Informatics and Documentation
• Identify key reasons for reporting and recording patient care.
• Describe guidelines for effective documentation and reporting in a variety of health care settings.
• Describe methods for interdisciplinary communication within the health care team.
• Compare different methods used in documentation.
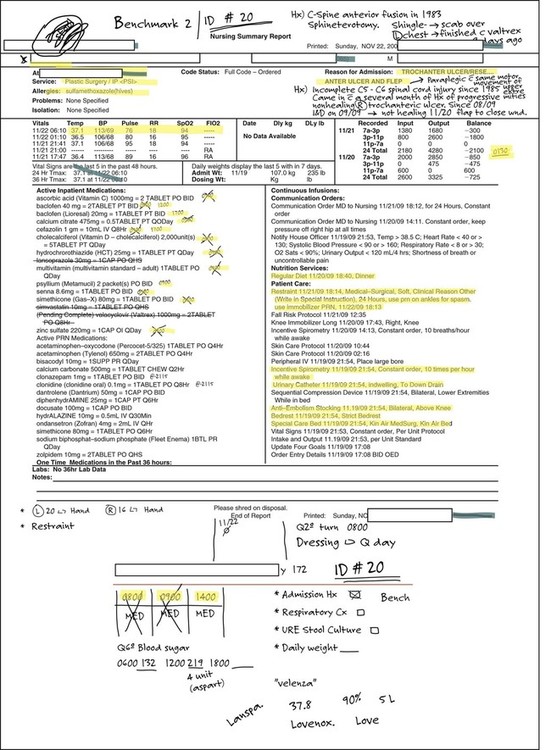
• Identify common record-keeping forms.
• Discuss advantages and disadvantages of standardized documentation forms.
• Discuss advantages of computerized documentation.
• Discuss the relationship between informatics and quality health care.
Introduction
Documentation is a vital aspect of nursing practice. It is a key element of nursing practice and a key communication strategy between health care professionals (Pirie, 2011). It is defined as anything written or printed within a patient record, which may be paper, electronic, or a combination of both formats. The information you communicate about patient care reflects the type and frequency of care and provides accountability for each health care team member's care. The patient record provides evidence for credentialing, research, and reimbursement and a database for planning health care (ANA, 2010). In the patient's record document the nursing care you provide for a patient (e.g., assessments and interventions).
The health care environment creates many challenges for accurately documenting and reporting patient care. Quality nursing care depends on your ability to communicate effectively verbally and in writing, and you are held accountable for the accuracy of documentation you enter into the patient's record. Regulations from agencies such as The Joint Commission (TJC) and the Centers for Medicare and Medicaid Services (CMS) require health care institutions to monitor and evaluate the quality and appropriateness of patient care (ANA, 2010) (see Chapters 3 and 13). Typically such monitoring and evaluation occur through auditing information that health care providers document in patient records. As of October 1, 2008, Medicare no longer reimburses hospitals for certain preventable conditions such as hospital-acquired illnesses and injuries, (e.g., a urinary tract infection following catheterization or new pressure ulcers) (Geiger, 2012; Hellier, 2010). Thus it becomes even more important that your documentation accurately reflects the status of the patient, especially on admission, transfer, or discharge.
Confidentiality
Nurses are legally and ethically obligated to keep information about patients confidential. Do not disclose information about a patient's status to other patients, family members (unless granted by the patient), or health care staff not involved in their care. Patients frequently request copies of their medical records, and they have the right to read them. Each institution has policies to control how medical records are shared. In most situations patients are required to give written permission for release of medical information.
The Health Insurance Portability and Accountability Act (HIPAA), which provides legislation to protect patient privacy for health information, governs all areas of health information management, including reimbursement, medical record coding, security, and patient record management. Under new regulations, to eliminate barriers that delay access to care, providers are required to notify patients of their privacy policy and make a reasonable effort to get written acknowledgment of this notification. HIPAA requires that disclosure or requests regarding health information be limited to the minimum necessary. This includes only the specific information required for a particular purpose. For example, if you need a patient's home telephone number to reschedule an appointment, access to the medical records is limited solely to telephone information.
Sometimes you have a reason for using health care records for data gathering, research, or continuing education. This is permitted if you use the records as specified and permission is granted. When you are a student in a clinical setting, confidentiality and compliance with HIPAA legislation are part of professional practice. You may review the medical record only for information needed to provide safe, efficient care. For example, when you are assigned to provide complete care for a patient, you need to review the current medical record and plan of care. However, you do not share this information with other classmates. In addition, never access the medical records of other patients on the specific clinical care area. Access to electronic health records (EHRs) is traced through the user log-in information. Not only is it unethical to view medical records of other patients, but breaches of confidentiality lead to disciplinary action by employers and even possible dismissal from work. To further maintain confidentiality and protect patient privacy, make sure that written materials used in your student clinical practice do not include patient identifiers such as room number, date of birth, medical record number, or other identifiable demographic information. Equally important, never print material from the EHR for personal use because it is a violation of HIPAA.
Standards
Within a health care organization there are standards that govern the type of information you document. Institutional standards or policies often dictate the frequency of documentation such as how often you record a nursing assessment or a patient's level of pain. Know the standards of your health care organization to ensure complete and accurate documentation. Nurses are expected to meet the standard of care for every nursing task they perform. Patient records are used as evidence in a court of law if standards are not met (ANA, 2010).
In addition, your documentation must conform to the standards of the National Committee for Quality Assurance (NCQA) and accrediting bodies such as TJC to maintain institutional accreditation and minimize liability. Usually an organization incorporates accreditation standards into its policies and revises documentation forms to suit these standards. Current documentation standards require that all patients admitted to a health care facility have an assessment of physical, psychosocial, environmental, self-care, knowledge level, and discharge planning needs. TJC standard for record of care, treatment, and services requires that your documentation be within the context of the nursing process, including evidence of patient and family teaching and discharge planning (TJC, 2012). Other standards such as HIPAA include those directed by state and federal regulatory agencies and are enforced through the Department of Justice and the CMS (ANA, 2010).
Interdisciplinary Communication within the Health Care Team
The typical patient has many caregivers, including nurses, physicians, nursing assistive personnel, and therapists. To maintain quality care it is essential that effective communication occurs among all health team members. A documentation system that reflects interdisciplinary plans of care for a patient provides continuity of care and prevents fragmented and possibly dangerous care. Thus the medical record helps to ensure that all health team members are working toward a common goal of providing safe and effective care.
Patients' records and reports are two means for effective communication. A patient's record or chart is a confidential, permanent legal documentation of information relevant to that patient's health care. Information about the patient's health care is recorded after each patient contact. The record is a continuing account of the patient's health care status and is available to all members of the health care team. Records are either paper or digital, depending on the system used by the health care agency. Whichever format is used, each patient record includes the following:
• Patient identification and demographic data
• Informed consent for treatment or procedures
• Nursing diagnoses or problems and nursing or interdisciplinary care plan
• Record of nursing care treatment and evaluation
• Medical history and physical examination
• Medical and other health discipline progress notes
• Results of diagnostic and therapeutic tests and procedures
• Summary of operative procedures
• Discharge diagnosis, plan and summary (TJC, 2012)
Reports are oral, written, or audiotaped exchanges of information between members of the health care team. Common reports given by nurses include change-of-shift reports, telephone reports, transfer reports, incident reports, and hand-off reports. Sometimes a physician or health care provider calls a nursing unit to receive a verbal report on a patient's condition and progress. The laboratory submits a written report providing the results of diagnostic tests. A transfer report informs the staff of a receiving health care setting about the type of care a patient will require.
Purpose of Records
A patient's record is a valuable source of data for all members of the health care team and the only permanent record documenting patient care from admission to discharge. Documentation serves multiple purposes, including communication, legal documentation, reimbursement, education, research, and quality process and performance improvement (ANA, 2010).
