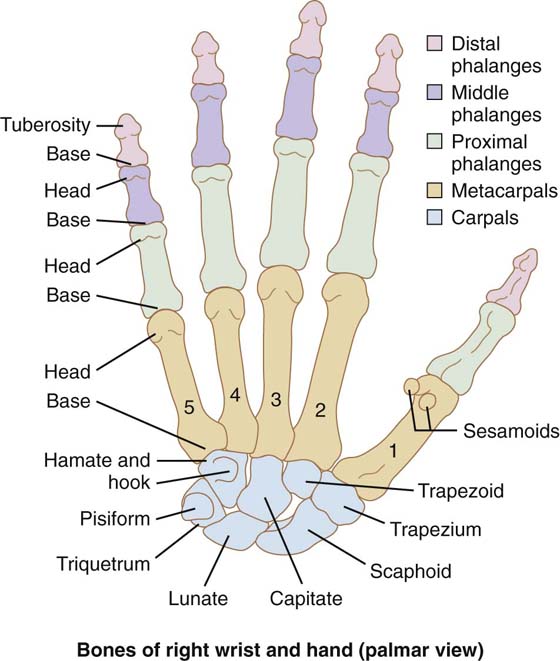
Figure 1-1 Volar view of the bones of the hand and wrist. Note that the thumb is rotated approximately 90 degrees relative to the rest of the digits.
SKIN, RETINACULAR SYSTEM, AND COMPARTMENTATION OF THE HAND
▪ The hand can assume almost countless positions and postures that allow it to perform numerous functions and manipulations.
▪ The muscles of the hand permit it to perform tasks that require both great strength and delicate precision.
▪ The skin of the hand, particularly that of the palm, is richly supplied with a large variety of sensory receptors that allow it to detect minute differences in texture and shape.
▪ The joints and muscles of the hand contain large numbers of proprioceptive receptors that enable it to detect miniscule differences in position and thus perform precise manipulations extremely smoothly.
The bones of the hand form its framework and are important in maintaining its shape and providing a stable base on which to anchor its various soft tissue structures. The bones are arranged to maximize the functional efficiency of the intrinsic muscles and the tendons of the extrinsic muscles of the hand. The 19 major bones are of only two types: the metacarpals and the phalanges (Fig. 1-1). All of these bones are classified as long bones and have central shafts and expanded proximal and distal ends (epiphyses). Additional small bones, sesamoids, are usually found in the tendons of certain intrinsic thumb muscles.
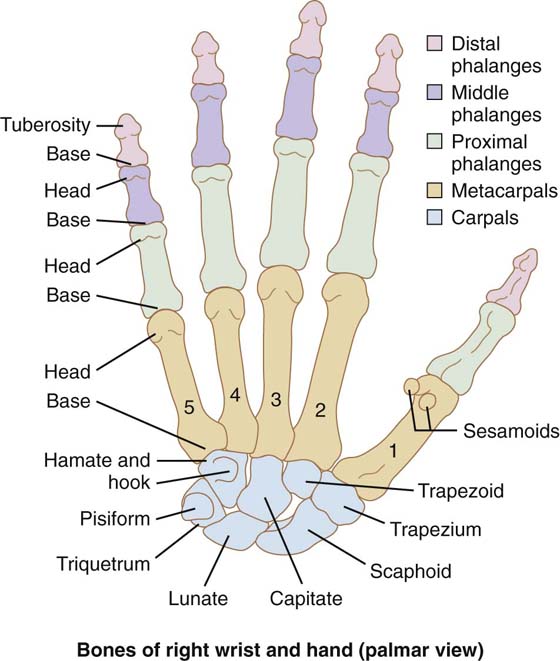
Figure 1-1 Volar view of the bones of the hand and wrist. Note that the thumb is rotated approximately 90 degrees relative to the rest of the digits.
One metacarpal is associated with each digit, that of the thumb being considerably shorter than the others. These bones form the bony base of the hand, and their integrity is essential for both its natural form and function. Each bone has a dorsally bowed shaft with an expanded base (proximally) and head (distally) (Fig. 1-2). From closely positioned bases, the bones diverge distally to their heads. This arrangement determines the shape of the hand and separates the digits so they can function independently as well as manipulate large objects. The metacarpal of the thumb is anterior to the others and rotated approximately 90 degrees so it is ideally positioned to oppose (see Fig. 1-1).
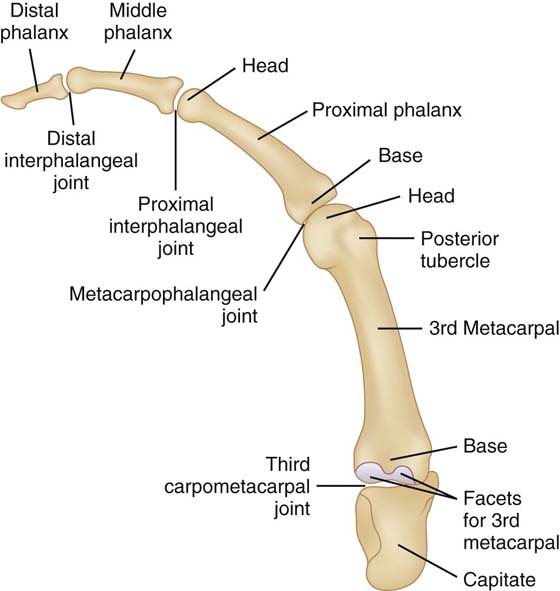
Figure 1-2 Lateral view of the middle finger and the capitate. Note the dorsal convexities of the metacarpal and proximal and middle phalanges.
The shaft of each metacarpal is triangular in cross section, with the apex of this triangle directed volarly and composed of more dense bone than the dorsal aspect of the shaft.1 This concentration of dense bone reflects the significant compressile force on the flexor side of the bone. The overall shape of each metacarpal (along with that of the phalanges) contributes to the longitudinal arch of the hand. The dorsal convexities of the metacarpals along with their triangular cross sections provide significant room for the soft tissue of the palm, the bulk of which consists of the intrinsic interossei muscles and the more volarly positioned long digital flexor tendons and accompanying intrinsic lumbrical muscles. The mechanical advantage of these muscles is also enhanced by the metacarpal shape; their lines of pull are located volar to the flexion–extension axes of the metacarpophalangeal (MCP) joints.
The bases of the four medial metacarpals are irregular in shape and less wide volarly than dorsally, thus contributing to the proximal transverse arch (Fig. 1-3). Articular surface is found on the sides as well as the proximal aspect of the base. The base of the thumb metacarpal is significantly different. The somewhat flattened proximal surface is in the shape of a shallow saddle, all of which is articular surface. The concave surface is oriented from medial to lateral; the convex from anterior to posterior. (Keep in mind that this bone is rotated about 90 degrees relative to the other metacarpals and this description is based on the anatomic position.) The most medial aspect of the base protrudes more proximally than the rest of the base and thus presents a triangular beak.
The heads of all the metacarpals are similar. The articular surface is rounded, both from side to side as well as dorsal to palmar. The side-to-side dimension is considerably shorter than the length from dorsal to palmar, but it is wider on the palmar aspect than it is dorsally. And importantly, the surface extends farther onto the volar aspect of the bone than dorsally. Prominent dorsal tubercles are found dorsally on each side of the head, just proximal to the articular surface.
The shapes of the metacarpals also contribute to the proximal and distal transverse arches of the hand (see Fig. 1-3). The proximal arch is at the level of the distal row of carpal bones and the bases of the metacarpals. The bases of the metacarpals as well as the distal row of carpals are wedge-shaped in cross section, and the apex of each wedge is directed volarly. Since the metacarpal bases and distal carpals are positioned very close to one another and are held tightly together, they collectively form a dorsal convexity and thus a side-to-side arch. The distal transverse arch is at the level of the metacarpal heads and is also a dorsal convexity. This arch is larger than the proximal arch and merely reflects the orientation of the metacarpals and the fact that the metacarpal heads are farther apart than their bases.
The hand contains 14 phalanges; the thumb has only 2, whereas each of the other digits has 3. The proximal and middle phalanges, like the metacarpals, are bowed dorsally along their long axis and thus contribute to the longitudinal arch of the hand. The shafts of the phalanges serve as anchors for the long digital flexor tendons. The volar aspect of the shaft is flat from side to side and rounded dorsally. The junctions of the rounded and flat surfaces are marked by longitudinal ridges that serve as the attachments for the fibrous part of the digital tendon sheath (see Fig. 1-1). Each bone has an expanded epiphysis on each end, with the base (proximally) being larger than the head (distally).
The surface of the base of the proximal phalanx is biconcave and consists entirely of articular surface. The bases of both the middle and distal phalanges are concave from dorsal to ventral, with a central ridge oriented in the same direction. This surface is entirely articular surface. The heads of the proximal and middle phalanges are cylindrical from side to side with a central groove oriented perpendicular to the cylinder. This surface is also articular surface. The distal phalanx is shorter than the others. It has no head but rather ends in an expanded and roughened palmar elevation, which supports the pulp of the fingertip as well as the fingernail.
The carpometacarpal (CMC) joints are the most proximal joints in the hand and connect it to the wrist. Even though they are all synovial joints, the thumb CMC joint is significantly different from those of the four medial digits. The CMC joint of the thumb allows significant and complex motion; those of the other digits allow a small amount to virtually none.
The four medial joints are between the bases of the four medial metacarpals and the distal row of carpal bones: the trapezium, trapezoid, capitate, and hamate. The articular surfaces of both sets of bones are irregular, continue on the medial and lateral aspects of the metacarpal bases and the carpals, but are quite congruent so the bones fit closely together. Each metacarpal base articulates with one, two, or even three carpal bones. Strong ligaments hold all of the bones tightly together, both side to side and across the CMC joint space. A single joint capsule encloses all of these joints so there is a single synovial cavity. This cavity extends not only across the span of the collective joints but also somewhat distally between the metacarpal bases and proximally between the distal carpal bones.
