Patient Safety and Team Training
David J. Birnbach MD, MPH, Eduardo Salas PhD
Chapter Outline
PATIENT SAFETY AND MEDICAL ERRORS
High-Reliability Organizations and Teams
Simulation-Based Training in Obstetrics
In 2000, the publication of the Institute of Medicine (IOM) report To Err is Human: Building a Safer Health Care System was a seminal event for the health care system in the United States.1 Prior to the publication of this report, many physicians and hospital administrators refused to acknowledge the frequent occurrence of preventable morbidity and the reality that our health care system was not adequately addressing the issue of patient safety. Subsequently, we have learned that tens of thousands of patients die each year as a result of medical errors. In the past decade, numerous changes have been advocated, including mandating minimum nurse-to-patient ratios,2 reducing working hours of resident physicians,3 and advancing the science of simulation training and teamwork, particularly in the medical environment.4,5 Data from high-risk organizations suggest that health care errors do not usually occur because of ill-trained medical personnel but rather are due to systems that “set up” both the patient and the health care provider. As Pratt6 eloquently stated in a 2012 review of simulation in obstetric anesthesia, “Historically, medicine was simple, largely ineffective, and mostly safe (excluding perhaps trephination and bloodletting). Modern medicine is complex, highly effective, but dangerous.” The field of patient safety attempts to reduce that danger, which is very real in the fields of obstetrics and obstetric anesthesiology. Each year in the United States, approximately 600 women die of pregnancy-related causes; 68,000 experience severe obstetric morbidity; and 1.7 million experience delivery-related complications.7 In this chapter, medical errors are reviewed and several modalities that can be used by labor and delivery unit personnel to reduce both the incidence and sequelae of these errors are highlighted.
Patient Safety and Medical Errors
Traditional assessments of medical error often blamed individuals and have failed to address the broader systems issues that allowed the error to occur. Newer approaches are based on an understanding that humans will make errors and therefore encourage creation of robust systems to prevent these errors from occurring or to minimize their impact on patients if they occur. This paradigm change has borrowed heavily from other high-risk arenas, such as the aviation and the nuclear industries.
The Swiss Cheese Model
Patients are typically not injured by a single event resulting from a single act of a careless individual. More often an underlying systems problem made the error possible, and numerous individual actions “fall through the cracks” of a system that does not catch them, resulting in error and harm. James Reason described the “Swiss cheese” model of error (Figure 11-1), in which he explained how numerous contributing factors are responsible for the ultimate harm.8 Reason developed this model to illustrate how analyses of major accidents and catastrophic systems failures tend to reveal multiple, smaller failures that led up to the actual adverse event. In the model, each slice of cheese represents a safety barrier or precaution relevant to a particular hazard. For example, if the hazard were wrong-site surgery, slices of the cheese might include processes for identifying the right or left side on radiology tests, a protocol for signing the correct site when the surgeon and patient first meet, and a second protocol for reviewing the medical record and checking the previously marked site in the operating room. Each barrier has “holes”; hence, the term Swiss cheese. For some serious events (e.g., operating on the wrong person) the holes will rarely align; however, even rare cases of harm are unacceptable. Reason's model highlights the need to think of safety as a system—a set of organizational and cultural layers that influence and shape one another. Reason has eloquently summarized the process, stating “rather than being the main instigators of an accident, operators tend to be the inheritors of system defects created by poor design, incorrect installation, faulty maintenance, and bad management decisions. Their part is usually that of adding the final garnish to a lethal brew whose ingredients have already been long in the cooking.”9
FIGURE 11-1 Swiss cheese model of organizational accidents. (From Reason JT. Human Error. Cambridge, UK, Cambridge University Press, 1990.)
Figure 11-2 illustrates the use of the Swiss cheese model to evaluate a real near-miss case involving the misidentification of an obstetric patient who nearly underwent the wrong procedure (an unwanted tubal ligation). It describes how the combination of numerous system errors came very close to allowing the wrong procedure to be performed. The events unfolded as follows:
1. A nulliparous woman in active labor at term arrived on the labor and delivery unit in severe pain. She spoke a foreign language and was poorly understood by the labor and delivery staff. No translator was called because her husband was helping with the translation.
2. Because the patient was in such severe pain, she rushed to answer all the questions and answered several incorrectly. As per hospital policy (due to HIPAA [Health Insurance Portability and Accountability Act of 1996] regulations), the husband was asked to leave the room while the history was being taken and was therefore not present to assist in the translation.
3. There was another patient on the labor and delivery unit with the same last name and a similar sounding first name. The hospital protocol for this occurrence was not followed. Patient initials, not last names, were listed on the labor and delivery “board,” so that other staff were unaware of the identical patient names.
4. The patient developed a nonreassuring fetal heart rate (FHR) tracing and was scheduled for urgent cesarean delivery. The obstetric resident physician informed the anesthesiologist of this decision and, mistaking the two patients with identical names, booked the case for a cesarean delivery plus bilateral tubal ligation. Unlike the other patient with the same name, the patient going to the operating room did not want or expect a tubal ligation.
5. The case was delayed because of a shift change, and the obstetricians urged the nurses to hurry. This caused friction between the nurses and obstetricians, and they did not work as a team. There were no “board rounds,” and communication between labor and delivery staff and operating room staff was suboptimal.
6. The patient arrived in the operating room and was very anxious and crying. The anesthesiologist administered fentanyl 50 µg to calm the patient and she became very sedated.
7. A “time-out” was performed, but it was not taken seriously. The patient was asleep and did not participate. The attending obstetrician was not present. Conversations continued during the time-out.
8. Following the flawed time-out, it was agreed that this patient was to undergo a primary cesarean delivery and tubal ligation. Her husband was not present during the time-out but was brought to the room immediately after this activity. The surgical procedure began.
9. The attending obstetrician arrived after the start of the procedure and questioned the planned tubal ligation, not because he knew about the second patient but because he was informed that this patient was nulliparous. Immediate investigation revealed that the patient was not supposed to receive a tubal ligation. A major error was narrowly averted.
