Inhaled route
 The rationale for using the inhaled route
The rationale for using the inhaled route
 The appropriate use of the most widely prescribed inhaled medicines
The appropriate use of the most widely prescribed inhaled medicines
 The role of the peak flow meter
The role of the peak flow meter
The role of the pharmacist
Inhaled products are specialized dosage forms, which are designed to deliver medicines directly to the lung. A variety of inhaler devices are in use, all of which require the user of the inhaler to adopt an appropriate inhaler technique. Failure to use the correct inhaler technique will result in treatment failure. The pharmacist, who is usually the person who gives (dispenses) the inhaler to the patient, is ideally placed to demonstrate the appropriate inhalation technique for that inhaler. Using an inhaler is a skill, subject to the development of ‘bad habits’, which can lead to poor technique. Inhaler technique should therefore be regularly checked to ensure that the technique is optimal; again the pharmacist is ideally placed to perform this function.
Pharmacists can also provide education to patients beyond a discussion of a patient’s inhalers and other medicines, to include education about the patient’s disease (e.g. asthma) and its management. Pharmacists also run asthma clinics and may do so as supplementary or independent prescribers. A few pharmacists have specialist respiratory consultant posts in secondary care. A pharmacist wishing to undertake a specialist role in respiratory medicine will need to gain appropriate experience and undertake further training.
This chapter describes the most frequently prescribed inhaled therapies in the context of asthma and chronic obstructive pulmonary disease (COPD). The most widely prescribed inhaler devices are outlined along with instructions in their use.
Introduction
Many patients on inhaled therapy will be using more than one inhaler and may also have been prescribed a peak flow meter (PFM) to aid in monitoring their condition. In order for pharmacists to be able to provide useful education and advice to these patients, pharmacists will need to understand the condition being treated and the role of the medicines and devices prescribed. This chapter will provide that understanding in the context of the two most common airways diseases treated with inhaled medicines, namely asthma and COPD. It is beyond the scope of the chapter to discuss the diseases themselves, or the role of oral therapy and non-drug management of these conditions. It should be remembered that the most important interventions in COPD are smoking cessation and pulmonary rehabilitation.
There are significant differences in the way that inhalers are prescribed for asthma and COPD. In COPD, the emphasis of treatment is on the use of bronchodilators, and it may be appropriate for a COPD patient to have a long-acting inhaled beta-agonist without an inhaled steroid. This is different from asthma treatment where a long-acting beta-agonist should always be prescribed with an inhaled steroid. The scope of this chapter is limited to commonly used inhaled treatments and devices used for these inhaled treatments. By being familiar with national treatment guidelines for asthma and COPD, pharmacists can be assured that the advice that they give patients is likely to be consistent with that given by other healthcare professionals. These guidelines are: BTS/SIGN Asthma Guideline, 2011 (January 2012 revision): http://www.brit-thoracic.org.uk/guidelines/asthma-guidelines.aspx and NICE CG101 Chronic Obstructive Pulmonary Disease: http://guidance.nice.org.uk/CG101/NICEGuidance/pdf/English.
Asthma is a very common condition in the UK, affecting at least 5% of adults and up to 10% of children; therefore many people will experience symptoms attributable to asthma at some time in their life.
COPD has been an under-publicized condition. Prevalence of COPD in the UK is thought to be 2–4% of the total population with 1.5% of the population with diagnosed COPD. The decline in lung function leading to COPD is age-related but this decline can be rapidly accelerated in some smokers. COPD is thus an increasing problem in an ageing population.
Asthma and COPD are not mutually exclusive and some patients will have features of both diseases; this is often referred to as ‘mixed disease’. The prevalence of asthma, COPD and related conditions means that pharmacists will not only frequently encounter patients on inhaled therapy during dispensing, but will also encounter patients on inhaled therapy when giving advice on the sale of over-the-counter medicines.
The inhaled route
The inhaled route delivers medicines to the lungs. Inhaled medicines may have a local effect on the lungs or may be absorbed to give a systemic effect. The inhaled route is generally used when the lung is the target organ, e.g.:
 The antibiotic colistimethate sodium is nebulized to treat lung infections associated with cystic fibrosis
The antibiotic colistimethate sodium is nebulized to treat lung infections associated with cystic fibrosis
 The antiviral zanamivir is presented as a dry-powder inhaler for treating influenza.