Communication
The record is a way for health care team members to provide continuity of care and communicate patient needs and progress toward meeting desired patient outcomes. TJC reports that poor communication, including verbal and written, among staff and with patients was one of the top ten reasons for sentinel events for 2011 (Sentinel events, 2012). The record includes the patient's assessment and responses to interventions and changes made in the plan of care. It is the most current and accurate source of information about a patient's health care status. The information communicated in a record prepares you to know a patient thoroughly so you make timely and appropriate care decisions. Base your communication on your assessment findings. It is best to document immediately following an assessment or intervention (ANA, 2010; Austin, 2011; Pirie, 2011).
Legal Documentation
Because jurors usually rely on information documented in the medical record to determine the patient care provided, effective documentation is one of the best defenses for legal claims associated with health care (Table 10-1). Record keeping is your professional responsibility; it is not an optional extra in your practice. To limit nursing liability your documentation must follow organizational standards for documentation, which include a clear indication of the individualized and goal-directed nursing care you provide. The best way to ensure that documentation meets legal standards is to record information timely, accurately, completely, legibly, and using standardized terminology as you provide care (ANA, 2010; Austin, 2011).
TABLE 10-1
LEGAL GUIDELINES FOR RECORDING
| GUIDELINES | RATIONALE | CORRECT ACTION |
| Do not erase, apply correction fluid, or scratch out errors made while recording. | Charting becomes illegible: it appears as if you were attempting to hide information or deface record. | Draw single line through error, write word error above it and sign your name or initials and title. Then record note correctly. Check agency policy (Austin, 2011; Pirie, 2011). |
| Do not write retaliatory or critical comments about patient or care by other health care professionals. | Statements can be used as evidence for nonprofessional behavior or poor quality of care. | Enter only objective descriptions of patient's behavior; patient comments should be quoted (Austin, 2011; Wood, 2010). |
| You need to add patient information. | New information is acquired. | If additional information is to be added to an existing entry, write the date and time of the new entry on the next available space and include and follow facility format (Austin, 2011). |
| You forgot to chart during a shift. | Write the current date and time in the next available space and rationale for delay; label entry late entry and follow the format established by your facility (Austin, 2011). Check facility guidelines for late entries into an EMR. Facilities may limit the time period the entry can be made (Austin, 2011; Wood, 2010). | |
| Correct all errors promptly. | Errors in recording can lead to errors in treatment. | Avoid rushing to complete charting; be sure that information is accurate (Austin, 2011). |
| Record all facts. | Record must be accurate and reliable. | Be certain that entry is factual; do not speculate or guess (Pirie, 2011). |
| Do not leave blank spaces in nurses' notes. | Another person can add incorrect information in space. | Chart consecutively, line by line; if space is left, draw line horizontally through it and sign your name at end (Austin, 2011). |
| Record all entries legibly and in black ink. | Illegible entries can be misinterpreted, causing errors and lawsuits; ink cannot be erased; black ink is more legible when records are photocopied or transferred to microfilm. | Never erase entries or use correction fluid and never use pencil or pens with erasable ink. |
| If order is questioned, record that clarification was sought. | If you perform an order known to be incorrect, you are just as liable for prosecution as the physician or health care provider is. | Do not record “physician made error.” Instead chart that “Dr. Smith was called to clarify order for analgesic” (Nettina, 2010). |
| Chart only for yourself. | You are accountable for information you enter into chart. | Never chart for someone else. Exception: If caregiver has left unit for day and calls with information that needs to be documented, include name of source of information in entry and include that information was provided via telephone. |
| Avoid using generalized, empty phrases such as “status unchanged” or “had good day.” | Specific information about patient's condition or case can be deleted accidentally if information is too generalized. | Use complete, concise descriptions of care. |
| Begin each entry with date and time and end with your signature and title. | This guideline ensures that correct sequence of events is recorded; signature documents who is accountable for care delivered. | Do not wait until end of shift to record important changes that occurred several hours earlier; be sure to sign each entry (Wood, 2010). |
| For computer documentation keep your password to yourself. | Maintains security and confidentiality. | Once logged onto computer, do not leave computer screen unattended and log out when you are finished charting (Wood, 2010). |
Reimbursement
Charting also determines the amount of reimbursement that a health care agency receives (Austin, 2011). Diagnosis-related groups (DRGs) are the basis for establishing reimbursement for patient care. A DRG is a classification based on patients' medical diagnoses. Under the prospective payment system, Medicare reimburses hospitals a set dollar amount for each DRG (see Chapter 3). Your nursing documentation verifies specific nursing care provided and thus supports the reimbursement that your health care agency receives.
A medical record verifies financial charges for equipment and services used in patient's care. Private insurance carriers and auditors from federal agencies review records to determine the reimbursement that a patient or a health care agency receives. Insurance companies do not reimburse for unskilled nursing care. They pay only for skilled medical and nursing care. Timely and accurate documentation of supplies and equipment used assists in accurate and timely reimbursement (ANA, 2010).
Education
A patient's record contains a variety of information (e.g., medical and nursing diagnoses, signs and symptoms of disease, successful and unsuccessful therapies, diagnostic findings, and patient behaviors). Reading the patient care record is an effective way to learn the nature of an illness and the patient's response to it. Review of patients with similar medical problems allows you to identify patterns and trends. Such information builds your clinical knowledge. As you identify patterns associated with specific diseases and conditions, you are able to anticipate the type of care your patients require and how patients respond to treatment.
Research
Statistical data are important elements of patient records, including the frequency of clinical disorders, complications, use of specific medical and nursing therapies, recoveries from illness, and mortality. After obtaining appropriate agency approvals, a nurse researcher reviews patients' records in a research study to collect information on a particular health problem. Analysis of the data collected contributes to evidence-based nursing practice and quality health care (ANA, 2010). For example, if a nurse researcher suspects that early ambulation decreases the complication rate in postoperative patients, the researcher reviews the records of select surgical patients to compare the rates of postoperative complications with early-versus-late ambulation.
Quality Process and Performance Improvement
TJC (2012) requires hospitals to establish quality improvement programs to conduct objective, ongoing reviews of patient care and asks institutions to establish standards for quality care. Audits help to determine whether standards of care are met. Audits assess the standard of records and identify areas for improvement and staff development. For example, nurses may monitor records to determine their success in documenting institution of fall precautions or evaluation of pain measures. The nurses then share any deficiencies identified during monitoring with all members of the nursing staff so corrections in policy or practice can be made. Auditing and monitoring programs keep you informed of the extent to which you meet standards of nursing practice and outcomes that patients experience (ANA, 2010) (see Chapter 3). Quality processes and performance improvement measures provide a method to evaluate quality of care to ensure the achievement of legislative mandates or address quality initiatives (ANA, 2010).
Guidelines for Quality Documentation and Reporting
High-quality documentation and reporting are necessary to enhance efficient, safe, individualized patient care. Quality documentation and reporting have five important characteristics: factual, accurate, complete, current, and organized (ANA, 2010). Problems arise when a record is reviewed in a malpractice suit and there are time gaps, information is squeezed between lines or crossed out, or key facts are omitted (Austin, 2011; Glasper, 2011; Johnson and Nicholls, 2011).
In some settings agency policy requires a registered nurse to cosign documentation completed by licensed practical or vocational nurses, nursing students, or assistive personnel. A cosignature indicates that the supervising nurse reviewed the record entry and was aware of the care and patient status even though others delivered the care. Nurses must assess the patient themselves and read medical record entries before cosigning another health care provider's assessment record.
Factual
A factual record contains descriptive, objective information about what you see, hear, feel, and smell. Objective data are data that are measurable and observable such as the size of a wound or a patient's pulse oximetry reading. To be factual, avoid words such as appears, seems, or apparently because they are vague and lead to conclusions that you cannot support by objective information.
The only subjective data included in a record are what the patient says. Write subjective information with quotation marks, using the patient's own words. For example, the patient's statement, “My lower back hurts” is subjective and acceptable documentation. Another example is stated as follows: Reports feeling a pressure in chest. It is acceptable not to use quotation marks when you paraphrase the patient's words. When documenting subjective information, it is also important to include complementary objective findings so your database is as descriptive as possible (Austin, 2011).
