Clinical Examination of the Wrist
▪ Successful clinical examination of the wrist requires a thorough knowledge of wrist anatomy, biomechanics, and pathology.
▪ The wrist examination includes a complete history, visual inspection, objective assessments, and a systematic physical examination, including palpation and provocative testing.
▪ The keys to a successful examination are to link the symptoms with the underlying palpable structures and to correlate the mechanism of the injury with the physical findings.
▪ Before the wrist is examined, a careful inspection of the entire upper extremity should be performed to rule out other extrinsic and more proximal causes for the wrist symptoms.
▪ The bony and soft tissue anatomy is systematically palpated to define areas of tenderness and to determine the area of maximum tenderness.
▪ The symptomatic wrist should always be compared with the uninvolved side.
▪ Starting the examination in an asymptomatic area helps the patient develop trust in the examiner and may reduce wrist guarding.
▪ By methodically examining each structure in each zone, the examiner can most effectively localize the patient’s symptoms and develop a differential diagnosis.
The diagnosis of “wrist sprain” was at one time a common and acceptable diagnosis for the patient with wrist pain. More recently, however, as the understanding of wrist anatomy, mechanics, and pathology has evolved, more sophisticated clinical examination procedures have been developed, allowing more specific diagnosis of wrist problems.
The wrist is a highly complex joint in a very compact space. Successful clinical evaluation of the wrist requires a thorough knowledge of wrist anatomy, biomechanics, and pathology. Also required is knowledge of surface anatomy and the corresponding underlying structures. The keys to a successful examination are to link the symptoms with the underlying palpable structures and to correlate the mechanism of the injury with the physical findings. Some common conditions may be easily identified on the basis of the clinical examination, whereas others may require additional diagnostic studies, imaging, and repeat evaluations.
The components of the wrist examination include a thorough history, visual inspection, objective assessments, and a systematic physical examination, including palpation and provocative testing to identify tenderness and abnormal motion between bones. Before the wrist is examined, the entire upper extremity should be inspected to rule out other extrinsic and more proximal causes for the wrist symptoms.
A detailed history can provide insight into the nature of the wrist problem and can help focus the subsequent physical examination. The patient’s age, dominance, occupation, and avocations should be noted. The date of onset of the problem and the circumstances related to the onset need to be explored. If the wrist problem resulted from a single incident or injury, the mechanism of the injury should be reviewed thoroughly, including the position of the wrist at the time of injury and the subsequent degree and direction of stress. For example, an acute rotational injury to the forearm or a fall on the pronated outstretched upper extremity can result in a triangular fibrocartilage complex (TFCC) injury.1 Mayfield2 describes a progression of perilunar instability initiated radially or ulnarly, depending on the position of the wrist during loading. For example, dorsiflexion and supination usually produce radially initiated perilunate injuries, whereas palmar-flexion and pronation forces may result in ulnarly initiated perilunar injuries. Weber and Chao3 found that load applied to the radial side of the palm with the wrist in extreme dorsiflexion produces scaphoid fracture.
If the wrist condition developed over time, and not as a result of a single injury, it is important to explore potential causes. Some patients have definite ideas about what caused their wrist to hurt, but others require careful questioning. New responsibilities at work or home that increase physical demands on the wrist, increased productivity requirements, an awkwardly configured workstation, and participation in a new hobby or sport are examples of factors that may precipitate symptoms.
The presence of symptoms such as pain; swelling; numbness and tingling; temperature and color changes; and abnormal sounds, such as clicks, grating, or clunks, should be noted. Their location, frequency, intensity, and duration should also be discussed. Some patients may present with very localized symptoms, whereas others report more diffuse discomfort. In the latter case, it is sometimes helpful to instruct the patient to point to the most painful spot or spots to attempt to localize the problem. Some patients may say they have pain all the time and have difficulty qualifying their symptoms. It is sometimes helpful to start by asking patients if they have pain at the present moment or “right now” as a way to help them begin to focus more specifically on when and how often their symptoms occur. The activities, positions, or conditions that aggravate the symptoms and the measures taken to obtain relief are discussed. It is important to review previous treatment interventions such as orthoses, anti-inflammatory medications, injections, and therapy, and to gauge the efficacy of the treatments. The effect the wrist condition has had on the patient’s ability to work and perform his or her usual life tasks needs to be discussed to determine the degree of disability caused by the wrist problem.
Visual inspection of the wrist and comparison to the uninvolved side can provide clues about the nature of the problem. As the patient enters the clinical setting, the examiner can observe the posture of the involved side and wrist. The posture of the neck, shoulder, and elbow should be noted because wrist symptoms may sometimes be referred from an extrinsic and more proximal site. Spontaneous use can be noted to give an indication of the extent of disability and to later correlate observations with the patient’s report of disability. If the patient enters holding a heavy briefcase or bag with the involved side and then later reports inability to lift any weight at all, the reliability of their symptom report would be in question.
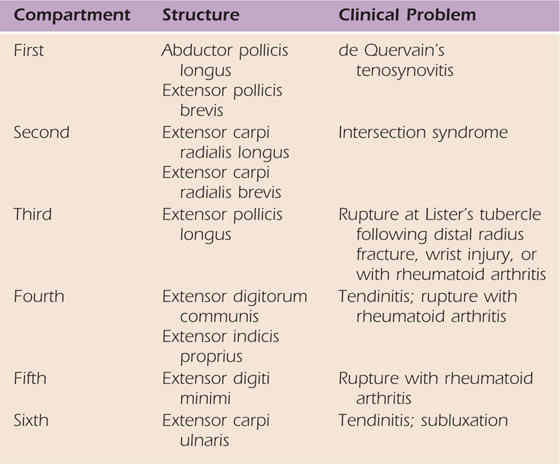
The wrist should be visually inspected and compared with the uninvolved side. On the dorsal side, the skin, nails, color, and muscle bulk should be observed. Any masses, such as a dorsal ganglion (Fig. 7-1) or traumatic or surgical scars are noted. The six extensor compartments can be inspected for any focal tubular swelling, as seen with tenosynovitis, or for any evidence of ruptures or extensor lags. Some predictable conditions involve the extensor tendons, and these should be kept in mind when examining the extensor compartments (Table 7-1, online).4 The contour, alignment, and profile of the wrist are observed in comparison with the contralateral side. Characteristic examples of abnormalities include the post-traumatic deformity that occurs with radius shortening following a malunited distal radius fracture. Another example is the prominent distal ulnar head indicative of distal radioulnar joint (DRUJ) disruption (Fig. 7-2). The profile of the wrist is observed to detect any malalignment such as a volar sag, or carpal supination (Fig. 7-3, online), compared with the other side. On the palmar side, the fingertips can be observed for callusing or atrophy to determine extent of use. The thenar and hypothenar eminences are inspected for muscle bulk.
Table 7-1 Extensor Tendon Conditions
The active and passive range of motion (ROM) of all planes of wrist motion, as well as of supination and pronation, should be assessed. Compensatory maneuvers used by the patient when motion is limited need to be identified and eliminated. For example, the patient may elevate the elbow when attempting wrist flexion. When forearm rotation is limited, the patient may substitute with shoulder motions. Measurement with a goniometer helps ensure an accurate assessment. The most reliable method for measuring wrist flexion and extension is the volar/dorsal technique5 (Fig. 7-4). The examiner needs to determine whether any restrictions are the result of pain or a mechanical cause, such as capsular contracture or a malunited fracture. Normal ROM of the wrist and functional ROM should be considered when evaluating wrist motion. Normal maximum ROM of the wrist has been documented with the use of wrist goniometry.6 However, there is some variation in normal values. Therefore the uninvolved side should be measured for comparison. Functional ROM (i.e., the motion of the wrist required to perform most activities of daily living [ADLs]) has also been documented. Palmer and colleagues7 found that functional wrist motion is between 5 degrees of flexion and 30 degrees of extension, 10 degrees of radial deviation, and 15 degrees of ulnar deviation. Ryu and coworkers8 found that 40 degrees of wrist extension, 40 degrees of wrist flexion, and a total of 40 degrees of radial and ulnar deviation are needed to perform most ADLs.
Swelling of the wrist and hand can be measured with a volumeter. Both involved and uninvolved sides are measured for comparison. The volumeter has been found by Waylett-Rendall and Seibly9 to be reliable to within 1% of the total volume when one examiner performs the measurements. van Velze and associates10 found that the left nondominant side was 3.3% smaller than the dominant right side with volume measurement in a study of 263 male laborers. She concluded that the volume of one hand could be used as a reliable predictor of the volume of the other. The measurement of bilateral wrist circumference may also be used as an indicator of swelling.
Grip strength testing is advocated by some as a reliable indicator of true impairment that deserves further investigation in cases of obscure wrist pain. Czitrom and Lister11 found a significant correlation between decreased grip strength and positive bone scans and confirmed pathology with chronic wrist complaints. Submaximal effort was ruled out with the use of rapid-exchange grip testing and a bell curve with five-position grip testing using the Jamar dynamometer.11
LaStayo and Weiss describe the GRIT (i.e., the gripping rotatory impaction test), which is used to identify ulnar impaction using a standard dynamometer to test grip with the forearm in three positions: neutral, supination, and pronation.12 The rationale for the test relates to the fact that ulnar impaction correlates with positive ulnar variance and gripping with pronation maximizes potential impaction and gripping with supination reduces it. The supination and pronation readings are calculated as a ratio, that is, supination/pronation, and the potential for impaction is considered high if the GRIT ratio is more than 1 on the involved and no different from 1 on the uninvolved side.
Sensibility examination is done to screen for possible nerve compressions. Semmes-Weinstein light-touch threshold testing has been found to be the most sensitive clinical test for detecting nerve compression.13 The median, ulnar, and dorsal radial sensory nerve (DRSN) can become compressed or irritated at the level of the wrist and can be a source of wrist symptoms. Particular attention is paid to the cutaneous distribution of these nerves with sensibility testing.
Injections are utilized to assist diagnosis and predict surgical success. Shin and coworkers14 recommend that injections should be performed in joints or along tendons that may be injured and that they can help to distinguish between intra-articular and extra-articular pathology. Bell and colleagues15 suggest that midcarpal injection with lidocaine is a useful diagnostic test to determine the presence or absence of intracarpal pathology in patients with chronic wrist pain and normal routine radiographs by evaluating grip strength and pain relief after injection. They found that midcarpal injection of lidocaine that resulted in a 28% improvement of grip strength had a statistically significant association with intracarpal pathology later diagnosed by wrist arthroscopy. These authors conclude that diagnostic injection can be an effective tool in the evaluation of the patient with chronic wrist pain. The authors point out limitations of their study, including the small sample size of normal subjects and uncertainty regarding penetration of the lidocaine into the radiocarpal joint, which would affect results if the TFCC or radiocarpal joint was the source of pathology. Freeland cautions that more study is needed to establish a reliable diagnostic test and threshold values.16
Green reported the results of a retrospective study that supports the value of carpal tunnel steroid injections as a reasonably accurate diagnostic test for carpal tunnel syndrome (CTS).17 Ninety-nine wrists in 89 patients receiving carpal tunnel injection were subsequently treated surgically. Correlations between results of injections and subsequent operations indicate that a good response to injection is an excellent diagnostic and prognostic sign. On the other hand, poor relief from injection does not mean that the patient is a poor candidate for surgery. In a more recent review of published studies, Boyer reports that the predictive value of corticosteroid injection should be considered unproved at this time.18
Palpation and provocative testing are the core of the examination. The goal is to define areas of tenderness by systematically palpating the bony and soft tissue anatomy and to determine the area of maximum tenderness. These tender areas are then related to a specific underlying structure, such as the bone, tendon, or joint. The provocative tests are performed to identify carpal instabilities. Patients with carpal instabilities often complain of pain, decreased motion, and “clicks or clunks” with motion of the wrist. The provocative tests may reproduce these sounds, which are the result of abnormal carpal movements. A painless click or clunk may be obtained in the asymptomatic wrist with lax ligaments and is not considered a sign of disease. The symptomatic wrist should always be compared with the uninvolved side. The sequence of the evaluation can be tailored to the patient’s area of maximum tenderness. Starting the examination in an asymptomatic area will help the patient to trust the examiner and may reduce the tendency toward wrist guarding.
Torosian et al19 describe a systematic approach to wrist examination. They divide the wrist into five zones: three dorsal and two volar. By methodically examining each structure in each zone, the examiner can most effectively localize the patient’s symptoms and develop a differential diagnosis. Table 7-2 (online) lists common wrist conditions for each zone and the corresponding clinical signs and tests.
Table 7-2 Wrist Conditions and Clinical Signs and Tests
AVN, avascular necrosis: CMC, carpometacarpal; DRSN, dorsal radial sensory nerve; DRUJ, distal radioulnar joint; ECU, extensor carpi ulnaris; EPL, extensor pollicis longus; FCR, flexor carpi radialis; PIN, posterior interosseous nerve; ST, scaphotrapezial; TFCC, triangular fibrocartilage complex.
The structures to examine in the radial dorsal zone include the radial styloid, the scaphoid, the scaphotrapezial (ST) joint and trapezium, the base of the first metacarpal and the first carpometacarpal (CMC) joint, the tendons of the first and third extensor compartments, and the DRSN.
The radial styloid is palpated on the radial aspect of the wrist proximal to the anatomic snuffbox with the wrist in ulnar deviation (Fig. 7-5). Tenderness of the styloid may indicate contusion, fracture, or radioscaphoid arthritis.20 The last is common with longstanding scapholunate dissociation and scaphoid instability.21 Tenderness may be aggravated by radial deviation.
The scaphoid is palpated just distal to the radial styloid in the snuffbox, which is formed by the tendons of the extensor pollicis longus (EPL) on the ulnar border and the extensor pollicis brevis (EPB) and abductor pollicis longus (APL) on the radial border. The scaphoid is most easily palpated when the wrist is in ulnar deviation because the proximal carpal row slides radially and the scaphoid assumes an extended or vertical position when the wrist is in ulnar deviation.22 Tenderness of the scaphoid in the snuffbox may indicate scaphoid fracture, nonunion, avascular necrosis (Preiser’s disease), or scaphoid instability.23 The clamp sign refers to the patients grasp of the volar and dorsal aspects of the scaphoid when asked to indicate where the wrist hurts (Fig. 7-6).24
The ST joint and trapezium are palpated just distal to the scaphoid. Opposition of the thumb to the small finger and ulnar deviation of the wrist makes the trapezium more prominent and easier to palpate. Circumduction of the thumb while palpating facilitates differentiation between the base of the thumb metacarpal and the adjacent trapezium. Tenderness in this region may indicate ST arthritis, which may result from scaphoid instability.25
The base of the first metacarpal and the first CMC joint are localized by palpating in a proximal direction along the dorsal aspect of the flexed first metacarpal until a small depression can be felt. This depression represents the first CMC joint. Tenderness here is often caused by degenerative arthritis. The grind test has been described for CMC arthritis26 and involves axial compression of the first metacarpal with rotation (Fig. 7-7). This clinical maneuver grinds the articular surfaces of the base of the first metacarpal and the trapezium. A positive test elicits pain, and crepitus may be felt. First CMC joint arthritis may be accompanied with radial subluxation of the base of the first metacarpal. If the subluxation is more than 2 to 3 mm, the outline of the thumb will form a step called the “shoulder sign”27 (Fig. 7-8). Occasionally, CMC joint pain may be caused by laxity or instability. To test for CMC joint instability or laxity, the metacarpal is distracted and moved in a side-to-side or radioulnar direction while the trapezium is stabilized. Comparison with the opposite side allows determination of whether joint laxity or instability is present.

