Fetopelvic relationship, mechanism of labour, normal labour, conduct of normal labour and partogram
Describe fetopelvic relationships.
Please refer to Chapter 8 of Holland and Brews Manual of Obstetrics for answer.
Describe the mechanism of labour in vertex presentation.
Definition – The series of changes in position and attitude that the presenting part has to make during its passage through the pelvis and the pelvic floor during the course of labour is known as the mechanism of labour. The fetal head which enters the pelvis in the transverse or one of the oblique diameters undergoes rotation and change in its attitude.
The different steps involved in the mechanism of labour are as follows (Fig. 10.1):
■ Descent (descent occurs throughout)
■ Internal rotation of the head
■ External rotation of head (corresponds to internal rotation of shoulder)
Engagement
The fetal head is said to have engaged when the maximum transverse (biparietal, 9.5 cm) and anteroposterior (which varies with the degree of flexion or extension of the head) diameters have crossed the plane of the pelvic brim.
Descent
Descent is almost a continuous movement throughout the first and second stages of labour. The gradual descent of the presenting part takes place because of uterine contraction and retraction. In the second stage, the bearing-down pains hasten the process resulting in complete expulsion.
Flexion
The fetal head is already flexed before the onset of labour in vertex presentation. Further, flexion occurs in the first stage when the head meets the resistance of the birth canal (pelvic floor to be precise consisting of levator ani muscle and other soft tissues) during descent.
Internal rotation
Internal rotation takes place when the head reaches the pelvic floor and meets with resistance. The disposition of the pelvic floor tends to rotate the leading part forward by causing torsion of the fetal neck. This movement carries the engaging diameter of the head into the anteroposterior diameter, which is the largest diameter of the pelvic outlet.
Extension
In the second stage of labour, two forces act on the head. Uterine contractions and the abdominal muscles push it downwards, while the pelvic floor muscles press it upwards and forwards. The downward and upward pressures counterbalance each other and the resultant force pushes the head forward. It cannot go forward as the nape of the neck is fixed against the symphysis pubis; the head therefore follows the curve of the birth canal by a process of extension.
Restitution
The fetal shoulder enters the pelvis in the left oblique diameter if the head descends with its suboccipitobregmatic diameter in the right oblique diameter. As the internal rotation takes place, the head is completely delivered and is free outside; it resumes its normal position with regard to the shoulders, turning the occiput towards the mother’s left thigh. This movement is called restitution, because by it the neck becomes untwisted and the head restores its natural relation to the shoulders.
External rotation
The shoulder now descends and the anterior shoulder being lower meets the resistance of the pelvic floor and so rotates forward, as did the occiput. The shoulders now occupy the anteroposterior diameter of the pelvis and as they rotate the head rotates with them. The occiput thus makes a further movement of one-eighth of a circle in the opposite direction of its internal rotation. The shoulders are then delivered, the anterior shoulder escaping under the pubic arch, while the posterior slides over the perineum.
The rest of the body is then expelled without difficulty as it is smaller than either the head or the shoulders.
Describe the conditions to be fulfilled to define normal labour.
In current practice, labour is considered normal if it meets following criteria: Pregnancy is singleton and has reached term. The fetus presents by vertex and labour starts spontaneously. Baby delivers vaginally without undue delay with or without minimal assistance (episiotomy/outlet forceps/vacuum). Mother and baby are healthy after the delivery.
Describe the physiological events and theories of onset of normal labour.
Please refer to Chapter 39 of Holland and Brews Manual of Obstetrics for answer.
Describe true and false labour pains.
True labour pain is intermittent and regular. It increases in frequency, duration and intensity over time. Pain is felt both in the back and in the front of the abdomen. It is associated with uterine contractions, progressive descent of the head, cervical effacement and dilatation. It is not relieved by enema, sedation or rest.
False labour pain is more common in the primigravida and is characterized by irregular uterine contractions of short duration with pain confined mostly to the lower abdomen, often relieved by sedatives. There is no dilatation of the cervical os. They are sometimes brought on by a digestive upset and are relieved by laxative.
Describe the stages of labour.
First stage
The first stage of labour is considered as the stage of cervical dilatation, during which effacement and dilatation of the cervix are initiated and completed. The end of the first stage is signalled by the full dilatation of the cervix (10 cm).
The first stage is generally divided into two phases (Fig. 10.2).
■ Latent phase: It is a variable but substantial period when little appears to be happening. In this period, the pains are not very distressing to the patient. The cervical dilatation progresses rather slowly. This lasts about 6–8 h.