The motion available at these joints is variable and minimal. There is essentially no motion permitted at the CMC joints of the index and middle fingers. These two metacarpals along with the distal carpal row form the rigid and stable central base of the hand. A small amount of motion is permitted at the CMC joints of the ring and small fingers. This motion, primarily a bit of flexion, permits slight cupping of the medial side of the hand and is important in both manipulation and grip (Fig. 1-4).
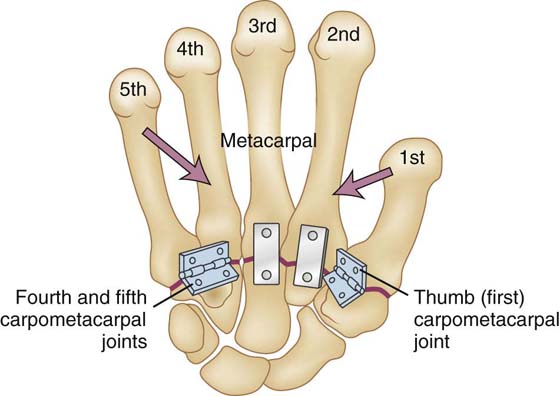
Figure 1-4 Volar view of the metacarpal and carpal bones of the right hand, showing the relative motion of the five carpometacarpal joints. Note that there is more motion at the thumb, ring, and little finger joints than at the index and middle fingers.
The first CMC (trapeziometacarpal) joint is between the base of the first metacarpal and the trapezium. Since the thumb articulates with only the trapezium, its location and orientation is the basis for the position of the thumb. The trapezium is obliquely oriented, almost in the sagittal plane, and projects more volarly than the trapezoid or scaphoid with which it articulates.
The articular surfaces (Fig. 1-5) of both the base of the first metacarpal and the distal aspect of the trapezium are shaped like shallow saddles. As a result, each surface has a convex and a concave component, and these elements are perpendicular to one another. The shapes dictate that the major amount of motion occurs in two planes, which also are perpendicular to one another. Motion in the coronal plane, where the thumb moves across the palm, is flexion and extension. These motions occur as the concave surface of the metacarpal base moves on the convex surface of the trapezium. Motion in the sagittal plane, where the thumb moves toward and away from the index finger, is adduction (toward) and abduction (away). This occurs as the convex surface of the metacarpal base moves on the concave surface of the trapezium. Since both saddles are shallow and the soft tissue restraints are somewhat lax, axial rotation is also permitted. This rotation, opposition (pronation), occurs primarily at this first CMC joint and represents an essential ingredient for the usefulness of the thumb. Retroposition (supination) is the opposite of opposition. In reality, certain motions are coupled. Abduction is accompanied by a bit of medial rotation (opposition). This is due to the slightly curved concave surface of the trapezium. Retroposition, then, is a combination of lateral rotation and adduction. Flexion and extension also involve some rotation, albeit less. Flexion is accompanied by a bit of opposition and extension by a bit of retroposition.2 This is caused by the slightly curved convex surface of the trapezium. Hanes3 suggested the coupling was due to the tautness of certain of the ligaments of the joint; Zancolli and colleagues4 considered the coupling was due both to the articular surfaces and the ligaments.
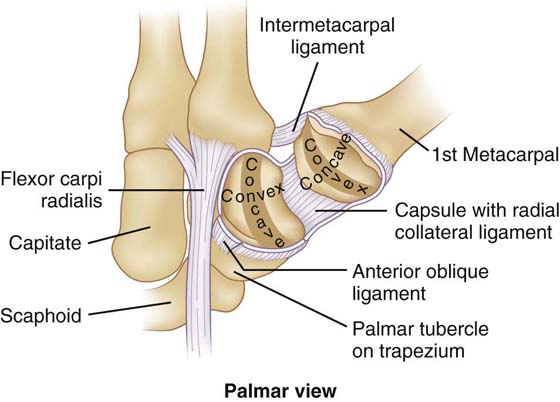
Figure 1-5 Palmar view of the carpometacarpal joint of the right thumb. The joint is open and the metacarpal reflected radially. Note the saddle-shaped articular surfaces of both bones and the concave and convex aspects of each.
The ligaments (Figs. 1-6 and 1-7) of this joint are found on all sides of the joint. Their nomenclature can be confusing because several systems are used to name them and there are differences of opinion relative to how many ligaments there are. The anterior oblique, or beak, ligament is a strong ligament that interconnects the palmar tubercle (beak) of the metacarpal base and the distal part of a ridge on the tubercle of the trapezium. This ligament is generally considered a major stabilizing ligament of the joint and is taut in abduction, extension, and opposition.5 Bettinger and coworkers6 described a superficial anterior oblique ligament and a deep anterior oblique ligament, which they considered the beak ligament. The ulnar collateral ligament is on the volar and medial aspects of the joint and extends from the transverse carpal ligament to the palmar-medial aspect of the first metacarpal base. The posterior oblique ligament is on the dorsal aspect of the joint and interconnects the dorsal aspect of the trapezium and the ulnar (medial) base of the metacarpal. An intermetacarpal ligament (or pair of intermetacarpal [anterior and posterior] ligaments) interconnects the bases of the first and second metacarpals. The dorsoradial ligament extends from the dorsolateral aspect of the trapezium to the dorsal base of the first metacarpal. The joint capsule is complete and somewhat loose, which is necessary for axial rotation.
The metacarpophalangeal (MCP) joints (Fig. 1-8) of the four medial digits are formed by the bases of the proximal phalanges and the heads of the metacarpals. The articular surface of the metacarpal head is biconvex, cam-shaped so it extends farther volarly than dorsally, and it is wider volarly than dorsally. The articular surface of the phalangeal base is biconcave, shallow and smaller in area than the articular surface of the metacarpal head. These shapes would appear to permit the phalanx to move in virtually any plane on the metacarpal head. However, due to soft tissue restraints, active motion is limited to flexion and extension and adduction and abduction. Adduction is movement of the digits toward the middle finger; abduction is movement away from the middle finger. The middle finger can be deviated either radially (laterally) or ulnarly (medially). Axial rotation is available only passively.
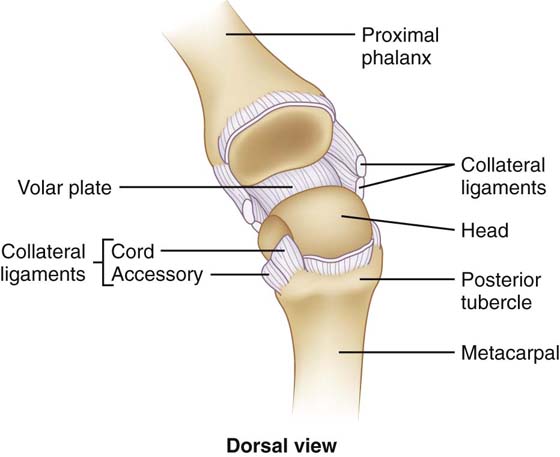
Figure 1-8 Dorsal view of the metacarpophalangeal joint that is opened dorsally to show the articular surfaces. Note the biconvex metacarpal head and the biconcave proximal phalangeal base.
The joint capsule of the MCP (Fig. 1-9) joint is highly specialized. Like any capsule it encloses the joint space and attaches to the edges of both articular surfaces. It is different in that its volar aspect is formed by a strong plate of fibrocartilage—palmar ligament, or volar plate. The medial and lateral edges of the plate serve as attachments for the fibrous part of the digital tendon sheath, specifically the first annular ligament (A1 pulley). Thus, the plate is important in the stability and positioning of the long digital flexor tendons. The plate is thick and rigid distally and its volar aspect has a thin side-to-side attachment to the volar base of the proximal phalanx. This hingelike attachment allows the plate to move as a unit relative to the proximal phalanx. Proximally the plate thins, is a bit loose and flexible, and attaches to volar base of the metacarpal head. With flexion the volar plate slides proximally (Fig. 1-10); this is possible because the proximal part of the plate can fold.
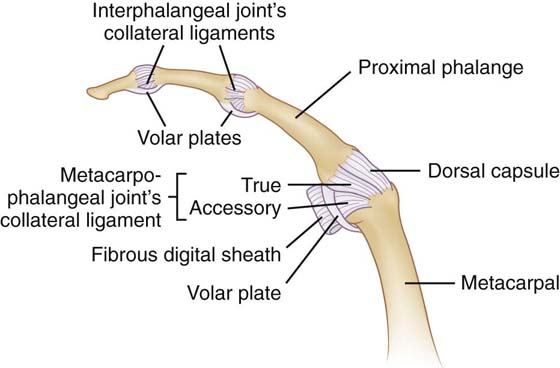
Figure 1-9 Lateral view of the joint capsules of the metacarpophalangeal and interphalangeal joints of a finger.
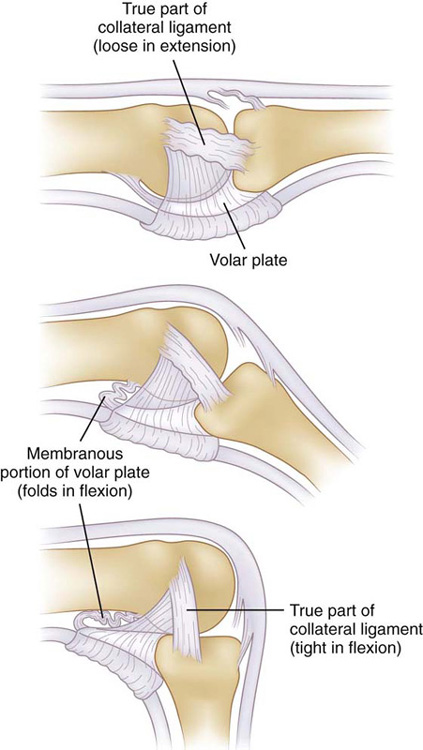
Figure 1-10 Lateral view of the metacarpophalangeal joint of a finger. The band part of the collateral ligament and the volar plate are depicted in full extension, partial flexion, and flexion. Note how the tension of the band part of the ligament changes as the proximal phalanx is flexed. Note also how the proximal part of the volar plate folds as flexion occurs.