Figure 7-7 Grind test for arthritis of the carpometacarpal joint of the thumb is performed by applying axial pressure with rotation.
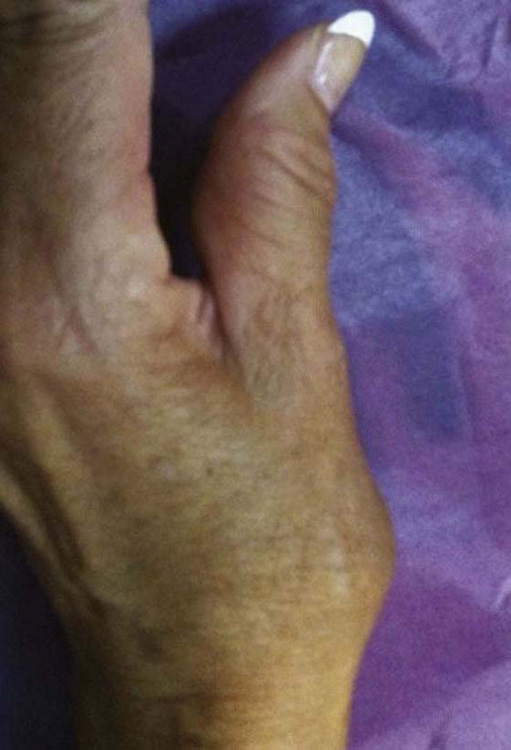
Figure 7-8 “Shoulder sign,” indicating radial subluxation of the base of the first metacarpal seen with first carpometacarpal joint arthritis.
The EPB and APL tendons make up the first extensor compartment and form the radial border of the anatomic snuffbox. The thumb is extended and radially abducted to allow identification and palpation of these tendons. Fullness, tenderness, and nodularity may be indicative of de Quervain’s tenosynovitis. Finkelstein’s test is used to detect de Quervain’s tenosynovitis.28 This test involves flexion of the thumb combined with ulnar deviation of the wrist (Fig. 7-9). A positive test produces pain localized to the radial aspect of the wrist.

