Head and Neck
1 Introduction
The head and neck area offers a unique challenge for students because of the density of small neurovascular structures; the complexity of its bony features, especially the skull; and the compactness of its anatomy. The head protects the brain, participates in communication and expresses our emotions, and houses the special senses (sight, sound, balance, smell, and taste). The neck connects the head to the thorax and is the conduit for visceral structures passing cranially or caudally within tightly partitioned fascial sleeves.
The anatomy of the head is best understood if you view it as a series of interconnected compartments, which include the following:
• Cranium: contains the brain and its meningeal coverings.
• Orbits: contain the eye and the muscles that move the eye.
• Nasal cavities and paranasal sinuses: form the uppermost part of the respiratory system.
• Ears: contain the apparatus for hearing and balance.
• Oral cavity: forms the proximal end of the digestive tract.
The anatomy of the neck is composed of a series of concentric-like compartments that provide a conduit for structures passing to the head or thorax, as follows:
• Musculofascial: superficial compartment encompassing the outer boundary of the neck.
• Visceral: anterocentral compartment that contains the upper respiratory (pharynx, larynx, trachea) and gastrointestinal (GI) tract (pharynx, esophagus), and the thyroid, parathyroid, and thymus glands.
• Neurovascular: two anterolateral compartments that contain the common carotid artery, internal jugular vein, and vagus nerve; called the carotid sheath.
• Prevertebral: posterocentral compartment that contains the cervical vertebrae and the associated paravertebral muscles.
2 Surface Anatomy
The key surface features of the head and neck and include the following (Fig. 8-1):
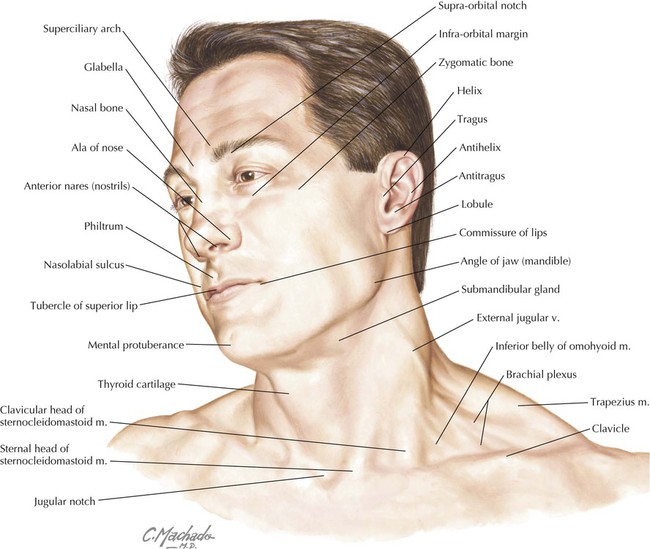
• Glabella: smooth prominence on the frontal bone above the root of the nose.
• Zygomatic bone: the cheekbone, which protrudes below the orbit and is vulnerable to fractures from facial trauma.
• Ear (auricle or pinna): skin-covered elastic cartilage with several consistent ridges, including the helix, antihelix, tragus, antitragus, and lobule.
• Philtrum: midline infranasal depression of the upper lip.
• Nasolabial sulcus: line between the nose and the corner of the lip.
• Thyroid cartilage: the laryngeal prominence (“Adam's apple”).
• Jugular (suprasternal) notch: midline depression between the two sternal heads of the sternocleidomastoid muscle.
3 Skull
The skull is composed of 22 bones (see Chapter 1). Eight of these bones form the cranium (neurocranium, which contains the brain and meninges), and 14 of these form the face (viscerocranium). There are seven associated bones: the auditory ossicles (three in each middle ear) and the unpaired hyoid bone (Fig. 8-2 and Table 8-1). Using your atlas and dry bone specimens, note the complexity of the maxillary, temporal, and sphenoid bones. These bones are in close association with many of the cranial nerves and encase portions of many of our special senses—balance, hearing, smell, sight, and even taste—as the maxillae form a portion of the oral cavity.
TABLE 8-1
| BONE | DESCRIPTION |
| Frontal | Forms forehead, is thicker anteriorly, contains frontal sinuses |
| Nasal | Paired bones that form the root of the nose |
| Lacrimal | Small, paired bones that form part of the anteromedial wall of the orbit and contain the lacrimal sac |
| Zygomatic | Paired cheekbones that form the inferolateral rim of the orbit and are frequently fractured by blunt trauma |
| Maxilla | Paired bones that form part of the cheek and contain 16 maxillary teeth |
| Mandible | Lower jaw bone that contains 16 mandibular teeth |
| Parietal | Forms the superolateral portion of the neurocranium |
| Temporal | Paired bones that form the lower portion of the lateral neurocranium and contain the middle and inner ear cavities, and the vestibular system for balance |
| Sphenoid | Complex bone composed of a central body, and greater and lesser wings |
| Occipital | Forms the inferoposterior portion of the neurocranium |
| Ethmoid | Forms the ethmoid sinuses, and contributes to the medial, lateral, and superior walls of the nasal cavity |
| Inferior concha | Paired bones of the lateral nasal wall that form the inferior nasal concha |
| Vomer | Forms the lower part of the nasal septum |
| Palatine | Contributes to the lateral nasal wall, a small part of the nasal septum, and the hard palate |
Other features of the skull are noted as we review each region of the head. However, general external features include the following (Figs. 8-2 and 8-3):
• Coronal suture: region between the frontal and two parietal bones.
• Sagittal suture: region between the two parietal bones.
• Lambdoid suture: region between the occipital bone and the two parietal bones.
• Nasion: point at which the frontal and nasal bones meet.
• Bregma: point at which coronal and sagittal sutures meet.
• Lambda: point at which sagittal and lambdoid sutures meet.
• Pterion: point at which frontal, sphenoid, temporal, and parietal bones meet; the middle meningeal artery lies beneath this region.
• Asterion: point at which temporal, parietal, and occipital bones meet.
Cranial Fossae
The cranial base is the floor of the neurocranium, which supports the brain, and is divided into the following three cranial fossae: (Fig. 8-4):
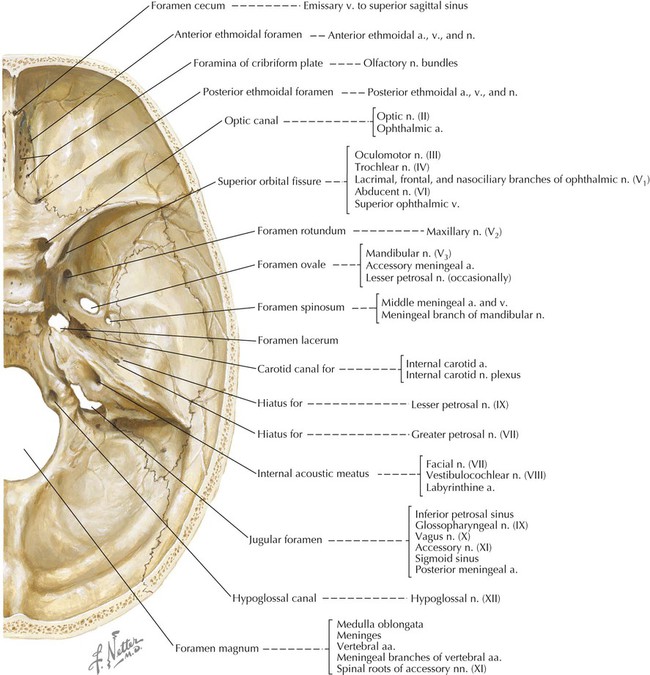
• Anterior: the roof of the orbits; accommodates the frontal lobes of the brain.
• Middle: accommodates the temporal lobes of the brain.
• Posterior: accommodates the cerebellum, pons, and medulla oblongata of the brain.
Each fossa has numerous foramina (openings) for structures to pass in or out of the neurocranium.
