CHAPTER 14
Diagnostic Imaging of the Shoulder and Elbow
CONOR P. SHORTT, MB, BCh, BAO, MSc, MRCPI, FRCR, FFR RCSI AND WILLIAM B. MORRISON, MD
CRITICAL POINTS
Shoulder Ultrasound Applications
▪ Rotator cuff integrity assessment (especially post arthroplasty)
▪ Evaluation and fenestration of rotator cuff calcific tendinosis
▪ Evaluation of rotator cuff muscle atrophy
▪ Dynamic imaging of impingement
▪ Assessment of glenohumeral effusion
▪ Guided subacromial-subdeltoid bursal or joint injection
Elbow Ultrasound Applications
▪ Evaluation and treatment of medial and lateral epicondylitis
▪ Dynamic assessment of medial and lateral collateral stabilizers
▪ Ulnar and posterior interosseous nerve impingement assessment
MRI Contraindications*
Absolute
▪ Cardiac pacemaker/implantable cardiac defibrillators
▪ Ferromagnetic CNS clips
▪ Orbital metallic foreign body
▪ Electronically, magnetically, and mechanically activated implants
Relative
▪ Prosthetic heart valves
▪ Foreign bodies in non-vital locations
▪ Infusion pumps/nerve stimulators
▪ Cochlear and stapedial implants
Shoulder MRI Applications
▪ Rotator cuff pathology
▪ Labral/capsular injury (best using direct MR arthrography)
▪ Rotator cuff interval lesions
▪ Muscle and other tendon tears
▪ Occult fracture/bone bruise
▪ Osseous and soft tissue neoplasms
▪ Infection
Elbow MRI Applications
▪ Occult fracture/bone bruise
▪ Cartilage injury
▪ Osteochondritis dissecans—evaluation of stability
▪ Medial and lateral collateral ligament injury
▪ Muscle and tendon tears around the elbow including epicondylitis
▪ Osseous and soft tissue neoplasms
▪ Infection
Diagnostic imaging is an invaluable adjunct to clinical examination in the assessment of many upper extremity disorders. Knowledge of available imaging modalities is essential to determining the most appropriate and cost-effective imaging test to be performed for a given clinical question. Some modalities, although perceived as superior to others, may be inappropriate in a particular clinical setting. For example, ultrasound in the assessment of rotator cuff tears after shoulder arthroplasty is, in most cases, superior to MRI.1 Ordering the correct testing with pertinent clinical details in the appropriate setting yields maximum information and facilitates optimum patient treatment.
Radiography of the shoulder and elbow should be considered in all cases, because it provides useful information about the bony anatomy and a baseline for comparison with follow-up studies as well as acting as a complementary test to advanced imaging techniques. Advanced imaging techniques, such as US, CT, MRI, and nuclear medicine, are invaluable in the appropriate clinical setting, providing clinicians with state-of-the-art radiologic assessment. This chapter first describes the modalities used in shoulder and elbow imaging, and then focuses on how imaging aids diagnosis with respect to specific shoulder and elbow pathologies.
Imaging Modalities
Radiography
Basic radiography has evolved from film-screen radiography, which is still in use today, to increasingly available digital and computed radiography techniques, which are more amenable to manipulation, image transfer and storage, and viewing on workstations.
Standard radiographic projections of the shoulder include an AP (anteroposterior) and lateral view (Y-view). Correctly performed AP and lateral views allow assessment of glenohumeral and acromioclavicular alignment as well as of osseous structures at the shoulder. Radiographs are of particular value in the initial assessment of trauma where fracture or dislocation is suspected, and in the assessment of arthritis, but they are also useful in other cases such as tumor evaluation and calcific rotator cuff tendinosis with hydroxyapatite deposition disease (HADD; Fig. 14-1). Further views of the shoulder are also of value in certain instances; for example, a transthoracic lateral view and axillary (axial) view.
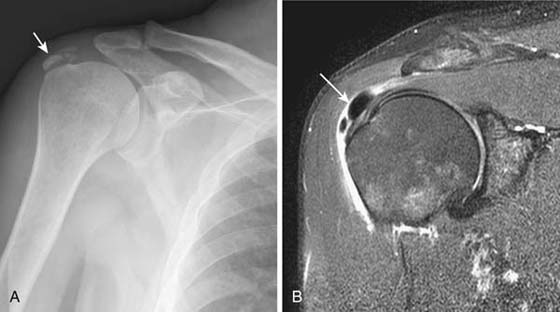
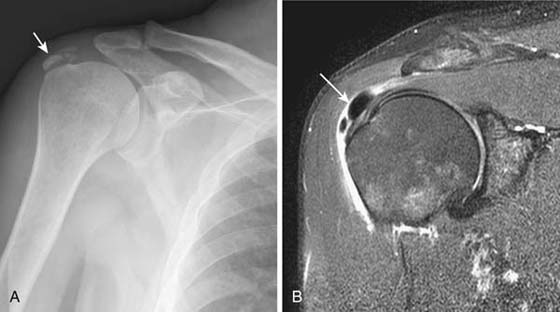
Figure 14-1 Calcific tendinosis of the rotator cuff and associated bursitis. A, Anteroposterior radiograph of the shoulder demonstrates calcific foci at the distal supraspinatus tendon consistent with calcific tendinosis or hydroxyapatite deposition disease (HADD). B, Coronal fat-saturated T2-weighted image of the shoulder in the same patient demonstrates foci of low (black) signal in the distal supraspinatus tendon (arrow) extruding into the adjacent subacromial/subdeltoid bursa with associated reactive bursitis (fluid bright signal).
Standard views of the elbow include AP and lateral radiographs. Oblique AP views may be of value in assessing for suspected radial head fractures not seen on conventional views.
Arthrography
Shoulder arthrography still has a role in the assessment of rotator cuff tears and adhesive capsulitis, although recently it is rarely used in isolation, being more often combined with MRI (direct MR arthrography) or sometimes CT arthrography. MR arthrography is usually performed when labral pathology is suspected and is of particular use in patients with instability signs and symptoms.2
For shoulder arthrography, a spinal needle (20–22 gauge) is used to gain access to the shoulder joint, using an anterior or posterior approach under fluoroscopic guidance (Fig. 14-2). The intra-articular position is confirmed with injection of a small amount of iodinated contrast medium, which is typically followed by 14 mL of dilute gadolinium when performing MR arthrography. Undiluted iodinated contrast material is injected when performing CT arthrography. Arthrography of the elbow, usually in association with MR (direct MR arthrography), is used in the assessment of medial and lateral stabilizing ligament integrity and in the assessment of cartilage loss and intra-articular bodies.

Figure 14-2 Shoulder arthrogram. For shoulder arthrography a 20- or 22-gauge spinal needle is used to gain access to the glenohumeral joint. High-density iodinated contrast material is seen flowing easily away from the needle tip into the joint, confirming intra-articular position.