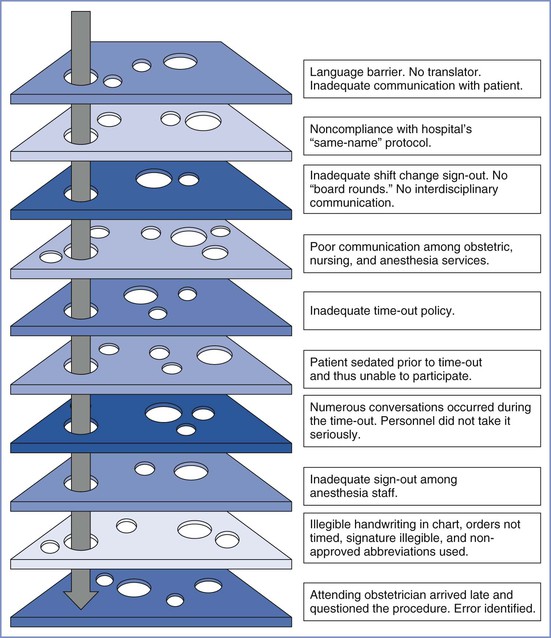
FIGURE 11-2 “Swiss cheese” diagram of near-miss event illustrating how numerous layers/barriers to harm were breached and how these events almost resulted in permanent harm (permanent sterility) to the patient. See text for explanation.
As in many such situations, a conglomeration of many missteps resulted in the potential for patient harm.
Medical Errors
Today there is widespread interest in changing the health care culture to build safer systems, including ensuring the appropriate physical work environment, developing redundancies in safety procedures, allowing health care workers to report their mistakes (including near misses) without fear of punishment, and providing mechanisms to learn from the experiences. None of these systems will achieve the ultimate goal of patient safety without the support of physicians as well as hospital administrators. In addition, although vital to improving the current condition, these steps do not obviate the need for well-trained and well-rested physicians and nurses. The American College of Obstetricians and Gynecologists (ACOG) Committee Opinion on Patient Safety in the Surgical Environment summarizes this well when it states: “Common sense dictates that the surgeon and the surgical team should be alert and well rested when initiating major surgical procedures.”10 The opinion also suggests that “adequate backup personnel should be available to relieve individuals who detect diminished performance in themselves or others due to fatigue, so that the risk for error is not increased.”10 Although the Accreditation Council on Graduate Medical Education has enacted restrictions on resident physician work hours to prevent sleep deprivation, there are no such limits on attending physician work hours. Rothschild et al.11 found that the risk for surgical complications was increased if attending physicians had slept less than 6 hours the night before the procedure.
Another ACOG committee opinion12 stated that promoting safety requires that all those in the health care environment recognize that the potential for errors exists and that women's health care should be delivered in an environment that encourages disclosure and exchange of information in the event of errors, near misses, and adverse outcomes. The ACOG12 has recommended the following seven safety objectives:
1. Develop a commitment to encourage a culture of patient safety.
2. Implement recommended safe medication practices.
3. Reduce the likelihood of surgical errors.
4. Improve communication with health care providers.
5. Improve communication with patients.
The IOM has defined medical error as a “failure of a planned action to be completed as intended, or the use of a wrong plan to achieve an aim.” Communication problems are consistently identified as a leading cause of medical errors in obstetrics,13 and the Joint Commission has found that although the majority of these events have multiple root causes, lack of effective communication along with leadership and human factors are often the primary causes of sentinel events.14 Several of the 2012 Joint Commission National Patient Safety Goals relate to error reduction on the labor and delivery unit (Box 11-1).15 Departments of anesthesiology and obstetrics and gynecology should regularly review the national patient safety goals established by the Joint Commission. Hospitals are regularly surveyed to verify their compliance with these goals.
Although those working in health care have made great efforts to reduce preventable patient harm,16 the progress has not been as dramatic as necessary. Leape and Berwick, two “fathers” of the field of patient safety, suggested that the lack of progress following the release of the initial IOM report is due to the “culture of medicine.”17 They believe that this culture is deeply rooted, both by custom and training, in autonomous individual performance. It remains possible that systematic and appropriate use of medical simulation, along with other important changes to our systems, will facilitate the necessary cultural changes and lead to improved patient safety. Labor and delivery units are no different than other medical care environments, and most still have many opportunities to change culture and practice to optimize patient safety. Nabhan and Ahmed-Tawfik18 suggested that the concept of patient safety in obstetrics is “not as strong as desirable for the provision of reliable health care.” In many units a punitive culture still exists and results in suppression of error reporting, lack of proper communication, and failure of appropriate feedback.18 Obviously, this culture needs to change before we can significantly improve patient safety. Pronovost and Freishlag19 eloquently described the operating room environment when they stated that “operating rooms are among the most complex political, social, and cultural structures that exist, full of ritual, drama, hierarchy, and too often conflict.” These authors concluded that poor teamwork contributes prominently to most adverse events, including those in the operating room.19
Teams and Teamwork
Health care should be considered a team activity. Teams take care of patients. Furthermore, health care teams operate in an environment characterized by acute stress, heavy workload, and high stakes for decision and action errors.20 Individuals have limited capabilities; when their limitations are combined with organizational and environmental complexity, human error is virtually inevitable.21 The labor and delivery unit is an exceedingly complex environment. In fact, the labor and delivery unit requires intense, error-free vigilance with effective communication and teamwork among various clinical disciplines who, although working together, have probably never trained together. This group includes obstetricians, midwives, nurses, anesthesiologists and nurse anesthetists, and pediatricians. The addition of trainees at all levels and in all disciplines enhances the potential for communication error. Siassakos et al.22 suggested that one of the most important components of effective training in obstetrics includes multiprofessional training and integration of teamwork training with clinical teaching.
A team consists of two or more individuals who have specific roles, perform independent tasks, are adaptable, and share common goals. Salas et al.23 have defined teamwork as a complex yet elegant phenomenon. It can be defined as a “set of interrelated behaviors, actions, cognitions, and attitudes that facilitate the required task work that must be completed.”23 Lack of teamwork has been identified as a leading cause of adverse events in medicine. Team behavior and coordination, particularly communication or team information sharing, are critical for optimizing team performance.24 Baker et al.25 stated that to work together effectively, team members must possess specific knowledge, skills, and attitudes (KSAs), including skill in monitoring each other's performance, knowledge of their own and their teammates' task responsibilities, and a positive disposition toward working in a team. These authors have described characteristics of effective teams, which include team leadership, mutual performance monitoring, backup behavior, adaptability, shared mental models, communication, team/collective orientation, and mutual trust. Moreover, effective team performance in complex environments requires that team members hold a shared understanding of the task, their equipment, and their teammates (Table 11-1).26,27
TABLE 11-1
Characteristics of Effective Teams
| Knowledge/Skills/Attitudes | Characteristics of the Team |
| Leadership | Roles are clear but not overly rigid. Team members believe leaders care about them. |
| Backup behavior | Members compensate for each other. Members provide feedback to each other. |
| Mutual performance monitoring | Members understand each other's roles. |
| Communication adaptability | Members communicate often and anticipate each other. |
| Mutual trust | Members trust each other's intentions. |
Modified from Salas E, Sims DE, Klein C. Cooperation and teamwork at work. In Spielberger CD, editor. Encyclopedia of Applied Physiology. San Diego, CA, Academic Press, 2004:499-505.