4 Brain
Meninges
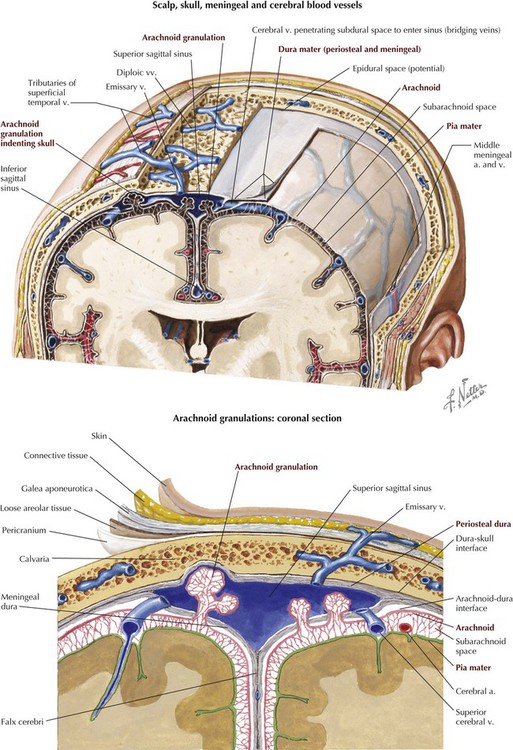
The brain and spinal cord are surrounded by three membranous connective tissue layers called the meninges, which include the following (Fig. 8-5):
• Dura mater: thick outermost meningeal layer that is richly innervated by sensory nerve fibers.
• Arachnoid mater: fine, weblike avascular membrane directly beneath the dural surface; the space between the arachnoid and the underlying pia is called the subarachnoid space and contains cerebrospinal fluid, which bathes and protects the central nervous system (CNS).
• Pia mater: delicate membrane of connective tissue that intimately envelops the brain and spinal cord.
The cranial dura is distinguished from the dura mater covering the spinal cord by its two layers. An outer periosteal layer is attached to the inner aspect of the cranium and is supplied by the meningeal arteries, which lie on its surface between it and the bony skull. Imprints of these meningeal artery branches can be seen as depressions on the inner table of bone. This periosteal dura is continuous with the periosteum on the outer surface of the skull at the foramen magnum and where other intracranial foramina open onto the outer skull surface. The inner dural layer is termed the meningeal layer and is in close contact with the underlying arachnoid mater and is continuous with the spinal dura at the level of the foramen magnum.
The dura mater is richly innervated by meningeal sensory branches of the trigeminal nerve (fifth cranial nerve, CN V); the vagus nerve (CN X), specifically to the posterior cranial fossa; and the upper cervical nerves. A portion of the dura in the posterior cranial fossa also may receive some innervation from the glossopharyngeal nerve (CN IX) and hypoglossal nerve (CN XII). The arachnoid and pia mater lack sensory innervation. The periosteal dura and meningeal dura separate to form thick connective tissue folds or layers that separate various brain regions and lobes (Figs. 8-5, 8-6, and 8-7):
• Falx cerebri: double layer of meningeal dura between the cerebral hemispheres.
• Falx cerebelli: sickle-shaped layer of meningeal dura that projects between the two cerebellar hemispheres.
• Tentorium cerebelli: fold of meningeal dura that covers the cerebellum and supports the occipital lobes of the cerebral hemispheres.
• Diaphragma sellae: horizontal shelf of meningeal dura that forms the roof of the sella turcica covering the pituitary gland; the infundibulum passes through this dural shelf to connect the hypothalamus with the pituitary gland.
Dural Venous Sinuses
The dura also separates to form several large endothelial-lined venous channels between its periosteal and meningeal layers—superior and inferior sagittal, straight, confluence of sinuses, transverse, sigmoid, and cavernous sinuses—and several smaller dural sinuses (Table 8-2 and Fig. 8-7). These dural venous sinuses drain blood from the brain, largely posteriorly, then into the internal jugular veins. These sinuses lack valves, however, so the direction of blood flow through the sinuses is pressure dependent. Of particular importance is the cavernous venous sinus, which lies on either side of the sella turcica and has an anatomical relationship with the internal carotid artery and several cranial nerves, including III, IV, V1, V2, and VI. Injury or inflammation in this region can affect all these important structures. Also, the optic chiasm lies just above this area, so CN II may be involved in any superior expansion of the cavernous sinus (e.g., pituitary tumor).
TABLE 8-2
| SINUS | CHARACTERISTICS |
| Superior sagittal | Midline sinus along the convex superior border of the falx cerebri |
| Inferior sagittal | Midline sinus along the inferior free edge of the falx cerebri and joined by the great cerebral vein (of Galen) |
| Straight | Runs in the attachment of the falx cerebri and the tentorium cerebelli, and is formed by the inferior sagittal sinus and great cerebral vein |
| Confluence of sinuses | Meeting of superior and inferior sagittal sinuses, the straight sinus, and the occipital sinus |
| Transverse | Extends from the confluence of sinuses along the lateral edge of the tentorium cerebelli |
| Sigmoid | Continuation of the transverse sinus that passes inferomedially in an S-shaped pathway to the jugular foramen (becomes internal jugular vein) |
| Occipital | Runs in the falx cerebelli to the confluence of sinuses |
| Basilar | Network of venous channels on basilar part of the occipital bone, with connections to the petrosal sinuses; drains into vertebral venous plexus |
| Cavernous | Lies between dural layers on each side of the sella turcica; connects to the superior ophthalmic veins, pterygoid plexus of veins, sphenoparietal sinuses, petrosal sinuses, and basilar sinus |
| Sphenoparietal | Runs along the posterior edge of the lesser wing of the sphenoid bone and drains into the cavernous sinus |
| Emissary veins | Small veins connect the dural sinuses with the diploic veins in the bony skull, which are connected to scalp veins |
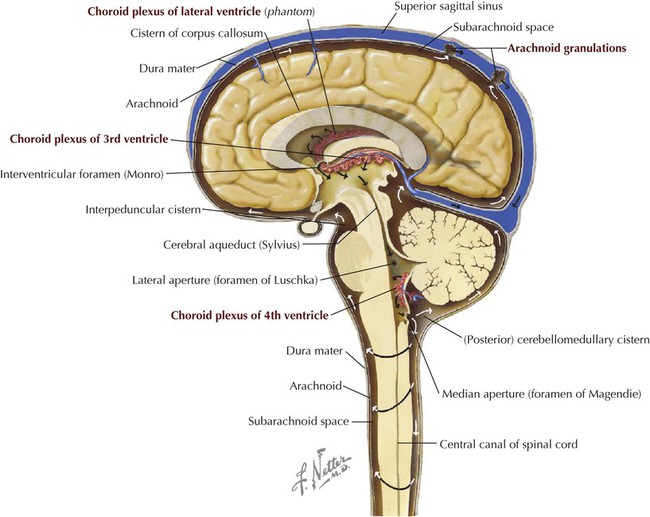
Subarachnoid Space
The subarachnoid space (between the arachnoid and pia mater) contains cerebrospinal fluid (CSF), which performs the following functions (Figs. 8-5 and 8-8):
• Supports and cushions the spinal cord and brain.
• Fulfills some functions normally provided by the lymphatic system.
• Occupies a volume of about 150 mL in the subarachnoid space.
• Is produced by choroid plexuses in the brain's ventricles.
• Is produced at a rate of about 500 to 700 mL/day.
• Is reabsorbed largely by arachnoid granulations and by small venules along the length of the spinal cord.
The arachnoid granulations absorb most of the CSF and deliver it to the dural venous sinuses (see Figs. 8-5 and 8-8). These granulations are composed of convoluted aggregations of arachnoid that extend as “tufts” into the superior sagittal sinus and function as one-way valves for the clearance of CSF; the CSF crosses into the venous sinus, but venous blood cannot enter the subarachnoid space. Small, microscopic arachnoid cell herniations also occur along the spinal cord, where CSF (which circulates at a higher pressure than venous blood) is delivered directly into small spinal cord veins.
Gross Anatomy of the Brain
The most notable feature of the human brain is its large cerebral hemispheres (Fig. 8-9). Several circumscribed regions of the cerebral cortex are associated with specific functions, and key surface landmarks of the typical human cerebrum are used to divide the brain into lobes: four or five, depending on classification, with the fifth either the insula or the limbic lobe. The lobes and their functions are as follows:
• Frontal: mediates precise voluntary motor control, learned motor skills, planned movement, eye movement, expressive speech, personality, working memory, complex problem solving, emotions, judgment, socialization, olfaction, and drive.