Accurate
The use of precise measurements makes documentation more accurate. For example, documenting “Voided 450 mL clear urine” is more accurate than “Voided an adequate amount.” To avoid misunderstandings and promote patient safety, write out any confusing abbreviations. The National Patient Safety Goals (NPSGs) require that health care institutions standardize abbreviations, acronyms, symbols, and dose designations throughout their system (TJC, 2012). The NPSGs also require institutions to identify a “do not use” list of abbreviations, acronyms, symbols, and dose designations (TJC, 2012) (see Chapter 17). It is important to know the acceptable and unacceptable abbreviation list of an institution to keep your documentation accurate and compliant with requirements.
Correct spelling demonstrates a level of competency and attention to detail. Misspelled words lead to confusion. For example, often words sound the same but have different meanings such as accept and except or dysphagia and dysphasia. Misspellings and incorrect use of terms alters the intended meaning.
TJC (2012) requires that all entries in medical records be dated and that there is a method to identify all authors' entries. Therefore any descriptive entry in a patient's record ends with the caregiver's identifiers (e.g., full name and status). Occasionally you include observations reported to another caregiver or interventions performed by someone else (e.g., “Patient suctioned by Judith Hill, RN.”) As a nursing student you need to enter your full name and student nurse abbreviation (e.g., “Marianne Smith, SN [student nurse]).” The abbreviation for student nurse often differs regionally, being either NS, which stands for nursing student, or SN, which stands for student nurse. Check with your educational institution for the preferred abbreviation. Your signature holds you accountable for information you record. Include your educational institution when required by agency policy.
Complete
The information within a recorded entry or a report needs to be clear, concise, and complete, containing appropriate and essential information. Criteria for thorough communication exist for certain health problems or nursing activities (Table 10-2). Make written entries in the patient's medical record describing nursing care that you administer and the patient's response. For example:
TABLE 10-2
EXAMPLES OF CRITERIA FOR DOCUMENTATION AND REPORTING
| TOPIC | CRITERIA TO DOCUMENT OR REPORT |
| Assessment | |
| Subjective data (patient behavior [e.g., anxiety, confusion, hostility]) | |
| Objective data (e.g., rash, tenderness, breath sounds) | |
| Nursing Interventions and Evaluation | |
| Treatments (e.g., enema, bath, dressing change) | |
| Medication administration | |
| Patient teaching | |
| Discharge planning | |

0845 Reports continuous throbbing pain on lateral aspect of left fractured femur increased with movement of the leg with a severity of 8 (scale 0-10). B/P: 132/74, T 37° C, P 92, R 18. Morphine sulfate 5 mg IV given for pain. Sue Jacobs, RN.
0915 Reports pain at 2 (scale 0-10) and able to turn in bed independently. States, “I feel much better now.” Sue Jacobs, RN.
Include routine activities such as daily hygiene measures, vital signs, and pain assessment in flow sheets or graphic records according to agency policy. Describe these activities in detail when it is relevant because of a change in functional ability or status. For example, you have a patient who has previously required a total bath; and now the patient has improved and is able to wash his or her face, hands, and upper body. This change in patient activity warrants additional documentation.
Current
Making entries promptly is essential in effective documentation (TJC, 2012). Delays in documentation result in serious omissions, untimely delays, and possible errors in patient care. To increase timely documentation and decrease unnecessary duplication, many health care agencies keep records or computers near the patient's bedside to facilitate immediate documentation of care. You need to communicate the following nursing care at the time of occurrence:
3. Administration of medications and treatments
4. Patient response to intervention
5. Preparation for diagnostic tests or surgery
6. Change in patient status and who was notified (e.g., physician, patient's family)
Most agencies use military time, a 24-hour time cycle. The military clock begins at 1 minute after midnight as 0001 and ends with midnight at 2400. For example, 10:22 am is 1022 military time; 1:00 pm is 1300 military time. Figure 10-1 shows military time on a clock face. Use of military time helps to minimize errors in interpretation of am and pm times.
Organized
Written communication is easier to understand when written in a logical, sequential order. For example, an organized note describes your assessment, interventions, and the patient's response in a sequence. It is also more effective when notes are concise, clear, and to the point. To make clear and organized entries it is often helpful to make a list of what you need to include before beginning to write in the permanent legal record. Organizing your information into categories minimizes frustration in trying to recall patient care activities provided. Suggested categories include what the patient tells you directly or from indirect sources if the patient is incapacitated; what you assess; what you do, including interventions performed in response to assessment findings; and what you teach the patient and family. Applying critical thinking skills along with the nursing process gives logic and order to nursing documentation.
Methods of Documentation
The documentation system selected by a nursing service reflects the philosophy of the department. Staff use the same documentation system throughout an agency. There are several acceptable methods for recording health care information (Table 10-3).
TABLE 10-3
| Case study continuation: Jane needs to record the information obtained from Mrs. Smith during the admission process. The following shows examples of various formats. | |
| Narrative note | Stated: “I'm dreading surgery. Last time it hurt so much when I got out of bed.” Discussed alternatives for pain control and importance of postoperative activity. Encouraged to ask for pain medication before pain is severe. Stated: “I feel better prepared now.” Able to verbalize that activity enhances circulation and healing. |
| SOAP | S (subjective data): “I'm dreading surgery. Last time it hurt so much when I got out of bed.” O (objective data): Noted muscle tension and loud voice. A (assessment/analysis): Fear of postoperative pain. P (plan): Assess pain level every 2 hours. Provide comfort measures and give analgesics as needed. |
| PIE charting | P (problem): “I'm dreading surgery. Last time it hurt so much when I got out of bed.” I (intervention): Discussed alternatives for pain control and importance of postoperative activity. Encouraged to ask for pain medication before pain is severe. E (evaluation): “I feel better prepared now.” Able to verbalize that activity enhances circulation and healing. |
| Focus charting | D (data): “I'm dreading surgery. Last time it hurt so much when I got out of bed.” A (action): Discussed alternatives for pain control and importance of postoperative activity. Encouraged to ask for pain medication before pain is severe. R (response): “I feel better prepared now.” Able to verbalize that activity enhances circulation and healing. Note: Some agencies add P (plan). Example: P (plan): Assess pain level every 2 hours. Provide comfort measures and give analgesics as needed. |

Paper and Electronic Documentation
Traditionally health care professionals documented on paper medical records. Paper records are episode oriented, with a separate record for each patient visit to a health care agency (Hebda and Czar, 2013). Key information such as patient allergies, current medications, and complications from treatment may be lost from one episode of care (e.g., hospitalization or clinic visit) to the next, jeopardizing a patient's safety. The need for patient safety has driven the increased usage of computerized documentation systems. The traditional paper medical record no longer meets the needs of today's health care industry. Thus hospitals and health care professionals are transitioning to use of EHRs.
The electronic health record (EHR) is a longitudinal electronic record of patient health information generated by one or more encounters in any care delivery setting (Healthcare Information and Management Systems Society [HIMSS], n.d.). It ensures coordination of care because all primary caregivers can view a common record of a patient's entire health care experience, including inpatient, outpatient, emergency care, and diagnostic studies. It integrates all pertinent patient information into one record, regardless of the number of times a patient enters a health care system. The EHR differs from the electronic medical record (EMR), although terms are used interchangeably. The EMR contains patient data gathered in a health care setting at a specific time and place and is part of the EHR. The EHR provides a more comprehensive picture of the clinical process (Brown et al., 2013).
In 2010 the Patient Protection and Affordable Care Act (ACA) mandated that health care agencies purchase a computerized information system and demonstrate “meaningful use.” Reimbursement is provided to health care professionals and hospitals that meet meaningful use benchmarks (Brown, et al., 2013). Meaningful use refers to the level with which information technology (IT) is available and used to support clinical decision making to improve quality, safety, and efficiency; reduce health disparities; engage patients and families in their health care; improve care coordination; improve population and public health; and maintain privacy and security. These benchmarks require health care providers to report certain data related to performance improvement and patient outcomes. Professional organizations and agencies also support the initiation of the EHR.
Guidelines are developed to assist you in safe computer charting.
1. Do not share your password with other caregivers. A good system requires frequent changes in personal passwords to prevent unauthorized persons from accessing and tampering with records.