Figure 7-9 Finkelstein’s test for de Quervain’s tenosynovitis involves flexion of the thumb combined with ulnar deviation of the wrist.
The EPL tendon forms the ulnar border of the snuffbox. With the palm facing down, the thumb is extended toward the ceiling to allow identification and palpation of the EPL. The excursion of the tendon should be noted and compared with the opposite side. The EPL tendon passes around Lister’s tubercle on its path to the thumb and can rupture or become adherent after distal radius fractures, resulting in loss of or incomplete thumb extension.4 EPL tendinitis, also referred to as drummer’s palsy,29 presents clinically as tenderness of the third extensor compartment just ulnar to Lister’s tubercle.
Intersection syndrome refers to friction at the point where the muscle bellies of the EPB and the APL cross over the radial wrist extensor tendons proximal to the wrist, resulting in an inflammatory peritendinitis.30 This condition may result from activities or sports that require forceful, repetitive wrist flexion and extension, such as rowing, weight lifting, and racquet sports. Friction and crepitus may be palpated 4 to 5 cm proximal to the radial styloid during wrist flexion and extension with radial deviation and has led to the name “squeaker’s wrist”31 (Fig. 7-10). The muscle bellies of the EPB and APL may be palpated proximally while the thumb is actively moving to further identify tenderness or crepitus.
The DRSN travels along the dorsal radial aspect of the wrist and can become implicated in a variety of radial-sided injuries. Irritation of the DRSN is referred to as Wartenberg’s syndrome or Wartenberg’s neuralgia.32 Because of its superficial location, the DRSN is easily susceptible to any compressive forces, such as tight externally applied wrist straps. Forearm position can accentuate the discomfort of DRSN compression. When the forearm is supinated, the DRSN lies between the tendons of the brachioradialis and the extensor carpi radialis longus (ECRL) without compression from these two tendons. When the forearm is pronated, however, the ECRL tendon crosses under the brachioradialis tendon and in a scissor-like fashion creates compression of the DRSN.33 Palmar, ulnar flexion of the wrist puts the nerve on stretch. When irritated, the DRSN causes numbness, tingling, burning, and pain over the dorsal radial aspect of the hand (Fig. 7-11). Percussion along the course of the nerve produces tingling and pain, and this may radiate distally. Sensibility over the dorsal web and dorsum of the thumb may be diminished and can be assessed with Semmes-Weinstein monofilaments.32
The structures of the central dorsal zone include the dorsal rim of the distal radius, Lister’s tubercle, the lunate, the scapholunate interval, the capitate, and the base of the second and third metacarpals. The soft tissue structures include the tendons of the second and fourth extensor compartments and the posterior interosseous nerve (PIN).
To locate the dorsal rim of the distal radius, the examiner should palpate the radial styloid and move dorsally. Tenderness in this area may be caused by impingement of the scaphoid on the distal radius. This condition may be caused by activities such as gymnastics in which repetitive contact of the scaphoid on the dorsal rim of the distal radius occurs during wrist hyperextension. As a response to the repeated stress, the body forms a spur, or osteophyte, on the distal radius, which is painful with pressure or with hyperextension and radial deviation of the wrist.34,35
Lister’s tubercle forms a bony prominence over the dorsal and distal end of the radius and can easily be palpated (Fig. 7-12, online). It is helpful to use as a landmark when localizing other structures.
The lunate is found just distal and ulnar to Lister’s tubercle with the wrist flexed. In this position the lunate forms a rounded prominence (Fig. 7-13, online). Tenderness with palpation of the lunate can indicate Keinböck’s disease—avascular necrosis of the lunate.36
The scapholunate interval is found just distal to Lister’s tubercle between the third and fourth extensor compartments. Dorsal wrist ganglions are the most common mass on the dorsum of the hand and often arise from the scapholunate interval.37 These ganglions are generally soft and freely moveable and are more easily palpable with the wrist flexed. Tenderness may be present with wrist flexion or extension secondary to compression of the ganglion. An occult ganglion is one that is suggested by patient history and complaints of pain with deep palpation but that is not detectable by clinical exam.38,39 Sometimes confused with a ganglion is the muscle belly of the extensor manus brevis, which is a vestigial wrist extensor. The extensor manus brevis is an extra muscle–tendon unit for the index or long fingers found distal to the retinaculum.40
Tenderness or fullness in the scapholunate region may indicate scapholunate ligament injury, occult ganglion, or dorsal wrist syndrome, described by Watson41 as localized scapholunate synovitis that occurs secondary to overstress of ligaments in this area. The finger extension test, used to demonstrate dorsal wrist syndrome, involves resisted long finger extension with the wrist in flexion (Fig. 7-14, online). The test is positive if pain is produced in the scapholunate region.41 Kayalar and associates compared surgical findings with preoperative test results of the finger extension test in a series of patients diagnosed with occult dorsal wrist ganglion and found 92% diagnostic accuracy of the finger extension test for occult dorsal wrist ganglion.42
Scapholunate ligament injury can lead to scaphoid instability and rotary subluxation of the scaphoid. This involves dissociation of the scaphoid and the lunate and rotation of the scaphoid to a volar-flexed position. Watson41 identified five clinical signs for rotary subluxation of the scaphoid. These include tenderness over the scaphoid in the snuffbox, scaphotrapezial-trapezoid (STT) joint synovitis and tenderness, dorsal scapholunate synovitis, a positive finger extension test, and an abnormal scaphoid shift test.41
The scaphoid shift test (SST), also referred to as the Watson test or the radial stress test, was described by Watson and coworkers43 as a provocative maneuver to assess scaphoid stability (Fig. 7-15). To perform the SST, pressure is applied over the volar prominence of the scaphoid, found at the base of the thenar crease as the wrist is moved from ulnar deviation to radial deviation with slight flexion. Normally, with radial deviation, the scaphoid palmar flexes. With ligament laxity or disruption, and under pressure from the examiner’s thumb, the proximal pole of the scaphoid shifts up onto the dorsal rim of the distal radius. When thumb pressure is withdrawn, the scaphoid returns with a clunk. A positive test is one that reproduces the patient’s symptoms, usually a painful clunk. The test may be falsely positive in up to one third of individuals and is thought to be due to ligamentous hyperlaxity that permits capitolunate translation with similar findings.44
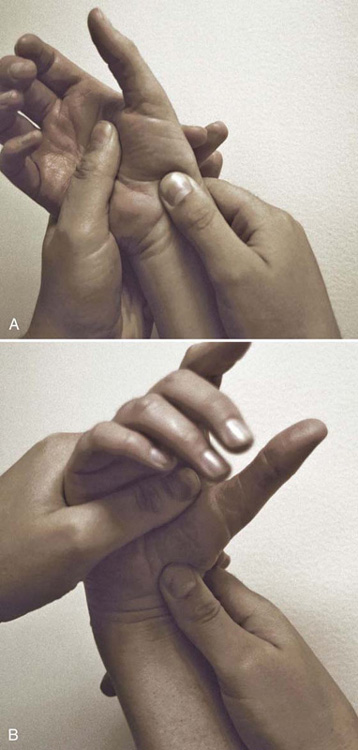
Figure 7-15 Watson’s test for scaphoid instability. A, Starting position is with the wrist in ulnar deviation and slight wrist extension with the examiner’s thumb over the volar prominence of the scaphoid. B, The wrist is moved to radial deviation with slight wrist flexion while maintaining thumb pressure over the scaphoid. A positive test produces a painful clunk, which reproduces the patient’s symptoms.
The validity of the SST has been studied by LaStayo and Howell.45 They found a 69% sensitivity and a 66% specificity, indicating that approximately one third of the scapholunate injuries in their sample population were missed and that approximately one third of those individuals who did not have an injury tested positively.
Lane46 has described the scaphoid thrust test, which involves pushing on the tubercle of the scaphoid in a dorsal direction. A dorsal shift of the scaphoid is apparent with scapholunate instability.
The scapholunate ballottement test may also be used to assess scapholunate instability.47 This test involves grasping the scaphoid with the thumb and finger with one hand while stabilizing the lunate with the other. The scaphoid is then moved in a volar and dorsal direction on the lunate, and any pain or increased movement relative to the other side is noted.
Palpating in a proximal direction over the dorsal surface of the third metacarpal until a small depression is felt localizes the capitate. Tenderness here may be associated with scapholunate or lunotriquetral instability or with capitolunate degenerative disease, which occurs with scapholunate advanced collapse, or SLAC, wrist. The SLAC wrist has undergone a pattern of degenerative change that is based on and caused by articular alignment problems among the scaphoid, the lunate, and the radius.21
The base of the second and third metacarpals and the CMC joints are localized by palpating proximally along the dorsal surfaces of the index and long metacarpals to their respective bases (Fig. 7-16). Tenderness may indicate injury to the CMC joints and ligaments, which can occur with forced palmar flexion of the wrist and hand.48 A bony prominence at the base of the second and third metacarpal may be a carpal boss. A carpal boss is not necessarily a pathologic process, but rather a variation found in some individuals. It may represent hypertrophic changes of traumatic origin. These can occasionally cause pain and irritation of the local soft tissues.49
The Linscheid test is performed to detect ligament injury and instability of the second and third CMC joints.50 This test is performed by supporting the metacarpal shafts and pressing distally over the metacarpal heads in a palmar and dorsal direction. A positive test produces pain localized to the CMC joints.
The metacarpal stress test involves fully flexing the metacarpophalangeal (MCP) joint and pronating and supinating the metacarpal (Fig. 7-17, online).51 This test helps detect pain and injury at the CMC joint.