• Parietal: affects sensory input, spatial discrimination, sensory representation and integration, taste, and receptive speech.
• Occipital: affects visual input and processing.
• Temporal: mediates auditory input and auditory memory integration, spoken language (dominant side), and body language (nondominant side).
• Insula: a fifth deep lobe that lies medial to the temporal lobe (sometimes included as part of temporal lobe); influences vestibular function, some language, perception of visceral sensations (e.g., upset stomach), emotions, and limbic functions.
• Limbic: also sometimes considered a fifth medial lobe (cingulate cortex); influences emotions and some autonomic functions.
Other key areas of the brain include the following components (Fig. 8-9):
• Thalamus: gateway to the cortex; simplistically functions as an “executive secretary” to the cortex (relay center between cortical and subcortical areas).
• Cerebellum: coordinates smooth motor activities, and processes muscle position; possible role in behavior and cognition.
• Brainstem: includes the midbrain, pons, and medulla oblongata; conveys motor and sensory information from the body and autonomic and motor information from higher centers to peripheral targets.
Internally, the brain contains four ventricles, two lateral ventricles, and a central third and fourth ventricle (Fig. 8-10). Cerebrospinal fluid, produced by the choroid plexus (see Fig. 8-5), circulates through these ventricles and then enters the subarachnoid space through two lateral apertures (foramina of Luschka) or a median aperture (foramen of Magendie) in the fourth ventricle.
Blood Supply to the Brain
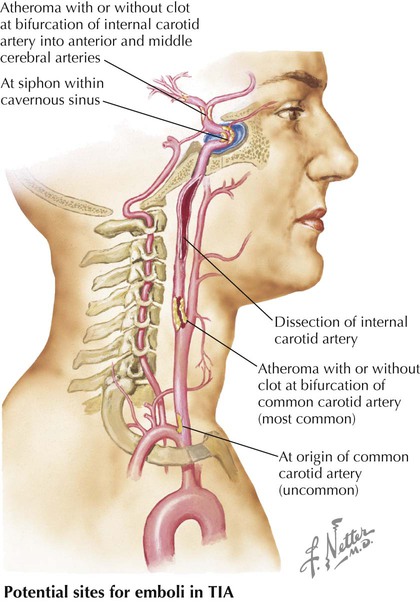
Arteries supplying the brain arise largely from the following two pairs of arteries (Fig. 8-11 and Table 8-3):
TABLE 8-3
| ARTERY | COURSE AND STRUCTURES SUPPLIED |
| Vertebral | From subclavian artery; supplies cerebellum |
| Posterior inferior cerebellar | From vertebral artery; supplies the posteroinferior cerebellum |
| Basilar | From both vertebrals; supplies brainstem, cerebellum, and cerebrum |
| Anterior inferior cerebellar | From basilar; supplies inferior cerebellum |
| Superior cerebellar | From basilar; supplies superior cerebellum |
| Posterior cerebral | From basilar; supplies inferior cerebrum and occipital lobe |
| Posterior communicating | Cerebral arterial circle (of Willis) |
| Internal carotid (IC) | From common carotid; supplies cerebral lobes and eye |
| Middle cerebral | From IC; supplies lateral aspect of cerebral hemispheres |
| Anterior communicating | Cerebral arterial circle (of Willis) |
| Anterior cerebral | From IC; supplies cerebral hemispheres (except occipital lobe) |
• Vertebrals: arise from the subclavian artery, ascend through the transverse foramina of the C1-C6 vertebrae, and enter the foramen magnum of the skull.
• Internal carotids: arise from the common carotid in the neck, ascend in the neck, enter the carotid canal, and traverse the foramen lacerum to terminate as the middle and anterior cerebral arteries, which anastomose with the arterial circle of Willis.
The vertebral arteries give rise to the anterior and posterior spinal arteries (a portion of the supply to the spinal cord) and the posterior inferior cerebellar arteries, and then join at about the level of the junction between the medulla and pons to form the basilar artery (Fig. 8-11). The internal carotid arteries each give rise to an ophthalmic artery, a posterior communicating artery, a middle cerebral artery, and an anterior cerebral artery. Table 8-3 summarizes the brain regions supplied by these vessels and their major branches.
Cranial Nerves
See Chapter 1 for an overview of the general organization of the nervous system.
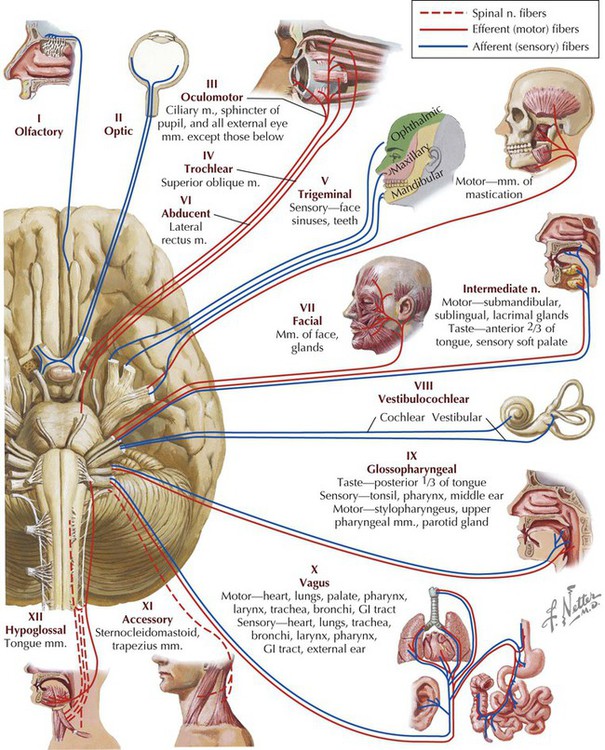
In addition to the 31 pairs of spinal nerves, 12 pairs of cranial nerves arise from the brain. As with the spinal nerves, cranial nerves are part of the peripheral nervous system and are identified both by name and by Roman numerals I to XII (Fig. 8-12). Cranial nerves are somewhat unique and may contain the following multiple functional components:
• General (G): same general functions as spinal nerves.
• Special (S): functions found only in cranial nerves (special senses).
• Afferent (A) or efferent (E): sensory or motor functions, respectively.
• Somatic (S) or visceral (V): related to skin and skeletal muscle innervation (somatic), or to smooth muscle, cardiac muscle, and glands (visceral).
By convention, each cranial nerve is classified as either general (G) or special (S), and then somatic (S) or visceral (V), and finally as afferent (A) or efferent (E). For example, a cranial nerve that is classified GVE (general visceral efferent) means it contains motor fibers to visceral structures, such as a parasympathetic or sympathetic fiber from the spinal cord.