The antiviral zanamivir is presented as a dry-powder inhaler for treating influenza.
Using the inhaled route when the lung is the target organ has a number of advantages:
 A smaller dose can be used. The normal adult oral dose of salbutamol is 4 mg, but the normal inhaled dose of salbutamol is 200 μg
A smaller dose can be used. The normal adult oral dose of salbutamol is 4 mg, but the normal inhaled dose of salbutamol is 200 μg
 The risk of unwanted systemic effects is reduced
The risk of unwanted systemic effects is reduced
 A faster onset of action may be achieved with some drugs, e.g. salbutamol
A faster onset of action may be achieved with some drugs, e.g. salbutamol
 Topically active drugs with poor oral bioavailability can be used.
Topically active drugs with poor oral bioavailability can be used.
The main disadvantage of the inhaled route is that inhaling a drug is more difficult than swallowing a tablet. Some drugs are ineffective by the inhaled route, e.g. theophylline.
Using the inhaled route does not result in the entire quantity of drug in the inhaler device reaching the lung. Even if an inhaler device is used perfectly, it is unlikely that any more than 20% of the drug reaches the lung. The majority of the rest of the drug remains in the oropharynx and is normally swallowed.
The lungs are designed to prevent the inhalation of anything other than gas. However, particles with a diameter of approximately 5 μm can be inhaled and have sufficient mass to settle in the lung. Particles larger than 10 μm remain in the oropharynx. Particles smaller than 1 μm are inhaled, but are then exhaled. Decreasing particle size increases the chance of penetration further down the tracheobronchial tree. It may be that a particle needs to be less than 3 μm to reach the 8th to 23rd branch generation. These particle sizes apply to the adult lung, and a smaller particle size of the order of 2.5 μm may be optimal in infant lungs.
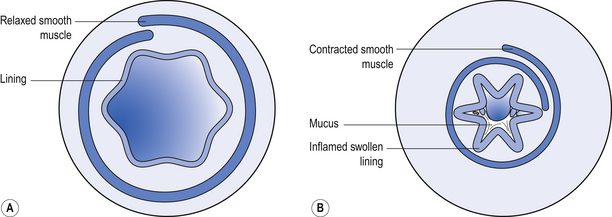
The specific target in the lung for medicines used in asthma and COPD is the bronchiole. Branching from bronchi, bronchioles are the first airways in the lung not to contain cartilage and are less than 1 mm in diameter. The absence of cartilage means that smooth muscle contraction reduces the size of the airway. Inflammation also results in reduction in size of the airway (Fig. 43.1).
Inhaled medicines used for asthma and COPD
Short-acting beta2 agonists (SABAs)
Salbutamol and terbutaline are widely used SABAs. They act on beta2 receptors in the smooth muscle of bronchioles to reverse bronchospasm. Symptoms caused by bronchospasm include wheeze, coughing, breathlessness and a feeling of tightness of the chest. For this reason, SABAs are often referred to as ‘relievers’ and should be used ‘as required’ to relieve symptoms. If a reliever inhaler is required for asthma more than twice a week most weeks, the addition of a ‘preventer’ (usually a steroid) inhaler should be considered.
Points to note
 The inhaler itself is not dangerous – but asthma is potentially life-threatening
The inhaler itself is not dangerous – but asthma is potentially life-threatening
 Appropriate, ‘as required’ use of a reliever inhaler provides a useful marker of the severity of the condition
Appropriate, ‘as required’ use of a reliever inhaler provides a useful marker of the severity of the condition
 Frequent usage of a reliever inhaler may indicate severe uncontrolled asthma
Frequent usage of a reliever inhaler may indicate severe uncontrolled asthma
 There is no risk that using the reliever inhaler whenever needed will result in a diminishing response, but worsening asthma will not respond to a reliever inhaler alone – additional treatment is required
There is no risk that using the reliever inhaler whenever needed will result in a diminishing response, but worsening asthma will not respond to a reliever inhaler alone – additional treatment is required
 If the reliever inhaler is not relieving symptoms, urgent medical attention is required
If the reliever inhaler is not relieving symptoms, urgent medical attention is required
 If reliever inhaler usage has increased, or is being used more than twice a week most weeks, review of treatment is required
If reliever inhaler usage has increased, or is being used more than twice a week most weeks, review of treatment is required
 The reliever inhaler can be used immediately before sport/exercise to prevent exercise-induced asthma in susceptible individuals
The reliever inhaler can be used immediately before sport/exercise to prevent exercise-induced asthma in susceptible individuals
Unwanted effects of inhaled beta2 agonists are rare but tremor can occur.