Figure 7-17 Metacarpal stress test performed by flexing the metacarpophalangeal joint and pronating and supinating the metacarpal. This test helps to detect pain and injury at the carpometacarpal joints.
The ECRL and the extensor carpi radialis brevis (ECRB) travel radial to Lister’s tubercle, insert at the base of the second and third metacarpals, and act to extend and radially deviate the wrist. The extensor digitorum communis (EDC) travels ulnar to Lister’s tubercle and acts to extend the MCP joints of the digits. Tenderness, nodularity, and fullness of the tendons and pain with resisted motion may indicate tendinitis. The function of the EDC tendons should be assessed by having the patient extend at the MCP joints and then fully extend the digit. Incomplete excursion of a digital extensor tendon suggests tendon adherence or incipient rupture, which can occur at the level of the wrist with rheumatoid arthritis or after distal radius fractures that have had dorsal plate fixation.52
The PIN, which is mainly a motor nerve to the finger extensors, ends in the dorsal capsule of the wrist. This nerve may be a source of pain when a ganglion develops and distends the wrist capsule. Neuromas of the PIN after wrist surgery performed from a dorsal approach can be a reason for persistent postoperative pain. PIN neuritis is characterized by pain with palpation over the dorsal aspect of the wrist and proximal to Lister’s tubercle.53
The structures of the ulnar dorsal zone include the ulnar styloid and the ulnar head, the DRUJ, the TFCC, the hamate, the triquetrum, the lunotriquetral (LT) interval, the fourth and fifth CMC joints, and the extensor carpi ulnaris (ECU).
The ulnar head forms a rounded prominence on the ulnar side of the wrist. It is easily palpated and most prominent with the forearm in pronation. The ulnar styloid is localized ulnar and slightly distal to the ulnar head. Tenderness in this region may be caused by an ulnar styloid fracture or nonunion.
The DRUJ is formed by the sigmoid notch of the radius and the ulnar head and is palpated just radial to the ulnar head (Fig. 7-18, online). Tenderness here may be caused by incongruity or instability with DRUJ arthritis. Prominence of the distal ulnar head is a sign of DRUJ instability and may be associated with a piano key sign (Fig. 7-19, online). Gentle downward pressure is applied to the distal end of the ulna with the forearm in pronation. The head moves volarly but springs back when pressure is released, resembling the action of a piano key. When this maneuver causes pain, the subject may vocalize a “note” of pain.54

Figure 7-18 Palpation of the distal radioulnar joint, just radial to the dorsal prominence of the head of the ulna.

Figure 7-19 Piano key sign for distal radioulnar joint instability. Gentle downward pressure is applied to the distal end of the ulna with the forearm in pronation. The head will move volarly and spring back when released, resembling the action of a piano key.
A variation of the piano key sign, the piano key test, is also used to assess DRUJ instability55 (Fig. 7-20, online). To perform this test, the distal ulna is grasped and moved passively in a volar and dorsal direction at the extremes of pronation and supination. Pain, tenderness, and increased mobility relative to the uninjured side suggest DRUJ instability.
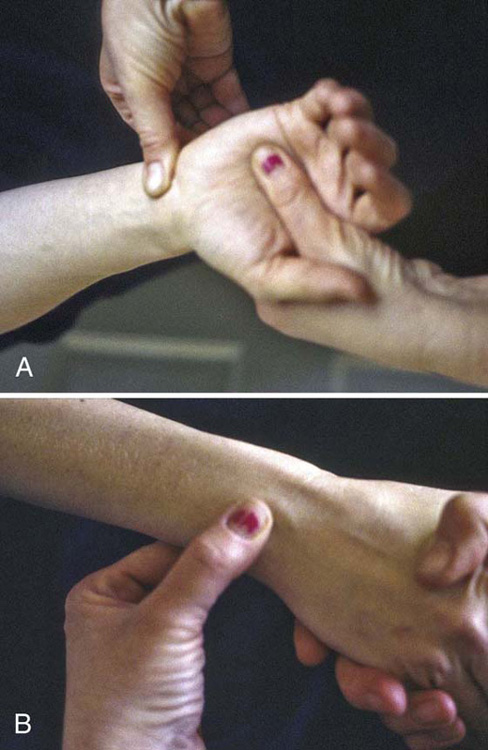
Figure 7-20 Piano key test for distal radioulnar joint instability. The distal ulna is grasped and moved in the volar or dorsal plane at the extremes of pronation (A) and supination (B).
The ulnar compression test involves the application of radially directed pressure on the ulnar head into the sigmoid notch of the radius. When combined with pronation and supination, compression of the DRUJ is painful in the presence of arthritis.20
The TFCC is the soft tissue and ligamentous support for the DRUJ and ulnar carpus. The components of the TFCC include the triangular fibrocartilage (TFC) proper or articular disk, the volar and dorsal radioulnar ligaments, the ulnocarpal ligaments, the ECU sheath, and the LT interosseous ligament.56
The TFCC is palpated between the head of the ulna and the triquetrum. By palpating the shaft of the ulna from proximal to distal along its lateral aspect, the examiner reaches the ulnar styloid. With continued palpation more deeply and in a palmar direction, the fovea can be detected (Fig. 7-21). The fovea is a groove at the base of the ulnar styloid that serves as an attachment point for the TFCC. Berger and Dobyns57 describe the ulnar fovea sign, which is detected by the examiner pressing his or her thumb distally into the interval between the patient’s ulnar styloid process and flexor carpi ulnaris (FCU) tendon, between the volar surface of the ulnar head and the pisiform. A positive sign is indicated by tenderness that replicates the patient’s pain.58 The ulnar fovea sign has been found to detect foveal disruptions of the distal radioulnar ligaments or ulnotriquetral (UT) ligament injuries with 95.2% sensitivity and 86.5% specificity.58 The authors state that differentiation between the two conditions can be made clinically by the presence or absence of DRUJ instability, which is present with foveal disruptions of the radioulnar ligaments but not with UT ligament injuries.