Computed Tomography
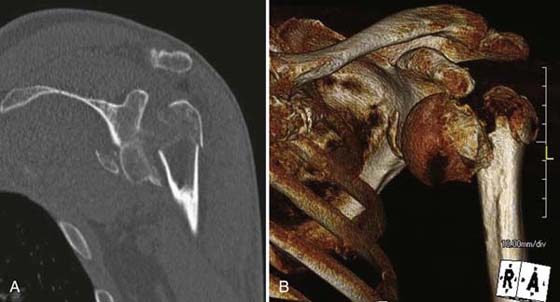
The latest generation CT scanners use multiple detector row arrays. Multidetector CT (MDCT) is a major improvement in CT technology because the activation of multiple detector rows positioned along the patient’s longitudinal axis allows for simultaneous acquisition of multiple slices. This also enables acquisition of thinner slices than were previously possible, allowing generation of exquisite multiplanar reformats (Fig. 14-3). In the setting of orthopedic prosthetic hardware, this technology results in decreased artifact.
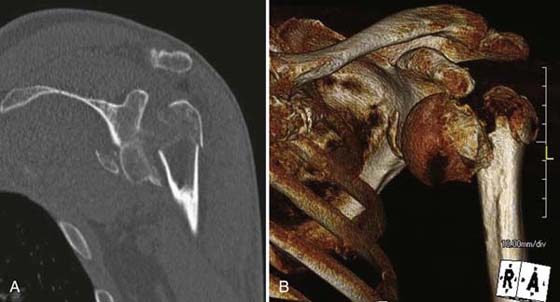
Figure 14-3 Comminuted intra-articular fracture. A, Coronal 2D CT image of a comminuted intra-articular right humeral head and glenoid fracture. B, Reconstructed 3D CT image in the same patient improves appreciation of fracture extent and pattern, assisting in operative planning.
CT allows precise characterization of fractures at the shoulder and elbow, defining degree of comminution and displacement, and identifying intra-articular osseous bodies if present. CT arthrography is an alternative to MR arthrography, allowing assessment of rotator cuff tears (especially full-thickness), labral tears, and cartilage loss at the glenohumeral joint (Fig. 14-4).3 CT may also be used for image-guided intervention.

Figure 14-4 CT arthrogram of the shoulder. In patients for whom MRI is contraindicated, valuable information can be obtained with CT arthrography. In this instance iodinated contrast medium is seen to fill the inferior axillary recess of the glenohumeral joint as expected (curved arrow). However, contrast material is also seen to fill the subacromial/subdeltoid bursa (straight arrow), secondary to a full-thickness rotator cuff tear (tear not shown).
Ultrasound
US is the medical imaging modality used to acquire and display the acoustic properties of tissues. A transducer array (transmitter and receiver of US pulses) sends sound waves into the patient and receives returning echoes, which are converted into an image.
For musculoskeletal imaging of more superficial structures (tendons, ligaments), a high-frequency beam with a smaller wavelength provides superior spatial resolution and image detail. Thus, use of an appropriate transducer is of critical importance in performing shoulder and elbow imaging. Higher-frequency transducers are now available, ranging from 7.5 MHz up to as much as 15 MHz.
The acquisition of high-quality US images depends on operator experience, but in the right hands US can be a powerful tool in the assessment of a wide range of shoulder4-6 and elbow7-9 pathologies. US has shown increased utility for diagnostic and therapeutic procedures and for specific clinical concerns by providing more infrastructural detail more cost-effectively through improved transducer technology.10,11 US is best used when a clinical question is well formulated and the condition is dichotomous (e.g., Is there a full-thickness rotator cuff tear or not?). US is also excellent for assessment of injuries that are only observed during certain motions or in certain positions. For example, ulnar nerve subluxation can be documented during flexion and extension. Performing percutaneous interventions with US ensures accurate needle tip placement and helps direct the needle away from other regional soft-tissue structures and neurovascular bundles.12 Applications of US at the shoulder and elbow are depicted in Boxes 14-1 and 14-2.
Box 14-1 Applications of Shoulder Ultrasound
Rotator cuff integrity assessment (especially after arthroplasty)
Evaluation and fenestration of rotator cuff calcific tendinosis and hypervascularity
Evaluation of rotator cuff muscle atrophy
Dynamic imaging of impingement
Assessment of glenohumeral effusion
Guided subacromial/subdeltoid bursal or joint injection
Box 14-2 Applications of Elbow Ultrasound
Evaluation and treatment of medial and lateral epicondylitis
Dynamic assessment of medial and lateral collateral stabilizers
Ulnar and posterior interosseous nerve impingement
Magnetic Resonance Imaging
MRI is the workhorse of musculoskeletal imaging throughout the body, including the shoulder and elbow. MRI relies on the magnetic properties of the proton and does not involve ionizing radiation. It utilizes a strong magnetic field (most commonly 1.5 T) to align these protons. Their energy level is altered by a transmitted radiofrequency (RF) pulse, after which they are allowed to relax back to their original state, releasing energy. This energy is used to formulate an image based on the different relaxation properties of tissues. Various “sequences” are prescribed to focus on the different relaxation properties of the tissues in question. The main components of an MRI system include a strong magnetic field, coils (to transmit and receive RF signals), and gradients to localize signals quickly. MRI technology continues to evolve, with recent developments focusing on higher field strength magnets (3 T) and improved coils and gradients. Limitations of MRI include patient contraindications (Box 14-3), metallic susceptibility artifact from hardware, and patient intolerance secondary to claustrophobia.
Box 14-3 MRI Contraindications*
ABSOLUTE
Cardiac pacemaker or implantable cardiac defibrillators
Ferromagnetic CNS clips
Orbital metallic foreign body
Electronically, magnetically, and mechanically activated implants
RELATIVE
Prosthetic heart valves
Foreign bodies in nonvital locations
Infusion pumps and nerve stimulators
Cochlear and stapedial implants
The principal applications of MRI of the shoulder and elbow are show in Boxes 14-4 and 14-5. Direct MR arthrography is the favored technique for examination of possible shoulder labral tears. It involves direct injection of dilute gadolinium under fluoroscopic guidance as described earlier. It is also of value in assessing the rotator cuff and the stabilizing structures of the elbow. Indirect MR arthrography of the shoulder and elbow involves an IV injection of gadolinium, which diffuses into the joint cavity causing an “arthrographic” effect.
Box 14-4 Shoulder MRI Applications
Rotator cuff pathology
Labral or capsular injury (best using direct MR arthrography)
Rotator cuff interval lesions
Muscle and other tendon tears
Nerve pathology and impingement
Osseous and soft tissue neoplasms
Infection
MR, magnetic resonance.