2. Avoid leaving the computer terminal unattended when logged on.
3. Follow the correct protocol for correcting errors according to agency policy.
4. Software systems have a system for backup files. If you inadvertently delete part of the permanent record, follow agency policy. It is necessary to type an explanation into the computer file with the date, time, and your initials and to submit an explanation in writing to your manager (Sewell and Thede, 2013).
5. Avoid leaving information about a patient displayed on a monitor where others can see it. Keep a log that accounts for every copy of a computerized file that you have generated from the system.
6. Follow agency confidentiality procedures for documenting sensitive material such as a diagnoses, insurance coverage, or family status.
7. Protect printouts of computerized records. Shredding printouts and logging the number of copies generated by each caregiver are ways to minimize duplicate records and protect the confidentiality of patient information (Sewell and Thede, 2013).
Problem-Oriented Medical Records
The problem-oriented medical record (POMR) is a structured method of documentation that emphasizes the patient's problems. The method is organized in a way to correspond to the nursing process and facilitates communication of patient needs. Organization of data is by problem or diagnosis. Ideally each member of the health care team contributes to a single list of identified patient problems. The POMR has the following major sections: database, problem list, initial care plan, discharge summary, and progress notes.
Problem List.
The problem list is developed after a review of the patient data. You identify priority problems and list all problems in chronological order to serve as an organizing guide for the patient's care. Add new problems to the list as you identify them on the basis of your ongoing nursing assessment. Once problems are resolved, record the date and draw a line through the problem and its number.
Care Plan.
TJC standards (2012) require that a care plan, also called a plan of care, be developed for all patients on admission to acute, subacute, rehabilitation, or extended care agencies. Disciplines involved in the patient's care develop a care plan, sometimes referred to as an interdisciplinary care plan, for each problem listed. For example, a physical therapist communicates a plan for increasing a patient's ambulation, whereas a speech therapist communicates a plan to improve the patient's swallowing. Nurses document a plan of care in a variety of formats. Generally these plans of care include nursing diagnoses, expected outcomes, and interventions (see Chapter 9).
Progress Notes.
Health care team members use progress notes to monitor and record the progress of a patient's problems. Narrative notes, flow sheets, discharge summaries, and structured notes are formats you use to document the patient's progress.
Narrative Documentation.
Narrative documentation is the traditional method for recording nursing care. However, in many settings other methods have replaced narrative charting. Narrative charting uses a storylike format to document information specific to patient conditions and nursing care. It is beneficial in emergency situations in which a chronological order of events is important. However, it does have some disadvantages, including the tendency to be repetitious and time consuming, and it requires the reader to sort through much information to locate the desired patient information (see Table 10-3).
SOAP Documentation.
One format for entering a progress note is the SOAP note. SOAP is an acronym for the following:
S: Subjective data (verbalizations of the patient)
O: Objective data (data that are measured and observed)
A: Assessment (diagnosis based on the subjective and objective data)
An I and E are sometimes added (i.e., SOAPIE) in various institutions. The I stands for intervention, and the E represents evaluation. The logic for SOAP(IE) notes is similar to that of the nursing process: Collect data about each of your patient's problems, draw conclusions, and develop a plan of care. Number each SOAP note and title it according to the problem on the list (see Table 10-3).
PIE Documentation.
The PIE note documentation format is similar to SOAP charting in its problem-oriented nature. However, it differs from the SOAP method in that PIE charting has a nursing origin, whereas SOAP originated from the medical model. PIE is an acronym for problem, interventions, evaluation as follows (see Table 10-3):
The PIE format simplifies documentation by unifying the care plan and progress notes into a complete record. It also differs from SOAP because the narrative note does not include assessment information. Your daily assessment data appear on special flow sheets, thus preventing duplication of information. You number or label the PIE notes according to the patient's problems. Once a patient's problem becomes resolved, you drop it from daily documentation. Continuing problems are documented daily.
Focus Charting.
A third format is focus charting. It is a unique narrative format in that it places less emphasis on patient problems and instead focuses on patient concerns such as a sign or symptom, a condition, a behavior, or a significant event (Carpentino-Moyet, 2009). Each entry includes data (D), actions (A), and patient response (R). Focus charting combines a shorthand approach to documenting normal assessments and routine care with a concise longhand method for documenting exceptions to predetermined norms. In addition, focus charting saves time because it is easy for multiple caregivers to understand, it is adaptable to most health care settings, and it enables all caregivers to track the patient's condition and progress toward the outcomes of care. A disadvantage of focus charting is that it can be challenging to write accurate logical notes (see Table 10-3).
Charting by Exception
Charting by exception (CBE) is an innovative approach to reduce the time required to complete documentation. In a CBE system an agency defines criteria for nursing assessments and standards of practice for nursing interventions. CBE involves completing a flow sheet that incorporates these standard assessment criteria and interventions. You use a check mark on the flow sheet to indicate normal findings or routine interventions. You write narrative information only if findings are abnormal. You create problems if you chart normal findings along with the exceptions. By following the agency standards for charting in the CBE system, when you see any entries in the chart, you know that something out of the ordinary has occurred. This makes it easier to track unexpected changes in a patient's condition as they develop.
Case Management Plan and Critical Pathways
The case management plan of delivering care uses an interdisciplinary approach to document patient care and focuses on providing quality care in a cost-effective manner. The case management plan incorporates critical pathways, which standardize practice and improve interdisciplinary coordination (Cesta, 2012; Sewell and Thede, 2013). The concept refers to specific guidelines for care that describe patient treatment goals and outline the sequence and timing of interventions for meeting the goals efficiently. They are usually organized according to categories such as activity, diet, treatments, protocols, and discharge planning. Critical pathways are also referred to as clinical pathways, integrated care pathways, care maps, or care paths.
Advantages of case management plans include the ability for various health care team members to note variances in care, establish outcomes, identify potential problems, specify standards from the patient perspective, and know what to expect. Disadvantages focus on the need for acceptance of the recording form by all health care providers and individuals knowledgeable in the process to develop pathways.
Common Record-Keeping Forms
The patient chart includes a variety of forms to make documentation easy, quick, and comprehensive. When possible avoid duplication within the record.
Admission Nursing History Forms
Admission nursing history forms provide baseline data for later comparisons with changes in the patient's condition. The admitting nurse uses the form to document a thorough assessment (e.g., biographical data, physical and psychosocial/cultural assessment, and review of health risk factors) and identify relevant nursing diagnoses or problems for the patient's care plan. Each institution designs nursing history forms based on its standards of practice and philosophy of nursing care.
Flow Sheets and Graphic Records
Flow sheets and graphic records are part of the permanent health record and allow documentation of certain routine observations or specific measurements made repeatedly such as height and weight and activities of daily living such as the bath, vital signs, pain assessment, and intake and output. These provide a quick and easy reference for assessing changes in a patient's status. Critical care units commonly use flow sheets for many types of data. They are an effective way to record information so you are able to observe trends over time.
When documenting a significant change on a flow sheet, describe the change in the progress notes and nursing measures implemented in response to the change. For example, if a patient's blood pressure becomes dangerously high, record in the progress note the blood pressure; related assessments such as flushing and headache; and the medication administered to lower the pressure. Also include evaluation of the interventions (e.g., serial blood pressure and other pertinent evaluation measures).
Patient Care Summary or Kardex
Many hospitals now have computerized systems that provide certain basic information in the form of a patient care summary. Data automatically update as orders enter the system and as nurses make decisions. In some settings a Kardex (flip-over card file) kept at the nurses' station provides information for the daily care of a patient. It often has two parts: an activity and treatment section and a nursing care plan section. The updated information in the Kardex eliminates the need for you to refer repeatedly to the medical record. Information commonly found in the Kardex or patient care summary includes the following:
1. Basic demographic data (name, age, sex, date of birth)
2. Primary medical diagnosis and significant medical history
3. Current health care provider's orders (e.g., diet, activity, vital signs, blood tests, diagnostic tests), name of primary care and consulting providers
4. A nursing care plan or plan of care
5. Nursing orders or nursing interventions (e.g., intake and output, positioning, comfort measures, fall prevention, teaching)
6. Scheduled tests and procedures
7. Safety precautions used in the patient's care
8. Factors related to activities of daily living
9. Nearest relative/guardian or person to contact in an emergency
10. Emergency code status (e.g., “do not resuscitate” order)
Standardized Care Plans
Some institutions use standardized care plans to make documentation more efficient. The plans, based on institution standards of nursing practice, are preprinted established guidelines of care for patients with similar health problems. After completing a nursing assessment, place the appropriate standard care plans in your patient's record. It is very important that you make necessary modifications to individualize each care plan. Most standardized plans also allow the addition of specific desired outcomes and the target dates of achievement of these outcomes (see Chapter 9).