The collateral ligament (see Fig. 1-10) is triangular in shape and consists of two distinct parts, both of which attach proximally to the dorsal tubercle of the metacarpal. From that attachment, the fibers of the ligament diverge as they pass distally. The true, or band, part of the ligament extends more distally and is the strongest part of the ligament. From the dorsal tubercle it passes obliquely volarly and attaches to the volar aspect of the side of the proximal phalangeal base. This true ligament is somewhat loose in extension and thus permits abduction and adduction. As the proximal phalanx is flexed, this part tightens because of the cam shape of the metacarpal head and because the metacarpal head is wider volarly. As a result of the tightness, abduction and adduction are very limited in flexion. The accessory, or fan, part of the ligament is more obliquely oriented and attaches to the volar plate. Since the fibrous tendon sheath also attaches to the volar plate, the accessory collateral ligament plays an important role in stabilizing the long digital flexor tendons. The accessory ligament loosens slightly as flexion occurs.
The MCP joints are reinforced dorsally and laterally by the extensor hood (see Fig. 1-20, online). This hood consists of a flat layer of fibers that is oriented perpendicular and oblique to the long axis of the digit and sweep around the joint from one edge of the volar plate to the other. The fibers on either side of the joint are in the sagittal plane and called the sagittal bands. The hood blends with the long digital extensor tendon, slides proximally and distally, respectively, with extension and flexion, and is the mechanism through which the proximal phalanx is extended. The hood is also important in centralizing the extensor tendons at the MCP joint.
The MCP joint of the thumb is both similar to and different from the other MCP joints. The articular surfaces and collateral ligaments are quite similar. In general, the joint capsule is similar but part of it, the volar plate, varies. The volar plate contains two sesamoids bones, which form a trough for the tendon of the flexor pollicis longus muscle. The sesamoids are also partial insertions for the adductor pollicis muscle on the ulnar side and the flexor pollicis brevis muscle on the radial side. The more superficial layer of fibrous support is a somewhat modified extensor hood. The ulnar side of the hood is stronger and heavier than the radial side and formed by the tendon and aponeurosis of the adductor pollicis muscle. It extends dorsally to blend with the tendons of the extensor pollicis brevis and extensor pollicis longus muscles. The radial side of the hood is formed by the tendons of the abductor pollicis brevis and flexor pollicis brevis, which also blend with the extensor pollicis brevis and extensor pollicis longus tendons dorsally. The aponeurosis on the ulnar side forms a strong restraint against abduction forces. However, since the thumb is in a different plane than the other digits it is more vulnerable to adduction and abduction forces.
The motion available at the thumb MCP is similar in direction to the other MCP joints but more limited because of the stability of the joint. Flexion and extension are less free, and adduction and abduction are significantly more limited. However, motion varies considerably from person to person so possible limitation should be compared with motion on the opposite side.
The proximal interphalangeal (PIP) joint (Fig. 1-11) is formed by the head of the proximal phalanx, which is shaped like a short transverse cylinder, and the base of the middle phalanx, which is concave from dorsal to ventral and thus conforms to the cylindrical head. In addition, the phalangeal head has a sagittally oriented groove and the phalangeal base has a sagittally oriented ridge. These surfaces enhance the stability of the joint and ensure that the motion is limited to one degree of freedom, which is in the sagittal plane (flexion and extension).
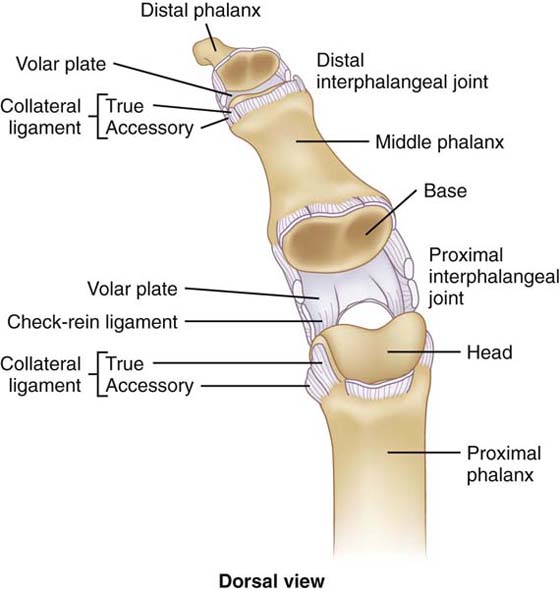
Figure 1-11 Dorsal view of the interphalangeal joints of a finger. The joints are opened dorsally to view the articular surfaces. Note the sagittal groove of the phalangeal heads and the sagittal ridge of the phalangeal bases.
The joint capsule is similar to that of the MCP joint. It is reinforced by the volar plate palmarly, the collateral and retinacular ligaments and the lateral bands on both sides, and the triangular membrane and central band dorsally. These structures blend with the capsule to different degrees and thus move (glide) differently relative to the capsule and to each other.
The volar plate (Fig. 1-12) is similar to that of the MCP joint and moves in the same way during flexion and extension. The sides of the proximal attachment are longer than the central part and are referred to as the “check-rein ligaments.”7 These ligaments tighten as the middle phalanx is extended and thus limit hyperextension at the PIP joint. The volar plate is also the attachment for the third annular ligament (A3 pulley) of the fibrous flexor digital tendon sheath. This pulley attaches along the sides of the plate and ensures the flexor tendons stay in place as they cross the joint. The stability of this plate is therefore essential for proper flexor tendon position and function.
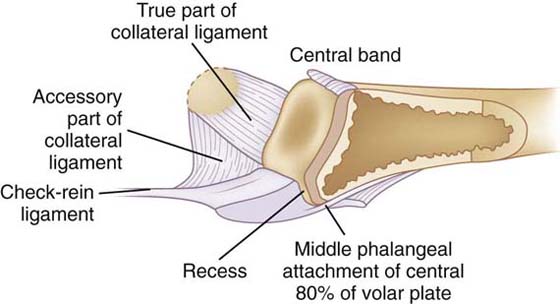
Figure 1-12 Sagittal view of the proximal aspect of the middle phalanx and volar plate of the proximal interphalangeal joint. Note that only one half of the volar plate is depicted.
The collateral ligaments (see Figs. 1-11 and Fig. 1-12) are similar to those of the MCP joints, are triangular in shape, and consist of true (band) and accessory (fan) parts. From their attachment to the dorsal tubercle of the proximal phalanx, the two parts diverge as they cross the joint—the true part attaching to the side of the base of the middle phalanx and the accessory part attaching to the volar plate. The true part is taut throughout the range of motion and thus stabilizes the joint in all positions; the accessory part stabilizes the volar plate.
Like the MCP joints, the PIP joints are reinforced to some degree by components of the extensor mechanism. The central band and triangular membrane are positioned dorsally, and the lateral band and retinacular ligament located on the sides. The tendons of both the flexor digitorum profundus and flexor digitorum superficialis pass volar to the joint.
The distal interphalangeal (DIP) joint is quite similar to the PIP joint. The architecture of the articular surfaces is similar, so the motion is limited to only the sagittal plane and that is flexion and extension. The joint capsule, volar plate, and collateral ligaments are also similar, so the motion of each and the support they provide are very much the same as the PIP joints. The volar plate provides an attachment for the fibrous part of the flexor digital tendon sheath; in this case it is the fifth annular ligament (A5 pulley).
The extra-articular structures that cross the joint are quite different. Only the tendon of the flexor digitorum profundus crosses its volar aspect. Dorsally, only the central band blends with the joint capsule as it crosses the joint.
The skin on the dorsum of the hand is different from that on the palmar aspect. The dorsal skin is thin, loose, and quite mobile. This mobility is due to a very thin subcutaneous tissue (superficial fascia) that is loosely attached to the deep fascia. The palmar skin is thicker and less mobile. The subcutaneous tissue of the thenar and hypothenar eminences is thick and fatty and thus forms considerable pads. Centrally the palmar skin is firmly attached to the palmar aponeurosis by multiple septa and is thus almost immobile. This arrangement greatly enhances grasp.
The entire upper limb is enclosed in a sleeve of connective tissue called the investing fascia. In the arm and forearm this layer is connected medially and laterally to the bones by intermuscular septa with resulting anterior and posterior compartments. This same layer continues into the hand, where it becomes a complex system of fibrous layers and septa that form multiple compartments. Structures of similar function are isolated and confined to individual compartments. Since a retinaculum is a structure (usually composed of connective tissue) that retains other anatomic structures, this is called the retinacular system.
At the wrist the investing fascia is reinforced by circumferential bands of fibers both dorsally (extensor retinaculum) and volarly (flexor retinaculum). Both of these retinacula stabilize tendons that enter the hand from the forearm. The flexor retinaculum has a more proximal superficial part, the superficial part of the flexor retinaculum or the volar carpal ligament, and a deeper distal part called the deep part of the flexor retinaculum or the transverse carpal ligament. The deep part forms the volar boundary of the carpal tunnel and is significantly thicker and stronger.
In the hand the investing fascia attaches to both the first and fifth metacarpals (Fig. 1-13). Dorsally it is thin, attaches to the other metacarpals, and is called the dorsal interosseous fascia. In the palm it is thin over the thenar (thenar fascia) and hypothenar (hypothenar fascia) eminences. Centrally it is greatly thickened to form the palmar aponeurosis.
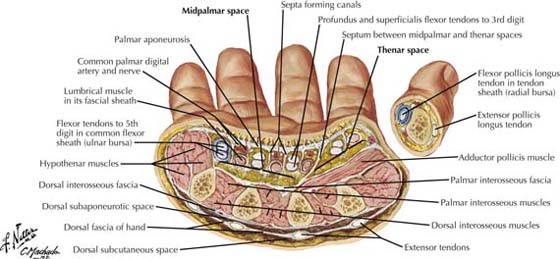
Figure 1-13 Transverse section through the palm of the hand. (Netter illustration from www.netterimages.com. © Elsevier Inc. All rights reserved.)