In general, cranial nerves are described as follows (Table 8-4):
TABLE 8-4
Functional Components of the Cranial Nerves
| CRANIAL NERVE | FUNCTIONAL COMPONENT |
| I Olfactory nerve | SSA (Special sense of smell) |
| II Optic nerve | SSA (Special sense of sight) |
| III Oculomotor nerve | GSE (Motor to extra-ocular muscles) |
| GVE (Parasympathetic to smooth muscle in eye) | |
| IV Trochlear nerve | GSE (Motor to one extra-ocular muscle) |
| V Trigeminal nerve | GSA (Sensory to face, orbit, nose, and anterior tongue) |
| SVE (Motor to skeletal muscles) | |
| VI Abducent nerve | GSE (Motor to one extra-ocular muscle) |
| VII Facial nerve | GSA (Sensory to skin of ear) |
| SVA (Special sense of taste to anterior tongue) | |
| GVE (Motor to salivary, nasal, and lacrimal glands) | |
| SVE (Motor to facial muscles) | |
| VIII Vestibulocochlear nerve | SSA (Special sense of hearing and balance) |
| IX Glossopharyngeal nerve | GSA (Sensory to posterior tongue) |
| SVA (Special sense of taste—posterior tongue) | |
| GVA (Sensory from middle ear, pharynx, carotid body, and sinus) | |
| GVE (Motor to parotid gland) | |
| SVE (Motor to one muscle of pharynx) | |
| X Vagus nerve | GSA (Sensory external ear) |
| SVA (Special sense of taste—epiglottis) | |
| GVA (Sensory from pharynx, larynx, and thoracic and abdominal organs) | |
| GVE (Motor to thoracic and abdominal organs) | |
| SVE (Motor to muscles of pharynx/larynx) | |
| XI Accessory nerve | GSE (Motor to two muscles) |
| XII Hypoglossal nerve | GSE (Motor to tongue muscles) |
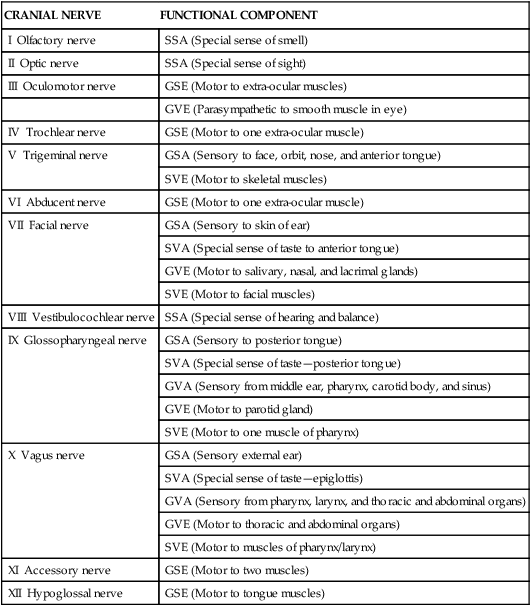
• CN I and II: arise from the forebrain; are really tracts of the brain for the special senses of smell and sight; they are brain extensions surrounded by all three meningeal coverings, with CSF in the subarachnoid space—but still are classified as cranial nerves.
• CN III, IV, and VI: move the extra-ocular skeletal muscles of the eyeball.
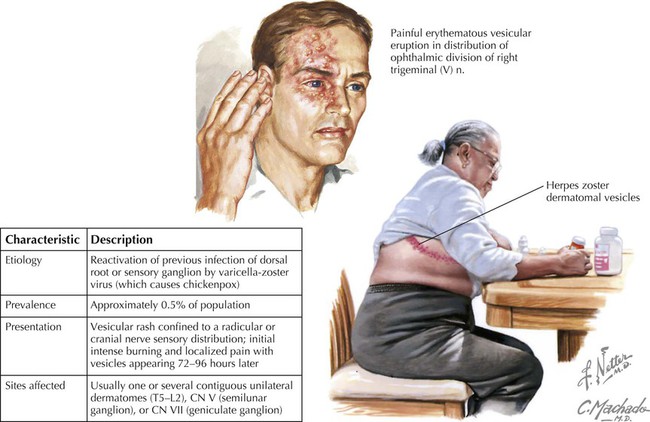
• CN V: has three divisions; V1 and V2 are sensory, and V3 is both motor and sensory.
• CN VII, IX, and X: are both motor and sensory.
• CN VIII: is the special sense of hearing and balance, but unlike CN I and II, is not a brain tract.
• CN XI and XII: are motor to skeletal muscle.
• CN III, VII, IX, and X: also contain parasympathetic (visceral) fibers of origin, although many of these autonomic fibers “jump” onto branches of CN V to reach their targets, because the branches of CN V pass almost everywhere in the head.
Rather than describe each cranial nerve and all its branches in detail at this time, we will review each nerve anatomically and clinically as we encounter it in the various regions of the head and neck. It may be helpful to refer back to this section each time you are introduced to a new region and its cranial nerve innervation. Autonomic components of the cranial nerves and their autonomic ganglia are summarized in Figure 1-25; the more complex cranial nerves also are summarized at the end of this chapter.
5 Scalp and Face
Layers of the Scalp
The layers of the SCALP include the following:
• Connective tissue that contains the blood vessels of the scalp
• Aponeurosis (galea aponeurotica) of the epicranial muscles (frontalis and occipitalis)
• Loose connective tissue deep to the aponeurosis, which contains emissary veins that communicate with the cranial diploë and dural sinuses within the cranium
The loose connective tissue layer allows the skin to move over the skull when one rubs the head and also allows infections to spread through this layer. Small emissary veins communicate with this layer and can pass infections intracranially.
Muscles of Facial Expression
The muscles of facial expression are skeletal muscles that lie in the subcutaneous tissue of the face. They are all innervated by the terminal motor branches of the facial nerve (CN VII), and most originate from the underlying facial skeleton but insert into the skin or facial cartilages (Fig. 8-13). Table 8-5 summarizes several of the major facial muscles, which are derived from the second branchial arch (see Embryology).
TABLE 8-5
Summary of Major Facial Muscles
| MUSCLE | ORIGIN | INSERTION | MAIN ACTIONS |
| Frontalis | Skin of forehead | Epicranial aponeurosis | Elevates eyebrows and forehead; wrinkles forehead |
| Orbicularis oculi | Medial orbital margin, medial palpebral ligament, and lacrimal bone | Skin around margin of orbit; tarsal plate | Closes eyelids; orbital part forcefully and palpebral part for blinking |
| Nasalis | Superior part of canine ridge of maxilla | Nasal cartilages | Draws ala of nose toward septum to compress opening |
| Orbicularis oris | Median plane of maxilla superiorly and mandible inferiorly; other fibers from deep surface of skin | Mucous membrane of lips | Closes and protrudes lips (e.g., purses them during whistling) |
| Levator labii superioris | Frontal process of maxilla and infra-orbital region | Skin of upper lip and alar cartilage | Elevates lip, dilates nostril, raises angle of mouth |
| Platysma | Superficial fascia of deltoid and pectoral regions | Mandible, skin of cheek, angle of mouth, and orbicularis oris | Depresses mandible and tenses skin of lower face and neck |
| Mentalis | Incisive fossa of mandible | Skin of chin | Elevates and protrudes lower lip and wrinkles chin |
| Buccinator | Mandible, pterygomandibular raphe, and alveolar processes of maxilla and mandible | Angle of mouth | Presses cheek against molar teeth, thereby aiding chewing |
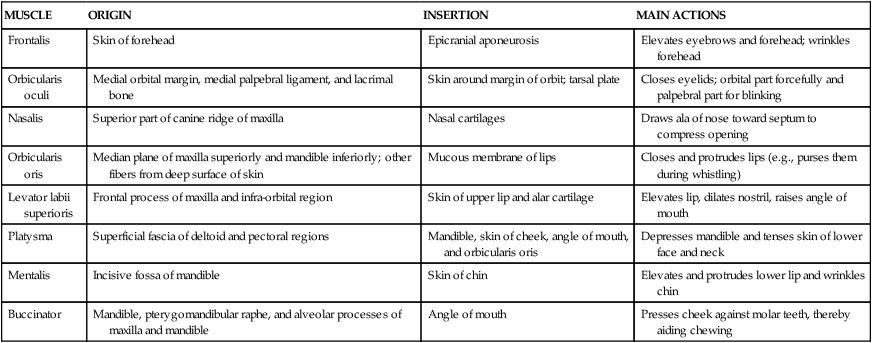
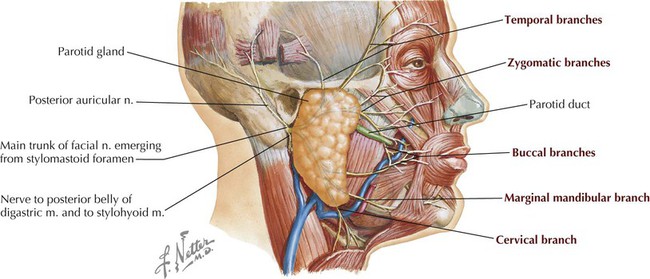
Innervation of the facial muscles is by the five terminal branches of CN VII. The facial nerve enters the internal acoustic meatus, passes through the facial canal in the petrous portion of the temporal bone, and then descends to emerge from the stylomastoid foramen. CN VII then passes through the parotid salivary gland and distributes over the face and neck (Fig. 8-14). The five terminal motor (branchial motor) branches are as follows:
The sensory innervation of the face is by the three divisions of the trigeminal nerve (CN V), with some contributions by the cervical plexus. Figure 8-15 lists the specific nerves for each division. All the sensory neurons in CN V reside in the trigeminal (semilunar, gasserian) ganglion. The trigeminal nerve is divided as follows:
• Ophthalmic (V1) division: exits the skull via the superior orbital fissure.