Figure 7-21 Palpation of the fovea, which is a groove at the base of the ulnar styloid. Tenderness may indicate triangular fibrocartilage complex injury.
Kleinman stresses the importance of testing the integrity of the palmar and dorsal fibers of the ligamentum subcruentum, which refers to the deep components of the TFCC inserting into the ulnar styloid fovea.59 With the patient’s forearm in full supination (dorsal fibers of the ligamentum subcruentum are under maximum tension), the examiner, sitting opposite the patient, applies a volarly directed pressure on the distal ulna while pulling the radiocarpal unit dorsally. If the deep dorsal fibers of the ligamentum subcruentum are injured this maneuver will result in pain and with greater injury, subluxation or gross instability. The test is repeated with the forearm in pronation (palmar fibers of the ligamentum subcruentum are under tension) and applying a dorsally directed pressure on the distal ulna and pulling the radiocarpal unit volarly. In this position, pain resulting is attributed to involvement of the palmar fibers of the ligamentum subcruentum.59
Ulnocarpal abutment, a condition involving abutment or impaction of the TFCC between the end of a long ulna (with positive variance) and the triquetrum, may also cause tenderness in this region.60 The TFCC load test is performed to detect ulnocarpal abutment or TFCC tears (Fig. 7-22, online). It is performed by ulnarly deviating and axially loading the wrist and moving it volarly and dorsally or by rotating the forearm. A positive test elicits pain, clicking, or crepitus and reproduces the subject’s symptoms.55 Friedman and Palmer61 describe the ulnocarpal stress test for the evaluation of ulnocarpal abutment. The test is performed by moving the forearm through supination and pronation with the wrist maximally deviated ulnarly, which increases the axial load on the ulnar wrist. A positive test reproduces ulnar wrist pain with rotation. Nakamura found that the test was sensitive but not specific for ulnar-sided pathology.62

Figure 7-22 Triangular fibrocartilage complex (TFCC) load test. Axial load, ulnar deviation, and rotation are applied to the wrist to detect a painful TFCC tear or ulnocarpal abutment.
Lester and colleagues describe the “press test,” which is a simple provocative test to detect TFCC tears. The seated patient pushes up off the chair using the affected wrist, thus creating an axial ulnar load.63 A positive test produces ulnar wrist pain that replicates the patient’s presenting complaint. The authors report 100% sensitivity in a review of 14 patients comparing preoperative test results with surgical findings.
Ulnocarpal instability is caused by disruption of the ulnocarpal ligaments and the TFCC and is characterized by a volar sag and supination of the ulnar carpus (see Fig. 7-3, online). The relocation test, described by Prosser,64 involves the combined movement of carpal pronation and anterior to posterior glide of the carpus on the ulna, which relocates the carpus into normal alignment (Fig. 7-23, online). The test is positive if the relocation of the subluxed ulnar carpus reduces the patient’s wrist pain.64

Figure 7-23 Relocation test described to detect ulnocarpal instability. The wrist with a volar sag and supinated posture is relocated into normal alignment.
The pisiform boost test is similar to the relocation test.57 Dorsally directed pressure is applied over the palmar aspect of the pisiform, resulting in a lifting of the carpus. This test may result in pain, crepitus, or clicking, suggestive of involvement of the ulnar support structures of the wrist.
The hamate is palpable proximal to the base of the fourth and fifth metacarpals. Dorsal tenderness of the hamate may indicate fracture.65
The triquetrum is palpated just distal to the ulnar styloid in the “ulnar snuffbox,” a term used by Beckenbaugh50 to refer to the interval between the FCU and the ECU tendons. The wrist should be radially deviated to palpate the triquetrum because the proximal carpal row slides ulnarly with wrist radial deviation. Tenderness may indicate triquetral fracture or instability.
Pain, swelling, and tenderness in the dorsal triquetral-hamate area is suggestive of midcarpal instability.66,67 This condition, which may be caused by ligament laxity or disruption, is characterized by a volar sag on the ulnar side of the wrist and a clunk that occurs as the wrist moves from radial to ulnar deviation. The midcarpal shift test (catch-up clunk test, pivot shift test) is performed by placing a palmarly directed load over the capitate and then ulnarly deviating the wrist with simultaneous axial load (Fig. 7-24).68 A positive test is one that produces a painful clunk, which reproduces the patient’s symptoms. The clunk represents the abrupt change in position of the proximal carpal row from flexion to extension as the head of the capitate engages the lunate and the hamate engages the triquetrum under compressive load as the wrist moves from radial to ulnar deviation. Lichtman and coworkers68 have developed a grading system for the midcarpal shift test based on the degree of palmar midcarpal translation and the presence of a clunk. Feinstein and associates’ quantitative assessment of the midcarpal shift test69 confirmed its validity and usefulness as an indicator of midcarpal instability.
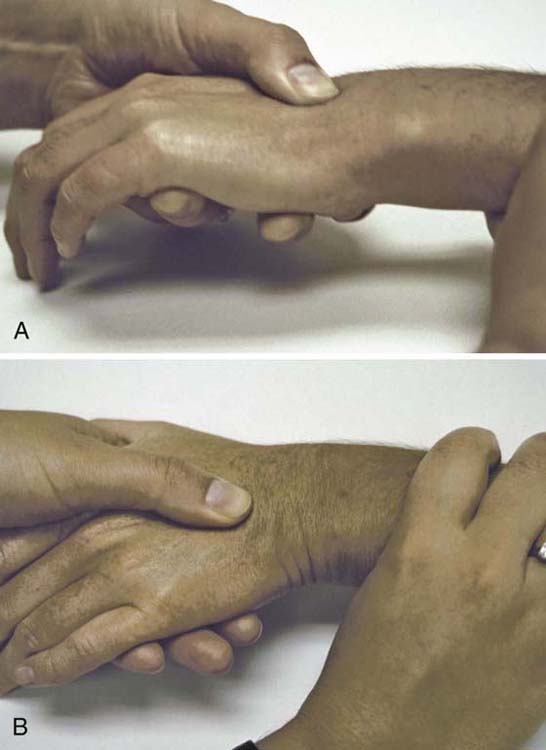
Figure 7-24 Midcarpal shift test. A, The palmarly directed load is placed over the capitate to achieve midcarpal palmar translation. B, This is followed by ulnar deviation with simultaneous axial load. A positive test produces a painful clunk, which reproduces the patient’s symptoms.
The LT interval is palpated just ulnar to the lunate in line with the fourth ray between the EDC and the extensor digiti quinti tendons. Tenderness and swelling in this region may be caused by LT instability. The ballottement test for LT instability is performed by stabilizing the lunate and attempting to displace the triquetrum volarly and dorsally with the other hand (Fig. 7-25). A positive test elicits pain, clicking, or laxity.70

Figure 7-25 Lunotriquetral (LT) ballottement test to assess for LT instability. The lunate is stabilized with one hand while the other attempts to displace the triquetrum volarly and dorsally on the lunate. A positive test elicits painful clicking.
LaStayo and Howell45 found that the sensitivity of the ballottement test to discover a true injury was 64%; that is, approximately one third of LT injuries were missed with this test. The specificity was 44%, suggesting that more than half of those who tested positively had no injury to the LT ligament.45
Kleinman has described a shear test for LT instability (Fig. 7-26). The examiner’s fingers are placed dorsal to the lunate and the thumb is placed on the pisotriquetral complex. With the lunate supported, the pisotriquetral complex is loaded in the anteroposterior plane, creating a shear force across the LT joint. The wrist is then ulnarly and radially deviated. The test is positive if pain or clicking is produced.71

Figure 7-26 Shear test for lunotriquetral (LT) instability. Shear force is applied to the LT joint by loading the pisotriquetral complex in a dorsal direction with the lunate stabilized dorsally and then deviating the wrist in an ulnar and radial direction.
The ulnar snuffbox test involves lateral pressure on the triquetrum in the sulcus distal to the ulnar head formed by the ECU and FCU tendons (Fig. 7-27, online). A positive test reproduces the patient’s pain, suggesting LT instability.72

Figure 7-27 Ulnar snuffbox test for lunotriquetral instability involves lateral pressure on the triquetrum in the sulcus distal to the ulnar head formed by the extensor carpi ulnaris and flexor carpi ulnaris tendons.
The fourth and fifth CMC joints are localized by palpating proximally along the dorsal surfaces of the fourth and fifth metacarpals to their base. Tenderness in this region may indicate ligament injury or fracture.
The ECU tendon is palpated in the gap between the ulnar styloid and the base of the fifth metacarpal with the forearm in pronation and during active ulnar deviation. Tenderness and pain with resisted motion may indicate tendinitis. Ruland and Hogan describe the ECU synergy test as an aid to diagnose ECU tendinitis.73 The test exploits an isometric contraction of the ECU during resisted radial abduction of the thumb with the wrist neutral and forearm supinated. During this maneuver the ECU and FCU fire synergistically to stabilize the wrist, which was confirmed by the authors electromyographically. The test is considered positive when the patient reports ulnar-sided wrist pain. The test minimizes loading of other ulnocarpal structures and allows differentiation between intra-articular and extra-articular pathology.
Pain and snapping with forearm rotation may be caused by ECU subluxation. The ECU tendon is normally held securely in the ulnar groove of the distal ulna by the ECU sheath. With disruption of the sheath, the ECU tendon subluxes and snaps during forearm rotation as it slides out of its groove and bowstrings ulnarly and volarly across the ulnar styloid73,74 (Fig. 7-28). To test for ECU subluxation, the forearm is supinated and the wrist is ulnarly deviated while the tendon is observed and palpated to assess for ulnar and volar subluxation.75

