Lower Limb
1 Introduction
As with the upper limb in Chapter 7, this chapter approaches our study of the lower limb by organizing its anatomical structures into functional compartments. The thigh and leg each are organized into three functional compartments, with their respective muscles and neurovascular bundles. The lower limb subserves the following important functions and features:
• Supports the weight of the body, and transfers that support to the axial skeleton across the hip and sacro-iliac joints.
• The hip and knee joints lock into position when standing still in anatomical position, adding stability and balance to the transfer of weight and conserving the muscles' energy; this allows one to stand erect for prolonged periods.
• Functions in locomotion through the process of walking (our gait).
• Anchored to the axial skeleton by the pelvic girdle, which allows for less mobility but significantly more stability than the pectoral girdle of the upper limb.
Be sure to review the movements of the lower limb as described in Chapter 1 (see Fig. 1-3). Note the terms dorsiflexion (extension) and plantarflexion (flexion), and inversion (supination) and eversion (pronation), which are unique to the movements of the ankle.
2 Surface Anatomy
The components of the lower limb include the gluteal region, thigh, leg, and foot. The key surface landmarks include the following (Fig. 6-1):
• Inguinal ligament: the folded, inferior edge of the external abdominal oblique aponeurosis that separates the abdominal region from the thigh (Poupart's ligament).
• Greater trochanter: the point of the hip and attachment site for several gluteal muscles.
• Quadriceps femoris: the muscle mass of the anterior thigh, composed of four muscles—rectus femoris and three vastus muscles—that extend the leg at the knee.
• Patella: the kneecap; largest sesamoid bone in the body.
• Popliteal fossa: the region posterior to the knee.
• Gastrocnemius muscles: the muscle mass that forms the calf.
• Calcaneal (Achilles) tendon: the prominent tendon of several calf muscles.
• Small saphenous vein: drains blood from the lateral dorsal venous arch and posterior leg (calf) into the popliteal vein posterior to the knee.
• Great saphenous vein: drains blood from the medial dorsal venous arch, leg, and thigh into the femoral vein just inferior to the inguinal ligament.
Superficial veins drain blood toward the heart and communicate with deep veins that parallel the arteries of the lower limb. When vigorous muscle contraction compresses the deep veins, venous blood is shunted into superficial veins and returned to the heart. All these veins have valves to aid in the venous return to the heart.
Corresponding cutaneous nerves are terminal sensory branches of major lower limb nerves that arise from lumbar (L1-L4) and sacral (L4-S4) plexuses (Fig. 6-2). Note that the gluteal region has superior, middle, and inferior cluneal nerves, and the thigh has posterior, lateral, anterior, and medial cutaneous nerves. The leg has lateral sural, superficial fibular, saphenous, and sural cutaneous nerves (named from the lateral leg to the posterior leg). The sural nerve on the posterior leg parallels the small saphenous vein, and the saphenous nerve (terminal portion of the femoral nerve) parallels the great saphenous vein from the medial ankle to the level of the knee.
3 Hip
Bones and Joints of the Pelvic Girdle and Hip
The pelvic girdle is the attachment point of the lower limb to the body's trunk and axial skeleton. The pectoral girdle is its counterpart for the attachment of the upper limb. The sacro-iliac ligaments (posterior, anterior, and interosseous) are among the strongest ligaments in the body and support its entire weight, almost pulling the sacrum into the pelvis. Note that the pelvis (sacrum and coxal bones) in anatomical position is tilted forward such that the pubic symphysis and the anterior superior iliac spines lie in the same vertical plane, placing great stress on the sacro-iliac joints and ligaments (see Figs. 5-3 and 6-3). In fact, the body's center of gravity when standing upright lies just anterior to the S2 vertebra of the fused sacrum.
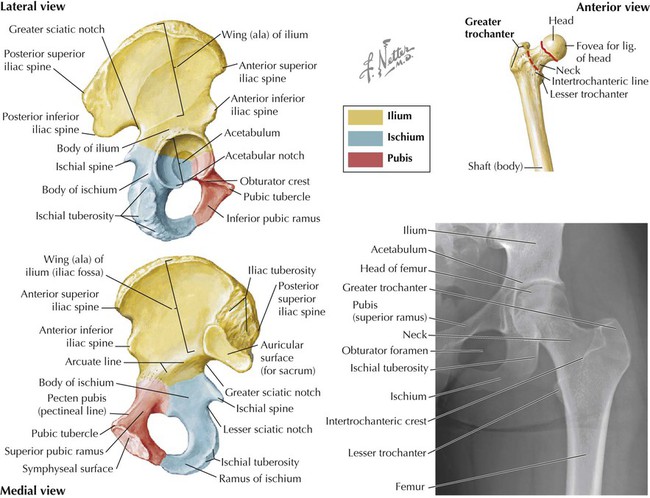
The bones of the pelvis include the following (Fig. 6-3 and Table 6-1):
TABLE 6-1
Features of the Pelvis and Proximal Femur
| FEATURE | CHARACTERISTICS |
| Coxal (Hip) Bone | |
| Fusion of three bones on each side to form the pelvis, which articulates with the sacrum to form the pelvic girdle | |
| Ilium | Body fused to ischium and pubis, all meeting in the acetabulum (socket for articulation with femoral head) Ala (wing): weak spot of ilium |
| Ischium | Body fused with other two bones; ramus fused with pubis |
| Pubis | Body fused with other two bones; ramus fused with ischium |
| Femur (Proximal) | |
| Long bone | Longest bone in the body and very strong |
| Head | Point of articulation with acetabulum of coxal bone |
| Neck | Common fracture site |
| Greater trochanter | Point of the hip; attachment site for several gluteal muscles |
| Lesser trochanter | Attachment site of iliopsoas tendon (strong hip flexor) |
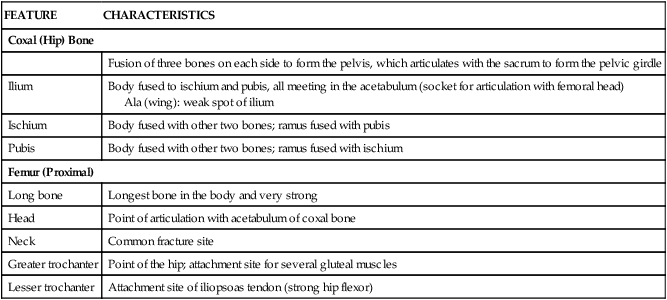
• Right and left pelvic bones (coxal or hip bones): the fusion of three separate bones called the ilium, ischium, and pubis, which join each other in the acetabulum (cup-shaped feature for articulation of the head of the femur).
• Sacrum: the fusion of the five sacral vertebrae; the two pelvic bones articulate with the sacrum posteriorly.
• Coccyx: the terminal end of the vertebral column, and a remnant of our embryonic tail.
Additionally, the proximal femur (thigh bone) articulates with the pelvis at the acetabulum (see Fig. 6-3 and Table 6-1).
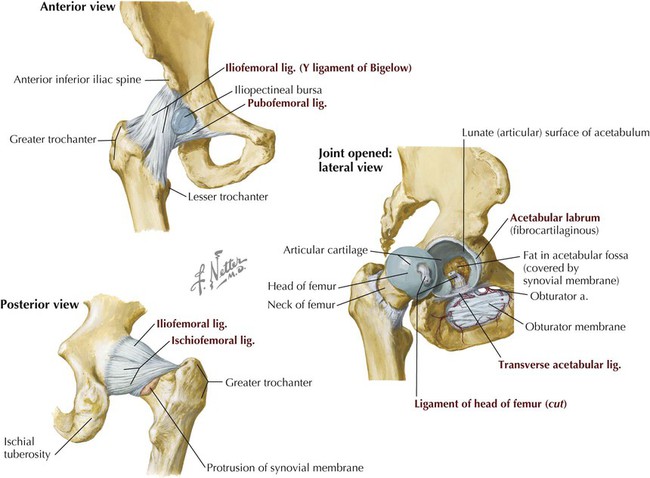
The hip joint is a classic ball-and-socket synovial joint that affords great stability, provided by both its bony anatomy and its strong ligaments (Fig. 6-4 and Table 6-2). As with most large joints, there is a rich vascular anastomosis around the hip joint, contributing a blood supply not only to the hip but also to the associated muscles (Fig. 6-5 and Table 6-3).
TABLE 6-2
Ligaments of the Hip Joint (Multiaxial Synovial Ball and Socket)
| LIGAMENT | ATTACHMENT | COMMENT |
| Capsular | Acetabular margin to femoral neck | Encloses femoral head and part of neck; acts in flexion, extension, abduction, adduction, medial and lateral rotation, and circumduction |
| Iliofemoral | Iliac spine and acetabulum to intertrochanteric line | Forms inverted Y (of Bigelow); limits hyperextension and lateral rotation; the stronger ligament |
| Ischiofemoral | Acetabulum to femoral neck posteriorly | Limits extension and medial rotation; the weaker ligament |
| Pubofemoral | Pubic ramus to lower femoral neck | Limits extension and abduction |
| Labrum | Acetabulum | Fibrocartilage, deepens socket |
| Transverse acetabular | Acetabular notch inferiorly | Cups acetabulum to form a socket for femoral head |
| Ligament of head of femur | Acetabular notch and transverse ligament to femoral head | Artery to femoral head runs in ligament |
TABLE 6-3
| ARTERY | COURSE AND STRUCTURES SUPPLIED |
| Medial circumflex | Usually arises from deep artery of thigh; branches supply femoral head and neck; passes posterior to iliopsoas muscle tendon |
| Lateral circumflex | Usually arises from deep artery of the thigh |
| Acetabular branch | Arises from obturator artery; runs in ligament of head of femur; supplies femoral head |
| Gluteal branches (superior and inferior) | Form anastomoses with medial and lateral femoral circumflex branches |
The other features of the pelvic girdle and its stabilizing lumbosacral and sacro-iliac joints are illustrated and summarized in Chapter 5.
Nerve Plexuses
Several nerve plexuses exist within the pelvis and send branches to somatic structures (skin and skeletal muscle) of the pelvis and lower limb. The lumbar plexus is composed of the ventral rami of spinal nerves L1-L4, which give rise to two large nerves, the femoral and obturator nerves, and several smaller branches (Fig. 6-6). The femoral nerve (L2-L4) innervates muscles of the anterior thigh, whereas the obturator nerve (L2-L4) innervates muscles of the medial thigh.
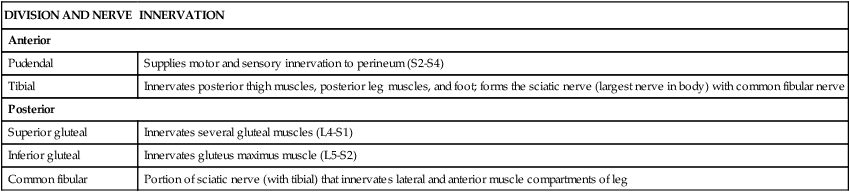
The sacral plexus is composed of the ventral rami of spinal nerves L4-S4. Its major branches are summarized in Figure 6-7 and Table 6-4. The small coccygeal plexus has contributions from S4-Co1 and gives rise to small anococcygeal branches that innervate the coccygeus muscle and skin of the anal triangle (see Chapter 5). Often the lumbar and sacral plexuses are simply referred to as the lumbosacral plexus.