• Maxillary (V2) division: exits the skull via the foramen rotundum.
• Mandibular (V3) division: exits the skull via the foramen ovale.
The blood supply to the face includes the following vessels (Fig. 8-16):
• Facial artery: arises from the external carotid artery.
• Superficial temporal artery: one of the terminal branches of the external carotid artery.
• Ophthalmic artery: arises from the internal carotid artery and distributes over the forehead.
• Facial vein: drains into the internal jugular vein, directly or as a common facial vein.
• Retromandibular vein: formed by the union of the maxillary and superficial temporal veins; ultimately drains into the external and/or the internal jugular vein.
• Ophthalmic veins: tributaries from the forehead drain into superior and inferior ophthalmic veins in the orbit (and also anastomose with the facial vein) and then posteriorly into the cavernous dural sinus and/or the pterygoid plexus of veins in the infratemporal region (see Fig. 8-28).
6 Orbit and Eye
Bony Orbit
The bones contributing to the orbit include the following (Fig. 8-17):
The back of the orbit has three large openings that include the following:
• Superior orbital fissure: CN III, IV, VI, and V1 (frontal, lacrimal, and nasociliary nerves) pass through the fissure along with the ophthalmic vein.
• Inferior orbital fissure: CN V2 and infraorbital vessels pass through this fissure.
• Optic canal: CN II and the ophthalmic artery pass through this canal.
The periosteum of the orbital bones is a distinct layer of connective tissue called the periorbita. It is continuous with the pericranium (periosteum) covering the skull and, where the orbit communicates with the cranial cavity (e.g., superior orbital fissure), the periorbita is continuous with the periosteal layer of the dura mater.
Eyelids and Lacrimal Apparatus
The eyelids protect the eyeballs and keep the corneas moist. Each eyelid contains a tarsal plate of dense connective tissue; tarsal glands that secrete an oily mixture into the tears; modified sebaceous glands associated with each eyelash; apocrine glands (modified sweat glands); accessory lacrimal glands along the inner surface of the upper eyelid; and in the superior eyelid only, a small slip of smooth muscle (superior tarsal [Müller's] muscle), which attaches to the tarsal plate along with the levator palpebrae superioris muscle (Fig. 8-18). The tears contain albumins, lactoferrin, lysozyme, lipids, metabolites, and electrolytes. The lacrimal glands secrete continuously, and as one blinks, the tears are evenly spread across the conjunctiva and cornea. Tears not only keep the eye surface moist but also possess antimicrobial properties. The lacrimal apparatus includes the following:
• Lacrimal glands: secrete tears; innervated by the facial nerve parasympathetics
• Lacrimal ducts: excretory ducts of the glands
• Lacrimal canaliculi: collect tears into openings on the medial aspect of each lid called the puncta, and convey them to the lacrimal sacs
• Lacrimal sacs: collect tears and release them into the nasolacrimal duct when one blinks (contraction of the orbicularis oculi muscle)
• Nasolacrimal ducts: convey tears from lacrimal sacs to the inferior meatus of the nasal cavity
The lacrimal glands receive secretomotor parasympathetic fibers from the facial nerve (CN VII) that originate in the superior salivatory nucleus. These preganglionic parasympathetic fibers travel in the greater petrosal nerve and in the nerve of the pterygoid canal (vidian nerve), and the fibers then synapse in the pterygopalatine ganglion. Postganglionic parasympathetic fibers travel through the maxillary nerve (V2), zygomatic nerve, and lacrimal nerve (V1) to the lacrimal gland (see Fig. 8-70). Postganglionic sympathetic nerves from the superior cervical ganglion (SCG) jump from the internal carotid plexus in the form of the deep petrosal nerve, join the greater petrosal nerve, and form the nerve of the pterygoid canal. These postganglionic sympathetic fibers then follow the same course up to the lacrimal glands. The sensory innervation of the lacrimal gland is through the ophthalmic division of the trigeminal nerve (via the lacrimal branch).
Muscles
The orbital muscles include six extra-ocular skeletal muscles that move the eyeball and one skeletal muscle that elevates the upper eyelid (Fig. 8-19 and Table 8-6). In addition to the movements of elevation, depression, abduction, and adduction, the superior rectus and superior oblique muscles medially rotate (intorsion) the eyeball, and the inferior rectus and inferior oblique muscles laterally rotate (extorsion) the eyeball. The actions of the extra-ocular muscles detailed in Table 8-6 reflect their “anatomical” actions; because of how the muscles insert into the globe, any single action of the eye often involves multiple muscles contracting at the same time. For example, two muscles elevate the eyeball (superior rectus, inferior oblique), and three muscles abduct the eyeball (lateral rectus, superior oblique, inferior oblique). Clinically, one needs to “isolate” the multiple actions of the muscles so that an individual muscle's action can be assessed (e.g., elevation or depression; see Clinical Focus 8-21).
TABLE 8-6
| MUSCLE | ORIGIN | INSERTION | INNERVATION | MAIN ACTIONS |
| Levator palpebrae superioris | Lesser wing of sphenoid bone, anterosuperior optic canal | Tarsal plate and skin of upper eyelid | Oculomotor nerve | Elevates upper eyelid |
| Superior rectus | Common tendinous ring | Sclera just posterior to cornea | Oculomotor nerve | Elevates, adducts, and rotates eyeball medially |
| Inferior rectus | Common tendinous ring | Anterior sclera | Oculomotor nerve | Depresses, adducts, and rotates eyeball laterally |
| Medial rectus | Common tendinous ring | Anterior sclera | Oculomotor nerve | Adducts eyeball |
| Lateral rectus | Common tendinous ring | Anterior sclera | Abducent nerve | Abducts eyeball |
| Superior oblique | Body of sphenoid bone | Passes through trochlea and inserts into sclera | Trochlear nerve | Medially rotates, depresses, and abducts eyeball |
| Inferior oblique | Floor of orbit | Sclera deep to lateral rectus muscle | Oculomotor nerve | Laterally rotates and elevates and abducts eyeball |
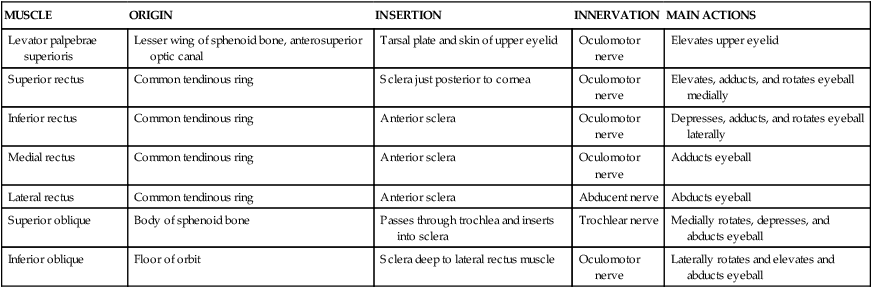
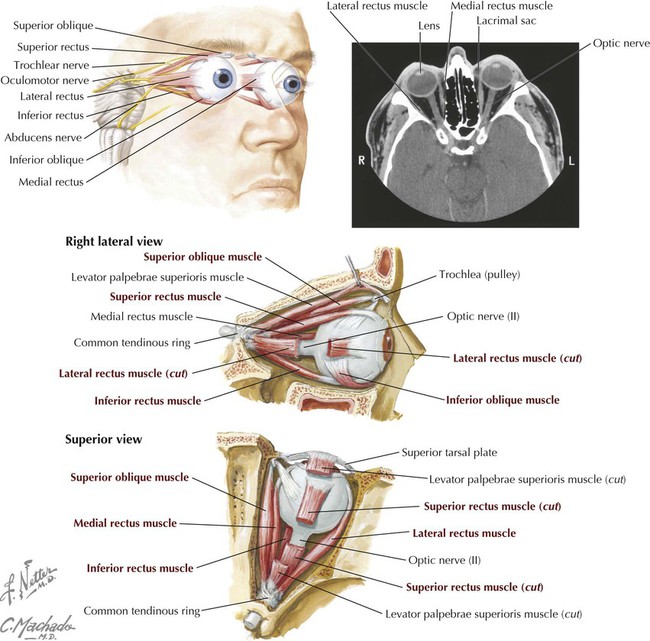
The levator palpebrae superioris muscle elevates the upper eyelid and, from its inferior surface, has a small amount of smooth muscle (superior tarsal muscle) connecting it to the tarsal plate. This smooth muscle is innervated by postganglionic sympathetic fibers from the superior cervical ganglion. The interruption of this sympathetic pathway can lead to a moderate ptosis, or drooping, of the upper eyelid. Interruption of the innervation of the levator palpebrae superioris from CN III can lead to a significant ptosis.