Discharge Summary Forms
Much emphasis is placed on preparing a patient for a timely discharge from a health care institution. Ideally you begin discharge planning on admission and in some cases even before admission, as is necessary with same-day surgery admissions and childbirth. When doing discharge planning, be responsive to changes in the patient's condition and involve the patient and family in the discharge planning process (see Chapter 3).
The primary goal of a discharge summary is to ensure the continuity of care, whether a patient is going home or transferring to another institution. A nursing discharge note needs to cover the reason for hospitalization; procedures performed; care, treatment, and services provided; patient's status at discharge; information provided to the patient and family; and provisions for follow-up care (TJC, 2012). Discharge summary forms make the summary concise and instructive. Many forms include copies that you give to the patient, family members, or home care nurses. Discharge summaries involve multiple disciplines and help to ensure that your patient leaves the hospital in a timely manner with the appropriate health care resources (Box 10-1).
Acuity Recording
An acuity recording system determines the hours of care for a nursing unit and the number of staff required to care for a given group of patients. Once a day staff nurses enter the acuity scores of each of their patients into a computerized documentation system. Managerial and administrative staff gather the acuity data electronically to make staffing decisions. For example, an acuity system rates a patient's activity from 1 to 5 (1 requires the least amount of time, 5 requires the most amount of time). A patient returning from surgery who requires frequent assessments and interventions rates as an acuity level 4. On the same continuum, another patient awaiting discharge after an uneventful recovery from surgery rates as an acuity level 1.
Home Care Documentation
Home care continues to grow as increasing numbers of older adults use home care services. Home health care services are reimbursed by Medicare, Medicaid, commercial insurance, and other managed care plans (ANA, 2008a; Nettina, 2010). Each payer has specific guidelines for establishing eligibility for home care reimbursement. When you provide home care, your documentation must specifically address the category of care and your patient's response to care. Home care agencies are evaluated for accurate, complete charting; adherence to standards that govern their reimbursement; and quality of care. Document all of your services for payment (e.g., direct skilled care, patient instructions, skilled observation, and evaluation visits) (TJC, 2012). Home care documentation includes the following: resource numbers in case of emergency; the ability of the patient or caregiver to perform needed home care procedures and troubleshoot equipment needs; and ability to recognize potential complications. Documentation also needs to show evidence that the home environment is safe for the treatment being received (ANA, 2008a).
Long-Term Care Documentation
The number of Americans needing long-term care (LTC) is expected to double by 2050 (Unwin et al., 2010). Documentation challenges in LTC are much different from those in the acute care setting. CMS established guidelines related to accidents and supervision of residents of long-term care facilities. Changes in the Medicare program in the form of the prospective payment system determine the standards and policies for reimbursement and documentation in long-term health care. Assess each resident in a long-term care agency receiving funding from Medicare and Medicaid programs using the Resident Assessment Instrument/Minimum Data Set (USDHHS, 2011). These tools provide standardized protocols for assessment and care planning and a minimum data set to promote quality improvement within and across facilities. When you review residents' records for reimbursement, there is an expectation that protocols such as skin assessments, wound care, and assisted ambulation are carried out. Quality documentation describes the services rendered and the patient's response to treatments, justifies the therapy services provided, and ensures that services are reimbursed by Medicare. The fiscal support for long-term care residents hinges on the justification of nursing care as demonstrated in sound documentation of the services rendered.
Reporting
Reports are an exchange of information among health care team members. A report reflects a summary of activities or observations seen, performed, or heard by the health care provider. The types of reports most commonly used by nurses include the hand-off report; telephone report; and incident report; sometimes referred to as occurrence or event report.
Hand-Off Report
A hand-off report occurs any time one health care provider transfers care of a patient to another health care provider. The purpose of hand-off reports is to provide better continuity and individualized care for patients. A hand-off is the process of transferring responsibility for patient care from one provider to another. For example, if you find that a patient breathes better in a certain position, you relay that information to the next nurse caring for the patient. Examples of hand-off reports include change-of-shift reports and transfer reports (Staggers et al., 2011) (Figure 10-2).
Standardizing communication during hand-off reports helps ensure patient safety. Hand-off communication includes up-to-date information about a patient's condition, required care, treatments, medications, services, and any recent or anticipated changes (TJC, 2012). The average time spent by nurses in giving a hand-off report is 40 minutes (Staggers et al., 2011).
Regardless of the way hand-off reports are given, it is essential for staff to have an opportunity for last-minute updates, to clarify information, or to receive information on care events or changes in a patient's condition. Properly performed, a hand-off report provides an opportunity to share essential information to provide for patient safety and continuity of care.
An effective hand-off report is quick and efficient. Nurses give hand-off reports using paper, a voice recording, or an electronic method. Electronic hand-off reports are beneficial to improving patient safety and continuity of care (Govier and Medcalf, 2012). Nurses prefer the paper hand-off report over electronic reports (Staggers et al., 2011). Whichever format is used, a good report provides a baseline for comparisons and indicates the kind of care anticipated for the next nurse who will be caring for the patient. An organized and concise approach helps you set goals and anticipate patient needs and lessens the chance of overlooking important information. A sample format is as follows: background information (name, age, and medical diagnosis); primary health problem; unusual occurrences; discharge planning issues; identification of significant changes in measurable terms (e.g., pain scale); observations; findings; time when new, STAT, or prn medications were given; care required such as medications that need to be started, when to assess the effectiveness of STAT/prn medications, or when a dressing needs to be changed next; progress with teaching interventions; and family involvement. It is especially important to report any recent changes or priority situations concerning the patient's condition. Do not include normal findings or routine information retrievable from other sources or derogatory or inappropriate comments about a patient or family.
Change-of-Shift Report.
The change-of-shift report is one type of hand-off report that occurs at the end of each shift. This report provides the transfer of relevant information from nurses who have completed a shift of care to nurses about to begin a shift of care. Shift reports happen in a variety of ways.
Sometimes nurses walk with each other from one patient's room to the next. This is called walking rounds. Walking reports given in person or during rounds allow you to obtain immediate feedback when questions arise about a patient's care. When you make rounds, the patient and family members also have the opportunity to participate in any discussions and care decisions. However, be careful about mentioning information that the patient should not hear (e.g., new laboratory or diagnostic reports not yet explained by the health care provider).
Nurses also give reports orally. Oral reports occur in person, with staff members from both shifts participating. They can also be audiotaped before the end of the shift by the nurse going off duty; the incoming staff listens to the report before assuming patient care. Recording reports often enhances efficiency and minimizes social interactions.
Transfer Reports.
Patients frequently transfer from one unit to another or to another facility to receive different levels of care. For example, they transfer from intensive care units to general nursing units when the level of care no longer requires intense monitoring. A transfer report is another type of hand-off report that involves communication of information about patients from the nurse on the sending unit to the nurse on the receiving unit. Nurses usually give transfer reports by phone or in person. When giving a transfer report, include the following information:
1. Patient's name, age, date of birth, health care provider(s), and medical diagnosis
2. Summary of medical progress up to the time of transfer
3. Current health status (physical and psychosocial)
7. Current nursing diagnoses or problems and care plan
8. Any critical assessments or interventions to be completed shortly after transfer (helps receiving nurse establish priorities of care)
9. Up-to-date reconciled medication list (TJC, 2012)
10. Need for any special equipment such as isolation equipment, suction equipment, or traction
At the completion of the transfer report, the receiving nurse clarifies information by asking questions about the patient's status. Some institutions require a written transfer report sheet that includes information communicated in the transfer report.