Teamwork is essential for safe patient care. The IOM suggested that team training and implementation of team behaviors may improve patient safety.28 The Joint Commission has recommended a risk-reduction strategy for decreasing perinatal death or injury. This strategy includes the implementation of team training and mock emergency drills for shoulder dystocia, emergency cesarean delivery, and maternal hemorrhage.29
Team training promotes the acquisition of adaptive behaviors, shared cognitions, and relevant attitudes. It is an instructional strategy that ideally combines practice-based delivery methods with realistic events, guided by medical teamwork competencies (i.e., behaviors, cognitions, and/or attitudes). Murray and Enarson30 stated that “when a crisis complicates patient care, teamwork among health care professionals is frequently strained, resulting in more frequent as well as more serious failures in managing critical events.” This scenario occurs all too often on the labor and delivery unit.
After many years of uncertainty, there is now encouraging evidence that team training improves safety of clinical outcomes, especially in the operating room31,32 and labor and delivery suite. Neily et al.32 reported that surgical mortality decreased by 18% at 74 United States Veterans Health Administration hospitals that implemented a team training program, compared with a 7% mortality reduction in 34 control hospitals that did not implement such a program. Nielson et al.33 reported that team training effectively reduced the decision-to-delivery time for emergency cesarean delivery. Similarly, after mandatory interdisciplinary team training for all labor and delivery staff in a unit in the United Kingdom, the median decision-to-delivery interval for a prolapsed umbilical cord decreased from 25 to 15 minutes. After initiation of team training in a community hospital, Shea-Lewis et al.34 reported a reduction in the adverse outcome index (AOI: a composite maternal and neonatal adverse outcome index35) from 7% to 4%.
Team Leadership
There is a clear difference between the leadership of individuals and team leadership. One who is leading independent individuals will diagnose a problem, generate possible solutions, and implement the most appropriate solution. In contrast, team leadership does not involve handing down solutions to team members but rather consists of defining team goals, setting expectations, coordinating activities, organizing team resources, and guiding the team toward its goals.36
Team leaders can improve team performance in many ways (e.g., by promoting coordination and cooperation). These individuals not only must be technically competent but also must be competent in leadership skills.20 Anesthesia providers and other physicians do not routinely train to be competent team leaders. Many of the tasks necessary can and must be learned during team training. Simulation may play a key role in this education. Team leadership training has been developed to successfully train specific team leader behaviors, and the implementation of these programs has been shown to improve team performance.23 Hackman37 described successful team performance as consisting of three primary elements:
1. Successful accomplishment of the team's goals
2. Satisfaction of team members with the team and commitment to the team's goals
3. The ability of the team to improve different facets of team effectiveness over time
High-Reliability Organizations and Teams
Despite the inevitability of human error, some organizations that operate in complex environments are able to maintain an exceptionally safe workplace. These organizations, including the aviation and nuclear power industries, have been termed high-reliability organizations (HROs). These organizations can also be hospitals and other health care organizations. Sundar et al.38 defined HROs as institutions where individuals, working together in high-acuity situations facing great potential for error and disastrous consequences, consistently deliver care with positive results and minimal errors. Teams that exhibit behaviors that facilitate the characteristics and values held by the HRO may be defined as high-reliability teams (HRTs). Wilson et al.21 have defined five guidelines for HRTs. These teams must:
1. Use closed-loop communication and other forms of information exchange to promote shared situational awareness regarding factors internal and external to the team.
2. Develop shared mental models that allow team members to monitor other members' performance and offer backup assistance when needed.
3. Demonstrate a collective organization that allows members to be assertive, to take advantage of functional expertise, and to seek and value input from other team members.
4. Seek to recognize complexities of their task environment and accordingly develop plans that are adequate and promote flexibility.
5. Use semi-structured feedback mechanisms such as team self-correction to manage, and quickly learn from, errors.
Hunt et al.39 defined characteristics associated with high-performing teams, including situational awareness, leadership, followership, closed-loop communication, critical language, standardized practice, assertive communication, adaptive behaviors, and workload management. An adaptive team performance framework that illustrates the relationship between variables, emergent states, and the multiple phases of the team adaptation cycle has been described by Salas et al.40 (Figure 11-3).
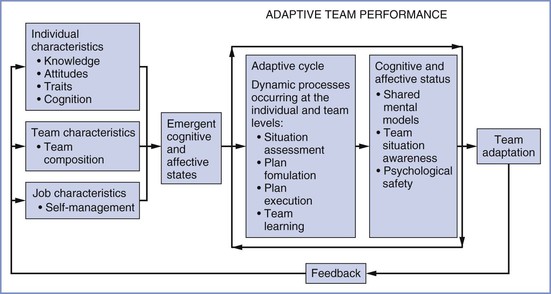
FIGURE 11-3 Adaptive team performance. (Modified from Salas E, Rosen MA, Burke CS, et al. The making of a dream team: when expert teams do best. In Ericsson KA, Charness N, Hoffman RR, Feltovich RJ, editors. The Cambridge Handbook of Expertise and Expert Performance. Cambridge, UK, Cambridge University Press 2006:439-456.)
Cultural factors may play a large role in team performance. According to Salas et al.,27 these factors include attitudes (especially as they relate to previous experiences with teams) and motivation. Although it has been suggested that an individual team member's personality may be counterbalanced by others, Janis41 suggested that openness, conscientiousness, and neuroticism are essential for individuals to succeed in command positions.