Figure 7-28 The extensor carpi ulnaris (ECU) tendon. To test for ECU subluxation, the forearm is supinated and the wrist ulnarly deviated; the tendon is then observed and palpated to assess for ulnar and volar subluxation.
Structures to assess in the radial volar zone include the radial styloid, the scaphoid tuberosity, the STT joint, the trapezial ridge, the flexor carpi radialis (FCR), the palmaris longus if present, the digital flexor tendons, the median nerve, and the radial artery.
The radial styloid is located at the base of the anatomic snuffbox. Palpate in a palmar direction to find its volar aspect (Fig. 7-29, online). Tenderness here may be caused by distal radius fractures or by radiocarpal ligament injury. Wrist extension and radial deviation accentuates discomfort in the case of extrinsic ligament injury.55
The scaphoid tuberosity can be found just distal to the volar aspect of the distal radius at the base of the thenar crease (Fig. 7-30, online). While palpating this area, the wrist can be moved from ulnar to radial deviation. The scaphoid assumes a flexed position and becomes more prominent and more easily identifiable in radial deviation. Tenderness over the volar scaphoid may indicate scaphoid disease.52

Figure 7-30 Palpation of the volar prominence of the scaphoid. Radial deviation of the wrist causes the scaphoid to assume a flexed position, making it more prominent and easier to palpate.
The STT joint can be found just distal to the scaphoid tuberosity. Tenderness here can be caused by STT arthritis, a common cause for radial volar wrist pain. As the wrist moves into radial deviation, the scaphoid is forced into a flexed position by the trapezium. With arthritis of the STT joint, radial deviation is often painful and restricted.52
Another cause for radial volar wrist symptoms is a volar wrist ganglion, which is the second most common mass of the hand after the dorsal wrist ganglion. The volar ganglion may arise from the radiocarpal or STT joints and manifests clinically as a swelling or soft mass at the base of the thumb to the distal third of the volar forearm.52
The trapezium is located just distal to the distal pole of the scaphoid. Tenderness over the trapezium may indicate trapezial fracture. Ulnar to the scaphoid tuberosity is the FCR tendon, which flexes and radially deviates the wrist. Tenderness and swelling of the tendon and pain with resisted movement are signs of tendinitis.
The digital flexor tendons and the palmaris longus, present in 87% of limbs,76 are ulnar to the FCR. To define the palmaris longus, the thumb and small finger are opposed and the wrist flexed. Swelling over the flexor tendons and discomfort with active finger flexion are associated with flexor tenosynovitis.
The median nerve is deep and ulnar to the palmaris longus. Tinel’s sign and Phalen’s tests are clinical tests used to identify median nerve compression at the wrist—that is, CTS. To perform Tinel’s test,77 the median nerve is gently percussed at the wrist level (Fig. 7-31, online). A positive test produces pain and tingling that radiates to the fingers in the median nerve distribution. Phalen’s test78 involves passive flexion of the wrist for 15 to 60 seconds (Fig. 7-32). A positive test produces numbness and tingling in the distribution of the median nerve.78 Smith and coworkers79 described a modification of Phalen’s test that involves pinching the thumb and index with the wrist flexed; they found that this was more reliable in young people. The Durkan carpal compression test involves application of direct pressure over the carpal tunnel.80 MacDermid and Doherty, in a narrative review, reported that Phalen’s test and the carpal compression test have the highest overall accuracy, whereas Tinel’s nerve percussion test is more specific to axonal damage that may occur as a result of moderate to severe CTS. Sensory evaluation of light touch and vibration can detect early sensory changes, but two-point discrimination and thenar atrophy indicate more advanced nerve compression.81

Figure 7-31 Tinel’s sign involves light percussion of the median nerve at the wrist level to detect median nerve compression within the carpal canal.
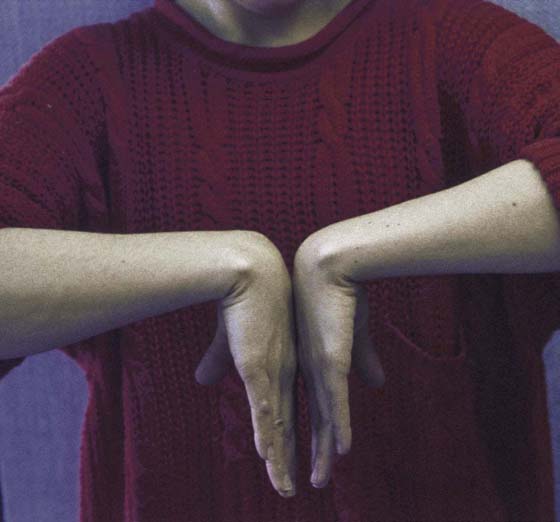
Figure 7-32 Phalen’s test for median nerve compression at the wrist involves passive flexion of the wrist for 15 to 60 seconds. A positive test produces numbness and tingling in the distribution of the median nerve.
Graham and colleagues developed standardized clinical diagnostic criteria for CTS, which include numbness in the median nerve distribution, nocturnal numbness, weakness or atrophy of the thenar musculature, positive Tinel’s sign, positive Phalen’s test, and loss of two-point discrimination.82 The authors assert that these criteria should lead to more effective treatment by improving the consistency of the diagnosis of CTS.
The radial artery lies radial to the FCR. Allen’s test is used to assess the patency of the radial and ulnar arteries (Fig. 7-33, online).83 To perform this test, the patient makes a tight fist and the examiner occludes both the radial and ulnar arteries. The subject opens and closes the hand until the skin is white and blanched. The radial artery is then released while compression of the ulnar artery is maintained, and the palm is observed for flushing, which indicates blood flow. If there is no flush or if flushing is delayed relative to the uninvolved side, occlusion may be present. The test is repeated to assess the ulnar artery. Symptoms of arterial occlusion include coldness and pain.

Figure 7-33 Allen’s test to evaluate the radial and ulnar arteries. A, Subject makes a tight fist several times while the examiner occludes both arteries until the skin is white and blanched. B, One of the arteries is released and the palm is observed for flushing. The test is repeated for the other artery.
Gelberman and Blasingame introduced a variation, the timed Allen test, which records the time it takes for color to return to the hand after either the ulnar or radial artery compression is released.84 He found the average time for radial artery refill was 2.4 seconds ±1.2 and 2.3 seconds ±1.0 for the ulnar artery in a study of 800 hands. The digital Allen test is performed by occluding both digital arteries at the base of the finger and having the patient flex and extend the finger several times to blanch the finger and then observe for return of color.85
The structures to assess in the ulnar volar zone include the pisiform, the hook of the hamate, the FCU, and the ulnar nerve and artery.
The pisiform is located at the base of the hypothenar eminence at the flexion crease of the wrist. It is a carpal sesamoid bone that overlies the triquetrum and lies within the fibers of the FCU. With the hand relaxed, the pisiform can be moved easily from side to side. Tenderness with palpation of the pisiform may indicate fracture or pisotriquetral arthritis, which can occur with impact loading on the ulnar side of the wrist and proximal palm, resulting in impaction of the pisotriquetral articular surface.86
The shear test for pisotriquetral arthritis involves pushing or rocking the pisiform into or across the triquetrum (Fig. 7-34, online). A positive test elicits pain or crepitus.55