TABLE 6-4
Major Branches of the Sacral Plexus
| DIVISION AND NERVE | INNERVATION |
| Anterior | |
| Pudendal | Supplies motor and sensory innervation to perineum (S2-S4) |
| Tibial | Innervates posterior thigh muscles, posterior leg muscles, and foot; forms the sciatic nerve (largest nerve in body) with common fibular nerve |
| Posterior | |
| Superior gluteal | Innervates several gluteal muscles (L4-S1) |
| Inferior gluteal | Innervates gluteus maximus muscle (L5-S2) |
| Common fibular | Portion of sciatic nerve (with tibial) that innervates lateral and anterior muscle compartments of leg |
Access to the Lower Limb
Structures passing out of or into the lower limb from the abdominopelvic cavity may do so through one of the following four passageways (see Figs. 5-3 and 6-10):
• Anteriorly between the inguinal ligament and bony pelvis into the anterior thigh
• Anteroinferiorly through the obturator canal into the medial thigh
• Posterolaterally through the greater sciatic foramen into the gluteal region
• Posterolaterally through the lesser sciatic foramen from the gluteal region into the perineum (via the pudendal [Alcock's] canal)
4 Gluteal Region
Muscles
The muscles of the gluteal (buttock) region are arranged into superficial and deep groups, as follows (Fig. 6-8 and Table 6-5):
TABLE 6-5
| MUSCLE | PROXIMAL ATTACHMENT (ORIGIN) | DISTAL ATTACHMENT (INSERTION) | INNERVATION | MAIN ACTIONS |
| Gluteus maximus | Ilium posterior to posterior gluteal line, dorsal surface of sacrum and coccyx, and sacrotuberous ligament | Most fibers end in iliotibial tract that inserts into lateral condyle of tibia; some fibers insert on gluteal tuberosity of femur | Inferior gluteal nerve (L5-S2) | Extends flexed thigh at the hip and assists in its lateral rotation; abducts and assists in raising trunk from flexed position |
| Gluteus medius | Lateral surface of ilium | Lateral surface of greater trochanter of femur | Superior gluteal nerve (L4-S1) | Abducts and medially rotates thigh at hip; steadies pelvis on limb when opposite limb is raised |
| Gluteus minimus | Lateral surface of ilium | Anterior surface of greater trochanter of femur | Superior gluteal nerve (L4-S1) | Abducts and medially rotates thigh at hip; steadies pelvis on limb when opposite limb is raised |
| Tensor fasciae latae | Anterior superior iliac spine and anterior iliac crest | Iliotibial tract that attaches to lateral condyle of tibia | Superior gluteal nerve (L4-L5) | Abducts, medially rotates, and flexes thigh at hip; helps to keep knee extended |
| Piriformis | Anterior surface of sacrum and sacrotuberous ligament | Superior border of greater trochanter of femur | Branches of ventral rami (L5-S2) | Laterally rotates extended thigh at hip and abducts flexed thigh at hip; steadies femoral head in acetabulum |
| Obturator internus | Pelvic surface of obturator membrane and surrounding bones | Medial surface of greater trochanter of femur | Nerve to obturator internus (L5-S2) | Laterally rotates extended thigh at hip and abducts flexed thigh at hip; steadies femoral head in acetabulum |
| Gemelli, superior and inferior | Superior: ischial spine Inferior: ischial tuberosity |
Medial surface of greater trochanter of femur | Superior gemellus: same nerve supply as obturator internus Inferior gemellus: same nerve supply as quadratus femoris |
Laterally rotate extended thigh at the hip and abducts flexed thigh at the hip; steady femoral head in acetabulum |
| Quadratus femoris | Lateral border of ischial tuberosity | Quadrate tubercle on intertrochanteric crest of femur | Nerve to quadratus femoris (L4-S1) | Laterally rotates thigh at hip; steadies femoral head in acetabulum |
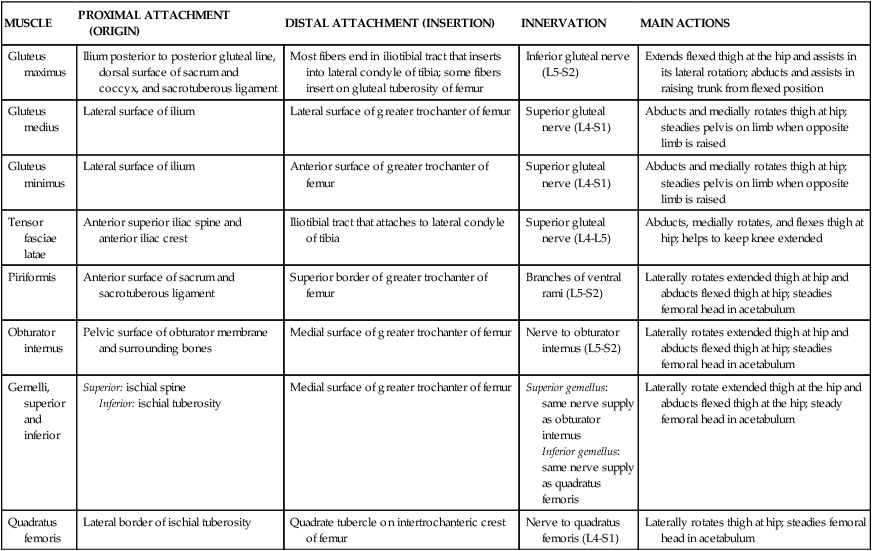
• Superficial muscles include the three gluteal muscles and the tensor fasciae latae laterally.
• Deep muscles act on the hip, primarily as lateral rotators of the thigh at the hip, and assist in stabilizing the hip joint.
The gluteus maximus muscle is one of the strongest muscles in the body in absolute terms and is a powerful extensor of the thigh at the hip (Fig. 6-8). It is especially important in extending the hip when rising from a squatting or sitting position, and when climbing stairs. The gluteus maximus also stabilizes and laterally rotates the hip joint. The gluteus medius and gluteus minimus muscles are primarily abductors and medial rotators of the thigh at the hip, steadying the pelvis over the lower limb when the opposite lower limb is raised off the ground (see Fig. 6-34).
The tensor fasciae latae muscle abducts, medially rotates, and stabilizes the extended knee. The deep fascia of the thigh (fascia lata) is especially thickened laterally and is known as the iliotibial tract. Both the tensor fasciae latae and most of the gluteus maximus muscles insert into this tract and help stabilize the hip and knee extension when standing. People may shift their weight from one lower limb to the other and stabilize the limb they are standing on by placing tension on this iliotibial tract.
Neurovascular Structures
The nerves innervating the gluteal muscles arise from the sacral plexus (see Figs. 6-7 and 6-8 and Tables 6-4 and 6-5) and gain access to the gluteal region largely by passing through the greater sciatic foramen. The blood supply to this region is via the superior and inferior gluteal arteries, which are branches of the internal iliac artery in the pelvis (see also Fig. 5-13 and Table 5-6) and also gain access to the gluteal region via the greater sciatic foramen. These neurovascular elements pass in the plane deep to the gluteus medius muscle (superior gluteal neurovascular bundle) or deep to the gluteus maximus muscle (inferior gluteal neurovascular structures). Also passing through the gluteal region is the largest nerve in the body, the sciatic nerve (L4-S3), which exits the greater sciatic foramen, passes through or more often inferior to the piriformis muscle, and enters the posterior thigh passing deep to the long head of the biceps femoris muscle (see Fig. 6-8).
The internal pudendal artery and pudendal nerve (a somatic nerve, S2-S4) pass out of the greater sciatic foramen, wrap around the sacrospinous ligament, and reenter the lesser sciatic foramen to gain access to the pudendal (Alcock's) canal (see Figs. 5-22 and 6-8). The pudendal nerve innervates the skeletal muscle and skin of the perineum (see Table 6-4). The internal pudendal artery is the major blood supply to the perineum and external genitalia.
5 Thigh
The thigh is the region of the lower limb between the hip and knee. As you learn the anatomical arrangement of the thigh and leg, organize your study around the functional muscular compartments. The thigh is divided into three muscular compartments: an anterior (extensor) compartment, a medial (adductor) compartment, and a posterior (flexor) compartment by intermuscular septae.
Bones
The femur, the longest bone in the body, is the bone of the thigh. It is slightly bowed anteriorly and runs slightly diagonally, lateral to medial, from the hip to the knee (Fig. 6-9 and Table 6-6). Proximally the femur articulates with the pelvis, and distally it articulates with the tibia and the patella (kneecap), which is the largest sesamoid bone in the body. The proximal femur is supplied with blood from the medial and lateral femoral circumflex branches of the deep femoral artery (see Fig. 6-13), an acetabular branch of the obturator artery, and by anastomotic branches of the inferior gluteal artery. The shaft and distal femur is supplied by femoral nutrient arteries and by anastomotic branches of the popliteal artery, the distal continuation of the femoral artery posterior to the knee.