Box 14-5 Elbow MRI Applications
Occult fracture or bone bruise
Cartilage injury
Osteochondritis dissecans—evaluation of stability
Medial and lateral collateral ligament injury
Muscle and tendon tears around the elbow including epicondylitis
Nerve pathology and impingement
Osseous and soft tissue neoplasms
Infection
Nuclear Medicine
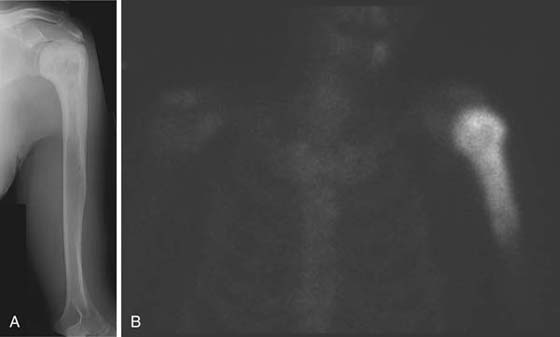
In nuclear medicine a radiopharmaceutical (radioactive isotope coupled with a pharmaceutical) is administered (usually intravenously), and subsequent gamma ray emissions are detected by a gamma camera. An isotope whole-body bone scan is used to detect areas of increased bone turnover, which may indicate pathology depending on the site and degree of activity (Fig. 14-5). The main application in the shoulder and elbow is in the evaluation of neoplasia (particularly to assess for metastatic disease) and osteomyelitis.13
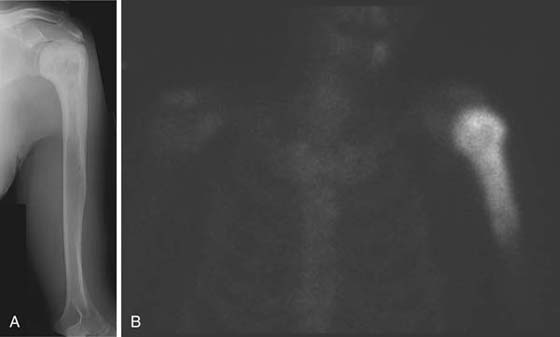
Figure 14-5 Paget’s disease. A, Anteroposterior radiograph of the left humerus demonstrates bony expansion and trabecular and cortical thickening proximally extending to the glenohumeral joint, consistent with Paget’s disease. B, Frontal image from an isotope whole-body bone scan shows marked tracer accumulation in the proximal humerus as expected in Paget’s disease.
The most significant recent advancement in nuclear medicine is positron emission tomography (PET) and combination PET CT scanners with important implications for oncology. (18F) fluorodeoxglucose (FDG) is a metabolic tracer most widely used in clinical PET oncology. PET applications are evolving, but it is currently approved for the diagnosis, staging, and restaging of many common malignancies and has shown efficacy for the detection of osseous metastasis from several malignancies, including lung carcinoma, breast carcinoma, and lymphoma.14 Such metastatic disease may be seen at the shoulder, but less commonly at the elbow and rarely more distally.
Other Modalities
Other modalities used rarely at the shoulder and elbow include fluoroscopy, which is used to assess joint stability, and arteriography, which is used in the assessment and sometimes treatment (embolization) of vascular lesions such as hemangiomas and pseudoaneurysms.
Imaging of Shoulder Pathology
Impingement
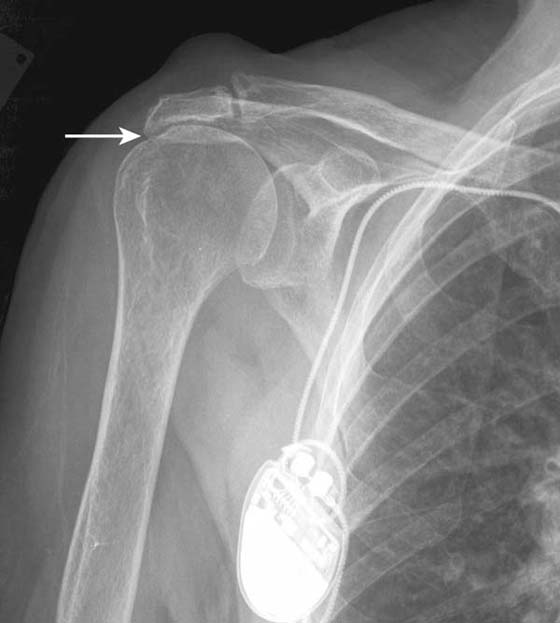
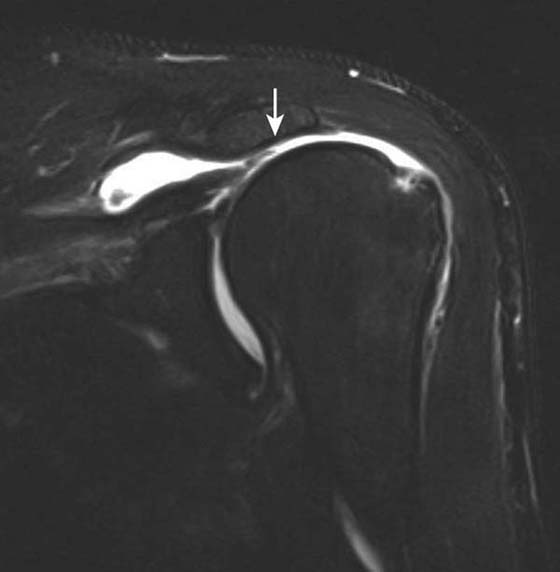
Although shoulder impingement is a clinical diagnosis, it has imaging manifestations that are helpful in guiding treatment. Radiography plays a role in the initial examination of impingement. Subacromial spurs, glenohumeral joint osteoarthritis, and evidence of chronic rotator cuff tear with a high riding humeral head may be identified with radiographs,5 which may further influence management decisions (Fig. 14-6). Noncontrast shoulder MRI is frequently employed in the assessment of impingement. Manifestations of impingement, such as subacromial spur, subacromial/subdeltoid (SASD) bursitis, and rotator cuff tears, are all easily demonstrated on MRI.15-17 Features of a rotator cuff tear that can be assessed on MRI include tear type (full vs. partial thickness), tear location, tear dimensions, tear morphology, tear gap/degree of tendon retraction, and the presence of rotator muscle atrophy (Fig. 14-7).
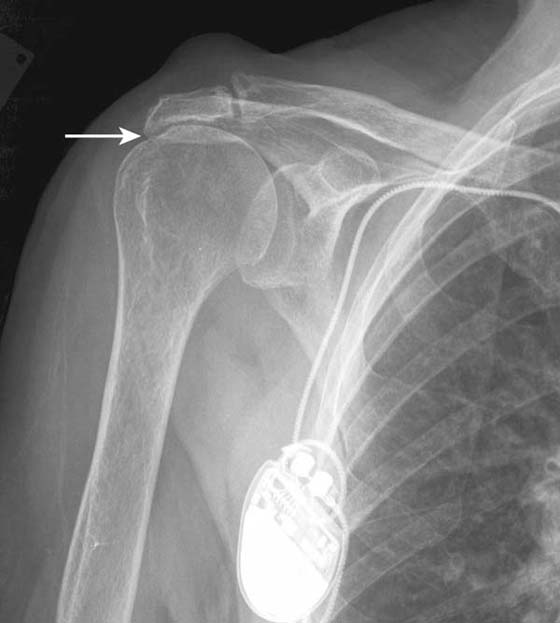
Figure 14-6 Chronic rotator cuff tear. Anteroposterior radiograph of the shoulder demonstrates severe narrowing of the acromiohumeral distance (arrow), indicating chronic rotator cuff tear. Marked subacromial spur formation is also seen. An MRI was contraindicated in this patient due to the presence of a cardiac pacemaker.