Thomas et al.42 conducted a qualitative assessment of teamwork and suggested that factors that influence the ability to work together could be divided into three categories: provider characteristics (personal attributes, reputation, expertise), workplace factors (staffing, work organization, work environment), and group influences (communication, relationships, and teamwork). These categories can be addressed, at least in part, by working together in teams in a simulated environment and evaluating teamwork and human performance. Lyndon43 suggested that the application of human performance-based theory has demonstrated that “communication patterns, team function, workload, and coping mechanisms affect both individual and group ability to identify evolving problems and make appropriate management decisions in complex decision-making situations.”43
Team Training
Patient safety is “predicated on trust, open communication, and effective interdisciplinary teamwork.”44 It is often the interactions among health care workers that determine whether a specific plan of care is effective or ineffective.45 However, in the current environment medical students, residents, attending physicians, nursing students, nurses, and midwives rarely learn or train to work as teams.
The Liaison Committee on Medical Education (LCME), which is jointly composed of members of the American Medical Association and the Association of American Medical Colleges, has affirmed the importance of teaching communications skills and teamwork. For example, LCME standard ED19 states that “there must be specific instruction in communication skills as they relate to professional responsibilities, including communication with patients, families, colleagues, and other health professionals.”46 Teamwork needs to be not only taught but also monitored. Box 11-2 summarizes best practices in team performance measurement for simulation-based training.
Why is teamwork training important for labor and delivery unit personnel? As previously noted, communication problems are consistently identified as a leading cause of medical error, and these problems can be addressed during team training. The 2000-2002 Confidential Enquiries into Maternal Deaths in the United Kingdom emphasized that “emergency drills for maternal resuscitation should be regularly practiced in clinical areas in all maternity units.”47 That report listed six direct maternal deaths plus one late maternal death due to anesthesia. Esophageal intubation was the cause of three maternal deaths. Each of these cases involved a trainee without immediate senior backup; and in two cases, capnography was not used, which was in direct violation of mandatory monitoring requirements. In an accompanying editorial, Ngan Kee48 stated, “This should give pause for thought to all involved with training in obstetric anesthesia” [italics added].48 These reports remind us not only of the need for appropriate supervision of trainees but also of the need to use simulation-based training for learning and practicing both crisis management and important techniques and procedures that are not frequently encountered in clinical practice. Emergency administration of general anesthesia for the parturient is such an event.
Simulation-Based Training in Obstetrics
Traditional medical and nursing education has relied on the treatment of real patients in actual clinical settings. Many educators now believe that the current availability of medical simulations and the knowledge gained from the science of team training may improve patient outcomes. Most medical and nursing schools have purchased simulators and are using them in undergraduate and graduate education.
Obstetricians have identified the importance of preparing for clinical emergencies and have reiterated that conducting emergency drills may reduce or prevent the severity of medical emergencies.49 In addition, simulation may impact patient safety because it offers opportunities to discover latent conditions and performance gaps that could adversely affect patient care.50,51 During 46 in situ simulations of obstetric emergencies, Riley et al.52 identified 965 breaches of defensive barriers (a system element that serves to prevent system errors from causing injury), of which 47.8% were classified as latent conditions (existing conditions that may interact with ongoing activities to precipitate error). The authors suggested that simulation helps providers recognize and remedy both active failures and latent conditions before they combine to cause bad outcomes.52
Research in simulation-based team training has shown that when trainees have an opportunity to practice relevant competencies in a structured scenario and receive diagnostic feedback on their individual and collective performance, simulation performance improves. This clearly indicates the importance of guided practice (by scenario events) and measurement.
Many authors have suggested that drills are useful on the labor and delivery unit.53-56 Sorenson54 stated that “mock emergency training is an opportunity for staff to learn to identify risk factors and prepare for interventions in the event of an obstetric emergency.” Gardner and Raemer55 suggested that simulation is a practical and safe approach to the acquisition and maintenance of task-oriented and behavioral skills across the spectrum of medical specialties. In the realm of obstetric anesthesia practice, investigators have demonstrated that simulation may be a useful tool for assessment of performance in a simulated emergency situation (e.g., failed intubation in an obstetric patient) when combined with practice and formal teaching.56
Training in perinatal emergencies with high-fidelity simulation improved the speed with which anesthesia providers responded to these emergencies and improved the quality of their care.57 Lipman et al.58 demonstrated, in a dramatic fashion, the use of simulation-based assessment to evaluate optimal performance of cardiopulmonary resuscitation during simulated maternal cardiac arrest. The authors demonstrated numerous deficiencies in the performance of key advanced cardiac life support (ACLS) tasks that are critical to resuscitation of a pregnant woman. These tasks included the ability to correctly deliver chest compressions (56% correct), ensure left uterine displacement (44% correct), switching chest compressors every 2 minutes (33% correct), and appropriate defibrillation (6% correct).58 Box 11-3 outlines the advantages of simulation for research, training, and performance assessment.
When an adverse perinatal outcome associated with an error occurs, it is likely that more than one individual will be involved and blamed.59 Similarly, when an unexpected injury occurs to a mother or infant, several providers are typically involved, and often there is a problem with the “system” that allowed the error to occur. Obstetricians, anesthesia providers, pediatricians, labor nurses, midwives, and operating room staff all work together as part of this system. Therefore, optimal simulation exercises involve all these key players and evaluate not only their behaviors and communication skills but also problems within the system in which they work. Simulation of reality-based scenarios in the labor and delivery unit or operating room allows anesthesia providers, obstetricians, midwives, nurses, and pediatricians to practice their roles and communication skills. Hunt et al.39 suggested that medical teams require practiced interaction and communication to be effective and efficient.
Simulation of perinatal events range from high-fidelity human simulators (typically located off site) to low-technology simulations and drills that can be performed on the labor and delivery unit.31 Simulated scenarios (guided by desired learning outcomes) can be designed to train nurses, obstetric and anesthesia resident physicians, and midwives individually or as teams. However, simulation should not be reserved for individuals in training; attending physicians may also benefit from participation. Simulated events commonly include maternal hemorrhage (antepartum as well as postpartum), failed intubation, failed neuraxial blockade, seizures, cardiac arrest, anaphylaxis, umbilical cord prolapse, and shoulder dystocia. Thomson et al.60 reported that drills to practice management of eclampsia were successful in the identification of deficiencies in team preparation. They concluded60:
Repetition of drills in our unit has improved the care of simulated patients with eclampsia. In subsequent drills patient management has followed evidence-based practice, with an enhanced level of efficiency. Staff [are] summoned faster, the resuscitation process is better organized, and drugs are prepared and administered more quickly.