Telephone Reports and Orders
Telephone Reports.
A registered nurse makes a telephone report when significant events or changes in a patient's condition have occurred. A telephone report needs to include clear, accurate, and concise information. TJC reported that in 2011 communication such as verbal and written among staff and with patients was listed as one of the ten most frequently identified root causes of medical errors, also called sentinel events (Sentinel events, 2012). To help improve communication some institutions use SBAR, an acronym that stands for situation-background-assessment-recommendation. SBAR standardizes telephone communication of significant events or changes in the patient's condition. It is a communication strategy designed to improve patient safety. For example, when describing the situation, you include the admitting and secondary diagnoses and the problem your patient is having as the current issue. Background information includes pertinent medical history, previous laboratory tests and treatments, psychosocial issues, allergies, and current code status. For assessment data include significant findings in your head-to-toe physical assessment, recent vital signs, current treatment measures, restrictions, recent laboratory results and diagnostics, and pain status. Then provide your recommendation, in which you suggest a plan of care and request orders and other needs to be addressed (Compton et al., 2012).
Document every phone call you make to a health care provider. Your documentation includes when the call was made, who made it (if you did not make the call), who was called, to whom information was given, what information was given, what information was received, and verification of the information with the provider. Health care institutions have a process for a verification “read-back” when receiving information or critical test results. An example follows: “Laboratory technician J. Ignacio reported a potassium level of 5.9. Information was transcribed and read back for verification. Dr. Wade notified at 2030. D. Markle, RN, read back.”
Telephone Orders and Verbal Orders.
A telephone order (TO) involves a health care provider stating a prescribed therapy over the phone to a registered nurse, whereas a verbal order (VO) involves a health care provider giving orders to a nurse while they are standing near each other. TOs and VOs frequently occur at night or during an emergency and frequently cause medical errors. The nurse receiving a VO or TO writes down the complete order or enters it into the computer as it is being given. Then the nurse reads it back, called read-back, and receives confirmation from the person who gave the order (TJC, 2012). An example follows: “4/16/2014: 0815, Tylenol 3, 2 tablets, every 6 hours for incisional pain. TO Dr. Knight/J. Woods, RN, read back.” The health care provider later verifies the TO or VO legally by signing it within a set time (e.g., 24 hours) as set by hospital policy. Use TOs and VOs only when absolutely necessary and not for the sake of convenience. In some situations a second person listens to TOs (verify agency policy). Box 10-2 provides guidelines that promote accuracy when receiving TOs.
Incident, Event, or Occurrence Reports
An incident is any event not consistent with the routine operation of a health care unit or routine care of a patient. Examples include patient falls, needlestick injuries, a visitor becoming ill, and medication errors. Completion of an incident report, also called either an occurrence or event report, occurs when there is an actual or potential injury; this report is not a part of the patient record (see Chapter 5).
Always contact the patient's health care provider when an incident happens. Note that you do not mention that an error occurred in the patient's medical record. Instead you document in the patient's medical record an objective description of what happened, what you observed, and which follow-up actions were taken. It is also important to evaluate and document the patient's response to the error or incident (Austin, 2011).
Follow agency policy when making an incident report. Incident reports are an important part of quality improvement. The overall goal is to identify changes needed to prevent future recurrence. File the report with the appropriate risk management department of the institution. Analysis of incident (or occurrence) reports helps identify trends within an organization to provide justification for changes in policies and procedures or for in-service programs. (See Chapter 5 for other examples and further discussion.)
Health Informatics
Health informatics is the application of computer and information science in all basic and applied biomedical sciences to facilitate the acquisition, processing, interpretation, optimal use, and communication of health-related data. The focus is the patient and the process of care, and the goal is to enhance the quality and efficiency of care provided (Hebda and Czar, 2013).
There is an increasing trend toward computerization of health care records in acute care, outpatient, home care, and long-term care settings (Box 10-3). Surveys show that approximately 27% of acute care hospitals and 12% of ambulatory care settings have adopted some form of EHRs (Moore and Fisher, 2012). Computerization of health care records provides a mechanism for identification, acquisition, manipulation, storage, and presentation of data so they can be transformed into information. The federal directive promoting the adoption of EMRs by 2014 mandates that nurses of the twenty-first century have broadened skill sets to deliver quality patient care (McBride et al., 2012; Walker, 2010). Today's nurses need to be knowledgeable in the science and application of nursing informatics.
Informatics is the science and art of turning data into information. It focuses on information and knowledge acquisition rather than the computer. All nurses deal with data, information, and knowledge (Hebda and Czar, 2013). Informatics describes the study of the retrieval, storage, presentation, and sharing of data, information, and knowledge to provide quality, safe patient care (Sensmeier, 2011).
Informatics includes four key concepts. Data include numbers, characters, or facts that are collected according to a perceived need for analysis and possible action. Data have no significance beyond their existence. For example, what does the number 180 mean? It could be a laboratory value, a street number, or a secret code. By itself 180 means nothing. It represents data. Information is data that are interpreted, organized, or structured. Information provides the answers to “who, what, when, where” questions. If you take the blood pressure of a 57-year-old postoperative patient and the systolic blood pressure reading is 180 mm Hg and the diastolic blood pressure is 90 mm Hg, you have useful information. When the number 180 is combined with other data, it becomes meaningful. The data become information. The vital signs now have meaning when interpreted. Knowledge is the application of data and information. It answers the “how” question. You know that the patient just had surgery, has a history of high blood pressure, and did not receive the morning dose of antihypertensive medication. Using knowledge is essential in making decisions. You synthesized information (knowledge) from past experiences of caring for other postoperative patients with high blood pressure. Knowledge creates new questions and areas of research. Wisdom answers the “why” question and focuses on the appropriate application of that knowledge (Hebda and Czar, 2013). Wisdom comes with experience. In the above scenario, you report changes to the patient's health care provider. You also apply knowledge of pharmacology and intervene to manage the patient's blood pressure.
It is a challenge in health care settings to easily access data and information about patients. This is especially the case when you record information manually on printed forms. For example, a nurse working in risk management who is interested in investigating patient falls has to review page by page the records of patients who have fallen to identify the common factors contributing to falls. Remember that three important purposes of medical records are communication, education, and research. When health care organizations rely on handwritten patient records, the process of locating, summarizing, and comparing information is slow and difficult. Finding information for medical record purposes of health care education, research, audits, and reimbursement becomes cumbersome and inefficient. The Institute of Medicine (IOM) (2010) recognized that the only way to use data and information to improve care delivery and for quality improvement, research, and education is through IT.
Information technology (IT) refers to the management and processing of information, generally with the assistance of computers (Hebda and Czar, 2013). IT includes not only the use of computers, but also the knowledge of how to use computer technology such as databases, programming languages and tools, and communication protocols. Technology serves as the tool that allows transfer of the information that improves care. However, technology alone does not improve the efficiency and effectiveness of patient care. You are expected to understand the capabilities and limitations of technology. IT supports the process of synthesizing data and information into knowledge and wisdom (ANA, 2008b). IT is critical to all aspects of clinical decision making, consumer education, professional development, research, and the delivery of patient care.
A health care information system (HIS) is a group of systems used within a health care enterprise that support and enhance health care (Hebda and Czar, 2013). The role of HIS has grown more important because the public has a heightened awareness of reports of medical errors through public media and various initiatives implemented nationally such as HIPAA, personal health records, and EHRs. Increasing numbers of health care agencies are expanding the use and integration of EHR into their settings.
An HIS consists of two major types of information systems: administrative information systems and clinical information systems (CISs). The two systems operate together to improve the efficiency of data entry and communication. Administrative information systems include databases such as payroll, financial, and quality assurance systems.