This palmar aponeurosis (palmar fascia) is a strong fibrous structure composed of fibers that are oriented from proximal to distal. It is narrow proximally where it is continuous with the tendon of the palmaris longus muscle and blends with the transverse carpal ligament. It widens as it is followed distally, and just proximal to the MCP joints it separates into four digital slips, which contribute to the formation of the fibrous digital tendon sheaths. The digital slips are interconnected by transverse fasciculi proximally and the transversely oriented superficial transverse metacarpal ligament at the level of the MCP joints. The palmar aponeurosis is firmly attached to the skin by multiple septa and to the metacarpals by several septa.
Additional fibrous layers separate various structures in the palm and define four definitive compartments. The thenar septum extends from the junction of the thenar fascia and the palmar aponeurosis to the first metacarpal and with the thenar fascia forms the thenar compartment. Similarly, on the ulnar side of the hand, the hypothenar septum extends from the junction of the hypothenar fascia and the palmar aponeurosis to the fifth metacarpal and with the hypothenar fascia forms the hypothenar compartment. A deep layer crosses the palm, attaching to the first, third, fourth, and fifth metacarpals. This adductor–interosseous fascia, together with a dorsal interosseous fascia that interconnects all of the metacarpals dorsally, forms the adductor–interosseous compartment, which more or less is between the metacarpals. The central area of the palm, the central compartment, is deep to the palmar aponeurosis, bounded medially and laterally by the hypothenar and thenar septa, respectively, and limited deeply by the adductor–interosseous fascia. Like the compartments in the arm and forearm, these compartments contain muscles that have similar function and are innervated by one or two nerves. The contents of the compartments are listed in Table 1-1 (online).
Table 1-1 Contents of the Compartments of the Hand
Compartment |
Contents |
Thenar |
Flexor pollicis brevis, abductor pollicis brevis, opponens pollicis, tendon of flexor pollicis longus, radial bursa |
Hypothenar |
Flexor digiti minimi, abductor digiti minimi, opponens digiti minimi |
Adductor–interosseous |
All (4) dorsal interossei, all (3) palmar interossei, adductor pollicis |
Central |
All (4) lumbricals; tendons of flexor digitorum superficialis and profundus, ulnar bursa; superficial palmar arterial arch |
In addition to these literal compartments that contain muscles and other structures, some potential spaces are fascial planes, bursae, or synovial tendon sheaths. These structures normally enhance movement between adjacent structures. However, these potential spaces can become actual spaces when they accumulate blood or inflammatory material, which would, in each case, produce a characteristic swelling.
The thenar and midpalmar clefts (Figs. 1-13 and 1-14), or spaces, are in a fascial plane between the long digital flexor tendons and the adductor–interosseous fascia. This plane is separated into ulnar midpalmar and radial thenar space by the midpalmar septum that extends between the palmar aponeurosis and the third metacarpal. The thenar space is located on the volar aspect of the adductor pollicis muscle; the midpalmar space on the volar aspects of the medial interossei muscles.
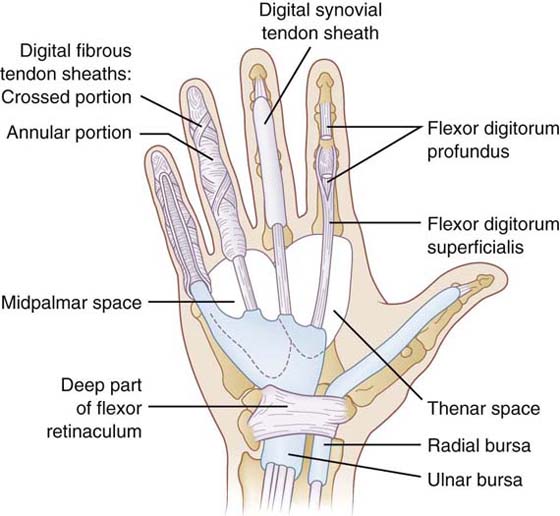
Figure 1-14 Volar view of the hand and wrist depicting the radial and ulnar bursae, digital tendon sheaths, and the thenar and midpalmar spaces.
The radial and ulnar bursae (see Fig. 1-14) are parts of the synovial tendon sheaths of the long digital flexor muscles. The radial bursa is associated with the flexor pollicis longus muscle and extends from just proximal to the carpal tunnel to the distal phalanx of the thumb. The ulnar bursa is associated with all eight tendons of the flexor digitorum superficialis and profundus muscles in the palm but continues distally into the digit with only those to the little finger. This bursa extends from proximal to the carpal tunnel into the palm and distally to the distal phalanx of the little finger. Digits two, three, and four have individual synovial digital tendon sheaths that extend from just proximal to the MCP joints to the distal phalanges. Each of these can also become enlarged.
On the dorsum of the hand there are two potential planes (see Fig. 1-13) where fluid can collect: one in the subcutaneous tissue and the other associated with the long extensor tendons. The subcutaneous tissue is dorsal to the metacarpals and contains the long digital extensor tendons, cutaneous nerves, dorsal venous network, and most of the afferent lymphatics from the hand. Since these lymphatics drain most of the hand, inflammation in virtually any part of the hand can lead to a general swelling on the dorsum of the hand. The long extensor tendons, aside from those to the thumb, are enclosed by supratendinous and infratendinous layers of fascia. These two layers unite on both sides of the group of tendons, thus forming a type of compartment around the tendons. Since the tendons do not occupy the entire side-to-side dimension of the dorsum of the hand, the subcutaneous plane is wider than the tendon plane.
The intrinsic muscles (Figs. 1-15 and 1-16) are those small muscles that both arise and insert within the hand and generally are involved in the finer movements of the digits. With the exception of the palmaris brevis, these muscles are found in the compartments of the hand, and those of each compartment have similar actions. The palmaris brevis is found in the subcutaneous tissue of the palm on the ulnar side at the base. This variable muscle extends from the ulnar side of the palmar aponeurosis to the skin of the medial hand. It is supplied by the superficial branch of the ulnar nerve and pulls the medial skin radially, which aids in grasp.
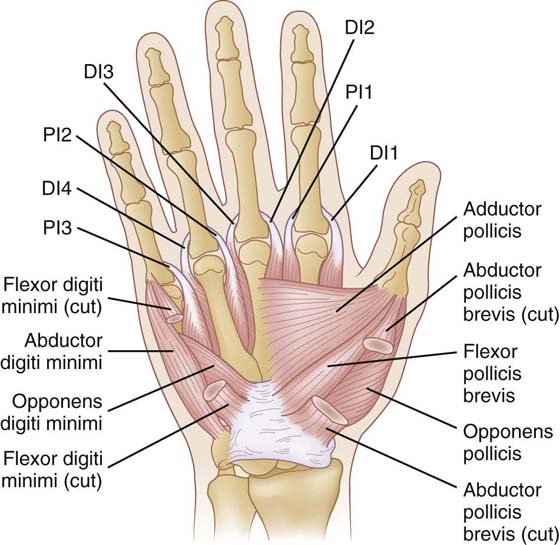
Figure 1-16 Volar view of the deep muscles of the hand. DI, dorsal interosseous; PI, palmar interosseous.
The thenar compartment contains three of the four intrinsic thumb muscles, and all three are supplied by the recurrent (thenar, motor) branch of the median nerve. The abductor pollicis brevis is superficial and volarly positioned, arising from the transverse carpal ligament and the trapezium and inserting on the ventral aspect of the base of the proximal phalanx of the thumb. It abducts the thumb; that is, moves it away from the index finger in the sagittal plane. The flexor pollicis brevis is in the same plane as the abductor and more medial in position. It arises from the transverse carpal ligament and trapezium and inserts on the ventromedial base of the thumb’s proximal phalanx. It flexes (coronal plane) both the thumb metacarpal and proximal phalanx. The opponens pollicis is the deepest of the three muscles and covers a good part of the shaft of the first metacarpal. From an origin on the transverse carpal ligament and trapezium its fibers pass radially and insert on a line along the volar aspect of the metacarpal. Since its fibers are oblique and it has a linear attachment to the metacarpal, the muscle is ideally positioned to produce axial rotation (opposition) of the metacarpal.
The muscles in the hypothenar compartment are similar to those of the thenar compartment and produce similar motions. All three of these muscles are supplied by the deep branch of the ulnar nerve. The abductor digiti minimi is the most medial in position and extends from the pisiform to the medial aspect of the base of the fifth proximal phalanx. It abducts the little finger at the MCP joint (moves the digit away from the middle finger). The flexor digiti minimi is positioned volarly and laterally. From its origin on the hook of the hamate and the transverse carpal ligament, it extends distally and a bit medially to insert on the medial base of the fifth proximal phalanx. This muscle flexes the little finger at the MCP joint. The opponens digiti minimi arises from the hook of the hamate. Its fibers diverge as they pass medially and distally, crossing the metacarpal obliquely, and insert along a line on the medial shaft of the fifth metacarpal. This muscle is in an ideal position to rotate the fifth metacarpal but due to the limited motion at the CMC joint it produces only a small amount of cupping of the medial aspect of the hand.
The central compartment contains the four lumbrical muscles. Each muscle arises from the flexor digitorum profundus tendon on its ulnar side or from both tendons between which it is positioned. The muscles pass distally, cross volar to the flexion–extension axes of the MCP joints, then insert into both the central and lateral bands of the extensor mechanism. Their actions are to produce flexion at the MCP joints and extension at both the PIP and DIP joints. The mechanism of these functions is more fully explained in the section on the extensor mechanism. The innervation of these muscles is similar to that of the flexor digitorum profundus muscle: the two ulnar muscles are supplied by the ulnar nerve; the two radial by the median.
