary first premolars during a prior orthodontic treatment. The infrazygomatic mini-plate was used as anchorage to extrude the mandibular right buccal segment, close the posterior open bite, and level the lower occlusal plane (Fig. 21-29).

Figure 21-29 A and B, Force delivered by an intermaxillary elastic to erupt the lower right buccal segment to match the intruded maxillary right buccal segment. C, No intrusive or extrusive mechanics were attempted on the left side.
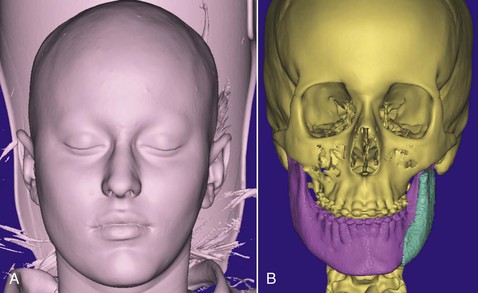
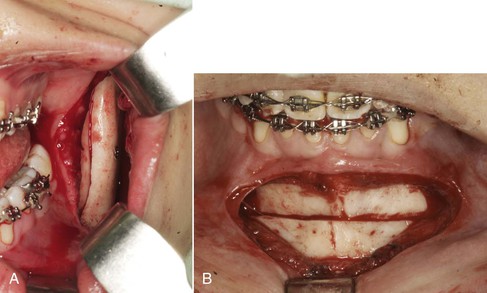
Figure 21-30 shows that even though the facial asymmetry improved after the condylectomy and the leveling of the occlusal plane, a deviation of the chin toward the left side and a difference in volume in the area of the mandibular corpus and ramus was still noticed. Larger facial tissue volume on the right side was evident when compared to the left side. A medical computed tomography (CT) was ordered to quantify the degree of asymmetry and define the amount of volume that was missing (Fig. 21-31, A). A mirror image of both sides was virtually analyzed and a polymethylmethacrylate (PMMA) implant was designed (Fig. 21-31, B), inserted, and fixed with two 2-mm × 13-mm titanium screws (Fig. 21-32, A) (Lomas, PSM Medical Solutions, Tuttlingen, Germany) on the left side to restitute the missing tissue volume. A lateral sliding genioplasty toward the right side refined the correction of the asymmetry (Fig. 21-32, B).

Figure 21-30 A, Facial asymmetry was improved, although a significant deficiency in tissue mass was observed on the left side compared to the right. B, Maxillary cant was corrected but the asymmetrical animation of the lower lip and general left to right asymmetry was more obvious on smile.
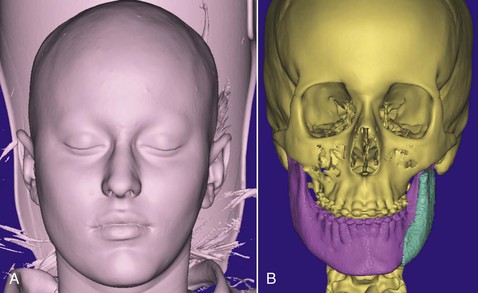
Figure 21-31 Medical computed tomography was used to evaluate the (A) soft tissue and (B) hard tissue asymmetry. Using a mirroring technique, a custom-made implant was designed to fill the missing hard and soft tissue volume on the left lower face.
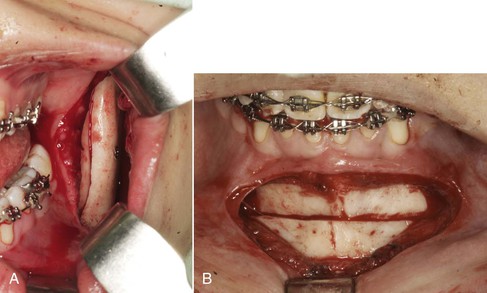
Figure 21-32 A, Insertion of the custom-made implant secured with two screws laterally to the left ramus. B, Lateral sliding genioplasty complemented the surgical procedure to significantly improve facial asymmetry.
Figure 21-33 shows the improvement in overall symmetry. The facial contour definition was refined and made symmetrical with secondary effects on the smile. An important aspect to highlight is that the left animation of the lower lip commissure, which was significantly asymmetrical, was improved with the tissue volume augmentation via the facial implant and the lateral displacement of the chin achieved with the genioplasty.