Similarly, another group reported significant improvement in participants' knowledge after multidisciplinary obstetric training.61
Maslovitz et al.51 used simulation to identify five recurrent obstetric management mistakes:
1. Delay in transporting a bleeding patient to the operating room
2. Unfamiliarity with prostaglandin administration to treat uterine atony
3. Poor cardiopulmonary resuscitation techniques
4. Inadequate documentation of shoulder dystocia (important for the legal defense of these cases)
5. Delayed administration of blood products to reverse disseminated intravascular coagulation
The drills advocated for use by labor and delivery staff at the University of Miami Miller School of Medicine/Jackson Memorial Hospital are outlined in Box 11-4.
Simulation-based training must be implemented appropriately if it is to be effective. Salas et al.5 suggested the following guidelines for appropriate implementation:
1. Understand the training needs and requirements.
2. Embed instructional features (e.g., performance measurement and feedback) within the simulation.
3. Craft the scenarios based on expected/desired learning outcomes.
4. Create opportunities for assessing and diagnosing individual and/or team performance within the simulation.
6. Focus on cognitive/psychological simulation fidelity.
7. Form a mutual partnership between subject matter experts and learning experts.
Simulation exercises may also impact outcome by teaching improved communication to individuals and teams during transfer of patients' care from one set of caregivers to another, (i.e., so-called handovers or hand-offs). A recent survey from the United Kingdom found that handovers were rarely documented in writing and that 4% of units reported critical incidents after inadequate handovers in the preceding 12-month period.62 This interesting study describes the use of the SBAR technique (situation–background–assessment–recommendation) and the potential to practice sign-offs and handovers during practice drills.
Team Training in Obstetrics
As noted, teamwork is critical for the delivery of quality health care, especially in complex environments such as the labor and delivery unit. Awad et al.63 reported that medical team training improved communication in the operating room as assessed by team members using a validated scoring system. Why initiate team training on the obstetric service? The following case report by Sachs64 illustrates the need:
A healthy 38-year-old woman needed emergency cesarean delivery after a failed instrumental delivery. At surgery, the uterus was found to be ruptured and the fetus was stillborn. After unsuccessful attempts to repair the uterus, the patient underwent a cesarean hysterectomy and required massive transfusion and a 3-week hospital stay.
Was anyone at fault? According to the root cause analysis, lack of teamwork on many levels played a significant role in this patient's hospital course. In particular, Sachs64 reported that communication was poor and there was a lack of mutual performance cross-monitoring, inadequate conflict resolution, suboptimal situational awareness, and work overload.
Crew Resource Management
Although relatively new to obstetrics, team drills have been successfully used in other areas of medicine, including anesthesia, intensive care, and emergency medicine, often using lessons learned from crew resource management (CRM) training. The human error aspects of many air crashes are thought to include failure of communication, decision making, and leadership.65 In the airline industry, CRM began as a program to train pilots to reduce error by making better use of human resources in the cockpit.66 CRM training has led to safety and performance improvements beyond those produced by improvements in equipment and technology.5,65
Airlines use many tools to reduce human error; CRM training is just one. Other tools include use of checklists, standardized maintenance, ability to report errors without disciplinary repercussions, and simulator training. Not all of these, however, are easily adaptable to medicine. That said, Helmreich67 identified several lessons learned from CRM that can be applied to the practice of medicine. He believes that errors in competence require technical training and that errors in decisions or communication require team training. Furthermore, Helmreich67 suggested that adaptation of CRM to health care similarly requires the development of nonpunitive methods to collect information on errors so that this information can be used to evaluate team performance. It has been suggested that elements of CRM that are useful in medical settings include briefings, conflict resolution procedures, and performance reviews.23 There is evidence that operator attitudes about teamwork, hierarchy, errors, and stress affect performance among aviators working together in teams.68 Evidence also suggests that these attitudes are relevant in the health care environment.69
Salas et al.70 suggested that CRM training will not be effective or achieve its desired outcomes in health care without the following 12 prerequisites:
1. The physicians must be “on board.”
2. The concept of teamwork becomes part of the “DNA” of the health care professional.
3. CRM is supplemented by other teamwork-focused training strategies.
4. The design, development, and delivery of CRM are scientifically rooted.
5. CRM training is designed systematically.
6. CRM is part of a learning organization's strategy to promote patient safety and quality care.
7. Teamwork is rewarded and reinforced by the health care provider.
8. CRM training is evaluated at multiple levels for specific outcomes.
9. CRM is supported by simulation or practice-based approaches.
10. The health care provider is “ready” to receive training.
Some health care providers will benefit more than others from CRM training and learning. For example, one study noted that physicians with poorer performance at the beginning of CRM training showed greater improvements after training.71
Disruptive Behavior
Whereas miscommunication is common on the labor and delivery unit, some events are not caused by difficulties with communication but rather result from disruptive behavior by a team member. It is estimated that 3% to 5% of physicians exhibit disruptive behavior.72 Disruptive and intimidating behavior occurs frequently on labor and delivery units and is observed in personnel of diverse disciplines, including obstetricians, anesthesia providers, family practitioners, pediatricians, nurses, midwives, and administrators. In one survey, disruptive behavior was reported on more than 60% of labor and delivery units from personnel who responded to a questionnaire.73
Disruptive behavior includes angry outbursts, rudeness or verbal attacks, physical threats, intimidation, noncompliance with policies, and sexual harassment. Disruptive behavior contributes to the nursing shortage, near misses, and adverse occurrences. This behavior does not always involve physicians. Termed horizontal hostility, it occurs among nurses as well, and includes rudeness, verbal abuse, humiliating statements, unjustly critical statements, withholding information, and gossip.74 Disruptive behavior is not always effectively managed by the organization73 and should be considered when using simulation to improve team behaviors.
Options for Simulator Training in Obstetrics
Both high-technology and low-technology approaches to simulation have been used for training labor and delivery staff.54 Simulation centers often use high-fidelity simulation with interactive computerized mannequins in a realistic working environment (e.g., labor room or operating room) that includes a full complement of working equipment and staff.75 The mannequin is quite realistic; it has a pulse, heart and breath sounds, ventilatory movements, and electrocardiographic and pulse oximetry tracings. All vital signs can be adjusted via computer control, as can the ability to intubate or ventilate.75
Not all simulation exercises and drills for obstetrics need to be performed in high-fidelity simulators. Some authors76 have argued that classroom training is a better option, particularly given the high cost77 and resources necessary for high-fidelity simulation. The inability to arrange for staff of several disciplines to be absent from the labor and delivery unit simultaneously often precludes the use of high-technology simulation and may make on-site exercises more practical.54
On the other hand, Gaba78 has countered that high-fidelity simulation need not be cost-prohibitive and that it provides the required “real-life” experience necessary for training in the management of complex real-life scenarios. Morgan et al.79 reported an obstetric simulation model that included the participation of real surgeons (rather than actors playing the role of surgeons). This was the first published report of high-fidelity simulation of obstetric team performance with anesthesia providers, nurses, and obstetricians involved in the hands-on management of obstetric crises.