Figure 7-34 Pisotriquetral shear test for arthritis involves pushing the pisiform into or across the triquetrum.
The hook of the hamate is found in the hypothenar eminence radial and 1 to 2 cm distal to the pisiform. Tenderness may indicate hamate fracture. Pain may be accentuated with resisted flexion of the ring and small fingers with the wrist in ulnar deviation because the flexor tendons of the ring and small fingers rub against the fractured surface of the hamate during flexion.87
Thrombosis of the ulnar artery may cause ulnar-sided pain and coldness. This may result from repeated impact on the ulnar side of the palm when using the hand to substitute for a hammer. This is referred to as ulnar hammer, or hypothenar hammer, syndrome.88 Allen’s test, described previously, is used to detect occlusion of the ulnar artery.
Cyclist’s palsy refers to ulnar-nerve compression within Guyon’s canal. Long-distance cyclists often develop numbness and paresthesias in the small and ring fingers secondary to sustained compression of the ulnar nerve on the handlebars of their bicycle.88,89
The FCU is palpated on the ulnar, volar side of the wrist. This tendon is easily identified with wrist flexion, ulnar deviation, and fifth-finger abduction. Tenderness, fullness, and discomfort with resisted motion are signs of tendinitis.
Additional tests for the assessment of wrist pain include the carpal shake test, the windmill test, and the sitting hands test. The carpal shake test is performed by grasping the distal forearm and “shaking” or passively extending and flexing the wrist. This is an “all or none” test; that is, lack of resistance or lack of complaint are significant, suggesting no pain at the wrist.57
The windmill test is performed by grasping the forearm and passively and rapidly moving the wrist in a circular pattern, simulating the rotation of a windmill.57 This is also an all or none test.
The sitting hands test is used to gauge the severity of wrist involvement.57 The subject places both hands on the seat of the chair and pushes off, attempting to hold himself or herself suspended using only hands. This maneuver produces great stresses in the wrist and is too difficult in the presence of significant synovitis.
Clinical examination of the wrist requires a thorough knowledge of wrist anatomy and pathology. The keys are to localize and identify the tender structures through systematic palpation and to reproduce the patient’s symptoms and identify instability through provocative testing. Not all of the previously described tests need to be performed for every clinical wrist examination. In general, tests are selected for their relevance to the most symptomatic area or structures of the wrist, identified after a screening assessment. It is important to keep in mind that clinical findings must be interpreted with caution. This is because many of the tests described require a subjective response from the patient and their response can be influenced by factors such as motivation to magnify symptoms or limited comprehension. North and Meyer90 correlated clinical and arthroscopic findings and concluded that it is possible to identify the region of injury based on a clinical examination, but not the specific ligament. Imaging and other diagnostic studies are needed to complete the evaluation of the wrist and to permit an accurate diagnosis.
1. Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg. 1989; 14A: 594–606.
2. Mayfield J. Patterns of injury to carpal ligaments. Clin Orthop Relat Res. 1984; 187: 36–42.
3. Weber ER, Chao EY. An experimental approach to the mechanism of scaphoid waist fractures. J Hand Surg. 1978; 3: 142–148.
4. Burman M. Stenosing tenovaginitis of the dorsal and volar compartments of the wrist. AMA Arch Surg. 1952; 65: 752–762.
5. LaStayo PC, Wheeler DL. Reliability of passive wrist flexion and extension goniometric measurements: a multicenter study. Phys Ther. 1994; 74: 162–174.
6. Joint Motion: Method of Measuring and Recording. Chicago: American Academy of Orthopaedic Surgeons; 1965.
7. Palmer AK, Werner FW, Murphy D, Glisson R. Functional wrist motion: a biomechanical study. J Hand Surg. 1985; 10A: 39–46.
8. Ryu J, Cooney WP 3rd, Askew LJ, et al. Functional ranges of motion of the wrist joint. J Hand Surg. 1991; 16A: 409–419.
9. Waylett-Rendall J, Seibly DS. A study of the accuracy of a commercially available volumeter. J Hand Ther. 1991; 4: 10–13.
10. van Velze CA, Kluever I, van der Merwe CA, Mennen U. The difference in volume of dominant and non-dominant hands. J Hand Ther. 1991; 4: 6–9.
11. Czitrom AA, Lister GD. Measurement of grip strength in the diagnosis of wrist pain. J Hand Surg. 1988; 13A: 16.
12. LaStayo P, Weiss S. The GRIT: a quantitative measure of ulnar impaction syndrome. J Hand Ther. 2001; 14: 173–179.
13. Gelberman RH., et al. Sensibility testing in peripheral nerve compression syndrome: an experimental study in humans. J Bone Joint Surg. 1983; 65A: 632–638.
14. Shin AY, Deitch MA, Sachar K, Boyer MI. Ulnar-sided wrist pain: diagnosis and treatment. Instr Course Lect. 2005; 54: 115–128.
15. Bell SJ, Hofmeister EP, Moran SL, Shin AY. The diagnostic utility of midcarpal anesthetic injection in the evaluation of chronic wrist pain. Hand. 2007; 2: 39–45.
16. Freeland AE. Comment on “The diagnostic utility of midcarpal anesthetic injection in the evaluation of chronic wrist pain”. Hand. 2007; 2: 46–47.
17. Green DP. Diagnostic and therapeutic value of carpal tunnel injection. J Hand Surg Am. 1984; 9 (6):850–854.
18. Boyer MI. Corticosteroid injection for carpal tunnel syndrome. J Hand Surg Am. 2008; 33A: 1414–1416.
19. Torosian CM, Brown DE, Skirven T, Lichtman DM. Physical examination of the wrist. In: Lichtman DM, Alexander AH, eds. The Wrist and its Disorders. 2nd ed Philadelphia: WB Saunders; 1997:73–89.
20. Whipple TL. Preoperative evaluation and imaging. In: Whipple TL, ed. Arthroscopic Surgery: The Wrist. Philadelphia: JB Lippincott; 1992:69.
21. Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984; 9A: 358–365.
22. Ruby LK., et al. Relative motion of selected carpal bones: a kinematic analysis of the normal wrist. J Hand Surg Am. 1988; 13A: 1–10.
23. Osterman AL, Mikulics M. Scaphoid nonunion. Hand Clin. 1988; 14: 437–455.
24. Kondoyannis PN. A clinical sign in suspected fractures of the carpal scaphoid. J Bone Joint Surg Am. 1982; 64A: 784.
25. Watson HK, Ryu J. Evaluation of arthritis of the wrist. Clin Orthop Relat Res. 1986; 202: 57–67.
26. Swanson A. Disabling arthritis at the base of the thumb: treatment by resection of the trapezium and flexible implant arthroplasty. J Bone Joint Surg Am. 1972; 54A: 456–471.
27. Young D, Papp S, Giachino A. Physical examination of the wrist. Orthop Clin North Am. 2007; 38: 149–165.
28. Finkelstein H. Stenosing tenovaginitis at the radial styloid process. J Bone Joint Surg. 1930; 12: 509–540.
29. Kiefhaber TR, Stern PJ. Upper extremity tendinitis and overuse syndromes in the athlete. Clin Sports Med. 1992; 11: 39–55.
30. Grundberg AB, Reagan DS. Pathologic anatomy of the forearm: intersection syndrome. J Hand Surg Am. 1985; 10A: 299–302.
31. Parmelee-Peters K, Eathorne SW. The wrist: common injuries and management. Prim Care Clin Office Pract. 2005; 32: 35–70.
32. Szabo RM. Superficial radial nerve compression syndrome. In: Szabo RM, ed. Nerve Compression Syndromes. Thorofare, NJ: Slack; 1989:59.
33. Dellon AL, Mackinnon SE. Radial sensory nerve entrapment in the forearm. J Hand Surg Am. 1986; 11A: 199–205.
34. Linscheid RL, Dobyns JH. Athletic injuries of the wrist. Clin Orthop. 1985; 198: 141–151.