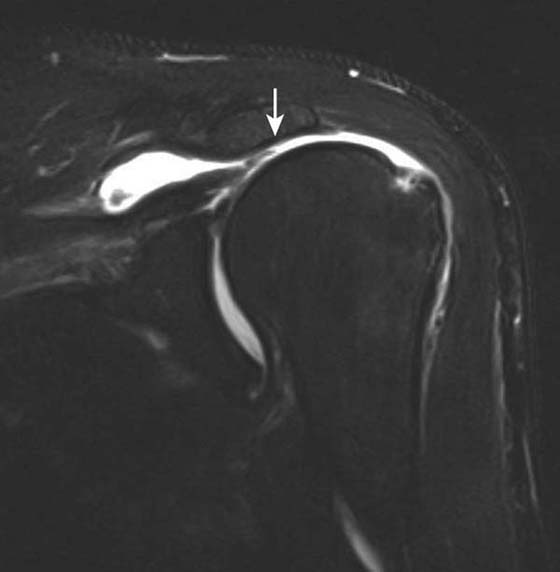
Figure 14-7 Full-thickness rotator cuff tear. Coronal fat-suppressed T2-weighted MRI of the shoulder demonstrates a large tear of the supraspinatus tendon. The tendon is torn, frayed, and retracted back, almost to glenohumeral joint level (arrow).
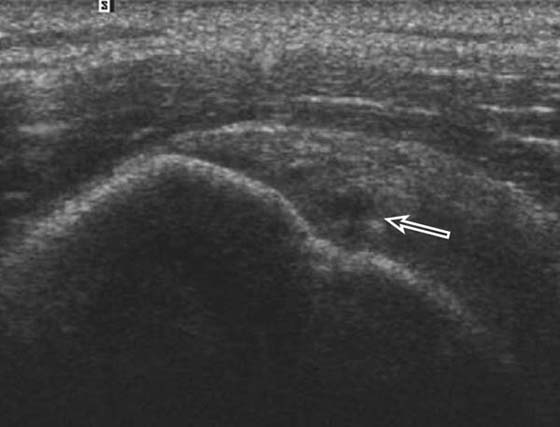
US is also a valuable tool in the assessment of impingement18 and is useful for the evaluation of rotator cuff pathology (Fig. 14-8) although it cannot give a global assessment including labral, capsular, cartilage, and marrow pathology. US is useful in the setting of rotator cuff repair and is particularly useful in shoulder arthroplasty where susceptibility artifact from the metallic prosthesis on MRI would limit interpretation of the adjacent cuff.19 In addition, calcific tendinosis of the rotator cuff is well demonstrated on US20 and is often amenable to SASD bursal injection of steroid and anesthetic or needling in refractory cases.
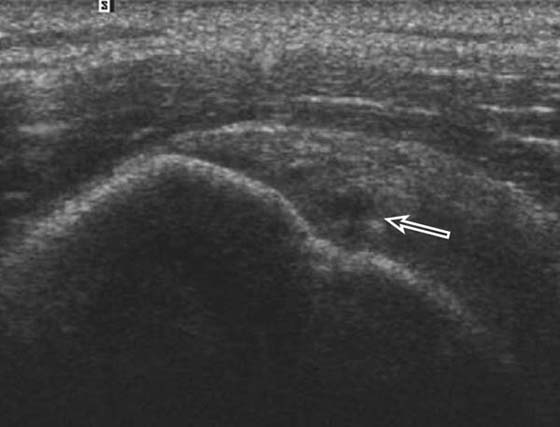
Figure 14-8 Partial-thickness rotator cuff tear. Ultrasound along the long axis of the distal supraspinatus tendon adjacent to its insertion on the greater tuberosity demonstrates a focal partial undersurface tear (arrow) as indicated by a hypoechoic (dark) defect.
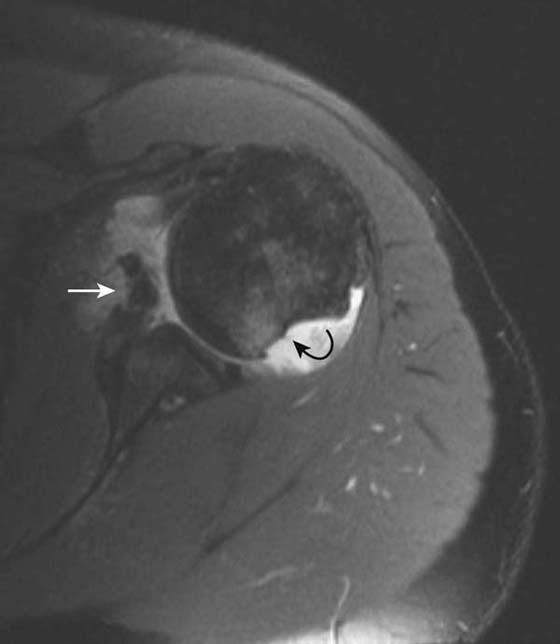
Instability
Radiography is useful in defining osseous alignment at the glenohumeral joint and may demonstrate a Hill–Sachs or bony Bankart’s lesion. CT also has utility in the assessment of osseous structures after subluxation/dislocation, particularly in evaluation of a subtle Bankart’s fracture with an equivocal MRI or intra-articular osseous fragments.21 CT is useful as a preoperative exam to assess fragment size and displacement. MR arthrography is the most sensitive test for evaluation of most of the causes, manifestations, and sequellae of glenohumeral instability.22-24 It allows for precise evaluation of the capsulolabral and ligamentous complex. Labral tears are diagnosed when intra-articular contrast material tracks into or underneath the labrum. Noncontrast MRI is also very sensitive, although use of a high-field scanner (≥0.7 T) is recommended. Labral tears most commonly associated with instability are anteroinferior or posterior (Fig. 14-9). Superior labral tears that track anterior to posterior (SLAP tears) are well seen with MR arthrography but are not usually associated with instability25,26 (Fig. 14-10). Tendon tears that can be associated with instability, including tears of the long head of the biceps tendon or subscapularis, are also well seen by MR arthrography and noncontrast MRI. Multidirectional instability typically shows no abnormality on imaging modalities, although capacious recesses may be observed.