The adductor–interosseous compartment contains all of the interossei muscles as well as an intrinsic thumb muscle, the adductor pollicis. All of these muscles are supplied by the deep branch of the ulnar nerve. The adductor pollicis is the largest of the intrinsic muscles and the only thumb intrinsic not in the thenar compartment. It has two heads: an oblique head, which arises from the lateral distal carpals and adjacent bases of the metacarpals and a transverse head, which arises from the shaft of the third metacarpal. The fibers from this wide origin converge and insert on the ventromedial base of the proximal phalanx of the thumb. This is the major muscle with the capability of adducting the thumb, that is, moving it toward the index finger.
The palmar and dorsal interossei muscles are found between the metacarpals and are responsible for adducting and abducting the four medial digits. Since the middle finger is the reference for this motion, the location and attachments relative to that finger determine their actions. The palmar interossei are the adductors (PAD) and the dorsal are the abductors (DAB). The interossei are also part of the extensor mechanism so they, like the lumbricals, produce flexion at the MCP joints and extension at both the PIP and DIP joints.
The three palmar interossei are positioned so they move the index, ring, and little fingers toward the middle finger. Hence, they arise from the lateral aspects of the fourth and fifth metacarpal shafts and the medial aspect of the second metacarpal shaft. They pass distally dorsal to the deep transverse metacarpal ligament but volar to the flexion–extension axis of the MCP joints and insert into both the central and lateral bands of the extensor mechanism. An insertion on the base of the proximal phalanx is variable.
Even though the four dorsal interossei are associated with the motion of only the index, middle, and ring fingers, they arise from all five metacarpals. Each of these muscles has two heads of origin so each muscle arises from the sides of adjacent metacarpal shafts. The muscles cross the MCP joints volar to the flexion–extension axes, insert into the sides of the bases of the proximal phalanges, and continue to insert into both the central and lateral bands of the extensor mechanism. The middle finger has two dorsal interossei, which deviate the finger medially and laterally; both of these motions are really abduction because they are moving the digit away from the central reference point.
The extrinsic muscles of the hand are those muscles that arise in the forearm and insert within the hand. These muscles, the long digital flexors and extensors, have muscle bellies located within the forearm and long tendons that cross the wrist and continue into the digits. These tendons have long courses through the hand, and their relationships and surrounding structures are constantly changing as they are followed from the wrist and into the digits. Since they are commonly injured, it is important to understand their relationships along their courses because different adjacent structures may be injured along with the tendons themselves and present different clinical issues. A general comparison of the long digital flexor and extensor tendons is presented in Table 1-2 (online).
Table 1-2 Comparison of Long Digital Flexor and Extensor Tendons
Flexor Tendons |
Extensor Tendons |
Cross section: large and oval or round |
Cross section: small, flat, and thin |
Connected to muscles of significant mass: some of pennate construction → power |
Connected to muscles of lesser mass: all parallel construction → extension and positioning |
Deeply positioned and thus protected in palm: significant tissue between skin and tendons. Fascial plane between tendons and metacarpals |
Very superficially positioned: minimal subcutaneous tissue between skin and tendons. Fascial plane between tendons and metacarpals |
Strongly attached and anchored to the volar aspects of the phalanges by fibrous digital tendon sheaths |
Centralized and held in position by system of fibrous bands called the extensor aponeurosis or mechanism |
Have synovial tendon sheaths along the digits |
No synovial sheaths along digits |
Tendons come together in common compartment (carpal tunnel) as they cross wrist |
Tendons in multiple compartments as they cross wrist: each compartment contains tendons of one or two muscles |
No intertendinous connection |
Intertendinous connection between tendons to index, middle, ring, and little digits: link some motions |
Even though each tendon exerts force primarily on one joint as it passes along digit, it also exerts some force on more proximal joints |
Each tendon exerts force primarily and almost exclusively at MCP joint: only in less functional positions can it potentially exert force at IP joints |
FDP and FDS tendons insert on bones just distal to joints, DIP and PIP, respectively, where they produce primary force |
ED, EI, and EDM do not have functional insertions to bones just distal to primary joint (MCP) of motion. Produce extension through extensor hood |
FDP serves as origin of lumbrical muscles in palm |
Distal to MCP joints extensions of these tendons (central and lateral bands) serve as tendons of lumbrical and interossei muscles |
DIP, distal interphalangeal; ED, extensor digitorum; EDM, extensor digiti minimi; EI, extensor indicis; FDP, flexor digitorum profundis; FDS, flexor digitorum superficialis; MCP, metacarpophalangeal.
The long digital flexor tendons (see Fig. 1-15) of the flexor digitorum profundus (FDP) and the flexor digitorum superficialis (FDS) muscles enter the hand by passing through the carpal tunnel. Just proximal to the tunnel the tendons are in three rows: the FDS tendons to the middle and ring fingers are volar, those to the index and little fingers are intermediate, and all four FDP tendons are dorsal. As the tendons continue into the tunnel, the FDS tendons are volar to those of the FDP. In the palm, they diverge toward their respective digits with the FDP tendons dorsal or deep to the FDS tendons. A lumbrical muscle is on the radial side of each pair of tendons. Each pair of tendons enters the digital tendon sheath just proximal to the volar plate of the MCP joint. The FDS tendon splits (Champer’s chiasm) as it crosses the proximal phalanx; the two parts curve dorsally around the FDP tendon and insert on the volar base of the middle phalanx. The orientation of the fibers at this split minimizes the constrictive force transferred to the FDP tendon as it passes through the chiasm.8 The FDP tendon continues across the middle phalanx and DIP joint and inserts on the volar base of the distal phalanx. The blood supply to these tendons is provided by vessels that enter the tendons in the palm and form longitudinal channels within the tendon itself and through the long and short vincula in the digits. Additionally, vessels enter both tendons through their boney insertions.9
The zones of the flexor tendons are described and summarized in Table 1-3 (online). These zones are numbered from distal to proximal, and in each zone both the number of structures and the biomechanical considerations change.
Table 1-3 Zones of the Long Digital Flexor Tendons
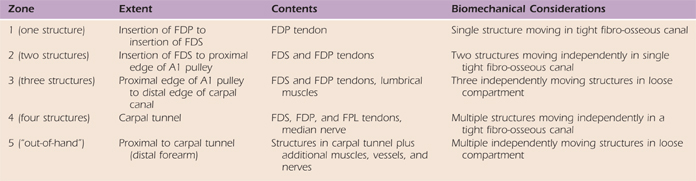
FDP, flexor digitorum profundis; FDS, flexor digitorum superficialis; FPL, flexor pollicis longus.
The effectiveness of the extrinsic digital flexor muscles depends on the positions of the joints that they cross. The FDP affects motion primarily at the DIP joints; the FDS, at the PIP joints. The force generated at all joints by muscle contraction is directly related to the position of the wrist because that position determines the physiologic range in which the muscle operates. Thus, most activities of the hand occur with the wrist in some degree of extension. The tendons of these two muscles glide differently and that is determined by the positions of the joints of the digits (Table 1-4, online). The lumbricals produce flexion at the MCP joints and extension at the PIP and DIP joints. When the FDP shortens the proximal attachments of the lumbrical moves proximally, which increases the physiologic advantage of the lumbrical. Likewise, when flexion occurs at the MCP joint, the proximal movement of the FDP tendon compensates for the shortened lumbrical.
Table 1-4 Differential Flexor Tendon Gliding
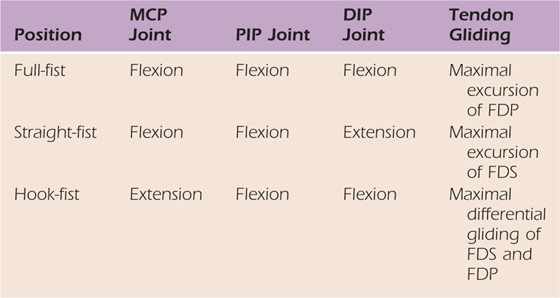
DIP, distal interphalangeal; FDP, flexor digitorum profundis; FDS, flexor digitorum superficialis; MCP, metacarpophalangeal; PIP, proximal interphalangeal.
From Wehbe MA, Hunter JM. Flexor tendon gliding in the band, Part II. Differential gliding. J Hand Surg. 1985;10A:575-579.
The flexor tendon sheaths have two distinct components: a synovial sheath that facilitates motion and a fibrous sheath that maintains tendon position. In most locations in the body, as in the digits, both components are present. In the palm, however, the synovial sheath is present by itself.
The fibrous digital tendon sheath (Fig. 1-17) is limited to each digit and extends from the proximal end of the MCP volar plate to the distal edge of the DIP volar plate. The sheath is considered to be anatomically continuous, but there are multiple points at which it is greatly reinforced by a concentration of transversely oriented fibers (annular ligaments or annular [A] pulleys) and points where less robust, obliquely oriented fibers (cruciform ligaments or curiae [C] pulleys) are found. The A pulleys are numbered from proximal to distal, so pulleys 1, 3, and 5 are attached to the MCP, PIP, and DIP volar plates, respectively, and pulleys 2 and 4 are associated with the proximal and middle phalanges, respectively.10 These A pulleys are strong and important functionally because they hold the tendons exactly in position at the most critical places. Pulleys A2 and A4 are the most important because they ensure the tendons follow the concave volar shafts of the proximal and middle phalanges. The reduction in motion caused by the loss of each A pulley is indicated in Table 1-5 (online). In addition to their importance in preventing bowstringing, the A2 and A4 pulleys, together with the head of the proximal phalanx, maintain a three-point force system that facilitates the onset of flexion at the PIP joint. In the extended digit, the flexor tendons are dorsal in position along the shafts of the proximal and middle phalanges and volar as they cross the PIP joint. As the flexor tendons tighten, they exert a dorsal force on the head of the proximal phalanx and volar forces on the A2 and A4 pulleys, which initiate flexion. This also occurs at the DIP joint but to a lesser degree.