Long-acting beta2 agonists (LABAs)
Salmeterol, formoterol and indacaterol are inhaled LABAs. Salmeterol and formoterol are licensed for use in both asthma and COPD and are used twice daily. Indacaterol is licensed for COPD only and is used once daily. These inhalers are sometimes referred to as ‘protectors’.
Points to note
 LABAs should be used regularly and not on an ‘as required’ basis
LABAs should be used regularly and not on an ‘as required’ basis
 A reliever inhaler (SABA in asthma) should be used to relieve breakthrough symptoms
A reliever inhaler (SABA in asthma) should be used to relieve breakthrough symptoms
 For asthma, inhaled steroids (preventer inhalers) should be continued
For asthma, inhaled steroids (preventer inhalers) should be continued
 For COPD it is appropriate to use a LABA without concomitant inhaled steroids
For COPD it is appropriate to use a LABA without concomitant inhaled steroids
For COPD, a long-acting bronchodilator is the next step to a short-acting bronchodilator. A SABA (or SAMA) will also be required to relieve breakthrough symptoms.
Long-acting muscarinic antagonists (LAMAs)
Tiotropium bromide, glycopyrronium bromide and aclidinium bromide are inhaled LAMAs indicated for maintenance bronchodilator therapy in COPD. They are not licensed for asthma.
Inhaled corticosteroids (ICS)
The anti-inflammatory actions of steroids are able to control the inflammatory processes in asthma. No steroid inhaler is licensed for use in COPD. Two combination inhalers (LABA+ICS) at specific doses are licensed for COPD.
The inhaled route allows small doses of steroid to be used, minimizing the risk of systemic effects. The ideal inhaled steroid’s properties would include:
 Poor absorption from the gastrointestinal tract to minimize systemic effects due to the swallowed portion
Poor absorption from the gastrointestinal tract to minimize systemic effects due to the swallowed portion
 Complete metabolism in the ‘first pass’ through the liver
Complete metabolism in the ‘first pass’ through the liver
 Metabolism in the lung to inactive metabolites (absorption from the lung circumvents the ‘first pass’ through the liver).
Metabolism in the lung to inactive metabolites (absorption from the lung circumvents the ‘first pass’ through the liver).
Using a spacer device with the steroid inhaler, and/or rinsing the mouth with water and spitting immediately after using the inhaled steroid may reduce systemic effects and unwanted local effects in the mouth and throat.
Beclomethasone, budesonide, fluticasone ciclesonide and mometasone are examples of inhaled steroids. They are used once or twice daily depending on their license. Inhaled steroids are often referred to as ‘preventers’.
Inhaled steroids should normally be introduced:
 After a severe exacerbation of asthma
After a severe exacerbation of asthma
 If an asthmatic is using his short-acting beta2 agonist more than twice a week
If an asthmatic is using his short-acting beta2 agonist more than twice a week
The above measures form the basis for assessing control of asthma; in addition, limitation of exercise due to asthmatic symptoms and measures of lung function can be considered.
Points to note
 Inhaled steroids should be used regularly, not on an ‘as required’ basis
Inhaled steroids should be used regularly, not on an ‘as required’ basis
 Inhaled steroids have no immediate effect
Inhaled steroids have no immediate effect
 Improved asthma control will take a minimum of 1–3 days, and it may be 14–28 days before maximum improvement is seen after starting or increasing the dose of inhaled steroid
Improved asthma control will take a minimum of 1–3 days, and it may be 14–28 days before maximum improvement is seen after starting or increasing the dose of inhaled steroid
Unwanted systemic effects of inhaled steroids are extremely rare provided that the total daily dose is less than the equivalent of 800–1000 μg beclomethasone dipropionate.