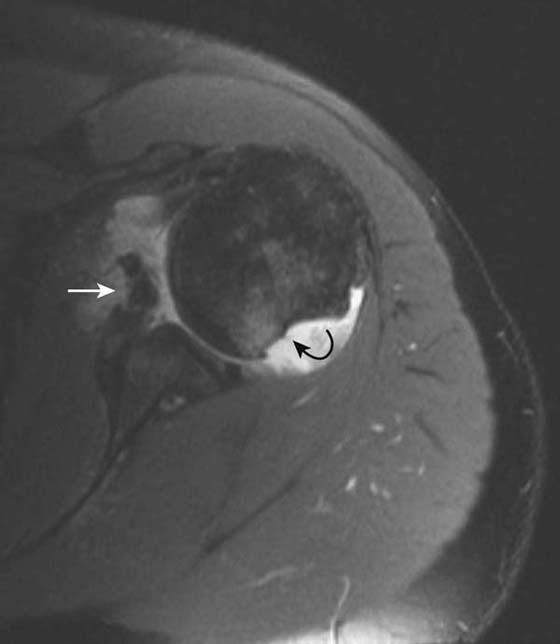
Figure 14-9 Bankart’s and Hill–Sachs lesions. Axial T1 fat-saturated MRI after administration of intra-articular gadolinium (direct MR arthrogram) demonstrates sequelae of anterior shoulder dislocation. The anteroinferior labrum and bony glenoid has been disrupted (white arrow) consistent with a bony Bankart lesion. A bony defect is also seen at the posterior humeral head (curved black arrow) consistent with a Hill–Sachs lesion.

Figure 14-10 Superior labral anterior to posterior (SLAP) lesion. Coronal fat-suppressed T1-weighted image of the shoulder after intra-articular gadolinium injection (direct MR arthrogram) demonstrates abnormal tracking of contrast material into the superior labrum (arrow) consistent with a SLAP tear.
Adhesive Capsulitis
Adhesive capsulitis, or frozen shoulder, has a variety of possible causes. Imaging features are usually nonspecific, but findings suggestive of adhesive capsulitis include a low joint capacity at arthrography, capsular thickening, and rotator cuff interval synovitis on MRI.27
Trauma
Radiography should always be the initial modality utilized in cases of trauma to the shoulder to evaluate for fracture or dislocation. Thereafter CT or MRI may be appropriate to assess for lesions occult on radiographs or for further characterization of fractures. CT with 2D and 3D reformats are excellent for preoperative planning (see Fig. 14-3). The excellent inherent soft tissue contrast afforded by MRI allows for assessment of injury to soft tissue structures such as tendon and muscle (Fig. 14-11).

Figure 14-11 Pectoralis major muscle tear. Axial short tau inversion recovery (STIR) image of the right chest wall and proximal upper extremity acquired on a low field strength open magnet (0.3 T) demonstrates a complete (grade 3) tear of the right pectoralis major muscle with intervening bright hemorrhagic fluid (arrow)
Arthritis
Radiography is the mainstay for initial assessment of shoulder arthritis. MRI may be helpful in equivocal cases, particularly for identifying synovitis in inflammatory arthritides.28
Radiography is routinely employed in the assessment of joint prostheses. Septic arthritis and osteomyelitis of the glenohumeral and acromioclavicular joints are uncommon and may not demonstrate radiographic findings in the early stages. Radiographic findings seen in septic arthritis and osteomyelitis include soft tissue swelling, joint space narrowing, and articular erosions. MRI is a more sensitive test for evaluation of septic arthritis and osteomyelitis demonstrating a joint effusion, subchondral edema, and fatty marrow replacement in the setting of osteomyelitis. Osteomyelitis is also seen on whole-body isotope bone scan, with increased activity being seen on all three phases. In reality, if a septic arthritis is suspected, it should be confirmed by joint aspiration.
Masses
Evaluation of soft tissue masses at the shoulder invariably requires advanced imaging, namely ultrasound or MRI. A variety of benign and malignant soft tissue masses, including lipomas, liposarcomas, desmoids, malignant fibrous histiocytoma (MFH), and synovial sarcoma, may occur at the shoulder. MRI prior to and following administration of IV gadolinium contrast material is recommended by most authors. US may not provide a complete characterization of the lesion if osseous involvement is present but does allow for image-guided sampling. Radiographs are essential in the initial characterization of osseous tumors. MRI frequently aids in narrowing the differential diagnosis, especially with regard to solid versus cystic nature (requiring IV contrast). MRI is also useful for documentation of extent. CT is excellent for evaluation of cortical destruction and pathologic fracture and improves characterization of calcified matrix over radiographs.
The role of whole-body bone scan in the assessment of bone tumors is primarily for the evaluation of multiplicity of osseous lesions.
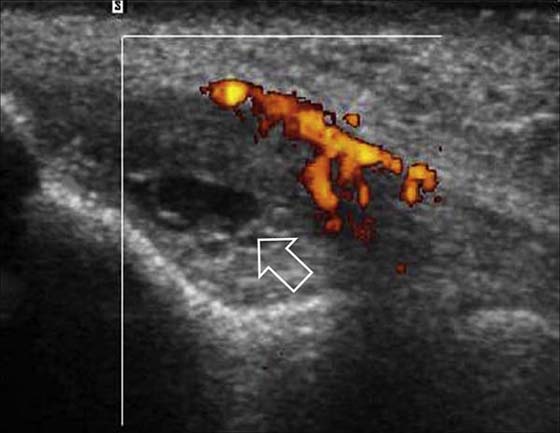
Imaging of Elbow Pathology
Tendon Injury
Lateral epicondylitis, or “tennis elbow,” is a chronic tendinopathy of the common extensor origin and is a frequent cause of lateral elbow pain. On MRI, abnormal high signal is seen at the common extensor origin on fluid-sensitive sequences, sometimes with associated partial tears, which are fluid-bright.29 In more severe cases, associated subtendinous bone marrow edema may be present at the lateral epicondyle, but this is not required for radiologic diagnosis. US is a valuable modality for examining the lateral epicondyle.30,31 Sonographic features include common extensor origin thickening, heterogeneous echogenicity, calcific deposits, partial tears, and hypervascularity on Doppler imaging (Fig. 14-12). US may also be used to guide steroid or anesthetic injections and tendon fenestration.32 Medial epicondylitis has similar MRI and US findings at the common flexor origin. Both of these entities may be associated with injury to the adjacent medial and lateral stabilizing structures.33 Evaluation of the other tendons, including the biceps, triceps, and brachialis, is optimized with MRI. US is also useful for directed examination of tendon pathology at the elbow.