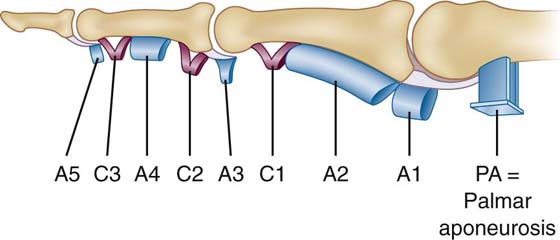
Figure 1-17 Lateral view of the annular (A) and cruciate (C) ligaments (pulleys) of the fibrous part of the flexor digital tendon sheath as described by Doyle. (Doyle JR. Anatomy of the finger flexor tendon sheath and pulley system. J Hand Surg. 1988;13A:473-484.)
Table 1-5 Predicted Loss of Annular (A) Pulleys*
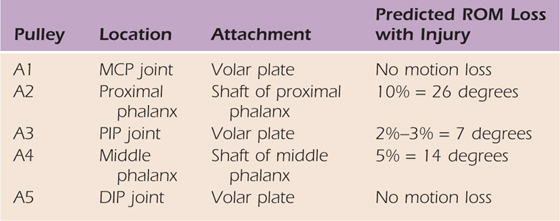
* Based on total of 260 degrees of flexion: MCP—90 degrees; PIP—110 degrees; DIP—60 degrees).
DIP, distal interphalangeal; MCP, metacarpophalangeal; PIP, proximal interphalangeal; ROM, range of motion.
From Amadio PC, Lin CT, An KN. Anatomy and pathomechanics of the flexor pulley system. J Hand Ther. 1989;2:138-141.
The cruciate, or C, pulleys are also numbered from proximal to distal. The term cruciate implies that these pulleys are X-shaped, but in reality they may exist only in an oblique form.11 The two most consistently present are C1 and C3, which are distal to the A2 and A4 pulleys, respectively. Pulley C1 extends from the proximal phalanx to the PIP volar plate; C3 interconnects the middle phalanx and the DIP volar plate. The presence of a C pulley proximal to either pulley A2 or A4 is highly variable.12 These pulleys may aid in preventing bowstringing, but if so it appears to be minimal.
The fibrous sheath of the thumb extends from the proximal margin of the MCP volar plate to the distal margin of the IP volar plate. Annular pulleys are associated with both the MCP and IP volar plates. The pulley associated with the proximal phalanx is oblique, extending from the ulnar base of the proximal phalanx to its radial side near the IP joint. Loss of any single pulley does not appreciably reduce motion. Loss of the proximal annular and the oblique pulleys significantly reduces motion.13
The synovial tendon sheath (Figs. 1-14 and 1-18) is very much like a bursa in that it consists of two layers, which are continuous and thus form a closed space. Think of a balloon that has lost all its air, so although it is collapsed it still has a potential space if it were reinflated. A bursa is generally more or less flat; a synovial tendon sheath wraps around a tendon until the two sides meet so it doesn’t entirely encircle the tendon. The two layers of the synovial sheath attach to whatever is adjacent to them. In the case of a digital tendon sheath, the inner (visceral) layer attaches to the tendon, and the outer (parietal) layer attaches to the fibrous part of the tendon sheath. When a tendon moves, the gliding motion occurs between the two layers of the synovial tendon sheath as opposed to between the tendon and the fibrous sheath. The inner surface of the sheath is lined by cells that are similar to those that line the synovial layer of a synovial joint capsule. These cells regulate a minuscule amount of lubricating fluid that is in the space, and they are sensitive to a variety of insults and react by initiating inflammation within the space. Inflammation within a synovial tendon sheath interferes with normal gliding of the tendon and forces the finger into flexion because the space can accommodate more fluid in that position.14
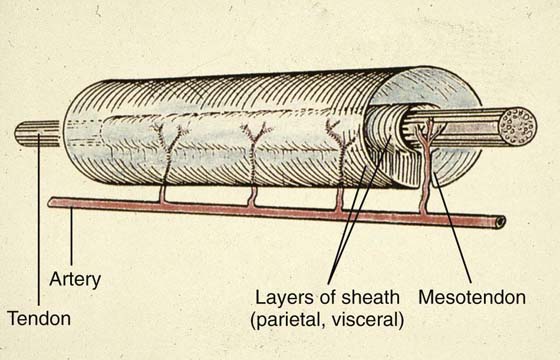
Figure 1-18 View of a synovial tendon sheath. Note that the sheath does not totally surround the tendon and that there is a space within the sheath in this illustration. In reality, that space is a potential space because the two layers of the sheath are separated only by a thin layer of fluid.
The fibrous part of the digital tendon sheath forms a very tight and rigid fibro-osseous canal, so there is very little room beyond that taken by the tendons and the synovial part of the sheath. Since the pulleys of the fibrous sheath are not continuous, the sheath is thinner, and thus weaker, between pulleys. Under normal circumstances the synovium bulges slightly, forming “cul-de-sacs,” in the weaker areas, either between or next to pulleys; this is particularly true proximal to the A1 pulley because the synovial sheath extends proximal to the fibrous sheath and forms a pouch.15 With flexion, the visceral layer of the synovial sheath slides proximally with the tendon so the pouch enlarges. With any inflammation in the sheath the bulges enlarge, particularly the pouch proximal to the A1 pulley.
There are five different synovial tendon sheaths in the palmar hand: the ulnar and radial bursae and three separate digital tendon sheaths (see Fig. 1-14). The ulnar bursa is associated with all of the tendons of the FDS and FDP muscles. It begins proximal to the carpal tunnel, extends through the tunnel into the palm, and follows the FDS and FDP tendons into the little finger, where it becomes its synovial digital tendon sheath. That part of the ulnar bursa associated with the tendons of the index, middle, and ring fingers ends in the midpalm so there is a “bare area” in the palm where there is no synovial sheath. The radial bursa is associated with the FPL tendon and extends from proximal to the carpal tunnel to the distal phalanx of the thumb. The three separate digital synovial sheaths are associated with the index, middle, and ring fingers and extend from just proximal to the MCP joints to the distal phalanges of those digits.
The tendons of the extrinsic extensor muscles enter the hand by passing deep to the extensor retinaculum; these muscles are three wrist extensors, the abductor pollicis longus, and five digital extensors. The extensor retinaculum extends from the radius laterally to the ulna medially and is connected to those bones by five septa that form six separate compartments deep to the retinaculum. These compartments are numbered from radial to ulnar and illustrated in Figure 1-19. The tendons of the extrinsic extensors pass through these compartments and thus are stabilized at the wrist. While in the compartments, the tendons have synovial sheaths that begin proximal to and extend distal to the retinaculum. Generally, a single synovial sheath is associated with all tendons in a compartment but there is variability, particularly in first compartment. The contents of these compartments, the synovial sheaths, and the terminations (insertions) of the tendons are summarized in Table 1-6 (online).
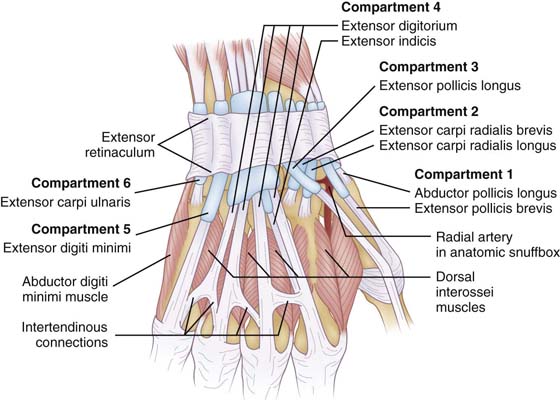
Figure 1-19 View of the tendons of the extrinsic extensor muscles on the dorsum of the wrist and hand.
Table 1-6 Extensor Tendon Compartments Deep to the Extensor Retinaculum
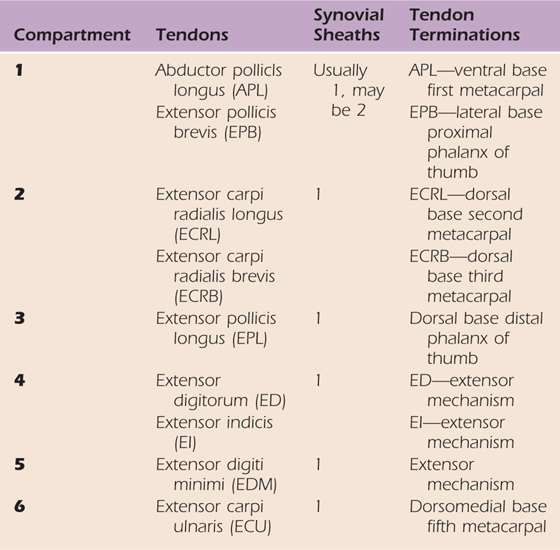
On the dorsolateral hand, in the region of the base of the thumb, the tendons of the APL, EPB, and EPL define the anatomic “snuff box” (see Fig. 1-19). The APL and EPB tendons form the anterior boundary. The EPL tendon forms the posterior boundary; it is positioned more posteriorly because it passes around the dorsal radial tubercle (of Lister) as it enters the hand. The floor of the snuff box is formed by the scaphoid. The radial artery passes diagonally across the scaphoid toward the first web space, and branches of the superficial radial nerve cross the tendons forming the boundaries.
The tendons to the four medial digits are the extensor digitorum (ED), extensor indicis proprius (EI), and the extensor digiti minimi (EDM). The tendons of the ED and EI muscles pass through extensor compartment four, and that of the EDM passes through compartment five. Distal to the wrist, the ED tendons diverge toward the MCP joints, with the EI and EDM tendons passing to the index and the little fingers, respectively. These tendons are thin and flat, and because there is minimal subcutaneous tissue, they are close to the metacarpals and dorsal interossei and the skin. Just proximal to the MCP joints, the ED tendons to all four digits may be interconnected by intertendinous connections (juncture tendinum) (see Fig. 1-19), but those of the middle, ring, and little fingers almost always are. These connections are oblique, passing distally from the ring finger tendon to those of the middle and little fingers. Because of this orientation, independent motion of the three fingers is limited, meaning that when the middle and little fingers are flexed at the MCP joints, it is difficult to actively extend the ring finger.16
The extensor mechanism (retinaculum, aponeurosis) (Fig. 1-20, online) is the system of fibrous bands on the dorsum and sides of the digits that extends from just proximal to the MCP joint to the distal phalanx on each digit. This structure is very important to both the motion and balance of the digit and has multiple components.