Combination LABA/ICS inhalers
There are a number of different combinations presented in a variety of inhaler devices, these include:
 Salmeterol+fluticasone, three strength combinations as a metered dose inhaler (MDI) and three strength combinations as a dry powder inhaler (DPI)
Salmeterol+fluticasone, three strength combinations as a metered dose inhaler (MDI) and three strength combinations as a dry powder inhaler (DPI)
 Formoterol+budesonide, three strength combinations as a DPI
Formoterol+budesonide, three strength combinations as a DPI
 Formoterol+beclomethasone, one strength combination as a MDI
Formoterol+beclomethasone, one strength combination as a MDI
 Formoterol+fluticasone, three strength combinations as a MDI
Formoterol+fluticasone, three strength combinations as a MDI
In general, these combination inhalers are used as regular preventative therapy with the dose adjusted to achieve long-term control of asthma; a short-acting beta agonist inhaler being used for control of breakthrough symptoms. However, a budesonide 200 μg/formoterol 6 μg dry powder inhaler has been granted a licence for preventer (maintenance) and reliever use for asthma. Thus, some asthmatics who are using a budesonide 200 μg/formoterol 6 μg inhaler may only need to have one inhaler. A budesonide 200 μg/formoterol 6 μg inhaler can only be used for relief of symptoms if also being used as a regular preventer. It is not licensed for use before exercise to prevent exercise-induced asthma; an additional short-acting beta2 agonist should be used for this purpose.
Fluticasone 500 μg/salmeterol 50 μg dry powder inhaler and budesonide 400 μg/formoterol 12 μg dry powder inhaler, twice daily, are licensed for patients with COPD whose forced expiratory volume in 1 s (FEV1) is less than 50–60% predicted and who are frequent exacerbators (two or more exacerbations per year).
The peak flow meter
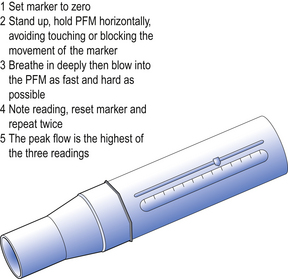
The peak flow meter (PFM) is a simple inexpensive device, prescribable on the NHS, which gives a useful objective measure of airways obstruction. A peak flow meter and its correct use is illustrated in Figure 43.2. The PFM measures peak expiratory flow rate (PEFR). PEFR is expressed in litres per minute (L/min). Flow rate of gas through a tube is proportional to the diameter of the tube when the pressure exerted on the gas is constant. Thus, the maximum rate at which individuals can expel air from their lungs is proportional to the patency of the tubes in their lungs. A reduced PEFR indicates that there is obstruction to airflow in the lungs.
Asthmatics will obtain useful information about their condition by using the PFM twice daily and charting their results for 2–4 weeks in the following situations:
 To confirm a diagnosis of asthma (a diurnal variation of PEFR of more than 20% is characteristic of asthma)
To confirm a diagnosis of asthma (a diurnal variation of PEFR of more than 20% is characteristic of asthma)
 To establish the level of control of asthma on current therapy
To establish the level of control of asthma on current therapy
 To track improvement of control of asthma following the introduction of a new treatment
To track improvement of control of asthma following the introduction of a new treatment
 To ensure asthma control is maintained when treatment is stepped down
To ensure asthma control is maintained when treatment is stepped down
Normal values are available for PEFR in graph or chart form or on ‘wheels’. In adults, normal values for PEFR vary by age, sex and height; for children, PEFR varies just by height. Normal or average values of PEFR are just that and values of 50–100 L/min above or below a predicted value fall within the normal range. An increase of at least 20% in PEFR following the use of an inhaled short-acting beta2 agonist such as salbutamol is diagnostic of asthma. This is known as a reversibility test.
The PFM is of less value in COPD as the airways obstruction tends to be fixed rather than variable, and lung volumes may be more important. Spirometry, which measures FEV1 and forced vital capacity (FVC), is a more useful test of lung function in COPD.