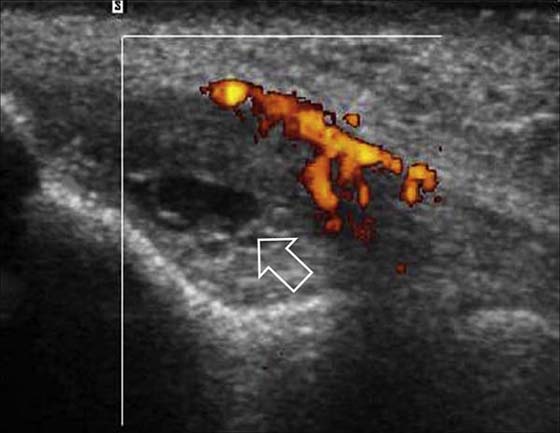
Figure 14-12 Lateral epicondylitis or common extensor tendinosis with partial tear. Ultrasound image demonstrates thickening of the common extensor origin consistent with tendinosis/epicondylitis with an associated hypoechoic (black) defect within the extensor tendon origin consistent with an interstitial partial tear (arrow). Power Doppler imaging demonstrates hypervascularity (orange areas), often seen with lateral epicondylitis/common extensor tendinosis.
Injury to Medial and Lateral Stabilizing Ligaments
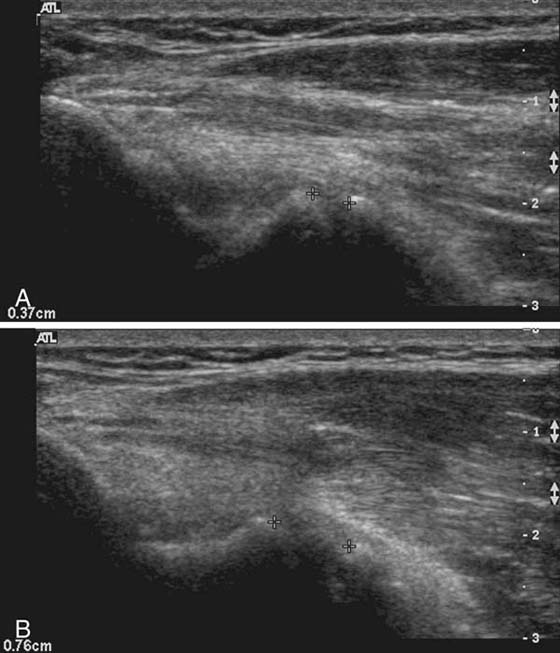
Direct MR arthrography is most useful in detecting suggested injury to the medial and lateral stabilizing ligaments. The medial (ulnar) collateral ligament, for example, is frequently injured in baseball pitchers and can be assessed accurately with MR arthrography34-36 (Fig. 14-13). US is also useful in assessing the elbow ligaments but has an advantage over MRI with its ability to assess ligamentous laxity in real time with dynamic imaging37,38 (Fig. 14-14). For example, during valgus stress for assessment of the medial collateral ligament, a difference in 2 mm between sides is diagnostic of abnormal ligamentous laxity.

Figure 14-13 Ulnar collateral ligament tear. Coronal fat-suppressed T1-weighted image of the elbow after intra-articular gadolinium injection (direct MR arthrogram) demonstrates abnormal tracking of contrast (arrow) between the anterior bundle of the ulnar collateral ligament and the coronoid process of ulna at the sublime tubercle, indicating a distal partial thickness undersurface tear.
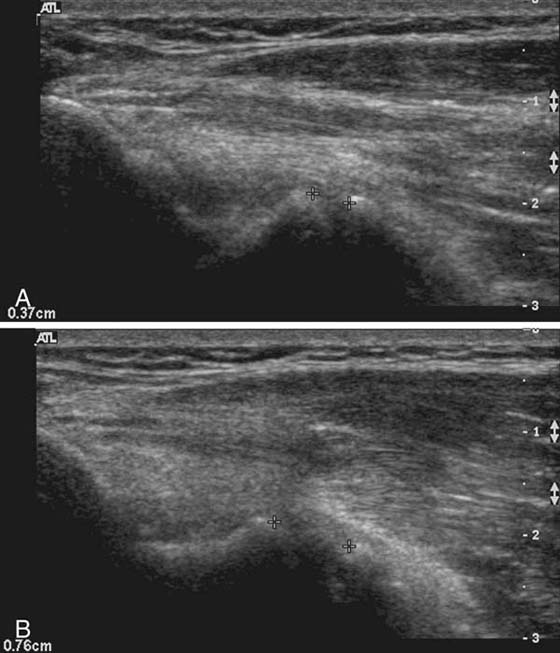
Figure 14-14 Ulnar collateral ligament (UCL) instability. A, Ultrasound at rest. Medial elbow joint demonstrates minimal gapping between the trochlea of humerus and ulna measured by crosshairs. B, When manual valgus stress is applied this gap increases significantly (difference of 3.9 mm) consistent with UCL instability. The difference between rest and stress measurement should be less than 2 mm. Multiple measurements (e.g., 3) should be taken and the average calculated. It is also useful to compare with the asymptomatic elbow.
Trauma
Like the shoulder, radiographs are indicated in the assessment of acute trauma at the elbow to determine the presence of fracture or malalignment. A useful sign on lateral radiographs is the visualization of a posterior fat pad or elevation on the anterior fat pad, indicative of elbow joint effusion39 (Fig. 14-15). In the setting of acute trauma the presence of such an effusion suggests an occult radial head fracture. CT is also useful in the setting of complex acute bony injury, facilitating accurate assessment of fracture fragments and degree of displacement before surgical intervention. MRI is of value in the assessment of suggested occult osseous trauma due to its high sensitivity for detection of bone marrow edema and associated fractures. MRI is also warranted where soft tissue injury is suggested, such as in cases of distal biceps tendon or triceps tendon injury.

Figure 14-15 Elbow effusion. Lateral radiograph of the elbow shows abnormal elevation of the anterior fat pad forming a “sail” shape (arrows). A faint posterior fat pad is seen (arrowhead). Elevation of the anterior fat pad as shown or the mere visualization of a posterior fat pad indicate an elbow joint effusion. Elbow effusion is often associated with occult fracture with otherwise normal radiographs in the setting of trauma.
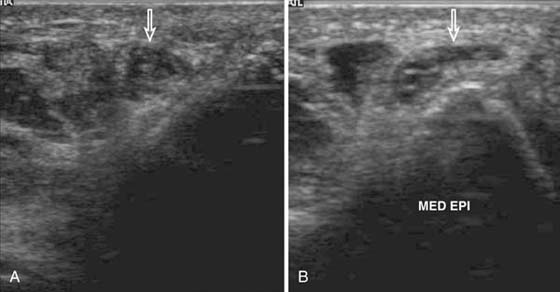
Neuropathy
US is particularly useful in the assessment of possible neuropathy at the elbow.40-42 The ulnar nerve is the most frequently involved. Neuropathy manifests as focal nerve enlargement at or proximal to the site of impingement at the cubital tunnel and is demonstrated by altered echogenicity. US also allows dynamic imaging of ulnar nerve subluxation or dislocation out of the cubital tunnel on elbow flexion43 (Fig. 14-16). The median nerve may also be compressed at the elbow by a number of structures, most commonly the pronator teres muscle. The radial nerve may be injured above the elbow secondary to trauma or more distally at the supinator, compressing its posterior interosseous nerve branch. Similar to the ulnar nerve, US is useful in assessing focal neural dilatation and altered echogenicity.