35. Weiker GG. Hand and wrist problems in the gymnast. Clin Sports Med. 1992; 11: 189–202.
36. Kienbock R. Concerning traumatic malacia of the lunate and its consequences: degeneration and compression fractures. Clin Orthop. 1980; 149: 4–8.
37. Kozin SH, Bishop AT. Ganglions of the wrist. In: Cooney WP, Linscheid RC, Dobyns JH, eds. The Wrist: Diagnosis and Operative Treatment. St Louis: Mosby; 1998:1166–1180.
38. Gunther SF. Dorsal wrist pain and the occult scapholunate ganglion. J Hand Surg. 1985; 10: 697–703.
39. Steinberg BD, Kleinman WB. Occult scapholunate ganglion: a cause of dorsal radial wrist pain. J Hand Surg Am. 1999; 24A: 225–231.
40. Shaw JA, Manders EK. Extensor digitorum brevis manus muscle, a clinical reminder. Orthop Rev. 1988; 17: 867–869.
41. Watson HK. Comments on the wrist. Presented at an ASHT continuing education program Comprehensive Approach to Challenging Wrist Problems. St Louis: 1993.
42. Kayalar M, Vatansever A, Bal E, et al. The importancy of finger extension test in the diagnosis of occult wrist ganglion. Acta Orthop Traumatol Turc. 2007; 41 (1):42–47.
43. Watson HK, Ashmead D, Makhlouf MV. Examination of the scaphoid. J Hand Surg Am. 1988; 13A: 657–660.
44. Wolfe SW, Gupta A, Crisco JJ. Kinematics of the scaphoid shift test. J Hand Surg Am. 1997; 22A: 801–806.
45. LaStayo P, Howell J. Clinical provocative tests used in evaluating wrist pain: a descriptive study. J Hand Ther. 1995; 3: 10–17.
46. Lane LB. The scaphoid shift test. J Hand Surg. 1993; 18: 366–368.
47. King GJ, McMurtry RY. Physical examination of the wrist and hand. In: Gilula LA, Yin Y, eds. Imaging of the Wrist and Hand. Philadelphia: WB Saunders; 1996:28.
48. Carroll RE, Carlson E. Diagnosis and treatment of injury to the second and third carpometacarpal joints. J Hand Surg Am. 1989; 14A: 102–107.
49. Joseph RB., et al. Chronic sprains of the carpometacarpal joints. J Hand Surg. 1981; 6: 172–180.
50. Beckenbaugh RD. Accurate evaluation and management of the painful wrist following injury. Orthop Clin North Am. 1984; 15: 289–306.
51. Fusi S, Watson HK, Cuono CB. The carpal boss: a 20 year review of operative management. J Hand Surg. 1995; 20: 405–408.
52. Cooney WP, Bishop AT, Linscheid RL. Physical exam of the wrist. In: Cooney WP, Linscheid RL, Dobyns JH, eds. The Wrist: Evaluation and Operative Treatment. St Louis: Mosby; 1998:236–261.
53. Dellon AL, Seif SS. Anatomic dissections relating to the posterior interosseous nerve to the carpus and the etiology of dorsal wrist ganglion pain. J Hand Surg. 1978; 3: 326–332.
54. Rana NA, Taylor AR. Excision of the distal end of the ulna in rheumatoid arthritis. J Bone Joint Surg Br. 1973; 55B: 96–105.
55. Lipschultz T, Osterman AL. New methods in the evaluation of chronic wrist pain. Univ Penn Orthop J. 1990; 6: 37–40.
56. Melone CP, Nathan R. Traumatic disruption of the triangular fibrocartilage complex. Clin Orthop Rel Res. 1992; 275: 65–73.
57. Berger RA, Dobyns JH. Physical examination and provocative maneuvers of the wrist. In: Gilula LA, Yin Y, eds. Imaging of the Wrist and Hand. Philadelphia: WB Saunders; 1996.
58. Tay SC, Tomita K, Berger RA. The “ulnar fovea sign” for defining ulnar wrist pain: an analysis of sensitivity and specificity. J Hand Surg Am. 2007; 32A: 438–444.
59. Kleinman WB. Stability of the distal radioulnar joint: biomechanics, pathophysiology, physical diagnosis, and restoration of function; what we have learned in 25 years. J Hand Surg Am. 2007; 32A (7):1086–1106.
60. Chun S, Palmer AK. The ulnar impaction syndrome: follow-up to ulnar shortening osteotomy. J Hand Surg Am. 1993; 18A: 46–53.
61. Friedman SL, Palmer AK. The ulnar impaction syndrome. Hand Clin. 1991; 7: 295–310.
62. Nakamura T, Yabe Y, Horiuchi Y. Functional anatomy of the triangular fibrocartilage complex. J Hand Surg. 1996; 21B: 581–586.
63. Lester B, Halbrecht J, Levy IM, Gaudinez R. “Press test” for office diagnosis of triangular fibrocartilage complex tears of the wrist. Ann Plast Surg. 1995; 35 (1):41–45.
64. Prosser R. Conservative management of ulnar carpal instability. Aust Physiother. 1996; 41: 41–48.
65. Polivy KD, Millender LH, Newberg A, et al. Fractures of the hook of the hamate: a failure of clinical diagnosis. J Hand Surg Am. 1985; 10A: 101–104.
66. Lichtman DM, Schneider JR, Swafford AR, Mack GR. Ulnar midcarpal instability: clinical and laboratory analysis. J Hand Surg Am. 1982; 7: 515–523.
67. Rao SB, Culver JE. Triquetralhamate arthrodesis for midcarpal instability. J Hand Surg Am. 1995; 20A: 583–589.
68. Lichtman DM, Gaenslen ES, Pollack GR. Midcarpal and proximal carpal instabilities. In: Lichtman DM, Alexander CE, eds. The Wrist and Its Disorders. Philadelphia: WB Saunders; 1997:316–328.
69. Feinstein WK, Lichtman DM, Nobel PC, et al. Quantitative assessment of the midcarpal shift test. J Hand Surg. 1999; 24A: 977–983.
70. Reagan DS, Linscheid RL, Dobyns JH. Lunotriquetral sprains. J Hand Surg Am. 1984; 9A: 502–514.
71. Bednar JM, Osterman AL. Carpal instability: evaluation and treatment. J Am Acad Orthop Surg. 1993; 1: 10–17.
72. Ambrose L, Posner M. Lunate-triquetral and midcarpal joint instability. Hand Clin. 1992; 8: 653–668.
73. Ruland RT, Hogan CJ. The ECU synergy test: an aid to diagnose ECU tendonitis. J Hand Surg Am. 2008; 33A: 1777–1782.
74. Burkhart SS, Wood MB, Linscheid RL. Posttraumatic recurrent subluxation of the extensor carpi ulnaris tendon. J Hand Surg. 1982; 7: 1–3.
75. Eckhardt WA, Palmer AK. Recurrent dislocation of the extensor carpi ulnaris tendon. J Hand Surg. 1981; 6: 629–631.
76. Reimann RF, Daseler EH, Anson BJ, Beaton LE. The palmaris longus muscle and tendon: a study of 1600 extremities. Anat Rec. 1944; 489: 495.
77. Moldaver J. Tinel’s sign: its characteristics and significance. J Bone Joint Surg Am. 1978; 60A: 412–414.
78. Phalen G. The carpal tunnel syndrome: seventeen years experience in diagnosis and treatment of 654 hands. J Bone Joint Surg Am. 1966; 48A: 211–228.
79. Smith EM, Sonstegard DA, Anderson WT. Carpal tunnel syndrome: contribution of flexor tendons. Arch Phys Med Rehabil. 1977; 58: 379–385.
80. Durkan JA. The carpal-compression test: an instrumental device for diagnosing carpal tunnel syndrome. Orthop Rev. 1994; 23: 522–525.
81. MacDermid JC, Doherty T. Clinical and electrodiagnostic testing of carpal tunnel syndrome: a narrative review. J Orthop Sports Phys Ther. 2004; 34: 565–588.
82. Graham B, Regehr G, Naglie G, Wright JG. Development and validation of diagnostic criteria for carpal tunnel syndrome. J Hand Surg Am. 2006; 31A: 919.e1–919.e7.
83. Levinsohn DG, Gordon L, Sessler DI. The Allen’s test: analysis of four methods. J Hand Surg. 1991; 16: 279–282.
84. Gelberman RH, Blasingame JP. The timed Allen’s test. J Trauma. 1981; 21: 477–479.
85. Chloros GD., et al. Noninvasive evaluation of upper extremity vascular perfusion. J Hand Surg Am. 2008; 33A: 591–600.
86. Carroll RE, Coyle MP. Dysfunction of the pisotriquetral joint: treatment by excision of the pisiform. J Hand Surg Am. 1985; 10A: 703–707.
87. Bishop AT, Beckenbaugh RD. Fractures of the hamate hook. J Hand Surg. 1988; 13: 135–139.
88. Topper SM, Wood MB, Cooney WP. Athletic injuries of the wrist. In: Cooney WP, Linscheid RL, Dobyns JH, eds. The Wrist: Evaluation and Operative Treatment. St Louis: Mosby; 1998:1031–1074.
89. Wood MB, Dobyns JH. Sports related extra-articular wrist syndromes. Clin Orthop Relat Res. 1986; 202: 93–102.
90. North ER, Meyer S. Wrist injuries: correlation of clinical and arthroscopic findings. J Hand Surg. 1990; 15: 915–920.