■ Active phase: The pain becomes distressing to the patient. The contractions become more frequent, occurring every 3–5 min. They last longer, 45–60 s and the intensity is increased. The dilatation of the cervix reaches 4 cm and it undergoes important alterations that make it more responsive and dilatation proceeds rapidly. In primigravida the rate of dilatation is 1 cm per hour and in multigravida it is 1.5 cm per hour. The active stage lasts about 6 h in primigravida and 4 h in multigravida.
The active phase is sometimes further divided as the acceleration phase, the phase with the maximum slope of the curve and the deceleration phase.
Second stage
The second stage is considered as the stage of delivery of the fetus during which the fetus is forced through the birth canal into the outside world. It lasts from full dilatation of the cervix to the final birth of the baby. The uterine contractions last 60–90 s and occur every 2–3 min.
■ Bearing-down pain – These occur due to voluntary expulsive efforts by the patient, probably because of nerve reflexes being initiated by the stretching of the vaginal wall by the presenting part. The main expulsive effort is from the abdominal muscles and the diaphragm. They contract during the uterine contractions to push the baby down against the perineum.
■ Descent – The patient feels considerable pressure on her rectum and sometimes the pain radiates down her legs due to pressure on the sacral plexus and obturator nerve by the head, which descends into the hollow of the sacrum. A little later, the rectum dilates exposing its anterior wall. The head can now be seen advancing with each contraction, and although it retreats in between the contractions some advance is made with every contraction.
■ Crowning – Soon the perineum is stretched and the anus flattened by the head and with each contraction a larger segment of the head is visible. The head is said to be ‘crowned’ when its maximum diameter stretches the vulval outlet and does not recede in between contractions. With some extra effort the baby is now born.
The average duration of the second stage in a primigravida is 1–2 h and ½–1 h in a multigravida. The second stage of labour is further divided into following:
Third stage
The third stage is considered as the stage of delivery of placenta and membranes and it starts at the birth of the baby and ends with the complete expulsion of the placenta and membranes. As there is retraction of the uterus after the baby is born, the placental bed is reduced to one-third of its size in pregnancy. The placenta itself remains unchanged and, therefore, the shearing effect starts separating the placenta and causes retroplacental bleeding from the torn blood vessels in the intervillous spaces which separate the placenta further, the plane of separation being the deep spongy layer of the decidua basalis. Usually, the whole process takes no longer than 5–15 min. However, one may wait up to 30 min, in the presence of uterine contraction and retraction, before branding it as retained placenta.
Phases of placental separation (as studied by ultrasonography) are the following:
■ Latent phase – placenta-free wall contracts
■ Contraction phase – thickening of wall at placental site
■ Detachment phase – actual separation of placenta from the adjacent uterine wall
Methods of placental separation
Traditionally two methods have been described:
The signs of separation of the placenta are the following:
■ A fresh gush of blood, which occurs when the retroplacental blood finds its way to the vagina separating the membranes.
■ An apparent lengthening of the cord as the placenta after separation drops to the lower segment.
■ A suprapubic bulge, which occurs as the placenta, fills up the collapsed lower segment and stretches it. The contracted upper segment then rides over it.
Once these signs appear the placenta is usually delivered by controlled cord traction to prevent the inversion of the uterus.
Fourth stage
The fourth stage is considered as the stage of permanent retraction of the uterus. Some consider it as ‘golden hour’ when the obstetrician should be highly vigilant following the completion of the third stage of labour. This is necessary to avoid the development of complications during the phase. One must monitor the following:
■ The fundal height and uterine consistency to ensure that the uterus is well contracted, retracted and not relaxing
■ Vaginal bleeding – need not wait for 500 mL of blood loss to administer uterotonins
■ Maternal vital signs – pulse and blood pressure should be recorded every 15 min till stable
■ Urine out especially, if the patient is catheterized or having any complications such as preeclampsia and abruption
Duration of labour
Normal duration of labour varies a great deal from one patient to the other. The average duration of labour in primigravida and in multigravida is given in Table 10.1.
Table 10.1
| Primigravida (h) | Multigravida (h) | |
| First stage – latent phase | 6–8 | 4–6 |
| First stage – active phase | 6 | 4 |
| Second stage | 1–2 | ½–1 |
| Third stage | ¼–½ | ¼–½ |
| Total | 10–12 | 8–10 |
Write the management/conduct of first and second stage of labour.
Please refer to Chapter 45 of Holland and Brews Manual of Obstetrics for answer.
Write the active management of 3rd stage of labour.
Management of the third stage of labour
Though the third stage of labour is a natural process, it is advisable to follow principles of active management of the third stage of labour/prevention of postpartum haemorrhage which involves the following:
1. Administration of 10 units of oxytocin IM (oxytocin should NOT be given as IV bolus to avoid hypotension) either at the time of delivery of anterior shoulder (as mentioned in management of the second stage of labour) or within 1 min of the delivery of the fetus (NOT placenta).