TABLE 6-6
| STRUCTURE | CHARACTERISTICS |
| Long bone | Longest bone in the body; very strong |
| Head | Point of articulation with acetabulum of coxal bone |
| Neck | Common fracture site |
| Greater trochanter | Point of hip; attachment site for several gluteal muscles |
| Lesser trochanter | Attachment site of iliopsoas tendon (strong hip flexor) |
| Distal condyles | Medial and lateral (smaller) sites that articulate with tibial condyles |
| Patella | Sesamoid bone (largest) embedded in quadriceps femoris tendon |
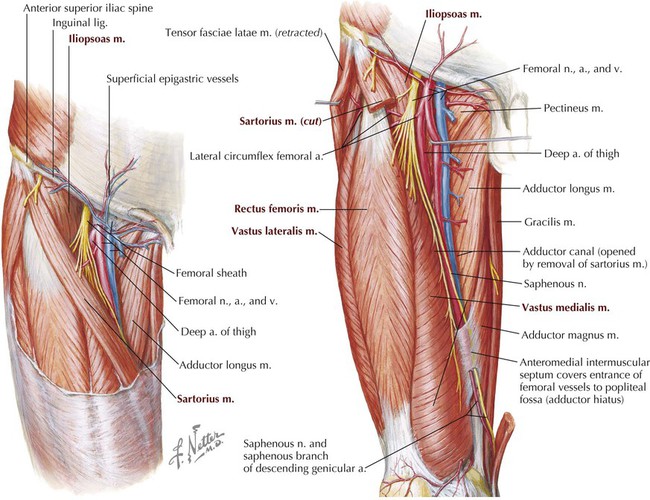
Anterior Compartment Thigh Muscles, Vessels, and Nerves
Muscles of the anterior compartment exhibit the following characteristics (Figs. 6-10 and 6-11 and Table 6-7):
TABLE 6-7
Anterior Compartment Thigh Muscles
| MUSCLE | PROXIMAL ATTACHMENT (ORIGIN) | DISTAL ATTACHMENT (INSERTION) | INNERVATION | MAIN ACTIONS |
| Psoas major (iliopsoas) | Sides of T12-L5 vertebrae and discs between them; transverse processes of all lumbar vertebrae | Lesser trochanter of femur | Ventral rami of lumbar nerves (L1-L3) | Acts jointly with iliacus in flexing thigh at hip joint and in stabilizing hip joint |
| Iliacus (iliopsoas) | Iliac crest, iliac fossa, ala of sacrum, and anterior sacro-iliac ligaments | Tendon of psoas major, lesser trochanter, and femur | Femoral nerve (L2-L3) | Acts jointly with psoas major in flexing thigh at hip joint and in stabilizing hip joint |
| Sartorius | Anterior superior iliac spine and superior part of notch inferior to it | Superior part of medial surface of tibia | Femoral nerve (L2-L3) | Flexes, abducts, and laterally rotates thigh at hip joint; flexes knee joint |
| Quadriceps Femoris | ||||
| Rectus femoris | Anterior inferior iliac spine and ilium superior to acetabulum | Base of patella and by patellar ligament to tibial tuberosity | Femoral nerve (L2-L4) | Extends leg at knee joint; also steadies hip joint and helps iliopsoas to flex thigh at hip |
| Vastus lateralis | Greater trochanter and lateral lip of linea aspera of femur | Base of patella and by patellar ligament to tibial tuberosity | Femoral nerve (L2-L4) | Extends leg at knee joint |
| Vastus medialis | Intertrochanteric line and medial lip of linea aspera of femur | Base of patella and by patellar ligament to tibial tuberosity | Femoral nerve (L2-L4) | Extends leg at knee joint |
| Vastus intermedius | Anterior and lateral surfaces of femoral shaft | Base of patella and by patellar ligament to tibial tuberosity | Femoral nerve (L2-L4) | Extends leg at knee joint |
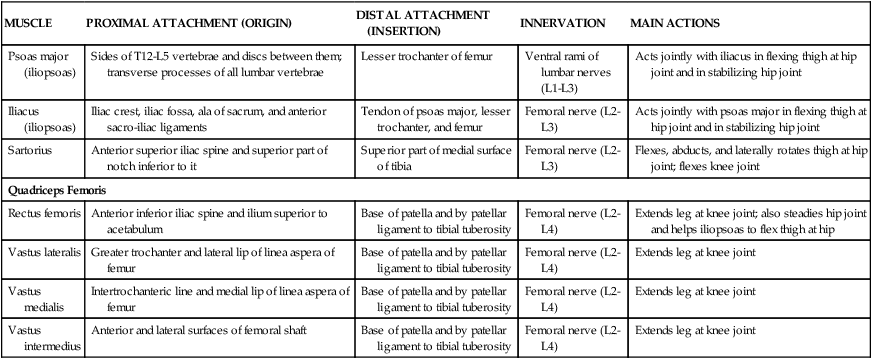
• Include the quadriceps muscles, which attach to the patella by the quadriceps femoris tendon and to the tibia by the patellar ligament (clinicians often refer to this ligament as the “patellar tendon”).
• Are primarily extensors of the leg at the knee.
• Two can secondarily flex the thigh at the hip (sartorius and rectus femoris).
• Are innervated by the femoral nerve.
• Are supplied by the femoral artery and its deep (femoral) artery of the thigh.
Additionally, the psoas major and iliacus muscles (which form the iliopsoas) pass from the posterior abdominal wall to the anterior thigh by passing deep to the inguinal ligament to insert on the lesser trochanter of the femur. These muscles act jointly as powerful flexors of the thigh at the hip joint (Table 6-7; see also Fig. 4-32).
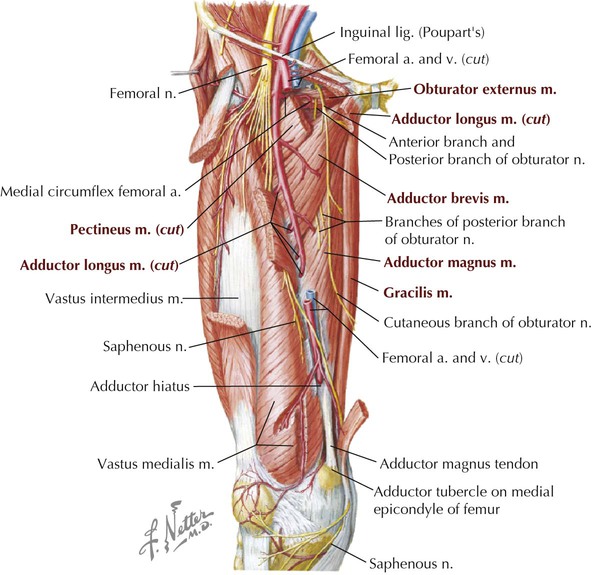
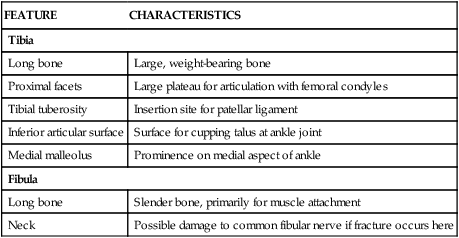
Medial Compartment Thigh Muscles, Vessels, and Nerves
Muscles of the medial compartment exhibit the following characteristics (see Figs. 6-10 and 6-11 and Table 6-8):
TABLE 6-8
Medial Compartment Thigh Muscles
| MUSCLE | PROXIMAL ATTACHMENT (ORIGIN) | DISTAL ATTACHMENT (INSERTION) | INNERVATION | MAIN ACTIONS |
| Pectineus | Superior ramus of pubis | Pectineal line of femur, just inferior to lesser trochanter | Femoral nerve; may receive a branch from obturator nerve | Adducts and flexes thigh at hip; assists with medial rotation of thigh |
| Adductor longus | Body of pubis inferior to pubic crest | Middle third of linea aspera of femur | Obturator nerve (L2-L4) | Adducts thigh at hip |
| Adductor brevis | Body and inferior ramus of pubis | Pectineal line and proximal part of linea aspera of femur | Obturator nerve (L2-L4) | Adducts thigh at hip and, to some extent, flexes it |
| Adductor magnus | Inferior ramus of pubis, ramus of ischium, and ischial tuberosity | Adductor part: gluteal tuberosity, linea aspera, medial supracondylar line. Hamstring part: adductor tubercle of femur |
Adductor part: obturator nerve Hamstring part: tibial part of sciatic nerve |
Adducts thigh at hip Adductor part: also flexes thigh at hip Hamstring part: extends thigh |
| Gracilis | Body and inferior ramus of pubis | Superior part of medial surface of tibia | Obturator nerve (L2-L3) | Adducts thigh at hip; flexes leg at knee and helps to rotate it medially |
| Obturator externus | Margins of obturator foramen and obturator membrane | Trochanteric fossa of femur | Obturator nerve (L2-L3) | Rotates thigh laterally at hip; steadies femoral head in acetabulum |
• Are primarily adductors of the thigh at the hip.
• Most can secondarily flex and/or rotate the thigh.
• Are largely innervated by the obturator nerve.
• Are supplied by the obturator artery and deep (femoral) artery of the thigh.
The pectineus muscle, while residing in the medial compartment, is largely innervated by the femoral nerve, although it also may receive a branch from the obturator nerve. The adductor magnus, being an exceptionally large and powerful muscle, also receives some innervation via the tibial portion of the sciatic nerve, which runs in the posterior compartment of the thigh.
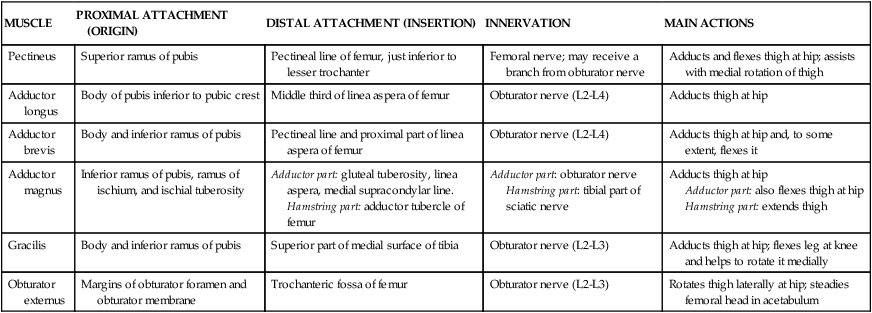
Posterior Compartment Thigh Muscles, Vessels, and Nerves
Muscles of the posterior compartment exhibit the following characteristics (Fig. 6-12 and Table 6-9; see Fig. 6-8):
TABLE 6-9
Posterior Compartment Thigh Muscles
| MUSCLE | PROXIMAL ATTACHMENT (ORIGIN) | DISTAL ATTACHMENT (INSERTION) | INNERVATION | MAIN ACTIONS |
| Semitendinosus | Ischial tuberosity | Medial surface of superior part of tibia | Tibial division of sciatic nerve (L5-S2) | Extends thigh at hip; flexes leg at knee and rotates it medially; with flexed hip and knee, extends trunk |
| Semimembranosus | Ischial tuberosity | Posterior part of medial condyle of tibia | Tibial division of sciatic nerve (L5-S2) | Extends thigh at hip; flexes leg at knee and rotates it medially; with flexed hip and knee, extends trunk |
| Biceps femoris | Long head: ischial tuberosity Short head: linea aspera and lateral supracondylar line of femur |
Lateral side of head of fibula; tendon at this site split by fibular collateral ligament of knee | Long head: tibial division of sciatic nerve (L5-S2) Short head: common fibular division of sciatic nerve (L5-S2) |
Flexes leg at knee and rotates it laterally; extends thigh at hip (e.g., when starting to walk) |

• Are largely flexors of the leg at the knee and extensors of the thigh at the hip (except the short head of the biceps femoris muscle).
• Are collectively referred to as the hamstrings; can also rotate the knee and are attached proximally to the ischial tuberosity (except the short head of biceps femoris).
• Are innervated by the tibial division of the sciatic nerve (except short head of biceps femoris, which is innervated by common fibular division).
• Are supplied by the deep (femoral) artery of the thigh and the femoral artery.
Femoral Triangle
The femoral triangle is located on the anterosuperior aspect of the thigh and is bound by the following structures (see Fig. 6-10):
• Inguinal ligament: forms the base of the triangle.
Inferiorly, a fascial sleeve extends from the apex of the femoral triangle and is continuous with the adductor (Hunter's) canal; the femoral vessels course through this canal and become the popliteal vessels posterior to the knee. The femoral triangle contains the femoral nerve and vessels as they pass beneath the inguinal ligament and gain access to the anterior thigh (see Fig. 6-10). Within this triangle is a fascial sleeve called the femoral sheath, a continuation of transversalis fascia and iliac fascia of the abdomen, that contains the femoral artery and vein and medially the lymphatics. Laterally the femoral nerve lies within the femoral triangle but outside this femoral sheath. The most medial portion of the femoral sheath is called the femoral canal and contains the lymphatics that drain through the femoral ring and into the external iliac lymph nodes. The femoral canal and ring are a weak point and the site for femoral hernias. The femoral ring is narrow, and consequently, femoral hernias may be difficult to reduce and may be prone to strangulation.