CISs support activities are used to plan, implement, and evaluate patient care. All clinicians, including nurses, physicians, pharmacists, social workers, and therapists, use CISs. CISs include the EHR, monitoring systems and laboratory, radiology, and pharmacy systems. A monitoring system includes devices that automatically monitor and record biometric measurements (e.g., vital signs, oxygen saturation, cardiac index, and stroke volume) in critical care and specialty areas. The devices send measurements electronically and directly to the nursing documentation system.
The CIS also includes order entry systems, one of the most important systems in use today. They automate orders, eliminating written order forms and expediting the delivery of supplies to a nursing unit. The computerized provider order entry (CPOE) is one type of order entry system gaining popularity across the country, particularly with medication orders. Advantages of CPOE include reduced use of resources, quicker turnaround of orders, reduced length of stay, and an overall reduction in costs. More important, most CPOE systems have significant potential to reduce medication errors associated with illegibility and inappropriate drug use and dosing (Tschannen et al., 2011). CPOE refers to a process by which the health care provider directly enters orders for patient care into the hospital information system. In advanced systems, CPOE has built-in reminders and alerts that help the patient's provider select the most appropriate medication or diagnostic test. There are major initiatives from the IOM to improve the quality of care and reduce medication errors. Many believe CPOE is the answer. When a provider puts an order entry into the EHR, the order is sent immediately to the appropriate department. The direct order eliminates issues related to illegible handwriting and transcription errors. A CPOE system potentially speeds the implementation of the ordered diagnostic tests and treatments, which improves staff productivity and saves money (Tschannen et al., 2011).
Typically a health care agency uses one or several CISs and administrative information systems. For example, a small community hospital uses a nursing information system, an order entry system, and laboratory, radiology, and pharmacy systems to coordinate its core patient care services. A nurse documents nursing care on a computer, locates and reviews laboratory test results, orders sterile supplies, and enters health care provider orders for x-ray films and patients' medications. The billing of patient care services and payroll occurs through use of administrative information systems (Hebda and Czar, 2013).
Nursing Information Systems
Nursing information systems (NISs) are one of many subspecialties of CISs. Many hospitals now have NISs that support the documentation of nursing process activities and offer resources for managing nursing care delivery. A reliable NIS is the product of nursing informatics. Nursing informatics is a nursing specialty that manages and communicates data, information, knowledge, and wisdom by integrating nursing, computer, and information science (ANA, 2008b). Nursing informatics facilitates the integration of data, information, and knowledge to support patients, nurses, and other providers in decision making in all roles and settings. It supports new initiatives occurring within the health care arena such as CPOE, electronic medication administration records, and clinical documentation. The application of nursing informatics results in an efficient and effective NIS. Nursing informatics improves the health of individuals, families, communities, and populations by effectively managing information and enhancing communication (ANA, 2008b). Because of rapidly advancing emerging health care technologies, nursing practice of the future will not be the same as it is today. Nurses need knowledge and skills in computer literacy, information literacy, informatics, and the use of information technologies (Skiba, 2010; Sensmeier, 2011).
Numerous organizations, including the National League for Nursing (NLN), the American Nurses Association (ANA), the Technology Informatics Guiding Education Reform (TIGER), and the Robert Wood Johnson Foundation Quality and Safety Education for Nurses Initiative (QSEN), recommend that all nurses acquire a minimal level of awareness and competence in informatics and use of IT. Competence in informatics is not the same as computer competency. To become competent in informatics you need to be able to use evolving methods of discovering, retrieving, and using information in your practice (Hebda and Czar, 2013). This means that you learn to recognize when you need information and have the skills to find, evaluate, and use needed clinical information effectively.
An effective NIS incorporates principles of nursing informatics and supports the work you do. You need to be able to access a computer program easily, review the patient's medical history and orders, and go to the patient's bedside to conduct a comprehensive assessment. Once you have completed the assessment, you enter data into the computer terminal at the patient's bedside and develop a plan of care from the information gathered. The plan of care incorporates evidence-based practice guidelines, which you have found using your information science skills. The computer allows you to quickly share the plan of care with the patient. Periodically you return to the computer to check on laboratory test results and document the therapies you administer. The computer screens and optional pop-up windows make it easy to locate information, enter and compare data, and make changes. The NIS helps you determine diagnosis, prepare and implement nursing care plans, and evaluate care provided.
The transition from paper to online documentation systems presents both opportunities and challenges to nurses. Successful implementation of computer-based nursing process documentation requires a high level of acceptance of the nursing process, careful preparation of predefined care plans, organizational preparation, and inclusion of future users, including bedside nurses, in the development process. It is also essential to have sufficient technical equipment with integration into the hospital information system.
A barrier to the successful implementation of an NIS is the reluctance on the part of some nurses and other clinical staff to accept technological advances. Often clinicians fail to understand how technology can improve the way they deliver care and enhance clinical decision processes. Successful integration requires nurses to understand the potential of informatics and IT.
Clinical decision support systems (CDSSs) are computerized programs used within a health care setting to provide you with clinical knowledge and relevant patient information to help you improve patient care (Hebda and Czar, 2013). A CDSS uses a complex system of rules for analyzing data and presents information to support the decision-making process of the nurse (Figure 10-3). The information within a CDSS is current, is evidence based, and has the ability to be updated. The CDSS links a nurse to the latest evidence-based practice guidelines at the point of care (Dontje and Coenen, 2011). For example, CDSSs are used to improve glycemic control in hospitalized patients who have diabetes mellitus (Harrison et al., 2013). Information provided by a CDSS is given to the right person at the right time. For example, after a medication order is entered, the CDSS provides an alert to the provider if the dosage falls outside of the safe range. This enhances patient safety during the medication ordering process. CDSSs also improve nursing care. When patient assessment data are combined with patient care guidelines, nurses are better able to implement evidence-based nursing care, resulting in improved patient outcomes (Harrison and Lyerla, 2012; Sewell and Thede, 2013).
Privacy, Confidentiality, and Security Mechanisms
There are risks associated with the electronic system. The most common risks center on violations of patient privacy, patient confidentiality, and security. Privacy is the individual's right to limit access to his or her health care information. Confidentiality is the expectation that information shared with the health care provider will be used only for its intended purposes and not redisclosed unless medically necessary. Security protects the EHR from hackers who try to obtain confidential information (McGonigle and Mastrian, 2012). More health care organizations have computers linked together to maximize communication both inside and outside the facilities. These networks allow for efficiency and minimize fragmentation of health care. However, breaches of network security remain a concern (Carrington and Effken, 2011). Organizations have mechanisms in place to minimize security breaches. Such mechanisms include authentication of users, a strong password policy, and acceptable use policies of the network that indicate the type of activities allowed on the network. If you make an error within the electronic documentation system, you must follow agency policy for making corrections. There is always an audit trail with electronic documentation. In some situations, if the EHR is “down” for any reason, nurses maintain a paper record of the care provided. If the EHR system is down, the paper documentation remains a part of the legal record (Harrington et al., 2011). You must remember that charting factual, accurate, complete, and current guidelines also pertains to the electronic document. Just as in a paper documentation system, “if it's not documented” within the electronic record, “it's not done.”
The implementation of HIPAA regulations heightened awareness about information security and privacy practices. HIPAA was the first federal legislation to protect automated patient records and provide uniform protection nationwide (Hebda and Czar, 2013). HIPAA regulations called for the establishment of an electronic patient records system and process to protect the privacy of individual health information. Electronic records facilitate efficient and effective sharing of information, but the ease of access raises concern among consumers. The California HealthCare Foundation (2010) survey found that two thirds of the American public were concerned about the privacy and security of their health information. Computerized documentation has legal risks. Just as you need to understand how violations occur in a paper documentation system, you must also understand how information systems influence privacy, confidentiality, and security.
Privacy includes the right to determine which information shared with a health care worker will become known to others. When using a computerized documenting system, you must make sure that the computer screen is not visible to anyone except the person who is charting (Hebda and Czar, 2013).
Confidentiality of access to computerized records is a major issue with electronic records just as it is with paper records. Protecting privacy through confidentiality policies and technology is a critical component of quality health care. Standards within HIPAA address criteria for standardizing electronic transmission of health information by focusing on the need to protect security, integrity, and authenticity of the information. HIPAA also requires institutions to protect the confidentiality of medical information stored in electronic records against reasonable and anticipated threats. The first line of maintaining patient confidentiality is achieved with a log-in process authenticating that the person is granted access. Authentication of the user is through an access code accompanied by a password.