Nerves in the Orbit
Three cranial nerves innervate the extra-ocular skeletal muscles (Table 8-6), one cranial nerve mediates the special sense of sight (CN II), and one cranial nerve conveys general sensory information from the orbit and eye (CN V1) (Fig. 8-20). The major branches of the ophthalmic nerve (CN V1) include the following:
• Frontal: runs on the superior aspect of the levator palpebrae superioris muscle and ends as the supratrochlear and supra-orbital nerves; sensory to forehead, scalp, frontal sinus, and upper eyelid.
• Lacrimal: courses laterally on the superior aspect of the lateral rectus muscle to the lacrimal gland; sensory to conjunctiva and skin of the upper eyelid, and the lacrimal gland.
• Nasociliary: gives rise to short and long ciliary nerves, posterior and anterior ethmoidal nerves, and infratrochlear nerve; sensory to iris and cornea, sphenoid and ethmoid sinuses, lower eyelid, lacrimal sac, and skin of the anterior nose.
The optic nerve (CN II) is actually a brain tract that conveys sensory information from the retina, via the ganglion cell axons, to the brain (see Fig. 8-12). The optic nerve is covered by the same three dural layers as the rest of the CNS, and the retina is really our “window” into the brain (see Clinical Focus 8-25).
In addition to supplying four of the seven skeletal muscles in the orbit (see Table 8-6), the oculomotor nerve (CN III) also provides parasympathetic fibers, which exhibit the following features (see Fig. 8-68):
• Parasympathetic fibers arise centrally from the nucleus of Edinger-Westphal (preganglionic fibers) and course along CN III and its inferior division to synapse in the ciliary ganglion on postganglionic parasympathetic neurons.
• Postganglionic parasympathetic fibers then course via short ciliary nerves to the eyeball.
• These postganglionic fibers innervate the sphincter muscle of the pupil (sphincter pupillae) and the ciliary muscle for accommodation.
Sympathetic innervation to the eyeball is arranged as follows (see Figs. 8-67 and 8-68):
• Sympathetic innervation arises from the upper thoracic intermediolateral cell column of the spinal cord (T1-T2) and sends preganglionic fibers into the sympathetic trunk, where these fibers ascend to synapse in the superior cervical ganglion (SCG).
• Postganglionic sympathetic fibers course along the internal carotid artery, enter the orbit on the ophthalmic artery and ophthalmic nerve, and pass through the ciliary ganglion or along the long and short ciliary nerves to the eyeball.
• These postganglionic fibers innervate the dilator muscle of the pupil (dilator pupillae) and the superior tarsal muscle of the upper eyelid.
Eyeball (Globe)
The human eyeball measures about 25 mm in diameter, is tethered in the bony orbit by six extraocular muscles that move the globe, and is cushioned by fat that surrounds the posterior two thirds of the globe (Fig. 8-21). The outer fibrous white coat of the eyeball is the sclera and is continuous anteriorly with the transparent cornea. A middle vascular layer called the choroid is continuous anteriorly with the ciliary body, ciliary process, and iris. The inner layer is the optically receptive retina posteriorly and an anterior nonvisual retinal extension that lines the internal surface of the ciliary body and iris (Table 8-7).
TABLE 8-7
| STRUCTURE | DEFINITION |
| Sclera | Outer fibrous layer of eyeball |
| Cornea | Transparent part of outer layer; very sensitive to pain |
| Choroid | Vascular middle layer of eyeball |
| Conjunctiva | Thin membrane that lines the inner aspect of the eyelids and reflects onto the sclera, ending at the scleral-corneal junction |
| Ciliary body | Vascular and muscular extension of choroid anteriorly |
| Ciliary process | Radiating pigmented ridge on ciliary body; secretes aqueous humor that fills posterior and anterior chambers |
| Iris | Contractile diaphragm with central aperture (pupil) |
| Lens | Transparent lens supported in capsule by zonular fibers |
| Refractive media | Light rays focused by the cornea, aqueous humor, lens, and vitreous humor |
| Retina | Optically receptive part of optic nerve (optic retina); contains rods (dim light vision) and cones (color vision) |
| Macula lutea | Yellowish region of retina lateral to the optic disc that contains the fovea centralis |
| Fovea centralis | Area of macula with the most acute vision; contains only cones and is the center of the visual axis (ideal focus point) |
| Optic disc | Nonreceptive area (blind spot) where retinal ganglion cell nerve axons leave the retina in the optic nerve and pass to the brain |
The large chamber behind the lens is the vitreous chamber (body) and is filled with a gel-like substance called the vitreous humor, which helps cushion and protect the fragile retina during rapid eye movements (see Fig. 8-21).
The chamber between the cornea and the iris is the anterior chamber; the space between the iris and lens is the posterior chamber. Both chambers are filled with aqueous humor, which is produced by the ciliary body and circulates from the posterior chamber, through the pupil, and into the anterior chamber, where it is absorbed by the trabecular meshwork into the scleral venous sinus (canal of Schlemm) at the angle of the cornea and iris.
Retina
The retina consists of the optic or neural retina, which is sensitive to light, and the nonvisual retina, which lines the internal surface of the ciliary body and iris. The junction separating the neural from the nonvisual retina is called the ora serrata (see Fig. 8-21).
The neural retina is composed of an outer retinal pigmented epithelium lying adjacent to the vascular choroid and a photosensitive region consisting of photoreceptive cells: rods are more sensitive to light and the receptors for low-light conditions (gray tones); cones are less sensitive to low light but very sensitive to red, green, and blue regions of the visual spectrum. Interspersed layers of conducting and association neurons and supporting cells lie more internally in the retina, closer to the vitreous body.
The axons of ganglion cells ultimately convey the photosensory information to the optic disc, where the cells course in the optic nerve and are relayed centrally. The optic disc is our “blind spot” because no cones or rods are present in this region of the retina.
The fovea centralis is the central focusing area and most sensitive portion of the retina. This region is thin because most of the other layers of the retina are absent. Here the photoreceptor layer consists only of cones, specialized for color vision and acute discrimination.
Accommodation of the Lens
The ciliary body contains smooth muscle arranged in a circular fashion like a sphincter (see Fig. 8-21). When relaxed, it pulls a set of zonular fibers attached to the elastic lens taut and flattens the lens for viewing objects at some distance from the eye. When focusing on near objects, the sphincter-like ciliary muscle (parasympathetically innervated by CN III) contracts and constricts closer to the lens, relaxing the zonular fibers and allowing the elastic lens to round up for accommodation (near vision).
Blood Supply to the Orbit and Eye
The ophthalmic artery arises from the internal carotid artery just as it exits the cavernous sinus, and it supplies the orbit and eye by the following branches (Fig. 8-22):
• Central artery of the retina: travels in the optic nerve; occlusion leads to blindness.
• Short and long posterior ciliary arteries: pierce the sclera and supply the ciliary body, iris, and choroid.
• Lacrimal arteries: supply the gland, conjunctiva, and eyelids.
• Ethmoidal arteries: supply the ethmoid and frontal sinuses, nasal cavity, and external anterior nose.