Several options are available for teaching teamwork and crisis intervention in obstetrics. Multidisciplinary obstetric simulated emergency scenarios (MOSES) was developed by the St. Bartholomew Hospital Group in the United Kingdom80 and involves participation of obstetricians, anesthesia providers, and midwives in team training on a high-fidelity simulator. MedTeams was developed by the U.S. Armed Forces and Dynamics Research Corporation. Originally employed in emergency departments,65,81,82 it has now been used for labor and delivery teams.33 The course consists of “train the trainer” sessions that focus on seven dimensions that are essential to teamwork. Behaviorally anchored rating scales (BARS) are used to assess various key behaviors. Additionally, in a 2006 review, Harris et al.83 discussed the challenges of implementation of team training in an obstetric care environment.
Other evidence-based programs have emerged. TeamSTEPPS was developed by the U.S. Department of Defense and Agency for Healthcare Research and Quality (AHRQ) as a team training and implementation toolkit.84 The program is adaptable, medically relevant, and based on findings from the science of team performance, and it is applicable to training on labor and delivery units.
What is the evidence that team training and simulation reduce errors and improve outcomes? Morey et al.65 reported that the MedTeams program reduced errors in the emergency department, and they observed a statistically significant improvement in team behaviors. The clinical error rate in providers who received MedTeams training decreased from 31% to 4%. Grunebaum et al.85 implemented team training as well as other comprehensive patient safety changes to their obstetric practice and found that their interventions resulted in decreased compensation payments and sentinel events. Clark et al.86 described implementation of a comprehensive redesign of patient safety processes that was associated with improved patient outcomes and a decline in litigation rates. The authors of the report stressed that “every member of the obstetric team should be not only empowered but also required to intervene and halt any process that is deemed to be dangerous.” This behavior can be achieved as part of a team training program.
Accumulating evidence suggests that medical simulation and team training improve teamwork and communication and allow recognition of potential areas of weakness in obstetric care. We, as well as others,25,38,87 believe that these are viable strategies to mitigate medical errors. We also agree with Pearlman et al.,88 who stated that “we have the moral imperative as a specialty to fully engage in the identification of our own best practices, to advance safety research in obstetrics and gynecology, and to implement broadly those practices which are best.”
In addition to better communication, team training, and simulation-based education, several other changes to our cultures and systems need to occur in order to significantly improve patient safety on the labor and delivery unit. These changes include:
• Changing the culture on the labor and delivery floor to one of a “just culture”89
• Having buy-in and support from hospital leadership to implement the necessary changes
• Improving the care of the high-risk parturient so that every member of the team is more prepared and working as a team member90
• Improving and automating the collection of quality metrics, collecting appropriate data on outcomes, and sharing the data with practitioners on a regular basis91
• Developing and implementing systems to reduce drug administration errors92,93
• Tearing down the silos so that we learn from each other's mistakes and improvement processes, whether from department to department, hospital to hospital, or country to country93
The challenge for the next decade will be to implement these changes and test their effectiveness in improving patient safety.
References
1. Kohn L, Corrigan J, Donaldson M. To err is human: building a safer health system. [Available at] http://www.nap.edu/catalog/9728.html; 2012 [Accessed November] .
2. Aiken LH, Clarke SP, Sloane DM, et al. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288:1987–1993.
3. Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–1848.
4. Gaba DM. Anaesthesiology as a model for patient safety in health care. BMJ. 2000;320:785–788.
5. Salas E, Wilson KA, Burke CS, Priest HA. Using simulation-based training to improve patient safety: what does it take? Jt Comm J Qual Patient Saf. 2005;31:363–371.
6. Pratt SD. Focused review: simulation in obstetric anesthesia. Anesth Analg. 2012;114:186–190.
7. Mhyre JM. What's new in obstetric anesthesia in 2009? An update on maternal patient safety. Anesth Analg. 2010;111:1480–1487.
8. Reason J. Human error: models and management. BMJ. 2000;320:768–770.
9. Reason J. Human Error. Cambridge University Press: Cambridge, UK; 1990.
10. American College of Obstetricians and Gynecologists. Patient safety in the surgical environment. ACOG Committee Opinion No. 464. [(Reaffirmed 2012)] Obstet Gynecol. 2010;116:786–790.
11. Rothschild JM, Keohane CA, Rogers S, et al. Risks of complications by attending physicians after performing nighttime procedures. JAMA. 2009;302:1565–1572.
12. American College of Obstetricians and Gynecologists Committee Committee on Patient Safety, Quality Improvement. Patient safety in obstetrics and gynecology. ACOG Committee Opinion No. 447. Obstet Gynecol. 2009;114:1424–1427.
13. Simpson KR, Knox GE. Adverse perinatal outcomes: recognizing, understanding and preventing common accidents. AWHONN Lifelines. 2003;7:224–235.
14. The Joint Commission. Sentinal event data: root causes by event type 2004-2Q 2012. [Available at] http://www.jointcommission.org/assets/1/18/Root_Causes_Event_Type_2004_2Q2012.pdf [Accessed November 2012] .
15. The Joint Commission. National patient safety goals. [Available at] http://www.jointcommission.org/standards_information/npsgs.aspx; 2012 [Accessed November] .
16. Pronovost PJ, Hudson DW. Improving healthcare quality through organisational peer-to-peer assessment: lessons from the nuclear power industry. BMJ Qual Saf. 2012;21:872–875.
17. Leape LL, Berwick DM. Five years after To Err Is Human: what have we learned? JAMA. 2005;293:2384–2390.
18. Nabhan A, Ahmed-Tawfik MS. Understanding and attitudes towards patient safety concepts in obstetrics. Int J Gynaecol Obstet. 2007;98:212–216.
19. Pronovost PJ, Freischlag JA. Improving teamwork to reduce surgical mortality. JAMA. 2010;304:1721–1722.
20. Salas E, Rosen MA, King H. Managing teams managing crises: principles of teamwork to improve patient safety in the emergency room and beyond. Theoret Issues Ergonom Sci. 2007;381–394.