A password is a collection of alphanumeric characters that a user types into the computer before accessing a program. A user is usually required to enter a password after the entry and acceptance of an access code or user name. A password does not appear on the computer screen when it is typed, nor should it be known to anyone but the user and information systems administrators (Hebda and Czar, 2013). Strong passwords use combinations of letters, numbers, and symbols that are not easy to guess. When using a health care agency computer system, it is essential that you do not share your computer password under any circumstances with anyone. A good system requires frequent and random changes in personal passwords to prevent unauthorized people from tampering with records. In addition, most staff have access only to patients in their work area. Select staff (e.g., administrators or risk managers) may be given authority to access all patient records. Most breaches of confidentiality come from inside the agency (Hebda and Czar, 2013).
Data security has three aspects: ensuring accuracy of data, protection of the data from unauthorized eyes inside or outside of the agency, and protection from data loss (Sewell and Thede, 2013). Data accuracy is ensured through mechanisms that check data during input and provide for correction of entries made in error. Accuracy of original data is the responsibility of the user.
Protection from inside intrusions occurs with audit trails. The trail reveals both unauthorized access and the identity of the person committing the violation. Keep in mind that audit trails are discoverable by a court of law. Another method to protect access to records from inside intrusions occurs with an automatic sign-off, a mechanism designed to log off a user from the computer system after a specified period of inactivity on the computer (Hebda and Czar, 2013). An automatic sign-off is often found in most patient care areas and other departments that handle sensitive data.
Protection from outside intrusions occurs with installation of firewalls and antivirus and spyware detection software. A firewall is a combination of hardware and software that protects private network resources (e.g., a hospital information system) from outside hackers, network damage, and theft or misuse of information. Computer data need protection from data loss resulting from either a system problem or a disaster (Sewell and Thede, 2013).
The data security process has taken on new meaning since the events of September 11, 2001. A disaster recovery plan must be in place. All agencies routinely create backup data and store the data off-site in a secure place (Hebda and Czar, 2013). Other considerations to maintain the security of the health care data include placing computers or file servers in restricted areas. Using a privacy shield on the computer screen helps to make information less visible. This form of security has limited benefit, especially if an organization uses mobile wireless devices such as notebooks, tablet personal computers (PCs), smartphones, and personal digital assistants (PDAs). These devices are easy to misplace or lose and can fall into the wrong hands. Some organizations use motion detectors or alarms with these devices to prevent theft. Password access with automatic logoff limits access to confidential information on these handheld devices.
Handling and Disposal of Information
Although it is important to keep medical records confidential, it is equally important to safeguard the information that is printed from the electronic record or extracted for report purposes. For example, a nurse prints a copy of a nursing activities work list to use as a day planner while administering care to patients. The nurse refers to information on the list and adds handwritten notes to enter later into the computer. Information on the list is considered personal health information (PHI). Thus the nurse must keep the information confidential and prevent unauthorized persons from viewing it. You destroy (e.g., shred) anything that is printed when the information is no longer needed.
The printing and faxing of information from a patient's record is a primary source for the unauthorized release of information. All papers containing PHI (e.g., Social Security number, date of birth or age, or patient's name or address) must be destroyed. Most agencies have shredders or locked receptacles for shredding and later incineration. Nurses also work in settings where they are responsible for erasing computer files from the hard drive containing calendars, surgery or diagnostic procedure schedules, or other daily records that contain PHI (Hebda and Czar, 2013). Be sure that you know the disposal policies for records in the institution where you work.
An institution needs to have sound policies for the use of fax machines, specifically which types of information you can send to which departments. You do not send more information by fax than what is needed or requested for immediate patient care needs. Take the following steps to enhance fax security (Hebda and Czar, 2013).
• Confirm that fax numbers are correct before sending to be sure that you direct information properly.
• Use a cover sheet, especially if a fax machine serves a number of different users.
• Authenticate at both ends of the transmission before data transmission to verify that source and destination are correct.
• Use programmed speed-dial keys to eliminate the chance of a dialing error and misdirected information.
• Use encryption to minimize ability to read confidential information.
• Use sealed envelopes for delivery.
• Place fax machines in a secure area.
• Limit machine access to designated individuals.
• Include a request to return documents by mail.
• Log fax transmissions. This feature is often available electronically on the machine.
Key Points
• The record is a confidential, legal, and continuing account of the patient's health care status and is available to all members of the health care team. It facilitates communication with health care providers for continuity of patient care, maintains a legal and financial record of care, aids in clinical research, and guides professional and organizational performance improvement.
• Accurate and timely record keeping requires an objective interpretation of data with precise measurements, correct spelling, and proper use of abbreviations.
• Effective documentation verifies the specific nursing care provided, use of services and equipment, and medications administered and thus supports the reimbursement that your health care agency receives.
• To limit liability nursing documentation describes what happened to a patient and clearly indicates that individualized, goal-directed nursing care was provided based on the nursing assessment.
• Organize problem-oriented medical records by the patient's health care problems.
• Medicare guidelines for establishing a patient's home care reimbursement are the basis for documentation by home care nurses.
• Long-term care documentation is interdisciplinary and closely linked with fiscal requirements of outside agencies.
• Computerized information systems provide information about patients in an accessible and organized manner.
• The major purpose of hand-off reports is patient safety and to maintain continuity of care.
• When information relevant to care is communicated by telephone, verify the information by a “read-back” process.
• Incident (occurrence/event) reports objectively describe any event not consistent with the routine care of a patient.
• Nursing informatics facilitates the integration of data, information, knowledge, and wisdom to support patients, nurses, and other providers in decision making in all roles and settings.
• Protection of the confidentiality of patient's health information and the security of computer systems must remain a top priority.
• The computerized health record improves continuity of health care by providing the ability to compare data from various health care encounters and offering easily accessible data for purposes of communication, reducing liability, reimbursement, education, research, and auditing and monitoring.
Clinical Decision-Making Exercises
You are caring for Mrs. Smith, who continues to have pain during the course of her postoperative stay in the hospital. Initially she received pain medication through her intravenous line. Now she is receiving oral pain medication, Ibuprofen one tab, on an as-needed basis. While you were at lunch, her roommate, Mrs. Jones, requested pain medication. The nurse covering for you inadvertently administered Vicodin one tab at 12:30 to Mrs. Smith instead of Mrs. Jones. When you return from lunch, you discover the medication error. You talk with the primary nurse about the current situation with Mrs. Smith. The EMR shows that Mrs. Smith has an allergy to acetaminophen (Tylenol). The nurse needs to contact Mrs. Smith's health care provider about the medication error.
1. Using the SBAR format, prepare the information that the nurse needs to provide to the health care provider about the medication error. Describe what each of the letters stand for in your description.
2. You note that the nurse who made the medication error charted the following in Mrs. Smith's medical record: Vicodin one tab given to Mrs. Smith accidently at 1230. Health care provider notified of wrong medication. Incident report completed as per hospital policy and put into Mrs. Smith's medical record. Orders received to monitor patient for signs of allergic reaction. Evaluate the documentation entry made by the nurse. Describe which parts of the documentation are recorded correctly and which part, if any, needs to be changed in the documentation?
3. Mrs. Smith is discharged. What information do you include in the discharge summary?
QSEN Activity: Informatics
It is now 3 days after surgery for Mrs. Smith, and you are working the 3 to 11 pm shift. You receive the hand-off report, which reports that Mrs. Smith has complaints of being “so weak” this afternoon. She refused to go to rehabilitation for her back strengthening exercises earlier in the day. You log into the EMR system and find Mrs. Smith's medical record. You review her recent laboratory data, including the complete blood count and earlier assessment information. You also note if any medications have been administered recently that might explain her weakness. The family is present and expresses concern over their mother's complaint of weakness. They note that it seems that the nursing staff spends much time on the computer. They ask how the EMR improves patient safety and quality care.