2. Controlled cord traction (Brandt–Andrews Method) to deliver the placenta and membranes. It is better to wait for the signs of separation of placenta (Fig. 10.3).
3. Massaging the uterus: This need not be done routinely according to recent guidelines. However, as part of the protocol of prevention of postpartum haemorrhage, it is better to massage the uterus if it is taking time to contract and retract.
Examination of the placenta and membranes
The maternal surface is first inspected by holding the placenta on the cup formed by palmar surface (some advocate dome formed by dorsal surface) of the hands. The membranes, the chorion and the amnion are now checked for completeness by holding the umbilical cord and allowing the membranes to hang from the placenta like an inverted umbrella. Usually the rent in the membrane is away from the placental margins, if it is closer then placenta praevia is reconfirmed, additional rents and abnormal vessels running across the membrane, may indicate the presence of a succenturiate lobe of the placenta.
Suturing of episiotomy is performed (see Chapter 41 for details).
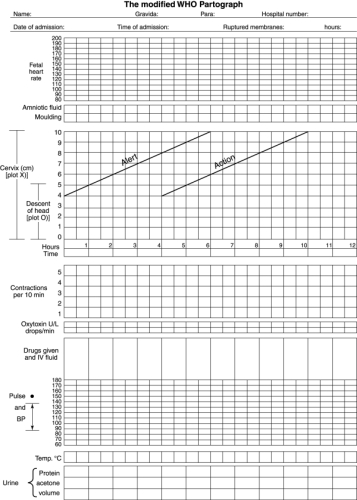
What is partogram? Describe the modified who partogram and the method of using the same.
Partogram is a graphical representation of the first-stage events in a single preprinted format. All events are pictorially represented on the time axis. It mainly focuses on cervical dilatation and fetal head descent. Progress of labour can be assessed at a glance. This record can be easily analysed and provides a basis for early recognition of any deviation from the normal.
Modified Who partogram (fig. 10.4)
In 2000, WHO made following changes to Philpott’s partogram:
■ Active phase started at 4 cm.
■ Descent of the head was recorded by abdominal examination.
■ Alert line and action line (4 h to the right) were made 4 h apart.
Components of the partogram are as follows:
■ Fetal heart rate (to be monitored every 15 min. See Table 8.2 for details)
■ Cervical dilatation and fetal head descent
■ Uterine contractions (to be checked every 10 min)
■ Oxytocic and other drugs administered
■ Maternal condition (vitals, urine output, urine protein ketones, etc.)
Amniotic fluid and moulding
Membrane status is recorded as follows:
Moulding is recorded as follows:
Cervical dilatation
The cervical dilatation is plotted in this component of the partogram. It is the most important component of the partogram in the diagnosis of prolonged/abnormal labour. The active phase starts at 4 cm dilatation and end at 10 cm. There are two lines in this component:
■ Alert line – drawn based on the rate of cervical dilatation in primigravida – 1 cm/h.
■ Action line – this line is parallel and is 4 h to the right of alert line.
Plotting the cervical dilatation – The plotting is started only when the cervix is 4 cm dilated. Zero hour begins at 4 cm dilatation for a patient who is already in the labour before 4 cm dilatation. However, when a patient comes to labour room with already 5 cm dilatation it should be recorded on the alert line and not on the zero-hour line, or else her cervical dilatation graph may not cross the alert line even if the cervix is dilating slowly.
Station of the head
The descent of the head is recorded as fifths of the head above the brim as described by Crichton (Fig. 10.5). The descent of the head is assessed at the time of a vaginal examination and the number of fifths of the head above the brim is plotted on lines 0–5. In this way, a slope of the descent of the head is constructed.
Uterine contractions
Below the timeline, there are five blank squares going across the length of the graph. Each square represents one contraction. Based on the type of shading and the number of squares shaded, one can make out the normalcy/abnormality of contractions (Fig. 10.6).
Oxytocics and other drugs
The concentration of oxytocin is noted on the upper line and the rate of the infusion in drops per minute on the bottom line from the time the intravenous drip starts is also noted. Record of other drugs administered should also be made.
Maternal condition
The blood pressure is recorded every 2 h and the pulse every 30 min. The maternal temperature is recorded in the bottom line.
Each time the patient passes urine the amount is measured and noted. The urine sample is checked for the presence of ketones and protein. If catheterization is performed, it is recorded as a C.
What are the active phase disorders and how are they managed?
Please refer to Chapter 44 of Holland and Brews Manual of Obstetrics for answer.
What are the advantages and limitations of the partogram?
Please refer to Chapter 44 of Holland and Brews Manual of Obstetrics for answer.