Femoral Artery
The femoral artery supplies the tissues of the thigh and then descends into the adductor canal to gain access to the popliteal fossa (Fig. 6-13 and Table 6-10). The superomedial aspect of the thigh also is supplied by the obturator artery. These vessels form anastomoses around the hip and, in the case of the femoral-popliteal artery, around the knee as well (see Fig. 6-13).
TABLE 6-10
| ARTERY | COURSE AND STRUCTURES SUPPLIED |
| Obturator | Arises from internal iliac artery (pelvis); has anterior and posterior branches; passes through obturator foramen |
| Femoral | Continuation of external iliac artery with numerous branches to perineum, hip, thigh, and knee |
| Deep artery of thigh | Arises from femoral artery; supplies hip and thigh |
Thigh in Cross Section
Cross sections of the thigh show the three compartments and their respective muscles and neurovascular elements (Fig. 6-14). Lateral, medial, and posterior intermuscular septae divide the thigh into the following three sections:
• Anterior compartment: contains muscles that primarily extend the leg at the knee and are innervated by the femoral nerve.
• Medial compartment: contains muscles that primarily adduct the thigh at the hip and are innervated largely by the obturator nerve.
• Posterior compartment: contains muscles that primarily extend the thigh at the hip and flex the leg at the knee and are innervated by the sciatic nerve (tibial portion).
Refer to the muscle tables to note several exceptions to these general divisions. However, learning the primary action and general innervation of the muscles by functional compartments will help you organize your study. Also, note that the large sciatic nerve usually begins to separate into its two component nerves—the tibial nerve and the common fibular nerve—in the thigh, although this separation may occur proximally in the gluteal region in some cases.
6 Leg
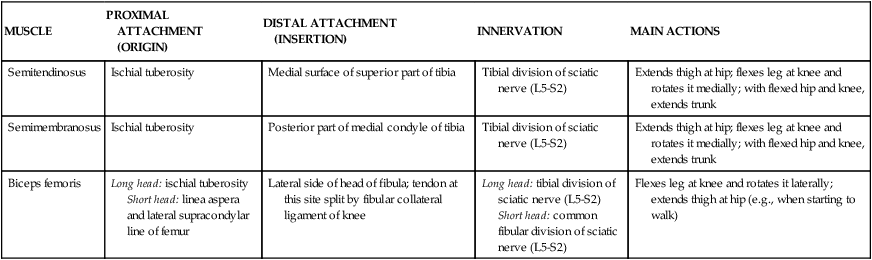
Bones
The bones of the leg (defined as knee to ankle) are the medially placed tibia and lateral fibula (Fig. 6-15 and Table 6-11). The tibia is weight-bearing in the leg, and the two bones are joined by a fibrous interosseous membrane. The tibia is subcutaneous from the knee to the ankle (our shin) and vulnerable to injury along its length. The fibula functions primarily for muscle attachments, forms part of the ankle joint, and acts as a pulley for the fibularis longus and fibularis brevis muscle tendons.
TABLE 6-11
Features of the Tibia and Fibula
| FEATURE | CHARACTERISTICS |
| Tibia | |
| Long bone | Large, weight-bearing bone |
| Proximal facets | Large plateau for articulation with femoral condyles |
| Tibial tuberosity | Insertion site for patellar ligament |
| Inferior articular surface | Surface for cupping talus at ankle joint |
| Medial malleolus | Prominence on medial aspect of ankle |
| Fibula | |
| Long bone | Slender bone, primarily for muscle attachment |
| Neck | Possible damage to common fibular nerve if fracture occurs here |
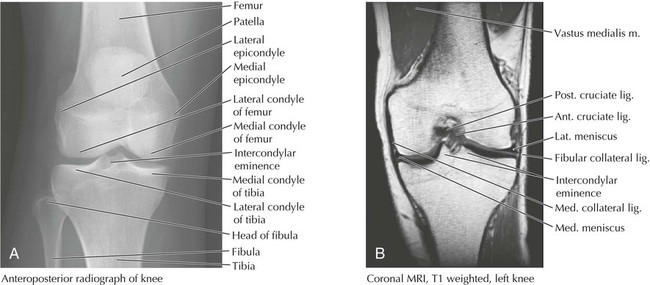
Knee Joint
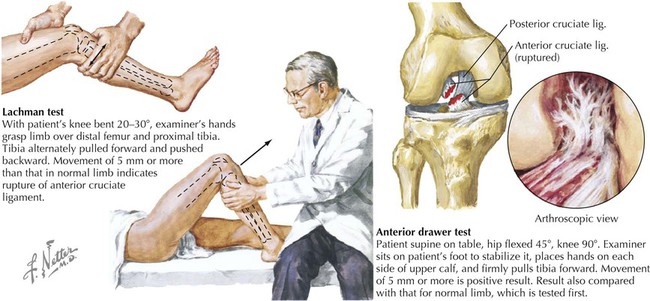
The knee is the most sophisticated joint in the body and the largest of the synovial joints. It participates in flexion, extension, and some gliding and rotation when flexed. With full extension, the femur rotates medially on the tibia, the supporting ligaments tighten, and the knee is locked into position. The knee consists of the articulation between the femur and the tibia (biaxial condylar synovial joint) and between the patella and the femur.
Features of the knee joint are shown in Figures 6-16 (muscle tendon support), 6-17 and 6-19 (ligaments), 6-18 (radiographs), and 6-19 (bursae) and are summarized in Tables 6-12 and 6-13. Because of the number of muscle-tendon units running across the knee joint, several bursae protect the underlying structures from friction (Fig. 6-19). The first four of the bursae listed in Table 6-14 also communicate with the synovial cavity of the knee joint. The vascular supply to the knee primarily arises from genicular branches of the popliteal artery, the inferior continuation of the femoral artery (Fig. 6-13).
TABLE 6-12
Muscle Tendon Support of the Knee
| MUSCLE AND TENDON | COMMENT |
| Lateral Aspect | |
| Biceps femoris | Posterolateral support, attaching to fibular head |
| Gastrocnemius (lateral) | Support somewhat more posteriorly |
| Iliotibial tract | Lateral support and stabilization |
| Popliteus | Located posterolaterally beneath the fibular collateral ligament |
| Medial Aspect | |
| Semimembranosus | Posteromedial support |
| Gastrocnemius (medial) | Support somewhat more posteriorly |
| Pes anserinus | Semitendinosus, gracilis, and sartorius (looks like a goose's foot) tendons, attaching to medial tibial condyle |

TABLE 6-13
| LIGAMENT | ATTACHMENT | COMMENT |
| Knee (Biaxial Condylar Synovial) Joint | ||
| Capsule | Surrounds femoral and tibial condyles and patella | Is fibrous, weak (offers little support); flexion, extension, some gliding and medial rotation |
| Extracapsular Ligaments | ||
| Tibial collateral | Medial femoral epicondyle to medial tibial condyle | Limits extension and abduction of leg; attached to medial meniscus |
| Fibular collateral | Lateral femoral epicondyle to fibular head | Limits extension and adduction of leg; overlies popliteus tendon |
| Patellar | Patella to tibial tuberosity | Acts in extension of quadriceps tendon |
| Arcuate popliteal | Fibular head to capsule | Passes over popliteus muscle |
| Oblique popliteal | Semimembranosus tendon to posterior knee | Limits hyperextension and lateral rotation |
| Intracapsular Ligaments | ||
| Medial meniscus | Interarticular area of tibia, lies over medial facet, attached to tibial collateral | Is semicircular (C-shaped); acts as cushion; often torn |
| Lateral meniscus | Interarticular area of tibia, lies over lateral facet | Is more circular and smaller than medial meniscus; acts as cushion |
| Anterior cruciate | Anterior intercondylar tibia to lateral femoral condyle | Prevents posterior slipping of femur on tibia; torn in hyperextension |
| Posterior cruciate | Posterior intercondylar tibia to medial femoral condyle | Prevents anterior slipping of femur on tibia; shorter and stronger than anterior cruciate |
| Transverse | Anterior aspect of menisci | Binds and stabilizes menisci |
| Posterior meniscofemoral (of Wrisberg) | Posterior lateral meniscus to medial femoral condyle | Is strong |
| Patellofemoral (Biaxial Synovial Saddle) Joint | ||
| Quadriceps tendon | Muscles to superior patella | Is part of extension mechanism |
| Patellar | Patella to tibial tuberosity | Acts in extension of quadriceps tendon; patella stabilized by medial and lateral ligament (retinaculum) attachment to tibia and femur |
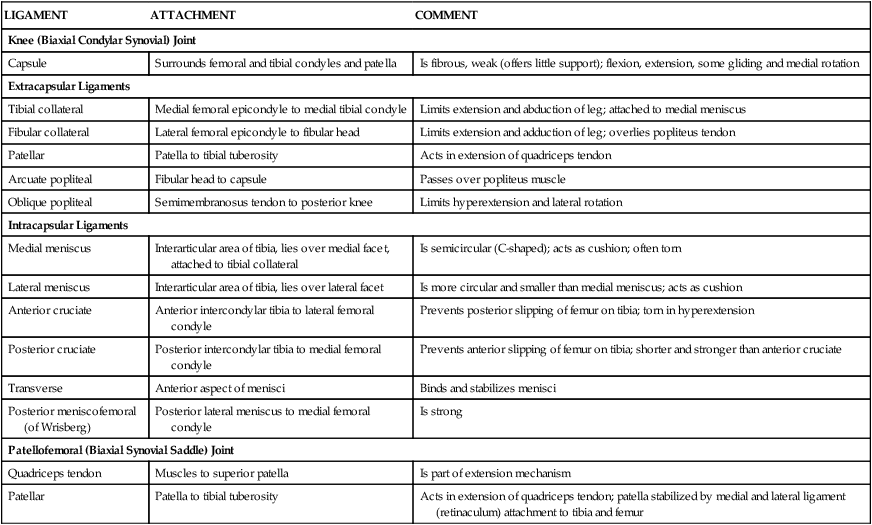
TABLE 6-14
Features of the Knee Joint Bursae
| BURSA | LOCATION |
| Suprapatellar | Between quadriceps tendon and femur |
| Popliteus | Between popliteus tendon and lateral tibial condyle |
| Anserine | Between pes anserinus and tibia and tibial collateral ligament |
| Subtendinous | Deep to heads of the gastrocnemius muscles |
| Semimembranosus | Deep to the tendon of the semimembranosus muscle |
| Prepatellar | Between skin and patella |
| Subcutaneous infrapatellar | Between skin and tibia |
| Deep infrapatellar | Between patellar ligament and tibia |
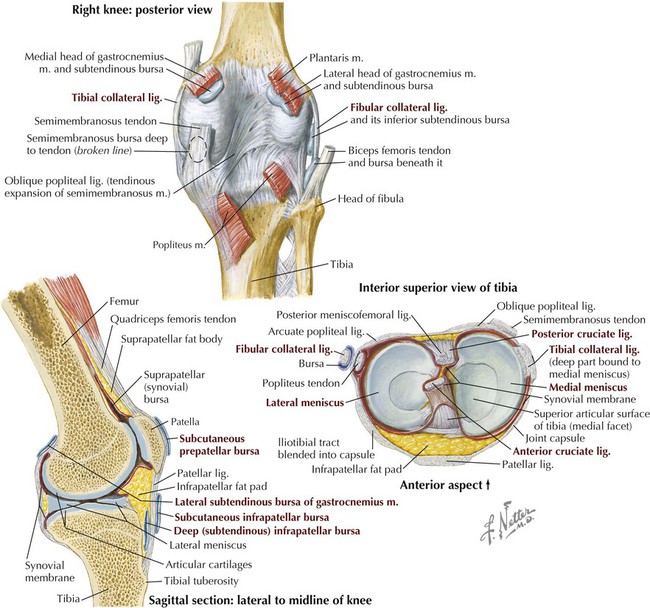
The innervation to the knee joint is via articular branches from the femoral, obturator, tibial, and common fibular nerves.