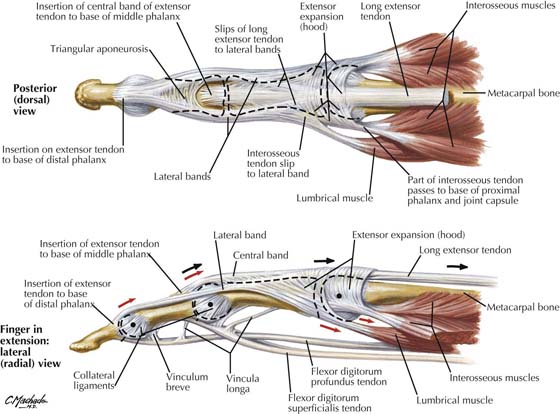
Figure 1-20 Dorsal (A) and lateral (B) views of the extensor mechanism. (Netter illustration from www.netterimages.com. © Elsevier Inc. All rights reserved.)
As the extensor tendon crosses the MCP joint, it is not functionally attached to the proximal phalanx but rather to the extensor hood. This hood is a circumferential band of fibers that sweeps around the joint. The sides of this hood are in the sagittal plane and attach volarly to the volar plate. They are known as the sagittal bands.17 Distal to the sagittal bands the fibers of the hood are more obliquely oriented. The hood functions as a sling, sliding distally with flexion and proximally with extension, and is the mechanism through which the extensor tendon(s) extends the proximal phalanx at the MCP joint. The hood also anchors and stabilizes the extensor tendon in its central position.
Just distal to the MCP joint the extensor tendon separates into a single central band (slip) and a pair of lateral bands (slips). The central band continues along the proximal phalanx, crosses the PIP joint, and attaches to the dorsal base of the middle phalanx. The lateral bands diverge as they pass distally, crossing the sides of the PIP joint just dorsal to its flexion–extension axis. They continue distally and converge dorsally to form a single band that crosses the dorsal aspect of the DIP joint and attaches to the dorsal base of the distal phalanx. Even though both the lateral and central bands are direct continuations of the extensor tendons, they are only minimally controlled by the extensor muscles because the excursion of the ED muscle is primarily utilized at the MP joint.18 However, since both the lumbrical and interossei muscles attach to the central and lateral bands, they effectively are the tendons of those muscles. The lumbricals and interossei pass ventral to the flexion–extension axis of the MCP joint and thus flex the proximal phalanx, and by virtue of their attachments to the central and lateral bands, these muscles extend both the middle and distal phalanges.
The maintenance of the position of the lateral bands as they cross the PIP joint is critical to the normal position and motion of the digit. This position is maintained by two fibrous supports. The triangular membrane interconnects the lateral bands dorsal to the middle phalanx and the PIP joint and prevents them from migrating volarly. That is, the membrane ensures that the lateral bands cross the PIP dorsal to the flexion–extension axis. The retinacular ligament has two components, and both of these prevent dorsal migration of the lateral bands.19 The transverse retinacular ligament originates from the volar capsule of the PIP joint and flexor pulleys and inserts at the conjoined lateral tendon at the proximal half of the middle plalanx. The oblique retinacular (Landsmeer’s) ligament originates on the palmar plate and flexor sheath volar to the PIP joint and inserts in the terminal tendon.20 The oblique retinacular ligament is likely the more important in stabilizing the lateral band. It passes volar to the flexion–extension axis of the PIP joint and it links motion at the PIP and DIP joints. As the distal phalanx is flexed, the lateral bands are pulled distally, which adds tension to the oblique ligaments. This increases the flexion force at the PIP joint and thus causes flexion of the middle phalanx. Conversely, as the middle phalanx is extended, the oblique ligaments are stretched, which adds tension to the lateral bands and causes extension of the distal phalanx. In other words, the distal phalanx cannot be flexed without the middle phalanx also being flexed, nor can the middle phalanx be extended without the distal phalanx also being extended. However, if Landsmeer’s ligaments are a bit slack, the lateral bands can slide dorsally and the PIP joint can be “locked” in extension. Then, the distal phalanx can be flexed while the middle phalanx remains extended.
Even though the thumb has a modified extensor hood, extension of the middle and distal phalanges is rather straightforward and performed by the extensor pollicis brevis (EPB) and extensor pollicis longus (EPL), respectively. The modified hood is the superficial layer of fibrous support on the dorsum and sides of the thumb and is considerably stronger and heavier on the ulnar side. That side is formed by the tendon and aponeurosis of the AP; it is wide and extends dorsally to blend with the tendons of the EPB and EPL. The radial side is formed by the APB and FPB tendons, which also pass dorsally to blend with the EPB and EPL tendons.
The position of a digit at rest, as well as during motion, is dependent on the forces on the flexor and extensor sides of the finger. These forces are both dynamic (muscular) and static (ligamentous). The relaxed posture of each digit—slight flexion at each joint with the amount of flexion increasing from the index to little fingers—reflects these forces and that the flexor forces exceed those on the extensor side. Loss of any force produces a predictable change in the natural posture (deformity) and typically an opposite dynamic loss. For example, loss of the central band as it crosses the DIP joint produces a flexed distal phalanx (mallet finger) and an inability to extend the distal phalanx.
The normal dorsal and volar forces at the MCP, PIP, and DIP joints are summarized in Table 1-7 (online) and illustrated in Figure 1-20 (online). On the volar aspect of the digit, the FDP muscle is the only force at the DIP joint, and it contributes to the flexor forces at both the PIP and MP joints. The FDS muscle is the primary force at the PIP joint, and it contributes to the volar force at the MP joint. Flexor force at the MP joint is provided by the lumbrical and interossei muscles as well as from the two long digital flexors. Although the flexor force at the MP joint is provided by multiple muscles, the specific source of that force varies considerably and is largely dependent on the position of the wrist. The force in a strong grasp occurs at the DIP and PIP joints, and, if the wrist is extended, at the MCP joints as well. Flexion of the proximal phalanges by the lumbricals and interossei occurs when the hand is performing delicate maneuvers. The only static force on the flexor side of the digit is at the PIP joint, which is provided by the oblique part of the retinacular ligament.
Table 1-7 Dynamic and Static Flexor and Extensor Forces of the Digits
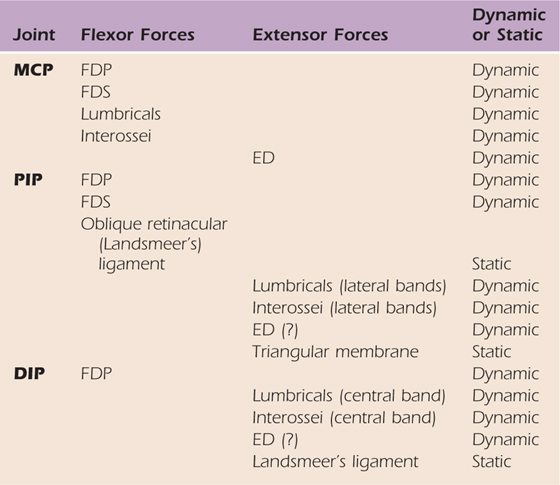
(?), questionable force; ED, extensor digitorum; FDP, flexor digitorum profundis; FDS, flexor digitorum superficialis.
The only extensor force across the MP joint is provided by the ED, EI, and EDM muscles; if they provide any force across the PIP and DIP joints it is minimal. At both the PIP and DIP joints, the major muscular force is supplied by the lumbrical and interossei muscles. The oblique portion of the retinacular ligament is a static support across the extensor aspect of the DIP joint, and the triangular membrane is a static support across the PIP joint.
Incompetence of the oblique retinacular ligament or the transverse retinacular ligament results in a dorsal displacement of the lateral bands, which increases the extensor force at the PIP joint. Loss of the oblique ligament also removes a flexor force at the PIP joint, so the net result is an imbalance of force in favor of the extensor side so there is hyperextension of the middle phalanx. This hyperextension causes an increase in the tension in the tendons of both the FDP and FDS muscles, which produces flexion of both the distal and proximal phalanges. The resulting position, hyperextension at the PIP joint and flexion at both the DIP and MP joints, is referred to as a swan-neck deformity.
Destruction of the soft structures dorsal to the PIP joint produces a different deformity. This is an example of a deformity resulting from loss of both static and dynamic forces. Loss of the central band removes the lumbrical and interossei force (and that of the ED if any exists) and loss of the triangular membrane allows the lateral bands to slide volarly. Force across the extensor side of the joint is reduced; if the volar displacement of the lateral bands is sufficient (volar to the flexion–extension axis), virtually all extensor force is lost, and force may be added to the flexor side. In either case the balance of power shifts toward the flexor side of the PIP joint and flexion results. The passive tension in the tendons of the FDP and FDS muscles is reduced, resulting in extension of the distal and proximal phalanges. This position, flexion of the PIP joint and extension at both the MP and DIP joints, is referred to as a boutonnière (buttonhole) deformity.
A deformity resulting from a nerve injury results from loss of dynamic forces. An injury of the ulnar nerve in Guyon’s canal is considered a “low” ulnar nerve injury. This type of injury results in loss of the AP, all interossei, the two medial lumbricals, and the muscles in the hypothenar compartment. Of those muscles, the ones contributing to the flexion–extension balance of the digits are the interossei and lumbricals. The deformity resulting from such an injury is aptly called the incomplete claw. The loss of the interossei and lumbrical muscles reduces the dynamic force across the volar aspect of the MCP joint and most, if not all, of the dynamic force across the dorsal aspects of the PIP and DIP joints. This reduces the flexor force at the MCP joints and the extensor force at the PIP and DIP joints, which results in an increase in extensor force at the MCP joints and the flexor force at the PIP and DIP joints. The result is the clawlike posture when hyperextension occurs at the MCP joints and flexion occurs at the PIP and DIP joints. Since the lumbricals and interossei are both lost in the little and ring fingers and only the interossei are lost in the ring and middle fingers, the claw is more severe in the little and ring fingers.