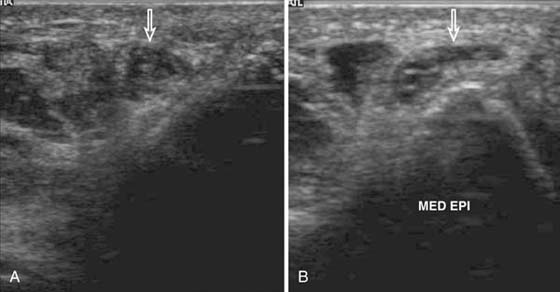
Figure 14-16 Ulnar nerve subluxation. A, Transverse ultrasound image at the cubital tunnel on elbow extension shows ulnar nerve (arrow) in normal position. B, On elbow flexion, the ulnar nerve (arrow) is seen to sublux medially, lying perched on the medial epicondyle.
Although lacking a dynamic component, MRI can identify nerve enlargement and edema and may also identify the specific site of impingement.40 In addition, MRI may demonstrate neurogenic muscle edema (early sign) or muscle fatty atrophy (late sign) in the muscle groups supplied by nerves that are impinged.
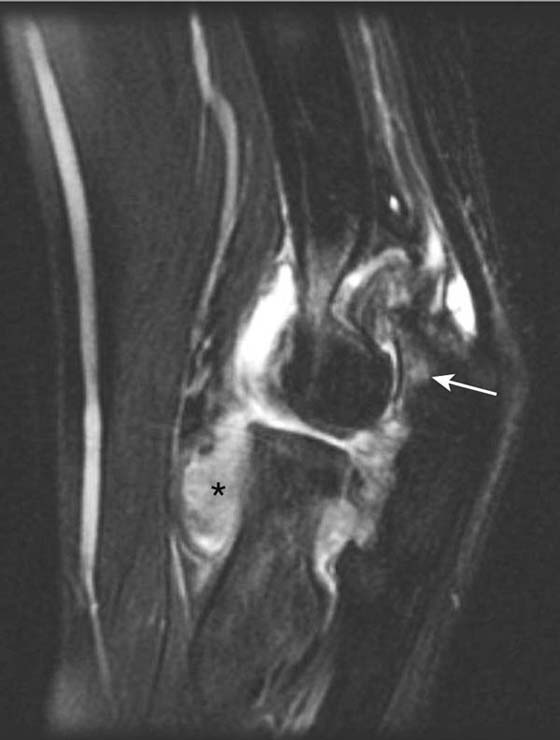
Arthritis
Arthopathies that affect the elbow include rheumatoid arthritis (Fig. 14-17), osteoarthritis, crystal deposition diseases (gout and calcium pyrophosphate deposition disease), synovial osteochondromatosis, and septic arthritis. As with the shoulder, radiographs should be performed first, followed by advanced imaging if warranted. CT or CT arthrography is useful for assessing intra-articular osseous bodies. MRI and MR arthrography are also useful in this instance and are superior for assessing synovitis in inflammatory arthropathies.
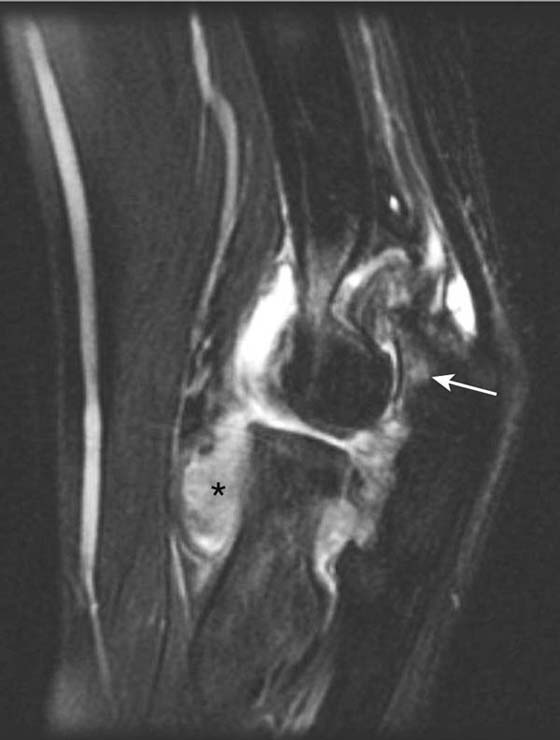
Figure 14-17 Rheumatoid arthritis of the elbow. Sagittal short tau inversion recovery (STIR) sequence of the elbow demonstrates intermediate signal extensive pannus/synovitis (asterisk) with high-signal subchondral edema (arrow) in a patient with rheumatoid arthritis.
Osteochondrosis and Osteochondritis Dissecans
In general, cartilage lesions are best evaluated using MRI or MR arthrography.
Panner’s disease (osteochondrosis of the capitellum in children) is best assessed by MRI. It manifests as focal T2 hyperintensity of the subchondral bone of the capitellum with T1 marrow replacement. Osteochondritis dissecans of the capitellum is common and is best assessed with MR arthrography for determining lesion instability. Unstable lesions are characterized by a rim of fluid surrounding the osteochondral fragment, which may be associated with disruption of overlying cartilage and underlying cyst formation. Stable lesions with intact overlying cartilage may respond to conservative therapy.
Summary
Diagnostic imaging is an invaluable adjunct to clinical examination in the assessment of many shoulder and elbow disorders. Radiography of the shoulder and elbow should be considered in all cases, especially if there is a history of trauma. Radiography provides useful information about bony anatomy and a baseline for comparison with follow-up studies, as well as providing a complementary test to advanced imaging techniques. Techniques such as US, CT, MRI, and bone scans are invaluable in providing state-of-the-art radiologic assessment and as a complement to radiography. Ordering the correct modalities with pertinent clinical details will yield maximum information and facilitate optimum patient management.
REFERENCES
1. Westhoff B, Wild A, Werner A, et al. The value of ultrasound after shoulder arthroplasty. Skeletal Radiol. 2002;31:695–701.
2. Magee T, Williams D, Mani N. Shoulder MR arthrography: which patient group benefits most? AJR Am J Roentgenol. 2004;183:969–974.
3. Lecouvet FE, Simoni P, Koutaissoff S, et al. Multidetector spiral CT arthrography of the shoulder Clinical applications and limits, with MR arthrography and arthroscopic correlations. Eur J Radiol. 2008;68:120–136.
4. Kolla S, Motamedi K. Ultrasound evaluation of the shoulder. Semin Musculoskelet Radiol. 2007;11:117–125.
5. Moosikasuwan JB, Miller TT, Burke BJ. Rotator cuff tears: clinical, radiographic, and US findings. Radiographics. 2005;25:1591–1607.