The proximal (superior) tibiofibular joint is a plane synovial joint between the fibular head and the lateral condyle of the tibia (Fig. 6-20). The joint is stabilized by a wider and stronger anterior ligament and a narrow weaker posterior ligament; this joint allows for some minimal gliding movement.
Popliteal Fossa
The popliteal fossa is a “diamond-shaped” region behind the knee and contains the popliteal vessels and the tibial and common fibular nerves (Fig. 6-21). This fossa marks the transition region between the thigh and the leg, where the vascular components of the thigh pass to the flexor side of the knee joint. (At most joints, the neurovascular bundles pass on the flexor side of the joint.) The superior margins of this diamond-shaped fossa are formed medially by the distal portions of the semitendinosus and semimembranosus muscles and laterally by the distal end of the long head of the biceps femoris muscle. The lower margins of the diamond are formed medially by the medial head of the gastrocnemius muscle and laterally by the plantaris and lateral head of the gastrocnemius muscles (see Figs. 6-12 and 6-21). The small saphenous vein courses subcutaneously upward toward the knee in the midline of the calf and drains into the popliteal vein (see Fig. 6-2).
Posterior Compartment Leg Muscles, Vessels, and Nerves
The posterior compartment leg muscles are arranged into a superficial group (gastrocnemius, plantaris, soleus) and a deep group (remaining posterior compartment muscles). These muscles exhibit the following general features (Fig. 6-21 and Table 6-15):
TABLE 6-15
Posterior Compartment Leg Muscles and Nerves
| MUSCLE | PROXIMAL ATTACHMENT (ORIGIN) | DISTAL ATTACHMENT (INSERTION) | INNERVATION | MAIN ACTIONS |
| Gastrocnemius | Lateral head: lateral aspect of lateral condyle of femur Medial head: popliteal surface of femur, superior to medial condyle |
Posterior surface of calcaneus via calcaneal tendon | Tibial nerve (S1-S2) | Plantarflexes foot at ankle; raises heel during walking; flexes leg at knee joint |
| Soleus | Posterior aspect of head of fibula, superior fourth of posterior surface of fibula, soleal line and medial border of tibia | Posterior surface of calcaneus via calcaneal tendon | Tibial nerve (S1-S2) | Plantarflexes foot at ankle; steadies leg on foot |
| Plantaris | Inferior end of lateral supracondylar line of femur and oblique popliteal ligament | Posterior surface of calcaneus via calcaneal tendon | Tibial nerve (L5-S1) | Weakly assists gastrocnemius in plantarflexing foot at ankle and flexing knee |
| Popliteus | Lateral condyle of femur and lateral meniscus | Posterior surface of tibia, superior to soleal line | Tibial nerve (L4-S1) | Weakly flexes leg at knee and unlocks it (rotates femur) |
| Flexor hallucis longus | Inferior two thirds of posterior surface of fibula and inferior interosseous membrane | Base of distal phalanx of great toe (big toe) | Tibial nerve (L5-S2) | Flexes great toe at all joints and plantarflexes foot at ankle; supports longitudinal arches of foot |
| Flexor digitorum longus | Medial part of posterior surface of tibia inferior to soleal line, and from fascia covering tibialis posterior | Bases of distal phalanges of lateral four digits | Tibial nerve (L5-S1) | Flexes lateral four digits and plantarflexes foot at ankle; supports longitudinal arches of foot |
| Tibialis posterior | Interosseous membrane, posterior surface of tibia inferior to soleal line, and posterior surface of fibula | Tuberosity of navicular, cuneiform, and cuboid and bases of metatarsals 2, 3, and 4 | Tibial nerve (L4-L5) | Plantarflexes foot at ankle and inverts foot |
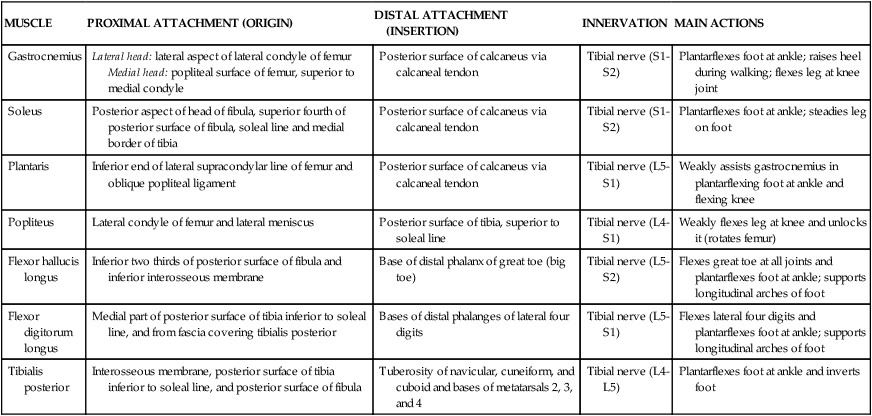
• Are primarily flexors of the foot at the ankle (plantarflexion) and flexors of the toes.
• Several can flex the leg at the knee or invert the foot.
• Are innervated by the tibial nerve.
• Are supplied by the posterior tibial artery (the popliteal artery divides into the anterior and posterior tibial arteries) with some supply from the fibular artery (a branch of the posterior tibial artery).
Anterior Compartment Leg Muscles, Vessels, and Nerves
The muscles of the anterior compartment exhibit the following features (Fig. 6-22 and Table 6-16):
TABLE 6-16
Anterior Compartment Leg Muscles and Nerves
| MUSCLE | PROXIMAL ATTACHMENT (ORIGIN) | DISTAL ATTACHMENT (INSERTION) | INNERVATION | MAIN ACTIONS |
| Tibialis anterior | Lateral condyle and superior half of lateral tibia and interosseous membrane | Medial and inferior surfaces of medial cuneiform and base of 1st metatarsal | Deep fibular nerve (L4-L5) | Dorsiflexes foot at ankle and inverts foot |
| Extensor hallucis longus | Middle part of anterior surface of fibula and interosseous membrane | Dorsal aspect of base of distal phalanx of great toe | Deep fibular nerve (L5-S1) | Extends great toe and dorsiflexes foot at ankle |
| Extensor digitorum longus | Lateral condyle of tibia and superior  of anterior surface of interosseous membrane and fibula of anterior surface of interosseous membrane and fibula |
Middle and distal phalanges of lateral four digits | Deep fibular nerve (L5-S1) | Extends lateral four digits and dorsiflexes foot at ankle |
| Fibularis tertius | Inferior third of anterior surface of fibula and interosseous membrane | Dorsum of base of 5th metatarsal | Deep fibular nerve (L5-S1) | Dorsiflexes foot at ankle and aids in eversion of foot |
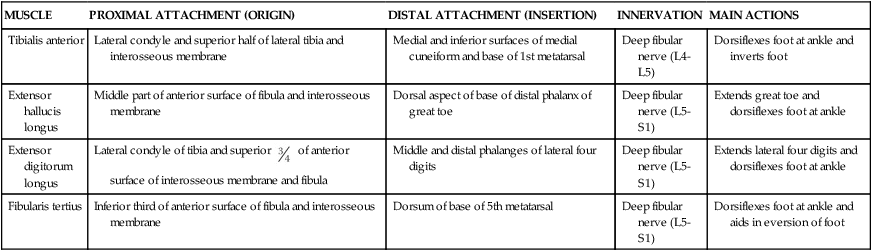
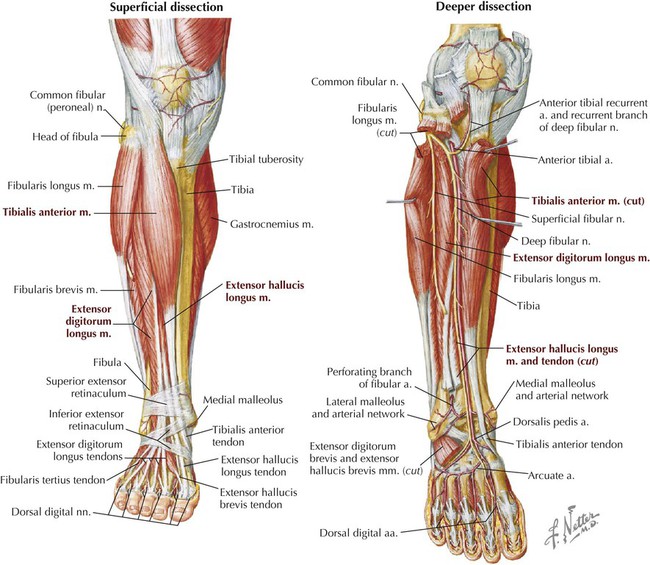
• Are primarily extensors of the foot at the ankle (dorsiflexion) and extensors of the toes.
• Several can invert the foot, and one muscle (fibularis tertius) can weakly evert the foot.
• Are innervated by the deep fibular nerve (the common fibular nerve divides into the superficial and deep branches).
Lateral Compartment Leg Muscles, Vessels, and Nerves
The two muscles of the lateral compartment exhibit the following features (Fig. 6-23 and Table 6-17):
TABLE 6-17
Lateral Compartment Leg Muscles and Nerves
| MUSCLE | PROXIMAL ATTACHMENT (ORIGIN) | DISTAL ATTACHMENT (INSERTION) | INNERVATION | MAIN ACTIONS |
| Fibularis longus | Head and superior  of lateral surface of fibula of lateral surface of fibula |
Base of 1st metatarsal and medial cuneiform | Superficial fibular nerve (L5-S2) | Everts foot and weakly plantarflexes foot at ankle |
| Fibularis brevis | Inferior  of lateral surface of fibula of lateral surface of fibula |
Dorsal surface of tuberosity on lateral side of 5th metatarsal | Superficial fibular nerve (L5-S2) | Everts foot and weakly plantarflexes foot at ankle |
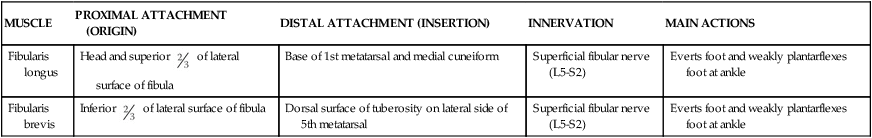
• Are primarily able to evert the foot, and can weakly plantarflex the foot at the ankle.
• Are innervated by the superficial fibular nerve.
• Are supplied by the fibular artery, a branch of the posterior tibial artery (see Fig. 6-21).