Types of inhaler device
Aerosol inhalers
Metered dose inhaler (MDI)
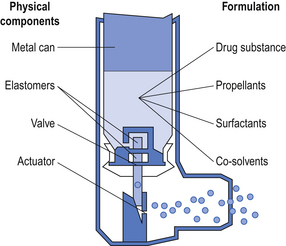
An MDI (Fig. 43.3) delivers an aerosol of drug dissolved or suspended in a propellant. Immediately an MDI is actuated, some of the propellant rapidly evaporates to produce droplets of appropriate size to be inhaled into the lung. Further evaporation of propellant may occur in the mouth and the so-called ‘cold-freon effect’ occurs if there is further evaporation of propellant (freon) when the aerosol impacts on the back of the throat. The sensation produced by the cold-freon effect can be sufficient in a minority of individuals to stop the inhalation and means that these individuals cannot use MDIs. The propellants currently used are generally hydrofluoroalkanes (HFAs). Chlorofluoroalkanes, also known as chlorofluorocarbons (CFCs), were formerly used as propellants, but are now banned by international treaty because of their ozone-depleting properties. It should perhaps be noted that while HFAs do not have the ozone-depleting effects of CFCs, both CFCs and HFAs are ‘greenhouse’ gases.
Surfactants such as oleic acid and co-solvents such as ethanol may be used to facilitate the production of an appropriate suspension or solution of drug in propellant.
The propellants, which are gases at room temperature, are maintained as liquids by filling under pressure into the metal aerosol canister.
A metered dose is achieved by having an appropriate size reservoir in the valve, which fills by gravity as the valve re-seats after each actuation.
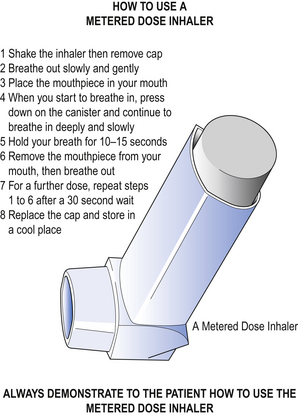
The correct method of using an MDI is shown in Figure 43.4.
Common errors in using an MDI include:
 Inability to coordinate actuation of the inhaler with inspiration
Inability to coordinate actuation of the inhaler with inspiration
 Taking a short, sharp inspiration, instead of a long, steady inspiration (this is often at least in part due to not exhaling before using the inhaler)
Taking a short, sharp inspiration, instead of a long, steady inspiration (this is often at least in part due to not exhaling before using the inhaler)
Breath-actuated MDI
Inhaling through a breath-actuated MDI triggers a mechanism that ‘fires’ (actuates) the aerosol. These inhalers are particularly useful for those patients who have difficulty coordinating inspiration with actuation of the MDI.
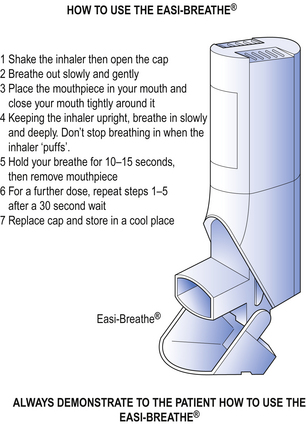
Easi-Breathe® is a type of breath-actuated MDI; its correct use is shown in Figure 43.5.
Autohaler® is another breath-actuated MDI. Using an Autohaler® is essentially the same as using an Easi-Breathe® except that the Autohaler® is primed by raising a lever on the top of the inhaler, whereas the Easi-Breathe® is primed by opening the mouthpiece cover.
MDI+spacer
A chamber device (spacer) may be attached to an MDI (Fig. 43.6).
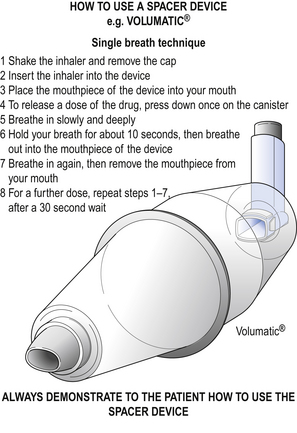
Figure 43.6 How to use a spacer device, e.g. Volumatic®. Method for patients who can use the device without help. (Source: Education for Health).
A spacer consists of a plastic chamber with a port at one end for the MDI and in most cases a one-way valve and mouthpiece at the other end.
An MDI+spacer is best used by firing a single dose from the MDI; inhalation should then start as soon as possible.