Figure 21-33 Improvement in overall asymmetry evaluated (A) at rest and (B) on smile. Note the more symmetrical soft tissue volume and animation of the lower lip. (Case from Villegas C, Janakiraman N, Nanda R, Uribe F. Management of unilateral condylar hyperplasia with a high condylectomy, skeletal anchorage, and a CAD/CAM alloplast. J Clin Orthod. 2013;47[6]:365–374.)
Summary
It is important to keep in mind several key factors when analyzing patients and deciding how they will benefit from a surgical-orthodontic treatment:
• Treatment plans must be individualized and should not only consider the significant esthetic changes that can be obtained with the proper rearrangement of the facial bones, but also pay close attention to the small details that differentiate a good outcome from an excellent outcome.
• Subjective and objective goals guide the treatment planning process in orthognathic surgery.
• Macroesthetics, miniesthetics, and microesthetics are components of a classification system that can be used as a framework to methodically approach esthetics from a global perspective to a more detailed focus. Symmetry, averageness, and proportion are important pillars in the achievement of optimal facial esthetics.
• The fourth dimension, time, can be addressed with the “surgery first approach,” which significantly shortens the duration of treatment. In addition, early surgery during adolescence should be considered in psychosocially compromised patients.
• Technology allows us to evaluate dentofacial deformities in three dimensions with great accuracy. Treatment plans and their execution should address those deviations to the full extent in order to justify the use of these technologies. Small refinements in symmetry may be one of the greatest advantages, where left to right asymmetries can be assessed in detail and corrected by subtraction or addition using these technologies. However, it is important to consider the cost-benefit of using these technologies on a case-by-case basis.
References
1. Hungerford MW. Molly Bawn. England: Smith, Elder, & Co: London; 1878.
2. Thornhill R, Gangestad SW. Facial attractiveness. Trends Cogn Sci. 1999;3:452–460.
3. Bashour M. History and current concepts in the analysis of facial attractiveness. Plast Reconstr Surg. 2006;118:741–756.
4. Grammer K, Fink B, Moller AP, Thornhill R. Darwinian aesthetics: sexual selection and the biology of beauty. Biol Rev Camb Philos Soc. 2003;78:385–407.
5. Langlois JH, Roggman LA. Attractive faces are only average. Psychol Sci. 1991;1:115–121.
6. Grammer K, Thornhill R. Human (Homo sapiens) facial attractiveness and sexual selection: the role of symmetry and averageness. J Comp Psychol. 1994;108:233–242.
7. Murphy C, Kearns G, Sleeman D, Cronin M, Allen PF. The clinical relevance of orthognathic surgery on quality of life. Int J Oral Maxillofac Surg. 2011;40:926–930.
8. Lee LH, Jun JH, Danganan M, Pogrel MA, Kushner H, Lee JS. Orthognathic surgery for the Asian patient and the influence of the surgeon's background on treatment. Int J Oral Maxillofac Surg. 2011;40:458–463.
9. Gateno J, Xia JJ, Teichgraeber JF, et al. Clinical feasibility of computer-aided surgical simulation (CASS) in the treatment of complex cranio-maxillofacial deformities. J Oral Maxillofac Surg. 2007;65:728–734.
10. Quevedo LA, Ruiz JV, Quevedo CA. Using a clinical protocol for orthognathic surgery and assessing a 3-dimensional virtual approach: current therapy. J Oral Maxillofac Surg. 2011;69:623–637.
11. Swennen GR, Mollemans W, De Clercq C, et al. A cone-beam computed tomography triple scan procedure to obtain a three-dimensional augmented virtual skull model appropriate for orthognathic surgery planning. J Craniofac Surg. 2009;20:297–307.
12. Ackerman JL, Proffit WR, Sarver DM, Ackerman MB, Kean MR. Pitch, roll, and yaw: describing the spatial orientation of dentofacial traits. Am J Orthod Dentofacial Orthop. 2007;131:305–310.
13. Nagasaka H, Sugawara J, Kawamura H, Nanda R. “Surgery first” skeletal Class III correction using the skeletal anchorage system. J Clin Orthod. 2009;43:97–105.
14. Villegas C, Uribe F, Sugawara J, Nanda R. Expedited correction of significant dentofacial asymmetry using a “surgery first” approach. J Clin Orthod. 2010;44:97–103.
15. Wolford LM, Karras SC, Mehra P. Considerations for orthognathic surgery during growth, part 1: mandibular deformities. Am J Orthod Dentofacial Orthop. 2001;119:95–101.
16. Wolford LM, Karras SC, Mehra P. Considerations for orthognathic surgery during growth, part 2: maxillary deformities. Am J Orthod Dentofacial Orthop. 2001;119:102–105.
17. Sarver DM. Augmenting and improving esthetics through surgical intervention. McNamara JA, Kapila SD. Surgical Enhancement of Orthodontic Treatment. The University of Michigan: Ann Arbor, MI; 2010:1–31.
18. Oberti G, Villegas C, Ealo M, Palacio JC, Baccetti T. Maxillary molar distalization with the dual-force distalizer supported by mini-implants: a clinical study. Am J Orthod Dentofacial Orthop. 2009;135 [282.e1–5] .
19. Hodder SC, Rees JI, Oliver TB, Facey PE, Sugar AW. SPECT bone scintigraphy in the diagnosis and management of mandibular condylar hyperplasia. Br J Oral Maxillofac Surg. 2000;38:87–93.