Leg in Cross Section
The interosseous membrane and intermuscular septae divide the leg into three compartments. The posterior compartment is further subdivided into the superficial and deep compartments. Moreover, the leg is ensheathed in a tight deep fascia, and some of the underlying muscle fibers actually attach to this fascial sleeve. The compartments may be summarized as follows (Fig. 6-24):
• Posterior compartment: muscles that plantarflex and invert the foot at the ankle and flex the toes, are innervated by the tibial nerve, and are supplied largely by the posterior tibial artery.
• Anterior compartment: muscles that dorsiflex (extend) and invert/evert the foot at the ankle and extend the toes, are innervated by the deep fibular nerve, and are supplied by the anterior tibial artery.
• Lateral compartment: muscles that evert the foot at the ankle and weakly plantarflex, are innervated by the superficial fibular nerve, and are supplied by the fibular artery.
7 Ankle and Foot
Bones and Joints
The ankle connects the foot to the leg and is composed of seven tarsal bones arranged in a proximal group (talus and calcaneus), intermediate group (navicular), and distal group (cuboid and three cuneiforms). The foot includes five metatarsals and the five digits and their phalanges (Figs. 6-25 and 6-26 and Table 6-18).
TABLE 6-18
Features of the Bones of the Ankle and Foot
| STRUCTURE | CHARACTERISTICS |
| Talus (ankle bone)* | Transfers weight from tibia to foot; no muscle attachment |
| Trochlea | Articulates with tibia and fibula |
| Head | Articulates with navicular bone |
| Calcaneus (heel bone)* | Articulates with talus superiorly and cuboid anteriorly |
| Sustentaculum tali | Medial shelf that supports talar head |
| Navicular* | Boat shaped, between talar head and three cuneiforms |
| Tuberosity | If large, can cause medial pain in tight-fitting shoe |
| Cuboid* | Most lateral tarsal bone |
| Groove | For fibularis longus tendon |
| Cuneiforms* | Three wedge-shaped bones |
| Metatarsals | |
| Numbered 1 to 5, from great toe to little toe | Possess base, shaft, and head Fibularis brevis tendon inserts on 5th metatarsal |
| Two sesamoid bones | Associated with flexor hallucis brevis tendons |
| Phalanges | |
| Three for each digit except great toe | Possess base, shaft, and head Termed proximal, middle, and distal Stubbed 5th toe common injury |

*Tarsal bones.
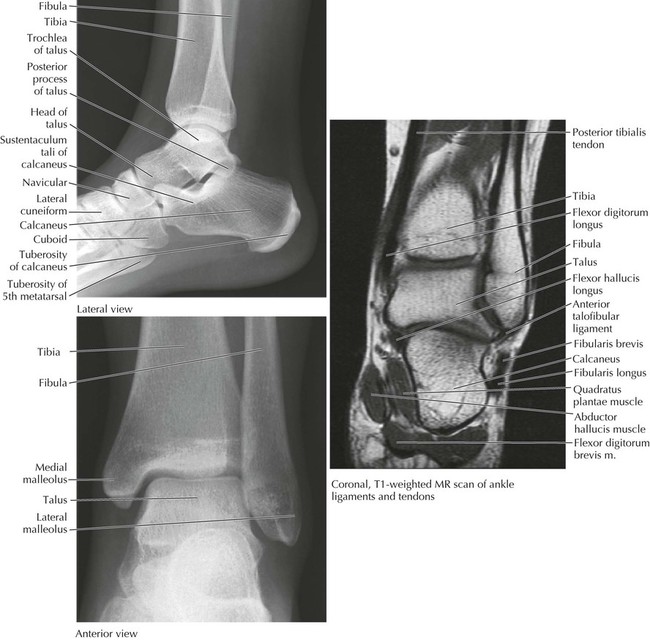
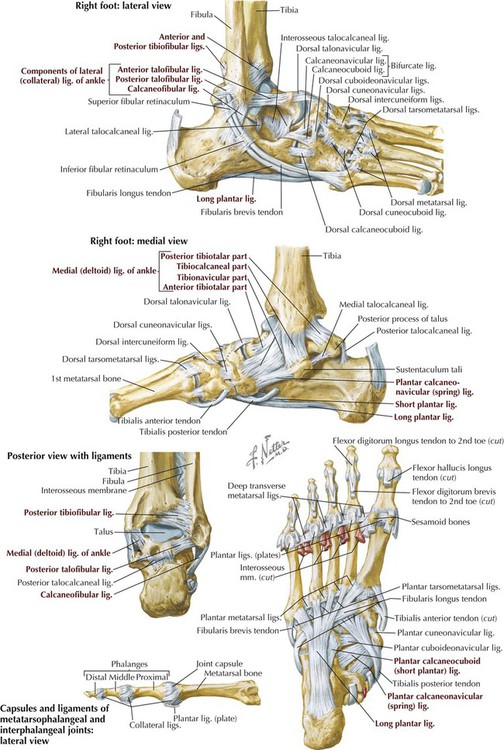
The ankle (talocrural) joint is a uniaxial synovial hinge joint between the talus and the tibia (inferior surface and medial malleolus) and fibula (lateral malleolus). This combination forms a mortise that is then covered by the capsule of the joint and reinforced medially and laterally by ligaments. The ankle joint functions primarily in plantarflexion and dorsiflexion. Intertarsal, tarsometatarsal, intermetatarsal, metatarsophalangeal, and interphalangeal joints complete the ankle and foot joint complex (Fig. 6-27 and Table 6-19). A variety of movements are possible at these joints, and the ankle and foot can provide a stable but flexible platform for standing, walking, and running. Because of the shape of the talus (the anterior portion of its superior articular aspect is wider), the ankle is more stable when dorsiflexed than when plantarflexed.
TABLE 6-19
Features of the Joints and Ligaments of the Ankle and Foot
| LIGAMENT | ATTACHMENT | COMMENT |
| Distal Tibiofibular (Fibrous [Syndesmosis]) Joint | ||
| Anterior tibiofibular | Anterior distal tibia and fibula | Runs obliquely |
| Posterior tibiofibular | Posterior distal tibia and fibula | Is weaker than anterior ligament |
| Inferior transverse | Medial malleolus to fibula | Is deep continuation of posterior ligament |
| Talocrural (Uniaxial Synovial Hinge [Ginglymus]) Joint | ||
| Capsule | Tibia and fibula to talus | Functions in plantarflexion and dorsiflexion |
| Medial (deltoid) | Medial malleolus to talus, calcaneus, and navicular | Limits eversion of foot; maintains medial long arch; has four parts |
| Lateral (collateral) | Lateral malleolus to talus and calcaneus | Is weak and often sprained; resists inversion of foot; has three parts |
| Intertarsal Joints (Next Three Joints) | ||
| Talocalcaneal (Subtalar Plane Synovial) Joints | ||
| Capsule | Margins of articulation | Functions in inversion and eversion |
| Talocalcaneal | Talus to calcaneus | Has medial, lateral, and posterior parts |
| Interosseous talocalcaneal | Talus to calcaneus | Is strong; binds bones together |
| Talocalcaneonavicular (Partial Ball-and-Socket Synovial) Joint | ||
| Capsule | Encloses part of joint | Functions in gliding and rotational movements |
| Plantar calcaneonavicular | Sustentaculum tali to navicular | Is strong plantar support for head of talus (called spring ligament) |
| Dorsal talonavicular | Talus to navicular | Is dorsal support to talus |
| Calcaneocuboid (Plane Synovial) Joint | ||
| Capsule | Encloses joint | Functions in inversion and eversion |
| Calcaneocuboid | Calcaneus to cuboid | Are dorsal, plantar (short plantar, strong), and long plantar ligaments |
| Tarsometatarsal (Plane Synovial) Joints | ||
| Capsule | Encloses joint | Functions in gliding or sliding movements |
| Tarsometatarsal | Tarsals to metatarsals | Are dorsal, plantar, interosseous ligaments |
| Intermetatarsal (Plane Synovial) Joints | ||
| Capsule | Base of metatarsals | Provides little movement, supports transverse arch |
| Intermetatarsal | Adjacent metatarsals | Are dorsal, plantar, interosseous ligaments |
| Deep transverse | Adjacent metatarsals | Connect adjacent heads |
| Metatarsophalangeal (Multiaxial Condyloid Synovial) Joints | ||
| Capsule | Encloses joint | Functions in flexion, extension, some abduction and adduction, and circumduction |
| Collateral | Metatarsal heads to base of proximal phalanges | Are strong ligaments |
| Plantar (plates) | Plantar side of capsule | Are part of weight-bearing surface |
| Interphalangeal (Uniaxial Hinge Synovial) Joints | ||
| Capsule | Encloses each joint | Functions in flexion and extension |
| Collateral | Head of one to base of other | Support the capsule |
| Plantar (plates) | Plantar side of capsule | Support the capsule |
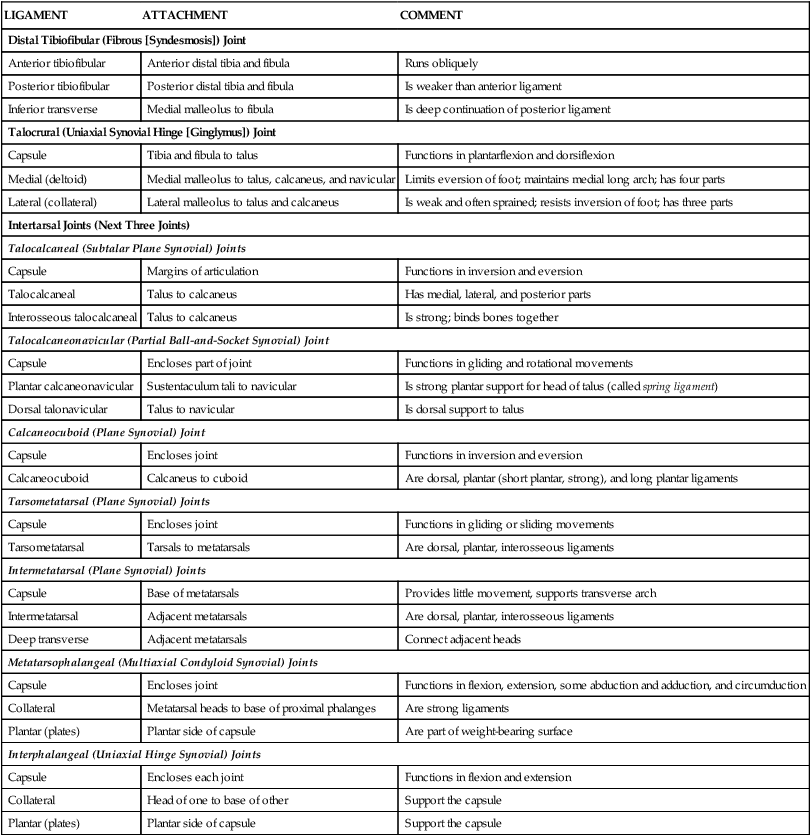
Cuboideonavicular, cuneonavicular, intercuneiform, and cuneocuboid joints: dorsal, plantar, and interosseous ligaments are present, but little movement occurs at these joints, and they have little clinical significance.
The bones of the foot do not lie in a flat plane but are arranged to form the following structures (see Fig. 6-25):
• Longitudinal arch: extends from the posterior calcaneus to the metatarsal heads; is higher medially (medial longitudinal arch) than laterally (lateral longitudinal arch).