A spacer may be used with an MDI for the following reasons:
 To overcome difficulty in coordinating inspiration with actuation of the MDI, as the inspirable particles remain available for inhalation for some seconds after actuation
To overcome difficulty in coordinating inspiration with actuation of the MDI, as the inspirable particles remain available for inhalation for some seconds after actuation
 To decrease deposition of non-respirable particles in the oropharynx. The larger particles are deposited in the spacer, rather than the oropharynx. This may be particularly important for high-dose inhaled steroids
To decrease deposition of non-respirable particles in the oropharynx. The larger particles are deposited in the spacer, rather than the oropharynx. This may be particularly important for high-dose inhaled steroids
 To allow those unable to distinguish between inspiration and expiration (e.g. young children) to benefit from inhaled therapy by simply inhaling and exhaling across the one-way valve
To allow those unable to distinguish between inspiration and expiration (e.g. young children) to benefit from inhaled therapy by simply inhaling and exhaling across the one-way valve
 To deliver a large dose of bronchodilator in an acute attack. Current guidelines advocate inhaling single doses serially. There has also been a practice of actuating a number of doses into the larger volume spacers (e.g. Volumatic®) and then breathing tidally across the one-way valve.
To deliver a large dose of bronchodilator in an acute attack. Current guidelines advocate inhaling single doses serially. There has also been a practice of actuating a number of doses into the larger volume spacers (e.g. Volumatic®) and then breathing tidally across the one-way valve.
A mask may be attached or be integral to a spacer. The mask can then be placed over the mouth and nose of babies or infants to enable them to benefit from inhaled therapy. The correct use of a spacer and face mask is shown in Figure 43.7.
Examples of spacers are Volumatic®, Nebuhaler® and AeroChamber®.
Dry powder inhaler (DPI)
Medicines for inhalation can be presented as a micronized powder. The powder may be pure drug as in some Turbohalers®, or be drug and a carrier powder such as lactose, as in Diskhaler® and Accuhaler®.
When a carrier powder is used, the drug particles are adhered by weak electrostatic forces to the much larger carrier particles. As the drug/carrier powder is inhaled from the inhaler, the small respirable drug particles fly off the larger non-respirable carrier particles. The lactose carrier thus remains in the mouth. Patients using DPIs that employ a carrier powder should be reassured that even when using the inhaler correctly they will have carrier powder left in the mouth.
Patients inhaling pure drug from a Turbohaler® providing only drug may experience little or no taste.
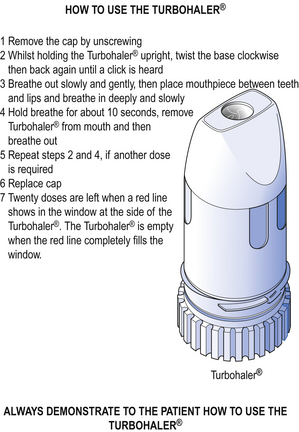
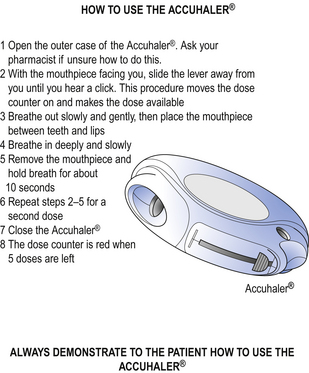
The correct method of using the Turbohaler® is shown in Figure 43.8 and the Accuhaler® in Figure 43.9.
All inhalers are boxed with instruction leaflets. However, the best way to learn how to use an inhaler is to have the technique demonstrated, then to attempt to use the inhaler under supervision so that any errors can be corrected. Many patients will benefit from pharmacists providing this service. Similarly, for pharmacists to best learn how to provide this service, they too should be shown how to use the inhaler and how to spot common errors. Medical representatives from companies that market inhalers are usually more than happy to train pharmacists how to use, demonstrate and check inhaler technique. As part of this service, the medical representative will provide placebo inhalers, to allow the pharmacist to demonstrate the correct inhaler technique, instruction leaflets and other patient education material. Pharmacists can also signpost patients to demonstration videos on websites such as www.asthma.org.uk.
The use and care of a DPI differs from that of an MDI, as shown in Table 43.1.