21. Wilson KA, Burke CS, Priest HA, Salas E. Promoting health care safety through training high reliability teams. Qual Saf Health Care. 2005;14:303–309.
22. Siassakos D, Crofts JF, Winter C, et al. The active components of effective training in obstetric emergencies. BJOG. 2009;116:1028–1032.
23. Salas E, Guthrie J, Wilson-Donnelly K, et al. Modeling team performance: the basic ingredients and research needs. Rouse WB, Boff KR. Organizational Simulation. Wiley-Interscience: Hoboken, NJ; 2005:185–216.
24. Blum RH, Raemer DB, Carroll JS, et al. A method for measuring the effectiveness of simulation-based team training for improving communication skills. Anesth Analg. 2005;100:1375–1380.
25. Baker DP, Day R, Salas E. Teamwork as an essential component of high-reliability organizations. Health Serv Res. 2006;41:1576–1598.
26. Salas E, Rosen MA, Burke CS, et al. Markers for enhancing team cognition in complex environments: the power of team performance diagnosis. Aviat Space Environ Med. 2007;78:B77–B85.
27. Salas E, Sims D, Klien C. Cooperation and teamwork at work. Spielberger C. Encyclopedia of Applied Psychology. Academic Press: San Diego, CA; 2004:499–505.
28. Committee on Quality Healthcare in America, Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. National Academy Press: Washington, DC; 2001.
29. The Joint Commission. Preventing infant death and injury during delivery. Jt Comm Perspect. 2004;24:14–15.
30. Murray D, Enarson C. Communication and teamwork: essential to learn but difficult to measure. Anesthesiology. 2007;106:895–896.
31. Weaver SJ, Rosen MA, DiazGranados D, et al. Does teamwork improve performance in the operating room? A multilevel evaluation. Jt Comm J Qual Patient Saf. 2010;36:133–142.
32. Neily J, Mills PD, Young-Xu Y, et al. Association between implementation of a medical team training program and surgical mortality. JAMA. 2010;304:1693–1700.
33. Nielsen PE, Goldman MB, Mann S, et al. Effects of teamwork training on adverse outcomes and process of care in labor and delivery: a randomized controlled trial. Obstet Gynecol. 2007;109:48–55.
34. Shea-Lewis A. Teamwork: crew resource management in a community hospital. J Healthc Qual. 2009;31:14–18.
35. Mann S, Pratt S, Gluck P, et al. Assessing quality obstetrical care: development of standardized measures. Jt Comm J Qual Patient Saf. 2006;32:497–505.
36. Salas E, Wilson-Donnelly K, Sims D, et al. Teamwork training for patient safety: Best practices and guiding principles. Carayon P. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. Lawrence Erlbaum Associates: Rahway, NJ; 2007.
37. Hackman JR. Groups that work (and those that don't): creating conditions for effective teamwork. Jossey-Bass: San Francisco, CA; 1990.
38. Sundar E, Sundar S, Pawlowski J, et al. Crew resource management and team training. Anesthesiol Clin. 2007;25:283–300.
39. Hunt EA, Shilkofski NA, Stavroudis TA, Nelson KL. Simulation: translation to improved team performance. Anesthesiol Clin. 2007;25:301–319.
40. Salas E, Rosen MA, Burke CS, et al. The making of a dream team: when expert teams do best. Ericsson K, Charness N, Feltovich P, Hoffman R. The Cambridge Handbook of Expertise and Expert Performance. Cambridge University Press: Cambridge, UK; 2006:439–456.
41. Janis IL. Crucial decisions: leadership in policymaking and crisis management. Free Press: New York; 1989.
42. Thomas EJ, Sherwood GD, Mulhollem JL, et al. Working together in the neonatal intensive care unit: provider perspectives. J Perinatol. 2004;24:552–559.
43. Lyndon A. Communication and teamwork in patient care: how much can we learn from aviation? J Obstet Gynecol Neonatal Nurs. 2006;35:538–546.
44. Simpson KR, James DC, Knox GE. Nurse-physician communication during labor and birth: implications for patient safety. J Obstet Gynecol Neonatal Nurs. 2006;35:547–556.
45. Rosen MA, Salas E, Wilson KA, et al. Measuring team performance in simulation-based training: adopting best practices for healthcare. Simul Healthcare. 2008;3:33–41.
46. Liaison Committee on Medical Education. Functions and Structure of a Medical School: Standards for Accreditation of Medical Education Programs Leading to the M.D. Degree, May 2012. [Available at] http://www.lcme.org/functions.pdf [Accessed November 2012] .
47. Confidential Enquiry Into Maternal and Child Health. Why mothers die: 2000-2002: The Sixth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom 2004. [Available at] http://www.hqip.org.uk/assets/NCAPOP-Library/CMACE-Reports/33.-2004-Why-Mothers-Die-2000-2002-The-Sixth-Report-of-the-Confidential-Enquiries-into-Maternal-Deaths-in-the-UK.pdf; 2012 [Accessed November 23] .
48. Ngan Kee WD. Confidential enquiries into maternal deaths: 50 years of closing the loop. Br J Anaesth. 2005;94:413–416.
49. American College of Obstetricians and Gynecologists. Preparing for clinical emergencies in obstetrics and gynecology. ACOG Committee Opinion No. 487. Obstet Gynecol. 2011;117:1032–1034.
50. Park CS. Simulation and quality improvement in anesthesiology. Anesthesiol Clin. 2011;29:13–28.
51. Maslovitz S, Barkai G, Lessing JB, et al. Recurrent obstetric management mistakes identified by simulation. Obstet Gynecol. 2007;109:1295–1300.
52. Riley W, Davis S, Miller KM, et al. Detecting breaches in defensive barriers using in situ simulation for obstetric emergencies. Qual Saf Health Care. 2010;19(Suppl 3):i53–i56.
53. Johannsson H, Ayida G, Sadler C. Faking it? Simulation in the training of obstetricians and gynaecologists. Curr Opin Obstet Gynecol. 2005;17:557–561.
54. Sorensen SS. Emergency drills in obstetrics: reducing risk of perinatal death or permanent injury. JONAS Healthc Law Ethics Regul. 2007;9:9–16.