• Transverse arch: extends from medial to lateral across the cuboid, cuneiforms, and base of the metatarsals; is higher medially than laterally.
These arches are supported by muscles and ligaments. Supporting muscles include the tibialis anterior, tibialis posterior, and fibularis longus. Ligaments include the plantar calcaneonavicular (spring) ligament, plantar calcaneocuboid (short plantar) ligament, and long plantar ligament. The plantar aponeurosis also provides some support.
Synovial sheaths provide protection and lubrication for muscle tendons passing from the leg to the foot. Various fibrous bands (retinacula) tether the tendons at the ankle (Fig. 6-28):
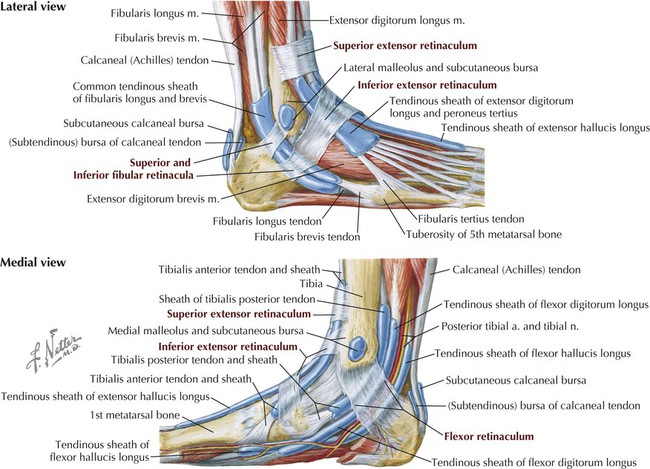
• Flexor retinaculum: medial malleolus to calcaneus (plantarflexor tendons)
• Extensor retinaculum: superior and inferior bands (dorsiflexor tendons)
• Fibular retinacula: superior and inferior bands (fibularis tendons of the lateral compartment)
Muscles, Vessels, and Nerves of the Dorsum of the Foot
The dorsum of the foot consists of two intrinsic muscles, the extensor digitorum brevis and the extensor hallucis brevis. These muscles function to extend the toes and are supplied by the anterior tibial artery from the leg via its dorsalis pedis branch (Fig. 6-29). A dorsal venous arch drains most of the blood from the foot, ultimately carrying the blood to the medially located great saphenous vein or laterally and posteriorly to the small saphenous vein (see Fig. 6-2). The deep fibular nerve, passing from the leg into the foot, innervates the two intrinsic muscles on the dorsum of the foot (see Fig. 6-29).
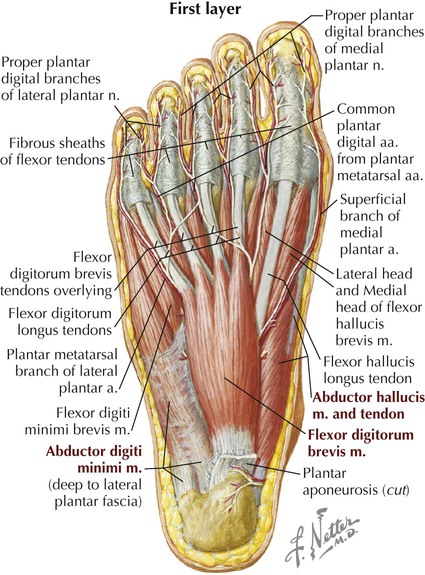
Muscles, Vessels, and Nerves of the Sole of the Foot
The sole of the foot is protected by a thick layer of the deep fascia called the plantar aponeurosis, which extends from the calcaneal tuberosity to individual bands of fascia that attach to the toes anteriorly (Fig. 6-30).
Beneath the plantar aponeurosis, the intrinsic muscles of the foot are arranged into four layers, shown in sequence in Figures 6-31, 6-32, and 6-33 and Tables 6-20, 6-21, and 6-22. These muscles functionally assist the long muscle tendons that pass from the leg into the foot. The lumbrical muscles and the interosseus muscles have the same actions as their counterparts in the hand. The lumbricals flex the metatarsophalangeal joints and extend the interphalangeal joints via the extensor hood. The plantar interossei adduct (PAD) the digits (2-4) and help flex the metatarsophalangeal joints, while the dorsal interossei abduct (DAB) the digits and help flex the metatarsophalangeal joints. All these intrinsic muscles of the sole are innervated by the medial or lateral plantar nerves (from the tibial nerve) (Tables 6-20, 6-21, and 6-22) and are supplied with blood from the medial and lateral plantar arteries (from the posterior tibial artery). Pulses may be palpated between the medial malleolus and the heel (posterior tibial artery) and on the dorsum of the foot just lateral to the extensor hallucis longus tendon (dorsalis pedis artery).
TABLE 6-20
Muscles of the Sole: First Layer
| MUSCLE | PROXIMAL ATTACHMENT (ORIGIN) | DISTAL ATTACHMENT (INSERTION) | INNERVATION | MAIN ACTIONS |
| Abductor hallucis | Medial tubercle of tuberosity of calcaneus, flexor retinaculum, and plantar aponeurosis | Medial side of base of proximal phalanx of 1st digit | Medial plantar nerve (S2-S3) | Abducts and flexes great toe |
| Flexor digitorum brevis | Medial tubercle of tuberosity of calcaneus, plantar aponeurosis, and intermuscular septa | Both sides of middle phalanges of lateral four digits | Medial plantar nerve (S2-S3) | Flexes lateral four digits |
| Abductor digiti minimi | Medial and lateral tubercles of tuberosity of calcaneus, plantar aponeurosis, and intermuscular septa | Lateral side of base of proximal phalanx of 5th digit | Lateral plantar nerve (S2-S3) | Abducts and flexes little toe |
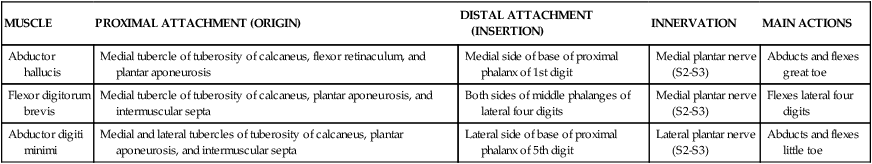
TABLE 6-21
Muscles of the Sole: Second and Third Layers
| MUSCLE | PROXIMAL ATTACHMENT (ORIGIN) | DISTAL ATTACHMENT (INSERTION) | INNERVATION | MAIN ACTIONS |
| Quadratus plantae | Medial surface and lateral margin of plantar surface of calcaneus | Posterolateral margin of tendon of flexor digitorum longus | Lateral plantar nerve (S1-S3) | Assist flexor digitorum longus in flexing lateral four digits |
| Lumbricals | Tendons of flexor digitorum longus | Medial aspect of dorsal expansion over lateral four digits | Medial one: medial plantar nerve Lateral three: lateral plantar nerve |
Flex metatarsophalangeal joints and extend interphalangeal joints of lateral four digits |
| Flexor hallucis brevis | Plantar surfaces of cuboid and lateral cuneiforms | Both sides of base of proximal phalanx of 1st digit | Medial plantar nerve (S1-S2) | Flexes proximal phalanx of great toe |
| Adductor hallucis | Oblique head: bases of metatarsals 2-4 Transverse head: plantar ligaments of metatarsophalangeal joints of digits 3-5 |
Tendons of both heads attach to lateral side of base of proximal phalanx of 1st digit | Deep branch of lateral plantar nerve (S2-S3) | Adducts great toe; assists in maintaining transverse arch of foot |
| Flexor digiti minimi brevis | Base of 5th metatarsal | Lateral base of proximal phalanx of 5th digit | Superficial branch of lateral plantar nerve (S2-S3) | Flexes proximal phalanx of little toe, thereby assisting with its flexion |
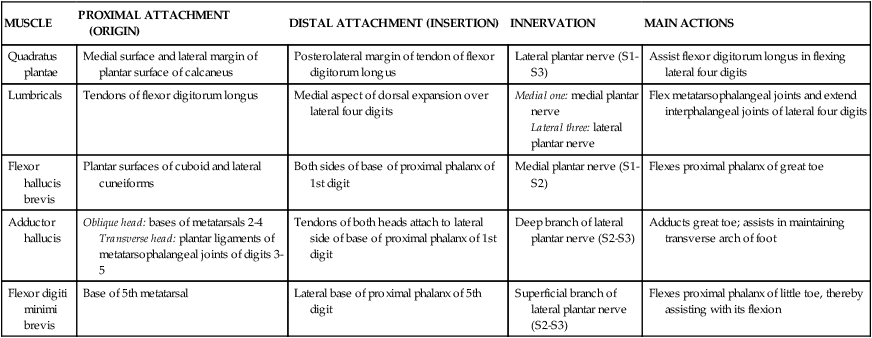
TABLE 6-22
Muscles of the Sole: Fourth Layer
| MUSCLE | PROXIMAL ATTACHMENT (ORIGIN) | DISTAL ATTACHMENT (INSERTION) | INNERVATION | MAIN ACTIONS |
| Plantar interossei (three muscles) | Bases and medial sides of metatarsals 3-5 | Medial sides of bases of proximal phalanges of digits 3-5 | Lateral plantar nerve (S2-S3) | Adduct digits 2-4, flex metatarsophalangeal joints, and extend phalanges |
| Dorsal interossei (four muscles) | Adjacent sides of metatarsals 1-5 | First: medial side of proximal phalanx of second digit Second to fourth: lateral sides of digits 2-4 |
Lateral plantar nerve (S2-S3) | Abduct digits 2-4, flex metatarsophalangeal joints, and extend phalanges |

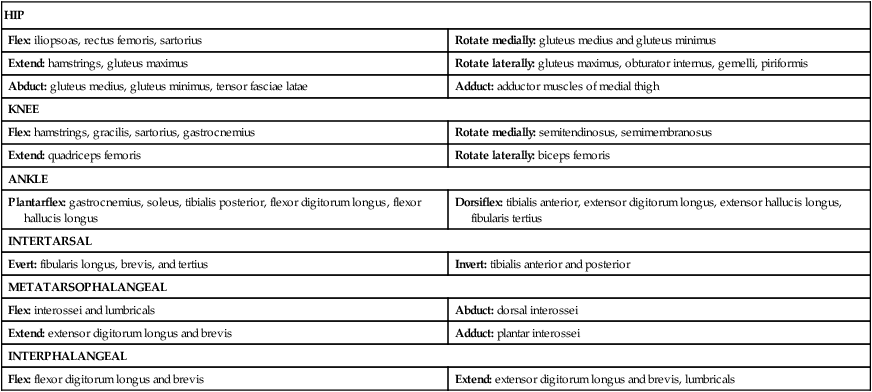
8 Lower Limb Muscle Summary and Gait
Table 6-23 summarizes the actions of major muscles on the joints. The list is not exhaustive and highlights only major muscles responsible for each movement; the separate muscle tables provide more detail. Realize that most joints move because of the action of multiple muscles working on that joint, and that this list only focuses on the more important of these muscles for each joint.