Table 43.1
Differences in the use and care of metered dose inhalers and dry powder inhalers
| MDI | DPI |
| Coordination of actuation and inhalation required | No coordination required as the release of powder and inhalation is a two-step process |
| Long, slow inhalation is the ideal to allow vaporization of propellants | Inhalation should be vigorous to disperse drug particles |
| The outer plastic housing of the inhaler (aerosol canister removed) can be washed to prevent blockage of actuator | Inhalers containing drug, e.g. Turbohaler®, must never be washed |
| Exhalation prior to inhalation can be into the inhaler | Exhalation must never be into the inhaler |
Nebulizers
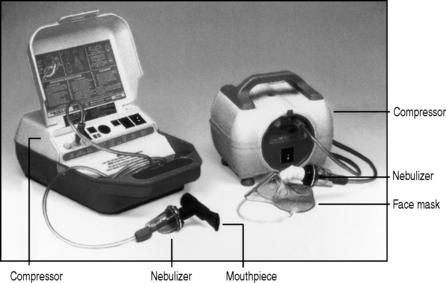
Medicines for inhalation can be presented as solutions or suspensions for nebulization. A nebulizing system (Fig. 43.10) usually consists of a compressor supplying compressed air to a nebulizing chamber, which delivers the nebulized drug to the patient via a mouthpiece or face mask. The face mask is most commonly used but when deposition of the nebulized drug on the face is undesirable (e.g. a steroid), then a mouthpiece is preferable, or the face under the mask should be protected with petroleum jelly. A mouthpiece is also needed with inhaled ipratropium to prevent the potential precipitation of closed angle glaucoma.
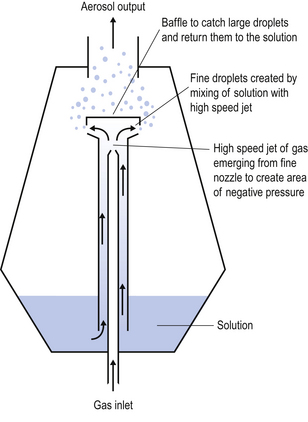
The principle of jet nebulization is shown in Figure 43.11. The gas used to drive the nebulization process may be oxygen or air, but in either case a minimum flow rate of 8 L/min at a pressure of at least 69 kPa (10 psi) is required.
Patients using more than one nebulized medicine may have two different solutions mixed in the nebulizing chamber to be nebulized together. The summary of product characteristics (SPC) may give advice on other solutions and diluents that may be appropriately mixed with a given medicine for nebulization. It is possible that one solution will precipitate the other; this can normally be detected by the mixed solutions in the nebulizer chamber changing from clear to cloudy. Such a change means that the mixed solutions are not compatible and should not be nebulized together. Consideration should also be given to the total volume of the mixed solutions, as the larger the volume, the longer it will take to be nebulized.
Nebulizers are used when high doses of drug are required and/or when the patient is unable to use any form of inhaler. Nebulizers do not require the patient to learn any technique and are effective on normal or shallow breathing.
Nebulizers are used in the treatment of severe acute asthma and this is best done under medical supervision:
 To ensure that an adequate objective and maintained response to treatment is achieved (e.g. by measuring PEFR before and after nebulization)
To ensure that an adequate objective and maintained response to treatment is achieved (e.g. by measuring PEFR before and after nebulization)
 To assess if other treatment is indicated, e.g. oral or parenteral steroids
To assess if other treatment is indicated, e.g. oral or parenteral steroids
 To plan follow-up and possible review of chronic medication.
To plan follow-up and possible review of chronic medication.
Nebulized treatment may also be used in the latter stages of COPD often in conjunction with domiciliary oxygen therapy. Domiciliary oxygen cylinders do not provide sufficient flow rates to produce adequate nebulization, so a compressor unit should be used.
Drugs for nebulization are normally presented as unit dose vials; examples of these are Nebules® and Respules®.