55. Gardner R, Raemer DB. Simulation in obstetrics and gynecology. Obstet Gynecol Clin North Am. 2008;35:97–127.
56. Goodwin MW, French GW. Simulation as a training and assessment tool in the management of failed intubation in obstetrics. Int J Obstet Anesth. 2001;10:273–277.
57. Chopra V, Gesink BJ, de Jong J, et al. Does training on an anaesthesia simulator lead to improvement in performance? Br J Anaesth. 1994;73:293–297.
58. Lipman SS, Daniels KI, Carvalho B, et al. Deficits in the provision of cardiopulmonary resuscitation during simulated obstetric crises. Am J Obstet Gynecol. 2010;203:179 e1–5.
59. Merien AE, van de Ven J, Mol BW, et al. Multidisciplinary team training in a simulation setting for acute obstetric emergencies: a systematic review. Obstet Gynecol. 2010;115:1021–1031.
60. Thompson S, Neal S, Clark V. Clinical risk management in obstetrics: eclampsia drills. BMJ. 2004;328:269–271.
61. Crofts JF, Ellis D, Draycott TJ, et al. Change in knowledge of midwives and obstetricians following obstetric emergency training: a randomised controlled trial of local hospital, simulation centre and teamwork training. BJOG. 2007;114:1534–1541.
62. Sabir N, Yentis SM, Holdcroft A. A national survey of obstetric anaesthetic handovers. Anaesthesia. 2006;61:376–380.
63. Awad SS, Fagan SP, Bellows C, et al. Bridging the communication gap in the operating room with medical team training. Am J Surg. 2005;190:770–774.
64. Sachs BP. A 38-year-old woman with fetal loss and hysterectomy. JAMA. 2005;294:833–840.
65. Morey JC, Simon R, Jay GD, et al. Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project. Health Serv Res. 2002;37:1553–1581.
66. Helmreich RL, Merritt AC, Wilhelm JA. The evolution of Crew Resource Management training in commercial aviation. Int J Aviat Psychol. 1999;9:19–32.
67. Helmreich RL. On error management: lessons from aviation. BMJ. 2000;320:781–785.
68. Bowers C, Jentsch F, Salas E, Braun C. Analyzing communication sequences for team training needs assessment. Human Factors. 1998;40:672–680.
69. Gaba DM, Singer SJ, Sinaiko AD, et al. Differences in safety climate between hospital personnel and naval aviators. Hum Factors. 2003;45:173–185.
70. Salas E, Wilson K, Murphy CK, Baker D. What crew resource management training will not do for patient safety: unless …. J Patient Saf. 2007;3:62–64.
71. Alder J, Christen R, Zemp E, Bitzer J. Communication skills training in obstetrics and gynaecology: whom should we train? A randomized controlled trial. Arch Gynecol Obstet. 2007;276:605–612.
72. Leape LL, Fromson JA. Problem doctors: is there a system-level solution? Ann Intern Med. 2006;144:107–115.
73. Veltman LL. Disruptive behavior in obstetrics: a hidden threat to patient safety. Am J Obstet Gynecol. 2007;196:587 e1–45.
74. Thomas SP. Horizontal hostility. Am J Nurs. 2003;103:87–91.
75. Blackburn T, Sadler C. The role of human patient simulators in health-care training. Hosp Med. 2003;64:677–681.
76. Pratt SD, Sachs BP. Point Counterpoint: Team training: Classroom training vs. high fidelity simulation. http://www.webmm.ahrq.gov/perspective.aspx?perspectiveID=21; 2012 [Accessed November] .
77. Kurrek MM, Devitt JH. The cost for construction and operation of a simulation centre. Can J Anaesth. 1997;44:1191–1195.
78. Gaba DM. Two examples of how to evaluate the impact of new approaches to teaching. Anesthesiology. 2002;96:1–2.
79. Morgan PJ, Pittini R, Regehr G, et al. Evaluating teamwork in a simulated obstetric environment. Anesthesiology. 2007;106:907–915.
80. Freeth D, Ayida G, Berridge EJ, et al. MOSES: Multidisciplinary Obstetric Simulated Emergency Scenarios. J Interprof Care. 2006;20:552–554.
81. Risser DT, Rice MM, Salisbury ML, et al. The potential for improved teamwork to reduce medical errors in the emergency department. The MedTeams Research Consortium. Ann Emerg Med. 1999;34:373–383.
82. Simon R, Salisbury M, Wagner G. MedTeams: teamwork advances emergency department effectiveness and reduces medical errors. Ambul Outreach. 2000;21–24.
83. Harris KT, Treanor CM, Salisbury ML. Improving patient safety with team coordination: challenges and strategies of implementation. J Obstet Gynecol Neonatal Nurs. 2006;35:557–566.
84. Alonso A, Baker DP, Holtzman A, et al. Reducing medical error in the Military Health System: How can team training help? Hum Resource Manage Rev. 2006;16:396–415.
85. Grunebaum A, Chervenak F, Skupski D. Effect of a comprehensive obstetric patient safety program on compensation payments and sentinel events. Am J Obstet Gynecol. 2011;204:97–105.
86. Clark SL, Belfort MA, Byrum SL, et al. Improved outcomes, fewer cesarean deliveries, and reduced litigation: results of a new paradigm in patient safety. Am J Obstet Gynecol. 2008;199:105 e1–7.
87. Grogan EL, Stiles RA, France DJ, et al. The impact of aviation-based teamwork training on the attitudes of health-care professionals. J Am Coll Surg. 2004;199:843–848.
88. Pearlman MD. Patient safety in obstetrics and gynecology: an agenda for the future. Obstet Gynecol. 2006;108:1266–1271.
89. Leape L, Berwick D, Clancy C, et al. Transforming healthcare: a safety imperative. Qual Saf Health Care. 2009;18:424–428.
90. Mhyre JM, Bateman BT, Leffert LR. Influence of patient comorbidities on the risk of near-miss maternal morbidity or mortality. Anesthesiology. 2011;115:963–972.
91. Ehrenfeld JM, Henneman JP, Peterfreund RA, et al. Ongoing professional performance evaluation (OPPE) using automatically captured electronic anesthesia data. Jt Comm J Qual Patient Saf. 2012;38:73–80.
92. Haller G, Clergue F. Drug administration errors in anaesthesia and beyond. BMJ. 2011;343:d5823.
93. Birnbach DJ, Vincent CA. A matter of conscience: a call to action for system improvements involving epidural and spinal catheters. Anesth Analg. 2012;114:494–496.