TABLE 6-23
Summary of Actions of Major Lower Limb Muscles
| HIP | |
| Flex: iliopsoas, rectus femoris, sartorius | Rotate medially: gluteus medius and gluteus minimus |
| Extend: hamstrings, gluteus maximus | Rotate laterally: gluteus maximus, obturator internus, gemelli, piriformis |
| Abduct: gluteus medius, gluteus minimus, tensor fasciae latae | Adduct: adductor muscles of medial thigh |
| KNEE | |
| Flex: hamstrings, gracilis, sartorius, gastrocnemius | Rotate medially: semitendinosus, semimembranosus |
| Extend: quadriceps femoris | Rotate laterally: biceps femoris |
| ANKLE | |
| Plantarflex: gastrocnemius, soleus, tibialis posterior, flexor digitorum longus, flexor hallucis longus | Dorsiflex: tibialis anterior, extensor digitorum longus, extensor hallucis longus, fibularis tertius |
| INTERTARSAL | |
| Evert: fibularis longus, brevis, and tertius | Invert: tibialis anterior and posterior |
| METATARSOPHALANGEAL | |
| Flex: interossei and lumbricals | Abduct: dorsal interossei |
| Extend: extensor digitorum longus and brevis | Adduct: plantar interossei |
| INTERPHALANGEAL | |
| Flex: flexor digitorum longus and brevis | Extend: extensor digitorum longus and brevis, lumbricals |
Gait
The gait (walking) cycle involves both a swing phase and a stance phase (when the foot is weight-bearing). Additionally, walking produces pelvic tilt and rotation, hip and knee flexion and extension, and a smoothly coordinated interaction among the pelvis, hip, knee, ankle, and foot.
The swing phase occurs from pre-swing toe-off (TO) position, in which the push-off of the toes occurs by the powerful plantarflexion of the ankle and the forward swing of the hips. The “ball” of the big toe, with its two sesamoid bones, provides the last push needed to accelerate into the swing phase. The foot then accelerates through the initial swing to the midswing (MSW) and terminal swing phase. (Follow the girl's right lower limb in images 5 to 7 of Figure 6-34.) When the right foot is off the ground, drooping of the pelvis (pelvic dip or tilt) to the unsupported side (right side) is prevented by the action of hip abductors, primarily the gluteus medius and minimus muscles. Paralysis of these muscles, as from polio or pelvic fractures that damage the superior gluteal nerves, can lead to a “gluteal or pelvic dip” and a positive Trendelenburg sign.
The limb then decelerates to the heel strike (HS) phase when the foot meets the ground (image 8 in Fig. 6-34). The stance phase occurs from the HS position, to the flat foot (FF) position, to the midstance (MST) phase, and then the heel-off (HO) (forward thrust to TO position and, correspondingly, the HS position for the opposite foot; follow the girl's right lower limb in images 1 to 4 in Fig. 6-34). Table 6-24 summarizes the major muscles involved in the gait cycle.
TABLE 6-24
Major Muscles Involved in the Gait Cycle
| GAIT CYCLE | MUSCLE ACTIONS |
| Toe-off (TO) to midswing (MSW) | Hip flexors accelerate the thigh, knee is flexed, and foot is dorsiflexed to clear the ground (swing phase). |
| MSW to heel strike (HS) | Knee is extended rapidly, and foot is dorsiflexed (swing phase). |
| HS to flat foot (FF) | Hip is flexed, knee is extended, and ankle is in neutral position, but foot then plantarflexes flat on the ground, and limb extensors stabilize the weight-bearing joints (stance phase). |
| FF to midstance (MST) | Body moves forward, extensors support limb while other limb is in the swing phase, and hip abductors control pelvic tilt (stance phase). |
| MST to heel-off (HO) | Body continues forward; plantarflexors contract as weight moves from heel to metatarsal heads, and hip abductors control pelvic tilt (stance phase). |
| HO to TO | Push-off as opposite heel strikes the ground, plantarflexors exert thrust, and knee flexes; foot goes into dorsiflexed position at beginning of HO to plantarflexed as toes push off at TO, and hip abductors relax while hip flexors ready for the swing phase (stance phase). |
9 Lower Limb Artery and Vein Summary
Arteries of the Lower Limb
The abdominal aorta (1) gives rise to the left and right common iliac arteries (2). These arteries divide into internal and external iliac arteries (Fig. 6-35). The internal iliac artery generally supplies the pelvis, perineum, and gluteal regions, while the external iliac artery (3) passes deep to the inguinal ligament and into the thigh to become the femoral artery (4). The femoral artery gives off a deep artery of thigh (profunda femoris) (5) and then continues inferiorly by passing through the adductor hiatus to become the popliteal artery (6) posterior to the knee. The popliteal artery divides in the leg to give rise to the anterior tibial artery (7) and posterior tibial artery (9). The posterior tibial artery gives rise to the small fibular artery (10) and passes into the sole of the foot, where it divides into the medial plantar artery (11) and lateral plantar artery (12). The anterior tibial artery supplies the anterior compartment of the leg, the ankle, and continues onto the dorsum of the foot as the dorsal artery of the foot (dorsalis pedis) (8) (Fig. 6-35).
Anastomoses occur around the hip joint, largely supplied by the deep artery of thigh with contributions from several other arteries (e.g., branch from obturator artery). The knee and ankle joints also have a rich vascular supply by genicular arteries (knee), and malleolar and tarsal arteries (ankle). Many of these arteries have small muscular branches (not listed) to supply the muscles of the limb and nutrient arteries to the adjacent bones (not named). Arteriovenous (AV) anastomoses are direct connections between small arteries and veins, and usually are involved in cutaneous thermoregulation.
Major pulse points of the lower limb include:
• Femoral pulse: just inferior to the inguinal ligament.
• Popliteal pulse: felt deep behind the knee (very difficult to feel).
• Posterior tibial pulse: on medial aspect of the ankle as it passes through the tarsal tunnel posterior to the medial malleolus.
• Dorsalis pedis pulse (farthest pulse from the heart): felt just lateral to the flexor hallucis longus tendon when pressed against the intermediate cuneiform bone.
In the outline of arteries, major vessels often dissected in anatomy courses include the first-order arteries (in bold and numbered) and their second-order major branches. Only more detailed courses in anatomy will dissect the third-order or fourth-order arteries.
Veins of the Lower Limb
Note that the venous drainage of the lower limb begins largely on the dorsum of the foot, with venous blood returning proximally in both a superficial (1) and deep (2) venous pattern (Fig. 6-36). The small saphenous vein (3) drains most of the foot and then this same vein and the deep veins (2) drain the leg, both largely terminating in the popliteal vein (4). Variable connections between these veins are common, so the flow patterns should never be considered absolute; the pattern outlined details the major flow pattern from distal to proximal.
Genicular veins, draining into the popliteal vein, drain the arterial anastomosis around the knee joint. The great saphenous vein (5) courses up the medial aspect of the leg and medioanterior thigh to drain into the femoral vein (7). The great saphenous vein (5) receives tributaries from the superficial perineal structures (labia and clitoris/scrotum and penis) and lower anterior abdominal wall adjacent to the inguinal region. The deep vein of the thigh (profunda femoris) (6) drains the deep thigh structures (muscles and bone) and is a major tributary of the femoral vein (7). The femoral vein then drains into the external iliac vein, which combined with the internal iliac vein, forms the common iliac vein. This then drains into the inferior vena cava and the right atrium of the heart (Fig. 6-36).
In the human body, the venous system is the compliance system, and, at rest, about 65% of the blood resides in the low-pressure venous system. Veins generally are larger than their corresponding arteries and have thinner walls; often multiple veins accompany a single artery (the body has many more veins than arteries).
10 Lower Limb Nerve Summary
Femoral Nerve
The femoral nerve (L2-L4) innervates the muscles in the anterior compartment of the thigh, which are largely extensors of the leg at the knee (Fig. 6-37). The patellar tendon reflex (L3-L4) (knee extension) tests the integrity of this nerve. Injury to this nerve can lead to an inability to fully extend the knee unless one pushes on the anterior thigh with one's hand. Major cutaneous branches include the separate lateral cutaneous nerve of the thigh and, from the femoral nerve directly, the following:
• Anterior cutaneous branches to the anterior thigh
• Saphenous nerve (terminal branch of femoral) to medial knee, leg, and ankle
Obturator Nerve
The obturator nerve (L2-L4) innervates the muscles of the medial compartment of the thigh, which are largely adductors of the thigh at the hip (Fig. 6-38). The nerve divides into anterior and posterior branches on both sides of the obturator externus and adductor brevis muscles (the anterior and posterior branches, in effect, “scissors” these two muscles). A small field of cutaneous innervation exists on the medial thigh. Injury to this nerve usually occurs inside the pelvis and can lead to weakened adduction of the thigh.
Sciatic Nerve
The sciatic nerve (L4-S3) is the largest nerve in the body and is composed of the tibial and common fibular (peroneal) nerves (Fig. 6-39). The sciatic nerve innervates muscles of the posterior compartment of the thigh (tibial component), which are largely extensors of the thigh at the hip and flexors of the leg at the knee. It also innervates all muscles below the knee, via its tibial and common fibular components.
Tibial Nerve
The tibial nerve (L4-S3), the larger of the two components of the sciatic nerve, innervates muscles of the posterior compartment of the leg and all muscles of the plantar foot (Fig. 6-40). These muscles are largely plantarflexors, and some have an inversion function. A lesion to this nerve may result in the loss of plantarflexion and weakened inversion of the foot, and thus a shuffling gait. The calcaneal (Achilles) tendon reflex (S1-S2) (plantarflexion) tests this nerve.
Fibular Nerve
The common fibular nerve (L4-S2) innervates muscles of the lateral compartment of the leg (everts the foot) via its superficial branch, and muscles of the anterior compartment of the leg and dorsum of the foot via its deep branch (Fig. 6-41). These muscles are largely dorsiflexors. Footdrop and steppage gait (high stepping) may occur if this nerve or its deep branch is injured (see Clinical Focus 6-27). The common fibular nerve is most vulnerable to injury as it passes around the fibular neck.
Dermatomes
The spiral dermatome pattern of the lower limb is the result of its embryonic medial rotation. Because of the stability of the hip joint, the spiral dermatome pattern is similar to a barbershop pole. Considerable overlap and some variability in the dermatome pattern is to be expected. However, the following key dermatome regions are generally constant:
Zones of autonomous sensory testing and spinal cord levels involved in primary movements of the joints are illustrated in Figure 6-42.
11 Embryology
While the upper limb rotates 90 degrees laterally, the lower limb rotates about 90 degrees medially so that the knee and elbow are oriented about 180 degrees from each other (Fig. 6-43; see also Fig. 7-43). The thumb lies laterally in anatomical position, with the great toe medially. Knee, ankle, and toe flexor muscles are on the posterior aspect of the lower limb, and knee, ankle, and toe extensor muscles are on the ventral aspect. The hip is unaffected, so hip flexors are anterior and extensors are posterior. This limb rotation pattern produces a spiral (barbershop pole) arrangement of the dermatomes as one moves distally along the limb (Fig. 6-43). All the muscles of the lower limb are from hypaxial (hypomeres) embryonic ventral mesoderm (see Fig. 2-22) and are innervated by ventral rami and their respective lumbosacral nerves (gluteal, obturator, femoral, and sciatic).