• Medial palpebrae arteries: supply the eyelids.
• Muscular arteries: supply skeletal muscles of the orbit and smooth muscles of the eyeball.
• Dorsal nasal arteries: supply the lateral nose and lacrimal sac.
• Supra-orbital artery: passes through supra-orbital notch and supplies the forehead and scalp.
The venous drainage is by the superior and inferior ophthalmic veins, with connections to the cavernous sinus posteriorly (principal drainage), the pterygoid plexus inferiorly, and the facial vein anteriorly (see Fig. 8-28).
7 Temporal Region
The temporal region includes the temporal bone region and infratemporal fossa, and focuses on the muscles of mastication, the mandibular division of the trigeminal nerve (CN V3), and the two terminal branches of the external carotid artery—the maxillary and superficial temporal arteries. The temporal fossa lies superior to the zygomatic arch, and the infratemporal fossa is a wedge-shaped area inferior and deep to the zygomatic arch. The lateral wall of this fossa is formed by the mandibular ramus.
Muscles of Mastication
The muscles of mastication provide a coordinated set of movements that facilitate biting and chewing (grinding action of lower jaw). These muscles participate in movements of elevation, retrusion (retraction), and protrusion of the mandible. Embryologically, the muscles are derived from the first branchial arch, and all are innervated by CN V3 (Fig. 8-23 and Table 8-8).
TABLE 8-8
Summary of the Muscles of Mastication
| MUSCLE | ORIGIN | INSERTION | MAIN ACTIONS |
| Temporalis* | Floor of temporal fossa and deep temporal fascia | Ramus of mandible and coronoid process | Elevates mandible; posterior fibers retrude mandible |
| Masseter | Zygomatic arch | Ramus of mandible and coronoid process | Elevates and protrudes mandible; deep fibers retrude mandible |
| Lateral pterygoid | Superior head: infratemporal surface of greater wing of sphenoid Inferior head: lateral pterygoid plate |
Pterygoid fovea, capsule of TMJ, articular disc | Acting together, protrude mandible; acting alone and alternately, produces side-to-side movements |
| Medial pterygoid | Deep head: medial surface of lateral pterygoid plate and palatine bone Superficial head: tuberosity of maxilla |
Ramus of medial mandible, inferior to mandibular foramen | Elevates mandible; acting together, protrude mandible; acting alone, protrudes side of jaw; acting alternately, produces grinding motion |
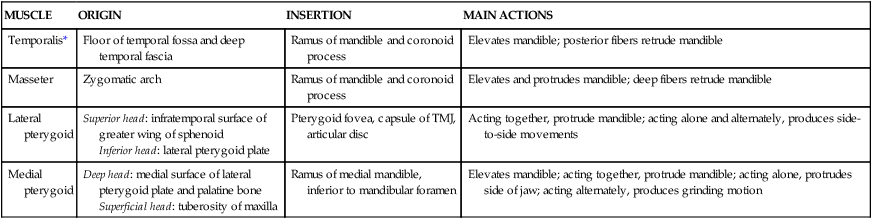
*All innervated by CN V3.
The temporomandibular joint (TMJ) is the articulation between the condylar process of the mandible and the squamous portion of the temporal bone (mandibular fossa) (Figs. 8-24 and 8-25 and Table 8-9). The TMJ is a modified hinge-type synovial joint. Unlike most synovial joints, the TMJ surfaces are covered with fibrous cartilage rather than hyaline cartilage and the joint cavity is divided by a fibrocartilaginous articular disc.
TABLE 8-9
| LIGAMENT | ATTACHMENT | COMMENT |
| Capsule | Temporal fossa and tubercle to mandibular head | Permits side-to-side motion, protrusion, and retrusion |
| Lateral (TMJ) | Temporal to mandible | Thickened fibrous band of capsule |
| Articular disc | Between temporal bone and mandible | Divides joint into two synovial compartments |
| Stylomandibular | Styloid process to posterior ramus and angle of jaw | Limits anterior protrusion of mandible |
| Sphenomandibular | Spine of sphenoid to lingula of mandible | May act as a pivot by providing tension during opening and closing |
Parotid Gland
The parotid gland is the largest of the three pairs of salivary glands and occupies the retromandibular space between the mandibular ramus and mastoid process (see Figs. 8-14 and 8-16). It is encased within the parotid sheath, a tough extension of the deep cervical fascia. The parotid duct courses medially across the medial border of the masseter muscle and then dives deeply into the buccal fat pad, piercing the buccinator muscle of the cheek and opening in the mouth just lateral to the second maxillary (upper) molar. As noted previously, the terminal portion of the facial nerve to the face exits the stylomastoid foramen and passes through the parotid gland to distribute to the muscles of facial expression (Fig. 8-14). The parotid gland is innervated by secretomotor parasympathetic fibers from the glossopharyngeal nerve (CN IX), which we will review in the next section (see Fig. 8-71).
Infratemporal Fossa
The wedge-shaped infratemporal fossa is the space inferior to the zygomatic arch, medial to the mandibular ramus and posterior to the maxilla. CN V3, the largest division of CN V, exits the foramen ovale, which is located in the roof of the fossa, and its branches in this region include the following (Fig. 8-26):
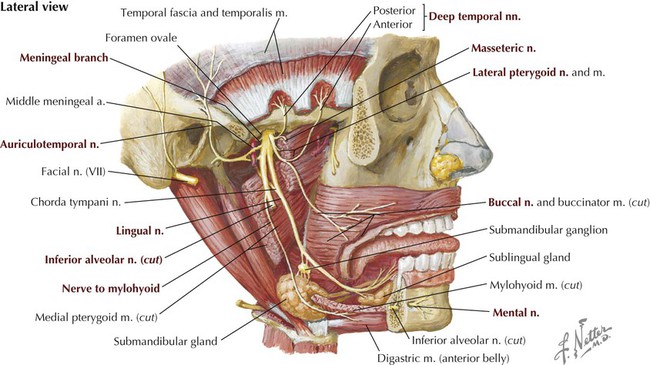
• Muscular: small motor nerves to the four muscles of mastication, and to the tensor veli palatini, mylohyoid, anterior belly of the digastric, and tensor tympani (in middle ear); embryologically, derived from the first branchial arch.
• Meningeal: accompanies the middle meningeal artery through the foramen spinosum; sensory to the dura.
• Auriculotemporal: conveys CN IX postganglionic parasympathetic secretory fibers from the otic ganglion to the parotid gland; sensory to the auricle and temple.
• Buccal: sensory to the cheek.
• Lingual: conveys CN VII preganglionic parasympathetics of the chorda tympani to the submandibular ganglion, and taste fibers from the tongue to the geniculate ganglion of CN VII; sensory to the tongue. These sensory fibers have their cell bodies in the trigeminal ganglion of CN V.
• Inferior alveolar: passes into the mandibular canal and is sensory to the mandibular teeth and gums via inferior dental and gingival branches and to the chin via the mental branch from the inferior alveolar nerve. The mylohyoid branch that leaves the inferior alveolar nerve before it enters the mandibular canal courses in the mylohyoid groove of the medial mandible and innervates the mylohyoid and anterior belly of the digastric muscles.
Parasympathetic preganglionic fibers from the glossopharyngeal nerve (CN IX) (inferior salivatory nucleus) run through the middle ear tympanic plexus and lesser petrosal nerve to synapse in the otic ganglion, which is located on the medial aspect of CN V3 as it exits the foramen ovale (see Figs. 8-69 and 8-71). Secretomotor postganglionic fibers join the auriculotemporal nerve and travel to the parotid gland, which they innervate.
Additionally, parasympathetic preganglionic fibers from CN VII (superior salivatory nucleus) pass through the middle ear and exit through a small fissure (petrotympanic) in the temporal bone as the chorda tympani nerve, to join the lingual branch of CN V3 and pass to the submandibular ganglion, where the fibers synapse (see Fig. 8-70). Secretomotor postganglionic fibers then innervate the submandibular and sublingual salivary glands.