The muscular and cutaneous nerve supply to the hand is summarized in Table 1-8 (online).
Table 1-8 Nerve Supply of the Hand
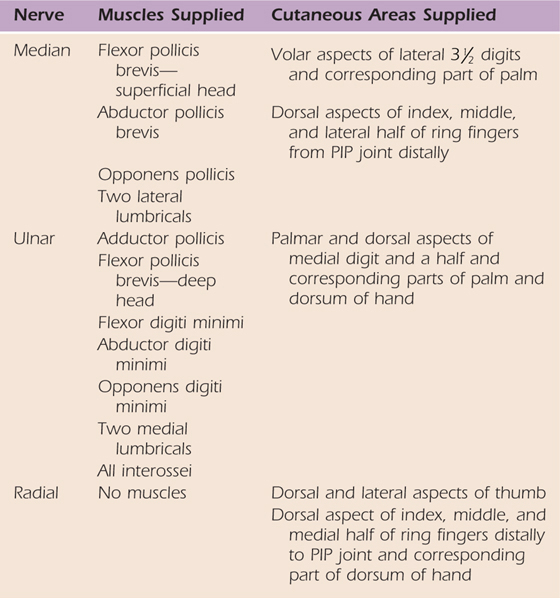
PIP, proximal interphalangeal.
Three peripheral nerves, the median, ulnar, and superficial radial, supply the hand (Figs. 1-21 and 1-22, online). The median nerve is the major cutaneous nerve of the hand. It has a small palmar branch in the distal forearm that passes superficially into the hand and supplies the skin of the base of the thumb. Just proximal to the wrist the median nerve is located between the tendons of the palmaris longus and flexor carpi radialis muscles. It enters the hand, passing through the carpal tunnel as the most volar structure. Just distal to the tunnel it branches into its terminal branches: the recurrent (motor, muscular) branch and several digital branches. The recurrent branch passes laterally and supplies the muscles in the thenar compartment. It is in a superficial position, about midway between the pisiform and the thumb MCP joint, and therefore vulnerable to laceration. The digital branches are of two types. A common palmar digital nerve supplies adjacent sides of two fingers; it passes toward a web-space, where it divides into two proper palmar digital nerves. Each proper digital nerve supplies the side of a single digit. It extends to the end of a digit and supplies the volar half of the skin to the PIP joint and the volar and dorsal aspects distal to that. A proper digital nerve also supplies the joints of the digit.
The ulnar nerve is the major muscular nerve of the hand. Just proximal to the wrist it is positioned deep to the tendon of the flexor carpi ulnaris muscle. It enters the hand in company with the ulnar artery by passing lateral to the pisiform, superficial to the pisohamate ligament, deep to the palmaris brevis muscle, and then medial to the hook of the hamate (Guyon’s canal). This is a vulnerable part of its course because it is superficial and thus vulnerable to laceration, and it crosses the robust pisohamate ligament so it is vulnerable to external compression. In the canal or just distal, the nerve branches into superficial and deep branches. Aside from supplying the palmaris brevis muscle, the superficial branch is a cutaneous nerve and usually divides into one common palmar and one proper palmar digital nerve. The deep branch is muscular and has no cutaneous distribution. It passes through the hypothenar compartment and then accompanies the deep palmar arterial arch, passing laterally in a position deep to the long digital flexor tendons. The deep branch terminates laterally, where it enters the adductor pollicis muscle. The ulnar nerve has a dorsal cutaneous branch, which arises proximal to the wrist. This branch enters the hand by passing dorsally across the medial aspect of the wrist. On the dorsum of the hand it has common and proper dorsal digital branches. Its distribution is variable but typically it supplies the medial digit and a half as far distally as the PIP joint and the corresponding part of the dorsum of the hand.
The superficial radial nerve is purely cutaneous and supplies the dorsolateral aspect of the hand. It enters the hand by passing superficially across the anatomic snuff box and the tendon of the extensor pollicis longus. It branches into common and proper dorsal digital nerves and, although variable, typically supplies the lateral three and a half digits as far distally as the PIP joints and the corresponding part of the dorsal hand.
The segmental innervation is provided by four spinal cord segments. The skin of the lateral hand, thumb, and index finger is supplied by spinal cord segment C6; that of the middle finger by C7; and the medial hand, ring, and little fingers by C8. The intrinsic muscles of the hand are supplied by spinal cord segments C8 and T1, the lateral ones by C8 and the medial by T1.
The hand is supplied by the radial and ulnar arteries (see Figs. 1-21 and 1-22, online). These arteries form two arterial arches, and the branches of these arches have multiple interconnections so arterial collateralization in the hand is rich.
The ulnar artery enters the hand by passing lateral to the pisiform and medial to the hook of the hamulus, in Guyon’s canal. It is accompanied by the ulnar nerve. While in the canal or just distally, the artery splits into its larger superficial branch and smaller deep branch. The superficial branch sweeps laterally across the palm and is the primary contributor to the superficial palmar arterial arch. This arch is at the level of the distal aspect of the fully extended thumb and positioned between the palmar aponeurosis and the long digital flexor tendons. The arch is typically completed by the superficial palmar branch of the radial artery although the connection may be very small or even absent. The branches of the arch are common palmar digital arteries to adjacent sides of two digits and proper palmar digital arteries to one side of a single digit. Typically, the branches are a proper digital to the medial aspect of the little finger and three common digitals to the little, ring, middle, and index fingers. The arteries to the thumb and lateral aspect of the index finger are usually branches of the radial artery but may branch from the superficial arch or both. The deep branch of the ulnar artery passes through the hypothenar compartment and then turns laterally to complete the deep palmar arterial arch.
Proximal to the wrist the radial artery is just lateral to the tendon of the flexor carpi radialis, where its superficial palmar branch arises. The radial artery then passes dorsally across the lateral aspect of the wrist and passes through the anatomic snuff box. Just distal to the tendon of the EPL it reaches the first webspace, where it turns volarly, passing between the two heads of the first dorsal interosseous to reach the palm. Once in the palm the radial artery becomes the deep palmar arterial arch; this arch is completed by the deep branch of the ulnar artery and positioned about a thumb’s width proximal to the superficial arch between the long digital flexor tendons and the interossei and metacarpals. The deep arch is accompanied by the deep branch of the ulnar nerve. The most lateral branch of the deep arch is usually the princeps pollicis artery to the thumb. The next branch is the radialis indicis artery, which supplies the lateral aspect of the index finger. A variable number of metacarpal arteries branch from the deep arch and join the common digital branches of the superficial arch in the distal palm.
Both the radial and ulnar arteries have palmar and dorsal carpal branches. The branches unite off of their respective surfaces of the carpus to form palmar and dorsal arches (rete) that are somewhat variable.
1. Jones WW. Biomechanics of small bone fixation. Clin Orth Relat Res. 1987; 214: 11–18.
2. Kuczynski K. Carpometacarpal joint of the human thumb. J Anat. 1974; 118: 119–126.
3. Haines RW. The mechanism of rotation at the first carpometacarpal joint. J Anat. 1944; 78: 44–46.
4. Zancolli EA, Ziadenberg C, Zancolli E Jr. Biomechanics of the trapeziometacarpal joint. Clin Orthop Relat Res. 1987; 220: 14–26.
5. Imaeda T, An KN, Cooney WP, et al. Anatomy of the trapeziometacarpal ligaments. J Hand Surg. 1993; 18A: 226–231.
6. Bettinger PC, Linscheid RL, Berger RA, et al. An anatomic study of the stabilizing ligaments of the trapezium and the trapeziometacarpal joint. J Hand Surg. 1999; 24A: 786–798.
7. Bowers WH, Wolf JW Jr, Nehil JL, et al. The proximal interphalangeal joint volar plate. I. An anatomical and biomechanical study. J Hand Surg. 1980; 5A: 79–88.
8. Schmidt HM, Ahang SX, Zieseniss K. Clinical anatomy of the chiasma tendinum (Camper) in the fingers. Clin Anat. 1994; 7: 65–71.
9. Stricklang JW. Flexor tendon injuries: I. Foundations of treatment. J Am Acad Orthop Surg. 1995; 3: 44–54.
10. Doyle JR. Anatomy of the finger flexor tendon sheath and pulley system. J Hand Surg. 1988; 13A: 473–484.
11. Lin GT, Amadio PC, An KN, et al. Functional anatomy of the human digital flexor pulley system. J Hand Surg. 1989; 14A: 949–956.
12. Amadio PC, Lin GT, An KN. Anatomy and pathomechanics of the flexor pulley system. J Hand Ther. 1989; 2: 138–141.
13. Doyle JR, Blythe WF. Anatomy of the flexor tendon sheath and pulleys of the thumb. J Hand Surg. 1977; 2A: 149–151.
14. Mester S, Schmidt D, Derczy K, et al. Biomechanics of the human flexor tendon sheath investigated by tenography. J Hand Surg. 1995; 14A: 949–956.
15. Strauch B, de Moura W. Digital flexor tendon sheath: An anatomic study. J Hand Surg. 1985; 10A: 185–189.
16. Von-Schroeder HP, Botte MJ. Anatomy of the extensor tendons of the fingers: variations and multiplicity. J Hand Surg. 1995; 20A: 17–34.
17. Rayan GM, Murray D, Chung KW, et al. The extensor retinaculum system at the metacarpophalangeal joint. J Hand Surg. 1997; 22B: 585–590.
18. Newport ML. Extensor tendon injuries in the hand. J Am Acad Orthop Surg. 1997; 5: 59–66.
19. El-Gammal TA, Steyers CM, Blair WF, et al. Anatomy of the oblique retinacular ligament of the index finger. J Hand Surg. 1993; 23B: 717–721.
20. Smith RJ. Balance and kinetics of the fingers under normal and pathological conditions. Clin Orthop Relat Res. 1974; 104: 92–111.