6. Papatheodorou A, Ellinas P, Takis F, et al. US of the shoulder: rotator cuff and non-rotator cuff disorders. Radiographics. 2006;26:e23.
7. Finlay K, Ferri M, Friedman L. Ultrasound of the elbow. Skeletal Radiol. 2004;33:63–79.
8. Martinoli C, Bianchi S, Giovagnorio F, Pugliese F. Ultrasound of the elbow. Skeletal Radiol. 2001;30:605–614.
9. Tran N, Chow K. Ultrasonography of the elbow. Semin Musculoskelet Radiol. 2007;11:105–116.
10. Nazarian LN. The top 10 reasons musculoskeletal sonography is an important complementary or alternative technique to MRI. AJR Am J Roentgenol. 2008;190:1621–1626.
11. Parker L, Nazarian LN, Carrino JA, et al. Musculoskeletal imaging: Medicare use, costs, and potential for cost substitution. J Am Coll Radiol. 2008;5:182–188.
12. Joines MM, Motamedi K, Seeger LL, DiFiori JP. Musculoskeletal interventional ultrasound. Semin Musculoskelet Radiol. 2007;11:192–198.
13. Schauwecker DS. The scintigraphic diagnosis of osteomyelitis. AJR Am J Roentgenol. 1992;158:9–18.
14. Even-Sapir E. PET/CT in malignant bone disease. Semin Musculoskelet Radiol. 2007;11:312–321.
15. Fritz RC. Magnetic resonance imaging of sports-related injuries to the shoulder: impingement and rotator cuff. Radiol Clin North Am. 2002;40:217–234. vi
16. Kassarjian A, Bencardino JT, Palmer WE. MR imaging of the rotator cuff. Radiol Clin North Am. 2006;44:503–viii.
17. Morag Y, Jacobson JA, Miller B, et al. MR imaging of rotator cuff injury: what the clinician needs to know. Radiographics. 2006;26:1045–1065.
18. Awerbuch MS. The clinical utility of ultrasonography for rotator cuff disease, shoulder impingement syndrome and subacromial bursitis. Med J Aust. 2008;188:50–53.
19. Woertler K. Multimodality imaging of the postoperative shoulder. Eur Radiol. 2007;17:3038–3055.
20. Garcia GM, McCord GC, Kumar R. Hydroxyapatite crystal deposition disease. Semin Musculoskelet Radiol. 2003;7:187–193.
21. Griffith JF, Antonio GE, Tong CW, Ming CK. Anterior shoulder dislocation: quantification of glenoid bone loss with CT. AJR Am J Roentgenol. 2003;180:1423–1430.
22. Beltran J, Rosenberg ZS, Chandnani VP, et al. Glenohumeral instability: evaluation with MR arthrography. Radiographics. 1997;17:657–673.
23. Robinson G, Ho Y, Finlay K, et al. Normal anatomy and common labral lesions at MR arthrography of the shoulder. Clin Radiol. 2006;61:805–821.
24. Van der Woude HJ, Vanhoenacker FM. MR arthrography in glenohumeral instability. JBR-BTR. 2007;90:377–383.
25. Jee WH, McCauley TR, Katz LD, et al. Superior labral anterior posterior (SLAP) lesions of the glenoid labrum: reliability and accuracy of MR arthrography for diagnosis. Radiology. 2001;218:127–132.
26. Waldt S, Burkart A, Lange P, et al. Diagnostic performance of MR arthrography in the assessment of superior labral anteroposterior lesions of the shoulder. AJR Am J Roentgenol. 2004;182:1271–1278.
27. Mengiardi B, Pfirrmann CW, Gerber C, et al. Frozen shoulder: MR arthrographic findings. Radiology. 2004;233:486–492.
28. Weishaupt D, Schweitzer ME. MR imaging of septic arthritis and rheumatoid arthritis of the shoulder. Magn Reson Imaging Clin N Am. 2004;12:111–124. vii
29. Potter HG, Hannafin JA, Morwessel RM, et al. Lateral epicondylitis: correlation of MR imaging, surgical, and histopathologic findings. Radiology. 1995;196:43–46.
30. Connell D, Burke F, Coombes P, et al. Sonographic examination of lateral epicondylitis. AJR Am J Roentgenol. 2001;176:777–782.
31. Levin D, Nazarian LN, Miller TT, et al. Lateral epicondylitis of the elbow: US findings. Radiology. 2005;237:230–234.
32. McShane JM, Nazarian LN, Harwood MI. Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow. J Ultrasound Med. 2006;25:1281–1289.
33. Bredella MA, Tirman PF, Fritz RC, et al. MR imaging findings of lateral ulnar collateral ligament abnormalities in patients with lateral epicondylitis. AJR Am J Roentgenol. 1999;173:1379–1382.
34. Carrino JA, Morrison WB, Zou KH, et al. Noncontrast MR imaging and MR arthrography of the ulnar collateral ligament of the elbow: prospective evaluation of two-dimensional pulse sequences for detection of complete tears. Skeletal Radiol. 2001;30:625–632.
35. Munshi M, Pretterklieber ML, Chung CB, et al. Anterior bundle of ulnar collateral ligament: evaluation of anatomic relationships by using MR imaging, MR arthrography, and gross anatomic and histologic analysis. Radiology. 2004;231:797–803.
36. Schwartz ML, al-Zahrani S, Morwessel RM, Andrews JR. Ulnar collateral ligament injury in the throwing athlete: evaluation with saline-enhanced MR arthrography. Radiology. 1995;197:297–299.
37. De Smet AA, Winter TC, Best TM, Bernhardt DT. Dynamic sonography with valgus stress to assess elbow ulnar collateral ligament injury in baseball pitchers. Skeletal Radiol. 2002;31:671–676.
38. Nazarian LN, McShane JM, Ciccotti MG, et al. Dynamic US of the anterior band of the ulnar collateral ligament of the elbow in asymptomatic major league baseball pitchers. Radiology. 2003;227:149–154.
39. O’Dwyer H, O’Sullivan P, Fitzgerald D, et al. The fat pad sign following elbow trauma in adults: its usefulness and reliability in suspecting occult fracture. J Comput Assist Tomogr. 2004;28:562–565.
40. Andreisek G, Crook DW, Burg D, et al. Peripheral neuropathies of the median, radial, and ulnar nerves: MR imaging features. Radiographics. 2006;26:1267–1287.
41. Martinoli C, Bianchi S, Gandolfo N, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics. 2000;20:S199–S213. Spec No
42. Martinoli C, Serafini G, Bianchi S, et al. Ultrasonography of peripheral nerves. J Peripher Nerv Syst. 1996;1:169–178.
43. Maffulli N. US in the diagnosis of ulnar nerve dislocation. Radiology. 2002;223:877–878.