Vascular Supply
The external carotid artery terminates as the superficial temporal and maxillary arteries (see Fig. 8-16). The superficial temporal artery supplies the scalp and upper face via its transverse facial branch. The maxillary artery supplies the infratemporal region, nasal cavities, palate, and maxillary teeth (Fig. 8-27). For descriptive purposes, the maxillary artery is divided into the following three parts:
• Retromandibular: arteries enter foramina and supply dura, mandibular teeth and gums, ear, and chin.
• Pterygoid: branches supply muscles of mastication and buccinator.
• Pterygopalatine: branches enter foramina and supply maxillary teeth and gums, orbital floor, nose, paranasal sinuses, palate, auditory tube, and superior pharynx.
Major branches of the maxillary artery include the inferior alveolar and middle meningeal branches from the first (retromandibular) part, branches to the muscles of mastication from the second (pterygoid) part, and the superior alveolar, infra-orbital, greater palatine, and sphenopalatine branches from the third (pterygopalatine) part (Fig. 8-27). The terminal portion of the maxillary artery passes into the pterygopalatine fossa (see Fig. 8-27) to gain access to the nasal cavity and nasopharynx. Here it is joined by the maxillary nerve (CN V2) and its branches.
The infratemporal fossa is largely drained by veins of the pterygoid plexus (Fig. 8-28), which have extensive anastomoses with dural, ophthalmic, and facial veins. Tributaries from each of the areas supplied by the branches of the maxillary artery ultimately drain into the pterygoid venous plexus and/or its principal anastomotic veins. These veins are valveless, so flow can go in either direction based on gravity and pressure.
8 Paranasal Sinuses and Nasal Cavity
Paranasal Sinuses
The four paired paranasal sinuses are the frontal, ethmoid, maxillary, and sphenoid sinuses, named for the bones in which they reside (Fig. 8-29). The paranasal sinuses surround the nose and orbits and are lined with respiratory epithelium (pseudostratified columnar with cilia). The sinuses lighten the weight of the facial skeleton, assist in warming and humidifying inspired air, add resonance to the voice, and drain mucus secretions into the nasal cavities. Sneezing and blowing the nose, as well as gravity, help to drain the paranasal sinuses of mucus.
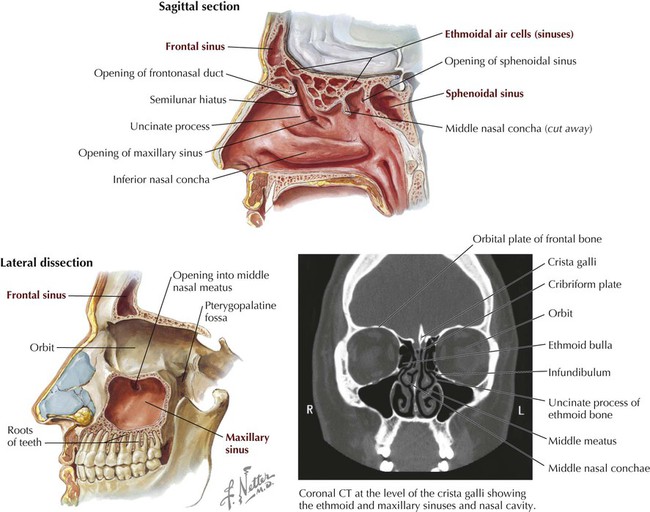
The innervation, blood supply, and drainage of the paranasal sinuses include the following (see Figs. 8-27 to 8-29, 8-31, 8-33, and 8-34):
• Frontal sinus: sensory fibers from V1 (supra-orbital); anterior ethmoidal arteries (from ophthalmic); the frontal sinus drains via the frontonasal duct into the semilunaris hiatus (middle meatus).
• Ethmoid sinus: sensory fibers from V1 (nasociliary nerve's ethmoidal branches) and V2 (orbital branches); blood from ethmoidal arteries (from ophthalmic); the anterior ethmoid sinus drains into the semilunaris hiatus (middle meatus); the middle ethmoid sinus drains into the ethmoid bulla (middle meatus); and the posterior ethmoid sinus drains into the superior meatus.
• Sphenoid sinus: sensory fibers from V2 (orbital branches); pharyngeal arteries (from maxillary); the sphenoid sinus drains into the spheno-ethmoidal recess above the superior concha.
• Maxillary sinus: sensory fibers from V2 (infra-orbital and alveolar branches); infraorbital and alveolar arteries (from maxillary); the maxillary sinus drains into the semilunar hiatus (middle meatus).
Note also that the nasolacrimal duct drains tears into the inferior meatus; thus your nose “runs” when you cry.
External Nose
The upper portion of the external nose is continuous with the forehead (frontal bone) through the nasal bones and laterally by the maxillae. The inferior two thirds of the external nose is cartilaginous and formed by the lateral processes of the septal cartilage, a midline septal cartilage, a major alar cartilage (tip of the nose), and several small, minor alar cartilages (Fig 8-30).
Nasal Cavities
Air entering the nose passes through the following areas (Fig. 8-31):
• Nares: anterior apertures or nostrils.
• Vestibule: dilated portion of the nose inside each aperture; highly vascular epithelium with hair.
• Respiratory region: nasal cavity proper, lined with highly vascular respiratory epithelium and three conchae, which increase the surface area for filtering, warming, and humidifying inspired air; conchae covered by respiratory epithelium are called turbinates.
• Olfactory region: small, apical region of nasal cavity where the olfactory receptors reside.
• Choanae: posterior apertures where the nasal cavity communicates with the nasopharynx.
Bones of the nasal cavity include the following (Fig. 8-32):
• Ethmoid: unpaired bone that contains the ethmoid air cells (sinuses); contributes to the roof and the lateral and medial walls of the nasal cavity.
• Sphenoid: unpaired bone that contains the sphenoid sinus; forms the posterior part of the cavity.
• Frontal: unpaired bone that contains the frontal sinus; forms part of the roof and septum of the cavity.
• Vomer: unpaired bone that contributes to the septum.
• Nasal: paired bones that form part of the anterior roof and lateral wall.
• Maxilla: paired bones that form the floor, septum, and lateral walls of the cavity.
• Palatine: paired bones that form the floor, septum, and lateral walls of the cavity.
• Lacrimal: bone that forms part of the lateral wall of the nasal cavity.
• Inferior nasal concha: paired bones that form part of the lateral wall.
Blood Supply and Innervation
Blood supply to the nasal cavities originates from the following major arteries (Fig. 8-33):
• Ophthalmic: anterior and posterior ethmoidal arteries
• Maxillary: sphenopalatine (terminal branch of the maxillary) and its septal branches, and the greater palatine arteries
• Facial: lateral nasal, septal branches, and superior labial artery
Corresponding veins drain the floor, lateral walls, and nasal septum, with most of the venous return passing into the pterygoid plexus of veins (Fig. 8-33). Some venous drainage also passes into the facial vein anteriorly and into the inferior ophthalmic veins superiorly.
The innervation of the nasal cavity includes the following (Fig. 8-34; see also Fig. 8-70):
• Olfactory: CN I olfactory receptors (special sense of smell) in the olfactory epithelium convey axons that pass from the upper part of the nasal cavity, through the cribriform plate, and synapse in the olfactory bulbs, which are actually brain tracts surrounded by the three meningeal layers, not unlike CN II.
• Ophthalmic: CN V1 general afferents are conveyed by the anterior and posterior ethmoidal nerves of the nasociliary nerve in the orbit to the trigeminal (sensory) ganglion.
• Maxillary: CN V2 general afferents are conveyed to the trigeminal (sensory) ganglion via small nasal branches and by the nasopalatine nerve on the septum.
• Sympathetics: comprised largely of postganglionic sympathetic vasomotor fibers from the SCG that reach the nose by traveling on blood vessels and existing nerves (mostly V2); other fibers also may course via the deep petrosal nerve to the nerve of the pterygoid canal and distribute with branches of CN V2.
• Parasympathetics: preganglionic secretomotor fibers to the mucosal glands of the nose and paranasal sinuses come from the superior salivatory nucleus of CN VII and travel via the greater petrosal nerve and the nerve of the pterygoid canal; the fibers synapse in the pterygopalatine ganglion; postganglionic parasympathetic fibers then distribute on existing nerves of CN V2.