Key Points
 Asthma and COPD are common conditions, treatment of which is largely dependent on the inhaled route
Asthma and COPD are common conditions, treatment of which is largely dependent on the inhaled route
 The vast majority of inhaled treatments for asthma and COPD can be divided into two pharmacological classes of drugs: inhaled bronchodilators and inhaled steroids
The vast majority of inhaled treatments for asthma and COPD can be divided into two pharmacological classes of drugs: inhaled bronchodilators and inhaled steroids
 Inhaled bronchodilators can be further subdivided into beta2 agonists and muscarinic agonists. Each of these classes can be further subdivided into short acting and long acting
Inhaled bronchodilators can be further subdivided into beta2 agonists and muscarinic agonists. Each of these classes can be further subdivided into short acting and long acting
 National and international management guidelines are available for asthma and COPD and treatment is based on a step-wise approach
National and international management guidelines are available for asthma and COPD and treatment is based on a step-wise approach
 A range of inhalation devices is available to deliver drugs directly to the lungs. This has clear advantages including using much lower doses compared with oral therapy
A range of inhalation devices is available to deliver drugs directly to the lungs. This has clear advantages including using much lower doses compared with oral therapy
 The use of inhalers is technique dependent and patients require training in their use
The use of inhalers is technique dependent and patients require training in their use
 Medicines to be inhaled are presented as aerosol inhalers, dry powder inhalers or liquids to be nebulized
Medicines to be inhaled are presented as aerosol inhalers, dry powder inhalers or liquids to be nebulized
 The most widely prescribed inhaler device is the aerosol metered dose inhaler (MDI). The MDI may be used in conjunction with a spacing device (a ‘spacer’). A modified form of the MDI, triggered to actuate by inhalation, is a breath-actuated MDI. Both the ‘spacer’ and the breath-actuated MDI overcome the main difficulty of using an MDI, the need to coordinate inhalation with actuation of the MDI, and allow a wider range of individuals to successfully use an MDI
The most widely prescribed inhaler device is the aerosol metered dose inhaler (MDI). The MDI may be used in conjunction with a spacing device (a ‘spacer’). A modified form of the MDI, triggered to actuate by inhalation, is a breath-actuated MDI. Both the ‘spacer’ and the breath-actuated MDI overcome the main difficulty of using an MDI, the need to coordinate inhalation with actuation of the MDI, and allow a wider range of individuals to successfully use an MDI
 Dry powder inhalers (DPIs) were originally developed to overcome the difficulty some patients have coordinating inhalation with actuation of an MDI
Dry powder inhalers (DPIs) were originally developed to overcome the difficulty some patients have coordinating inhalation with actuation of an MDI
 DPIs vary widely in appearance and the method by which the powder is made available for inhalation, but all rely on inhalation to mobilize the powder from the inhaler and through the mouthpiece
DPIs vary widely in appearance and the method by which the powder is made available for inhalation, but all rely on inhalation to mobilize the powder from the inhaler and through the mouthpiece
 Liquids for nebulization are either solutions or permanent suspensions. It may be that solutions are more reliably nebulized and inhaled than permanent suspensions
Liquids for nebulization are either solutions or permanent suspensions. It may be that solutions are more reliably nebulized and inhaled than permanent suspensions
 Caution should be exercised when mixing two liquids for nebulization in the nebulizer, as one liquid can cause precipitation in the other
Caution should be exercised when mixing two liquids for nebulization in the nebulizer, as one liquid can cause precipitation in the other
 The peak flow meter is a simple prescribable device which gives an objective measurement of lung function, and can be useful from time to time for asthmatics, e.g. when commencing a new treatment. It may also be used to aid self-management of asthma
The peak flow meter is a simple prescribable device which gives an objective measurement of lung function, and can be useful from time to time for asthmatics, e.g. when commencing a new treatment. It may also be used to aid self-management of asthma
 Many asthmatic and COPD patients will have at least two or three different inhalers. They will obtain greatest benefit from their inhalers if they understand something about their condition, the rationale for the different inhalers and how and when to use them
Many asthmatic and COPD patients will have at least two or three different inhalers. They will obtain greatest benefit from their inhalers if they understand something about their condition, the rationale for the different inhalers and how and when to use them
 Pharmacists with an understanding of asthma and COPD treatment and the correct use of inhalers can provide advice, education and training for patients on inhaled therapy which can markedly improve patients’ quality of life.
Pharmacists with an understanding of asthma and COPD treatment and the correct use of inhalers can provide advice, education and training for patients on inhaled therapy which can markedly improve patients’ quality of life.